Abstract
Background: Insufficient antimicrobial-related training for physicians during their undergraduate education could have a negative impact on their prescribing. Unlike previous studies, this study not only explored the understanding and perception of Pakistani medical students about antibiotics and resistance, but also their preparedness towards antimicrobial stewardship programs.
Methods: An online cross-sectional study was undertaken with final-year medical students using a validated questionnaire from January 2021 to May 2021. Descriptive and inference statistics were applied for data analysis.
Results: Of 411 students, only 6.3% had undergone antimicrobial resistance (AMR) training. 16.1% of students believed that antibiotics are effective for viral ailments. More than half of the students agreed that AMR is a major healthcare problem in Pakistan (65.9%). Most students viewed poor infection control practices (66.9%), the use of too many broad-spectrum antibiotics (68.4%) for a longer duration (62.8%) with inadequate doses (67.9%) as the causes of AMR. The student’s preparation was insufficient in interpreting microbiological and pathological results (26.3%), selecting the correct antibiotics (22.1%), and awareness of the antibiotic spectrum (20.9%). The median preparedness score showed significant differences with sex (p = 0.049), age (p < 0.001), institute type (p = 0.014), and family income (p = 0.006).
Conclusion: Pakistani medical students showed adequate understanding of antibiotics, but lacked preparedness for several components of ASPs, including interpretation of microbiological results and spectrum of antibiotics. More steps need to be taken to prepare medical students for AMR and stewardship initiatives adequately.
Keywords: antimicrobial resistance, antibiotics, antimicrobial stewardship programs, medical students, preparedness, Pakistan
Introduction
Antimicrobial resistance (AMR) inherits a significant potential to affect people’s health globally (Ferri et al., 2017). Resistant infections are responsible for one in every three deaths globally, according to the World Health Organization (WHO, 2021), which attributes the increase to the inappropriate use of antimicrobials, including antibiotics. More than 700,000 people worldwide die each year from resistant infections (O’neill, 2016). In the U.S., which provides one-third of all antibiotic prescriptions globally, resistant infections affect at least two million people each year.
Misuse and overuse of antimicrobials contribute to the spread of resistant strains of microbes (Markogiannakis et al., 2021). Antibiotic overuse is becoming increasingly common as a result of the belief that they are safe and that patient satisfaction is dependent on being prescribed an antibiotic. (Foster et al., 2019). The way doctors give antibiotics, patients’ nonadherence to therapy, unjudicial prescribing, inadequate public awareness, self-medication, pharmaceutical industry’s lack of new antimicrobial-related research due to lower economic incentives and rigorous compliance requirements have an obvious impact on the increase of AMR (Baig et al., 2017; Hutchings et al., 2019; Aslam et al., 2020; Gillani et al., 2021). Both the WHO and the UN have recognized the worldwide scope of AMR with the need for global policies (World Health Organization, 2015; United Nations, 2016). The WHO publication “Global Action Plan on Antimicrobial Resistance” states that “there is an international agreement that AMR is a critical public health concern,” underlining the importance of attaining the WHO Global Action Plan’s five strategic goals (2015).
AMR continues to become more widespread in many parts of the world, including Pakistan, and is largely responsible for the rise in healthcare costs and mortality rates (Abrar et al., 2018). In Pakistan, the AMR rate is amplifying at a rapid pace (Bilal et al., 2021). During the last few years, multidrug-resistant and extensively drug-resistant (XDR) bacterial strains have been reported among hospitalized patients. Enterobacteriaceae have demonstrated significant resistance to quinolones (Qamar et al., 2020). XDR typhoid patients showed resistance to most antimicrobials, including ampicillin, chloramphenicol, trimethoprim-sulfamethoxazole, third-generation cephalosporins and fluoroquinolones (Qamar et al., 2018; Azhar et al., 2019; Qureshi et al., 2020). Additionally, several previous studies have reported the continuously swelling burden of resistant pathogens in Pakistan including carbapenem-resistant extended-spectrum beta-lactamase-producing bacteria and methicillin-resistant Staphylococcus aureus, in clinical isolates (Bilal et al., 2021). According to the legislation, antibiotics are not allowed to be sold in Pakistan without a valid prescription from a qualified medical practitioner; nonetheless, studies have reported that drug outlets still dispense antibiotics irrationally in several medial ailments including upper respiratory tract infections owing to business interest, poor training, and inadequate knowledge of staff (NIH, 2017; Malik et al., 2021).
In order to address the resistance problem, a significant and permanent amount of research, policies, regulations, and development is required to ensure the growth of new, powerful antibiotics and rationalize the use of antimicrobial across health facilities, agriculture, and the veterinary sector. Antimicrobial stewardship programs (ASPs) are among the potential approaches used globally to cope with the rising level of AMR (Hayat et al., 2019). ASPs primarily prevent unjudicial use of antimicrobials by educating all major stakeholders of the healthcare system, including physicians, pharmacists, and nurses, regarding rationality checking in antimicrobial prescriptions (Science et al., 2019; Scobie et al., 2019).
Medical students need to learn how to prescribe drugs safely and effectively because once graduating and licensed to practice as medical practitioners, they will indeed be prescribing medication daily with minimal supervision (Van Der Voort et al., 2019; Augie et al., 2021). Strong prescribing skill sets can facilitate rational and judicial prescribing, which improves patient benefits, medication compliance, and limit healthcare-associated costs (Essack et al., 2019). Therefore, it is vital to be aware that future medical students have a complete awareness of the growing issue of AMR as they will act as next-generation antimicrobial providers (Haque et al., 2019). Unfortunately, only a limited part of the curricula of Pakistani medical students emphasize on AMR and information on ASPs is completely absent (PMDC, 2011).
Several studies have shown that poor prescribing amongst doctors could be linked to inadequate training during their undergraduate medical education (Okedo-Alex et al., 2019). For example, in a Chinese study, only one-fourth of the medical students sampled had undergone training specifically relevant to antimicrobials and AMR (Hu et al., 2018). In an Italian study, 20% of study respondents deemed antibiotics effective for viral ailments (Scaioli et al., 2015). Consequently, adequate medical education coupled with sufficient training is vital to prepare medical students for the rational use of antimicrobials and approaches to eradicating AMR. The literature is scarce from Pakistani medical students’ understanding about antibiotics and preparedness for antimicrobial stewardship activities. Therefore, the primary objective of this study was to determine the understanding of medical students about antibiotics, perception towards resistance problem, and preparedness for stewardship activities in Punjab, Pakistan.
Materials and Methods
Study Design and Population
This cross-sectional study was conducted among medical students from Punjab province, Pakistan, from January 2021 to May 2021. There are 144 medical colleges in Pakistan, and nearly half are in Punjab province (Sadiq, 2021). Medical students in their final year (5th year) of medical education participated in this study.
Study Instrument
A questionnaire was developed after a comprehensive, relevant literature review (Gupta et al., 2019; Okedo-Alex et al., 2019; Saleem et al., 2019; Struzycka et al., 2019; Van Der Voort et al., 2019; Efthymiou et al., 2020; Tiong and Chua, 2020). Questionnaire validation, including face and content validity, was ensured from an expert team (2 professors and 2 physicians) and a group of potential subjects. Few modifications were made as per the recommendations of experts.
The questionnaire was divided into seven sections with subdivided components, each based on different assessment criteria. The first section was about the demographic components of the students, including gender, age, family income, the professional field of parents, the type of institute, and AMR training. The second section recorded the understanding of students towards antibiotics with options of “Yes” “No” and “Unsure”. One mark was given to a student for each correct response, and their scoring was categorized as either good (≥6 correct responses) or poor (<6 correct responses). The third section was about potential causes of AMR. The fourth section focused on the student’s perception of the problem of AMR. The third and fourth sections were rated on a Likert scale from “strongly agree” to “strongly disagree”. The fifth section determined resources used by medical students for learning about antimicrobial prescribing and AMR with five options including “Always,” “Often,” “Sometimes” “Seldom” and “Never”. The sixth section measured the preparedness of the medical student for numerous activities related to ASPs. Here again, a 5-point Likert scale was chosen to record the response, including “Very good” “Good” “Average” “Poor” and “Very poor”. The last section was about ways to reduce AMR. In this section, students were asked about different approaches through which AMR could be eradicated with options ranging from “Strongly agree” to “Strongly disagree”.
A pilot study was conducted on twenty final-year medical students through which the reliability of the questionnaire was measured. The overall value of Cronbach’s alpha was 0.891, ensuring an acceptable level of internal consistency.
Sampling
A convenience sampling approach was opted to recruit medical students. The sample size of this study was measured using an online sample size calculator (Raosoft) with a 50% response rate, 5% margin of error, and 95% confidence interval.
Data Collection
Data were collected using a questionnaire designed on Google forms distributed through social media applications. The students were able to fill the questionnaire by clicking on the link. A brief introduction and objective of the study coupled with informed consent were provided on the first page.
Inclusion and Exclusion Criteria
This study included only medical students who were in the final year (fifth) of their education. Non-medical students were excluded from this study.
Statistical Analysis
Using descriptive statistics, the data were displayed as frequency and percentages. As the data had a nonnormal distribution, the median and interquartile ranges (IQRs) were calculated. The study participants’ median knowledge score, perception score, median AMR causes score, median preparedness score, and median eradication score were measured. On continuous data, Kruskal–Wallis and Mann-Whitney tests were used, which were then compared with demographic variables. The IBM Statistical Package for the Social Sciences (SPSS) version 19 was used to analyze all of the data by setting a p < 0.05 was set as statistical significance.
Results
Of 600 students approached, 411 completed the questionnaire (response rate = 68.5%). Most of the students were female (n = 299, 72.7%), aged 23–25 years (n = 357, 86.9%) and belonged to the public sector medical institutes (n = 279, 67.9%). Only a few students had undergone training related to AMR (n = 26, 6.3%). As indicated in Table 1, the profession of parents of most of the students was related to medical (n = 275, 66.9%) with a monthly income higher than 50,000 (n = 242, 58.9%).
TABLE 1.
Demographic information of participants (n = 411).
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 112 | 27.3 |
| Female | 299 | 72.7 |
| Age (years) | ||
| 22 years | 13 | 3.2 |
| 23–25 years | 357 | 86.9 |
| >25 years | 41 | 10.0 |
| Family income | ||
| <50,000 | 242 | 58.9 |
| >50,000 | 169 | 41.1 |
| Type of institute | ||
| Public | 279 | 67.9 |
| Private | 132 | 32.1 |
| Type of parents’ profession | ||
| Medial | 275 | 66.9 |
| Non-medical | 136 | 33.1 |
| AMR training | ||
| Yes | 26 | 6.3 |
| No | 385 | 93.7 |
Exploration of Students’ Understanding of Antibiotics
Overall, students’ knowledge of antibiotics fell into the category of good (n = 256, 62.3%) with a mean score of 7.68 ± 1.72. The students were well aware of the ineffectiveness of antibiotics against viral infections (n = 343, 83.5%) and destruction of the normal microbiota of the body, thus increasing the potential for secondary infections (n = 358, 87.1%). Most students correctly said that the resistant bacteria could spread across healthcare facilities (n = 331, 80.5%); nonetheless, only a few students were familiar with the fact that skipping antibiotics could enhance the resistance potential (n = 116, 28.2%). The awareness of students of antibiotic resistance was higher compared to antimicrobial stewardship programs (n = 376, 91.5% vs. n = 255, 62.0%) as indicated in Table 2. The median knowledge score demonstrated a significant association with gender (<0.001), age (<0.001), type of institute (<0.001), family income (<0.001), and AMR training (<0.001). Female students (Median = 9.00, IQR = 8–9), students aged 23–25 years (Median = 9.00, IQR = 7–9), and students from public institutes (Median = 9.00, IQR = 7–9) had significantly higher median scores compared to other groups (Table 3).
TABLE 2.
Knowledge about antibiotics.
| Questions | Yes | No | Unsure | Correct rate |
|---|---|---|---|---|
| Antibiotics are useful in treating viral infections | 66 (16.1) | 343 (83.5) | 2 (0.5) | 343 (83.5) |
| Antibiotics can cause secondary infections by killing normal flora | 358 (87.1) | 42 (10.2) | 11 (2.7) | 358 (87.1) |
| Antibiotics can cause allergic reactions | 386 (93.9) | 15 (3.6) | 10 (2.4) | 386 (93.9) |
| A resistant bacterium cannot spread in healthcare institutions | 63 (15.3) | 331 (80.5) | 17 (4.1) | 331 (80.5) |
| Skipping one or two doses does not contribute to the development of antibiotic resistance | 277 (67.4) | 116 (28.2) | 18 (4.4) | 116 (28.2) |
| Cross-resistance is the condition in which the resistance occurs to a particular antibiotic that often results in resistance to other antibiotics, usually from a similar class | 353 (85.9) | 42 (10.2) | 16 (3.9) | 353 (85.9) |
| Pain and inflammation without any possibility of infection are indications for antimicrobial therapy | 84 (20.4) | 299 (72.7) | 28 (6.8) | 299 (72.7) |
| Have you ever heard of antibiotic resistance? | 376 (91.5) | 28 (6.8) | 7 (1.7) | 376 (91.5) |
| Have you been ever taught antibiotic resistance in your curriculum? | 365 (88.8) | 37 (9.0) | 9 (2.2) | 365 (88.8) |
| Have you ever heard of antibiotic stewardship? | 255 (62.0) | 137 (33.3) | 19 (4.6) | 255 (62.0) |
| Have you been ever taught about antibiotic stewardship in your curriculum? | 251 (61.1) | 128 (31.1) | 32 (7.8) | 251 (61.1) |
TABLE 3.
Median scores association with demographics.
| Variable | Median knowledge score | p-value | Median AMR cause score | p-value | Median perception score | p-value | Median ASP preparedness score | p-value | Median AMR eradication score | p-value |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||||
| Male | 7.00 (5–7) | <0.001 | 41.50 (38–45) | 0.003 | 38.00 (35–41) | 0.838 | 40.00 (33–44) | 0.049 | 41.00 (37–43) | <0.001 |
| Female | 9.00 (8–9) | 40.00 (40–40) | 37.00 (37–39) | 36.00 (36–38) | 45.00 (35–43) | |||||
| Age (years) | ||||||||||
| 22 years | 5.00 (3–6) | <0.001 | 42.00 (40–46) | <0.001 | 39.00 (35–41) | 0.572 | 44.00 (33–47) | <0.001 | 43.00 (37–45) | <0.001 |
| 23–25 years | 9.00 (7–9) | 40.00 (40–41) | 37.00 (37–39) | 36.00 (36–40) | 35.00 (35–43) | |||||
| >25 years | 7.00 (6–7) | 42.00 (40–45) | 39.00 (36–40) | 42.00 (40–45) | 41.00 (39–44) | |||||
| College type | ||||||||||
| Public | 9.00 (7–9) | <0.001 | 40.00 (40–40) | 0.173 | 37.00 (37–37) | <0.001 | 36.00 (36–36) | 0.014 | 35.00 (35–41) | <0.001 |
| Private | 7.00 (6–8) | 41.00 (37–45) | 39.00 (37–41) | 40.00 (33–45) | 42.00 (39–45) | |||||
| Family income | ||||||||||
| <50,000 | 7.00 (8–9) | <0.001 | 40.00 (40–40) | 0.005 | 37.00 (37–37) | <0.001 | 36.00 (36–36) | 0.006 | 35.00 (35–35) | <0.001 |
| >50,000 | 9.00 (6–8) | 41.00 (37–45) | 39.00 (37–41) | 40.00 (33–45) | 42.00 (40–45) | |||||
| Parents profession | ||||||||||
| Medial | 9.00 (7–9) | <0.001 | 40.00 (40–40) | 0.906 | 37.00 (37–37) | <0.001 | 36.00 (36–37) | 0.182 | 35.00 (35–39) | <0.001 |
| Non-medical | 7.00 (6–8) | 41.00 (36–45) | 40.00 (37–42) | 40.00 (32–45.50) | 43.00 (40–46) | |||||
| AMR training | ||||||||||
| Yes | 9.00 (5–7) | <0.001 | 44.00 (35–45) | 0.215 | 40.00 (37–42) | 0.033 | 43.00 (32–46) | 0.281 | 35.00 (35–41) | 0.029 |
| No | 6.00 (7–9) | 40.00 (40–42) | 37.00 (37–39) | 36.00 (36–42) | 42.00 (39–45) | |||||
Perception of Students About Antibiotic Use and Antimicrobial Resistance
Most of the students agreed that AMR is not only a global concern (n = 297, 72.3%) but also a major healthcare problem of the public in Pakistan (n = 271, 65.9%) (Table 4). More than half of the students believed that AMR is a major issue (n = 273, 66.4%) and that antimicrobials are overused in hospitals where they are rotated (n = 245, 59.6%). Many students said that unjudicial antibiotic use is not only unethical (n = 251, 61.1%) but could also lead to significant patient harm (n = 249, 60.6%). Students believed that adequate education (n = 257, 62.5) and the development of newer antibiotics are integral to curtail the AMR issue (n = 271, 65.9%). The median perception score was significantly higher among students of the private institute (p < 0.001), family income >50,000 (p < 0.001), and had undergone AMR training (p = 0.033) (Table 3).
TABLE 4.
Perception about antibiotic use and antimicrobial resistance.
| Question | Strongly agree; strongly disagree. N (%) | ||||
|---|---|---|---|---|---|
| SA | A | N | D | SD | |
| Antimicrobial resistance is a global issue | 297 (72.3) | 95 (23.1) | 15 (3.6) | 3 (0.7) | 1 (0.2) |
| Antimicrobial resistance is a serious problem in Pakistan | 116 (28.2) | 271 (65.9) | 20 (4.9) | 3 (0.7) | 1 (0.2) |
| Antimicrobial are overused at the hospitals where I have rotated | 88 (21.4) | 245 (59.6) | 61 (14.8) | 14 (3.4) | 3 (0.7) |
| Antimicrobial resistance is a significant problem at the hospitals where I have rotated | 61 (14.8) | 273 (66.4) | 65 (15.8) | 10 (2.4) | 2 (0.5) |
| Strong knowledge of antibiotic is important in career | 143 (34.8) | 241 (58.6) | 17 (4.1) | 5 (1.2) | 5 (1.2) |
| Inappropriate use of antibiotic is professionally unethical | 133 (32.4) | 251 (61.1) | 18 (4.4) | 3 (0.7) | 6 (1.5) |
| Inappropriate use of antibiotic can harm patients | 144 (35.0) | 249 (60.6) | 14 (3.4) | 3 (0.7) | 1 (0.2) |
| I would like more education on antibiotic resistance | 137 (33.3) | 257 (62.5) | 8 (1.9) | 6 (1.5) | 3 (0.7) |
| New antibiotics will be developed in the future that will counter the problem of “resistance” | 87 (21.2) | 271 (65.9) | 39 (9.5) | 12 (2.9) | 2 (0.5) |
SA, strongly agree; A, agree; N, neutral; D, disagree; SD, strongly disagree.
Potential Cause of Antimicrobial Resistance and Educational Resources
More than two-quarters of the students agreed that the sale of over-the-counter antibiotics (n = 248, 60.3%), poor infection control practices (n = 275, 66.9%), the use of too many broad-spectrum antibiotics (n = 281, 68.4%) for a longer duration (n = 258, 62.8%) with inadequate doses (n = 279, 67.9%) could aggravate the risk of AMR. Likewise, most students also felt that patients’ non-compliance with their antibiotic therapy (n = 257, 62.5%) and extensive antibiotic usage in livestock might lead to AMR (n = 268, 65.2%) (Table 5). Gender (p = 0.003), age (p < 0.001), and family income (p = 0.005) showed a significant association with the median score of AMR cause (Table 3).
TABLE 5.
Potential causes of antimicrobial resistance.
| Question | Strongly agree; strongly disagree. N (%) | ||||
|---|---|---|---|---|---|
| SA | A | N | D | SD | |
| Too many antibiotic prescriptions | 118 (28.7) | 266 (64.7) | 9 (2.2) | 5 (1.2) | 13 (3.2) |
| Too many broad-spectrum antibiotics used | 103 (25.1) | 281 (68.4) | 9 (2.2) | 11 (2.7) | 7 (1.7) |
| Too long durations of antibiotic treatment | 84 (20.4) | 258 (62.8) | 31 (7.5) | 33 (8.0) | 5 (1.2) |
| Dosing of antibiotics are too low | 44 (10.7) | 279 (67.9) | 37 (9.0) | 34 (8.3) | 17 (4.1) |
| Excessive use of antibiotics in livestock | 81 (19.7) | 268 (65.2) | 31 (7.5) | 23 (5.6) | 8 (1.9) |
| Not removing the focus of infection (e.g. medical devices or catheters) | 70 (17.0) | 286 (69.6) | 25 (6.1) | 21 (5.1) | 9 (2.2) |
| Antibiotic sale without prescription from community pharmacies | 130 (31.6) | 248 (60.3) | 14 (3.4) | 7 (1.7) | 12 (2.9) |
| Patient non-compliance with antibiotic treatment | 129 (31.4) | 257 (62.5) | 9 (2.2) | 10 (2.4) | 6 (1.5) |
| Poor infection-control practices by healthcare professionals | 90 (21.9) | 275 (66.9) | 24 (5.8) | 12 (2.9) | 10 (2.4) |
| Paying too much attention to pharmaceutical representatives/advertising | 20 (4.9) | 8 (1.9) | 26 (6.3) | 263 (64.0) | 94 (22.9) |
SA, strongly agree; A, agree; N, neutral; D, disagree; SD, strongly disagree.
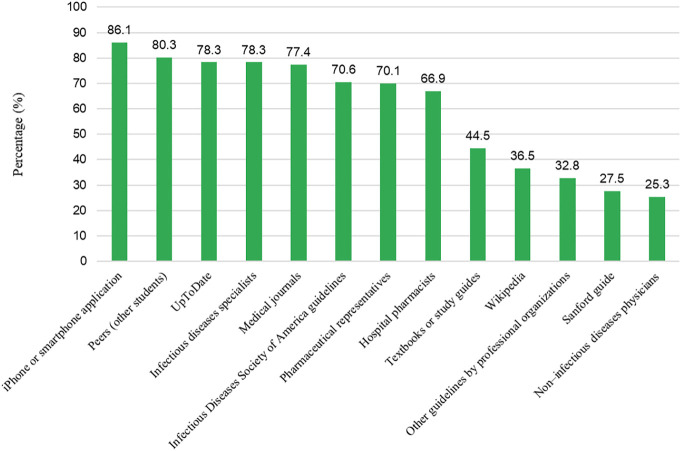
Various educational resources utilized by medical students to enhance their antimicrobial related information include iPhone and smartphone applications (86.1%), peers (80.3%), UpToDate (medical app) (78.3%), infectious disease specialists (78.3%), medical journals (77.4%), American guidelines (70.6%), pharmaceutical representatives (70.1%), and hospital pharmacists (66.9%) (Figure 1).
FIGURE 1.
Resources used by medial students for antimicrobial resistant related information (Always and often combined).
Preparedness for Antimicrobial Stewardship Activities
The preparedness of students about antimicrobial stewardship activities has been summarized in Table 6. Most of the students rated their preparedness good for accurate infection diagnosis of infection (n = 265, 64.5%), when to initiate antibiotic therapy (n = 257, 62.5%), de-escalation to narrow-spectrum antibiotics (n = 267, 65.0%), switching from oral to IV antibiotics (n = 260, 63.3%) and interpretation of antibiograms (n = 263, 64.0%). Nevertheless, only a few of the students considered themselves good enough to interpret microbiological and pathology results (n = 108, 26.3%), selection of correct antibiotics (n = 91, 22.1%), and awareness of the spectrum of antibiotics (n = 86, 20.9%). Similarly, students’ preparedness for antibiotic mechanisms was also suboptimal (98, 23.8%). The preparedness towards stewardship activities was significantly higher among students who were female (p = 0.049), aged 22 years (p < 0.001), belonged to private institutes (p = 0.014), and had a family income higher than 50,000 (p = 0.006) (Table 3).
TABLE 6.
Preparedness about antimicrobial stewardship activities.
| Question | Very good; very poor. N (%) | ||||
|---|---|---|---|---|---|
| Very Good | Good | Average | Poor | Very Poor | |
| Making accurate diagnosis of infection | 90 (21.9) | 265 (64.5) | 46 (11.2) | 9 (2.2) | 90 (21.9) |
| Interpreting pathology and microbiology results | 66 (16.1) | 108 (26.3) | 220 (53.5) | 15 (3.6) | 2 (0.5) |
| Knowing when to start antibiotics | 88 (21.4) | 257 (62.5) | 53 (12.9) | 11 (2.7) | 2 (0.5) |
| Choosing the correct antibiotic | 79 (19.2) | 91 (22.1) | 221 (53.8) | 18 (4.4) | 2 (0.5) |
| Knowledge of dosing/calculations and duration of antibiotics | 76 (18.5) | 253 (61.6) | 52 (12.7) | 23 (5.6) | 7 (1.7) |
| How to de-escalate to narrower spectrum antibiotics | 62 (15.1) | 267 (65.0) | 56 (13.6) | 18 (4.4) | 8 (1.9) |
| How and when to transition from intravenous to oral antibiotics | 74 (18.0) | 260 (63.3) | 50 (12.2) | 19 (4.6) | 8 (1.9) |
| How to interpret antibiograms | 55 (13.4) | 263 (64.0) | 54 (13.1) | 24 (5.8) | 15 (3.6) |
| Understanding spectrums of activity of antibiotics | 85 (20.7) | 86 (20.9) | 213 (51.8) | 17 (4.1) | 10 (2.4) |
| Understanding basic mechanisms of resistance of antibiotics | 90 (21.9) | 98 (23.8) | 206 (50.1) | 10 (2.4) | 7 (1.7) |
Attitude Towards Eradicating Antimicrobial Resistance
Most students agreed that judicial antimicrobials utilization related to formal teaching should be offered to the students (n = 279, 67.9%) coupled with the development of institutional treatment guidelines (n = 265, 64.5%). Besides, most students said that patients should prohibit the practice of keeping left-over antibiotics (n = 266, 64.7%) and self-medication (n = 253, 61.6%). Most students remained neutral when they were asked about the “implementation of antimicrobial stewardship programs” (n = 202, 49.1%) and “improving diagnostic facilities” (n = 186, 45.3%) (Table 7). The median score of eradicating AMR was noted to be significantly associated with gender (p < 0.001), age (p < 0.001), institute type (p < 0.001), family income (p < 0.001), AMR training (p = 0.029), and parent’s profession (p < 0.001) (Table 3).
TABLE 7.
Attitude towards eradicating antimicrobial resistance.
| Question | Strongly agree; strongly disagree. N (%) | ||||
|---|---|---|---|---|---|
| SA | A | N | D | SD | |
| Educating healthcare professional in terms of appropriate antibiotic prescribing | 145 (35.3) | 75 (18.2) | 189 (46.0) | 1 (0.2) | 1 (0.2) |
| Formal teaching on proper usage of antimicrobial agents among health care students | 111 (27.0) | 279 (67.9) | 15 (3.6) | 6 (1.5) | 0 (0.0) |
| Implementing antimicrobial stewardships programs | 111 (27.0) | 91 (22.1) | 202 (49.1) | 5 (1.2) | 2 (0.5) |
| Rationalizing antimicrobial use in veterinary sector | 89 (21.7) | 269 (65.5) | 45 (10.9) | 5 (1.2) | 3 (0.7) |
| Improving diagnostic facilities | 128 (31.1) | 88 (21.4) | 186 (45.3) | 5 (1.2) | 4 (1.0) |
| Development of institutional standard treatment guidelines | 123 (29.9) | 265 (64.5) | 13 (3.2) | 5 (1.2) | 5 (1.2) |
| Prescribing antibiotics over the phone | 35 (8.5) | 74 (18.0) | 231 (56.2) | 38 (9.2) | 33 (8.0) |
| Patient should be advised not to keep part of the antibiotic course for another occasion | 94 (22.9) | 266 (64.7) | 32 (7.8) | 9 (2.2) | 10 (2.4) |
| Pharmacists should be discouraged to dispense antibiotics to meet the patients demands | 99 (24.1) | 92 (22.4) | 203 (49.4) | 11 (2.7) | 6 (1.5) |
| Self-medication with antibiotics in community should be discouraged | 133 (32.4) | 253 (61.6) | 16 (3.9) | 8 (1.9) | 1 (0.2) |
SA, strongly agree; A, agree; N, neutral; D, disagree; SD, strongly disagree.
Discussion
This study is the first among Pakistani medical students which assessed their understanding of antimicrobial resistance coupled with its causes and preparedness towards antimicrobial stewardship activities. Our study respondents had a good understanding of certain aspects of antimicrobial use and resistance; nevertheless, their preparedness for certain activities of antimicrobial stewardship programs was suboptimal.
It is widely accepted that antibiotics are unable to cure viral infections, including flu (Alsan et al., 2015). However, 16.1% of our study respondents still believe that antibiotics are effective in viral diseases. A study in Saudi Arabia reported similar findings where 18.1% of medical students perceived that antibiotics could be used against viral infections (Harakeh et al., 2015). Likewise significant gaps in knowledge of medical students about antibiotics including their use in flu and cold have been highlighted (Nogueira-Uzal et al., 2020). Most of the respondents in our study (72.7%) correctly identified that antibiotics should not be administered to relieve pain and inflammation. This agrees with previous studies (Sakeena et al., 2018; Haque et al., 2019). Our respondents better understood the term “antibiotic resistant” compared to “antimicrobial stewardship programs”. This might be because the concept of implementing stewardship programs in hospitals is still new and faces numerous challenges in LMICs, including Pakistan. Previous studies conducted in Pakistan with healthcare professionals and students have also revealed similar findings. The overall understanding of our study respondents regarding antibiotics was still adequate, which might be due to several reasons. First, our respondents were in their last year (5th year) of medical education and had already read about the basic concept of antibiotics and AMR. Second, the parent’s profession of most of our respondents was medical, which could have a positive impact on medical students’ antibiotics-related understanding.
Most of the study respondents believed that AMR is a global threat, and its intensity is also higher in Pakistan. Numerous studies have already revealed that AMR affects nearly every corner of the world and demands certain serious steps to help combat it (Nathan, 2020; Watkins and Bonomo, 2020). In Pakistan, the situation of AMR could be grimmer due to inadequate diagnostic laboratories, the poor performance of the infection control committee, lack of a sufficient number of infectious disease physicians, and antibiotic sales without a prescription (Hayat et al., 2019; Atif et al., 2021). Interestingly, more than half of our survey respondents also agreed that there is an overuse of antibiotics in health facilities where they are getting training. Several studies from Pakistan have also confirmed this point, making the situation severe (Mustafa et al., 2020; Mustafa et al., 2021).
Most of our respondents said that the discovery of newer antibiotics could counter the problem of AMR. The WHO has already stated that global efforts to curtail the global resistance issue have been threatened due to the lack of new antibiotic molecules. To address this issue, the WHO has issued a list of pathogens against which antibiotics should be prepared in priority (Tacconelli et al., 2018).
As indicated in previous studies (Atif et al., 2019; Hayat et al., 2019; Asghar et al., 2020; Malik et al., 2021; Umair et al., 2021), our study respondents believed that the use of antibiotics in livestock, inadequate dosing and duration of antibiotics, antibiotic sale without prescription, and excessive use of broad-spectrum antibiotics are potential causes of AMR. These irrational practices are common in LMICs, including Pakistan. For example, a recent study conducted in Pakistan found antibiotic dispensing without any prescription from more than half of the drug stores (Malik et al., 2021). Similarly, in another Pakistani study, the trend to use antimicrobials in livestock was noted to be very high (Mohsin et al., 2019).
Our study respondents were well prepared regarding certain activities of stewardship programs, including infectious disease diagnosis and initiation of antibiotic therapy coupled with dosing, which is in line with previous studies conducted on South and East African medical students (Wasserman et al., 2017; Lubwama et al., 2021). Nonetheless, students lacked preparedness regarding knowledge of the spectrum of antibiotics and proper antibiotic selection, which are integral components of judicial antibiotic prescribing. Similar results have previously been reported in which more than half of the students agreed that they are unable to know the spectrum of antibiotics and the selection of the correct antibiotics (Wasserman et al., 2017). This might be due to the lack of adequate antimicrobial education of students, which could have a negative impact on the preparedness of students for stewardship programs. The students in our study (67.9%) were also agreed that formal teaching pointed towards antimicrobial agents should be initiated for medical students. We have previously highlighted this point that there is an urgent need to review the curriculum of medical students, including pharmacy students, considering the need for antimicrobial education (Hayat et al., 2021). Unfortunately, developed countries like the U.S. are also facing similar challenges (Abbo et al., 2013).
Most respondents utilized iPhone or smartphone applications, peers, UpToDate, medical journals, and IDSA guidelines. This could have a positive impact on the understanding of antimicrobials and AMR among medical students. Similar findings have been reported previously (Saleem et al., 2019; Hand et al., 2021).
The presence of and adherence to institution-based standard treatment guidelines (STGs) is integral in managing infections as they have proven benefits in reducing mortality, morbidity, and therapy cost (Wiedenmayer et al., 2021). Besides, STGs also minimize the probability of AMR emergence. Our study respondents agreed that STGs should be devised in every institution to help limit the increasing risk of AMR. Unfortunately, most health facilities in Pakistan lack STGs, specifically primary and secondary healthcare facilities, which could contribute to unjudicial antimicrobial use in hospitals (Mustafa et al., 2021). Among other AMR eradication strategies to which our respondents agreed include patient counseling about leftover antibiotics and discouraging self-medication with antibiotics in the community. These practices have already been reported in Pakistan (Gillani et al., 2017; Akram et al., 2019). The government should launch mass-level campaigns to educate the public about rational antibiotic use and AMR risk.
There are certain potential limitations of our study. First, the study was conducted on a limited number of medical students in a single province (Punjab) of Pakistan, and the results are not generalizable to the entire study population. However, Punjab is the largest province in Pakistan, where more than 50% of the population of Pakistan resides, and the medical education in Punjab is exemplary for other provinces. Second, the study was carried out online with a convenience sampling approach that could show bias; nevertheless, it was the only suitable option to collect data due to the ongoing COVID-19 pandemic (Hayat et al., 2020). Third, we were unable to determine cause and effect owing to the typical nature of cross-sectional studies. Despite the above-mentioned limitations, the findings of our study are robust and helpful in designing policies to improve antimicrobial education in medical institutes in Pakistan.
Conclusion
Our study respondents had an acceptable level of understanding of antibiotics with a positive perception of AMR. Nevertheless, their preparedness towards numerous aspects of antimicrobial stewardship programs was suboptimal. Formal teaching about rational antimicrobial usage, developing institutional treatment guidelines, and limiting self-medication were practical approaches suggested by the respondents to tackle AMR.
Recommendations
Our study findings suggest that the government should make serious efforts to develop outcome-based curricula for medical education that emphasize AMR education and stewardship. Numerous learning methods, including clinical scenarios, interactive workshops, seminars, conferences, and awareness campaigns, should be opted to equip better medical students about integral components of AMR and stewardship programs. It would be instrumental in providing AMR-related training to medical students in the form of a course that should be part and parcel of their medical curricula. Aside from that, there is a pressing need to adhere to the WHO’s AMR education and training framework, which could assist all medical practitioners in restoring health by conserving the potential of antimicrobials.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics Statement
This study was reviewed and approved by the Xi'an Jiaotong University (No. 2021-0135, dated 20 October 2019). The permission to conduct this study was also obtained from Al-Shifa School of Public health. The participants provided online informed consent to participate in this study.
Author Contributions
KH made a major contribution to this study. NF, MU, MG, ZN, and SR helped in the data collection. FK, FUK, WL, CC, and KH conducted data analysis. KH wrote the manuscript. YF revised the manuscript critically. All authors read and approved the final version of the manuscript.
Funding
This work was funded by the National Natural Science Fund (71974156), “Young Talent Support Plan,” “High Achiever Plan” of Health Science Center, Xi’an Jiaotong University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- Abbo L. M., Cosgrove S. E., Pottinger P. S., Pereyra M., Sinkowitz-Cochran R., Srinivasan A., et al. (2013). Medical Students' Perceptions and Knowledge about Antimicrobial Stewardship: How Are We Educating Our Future Prescribers. Clin. Infect. Dis. 57 (5), 631–638. 10.1093/cid/cit370 [DOI] [PubMed] [Google Scholar]
- Abrar S., Hussain S., Khan R. A., Ul Ain N., Haider H., Riaz S. (2018). Prevalence of Extended-Spectrum-β-Lactamase-Producing Enterobacteriaceae: First Systematic Meta-Analysis Report from Pakistan. Antimicrob. Resist. Infect. Control. 7 (26), 26–0309. 10.1186/s13756-018-0309-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akram A., Maqsood U., Latif M. Z., Arshad H. S., Riaz H., Qureshi M. A. (2019). Self-Medication Phenomenon; A Population Based Study from Lahore. J. Pak Med. Assoc. 69 (4), 523–526. [PubMed] [Google Scholar]
- Alsan M., Morden N. E., Gottlieb J. D., Zhou W., Skinner J. (2015). Antibiotic Use in Cold and Flu Season and Prescribing Quality: A Retrospective Cohort Study. Med. Care 53 (12), 1066–1071. 10.1097/MLR.0000000000000440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asghar S., Atif M., Mushtaq I., Malik I., Hayat K., Babar Z. U. (2020). Factors Associated with Inappropriate Dispensing of Antibiotics Among Non-pharmacist Pharmacy Workers. Res. Soc. Adm Pharm 16 (6), 805–811. 10.1016/j.sapharm.2019.09.003 [DOI] [PubMed] [Google Scholar]
- Aslam A., Gajdács M., Zin C. S., Ab Rahman N. S., Ahmed S. I., Zafar M. Z., et al. (2020). Evidence of the Practice of Self-Medication with Antibiotics Among the Lay Public in Low- and Middle-Income Countries: A Scoping Review. Antibiotics (Basel) 9 (9). 10.3390/antibiotics9090597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atif M., Asghar S., Mushtaq I., Malik I., Amin A., Babar Z. U., et al. (2019). What Drives Inappropriate Use of Antibiotics? A Mixed Methods Study from Bahawalpur, Pakistan. Infect. Drug Resist. 12, 687–699. 10.2147/IDR.S189114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atif M., Zia R., Malik I., Ahmad N., Sarwar S. (2021). Treatment Outcomes, Antibiotic Use and its Resistance Pattern Among Neonatal Sepsis Patients Attending Bahawal Victoria Hospital, Pakistan. PLoS One 16 (1). 10.1371/journal.pone.0244866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augie B. M., Van Zyl R. L., Mcinerney P. A., Miot J. (2021). Knowledge and Perceptions about Antibiotic Resistance and Prudent Antibiotic Prescribing Among Final Year Medical Students in Two African Countries. Int. J. Pharm. Pract. 29 (5), 508–514. 10.1093/ijpp/riab044 [DOI] [PubMed] [Google Scholar]
- Azhar A. B., Khalid A., Shah S. (2019). The Implications of Extensive Drug-Resistant Typhoid Fever: A Case Report. Cureus 11 (6), e5032. 10.7759/cureus.5032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baig M. T., Huma A., Ahmed M., Shahid U., Syed N. (2017). Irrational Antibiotic Prescribing Practice Among Children in Critical Care of Tertiary Hospitals. Pak J. Pharm. Sci. 30 (4Suppl. l), 1483–1489. [PubMed] [Google Scholar]
- Bilal H., Khan M. N., Rehman T., Hameed M. F., Yang X. (2021). Antibiotic Resistance in Pakistan: a Systematic Review of Past Decade. BMC Infect. Dis. 21 (1), 021–05906. 10.1186/s12879-021-05906-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) (2021). Antibiotic Resistance Threats in the United States. Online. Available at: https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (Accesse June 1st, 2021).
- Efthymiou P., Gkentzi D., Dimitriou G. (2020). Knowledge, Attitudes and Perceptions of Medical Students on Antimicrobial Stewardship. Antibiotics (Basel) 9 (11). 10.3390/antibiotics9110821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essack S., Bell J., Burgoyne D. S., Duerden M., Shephard A. (2019). Topical (Local) Antibiotics for Respiratory Infections with Sore Throat: An Antibiotic Stewardship Perspective. J. Clin. Pharm. Ther. 44 (6), 829–837. 10.1111/jcpt.13012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferri M., Ranucci E., Romagnoli P., Giaccone V. (2017). Antimicrobial Resistance: A Global Emerging Threat to Public Health Systems. Crit. Rev. Food Sci. Nutr. 57 (13), 2857–2876. 10.1080/10408398.2015.1077192 [DOI] [PubMed] [Google Scholar]
- Foster C. B., Martinez K. A., Sabella C., Weaver G. P., Rothberg M. B. (2019). Patient Satisfaction and Antibiotic Prescribing for Respiratory Infections by Telemedicine. Pediatrics 144 (3), 2019–0844. 10.1542/peds.2019-0844 [DOI] [PubMed] [Google Scholar]
- Gillani A. H., Ji W., Hussain W., Imran A., Chang J., Yang C., et al. (2017). Antibiotic Self-Medication Among Non-medical University Students in Punjab, Pakistan: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 14 (10). 10.3390/ijerph14101152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillani A. H., Chang J., Aslam F., Saeed A., Shukar S., Khanum F., et al. (2021). Public Knowledge, Attitude, and Practice Regarding Antibiotics Use in Punjab, Pakistan: a Cross-Sectional Study. Expert. Rev. Anti-infective Ther. 19 (3), 399–411. 10.1080/14787210.2021.1823216 [DOI] [PubMed] [Google Scholar]
- Gupta M. K., Vohra C., Raghav P. (2019). Assessment of Knowledge, Attitudes, and Practices about Antibiotic Resistance Among Medical Students in India. J. Fam. Med Prim Care 8 (9), 2864–2869. 10.4103/jfmpc.jfmpc_504_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hand K. S., Clancy B., Allen M., Mayes A., Patel Y., Latter S. M. (2021). 'It Makes Life So Much Easier'-Experiences of Users of the MicroGuide™ Smartphone App for Improving Antibiotic Prescribing Behaviour in UK Hospitals: an Interview Study. JAC Antimicrob. Resist. 3 (3), dlab111. 10.1093/jacamr/dlab111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque M., Rahman N. A. A., Mckimm J., Sartelli M., Kibria G. M., Islam M. Z., et al. (2019). Antibiotic Use: A Cross-Sectional Study Evaluating the Understanding, Usage and Perspectives of Medical Students and Pathfinders of a Public Defence University in Malaysia. Antibiotics (Basel) 8 (3). 10.3390/antibiotics8030154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harakeh S., Almatrafi M., Ungapen H., Hammad R., Olayan F., Hakim R., et al. (2015). Perceptions of Medical Students towards Antibiotic Prescribing for Upper Respiratory Tract Infections in Saudi Arabia. BMJ Open Respir. Res. 2 (1), e000078–000078. 10.1136/bmjresp-2014-000078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayat K., Jamshed S., Rosenthal M., Haq N. U., Chang J., Rasool M. F., et al. (2021). Understanding of Pharmacy Students towards Antibiotic Use, Antibiotic Resistance and Antibiotic Stewardship Programs: A Cross-Sectional Study from Punjab, Pakistan. Antibiotics (Basel) 10 (1). 10.3390/antibiotics10010066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayat K., Rosenthal M., Gillani A. H., Zhai P., Aziz M. M., Ji W., et al. (2019). Perspective of Pakistani Physicians towards Hospital Antimicrobial Stewardship Programs: A Multisite Exploratory Qualitative Study. Int. J. Environ. Res. Public Health 16 (9). 10.3390/ijerph16091565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayat K., Rosenthal M., Xu S., Arshed M., Li P., Zhai P., et al. (2020). View of Pakistani Residents toward Coronavirus Disease (COVID-19) during a Rapid Outbreak: A Rapid Online Survey. Int. J. Environ. Res. Public Health 17 (10). 10.3390/ijerph17103347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y., Wang X., Tucker J. D., Little P., Moore M., Fukuda K., et al. (2018). Knowledge, Attitude, and Practice with Respect to Antibiotic Use Among Chinese Medical Students: A Multicentre Cross-Sectional Study. Int. J. Environ. Res. Public Health 15 (6). 10.3390/ijerph15061165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutchings M. I., Truman A. W., Wilkinson B. (2019). Antibiotics: Past, Present and Future. Curr. Opin. Microbiol. 51, 72–80. 10.1016/j.mib.2019.10.008 [DOI] [PubMed] [Google Scholar]
- Lubwama M., Onyuka J., Ayazika K. T., Ssetaba L. J., Siboko J., Daniel O., et al. (2021). Knowledge, Attitudes, and Perceptions about Antibiotic Use and Antimicrobial Resistance Among Final Year Undergraduate Medical and Pharmacy Students at Three Universities in East Africa. PLoS One 16 (5), e0251301. 10.1371/journal.pone.0251301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik U. R., Chang J., Hashmi F., Atif N., Basir H., Hayat K., et al. (2021). A Simulated Client Exploration of Nonprescription Dispensing of Antibiotics at Drugstores for Pediatric Acute Diarrhea and Upper Respiratory Infection in Lahore, Pakistan. Infect. Drug Resist. 14, 1129–1140. 10.2147/IDR.S301812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markogiannakis A., Korantanis K., Gamaletsou M. N., Samarkos M., Psichogiou M., Daikos G., et al. (2021). Impact of a Non-compulsory Antifungal Stewardship Program on Overuse and Misuse of Antifungal Agents in a Tertiary Care Hospital. Int. J. Antimicrob. Agents 57 (1), 3. 10.1016/j.ijantimicag.2020.106255 [DOI] [PubMed] [Google Scholar]
- Mohsin M., Van Boeckel T. P., Saleemi M. K., Umair M., Naseem M. N., He C., et al. (2019). Excessive Use of Medically Important Antimicrobials in Food Animals in Pakistan: a Five-Year Surveillance Survey. Glob. Health Action. 12 (Suppl. 1), 1697541. 10.1080/16549716.2019.1697541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustafa Z. U., Salman M., Rao A. Z., Asif N., Butt S. A., Shehzadi N., et al. (2020). Assessment of Antibiotics Use for Children Upper Respiratory Tract Infections: a Retrospective, Cross-Sectional Study from Pakistan. Infect. Dis. (Lond) 52 (7), 473–478. 10.1080/23744235.2020.1753887 [DOI] [PubMed] [Google Scholar]
- Mustafa Z. U., Salman M., Yasir M., Godman B., Majeed H. A., Kanwal M., et al. (2021). Antibiotic Consumption Among Hospitalized Neonates and Children in Punjab Province, Pakistan. Expert Rev. Anti-infective Ther. 12, 1–9. 10.1080/14787210.2021.1986388 [DOI] [PubMed] [Google Scholar]
- Nathan C. (2020). Resisting Antimicrobial Resistance. Nat. Rev. Microbiol. 18 (5), 259–260. 10.1038/s41579-020-0348-5 [DOI] [PubMed] [Google Scholar]
- NIH (2017). Antimicrobial Resistance: National Action Plan Pakistan. Online. Available at: https://www.nih.org.pk/amr-national-action-plan-pakistan/ (Accessed October 21, 2021).
- Nogueira-Uzal N., Zapata-Cachafeiro M., Vázquez-Cancela O., López-Durán A., Herdeiro M. T., Figueiras A. (2020). Does the Problem Begin at the Beginning? Medical Students' Knowledge and Beliefs Regarding Antibiotics and Resistance: a Systematic Review. Antimicrob. Resist. Infect. Control. 9 (1), 172. 10.1186/s13756-020-00837-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’neill J. (2016). Tackling Drug-Resistant Infections Globally: Final Report and Recommendations Online. Available at: https://amr-review.org/sites/default/files/160525_Final%20paper_with%20cover.pdf [Accessed July 25, 2019].
- Okedo-Alex I., Madubueze U. C., Umeokonkwo C. D., Oka O. U., Adeke A. S., Okeke K. C. (2019). Knowledge of Antibiotic Use and Resistance Among Students of a Medical School in Nigeria. Malawi Med. J. 31 (2), 133–137. 10.4314/mmj.v31i2.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- PMDC (2011). Curriculum of MBBS. Online. Available at: http://www.pgmipunjab.edu.pk/system/files/PMDC%20and%20HEC%20Curriculum%20MBBS.PDF (Accessed October 21, 2021).
- Qamar F. N., Yousafzai M. T., Dehraj I. F., Shakoor S., Irfan S., Hotwani A., et al. (2020). Antimicrobial Resistance in Typhoidal Salmonella: Surveillance for Enteric Fever in Asia Project, 2016-2019. Clin. Infect. Dis. 71 (Suppl. 3), S276–s284. 10.1093/cid/ciaa1323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qamar F. N., Yousafzai M. T., Khalid M., Kazi A. M., Lohana H., Karim S., et al. (2018). Outbreak Investigation of Ceftriaxone-Resistant Salmonella enterica Serotype Typhi and its Risk Factors Among the General Population in Hyderabad, Pakistan: a Matched Case-Control Study. Lancet Infect. Dis. 18 (12), 1368–1376. 10.1016/S1473-3099(18)30483-3 [DOI] [PubMed] [Google Scholar]
- Qureshi S., Naveed A. B., Yousafzai M. T., Ahmad K., Ansari S., Lohana H., et al. (2020). Response of Extensively Drug Resistant Salmonella Typhi to Treatment with Meropenem and Azithromycin, in Pakistan. Plos Negl. Trop. Dis. 14 (10), e0008682. 10.1371/journal.pntd.0008682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadiq M. I. (2021). Medical Colleges in Pakistan. Online. Available at: https://mbbs.com.pk/medical-colleges-pakistan/ (Accessed August 12, 2021).
- Sakeena M. H. F., Bennett A. A., Jamshed S., Mohamed F., Herath D. R., Gawarammana I., et al. (2018). Investigating Knowledge Regarding Antibiotics and Antimicrobial Resistance Among Pharmacy Students in Sri Lankan Universities. BMC Infect. Dis. 18 (1), 209–3107. 10.1186/s12879-018-3107-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleem Z., Hassali M. A., Hashmi F., Azhar F., Mubarak R., Afzaal A., et al. (2019). Medical and Pharmacy Students’ Knowledge, Attitude and Perception Concerning Antimicrobial Use and Resistance in Pakistan. Pharm. Edu. 19, 199–205. [Google Scholar]
- Scaioli G., Gualano M. R., Gili R., Masucci S., Bert F., Siliquini R. (2015). Antibiotic Use: a Cross-Sectional Survey Assessing the Knowledge, Attitudes and Practices Amongst Students of a School of Medicine in Italy. PLoS One 10 (4), e0122476. 10.1371/journal.pone.0122476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Science M., Timberlake K., Morris A., Read S., Le Saux N. (2019). Quality Metrics for Antimicrobial Stewardship Programs. Pediatrics 143 (4), 2018–2372. 10.1542/peds.2018-2372 [DOI] [PubMed] [Google Scholar]
- Scobie A., Budd E. L., Harris R. J., Hopkins S., Shetty N. (2019). Antimicrobial Stewardship: an Evaluation of Structure and Process and Their Association with Antimicrobial Prescribing in NHS Hospitals in England. J. Antimicrob. Chemother. 74 (4), 1143–1152. 10.1093/jac/dky538 [DOI] [PubMed] [Google Scholar]
- Struzycka I., Mazinska B., Bachanek T., Boltacz-Rzepkowska E., Drozdzik A., Kaczmarek U., et al. (2019). Knowledge of Antibiotics and Antimicrobial Resistance Amongst Final Year Dental Students of Polish Medical Schools-A Cross-Sectional Study. Eur. J. Dent. Educ. 23 (3), 295–303. 10.1111/eje.12430 [DOI] [PubMed] [Google Scholar]
- Tacconelli E., Carrara E., Savoldi A., Harbarth S., Mendelson M., Monnet D. L., et al. (2018). Discovery, Research, and Development of New Antibiotics: the WHO Priority List of Antibiotic-Resistant Bacteria and Tuberculosis. Lancet Infect. Dis. 18 (3), 318–327. 10.1016/S1473-3099(17)30753-3 [DOI] [PubMed] [Google Scholar]
- Tiong T. W., Chua S. S. (2020). Knowledge and Attitude of University Students on Antibiotics: A Cross-Sectional Study in Malaysia. Drug Healthc. Patient Saf. 12, 135–144. 10.2147/DHPS.S253301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umair M., Tahir M. F., Ullah R. W., Ali J., Siddique N., Rasheed A., et al. (2021). Quantification and Trends of Antimicrobial Use in Commercial Broiler Chicken Production in Pakistan. Antibiotics (Basel) 10 (5). 10.3390/antibiotics10050598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations (2016). High-level Meeting on Antimicrobial Resistance. Online. Available at: https://www.un.org/pga/71/event-latest/high-level-meeting-on-antimicrobial-resistance/ (Accessed August 13, 2021).
- Van Der Voort T., Brinkman D. J., Benemei S., Böttiger Y., Chamontin B., Christiaens T., et al. (2019). Appropriate Antibiotic Prescribing Among Final-Year Medical Students in Europe. Int. J. Antimicrob. Agents 54 (3), 375–379. 10.1016/j.ijantimicag.2019.05.008 [DOI] [PubMed] [Google Scholar]
- Wasserman S., Potgieter S., Shoul E., Constant D., Stewart A., Mendelson M., et al. (2017). South African Medical Students' Perceptions and Knowledge about Antibiotic Resistance and Appropriate Prescribing: Are We Providing Adequate Training to Future Prescribers. S. Afr. Med. J. 107 (5), 405–410. 10.7196/SAMJ.2017.v107i5.12370 [DOI] [PubMed] [Google Scholar]
- Watkins R. R., Bonomo R. A. (2020). The Ongoing Threat of Antimicrobial Resistance. Infect. Dis. Clin. North. Am. 34 (4), xiii. 10.1016/j.idc.2020.09.001 [DOI] [PubMed] [Google Scholar]
- WHO (2021). World Health Organization. Online. Available at: http://www.wpro.who.int/entity/drugresistance/resources/global_action_plan_eng (Accessed August 13, 2021).
- Wiedenmayer K., Ombaka E., Kabudi B., Canavan R., Rajkumar S., Chilunda F., et al. (2021). Adherence to Standard Treatment Guidelines Among Prescribers in Primary Healthcare Facilities in the Dodoma Region of Tanzania. BMC Health Serv. Res. 21 (1), 272. 10.1186/s12913-021-06257-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2015). Global Action Plan on Antimicrobial Resistance. Geneva, Switzerland: WHO Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.