Abstract
Objective:
To evaluate the success of osseointegrated implants under immediate prosthetic and orthodontic forces after a follow-up period of at least 2 years.
Materials and Methods:
The sample included 20 titanium implants which were used as orthodontic and prosthetic anchorage of immediately loaded single-crowns on a total of 13 patients. A 40 N initial torque was considered the minimum for inclusion in the sample. All implants received screwed provisional crowns immediately after surgery. The implants were randomly divided into two groups: the control group (9 implants) and the immediate orthodontic loading group (11 implants). A healing period of 4 months was observed before orthodontic loads were applied to the control group implants. For the immediate orthodontic loading group, orthodontic forces were applied within 24 hours. The maximum orthodontic force applied in both groups was 200 g. After 6 months of orthodontic movement, clinical and radiographic evaluations were obtained. Implants were considered successful when favorable results were obtained in all evaluations.
Results:
After a 2-year follow-up, the success rates were 90.9% and 88.9%, respectively, in the orthodontic loading group and the control group. Each group had one failure.
Conclusion:
Shortening the healing period for the application of orthodontic forces did not seem to affect the success of osseointegrated implants used as anchorage.
Keywords: Orthodontic anchorage, Osseointegration
INTRODUCTION
The need for orthodontic treatment has increased in the adult population. However, many adult or aging patients frequently require integrated multidisciplinary treatment because of dental loss, which leads to difficulties or even impairment in solving biomechanical problems related to orthodontic anchorage. The use of osseointegrated implants has been a valid alternative in such cases. Besides promoting absolute anchorage during orthodontic movement, osseointegrated implants may also be used with no damage as a base for posterior oral fixed prosthetic rehabilitation, as they are considered a secure, predictable, and durable method.1
Although high success rates have been reported for immediate load applied to implants and for implants used for orthodontic anchorage, few studies have combined these two purposes to evaluate the possible use of immediate orthodontic load on osseointegrated implants used for anchorage.2–5
Considering the null hypothesis that there is no difference in the success rate of immediately loaded implant-supported crowns that are used as orthodontic anchorage immediately or after 4 months of healing, the present study aimed to evaluate the success rate after application of immediate orthodontic load to implants.
MATERIALS AND METHODS
This is a prospective clinical study in which 20 implant sites were randomly allocated to two groups: immediate orthodontic load on provisional crowns (Group A) and delayed orthodontic load (Group B). Each sample was evaluated before and after orthodontic forces were applied to the prosthetic restorations performed on the implants of each group. This study had institutional approval.
Adult patients seeking orthodontic treatment at the Clinic for Orthodontic Graduate and Postgraduate Studies of Rio de Janeiro State University, Brazil, who were in need of corrective orthodontic therapy and prosthetic rehabilitation, including one or more single osseointegrated implants, were prospectively selected for this study. After exclusion criteria were applied for patients in this randomized controlled trial (RCT) (the same as described by Chiapasco and Gatti6), 13 patients were enrolled in the trial, seven men and six women. Patients' ages ranged from 22 to 56 years (mean, 35.7 years). A total of 20 edentulous areas were considered to be adequate sites for ultra self-tapping titanium implants. These implants were 4-mm wide and 13-mm long and had an enhanced surface treatment with double acid attack (SIN (Sistema de Implante), São Paulo, Brazil), which would receive further orthodontic loads on provisional crown restorations with a bracket embedded. None of the implants were the primary centric stop in occlusion in the segment, so the prosthetic load could be distributed among other posterior teeth.
As the primary purpose of implant positioning in the patients in the present study was related to the function of implants as orthodontic anchorage, the surgical guide filled with gutta-percha was built from a correctly made set-up diagnosis. Patients also used that guide during the computed tomography exam. As gutta-percha is a radiopaque material, the precise location for future implant placement was determined, thus allowing for quantitative and qualitative bone evaluation of the site.
The 20 implant sites were randomly assigned to Group A and Group B using Microsoft Office Excel 2003 software (Redmond, Wash). The group for each implant was determined at the day of surgery. Initially, anesthesia was performed for mandibular nerve block with lidocaine 1∶100,000 (DFL Ind. e Com SA, Rio de Janeiro, Rio de Janeiro, Brazil). An incision for a mucoperiosteal flap was performed using a 15C scalpel blade (Benco Dental, Wilkes-Barre, Pa). The surgical guide was used to correctly position the implants. The last drill used was 0.7 mm smaller than the implant to be installed. All drills were used with an engine (Driller, São Paulo, São Paulo, Brazil) at 1200 rpm and a torque of 50 N/cm. After insertion of the implant, a prosthetic antirotational component (Connection, São Paulo, São Paulo, Brazil) was installed with a torque of 20 N/cm. The surgical procedure was completed with sutures of mononylon 5.0 (Ethicon, Johnson & Johnson Com, São Paulo, São Paulo, Brazil).
After surgery, oral hygiene instructions were given. Mouthwash with chlorhexidine gluconate 0.12% (Periogard, Colgate-Palmolive Industria e Comercio Ltda, São Paulo, São Paulo, Brazil) was recommended twice a day for 7 days after surgery. In addition, we prescribed 500 g of amoxicillin (Amoxil, GlaxoSmithKline, Brentford, UK) every 8 hours for 7 days and 750 mg of acetaminophen (Tylenol, Johnson & Johnson Com, Sao Paulo, Sao Paulo, Brazil) every 6 hours in case of pain.
In Group A, the implants were immediately used as orthodontic anchorage under loads ranging from 60 to 200 g, as assessed with a dynamometer. Only implants assessed as presenting primary stability, that is, could support a load of 40 N,7–9 were able to receive immediate load. In Group B, the traditional protocol was used of waiting 4 months before adding any orthodontic load over the implants,10 although the provisional crown restorations had been already placed.
Group A consisted of 11 implants, placed in 5 female and 6 male patients ranging in age from 22 to 56 years (mean age, 35.9 years). Group B consisted of nine implants, placed in 3 female and 6 male patients ranging in age from 22 to 52 years (mean age, 35.3 years). Some patients received both types of implants and were assigned to Group A and Group B. The implants were evaluated clinically each six months after orthodontic load.
The following criteria was used to denote clinical success:6
—Absence of signs and symptoms of pain, infection, or discomfort;
—Absence of implant mobility, determined with the aid of the handles of two dental mirrors;
—Absence of peri-implantar radiolucency shown on periapical radiographs, indicating bone resorption.
RESULTS
No dropouts were recorded. Of the 20 implants evaluated after 6 months of orthodontic load application on provisional crown restorations, 18 implants were not associated with any signs or symptoms of pain, infection, or neuropathy. Two implants were lost because of excess of mobility and lack of osseointegration: one in Group A (47 site) 2 months after the surgery and the other in Group B (46 site) 1 month after the surgery. Both failures apparently happened because of poor hygiene with an excess of bacterial plaque in the cervical portion of the provisional crown.
Of the 11 implants in Group A, 10 were successful and only one failed (success rate of 90.9%). Of the nine implants in Group B, eight were successful and one failed (success rate of 88.9%).
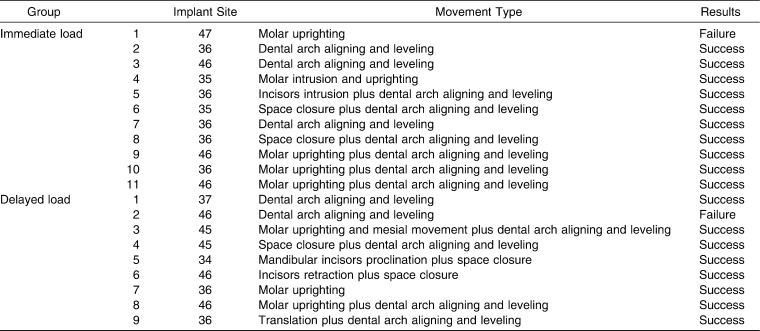
After a minimum of 2 years of clinical and radiographic observation, no additional implants were found to be unsuccessful. Table 1 illustrates all the details of the 20 implants showing each implant site, movement type, and final result.
Table 1.
Implant Survival: Results of the Immediate Load and Delayed Load Groups After a Minimum of 2 Years of Observation After Orthodontic Load
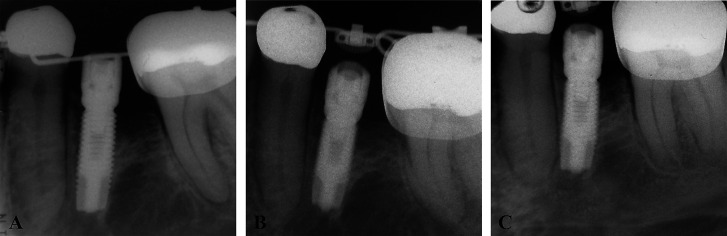
As for the radiographic evaluation, none of the successful cases in either group showed any radiolucent area indicating peri-implantar resorption. Bone ridge level appeared located above the second spiral ridge of the implant screw in all the successful implants of both groups (Figure 1).
Figure 1.
Radiographs taken (A) just after implant surgery, (B) 6 months after orthodontic and prosthetic loading, and (C) after 2 years and 7 months of follow-up. All the radiographs were taken using the paralleling method by means of radiographic positioners that standardized the distance (40 cm of focus/film distance) and angulation.
DISCUSSION
The posterior segments of the mandible were chosen as sites for the placement of single implants in this study as shown in Table 1. A recent systematic review revealed that those areas are the most well suited alveolar regions to receive immediately loaded implants.11 Further, the posterior mandibular area is where edentulism is more frequent because of caries12 or periodontal disease,13 and it is a less esthetically demanding area compared with the anterior dentoalveolar regions. Also, a greater success rate of immediate occlusal load14,15 has been reported for implants placed in the mandibular posterior area with respect to the posterior area of maxilla, which is more susceptible to failures.16–18 The magnitude of force applied was the same described by several authors as being secure.2,5,19–27 Moreover, a 200 g force is considered appropriate to various orthodontic movements and potentially safe.
In this study, the handles of two dental mirrors were used to evaluate whether there was absence of implant mobility. Although this evaluation method is considered to have low sensitivity,28 other evaluation methods, like the Periotest and resonance frequency analysis (RFA), have also shown poor quantitative information.29 In addition, the RFA showed the same sensitivity as the manual test.30
In an extensive systematic review on reinforcement of anchorage during orthodontic treatment using implants and other surgical methods, Skeggs et al.1 reported that evidence regarding the favorable outcomes of immediate orthodontic load in osseointegrated implants is reasonable, although they recommended further studies in adult human patients. The present RCT with 13 patients and 20 osseointegrated implants contributed to preliminary data about this issue in human subjects instead of animal or laboratory studies,2 and it compared immediate vs delayed orthodontic and prosthetic load in single mandibular implants.
The present study found no difference in the success rate of implants immediately loaded with orthodontic forces and implants where the application of the orthodontic force was delayed after the recommended 4 months for osteointegration (91% vs 89%, respectively). Both clinical and radiographic assessments of successful implants in both groups revealed favorable outcomes. Therefore, the results of the present RCT confirm the observations reported in the systematic review by Skeggs and coworkers.1 Nevertheless, the hazard of the occlusal force needs to be evaluated apart from the orthodontic force applied to the implants, and a follow-up study is needed using a large sample, according to a standardized magnitude of force.
Although the minimum follow-up time was 2 years, the sample was observed for a mean of 3.4 years (SD = 1.3) to validate the implants' stability for a longer period. All 18 implants that were successful at the first 6-month evaluation were still in perfect condition in terms of the aforementioned criteria.
Roberts et al.2 reported the first observations about the use of immediate orthodontic load in osseointegrated implants. The success rate in that study was 0% within the four evaluated implants. In that study the implants were placed in rabbit femurs, so a comparison with the present study is not possible because the evaluation was performed in animals and not in humans. Moreover, the establishment of initial stability of implants of any magnitude was not determined, and this could have interfered with the results. Also, the comparison of the outcomes of the present study with those of previous investigations that used immediate orthodontic load in osseointegrated implants placed in human subjects is challenging because of the different methodologies used. The number of implants receiving immediate orthodontic load in the present study is greater than in previously reported studies,3,5 and the present trial was conceived as a prospective randomized investigation. The utilization of implants not only for orthodontic anchorage but also as support for future prosthetic crowns represents another variable that distinguishes the present study from others that evaluated immediate orthodontic load. As a consequence, the treatment plan for each of the patients enrolled in the present study did not include implant removal at the time the orthodontic treatment was accomplished.
Although the initial results from this study are encouraging, the long-term outcomes require further investigation with larger samples. The follow-up evaluation of the samples investigated here provides useful insights on the effects of continued orthodontic treatment, including immediately loaded implants. This result reinforces the findings of Chen et al.31 They created finite element models of the human mandible and showed that typical orthodontic loads are several orders of magnitude lower than the peak occlusal loads of mastication. Thus, occlusal loading is much more likely to precipitate implant failure than a routine orthodontic load.
CONCLUSIONS
Of the 11 evaluated implants under immediate orthodontic load, 10 were successful after a minimum of 2 years of clinical and radiographic observation, resulting in a success rate of 91%.
Of the nine implants that received orthodontic load after 4 months of healing, eight were successful, resulting in a success rate of 89%.
The reduction in waiting time for application of orthodontic load may not negatively influence the success of osseointegrated implants bearing provisional crown restorations.
REFERENCES
- 1.Skeggs R. M, Benson P. E, Dyer F. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database Syst Rev. 2007 doi: 10.1002/14651858.CD005098.pub2. Issue 3. Art. No.: CD005098. [DOI] [PubMed] [Google Scholar]
- 2.Roberts W. E, Smith R. K, Zilberman Y, Mozsary P. G, Smith R. S. Osseous adaptation to continuous loading of rigid endosseous implants. Am J Orthod. 1984;86:95–111. doi: 10.1016/0002-9416(84)90301-4. [DOI] [PubMed] [Google Scholar]
- 3.Karaman A. I, Basciftci F. A, Polat O. Unilateral distal molar movement with an implant-supported distal jet appliance. Angle Orthod. 2002;72:167–174. doi: 10.1043/0003-3219(2002)072<0167:UDMMWA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Trisi P, Rebaudi A. Progressive bone adaptation of titanium implants during and after orthodontic load in humans. Int J Periodontics Restorative Dent. 2002;22:31–43. [PubMed] [Google Scholar]
- 5.Trisi P, Rebaudi A. Peri-implant bone reaction to immediate, early, and delayed orthodontic loading in humans. Int J Periodontics Restorative Dent. 2005;25:317–329. [PubMed] [Google Scholar]
- 6.Chiapasco M, Gatti C. Implant-retained mandibular overdentures with immediate loading: a 3- to 8-year prospective study on 328 implants. Clin Oral Implants Res. 2003;5:29–38. doi: 10.1111/j.1708-8208.2003.tb00179.x. [DOI] [PubMed] [Google Scholar]
- 7.Hruska A, Borelli P, Bordanaro A. C, Marzaduri E, Hruska K. L. Immediate loading implants: a clinical report of 1301 implants. J Oral Implantol. 2002;28:200–209. doi: 10.1563/1548-1336(2002)028<0200:ILIACR>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Lorenzoni M, Pertl C, Zhang K, Wimmer G, Wegscheider W. A. Immediate loading of single-tooth implants in the anterior maxilla. Preliminary results after one year. Clin Oral Implants Res. 2003;14:180–187. doi: 10.1034/j.1600-0501.2003.140207.x. [DOI] [PubMed] [Google Scholar]
- 9.Calandriello R, Tomatis M, Vallone R, Rangert B, Gottlow J. Immediate occlusal loading of single lower molars using Brånemark System Wide-Platform TiUnite implants: an interim report of a prospective open-ended clinical multicenter study. Clin Implant Dent Relat Res. 2003;5(suppl 1):74–80. doi: 10.1111/j.1708-8208.2003.tb00018.x. [DOI] [PubMed] [Google Scholar]
- 10.Shapiro P. A, Kokich V. G. Uses of implants in orthodontics. Dent Clin North Am. 1988;32:539–550. [PubMed] [Google Scholar]
- 11.Nkenke E, Fenner M. Indications for immediate loading of implants and implant success. Clin Oral Implants Res. 2006;17(suppl 2):19–34. doi: 10.1111/j.1600-0501.2006.01348.x. [DOI] [PubMed] [Google Scholar]
- 12.Carlos J. P, Gittelsohn A. M. Longitudinal studies of the natural history of caries II: a life-table studies of caries incidence in the permanent teeth. Arch Oral Biol. 1965;10:739–751. doi: 10.1016/0003-9969(65)90127-5. [DOI] [PubMed] [Google Scholar]
- 13.Wood W. R, Greco G. W, McFall W. T. Tooth loss in patients with moderate periodontitis after treatment and long-term maintenance care. J Periodontol. 1989;60:516–520. doi: 10.1902/jop.1989.60.9.516. [DOI] [PubMed] [Google Scholar]
- 14.Balleri P, Cozzolino A, Ghelli L, Momicchioli G, Varriale A. Stability measurements of osseointegrated implants using Osstell in partially edentulous jaws after one year of loading: a pilot study. Clin Implant Dent Relat Res. 2002;4:128–132. doi: 10.1111/j.1708-8208.2002.tb00162.x. [DOI] [PubMed] [Google Scholar]
- 15.Finne K, Rompen E, Toljanic J. Clinical evaluation of a prospective multicenter study on 1-piece implants: part 1: marginal bone level evaluation after 1 year of follow-up. Int J Oral Maxillofac Implants. 2007;22:226–234. [PubMed] [Google Scholar]
- 16.Jaffin R. A, Berman C. L. The excessive loss of Branemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 17.Glauser R, Rée A, Lundgren A, Gottlow J, Hãmmerle C. H, Schãrer P. Immediate occlusal loading of Branemark implants applied in various jawbone regions: a prospective, 1-year clinical study. Clin Implant Dent Relat Res. 2001;3:204–213. doi: 10.1111/j.1708-8208.2001.tb00142.x. [DOI] [PubMed] [Google Scholar]
- 18.Weng D, Jacobson Z, Tarnow D, Hürzeler M. B, Faehn O, Sanavi F, Barkvoll P, Stach R. M. A prospective multicenter clinical trial of 3i machined-surface implants: results after 6 years of follow-up. Int J Oral Maxillofac Implants. 2003;18:417–423. [PubMed] [Google Scholar]
- 19.Gray J. B, Steen M. E, King G. J, Clark A. E. Studies on the efficacy of implants as orthodontic anchorage. Am J Orthod. 1983;83:311–317. doi: 10.1016/0002-9416(83)90226-9. [DOI] [PubMed] [Google Scholar]
- 20.Linder-Aronson S, Nordenram A, Anneroth G. Titanium implant anchorage in orthodontic treatment: an experimental investigation in monkeys. Eur J Orthod. 1990;12:414–419. doi: 10.1093/ejo/12.4.414. [DOI] [PubMed] [Google Scholar]
- 21.Wehrbein H, Diedrich P. Endosseous titanium implants during and after orthodontic—an experimental study in the dog. Clin Oral Implants Res. 1993;4:76–82. doi: 10.1034/j.1600-0501.1993.040203.x. [DOI] [PubMed] [Google Scholar]
- 22.Southard T. E, Buckley M. J, Spivey J. D, Krizan K. E, Casko J. S. Intrusion anchorage potential of teeth versus rigid endosseous implants: a clinical and radiographic evaluation. Am J Orthod Dentofacial Orthop. 1995;107:115–120. doi: 10.1016/s0889-5406(95)70125-7. [DOI] [PubMed] [Google Scholar]
- 23.Drago C. J. Use of osseointegrated implants in adult orthodontic treatment: a clinical report. J Prosthet Dent. 1999;82:504–509. doi: 10.1016/s0022-3913(99)70045-4. [DOI] [PubMed] [Google Scholar]
- 24.Majzoub Z, Finotti M, Miotti F, Giardino R, Aldini N. N, Cordioli G. Bone response to orthodontic loading of endosseous implants in the rabbit calvaria: early continuous distalizing forces. Eur J Orthod. 1999;21:223–230. doi: 10.1093/ejo/21.3.223. [DOI] [PubMed] [Google Scholar]
- 25.Saito S, Sugimoto N, Morohashi T, et al. Endosseous titanium implants as anchors for mesiodistal tooth movement in beagle dog. Am J Orthod Dentofacial Orthop. 2000;118:601–607. doi: 10.1067/mod.2000.110636. [DOI] [PubMed] [Google Scholar]
- 26.Re S, Cardaropoli D, Corrente G, Abundo R. Bodily tooth movement through the maxillary sinus with implant anchorage for single tooth replacement. Clin Orthod Res. 2001;4:177–181. doi: 10.1034/j.1600-0544.2001.040308.x. [DOI] [PubMed] [Google Scholar]
- 27.Aldikaçti M, Açikgöz G, Türk T, Trisi P. Long-term evaluation of sandblasted and acid-etched implants used as orthodontic anchors in dogs. Am J Orthod Dentofacial Orthop. 2004;125:139–147. doi: 10.1016/S0889540603006292. [DOI] [PubMed] [Google Scholar]
- 28.Romeo E, Chiapasco M, Lazza A, Casentini P, Ghisolfi M, Iorio M, Vogel G. Implant-retained mandibular overdentures with ITI implants. Clin Oral Implants Res. 2002;13:495–501. doi: 10.1034/j.1600-0501.2002.130508.x. [DOI] [PubMed] [Google Scholar]
- 29.Cehreli M. C, Akkocaoglu M, Comert A, Tekdemir I, Akca K. Human ex vivo bone tissue strains around natural teeth vs. immediate oral implants. Clin Oral Implants Res. 2005;16:540–548. doi: 10.1111/j.1600-0501.2005.01140.x. [DOI] [PubMed] [Google Scholar]
- 30.Meredith N, Shagaldi F, Alleyne D, Sennerby L, Cawley P. The application of resonance frequency measurements to study the stability of titanium implants during healing in the rabbit tibia. Clin Oral Implants Res. 1997;8:234–243. doi: 10.1034/j.1600-0501.1997.080310.x. [DOI] [PubMed] [Google Scholar]
- 31.Chen J, Chen K, Garetto L, Roberts W. E. Mechanical response to functional and therapeutic loading of a retromolar endosseous implant used for orthodontic anchorage to mesially translate mandibular molars. Implant Dent. 1995;4:246–258. doi: 10.1097/00008505-199500440-00004. [DOI] [PubMed] [Google Scholar]