Abstract
According to a national claims database, remote retinal imaging utilization in the U.S. increased rapidly from 2011 to 2020, but insurance coverage declined, with disproportionate impact on vulnerable populations including older, Black, and lower-income patients.
Keywords: remote retinal imaging, telemedicine, claims data, diabetic retinopathy
Recent increases in eye care demand and the COVID-19 pandemic emphasize the need for tele-ophthalmology services such as remote eye imaging to screen for diabetic retinopathy (DR). Only half of older Americans with diabetes undergo annual retinopathy screening as recommended by the American Academy of Ophthalmology.1 Remote retinal imaging reduces costs, improves screening rates, and enhances care access for rural and underserved populations.2 Before passage of the H.R. 6074 Coronavirus Preparedness and Response Supplement Appropriations Act of 2020,3 which relaxed restrictions on telemedicine reimbursement, inconsistent insurance coverage and dwindling reimbursements were major barriers to implementing tele-retinal services.4 Here, we analyzed trends in remote retinal imaging utilization using a national claims database and evaluated factors associated with insurance payments.
Using the OptumLabs® Data Warehouse (OLDW) database of over 160 million de-identified administrative claims for commercial and Medicare Advantage enrollees,5 we identified claims from January 1, 2011 to December 31, 2020 with Current Procedural Terminology (CPT) codes for remote eye imaging (92227 and 92228) by any provider, and fundus photography (92250) by non-eye care providers. Visit diagnoses were categorized using International Classification of Disease (ICD) 9th/10th edition codes (Table S1). Provider specialty, practice settings, insurance types, patient demographic, and socioeconomic status variables including Rural Urban Commuting Area (RUCA) codes were collected also (Table S1). Claim incidences were standardized to total claims in 2020. Insurance payment coverage (paid versus denied) and insurer-paid amounts (USD; inflation adjusted to 2020 using the Consumer Price Index) were reported by year and stratified by CPT, visit diagnosis, insurance type, demographic, and socioeconomic factors. For each CPT code, a multiple logistic regression model was fit with the binomial outcome insurance payment and year as a continuous, main independent variable. Common mediators that affect likelihood of claim payment—visit diagnosis, provider specialty, provider setting, and insurance— were chosen a priori and were also adjusted for in the models. General estimating equations were used to adjust for patients with multiple visits. Analyses were conducted in SAS (v9.4).
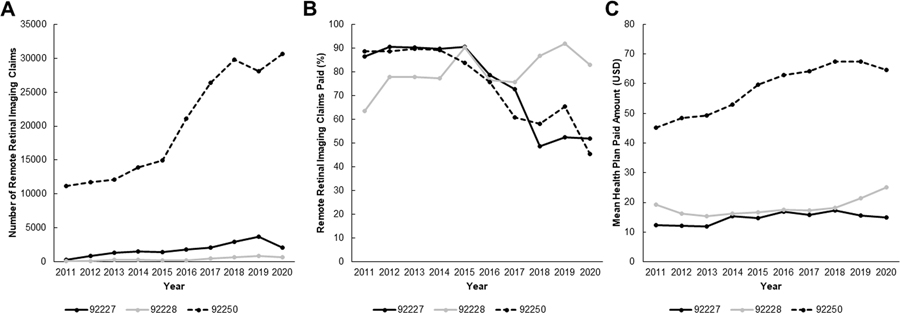
Remote retinal imaging use increased from 11,603 claims in 2011 to 33,392 in 2020 (Figure 1A). Most claims used CPT 92250 (90.0%) rather than more specific remote imaging codes 92227 (8.2%) or 92228 (1.8%). The proportion of claims paid to physicians decreased from 88% in 2011 to 47% in 2020, with claims for 92227 and 92250 showing the greatest decline in coverage in recent years (Figure 1B). For claims that were paid, the mean[SD] inflation-adjusted insurer-paid amounts (USD) for codes 92227 and 92228 remained mostly unchanged from 2011 to 2020 from $12.38[$14.54] to $14.85[$7.15] for 92227 and from $19.31[$9.04] to $25.10[$10.74] for 92228. By contrast, payments for 92250 were much higher and increased from $45.15[$36.17] in 2011 to $64.70[$37.38] in 2020 (Figure 1C).
Figure 1. Utilization of Remote Retinal Imaging Services Over Time by Diagnosis.
Line graphs showing (A) remote retinal imaging utilization by year and CPT codes, (B) the proportion of approved payments by year and CPT code, and (C) mean insurer-paid amount in USD over time for each CPT code.
While use of remote imaging for diabetic and non-diabetic eye conditions remained unchanged, screening for diabetes without eye disease increased, especially over the latter half of the decade, and constituted the majority of claims by 2019 (Figures S1A–S1C). CPT 92227 was inappropriately utilized for non-diabetic eye diseases after the code’s inception in 2011, but its use declined after 2015. Insurance payments for 92227 and 92250 decreased the most for diabetics without eye disease (Figures S1D & S1F), while coverage for 92228 varied between years, likely due to the overall lower utilization, and did not impact the overall trend of declining insurance coverage (Figure S1E). The adjusted odds ratio (OR) [95% Confidence Interval] for claims payment per year was 0.90[0.88–0.93] for 92227 and 0.84[0.88–0.93] for 92250, and increased for 92228 (OR 1.16[1.11–1.21])(Table S1).
Payments for remote imaging across all demographic and socioeconomic factors decreased over time (Figure S2A–S2G). The decline in insurance coverage was greatest for older patients, more in women than men, and among Blacks compared to other racial groups. Coverage for lower income enrollees was also lower and exhibited greater decline, but did not differ between education levels or population densities. Reimbursement rates were much lower for Medicare Advantage than commercial insurance enrollees, and also decreased with time.
Our study showed a major decline in proportion of claims paid for remote retinal imaging over the decade, especially for CPT 92227 which decreased from 86.5% in 2011 to 51.9% in 2020, similar to findings from our tele-retinal screening program in California that used the same billing code.6 Yet, this decline is occurring at a time of rapid expansion in using remote imaging to screen diabetics without eye diseases. In fact, claims for these patients were more often denied compared to those with eye diseases, even for 92227 which is designated for screening patients without retinopathy. This inconsistency in insurance coverage illustrates the confusing reimbursement landscape for tele-ophthalmology services.
Mean payment amounts were higher for 92250 than 92227 or 92228, consistent with their total RVU in 2020 of 1.27, 0.38, and 0.96, respectively. However, while inflation-adjusted payments for remote imaging codes 92227 and 92228 remained stagnant over 10 years, payment amounts for the less-specific fundus photography code 92250 steadily increased. These differences may incentivize providers to utilize billing codes with higher reimbursements rather than the appropriate indications. Also jarring is the striking difference in coverage between Medicare Advantage and commercial insurance enrollees, which likely explains the disproportionate decrease in coverage of older individuals, a group most likely to benefit from remote eye care. We additionally found payment frequencies lower among women, Blacks, and lower income households, further emphasizing the differential impact of declining payments.
This study may have limited generalizability as OLDW only includes commercially insured and Medicare Advantage enrollees. Furthermore, while CPT 92227 and 92228 are used for asynchronous or “store-and-forward” remote retinal imaging, tele-ophthalmology using synchronous or live interfaces may not be captured.7 Because we included 92250 billed by non-eye care providers only, ophthalmologists billing 92250 for remote services were excluded.
Although remote retinal imaging can reduce screening costs and detect vision-threatening disease earlier, declining and inconsistent insurance coverage pose substantial barriers against widespread adoption. Stakeholders and payers should be encouraged to expand coverage for remote imaging to improve eye care access and reduce vision loss.
Supplementary Material
Financial Support:
This work is supported by the UC Davis Eye Center. GY is supported by NIH R01 EY032238, NIH R21 EY031108, the BrightFocus Foundation, and the Macula Society. This project was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860. Dr. Lieng was supported by training funds from the J. William Kohl Summer Scholarship for Medical Students. The funding organizations did not play any role in the design or conduct of this retrospective study; the collection, management, analysis, or interpretation of data; or the preparation, review, approval, submission decision of the manuscript. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
Conflict of Interest:
All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr. Yiu reports grants and personal fees from Alimera, Allergan, Carl Zeiss Meditec, Clearside Biomedical, Genentech, Gyroscope Therapeutics, Intergalactic Therapeutics, Iridex, NGM Biopharmaceutical, Regeneron, Topcon, and Verily, all outside of the submitted work. No other disclosures were reported.
Meeting Presentation: Presented at the Association for Research in Vision and Ophthalmology Annual Meeting, 2021 and Women in Ophthalmology Summer Symposium, 2021
This article contains additional online-only material. The following should appear online-only: Figures S1 and S2, Table S1.
REFERENCES
- 1.Lee PP, Feldman ZW, Ostermann J, et al. Longitudinal rates of annual eye examinations of persons with diabetes and chronic eye diseases. Ophthalmology 2003;110(10):1952–9. [DOI] [PubMed] [Google Scholar]
- 2.Mansberger SL, Sheppler C, Barker G, et al. Long-term Comparative Effectiveness of Telemedicine in Providing Diabetic Retinopathy Screening Examinations: A Randomized Clinical Trial. JAMA Ophthalmol 2015;133(5):518–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.[D-NY-17] RNML. H.R.6074 - Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020. In: Congress USt, ed. HR 6074. House-Appropriations; Budget 2020; v. 116–123. [Google Scholar]
- 4.Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med 2016;375(14):1400. [DOI] [PubMed] [Google Scholar]
- 5.OptumLabs. OptumLabs and OptumLabs Data Warehouse (OLDW) Descriptions and Citation. Reproduced with permission from OptumLabs. ed. Eden Prairie, MN: n.p., July 2020. [Google Scholar]
- 6.Ellis MP, Bacorn C, Luu KY, et al. Cost Analysis of Teleophthalmology Screening for Diabetic Retinopathy Using Teleophthalmology Billing Codes. Ophthalmic Surg Lasers Imaging Retina 2020;51(5):S26–S34. [DOI] [PubMed] [Google Scholar]
- 7.Ophthalmology AAo. Telehealth Retinal Codes 2019. v. 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.