The risk of venous thromboembolism (VTE) is markedly increased in patients with COVID-19 (COVID-19 VTE) and is associated with higher COVID-19 mortality.1 Whether the presence of inherited thrombophilias is associated with a higher risk of COVID-19 VTE remains a key outstanding issue, because the identification of risk factors that predispose to COVID-19 VTE is likely to be important in determining thrombotic risk and defining optimal antithrombotic regimens. Common inherited thrombophilias, including Factor V Leiden (FVL) and prothrombin mutation, have an estimated prevalence of 30% and are associated with a higher risk of VTE in the general population.2
Using data from the UK Biobank, we report on the association between inherited thrombophilias, COVID-19 VTE, and COVID-19 mortality. Participants included in the analysis were 45 to 69 years old when they were prospectively enrolled in the UK Biobank between 2006 and 2010 and subsequently tested positive for COVID-19 between January 2020 and May 2021. The study population was characterized by demographic information, body mass index, smoking status, medical comorbidities on enrollment to the UK Biobank, and the presence of defined genetic thrombophilias. To account for potential population genetic variation, we performed principal component analysis and estimated the top 10 principal components from highest to lowest variance. Participants were excluded if demographic, health, or genetic data were incomplete.
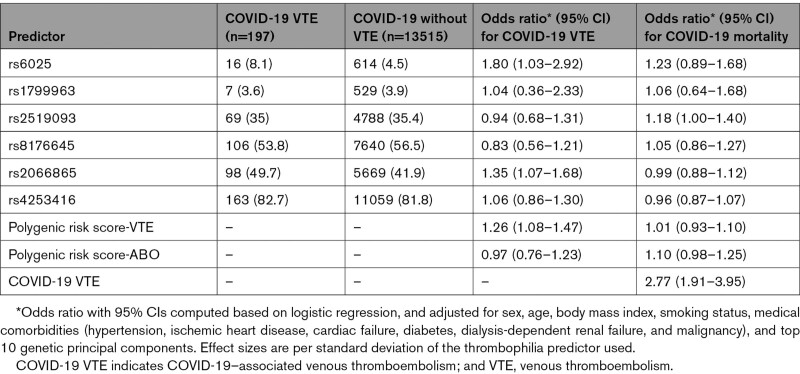
The study cohort was analyzed for 6 single-nucleotide polymorphisms (SNPs) resulting in inherited thrombophilia, including FVL (rs6025) and prothrombin mutation (rs1799963), in addition to variants in fibrinogen gamma gene (rs2066865), coagulation factor XI (rs4253416), and ABO blood group (rs2519093 and rs8176645). In addition, the utility of 2 polygenic risk scores (PRS) were examined that have been used to predict VTE risk in non–COVID-19 populations. The venous thromboembolism PRS (PRS-VTE) uses 297 variants, excluding SNPs defining FVL and prothrombin mutation, and identifies 5% of the population with a risk profile similar to carriers of FVL and prothrombin mutation.3 A second PRS (PRS-ABO) uses tag SNPs for ABO blood groups to assign a score associated with VTE risk.4
COVID-19 VTE was defined using International Classification of Diseases, 10th Revision coding for VTE (ie, International Classification of Diseases, 10th Revision codes I260, I269, I801, I802, and I822) after a COVID-19 diagnosis. COVID-19 mortality was defined using International Classification of Diseases, 10th Revision codes for COVID-19 on the death certificate.
Logistic regression was used to evaluate whether the SNPs or PRS were associated with COVID-19 VTE or COVID-19 mortality. Multivariable analysis was performed using the variables of age, sex, body mass index, smoking status, hypertension, ischemic heart disease, cardiac failure, diabetes, dialysis-dependent renal failure, malignancy, and the top 10 principal components. We report adjusted odds ratio (OR) with 95% CIs for the outcomes. Analysis was performed in R version 4.0.3. The data supporting this study are available from the corresponding author on reasonable request. The UK Biobank received ethical approval (11/NW/0382), and all participants gave informed consent.
Overall, 13 712 individuals with COVID-19 were included with a median age of 54 years, median body mass index of 27.6, and 52.5% were female. COVID-19 VTE was identified in 197 cases (1.4%), and there were 890 deaths from COVID-19 (6.5%; Table). The median follow-up time was 146 days (interquartile range, 115–198) and the median time to COVID-19 VTE diagnosis was 12 days (interquartile range, 6–27). The presence of rs6025, synonymous with the FVL mutation, was associated with an approximate 1.8-fold odds of COVID-19 VTE (OR, 1.80 [95% CI, 1.03–2.92]; Table). Moreover, both rs2066865 (OR, 1.35 [95% CI, 1.07–1.68]) and the PRS-VTE (OR, 1.26 [95% CI, 1.08–1.47]) were also associated with a higher risk of COVID-19 VTE (Table). In contrast, neither the PRS-ABO nor the presence of rs4253416, rs2519092, rs8176645, or rs1799963 was associated with COVID-19 VTE (Table).
Table 1.
Association of Genetic Thrombophilia With Venous Thromboembolism and Mortality in Individuals With COVID-19
Consistent with previous reports,1 we observed that COVID-19 VTE was associated with higher COVID-19 mortality (OR, 2.77 [95% CI, 1.91–3.95]; Table), but no association was observed between either the SNPs or PRS with COVID-19 mortality.
These findings demonstrate for the first time that the thrombophilic SNPs, rs6025 and rs2066865, in addition to the PRS-VTE, are associated with a higher risk of COVID-19 VTE. Limitations of this study include the predominance of European ancestry in the study population and the absence of a general population control cohort. Moreover, timely access to genetic testing remains an outstanding issue. Although prospective validation of these findings is required to determine the utility of routine thrombophilia testing in COVID-19, significant interest remains regarding the optimal antithrombotic regimen for the prevention of COVID-19 thrombotic complications. To date, studies evaluating the benefit of anticoagulation in patients with COVID-19 have been conflicting, and these regimens have consistently been associated with higher bleeding complications.5 Therefore, the identification of novel risk factors, such as genetic thrombophilias, may stratify patients with a higher risk of COVID-19 VTE, and ultimately help identify patients with COVID-19 who are more likely to benefit from higher-dose antithrombotic regimens.
Article Information
Acknowledgments
This research was conducted using the UK Biobank Resource (https://www.ukbiobank.ac.uk/) under application number 55469.
Sources of Funding
Dr Stevens is supported by a Monash University Research Training Program Scholarship, Wheaton Family Scholarship, and Haematology Society of Australia and New Zealand New Investigator Scholarship. Dr Peter is supported by a National Health and Medical Research Council Senior Principal Research Fellowship. Dr McFadyen is supported by a National Health and Medical Research Council and Heart Foundation Early Career Fellowship.
Disclosures
None.
Nonstandard Abbreviations and Acronyms
- FVL
- Factor V Leiden
- PRS
- polygenic risk score
- SNP
- single-nucleotide polymorphism
- VTE
- venous thromboembolism
H. Stevens and R. Canovas contributed equally.
K. Peter and J.D. McFadyen contributed equally.
For Sources of Funding and Disclosures, see page 942.
Circulation is available at www.ahajournals.org/journal/circ
Continuing medical education (CME) credit is available for this article. Go to http://cme.ahajournals.org to take the quiz.
Contributor Information
Hannah Stevens, Email: hannah.stevens1@monash.edu.
Rodrigo Canovas, Email: rodrigo.canovas@baker.edu.au.
Huyen Tran, Email: huyen.tran@monash.edu.
Karlheinz Peter, Email: karlheinz.peter@baker.edu.au.
References
- 1.McFadyen JD, Stevens H, Peter K. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res. 2020; 127:571–587. doi: 10.1161/CIRCRESAHA.120.317447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Middeldorp S. Inherited thrombophilia: a double-edged sword. Hematology Am Soc Hematol Educ Program. 2016; 2016:1–9. doi: 10.1182/asheducation-2016.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klarin D, Busenkell E, Judy R, Lynch J, Levin M, Haessler J, Aragam K, Chaffin M, Haas M, Lindström S, et al. ; INVENT Consortium; Veterans Affairs’ Million Veteran Program. Genome-wide association analysis of venous thromboembolism identifies new risk loci and genetic overlap with arterial vascular disease. Nat Genet. 2019; 51:1574–1579. doi: 10.1038/s41588-019-0519-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goumidi L, Thibord F, Wiggins KL, Li-Gao R, Brown MR, van Hylckama Vlieg A, Souto JC, Soria JM, Ibrahim-Kosta M, Saut N, et al. Association between ABO haplotypes and the risk of venous thrombosis: impact on disease risk estimation. Blood. 2021; 137:2394–2402. doi: 10.1182/blood.2020008997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ten Cate H. Surviving Covid-19 with heparin? N Engl J Med. 2021; 385:845–846. doi: 10.1056/NEJMe2111151 [DOI] [PMC free article] [PubMed] [Google Scholar]