Version Changes
Revised. Amendments from Version 2
Two new sections were added to the discussion:
A paragraph to specify whether or not the participants were diagnosed with COVID-19.
A paragraph to elaborate further on what kind of interventions should be put in place, by governments and health authorities, to promote and protect the mental health of this vulnerable population during and after the pandemic.
Abstract
Background: Mental health problems such as anxiety, depression and their aggravation have been studied extensively in the general population. However, there are few studies on depression in older adults and the few existing results may be contradictory, especially in the context of the COVID-19 pandemic. The aim of this study is to determine the factors associated with depression in older adults in two coastal regions of Peru during the COVID-19 pandemic.
Methods: This study uses an analytical cross-sectional design in a population of older adults, who participated in a non-governmental ambulatory social support program in Callao and Ica, two coastal regions of Peru. We administered an on-site structured questionnaire to record sociodemographic data, the Geriatric Depression Scale by Yesavage to measure depression, and the Barthel Index to assess physical function. In order to determine cognitive impairment as an exclusion criterion, the MEC-30 was used. The association between variables was assessed through contingency tables, using the odds ratio (OR) with its corresponding confidence interval (95% CI) and the X2 test. Finally, a binary logistic regression analysis was performed.
Results: Out of the 244 older adults surveyed, 39% had depressive symptoms, of which 28.3% (n=69) and 10.7% (n=26) were moderately and severely depressive, respectively. The findings significantly associated with the presence of depressive symptoms were being 76 years old or older [p=0.005, OR: 2.33, 95% CI: 1.29-4.20], not participating in weekly recreational activities [p=0.004, OR: 2.28, 95% CI: 1.31-3.99] and the presence of comorbidities [p=0.026, OR: 1.88, 95% CI: 1.07-3.29].
Conclusion: There are few studies exploring depression in older adults during the COVID-19 pandemic; this research shows the importance of mental health care in this population and, particularly, of those who are 76 or older because they suffer from comorbid conditions and have interrupted recreational activities.
Keywords: COVID-19; mental health; depression; associated factors; older adult; Peru
Introduction
Prior to the COVID-19 pandemic, the world was concerned with the aging population, a situation that was by no means alien to developing countries. 1 , 2 In the same context, the relationship between older age and health status is well known; the former is the expression of a process that occurs throughout life and involves changes in biopsychosocial and cognitive aspects; the latter is a biopsychosocial construct based on a variety of circumstances that have to do with physical and mental adaptation and the environment. 3 , 4
Depression is a common condition in older adults. According to the World Health Organization, it is the second cause of global morbidity, after cardiovascular diseases, and has a multifactorial origin. 5 Depression has a diverse clinical manifestation that is difficult to identify, which causes a decrease in the quality of life and an increase in suffering, often leading to fatal outcomes. 6 – 8
A study conducted in Peru determined depressive disorders in older adults in rural communities of high Andean regions during the period 2013-2017. This identified 40.2% of people suffering some kind of depression according to the Yesavage questionnaire. 9 However, a subsequent study showed an estimated prevalence of depression in older adults of 14% and identified risk factors such as female gender, being 75 or older, living without a partner, low income, rurality and having at least one disability. 10
Peru has a population made up of 29,381,884 inhabitants, where older adults represent 6.2%. Callao, the country's first seaport, is one of the smallest and most densely populated regions, as well as one of the most industrialized after Lima, the capital city. On the other hand, Ica is one of the most productive regions, with less total poverty and extreme poverty than the national average. Both regions are home to 6.3% of the country's elderly. 11
The COVID-19 pandemic, which started in China at the end of December 2019, also affected Peru. By December 20, 2020, there were 998,475 confirmed cases and 37,173 deaths; by January 10, 2021, there were already 1,037,350 cases and 38,335 deaths, placing Peru in the 17th place out of 20 countries that reported the highest number of cases in the world. 12
Mental health can be affected as a consequence of events related to natural disasters, armed conflicts, threats to individual or collective health, among others. Older adults are a high-risk group and highly vulnerable to these situations. 13 As a consequence, the quality of life of older adults in a pandemic scenario is a cause for concern, characterized by high levels of uncertainty which, together with voluntary or mandatory confinement, physical and social isolation, can cause emotional imbalance. However, these are not the only factors that can influence this situation: comorbidities, degree of dependency, exposure to family abuse, loneliness, low educational level, lack of income or insufficient income can contribute to the deterioration of mental health, causing pathologies that are a challenge for public health. 14 – 18
The aim of this study was to determine the factors associated with depression in older adults, under COVID-19 pandemic conditions. It is hoped to characterise the factors that are associated with depression in this vulnerable population in order to generate scientific evidence that will allow the design of more specific interventions that contribute to the improvement of care and quality of life in older adults.
Methods
Study design and population
This is an analytical cross-sectional study. The population consisted of 263 older adults who received ambulatory care through the Community Promotion Development Liberation (COPRODELI) social program. This is a nonprofit association of Spanish origin that helps high-risk populations in marginal urban areas of two regions of Peru, Ica and Callao.
For the present study, the entire population of older adults receiving outpatient support through the COPRODELI social programme was considered. Since the total universe of patients (n = 263) is not very large, all patients were invited in order to have an adequate number of participants so as not to affect the statistical power in the logistic regression analyses.
A non-probabilistic convenience sample of older adults with the following inclusion criteria was included: (i) aged 60 years or older living in the community and not in asylums or other similar institutions (ii) enrolled in the COPRODELI older adult social program where they participate voluntarily, (iii) with no previous psychiatric diagnosis or with neurological diseases that would prevent them from participating in this study, (iv) receiving any type of psychiatric/neurological treatment, (v) not presenting with cognitive impairment (score greater than 23 points) according to the Mini-Mental Status Examination ( Mini-Examen Cognoscitivo, MEC-30) 19 and (vi) voluntarily signing the informed consent.
Data collection
Data were collected during December 20, 2020 to January 10, 2021. This period was included in the second wave of the COVID-19 pandemic in Peru.
The instruments used were not modified and the instructions of the authors who designed the instrument were followed. The printed questionnaires were applied by the research team on site at the facilities of the COPRODELI association.
Biosecurity measures to avoid COVID-19 transmission were respected at all times during data collection. The research assistants were trained on the correct administration of the instruments and related ethical issues. Data collection was supervised by the authorities of the COPRODELI association and by the head researcher . A copy of the questionnaire can be found in the Extended Data.
Variables and instruments
Data were collected using a structured questionnaire to record sociodemographic data such as gender, age, educational level, area of residence, family/social support, lifestyles and impact of the COVID-19 pandemic. Thus, we used the Geriatric Depression Scale, created by Yesavage20, to assess depressive symptoms; the Barthel Index17 to assess physical function; and the MEC-3021 to evaluate cognitive impairment.
The Yesavage Geriatric Scale and the Barthel Index showed a reliability coefficient of 0.653 and 0.630, respectively, measured through the KR-20 test.
Statistical analysis
Two data entries were entered in Excel in parallel and independently and were analyzed in IBM SPSS version 22, using the Universidad Privada San Juan Bautista’s license, Lima, Peru. All questionnaires were coded, and data processing was supervised by the principal investigator . Data analysis was performed in four phases. The first phase included the descriptive analysis of the variables, using frequencies for the categorical variables. Analysis of the total population and by region were considered for subsequent analyses. In the second phase, a quantitative analysis of the scores obtained by the participants was performed. The scores showed a non-parametric distribution (Kolmogorov- Smirnov test: p < 0.001 in all cases) with the median value and the interquartile range (IQR). The Mann-Whitney U test was used to compare the scores between the populations of the regions of Ica and Callao. The third phase considered a bivariate analysis, where the association between variables was evaluated by means of contingency tables, using the odds ratio (OR) with its corresponding confidence interval (95% CI) and the X2 test. Finally, in the third phase, a binary logistic regression analysis was performed to determine the factors associated with depressive symptoms in the older adult population. Statistically significant was considered when the p value lower than 0.05.
Ethical considerations
Ethical standards were respected throughout the research process. The Institutional Research Ethics Committee of San Juan Bautista University approved the study protocol and informed consent procedures with file Number 185-2020-CIEI-UPSJB. The questionnaires were administered on site and written informed consents were obtained. We considered that participants should be older adults with orientation to time, space and person, without either cognitive impairment, a limiting neurological or psychiatric diagnosis/treatment who do not have hearing impairment. In addition, biosafety prevention and control protocols were strictly followed to avoid the spread and infection of COVID-19 by respondents and survey personnel (use of double masks, face shields and a distance of 1.5 meters), in accordance with national legal standards and international technical documentation in force.
Before completing the questionnaires, participants were informed about the purpose of the study and the voluntary nature of their participation. The surveys were anonymous, and the data were treated with strict confidentiality. Older adults who presented with depressive symptoms were reported to the COPRODELI association so that they could be considered in the management of their social care.
Results
Characteristics of the participants
A total of 259 older adults enrolled in the COPRODELI Social Program were recruited. According to the selection criteria, a total of 15 participants were excluded: older adults with cognitive impairment (score ≤ 23, MEC-30). A total of 244 participants were considered ( Figure 1).
Figure 1. Recruitment and selection process of older adult participants enrolled in the COPRODELI Social Program during the COVID-19 pandemic, Peru.
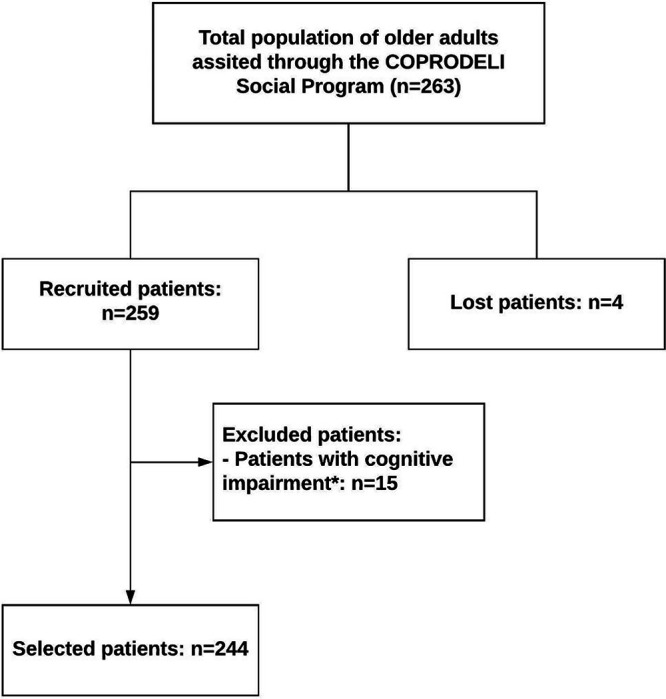
*Patient with cognitive impairment: score ≤ 23 on the Mini-Mental Status Examination -30.
The mean age of the older adults was 73 (± 6.0) years old (range: 60-95). Of the total, 61.9% (n = 151) identified themselves as female, 36.5% (n = 89) were married, 77.9% (n = 190) completed school education, 53.1% (n = 130) were from urban areas and 60.7% (n = 148) resided in Callao. On the other hand, 28.3% (n = 69) and 10.7% (n = 26) of the participants presented with moderate and severe depressive symptoms, respectively. The other characteristics were described in Table 1.
Table 1. Characteristics of older adults in the COPRODELI Social Program during the COVID-19 Pandemic, Peru.
| Characteristics | n | % |
|---|---|---|
| Sociodemographic factors | ||
| Gender | ||
| Man | 93 | 38.1 |
| Woman | 151 | 61.9 |
| Age | ||
| 60-75 | 176 | 72.1 |
| 76 or older | 68 | 27.9 |
| Civil status | ||
| Married | 89 | 36.5 |
| Widow | 54 | 22.1 |
| Single | 88 | 36.1 |
| Divorced | 13 | 5.3 |
| Residence area | ||
| Urban | 130 | 53.1 |
| Rural | 114 | 46.9 |
| Level of education | ||
| Incomplete schooling | 54 | 22.1 |
| Complete schooling | 190 | 77.9 |
| Region | ||
| Ica | 96 | 39.3 |
| Callao | 148 | 60.7 |
| Family/social support | ||
| Who do you live with? | ||
| With family | 147 | 60.2 |
| Alone | 97 | 39.8 |
| Social programs support | ||
| Only COPRODELI | 189 | 77.5 |
| More than one social program | 55 | 22.5 |
| Lifestyle | ||
| Weekly recreational activities | ||
| No | 108 | 44.3 |
| Yes | 136 | 55.7 |
| Presence of comorbidity | ||
| No | 100 | 41.0 |
| Yes | 144 | 59.0 |
| Hypertension | 50 | 20.5 |
| Diabetes | 18 | 7.4 |
| Arthrosis | 14 | 5.7 |
| Others | 109 | 44.7 |
| Impact of the COVID-19 pandemic | ||
| Death of a close relative due to COVID-19 | ||
| No | 186 | 76.2 |
| Yes | 58 | 23.8 |
| COVID-19 test | ||
| Negative/Without a diagnosis | 221 | 90.6 |
| Positive | 23 | 9.4 |
| Physical function according to the Barthel index | ||
| Independency | 169 | 69.3 |
| Low dependency | 35 | 14.3 |
| Moderate dependency | 36 | 14.8 |
| Severe dependency | 4 | 1.6 |
| Depressive symptoms according to the Yesavage Scale | ||
| Normal | 149 | 61.1 |
| Moderate | 69 | 28.3 |
| Severe | 26 | 10.6 |
Scores for depressive symptoms
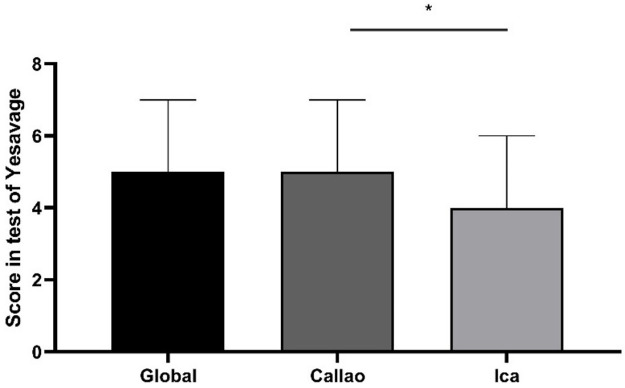
The score obtained from the total number of participants had a median of 5 [IQR: 3-7] on the Yesavage Scale. We found 0 as a minimum value and the maximum value was 14 points. In addition, in Ica, the participants obtained a median score of 4 [IQR: 2-6] and in Callao, 5 [IQR: 3-7]. A statistical difference (p = 0.028) was found between the obtained scores among participants from the region of Ica compared to those from Callao ( Figure 2).
Figure 2. Scores obtained by older adult participants on the Yesavage Scale during the COVID-19 Pandemic in two regions of Peru.
Error bars represent the median and interquartile range, respectively. *p = 0.028 in the Mann-Whitney test.
Bivariate analysis
An exploratory analysis between all the co-variables and the presence of depressive symptoms in all the older adult participants and by region (Callao and Ica) was performed. It was demonstrated that there was a significative association between the population older than 75 and the presence of depressive symptoms with respect to the total population (p = 0.005, OR: 2.23, 95% CI: 1.26-3.94). Similarly, being older than 75 was associated significantly with being part of the population of the region of Callao (p = 0.01, OR: 2.61, 95% CI: 1.24-5.48). When the two regions were analyzed in the total population, it was found that belonging to Callao was associated with the presence of depressive symptoms (p = 0.047, OR: 1.73; 95% CI: 1.01-2.95). Interestingly, it was also found that participating in more than one social program was a protective factor solely for the inhabitants of the Callao region (p = 0.005; OR: 0.24, 95% CI: 0.08-0.69).
On the other hand, not engaging in weekly recreational activities and presenting with comorbidities were also factors associated with depressive symptoms for the total population (p = 0.003, OR: 2.20, 95% CI: 1. 29-3.77 and p = 0.017, OR: 1.92, 95% CI: 1.12-3.29, respectively) and for the inhabitants of the region of Ica (p = 0.006; OR: 3.45; 95% CI: 1.40-8.51 and p = 0.006, OR: 3.45, 95% CI:1.40-8.51, respectively).
Finally, physical function according to the Barthel index was also statistically associated with depression in older adults for the total population and for the region of Callao (p = 0.026 and p = 0.015, respectively), but only moderate-severe dependency had a significant risk in both populations (total: OR: 2.59, 95% CI: 1.28-5.23 and Callao: OR: 2.81; 95% CI: 2.81-6.54). In the low dependency category, no significant risk for developing depressive symptoms was found for any group (p > 0.05) ( Table 2).
Table 2. Bivariate analysis of depression in older adults enrolled in the COPRODELI Social Program during the COVID-19 pandemic, Peru.
| Characteristic | Presence of depressive symptoms *
(n = 95) |
Absence of depressive symptoms *
(149) |
Total (n = 244) | Ica (n = 96) | Callao (n = 148) | |||
|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | p-value | OR [95% IC] | p-value | OR [95% IC] | p-valor | OR [95% IC] | |
| Sociodemographic factors | ||||||||
| Gender | ||||||||
| Man | 37 (39.8) | 56 (60.2) | 0.831 | 0.94 [0.55-1.60] | 0.597 | 0.791 [0.33-1.88] | 0.955 | 0.98 [0.49-1.93] |
| Woman | 58 (38.4) | 93 (61.6) | ||||||
| Age | ||||||||
| 60-75 | 59 (33.5) | 114 (66.5) | 0.005 | 2.23 [1.26-3.94] | 0.209 | 1.80 [0.71-4.59] | 0.01 | 2.61 [1.24-5.48] |
| 76 | 36 (52.9) | 32 (47.1) | ||||||
| Civil status | ||||||||
| Married | 36 (40.4) | 53 (59.6) | 0.71 | 0.90 [0.53-1.54] | 0.698 | 0.84 [0.35-2.01] | 0.629 | 0.84 [0.42-1.68] |
| Single/widow/divorced | 59 (38.1) | 96 (61.9) | ||||||
| Residence area | ||||||||
| Urban | 48 (36.9) | 82 (63,1) | 0.49 | 1.19 (0.71-2.00) | 0.34 | 1.53 [0.63-3.71] | 0.58 | 1.26 [0.62-2.33] |
| Rural | 47 (41.2) | 67 (58.8) | ||||||
| Level of education | ||||||||
| Incomplete schooling | 15 (27.8) | 39 (72.2) | 0.06 | 1.86 [0.96-3.60] | 0.105 | 2.88 [0.77-10,77] | 0.189 | 1.69 [0.76-3.72] |
| Complete schooling | 80 (42.1) | 110 (57.9) | ||||||
| Region | ||||||||
| Ica | 30 (31.3) | 66 (68.8) | 0.047 | 1.73 [1.01-2.95] | NA | NA | NA | NA |
| Callao | 65 (43.9) | 83 (56.1) | ||||||
| Family/social support | ||||||||
| Who do you live with? | ||||||||
| With my family | 61 (41.5) | 86 (58.5) | 0.312 | 0.761 [0.44-1.29] | 0.153 | 0.51 [0.20-1.28] | 0.873 | 0.94 [0.48-1.84] |
| Others | 34 (35.1) | 6 (64.9) | ||||||
| Social programs support | ||||||||
| Only COPRODELI | 79 (41.8) | 110 (58.2) | 0.08 | 0.57 [0.29-1.09] | 0.353 | 1.54 [0.61-3.87] | 0.005 | 0.24 [0.08-0.69] |
| More than one social program | 16 (29.1) | 39 (70.9) | ||||||
| Lifestyle | ||||||||
| Weekly recreational activities | ||||||||
| Yes | 31 (28.7) | 77 (71.3) | 0.003 | 2.20 [1.29-3.77] | 0.028 | 2.71 [1.01-6.69] | 0.071 | 1.85 [0.94-3.64] |
| No | 64 (47.1) | 72 (52.9) | ||||||
| Presence of comorbidity | ||||||||
| No | 30 (30.0) | 70 (70.0) | 0.017 | 1.92 [1.12-3.29] | 0.006 | 3.45 [1.40-8.51] | 0.783 | 1.10 [0.54-2.24] |
| Yes | 65 (45.1) | 79 (54.9) | ||||||
| Impact of the COVID-19 pandemic | ||||||||
| Death of a family member due to COVID-19 | ||||||||
| No | 73 (60.8) | 113 (39.2) | 0.85 | 0.94 [0.51-1.73] | 0.892 | 0.92 [0.32-2.71] | 0.794 | 0.90 [0.43-1.98] |
| Yes | 22 (37.9) | 36 (62.1) | ||||||
| COVID-19 test | ||||||||
| Negative/without a diagnosis | 84 (38.0) | 137 (62.0) | 0.35 | 1.49 [0.63-3.54] | 0.15 | 3.55 [0.56-22.49] | 0.962 | 1.02 [0.38-2.76] |
| Positive | 11 (47.8) | 12 (52.2) | ||||||
| Physical function according to the Barthel index | ||||||||
| Independency | 58 (34.3) | 111 (65.7) | 0.026 | Ref. | 0.729 | Ref | 0.015 | Ref |
| Low dependency | 14 (40.0) | 21 (60.0) | 1.26 [0.60-2.69] | 1.349 [0.40-4.50] | 1.21 [0.46-3.16] | |||
| Moderate-severe dependency | 23 (57.5) | 17 (42.5) | 2.59 [1.28-5.23] | 1.61 [0.41-6.33] | 2.81 [1.19-6.54] | |||
Percentage values are shown according to the values of the variables horizontally. NA: Not applicable; CI: Confidence interval; Ref: Reference. *Distributions calculated over the total number of participants.
Logistic regression analysis
For multivariate analysis, the model was constructed with the variables that were significantly associated with the presence of depressive symptoms in the bivariate analysis for the total population. Being older than 75 (p = 0.005, OR: 2.33, 95% CI: 1.29-4.20), not participating in weekly recreational activities (p = 0.004, OR: 2.28, 95% CI: 1.31-3.99) and the presence of comorbidities (p = 0.026, OR: 1.88, 95% CI: 1.07-3.29) were factors associated with the presence of depressive symptoms in our studied sample ( Table 3). On the other hand, physical function according to the Barthel index and belonging to any region did not have significant association with the presence of depressive symptoms (p > 0.05).
Table 3. Logistic regression analysis of depression in older adults enrolled in the Social Program-COPRODELI during the COVID-19 Pandemic, Peru.
| Characteristic | Total population | |
|---|---|---|
| p-value | Adj a OR (95% IC) | |
| Age | ||
| 60-75 | 0.005 | Ref. |
| 76 or older | 2.33 [1.29-4.20] | |
| Region | ||
| Ica | NS | Ref. |
| Callao | NS | |
| Social program support | ||
| Only COPRODELI | - | - |
| More than one social program | - | - |
| Weekly recreational activities | ||
| Yes | 0.004 | Ref. |
| No | 2.28 [1.31-3.99] | |
| Presence of comorbidity | ||
| No | 0.026 | Ref. |
| Yes | 1.88 [1.07-3.29] | |
| Physical function according to the Barthel index | ||
| Independency | Ref. | |
| Low dependency | NS | NS |
| Moderate-severe independency | NS | NS |
Adjusted by age, region, weekly recreational activities, presence of comorbid conditions and physical function according to the Barthel index.
Discussion
During the second wave of the COVID-19 pandemic, ten months after the identification of the first case in Peru on March 05, 2020, depression was investigated in a sample of older adults participating in a non-governmental ambulatory support program. The findings significantly associated to the presence of depressive symptoms were being 76 or older, not participating in weekly recreational activities and the presence of comorbid conditions. The results are generalizable to older population that comes from urban-marginal areas at high social risk, and we need to be precautious when extending the results to the general population in this age group.
Regarding the COVID-19 pandemic, there are innumerable studies in the general population on mental health problems such as anxiety, depression and its aggravation, 22 but there are few studies focused on depression in older adults and the few existing results may be contradictory. 23 In addition, this research was one of the few studies where the instrument was administered on site. Moreover, depression in older adults is, because of its nature, the result of the complex multidirectional interaction of a series of biological, psychological and social variables, expressed through clinical-epidemiological, cultural, economic and geographic aspects.
Through this study, we found that 9.4% (n = 23) participants reported having a positive COVID-19 diagnosis. In Pearson's Chi-squared test analysis, no statistical association was found between the development of depression and COVID-19 diagnosis (p > 0.05). It is possible that some patients may have had COVID-19, been asymptomatic and not had the appropriate diagnosis for COVID-19; however, in the proposed design for this study, it would not have been possible to identify these participants.
The participants from the region of Callao showed higher levels of depression than those from the region of Ica. Probably, this can be explained due to the difference in the economic income of both populations. There exist studies that showed that socioeconomic level and residence area are protective factors for health, especially when associated with educational level and family income. 24 , 25 In Peru, Saenz et al. 9 and Martina et al. 10 found similar results about the association between depression in older adults and economic income in periods prior to the pandemic, which would permit us to understand the differences we found in our study. It is important to mention the lack of research regarding economic income and depression in older adults in the context of COVID-19 pandemic, which implies a challenge for future research.
The pandemic represents a serious public health issue, especially in older adults due to the association between comorbidities and high mortality, 26 in addition to the increased risk of depression 27 that affects them disproportionately due to the scarce social contact outside the home and with family or close friends. Some of them depend on the support of voluntary services or social assistance, but it can affect even more those who are already alone, isolated or reclusive. 28 , 29 An additional aspect related to the COVID-19 pandemic has to do with the health care approach implemented in terms of confinement, physical and social distancing, together with the loss of family and friends, including the alarming news broadcast by the media that increase the risk of mental health problems, especially in this population group. 13
The analysis by age group in this study shows significant differences in the group aged 76 and older, similar to what was found in the pre-pandemic period in Peru. 9 These findings are important to highlight because depressive disorders are more frequent in young adults, 5 a situation that continues in the context of the COVID-19 pandemic. 30 Age is an important sociodemographic variable in mental health, with the group of young adults showing higher levels of anxiety and depression compared to older adults. This is because they are less likely to have lived stressful experiences and to be unaccustomed to lower levels of social interaction, hence their low resilience. 31 In contrast, a study in China and India found that mental health problems are more frequent among older adults, especially the elderly, because they are more fragile, vulnerable and affected by multimorbidity. 32 It is within this last context that the explanation of what may be happening with the study population in this research is inserted.
Stanton 33 stated that during the pandemic, as a consequence of physical and social distancing, older adults dramatically decreased their recreational and daily activities, which increased their psychological distress. This situation makes it necessary to implement strategies to promote physical activity. In this regard, the findings of this research confirm the above. It should be emphasized that participation in recreational activities or physical activity has a protective effect on depression. This favors better cognitive productivity while, at the same time, allows the alleviation of possible social isolation when interactive activities are carried out, increasing the perception of quality of life in older adults. In contrast, there is evidence that retirement significantly reduces the risk of suffering from health problems, which is not associated with a higher level of depression. The explanation is that it could be due to the decrease in work stress.
Linked to the above, the findings are consistent with other studies that report more signs of depression in people with comorbidities. 17, 29, 35, 36 Arterial hypertension is the most important risk factor for developing cerebrovascular disease in the frontal lobe or putamen. However, it is not the only cause as there are other comorbidities such as heart disease, dyslipidemia, diabetes mellitus and insulin resistance. Older adults are at greater risk for developing these chronic diseases and all of them can contribute to the presence of depression.
Depression is the third leading cause of disability in the world. Despite the burden of these disorders, their correlation with other medical conditions such as chronic diseases tends to be underestimated. Depression is a current public health problem in the world and a challenge for decision makers.
It should be added that we need to pay special attention to older adults with comorbidities. They may cause the decrease in their functional suitability to participate in recreational activities as these conditions may limit their physical capacity for exercise.
It is important to highlight that the descriptive data collected in this study, in comparison with those conducted during the pandemic in other countries, indicate that 38% of older adults reported moderate to severe depression, which is higher than the 16.8% reported in the general population in China 40 and 19.1% that reported prevalence of moderate to severe depression in Australia. 33 Another study conducted in China in the general population showed that 14.6% had depression, which was lower than what was reported in studies of other health emergencies. These differences can be explained due to the rapid and energetic government response to guarantee safe care. Other explanations are based on the level of knowledge of COVID-19 of citizens due to the rapid dissemination of information that reduced public panic and the implementation of a system of psychological assistance. 41 Something similar was found in an investigation in Spain, which identified less emotional distress in the elderly with no differences between men and women. 23
Although in the USA a nationally representative study showed that depression had more than a threefold increase in the general population and double increase in the population aged 60 years and older during the COVID-19 pandemic. However, these results were less than what is reported in this study. 14
In comparison with research on depression in older adults in Peru, in the pre-pandemic period, the study by Martina et al., 10 closer to this study, showed that depression was lower by 24 percentage points, unlike the study by Saenz et al., 9 conducted exclusively with a rural high Andean population, where the results are similar to those presented here, although it is noteworthy that slightly more than 50% of the participants in our study came from urban areas. Both studies showed rural origin as a risk factor for depression in older adults. The results of this research allow us to hypothesize that rurality alone does not explain these differences, since they could be justified by the economic conditions of poverty and extreme poverty in which these populations live and which may eventually be aggravated by traumatic conditions, such as what happened during the COVID-19 pandemic.
Contrary to the results of research indicating that loneliness is a risk factor for depression, 23 , 42 in this study, 60.2% of the older adults lived with their families and 62.3% maintained frequent telephone communication with their families. The explanation for this difference in the high presence of depression is the known fact that living together and greater socialization during the pandemic increases the risk of contagion and therefore, older adults in these cases have greater psychological pressure: feeling afraid of contracting the disease and dying, as well as the possibility that other close relatives may be affected by COVID-19. 30
Although the instrument was applied ten months after the start of the pandemic, during the second wave, when uncertainty is expected to be lower due to the time elapsed, the levels of depression were higher than expected compared to other studies, which may be explained by the excess of sensationalist news and rumors or misinformation about the pandemic. 43
Research in the general population has found that anxiety disorders and depression were more frequent in women in all age groups. During the COVID-19 pandemic, these similarities continued, and they are even being identified as the strongest predictor of post-traumatic stress symptoms after pandemics. 29 , 32 , 44 This is in agreement with our findings, where 61.9% of the studied sample were women. This situation allows us to propose as a new hypothesis: given that women are more common in all age groups and that the feeling of loss of a family member is more accentuated among them, these may lead to higher levels of depression.
The results of this study should be analyzed in light of some limitations; certain results are based on descriptive analysis; therefore, causality cannot be inferred. Moreover, the study sample was obtained from a population receiving ambulatory social support and may not be representative of the general population; additionally, the study could be exposed to sampling bias. Our study has considered variables that explain the multifactor nature of depression in older adults. However, we did not include quality of life, quality of sleep and level of physical exercise that could lead to the onset of depressive symptoms, which are particularly relevant issues to explore in future research.
This research could serve as a basis for future studies to analyze the behavior of older adults under pandemic conditions and to determine how the measures implemented to ensure their well-being, in the face of COVID-19, cannot lead to mental health problems such as depression.
The demographic and epidemiological transition in the world will lead to an increase in life expectancy at birth and an increase in chronic non-communicable diseases. These changes will accentuate the existence of a greater number of older adults in the coming years, and a high proportion of them, with depression. In this perspective, it is necessary to reorient public health strategies focused on older adults in order to respond to this problem. There is a clear need to strengthen mental health services and resources at the first level of care through an integral action.
Definitely, depression in older adults is a challenge for public health and health systems; hence, there is a need for governments and health authorities to improve care in this serious risk and high vulnerability population during and after traumatic situations such as the COVID 19 pandemic. Consequently, prevention and promotion strategies are proposed, based on the evidence generated by this study. We can emphasize those interventions that promote the implementation of physical and recreational activity to avoid the development of chronic conditions such as depression and reduce their impact on health and quality of life. It is also advisable to include interventions of digital health and self-care literacy that favor cognitive and physical stimulation in the performance of daily life actions and in the relationship with family and friends. As depression is a multifactorial condition, the approach should be comprehensive, based on continuous care, focused and adapted to the needs of older adults, contributing to active aging. Another aspect to be explored is the preparation of health personnel in terms of old age, aging and their approach strategies due to the stigmatization in the care of older adults. This preparation will allow real comprehensive health care, which contributes toward the improvement of competencies in working with older adults and increases the social value of the intervention. It should not be forgotten to close gaps in knowledge through research, generating national evidence to improve the protective factors for older adults’ mental health.
This research is one of the few studies exploring depression in older adults. The results allowed us to infer that mental health care is fundamental in this population and, specially, in those who are 76 and older because they suffer from comorbidities and have interrupted recreational activities. There is a need for protection of these highly vulnerable people at high risk of developing depression. There should be health promotion interventions and prevention of mental illness, with emphasis on the first level of care that allows the attenuation of the effects of compulsory confinement, physical and social distancing, in addition to the excess of sensationalist information.
Data availability
Underlying data
Zenodo: Factors related to depression in older adults during the COVID 19 pandemic in two coastal regions of Peru: An analytical cross-sectional study. https://doi.org/10.5281/zenodo.5498990. 45
This project contains the following underlying data:
-
-
DATABASE_V4. 09-09.xlsx (dataset)
Extended data
Zenodo: Factors related to depression in older adults during the COVID 19 pandemic in two coastal regions of Peru: An analytical cross-sectional study. https://doi.org/10.5281/zenodo.5498990. 45
This project contains the following extended data:
-
-
FICHA DE RECOLECCIÓN DE DATOS 9-09.docx (a copy of the questionnaire)
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0).
Acknowledgements
We would like to thank the directors of the nonprofit association COPRODELI, who assist high-risk populations in marginal urban areas of two regions of Peru, Ica and Callao, and who facilitated the participation of the older adults.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 3; peer review: 2 approved]
References
- 1. Skirbekk VF, Staudinger UM, Cohen JE: How to Measure Population Aging? the Answer Is Less than Obvious: A Review. Gerontology. 2019;65:136–144. 10.1159/000494025 [DOI] [PubMed] [Google Scholar]
- 2. Gonzales E, Matz-Costa C, Morrow-Howell N: Increasing opportunities for the productive engagement of older adults: A response to population aging. Gerontologist .2015;55(2):252–261. 10.1093/geront/gnu176 [DOI] [PubMed] [Google Scholar]
- 3. Lee R, Mason A: Finance Dev. 2017;54(1):7–9. [PMC free article] [PubMed] [Google Scholar]
- 4. Lim GY, Tam WW, Lu Y, et al. : Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci Rep. 2018;8:1–10. 10.1038/s41598-018-21243-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Organización Mundial de la Salud: Informe Mundial sobre el envejecimiento y la salud. 2015.
- 6. Padayachey U, Ramlall S, Chipps J: Depression in older adults: Prevalence and risk factors in a primary health care sample. South African Fam Pract. 2017;59(2):61–66. 10.4102/safp.v59i2.4536 [DOI] [Google Scholar]
- 7. Grover S, Malhotra N: Depression in elderly: A review of Indian research. J Geriatr Ment Heal. 2015;2(1):4–15. 10.4103/2348-9995.161376 [DOI] [Google Scholar]
- 8. Cervantes Becerra RG, Villarreal Ríos E, Galicia Rodríguez L, et al. : Estado de salud en el adulto mayor en atención primaria a partir de una valoración geriátrica integral. Aten Primaria. 2015;47(6):329–335. 10.1016/j.aprim.2014.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Saenz-Miguel S, Runzer-Colmenares FM, Parodi JF: Trastornos depresivos en adultos mayores de once comunidades altoandinas del Perú, 2013-2017. Acta Medica Peru. 2019;36(1):26–31. [Google Scholar]
- 10. Martina M, Ara MA, Gutiérrez C, et al. : Depression and associated factors in the Peruvian elderly population according to ENDES 2014-2015. An Fac Med. 2014;78(4):393–397. [Google Scholar]
- 11. Instituto Nacional de Estadística e Informática: Perú Resultados definitivos de los censos nacionales 2017-2018.
- 12. World Health Organization [Internet]. Switzerland: World Health Organization;[cited Jul 16th 2021]: Covid-19 Explorer. Reference Source
- 13. Benke C, Autenrieth L, Asselmann E, et al. : Pané-Farré.l. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. 2020;293:3–9. 10.1016/j.psychres.2020.113462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ettman CK, Abdalla SM, Cohen GH, et al. : Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2021;3(9):1–12. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pilania M, Yadav V, Bairwa M, et al. : Prevalence of depression among the elderly (60 years and above) population in India, 1997-2016: A systematic review and meta-analysis. BMC Public Health. 2019;19:1–18. 10.1186/s12889-019-7136-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Toledo-Fernández A, Betancourt-Ocampo D, González-González A: Distress, depression, anxiety, and concerns and behaviors related to covid-19 during the first two months of the pandemic: A longitudinal study in adult mexicans. Behav Sci. 2021;11:2–15. 10.3390/bs11050076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hyland P, Shevlin M, McBride O, et al. : Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. Acta Psychiatr Scand. 2020;142:249–256. 10.1111/acps.13219 [DOI] [PubMed] [Google Scholar]
- 18. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, et al. : Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica. 2020;36(4):1–10. 10.1590/0102-311X00054020 [DOI] [PubMed] [Google Scholar]
- 19. Quiroga LP, Albala BC, Klaasen PG: Validación de un test de tamizaje para el diagnóstico de demencia asociada a edad, en Chile. Rev Med Chil. 2004;132:467–478. 10.4067/S0034-98872004000400009 [DOI] [PubMed] [Google Scholar]
- 20. Cabañero-Martínez MJ, Cabrero-García J, Richart-Martínez M, et al. : Revisión estructurada de las escalas de depresión en personas mayores. Int J Clin Heal Psychol. 2007;7(3):823–846. [Google Scholar]
- 21. Martínez-Martín P, Fernández-Mayoralas G, Frades-Payo B, et al. : Validación de la Escala de Independencia Funcional. Gac Sanit. 2009;23(1):49–54. [DOI] [PubMed] [Google Scholar]
- 22. Ganz F, Torralba R, Oliveira DV: Impacto de la inmovilización social por COVID-19 en la salud de personas adultas mayores: efectos físicos y mentales y recomendaciones. Nutr Health Aging. 2020;24(9):938–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. García-Fernández L, Romero-Ferreiro V, López-Roldán PD, et al. : Mental Health in Elderly Spanish People in Times of COVID-19 Outbreak. Am J Geriatr Psychiatry. 2020;28(10):1040–1045. 10.1016/j.jagp.2020.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Assari S, Gibbons FX, Simons R: Depression among black youth; interaction of class and place. Brain Sci. 2018;8:1–17. 10.3390/brainsci8060108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Baum A, Wisnivesky J, Basu S, et al. : Association of Geographic Differences in Prevalence of Uncontrolled Chronic Conditions with Changes in Individuals’ Likelihood of Uncontrolled Chronic Conditions. JAMA - J Am Med Assoc. 2020;324(14):1429–1438. 10.1001/jama.2020.14381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Atkins JL, Masoli JAH, Delgado J, et al. : Preexisting Comorbidities Predicting COVID-19 and Mortality in the UK Biobank Community Cohort. J Gerontol - Ser A Biol Sci Med Sci. 2020;75(11):2224–2230. 10.1093/gerona/glaa183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Armitage R, Nellums LB: COVID-19 and the consequences of isolating the elderly. Lancet Public Heal. 2020;5:256. 10.1016/S2468-2667(20)30061-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Choi EPH, Hui BPH, Wan EYF: Depression and anxiety in Hong Kong during covid-19. Int J Environ Res Public Health. 2020;17:1–11. 10.3390/ijerph17103740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Özdin S, Bayrak ÖŞ: Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int J Soc Psychiatry. 2020;66(5):504–511. 10.1177/0020764020927051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Solomou I, Constantinidou F: Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: Age and sex matter. Int J Environ Res Public Health. 2020;17:1–19. 10.3390/ijerph17144924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nwachukwu I, Nkire N, Shalaby R, et al. : Covid-19 pandemic: Age-related differences in measures of stress, anxiety and depression in Canada. Int J Environ Res Public Health. 2020:1–10. 10.3390/ijerph17176366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Chew NWS, Lee GKH, Tan BYQ, et al. : A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. 10.1016/j.bbi.2020.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stanton R, To QG, Khalesi S, et al. : Depression, anxiety and stress during COVID-19: Associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020;17:1–13. 10.3390/ijerph17114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Portellano-Ortiz C, Garre-Olmo J, Calvo-Perxas L, et al. : Depresión y variables asociadas en personas mayores de 50 años en España. Rev Psiquiatr Salud Ment (Barc.). 2018;11(4):216–226. 10.1016/j.rpsm.2016.10.003 [DOI] [PubMed] [Google Scholar]
- 35. Picaza M, Eiguren A, Dosil M, et al. : Stress, Anxiety, and Depression in People Aged Over 60 in the COVID-19 Outbreak in a Sample Collected in Northern Spain. Am J Geriatr Psychiatry. 2020;28(9):993–998. 10.1016/j.jagp.2020.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hossain MM, Tasnim S, Sultana A, et al. : Epidemiology of mental health problems in COVID-19: A review. F1000Res. 2020;9:1–16. 10.12688/f1000research.24457.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ávila-Funes JA, Garant MP, Aguilar-Navarro S, et al. : Relación entre los factores que determinan los síntomas depresivos y los hábitos alimentarios en adultos mayores de México. Rev Panam Salud Publica. 2006;19(5):321–330. [DOI] [PubMed] [Google Scholar]
- 38. König H, König HH, Konnopka A: The excess costs of depression: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. 2019;29:e30. 10.1017/S2045796019000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Schuch FB, Vancampfort D, Rosenbaum S, et al. : Exercise for depression in older adults: a meta-analysis of randomized controlled trials adjusting for publication bias. Braz J Psychiatry. 2016;38(3):247–254. 10.1590/1516-4446-2016-1915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cuiyan W, Riyu P, Xiaoyang W, et al. : Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17:1–25. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lei L, Huang X, Zhang S, et al. : Comparison of Prevalence and Associated Factors of Anxiety and Depression among People Affected by versus People Unaffected by Quarantine during the COVID-19 Epidemic in Southwestern China. Med Sci Monit. 2020;26:1–12. 10.12659/MSM.924609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huang Y, Zhao N: Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res .2020;288:2–6. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Pérez-Cano HJ, Moreno-Murguía MB, Morales-López O, et al. : Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic. Cir y Cir. 2020;88(5):562–568. 10.24875/CIRU.20000561 [DOI] [PubMed] [Google Scholar]
- 44. Tee ML, Tee CA, Anlacan JP, et al. : Psychological impact of COVID-19 pandemic in the Philippines. J Affective Disorders. 2020;277:379–391. 10.1016/j.jad.2020.08.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lozada OR, Asalde CAB, Carrillo JFS: Factors related to depression in older adults during the COVID 19 pandemic in two coastal regions of Peru: An analytical cross-sectional study [Data set]. Zenodo. 2021. 10.5281/zenodo.5498990 [DOI] [PMC free article] [PubMed] [Google Scholar]