Abstract
This randomized clinical trial assesses whether gamification with social incentives increases daily steps among adults with stroke.
The annual costs of stroke in the US have exceeded $30 billion and are largely attributed to poststroke morbidity.1 Regular physical activity after stroke is associated with reduced morbidity and helps prevent recurrent strokes, but some individuals remain inactive.2 Previous interventions were primarily delivered in clinics and lacked support to facilitate skill translation to homes.3 Remote, individualized interventions paired with behavioral economic principles are efficacious for increasing physical activity4,5 but are untested in patients with stroke. We assessed the effect of gamification with social incentives on daily steps among community-dwelling adults with stroke.
Methods
The protocol for this randomized clinical trial (NCT04607811) was approved by the University of Pennsylvania institutional review board (Supplement 1). Recruitment occurred from November 2020 to May 2021. Study details are reported elsewhere.6 This study followed the CONSORT reporting guideline; the CONSORT diagram and exclusion reasons are given in eFigures 1 and 2 in Supplement 2. Participants were adults who had a stroke 3 months or more before enrollment, were not receiving physical therapy, and did not have cognitive impairment.6 Participants provided informed consent online using a remote monitoring platform.4,5,6
Participants were randomized 1:1 to a control arm or a gamification with social incentives arm, received a wearable device worn on the unaffected wrist, and selected a step goal that was a 33%, 40%, or 50% increase from their baseline. The control arm received device feedback and no further intervention. The gamification arm engaged in an 8-week game with loss-framed points and levels to help achieve their step goal and received daily (text message) and weekly (email) feedback describing their progress. Participants selected a support partner who identified 3 goals and received weekly email updates on the participant’s progress.6
Consistent with previous work,4,5 data were considered missing if the participant did not record a step value or if total steps were fewer than 1000 per day (10.2% of data). We used multiple imputation for missing data, and model results were pooled using Rubin standard rules.
We assessed our primary outcome (change in daily steps from baseline) using a linear mixed-effects model adjusted for participant random effects, baseline steps, and calendar month. Our secondary outcome (difference in the proportion of days participants achieved their step goal) was examined using a generalized mixed-effects model adjusted for participant random effects and calendar month. We performed 1000 bootstrap samples. Analyses were conducted in R, version 3.6.1 using 2-sided hypothesis tests, with P < .05 indicating significance.
Results
A total of 34 participants were randomized (17 in each arm) and included in the analysis; 23 participants (67.6%) had an ischemic stroke, and the mean (SD) time since stroke was 27.7 (58.7) months (Table). Baseline steps were similar in the control (mean [SD], 4312 [1515]) and gamification (mean [SD], 4284 [1316]) arms.
Table. Demographics of Trial Participants With Stroke.
| Characteristic | Control arm (n = 17) | Gamification and social incentives arm (n = 17) |
|---|---|---|
| Age, mean (SD), y | 61 (16.9) | 57 (13.8) |
| Gender, No. (%) | ||
| Female | 11 (64.7) | 11 (64.7) |
| Male | 6 (35.3) | 6 (35.3) |
| Race and ethnicity, No. (%)a | ||
| Asian, non-Hispanic | 2 (11.8) | 1 (5.9) |
| Black or African American, non-Hispanic | 3 (17.6) | 2 (11.8) |
| White, non-Hispanic | 12 (70.6) | 14 (82.4) |
| Married, No. (%) | 11 (64.7) | 12 (70.6) |
| Household income>$50 000, No. (%) | 15 (88.2) | 12 (70.6) |
| Baseline measures | ||
| Stroke chronicity, mean (SD), mo | 39.2 (82.1) | 16.2 (9.2) |
| Ischemic stroke, No. (%) | 12 (70.6) | 11 (64.7) |
| Mini MoCA score, mean (SD)b | 12.5 (1.2) | 12.8 (1.2) |
| Body mass index, mean (SD)c | 30.9 (7.5) | 30.4 (6.7) |
| Charlson Comorbidity Index score, median (IQR) | 2 (0-4.5) | 1 (0-8.5) |
| Baseline steps, mean (SD), No. | 4312 (1515) | 4284 (1316) |
| PHQ-9 score, mean (SD)d | 3.7 (3.2) | 4.6 (3.9) |
| Stroke Self-efficacy Questionnaire score, mean (SD)e | 123 (9.7) | 120 (12.5) |
| Activities-Specific Balance Confidence Scale score, mean (SD), %f | 91.1 (7.8) | 83.1 (14.8) |
| FACIT Fatigue Scale score, mean (SD)g | 43.6 (6.2) | 40.8 (9.7) |
| MOS Social Support Survey score, mean (SD)h | 81.0 (20.9) | 77.6 (21.9) |
| Life-Space Mobility score, mean (SD)i | 75.3 (21.4) | 72.2 (25.7) |
Abbreviations: FACIT, Functional Assessment of Chronic Illness Therapy; MoCA, Mini Montreal Cognitive Assessment; MOS, Medical Outcomes Study; PHQ-9, Patient Health Questionnaire–9.
Race and ethnicity were self-reported and are reported because of the variability in stroke prevalence and outcomes by race and ethnicity.
Administered via telephone; scores range from 0 to 15, with scores of 11 or higher indicating no cognitive impairment.
Calculated as weight in kilograms divided by height in meters squared.
Scores range from 0 to 27, with higher scores indicating more severe depression.
Scores range from 0 to 130, with higher scores indicating greater self-efficacy.
Scores range from 0% to 100%, with scores greater than 80% indicating high levels of physical functioning.
Scores range from 0 to 52, with higher scores indicating greater quality of life.
Scores range from 0 to 100, with higher scores indicating greater social support.
Scores range from 0 to 120, with higher scores indicating greater mobility across different environments.
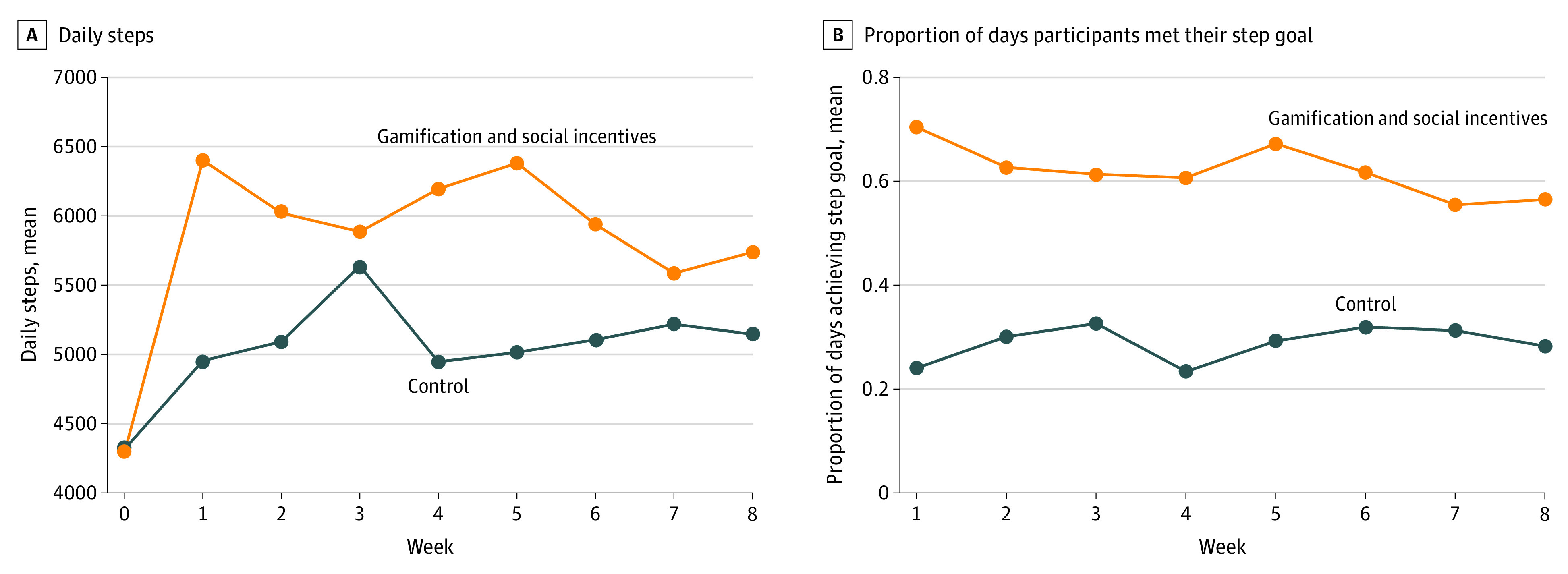
Unadjusted daily steps are presented in Figure, A. In adjusted analyses, the gamification arm had a significantly greater increase in mean daily steps from baseline (981 steps; 95% CI, 201-1762 steps; P = .01) compared with the control arm. The proportion of days participants met their step goal was significantly higher in the gamification arm (adjusted difference, 0.41; 95% CI, 0.38-0.43; P < .001); unadjusted mean proportions are presented in Figure, B.
Figure. Unadjusted Daily Steps and Proportion of Days Participants Met Their Step Goal by Study Week.
Discussion
In this trial, gamification with social incentives significantly increased daily steps among community-dwelling adults with stroke. To our knowledge, previous interventions required in-person visits, limiting access and scalability, and did not include behavioral economic principles. This trial eliminated in-person visits, incentivized individuals to increase activity at home, and did not rely on clinic to home skill translation.
Limitations include the sample size and lack of follow-up. These data may inform a future clinical trial with a larger sample of patients earlier after stroke and follow-up to evaluate long-term impact. Remote interventions that incorporate scalable technologies with behavioral economic principles may be critical for mitigating health care costs and improving long-term outcomes.
Trial Protocol
eFigure 1. Study CONSORT Diagram
eFigure 2. Reasons for Study Exclusion
Data Sharing Statement
References
- 1.Girotra T, Lekoubou A, Bishu KG, Ovbiagele B. A contemporary and comprehensive analysis of the costs of stroke in the United States. J Neurol Sci. 2020;410:116643. doi: 10.1016/j.jns.2019.116643 [DOI] [PubMed] [Google Scholar]
- 2.Liu C, Roth DL, Gottesman RF, et al. Change in life’s simple 7 measure of cardiovascular health after incident stroke: the REGARDS study. Stroke. 2021;52(3):878-886. doi: 10.1161/STROKEAHA.120.030836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dobkin BH. A rehabilitation-internet-of-things in the home to augment motor skills and exercise training. Neurorehabil Neural Repair. 2017;31(3):217-227. doi: 10.1177/1545968316680490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel MS, Small DS, Harrison JD, et al. Effectiveness of behaviorally designed gamification interventions with social incentives for increasing physical activity among overweight and obese adults across the United States: the STEP UP randomized clinical trial. JAMA Intern Med. 2019;179(12):1624-1632. doi: 10.1001/jamainternmed.2019.3505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agarwal AK, Waddell KJ, Small DS, et al. Effect of gamification with and without financial incentives to increase physical activity among veterans classified as having obesity or overweight: a randomized clinical trial. JAMA Netw Open. 2021;4(7):e2116256. doi: 10.1001/jamanetworkopen.2021.16256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waddell KJ, Patel MS, Clark K, Harrington TO, Greysen SR. Leveraging insights from behavioral economics to improve mobility for adults with stroke: design and rationale of the BE Mobile clinical trial. Contemp Clin Trials. 2021;107:106483. doi: 10.1016/j.cct.2021.106483 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eFigure 1. Study CONSORT Diagram
eFigure 2. Reasons for Study Exclusion
Data Sharing Statement


