Abstract
Objective
To explore the various stakeholders’ perspectives on barriers and facilitators for medication adherence among patients with cardiovascular diseases (CVDs) and diabetes mellitus (DM)in India.
Design
Systematic review of qualitative studies.
Data sources
A comprehensive systematic search was conducted in Medline, Cochrane Library, Science Direct and Google Scholar from January 2010 to July 2020. We included all qualitative peer-reviewed studies, reporting barriers and facilitators of medication adherence, from India, for our current review.
Data extraction and synthesis
Data extraction was performed by two independent authors who also assessed the quality of included studies using the Critical Appraisal Skills Programme criteria. This qualitative evidence synthesis adhered to the enhancing transparency in reporting the synthesis of qualitative research checklist
Results
In total, 18 studies were included. Major barriers reported were lack of understanding about the disease, complications related to non-adherence, followed by forgetfulness, lack of family support and risk communication. Health system-related barriers such as accessibility, affordability and acceptability were also reported by majority of the studies. Creation of peer support groups, digital reminder systems, integration of native Indian systems of India, physiotherapy and geriatric clinics at the primary healthcare level and innovations in patient care were suggested to counter these barriers in medication adherence.
Conclusion
Such patient-specific targeted interventions need to be developed to achieve better control among patients with CVD and DM.
PROSPERO registration number
CRD42020199529.
Keywords: qualitative research, preventive medicine, primary care, coronary heart disease, diabetes & endocrinology
Strengths and limitations of this study.
This is the first review exploring factors associated with drug adherence among patients with cardiovascular diseases and diabetes mellitus in India.
We have adhered to the enhancing transparency in reporting the synthesis of qualitative research statement ensuring transparency and reproducibility of the study findings.
We cannot rule out dissemination bias, causing selective reporting of studies with more non-adherence to medications.
We focused primarily on the patient and provider perspective on medication adherence. Hence, we cannot comment on the organisational or political influences on the adherence to long-term therapies.
The sample size of the included studies can be considered relatively low (median sample size—30).
Introduction
Cardiovascular diseases (CVDs) are the leading cause of mortality globally and in India.1 2 More than a quarter, (28%) of all-cause mortality in India is attributed to CVDs, where ischaemic heart disease and stroke constitute the majority (83%).3 On the other hand, India ranks second after China in the global diabetes epidemic, with a prevalence of around 10%.4 Both diabetes mellitus (DM) and hypertension have long been recognised as independent risk factors for CVDs, whereas adherence to prescribed hypoglycaemic and antihypertensive drug therapies have significantly reduced the risk.5–8 At least half of these chronic disease patients stop taking medications within a year, often without informing their provider. With further non-adherence and attrition over time, medication adherence has emerged as a significant public health priority.9
Medication adherence is defined as the extent to which a person’s behaviour coincides with the agreed medication regimen or health advice from a healthcare provider.10 It has three components: initiation (when the patient takes the first dose of prescribed medication), implementation (the extent to which a patient’s actual dosing corresponds to the prescribed dosing regimen) and discontinuation (when no more doses are taken after that).11 Medication adherence is of growing interest to clinicians, healthcare systems and other stakeholders. There is soaring evidence that links non-adherence with lower quality of life, adverse clinical events, increased need for medical interventions and mortality, thus giving rise to avoidable out-of-pocket expenditure in health.12 Patients with non-adherent hypertensive and stable coronary heart disease (CHD) have a four to five times higher risk of developing CHD and death, when compared with adherent patients.13 14 Similarly, the likelihood of hospitalisation is doubled among DM and hypertensive patients who are non-adherent to prescribed therapies compared with the general population. Despite recent advancements in pharmacologic treatment and technology to treat and monitor patients with DM and CVD, medication adherence is of particular concern in low-and-middle-income countries (LMIC) like India, where accessibility and affordability issues are still pertinent.3 15
Barriers to adherence are often related to patient, medication, provider, and health system factors, with interactions between them.16 17 Patient factors that influence adherence include poor health literacy, faulty cultural beliefs regarding medication effectiveness and religious healing practices.17 Low income, forgetting to take medication, and perceptions regarding pills like safety concerns, convenience and necessity add to the above list. Inadequate knowledge about a drug and its use, not being convinced of the need for medication, fear of adverse effects and long-term treatment regimens also prompt medication discontinuation.15 Clinician factors include: failure to recognise non-adherence, prescription of complex and multidrug regimens, ineffective communication of benefits of medications and excluding patients in the treatment decision-making process.17 Health system factors comprise limited insurance coverage, poor coordination of care between inpatient and outpatient settings and inadequate communication between prescribers (ie, specialists and primary care clinicians). In addition, the caregivers’ aspects also become relevant in determining patients’ adherence, as it is proven that patients with CVD with caregivers are more likely to be adherent to medications.18 Hence, identifying patient-specific barriers and adopting suitable techniques to overcome them is imperative to improve medication adherence. A few successful facilitators that has helped us overcoming these barriers include: inclusion of medication counsellors into the continuum of care to guide patients, single-pill fixed-dose combinations, training pharmacists as coaches for drug therapies, building peer groups for chronic conditions and developing information systems in the follow-up of patients.19
Quantitative studies have extensively studied medication adherence and its determinants. They do not, however, uncover life circumstances that may influence adherence from the patient perspective. A systematic review of qualitative studies will provide us with a better understanding of the barriers and facilitators from the first-hand experiences of patients, healthcare providers and caregivers.20 Qualitative evidence synthesis, a novel research method, brings together the available qualitative evidence from primary studies through a systematic review process. Despite the conceptually rich evidence generated from primary qualitative studies, a qualitative evidence synthesis can aid policymakers and clinicians to get an overall insight into the findings, thereby enabling them to address all subtle and sensitive issues that most primary studies encounter. The findings from this qualitative evidence synthesis can guide various stakeholders to frame specific policy recommendations in non-communicable disease care.21 Thus, we undertook this review to understand the perspective of various stakeholders (patients, caregivers and healthcare providers) on the barriers and facilitators for medication adherence among patients with CVD and DM in India. We also explored the suggestions and solutions provided by these stakeholders in overcoming the reported barriers.
Methods
This review was performed by adhering to the ‘enhancing transparency in reporting the synthesis of qualitative research (ENTREQ)’ statement (online supplemental file 1)22 We registered our protocol in the PROSPERO database. We also searched PROSPERO and Cochrane to ensure that no similar review protocol has been reported. We also performed a preliminary search to ensure that no previous reviews of our similar topic targeting the Indian population were published.
bmjopen-2021-055226supp001.pdf (101.1KB, pdf)
Study design
We performed a qualitative evidence synthesis of all available qualitative studies on the barriers and facilitating factors for medication adherence among patients with CVD and DM in India. This review would help to aggregate the evidence of peer-reviewed articles and build an organised empirical research outline based on prior knowledge.
Eligibility criteria
Study type
We have included peer-reviewed qualitative studies conducted in India for our current review. Furthermore, qualitative evidence from other mixed methods studies was screened for eligibility and included in the qualitative component was relevant to our review. In addition, we included studies using qualitative techniques for data collection such as focused group discussion (FGD), in-depth interviews (IDI) and key informant interviews.
Participant type
We have included the studies reporting the barriers and facilitators of medication adherence from patients’ perspectives (CVD and DM), family members, healthcare workers (HCWs) or health system policymakers perspectives. HCWs were defined as per WHO recommendation as ‘all the persons involved in the actions whose primary intent is to enhance the health’."23
Outcome
The phenomenon of interest was to explore the barriers and facilitators for medication adherence among patients with CVD and DM in India. We also explored the possible suggestions and solutions to address the barriers and improve compliance, as experienced by the patients, caregivers, family members, HCWs and other relevant stakeholders.
Exclusion criteria
We have excluded the studies not available in English, books, conference abstracts, grey literature or editorial comments. We have also excluded the studies reporting only quantitative data such as cross-sectional surveys, case–control, cohort studies or intervention trials.
Search strategy
We have conducted a comprehensive and systematic search in databases and search engines such as Medline, Cochrane Library, ScienceDirect and Google Scholar. A combination of medical subject heading and free-full text terms was used for carrying out a literature search. The detailed search strategy and search results in the databases mentioned above and search engines are provided in online supplemental file 2. In addition to this, we also checked the reference list of primary studies obtained via electronic search and included articles relevant to our review and analysis. The search was conducted in all above-mentioned databases from January 2010 to July 2020. Our search timeline was restricted to the past decade alone to ensure the identification of emerging issues.
bmjopen-2021-055226supp002.pdf (32.4KB, pdf)
Study selection process
Two investigators (YK and TR) independently performed the literature search, screened the title and abstract of all the identified studies and retrieved the full text for articles relevant to our review. Further full-text screening of the retrieved articles was done again independently by the two investigators (YK and TR) to select the studies matching the eligibility criteria of our review. Disagreements during this process between the two investigators were resolved through consultation with a third investigator (SR).
Data extraction and management
After the study selection, two investigators (YK and TR) independently extracted the relevant data and study characteristics onto a predetermined data extraction format. Data entry was double checked for accuracy by a third investigator (SR) by comparing the data presented in the review and individual study reports. As a result, we have extracted the following study characteristics: general information such as the name of the first author, the country in which the study was done and year of publication, in the methods section, data collection period, study design, study participants, sample size, sampling technique and data collection procedure. In addition, barriers, facilitators, suggestions and solutions to medication adherence were identified systematically.
Quality assessment
Two investigators (YK and SR) independently performed the quality check using the Critical Appraisal Skills Programmecriteria.24 This checklist has been widely used for assessing the quality of studies included in Qualitative Evidence synthesis.25 This checklist helps us to determine the coherence of included studies with the quality appraisal standard for qualitative studies. This checklist consists of 10 questions concerning the study’s clarity, methodology and results to rank the included studies. Subsequently, these studies were stratified into high quality (three stars for studies scoring 8 to 10 points), medium quality (two stars for studies scoring 4 to 7 points) and low rate (one star for studies scoring 0 to 3 points). We did not exclude the low-quality studies, but the interpretation of results was made with caution. Disagreements during the quality assessment process were resolved by discussion with the third investigator (TR).
Data analysis
We analysed and reported the findings in separate clusters such as patients, caregivers, family members, HCWs and policymakers to demonstrate the differences among these subgroups. We have adopted a thematic framework analysis to analyse and synthesise the data. Thematic framework analysis has been helpful as the evidence was primarily descriptive and improved our understanding of the barriers and facilitators in medication adherence among patients with CVD and DM. This framework synthesis has five stages of synthesising the qualitative data.
First stage—familiarisation with the data
Primary investigator (YK) did the process of familiarisation with data by reviewing all the selected articles against the objective of our review and found the recurrent themes across the included studies.
The second stage—identifying the thematic framework
The investigators used a predetermined thematic framework developed using literature to guide the thematic analysis. The final framework comprised of a detailed list of facilitators and barriers for medication adherence and also solutions to address the issue.
Third stage—indexing
Two independent investigators (YK and SR) read the extracted information and searched for themes as per the predetermined thematic framework and found additional emerging themes. The framework underwent several revisions as and when a new theme emerged, after discussing with the entire team of investigators. Next, all the studies were completely read and examined till there was no new emergent theme. Coding of the data was then done as per the themes identified in our analysis. Finally, each preliminary study indexing was done using the codes related to the thematic framework. Whenever appropriate, sections of the studies were indexed with one or more codes.
Fourth stage—charting
The investigators then sorted the data based on themes and presented these themes in the tabular format (chart). The rows and columns of the table indicate the themes related to the studies, which enabled us to compare the study findings across various themes and subthemes.
Fifth stage—mapping and interpretation
The investigators then used these charts to define the concepts identified and finally mapped the nature and range of the phenomena. Our review explored the associations between the various emerging themes and helped in clarifying the findings. Finally, we mapped and interpreted the findings in line with our objectives and emergent themes.
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting or dissemination plans of our research.
Results
Study selection
A comprehensive and systematic search was done to identify the relevant studies from January 2010 to July 2020. In total, we identified 1187 citations, and after the removal of duplicates from multiple databases, 982 records were screened for their title and abstract and assessed for eligibility. From these records, we retrieved 33 articles, and after going through the full text of these articles, 18 studies were included in the review (figure 1).26–43
Figure 1.
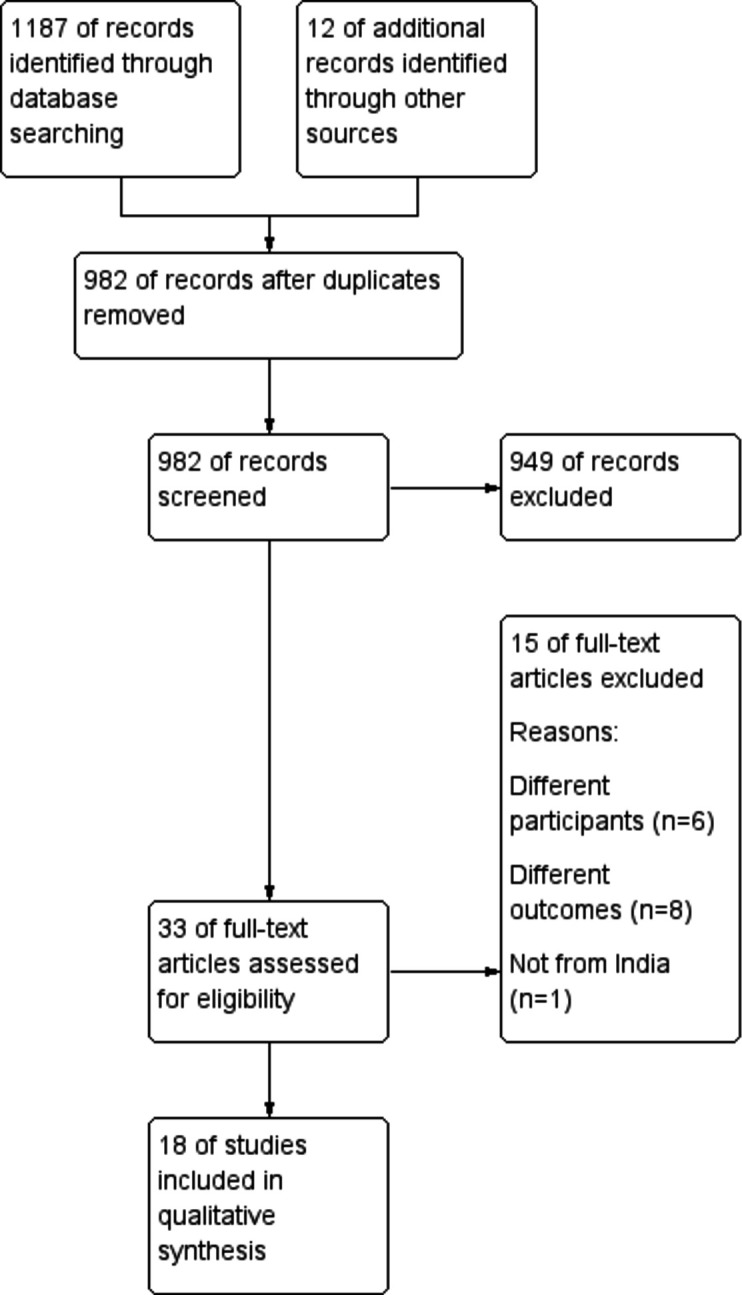
Flowchart showing the search strategy and selection of studies.
Characteristics of the studies included
Characteristics of the included studies are reported in table 1. Of the 18 studies included, 9 (50%) were from the southern region, followed by 7 (38%) from the northern part of India. The mean age of the participants ranged from 25 to 76 years. The typology of the studies comprised of IDIs and FGDs. The study participants were primarily patients with diabetes, hypertension or any CVDs (to explore the patient perspective), and HCWs (four studies) providing care to them (to obtain the provider perspective). The total sample size of the included studies ranged from 6 to 100. The majority (10 of the included studies) were from the community, while the rest were either facility-based or had participants from ongoing trials. Four of the included studies used software for analysing the qualitative data, while the rest followed manual methods. Most of the included studies (14 out of 18) had high-quality evidence.
Table 1.
Characteristics of the studies included (N=18)
| Serial number | Author and year | State | Data collection method | Study participants | Study setting | Approach | Coding | Theoretical framework used | Method of analysis | Sample size | Mean age in years | Study quality |
| 1. | Agarwal et al 201926 | Kerala | IDI | Clinical and administrative staff | Facility based | NR | Inductive | NR | Dedoose Software |
21 | NR | *** |
| 2. | Dhar 201627 | Delhi | IDI | Hypertensive women aged 35–59 years | Community based | NR | Inductive | Yes | Manual content analysis | 30 | 48 | *** |
| 3. | George et al 201628 | Karnataka | IDI | Physicians providing non-communicable disease care | Community based | NR | Inductive | NR | Manual content analysis | 36 | 46 | *** |
| 4. | Gupta et al 201929 | Rajasthan | IDI | Hypertensive women | Facility based | NR | NR | NR | Manual content analysis | 30 | 56 | ** |
| 5. | Gupta et al 202030 | Haryana | IDI | Hypertension patients | Facility based | NR | NR | NR | Manual content analysis | 100 | 38–76 | *** |
| 6. | Jayanna et al 201931 | Karnataka | IDI & FGD |
Diabetes and hypertension patients | Facility based | NR | NR | Yes | Manual content analysis | 10 IDI+20 FGDs | NR | *** |
| 7. | Krishnamoorthy et al 201832 | Puducherry | IDI & KII | Diabetes and hypertension patients and healthcare workers | Community based | NR | Inductive | NR | Manual content analysis | 6 IDI+4 KII | NR | *** |
| 8. | Kusuma 201033 | Delhi | KII & FGD | Recent and settled migrants having hypertension inhabited in Delhi | Community based | NR | NR | NR | Manual content analysis | 14 (KII)+20 (FGD) | 38–50 (KII) & 25–40 (FGD) | *** |
| 9. | Miller et al 201734 | Delhi | IDI | Cardiovascular disease patients | Trial based | Descriptive | NR | NR | Manual content analysis | 14 | NR | *** |
| 10. | Newtonraj et al 201735 | Tamil Nadu | Personal interviews | Hypertensive patients | Community based | NR | NR | NR | Manual content analysis | 40 | NR | ** |
| 11. | Nimesh et al 201936 | Madhya Pradesh | IDI | Individuals with diabetes | Community based | NR | Inductive | Yes | Manual content analysis | 60 | 52 | *** |
| 12. | Patti et al 202037 | Orissa | IDI | Primary care physicians | Facility based | NR | NR | NR | Manual content analysis | 17 | 40 | *** |
| 13. | Rani and Shriraam 201938 | Tamil Nadu | FGD | Individuals with diabetes | Community based | Descriptive | NR | NR | Manual content analysis | 50 | 50 | ** |
| 14. | Salaam et al 201939 | Andhra Pradesh | IDI | Patients with cardiovascular disease | Community based | NR | NR | Yes | NVivo version 11 software | 12 | 62 | *** |
| 15. | Satish et al 201940 | West Bengal | FGD | Patients with hypertension and/or diabetes | Trial based | NR | NR | Yes | Manual content analysis | 70 | 53 | *** |
| 16. | Thakur et al 201641 | Chandigarh | IDI & FGD | Coronary artery disease patients | Facility based | NR | NR | NR | Manual Thematic analysis | 20 | NR | * |
| 17. | Venkatesan et al 201842 | Tamil Nadu | IDI | Healthcare workers | Community based | NR | NR | NR | Anthropac software | 10 | NR | *** |
| 18. | Wood et al 201543 | Hyderabad and Delhi | IDI | Patients with cardiovascular diseases | Trial based | NR | NR | Yes | NVivo software | 52 | 57 | *** |
FGD, focused group discussion; IDI, in depth Interview; KII, key informant interview; NR, not reported.
Narrative synthesis
Findings from our review showed that significant factors contributing to adherence were grouped under three themes: patient-related, family-related and health system-related factors. The barriers, facilitators and suggestions to improve medication adherence were summarised under these three themes.
Barriers in medication adherence
Table 2 shows the thematic framework analysis related to barriers in medication adherence among patients with CVD and DM. All the 18 included studies have explored and reported on these barriers.
Table 2.
Thematic framework analysis for summarising barriers in medication adherence experienced by CVD and DM patients in India
| Main theme/subthemes | Barriers in medication adherence | Studies |
| Patients | 1. Lack of awareness/knowledge: lack of knowledge and understanding about the disease, its complications and treatment among the patients | 4 27–29 32 33 35 37 41–43 |
| 2. Forgetfulness: patients forget to take medicine because of busy schedule | 4 27 29 30 38 41–43 | |
| 3. Misconception about medications: Patient has wrong perception about the medications, especially about its side effects and quality | 4 28 30 37–39 42 | |
| 4. Preference to alternate system of medicine: patients prefer taking herbal and other alternate system of medicines for their condition | 4 28 42 | |
| 5. Ill effects of substance abuse: patients have difficulty in adhering to medications during the bout of tobacco or alcohol consumption | 31 32 | |
| 6. Effect of side effects: patients stop their medication once they develop side effects related to the drugs | 42 43 | |
| 7. Stress: patients developing stress due to personal or work-related problems are more non-adherent to medications | 32 | |
| 8. Stigma: patients feel stigmatised in revealing their disease status to other family/friends leading to lack of support from them | 32 | |
| Care team (Frontline care providers—healthcare professionals, family members and others) |
1. Family support: lack of physical, emotional and social support as the family members are pre-occupied with domestic works, crisis, other priorities and commitments | 27 28 30 32 33 35 38 43 |
| 2. Risk communication: poor risk communication or counselling to patients and family members about non-adherence to medication by the treating physicians | 27–29 32 34 41 | |
| 3. Physician attitude: lack of respect, empathy, communication and attention towards patients by the treating physicians | 27 29 31 33 | |
| Healthcare organisation (infrastructure/resources) |
1. Affordability: patients lose their daily wages due to inconvenient consultation timings in public facilities, which is aggravated by travel costs due to poor access, and higher medication costs while preferring private facilities | 26–31 33 34 36 39–43 |
| 2. Accessibility: lack of access to healthcare facilities (more distance) requiring longer travel and waiting time. | 4 27–35 41–43 | |
| 3. Availability: non-availability of essential medicines in public healthcare facilities | 27 31 33–35 37 39 43 | |
| 4. Acceptability: medications from public health facilities are not acceptable to the patients due to poorer quality | ||
| 5. Overburdening of primary health centres: burdening of primary health facilities lead to time constraints in patient counselling regarding medication adherence | 31 32 34 37 42 |
CVD, cardiovascular disease; DM, diabetes mellitus.
Patient-related factors
Significant patient-related barriers (10 studies) reported were lack of knowledge or understanding about the disease, its complications and the treatment schedule, followed by forgetfulness to take medicines (seven studies). Reasons provided for the same were the patients’ busy schedule, laziness or forgetting to take the medication while travelling out-of-station. Patients have also reported certain misconceptions about the medicines like the risk of long-term neurological illness because of medication intake, inferior quality of drugs provided in hospitals and wrong perception about stopping the medications once the patient feels normal. Patients in some studies have reported that they practice alternate systems of medicine such as herbal medicines and avoid taking allopathic medicines, leading to poorer control. Substance use such as alcohol or tobacco use, side effects related to drugs, stress and stigma were reported to be other barriers
Family-related factors
The patients and providers have reported lack of family support as a significant contributing factor for non-adherence. In addition, the lack of social and emotional support to the patients further promote non-adherence. Domestic works, personal priorities, commitments or other family-related issues hinder the family members from adequate support.
Health system-related factors
In most of these studies, providers were also interviewed to understand the health system barriers responsible for non-adherence among patients with CVD and DM. Healthcare providers and stakeholders interviewed, in almost all these studies, have reported affordability, accessibility and acceptability as major factors hindering medication adherence. Affordability is of prime concern among patients seeking healthcare from private facilities. Though there are no direct medical costs involved in availing services from the public sector or primary healthcare centres, direct non-medical costs such as transport (due to poor accessibility) and indirect costs such as loss of wages (due to inconvenient consultation timing) were contributory. In addition, studies reported that patients, in general, had wrong perceptions about the quality of medications provided in public facilities, influencing them to choose private health facilities, including those belonging to lower socioeconomic status. Lack of risk communication, counselling or empathy by the physicians mainly due to overburdened public health facilities and time constraints were the other health system-related barriers reported by the providers and patients.
Facilitators in medication adherence
Facilitators in medication adherence were also summarised using the pre-existing thematic framework (table 3). In total, 10 studies have explored the facilitators in medication adherence from the patient or providers’ perspective.
Table 3.
Thematic framework for summarising facilitators in medication adherence experienced by CVD and DM patients in India
| Main theme/subthemes | Facilitators in medication adherence | Studies |
| Patients | 1. Self-awareness and fear: patient’s understanding about medicine adherence and fear about complications of non-adherence keeps them healthy | 4 32 34 37 40 43 |
| 2. Medicine reminder system: separate pill boxes/cases/covers, personalised shelf and maintaining drug record notebook helps them in remembering daily doses | 4 27 32 34 | |
| 3. Integrating drug intake with the daily routine: fixed time for medicine intake, separate place for keeping drug, and making arrangements during travel helps them in adherence | 27 32 | |
| 4. Positive peer influence: good adherence to medication by the patient’s peers motivates the patient to be compliance to their own drug intake | 29 32 | |
| Care team (Frontline care providers—healthcare professionals, family members and others) |
1. Family support: constant reminders by family members for drug intake | 27 30 32 34 43 |
| 2. Past adverse experiences: death of patients’ own family members due to complications of the condition has motivated them to adhere to medication | 27 32 | |
| 3. Healthcare provider counselling and empathy: patients described that counselling from their healthcare providers has motivated them to remain adherent | 4 33 34 37 39 | |
| 4. Trust in physician: adherence is more when a positive rapport and trust is established between the patient and healthcare providers. | 27 32 40 | |
| Healthcare organisation (infrastructure/resources) |
1. Dedicated pill boxes/covers: provision of different medications in separate boxes/covers in the healthcare facility has helped as the patient to remember which medication to take at what time | 32 43 |
| 2. Combination drugs (polypills): polypills had the following advantages to facilitate the medication adherence: a smaller number of pills, lower frequency, less chance of forgetting, potential for lower cost and convenient simpler regimen | 39 43 | |
| 3. Availability of medications: proper pharmacy inventory control and stock delivery has aided in medication adherence | 34 | |
| Environment (regulatory, market and policy framework) |
1. NGO support: Patients have reported that sharing their concerns and receiving counselling from NGO/health officers acted as a facilitator for drug intake | 4 43 |
CVD, cardiovascular disease; DM, diabetes mellitus; NGO, non-governmental organisation.
Patient-related factors
Most of the studies (five studies) reported fear of complications due to non-adherence and self-perception of being healthy (once they adhere to the medications) as the significant facilitators. In addition, having a reminder system in the form of reminder notebooks, separate pillboxes/cases/covers or personalised shelf facilitates the patients in adhering to the medications. Some studies have also reported that integrating drug intake into daily routine activities and peer influence acts as good facilitators for compliance with medications.
Family-Related factors
Family support was reported as a major facilitating factor for compliance with medication. Apart from the support, adverse experiences in the past, such as death or severe complications among the family members, instilled fear in the patients and making them more compliant to the medications.
Health system-related factors
Barriers reported in some of the studies, such as empathy and counselling by healthcare providers, were considered facilitators by other studies’ patients. Another major facilitator from the health system side is the trust that patient has in their physician and their willingness to effectively follow advices related to self-care and adherence. Other familiar facilitators reported by the patients and providers were the use of dedicated pill cover/boxes for each drug provided in the clinic, linkage of health services with other non-governmental organisation (NGO) for provision of counselling and generating awareness, availability of medication and use of polypills.
Suggestions to improve medication adherence
Suggestions and solutions to enhance the compliance to medication were reported in 16 out of the 18 included studies based on either patient or provider’s perspective (table 4). Few suggestions were related to patients and family members, while the majority were related to the change in the health system.
Table 4.
Thematic framework for summarising suggestions to improve medication adherence among CVD and DM patients in India
| Main theme/subthemes | Suggestions to improve medication adherence | Studies |
| Patients | 1. Peer support groups: patients can motivate each other by forming support groups among themselves | 32 |
| 2. Digital reminder system: patient can use digital reminders such as watch, mobile phone to adhere to their drug schedule | 32 34 | |
| Care team (frontline care providers—healthcare professionals, family members and others) |
1. Social support: family members can be educated and asked to provide support by reinforcing compliance, reminding about drug intake, motivating them patients to avoid substance abuse | 26 27 32 36 43 |
| 2. Financial support: family members can provide financial support to cover the cost of medications, travel etc. | 29 | |
| 3. Regular training of healthcare workers: physicians and other healthcare workers involved in prescribing drugs and counselling should undergo regular training on standard treatment protocols | 28 31 34 37 40 | |
| 4. Team work approach: integration of AYUSH, mental health counsellors, physiotherapist and geriatric clinics at primary healthcare level | 28 34 37 | |
| Healthcare organisation (infrastructure/resources) |
1. Innovations in patient care: healthcare workers can make innovations like dedicated day for specific conditions (diabetes day, etc), dedicated counselling station/session with additional staff for detailing the importance of adherence and complications related to non-adherence, unique pill dispensing mechanism (colour coding) | 26 27 31 32 34 35 37 40 42 43 |
| 2. IEC/BCC/awareness campaigns: putting up of IEC materials and conducting campaigns on importance of adherence in public places and workplaces | 27–32 35 37 38 | |
| 3. Digitalising patient treatment record: digitalising a dedicated treatment record for each patient can help in better follow-up of the patient and improve adherence | 31 34 37 40 43 | |
| 4. Polypills: disseminating the advantages of polypills to healthcare professionals by CME/conferences and patients by public education campaigns; integration of polypills into clinical practice, etc | 39 43 | |
| Environment (regulatory, market and policy framework) |
1.Linkage of health services with NGO and community-based organisations: community members, volunteers, anganwadi workers, self-help groups and NGO workers can be trained in counselling the patients to improve medication adherence | 4 27 31–34 |
AYUSH, Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy; BCC, behaviour change communication; CME, Continuing Medical Education; IEC, information education and communication; NGO, non-governmental organisation.
Patient and family-related factors
Creating or joining a peer support group was one among the major suggestions related to the patients. Digital reminder systems using a watch or a mobile phone were other uncommon suggestions to improve medication adherence.
Health system-related factors
Innovations in patient care have been necessitated as an important factor to promote drug adherence. Some possible recommendations were hosting dedicated days for specific disease conditions to avoid overburdening the facilities, a dedicated counselling station for drug adherence during the clinic with separate human resources and a unique pill dispensing mechanism like colour coding, etc, were the other suggestions. In addition, information education and communication/behaviour change communication campaigns, digitalising the patient treatment records, linkage of healthcare services with NGOs or community-based organisations, regular training of HCWs and promotion of polypill use were other common suggestions offered by the healthcare providers.
Discussion
We conducted this review to integrate qualitative evidence on barriers and facilitators for medication adherence among patients with CVD and DM in India. We also further explored the suggestions to improve medication adherence. The studies included in our review involved a total of 636 participants (534 CVD and DM patients, 102 healthcare providers). The majority of the included studies were of high quality concerning study clarity, methodology and results. We summarised the three major themes: barriers, facilitators, suggestions and reported our findings under the following four subthemes: patients, care team, healthcare organisation and environment-related factors.
Comparison of findings with previous literature
Barriers in medication adherence
Major barriers were lack of patient’s understanding about the disease and its complications, forgetfulness and misconception about the medications. Lack of family support was seen as a major barrier from both patients’ and providers’ perspectives. In addition to these factors, stress and stigma were other contributory barriers. In addition to the above, adherence to medications was decided by patients’ cultural beliefs, perceived discrimination and social customs, which are largely prevalent in a culturally influenced country like India. A few studies have also shown evidence of improvement in medication adherence in settings, where efforts were taken to overcome the cultural barriers.44 We also found that the major health system-related barriers were lack of accessibility and availability, higher cost of medications and poor physician attitude. These findings were in line with the previous review conducted among South-East Asian patients with DM.44–46 In addition, our findings of patients related factors were found to be similar to other patients belonging to non-English-speaking Hispanic and south American ethnic groups, such as lack of understanding about their condition, along with additional stress and stigma.47–49
Facilitators in medication adherence
Fear of complications, self-perception of being healthy, having a reminder system were reported as major facilitators by patients. Physician trust, advice, empathy and counselling were the common provider-related facilitators facilitating adherence. Common facilitators as reported by the patients and providers were dedicated pill cover/boxes for each drug provided in the clinic, availability of medication and use of polypills. These findings were also in line with the previous qualitative reviews conducted in LMICs including India.47–50
Suggestions to improve medication adherence
The solutions provided by the patients and health professionals were in line with the barriers identified in our review. Comprehensive physician counselling to make the patients understand their own condition, complications of the disease and avoid misconception about the drugs and their side effects, along with good family support, and making the medication accessible and available free of cost were suggested as major suggestions to improve medication adherence. Similar interventions were also suggested by previous qualitative evidence on medication adherence among patients with CVD and DM.45–49 It is also interesting to note that medication adherence was also hurdled by the patients’ intention towards adherence, and this intention might vary across nations and cultural groups. The patient’s intention not to refill prescriptions due to cost, not to take medication because he feels better, also influences the patient’s decision. Thus, future research exploring these reasons on patient’s choice to adhere or not, rather than an inability to adhere (eg, forgetting, no access), needs to be encouraged.
Strengths and limitations of the study
To the best of our knowledge, this is the first review synthesising all possible qualitative factors associated with medication adherence among patients with CVD and DM in India. We have provided comprehensive and systematic evidence on the barriers, facilitators related to medication adherence, adhering to the ENTREQ statement, thereby ensuring transparency and reproducibility. We examined this evidence through the lenses of a well-established theoretical framework model. Furthermore, our study was able to provide valuable suggestions to promote medication adherence from both patient’s and provider’s perspectives. In addition to these strengths, we found that the majority of the studies included in our review were of high-quality evidence. This in turn ensures the transferability (external validity) of our review findings.
However, our review has certain limitations. We did not search grey literature, possibly missing some insights into our review. Hence, we cannot rule out the dissemination bias for an accurate and complete representation of medication adherence. We focused primarily on the patient and provider perspective on medication adherence.51 Hence, we cannot comment on the organisational or political influences on the adherence to long-term therapies as mentioned in the WHO report.16 The sample size of the included studies can be considered relatively low (median sample size—30). However, all the studies were conducted till the achievement of data saturation. In addition to the above, these results and suggestions need to be considered after taking into account India’s cross-cultural adaptations, customs, linguistic variations, genetic susceptibility and higher prevalence of risk factor profile.
Implications for clinical and public health practice
Improving medication adherence is essential to achieve better control and prevent life-threatening complications. Factors related to patients such as self-awareness and fear about the condition and its complications acted as a major facilitator for medication adherence. We also observed that most of the barriers identified were modifiable, in nature. Interventions should focus on these modifiable barriers such as knowledge barriers, intention barriers and health system-related barriers to achieve better adherence. In addition, the family members need to help the patients in mapping their daily routine and link the medicine intake with these routines to facilitate adherence. Our review also suggested that healthcare providers play an important role in promoting medication adherence. Hence, the interventions should not only target the patients but also the family members and healthcare providers and they should be tailored to suit differences in setting, culture and type of the patients.
Implications for future research
More evidence needs to be generated concerning the effectiveness and feasibility of possible solutions obtained in our review including the digital solutions, polypills, peer support groups, etc. Further qualitative studies including the subgroup of patients with CVD and DM under different stages and treatment regimens are required to contextualise the medication adherence on a larger scale. Exploring the barriers using a theoretical framework with the same methodological approach can provide more reliable evidence to develop patient-centred interventions and achieve better control among patients with CVD and DM.
Conclusion
In our review, we categorised the facilitating factors and barriers influencing medication adherence into patient-related, health system-related and care team-related factors. Thus, we advocate the creation of peer support groups, use of a digital reminder system for overcoming patients related factors, integration of Indian systems of medicine, physiotherapy and geriatric clinics even at the primary healthcare level for overcoming the health system-related barriers towards medication adherence.
Supplementary Material
Footnotes
Contributors: Conceived and designed the study: YK and SR, data management and extraction: YK, SR and TR, analysed the data and wrote the paper: SR, YK and TR. Provided comments and inputs to revise the manuscript: SR, YK, TR and MT. SR IS responsible for the overall content as guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. Data will be available upon reasonable request by investigators.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Approval from an ethics committee is not required since our review included only publicly available data without involving the human participants directly.
References
- 1.Walker IF, Garbe F, Wright J, et al. The economic costs of cardiovascular disease, diabetes mellitus, and associated complications in South Asia: a systematic review. Value Health Reg Issues 2018;15:12–26. 10.1016/j.vhri.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 2.Glovaci D, Fan W, Wong ND. Epidemiology of diabetes mellitus and cardiovascular disease. Curr Cardiol Rep 2019;21:21. 10.1007/s11886-019-1107-y [DOI] [PubMed] [Google Scholar]
- 3.India State-Level Disease Burden Initiative CVD Collaborators . The changing patterns of cardiovascular diseases and their risk factors in the states of India: the global burden of disease study 1990-2016. Lancet Glob Health 2018;6:e1339–51. 10.1016/S2214-109X(18)30407-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.India State-Level Disease Burden Initiative Diabetes Collaborators . The increasing burden of diabetes and variations among the states of India: the global burden of disease study 1990-2016. Lancet Glob Health 2018;6:e1352–62. 10.1016/S2214-109X(18)30387-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Durand H, Hayes P, Morrissey EC, et al. Medication adherence among patients with apparent treatment-resistant hypertension: systematic review and meta-analysis. J Hypertens 2017;35:2346–57. 10.1097/HJH.0000000000001502 [DOI] [PubMed] [Google Scholar]
- 6.Diabetes Care . Polypharmacy and medication adherence in patients with type 2 diabetes. Available: https://care.diabetesjournals.org/content/26/5/1408.short [Accessed 30 Jul 2020].
- 7.Vrijens B, Antoniou S, Burnier M, et al. Current situation of medication adherence in hypertension. Front Pharmacol 2017;8:100. 10.3389/fphar.2017.00100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rehman T, Rajaa S, Kumar G, et al. Prevalence and factors influencing diabesity among persons with type 2 diabetes mellitus in urban Puducherry: a cross-sectional analytical study. Indian J Community Med 2020;45:315. 10.4103/ijcm.IJCM_324_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polonsky WH, Henry RR. Poor medication adherence in type 2 diabetes: recognizing the scope of the problem and its key contributors. Patient Prefer Adherence 2016;10:1299–307. 10.2147/PPA.S106821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leporini C, De Sarro G, Russo E. Adherence to therapy and adverse drug reactions: is there a link? Expert Opin Drug Saf 2014;13 Suppl 1:S41–55. 10.1517/14740338.2014.947260 [DOI] [PubMed] [Google Scholar]
- 11.Lam WY, Fresco P. Medication adherence measures: an overview. Biomed Res Int 2015;2015:1–12. 10.1155/2015/217047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kvarnström K, Airaksinen M, Liira H. Barriers and facilitators to medication adherence: a qualitative study with general practitioners. BMJ Open 2018;8:e015332. 10.1136/bmjopen-2016-015332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferdinand KC, Senatore FF, Clayton-Jeter H, et al. Improving medication adherence in cardiometabolic disease. J Am Coll Cardiol 2017;69:437–51. 10.1016/j.jacc.2016.11.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krueger KP, Berger BA, Felkey B. Medication adherence and persistence: a comprehensive review. Adv Ther 2005;22:313–56. 10.1007/BF02850081 [DOI] [PubMed] [Google Scholar]
- 15.Dennis T, Meera NK, Binny K. Medication adherence and associated barriers in hypertension management in India. CVD Prev Control 2011;6:9–13. [Google Scholar]
- 16.Miller NH, Hill M, Kottke T, et al. The multilevel compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation 1997;95:1085–90. 10.1161/01.cir.95.4.1085 [DOI] [PubMed] [Google Scholar]
- 17.WHO . Adherence to long-term therapies: evidence for action [Internet]. Available: http://www.who.int/chp/knowledge/publications/adherence_report/en/ [Accessed 30 Jul 2020].
- 18.Aggarwal B, Liao M, Mosca L. Medication adherence is associated with having a caregiver among cardiac patients. Ann Behav Med 2013;46:237–42. 10.1007/s12160-013-9492-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daliri S, Bekker CL, Buurman BM, et al. Barriers and facilitators with medication use during the transition from hospital to home: a qualitative study among patients. BMC Health Serv Res 2019;19:204. 10.1186/s12913-019-4028-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rathbone AP, Todd A, Jamie K, et al. A systematic review and thematic synthesis of patients' experience of medicines adherence. Res Social Adm Pharm 2017;13:403–39. 10.1016/j.sapharm.2016.06.004 [DOI] [PubMed] [Google Scholar]
- 21.Flemming K, Booth A, Garside R, et al. Qualitative evidence synthesis for complex interventions and Guideline development: clarification of the purpose, designs and relevant methods. BMJ Glob Health 2019;4:e000882. 10.1136/bmjgh-2018-000882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181. 10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mohanty A, Kabi A, Mohanty A. Health problems in healthcare workers: a review. J Family Med Prim Care 2019;8:2568. 10.4103/jfmpc.jfmpc_431_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Critical Appraisal Skills Programme . Casp (qualitative) checklist, 2018. Available: https://casp-uk.net/wp-content/uploads/2018/01/CASP-Qualitative-Checklist-2018.pdf [Accessed 12 Sep 2020].
- 25.Booth A, Noyes J, Flemming K, et al. Structured methodology review identified seven (retreat) criteria for selecting qualitative evidence synthesis approaches. J Clin Epidemiol 2018;99:41–52. 10.1016/j.jclinepi.2018.03.003 [DOI] [PubMed] [Google Scholar]
- 26.Agarwal A, Davies D, Goenka S, et al. Facilitators and barriers of heart failure care in Kerala, India: a qualitative analysis of health-care providers and administrators. Indian Heart J 2019;71:235–41. 10.1016/j.ihj.2019.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhar L. Perceptions of global coronary heart disease risk, and adherence to antihypertensive treatment among low income urban women in Delhi, India. (Doctoral dissertation, Curtin University). [Google Scholar]
- 28.George CE, Ramadas D, Norman G, et al. Barriers to cardiovascular disease risk reduction: does physicians' perspective matter? Indian Heart J 2016;68:278–85. 10.1016/j.ihj.2015.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta S, Dhamija JP, Mohan I, et al. Qualitative study of barriers to adherence to antihypertensive medication among rural women in India. Int J Hypertens 2019;2019:1–7. 10.1155/2019/5749648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gupta S, Virk A, Mittal A, et al. Patterns and determinants of healthcare-seeking behavior among hypertensive patients in a rural population of North India: a mixed-method study. J Family Med Prim Care 2020;9:2830. 10.4103/jfmpc.jfmpc_200_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jayanna K, Swaroop N, Kar A, et al. Designing a comprehensive non-communicable diseases (Ncd) programme for hypertension and diabetes at primary health care level: evidence and experience from urban Karnataka, South India. BMC Public Health 2019;19:409. 10.1186/s12889-019-6735-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krishnamoorthy Y, Giriyappa DK, Eliyas SK, et al. Patient and provider's experience and perspective in addressing barriers to medication adherence among noncommunicable disease patients in rural Puducherry, South India-A qualitative study. J Patient Exp 2019;6:216–23. 10.1177/2374373518787288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kusuma YS. Migrants’ Perceptions on Barriers to Treatment Seeking for Hypertension: A Qualitative Study from Delhi, India. Studies on Ethno-Medicine 2010;4:173–6. 10.1080/09735070.2010.11886377 [DOI] [Google Scholar]
- 34.Miller V, Nambiar L, Saxena M, et al. Exploring the barriers to and facilitators of using evidence-based drugs in the secondary prevention of cardiovascular diseases: findings from a multistakeholder, qualitative analysis. Glob Heart 2018;13:27–34. 10.1016/j.gheart.2017.08.001 [DOI] [PubMed] [Google Scholar]
- 35.Newtonraj A, Arun S, Bazroy J, et al. Lay perspectives on causes and complications of hypertension; and barrier to access health care by known hypertensive patients: a qualitative study from a rural area of South India. Int J Community Med Public Health 2017;4:704. 10.18203/2394-6040.ijcmph20170743 [DOI] [Google Scholar]
- 36.Nimesh VV, Halder A, Mitra A, et al. Patterns of healthcare seeking behavior among persons with diabetes in central India: a mixed method study. J Family Med Prim Care 2019;8:677. 10.4103/jfmpc.jfmpc_433_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pati S, Van den Akker M, Schellevis FF. Managing diabetes mellitus with comorbidities in primary healthcare facilities: a qualitative study among physicians in Odisha, India. Research square [preprint] 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anitha Rani M, Shriraam V. Are patients with type 2 diabetes not aware or are they unable to practice self-care? A qualitative study in rural South India. J Prim Care Community Health 2019;10:2150132719865820. 10.1177/2150132719865820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salam A, Praveen D, Patel A, et al. Barriers and facilitators to the use of cardiovascular fixed-dose combination medication (polypills) in Andhra Pradesh, India: a mixed-methods study. Glob Heart 2019;14:303–10. 10.1016/j.gheart.2019.07.002 [DOI] [PubMed] [Google Scholar]
- 40.Satish P, Khetan A, Barbhaya D, et al. A qualitative study of facilitators and barriers to cardiovascular risk factor control in a semiurban population in India. J Family Med Prim Care 2019;8:3773–8. 10.4103/jfmpc.jfmpc_492_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thakur J, Vijayvergiya R, Jaswal N, et al. Assessment and barriers to medication adherence for secondary prevention of cardiovascular disease among patients with coronary artery disease in Chandigarh, India. Int J Noncommun Dis 2016;1:37–41. 10.4103/2468-8827.184863 [DOI] [Google Scholar]
- 42.Venkatesan M, Dongre AR, Ganapathy K. A community-based study on diabetes medication nonadherence and its risk factors in rural Tamil Nadu. Indian J Community Med 2018;43:72–6. 10.4103/ijcm.IJCM_261_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wood F, Salam A, Singh K, et al. Process evaluation of the impact and acceptability of a polypill for prevention of cardiovascular disease. BMJ Open 2015;5:e008018. 10.1136/bmjopen-2015-008018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saha S, Korthuis PT, Cohn JA, et al. Primary care provider cultural competence and racial disparities in HIV care and outcomes. J Gen Intern Med 2013;28:622–9. 10.1007/s11606-012-2298-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sohal T, Sohal P, King-Shier KM, et al. Barriers and facilitators for type-2 diabetes management in South Asians: a systematic review. PLoS One 2015;10:e0136202. 10.1371/journal.pone.0136202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sears K, Scobie A, Mackinnon NJ. Patient-Related risk factors for self-reported medication errors in hospital and community settings in 8 countries. Can Pharm J 2012;145:88–93. 10.3821/145.2.cpj88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nam S, Chesla C, Stotts NA, et al. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract 2011;93:1–9. 10.1016/j.diabres.2011.02.002 [DOI] [PubMed] [Google Scholar]
- 48.Lipton RB, Losey LM, Giachello A, et al. Attitudes and issues in treating Latino patients with type 2 diabetes: views of healthcare providers. Diabetes Educ 1998;24:67–71. 10.1177/014572179802400109 [DOI] [PubMed] [Google Scholar]
- 49.Sridharan SG, Chittem M, Maya S. Patients’ Experiences of Barriers and Facilitators for Adherence to Type 2 Diabetes Mellitus: A Meta-Ethnography. Journal of Social Health and Diabetes 2019;7:61–72. 10.1055/s-0039-3402529 [DOI] [Google Scholar]
- 50.Al Hamid A, Ghaleb M, Aljadhey H, et al. A systematic review of qualitative research on the contributory factors leading to medicine-related problems from the perspectives of adult patients with cardiovascular diseases and diabetes mellitus. BMJ Open 2014;4:e005992. 10.1136/bmjopen-2014-005992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Toews I, Booth A, Berg RC, et al. Further exploration of dissemination bias in qualitative research required to facilitate assessment within qualitative evidence syntheses. J Clin Epidemiol 2017;88:133–9. 10.1016/j.jclinepi.2017.04.010 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-055226supp001.pdf (101.1KB, pdf)
bmjopen-2021-055226supp002.pdf (32.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request. Data will be available upon reasonable request by investigators.


