Abstract
PURPOSE
Mailed fecal immunochemical test (FIT) programs can facilitate colorectal cancer (CRC) screening. We sought to identify modifiable, clinic-level factors that distinguish primary care clinics with higher vs lower FIT completion rates in response to a centralized mailed FIT program.
METHODS
We used baseline observational data from 15 clinics within a single urban federally qualified health center participating in a pragmatic trial to optimize a mailed FIT program. Clinic-level data included interviews with leadership using a guide informed by the Consolidated Framework for Implementation Research (CFIR) and FIT completion rates. We used template analysis to identify explanatory factors and configurational comparative methods to identify specific combinations of clinic-level conditions that uniquely distinguished clinics with higher and lower FIT completion rates.
RESULTS
We interviewed 39 clinic leaders and identified 58 potential explanatory factors representing clinic workflows and the CFIR inner setting domain. Clinic-level FIT completion rates ranged from 30% to 56%. The configurational model for clinics with higher rates (≥37%) featured any 1 of the following 3 factors related to support staff: (1) adding back- or front-office staff in past 12 months, (2) having staff help patients resolve barriers to CRC screening, and (3) having staff hand out FITs/educate patients. The model for clinics with lower rates involved the combined absence of these same 3 factors.
CONCLUSIONS
Three factors related to support staff differentiated clinics with higher and lower FIT completion rates. Adding nonphysician support staff and having those staff provide enabling services might help clinics optimize mailed FIT screening programs.
Key words: primary health care, configurational comparative methods, federally qualified health center, colorectal cancer, screening, fecal immunochemical testing, mailed FIT, pragmatic trial, practice-based research, support staff
INTRODUCTION
Colorectal cancer (CRC) is preventable with screening such as colonoscopy every 10 years or a fecal immunochemical test (FIT) annually.1 Whereas national targets call for 80% screening, only 66% of the US population was up to date in 2018.2 In federally qualified health centers (FQHCs) nationally—which serve low-income, racially diverse populations—only 44% of eligible adults were up to date in 2018.3,4 Over the past year in the United States, CRC screening rates dropped precipitously, owing to the coronavirus disease 2019 (COVID-19) pandemic5; this was likely amplified in FQHC settings, where patients face multiple barriers to preventive care.3,6
Mailed FIT programs—whereby fecal immunochemical tests are mailed directly to patients’ homes and can be returned via mail or in person—increase CRC screening rates.7–10 Implementation is prudent in light of the COVID-19 pandemic.11,12 Compared with visit-based screening, mailed FIT programs reach a broader population and might decrease screening disparities.13–16 However, return rates vary widely,7,17 owing in part to patient, intervention, and clinic characteristics.7,8,18–20 Although mailed FIT programs comprise a population outreach strategy, return rates are greater among patients who attend a clinic visit in the same year,21,22 underscoring the importance of clinic support.23 Resources exist to help implement mailed FIT programs,18,24 but research is needed to identify mutable clinic-level factors that optimize these programs.
Therefore, we applied configurational comparative methods (CCMs) to identify clinic-level factors that distinguish clinics with higher vs lower FIT completion rates among patients eligible for mailed FITs. We analyzed baseline data from Participatory Research to Advance Colon Cancer Prevention (PROMPT), a pragmatic trial to optimize a mailed FIT program within an urban FQHC system (ClinicalTrials. gov: NCT03167125).25
METHODS
The PROMPT trial used a patient engagement approach to refine and test the messages, format, and timing of alerts and reminders for the FQHC’s mailed FIT program.25,26 Baseline observational data from PROMPT were collected in 2018-2019 and analyzed in 2019-2020. Our approach was theoretically informed by literature on context,27 constructs from the Consolidated Framework for Implementation Research (CFIR),28,29 and research defining clinical workflows.23,30 The Kaiser Permanente Northwest Institutional Review Board (Portland, Oregon) approved PROMPT, with ceding agreements from partnering institutions.
Study Setting
The participating FQHC has a mission to eliminate disparities in health care access and outcomes. At the time of data collection, the FQHC operated 27 medical clinics serving nearly 220,000 patients; 84% were Hispanic, and 22% were served in a language other than English. A majority (57%) of providers and staff deliver services in Spanish, and clinic staff access qualified interpretation for other languages. Fifteen clinics participated in the present study. We excluded clinics that (1) provided only pediatric care, (2) focused on specific populations (HIV, dental), (3) were closing, or (4) had no paneled patients (patients not assigned primary care providers). The FQHC tracks CRC screening rates annually for Uniform Data System reporting.31
In 2012, the FQHC hired a new Medical Director of Quality, focused on a culture of quality improvement. In 2015, CRC screening became an FQHC quality measure, was tied to performance reviews for clinic leadership, and led to implementation of a centralized mailed FIT program. Table 1 summarizes components of the centralized mailed FIT program led by the quality department and workflows for individual clinic sites. Program components vary because they are operationalized by each clinic. We designed our analysis to identify mutable clinic-level factors that distinguished higher- from lower-performing clinics.
Table 1.
Overview of FQHC Program Components for CRC Screening
| Program Component | Standardized Workflows | Flexible Workflows |
|---|---|---|
| Centralized mailed FIT | Annually, the quality department is responsible for (1) identifying age-eligible members due for CRC screening, (2) partnering with a vendor to mail FITs and an information sheet in English and Spanish to each member’s address of record, and (3) generating a list of patients 4 weeks after the mailing who have not returned the mailed FIT. | The quality department distributes these lists to each clinic; clinics are encouraged but not required to conduct patient outreach calls to encourage FIT completion. |
| Clinic-level workflows | Daily, staff at individual clinics are expected to promote visit-based CRC screening emphasizing FIT by (1) chart scrubbing 1-2 days before scheduled appointments to identify patients due, (2) communicating to care team verbally (eg, huddle) or via notations on the schedule regarding who is coming in and due for CRC screening, and (3) reviewing the EHR point-of-care reminder system during patient rooming. Medical assistants place a standing medical order for patients due and educate patients on CRC screening importance and how to complete the FIT. If patients decline FIT or prefer colonoscopy, medical assistants inform the provider, who will then engage the patient in a CRC screening discussion. |
Other decisions regarding the type and frequency of CRC screening outreach, follow-up (eg, number and timing of patient reminders, patient incentives for FIT completion), and other strategies (eg, promotional flyers, health fairs) to encourage completion of FIT testing are determined by local clinic leadership and staff. |
CRC = colorectal cancer; EHR = electronic health record; FIT = fecal immunochemical test; FQHC = federally qualified health center.
Key Informant Interviews
We conducted key informant interviews with health system and clinic leaders from June to July 2018. We first conducted a group interview with 2 administrators from the FQHC quality department to understand standard clinic-level CRC screening workflows and activities. Research team members (J.L.S., G.D.C., M.M.D., J.H.T.) used data from this interview to prepare the semistructured interview guide for clinic leaders, aligned with CFIR categories28,29 and the team’s prior experience with CRC workflows (Supplemental Appendix 1).23,32,33 The interview guide addressed the CFIR domains for inner setting (CRC screening workflows), intervention characteristics (mailed FIT perceptions), outer setting (state/national factors), process (clinical champions), and individual characteristics (role) (Supplemental Table 1).28
We invited the “leadership triad” at each clinic to participate, which typically included the clinic administrator, back-office manager or nurse supervisor, and the site medical director. An executive assistant in the FQHC quality department identified leaders for the 15 clinics and scheduled telephone interviews. Interviews were conducted by an experienced qualitative researcher (J.L.S.),17,19,33,34 lasted approxi-
mately 60 minutes, and were audio recorded and transcribed.
Screening Outcome Calibration
The primary outcome variable was the clinic-level percentage of FIT completion among patients eligible for the mailed FIT program. To identify eligible patients, centralized FQHC staff used electronic health record codes aligned with the Uniform Data System metric to identify patients overdue for CRC screening who had a visit during the prior year (June 25, 2017-June 24, 2018) and no prior history of colon cancer (Supplemental Figure 1).35 Table 2 summarizes characteristics of the 29,329 patients eligible for the mailed FIT program, at the clinic level.
Table 2.
Clinic-Level, Mailed-FIT–Eligible Patient Characteristics (n = 29,329)
| Characteristic | Mean % (Range) |
|---|---|
| Hispanic | 79.7 (47.6-96.8) |
| Non-English speaker | 69.3 (43.5-87.5) |
| Female | 57.4 (40.0-62.8) |
| Medicaid | 54.3 (40.4-71.7) |
| Uninsured | 9.8 (4.1-21.0) |
FIT = fecal immunochemical test.
Completion rates for FIT ranged from 30% to 56% across clinics (mean, 41%). We were unable to distinguish if completed FITs were from the mailing or from a visit. To identify higher- and lower-performing clinics, we set the threshold for dichotomization at the 40th percentile, which was 37%; this threshold for FIT completion was clinically meaningful,2,3 and a break also occurred here in the distribution of clinic-level completion rates, a sizable gap of 3.6 points. There were 9 clinics classified with higher completion rates (38.5%-56.3%) and 6 with lower completion rates (29.7%-34.9%). The mean (range) data for patient demographics across these 2 clinic groups are provided in Supplemental Table 2.
Data Analysis
Qualitative Data
We analyzed interviews using a template analysis approach.36–38 After transcript review, staff trained in qualitative analysis (J.L.S., J.S.R.) developed an Excel spreadsheet for the analysis, in which columns represented each clinic, and rows represented topics covered during the interview; J.L.S. and J.S.R. entered data into the template and discussed preliminary results with the study team. A final spreadsheet was produced after multiple reviews of the template and transcripts that detailed activities, workflows, and barriers and facilitators, indicated by a binary (yes/no) endorsement from each clinic. This approach, when combined with 6 quantitative factors (eg, age/years site in service, total number of changes endorsed), yielded 58 different potential explanatory factors for the configurational analysis (Supplemental Table 3). Factors were predominantly related to CFIR inner context (clinic description, changes in past 12 months) and clinical workflows (FIT distribution, reminders, processing).
Configurational Comparative Methods
We applied CCMs to identify mutable clinic-level factors directly linked to higher or lower FIT completion rates; CCMs provide a formal mathematical approach to conduct cross-case analysis that uses Boolean algebra, set theory, and applied logic to identify a “minimal theory”—a crucial set of difference-making combinations that uniquely distinguish one group of cases from another.17,39–50 A particular analytic strength of CCMs is their ability to identify causal complexity (when specific combinations of conditions together explain an outcome) and equifinality (when multiple paths lead to the same outcome).51 Configurational comparative methods can be applied with samples of various sizes including small-n studies. The objective of CCMs is to identify necessary and sufficient conditions, a fundamentally different search target than that of correlation-based methods. The use of CCMs is gaining traction in health care research.40,46,52–54
To decrease our data set of 58 factors, we applied a multistep configurational approach, as described previously.17,43,44 We started by using the minimally sufficient conditions (msc) function in the R package Coincidence Analysis (cna; the R Foundation)55 to analyze all candidate factors and clinics at once to identify specific configurations of conditions with particularly strong connections to the outcome—higher or lower FIT completion rates. We considered all 1-, 2-, 3-, and 4-condition configurations that met predetermined thresholds for consistency (≥80%) and coverage (≥80%). Consistency indicates how reliably a solution yields an outcome and is calculated as the proportion of cases that have the outcome and are covered by the solution over the total number of cases covered by the solution. Coverage indicates how well a solution accounts for an outcome and is calculated as the proportion of cases that have the outcome and are covered by the solution over the total number of cases with the outcome.41 We then generated a condition table to organize and list the Boolean output, in which rows contained specific configurations of conditions that met a specified consistency level. Using this approach, we inductively analyzed the entire data set and narrowed the initial set of potential explanatory factors to a subset of 7 candidate factors to model.
We then developed models by iteratively using model-building functions in the cna software package. We assessed final models on the basis of their overall consistency and coverage, prioritizing solutions that aligned with logic, theory, and background knowledge; for which different values for the exact same set of factors could explain both the presence and the absence of the outcome with ≥80% consistency and ≥80% coverage; with no model ambiguity.17,56
RESULTS
We interviewed 39 leaders; an average of 3 informants participated per clinic (range, 1-4). Participant roles included site medical directors (n = 8), clinic administrators (n = 13), back-office managers (n = 14), and other staff leaders (n = 4). Reasons for nonparticipation included clinic priorities or staff leave.
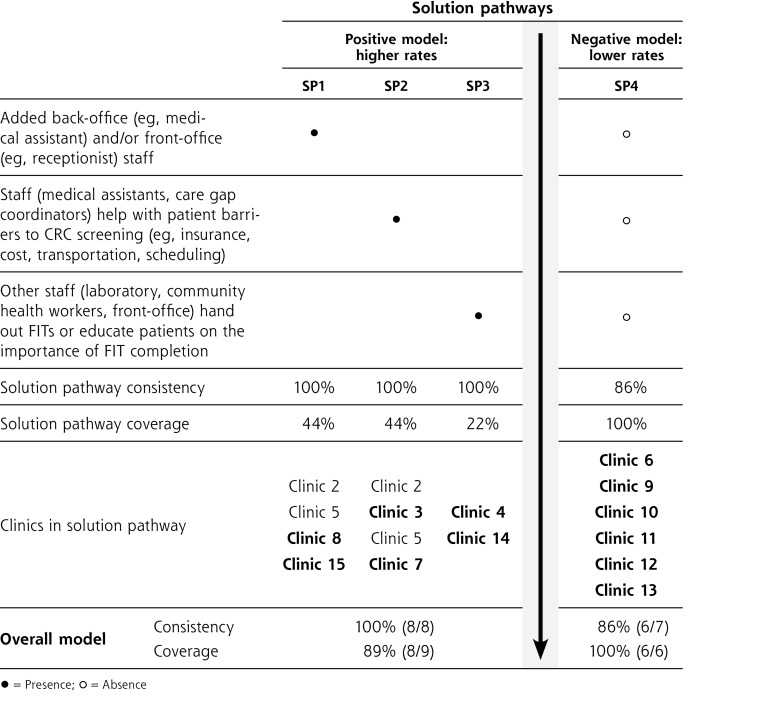
The CCM analysis identified 2 models with the same 3 factors (Figure 1). For the positive model, the presence of any 1 of the 3 factors consistently distinguished clinics with higher FIT completion rates (solution pathways [SPs] 1-3). For the negative model, the combined absence of all 3 factors consistently distinguished clinics with lower rates (see SP 4).
Figure 1.
Final model from CCM analysis: 3 clinic-level factors that distinguish clinics with higher and lower FIT completion rates.
CCM = configurational comparative method; CRC = colorectal cancer; FIT = fecal immunochemical test; SP = solution pathway.
Note: This figure displays how the same 3 factors operate in both the positive and negative solutions. This means that the presence of any of the 3 factors can appear in the positive model (clinics with higher FIT screening rates) and that these same 3 factors are all absent in the negative model (clinics with lower screening rates). For the positive model, clinics in bold only fall in 1 solution pathway, such that each pathway uniquely explains at least 2 clinics. Although Clinic 1 (a higher-performing clinic) was not accounted for by the positive solution, overall consistency and coverage for both models was high.
Clinics with higher FIT completion rates consistently had the presence of any 1 of the following 3 factors (Figure 1):
The addition of back-office (eg, medical assistants) and/or front-office (receptionists) staff in the past 12 months
Medical assistants or care gap coordinators to help with patient barriers (insurance, cost, transportation, scheduling) if patients ask and staff have time
Staff (laboratory, community health workers, front office) to hand out kits/educate patients on the importance of FIT completion
All 3 factors related to the addition of nonphysician support staff or team-based care to facilitate patient education, FIT distribution, and addressing screening barriers. The positive model featuring the presence of any 1 of these 3 factors showed 100% consistency (8/8) and 89% coverage (8/9). In addition, each of the 3 SPs in the positive model uniquely explained 2 clinics with higher completion rates.
In the negative model, the same 3 factors also distinguished clinics with lower FIT completion rates, with 86% consistency (6/7) and 100% coverage (6/6). In this case, the combined absence of all 3 factors linked directly to lower performance in these clinics.
DISCUSSION
We used CCMs to identify combinations of factors that uniquely distinguish clinics with high vs low FIT completion rates for patients exposed to a mailed FIT program. Clinics with higher FIT completion rates added office staff in the past 12 months, had staff help patients overcome barriers to screening, or relied on nonphysician team members to distribute FITs and deliver education on FIT completion during visits. The absence of these factors in combination was found in clinics with lower FIT completion rates.
Our present results highlight the difference-making role of support staff presence and activities on FIT completion. These findings are useful given a recent CCM analysis that identified the role of immutable clinic factors (eg, size, ownership) in changes in preventive care delivery.54 Our approach identified modifiable factors that individual clinics or learning health care systems57,58 can address to improve FIT screening. Although systems might have standardized protocols and centralized programs to support population outreach, clinic-level activities also contribute to program effectiveness.27,59 Research has shown that CRC screening rates are higher for those who attend ≥1 clinic visit in the prior year, compared with those with no clinic visits.21,22,60 Our findings add to this literature by identifying mutable clinic-level factors, related to staffing and team-based care models, that are difference makers for FIT completion. Future research should explore if improvements are due to visit-based behaviors, enhanced population outreach, or both.
Our observation that adding support staff was linked to program outcomes is consistent with prior research on CRC and preventive services in primary care. In a prior CCM analysis conducted by our team, centralized dedicated staffing was linked to the successful implementation of a mailed FIT program.17 Similarly, qualitative analysis of interviews with health plan and clinic leaders identified the importance of funding in-clinic staff to support CRC screening.61 Recent studies highlight the importance of adequate staffing to enable team-based care models in delivering primary care and preventive services.62–64 Recommendations for staffing patient-centered medical home programs suggest 1.57 full-time personnel more (per primary care clinician) than current Medical Group Management Association medians.62 Unfortunately, physician and staff turnover rates in community practices have been estimated at 41% to 53% over a period of 1 to 3 years.65–67 Inadequate staffing and clinic turnover are detrimental to mailed FIT program implementation.32,33
Our findings show the importance of clinical workflows that support a team-based approach, in which nonphysician staff can educate patients about CRC screening and assist in overcoming barriers. Although our partner FQHC had standardized workflows, the varied efforts of medical assistants, care gap coordinators, laboratory staff, and front-office staff at the clinic level influenced FIT completion rates.
Federally qualified health centers are required to provide enabling services such as health education and transportation.68 Research points to the importance of team-based care69 and to the increasing role played by medical assistants and front-office staff in preventive and chronic illness care,64 population health efforts, and patient education.70–72 New roles (panel managers, community health workers) are also being added in primary care.73,74 Our findings highlight the importance of evaluating clinic-level workflows that support enabling services as possible mediators of successful implementation.27,59,75 In addition, whereas quality metrics might help motivate clinics to promote FIT screening, work is needed to align FIT reimbursement to cover tasks (reminders, education) associated with completion.14,61,76
Care disruptions as a result of COVID-19 have led to fewer in-person visits and restrictions on endoscopy.5 Mailed FIT testing is a cost-effective alternative to colonoscopy and does not require a visit. Establishing workflows to support mailed FIT programs or mail FITs to patients attending telehealth visits might help overcome COVID-19–related disruptions. In addition, mailed FIT interventions are associated with increased adherence to CRC testing over time.77 Future studies could compare mailed FIT program effectiveness as a first line of outreach for patients or as a strategy for follow-up after visits. Findings from our study are suggestive of recent recommendations to enable high-quality primary care in the United States broadly.78
Strengths and Limitations
The present study had several strengths, including systematic data collection, a large number of factors included in the CCM analysis, and our use of a conceptual model to guide data collection and analysis. We applied CCMs to understand clinic-level factors associated with FIT completion rates, a knowledge gap identified in prior research.17,79
Our study also had limitations including the use of observational data. Thus, we cannot conclude that adding staff or team-based care caused improved FIT completion rates. Second, we only looked within 1 system at 1 point in time. Nevertheless, the number of observations was large, and the clinics showed a robust (26.5-percentage point) variation in completion rates. Third, we were not able to interview the full leadership triad at each clinic, engage patients, or conduct observation visits; this could have limited our ability to capture the full range of clinic activities. Finally, we prioritized mutable clinic-level conditions, which limited our ability to explore the effect of policy or patient characteristics.
Conclusions
The present study identified 3 factors that distinguished clinics with higher FIT completion rates from clinics with lower rates. Our findings emphasize the difference-making role of nonphysician support staff. Clinics seeking to optimize mailed FIT outreach should consider adding office staff and supporting team-based care models to provide enabling services to facilitate CRC completion.
Supplementary Material
Acknowledgments
The authors would like to thank the participating patients and our federally qualified health center collaborators in research. We especially appreciate Shelby Harbison’s manuscript comments, Rose Gunn’s assistance with data collection and analysis, and Jill Pope’s editing.
Footnotes
Conflicts of interest: From November 2014 to August 2015, Dr Coronado served as a Co-Investigator on an industry-funded study (EpiGenomics) to evaluate patient adherence to an experimental blood test for colorectal cancer. From September 2017 to June 2018, Dr Coronado served as the Principal Investigator on an industry-funded study (Quidel Corporation) to compare the clinical performance of an experimental fecal immunochemical test (FIT) with an FDA-approved FIT. In 2020, Dr Coronado served as a scientific advisor for Exact Sciences and Guardant Health. All other authors report none.
Author contributions: M.M.D., J.L.S., A.F.P., J.H.T., and G.D.C. helped conceptualize the study. M.M.D., J.L.S., A.F.P., E.J.M., A.L.E., B.Y., J.S.R., and D.N. played key roles in helping collect and analyze the data. M.M.D., E.J.M., J.L.S., A.F.P., and J.H.T. drafted the manuscript. All authors helped revise the manuscript. All authors read and approved the final manuscript.
Funding support: This study was funded by the National Institute on Minority and Health Disparities (U01MD010665). Dr Davis was supported in part by a Cancer Prevention, Control, Behavioral Sciences, and Populations Sciences Career Development Award from the National Cancer Institute (K07CA211971). The findings and conclusions in this study are those of the authors and do not necessarily represent the official position of the funders.
Trial registration: National Clinical Trial (NCT) Identifier NCT03167125.
References
- 1.Bibbins-Domingo K, Grossman DC, Curry SJ, et al. ; US Preventive Services Task Force . Screening for colorectal cancer: US Preventive Services Task Force recommendation statement. JAMA. 2016; 315(23): 2564–2575. 10.1001/jama.2016.5989 [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society . Colorectal cancer facts & figures 2020-2022. Published 2020. Accessed Jan 14, 2022. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/colorectal-cancer-facts-and-figures/colorectal-cancer-facts-and-figures-2020-2022.pdf
- 3.National Colorectal Cancer Roundtable . Colorectal cancer screening rates reach 44.1% in FQHCs in 2018. Accessed Jan 14, 2022. https://nccrt.org/colorectal-cancer-screening-rates-reach-44-1-in-fqhcs-in-2018/
- 4.Health Resources & Services Administration, Health Center Program . 2018 National Health Center data. Accessed Jan 14, 2022. https://bphc.hrsa.gov/uds/datacenter.aspx
- 5.Gupta S, Lieberman D.. Screening and surveillance colonoscopy and COVID-19: avoiding more casualties. Gastroenterology. 2020; 159(4): 1205–1208. 10.1053/j.gastro.2020.06.091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ylitalo KR, Camp BG, Umstattd Meyer MR, et al. Barriers and facilitators of colorectal cancer screening in a federally qualified health center (FQHC). J Am Board Fam Med. 2019; 32(2): 180–190. 10.3122/jabfm.2019.02.180205 [DOI] [PubMed] [Google Scholar]
- 7.Davis MM, Freeman M, Shannon J, et al. A systematic review of clinic and community intervention to increase fecal testing for colorectal cancer in rural and low-income populations in the United States - how, what and when? BMC Cancer. 2018; 18(1): 40. 10.1186/s12885-017-3813-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dougherty MK, Brenner AT, Crockett SD, et al. Evaluation of interventions intended to increase colorectal cancer screening rates in the United States: a systematic review and meta-analysis. JAMA Intern Med. 2018; 178(12): 1645–1658. 10.1001/jamainternmed.2018.4637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rat C, Latour C, Rousseau R, et al. Interventions to increase uptake of faecal tests for colorectal cancer screening: a systematic review. Eur J Cancer Prev. 2018; 27(3): 227–236. 10.1097/CEJ.0000000000000344 [DOI] [PubMed] [Google Scholar]
- 10.Issaka RB, Avila P, Whitaker E, Bent S, Somsouk M.. Population health interventions to improve colorectal cancer screening by fecal immunochemical tests: a systematic review. Prev Med. 2019; 118: 113–121. 10.1016/j.ypmed.2018.10.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Issaka RB, Somsouk M.. Colorectal cancer screening and prevention in the COVID-19 era. JAMA Health Forum. 2020; 1(5): e200588. 10.1001/jamahealthforum.2020.0588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cancino RS, Su Z, Mesa R, Tomlinson GE, Wang J.. The impact of COVID-19 on cancer screening: challenges and opportunities. JMIR Cancer. 2020; 6(2): e21697. 10.2196/21697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gupta S, Sussman DA, Doubeni CA, et al. Challenges and possible solutions to colorectal cancer screening for the underserved. J Natl Cancer Inst. 2014; 106(4): dju032. 10.1093/jnci/dju032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davis MM, Nambiar S, Mayorga ME, et al. Mailed FIT (fecal immunochemical test), navigation or patient reminders? Using microsimulation to inform selection of interventions to increase colorectal cancer screening in Medicaid enrollees. Prev Med. 2019; 129S: 105836. 10.1016/j.ypmed.2019.105836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Connor EA, Vollmer WM, Petrik AF, Green BB, Coronado GD.. Moderators of the effectiveness of an intervention to increase colorectal cancer screening through mailed fecal immunochemical test kits: results from a pragmatic randomized trial. Trials. 2020; 21(1): 91. 10.1186/s13063-019-4027-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castañeda SF, Bharti B, Espinoza-Giacinto RA, et al. Evaluating two evidence-based intervention strategies to promote CRC screening among Latino adults in a primary care setting. J Racial Ethn Health Disparities. 2018; 5(3): 530–535. 10.1007/s40615-017-0395-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petrik AF, Green B, Schneider J, et al. Factors influencing implementation of a colorectal cancer screening improvement program in community health centers: an applied use of configurational comparative methods. J Gen Intern Med. 2020; 35(Suppl 2): 815–822. 10.1007/s11606-020-06186-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gupta S, Coronado GD, Argenbright K, et al. Mailed fecal immunochemical test outreach for colorectal cancer screening: summary of a Centers for Disease Control and Prevention-sponsored summit. CA Cancer J Clin. 2020; 70(4): 283–298. 10.3322/caac.21615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davis MM, Schneider JL, Gunn R, Rivelli JS, Vaughn KA, Coronado GD.. A qualitative study of patient preferences for prompts and reminders for a direct-mail fecal testing program. Transl Behav Med. 2021; 11(2): 540–548. 10.1093/tbm/ibaa010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pham R, Cross S, Fernandez B, et al. “Finding the right FIT”: rural patient preferences for fecal immunochemical test (FIT) characteristics. J Am Board Fam Med. 2017; 30(5): 632–644. 10.3122/jabfm.2017.05.170151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Halm EA, Beaber EF, McLerran D, et al. Association between primary care visits and colorectal cancer screening outcomes in the era of population health outreach. J Gen Intern Med. 2016; 31(10): 1190–1197. 10.1007/s11606-016-3760-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis MM, Renfro S, Pham R, et al. Geographic and population-level disparities in colorectal cancer testing: a multilevel analysis of Medicaid and commercial claims data. Prev Med. 2017; 101: 44–52. 10.1016/j.ypmed.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mojica CM, Gunn R, Pham R, et al. An observational study of workflows to support fecal testing for colorectal cancer screening in primary care practices serving Medicaid enrollees. BMC Cancer. 2022;22(1):106. 10.1186/s12885-021-09106-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaiser Permanente Center for Health Research . Mailed FIT – resources to optimize colorectal cancer screening. Published 2021. Accessed Jan 14, 2022. https://research.kpchr.org/mailedfit
- 25.Thompson JH, Davis MM, Leo MC, et al. Participatory Research to Advance Colon Cancer Prevention (PROMPT): study protocol for a pragmatic trial. Contemp Clin Trials. 2018; 67: 11–15. 10.1016/j.cct.2018.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson JH, Davis MM, Michaels L, et al. Developing patient-refined messaging for a mailed colorectal cancer screening program in a Latino-based community health center. J Am Board Fam Med. 2019; 32(3): 307–317. 10.3122/jabfm.2019.03.180026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nilsen P, Bernhardsson S.. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019; 19(1): 189. 10.1186/s12913-019-4015-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Consolidated Framework for Implementation Research. Constructs. Published 2019. Accessed Jan 14, 2022. https://cfirguide.org/constructs/
- 29.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC.. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009; 4: 50. 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coronado GD, Retecki S, Petrik AF, et al. Mapping multi-site clinic workflows to design systems-enabled interventions. EGEMS (Wash DC). 2017; 5(1): 13. 10.5334/egems.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Health Resources & Services Administration . Uniform Data System (UDS) resources. Published 2020. Accessed Jan 14, 2022. https://bphc.hrsa.gov/datareporting/reporting/index.html
- 32.Coronado GD, Schneider JL, Green BB, et al. Health plan adaptations to a mailed outreach program for colorectal cancer screening among Medicaid and Medicare enrollees: the BeneFIT study. Implement Sci. 2020; 15(1): 77. 10.1186/s13012-020-01037-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coronado GD, Schneider JL, Petrik A, Rivelli J, Taplin S, Green BB.. Implementation successes and challenges in participating in a pragmatic study to improve colon cancer screening: perspectives of health center leaders. Transl Behav Med. 2017; 7(3): 557–566. 10.1007/s13142-016-0461-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Coronado GD, Schneider JL, Sanchez JJ, Petrik AF, Green B.. Reasons for nonresponse to a direct-mailed FIT kit program: lessons learned from a pragmatic colorectal-cancer screening study in a federally sponsored health center. Transl Behav Med. 2015; 5(1): 60–67. 10.1007/s13142-014-0276-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Centers for Medicare and Medicaid Services . Health Insurance Exchange. 2020 quality rating system measure technical specifications. Published Sep 2019. Accessed Jan 14, 2022. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/QualityInitiativesGenInfo/ACA-MQI/Downloads/2020-QRS-Measure-Tech-Specs.pdf
- 36.King N. Doing template analysis. In: Symon G, Cassell C, eds. Qualititative Organizational Research: Core Methods and Current Challenges. Sage Publications; 2012: 426–450. [Google Scholar]
- 37.Bernard HR, Wutch A, Ryan GW.. Analyzing Qualitative Data: Systematic Approaches. 2nd ed. Sage Publications Inc; 2017. [Google Scholar]
- 38.Lofland J, Snow DA, Anderson L, Lofland LH.. Analyzing Social Settings: A Guide to Qualitative Observation and Analysis. 4th ed. Wadsworth Publishing, Inc; 2005. [Google Scholar]
- 39.Baumgartner M. Parsimony and causality. Qual Quant. 2015; 49(2): 839–856. 10.1007/s11135-014-0026-7 [DOI] [Google Scholar]
- 40.Cragun D, Pal T, Vadaparampil ST, Baldwin J, Hampel H, DeBate RD.. Qualitative comparative analysis: a hybrid method for identifying factors associated with program effectiveness. J Mix Methods Res. 2016; 10(3): 251–272. 10.1177/1558689815572023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thiem A. Conducting configurational comparative research with qualitative comparative analysis: a hands-on tutorial for applied evaluation scholars and practitioners. Am J Eval. 2017; 38(3): 420–433. 10.1177/1098214016673902 [DOI] [Google Scholar]
- 42.Rohlfing I, Zuber CI.. Check your truth conditions! Clarifying the relationship between theories of causation and social science methods for causal inference. Sociol Methods Res. 2021; 50(4): 1623–1659. 10.1177/0049124119826156 [DOI] [Google Scholar]
- 43.Yakovchenko V, Miech EJ, Chinman MJ, et al. Strategy configurations directly linked to higher hepatitis C virus treatment starts: an applied use of configurational comparative methods. Med Care. 2020; 58(5): e31–e38. 10.1097/MLR.0000000000001319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hickman SE, Miech EJ, Stump TE, Fowler NR, Unroe KT.. Identifying the implementation conditions associated with positive outcomes in a successful nursing facility demonstration project. Gerontologist. 2020; 60(8): 1566–1574. 10.1093/geront/gnaa041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rogal SS, Yakovchenko V, Morgan T, et al. Getting to implementation: a protocol for a Hybrid III stepped wedge cluster randomized evaluation of using data-driven implementation strategies to improve cirrhosis care for veterans. Implement Sci. 2020; 15(1): 92. 10.1186/s13012-020-01050-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hudon C, Chouinard MC, Pluye P, et al. Characteristics of case management in primary care associated with positive outcomes for frequent users of health care: a systematic review. Ann Fam Med. 2019; 17(5): 448–458. 10.1370/afm.2419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Whitaker RG, Sperber N, Baumgartner M, et al. Coincidence analysis: a new method for causal inference in implementation science. Implement Sci. 2020; 15(1): 108. 10.1186/s13012-020-01070-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harris K, Kneale D, Lasserson TJ, McDonald VM, Grigg J, Thomas J.. School-based self-management interventions for asthma in children and adolescents: a mixed methods systematic review. Cochrane Database Syst Rev. 2019; 1(1): CD011651. 10.1002/14651858.CD011651.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cragun D. Configurational comparative methods. In: Nilsen P, Birken SA, eds. Handbook on Implementation Science. Edward Elgar Publishing; 2020: 497–504. [Google Scholar]
- 50.Baumgartner M, Falk C.. Boolean difference-making: a modern regularity theory of causation. Br J Philos Sci. 2019. 10.1093/bjps/axz047 [DOI] [Google Scholar]
- 51.Furnari S, Crilly D, Misangyi VF, Greckhamer T, Fiss PC, Aguilera R.. Capturing causal complexity: heuristics for configurational theorizing. Acad Manage Rev. 2021; 46(4): 778–799. 10.5465/amr.2019.0298 [DOI] [Google Scholar]
- 52.Rihoux B, Ragin CC.. Configurational Comparative Methods: QualitativeComparative Analysis (QCA) and Related Techniques. Sage Publications; 2008. [Google Scholar]
- 53.Palinkas LA, Mendon SJ, Hamilton AB.. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019; 40: 423–442. 10.1146/annurev-publhealth-040218-044215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Cohen DJ, Sweeney SM, Miller WL, et al. Improving smoking and blood pressure outcomes: the interplay between operational changes and local context. Ann Fam Med. 2021; 19(3): 240–248. 10.1370/afm.2668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ambuehl M, Baumgartner M, Epple R, Parkkinen VP, Thiem A.. CNA: causal modeling with Coincidence Analysis. R Package Version 3.0.0. Published 2020. Accessed Nov 1, 2020. https://cran.r-project.org/package=cna
- 56.Baumgartner M, Thiem A.. Model ambiguities in configurational comparative research. Sociol Methods Res. 2017; 46(4): 954–987. 10.1177/0049124115610351 [DOI] [Google Scholar]
- 57.Agency for Healthcare Research and Quality . About learning health systems. Published 2019. Accessed Sep 2, 2019. https://www.ahrq.gov/learning-health-systems/about.html
- 58.Stoto M, Oakes M, Stuart E, Savitz L, Priest EL, Zurovac J.. Analytical methods for a learning health system: 1. Framing the research question. EGEMS (Wash DC). 2017; 5(1): 28. 10.5334/egems.250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Levin T, Schottinger J, Ross M.. Reaching beyond delivery system walls to improve colorectal cancer screening. Health Affairs blog. March 24, 2017. Accessed Jan 15, 2022. https://www.healthaffairs.org/do/10.1377/hblog20170324.059313/full/
- 60.Mojica CM, Bradley SM, Lind BK, Gu Y, Coronado GD, Davis MM.. Initiation of colorectal cancer screening among Medicaid enrollees. Am J Prev Med. 2020; 58(2): 224–231. 10.1016/j.amepre.2019.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Davis MM, Gunn R, Pham R, et al. Key collaborative factors when Medicaid Accountable Care Organizations work with primary care clinics to improve colorectal cancer screening: relationships, data, and quality improvement infrastructure. Prev Chronic Dis. 2019; 16: E107. 10.5888/pcd16.180395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.DiPadova P, John Snow Inc. . Health provider mix and staffing ratios. Star2Center: Solutions Training and Assistance for Recruitment & Retention; Published Jun 2017. Accessed Jan 15, 2022. https://chcworkforce.org/sites/default/files/STAR2%20Center%20-%20Report%20-%20Staffing%20Mix%20and%20Ratios%20-%202017.pdf [Google Scholar]
- 63.Fowler T, Garr D, Mager NDP, Stanley J.. Enhancing primary care and preventive services through interprofessional practice and education. Isr J Health Policy Res. 2020; 9(1): 12. 10.1186/s13584-020-00371-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wagner EH, Flinter M, Hsu C, et al. Effective team-based primary care: observations from innovative practices. BMC Fam Pract. 2017; 18(1): 13. 10.1186/s12875-017-0590-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ruhe M, Gotler RS, Goodwin MA, Stange KC.. Physician and staff turnover in community primary care practice. J Ambul Care Manage. 2004; 27(3): 242–248. 10.1097/00004479-200407000-00008 [DOI] [PubMed] [Google Scholar]
- 66.Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K.. Burnout and health care workforce turnover. Ann Fam Med. 2019; 17(1): 36–41. 10.1370/afm.2338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Magnan S, Solberg LI, Giles K, Kottke TE, Wheeler JW.. Primary care, process improvement, and turmoil. J Ambul Care Manage. 1997; 20(4): 32–38. 10.1097/00004479-199710000-00006 [DOI] [PubMed] [Google Scholar]
- 68.Yue D, Pourat N, Chen X, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff (Millwood). 2019; 38(9): 1468–1474. 10.1377/hlthaff.2018.05228 [DOI] [PubMed] [Google Scholar]
- 69.Wranik WD, Price S, Haydt SM, et al. Implications of interprofessional primary care team characteristics for health services and patient health outcomes: a systematic review with narrative synthesis. Health Policy. 2019; 123(6): 550–563. 10.1016/j.healthpol.2019.03.015 [DOI] [PubMed] [Google Scholar]
- 70.Fraher EP, Cummings A, Neutze D.. The evolving role of medical assistants in primary care practice: divergent and concordant perspectives from MAs and family physicians. Med Care Res Rev. 2021; 78(1_suppl): 7S–17S. 10.1177/1077558720966148 [DOI] [PubMed] [Google Scholar]
- 71.Chapman SA, Marks A, Dower C.. Positioning medical assistants for a greater role in the era of health reform. Acad Med. 2015; 90(10): 1347–1352. 10.1097/ACM.0000000000000775 [DOI] [PubMed] [Google Scholar]
- 72.Litchfield I, Gale N, Burrows M, Greenfield S.. The future role of receptionists in primary care. Br J Gen Pract. 2017; 67(664): 523–524. 10.3399/bjgp17X693401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M.. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world? Int J Nurs Stud. 2015; 52(3): 727–743. 10.1016/j.ijnurstu.2014.11.014 [DOI] [PubMed] [Google Scholar]
- 74.George R, Gunn R, Wiggins N, et al. Early lessons and strategies from state-wide efforts to integrate community health workers into Medicaid. J Health Care Poor Underserved. 2020; 31(2): 845–858. 10.1353/hpu.2020.0064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jacobsen PB. Understanding and addressing clinical workflow to facilitation implementation. National Cancer Institute. Division of Cancer Control & Population Sciences. Published May 2019. Accessed Jun 3, 2019. https://cancercontrol.cancer.gov/IS/blog/2019/05-understanding-and-addressing-clinical-workflow-to-facilitate-implementation.html [Google Scholar]
- 76.O’Leary MC, Lich KH, Gu Y, et al. Colorectal cancer screening in newly insured Medicaid members: a review of concurrent federal and state policies. BMC Health Serv Res. 2019; 19(1): 298. 10.1186/s12913-019-4113-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Green BB, Anderson ML, Cook AJ, et al. A centralized program with stepped support increases adherence to colorectal cancer screening over 9 years: a randomized trial. J Gen Intern Med. 2021 May 28: 1–8. 10.1007/s11606-021-06922-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.The National Academies of Sciences, Engineering, and Medicine . Implementing high-quality primary care: rebuilding the foundation of health care. The National Academies Press; 2021. 10.17226/25983 [DOI] [PubMed] [Google Scholar]
- 79.Coury J, Miech EJ, Styer P, et al. What’s the “secret sauce”? How implementation variation affects the success of colorectal cancer screening outreach. Implement Sci Commun. 2021; 2(1): 5. 10.1186/s43058-020-00104-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.