Abstract
Background
Coronavirus disease 2019 (COVID-19) is a highly contagious and quickly spreading disease, especially if associated with poor awareness and unwanted behavioral practices. Unvaccinated people are at high risk of infection, mortality, and morbidity. Practices and intent toward the COVID-19 vaccine are mainly influenced by the perception of vaccine safety. This study aimed to assess the perception, practices, intent, and challenges toward the COVID-19 vaccine in Asir region, Saudi Arabia.
Methodology
A quantitative, cross-sectional study was conducted among the available population in Asir region, southwest of Saudi Arabia. Data were collected from participants using a semi-structured electronic questionnaire. The questionnaire included sections on participants’ socio-demographic data and their family and personal history of COVID-19 infection. Additionally, the effects of the COVID-19 pandemic on their daily life were assessed. The second section of the questionnaire included knowledge questions regarding the COVID-19 vaccine with only one correct answer for each question. The last section covered participants’ attitudes toward the COVID-19 vaccine and their intent to take the vaccine with their previous vaccination practice.
Results
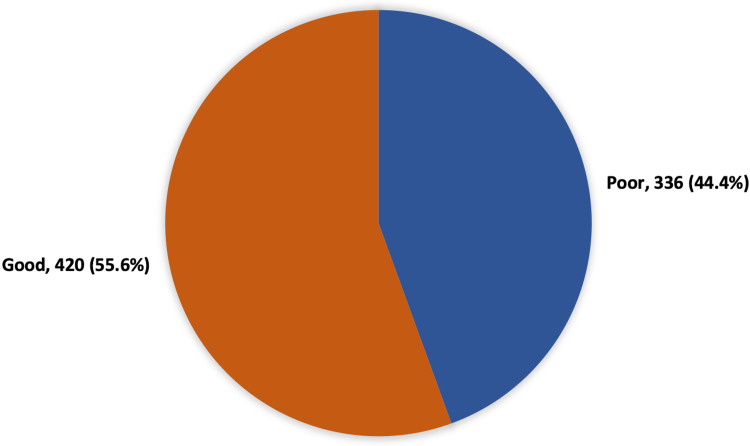
A total of 756 participants who met the inclusion criteria participated in the study. Participants’ ages ranged from 18 to 65 years, with a mean age of 22.6 ± 12.8 years. A total of 518 respondents were females. Regarding the level of education, 72.2% were university graduates or postgraduates, and 195 (25.8%) were in high school. Regarding the overall knowledge level toward the COVID-19 vaccine among study participants, 420 (55.6%) participants had good knowledge regarding the COVID-19 vaccine. In total, 158 (20.9%) participants were of the view that the COVID-19 vaccine is risky. Approximately 26.9% of the participants were told by their doctor that vaccination is necessary, and 49.3% thought that they need more information about the COVID-19 vaccine.
Conclusions
This study revealed that public awareness regarding the COVID-19 vaccine was satisfactory, especially concerning its benefit in reducing infection and associated complications; however, poor awareness was reported regarding their perception of the pandemic and COVID-19 vaccine definition.
Keywords: vaccine hesitancy, hesitancy, saudi arabia, public, intent, covid-19 vaccine
Introduction
Coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), is a highly transmissible and quickly spreading disease [1]. The COVID-19 outbreak started in Wuhan, Hubei province, China, in December 2019, and by early 2020, the world was facing a rapidly spreading epidemic, which was later classified by the World Health Organization (WHO) as a pandemic [2]. WHO classified the disease as a Public Health Emergency of International Concern on January 30, 2020, and recognized it as a pandemic on March 11, 2020 [3,4].
Considerable efforts were made toward the development of vaccines against COVID-19 to prevent the pandemic. The majority of the emerging vaccines have used the S-protein of SARS-CoV-2 [5]. The most efficient approach to control the spread of the COVID-19 pandemic, in the long run, is mass vaccination [6]. The efficacy of the COVID-19 vaccination is mainly based on continuous vaccination, and its preparation and delivery inventiveness. In November 2020, several international pharmaceutical companies reported the effectiveness and benefit of their vaccines according to large clinical trials [7]. Because of the urgent situation caused by the pandemic, these vaccines received emergency regulatory approvals by national drug and pharmaceutical agencies in December 2020, and vaccination programs were rolled out in many countries soon after [8,9].
Owing to poor knowledge, attitude, and practices toward preventing COVID-19 among communities in Saudi Arabia, the absence of vaccines or treatments can lead to further disease transmission and place these communities at higher risk of infection, mortality, and morbidity [10]. Recently, COVID-19 vaccines have become available in Saudi Arabia, which is a significant preventative measure against virus transmission. However, it is important to determine the knowledge, attitudes, practices, and intent of individuals toward getting the COVID-19 vaccine, which are mainly influenced by their knowledge level, attitudes, practices, and intent [11]. This study aimed to assess the perception, practices, intent, and challenges toward the COVID-19 vaccine in the Asir region of Saudi Arabia.
Materials and methods
A quantitative, cross-sectional survey was conducted among the available population in the Asir region, Saudi Arabia. This study was approved by the Research Ethics Committee at King Khalid University (Approval number: ECM#2021-5307). Individuals aged 18 years or more living in the Asir region for at least six months were invited to voluntarily participate in the survey. A total of 1,200 eligible individuals were included in the survey. In total, 756 participants completed the study questionnaire, with a response rate of 63.8%. Data were collected from participants using a semi-structured electronic questionnaire. Questionnaire items were reviewed by a panel of three experts from the College of Medicine at King Khalid University to check their applicability and content validity. Tool reliability was assessed using a pilot study of 25 participants, with a reliability coefficient (Cronbach’s alpha) of 0.71. The questionnaire included the following items: participants’ socio-demographic data, such as age, gender, education, income, and employment status, their family and personal history of COVID-19 infection, and the effect of the COVID-19 pandemic on their daily life. The second section included knowledge questions regarding the COVID-19 vaccine, with only one correct answer for each question. The final section covered participants’ attitudes toward the COVID-19 vaccine and their intent to take the vaccine with their previous vaccination practice. The questionnaire was uploaded online using social media platforms by researchers and their friends, and all eligible individuals were invited to fill it after explaining the study purpose and assuring them of data confidentiality.
Data analysis
After extraction, data were revised, coded, and analyzed using SPSS version 22 (IBM Corp., Armonk, NY, USA). All statistical analyses were done using two-tailed tests. P-values less than 0.05 were considered statistically significant. For knowledge and awareness items, each correct answer was scored one point, and the total sum of the discrete scores of the different items was calculated. A patient with a score less than 60% (0-3 points) of the total score was considered to have poor awareness, while good awareness was considered if the score was 60% (4 points or more) of the total or more. Descriptive analysis based on the frequency and percentage distribution was performed for all variables, including participants’ socio-demographic data, family and personal history of COVID-19 infection, the risk level for being infected with COVID-19, and the impact of the pandemic on their life. Moreover, participants’ knowledge and awareness regarding the COVID-19 vaccine, attitude, and intent to get the vaccine were presented as frequency tables and graphs. Crosstabulation was used to assess the distribution of public knowledge and the awareness level regarding the COVID-19 vaccine according to their personal data, disease history, and family history. Furthermore, the relationship between participants’ knowledge level and their attitude with intent to have the vaccine was tabulated. Relationships were determined using Pearson’s chi-square test and exact probability test for small frequency distributions.
Results
A total of 756 participants who met the inclusion criteria participated in the study. Participants’ ages ranged from 18 to 65 years, with a mean age of 22.6 ± 12.8 years. In total, 518 respondents were females. Regarding the level of education, 72.2% were university graduates or postgraduates, and 195 (25.8%) were in high school. Of the total study population, 435 (57.5%) were students, 146 (19.3%) were not employed, and 23.1% were employed in the government or private sector. In total, 98 (13%) participants had chronic health problems, including chronic respiratory disease (33.8%), diabetes (14.3%), obesity (6%), and hypertension (4.5%), while 3% had autoimmune health problems. A total of 464 (61.4%) participants had a history of COVID-19 infection among their family and friends. Moreover, 25.9% reported that they were at very high to high risk for contracting COVID-19 infection in the coming months, while 28.1% reported being at low to very low risk. Regarding the impact of the pandemic on daily life, large to extremely large effect was reported by 65.6% of the study participants, while only 8.2% reported low impact (Table 1).
Table 1. Socio-demographic data of study participants.
COVID-19: coronavirus disease 2019
| Socio-demographic data | No. | % | |
| Age (years) | 18–25 | 515 | 68.1% |
| 26–30 | 83 | 11.0% | |
| 31–40 | 85 | 11.2% | |
| 41–50 | 43 | 5.7% | |
| 51+ | 30 | 4.0% | |
| Gender | Male | 238 | 31.5% |
| Female | 518 | 68.5% | |
| Highest level of education | Middle school/below | 15 | 2.0% |
| High school | 195 | 25.8% | |
| University graduate | 497 | 65.7% | |
| Postgraduate degree | 49 | 6.5% | |
| Marital status | Single | 574 | 75.9% |
| Married | 170 | 22.5% | |
| Divorced/Widowed | 12 | 1.6% | |
| Employment | Unemployed/Retired | 146 | 19.3% |
| Student | 435 | 57.5% | |
| Governmental employee | 94 | 12.4% | |
| Private sector employee | 81 | 10.7% | |
| Chronic diseases | Yes | 98 | 13.0% |
| No | 658 | 87.0% | |
| Type of the disease | Respiratory chronic diseases | 45 | 33.8% |
| Diabetes | 19 | 14.3% | |
| Obesity | 8 | 6.0% | |
| Hypertension | 6 | 4.5% | |
| Autoimmune diseases | 4 | 3.0% | |
| Cardiac diseases | 3 | 2.3% | |
| Other | 47 | 35.3% | |
| History of COVID-19 infection in family and friends | Yes | 464 | 61.4% |
| No | 292 | 38.6% | |
| What is your level of risk for COVID-19 infection in the coming months | Very high | 72 | 9.5% |
| High | 124 | 16.4% | |
| Average | 348 | 46.0% | |
| Low | 145 | 19.2% | |
| Very low | 67 | 8.9% | |
| Impact of the pandemic on daily life | Extremely large | 402 | 53.2% |
| Large | 94 | 12.4% | |
| Fair | 198 | 26.2% | |
| Small | 15 | 2.0% | |
| Extremely small | 47 | 6.2% | |
As shown in Table 2, 16.9% of the participants correctly defined COVID-19 infection, while 22.5% knew about the COVID-19 vaccine. Additionally, 57.5% of the respondents agreed that the vaccine will reduce/prevent the risk of infection, and 80.7% knew that the COVID-19 vaccine was beneficial. Further, 53.2% agreed that taking the COVID-19 vaccine can lower the risk of complications. The most reported source of information regarding the COVID-19 vaccine was social media (48.8%), followed by healthcare staff (13.1%), internet (11.5%), and others (5%).
Table 2. Participants’ knowledge regarding the COVID-19 vaccine.
COVID-19: coronavirus disease 2019
| Knowledge items | No | % |
| What is COVID-19 infection? | ||
| Incorrect definition | 128 | 16.9% |
| Correct definition | 628 | 83.1% |
| What is vaccination? | ||
| Incorrect definition | 170 | 22.5% |
| Correct definition | 586 | 77.5% |
| The vaccine will reduce/prevent the risk the infection | ||
| Agree | 435 | 57.5% |
| Maybe | 230 | 30.4% |
| Disagree | 53 | 7.0% |
| I don’t know | 38 | 5.0% |
| Is COVID-19 vaccination beneficial? | ||
| Yes | 610 | 80.7% |
| No | 146 | 19.3% |
| Source of information | ||
| Social media | 369 | 48.8% |
| General physician or family physician | 99 | 13.1% |
| Internet | 87 | 11.5% |
| Other | 38 | 5.0% |
| Family | 20 | 2.6% |
| Friends | 10 | 1.3% |
| None | 133 | 17.6% |
| Taking the COVID-19 vaccine lowers complications | ||
| Agree | 402 | 53.2% |
| Maybe | 246 | 32.5% |
| Disagree | 67 | 8.9% |
| I don’t know | 41 | 5.4% |
Figure 1 shows that 420 (55.6%) participants had a good knowledge level regarding the COVID-19 vaccine while 336 (44.4%) had a poor knowledge level.
Figure 1. The overall knowledge level regarding the COVID-19 vaccine among study participants.
COVID-19: coronavirus disease 2019
Table 3 demonstrates that 158 (20.9%) participants thought that the COVID-19 vaccine was risky. The most reported sources regarding the vaccine risk were social media (40.5%), the internet (18.4%), and family and friends (17.1%). On the other hand, 26.9% of the participants were told by their doctor that vaccination was necessary, and 49.3% thought that they needed more information about the vaccine.
Table 3. Participants’ attitude and perception toward the COVID-19 vaccine.
COVID-19: coronavirus disease 2019
| Attitude and perception | No | % |
| Do you think the vaccine is risky? | ||
| Yes | 158 | 20.9% |
| No | 598 | 79.1% |
| Source of risk information | ||
| Social media | 64 | 40.5% |
| Other | 38 | 24.1% |
| Internet | 29 | 18.4% |
| Family | 16 | 10.1% |
| Friends | 11 | 7.0% |
| Have you ever been told by your doctor that vaccination is absolutely necessary? | ||
| Yes | 203 | 26.9% |
| No | 92 | 12.2% |
| I didn’t ask about it | 461 | 61.0% |
| Do you need more information about the COVID-19 vaccine? | ||
| Yes | 373 | 49.3% |
| No | 383 | 50.7% |
As presented in Table 4, 24.3% of the participants reported they could change their mind about agreeing or refusing to take the vaccine while 58.6% may change their mind. Moreover, 77.9% of the participants reported that they will accept taking the vaccine themselves or for their family, and 78.7% told if a lot of people had the vaccine, they will take it. In total, 116 (15.3%) participants reported that they had refused vaccination of a certain vaccine in the past.
Table 4. Participants’ intent and practice regarding the COVID-19 vaccine.
COVID-19: coronavirus disease 2019
| Vaccine intent and practice | No | % |
| Do you think you can change your mind about accepting or refusing to take the vaccine? | ||
| Yes | 184 | 24.3% |
| Maybe | 445 | 58.9% |
| No | 127 | 16.8% |
| If you were asked to take the vaccine for yourself and your family, will you accept it? | ||
| Yes | 589 | 77.9% |
| Maybe | 112 | 14.8% |
| No | 55 | 7.3% |
| If a lot of people had the vaccine, are you going to take it? | ||
| Yes | 595 | 78.7% |
| May be | 98 | 13.0% |
| No | 63 | 8.3% |
| Did you refuse vaccination of a certain type of vaccine in the past? | ||
| Yes | 116 | 15.3% |
| No | 640 | 84.7% |
Table 5 shows that a good knowledge level was detected among 62.2% of male participants versus 52.5% of female participants, which was statistically significant (P = 0.013). Further, 62.8% of governmental employees had good knowledge regarding the vaccine compared to 44.4% of those employed in the private sector and 47.9% of the unemployed group (P = 0.011). Good knowledge level was detected among 59.2% of those with an average level of risk for COVID-19 infection compared to 41.8% of those with a low level of risk (P = 0.049).
Table 5. Distribution of participants’ knowledge level regarding the COVID-19 vaccine according to their socio-demographic data.
P: Pearson’s chi-square test; $: exact probability test; *: P < 0.05 (significant).
COVID-19: coronavirus disease 2019
| Factors | Knowledge level | P-value | |||
| Poor | Good | ||||
| No | % | No | % | ||
| Age (years) | 0.664 | ||||
| 18–25 | 222 | 43.1% | 293 | 56.9% | |
| 26–30 | 38 | 45.8% | 45 | 54.2% | |
| 31–40 | 39 | 45.9% | 46 | 54.1% | |
| 41–50 | 20 | 46.5% | 23 | 53.5% | |
| 51+ | 17 | 56.7% | 13 | 43.3% | |
| Gender | 0.013* | ||||
| Male | 90 | 37.8% | 148 | 62.2% | |
| Female | 246 | 47.5% | 272 | 52.5% | |
| Highest level of education | 0.838$ | ||||
| Middle school/below | 5 | 33.3% | 10 | 66.7% | |
| High school | 88 | 45.1% | 107 | 54.9% | |
| University graduates | 222 | 44.7% | 275 | 55.3% | |
| Postgraduate degree | 21 | 42.9% | 28 | 57.1% | |
| Employment | 0.011* | ||||
| Unemployed/Retired | 76 | 52.1% | 70 | 47.9% | |
| Student | 180 | 41.4% | 255 | 58.6% | |
| Governmental employee | 35 | 37.2% | 59 | 62.8% | |
| Private sector employee | 45 | 55.6% | 36 | 44.4% | |
| Had chronic diseases | 0.333 | ||||
| Yes | 48 | 49.0% | 50 | 51.0% | |
| No | 288 | 43.8% | 370 | 56.2% | |
| History of COVID-19 infection in family and friends | 0.124 | ||||
| Yes | 196 | 42.2% | 268 | 57.8% | |
| No | 140 | 47.9% | 152 | 52.1% | |
| What is your level of risk for COVID-19 infection in the coming months | 0.049* | ||||
| Very high | 34 | 47.2% | 38 | 52.8% | |
| High | 60 | 48.4% | 64 | 51.6% | |
| Average | 142 | 40.8% | 206 | 59.2% | |
| Low | 61 | 42.1% | 84 | 57.9% | |
| Very low | 39 | 58.2% | 28 | 41.8% | |
| Impact of the pandemic on daily life | 0.103 | ||||
| Extremely large | 169 | 42.0% | 233 | 58.0% | |
| Large | 35 | 37.2% | 59 | 62.8% | |
| Fair | 99 | 50.0% | 99 | 50.0% | |
| Small | 9 | 60.0% | 6 | 40.0% | |
| Extremely small | 24 | 51.1% | 23 | 48.9% | |
Table 6 shows that a higher knowledge level was significantly associated with a lower attitude about the vaccine risk. Overall, 93.1% of those with a good knowledge level accepted to get the vaccine compared to 58.9% of those with poor knowledge (P = 0.001). In addition, 92.6% of participants with good knowledge regarding the vaccine agreed to take the vaccine if many people had it versus 61.3% of those with poor knowledge level (P = 0.001). On the other hand, changing their mind regarding vaccine acceptance was significantly higher among those with poor knowledge levels compared to those with higher knowledge (29.5% vs. 20.2%, respectively).
Table 6. Distribution of participants’ attitude and intent toward the COVID-19 vaccine according to their knowledge level.
P: Pearson’s chi-square test; $: exact probability test; *: P < 0.05 (significant).
COVID-19: coronavirus disease 2019
| Vaccine attitude and intent | Knowledge level | P-value | |||
| Poor | Good | ||||
| No | % | No | % | ||
| Do you think the vaccine is risky? | 0.001* | ||||
| Yes | 116 | 34.5% | 42 | 10.0% | |
| No | 220 | 65.5% | 378 | 90.0% | |
| Have you ever been told by your doctor that vaccination is absolutely necessary? | 0.001* | ||||
| Yes | 67 | 19.9% | 136 | 32.4% | |
| No | 44 | 13.1% | 48 | 11.4% | |
| I didn’t ask about it | 225 | 67.0% | 236 | 56.2% | |
| Do you need more information about the COVID-19 vaccine? | 0.026* | ||||
| Yes | 181 | 53.9% | 192 | 45.7% | |
| No | 155 | 46.1% | 228 | 54.3% | |
| Do you think you can change your mind about accepting or refusing to take the vaccine? | 0.001* | ||||
| Yes | 99 | 29.5% | 85 | 20.2% | |
| Maybe | 198 | 58.9% | 247 | 58.8% | |
| No | 39 | 11.6% | 88 | 21.0% | |
| If you were asked to take the vaccine for yourself and your family, will you accept it? | 0.001* | ||||
| Yes | 198 | 58.9% | 391 | 93.1% | |
| Maybe | 89 | 26.5% | 23 | 5.5% | |
| No | 49 | 14.6% | 6 | 1.4% | |
| If a lot of people had the vaccine, are you going to take it? | 0.001*$ | ||||
| Yes | 206 | 61.3% | 389 | 92.6% | |
| Maybe | 73 | 21.7% | 25 | 6.0% | |
| No | 57 | 17.0% | 6 | 1.4% | |
Discussion
The public unwillingness to receive safe and suggested available vaccines, known as “vaccine hesitancy,” was already a rising issue before the COVID-19 pandemic [12]. An outline established from research in high-income countries, namely, “the 5C model of the drivers of vaccine hesitancy,” describes the following five main person-level factors for vaccine hesitancy: confidence, complacency, convenience (or constraints), risk calculation, and collective responsibility [13,14]. Encouraging the intake of vaccines, especially those against COVID-19, requires understanding whether people are willing to be vaccinated, the motives why they are ready or not ready to do so, the most trusted sources of information in their decision-making, and their awareness levels. Wouters et al. assessed these factors using a public set of surveys conducted between June 2020 and January 2021 in 15 studies carried out in Africa, South Asia, Latin America, Russia, and the United States [15].
Health knowledge establishes a solid contextual factor that endorses health prevention activities. Higher knowledge levels about health risks, signs and symptoms, and the benefits of preventive actions promote healthier lifestyles [16]. The knowledge, attitude, and behavior assume that a person’s health awareness and information play an important role in health-related behavior [17].
This study aimed to assess the public knowledge level, attitude, and intent toward the COVID-19 vaccine and their effect on the willingness to get the vaccine. Regarding public knowledge and awareness, the findings showed that more than half of the participants had a good knowledge level regarding the COVID-19 vaccine. More than half of the participants (57.5%) knew that the vaccine will reduce/prevent the risk of the infection, while a vast majority of the participants (80.7%) knew that the COVID-19 vaccine is beneficial. Furthermore, more than half agreed that taking the COVID-19 vaccine will reduce the risk of complications. On the other hand, lower awareness regarding the virus and vaccine was reported, with less than one-fifth of the respondents correctly defining COVID-19 infection while about one-fifth (22.5%) knew about the COVID-19 vaccine. Additionally, the most reported source of information regarding the COVID-19 vaccine was social media (48.8%), followed by healthcare staff (13.1%), the internet (11.5%), and others (5%). A higher awareness level was reported by Elgendy et al [18], where the median score of the survey was 20/22 regarding knowledge about the COVID-19 vaccine. Overall, the study participants had good knowledge about the COVID-19 vaccine and accepted to take the vaccine, indicating the highly commendable efforts to control the coronavirus. In Saudi Arabia, Alrefaei et al. [19] found that all respondents knew that the coronavirus is contagious, and 89.8% agreed that the symptoms of COVID-19 are similar to those of the seasonal flu. A high level of knowledge of the main factors of SARS-CoV-2 transmission was also reported. More than 98.7% of respondents knew about the role of large gatherings and events in the further spread of the virus. However, the respondents considered COVID-19 vaccines to be effective, but some respondents were not aware of their side effects, and 38.8% planned to receive a vaccine. Similar findings were reported among participants in Riyadh [20].
Regarding participants’ attitudes and intent toward the COVID-19 vaccine, the findings showed that one-fifth of the participants thought that the COVID-19 vaccine is risky. Moreover, only about one-fourth of the participants were told by their doctor that vaccination is necessary, which explains that about half of the respondents thought that they need more information about the COVID-19 vaccine. Additionally, about one out of four participants reported possibly changing their mind about accepting or refusing to take the vaccine, while more than half (58.6%) may change their opinion. Nearly three-quarters of the respondents reported that they will accept the vaccine for themselves or for their family, reported if a lot of people had the vaccine, they will take it. Similar findings were reported by Al-Zalfawi et al. [21] as the majority of respondents (76%) had satisfactory knowledge, a positive attitude (72.4%), and perception (71.3%) toward the use of COVID-19 vaccines. In Jazan, Almalki [22] reported that participants demonstrated a good knowledge of COVID-19, correctly answering 77% of the knowledge questions. Most of the participants exhibited good attitudes and acceptable practices toward COVID-19.
Limitations and strengths
Even though this study is one of the few studies in the region identifying the challenges associated with COVID-19 vaccine hesitancy, the study had some limitations. First, as the data were collected through a self-reported method, recall bias and question misinterpretation could have occurred. Further, we relied on online platforms as a primary tool to collect the data, which might explain the gender differences in our sample. In addition, we conducted this study in the Asir region of Saudi Arabia, which might affect its generalizability.
Conclusions
This study revealed that public awareness regarding the COVID-19 vaccine was satisfactory, especially regarding its benefit in reducing infection and associated complications; however, poor awareness was reported regarding their perception of the pandemic and COVID-19 vaccine definition. Furthermore, participants’ attitudes and intent to have the vaccine were high, especially among those with high knowledge levels. The study showed that the role of the healthcare staff in providing information regarding the pandemic and vaccine efficacy was not satisfactory, with more effort needed to improve their awareness and perception regarding the vaccine. Providing adequate information about the vaccines is recommended. Continuous training and education are needed to improve public vaccine acceptance and reduce vaccine hesitancy.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Research Ethics Committee at King Khalid University (HAPO-06-B-001) issued approval ECM#2021-5307
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.The COVID-19 pandemic. Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. Crit Rev Clin Lab Sci. 2020;57:365–388. doi: 10.1080/10408363.2020.1783198. [DOI] [PubMed] [Google Scholar]
- 2.A global respiratory perspective on the COVID-19 pandemic: commentary and action proposals. To T, Viegi G, Cruz A, et al. Eur Respir J. 2020;56:2001704. doi: 10.1183/13993003.01704-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epidemiology and diagnosis, environmental resources quality and socio-economic perspectives for COVID-19 pandemic. Suthar S, Das S, Nagpure A, Madhurantakam C, Tiwari SB, Gahlot P, Tyagi VK. J Environ Manage. 2021;280:111700. doi: 10.1016/j.jenvman.2020.111700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO Director-General's opening remarks at the media briefing on COVID-19. [ Mar; 2020 ];https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 2020
- 5.COVID-19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Dhama K, Sharun K, Tiwari R, Dadar M, Malik YS, Singh KP, Chaicumpa W. Hum Vaccin Immunother. 2020;16:1232–1238. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Effectiveness of the BNT162b2mRNA Covid-19 vaccine in patients with hematological neoplasms [In Press] Mittelman M, Magen O, Barda N, Dagan N, Oster HS, Leader A, Balicer R. http://10.1182/blood.2021013768. Blood. 2021 doi: 10.1182/blood.2021013768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.COVID-19 vaccines: where we stand and challenges ahead. Forni G, Mantovani A. Cell Death Differ. 2021;28:626–639. doi: 10.1038/s41418-020-00720-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The European Medicines Agency's EU conditional marketing authorisations for COVID-19 vaccines. Cavaleri M, Enzmann H, Straus S, Cooke E. Lancet. 2021;397:355–357. doi: 10.1016/S0140-6736(21)00085-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.What to know about the global COVID-19 vaccine rollout so far. [ Jan; 2021 ];Felter C. https://www.cfr.org/in-brief/what-know-about-global-covid-19-vaccine-rollout-so-far 2021
- 10.Knowledge, attitude and practice toward COVID-19 among the public in the Kingdom of Saudi Arabia: a cross-sectional study. Al-Hanawi MK, Angawi K, Alshareef N, et al. Front Public Health. 2020;8:217. doi: 10.3389/fpubh.2020.00217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.COVID-19 vaccine hesitancy among patients with diabetes in Saudi Arabia. Aldossari KK, Alharbi MB, Alkahtani SM, Alrowaily TZ, Alshaikhi AM, Twair AA. Diabetes Metab Syndr. 2021;15:102271. doi: 10.1016/j.dsx.2021.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaccine hesitancy: definition, scope and determinants. MacDonald NE. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 13.Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. Betsch C, Schmid P, Heinemeier D, Korn L, Holtmann C, Böhm R. PLoS One. 2018;13:0. doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaccine hesitancy in the era of COVID-19: could lessons from the past help in divining the future? [In Press] Wiysonge CS, Ndwandwe D, Ryan J, Jaca A, Batouré O, Anya BM, Cooper S. Hum Vaccin Immunother. 2021 doi: 10.1080/21645515.2021.1893062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, Jit M. Lancet. 2021;397:1023–1034. doi: 10.1016/S0140-6736(21)00306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Knowledge, attitude and practice for cervical cancer prevention and control among women of childbearing age in Hossana Town, Hadiya zone, Southern Ethiopia: community-based cross-sectional study. Aweke YH, Ayanto SY, Ersado TL. PLoS One. 2017;12:0. doi: 10.1371/journal.pone.0181415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Access to attitude-relevant information in memory as a determinant of attitude-behaviour consistency. Kallgren CA, Wood W. https://www.sciencedirect.com/science/article/abs/pii/0022103186900181 J Exp Social Psychol. 1986;22:328–338. [Google Scholar]
- 18.Public awareness about coronavirus vaccine, vaccine acceptance, and hesitancy. Elgendy MO, Abdelrahim ME. J Med Virol. 2021;93:6535–6543. doi: 10.1002/jmv.27199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Assessment of health awareness and knowledge toward SARS-CoV-2 and COVID-19 vaccines among residents of Makkah, Saudi Arabia. Alrefaei AF, Almaleki D, Alshehrei F, et al. Clin Epidemiol Glob Health. 2022;13:100935. doi: 10.1016/j.cegh.2021.100935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.An analytical study on the awareness, attitude and practice during the COVID-19 pandemic in Riyadh, Saudi Arabia. Alahdal H, Basingab F, Alotaibi R. J Infect Public Health. 2020;13:1446–1452. doi: 10.1016/j.jiph.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Public knowledge, attitude, and perception towards COVID-19 vaccination in Saudi Arabia. Al-Zalfawi SM, Rabbani SI, Asdaq SM, et al. Int J Environ Res Public Health. 2021;18:10081. doi: 10.3390/ijerph181910081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knowledge, attitudes, and practices toward COVID-19 among the general public in the border region of Jazan, Saudi Arabia: a cross-sectional study. Almalki MJ. Front Public Health. 2021;9:733125. doi: 10.3389/fpubh.2021.733125. [DOI] [PMC free article] [PubMed] [Google Scholar]