Abstract
Back ground
Rotational atherectomy (RA) is used for plaque modification in patients with heavily calcified coronary lesions. Rotational atherectomy can induce significant bradycardia or atrioventricular block requiring for temporary pacemaker insertion. In this report, we present a case of trans-coronary pacing via a Rota wire to prevent bradycardia during RA in the proximal right coronary artery (RCA).
Case summary
A 72-year-old woman with a 1 month history of worsening effort angina was admitted to our hospital. Computed tomography coronary angiography disclosed significant coronary stenosis with severe calcification in proximal RCA. Coronary angiography revealed significant coronary stenosis with severe calcification in the proximal RCA. Subsequently, percutaneous coronary artery intervention was performed under the guidance of intravascular ultrasound (IVUS). The pull-back IVUS showed a circumferential calcified lesion in the proximal RCA that was treated using RA, which induced significant bradycardia requiring temporary pacemaker insertion. Immediately, trans-coronary pacing was provided via a Rota wire placed in the far distal RCA; this was used for back-up pacing during RA. Rotational atherectomy was completed by safely modifying the calcified lesion. After successful debulking of the calcified lesion, we dilated with a balloon, and a drug-eluting stent was implanted at the proximal RCA. Final IVUS and angiography showed good stent apposition and expansion. We did not observe any serious intraprocedural complications.
Discussion
Rotational atherectomy is used for plaque modification in patients with heavily calcified coronary lesions. Rotational atherectomy can induce significant bradycardia or atrioventricular block requiring for temporary pacemaker insertion via the transvenous route. This method could be an effective method to prevent bradycardia during RA.
Keywords: Rotational atherectomy, Trans-coronary pacing, Calcified lesion, Percutaneous coronary artery intervention, Case report
Learning points.
Rotational atherectomy can induce significant bradycardia or atrioventricular block requiring temporary pacemaker insertion.
Trans-coronary pacing via Rota wire can be useful for back-up pacing during rotational atherectomy.
Introduction
Rotational atherectomy (RA) is used for plaque modification in heavily calcified coronary artery lesions. Rotational atherectomy can be associated with distal embolization of calcific particles, resulting in clinically significant bradycardia or atrioventricular block requiring temporary pacemaker insertion in lesions involving the right coronary artery (RCA) and heavily calcified lesions. Michael et al.1 reported that heart block or temporary pacing occurred in 53% of RA cases in the RCA. Although transvenous right ventricular (RV) temporary pacing is an efficient and stable procedure, it requires an additional catheter and central venous catheterization, which is unsuitable under haemodynamically unstable conditions as in the current case. However, trans-coronary pacing requires no additional catheter and can be performed easily and rapidly.2 Here, we present a case of trans-coronary pacing via a Rota wire to prevent bradycardia induced by RA in the proximal RCA.
Timeline
| Day 1 13:00 | A 72-year-old woman with worsening effort angina was admitted to our hospital. Computed tomography coronary angiography revealed severe calcified stenosis of the proximal right coronary artery (RCA). |
| Day 2 09:57 | Coronary angiography (CAG) revealed severe calcified stenosis of the proximal RCA. |
| 10:08 | Pull-back intravascular ultrasound (IVUS) showed a circumferential calcified lesion in the proximal RCA. |
| 10:17 | After rotational atherectomy (RA) was performed with a 1.75 mm burr, heart block and bradycardia occurred. Trans-coronary pacing was provided via a Rota wire and used for back-up pacing during RA. |
| 10:48 | Additional RA of Rota burr 2.0 mm was performed, and we safely modified the calcified lesion. The heart block had occurred only during RA, and the patient recovered from the heart block soon after RA. |
| 11:04 | The drug-eluting stent was implanted at the proximal RCA. |
| 11:10 | Final IVUS and CAG showed good stent apposition and expansion. Pacing was not required after procedure. |
| Day 4 | The patient was discharged without any complication. |
| 6 months follow-up | The patients had no clinical symptom or cardiac events. |
Case presentation
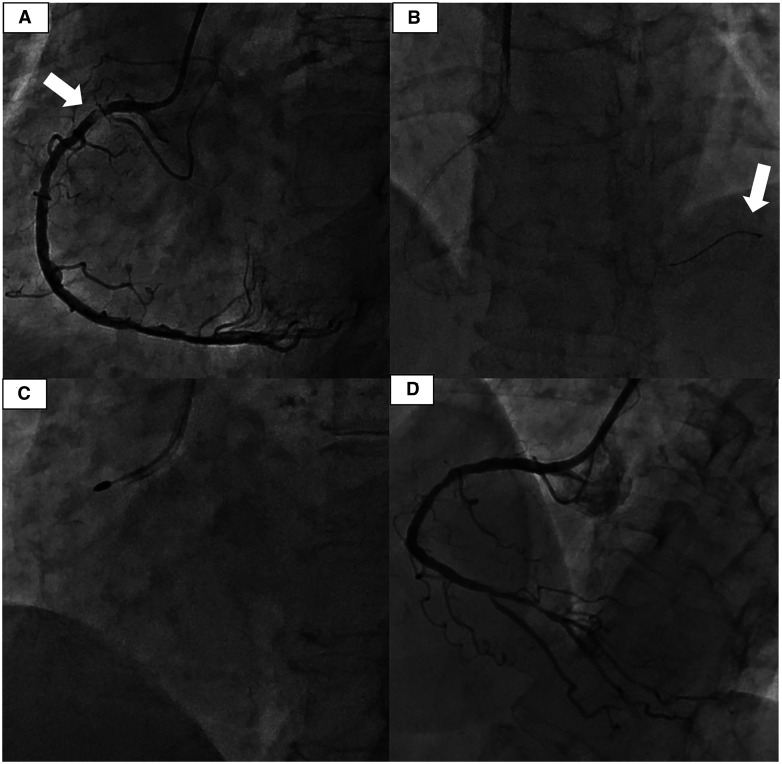
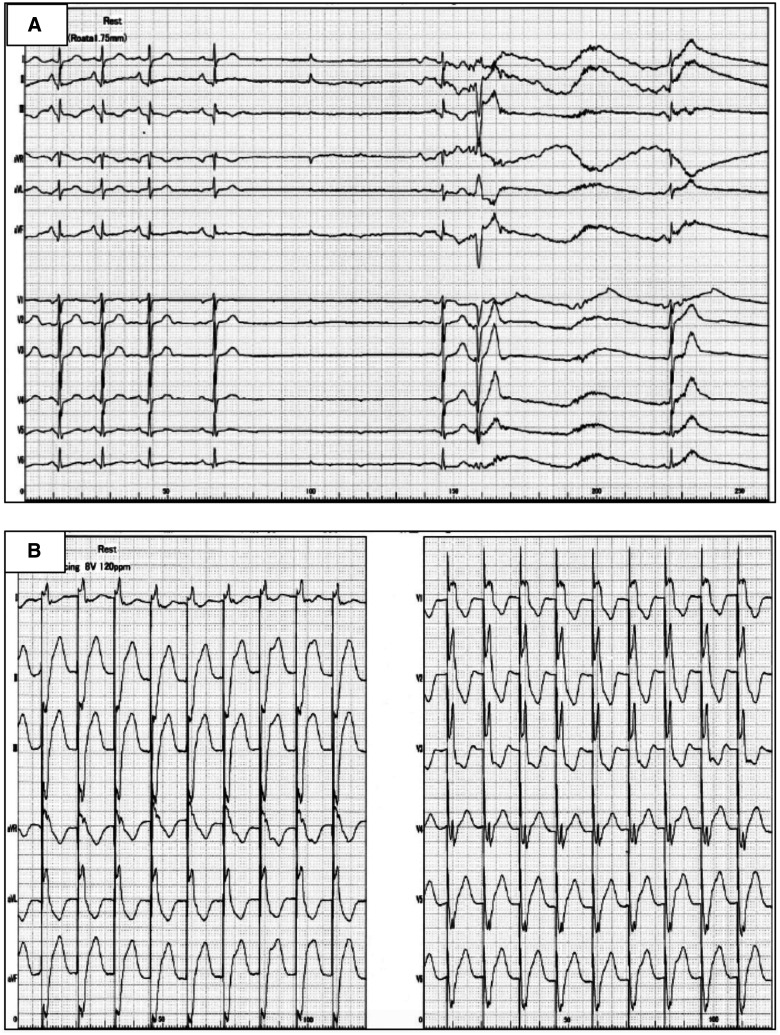
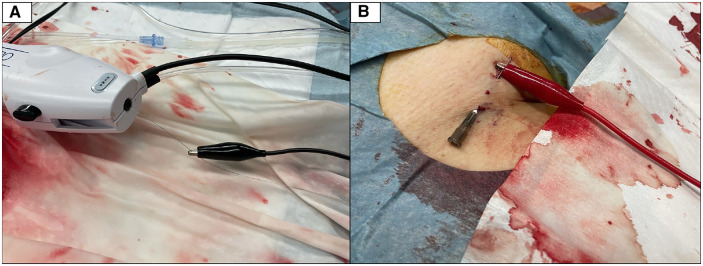
A 72-year-old woman with worsening effort angina CCS Class III was admitted to our hospital. The patient had some risk factors for coronary artery disease, including hypertension and hyperlipidaemia. Her medical conditions had been well controlled with an angiotensin II receptor blocker, and a statin. The physical examination revealed the following: blood pressure, 130/80 mmHg, and heart rate, 80 b.p.m. There was no cardiac murmur and pulmonary rales. Blood tests showed serum creatinine of 0.72 mg/dL, haemoglobin of 13.1 gm/dL, and troponin level to be as low as 50–100 ng/L. Although the electrocardiogram showed no remarkable ST-segment changes, and echocardiography showed normal wall motion with preserved left ventricular systolic function, computed tomography coronary angiography disclosed significant coronary stenosis at proximal RCA. Coronary angiography performed after loading dual antiplatelet therapy with prasugrel and aspirin, revealed severe calcified stenosis of the proximal RCA (Figure 1A, Video 1). We planned to treat the severely calcified RCA using RA. Left radial artery access was gained using a 7 Fr Glide Sheath® (Terumo, Japan), and a 7 Fr Judkins Right 4.0 guide catheter was used to intubate the RCA. A 0.014″ guidewire (SION blue®, Asahi Intecc, Japan) was successfully passed through the stenotic lesion with the support of a microcatheter (Corsair Pro®, Asahi Intecc, Japan). Pull-back intravascular ultrasound (IVUS) (Boston Scientific, USA) showed a circumferential calcified lesion in the proximal RCA. We then switched the Rota wire® floppy (Boston Scientific, USA) to perform RA (Figure 1B). After RA was performed with a 1.75 mm burr at 180 000 rpm, heart block and significant bradycardia occurred (Figure 3A). Immediately trans-coronary pacing was provided via a Rota wire placed far distal to the RCA and used for back-up pacing during RA. The cathode of an external pacemaker was attached to the distal external end of the guide wire using a crocodile clip (Figure 2A). The anode was attached to the needle which was inserted under the skin of the anaesthetized groin (Figure 2B). Pacing was instituted at 60 beats per minute, with the output set at 8 V for back-up pacing during RA (Figure 3B, Video 2). Additional RA of Rota burr 2.0 mm was performed, and we safely modified the calcified lesion (Figure 1C). The heart block had occurred only during RA, and the patient recovered from the heart block soon after RA. After successfully debulking the calcified lesion, we predilated with Wolverine 2.75/15 mm (Boston Scientific, USA) and delivered a drug-eluting stent (DES): Synergy XD 3.0/16 mm (Boston Scientific, USA). The DES was implanted at the proximal RCA under nominal pressure. Finally, we optimized the stent deployment with using a non-compliant balloon: NC Emerge 3.25/12 mm (Boston Scientific, USA). Final IVUS and angiography showed good stent apposition and expansion (Figure 1D, Video 3). Pacing was not required during balloon angioplasty and stent implantation, and permanent pacemaker implantation was not required after the procedure.
Figure 1.
Result of coronary angiography. (A) Initial angiography. Severely calcified lesion of the proximal right coronary artery (white arrow). (B) The tip of the Rota wire is advanced to the far distal end of the coronary artery (white arrow). (C) Rota burr was used in modifying heavily calcified stenosis. (D) Final PCI results.
Figure 3.
Results of electrocardiogram. (A) First atherectomy induced significant bradycardias and heart block. (B) Back-up pacing at 120 beats per minute with an output set at 8 V during rotational atherectomy.
Figure 2.
How to attach the electrodes. (A) The cathode of an external pacemaker is attached to the distal external end of the guide wire using a crocodile clip. (B) The anode is attached to the needle which is inserted under the skin of the anaesthetized groin.
The patient was discharged 2 days after the procedure without any complications. The maintenance dose of prasugrel and aspirin was administered for 6 months, and then prasugrel as a single antiplatelet therapy was continued. At the 6-month follow-up visit, the patients had no clinical symptom or cardiac events. The electrocardiogram showed normal sinus rhythm and echocardiography showed no regional wall motion abnormality.
Discussion
Rotational atherectomy is used for plaque modification in patients with heavily calcified coronary lesions. Rotational atherectomy can be associated with distal embolization of calcific particles resulting in clinically significant bradycardias or atrioventricular block requiring temporary pacemaker insertion in lesions involving the RCA and heavily calcified lesions. Michael et al.1 reported that heart block or temporary pacing occurred in 53% of patients who underwent RA to the RCA.
Although studies are limited and mostly updated in animal models, a few studies have attempted trans-coronary pacing during RA.3 Heinroth et al.2 reported that trans-coronary guidewire pacing has been used as a technique for controlling bradycardia during balloon angioplasty. Some studies indicated the usefulness of rapid trans-coronary pacing during stent positioning.4,5
In this case, we performed trans-coronary pacing using a Rota wire. Trans-coronary pacing worked well and did not require intravenous pacing insertion. The procedural advantages and limitations compared with conventional RV pacing are listed in Table 1. Although transvenous RV pacing is an efficient and stable procedure, it requires an additional catheter and requires central venous catheterization, which is unsuitable under haemodynamically unstable conditions as in the current case. However, trans-coronary pacing requires no additional catheter and can be introduced easily and rapidly. Even if trans-coronary pacing is unstable, it may serve as a backup before inserting intravenous pacing.
Table 1.
Advantages and limitations of trans-coronary pacing compared with conventional right ventricular pacing.
| Advantages | Limitations |
|---|---|
| • Temporary guidewire pacing is easily and quickly performed. | • Some wires coated with non-conductive polymer have high resistance and may not be suitable.6 Rota wire also may lack of sufficient insulation due to no coating. |
| • Avoiding the need for central venous catheterization under haemodynamically unstable conditions. | • The tip of the wire may move during RA, it may lack of adequate sensing. |
| • Required only negligible additional costs. | • Coronary spasm may occur and need intracoronary application of nitroglycerine.4 |
| • This method generates only unipolar pacing. That may frequently provoke twitching diaphragm. |
This technique consists of the following steps: (1) The tip of the Rota wire should be advanced as far as possible to the distal end of the coronary artery; advancing the wire to the intramyocardial branch is also useful for getting back-up. (2) The Rota burr is advanced the platform. The Rota catheter itself acts as an insulator; therefore, it should be better to place the Rota tip in the coronary artery. (3) The cathode of an external pacemaker is attached to the distal external end of the Rota wire using a crocodile clip. (4) The anode is attached to the needle that was inserted under the skin. (5) Institute pacing rate and output for back-up pacing during RA.
Before starting RA, pretesting of the trans-coronary pacing is required. Pacing is started at maximum output (10 V at 2.5 ms impulse duration) and subsequently reduces the output voltage to determine the pacing threshold. The pacing output is set with a safety margin, and the pulse generator is set in demand mode. If pacing is not effective at maximum output, the vessel is considered unsuitable for trans-coronary pacing, and pacing should be inserted intravenously.
This case report was obtained from a single centre. Further investigation is required to implement this technique in routine practice. Nonetheless, we did not observe serious intraprocedural complications. This method could be an effective, simple, and safe method to prevent bradycardia or heart block during RA.
Lead author biography

Dr Hirofumi Kusumoto studied Medicine at Kindai University (Japan). Since 2016, he has been a cardiology resident at Osaka Medical College Hospital. Since 2018, he has worked as a cardiologist in the Higashi Takarazuka Satoh Hospital. He has been undertaking percutaneous coronary intervention and electrophysiology ablations for last 5 years.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Supplementary Material
Acknowledgements
The authors thank the staff in the catheterization laboratory at Higashi Takarazuka Satoh Hospital for their excellent assistance.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report, including images and associated text has been obtained from the patient in line with COPE guidance.
Funding: None declared.
Conflict of interest: None declared.
References
- 1.Mitar MD, Ratner S, Lavi S.. Heart block and tempolary pacing during rotational atherectomy. Can J Cardiol 2015;31:335–340. [DOI] [PubMed] [Google Scholar]
- 2.Heinroth KM, Stabenow I, Moldenhauer I, Unverzagt S, Buerke M, Werdan K. et al. Temporary trans-coronary pacing by coated guidewires: a safe and reliable method during percutaneous coronary intervention. Clin Res Cardiol 2006;95:206–211. [DOI] [PubMed] [Google Scholar]
- 3.Heinroth KM, Unverzagt S, Mahnkopf D, Horenburg C, Melnyk H, Sedding D. et al. Transcoronary pacing in an animal model: second coated guidewire versus cutaneous patch as indifferent electrodes. Med Klin Intensivmed Notfmed 2021;doi: 10.1007/s00063-021-00806-3. [DOI] [PubMed] [Google Scholar]
- 4.Lasa G, Larman M, Gaviria K, Sanmartin JC, Sadaba M, Rumoroso JR.. Coronary stent immobilization during angioplasty by transcoronary ventricular pacing via a guidewire. Rev Esp Cardiol 2009;62:288–292. [DOI] [PubMed] [Google Scholar]
- 5.Mallek K, Dalton RT, Pareek N, Dworakowski R.. Rapid transcoronary pacing to facilitate ostial stent placement. JACC Cardiovasc Interv 2021;14: e111–e112. [DOI] [PubMed] [Google Scholar]
- 6.Mixon TA, Cross DS, Lawrence ME, Gantt DS, Dehmer GJ.. Temporary coronary guidewirepacing during percutaneous coronary intervention. Catheter Cardiovasc Interv 2004;61:494–500. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.