Abstract
Experiences of potentially traumatic events (PTE), commonly assessed with the Life Events Checklist for DSM-5 (LEC-5), can be both varied in pattern and type. An understanding of LEC-assessed PTE type clusters and their relation to psychopathology can enhance research feasibility (e.g., address low base rates for certain PTE types), research communication/comparisons via the use of common terminology, and nuanced trauma assessments/treatments. To this point, the current study examined (1) clusters of PTE types assessed by the LEC-5; and (2) differential relations of these PTE type clusters to mental health correlates (i.e., posttraumatic stress disorder [PTSD] severity, depression severity, emotion dysregulation, reckless and self-destructive behaviors [RSDBs]). A trauma-exposed community sample of 408 participants was recruited via Amazon’s Mechanical Turk (Mage = 35.90 years; 56.50% female). Network analyses indicated three PTE type clusters: Accidental/Injury Traumas (LEC-5 items 1, 2, 3, 4, 12), Victimization Traumas (LEC-5 items 6, 8, 9), and Predominant Death Threat Traumas (LEC-5 items 5, 7, 10, 11, 13-16). Multiple regression analyses indicated that the Victimization Trauma Cluster significantly predicted PTSD severity (β = .23, p <.001), depression severity (β = .20, p =.001), and negative emotion dysregulation (β = .22, p <.001); and the Predominant Death Threat Trauma Cluster significantly predicted engagement in RSDBs (β = 31, p <.001) and positive emotion dysregulation (β = .26, p <.001), accounting for the influence of other PTE Clusters. Results support three PTE type classifications assessed by the LEC-5, with important clinical and research implications.
Keywords: Life Events Checklist for DSM-5, trauma type classification, network analyses, psychopathology correlates
Introduction
Experience of traumatic events is a critical etiological factor for several disorders within the Diagnostic and Statistical Manual of Mental Disorders (DSM; e.g., posttraumatic stress disorder [PTSD]; American Psychiatric Association, 2013). Thus, greater clinical and research attention is needed on screening and assessing potentially traumatic events (PTEs); yet this aspect is quite understudied compared to trauma-related health outcomes. One of the most widely used self-report measures of diverse PTEs is the Life Events Checklist (LEC; Gray, Litz, Hsu, & Lombardo, 2004; Weathers et al., 2013). Despite their inherent diversity (Contractor, Caldas, Fletcher, Shea, & Armour, 2018; Litz et al., 2018; Luz et al., 2011), PTEs can be meaningfully clustered together based on underlying shared risk factors (e.g., neuroticism) and/or characteristics (e.g., perpetrated by other individuals; Breslau, Davis, & Andreski, 1995; Finkelhor, 2008). To extend this line of research, the current study examined clusters of lifetime PTE types assessed by the LEC, and their relations with mental health correlates.
Clinicians and researchers use a wide array of measures to assess lifetime PTEs. One such widely used self-report measure is the LEC, which is either administered in conjunction with the Clinician-administered PTSD Scale (Blake et al., 1995) or as a screening instrument by itself (Weathers et al., 2013). Specifically, the LEC for DSM-5 (LEC-5; Weathers et al., 2013), adapted from the DSM-IV version (Gray et al., 2004), is composed of 17 items assessing different lifetime PTEs. This scale uses six nominal categories of responses: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. Psychometrically, the LEC for DSM-IV has demonstrated good convergent and discriminant validity, test-retest reliability over a seven-day period, and concurrent validity with other trauma measures (Bae, Kim, Koh, Kim, & Park, 2008; Gray et al., 2004). There is no known study on the psychometrics of the LEC-5, although the LEC-5 only differs from the LEC for DSM-IV in the addition of the response option “part of my job” corresponding to DSM-5 changes in the PTSD diagnostic criteria (American Psychiatric Association, 2013).
Moreover, relatively unexplored are clusters of PTE types as examined by the LEC-5. Supporting this line of investigation, evidence indicates that most individuals experience more than one PTE type in their lifetime (Carlson et al., 2011; Higgins & McCabe, 2001), and PTEs could be clustered together attributed to various reasons. One, common risk factors such as higher levels of trait neuroticism and lower education may contribute to clusters of PTE types (Breslau et al., 1995). Two, different PTE types may share common characteristics. For example, physical and sexual assault are perpetrated by another individual and considered victimization experiences involving malevolence, betrayal, and/or immorality (Finkelhor, 2008); while hurricanes, tornados, and earthquakes, as natural disasters, are conceptualized as uncontrollable, hazardous, and threatening natural phenomena with profound impacts on society and functioning (e.g., loss of life and livelihood; Alcántara-Ayala, 2002; Fritz, 1961). Indeed, preliminary evidence has supported clusters of PTE types across diverse trauma measures: interpersonal vs. non-interpersonal traumas (Sijbrandij et al., 2013); intentional (e.g., assault) vs. non-intentional traumas (e.g., natural disaster; Santiago et al., 2013); different military-related traumas (e.g., traumatic loss, being betrayed by others; Litz et al., 2018); and traumas differentiated by affected developmental functions (e.g., attachment) and trauma characteristics (e.g., cumulative stress, Kira, Lewandowski, Somers, Yoon, & Chiodo, 2012).
There are two noteworthy limitations in this regard. First, most existing PTE type clusters were not empirically-derived using recommended statistical techniques. Relatedly, some trauma assessments have been factor-analyzed such as the Stressful Life Events Screening Questionnaire (Allen, Madan, & Fowler, 2015) and Childhood Trauma Questionnaire (Spinhoven et al., 2014). Such an approach is problematic and unsuited to examining clusters of PTE types (Hooper, Stockton, Krupnick, & Green, 2011) because it assumes (1) that a latent variable of “trauma/stressor type” is causing specific PTEs, and (2) the association between all PTE types within a cluster will be accounted for by the latent variable disregarding any potential directional relations among the PTE types (i.e., assumption of local independence; Hodgdon et al., 2019). Second only one study, to our knowledge, has examined clusters of PTE types as assessed by the LEC. Bae et al. (2008) found an optimal six-factor solution: physical assault/others (items 6, 9, 13, 16, 17), accident/injury (items 2, 3, 4, 12, 17), natural disaster/witnessing death (items 1, 14, 15), sexual abuse (items 8, 9), criminal assault (items 7, 11, 16), and man-made disaster (items 5, 7, 10). Notably, this study used the LEC for DSM-IV, a Korean version of the LEC, and a factor-analytical approach to clustering PTE types. Further, although research indicates clusters of PTE types assessed by other trauma measures (Allen et al., 2015; Spinhoven et al., 2014), these measures are not comparable to the LEC; the number and nature of items are vastly different, hence limiting transferability and applicability of findings to the LEC.
Overall, we know very little about empirically-derived clusters of PTE types for trauma assessments in general, and specifically for those examined by the LEC. Addressing these limitations, the current study examined (1) clusters of lifetime PTE types assessed by the LEC-5 using a novel and empirically-supported statistical approach of network analysis; and (2) differential relations of the obtained clusters to theoretically- and empirically-relevant mental health correlates (i.e., PTSD severity, depression severity, emotion dysregulation, and reckless and self-destructive behaviors [RSDBs]). The network approach to psychopathology conceptualizes mental disorders as a group of causally-related symptoms that influence each other; this symptom-to-symptom interaction pattern represents a network structure (Borsboom, 2017; Borsboom, Cramer, & Kalis, 2019). Symptoms that are closely related to each other, those that influence each other to a greater extent, and those that have more associations with each other form clusters or network communities (Borsboom, Cramer, Schmittmann, Epskamp, & Waldorp, 2011; Jones, Mair, & McNally, 2018). The network approach has rarely examined PTEs compared to post-trauma psychopathology (Contractor, Greene, Dolan, Weiss, & Armour, 2020; Weiss, Contractor, Raudales, Greene, & Short, 2020). This being said, the network approach to psychopathology as well as the corresponding analytical tool of network analyses has direct relevance to the current study’s research questions for three reasons. One, PTE types (i.e., nodes), conceptually, form a network of mutually interactive components connected by associational parameters (i. e., edges; degree of co-occurrence; Hodgdon et al., 2019). If two PTE types co-occur together, they are statistically connected within the network (Hodgdon et al., 2019). Second, this approach can identify network communities or clusters of PTE types that co-occur in meaningful ways across individuals (Hodgdon et al., 2019; Jones et al., 2018). Results can enhance our understanding regarding mechanisms/types of co-occurrence across PTE types (Fried et al., 2017). The concept of network communities/clusters is parallel to the concept of factor loadings on a latent factor as discussed in factor analyses (Borsboom, 2017). Lastly, network analyses overcome limitations of applying a latent variable model approach to examining PTE type clusters as elaborated in the earlier text (Hodgdon et al., 2019).
Given the lack of research in this area, we considered the study aims to be exploratory; however, expected to find a PTE type cluster including interpersonal/sexual traumas drawing from relevant research (Allen et al., 2015; Contractor, Brown, & Weiss, 2018; Contractor, Caldas, et al., 2018; Hodgdon et al., 2019; Spinhoven et al., 2014). Moreover, based on existing research, we expected that the interpersonal/sexual trauma category would be more strongly associated with psychopathology correlates. As examples, Breslau et al. (1998) found that assaultive violence was most likely to trigger PTSD; Kilpatrick et al. (2013) indicated that the highest prevalence rates of lifetime PTSD was among those experiencing interpersonal violence or military combat; Allen et al. (2015) found that sexual traumas was more related to negative emotion dysregulation and RSDBs such as suicide attempts, and assaults were more related to RSDBs such as substance misuse; and Vrana and Lauterbach (1994) indicated that sexual assault explained 7% of the variance in depression.
Delineating empirically-derived PTE type clusters is an optimal and feasible compromise between options of using a composite score of PTE exposure (which is most parsimonious but at the cost of considering heterogenous PTE types) vs. examining each PTE type separately in trauma research (which is not always feasible and/or meaningful; Hodgdon et al., 2019). Regarding the latter approach, there is “low base rate” problem, wherein certain PTE types are less prevalent in certain study samples (Gray et al., 2004), which makes it difficult to consider all PTE types meaningfully in research. As an example, combat-related PTEs are less frequently endorsed in student samples (Frazier et al., 2009; Read, Ouimette, White, Colder, & Farrow, 2011). Further, empirically-derived PTE type clusters will facilitate: (1) research on impacts of PTEs on diverse psychopathology using derived PTE type clusters as LEC-5 subscales (Floyd & Widaman, 1995); (2) comparisons across research studies; and (3) communication via common terminology among researchers/clinicians using the LEC-5 (Luz et al., 2011). Lastly, understanding relations of different PTE type clusters to psychopathology may enable a more nuanced assessment and treatment approach for trauma clinicians.
Methods
Procedure and Participants
Participants were recruited from Amazon’s Mechanical Turk (MTurk) platform. The current study was described as a 45-60-minute survey about stressful life experiences. Inclusion criteria were (1) 18 years or older, (2) living in North America, (3) fluency in English, and (4) the presence of PTE(s) screened with the Primary Care PTSD Screen for DSM-5 (Prins et al., 2015). Participants who met eligibility criteria, provided informed consent, and completed the survey on Qualtrics validly received $1.25. These procedures were approved by the University of North Texas Institutional Review Board.
Exclusions and Missing Data
We implemented several steps to ensure data quality and integrity. Of the obtained 891 responses, 47 responses from 18 participants who attempted to answer the questionnaire multiple times were excluded (remainder n = 844). We further excluded 150 participants not meeting all inclusionary criteria, 122 participants not passing all four validity checks to ensure attentive responding and comprehension (Meade & Craig, 2012; Thomas & Clifford, 2017), 97 participants missing data on all measures, and 11 participants not endorsing a PTE/most distressing PTE on the LEC-5 (Weathers et al., 2013). We also excluded 56 participants who missed >30% item-level data on the primary study variables. The final sample included 408 trauma-exposed participants, averaging 35.90 years with 56.50% female and 62.50% having a probable PTSD diagnosis. Further, the majority of participants identified as non-Hispanic or Latino/a (n = 348, 85.30%) and as White (n = 314, 77%). See Table 1 for detailed information on socio-demographic variables. Missing data in this sample was minimal (e.g., one participant was missing one LEC-5 item; 9 participants were missing one Patient Health Questionnaire-9 item; one participant was missing one Difficulties in Emotion Regulation Scale–16 item; two individuals were missing one Difficulties in Emotion Regulation Scale–Positive item; and 77 participants were missing two Posttrauma Risky Behaviors Questionnaire items).
Table 1.
Descriptive Information on Demographic, Psychopathology, and Traumatic Events Data (n = 408)
| M | SD | Skewness Values | Kurtosis Values | |
|---|---|---|---|---|
| Age | 35.90 | 11.22 | .88 | .12 |
| Years of schooling | 15.26 | 2.40 | −.39 | 4.84 |
| PTSD severity | 24.84 | 20.16 | .61 | −.60 |
| Depression severity | 7.06 | 6.41 | .80 | −.20 |
| Reckless and self-destructive behaviors | 6.74 | 9.27 | 1.83 | 2.73 |
| Negative emotion dysregulation | 34.68 | 15.78 | .62 | −.66 |
| Positive emotion dysregulation | 19.47 | 10.55 | 1.77 | 1.96 |
| PTE Type Cluster 1 | 2.89 | 1.58 | −.14 | −1.14 |
| PTE Type Cluster 2 | 1.50 | 1.23 | .02 | −1.60 |
| PTE Type Cluster 3 | 2.35 | 2.46 | 1.03 | −.05 |
| n | % within column* | |||
| Gender | ||||
| Female | 234 | 57.4% | ||
| Male | 168 | 41.2% | ||
| Male to female transgender | 1 | 0.2% | ||
| Female to male transgender | 3 | 0.7% | ||
| Other | 2 | 0.5% | ||
| Ethnicity | ||||
| Hispanic or Latino/a | 54 | 13.2% | ||
| Non-Hispanic or Latino/a | 348 | 85.3% | ||
| Unknown | 6 | 1.5% | ||
| Race (could endorse multiple responses) | ||||
| White or Caucasian | 314 | 77% | ||
| African American or Black | 39 | 9.6% | ||
| Asian | 44 | 10.8% | ||
| American Indian or Alaska Native | 19 | 4.7% | ||
| Native Hawaiian or other Pacific | 3 | 0.7% | ||
| Islander | ||||
| Unknown | 6 | 1.5% | ||
| Employment | ||||
| Full-time | 289 | 70.8% | ||
| Part-time | 64 | 15.7% | ||
| Unemployed | 34 | 8.3% | ||
| Unemployed student | 8 | 2% | ||
| Retired | 13 | 3.2% | ||
| Income | ||||
| < $15,000 | 39 | 9.6% | ||
| $15,000 to $24,999 | 54 | 13.2% | ||
| $25,000 to $34,999 | 62 | 15.2% | ||
| $35,000 to $49,999 | 55 | 13.5% | ||
| $50,000 to $64,999 | 77 | 18.9% | ||
| $65,000 to $79,999 | 37 | 9.1% | ||
| ≥ $80,000 | 84 | 20.6% | ||
| Relationship status | ||||
| Not dating | 66 | 16.2% | ||
| Casually dating | 30 | 7.4% | ||
| Seriously dating | 99 | 24.3% | ||
| Married | 180 | 44.1% | ||
| Divorced | 18 | 4.4% | ||
| Separated | 8 | 2% | ||
| Widowed | 7 | 1.7% | ||
| Currently receiving mental health treatment | 45 | 11% | ||
| Received past mental health treatment | 180 | 44.1% | ||
| Currently taking medications for mental health or emotional problems | 69 | 16.9% | ||
| Taken medications for mental health or emotional problems in the past | 77 | 18.9% | ||
| Potentially traumatic event types endorsed on the Life Events Checklist for DSM-5 | ||||
| Natural disaster | 267 | 65.4% | ||
| Fire or explosion | 209 | 51.2% | ||
| Transportation accident | 318 | 77.9% | ||
| Serious accident at work/home/during recreational activity | 180 | 44.1% | ||
| Exposure to a toxic substance | 100 | 24.5% | ||
| Physical assault | 228 | 55.9% | ||
| Assault with a weapon | 151 | 37% | ||
| Sexual assault | 185 | 45.3% | ||
| Other unwanted/uncomfortable sexual experience | 198 | 48.5% | ||
| Combat or exposure to war | 106 | 26% | ||
| Forced captivity | 68 | 16.7% | ||
| Life-threatening illness or injury | 204 | 50% | ||
| Severe human suffering | 129 | 31.6% | ||
| Sudden, violent death | 165 | 40.4% | ||
| Sudden, accidental death | 169 | 41.4% | ||
| Serious injury/harm/death you caused to someone else | 69 | 16.9% | ||
| Any other stressful event or experience | 165 | 40.4% | ||
Note.
percentages are reported accounting for missing data; PTE Type Cluster 1 - Accidental/Injury Traumas, PTE Type Cluster 2 - Victimization Traumas, PTE Type Cluster 3 - Predominant Death Threat Traumas.
Measures
Life Event Checklist for DSM-5 (LEC-5; F. W. Weathers et al., 2013).
It is a 17-item self-report measure assessing lifetime PTE types. Participants rate each item with 6 response options: happened to me, witnessed it, learned about it, part of my job, not sure, or doesn’t apply. For the current study, a positive trauma endorsement was indicated when individuals selected either of the first four response options consistent with PTSD DSM-5 Criterion A (American Psychiatric Association, 2013).
Posttrauma Risky Behaviors Questionnaire (PRBQ; Contractor, Weiss, Kearns, Caldas, & Dixon-Gordon, in press).
It is a 16-item self-report measure assessing the extent of engaging in post-trauma RSDBs in the past month. The first 14 PRBQ items assess the extent of engaging in specific RSDBs with response options ranging from 0 (never) to 4 (very frequently). The last two items assess functional impairment and relation of RSDB frequency to onset of the worst PTE. In the current study, scores for 14 items were summed; higher scores represented greater extent of RSDB engagement. The PRBQ has good psychometric properties (Contractor, Weiss, Dolan, & Mota, 2019; Contractor et al., in press); the Omega value was .95 in the current study.
PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013).
It is a 20-item self-report measure assessing PTSD severity referencing the past month. Response options range from 0 (not at all) to 4 (extremely). The PCL-5 has excellent psychometric properties (Bovin et al., 2016); the Omega value was .97 in the current study. Participants completed the PCL-5 referencing the most distressing PTE endorsed on the LEC-5 (Weathers et al., 2013).
Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002).
It is a 9-item self-report measure assessing depression symptoms over the past two weeks. Response options range from 0 (not at all) to 3 (nearly every day). The PHQ-9 has good psychometric properties (Kroenke, Spitzer, & Williams, 2001); the Omega value was .83 in the current study.
The Difficulties in Emotion Regulation Scale-16 (DERS-16; Bjureberg et al., 2016).
It is a 16-item self-report measure of negative emotional dysregulation using a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always). For the current study, we used the DERS-16 total score; higher scores indicated greater difficulties regulating negative emotions. The DERS-16 has good psychometric properties (Hallion, Steinman, Tolin, & Diefenbach, 2018); the Omega value was .99 in the current study.
The Difficulties in Emotion Regulation Scale–Positive (DERS-P; Weiss, Gratz, & Lavender, 2015).
It is a 13-item self-report measure of positive emotion dysregulation using a 5-point Likert scale ranging from 1 (almost never) to 5 (almost always). For the current study, we used the DERS-P total score; higher scores indicated greater difficulties regulating positive emotions. The DERS-P has good psychometric properties (Weiss, Darosh, Contractor, Schick, & Dixon-Gordon, 2019; Weiss et al., 2015); the Omega value was .96 in the current study.
Statistical Plan
For the primary analyses, we excluded LEC-5 item 17 which asked for another stressful life event not captured by the other items because of the ambiguity in obtained content. Following guidelines of utilizing samples of ~500 participants to estimate binary variable-based networks of low-moderate sizes (i. e., 10-30 nodes; Dalege, Borsboom, van Harreveld, & van der Maas, 2017), our sample size was sufficient for exploratory data-driven analyses for 16 binary nodes. The network was estimated using complete pairwise observations (i.e., using all available data).
Network Estimation, Visualization, and Accuracy.
We used the bootnet (which imports the IsingFit package; Epskamp, Borsboom, & Fried, 2018) and qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012) packages in R. For network estimation, we used the Ising model that is appropriate for binary data and estimates parameters with logistic regression (van Borkulo et al., 2014). To reduce the likelihood of spurious edges and obtain a sparse/parsimonious network, we estimated a regularized partial correlation network structure using the enhanced least absolute shrinkage and selection operator (eLasso; van Borkulo et al., 2014), with Extended Bayesian Information Criterion (EBIC; Chen & Chen, 2008) to select a value for the tuning parameter. In the current network, a node indicated a psychological variable (PTE type) and an edge was a regularized partial correlation between two nodes after statistically controlling for other network nodes (Borsboom & Cramer, 2013). For each edge, we examined its weight reflecting strength and its sign reflecting direction; weights were graphically represented by line thickness (Borsboom & Cramer, 2013; Costantini et al., 2019). The network’s graphical layout was based on the Fruchterman-Reingold algorithm (Fruchterman & Reingold, 1991); weaker nodes with fewer connections were placed further apart and stronger nodes with more connections were placed closer together (Hevey, 2018).
To examine network accuracy, we estimated confidence intervals (CIs) on the edge-weights (nonparametric bootstrapping with replacement) and statistically significant differences between edge-weights (bootstrapped difference test; Epskamp et al., 2018). Finally and most relevant to the current study, to detect network communities (i.e., clusters of nodes highly connected with one another and less connected with nodes outside their clusters), we used the walktrap algorithm (Pons & Latapy, 2005) derived from the R package igraph (Csardi & Nepusz, 2006). The walktrap algorithm computes a community structure in time depending on the density of the community, the height of the corresponding hierarchical community structure, the number of vertices, and the number of edges.
Examination of Influential Nodes and Predictability of Nodes.
The one-step expected influence (EI1) estimate is a measure of a node’s influence with other neighboring nodes (i.e., nodes connected to and share edges with the target node) and considers positive and negative edge weight values in its computation (Robinaugh, Millner, & McNally, 2016). With a positive EI1 estimate, changes in the node are associated with changes in the overall network in the same direction; with a negative EI1 estimate, changes in the node are associated with changes in the overall network in the opposite direction (Robinaugh et al., 2016). We computed EI1 estimates using the R package networktools (Jones, 2018).
Additionally, we computed predictability of nodes, which indicates how well a certain node can be predicted by neighboring nodes in the network (Haslbeck & Waldorp, 2018; Haslbeck & Fried, 2012). In other words, the predictability estimate indicates how much of the variance in a certain node can be explained by all edges connected to that node (Haslbeck & Waldorp, 2018; Haslbeck & Fried, 2012). In the current study, we computed a predicted probability for each category of the binary nodes (i.e., endorsed vs. not endorsed) using a multinomial distribution (Haslbeck & Waldorp, 2018). We computed a normalized accuracy measure for the binary nodes which quantifies predication of a node by its neighboring nodes beyond the intercept model; for instance, this measure is 0 when other variables do not predict the node beyond the intercept model (Haslbeck & Fried, 2012). The normalized accuracy measure ranges from 0 (no predictability) to 1 (perfect prediction; Haslbeck & Fried, 2012); higher predictability of a node is indicated by prediction estimates that are closer to the actual values of a node (Haslbeck & Waldorp, 2018). We used R packages mgm (Haslbeck & Waldorp, 2015, 2020) and qgraph (Epskamp et al., 2012) to compute and visualize predictability estimates.
PTE Type Clusters and Mental Health Correlates.
We created a score for the PTE type clusters by summing scores of all LEC-5 items within each cluster based on results from network analyses (i.e., network communities/clusters). All study variables were normally distributed (−2 < skewness < 2; −7 < kurtosis < 7; Curran, West, & Finch, 1996). We examined multicollinearity for the PTE type clusters using the Variance Inflation Factor (VIF) ≥ 10 and tolerance value < .01 rules (Hair, Black, Babin, & Anderson, 2009); multicollinearity was not violated. To examine the differential relations of the obtained PTE type clusters to mental health correlates, we used the PTE type cluster scores as predictors of each mental health correlate (PTSD severity, depression severity, difficulties regulating negative and positive emotions, RSDBs) in a multiple regression model. We used SPSS v. 26 (IBM Corp, 2017) for these analyses.
Results
Network Estimation, Visualization, and Accuracy.
Figure 1 indicates the regularized partial correlation network corresponding to Table 2 values. Examining the edge weights, the strongest associations were between these nodes: LEC-5 4 with LEC-5 5 (1.03) and LEC-5 7 (.80), LEC-5 5 with LEC-5 10 (1.04) and LEC-5 11 (1.22), LEC-5 6 with LEC-5 7 (.96) and LEC-5 9 (.81), LEC-5 7 with LEC-5 10 (1.08) and LEC-5 11 (.94), LEC-5 8 with LEC-5 9 (1.79), LEC-5 11 with LEC-5 13 (1.01), and LEC-5 14 with LEC-5 15 (.95). Regarding network accuracy (Supplemental Figures 1 and 2), results indicated that the edge weight connecting LEC-5 8 with LEC-5 9 was significantly stronger than all other edge weights; both of these nodes represented sexual interpersonal traumas. Importantly, we found three PTE type clusters/communities: PTE Type Cluster 1 (LEC-5 items 1, 2, 3, 4 and 12); PTE Type Cluster 2 (LEC-5 items 6, 8, and 9); and PTE Type Cluster 3 (LEC-5 items 5, 7, 10, 11, 13-16). We created cluster descriptions based on prominent patterns; notably PTE Type Cluster 3 was more heterogenous than other clusters. PTE Type Cluster 1 was described as Accidental/Injury Traumas; PTE Type Cluster 2 was described as Victimization Traumas; and PTE Type Cluster 3 was described as Predominant Death Threat Traumas (this had prominent death-related traumas).1
Figure 1.
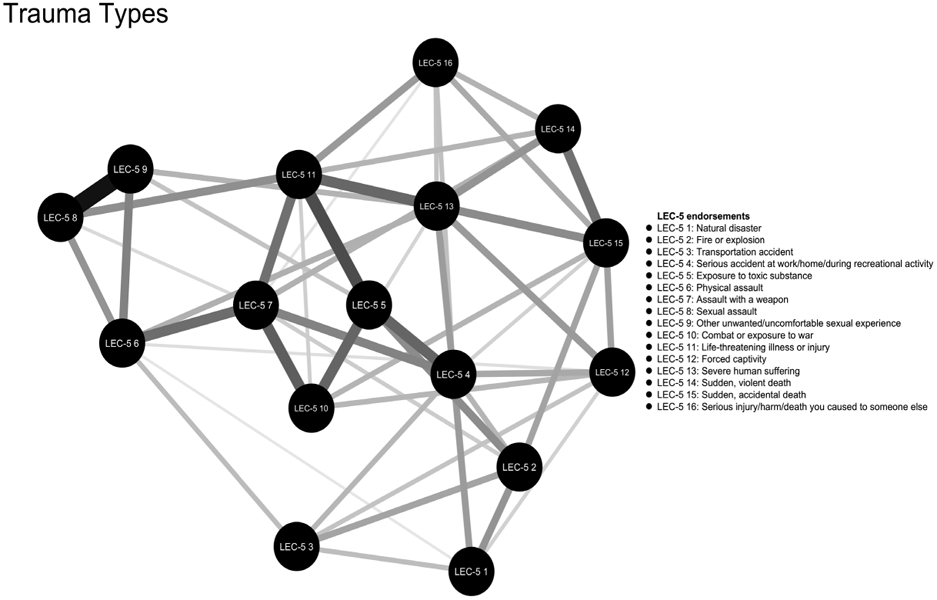
Regularized partial correlation network.
Table 2.
Regularized partial correlation matrix
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. LEC-5 1 | 0 | .68 | .41 | .63 | 0 | .15 | 0 | 0 | 0 | 0 | 0 | .28 | 0 | 0 | 0 | 0 |
| 2. LEC-5 2 | 0 | .60 | .46 | .74 | 0 | .32 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | .58 | 0 | |
| 3. LEC-5 3 | 0 | .45 | 0 | .42 | 0 | 0 | 0 | 0 | 0 | .37 | 0 | 0 | 0 | 0 | ||
| 4. LEC-5 4 | 0 | 1.03 | 0 | .31 | .80 | 0 | 0 | 0 | .54 | .63 | 0 | .28 | .39 | |||
| 5. LEC-5 5 | 0 | 0 | 0 | 0 | .37 | 1.04 | 1.22 | 0 | 0 | 0 | 0 | 0 | ||||
| 6. LEC-5 6 | 0 | .96 | .68 | .81 | 0 | 0 | .20 | .50 | 0 | 0 | 0 | |||||
| 7. LEC-5 7 | 0 | .23 | 0 | 1.08 | .94 | 0 | 0 | .50 | 0 | .18 | ||||||
| 8. LEC-5 8 | 0 | 1.79 | 0 | .72 | 0 | 0 | 0 | 0 | 0 | |||||||
| 9. LEC-5 9 | 0 | 0 | 0 | 0 | .47 | 0 | 0 | 0 | ||||||||
| 10. LEC-5 10 | 0 | .29 | .46 | .26 | 0 | .47 | 0 | |||||||||
| 11. LEC-5 11 | 0 | 0 | 1.01 | .47 | 0 | .64 | ||||||||||
| 12. LEC-5 12 | 0 | .64 | 0 | .60 | 0 | |||||||||||
| 13. LEC-5 13 | 0 | .68 | .75 | .38 | ||||||||||||
| 14. LEC-5 14 | 0 | .95 | .48 | |||||||||||||
| 15. LEC-5 15 | 0 | .53 | ||||||||||||||
| 16. LEC-5 16 | 0 |
Note. LEC-5 is the Life Events Checklist for DSM-5; LEC-5 1 is natural disaster; LEC-5 2 is fire/explosion; LEC-5 3 is transportation accident; LEC-5 4 is serious accident at work/home/during recreational activity; LEC-5 5 is exposure to toxic substance; LEC-5 6 is physical assault; LEC-5 7 is assault with a weapon; LEC-5 8 is sexual assault; LEC-5 9 is other unwanted/uncomfortable sexual experience; LEC-5 10 is combat or exposure to war; LEC-5 11 is forced captivity; LEC-5 12 is life-threatening illness/injury; LEC-5 13 is severe human suffering; LEC-5 14 is sudden, violent death; LEC-5 15 sudden, accidental death; LEC-5 16 is serious injury/harm/death you caused to someone else.
Examination of Influential Nodes and Predictability of Nodes.
See Table 3 for the EI1 and predictability estimates. Results indicated that all EI1 estimates were positive meaning that changes in each PTE type node was associated with changes in the overall network in the same direction (i.e., increase or decrease in the activation of each PTE type node was associated with an increase or decrease in the activation of neighboring nodes respectively). Further, nodes with the highest EI1 estimates included LEC-5 items 13, 11, 4 and 7 in that order (most belonged to PTE Type Cluster 3). Additionally, results indicated that nodes with the highest predictability values (normalized accuracy measure) included LEC-5 items 9, 8, 4, 7, and 6 in that order (most belonged to PTE Type Cluster 2). See Supplemental Figure 3 for the visualization of node predictability estimates.
Table 3.
One-step expected influence and predictability estimates for each of the potentially traumatic events type node.
| Nodes | One-step expected influence Estimates |
Predictability Estimates | ||
|---|---|---|---|---|
| Accuracy/Correct Classification (CC) |
Normalized Accuracy (nCC) |
Accuracy of intercept/marginal model (CCmarg) |
||
| LEC-5 1 | 2.16 | 0.70 | 0.14 | 0.65 |
| LEC-5 2 | 3.35 | 0.75 | 0.48 | 0.51 |
| LEC-5 3 | 2.22 | 0.78 | 0 | 0.78 |
| LEC-5 4 | 5.23 | 0.79 | 0.52 | 0.56 |
| LEC-5 5 | 4.39 | 0.88 | 0.49 | 0.76 |
| LEC-5 6 | 3.73 | 0.78 | 0.50 | 0.56 |
| LEC-5 7 | 5.01 | 0.82 | 0.51 | 0.63 |
| LEC-5 8 | 3.42 | 0.81 | 0.58 | 0.55 |
| LEC-5 9 | 3.45 | 0.82 | 0.63 | 0.52 |
| LEC-5 10 | 3.60 | 0.86 | 0.47 | 0.74 |
| LEC-5 11 | 5.30 | 0.91 | 0.49 | 0.83 |
| LEC-5 12 | 3.10 | 0.72 | 0.45 | 0.50 |
| LEC-5 13 | 5.34 | 0.83 | 0.46 | 0.68 |
| LEC-5 14 | 3.08 | 0.78 | 0.46 | 0.60 |
| LEC-5 15 | 4.16 | 0.78 | 0.47 | 0.59 |
| LEC-5 16 | 2.60 | 0.87 | 0.25 | 0.83 |
Note. LEC-5 is the Life Events Checklist for DSM-5; LEC-5 1 is natural disaster; LEC-5 2 is fire/explosion; LEC-5 3 is transportation accident; LEC-5 4 is serious accident at work/home/during recreational activity; LEC-5 5 is exposure to toxic substance; LEC-5 6 is physical assault; LEC-5 7 is assault with a weapon; LEC-5 8 is sexual assault; LEC-5 9 is other unwanted/uncomfortable sexual experience; LEC-5 10 is combat or exposure to war; LEC-5 11 is forced captivity; LEC-5 12 is life-threatening illness/injury; LEC-5 13 is severe human suffering; LEC-5 14 is sudden, violent death; LEC-5 15 sudden, accidental death; LEC-5 16 is serious injury/harm/death you caused to someone else.
PTE Type Clusters and Mental Health Correlates.
To account for multiple comparisons, we used Bonferroni corrections (.05/15) resulting in a p = .003 benchmark to detect significance (Huberty, 1999; Mulaik, Raju, & Harshman, 1997). See Table 4 for results of the multiple regression analyses. PTE Type Cluster 1 had near zero correlations with all dependent variables (ranging from −.03 to .09), whereas the other two PTE Type Clusters had medium to large correlations (.41 to .60) with the dependent variables. Therefore, in the regression equation, the near-zero relationships between PTE Type Cluster 1 and the dependent variables ended up as statistically non-significant negative relationships in each regression model. This relationship does not warrant substantive interpretation. PTE Type Cluster 2 was a statistically significant predictor of PTSD severity, depression severity, and negative emotion dysregulation, accounting for the influence of other PTE type clusters. PTE Type Cluster 3 was a statistically significant predictor of engagement in RSDBs and positive emotion dysregulation, accounting for the influence of other PTE type clusters.
Table 4.
Results of the regression analyses on relations between trauma type clusters and mental health correlates.
| B | SE | β | t | R2 | F | |
|---|---|---|---|---|---|---|
| Posttraumatic Stress Disorder Severity | ||||||
| Step 2 | .06 | 9.15p <.001 | ||||
| PTE Cluster 1 | −1.82 | .77 | −.14 | −2.35 p = .019 | ||
| PTE Cluster 2 | 3.67 | .96 | .23 | 3.83 p < .001 | ||
| PTE Cluster 3 | .85 | .55 | .10 | 1.54 p = .125 | ||
| Depression Severity | ||||||
| .06 | 8.09 p < .001 | |||||
| PTE Cluster 1 | −.55 | .25 | −.14 | −2.24 p = .025 | ||
| PTE Cluster 2 | 1.02 | .31 | .20 | 3.33 p = .001 | ||
| PTE Cluster 3 | .31 | .18 | .12 | 1.79 P = .075 | ||
| Engagement in Reckless and Self-Destructive Behaviors | ||||||
| .11 | 16.06 p < .001 | |||||
| PTE Cluster 1 | −.84 | .35 | −.14 | −2.43 p = .016 | ||
| PTE Cluster 2 | .92 | .43 | .12 | 2.14 p = .033 | ||
| PTE Cluster 3 | 1.17 | .25 | .31 | 4.73 p < .001 | ||
| Negative Emotion Dysregulation | ||||||
| .05 | 6.80 p < .001 | |||||
| PTE Cluster 1 | −1.33 | .61 | −.13 | −2.17 p = .03 | ||
| PTE Cluster 2 | 2.82 | .76 | .22 | 3.71 p <.001 | ||
| PTE Cluster 3 | .29 | .43 | .05 | 67 p = .502 | ||
| Positive Emotion Dysregulation | ||||||
| 6.48 p <.001 | ||||||
| PTE Cluster 1 | −.68 | .42 | −.10 | −1.64 p = .103 | ||
| PTE Cluster 2 | .03 | .51 | .003 | .06 p = .956 | ||
| PTE Cluster 3 | 1.13 | .30 | .26 | 3.82 p <.001 | ||
Note. PTE Type Cluster 1 - Accidental/Injury Traumas, PTE Type Cluster 2 - Victimization Traumas, PTE Type Cluster 3 - Predominant Death Threat Traumas; Bolded results are significant considering the p = .003 benchmark correcting for multiple comparisons.
Discussion
The current study identified clusters of PTE types assessed by the LEC-5 using network analyses and examined their differential relations with mental health correlates. Results provided support for a three-cluster LEC-5 model. Most clusters were differentiated in their relations to PTSD severity, depression severity, emotion dysregulation, and RSDBs, providing partial support for their construct validity. Our findings suggest the potential utility of these PTE type classifications for research and clinical practice.
Results provided support for three PTE type clusters characterized by (1) Accidental/Injury Traumas (e.g., fire, transportation accident); (2) Victimization Traumas (e.g., physical or sexual assault); and (3) Predominant Death Threat Traumas (e.g., sudden or violent death). These findings differ from Bae et al. (2008) who found support for six PTE type factors: physical assault/others, accident/injury, natural disaster/witnessing death, sexual abuse, criminal assault, and man-made disaster. Among explanations for these divergent results, to cluster PTE types, Bae et al. (2008) used a factor-analytical approach, whereas the current study used a more appropriate statistical tool of network analysis which overcomes limitations of applying a latent variable model approach to examining PTE type clusters. Further, Bae et al. (2008) used a translated (Korean) version of the LEC for DSM-IV within a Korean sample of psychiatric patients, whereas the current study used the original (English) version of the LEC-5 within a trauma-exposed community sample in the United States. Indeed, evidence supports cultural variation in PTEs types (e.g., exposure to genocide; Hinton & Lewis-Fernández, 2011), and the prevalence rates of some PTE types reported in the Bae et al. (2008) study varied considerably from those found in the current study (e.g., severe human suffering = 54.30% vs. 31.60%, respectively; physical assault = 82.90% vs. 55.90%, respectively). Further, clusters of PTE types may vary as a function of culture (e.g., individuals within war-affected countries may be more likely to report exposure to war and sexual victimization than individuals not affected by war; Foster & Brooks-Gunn, 2015). Additionally, differences in the obtained LEC clusters may relate to the clinical vs. non-clinical nature of the samples. Specifically, evidence suggests that certain PTE types (e.g., sexual victimization, combat exposure) are more strongly linked to clinically-relevant outcomes including PTSD and depression severity (Kilpatrick et al., 2013; Tracy, Morgenstern, Zivin, Aiello, & Galea, 2014). Future research is needed to validate this empirically-derived three-cluster LEC-5 model across diverse samples.
The most important network properties examined in this study were network communities/clusters of nodes, one-step expected influence (EI1) as a measure of node influence, and predictability values of nodes (Haslbeck & Waldorp, 2018; Jones et al., 2018; Robinaugh et al., 2016). In terms of what results of these network properties mean to our study, we found PTE type nodes to be clustered in three meaningful communities (elaborated above), perhaps, indicating that the experience of a certain PTE type may correlate with the experience of other PTE types within each cluster as supported by research indicating an increased likelihood of experiencing future victimization traumas after the experience of one victimization trauma (Coid et al., 2001). Reasons for such co-occurrence could be common vulnerability factors or certain characteristics (e.g., Breslau et al., 1995; Finkelhor, 2008); these need further exploration. Additionally, Predominant Death Threat Traumas had the highest EI1 estimates, indicating their dominant influence on other PTE types assessed by the LEC-5. Given positive EI1 estimates, the experience of Predominant Death Threat Traumas may increase the likelihood of experiencing other PTE types, and the lack of an experience of Predominant Death Threat Traumas may decrease the likelihood of experiencing other PTE types. Lastly, Victimization Traumas, in particular, were most predicted by the neighboring nodes in the network, with implications for remedial and preventive interventions. Victimization Traumas were predicted to a large extent by the PTE types connected to them (e.g., assault with a weapon; life-threatening illness/injury); thus, perhaps, intervening on and addressing the impacts of the PTE types connected to each of those Victimization Traumas may have beneficial impacts for preventing or dealing with Victimization Traumas (Haslbeck & Fried, 2012). Notably, all such network properties depend on the number and strength of edges of the neighboring nodes for a target node (Haslbeck & Fried, 2012). For instance, a node with many strong edges will have higher EI1 and predictability estimates and a well-defined/dense cluster with connected nodes; hence, this technique is data-driven and important to replicate with different samples to ascertain generalizability.
Notably, the three PTE type clusters had construct validity; they had differential relations with psychopathology symptom severity, engagement in RSDBs, and emotion dysregulation. Regarding psychopathology symptoms, PTE Type Cluster 2 (Victimization Traumas) was a significant predictor of PTSD and depression severity, accounting for the influence of other PTE type clusters. Results are consistent with empirical evidence indicating a detrimental psychological impact of interpersonal traumas including sexual/physical assault (Contractor, Caldas, et al., 2018). The strong association between victimization traumas and greater psychological harm relates to the intentional, purposeful nature of victimization and interpersonal traumas (Herman, 1992); victim’s sense of betrayal following these traumas (Freyd, 1994); shifts in beliefs regarding interpersonal loss and benevolence of others from pre- to post-trauma (Janoff-Bulman, 1992), and more frequent and intense trauma-related emotions post-trauma (Creamer, McFarlane, & Burgess, 2005). Indeed, such results are consistent with findings that PTE types within the Victimization Trauma Cluster (e.g., sexual assault) are associated with the highest conditional probabilities of clinically-relevant variables (e.g., PTSD; Breslau et al., 1998; Kilpatrick et al., 2013; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993).
Conversely, PTE Type Cluster 3 (Predominant Death Threat Traumas) was a significant predictor of engagement in RSDBs, accounting for the influence of other PTE type clusters. PTE Type Cluster 3 was most heterogenous compared to other clusters, and perhaps, specific PTE types within that cluster are driving the current study findings. For instance, combat exposure, which is one of the PTE types in this cluster, has been associated with an elevated likelihood of RSDBs, such as substance use (Larson, Wooten, Adams, & Merrick, 2012) and aggressive behaviors (Taft, Vogt, Marshall, Panuzio, & Niles, 2007). Alternatively, perhaps, the cumulative effect of multiple PTE types within this cluster may have influenced their relations to RSDBs, consistent with the building block effect (Kolassa et al., 2010; Schauer et al., 2003); this needs further empirical investigation.
Lastly, PTE Type Cluster 2 (Victimization Traumas) was a unique predictor of negative emotion dysregulation and PTE Type Cluster 3 (Predominant Death Threat Traumas) was a unique predictor of positive emotion dysregulation. To our knowledge, this is the first study to examine the impact of PTE type assessed via the LEC-5 on emotion dysregulation. The finding that negative emotion dysregulation was uniquely associated with Victimization Traumas is consistent with evidence indicating (1) associations between negative emotion dysregulation and the examined psychopathology correlates (Tull, Barrett, McMillan, & Roemer, 2007; Weiss, Tull, Anestis, & Gratz, 2013); (2) higher negative emotion dysregulation among individuals endorsing sexual and physical victimization (Weiss, Tull, Lavender, & Gratz, 2013); and (3) greater negative emotion dysregulation linked to early chronic interpersonal trauma compared to early single interpersonal trauma, late interpersonal trauma, and non-interpersonal trauma (Ehring & Quack, 2010). Evidence for the unique role of Predominant Death Threat Traumas on positive emotion dysregulation extends research in this area considering that emerging research has begun to link traumatic experiences and consequent post-trauma outcomes to positive emotion dysregulation (Weiss, Contractor, Forkus, Goncharenko, & Raudales, in press; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018). Perhaps, the potential interpersonal nature of many PTE types (e.g., combat exposure, violent or accidental death) captured with this cluster may be driving the obtained findings through the mechanisms mentioned above (e.g., intentional nature of the trauma, sense of betrayal, interpersonal loss; Freyd, 1994; Herman, 1992; Janoff-Bulman, 1992). Further, certain characteristics specific to combat experiences and learning about/witnessing death may explain the obtained findings, such as moral and ethical challenges embedded in those experiences (Litz et al., 2009); this needs further empirical investigation.
Results should be considered in the context of study limitations. First, the cross-sectional nature of the data precludes causal determination of relations among PTE type clusters and psychopathology correlates. Hence, prospective, longitudinal studies are needed. Second, collecting data via the internet (e.g., MTurk) has disadvantages that may limit generalizability of results. Concerns include sample biases because of self-selection (Kraut et al., 2004) and lack of control over the research environment with no opportunity to clarify questions (Kraut et al., 2004). Thus, we implemented steps to enhance data quality such as using validity checks, excluding individuals missing too much data, and excluding individuals attempting the survey multiple times (Aust, Diedenhofen, Ullrich, & Musch, 2013; Buhrmester, Kwang, & Gosling, 2011; Oppenheimer, Meyvis, & Davidenko, 2009). The drawback is that such steps resulted in sample truncation, notably though, the extent of our sample truncation (~47%) was comparable to other MTurk trauma studies (57%; van Stolk-Cooke et al., 2018). Future research may benefit from using other data enhancement and quality checks such as restricting participation to MTurk workers with a high reputation (Hauser, Paolacci, & Chandler, 2019; Peer, Vosgerau, & Acquisti, 2014).
Third, we note concerns specific to a network perspective to psychopathology. Specifically, evidence indicates concerns about replicability of network models, primarily for estimates of edges, most central nodes, and rank-order of node centrality attributed to measurement error of nodes (Forbes, Wright, Markon, & Krueger, 2017). Relatedly, this data-driven network methodology is specific to sample characteristics (Epskamp et al., 2018) including cultural and other contextual factors (Borsboom et al., 2019). Thus, replication in demographically and clinically diverse samples is needed to ascertain generalizability of the current study findings. Further, it is important to acknowledge contrasts between a network perspective vs. a latent variable approach to disorders in terms of their underlying premise of whether co-occurring symptoms interact dynamically to reflect a disorder vs. share a common underlying cause (the disorder itself; Borsboom & Cramer, 2013).
Fourth, we used the selected LEC-5 scoring method in the current study to be consistent with PTSD DSM-5 Criterion A (American Psychiatric Association, 2013). Additionally, while we acknowledge differential impacts of direct vs. indirect trauma exposure on psychopathology (Kim et al., 2009), other trauma characteristics beyond type/count such as age of exposure (Dunn, Nishimi, Powers, & Bradley, 2017) and trauma appraisal (Kucharska, 2017) may have additional variance in explaining relations of PTE type clusters to psychopathology. Lastly, we acknowledge concerns regarding the definition and measurement of PTSD DSM-5 Criterion A. Criterion A has been controversial since its inception (Breslau & Kessler, 2001; Kilpatrick, Resnick, & Acierno, 2009), resulting in several revisions across DSM versions. For DSM-5, significant revisions including the removal of the subjective component to the definition of trauma and broadening the definition of trauma to include PTEs experienced as part of one’s job (American Psychiatric Association, 2013; Brewin, Lanius, Novac, Schnyder, & Galea, 2009). Nonetheless, concerns regarding the definition and measurement of trauma persist (Larsen & Berenbaum, 2017; Stein, Wilmot, & Solomon, 2016). In fact, one recent study found that adding non-Criterion A traumas (i.e., attachment and collective identity) increased the incremental predictive validity of Criterion A (Kira et al., 2019). Thus, it appears that the definition of trauma will continue to evolve in response to empirical data, which is important to consider in the further examination of the current study’s research questions.
Despite these limitations, results of the current study advance our preliminary understanding of clusters of PTE types using the LEC-5. Specifically, we found empirical support for three PTE type clusters characterized by accidental/injury, victimization, and predominant death threat traumas. Moreover, these PTE type clusters were differentiated by clinically-relevant variables; Victimization Traumas were uniquely related to PTSD severity, depression severity, and negative emotion dysregulation; and Predominant Death Threat Traumas were uniquely related to RSDBs and positive emotion dysregulation. Broadly, while Predominant Death Threat Traumas were most influential in the network, Victimization Traumas were most predicted by connected PTE types. Regarding research implications, our results provide a framework for conceptualizing and measuring PTE types. Given the low base rates of some PTE types, these clusters, if replicated in future research, may spur additional research on the influence of PTE types on health behaviors. Moreover, they may promote comparisons of PTE types across studies and improve communication via common terminology among researchers and clinicians using the LEC-5. Clinically, our findings may inform trauma assessments to identify individuals at a higher risk for negative post-trauma outcomes. For instance, clinicians may benefit from assessing victimization and death threat PTE types, and intervening with individuals who endorse these traumas early in the therapeutic process to reduce detrimental health impacts. Relatedly, intervening on the impacts of traumas (e.g., being assaulted with a weapon) co-occurring with victimization traumas may help to reduce detrimental impacts and occurrence of victimization traumas; this is an empirical question worthy of future research. Additional empirical investigations would benefit from examining relations of these PTE type clusters to intervention outcomes using clinical trial data.
Supplementary Material
Funding:
The research described here was supported, in part, by the National Institute on Drug Abuse under Grant Number K23DA039327 awarded to the second author.
Footnotes
Of note, using a latent variable approach, almost similar clusters (i.e., latent variables) were obtained with Exploratory and Confirmatory Factor Analyses; Factor 1 (Accidental Traumas) - LEC-5 items 1 -5; Factor 2 (Injury/Death Traumas) - LEC-5 items 10-16; Factor 3 (Victimization Traumas) - LEC-5 items 6-9.
Contributor Information
Ateka A. Contractor, Department of Psychology, University of North Texas, Denton, TX, USA
Nicole H. Weiss, Department of Psychology, University of Rhode Island, Kingston, RI, USA
Prathiba Natesan, Department of Educational Psychology, University of North Texas, USA.
Jon D. Elhai, Department of Psychology, University of Toledo, OH, USA; Department of Psychiatry, University of Toledo, OH, USA
References
- Alcántara-Ayala I (2002). Geomorphology, natural hazards, vulnerability and prevention of natural disasters in developing countries. Geomorphology, 47, 107–124. doi: 10.1016/S0169-555X(02)00083-1 [DOI] [Google Scholar]
- Allen JG, Madan A, & Fowler JC (2015). Reliability and validity of the Stressful Life Events Screening Questionnaire among inpatients with severe neuropsychiatric illness. Bulletin of the Menninger Clinic, 79, 187–202. doi: 10.1521/bumc.2015.79.3.187 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Aust F, Diedenhofen B, Ullrich S, & Musch J (2013). Seriousness checks are useful to improve data validity in online research. Behavior Research Methods, 45, 527–535. doi: 10.3758/s13428-012-0265-2 [DOI] [PubMed] [Google Scholar]
- Bae H, Kim D, Koh H, Kim Y, & Park JS (2008). Psychometric properties of the life events checklist-Korean version. Psychiatry Investigation, 5, 163–167. doi: 10.4306/pi.2008.5.3.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjureberg J, Ljütsson B, Tull MT, Hedman E, Sahlin H, Lundh LG, … Gratz KL (2016). Development and Validation of a Brief Version of the Difficulties in Emotion Regulation Scale: The DERS-16. Journal of Psychopathology and Behavioral Assessment, 38, 284–296. doi: 10.1007/s10862-015-9514-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. doi: 10.1002/jts.2490080106 [DOI] [PubMed] [Google Scholar]
- Borsboom D (2017). A network theory of mental disorders. World Psychiatry, 16, 5–13. doi: 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, & Cramer AO (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. doi : 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ, & Kalis A (2019). Brain disorders? Not really: Why network structures block reductionism in psychopathology research. Behavioral and Brain Sciences, 42, 1–63. doi: 10.1017/S0140525X17002266 [DOI] [PubMed] [Google Scholar]
- Borsboom D, Cramer AOJ, Schmittmann VD, Epskamp S, & Waldorp LJ (2011). The small world of psychopathology. PLOS ONE, 6, e27407. doi: 10.1371/journal.pone.0027407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, & Andreski P (1995). Risk factors for PTSD-related traumatic events: A prospective analysis. The American Journal of Psychiatry, 152, 529–535. doi: 10.1176/ajp.152.4.529 [DOI] [PubMed] [Google Scholar]
- Breslau N, & Kessler RC (2001). The stressor criterion in DSM-IV posttraumatic stress disorder: An empirical investigation. Biological Psychiatry, 50, 699–704. doi: 10.1016/S0006-3223(01)01167-2 [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry, 55, 626–632. doi: 10.1001/archpsyc.55.7.626 [DOI] [PubMed] [Google Scholar]
- Brewin CR, Lanius RA, Novac A, Schnyder U, & Galea S (2009). Reformulating PTSD for DSM-V: Life after criterion A. Journal of Traumatic Stress, 22, 366–373. doi: 10.1002/jts.20443 [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon's Mechanical Turk a new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, 3–5. doi: 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Carlson EB, Smith SR, Palmieri PA, Dalenberg C, Ruzek JI, Kimerling R, … Spain DA (2011). Development and validation of a brief self-report measure of trauma exposure: The Trauma History Screen. Psychological Assessment, 23, 463–477. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, & Chen Z (2008). Extended Bayesian information criteria for model selection with large model spaces. Biometrika, 95, 759–771. doi: 10.1093/biomet/asn034 [DOI] [Google Scholar]
- Coid J, Petruckevitch A, Feder G, Chung WS, Richardson J, & Moorey S (2001). Relation between childhood sexual and physical abuse and risk of revictimisation in women: a cross-sectional survey. The Lancet, 358, 450–454. doi: 10.1016/S0140-6736(01)05622-7 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Brown LA, & Weiss NH (2018). Relation between lifespan polytrauma typologies and post-trauma mental health. Comprehensive Psychiatry, 80, 202–213. doi: 10.1016/j.comppsych.2017.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Caldas S, Fletcher S, Shea MT, & Armour C (2018). Empirically-derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74, 1137–1159. doi: 10.1002/jclp.22586 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Greene T, Dolan M, Weiss NH, & Armour C (2020). Relation between PTSD clusters and positive memory characteristics: A network perspective. Journal of Anxiety Disorders, 69. doi: 10.1016/j.janxdis.2019.102157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Dolan M, & Mota N (2019). Examination of the structural relations between PTSD symptoms and reckless/self-destructive behaviors. International Journal of Stress Management. doi : 10.1037/str0000133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Weiss NH, Kearns NT, Caldas S, & Dixon-Gordon K (in press). Assessment of posttraumatic stress disorder’s E2 criterion: Development, pilot testing, and validation of the Posttrauma Risky Behaviors Questionnaire. International Journal of Stress Management. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini G, Richetin J, Preti E, Casini E, Epskamp S, & Perugini M (2019). Stability and variability of personality networks. A tutorial on recent developments in network psychometrics. Personality and Individual Differences, 136, 68–78. doi: 10.1016/j.paid.2017.06.011 [DOI] [Google Scholar]
- Creamer M, McFarlane AC, & Burgess P (2005). Psychopathology following trauma: The role of subjective experience. Journal of Affective Disorders, 86, 175–182. doi: 10.1016/j.jad.2005.01.015 [DOI] [PubMed] [Google Scholar]
- Csardi G, & Nepusz T (2006). The igraph software package for complex network research. InterJournal. Retrieved from http://igraph.org. [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1, 16–29. doi: 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- Dalege J, Borsboom D, van Harreveld F, & van der Maas HL (2017). Network analysis on attitudes: A brief tutorial. Social Psychological and Personality Science, 8, 528–537. doi: 10.1177/1948550617709827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn EC, Nishimi K, Powers A, & Bradley B (2017). Is developmental timing of trauma exposure associated with depressive and post-traumatic stress disorder symptoms in adulthood? Journal of Psychiatric Research, 84, 119–127. doi: 10.1016/j.jpsychires.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, & Quack D (2010). Emotion regulation difficulties in trauma survivors: The role of trauma type and PTSD symptom severity. Behavior Therapy, 41, 587–598. doi: 10.1016/j.beth.2010.04.004 [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195–212. doi: 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer A, Waldorp L, Schmittmann VD, & Borsboom D (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48, 1–18. [Google Scholar]
- Finkelhor D (2008). Childhood victimization. New York, NY: Oxford University Press. [Google Scholar]
- Floyd FJ, & Widaman KF (1995). Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment, 7, 286–299. doi: 10.1037/1040-3590.7.3.286 [DOI] [Google Scholar]
- Forbes MK, Wright AG, Markon KE, & Krueger RF (2017). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology, 126, 969–988. doi: 10.1037/abn0000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster H, & Brooks-Gunn J (2015). Children's exposure to community and war violence and mental health in four African countries. Social Science & Medicine, 146, 292–299. doi: 10.1016/j.socscimed.2015.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier P, Anders S, Perera S, Tomich P, Tennen H, Park C, & Tashiro T (2009). Traumatic events among undergraduate students: Prevalence and associated symptoms. Journal of counseling psychology, 56, 450–460. doi: 10.1037/a0016412 [DOI] [Google Scholar]
- Freyd JJ (1994). Betrayal trauma: Traumatic amnesia as an adaptive response to childhood abuse. Ethics & Behavior, 4, 307–329. doi: 10.1207/s15327019eb0404_1 [DOI] [Google Scholar]
- Fried EI, van Borkulo CD, Cramer AO, Boschloo L, Schoevers RA, & Borsboom D (2017). Mental disorders as networks of problems: A review of recent insights. Social Psychiatry and Psychiatric Epidemiology, 52, 1–10. doi: 10.1007/s00127-016-1319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz CE (1961). Disasters. Harcourt, New York. [Google Scholar]
- Fruchterman TM, & Reingold EM (1991). Graph drawing by force-directed placement. Software: Practice and Experience, 21, 1129–1164. doi: 10.1002/spe.4380211102 [DOI] [Google Scholar]
- Gray CL, Litz BT, Hsu J, & Lombardo T (2004). Psychometric properties of the Life Events Checklist. Assessment, 11, 330–341. doi: 10.1177/1073191104269954 [DOI] [PubMed] [Google Scholar]
- Hair JF, Black WC, Babin BJ, & Anderson RE (2009). Multivariate Data Analysis (7th ed.). New York City, NY: Pearson. [Google Scholar]
- Hallion LS, Steinman SA, Tolin DF, & Diefenbach GJ (2018). Psychometric properties of the Difficulties in Emotion Regulation Scale (DERS) and its short forms in adults with emotional disorders. Frontiers in Psychology, 9, 539. doi: 10.3389/fpsyg.2018.00539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck JM, & Waldorp LJ (2018). How well do network models predict observations? On the importance of predictability in network models. . Behavior Research Methods, 50, 853–861. doi: 10.3758/s13428-017-0910-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haslbeck JMB, & Fried E (2012). How predictable are symptoms in psychopathological networks? A reanalysis of 18 published datasets. Psychological Medicine, 47, 2767–2776. doi: 10.1017/S0033291717001258 [DOI] [PubMed] [Google Scholar]
- Haslbeck JMB, & Waldorp LJ (2015). Structure estimation for mixed graphical models in high-dimensional data. arXiv preprint arXiv:1510.05677. [Google Scholar]
- Haslbeck JMB, & Waldorp LJ (2020). mgm: Structure estimation for time-varying mixed graphical models in high-dimensional data. Journal of Statistical Software. [Google Scholar]
- Hauser D, Paolacci G, & Chandler JJ (2019). Common concerns with MTurk as a participant pool: Evidence and solutions. New York, NY: Routledge. [Google Scholar]
- Herman JL (1992). Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress, 5, 377–391. doi: 10.1002/jts.2490050305 [DOI] [Google Scholar]
- Hevey D (2018). Network analysis: a brief overview and tutorial. Health Psychology and Behavioral Medicine, 6, 301–328. doi: 10.1080/21642850.2018.1521283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins DJ, & McCabe MP (2001). Multiple forms of child abuse and neglect: Adult retrospective reports. Aggression and Violent Behavior., 6, 547–578. doi: 10.1016/s1359-1789(00)00030-6 [DOI] [Google Scholar]
- Hinton DE, & Lewis-Fernández R (2011). The cross-cultural validity of posttraumatic stress disorder: Implications for DSM-5. Depression and Anxiety, 28, 783–801. doi: 10.1002/da.20753 [DOI] [PubMed] [Google Scholar]
- Hodgdon HB, Suvak M, Zinoviev DY, Liebman RE, Briggs EC, & Spinazzola J (2019). Network analysis of exposure to trauma and childhood adversities in a clinical sample of youth. Psychological Assessment, 31, 1294–1306. doi: 10.1037/pas0000748 [DOI] [PubMed] [Google Scholar]
- Hooper LM, Stockton P, Krupnick JL, & Green BL (2011). Development, use, and psychometric properties of the Trauma History Questionnaire. Journal of Loss and Trauma, 16, 258–283. doi: 10.1080/15325024.2011.572035 [DOI] [Google Scholar]
- Huberty CJ (1999). On some history regarding statistical testing,. In Thompson B (Ed.), Advances in Social Science Methodology (Vol. 5, pp. 1–23). Stamford: JAI Press. [Google Scholar]
- IBM Corp. (2017). IBM SPSS Statistics for Windows, Version 25.0. . Armonk, NY: IBM Corp. [Google Scholar]
- Janoff-Bulman R (1992). Shattered assumptions: Toward a new psychology of trauma. New York, NY: Free Press. [Google Scholar]
- Jones P (2018). Networktools: Tools for identifying important nodes in networks R package version 1.1.1. Retrieved from https://CRAN.R-project.org/package=networktools [Google Scholar]
- Jones PJ, Mair P, & McNally RJ (2018). Visualizing psychological networks: A tutorial in R. Frontiers in Psychology, 9, 1742. doi: 10.3389/fpsyg.2018.01742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, & Acierno R (2009). Should PTSD criterion A be retained? Journal of Traumatic Stress, 22, 374–383. doi: 10.1002/jts.20436 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. doi: 10.1002/jts.21848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim BN, Kim JW, Kim HW, Shin MS, Cho SC, Choi NH, … Yun MJ (2009). A 6-month follow-up study of posttraumatic stress and anxiety/depressive symptoms in Korean children after direct or indirect exposure to a single incident of trauma. The Journal of clinical psychiatry, 70, 1148–1154. doi: 10.4088/jcp.08m04896 [DOI] [PubMed] [Google Scholar]
- Kira I, Fawzi M, Shuwiekh H, Lewandowski L, Ashby J, & Al Ibraheem B (2019). Do adding attachment, oppression, cumulative and proliferation trauma dynamics to PTSD Criterion "A" improve its predictive validity: Toward a paradigm shift? Current Psychology, doi: 10.1007/s12144-019-00206-z [DOI] [Google Scholar]
- Kira I, Lewandowski L, Somers CL, Yoon JS, & Chiodo L (2012). The effects of trauma types, cumulative trauma, and PTSD on IQ in two highly traumatized adolescent groups. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 128–139. doi: 10.1037/a0022121 [DOI] [Google Scholar]
- Kolassa IT, Ertl V, Eckart C, Kolassa S, Onyut LP, & Elbert T (2010). Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychological Trauma Theory Research Practice and Policy, 2, 169–174. doi: 10.1037/a0019362 [DOI] [Google Scholar]
- Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, & Couper M (2004). Psychological research online: Report of Board of Scientific Affairs' Advisory Group on the Conduct of Research on the Internet. American Psychologist, 59, 105–117. doi: 10.1037/0003-066X.59.2.105 [DOI] [PubMed] [Google Scholar]
- Kroenke K, & Spitzer RL (2002). The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals, 32, 509–515. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ 9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharska J (2017). Sex differences in the appraisal of traumatic events and psychopathology. Psychological Trauma: Theory, Research, Practice, and Policy, 9, 575–582. doi: 10.1037/tra0000244 [DOI] [PubMed] [Google Scholar]
- Larsen SE, & Berenbaum H (2017). Did the DSM-5 improve the traumatic stressor criterion? Association of DSM-IV and DSM-5 criterion A with posttraumatic stress disorder symptoms. . Psychopathology, 50, 373–378. doi: 10.1159/000481950 [DOI] [PubMed] [Google Scholar]
- Larson MJ, Wooten NR, Adams RS, & Merrick EL (2012). Military combat deployments and substance use: Review and future directions. Journal of Social Work Practice in the Addictions, 12, 6–27. doi: 10.1080/1533256X.2012.647586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Contractor AA, Rhodes C, Dondaville KA, Jordan AH, Resick PA, … Peterson AL (2018). Distinct trauma types in military service members seeking treatment for posttraumatic stress disorder. Journal of Traumatic Stress, 31, 286–295. doi : 10.1002/jts.22276. [DOI] [PubMed] [Google Scholar]
- Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, & Maguen S (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29, 695–706. doi: 10.1016/j.cpr.2009.07.003 [DOI] [PubMed] [Google Scholar]
- Luz MP, Mendlowicz M, Marques-Portella C, Gleiser S, Berger W, Neylan TC, … Figueira I (2011). PTSD criterion A1 events: A literature-based categorization. Journal of Traumatic Stress, 24, 243–251. doi: 10.1002/jts.20633 [DOI] [PubMed] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. doi: 10.1037/a0028085 [DOI] [PubMed] [Google Scholar]
- Mulaik SA, Raju NS, & Harshman RA (1997). There is a time and place for significance testing. In Harlow LL, Mulaik SA, & Steiger JH (Eds.), What if there were no Significance Tests? (pp. 65– 115). Mahwah, N. J.: Erlbaum. [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, 867–872. doi: 10.1016/j.jesp.2009.03.009 [DOI] [Google Scholar]
- Peer E, Vosgerau J, & Acquisti A (2014). Reputation as a sufficient condition for data quality on Amazon Mechanical Turk. Behavior Research Methods, 46, 1023–1031. doi: 10.3758/s13428-013-0434-y [DOI] [PubMed] [Google Scholar]
- Pons P, & Latapy M (2005). Computing communities in large networks using random walks. In Yolum P, Güngör T, Gürgen F, & Ö zturan C (Eds.), Computer and information sciences—ISCIS (pp. 284–293). Berlin, Germany: Springer. [Google Scholar]
- Prins A, Bovin MJ, Kimerling R, Kaloupek DG, Marx BP, Pless Kaiser A, & Schnurr PP (2015). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov. Retrieved from http://www.ptsd.va.gov/professional/assessment/screens/pc-ptsd.asp [Google Scholar]
- Read JP, Ouimette P, White J, Colder C, & Farrow S (2011). Rates of DSM-IV-TR trauma exposure and posttraumatic stress disorder among newly matriculated college students. Psychological Trauma: Theory, Research, Practice, and Policy, 3, 148–156. doi: 10.1037/a0021260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, & Best CL (1993). Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology, 61, 984–991. doi: 10.1037/0022-006X.61.6.984 [DOI] [PubMed] [Google Scholar]
- Robinaugh DJ, Millner AJ, & McNally RJ (2016). Identifying highly influential nodes in the complicated grief network. Journal of Abnormal Psychology, 125, 747–757. doi: 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santiago PN, Ursano RJ, Gray CL, Pynoos RS, Spiegel D, Lewis-Fernandez R, … Fullerton CS, (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLOS ONE, 8, e59236. doi: 10.1371/journal.pone.0059236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schauer M, Neuner F, Karunakara U, Klaschik C, Robert C, & Elbert T (2003). PTSD and the building block effect of psychological trauma among West Nile Africans. European Society for Traumatic Stress Studies Bulletin, 10, 5–6. [Google Scholar]
- Sijbrandij M, Engelhard IM, de Vries GJ, Luitse JS, Carlier IV, Gersons BP, & Olff M (2013). The role of injury and trauma-related variables in the onset and course of symptoms of posttraumatic stress disorder. Journal of Clinical Psychology in Medical Settings, 20, 449–455. doi: 10.1007/s10880-012-9348-6 [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Penninx BW, Hickendorff M, van Hemert AM, Bernstein DP, & Elzinga BM (2014). Childhood Trauma Questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychological Assessment, 26, 717–729. doi : 10.1037/pas0000002 [DOI] [PubMed] [Google Scholar]
- Stein JY, Wilmot DV, & Solomon Z (2016). Does one size fit all? Nosological, clinical, and scientific implications of variations in PTSD Criterion A. Journal of Anxiety Disorders, 43, 106–117. doi: 10.1016/j.janxdis.2016.07.001 [DOI] [PubMed] [Google Scholar]
- Taft CT, Vogt DS, Marshall AD, Panuzio J, & Niles BL (2007). Aggression among combat veterans: Rationships with combat exposure and symptoms of posttraumatic stress disorder, dysphoria, and anxiety. Journal of Traumatic Stress, 20, 135–145. doi: 10.1002/jts.20197 [DOI] [PubMed] [Google Scholar]
- Thomas KA, & Clifford S (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Computers in Human Behavior, 77, 184–197. doi: 10.1016/j.chb.2017.08.038 [DOI] [Google Scholar]
- Tracy M, Morgenstern H, Zivin K, Aiello AE, & Galea S (2014). Traumatic event exposure and depression severity over time: Results from a prospective cohort study in an urban area. Social Psychiatry and Psychiatric Epidemiology, 49, 1769–1782. doi: 10.1007/s00127-014-0884-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, & Roemer L (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38, 303–313. doi: 10.1016/j.beth.2006.10.001 [DOI] [PubMed] [Google Scholar]
- van Borkulo CD, Borsboom D, Epskamp S, Blanken TF, Boschloo L, Schoevers RA, & Waldorp LJ (2014). A new method for constructing networks from binary data. Scientific Reports, 4, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M (2018). Crowdsourcing trauma: Psychopathology in a trauma-exposed sample recruited via Mechanical Turk. Journal of Traumatic Stress, 31, 549–557. doi: 10.1002/jts.22303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrana S, & Lauterbach D (1994). Prevalence of traumatic events and post-traumatic psychological symptoms in a nonclinical sample of college students. Journal of Traumatic Stress, 7, 289–302. doi: 10.1007/BF02102949 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weiss NH, Contractor AA, Forkus SR, Goncharenko S, & Raudales AM (in press). Positive emotion dysregulation among community individuals: The role of traumatic exposure and posttraumatic stress disorder. Journal of Traumatic Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Contractor AA, Raudales AM, Greene T, & Short NA (2020). Extending our understanding of the association between posttraumatic stress disorder and positive emotion dysregulation: A network analysis approach. Journal of Anxiety Disorders, 7. doi: 10.1016/j.janxdis.2020.102198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Darosh AG, Contractor AA, Schick MM, & Dixon-Gordon KL (2019). Confirmatory validation of the factor structure and psychometric properties of the Difficulties in Emotion Regulation Scale – Positive. Journal of Clinical Psychology, 75, 1267–1287. doi: 10.1002/jclp.22768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31, 775–780. doi: 10.1002/jts.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender JM (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-positive. Behavior Modification, 39, 431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128, 45–51. doi: 10.1016/j.drugalcdep.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Lavender J, & Gratz KL (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37, 944–954. doi: 10.1016/j.chiabu.2013.03.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


