Abstract
Background:
The Obsessive-Compulsive Inventory-Children’s Version (OCI-CV) was developed to assess obsessive-compulsive symptoms in youth. Recent changes in the Diagnostic and Statistical Manual (DSM-5) exclude hoarding from inclusion in the diagnosis of obsessive-compulsive disorder (OCD). Accordingly, the present study examined the reliability, validity, factorial structure, and diagnostic sensitivity of a revised version of the scale – the OCI-CV-R– that excludes items assessing hoarding.
Methods:
Participant were 1047 youth, including 489 meeting DSM criteria for primary OCD, 298 clinical controls, and 260 nonclinical controls, who completed the OCI-CV and measures of obsessive-compulsive symptom severity, depression, and anxiety at various treatment and research centers.
Results:
Findings support a five-factor structure (doubting/checking, obsessing, washing, ordering, and neutralizing), with a higher order factor. Factorial invariance was found for older (12 to 17 years) and younger (7 to 11 years) children. Internal consistency of the OCI-CV-R was acceptable, and discriminant and convergent validity were adequate and akin to that of its progenitor. Diagnostic sensitivity and specificity were found for a total score of 8 and higher.
Conclusion:
It is recommended that the OCI-CV-R replace the former version, and that this measure serve as part of a comprehensive clinical assessment of youth with OCD. Recommendations for further research with ethnically and racially diverse samples, as well as the need to establish benchmark scores are discussed.
Keywords: Obsessive compulsive disorder, youth, assessment, factor analysis, diagnostic sensitivity
1. Introduction
Obsessive-compulsive disorder (OCD) is a prevalent and chronic psychological condition marked by significant disability and high societal economic burden (Murray et al., 2004). The disorder is heterogeneous, marked by high variability in symptom expression as well as age of onset (Anholt et al., 2014). Although most adults with OCD can trace their symptoms to childhood, OCD is associated with a bimodal onset, with one peak at approximately 10 years old, and the second in early adulthood (Geller, 2006). Moreover, there is ample evidence that the presentation of pediatric OCD differs from that of adult OCD. For example, whereas in adults, higher rates have been observed among females (Fawcett et al., 2020), in childhood, OCD is associated with preponderance of males, as well as higher comorbidity with tic disorders, and lower insight (Geller, 2006; Lewin et al., 2006). Indeed, it has been suggested that childhood versus adult-onset OCD represent different subtypes of the disorder (Geller et al., 1998; Taylor, 2011), that may also differ in terms of brain morphology (Boedhoe et al., 2018). Thus, effective assessment tools are necessary for establishing symptom severity and the domain of symptom expression among youth.
Although there are several rating scales to assess OCD severity (for a review see Rapp et al., 2016), the Obsessive-Compulsive Inventory-Children’s Version (OCI-CV; Foa et al., 2010) is a well-established self-report measure of childhood obsessive-compulsive symptoms that is commonly used in research and practice. The scale is comprised of 21-items and roughly modeled on the adult version, the Obsessive-Compulsive Inventory-Revised (Foa et al., 2002). The OCI-CV assesses symptoms associated with doubting/checking, obsessing, washing, ordering, and hoarding, as well as neutralizing. It also has a factor analytically derived total score. Since the development of the OCI-CV, psychometric analyses have replicated the originally identified six-factor structure, as well as the adequate convergent validity with the Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS; Scahill et al., 1997), and moderate discriminant validity (e.g., Jones et al., 2013). Benchmarks have also been established that enhance the clinical utility of the measure in determining symptom severity and response to treatment (McGuire et al., 2019).
The OCI-CV, however, was developed when hoarding was considered a symptom of OCD. Yet substantial evidence indicates that hoarding is distinct from other symptoms of OCD (Pertusa et al., 2010), including in youth (Morris et al., 2016; Samuels et al., 2014), and thus it is now considered a separate condition (i.e., Hoarding Disorder) in the Diagnostic and Statistical Manual (DSM-5; American Psychiatric Association, 2013). Consistent with these developments, a recent network analysis with the OCI-CV revealed that of all the symptoms assessed by the scale, hoarding demonstrated the weakest connection to the other symptoms (Cervin et al., 2020). Further, in a study that evaluated the diagnostic sensitivity of the OCI-CV, the hoarding subscale was the least predictive of an OCD diagnosis (Rough et al., 2020), and some studies found no association between the OCI-CV hoarding subscale and the total CY-BOCS score (r=0.01; Jones et al., 2013).
When considering the psychometric properties and wide usage of the OCI-CV along with the aforementioned changes in the status of hoarding symptoms, the importance of evaluating a revision of the scale to maintain its syndromal validity becomes apparent. Moreover, given the broad range of age of onset in OCD, and studies showing differences in symptom presentation between younger and older youth with OCD, an examination of the OCI-CV factor structure in both age groups is warranted. This analysis was performed recently for the first time among Swedish speaking youth (Aspvall et al., 2020), but to our knowledge no such analysis has been conducted using the original English version. Accordingly, the present study had the following aims: First, to evaluate the reliability and factor structure of the OCI-CV without the items assessing hoarding (henceforth called the OCI-CV-Revised, OCI-CV-R). As part of this aim, factor invariance for the scale in younger (ages 7 - 11) and older (ages 12 to 17) children was evaluated. Second, we aimed to develop contemporary norms and a clinical diagnostic cutoff for the OCI-CV-R. Finally, we aimed to examine the convergent and discriminant validity of the OCI-CV-R with measures of depression and anxiety.
2. Methods
2.1. Participants
The study sample was comprised of 1047 youth, including 489 with a DSM-IV or DSM-5 primary OCD diagnosis, 298 clinical controls (CC), and 260 nonclinical controls (NCC). Data were collected internationally at several clinics, hospitals, and universities, including, the University of Michigan (n = 669), the University of South Florida (n = 133), the Massachusetts General Hospital (n = 107), Griffith University in Australia (n = 107), and the British Columbia Children’s Hospital (n = 31). Diagnosis was established through semi-structured diagnostic interviews, including the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997), the Anxiety Disorders Interview Schedule for DSM-IV, the Child/Parent Version (ADIS-IV; Silverman & Albano, 1996), and the Schedule for Obsessive-Compulsive and Other Behavioral Syndromes (SOCOBS; Hanna, 2007). The CC sample was comprised of youth with anxiety and developmental disorders, excluding OCD and autism spectrum disorder1. The entire study sample was primarily White (85.8%) and consisted of approximately the same proportion of girls (51.1%) and boys (48.9%). Ages ranged from 6 to 17 years old for the entire sample, with an average age of 12.79 (SD = 2.95) years. Table 1 displays the demographic information for each group of participants.
Table 1.
Demographic and clinical characteristics of the three samples
| OCD (n=489) |
CC (n=298) |
NCC (n=260) |
|
|---|---|---|---|
| Variable | Mean (SD); %(n) | ||
| Gender | |||
| Female | 52.2% (255) | 51.0% (152) | 49.2% (128) |
| Male | 47.9% (234) | 49.0% (146) | 50.8% (132) |
| Age (years) | 12.39 (2.92) | 13.01 (2.94) | 13.26 (2.93) |
| Ethnicity | |||
| Asian American | 3.1% (15) | 0.3% (1) | 0.0% (0) |
| Black American | 0.8% (4) | 0.7% (2) | 1.5% (4) |
| Hispanic American | 2.0% (10) | 5.2% (15) | 4.2% (11) |
| non-Hispanic White American | 83.0% (406) | 87.3% (260) | 89.2% (232) |
| Other/not identified | 11.1% (54) | 6.7% (20) | 5.1% (13) |
| OCD Severity | |||
| CY-BOCS Total Score | 22.76 (7.76) | - | - |
| CY-BOCS Obsessions | 10.92 (4.23) | - | - |
| CY-BOCS Compulsions | 11.84 (4.08) | - | - |
OCD: Obsessive-compulsive disorder; CC: Clinical controls; NCC: Non-clinical controls; CY-BOCS: Children’s Yale-Brown obsessive-compulsive scale.
2.2. Measures
2.2.1. Obsessive-Compulsive Inventory – Child Version (OCI-CV).
The OCI-CV (Foa et al., 2010) is a 21-item self-report measure of OCD symptoms in children and adolescents. Items (e.g., I think about bad things and can’t stop) are rated on their estimated frequency using a Likert scale from 0 (never) to 2 (always) and belong to six subscales: 1) washing, 2) hoarding, 3) doubting/checking, 4) ordering, 5) obsessing, and 6) neutralizing. The total score demonstrates good internal consistency across different populations and languages with Cronbach’s αs > .85 for the scale’s total score (Foa et al., 2010; Martinez-Gonzalez et al., 2015; Opakunle et al., 2018). In the current study, the OCI-CV displayed good internal consistency with Cronbach’s α of .86, .89 and .83 for the OCD, CC, and NCC samples, respectively.
2.2.2. Children’s Yale-Brown Obsessive-Compulsive Scale (CY-BOCS).
The CY-BOCS (Scahill et al., 1997) is a semi-structured interview that contains a 60-item checklist used to identify the respondent’s various types of obsessions (e.g., thoughts of harming a loved one) and compulsions (e.g., asking for reassurance). Next, a 10-item severity scale is used to assess the following parameters of the respondent’s most severe obsessions (items 1-5) and compulsions (items 6-10): time consumed with the symptom, associated distress, interference in functioning, resistance to the symptom, control over the symptom. Reponses on each item range from 0 (none) to 4 (severe), yielding a maximum score of 20 for each subscale (obsessions, compulsions) and 40 for the total score. The CY-BOCS possesses good to excellent psychometric properties including interrater reliability, test-retest reliability, and internal consistency (Cronbach’s α > .82; Scahill et al., 1997; Storch et al., 2019). The CY-BOCS demonstrated excellent reliability in the present study (α = .94).
2.2.3. Children’s Depression Inventory (CDI).
The CDI is a self-rated 27-item assessment of depression severity in children [28]. The instrument measures various components of depression including sadness, anhedonia, and disturbance in appetite and sleep. Items are rated on a 3-point Likert scale ranging from 0 (not at all) to 2 (definite), providing a total score range of 0 to 54. The CDI has demonstrated good psychometric properties (Saylor et al., 1984). A revised version (CDI-2; Kovacs & MHS, 2011) was administered to some of the present study’s participants. The CDI-2 has 28 items and is rated on the same Likert scale as the first version, providing a total score range of 0 to 56. The CDI-2 has two subscales that measure Emotional and Functional Problems. The CDI-2 has demonstrated good to excellent internal consistency in clinical and community populations (Bae, 2012). Both the CDI was administered to the OCD groups only. In the present study, the CDI-2 exhibited good internal consistency (Cronbach’s α = .87).
2.2.4. Multidimensional Anxiety Scale for Children (MASC).
The MASC (March et al., 1997) is a widely used 39-item self-report measure of anxiety that contains four main factors: Physical Symptoms, Social Anxiety, Separation Anxiety, and Harm Avoidance. Items are rated on a 4-point Likert scale ranging from 0 (never true about me) to 3 (often true about me). Previous research has demonstrated that the MASC possesses good internal consistency and discriminant validity in community and clinical samples (Baldwin & Dadds, 2007; March et al., 1997). The MASC was administered to the OCD group only and demonstrated excellent internal consistency in the current study (Cronbach’s α = .92).
2.3. Procedure
Participants were recruited either through an existing relationship with their respective hospital, university, or clinic, or via paid advertisements and flyers in their community. To determine their diagnosis, all participants were assessed using one of the aforementioned semi-structured diagnostic interviews. All diagnostic interviews were administered by a licensed psychologist or Master’s-level clinician and all diagnoses were confirmed by a licensed/registered psychologist or a child and adolescent psychiatrist with expertise in OCD. Two sites (University of Michigan and Griffith University) independently computed diagnostic agreement (Kappa) among 16% of their respective samples, and reported Kappas of 0.91, and 1.00 respectively. Although the other three sites did not calculate Kappa, diagnostic consensus was achieved for all clinical participants. Indeed, all data included in this investigation had been collected as part of large funded studies in which assessment and diagnostic procedures had been carefully conducted. All participants were administered the OCI-CV in addition to their diagnostic interview. Written parental consent and/or child assent was provided for all participants.
3. Results
3.1. Factor Structure
In the OCD sample, the average missing rate of the OCI-CV items was 3.4% (ranging from 2.9% to 4.3%). Little’s missing completely at random test (Little & Rubin, 2019) shows that the means of the OCI-CV items were different across missing data patterns. (χ2(df = 340) = 390.19, p = .03). This suggested that the variables are not missing completely at random. Accordingly, we used multiple imputation to handle the missing values of the OCI-CV items within the OCD sample for factor analyses and factorial invariance tests. Multiple imputation assumes data are missing at random, and that the observed variables in the data account for the missing values (Enders, 2010). We used Mplus 8.7 (Muthén & Muthén, 2017) to create 30 imputed datasets. The correlations between the missingness of these variables with CY-BOCS, CDI, MASC, gender, age, ethnicity were small (average = .07, ranging from .01 to .29). Because of the small correlations and model convergence difficulty, we decided not to add these variables to the imputation. We used the formulas by Little and Rubin (Little & Rubin, 2019) to pool the parameter estimates and their statistical inferences across imputed datasets.
We used Mplus 8.7 (Muthén & Muthén, 2017) for factor analyses using the OCD sample, and the weighted least squares means and variance adjusted (WLSMV) estimation to handle the ordinal (3-point scale) OCI-CV items (Rhemtulla et al., 2012). We conducted confirmatory factor analyses to determine model structure, excluding the hoarding items. We fitted the following models: (1) the correlated five-factor model where the corresponding items loaded on the doubting/checking, obsessing, washing, ordering, and neutralizing factors, and the five factors are correlated among each other; (2) the second-order factor model where the corresponding items loaded on the five factors, and the five factors loaded on the second-order factor; (3) the bifactor model where all the items loaded on a general factor and the items also loaded on the five specific factors correspondingly. To compare the fit of these models, we considered the following parameters: the root mean square error of approximation (RMSEA) and comparative fit index (CFI). We used the following suggested cutoffs for satisfactory model fit: RMSEA < .08; CFI > .95 (Browne & Cudeck, 1993; Hu & Bentler, 1999).
After selecting the factor model, we tested the factorial invariance between the younger (ages 7 - 11) and older participants (ages 12 to 17) with OCD. We tested three invariance models in sequence: configural invariance, metric invariance, and scalar invariance. Configural invariance model means that the two age groups has the same factor model (e.g., correlated factor model) but the factor loadings and item thresholds are all freely estimated in the two groups. Metric invariance model is nested within the configural invariance model, and all the factor loadings are constrained to be equal between the age groups. Scalar invariance model is nested with the metric invariance model, and all the factor loadings and item thresholds are constrained to be equal between the age groups. We evaluated the three models using the small reduction of RMSEA (ΔRMSEA < .015) and CFI (ΔCFI > −.010) between consecutive nesting models supports the more restrictive model. Based on Chen (2007), ΔCFI < −.01 or ΔRMSEA < .015 from configural to metric invariance supports metric invariance. ΔCFI < −.01 or ΔRMSEA < .015 from metric to scalar invariance supports scalar invariance. Metric invariance indicates that one can compare the factor variances and covariances between groups. Scalar invariance indicates that one can compare the factor mean, variances, and covariances between groups2.
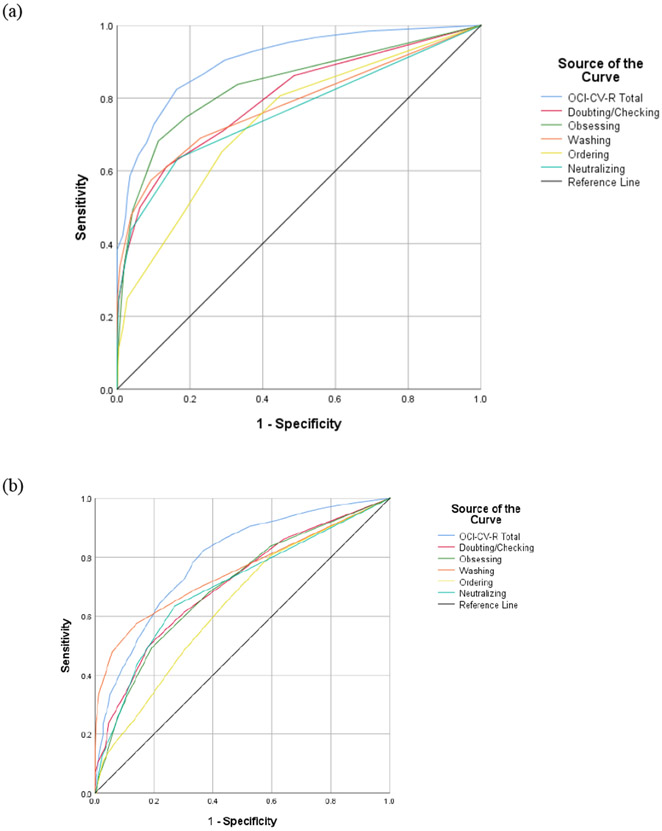
The correlated five-factor model had RMSEA = .078 and CFI = .966, the second-order factor model had RMSEA = .071 and CFI = .971, and the bifactor model had RMSEA = .042 and CFI = .991. Figures 1, 2, and 3 depict these models along with standardized factor loadings and factor correlations of the correlated five-factor, second-order factor, and bifactor models. In the correlated five-factor model, all items loaded on the corresponding factors with standardized factor loadings > .6. In the second-order factor model, the washing factor had low standardized factor loading on the second-order factor (.36) because of the low correlations between this factor and other factors (rs < .32). In the bifactor model, some items had low standardized factor loadings on the general factor or corresponding specific factors (< .3). We selected the correlated five-factor model because it had satisfactory global model fit and reasonable standardized factor loadings and factor correlations.
Figure 1.
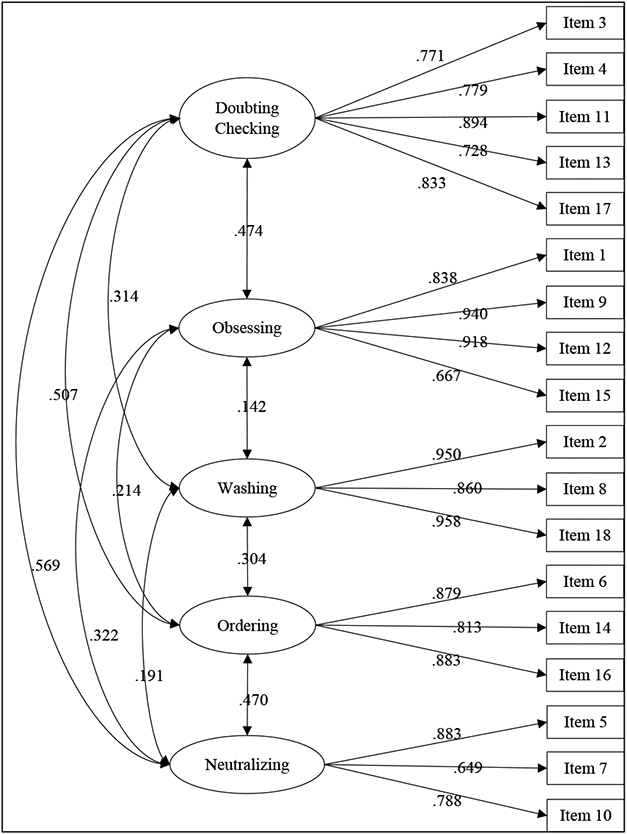
Standardized factor loadings and factor correlations of the correlated five-factor model of the entire sample (N = 489).
Figure 2.
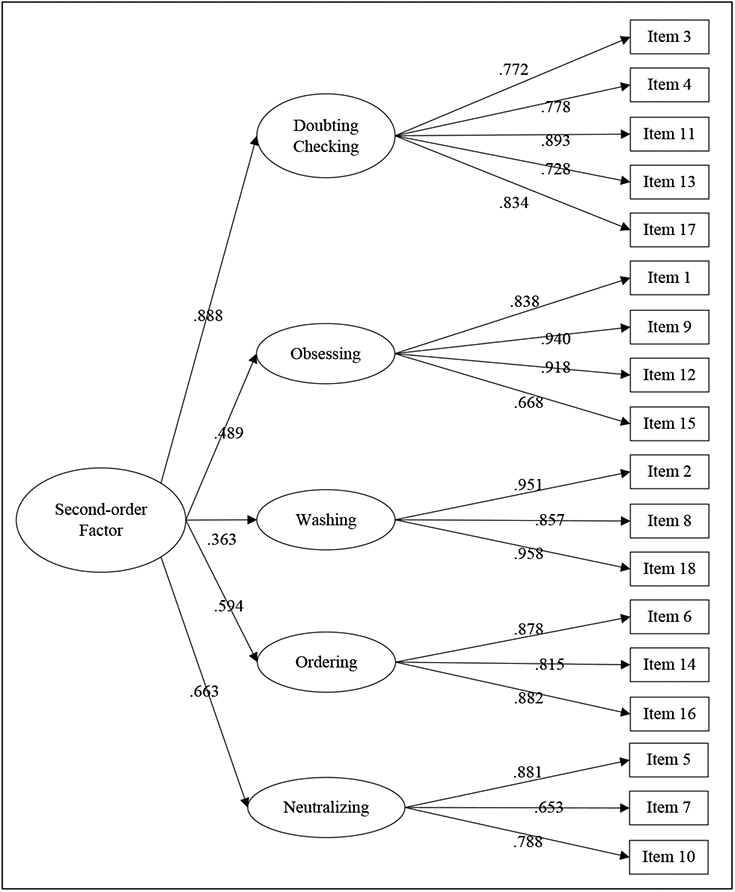
Standardized factor loadings of the second-order factor model of the entire sample (N = 489).
Figure 3.
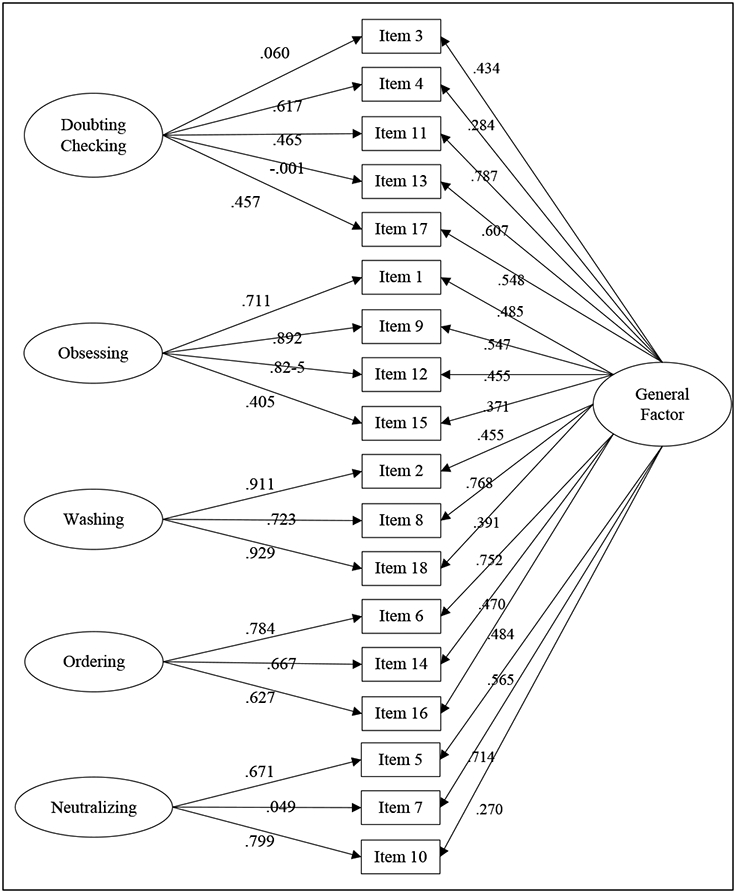
Standardized factor loadings of the bifactor model of the entire sample (N = 489).
Within our OCD sample, 186 participants (39.2%; 52.7% female) fell between the ages of 7 and 11 years (younger group) and 288 (60.7%; 51.4% female) between the ages of 12 and 17 (older group), with mean ages of 9.4 (SD = 1.3) and 14.2 (SD = 1.6), respectively. Comparisons between the two age groups on OCI-CV-R scores (Table 2) indicated significantly higher scores among the older group on the total score and all subscale scores, with small to medium effect sizes. Based on findings that the presentation of OCD can differ between younger and older youth with the disorder (e.g., Tanidir et al., 2015), we tested the factorial invariance of the correlated five-factor model between the two age groups (Table 3). The configural invariance model had satisfactory model fit, with ΔRMSEA = .069 and CFI = .973. The metric invariance model fit the data as well as the configural invariance model, with ΔRMSEA = −.002 and ΔCFI = .000. The scalar invariance model fit the data as well as the metric invariance model, with ΔRMSEA = −.003 and ΔCFI = .001. We concluded that scalar invariance was established between the two age groups. Notably, in order to identify potential local misspecifications we calculated the configural invariance model to provide the factor loadings and thresholds of the younger and older OCD subgroups. While there were no standardized effect size measures for the difference between the factor loadings and thresholds, a read of the understood results concluded no outstanding local misspecifications (constraints) of the factor loading and thresholds in the selected scalar invariance model.
Table 2.
OCI-CV-R scores across age groups
| OCI-CV-R scores | Ages< 12 |
Ages≥ 12 |
t | p | Cohen’s d |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| Total Score | 11.27 (6.03) | 15.01 (7.30) | 5.76 | < .001 | 0.55 |
| Doubting/Checking | 2.90 (2.21) | 4.04 (2.92) | 4.48 | < .001 | 0.43 |
| Obsessing | 3.05 (2.17) | 3.84 (2.45) | 3.50 | .001 | 0.33 |
| Washing | 2.05 (2.10) | 2.77 (2.24) | 3.46 | .001 | 0.33 |
| Ordering | 2.19 (1.81) | 2.64 (1.88) | 2.51 | .01 | 0.24 |
| Neutralizing | 1.07 (1.28) | 1.73 (1.64) | 4.57 | < .001 | 0.44 |
OCI-CV-R; obsessive-compulsive inventory – child version – revised; M: Mean; SD: Standard deviation; Cohen’s d: Effect size
Table 3.
Correlations between the OCI-CV-R, OCI-CV, and symptom measures among youth with OCD (N = 489)
| Invariance Model |
χ 2 | df | RMSEA | CFI | Comparison Model | ΔRMSEA | ΔCFI |
|---|---|---|---|---|---|---|---|
| Configural | 521.189 | 250 | .069 | .973 | |||
| Metric | 534.660 | 263 | .067 | .973 | Metric - Configural | −.002 | .000 |
| Scalar | 536.702 | 276 | .064 | .974 | Scalar - Metric | −.003 | .001 |
df: degrees of freedom; RMSEA: Root mean square error of approximation; CFI: Comparative fit index; ΔRMSEA: Change of RMSEA; ΔCFI: Change of CFI.
Given the support of scalar invariance, we compared the factor mean differences between the two age groups (older – younger). Results were consistent with those in Table 2. The older group had significantly higher scores on doubting/checking (Cohen’s d = .43. p = .007), obsessing (Cohen’s d = .34, p = .001), washing (Cohen’s d = 35, p = .001), ordering (Cohen’s d = .28, p = .004), and neutralizing (Cohen’s d = .50, p .001) than the younger group.
3.2. Internal Consistency
Internal consistency was calculated for each of the samples (OCD, CC, and NCC) using Cronbach’s alpha (α). The OCI-CV-R total score demonstrated good internal consistency: OCD (α = .86), CC (α = .88), and NCC (α = .83). Apart from neutralizing (α = .68), the subscales also showed good internal consistency: doubting/checking = .84, obsessing = .87, washing = .89, and ordering = .85.
3.3. Convergent and Discriminant Validity
To assess convergent and discriminant validity of the OCI-CV-R total score, correlations were computed between the OCI-CV, OCI-CV-R, and other measures for participants in the OCD group. As can be seen in Table 4, the correlation between the OCI-CV-R total score and the CY-BOCS total score, our measure of convergent validity, fell within the moderate range. Likewise, correlations between the OCI-CV-R total score and the MASC and CDI-2 fell within the moderate range. As is also shown in Table 4, these coefficients were similar to those found for the OCI-CV.
Table 4.
Correlations between the OCI-CV-R, OCI-CV, and symptom measures among youth with OCD
| Measure | n | OCI-CV | OCI-CV-R |
|---|---|---|---|
| OCD symptoms | |||
| CY-BOCS total score | 446 | .30** | .32** |
| Other symptoms | |||
| MASC Total | 208 | .50** | .48** |
| CDI-1 | 102 | .32** | .35** |
| CDI-2 | 128 | .51** | .49** |
OCD: Obsessive-compulsive disorder; OCI-CV: The obsessive-compulsive inventory – child version; OCI-CV-R: Obsessive-compulsive inventory – child version – revised; CY-BOCS: Children’s Yale-Brown obsessive-compulsive scale; MASC: Multidimensional Anxiety Scale for Children; CDI: Children’s Depression Inventory
= p < .05
= p < .001.
3.4. Norms
Norms for the 18-item OCI-CV-R total score and subscale scores are presented in Table 5. A univariate analysis of variance (ANOVA) identified a significant main effect of group on the total score, F(2, 995) = 280.28, p < .001, partial η2 = .36. Games-Howell post hoc contrasts revealed that the OCD group had a significantly greater total mean score than the CC group (p < .001), whose mean score was in turn greater than the NCC group (p < .001). A multivariate analysis of variance (MANOVA) across OCI-CV-R subscales revealed a significant difference between groups, Wilk’s Λ = .59, F(10, 1982) = 60.87, p < .001, partial η2 = .24. Further univariate analyses revealed a significant main effect for all OCI-CV-R subscales (all ps < .001). Planned contrasts (Games-Howell) revealed that the OCD group scores were significantly greater than the CC and NCC groups on all subscales (all ps < .001). The CC group also had significantly greater scores than the NCC group on all subscales (all ps < .05).
Table 5.
Norms for the OCI-CV-R total and subscale scores across clinical and non-clinical samples
| OCI-CV-R Scores |
OCD |
CC |
NCC |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mdn | IQR | Mean | SD | Mdn | IQR | Mean | SD | Mdn | IQR | |
| Total Score | 13.62 | 7.19 | 13 | 11 | 6.29 | 5.59 | 5 | 8 | 3.27 | 3.64 | 2 | 5 |
| Doubting/Checking | 3.63 | 2.73 | 3 | 4 | 1.78 | 1.94 | 1 | 3 | 1.00 | 1.32 | 0 | 2 |
| Obsessing | 3.54 | 2.36 | 3 | 3 | 1.88 | 2.05 | 1 | 3 | 0.71 | 1.27 | 0 | 1 |
| Washing | 2.51 | 2.23 | 2 | 4.25 | 0.56 | 0.93 | 0 | 1 | 0.37 | 0.79 | 0 | 0 |
| Ordering | 2.48 | 1.88 | 2 | 2.50 | 1.60 | 1.76 | 1 | 3 | 0.96 | 1.29 | 0 | 2 |
| Neutralizing | 1.49 | 1.54 | 1 | 2 | 0.52 | 1.06 | 0 | 1 | 0.21 | 0.51 | 0 | 0 |
OCI-CV-R: Obsessive-compulsive inventory – child version - revised; OCD: Obsessive-compulsive disorder; CC: Clinical controls; NCC: Non-clinical controls; SD: Standard deviation; Mdn: Median; IQR = Inter-quartile range.
3.5. Diagnostic Sensitivity
We examined the OCI-CV-R’s potential as a diagnostic tool in two steps. First, we conducted receiver operating characteristic (ROC) analyses, which uses the association between sensitivity and specificity to estimate the area under the curve (AUC) to indicate how well scores on a measure distinguish between positive (i.e., a diagnosis of OCD) and negative (i.e., nonclinical control [NC] or clinical controls diagnosed with other psychiatric disorders [CC]) cases. Next, we established cutoff scores with optimal diagnostic accuracy for distinguishing between individuals with OCD and those in the NC and CC groups. Classification properties (e.g., sensitivity and specify for the entire range of scores can be found in the manuscript supplementary materials.
3.6. Diagnostic accuracy of OCI-CV-R total and subscale scores
We conducted ROC analyses for the OCI-CV-R total and subscale scores to determine which best distinguished individuals with OCD from (a) the NC group and (b) the CC group. An AUC value of 1.0 indicates perfect diagnostic prediction, whereas a value of .50 indicates the level of chance. In distinguishing the OCD group from the NC group, AUC estimates for the five OCI-CV-R subscales ranged from .74 (ordering) to .84 (obsessing) (see Figure 4A). The total score, however, evidenced the highest AUC (.90, 95% confidence interval [CI] = .87 to .92). In distinguishing individuals with OCD from the CC group, AUC estimates for the five subscales ranged from .64 (ordering) to .75 (washing) (see Figure 4B). Again, however, the OCI-CV total score evidenced the highest AUC (.79, 95% CI = [.76, .83]). These data indicate that the OCI-CV-R total score discriminates children with OCD extremely well from children without psychiatric diagnoses, and quite well from those with other psychiatric disorders. Accordingly, we used total scores in the analyses that follow.
Fig. 4.
Receiver operating characteristics (ROC) curves for the (a) OCD-NCC samples and (b) OCD-CC, samples. (OCD: obsessive-compulsive disorder; NCC: nonclinical sample; CC: clinical control sample).
3.7. Diagnostically accurate cutoff scores
Next, we examined the accuracy of different OCI-CV-R cutoff scores in correctly classifying children as having a primary diagnosis of OCD versus belonging to the NC group. Diagnostic accuracy was evaluated by calculating the sensitivity and specificity of OCI-CV-R total scores. A cutoff score of 6 or higher provided the best balance between sensitivity and specificity, correctly classifying about 86% of OCD patients (sensitivity) and 76% of NC participants (specificity), with an overall classification accuracy of 83%. Notably, since positive and negative predictive values are heavily influenced by condition’s base rate in the study sample, we computed positive and negative likelihood ratios (PLR, NLR). These calculations yielded a PLR=3.69 (CI, 2.95-4.62), and NLR=0.18 (CI, 0.14-0.23). Furthermore, these analyses yielded a Diagnostic Odds Ratio = 20.8, that translates to the odds of the OCI-CV-R screening positive in participants with OCD compared to the odds of the tool screening positive in individuals without OCD. Thus, individuals who score above the cutoff are nearly 20 times more likely to meet diagnostic criteria for OCD. Similar analyses revealed that a cutoff score of 8 or higher provided the best balance between sensitivity and specificity in classifying OCD patients versus CC patients, correctly classifying about 73% (sensitivity) of OCD patients and 70% of CC patients (specificity). These calculations yielded a PLR=2.34 (CI, 1.98-2.77), and NLR=0.33 (CI, 0.27-0.39). These analyses yielded a Diagnostic Odds Ratio = 7.2.
4. Discussion
The OCI-CV is a widely used self-report measures of OCD symptoms in youth. Yet since the development of the measure, there have been significant changes in our understanding of the relationship between hoarding symptoms and OCD that have resulted in hoarding becoming its own separate (but related) disorder in DSM-5 (Pertusa et al., 2010). As a result, the inclusion of hoarding items in measures of OCD may lead to erroneous assessments of severity. Further, recent research has shown that the hoarding subscale had the weakest association with the other symptoms assessed on the OCI-CV (Cervin et al., 2020). One aim of the present study, therefore, was to examine the psychometric properties of the OCI-CV without the items assessing hoarding. Additionally, given the differences in clinical presentation between older and younger children with OCD (Tanidir et al., 2015), we also examined the factorial invariance of the factor structure between these age groups. The results show that the five-factor model for the revised version of the OCI-CV (termed the OCI-CV-R) has good fit, with factorial invariance observed for younger and older age groups. A factor model with a higher-order total score was also observed. This suggests that the OCI-CV-R can be used to reliably assess symptom dimension of the condition in children, and the total score is a reliable estimate of total symptom severity.
Our analyses of internal consistency suggest that the OCI-CV-R demonstrates good reliability that is similar to its adult counterpart measure, the OCI-12 (Abramovitch et al., 2021b). Yet our convergent and discriminant validity findings deserve more in-depth comment. Specifically, the OCI-CV-R was only moderately associated with scores on the CY-BOCS. Although this might be taken to indicate poor convergent validity, such a result is not surprising given that these two instruments assess OCD in different ways. Indeed, scores on the CY-BOCS reflect global OCD severity since respondents first identify their primary obsessions and compulsions (using the symptom checklist) before rating these symptoms on the five severity parameters. Thus, the CY-BOCS is an idiographic measure that assesses severity independent of symptom presentation. The OCI-CV-R, however, is a nomothetic measure, that confounds severity with the presentation of symptoms since it contains items tapping into only the most quintessential of obsessions and compulsions and assesses only the frequency of these symptoms. To illustrate, consider a child (Child A) with frequent, yet mild doubting/checking, washing, and ordering symptoms and another (Child B) with less frequent, yet highly distressing and impairing washing symptoms only. Here, Child A would likely have a higher OCI-CV-R total score than Child B, whereas the reverse would be true of their CY-BOCS scores. Thus, similar to the OCI-CV, it is not surprising that the relation between the OCI-CV-R and the CY-BOCS was not stronger and highlights the importance of a multi-modal assessment approach in determining overall clinical severity among youth with OCD. Meanwhile, moderate correlations indicated that the OCI-CV-R possesses good discriminant validity.
We also evaluated the diagnostic accuracy of the OCI-CV-R. The subscales all showed good diagnostic accuracy from ROC analyses, although the total score was most sensitive; scores of 6 and 8 emerged as the most accurate cutoff scores between individuals with OCD and those with no confirmed diagnosis and with other psychological disorders, respectively. Moreover, our findings are consistent with the specificity and sensitivity observed in Rough et al. (2020). It must be stressed, however, that the identification of a cutoff score that corresponds to a high likelihood of a respondent meeting criteria for OCD should not lead to the OCI-CV-R being used as a stand-alone diagnostic instrument. Considering the complexity of OCD, a full diagnostic assessment would remain warranted, and the OCI-CV-R should be viewed as one tool in the set of clinical methods for establishing a diagnosis.
While the findings from this study are encouraging in establishing the utility of the OCI-CV-R in clinical settings, a limitation of the present study is that the sample overwhelmingly included White participants. Accordingly, when assessing members of other ethnic and racial groups, caution must be exercised in drawing conclusions regarding diagnostic classification and interpretation of clinical severity. While recent research suggests youth with OCD may present similarly across ethnic groups (Fernández de la Cruz et al., 2015; Wang et al., 2021), there remains a dearth of research on how OCD manifests in children from a wide range of ethnic backgrounds. In addition, different diagnostic measures and methods were used to diagnose different participants across the samples. However, all methods were DSM-based and in all cases a diagnostic consensus has been achieved.
5. Conclusions
The results of this study indicate that the OCI-CV-R has a robust five-factor structure (doubting/checking, obsessing, washing, ordering, and neutralizing) and second order factor. The original OCI-CV has several strengths as well as weaknesses but given the shift in the diagnostic standards that removed hoarding from the diagnosis of OCD, the OCI-CV-R should replace the original OCI-CV. Notably, after removing the hoarding items, the OCI-CV-R largely retains the psychometric properties of the OCI-CV. In addition, its factor structure is consistent for older and younger children and sensitive and specific cutoff scores that accurately predict the age group membership are available. Additional research remains necessary with youth with OCD from a wide range of ethnic and racial backgrounds to further refine the utility of the OCI-CV-R. Further, research into clinical benchmarks is warranted with the OCI-CV-R, consistent with recent research on the modified adult versions of the scale (Abramovitch et al., 2021a, 2021b). Finally, there a need for diagnostically sensitive brief screening measures for pediatric OCD. The complete scale including instructions (derived from the original OCI-CV; Foa et al., 2010), new item numbering, and scoring guidelines can be found in the Appendix.
Supplementary Material
Highlights.
The OCI-CV is a common measure of obsessive-compulsive symptom severity in youth.
The OCI-CV assesses hoarding, which is no longer considered a symptom of OCD.
We used large clinical and control samples to revise the OCI-CV to exclude hoarding.
The OCI-CV-R, demonstrates comparable psychometric properties to the OCI-CV.
The full OCI-CV-R, as well as norms and a clinical cutoff are provided.
Acknowledgments:
This work was supported by National Institute of Mental Health (NIMH) grants 1R01MH093381 (EAS, DAG, SW), R01MH093381-02S1 (EAS, JFM), R01MH101493 (GLH), and R01MH08321 (GLH, DRR). Note: Following the first five authors, order of authorship was determined alphabetically.
Appendix
| OCI-CV-R | |||
|---|---|---|---|
| On this page there are several questions that we want you to answer. Read each sentence carefully and tell us how much it has happened to you in the last month. If it never happens to you, circle the word “never.” If it sometimes happens to you, circle the word “sometimes.” If it happens to you almost always, circle the word “always.” This is not a test, so there are no right and wrong answers. | |||
| Example: I think a lot about dogs. | never | sometimes | always |
| 1. I think about bad things and can't stop. | never | sometimes | always |
| 2. I feel like I must wash and clean over and over again. | never | sometimes | always |
| 3. I check many things over and over again. | never | sometimes | always |
| 4. After I have done things, I'm not sure if I really did them. | never | sometimes | always |
| 5. I need to count while I do things. | never | sometimes | always |
| 6. I get upset if my stuff is not in the right order. | never | sometimes | always |
| 7. I get behind in my schoolwork because I repeat things over and over again. | never | sometimes | always |
| 8. I worry a lot about things being clean. | never | sometimes | always |
| 9. I'm upset by bad thoughts. | never | sometimes | always |
| 10. I have to say some numbers over and over. | never | sometimes | always |
| 11. Even after I'm done, I still worry that I didn't finish things. | never | sometimes | always |
| 12. I get upset by bad thoughts that pop into my head when I don't want them to. | never | sometimes | always |
| 13. I check doors, windows, and drawers over and over again. | never | sometimes | always |
| 14. I get upset if people change the way I arrange things. | never | sometimes | always |
| 15. If a bad thought comes into my head, I need to say certain things over and over. | never | sometimes | always |
| 16. I need things to be in a certain way. | never | sometimes | always |
| 17. Even when I do something very carefully, I don't think I did it right. | never | sometimes | always |
| 18. I wash my hands more than other kids. | never | sometimes | always |
The Obsessive-Compulsive Inventory Child Version – Revised (OCI-CV-R)
Administration & Scoring
The OCI-CV-R is a self-report measure of OCD symptoms in youth. It consists of 18 items that a child endorses on a 3-point Likert scale (never=0, sometimes=1, always=2). Scores are generated by adding the item scores. The possible range of scores is 0-36.
Checking/Doubting: 3, 4, 11, 13, 17
Obsessing: 1, 9, 12, 15
Washing: 2, 8, 18
Ordering: 6, 14, 16
Neutralizing: 5, 7, 10
Clinical cutoff score:
The mean total score for youth with OCD is 13.62 (SD=7.19). The total mean score for youth with OCD that are younger than 12 years is 11.41 (SD = 6.33), and among youth 12 years or older is 15.08 (SD=7.37).
Recommended total cutoff score is 6, with scores at or above this level indicating the likely presence of OCD.
Reference: Abramovitch, A., Abramowitz, J.S., McKay, D., Cham, H., Anderson, K.S., Farrell, L., Geller, D.A., Hanna, G.L., Mathieu, S., McGuire, J.F., Rosenberg, D.R., Stewart, S.E., Storch, E.A., Wilhelm, S.(2021) A Revision of the Obsessive-Compulsive Inventory - Child Version: The OCI-CV-R. Journal of Anxiety Disorders.
Footnotes
We did not attempt to determine the principal diagnosis for two reasons. First, assigning a primary diagnosis relative to other co-occurring diagnoses is often subjective. Second, the CC group is meant to serve as a heterogeneous clinical reference group, and information regarding the primary disorder of each participant does not affect the results of the present psychometric investigation.
To date, there is no suggestion how to pool the likelihood ratio tests of the WLSMV estimation in multiple imputation. We decided not calculating the likelihood ratio tests between configural, metric, and scalar invariance models.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abramovitch A, Abramowitz JS, & McKay D (2021a). The OCI-4: An ultra-brief screening scale for obsessive-compulsive disorder. Journal of Anxiety Disorders, 78, 102354. 10.1016/j.janxdis.2021.102354 [DOI] [PubMed] [Google Scholar]
- Abramovitch A, Abramowitz JS, & McKay D (2021b). The OCI-12: A syndromally valid modification of the obsessive-compulsive inventory-revised. Psychiatry Research, 298, 113808. 10.1016/j.psychres.2021.113808 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders : DSM-5. American Psychiatric Association. [Google Scholar]
- Anholt GE, Aderka IM, van Balkom AJ, Smit JH, Schruers K, van der Wee NJ, Eikelenboom M, De Luca V, & van Oppen P (2014). Age of onset in obsessive-compulsive disorder: admixture analysis with a large sample. Psychol Med, 44(1), 185–194. 10.1017/s0033291713000470 [DOI] [PubMed] [Google Scholar]
- Aspvall K, Cervin M, Andrén P, Perrin S, Mataix-Cols D, & Andersson E (2020). Validity and clinical utility of the obsessive compulsive inventory - child version: further evaluation in clinical samples. BMC Psychiatry, 20(1), 42. 10.1186/s12888-020-2450-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae Y (2012). Test Review: Children’s Depression Inventory 2 (CDI 2). Journal of Psychoeducational Assessment, 30(3), 304–308. 10.1177/0734282911426407 [DOI] [Google Scholar]
- Baldwin JS, & Dadds MR (2007). Reliability and validity of parent and child versions of the multidimensional anxiety scale for children in community samples. J Am Acad Child Adolesc Psychiatry, 46(2), 252–260. 10.1097/01.chi.0000246065.93200.a1 [DOI] [PubMed] [Google Scholar]
- Boedhoe PSW, Schmaal L, Abe Y, Alonso P, Ameis SH, Anticevic A, Arnold PD, Batistuzzo MC, Benedetti F, Beucke JC, Bollettini I, Bose A, Brem S, Calvo A, Calvo R, Cheng Y, Cho KIK, Ciullo V, Dallaspezia S, Denys D, Feusner JD, Fitzgerald KD, Fouche JP, Fridgeirsson EA, Gruner P, Hanna GL, Hibar DP, Hoexter MQ, Hu H, Huyser C, Jahanshad N, James A, Kathmann N, Kaufmann C, Koch K, Kwon JS, Lazaro L, Lochner C, Marsh R, Martínez-Zalacaín I, Mataix-Cols D, Menchón JM, Minuzzi L, Morer A, Nakamae T, Nakao T, Narayanaswamy JC, Nishida S, Nurmi E, O'Neill J, Piacentini J, Piras F, Piras F, Reddy YCJ, Reess TJ, Sakai Y, Sato JR, Simpson HB, Soreni N, Soriano-Mas C, Spalletta G, Stevens MC, Szeszko PR, Tolin DF, van Wingen GA, Venkatasubramanian G, Walitza S, Wang Z, Yun JY, Thompson PM, Stein DJ, & van den Heuvel OA (2018). Cortical Abnormalities Associated With Pediatric and Adult Obsessive-Compulsive Disorder: Findings From the ENIGMA Obsessive-Compulsive Disorder Working Group. Am J Psychiatry, 175(5), 453–462. 10.1176/appi.ajp.2017.17050485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit. In Testing structural equation models (pp. 136–162). Sage. [Google Scholar]
- Cervin M, Perrin S, Olsson E, Aspvall K, Geller DA, Wilhelm S, McGuire J, Lázaro L, Martínez-González AE, Barcaccia B, Pozza A, Goodman WK, Murphy TK, Seçer İ, Piqueras JA, Rodríguez-Jiménez T, Godoy A, Rosa-Alcázar AI, Rosa-Alcázar Á, Ruiz-García BM, Storch EA, & Mataix-Cols D (2020). The Centrality of Doubting and Checking in the Network Structure of Obsessive-Compulsive Symptom Dimensions in Youth. J Am Acad Child Adolesc Psychiatry, 59(7), 880–889. 10.1016/j.jaac.2019.06.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FF (2007). Sensitivity of Goodness of Fit Indexes to Lack of Measurement Invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. 10.1080/10705510701301834 [DOI] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. Guilford press. [Google Scholar]
- Fawcett EJ, Power H, & Fawcett JM (2020). Women Are at Greater Risk of OCD Than Men: A Meta-Analytic Review of OCD Prevalence Worldwide. J Clin Psychiatry, 81(4). 10.4088/JCP.19r13085 [DOI] [PubMed] [Google Scholar]
- Fernández de la Cruz L, Jassi A, Krebs G, Clark B, & Mataix-Cols D (2015). Phenomenology and treatment outcomes in children and adolescents from ethnic minorities with obsessive–compulsive disorder. Journal of Obsessive-Compulsive and Related Disorders, 4, 30–36. 10.1016/j.jocrd.2014.11.003 [DOI] [Google Scholar]
- Foa EB, Coles M, Huppert JD, Pasupuleti RV, Franklin ME, & March J (2010). Development and validation of a child version of the obsessive compulsive inventory. Behav Ther, 41(1), 121–132. 10.1016/j.beth.2009.02.001 [DOI] [PubMed] [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, & Salkovskis PM (2002). The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological Assessment, 14(4), 485–496. [PubMed] [Google Scholar]
- Geller DA (2006). Obsessive-compulsive and spectrum disorders in children and adolescents [Review]. Psychiatr Clin North Am, 29(2), 353–370. 10.1016/j.psc.2006.02.012 [DOI] [PubMed] [Google Scholar]
- Geller DA, Biederman J, Jones J, Park K, Schwartz S, Shapiro S, & Coffey B (1998). Is juvenile obsessive-compulsive disorder a developmental subtype of the disorder? A review of the pediatric literature [Review]. J Am Acad Child Adolesc Psychiatry, 37(4), 420–427. 10.1097/00004583-199804000-00020 [DOI] [PubMed] [Google Scholar]
- Hanna G (2007). Schedule for Obsessive-Compulsive and Other Behavioral Syndromes. Ann Arbor, MI: University of Michigan. [Google Scholar]
- Hu L. t., & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jones AM, De Nadai AS, Arnold EB, McGuire JF, Lewin AB, Murphy TK, & Storch EA (2013). Psychometric properties of the obsessive compulsive inventory: child version in children and adolescents with obsessive-compulsive disorder. Child Psychiatry Hum Dev, 44(1), 137–151. 10.1007/s10578-012-0315-0 [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, & Ryan N (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry, 36(7), 980–988. 10.1097/00004583-199707000-00021 [DOI] [PubMed] [Google Scholar]
- Kovacs M, & MHS. (2011). Children’s Depression Inventory 2nd Edition (CDI 2) technical manual. Multi-Health Systems. [Google Scholar]
- Lewin AB, Storch EA, Geffken GR, Goodman WK, & Murphy TK (2006). A neuropsychiatric review of pediatric obsessive-compulsive disorder: etiology and efficacious treatments. Neuropsychiatric disease and treatment, 2(1), 21–31. [PMC free article] [PubMed] [Google Scholar]
- Little RJ, & Rubin DB (2019). Statistical analysis with missing data (Vol. 793). John Wiley & Sons. [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, & Conners CK (1997). The Multidimensional Anxiety Scale for Children (MASC): factor structure, reliability, and validity. J Am Acad Child Adolesc Psychiatry, 36(4), 554–565. 10.1097/00004583-199704000-00019 [DOI] [PubMed] [Google Scholar]
- Martinez-Gonzalez AE, Rodriguez-Jimenez T, Piqueras JA, Vera-Villarroel P, & Godoy A (2015). Psychometric Properties of the Obsessive-Compulsive Inventory-Child Version (OCI-CV) in Chilean Children and Adolescents. PLoS One, 10(8), e0136842. 10.1371/journal.pone.0136842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire JF, Geller DA, Murphy TK, Small BJ, Unger A, Wilhelm S, & Storch EA (2019). Defining Treatment Outcomes in Pediatric Obsessive-Compulsive Disorder Using a Self-Report Scale. Behavior Therapy, 50(2), 314–324. 10.1016/j.beth.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SH, Jaffee SR, Goodwin GP, & Franklin ME (2016). Hoarding in Children and Adolescents: A Review. Child Psychiatry Hum Dev, 47(5), 740–750. 10.1007/s10578-015-0607-2 [DOI] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD, & Wibulpolprasert S (2004). Monitoring global health: time for new solutions. Bmj, 329(7474), 1096–1100. 10.1136/bmj.329.7474.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide. Eighth Edition. Muthén & Muthén. [Google Scholar]
- Opakunle T, Aloba O, & Akinsulore A (2018). Obsessive Compulsive Inventory - Child Version (OCI-CV): Confirmatory factor analysis, reliability, validity and correlates among Nigerian adolescents. Malawi Med J, 30(4), 262–269. 10.4314/mmj.v30i4.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertusa A, Frost RO, Fullana MA, Samuels J, Steketee G, Tolin D, Saxena S, Leckman JF, & Mataix-Cols D (2010). Refining the diagnostic boundaries of compulsive hoarding: A critical review [DOI 10.1016/j.cpr.2010.01.007]. Clinical psychology review, 30(4), 371–386. 10.1016/j.cpr.2010.01.007 (NOT IN FILE) [DOI] [PubMed] [Google Scholar]
- Rapp AM, Bergman RL, Piacentini J, & McGuire JF (2016). Evidence-Based Assessment of Obsessive-Compulsive Disorder. Cent Nerv Syst Dis, 8, 13–29. 10.4137/jcnsd.S38359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhemtulla M, Brosseau-Liard PÉ, & Savalei V (2012). When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychological Methods, 17(3), 354–373. 10.1037/a0029315 [DOI] [PubMed] [Google Scholar]
- Rough HE, Hanna BS, Gillett CB, Rosenberg DR, Gehring WJ, Arnold PD, & Hanna GL (2020). Screening for Pediatric Obsessive-Compulsive Disorder Using the Obsessive-Compulsive Inventory-Child Version. Child Psychiatry Hum Dev, 51(6), 888–899. 10.1007/s10578-020-00966-x [DOI] [PubMed] [Google Scholar]
- Samuels J, Grados MA, Riddle MA, Bienvenu OJ, Goes FS, Cullen B, Wang Y, Greenberg BD, Fyer AJ, McCracken JT, Geller D, Murphy DL, Knowles JA, Rasmussen SA, McLaughlin NC, Piacentini J, Pauls DL, Stewart SE, Shugart YY, Maher B, Pulver AE, & Nestadt G (2014). Hoarding in Children and Adolescents with Obsessive-Compulsive Disorder. J Obsessive Compuls Relat Disord, 3(4), 325–331. 10.1016/j.jocrd.2014.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saylor CF, Finch AJ Jr., Spirito A, & Bennett B (1984). The children's depression inventory: a systematic evaluation of psychometric properties. J Consult Clin Psychol, 52(6), 955–967. 10.1037//0022-006x.52.6.955 [DOI] [PubMed] [Google Scholar]
- Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, & Leckman JF (1997). Children's Yale-Brown Obsessive Compulsive Scale: reliability and validity. J Am Acad Child Adolesc Psychiatry, 36(6), 844–852. 10.1097/00004583-199706000-00023 [DOI] [PubMed] [Google Scholar]
- Silverman WK, & Albano AM (1996). The Anxiety Disorders Interview Schedule for DSM–IV—Child and Parent Versions. Psychological Corporation. [Google Scholar]
- Storch EA, McGuire JF, Wu MS, Hamblin R, McIngvale E, Cepeda SL, Schneider SC, Rufino KA, Rasmussen SA, Price LH, & Goodman WK (2019). Development and Psychometric Evaluation of the Children's Yale-Brown Obsessive-Compulsive Scale Second Edition. J Am Acad Child Adolesc Psychiatry, 58(1), 92–98. 10.1016/j.jaac.2018.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanidir C, Adaletli H, Gunes H, Kilicoglu AG, Mutlu C, Bahali MK, Aytemiz T, & Uneri OS (2015). Impact of Gender, Age at Onset, and Lifetime Tic Disorders on the Clinical Presentation and Comorbidity Pattern of Obsessive-Compulsive Disorder in Children and Adolescents. J Child Adolesc Psychopharmacol, 25(5), 425–431. 10.1089/cap.2014.0120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S (2011). Early versus late onset obsessive–compulsive disorder: evidence for distinct subtypes. Clinical psychology review, 31(7), 1083–1100. [DOI] [PubMed] [Google Scholar]
- Wang JJ, Lin S, Best JR, Selles RR, & Stewart SE (2021). Race and ethnicity in pediatric OCD: An exploratory study of a clinical North American sample. Ann Clin Psychiatry, 33(1), 4–17. 10.12788/acp.0007 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.