Abstract
Background
Children with sickle cell anemia (SCA) are at increased risk of acute kidney injury (AKI) that may lead to death or chronic kidney disease. This study evaluated AKI prevalence and risk factors in children with SCA hospitalized with a vaso-occlusive crisis (VOC) in a low-resource setting. Further, we evaluated whether modifications to the Kidney Disease: Improving Global Outcomes (KDIGO) definition would influence clinical outcomes of AKI in children with SCA hospitalized with a VOC.
Methods
We prospectively enrolled 185 children from 2 – 18 years of age with SCA (Hemoglobin SS) hospitalized with a VOC at a tertiary hospital in Uganda. Kidney function was assessed on admission, 24–48 h of hospitalization, and day 7 or discharge. Creatinine was measured enzymatically using an isotype-dilution mass spectrometry traceable method. AKI was defined using the original-KDIGO definition as ≥ 1.5-fold change in creatinine within seven days or an absolute change of ≥ 0.3 mg/dl within 48 h. The SCA modified-KDIGO (sKDIGO) definition excluded children with a 1.5-fold change in creatinine from 0.2 mg/dL to 0.3 mg/dL.
Results
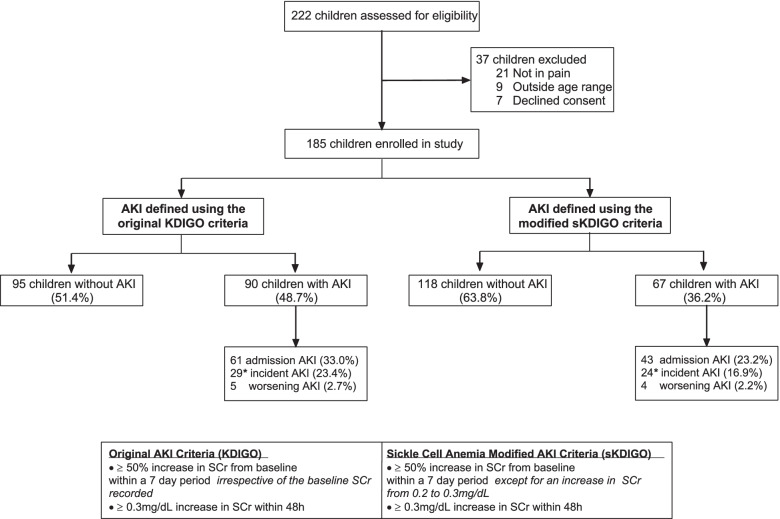
Using KDIGO, 90/185 (48.7%) children had AKI with 61/185 (33.0%) AKI cases present on admission, and 29/124 (23.4%) cases of incident AKI. Overall, 23 children with AKI had a 1.5-fold increase in creatinine from 0.2 mg/dL to 0.3 m/dL. Using the sKDIGO-definition, 67/185 (36.2%) children had AKI with 43/185 (23.2%) cases on admission, and 24/142 (16.9%) cases of incident AKI. The sKDIGO definition, but not the original-KDIGO definition, was associated with increased mortality (0.9% vs. 7.5%, p = 0.024). Using logistic regression, AKI risk factors included age (aOR, 1.10, 95% CI 1.10, 1.20), hypovolemia (aOR, 2.98, 95% CI 1.08, 8.23), tender hepatomegaly (aOR, 2.46, 95% CI 1.05, 5.81), and infection (aOR, 2.63, 95% CI 1.19, 5.81) (p < 0.05).
Conclusion
These results demonstrate that AKI is a common complication in children with SCA admitted with VOC. The sKDIGO definition of AKI in children with SCA was a better predictor of clinical outcomes in children. There is need for promotion of targeted interventions to ensure early identification and treatment of AKI in children with SCA.
Keywords: Sickle cell anemia, Acute kidney injury, Children, Sub-Saharan Africa, Vaso-occlusive crises, Malaria, Infection, Hemoglobinuria, Cystatin C, Serum creatinine
Background
Sickle cell anemia (SCA) is an inherited hemoglobinopathy that disproportionately impacts children in sub-Saharan Africa. Globally, 300,000 children are born with SCA annually with 80% of affected children residing in Africa [1, 2]. Vaso-occlusive pain crises (VOC) are a common complication in children with SCA [3] and a risk factor for AKI with an estimated 2.5–17% of children hospitalized with a VOC developing AKI in high-income countries (HIC) [4–7]. Risk factors for AKI in children with VOC include hypovolemia, and exposure to nephrotoxic medications, including non-steroidal anti-inflammatory drugs for pain management and aminoglycosides for the management of suspected infections [8, 9]. However, there are limited data on AKI prevalence, risk factors and outcomes in children with SCA and VOC in LMIC.
AKI is a sudden change in kidney function denoted by either a change in serum creatinine or urine output. AKI is defined as a 1.5-fold increase in serum creatinine from estimated baseline, a 0.3 mg/dL increase in serum creatinine (SCr) over 48 h, or a decrease in urine output according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [10]. Children with SCA have underlying abnormalities in kidney function including hyperfiltration [11], resulting in baseline SCr levels that are lower than expected for age. This makes defining AKI challenging in this population and raises questions about whether a 1.5-fold increase in SCr is clinically relevant in populations with low baseline SCr.
To address these questions, we conducted a prospective observational study of children with SCA hospitalized with a VOC. We hypothesized that modifications to the KDIGO definition in the context of a population of children with SCA and low baseline SCr levels would be associated with more clinically meaningful changes in AKI outcomes. The primary objective of this study was to define AKI prevalence and risk factors in children with SCA hospitalized with a VOC. Our secondary objective was to evaluate differences in AKI biomarkers (Cystatin C) and outcomes in children with the original and sickle cell modified KDIGO definition.
Materials and methods
Study design and setting
Between January and August in 2019, children admitted to Mulago National Referral Hospital with SCA and VOC were screened for eligibility. Eligible children were prospectively recruited in a hospital-based study to define AKI prevalence, risk factors, and outcomes. Inclusion criteria were hospital admission, documented SCA by hemoglobin electrophoresis, age 2 to 18 years, a pain score ≥ 2 using an age-specific pain scale, and a willingness to complete study procedures. Pain in children aged 2–3 years was assessed using the face, legs, activity, cry, and consolability (FLACC) scale [12], the Wong-Baker Faces pain scale in children 3–7 years of age, and the numeric pain scale in children ≥ 8 years [13].
Children were recruited from the paediatric emergency unit that admits an average of 3 children daily with SCA and VOC. Most of the children admitted with VOC also attend the hospital's dedicated sickle cell clinic that provides medical care to approximately 1400 children per year. Routine care includes malaria prophylaxis using sulfadoxine-pyrimethamine, daily folic acid, and penicillin V for children < 5 years of age. Only a small proportion of children receive hydroxyurea.
The sample size was calculated using the formula , where; z = standard normal variate corresponding to the 95% confidence interval and is 1.96, d = the required precision of the estimate (0.05), p = prevalence rate [14]. The sample size was calculated based on previous studies indicating AKI prevalence of 2.3%, 6.9%, and 13% among children with SCA and VOC [6], generating a sample size of 173.
Study procedures
After informed consent and enrolment, all children had a complete history and physical examination conducted by a study doctor to assess medication use, signs of infection, the site and severity of pain. Blood pressure was calculated as the mean of three independent measurements and hypertension was defined as a systolic blood pressure > 95% percentile and/or a diastolic blood pressure > 95% for children < 13 years of age or a systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 80 mmHg for children 13 years of age or older [15]. Liver size was evaluated by abdominal palpation below the subcostal margin and defined as: i) no hepatomegaly, liver not palpable; ii) hepatomegaly, liver palpable below the costal margin; iii) tender hepatomegaly, tenderness on palpation of the liver. A spot urine sample was collected from each recruited child for dipstick urinalysis, urine microscopy, assessment of urine albumin and urine creatinine. Microalbuminuria was defined as urine albumin-to-creatinine ratio of 3-30 mg/mmol and macroalbuminuria as urine albumin-to-creatinine ratio, > 30 mg/mmol.
Children were assessed for symptoms, signs of infection and had a complete blood count and malaria evaluation by Giemsa microscopy. Sepsis was defined using International paediatric sepsis consensus guidelines [16] based on two or more of the following criteria, one of which must be abnormal temperature > 38.5 °C or < 36 °C: age-specific tachycardia, age-specific tachypnea, or leukocytosis. We used age-specific thresholds for leukocytosis in children with SCA [17]. We categorised children as having hypovolemia if they were unable to drink or breastfeed, had diarrhea or vomiting, were hypotensive, or capillary refill time > 3 s (features of dehydration). Children were diagnosed with a urinary tract infection based on a positive nitrite or leukocyte test by urinalysis in a child with a history of fever. An acute infection was defined by the presence of sepsis, malaria or urinary tract infection. Microbiology to culture blood or urine samples was not feasible.
Measurement of Cystatin C
Cystatin C— a biomarker of glomerular filtration [6] — was measured on cryopreserved serum using an ELISA correlated to the reference standard (Catalog # ERM-DA471/IFCC) with a slope of 1.07 and R2 value of 0.998 (Quantikine® immunoassay, R&D Systems, Minneapolis, MN) [18]. The assay has been evaluated for matrix effects using samples from apparently healthy donors with a mean (SD) of 0.79 mg/L (1.6) for serum and 0.77 mg/L (1.6) for EDTA plasma [18]. On each plate pooled serum samples were tested in duplicate alongside a commercial control (QC23: Quantikine Immunoassay Control Group 8, R&D Systems, Minneapolis, MN). Laboratory technicians were blinded to participant details.
Assessment of kidney function
AKI was defined based on the Kidney Disease: Improving Global Outcomes (KDIGO) guidelines as an increase in SCr of ≥ 0.3 mg/dl within 48 h or a 50% increase in baseline creatinine within 7 days [10]. Daily 24 h urine output was not quantified over hospitalization. SCr was assessed in whole blood on enrolment, at 24–48 h, and day 7 or discharge (whichever happened earlier) using iSTAT CHEM8 + cartridges (Abbott Point of Care Inc., Princeton, NJ). This approach of SCr measurement uses an enzymatic assay with values traceable to the U.S. National Institute of Standards and Technology (NIST) standard reference material SRM909, with a reportable range of 0.20–20.0 mg/dL. To define AKI, SCr values below the reportable range were assigned a value of 0.19 mg/dL. Each participant’s lowest measured creatinine, or the nadir, was taken as the baseline SCr for AKI determination. None of the patients had a known baseline creatinine prior to hospitalization. As SCA is a risk factor for kidney disease, population-based estimates of baseline serum creatinine would be inaccurate in this patient population. In instances where a child had only a single creatinine measure (n = 7), the Pottel height-independent GFR estimating equation was used to back-calculate baseline creatinine, assuming a normal GFR of 120 mL/min per 1.73m2 [19, 20].
Using the KDIGO guidelines, AKI was staged based on creatinine fold change from the nadir to the maximum, where: stage 1 included a 1.5- <2.0-fold change in creatinine from baseline or a ≥ 0.3 mg/dl increase in creatinine within 48 h; stage 2, 2– <3.0-fold change in serum creatinine from baseline; stage 3, ≥3.0-fold change in creatinine from baseline, or an increase in creatinine to ≥ 4.0 mg/dl, or an eGFR ≤ 35 ml/min per 1.73 m2. AKI was assessed in two ways: using the original KDIGO definition and using a sickle cell anemia modified KDIGO definition (sKDIGO). The point-of-care i-STAT system reports creatinine in 0.1 mg/dL increments so a one-unit change in creatinine from 0.2 to 0.3 mg/L constituted AKI using the KDIGO definition. In the sKDIGO definition, children with a nadir creatinine of 0.2 mg/dL with 1.5-fold increase to 0.3 mg/dL were excluded from the AKI definition. The eGFR was calculated using the CKiD creatinine and Cystatin C based formulae [21]: creatinine, eGFR = (0.413*height)/SCr; Cystatin C, eGFR = 70.69 *(Serum Cystatin C)−0.931; SCr & Cystatin C, eGFR = 39.8*((height/SCr)0.456)*((1.8/Cystatin C)0.418)* ((30/bun) 0.079)*(1.076male) *((height/1.4)0.179).
Statistical analysis
Data was analysed using STATA v14.0 (StataCorp) and GraphPad Prism v7.03. Data was summarised descriptively using median and interquartile range (IQR) for continuous variables and the number and frequency for discrete variables. Differences between continuous variables and AKI status were assessed using the Wilcoxon rank-sum test or a non-parametric test of trend across stages of AKI. Differences between categorical variables were analysed using the Pearson’s Chi-square test or Fisher’s exact test, as appropriate. To identify risk factors for AKI we used logistic regression and computed unadjusted and adjusted odds ratios. Variables were considered for inclusion in the multivariable models based on an a priori hypothesized relationship or a p < 0.20 in bivariate analysis. Age and sex were included in all models.
Results
Characteristics of the study population
A total of 185 children with SCA and VOC were enrolled into the study (Fig. 1). The median age was 8.9 years (IQR, 5.9—11.8) and 41.6% of participants were female (Table 1). The prevalence of undernutrition was high with 30.8% of children stunted (height-for-age z score < –2), 25.9% underweight (weight-for-age z score < -2), and 29.7% wasted (weight-for-height z score or BMI-for-age z score < -2). Of the 185 children enrolled, 24 (13.0%) children had a history of stroke, and 78 (42.2%) had been hospitalized in the previous six months (Table 1). The majority (70.3%) of children had severe anemia with a hemoglobin < 8 g/dL and 38 (20.5%) children had evidence of an acute infection defined as sepsis (n = 19, 10.3%), malaria (n = 17, 9.6%), or urinary tract infection (n = 4, 2.2%). Six (3.2%) of the participants died during hospitalization and all deaths occurred in female participants (mortality, 7.8%).
Fig. 1.
Flow chart of study population. AKI was defined in children according to the original KDIGO definition or a modified definition (sKDIGO) where children with a 1.5-fold increase in serum creatinine (SCr) from 0.2 to 0.3 mg/dL was not considered AKI. AKI status was defined as admission AKI if a child met criteria for AKI using the admission SCr based on the nadir SCr measured over hospitalization or incident AKI in children whom did not have AKI on admission but developed it over hospitalization. When assessing the incidence of AKI over hospitalization, children with AKI present on admission were excluded from the denominator. *Children with a maximum AKI stage higher than the admission AKI stage were considered to have worsening AKI
Table 1.
Demographic and clinical characteristics of the participants
| N (% missing) | Study population (n = 185) | |
|---|---|---|
| Demographics | ||
| Age, years, median (IQR) | 185 (0.0) | 8.9 (5.9, 11.8) |
| Age categories, n (%) | ||
| < 5 years | 185 (0.0) | 36 (19.5) |
| 5–10 years | 73 (39.5) | |
| > 10 years | 76 (41.1) | |
| Sex, n (%) Female | 185 (0.0) | 77 (41.6) |
| Height-for-age z score | 184 (0.1) | -1.36 (-2.28, -0.40) |
| Weight-for-age z scorea | 112 (39.5) | -1.47 (-2.04, -0.47) |
| Weight-for-height z scorea | 38 (79.5) | -1.59 (-2.19, -0.39) |
| BMI-for-age z scorea | 149 (19.5) | -1.31(-2.26, -0.40) |
| HIV infection, n (%) | 185 (0.0) | 1 (0.5) |
| Routine Medication Use | ||
| Folic acid, n (%) | 185 (0.0) | 117 (63.2) |
| Hydroxyurea, n (%) | 185 (0.0) | 61 (33.0) |
| Penicillin V prophylaxis, n (%) | 185 (0.0) | 11 (6.0) |
| Children < 5 years of age | 36 (0.0) | 5 (13.9) |
| Medical History | ||
| Hospital admission past 6 months, n (%) | 185 (0.0) | 78 (42.2) |
| Prior transfusion, n (%) | 185 (0.0) | 140 (75.7) |
| History of stroke, n (%) | 185 (0.0) | 24 (13) |
| Clinical characteristics on admission | ||
| Fever, n (%) | 185 (0.0) | 64 (34.6) |
| Heart rate, bpm | 185 (0.0) | 108 (98, 121) |
| Blood pressure category, n (%) | ||
| Hypotensive | 185 (0.0) | 2 (1.1) |
| Normotensive | 149 (80.5) | |
| Hypertension | 31 (18.4) | |
| Diarrhea, n (%) | 185 (0.0) | 4 (2.2) |
| Vomiting, n (%) | 185 (0.0) | 13 (7.0) |
| Unable to drink/breastfeed, n (%) | 185 (0.0) | 8 (4.3) |
| Severe anemia, Hemoglobin < 8.0 g/dL, n (%) | 185 (0.0) | 130 (70.3) |
| Splenomegaly, n (%) | 179 (3.2) | 18 (9.7) |
| Liver assessment | ||
| No hepatomegaly | 185 (0.0) | 107 (57.8) |
| Hepatomegaly | 40 (21.6) | |
| Tender Hepatomegaly | 38 (20.5) | |
| History of reduced urine output, n (%) | 185 (0.0) | 15 (8.1) |
| History of tea coloured urine, n (%) | 185 (0.0) | 79 (42.7) |
| Laboratory findings | ||
| WBC × 103/μL | 185 (0.0) | 22.6 (16.7, 33.4) |
| Neutrophil count × 103/μL | 185 (0.0) | 12.1 (8.3, 17.2) |
| Hemoglobin, g/dL | 185 (0.0) | 7.3 (6.3, 8.3) |
| Platelet count × 109/L | 185 (0.0) | 418 (306, 525) |
| Sepsis, n (%) | 185 (0.0) | 19 (10.3) |
| Malaria, n (%) | 177 (4.3) | 17 (9.6) |
| Urinary tract infection, n (%) | 182 (1.6) | 4 (2.2) |
| Acute infection, n (%) | 185 (0.0) | 38 (20.5) |
| Kidney Function | ||
| Creatinine, mg/dL | 185 (0.0) | 0.3 (0.19, 0.4) |
| Urine albumin to creatinine ratio, n (%) | ||
| < 3 mg/mmol | 175 (5.4) | 105 (60.0) |
| 3–30 mg/mmol | 55 (31.4) | |
| > 30 mg/mmol | 15 (8.6) | |
| Admission eGFR, mL/min per 1.73m2 | ||
| CKiD SCr equation | 184 (0.1) | 184 (139, 227) |
| CKiD Cystatin C equation | 184 (0.1) | 86 (68, 107) |
| CKiD SCr + Cystatin C equation | 184 (0.1) | 133 (104, 160) |
| Outcome | ||
| In-hospital mortality, n (%) | 185 (0.0) | 6 (3.2) |
Data presented as median (IQR) or n (%)
a Weight-for-age available for children ≤ 10 years of age (n = 113); weight-for-height for children < 5 years or age, BMI-for-age for children ≥ 5 years of age (WHO standards, 2009)
The median duration of pain prior to admission was 3 days. The reported locations of pain included the lower limbs (64.9%), abdomen (41.6%), upper limbs (30.3%), back (29.7%), chest (34.6%) and others (3.8%). Analgesia use for children included paracetamol (93.0%), morphine (86.0%), ibuprofen (83.8%), diclophenac (10.3%), codeine (2.2%) and tramadol (1.1%).
Prevalence of AKI in children with SCA
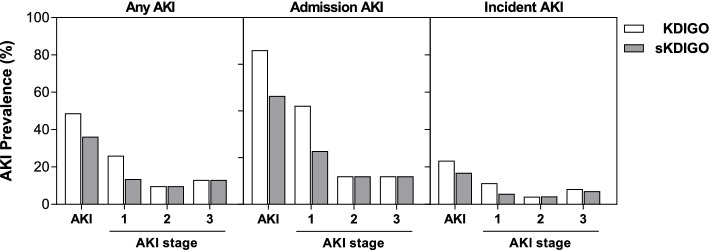
Overall, 90/185 (48.7%) children had AKI using the KDIGO definition with the majority of AKI cases occurring on admission 61/90 (67.8%) while 34/90 (37.8%) children had incident or worsening AKI over hospitalization (Fig. 2). In children with AKI, 23/90 (25.6%) of cases occurred in children with a baseline creatinine of 0.2 mg/dL that increased to 0.3 mg/dL over hospitalization. Using the sKDIGO definition, 67/185 (36.2%) children had AKI with 26 cases diagnosed based on a 0.3 mg/dL increase in creatinine within 48 h and 41 cases based on a fold increase in creatinine over 7 days; 43/67(64.2%) had AKI on admission and 28/67 (41.8%) developed incident or worsening AKI during hospitalization (Fig. 2). There were no relationships between medication use and AKI (p > 0.05 for all).
Fig. 2.
AKI prevalence and stage based on KDIGO or sKDIGO definition. The prevalence of AKI and AKI stage over hospitalization (any AKI), admission, and incident AKI (developed in-hospital). Creatinine was measured on admission, 24–48 h of hospitalization, and discharge or day 7 (whichever happened earlier). For sKDIGO definition children with a 50% increase in creatinine from a baseline measure of 0.2 mg/dL were not considered to have AKI
Comparison of laboratory findings and clinical outcomes based on KDIGO or sKDIGO definition of AKI
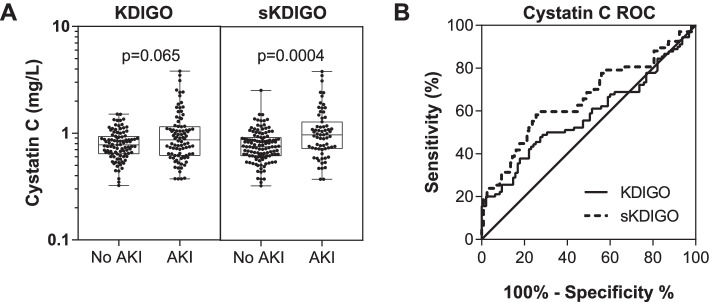
We evaluated the relationship between both AKI definitions and clinical chemistries and urinalysis results (Table 2). Overall, differences in laboratory parameters were larger in children who had AKI defined using sKDIGO definition compared to KDIGO (Table 2). We further evaluated the KDIGO and sKDIGO definition using Cystatin C, an alternative marker of GFR (Fig. 3). Cystatin C was only elevated in children meeting the sKDIGO definition of AKI (p < 0.001).
Table 2.
Laboratory findings in children based on acute kidney injury definition
|
KDIGO ≥ 50% from baseline (nadir) or 0.3 mg/dL increase in SCr |
asKDIGO ≥ 50% from baseline (nadir, excluding 0.2 mg/dL to 0.3md/dL) or 0.3 mg/dL increase in SCr |
|||||
|---|---|---|---|---|---|---|
| No AKI (n = 95) | AKI (n = 90) | P value | No AKI (n = 118) | AKI (n = 67) | P value | |
| Laboratory Findings | ||||||
| WBC × 103/μL | 22.2 (16.2, 32.4) | 24.3 (16.7, 39.2) | 0.5257 | 20.1 (15.4, 30.3) | 25.5 (18.2, 46.7) | 0.0072 |
| Hemoglobin, g/dL | 7.4 (6.4, 8.3) | 7.1 (6.1, 8.0) | 0.3362 | 7.4 (6.5, 8.4) | 6.9 (5.9, 7.7) | 0.0068 |
| Neutrophil count × 103/μL | 11.4 (8.2, 16.4) | 13.4 (8.4, 19.2) | 0.2577 | 11.3 (8.0, 16.2) | 14.3 (8.9, 20.4) | 0.0143 |
| Platelet count × 103/μL | 439 (334, 560) | 387 (282, 505) | 0.0361 | 435 (330, 557) | 382 (265, 488) | 0.0529 |
| BUN, mg/dL | 3 (3, 4) | 5 (3, 9) | < 0.0001 | 3 (3, 4) | 6 (3, 11) | < 0.0001 |
| Liver function | ||||||
| Aspartate transaminase (AST) | 43.0 (33.0, 68.0) | 65 (39.8, 120.0) | 0.0001 | 43.5 (33.0, 70.0) | 67 (48, 148) | < 0.0001 |
| Alkaline phosphatase (ALP) | 207 (171, 256) | 247 (170, 321) | 0.0360 | 211 (165, 255) | 254 (183, 337) | 0.0049 |
| Gamma glutamyl transpeptidase (GGT), IU/L | 29 (17.2, 49.2) | 35.2 (23.6, 74.5) | 0.0418 | 27.7 (16.5, 49.1) | 40.4 (25.3, 82.0) | 0.0007 |
| Albumin, mg/dL | 39.7 (35.8, 43.2) | 38.6 (33.7, 42.5) | 0.1361 | 39.7 (35.9, 43.3) | 37.8 (32.9, 42.0) | 0.0323 |
| Total bilirubin, mg/dL | 1.7 (1.0, 2.9) | 2.5 (1.1, 4.6) | 0.0224 | 1.6 (0.9, 2.8) | 3.1 (1.3, 5.1) | 0.0008 |
| Conjugated bilirubin, mg/dL | 0.6 (0.5, 1.0) | 0.8 (0.5, 2.6) | 0.0445 | 0.6 (0.5, 1.0) | 1.1 (0.5, 3.9) | 0.0008 |
| Creatinine measures | ||||||
| Admission SCr, mg/dL | 0.2 (0.19, 0.3) | 0.3 (0.3, 0.5) | < 0.0001 | 0.2 (0.19, 0.3) | 0.4 (0.3, 0.6) | < 0.0001 |
| Maximum SCr, mg/dL | 0.2 (0.19, 0.3) | 0.4 (0.3, 1.0) | < 0.0001 | 0.2 (0.2, 0.3) | 0.6 (0.3, 1.5) | < 0.0001 |
| Minimum SCr, mg/dL | 0.19 (0.19, 0.3) | 0.2 (0.19, 0.3) | 0.0087 | 0.2 (0.19, 0.3) | 0.2 (0.19, 0.4) | 0.0543 |
| Urinalysis | ||||||
| uAlbumin:uCr ratio, mg/mmol | 1.8 (0.7, 6.5) | 2.1 (0.8, 15.1) | 0.2706 | 1.4 (0.7, 3.9) | 3.1 (0.9, 23.1) | 0.0034 |
| Albumin-to-creatinine ratio, n (%) | ||||||
| < 3 mg/mmol | 54 (60.0) | 51 (60.0) | 0.607 | 74 (66.7) | 31 (48.4) | 0.030 |
| 3–30 mg/mmol | 30 (33.3) | 25 (29.4) | 31 (27.9) | 24 (37.5) | ||
| > 30 mg/mmol | 6 (6.7) | 9 (10.6) | 6 (5.4) | 9 (14.1) | ||
| Hematuria by dipstick, n (%) | 4 (4.2) | 10 (11.1) | 0.076 | 4 (3.4) | 10 (14.9) | 0.009 |
| Proteinuria by dipstick, n (%) | 8 (8.4) | 20 (22.2) | 0.009 | 9 (7.6) | 19 (28.4) | < 0.001 |
| Bilirubinuria by dipstick, n (%) | 3 (3.2) | 13 (14.4) | 0.006 | 3 (2.5) | 13 (19.4) | 0.001 |
Continuous data presented as median (IQR) and analyzed using the Wilcoxon rank sum test
Categorical data analyzed using Pearson’s Chi square test or Fisher’s exact test (if n < 5 per cell)
aChildren with a baseline creatinine of 0.2 mg/dL with a 50% increase in creatinine to 0.3 mg/dL were not considered to have AKI
Fig. 3.
Comparison of Cystatin C levels based on the KDIGO AKI definition. A Box and whisker plots showing the median (interquartile range) and range of serum Cystatin C with the individual data points overlaid. Differences between groups were compared using Wilcoxon rank-sum test with the p values presented on the graphs. B Receiver operating characteristic (ROC) curve to measure the association between the biomarker level and AKI status. Serum Cystatin C had a higher area under the receiver operating characteristic (ROC) curve (AUROC) using sKDIGO compared to KDIGO
Finally, we compared outcomes in children based on AKI status. AKI was associated with increased mortality using sKDIGO (mortality, 0.9% no AKI vs. 7.5% AKI, p = 0.024) but not the original-KDIGO definition (mortality, no AKI, 1.1% vs. 5.6% AKI, p = 0.110). AKI on admission was not associated with increased mortality. Rather, children who developed incident AKI in-hospital or those with worsening AKI had increased mortality (p < 0.05 for both). As the sKDIGO definitions was a better predictor of mortality, subsequent analyses evaluating risk factors for AKI and AKI progression are conducted using sKDIGO.
Risk factors for AKI in children with SCA and VOC
In order to improve recognition of AKI in children with SCA who require hospitalization, we evaluated differences in the demographic characteristics, signs and symptoms on admission and laboratory findings in children with AKI (Table 3). As 43/67 (64.2%) children had AKI on admission to hospital, we are unable to attribute causality to these risk factors. However, understanding risk factors in this high-risk population may enable clinicians to identify features that raise their index of suspicion minimizing exposure to potential nephrotoxic agents and prioritizing monitoring in children at highest risk of AKI. Using logistic regression, AKI risk factors included age (aOR, 1.10, 95% CI 1.01, 1.20), hypovolemia (aOR, 2.98, 95% CI 1.08, 8.24), tender hepatomegaly (aOR, 2.46, 95% CI 1.05, 5.77), and an acute infection (aOR, 2.63, 95% CI 1.19, 5.81) (p < 0.05).
Table 3.
Risk factors for AKI in children admitted to hospital for a vaso-occlusive crisis (sKDIGO)
| Bivariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| No AKI (n = 118) | AKI* (n = 67) | OR (95% CI) | P value | aOR (95% CI) | P value | |
| Demographics and Clinical Characteristics | ||||||
| Age, years, median (IQR) | 8.0 95.1, 11.3) | 10 (7.3, 12.4) | 1.11 (1.03–1.20) | 0.010 | 1.10 (1.10, 1.20) | 0.022 |
| Age categories, n (%) | ||||||
| < 5 years | 28 (23.7) | 8 (11.9) | 1 (reference) | |||
| 5–10 years | 47 39.8) | 26 (38.8) | 1.94 (0.77–4.86) | 0.159 | ||
| > 10 years | 43 (36.4) | 33 (49.3) | 2.69 (1.08–6.65) | 0.033 | ||
| Sex, n (%) Female | 42 (35.6) | 35 (52.2) | 1.98 (1.08–3.64) | 0.028 | 1.74 (0.88, 3.45 | 0.110 |
| Height-for-age z score | -1.2 (-2.1, -0.3) | -1.7 (-2.6, -1.0) | 0.8 (0.64–0.99) | 0.044 | ||
| Blood pressure category, n (%) | ||||||
| Hypotensive | 1 (0.9) | 1 (1.5) | 1.81 (0.11–29.55) | 0.677 | ||
| Normotensive (reference) | 96 (81.4) | 53 (79.1) | 1 (reference) | –- | ||
| Hypertensive | 21 (17.8) | 13 (19.4) | 1.12 (0.52–2.42) | 0.770 | ||
| Diarrhea, n (%) | 1 (0.9) | 3 (4.5) | 5.48 (0.56–53.81) | 0.144 | ||
| Vomiting, n (%) | 5 (4.2) | 8 (11.9) | 3.06 (0.96–9.78) | 0.059 | ||
| Unable to drink/breastfeed, n (%) | 1 (0.9) | 7 (10.5) | 13.65 (1.64–113.52) | 0.016 | ||
| Hypovolemia (%) | 8 (6.8) | 16 (23.9) | 4.31 (1.73–10.73) | 0.002 | 2.98 (1.08, 8.23) | 0.035 |
| Severe anemia, hemoglobin < 8.0 g/dL, n (%) | 77 (65.3) | 54 (80.6) | 2.21 (1.08–4.52) | 0.029 | ||
| Splenomegaly, n (%) | 9 (7.6) | 9 (13.4) | 1.88 (0.70–4.99) | 0.208 | ||
| No hepatomegaly | 77 (65.3) | 30 (44.8) | 1 (reference) | –- | 1 (reference) | –- |
| Hepatomegaly | 24 (20.3) | 16 (23.9) | 1.71 (0.80–3.66) | 0.166 | 1.57 (0.69, 3.59) | 0.281 |
| Tender hepatomegaly | 17 (14.4) | 21 (31.3) | 3.17 (1.73–6.82) | 0.003 | 2.46 (1.05, 5.77) | 0.038 |
| History of reduced urine output, n (%) | 8 (6.8) | 7 (10.5) | 1.60 (0.55–4.63) | 0.383 | ||
| History of tea coloured urine, n (%) | 41 (34.8) | 38 (56.7) | 2.46 (1.33–4.55) | 0.004 | 1.63 (0.83, 3.22) | 0.157 |
| Laboratory Findings | ||||||
| WBC × 103/μL | 20.1 (15.4, 30.3) | 25.5 (18.2, 46.7) | 1.01 (1.002–1.026) | 0.015 | ||
| Neutrophil count × 103/μL | 11.3 (8.0, 16.2) | 14.3 (8.9, 20.4) | 1.04 (1.004–1.072) | 0.029 | ||
| Hemoglobin, g/dL | 7.4 (6.5, 8.4) | 6.9 (5.9, 7.7) | 0.79 (0.65–0.97) | 0.022 | ||
| Platelet count × 103/μL | 435 (330, 557) | 382 (265, 488) | 1.00 (1.00–1.00) | 0.079 | ||
| Sepsis, n (%) | 9 (7.6) | 10 (14.9) | 2.12 (0.82–5.52) | 0.122 | ||
| Malaria, n (%) | 7 (6.3) | 10 (15.2) | 2.65 (0.96–7.35) | 0.061 | ||
| Urinary tract infection, n (%) | 1 (0.9) | 3 (4.6) | 5.48 (0.56–53.74) | 0.145 | ||
| Acute infection, n (%) | 17 (14.4) | 21 (31.3) | 2.71 (1.31–5.62) | 0.007 | 2.63 (1.19, 5.81) | 0.017 |
| Urine ACR, n (%) | ||||||
| < 3 mg/mmol | 74 (66.7) | 31 (48.4) | 1 (reference) | –- | ||
| 3–30 mg/mmol | 31 (27.9) | 24 (37.5) | 1.85 (0.94–3.64) | 0.076 | ||
| > 30 mg/mmol | 6 (5.4) | 9 (14.1) | 3.58 (1.17–10.92) | 0.025 | ||
Variables in the multivariate analysis included age, sex, hypovolemia, hepatomegaly, reported history of tea coloured urine, and an acute infection
Risk factors for AKI on admission and worsening or incident AKI during hospitalization
To determine risk factors in children with community-acquired AKI versus hospital-acquired or worsening AKI, we stratified analyses based on the timing of diagnosis (Table 4). Children with community-acquired AKI were older, were more likely to have tea coloured urine, and hepatomegaly or tender hepatomegaly. In addition, AKI on admission was associated with hypovolemia and an acute infection and laboratory findings consistent with an acute inflammatory event. In contrast, participants with incident or worsening AKI over hospitalization were similar in age, with comparable frequencies of infection and similar laboratory findings. There were no differences in nephrotoxic medications use in children with incident or worsening AKI (Table 4). Participants who developed incident or worsening AKI were more likely to be female.
Table 4.
Risk factors of AKI on admission and incident or worsening AKI using sKDIGO
| Admission AKI | Incident or worsening AKI | ||||||
|---|---|---|---|---|---|---|---|
| No AKI (n = 142) | AKI (n = 43) | P value | No AKI (n = 118) | AKI (n = 28) | P value | ||
| Demographics and Clinical Characteristics | |||||||
| Age, years, median (IQR) | 8.3 (5.1, 11.4) | 10.3 (7.3, 12.3) | 0.021 | 8.0 (5.1, 11.3) | 9.6 (5.6, 13.0) | 0.264 | |
| Sex, n (%) Female | 57 (40.1) | 20 (46.5) | 0.458 | 42 (35.6) | 17 (60.7) | 0.015 | |
| Blood pressure category, n (%) | |||||||
| Hypotensive | 1 (0.7) | 1 (2.3) | 0.441 | 1 (0.9) | 0 (0.0) | 1.000 | |
| Normotensive (reference) | 116 (81.7) | 33 (76.7) | 96 (81.4) | 23 (82.1) | |||
| Hypertensive | 25 (17.6) | 9 (20.9) | 21 (17.8) | 5 (17.9) | |||
| Diarrhea, n (%) | 2 (1.4) | 2 (4.7) | 0.231 | 1 (0.9) | 1 (3.6) | 0.348 | |
| Vomiting, n (%) | 8 (5.6) | 5 (11.6) | 0.178 | 5 (4.2) | 3 (10.7) | 0.180 | |
| Unable to drink/breastfeed, n (%) | 2 (1.4) | 6 (14.0) | 0.002 | 1 (0.9) | 1 (3.6) | 0.348 | |
| Hypovolemia, n (%) | 13 (9.2) | 11 (25.6) | 0.005 | 8 (6.8) | 5 (17.9) | 0.064 | |
| Splenomegaly, n (%) | 13 (9.2) | 5 (11.6) | 0.733 | 9 (7.6) | 5 (17.9) | 0.252 | |
| No hepatomegaly | 92 (64.8) | 15 (34.9) | 0.001 | 77 (65.3) | 16 (57.1) | 0.620 | |
| Hepatomegaly | 28 (19.7) | 12 (27.9) | 24 (20.3) | 6 (21.4) | |||
| Tender Hepatomegaly | 22 (15.5) | 16 (37.2) | 17 (14.4) | 6 (21.4) | |||
| History of reduce urine output, n (%) | 9 (6.3) | 6 (14.0) | 0.109 | 8 (6.8) | 1 (3.6) | 1.000 | |
| History of tea coloured urine, n (%) | 53 (37.3) | 26 (60.5) | 0.007 | 41 (34.8) | 14 (50.0) | 0.134 | |
| Nephrotoxic medication use in hospital | |||||||
| Ibuprofen, n (%) | 120 (84.5) | 35 (81.4) | 0.628 | 99 (83.9) | 24 (85.7) | 0.813 | |
| Diclophenac, n (%) | 16 (11.3) | 3 (7.0) | 0.571 | 15 (12.7) | 2 (7.1) | 0.528 | |
| Gentamicin, n (%) | 0 (0.0) | 1 (2.3) | 0.232 | 0 (0.0) | 0 (0.0) | –- | |
| Laboratory Findings | |||||||
| WBC × 103/μL | 21.0 (15.5, 30.2) | 30.8 (19.3, 51.8) | 0.0002 | 20.1 (15.4, 30.3) | 21.7 (15.5, 30.2) | 0.980 | |
| Neutrophil count × 103/μL | 11.4 (8.0, 16.2) | 16.1 (10.5, 25.3) | 0.001 | 11.3 (8.0, 16.2) | 12.2 (8.0, 16.9) | 0.585 | |
| Hemoglobin, g/dL | 7.4 (6.5, 8.4) | 6.2 (5.6, 7.4) | < 0.0001 | 7.4 (6.5, 8.4) | 7.5 (7.0, 8.6) | 0.388 | |
| Platelet count × 103/μL | 434 (330. 557) | 372 (251, 449) | 0.0140 | 435 (330, 557) | 422 (302, 570) | 0.831 | |
| Sepsis5, n (%) | 12 (8.5) | 7 (16.3) | 0.138 | 9 (7.6) | 3 (10.7) | 0.701 | |
| Malaria, n (%) | 9 (6.7) | 8 (19.1) | 0.017 | 7 (6.3) | 3 (10.7) | 0.421 | |
| Urinary tract infection, n (%) | 1 (0.7) | 3 (7.1) | 0.039 | 1 (0.9) | 0 | 1.000 | |
| Acute infection, n (%) | 22 (15.5) | 16 (37.2) | 0.002 | 17 (14.4) | 6 (21.4) | 0.359 | |
| Hematuria, n (%) | 5 (3.5) | 9 (20.9) | < 0.001 | 4 (3.4) | 2 (7.1) | 0.324 | |
| Proteinuria, n (%) | 14 (9.9) | 14 (32.6) | < 0.001 | 9 (7.6) | 5 (17.9) | 0.098 | |
| Bilirubinuria, n (%) | 9 (6.3) | 7 (16.3) | 0.042 | 3 (2.5) | 6 (21.4) | 0.002 | |
| Pain characteristics | |||||||
| Pain Score, median (IQR) | 6 (4,8) | 6 (4, 8) | 0.242 | 6 (4,8) | 6 (4,8) | 0.755 | |
| Duration of pain in days | 3 (2,4) | 3 (2,6) | 0.126 | 3 (2,4) | 3 (2, 5) | 0.978 | |
Discussion
While AKI is a recognised clinical complication of VOC in children with SCA [8], there is a paucity of prospective studies evaluating the incidence of AKI in children with SCA from LMIC. In this study we used the KDIGO consensus guidelines to define AKI in children with SCA presenting with VOC, using serial creatinine measures over hospitalization. Given the percentage of children that had low creatinine values as a result of hyperfiltration and undernutrition, we also considered sKDIGO definition. Overall, the sKDIGO was associated with higher mortality compared to the original KDIGO definition. Risk factors of AKI on admission included older age, an acute infection, tender hepatomegaly, hypovolemia and tea coloured urine.
SCA is associated with a number of kidney abnormalities including hyperfiltration, papillary necrosis, glomerulosclerosis and chronic kidney disease, which collectively may predispose people living with SCA to AKI [8]. Using sKDIGO, 36.2% of participants had AKI with 13.5% stage 1, 9.7% stage 2 and 13.0% stage 3. The prevalence of AKI in the present study is higher than previous studies that reported an AKI prevalence between 2.5% to 17% in children hospitalised with VOC [4–7]. However, these studies were largely conducted in high income countries. Children with SCA in LMICs may have additional risk factors that affect a child’s risk of developing AKI during hospitalization [9], including endemic infections like malaria that contribute to substantial AKI in Ugandan children [22–24]. The majority of AKI in this study was community-acquired AKI and consistent with global trends of increased community-acquired AKI in LMIC [25].
AKI on admission was associated with being unable to drink or breastfeed, vomiting and diarrhea, which are risk factors for hypovolemia and pre-renal AKI. Infections may increase AKI risk by exacerbating dehydration and hypovolemia through increased insensible losses secondary to fever. Infections— especially malaria and sepsis— are common in children with SCA in LMICs and contribute significant morbidity and mortality in these children [9]. Malaria and sepsis are well-established risk factors for AKI [23, 26] that can exacerbate microvascular dysfunction in VOCs as endothelial activation can lead to microvascular dysfunction, inflammation, and the release of endogenous nephrotoxins like cell-free hemoglobin and free heme that increase oxidative stress and contribute to tubular injury [27–31]. Infections are a risk factor for VOC in children with SCA thus enhanced infection prevention may reduce the burden of SCA-related complications including AKI. Further, as children with SCA receive routine clinical follow-up through the sickle cell clinic, education on preventing dehydration and counselling on how to adequately manage pain and fever at home while minimizing exposure to nephrotoxic agents like non-steroidal anti-inflammatory drugs may reduce the burden of community-acquired AKI.
In the present study all study deaths occurred in females with a history of passing tea coloured urine (a feature of hemoglobinuria), and being female was associated with the development of incident or worsening AKI. Additional studies are needed to understand social and biological determinants of health in this population. There was a trend of increased hemoglobinuria in females (49.4%) compared to males (35.9%). In addition to being a risk factor for mortality, hemoglobinuria was also a risk factor for AKI on admission. Hemoglobinuria is a common complication in children with SCA associated with ongoing hemolysis and is associated with progression to chronic kidney disease (CKD) [32]. Although the etiology of hemoglobinuria in children presenting with AKI maybe attributed to ongoing hemolysis, there are reports of a rising incidence of hemoglobinuria (blackwater fever) in Uganda [33, 34]. Blackwater fever often occurs in children with anemia and a history of malaria infection and is a known risk factor for AKI in severe malaria [35–37] and is associated with increased post-discharge morbidity and mortality [34].
AKI is defined by reduced urine output or an increase in serum creatinine. In the context of this study AKI was defined based on serum creatinine alone, as data on urine output was not available. It is challenging to define AKI in children with SCA as glomerular hyperfiltration and increased tubular secretion of creatinine affect serum creatinine levels [8]. Further, creatinine is affected by non-renal factors like muscle wasting [38–40]. Undernutrition was common in the study with 29.7% of the population wasted. As the pre-morbid baseline creatinine was not known in the study population, we employed the participants’ individual trajectory. Increased access to creatinine testing and more routine creatinine testing in children with SCA would enable more precise classification of AKI in children during acute infections or VOC. In this study Cystatin C was elevated in children with AKI highlighting that AKI is associated with both functional changes in filtration as well as tubular injury [41]. Additional research is needed to evaluate alternative biomarkers of AKI in children with SCA.
This study evaluated AKI during a single hospital admission for a VOC. However, children often have multiple occurrences of VOC annually [42, 43]. Currently, the Uganda clinical guidelines recommend initiation of hydroxyurea in children with frequent VOC (> 5 episodes per year). In the NOHARM trial, 308 VOC were recorded in 88 participants over one year [17]. With a prevalence rate of AKI of 36.2% in children evaluated for a single episode of VOC, children with SCA are at risk of repeated AKI episodes. In a large hospital-based study of Black Americans, multiple pain crises annually were associated with a faster decline in glomerular filtration rates (GFR) compared to patients with SCA without frequent pain crises [44]. AKI is an established risk factor for development of CKD [45–48]. Further, individuals living with CKD are at increased risk of AKI, which may further accelerate progression of the CKD [49]. This study highlights the need for further studies to evaluate the incidence of AKI over several years in children with SCA to understand how AKI affects the development of CKD in LMIC where the majority of children with SCA reside. This information will be important to guide the development of guidelines on clinical follow-up of children at risk of CKD following AKI.
Albuminuria is a risk factor for CKD [50–52] and 20% of study participants had an albumin-to-creatinine ratio > 30 mg/mmol suggestive of glomerular damage [49]. SCA is associated with an early age of CKD onset and a faster decline in GFR [44, 53]. In the present study, 54.6% of children < 5 years of age had albuminuria with 45.5% microalbuminuria and 9.1% macroalbuminuria. This is higher than in an ongoing study following 2582 participants > 3 years of age with SCA across four West African countries, where the prevalence of micro- and macroalbuminuria was 29% and 5% respectively (median age of 14 years) [54]. Additional studies are needed to assess the prevalence of albuminuria in children with SCA in steady state to determine the appropriate age to start screening for albuminuria. There is need for early identification of CKD, appropriate clinical management, and earlier referral to specialist kidney services that could have a measurable improvement on child health and quality of life.
One of the limitations of the study was a lack of steady state SCr measurement to estimate baseline serum creatinine which reflects limitations in routine SCr measurements in the setting. We assessed SCr at pre-specified time points to coincide with the KDIGO definition of AKI and did not have daily SCr measurements or measurements beyond 7 days, which may have resulted in missed AKI episodes over hospitalization. Further, a recent prospective multi-national study (AWARE) assessing AKI in critically ill children in 32 pediatric intensive care units across five continents found AKI defined using SCr alone, failed to identify AKI in 67% of children with low urine output [55]. In this study AKI was defined on the basis of serum creatinine alone and thus AKI may be underestimated as we did not assess urine output. Further studies are needed with broader definitions of AKI such as additional use of urine output to define AKI as well as longer follow up periods to evaluate incident AKI over hospitalization, persistence of the kidney injury and kidney recovery. Recognition and validation of AKI risk factors may facilitate identification of children likely to benefit from creatinine testing and targeted interventions to promote kidney recovery.
This study has several strengths including its prospective design and the serial evaluation of creatinine over hospitalization. By using a participant’s individual trajectory of SCr over hospitalization to define AKI, we avoid misclassifying children with pre-existing chronic kidney disease as having AKI based on population estimates of baseline SCr. There are few prospective studies on AKI in children with SCA in LMIC and this study adds to the existing literature on the complications of SCA in children. In addition, this study included a number of clinical laboratory evaluations and assessed biomarkers of AKI which allowed us to evaluate the utility of different definitions to define AKI. Our study highlights the need for more targeted programs aimed at prevention and management of both community-acquired and hospital-acquired AKI in LMICs.
Conclusion
Our study demonstrates that AKI is a frequent complication of hospitalized children with SCA and highlights the need for a heightened index of suspicion in children admitted with a VOC irrespective of pain severity. Modified KDIGO guidelines (sKDIGO) that excluded an increase from 0.2 to 0.3 as a 1.5-fold increase in SCr correlated better with biomarkers of acute kidney injury and mortality than standard KDIGO AKI guidelines, highlighting the importance of accounting for the hyperfiltration that occurs in children with SCA when defining AKI. The study builds on existing literature on complications of SCA in LMICs and demonstrates that a significant proportion of the AKI is community-acquired. There is thus need for interventions aimed at prevention and management of AKI in children with SCA especially during VOC which are often recurrent. Simple steps including prompt rehydration in children unable to tolerate oral fluids or with fluid loss as a result of diarrhea or vomiting may reduce AKI progression, and in this high risk population, nephrotoxic medications for pain management should be used judiciously.
Acknowledgements
We are grateful to the children and their caretakers who participated in the study. We are grateful to the medical officers, nurses, laboratory team and all staff who were involved in this study and provided support to the study activities.
Abbreviations
- AKI
Acute kidney injury
- AOR
Adjusted odds ratio
- CI
Confidence interval
- eGFR
Estimated glomerular filtration rate
- FLACC
Face, legs, activity, cry, and consolability
- IDMS
Isotope dilution mass spectrometry
- IQR
Interquartile range
- KDIGO
Kidney Disease: Improving Global Outcomes
- SCA
Sickle cell anemia
- SCr
Serum creatinine
- LMIC
Low and middle income countries
- NSAIDS
Non-steroidal anti-inflammatory drugs
- UTI
Urinary tract infection
- VOC
Vaso-occlusive crises
Authors’ contributions
AB and ALC conceptualised and designed the study with input from SK, RK, EIM and CCJ. Data analysis and interpretation was conducted by AB, ALC, SM and JS with input from SK, RK, JL, EIM, ROO, CCJ, MS. All authors provided input into the writing and editing of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by Grant Number D43TW010132 supported by Office of the Director, National Institutes of Health (OD), National Institute of Dental & Craniofacial Research (NIDCR), National Institute of Neurological Disorders and Stroke (NINDS), National Heart, Lung, and Blood Institute (NHLBI), Fogarty International Center (FIC), National Institute on Minority Health and Health Disparities (NIMHD). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the supporting offices. The study was also supported by Grant number 1R25TW011213 (Fogarty International Center of the National Institutes of Health, U.S. Department of State’s Office of the U.S. Global AIDS Coordinator and Health Diplomacy (S/GAC), and President’s Emergency Plan for AIDS Relief, PEPFAR). This study was also supported by the Fogarty International Center (FIC) of the National Institutes of Health and the National Heart, Lung, and Blood Institute (NHLBI) under grant #D43TW009345 awarded to the Northern Pacific Global Health Fellows Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Written informed consent was obtained from parents or legal guardians of all study participants, and assent was obtained for children 8 years of age and older. The study was approved by the Institutional Review Board at Makerere University School of Biomedical Sciences Research and Ethics Committee (IRB number SBS-S46) and the Uganda National Council for Science and Technology (approval number; HS 2443). All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chakravorty S, Williams TN. Sickle cell disease: a neglected chronic disease of increasing global health importance. Arch Dis Child. 2015;100(1):48–53. doi: 10.1136/archdischild-2013-303773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McGann PT, Hernandez AG, Ware RE. Sickle cell anemia in sub-Saharan Africa: advancing the clinical paradigm through partnerships and research. Blood. 2017;129(2):155–161. doi: 10.1182/blood-2016-09-702324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tshilolo L, Tomlinson G, Williams TN, Santos B, Olupot-Olupot P, Lane A, Aygun B, Stuber SE, Latham TS, McGann PT. Hydroxyurea for children with sickle cell anemia in sub-Saharan Africa. N Engl J Med. 2019;380(2):121–131. doi: 10.1056/NEJMoa1813598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormick M, Richardson T, Warady BA, Novelli EM, Kalpatthi R. Acute kidney injury in paediatric patients with sickle cell disease is associated with increased morbidity and resource utilization. Br J Haematol. 2020;189(3):559–565. doi: 10.1111/bjh.16384. [DOI] [PubMed] [Google Scholar]
- 5.Baddam S, Aban I, Hilliard L, Howard T, Askenazi D, Lebensburger JD. Acute kidney injury during a pediatric sickle cell vaso-occlusive pain crisis. Pediatric Nephrol. 2017;32:1–6. doi: 10.1007/s00467-017-3623-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Audard V, Homs S, Habibi A, Galacteros F, Bartolucci P, Godeau B, Renaud B, Levy Y, Grimbert P, Lang P, et al. Acute kidney injury in sickle patients with painful crisis or acute chest syndrome and its relation to pulmonary hypertension. Nephrol Dial Transplant. 2010;25(8):2524–2529. doi: 10.1093/ndt/gfq083. [DOI] [PubMed] [Google Scholar]
- 7.Lebensburger JD, Palabindela P, Howard TH, Feig DI, Aban I, Askenazi DJ. Prevalence of acute kidney injury during pediatric admissions for acute chest syndrome. Pediatr Nephrol. 2016;31(8):1363–1368. doi: 10.1007/s00467-016-3370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nath KA, Hebbel RP. Sickle cell disease: renal manifestations and mechanisms. Nat Rev Nephrol. 2015;11(3):161–171. doi: 10.1038/nrneph.2015.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Serjeant G, Ndugwa C. Sickle cell disease in Uganda: a time for action. East Afr Med J. 2003;80(7):384–387. doi: 10.4314/eamj.v80i7.8724. [DOI] [PubMed] [Google Scholar]
- 10.KDIGO KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1):1–138. [Google Scholar]
- 11.Scheinman JI. Sickle cell disease and the kidney. Nat Clin Pract Nephrol. 2009;5(2):78–88. doi: 10.1038/ncpneph1008. [DOI] [PubMed] [Google Scholar]
- 12.Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19(1):55–61. doi: 10.4037/ajcc2010624. [DOI] [PubMed] [Google Scholar]
- 13.Young KD. Assessment of acute pain in children. Clinical Pediatric Emergency Medicine. 2017;18(4):235–241. [Google Scholar]
- 14.Wiegand H. Kish, L.: Survey Sampling. John Wiley & Sons, Inc., New York, London 1965. Biom Z. 1968;10(1):88–89. [Google Scholar]
- 15.Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, de Ferranti SD, Dionne JM, Falkner B, Flinn SK. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904. doi: 10.1542/peds.2017-1904. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8. doi: 10.1097/01.PCC.0000149131.72248.E6. [DOI] [PubMed] [Google Scholar]
- 17.Opoka RO, Ndugwa CM, Latham TS, Lane A, Hume HA, Kasirye P, Hodges JS, Ware RE, John CC. Novel use Of Hydroxyurea in an African Region with Malaria (NOHARM): a trial for children with sickle cell anemia. Blood. 2017;130(24):2585–2593. doi: 10.1182/blood-2017-06-788935. [DOI] [PubMed] [Google Scholar]
- 18.R&D Systems®: Human Cystatin C Immunoassay. Product Datasheet 2017.
- 19.Pottel H, Hoste L, Martens F. A simple height-independent equation for estimating glomerular filtration rate in children. Pediatr Nephrol. 2012;27(6):973–979. doi: 10.1007/s00467-011-2081-9. [DOI] [PubMed] [Google Scholar]
- 20.Batte A, Starr MC, Schwaderer AL, Opoka RO, Namazzi R, Phelps Nishiguchi ES, Ssenkusu JM, John CC, Conroy AL. Methods to estimate baseline creatinine and define acute kidney injury in lean Ugandan children with severe malaria: a prospective cohort study. BMC Nephrol. 2020;21(1):417. doi: 10.1186/s12882-020-02076-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–637. doi: 10.1681/ASN.2008030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Imani PD, Odiit A, Hingorani SR, Weiss NS, Eddy AA. Acute kidney injury and its association with in-hospital mortality among children with acute infections. Pediatr Nephrol. 2013;28(11):2199–2206. doi: 10.1007/s00467-013-2544-2. [DOI] [PubMed] [Google Scholar]
- 23.Conroy AL, Hawkes M, Elphinstone RE, Morgan C, Hermann L, Barker KR, Namasopo S, Opoka RO, John CC, Liles WC, et al. Acute kidney injury is common in pediatric severe malaria and is associated with increased mortality. Open Forum Infect Dis. 2016;3(2):ofw046. doi: 10.1093/ofid/ofw046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olowu WA, Niang A, Osafo C, Ashuntantang G, Arogundade FA, Porter J, Naicker S, Luyckx VA. Outcomes of acute kidney injury in children and adults in sub-Saharan Africa: a systematic review. Lancet Glob Health. 2016;4(4):e242–250. doi: 10.1016/S2214-109X(15)00322-8. [DOI] [PubMed] [Google Scholar]
- 25.Lewington AJ, Cerdá J, Mehta RL. Raising awareness of acute kidney injury: a global perspective of a silent killer. Kidney Int. 2013;84(3):457–467. doi: 10.1038/ki.2013.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poston JT, Koyner JL. Sepsis associated acute kidney injury. BMJ. 2019;364:k4891. doi: 10.1136/bmj.k4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Larsen R, Gozzelino R, Jeney V, Tokaji L, Bozza FA, Japiassú AM, Bonaparte D, Cavalcante MM, Chora Â, Ferreira A, et al. A central role for free heme in the pathogenesis of severe sepsis. Sci Transl Med. 2010;2(51):51ra71–51ra71. doi: 10.1126/scitranslmed.3001118. [DOI] [PubMed] [Google Scholar]
- 28.Barber BE, Grigg MJ, Piera KA, William T, Cooper DJ, Plewes K, Dondorp AM, Yeo TW, Anstey NM. Intravascular haemolysis in severe plasmodium knowlesi malaria: association with endothelial activation, microvascular dysfunction, and acute kidney injury. Emerg Microbes Infect. 2018;7(1):106. doi: 10.1038/s41426-018-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Plewes K, Kingston HWF, Ghose A, Maude RJ, Herdman MT, Leopold SJ, Ishioka H, Hasan MMU, Haider MS, Alam S, et al. Cell-free hemoglobin mediated oxidative stress is associated with acute kidney injury and renal replacement therapy in severe falciparum malaria: an observational study. BMC Infect Dis. 2017;17(1):313. doi: 10.1186/s12879-017-2373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elphinstone RE, Conroy AL, Hawkes M, Hermann L, Namasopo S, Warren HS, John CC, Liles WC, Kain KC. Alterations in systemic extracellular heme and hemopexin are associated with adverse clinical outcomes in Ugandan children with severe malaria. J Infect Dis. 2016;214(8):1268–1275. doi: 10.1093/infdis/jiw357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Van Avondt K, Nur E, Zeerleder S. Mechanisms of haemolysis-induced kidney injury. Nat Rev Nephrol. 2019;15(11):671–692. doi: 10.1038/s41581-019-0181-0. [DOI] [PubMed] [Google Scholar]
- 32.Saraf SL, Zhang X, Kanias T, Lash JP, Molokie RE, Oza B, Lai C, Rowe JH, Gowhari M, Hassan J, et al. Haemoglobinuria is associated with chronic kidney disease and its progression in patients with sickle cell anaemia. Br J Haematol. 2014;164(5):729–739. doi: 10.1111/bjh.12690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olupot-Olupot P, Engoru C, Uyoga S, Muhindo R, Macharia A, Kiguli S, Opoka RO, Akech S, Ndila C, Nyeko R, et al. High frequency of blackwater fever among children presenting to hospital with severe febrile illnesses in Eastern Uganda. Clin Infect Dis. 2017;64(7):939–946. doi: 10.1093/cid/cix003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Opoka RO, Waiswa A, Harriet N, John CC, Tumwine JK, Karamagi C. Blackwater fever in Ugandan children with severe anemia is associated with poor postdischarge outcomes: a prospective cohort study. Clin Infect Dis. 2020;70(11):2247–2254. doi: 10.1093/cid/ciz648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aloni MN, Nsibu CN, Meeko-Mimaniye M, Ekulu PM, Bodi JM. Acute renal failure in Congolese children: a tertiary institution experience. Acta Paediatr. 2012;101(11):e514–518. doi: 10.1111/j.1651-2227.2012.02827.x. [DOI] [PubMed] [Google Scholar]
- 36.Conroy AL, Opoka RO, Bangirana P, Idro R, Ssenkusu JM, Datta D, Hodges JS, Morgan C, John CC. Acute kidney injury is associated with impaired cognition and chronic kidney disease in a prospective cohort of children with severe malaria. BMC Med. 2019;17(1):98. doi: 10.1186/s12916-019-1332-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bodi JM, Nsibu CN, Aloni MN, Lukute GN, Kunuanuna TS, Tshibassu PM, Pakasa N. Black water fever associated with acute renal failure among congolese children in Kinshasa. Saudi J Kidney Dis Transpl. 2014;25(6):1352–1358. doi: 10.4103/1319-2442.144326. [DOI] [PubMed] [Google Scholar]
- 38.Mårtensson J, Martling C-R, Bell M. Novel biomarkers of acute kidney injury and failure: clinical applicability. Br J Anaesth. 2012;109(6):843–850. doi: 10.1093/bja/aes357. [DOI] [PubMed] [Google Scholar]
- 39.Coca S, Yalavarthy R, Concato J, Parikh C. Biomarkers for the diagnosis and risk stratification of acute kidney injury: a systematic review. Kidney Int. 2008;73(9):1008–1016. doi: 10.1038/sj.ki.5002729. [DOI] [PubMed] [Google Scholar]
- 40.Greenberg JH, Parikh CR. Biomarkers for diagnosis and prognosis of AKI in children: one size does not fit all. Clin J Am Soc Nephrol. 2017;12(9):1551–1557. doi: 10.2215/CJN.12851216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Audard V, Moutereau S, Vandemelebrouck G, Habibi A, Khellaf M, Grimbert P, Levy Y, Loric S, Renaud B, Lang P. First evidence of subclinical renal tubular injury during sickle-cell crisis. Orphanet J Rare Dis. 2014;9(1):67. doi: 10.1186/1750-1172-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dampier C, Setty BY, Eggleston B, Brodecki D, O’Neal P, Stuart M. Vaso-occlusion in children with sickle cell disease: clinical characteristics and biologic correlates. J Pediatr Hematol Oncol. 2004;26(12):785–90. [PubMed]
- 43.Frei-Jones MJ, Baxter AL, Rogers ZR, Buchanan GR. Vaso-occlusive episodes in older children with sickle cell disease: emergency department management and pain assessment. J Pediatr. 2008;152(2):281–285. doi: 10.1016/j.jpeds.2007.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Olaniran KO, Allegretti AS, Zhao SH, Achebe MM, Eneanya ND, Thadhani RI, Nigwekar SU, Kalim S. Kidney function decline among black patients with sickle cell trait and sickle cell disease: an observational cohort study. J Am Soc Nephrol. 2020;31(2):393–404. doi: 10.1681/ASN.2019050502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Coca SG, Singanamala S, Parikh CR. Chronic kidney disease after acute kidney injury: a systematic review and meta-analysis. Kidney Int. 2012;81(5):442–448. doi: 10.1038/ki.2011.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Heung M, Chawla LS. Predicting progression to chronic kidney disease after recovery from acute kidney injury. Curr Opin Nephrol Hypertens. 2012;21(6):628–634. doi: 10.1097/MNH.0b013e3283588f24. [DOI] [PubMed] [Google Scholar]
- 47.Jones J, Holmen J, De Graauw J, Jovanovich A, Thornton S, Chonchol M. Association of complete recovery from acute kidney injury with incident CKD stage 3 and all-cause mortality. Am J Kidney Dis. 2012;60(3):402–408. doi: 10.1053/j.ajkd.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mammen C, Al Abbas A, Skippen P, Nadel H, Levine D, Collet JP, Matsell DG. Long-term risk of CKD in children surviving episodes of acute kidney injury in the intensive care unit: a prospective cohort study. Am J Kidney Dis. 2012;59(4):523–530. doi: 10.1053/j.ajkd.2011.10.048. [DOI] [PubMed] [Google Scholar]
- 49.KDIGO KDIGO 2012 Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3(1):1–150. doi: 10.1038/ki.2013.243. [DOI] [PubMed] [Google Scholar]
- 50.Warady BA, Abraham AG, Schwartz GJ, Wong CS, Muñoz A, Betoko A, Mitsnefes M, Kaskel F, Greenbaum LA, Mak RH, et al. Predictors of rapid progression of glomerular and nonglomerular kidney disease in children and adolescents: the Chronic Kidney Disease in Children (CKiD) Cohort. Am J Kidney Dis. 2015;65(6):878–888. doi: 10.1053/j.ajkd.2015.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.LambersHeerspink HJ, Gansevoort RT, Brenner BM, Cooper ME, Parving HH, Shahinfar S, de Zeeuw D. Comparison of different measures of urinary protein excretion for prediction of renal events. J Am Soc Nephrol. 2010;21(8):1355–1360. doi: 10.1681/ASN.2010010063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Group ET. Wuhl E, Trivelli A, Picca S, Litwin M, Peco-Antic A, Zurowska A, Testa S, Jankauskiene A, Emre S, et al. Strict blood-pressure control and progression of renal failure in children. N Engl J Med. 2009;361(17):1639–1650. doi: 10.1056/NEJMoa0902066. [DOI] [PubMed] [Google Scholar]
- 53.Ciccone E, Kilgore RR, Zhou Q, Cai J, Derebail VK, Ataga KI. Progression of chronic kidney disease in sickle cell disease. Blood. 2016;128(22):1323–1323. [Google Scholar]
- 54.Ranque B, Menet A, Diop IB, Thiam MM, Diallo D, Diop S, Diagne I, Sanogo I, Kingue S, Chelo D, et al. Early renal damage in patients with sickle cell disease in sub-Saharan Africa: a multinational, prospective, cross-sectional study. Lancet Haematol. 2014;1(2):e64–e73. doi: 10.1016/S2352-3026(14)00007-6. [DOI] [PubMed] [Google Scholar]
- 55.Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL, Investigators A. Epidemiology of acute kidney injury in critically Ill children and young adults. N Engl J Med. 2017;376(1):11–20. doi: 10.1056/NEJMoa1611391. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.