Abstract
Objectives. To identify and describe differences in exposure to adverse childhood events (ACEs) by birth generation and lesbian, gay, bisexual, transgender, and queer plus (LGBTQ+) identity.
Methods. Using data from the 2019 Behavioral Risk Factor Surveillance System, we examined the odds of experiencing 4 or more ACEs for Generation X, millennials, and Generation Z relative to baby boomers (n = 56 262). We also explored differences between generations based on LGBTQ+ identity.
Results. The odds of experiencing 4 or more ACEs were higher for Generation X (odds ratio [OR] = 1.67; 95% confidence interval [CI] = 1.52, 1.83), millennials (OR = 2.12; 95% CI = 1.92, 2.35), and Generation Z (OR = 2.12; 95% CI = 1.79, 2.52) than for baby boomers. This disparity was amplified by LGBTQ+ identity (P = .016). The frequency of individual ACEs also varied by generation.
Conclusions. Exposure to 4 or more ACEs has increased for each generation since the baby boomers, and more so for the LGBTQ+ population. The ACEs experienced differ by generation.
Public Health Implications. Increasing ACE scores suggest that younger generations may have an increased risk of ACE-related health problems. Policies are needed to prevent ACE exposure and address the potential fallout from the ACEs that have seen the largest increases. (Am J Public Health. 2022;112(4):662–670. https://doi.org/10.2105/AJPH.2021.306642)
Adverse childhood experiences (ACEs) refer to distressing, often traumatic, events that happen in a person’s life before the age of 18 years, such as physical, sexual, and emotional abuse; neglect; and household dysfunction.1 ACEs can lead to deleterious effects in adulthood, including worse physical, behavioral, and economic health.2,3 Parental ACE scores have been linked to the child’s ACE score, raising concerns about intergenerational transfer of ACEs.4,5 A recent systematic review found that national trends for certain ACEs are increasing over time, including incarceration and drug use.6 However, there is a paucity of evidence comparing the variation in frequency of exposure and type of ACEs experienced between recent birth cohorts (hereafter, generations).
There are several structural and sociological factors that vary across generations with the potential to increase ACE exposure. At the structural level, incarceration rates began climbing in the 1980s, largely from the War on Drugs.7 Similarly, the crack epidemic of the 1980s and the opioid epidemic of the 1990s and 2000s have contributed to increased drug use and drug-related deaths.8 Socially, income inequality in the United States has increased sharply since the late 1970s, with top-earning families seeing substantial income gains while the incomes of the bottom 50% of families have stagnated.9 Children in families with lower incomes experience more ACEs, suggesting that increasing income inequality may contribute to higher ACE exposure in children born after the 1970s.10 Combined, these changing structural and sociological factors suggest that exposure to ACEs may vary among generations.
Nonmajority groups more heavily impacted by these structural and sociological changes may have experienced different patterns in ACE exposure. One group with potential for change in ACE exposure is the lesbian, gay, bisexual, transgender, and queer plus (LGBTQ+) population. Because of stigma and discrimination, the LBGTQ+ population is at higher risk of substance use and having a lower income than non-LGBTQ+ individuals, making them more likely to be affected by these structural and sociological changes.11,12 Correspondingly, the LGBTQ+ population may be more affected by changes in exposure to ACEs. In addition, there are more openly LGBTQ+ individuals among millennials and Generation Z (Gen-Z) than in any other generation, at 20% compared with 12% of Generation X (Gen-X) and 7% of baby boomers.13 Unfortunately, LGBTQ+ status remains strongly linked to ACEs, and this increase in open LGBTQ+ individuals may result in increased exposure to ACEs for younger generations.14,15
We explored whether there is a difference in ACE scores among Gen-Z, millennials, Gen-X, and baby boomers, and how that relationship varies for people with LGBTQ+ identities. Given the increases in ACE-associated structural and sociological factors between generations, we hypothesized that exposure to multiple ACEs has increased for each generation cohort. Furthermore, given their sensitivity to these changing factors and underlying elevated risk of ACEs, we anticipated that the relationship between generation and ACE exposure will be greater for LBGTQ+ individuals.
METHODS
This cross-sectional cohort study used data from the 2019 Behavioral Risk Factor Surveillance System (BRFSS). The BRFSS is an annual survey conducted by the Centers for Disease Control and Prevention that collects health risk‒related data using a complex sampling strategy designed to generalize to the noninstitutionalized adult US population.16 The survey is administered via a computer-assisted telephone interview on landlines and cell phones. The BRFSS consists of core modules covering demographics and common health indicators, as well as several optional modules that vary by state. In 2019, 21 states included the ACEs module, and 14 of those included the Sexual Orientation and Gender Identity module (Delaware, Florida, Iowa, Kansas, Mississippi, New York, Ohio, Oklahoma, Rhode Island, South Carolina, Tennessee, Virginia, West Virginia, and Wisconsin).16 We used data from the 14 states that included both modules.
Measures
Adverse childhood experiences
We calculated participant ACE scores by using the ACE module of the BRFSS.16 The ACE module contains 11 items: 5 questions indicating household stressors (e.g., “Did you live with anyone who served time or was sentenced to serve time in a prison, jail, or other correctional facility?”) and 6 questions indicating household violence (e.g., “Before age 18, how often did a parent or adult in your home ever hit, beat, kick, or physically hurt you in any way? Do not include spanking.”). Responses were dichotomized into exposed or unexposed for each question and summed to form a total ACE score as described elsewhere.17 Responses of “don’t know” or “refused” were recoded as missing. Finally, we dichotomized the total ACE score as either “less than four ACEs” or “greater than or equal to four ACEs,” as a cut-score of 4 or more ACEs is frequently identified as a point of concern in the ACEs outcome literature.1,2
Generation
Generational ranges from the Pew Research Center were used to define birth cohorts based on participant birth year (derived using age at the time of data collection).18 According to birth year, participants were classified as Gen-Z (1997–2001), millennials (1981–1996), Gen-X (1965–1980), or baby boomers (1946–1964). Individuals from earlier generations, born before 1946, were excluded to reduce survivorship bias relating to the long-term health effects of ACEs.
Sexual orientation and gender identity status
We used the Sexual Orientation and Gender Identity module in the BRFSS to create a binary indicator variable for self-identified LGBTQ+ status. The Sexual Orientation and Gender Identity module contains 1 sexual orientation question and 1 gender identity question.16 The sexual orientation question asks, “Which of the following best represents how you think of yourself?” with response options including gay, lesbian, bisexual, something else, or “straight, that is, not gay.” The gender identity question asks “Do you consider yourself to be transgender?” Participants providing any response other than straight and not transgender were coded as self-identifying as LGBTQ+. Responses of “don’t know” or “refused” were recoded as missing.
Statistical Analysis
Of 71 069 people eligible to respond to both the ACE and Sexual Orientation and Gender Identity modules, 20.8% (14 807) were missing data for at least 1 module, and 76.5% (n = 11 326) of those were missing data for both modules. The degree of missingness was not unexpected given the sensitive nature of the measures and aligns with missingness reported in previous studies.14,15 We included an examination of ACE missingness rates by generation as part of our initial descriptive analysis of the sample. We used a complete-case analysis for the main analyses such that respondents missing information for any variables were excluded from the analyses. For our primary analysis examining differences in ACE score by generation, we evaluated an unadjusted logistic regression model. Next, we evaluated a multiple logistic regression model that included generation, LGBTQ+ status, and the interaction between generation and LGBTQ+ status. Given the use of a logistic model, interactions were interpreted with a focus on the direction and magnitude of the association. For both models, we conducted sensitivity analyses in which the reference generation was changed to Gen-X and then millennials. Finally, we used χ2 analyses to examine the proportion of respondents exposed to each individual ACE across generation and LGBTQ+ status to explore underlying patterns in exposure that may inform interpretation of the overall ACE scores. To account for the complex sampling strategy of the BRFSS, all analyses included the appropriate design variables provided by the BRFSS (weight, cluster, and strata) and were analyzed using PROC SURVEYLOGISTIC and PROC SURVEYFREQ in SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
Our total unweighted sample included a total of 56 262 respondents and was predominantly non-Hispanic White (79.98%) and female (54.37%). Four or more ACEs were reported by 19.26% of the sample. The majority of the sample was from the baby boomer generation (52.89%), followed by Gen-X (25.43%), millennials (17.86%), and Gen-Z (3.81%). A total of 5.11% of the respondents self-identified as LGBTQ+. LGBTQ+ identity was most common among Gen-Z (16.2%), followed by millennials (9.7%), Gen-X (4.5%), and baby boomers (3.1%). Millennials had the highest missingness for the ACEs measure at 34.6%, Gen-Z had the lowest at 8.6%, and baby boomers and Gen-X were in the middle with 28.2% and 28.6%, respectively (Appendix A, available as a supplement to the online version of this article at http://www.ajph.org).
Generational Differences
The odds of having 4 or more ACEs varied by generation (F3,55657 = 88.34; P < .001), with younger generations having a higher proportion of individuals reporting a high ACE score (Table 1). Compared with baby boomers, the odds of having 4 or more ACEs were 1.67 times higher for Gen-X (95% confidence interval [CI] = 1.52, 1.83), 2.12 times higher for millennials (95% CI = 1.92, 2.35), and 2.12 times higher for Gen-Z (95% CI = 1.79, 2.52). All comparisons were significant in the sensitivity analyses, with the exception that millennials and Gen-Z were not significantly different.
TABLE 1—
Prevalence of Exposure to 4 or More Adverse Childhood Experiences (ACEs) by Generation: Behavioral Risk Factor Surveillance System, United States, 2019
| Generation, % (95% CI) | P | ||||
| Baby Boomers | Generation X | Millennials | Generation Z | ||
| ACEs | < .001 | ||||
| ≥ 4 | 14.69 (13.92, 15.46) | 22.31* (21.06, 23.56) | 26.77* (25.21, 28.33) | 26.78* (23.64, 29.92) | |
| < 4 | 85.31 (84.54, 86.08) | 77.69* (76.44, 78.94) | 73.23* (71.67, 74.79) | 73.22* (70.08, 76.36) | |
Note. CI = confidence interval. Weighted percentage of people with ≥ 4 ACEs in 2019 for baby boomers (1946–1964), Generation X (1965–1980), millennials (1981–1996), and Generation Z (1997–2001). Percentages are weighted using the design variables for the 2019 Behavioral Risk Factor Surveillance System. The P values are for the goodness-of-fit χ2 test for each ACE.
*Significantly different from baby boomers at P < .05.
In examining the frequency of each ACE by generation, we found several significant differences between the generations for all ACEs with the exception of having lived with someone who had alcohol dependency (Table 2). Gen-X, millennials, and Gen-Z all experienced more household depression, drug use, incarceration, parental divorce, and emotional abuse than did baby boomers. Millennials and Gen-Z reported more household depression, incarceration, parental divorce, and emotional abuse than Gen-X. Millennials and Gen-X reported more interparental violence and sexual abuse than Gen-Z or baby boomers, with both reporting higher proportions of being forced to touch an adult sexually. Gen-X also reported receiving more sexual touching, rape, and physical abuse than any other generation.
TABLE 2—
Prevalence of Exposure to Each Adverse Childhood Experience (ACE) by Generation: Behavioral Risk Factor Surveillance System, United States, 2019
| ACEs | Generation, % (95% CI) | P | |||
| Baby Boomers | Generation X | Millennials | Generation Z | ||
| Household depression | 12.28 (11.52, 13.04) | 17.84* (16.69, 18.99) | 26.37* (24.85, 27.88) | 31.47* (28.01, 34.93) | < .001 |
| Household alcoholism | 21.95 (21.06, 22.83) | 23.41 (22.19, 24.63) | 23.94 (22.52, 25.35) | 22.89 (19.84, 25.94) | .17 |
| Household drug use | 6.25 (5.73, 6.76) | 12.04* (11.05, 13.02) | 17.04* (15.80, 18.27) | 15.74* (13.39, 18.10) | < .001 |
| Household incarceration | 4.18 (3.64, 4.71) | 7.85* (7.03, 8.68) | 13.86* (12.65, 15.08) | 16.43* (13.88, 18.99) | < .001 |
| Parental divorce | 19.87 (18.97, 20.76) | 35.64* (34.15, 37.12) | 42.38* (40.62, 44.14) | 40.87* (37.18, 44.55) | < .001 |
| Interparental violence | 15.63 (14.82, 16.45) | 19.10* (17.91, 20.30) | 17.77* (16.48, 19.06) | 17.38 (14.70, 20.05) | < .001 |
| Physical abuse | 23.74 (22.78, 24.71) | 26.74* (25.36, 28.12) | 24.67 (23.12, 26.22) | 23.45 (20.37, 26.53) | .017 |
| Emotional abuse | 29.99 (28.94, 31.03) | 35.28* (33.87, 36.70) | 41.77* (40.02, 43.53) | 44.53* (40.73, 48.33) | < .001 |
| Touched sexually | 10.87 (10.16, 11.58) | 13.19* (12.17, 14.22) | 11.15 (10.00, 12.31) | 8.9 (6.94, 10.86) | < .001 |
| Forced to touch sexually | 7.40 (6.82, 7.97) | 10.41* (9.49, 11.33) | 9.04* (7.99, 10.09) | 7.41 (5.47, 9.35) | < .001 |
| Rape | 4.37 (3.93, 4.82) | 6.44* (5.68, 7.20) | 5.54 (4.66, 6.42) | 4.19 (2.66, 5.72) | < .001 |
Note. CI = confidence interval; LGBTQ+ = lesbian, gay, bisexual, transgender, and queer plus. Percentages are weighted using the design variables for the 2019 Behavioral Risk Factor Surveillance System. The P values are for the goodness-of-fit χ2 test for each ACE.
*Significantly different from baby boomers at P < .05.
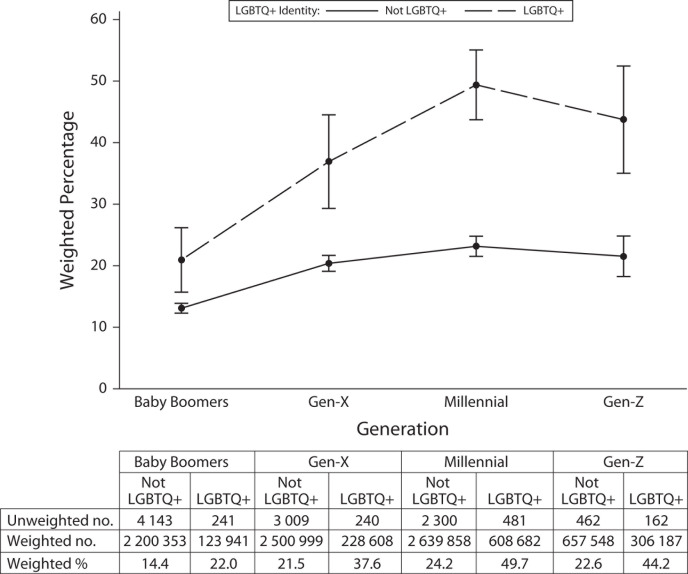
Sexual Orientation and Gender Identity Status
Our analysis examining self-identified LGBTQ+ status and generation yielded significant main effects for both generation (F3,55657 = 32.10; P < .001) and LGBTQ+ status (F1,55659 = 111.71; P < .001). The interaction between LGBTQ+ status and generation was also significant (F3,55657 = 3.46; P = .016; Figure 1). LGBTQ+ respondents from Gen-X were not differently likely to experience 4 or more ACEs than LGBTQ+ baby boomers (odds ratio [OR] = 1.31; 95% CI = 0.84, 2.04). LGBTQ+ millennials were more likely to experience 4 or more ACEs than LGBTQ+ baby boomers (OR = 1.84; 95% CI = 1.26, 2.71). Finally, LGBTQ+ individuals from Gen-Z had higher odds of experiencing ACEs than LGBTQ+ baby boomers, but the difference did not reach statistical significance (OR = 1.61; 95% CI = 0.99, 2.64). In the sensitivity analyses, no LGBTQ+ individuals from any generation significantly differed from LGBTQ+ members of Gen-X, and only LGBTQ+ baby boomers differed from LGBTQ+ millennials.
FIGURE 1—
Prevalence of Exposure to 4 or More Adverse Childhood Experiences by Generation and LGBTQ+ Identity: Behavioral Risk Factor Surveillance System, United States, 2019
Note. LGBTQ+ = lesbian, gay, bisexual, transgender, and queer plus. Weighted frequency of people with 4 or more adverse childhood experiences (ACEs) in 2019 by LGBTQ+ identity for baby boomers (1946–1964), Generation X (1965–1980), millennials (1981–1996), and Generation Z (1997–2001). Vertical error bars represent the 95% confidence interval for the estimated percentages. Tests of main effects and interaction for generation (F7,55653 = 32.10; P < .001), LGBTQ+ (F7,55659 = 111.71; P < .001), and generation * LGBTQ+ (F7,55657 = 32.10; P = .016).
There were noticeable differences in the individual ACEs reported by generation for LGBTQ+ respondents (Table 3). Gen-X, millennials, and Gen-Z were all more likely to have experienced household depression, incarceration, and divorce than were baby boomers. Gen-X and millennials reported more exposure to interparental violence than baby boomers. Millennials and Gen-Z both had higher rates of emotional abuse than Gen-X and baby boomers. Gen-X more frequently reported rape than other generations. Millennials experienced more household drug use than other generations.
TABLE 3—
Prevalence of Exposure to Each Adverse Childhood Experience (ACE) by Generation and LGBTQ+ Identity: Behavioral Risk Factor Surveillance System, United States, 2019
| ACEs | Generation, % (95% CI) | ||||
| Baby Boomers | Generation X | Millennials | Generation Z | P | |
| LGBTQ+ | |||||
| Household depression | 15.35 (11.23, 19.47) | 35.33* (28.02, 42.63) | 48.78* (43.27, 54.28) | 44.82* (36.52, 53.11) | < .001 |
| Household alcoholism | 28.95 (22.38, 35.51) | 36.9 (29.46, 44.33) | 34.94 (29.97, 39.91) | 32.56 (24.85, 40.28) | .47 |
| Household drug use | 11.89 (7.71, 16.08) | 22.81 (15.71, 29.9) | 28.96* (23.97, 33.96) | 21.91 (15.67, 28.16) | < .001 |
| Household incarceration | 6.08 (2.99, 9.17) | 20.32* (13.18, 27.46) | 21.11* (17.09, 25.12) | 23.18* (16.73, 29.62) | < .001 |
| Parental divorce | 25.11 (17.68, 32.55) | 40.72* (33.04, 48.40) | 47.15* (41.67, 52.64) | 47.40* (38.88, 55.92) | < .001 |
| Interparental violence | 17.37 (12.97, 21.77) | 31.37* (24.02, 38.71) | 28.15* (23.52, 32.77) | 24.95 (17.81, 32.09) | .021 |
| Physical abuse | 30.18 (23.55, 36.81) | 38.16 (30.67, 45.65) | 39.78 (34.40, 45.16) | 33.65 (25.83, 41.47) | .19 |
| Emotional abuse | 36.29 (29.90, 42.67) | 49.50 (41.85, 57.15) | 63.08* (57.68, 68.48) | 57.19* (48.44, 65.94) | < .001 |
| Touched sexually | 21.98 (15.20, 28.76) | 33.21 (25.93, 40.49) | 24.63 (19.79, 29.48) | 16.63 (10.34, 22.93) | .008 |
| Forced to touch sexually | 18.87 (12.21, 25.54) | 30.39 (23.12, 37.67) | 19.97 (15.75, 24.19) | 15.25 (8.99, 21.51) | .011 |
| Rape | 10.24 (6.28, 14.19) | 22.57* (15.77, 29.36) | 14.02 (10.38, 17.66) | 10.54 (4.68, 16.39) | .008 |
| Not LGBTQ+ | |||||
| Household depression | 12.16 (11.39, 12.94) | 16.93* (15.78, 18.07) | 23.85* (22.31, 25.39) | 28.29* (24.47, 32.10) | < .001 |
| Household alcoholism | 21.69 (20.81, 22.57) | 22.70 (21.48, 23.92) | 22.70 (21.23, 24.17) | 20.59 (17.31, 23.86) | .4 |
| Household drug use | 6.04 (5.53, 6.55) | 11.47* (10.51, 12.43) | 15.70* (14.45, 16.94) | 14.27* (11.78, 16.77) | < .001 |
| Household incarceration | 4.11 (3.56, 4.65) | 7.20* (6.43, 7.97) | 13.05* (11.77, 14.33) | 14.82* (12.06, 17.59) | < .001 |
| Parental divorce | 19.67 (18.79, 20.55) | 35.37* (33.86, 36.88) | 41.84* (39.98, 43.70) | 39.31* (35.23, 43.38) | < .001 |
| Interparental violence | 15.57 (14.74, 16.40) | 18.46* (17.27, 19.65) | 16.61 (15.27, 17.94) | 15.57 (12.75, 18.39) | .006 |
| Physical abuse | 23.50 (22.54, 24.47) | 26.14* (24.75, 27.54) | 22.98 (21.37, 24.58) | 21.02 (17.72, 24.32) | .003 |
| Emotional abuse | 29.75 (28.69, 30.81) | 34.54* (33.11, 35.96) | 39.38* (37.55, 41.21) | 41.51* (37.32, 45.70) | < .001 |
| Touched sexually | 10.46 (9.78, 11.14) | 12.15* (11.15, 13.14) | 9.64 (8.49, 10.79) | 7.06* (5.20, 8.92) | < .001 |
| Forced to touch sexually | 6.97 (6.44, 7.50) | 9.37* (8.49, 10.24) | 7.81 (6.75, 8.88) | 5.54 (3.70, 7.38) | .001 |
| Rape | 4.16 (3.72, 4.59) | 5.59* (4.89, 6.30) | 4.59 (3.70, 5.48) | 2.68 (1.46, 3.90) | .001 |
Note. CI = confidence interval; LGBTQ+ = lesbian, gay, bisexual, transgender, and queer plus. Weighted frequency of people with each ACE in 2019 by LGBTQ+ identity for baby boomers (1946–1964), Generation X (1965–1980), millennials (1981–1996), and Generation Z (1997–2001). Percentages are weighted using the design variables for the 2019 Behavioral Risk Factor Surveillance System. The P values are for the goodness-of-fit χ2 test for each ACE.
*Significantly different from baby boomers at P < .05.
DISCUSSION
We examined ACE exposure through a new lens by exploring generational differences in ACEs in general and by LGBTQ+ status. The proportion of people with 4 or more ACEs, considered to be an indicator of potential toxic stress and trauma, is substantially higher for generations following the baby boomers. Millennials reported the highest proportion of 4 or more ACEs, followed by Gen-Z and Gen-X. Household depression, drug use, incarceration, divorce, and emotional abuse appeared to be universally higher across Gen-X, millennials, and Gen-Z, while several other unique ACEs were elevated for each generation. This finding is consistent with a recent systematic review on trends in individual ACEs that found increases in drug overdoses from 1979 to 2016 and an increase in the divorce rate from 1950 to 2000.6
LGBTQ+ identity was associated with greater differences between generations when compared with baby boomers, but not Gen-X. Upon examination of individual ACEs experienced by generation and by LGBTQ+ status, ACEs were higher overall for LGBTQ+ individuals, and there were also differences in ACE exposure across generations for LGBTQ+ individuals. These findings suggest that exposure to ACEs has been increasing over time and more so for LGBTQ+ individuals. These findings are relevant as they may have substantial long-term health implications for younger generations, especially LGBTQ+ individuals. In addition, these differences in exposure to individual ACEs across generations may provide guidance toward structural factors that could be addressed to stem the exposure to ACEs. Furthermore, while we described changes in the individual ACEs to which each generation was exposed, we believe these differences may warrant a more thorough analysis than was within the scope of this study. Future studies should apply advanced analytic techniques to better characterize these different profiles of exposure and identify potential health outcomes associated with different ACE exposure profiles.
Limitations
This study had several limitations. First, we conducted this study by using data from a cross-sectional survey. While the BRFSS is designed and weighted to be representative, the self-report nature of this sample does include a risk for bias. In particular, recall bias may be a factor that affects how many ACEs are reported by each generation because of the differences in age at data collection. Thankfully, previous studies have shown that ACE recall is generally stable over time, but caution may still be warranted.19 Furthermore, the use of these cross-sectional data also confers some additional strengths by facilitating the examination of LGBTQ+ individuals, as longitudinal data of this population is scarce and often limited to more recent years. These data also mitigate some generational differences in responding, as all respondents were subject to the same social norms at the time of the survey. Future studies should seek to replicate this study prospectively via longitudinal cohorts or by examining ACEs reported at a fixed time point for each generation (e.g., at age 18 years). In addition, there is a risk of nonresponse bias because of the elevated missingness in the data. In particular, there was some concern that older generations may be less willing to report ACEs because of generational differences in social norms. Upon examination, there was generational variation in nonresponse to the ACE items. However, it was not driven by older generations. Future work is needed to assess the impact of differential missingness in ACE studies.
Second, our assessment of ACEs was limited to the ACEs included in the BRFSS. There remains an ongoing discourse regarding which additional childhood experiences should be added to the ACEs module, such as bullying and economic hardship.20 Future studies should seek to examine generational differences in exposure to ACEs that are not included in the BRFSS.
Third, Gen-Z only accounted for approximately 4% of our sample, potentially limiting our findings. This limitation is primarily attributable to Gen-Z being the youngest cohort, as most of Gen-Z was aged younger than 18 years and ineligible to be included in the 2019 BRFSS sample. Future studies will need to examine the prevalence of ACEs in Gen-Z further to identify potential differences between older and younger members of Gen-Z.
Health Implications
Our findings have concerning health implications, as ACEs are a well-established and highly documented risk factor for myriad chronic physical and mental health conditions.2,3 An increase in 4 or more ACEs among younger generations may in part explain observed upward trends in ACE-associated chronic conditions relative to baby boomers. For example, millennials and Gen-Z have been found to have higher incidences of mental health conditions and suicide deaths than previous generations.21,22 While it is too early to identify any real differences in the long-term health of Gen-Z, there is some early evidence that millennials are experiencing worse chronic health outcomes than Gen-X, and that the health trajectory of Gen-X and millennials is worse than that of baby boomers.22,23 It will be important for future studies to examine trends in ACE-related outcomes to identify any increases that may be related to the increased prevalence of ACEs. In addition, work is needed to understand the role that increased effort to mitigate the effects of ACEs may have on the relationship between increased generational ACEs and any potential health outcomes. Current and future efforts to address chronic health may need to be updated to account for the shifting ACE landscape.
Our study results showing increased disparity between generations for people who identify as LGBTQ+ is cause for additional concern, as there is already existing literature on the health disparities the LGBTQ+ population faces, and increasing ACEs may serve to exacerbate those disparities.14,24 Particularly concerning are the findings that 49.7% of LGBTQ+ millennials and 44.2% of LGBTQ+ Gen-Z reported 4 or more ACEs. With previous surveys finding that 20% of millennials and Gen-Z self-identify as LGBTQ+, the potential public health impact of these high ACE scores is immense.13 There is a documented need for targeted efforts seeking to improve the health of the LGBTQ+ population, and our findings suggest that this effort may be more critical than previously anticipated.24,25
Broadly, several intervention strategies have been found to effectively reduce ACE exposure at the family, school, and clinic level, and efforts to implement these strategies should be expanded and targeted toward the ACEs most frequently experienced in the current generation.26 For example, psychoeducational trainings on family conflict management and integrating social-emotional learning in schools have been successful.26 Regardless of the specific strategy, 1 of the key components is improving the frequency with which clinicians screen for and discuss ACEs.26 Previous work on LGBTQ+ health care has suggested the broad adoption of trauma-informed care for this population, a position that is reinforced by our findings.24 Given the increased prevalence of ACEs in younger generations, however, adopting a trauma-informed approach to care more broadly may be prudent.
Policy Implications
Our results suggest that each generation has faced unique challenges regarding exposure to ACEs. In addition to the universal increases in several ACEs, Gen-X experienced the most sexual abuse and physical abuse, while Gen-Z had the most exposure to household depression, parental incarceration, and emotional abuse. The millennial generation appeared to be a transitional generation, experiencing some of the interparental violence and sexual abuse reported by Gen-X as well as the emotional abuse and household dysfunction experienced by Gen-Z. If the differential exposure to ACEs among generations reflects the influence of structural factors, then our findings may be suggestive of policy areas that should be evaluated for their role in exposure to ACEs.
There is an extensive literature documenting effective strategies for reducing ACE exposure. Universal clinical approaches, such as increasing mental health and intimate partner violence screenings for all parents during perinatal care, as well as targeted interventions, such as nurse‒family partnership programs, have achieved success in reducing ACEs.27,28 In addition, economic and social policies have shown considerable promise regarding ACEs, such as implementing an earned income tax credit, raising the minimum wage, and providing quality early childhood education.28,29 Increasing financial support for these strategies at the federal, state, and county level has significant potential to reduce future ACE exposure and represents an opportunity for improving the health of future generations.
Gen-X, millennials, and Gen-Z have seen increased exposure to household depression and emotional abuse, both of which may be addressed through increasing access to mental health care. Depression is highly treatable with evidence-based therapies, and mental health care for parents has been identified as a highly effective method for preventing child abuse.30 More broadly, improving the use of mental health care among millennials and Gen-Z may aid in reducing the health impacts of ACEs while also reducing the risk of intergenerational transfer of ACEs to the next generation. However, there are currently well-established barriers to mental health care, including workforce shortages and insurance limitations, which will need to be modified at the policy level.31,32 Gen-X, millennials, and Gen-Z all have experienced increases in household drug use and parental incarceration. Both increasing drug use and increasing incarceration have been at least partially attributed to the War on Drugs and could be addressed through substance use policy reform addressing mandatory minimums for nonviolent drug offenses and improving access to substance use treatment.33
As the prevalence of people openly identifying as LGBTQ+ increases, implementing policies that promote LGBTQ+ acceptance and reduce stigma will be vital for reducing ACEs. Policies codifying equal rights protection for LGBTQ+ individuals are essential in addressing discrimination. In addition, policies designed to promote inclusivity in schools, such as the formation of gay‒straight alliance student groups and providing funding for SafeZone training programs have been shown to reduce stigma.34 Finally, providers competent and comfortable treating the LGBTQ+ population are in short supply, and health policies that increase access to physical and mental health care for LGBTQ+ individuals will be paramount in efforts to mitigate the deleterious effect of ACEs.24,25 In particular, improving access to mental health care for the LGBTQ+ population should be addressed, as 63% of LGBTQ+ millennials and 57% of LGBTQ+ people from Gen-Z reported emotional abuse.
Public Health Implications
Our results indicate that exposure to ACEs varies by generation, several ACEs are increasing among younger generations, and LGBTQ+ status is associated with greater ACE exposure and generational differences. These findings suggest that there may be an increase in ACE-related chronic health conditions as Gen-X, millennials, and Gen-Z age, which has implications for health care spending and the available workforce trained in trauma-informed care for these populations as they age. There may be opportunities for policy-level changes to reduce ACEs among future generations, such as improving ACE screening, increasing access to mental health care and substance use treatment, ending the War on Drugs, raising the minimum wage, and increasing access to quality early childhood education. Further effort is needed to identify and implement effective preventive measures.
ACKNOWLEDGMENTS
P. M. Hughes is supported by an Eshelman Fellowship from the Eshelman School of Pharmacy, UNC at Chapel Hill.
An earlier version of this work was presented at the 2021 American Public Health Association annual conference.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
HUMAN PARTICIPANT PROTECTION
This study was deemed exempt by the institutional review board of UNC Chapel Hill.
REFERENCES
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Hughes K, Bellis MA, Hardcastle KA, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- 3.Hughes P, Ostrout TL. Adverse childhood experiences as predictors of perceived health: assessing the ACE pyramid model using multiple-mediation. HCA Healthcare Journal of Medicine. 2020;1(5) doi: 10.36518/2689-0216.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narayan AJ, Lieberman AF, Masten AS. Intergenerational transmission and prevention of adverse childhood experiences (ACEs) Clin Psychol Rev. 2021;85:101997. doi: 10.1016/j.cpr.2021.101997. [DOI] [PubMed] [Google Scholar]
- 5.Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry. 2017;87(1):3–14. doi: 10.1037/ort0000133. [DOI] [PubMed] [Google Scholar]
- 6.Finkelhor D. Trends in adverse childhood experiences (ACEs) in the United States. Child Abuse Negl. 2020;108:104641. doi: 10.1016/j.chiabu.2020.104641. [DOI] [PubMed] [Google Scholar]
- 7.National Research Council.; . The Growth of Incarceration in the United States: Exploring Causes and Consequences. Washington, DC: National Academies Press; 2014. p. 444. [DOI] [Google Scholar]
- 8.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Trends and patterns of geographic variation in mortality from substance use disorders and intentional injuries among US counties, 1980‒2014. JAMA. 2018;319(10):1013–1023. doi: 10.1001/jama.2018.0900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piketty T, Saez E, Zucman G. Distributional national accounts: methods and estimates for the United States. Q J Econ. 2018;133(2):553–609. doi: 10.1093/qje/qjx043. [DOI] [Google Scholar]
- 10.Halfon N, Larson K, Son J, Lu M, Bethell C. Income inequality and the differential effect of adverse childhood experiences in US children. Acad Pediatr. 2017;17(7S):S70–S78. doi: 10.1016/j.acap.2016.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Badgett MVL, Choi SK, Wilson B. LGBT Poverty in the United States. Williams Institute; 2019. p. 46.https://williamsinstitute.law.ucla.edu/wp-content/uploads/National-LGBT-Poverty-Oct-2019.pdf [Google Scholar]
- 12.Schuler MS, Stein BD, Collins RL. Differences in substance use disparities across age groups in a national cross-sectional survey of lesbian, gay, and bisexual adults. LGBT Health. 2019;6(2):68–76. doi: 10.1089/lgbt.2018.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.GLAAD. Accelerating Acceptance 2017. 2017:8. Available at. 2021. https://www.glaad.org/files/aa/2017_GLAAD_Accelerating_Acceptance.pdf
- 14.Bertolino DF, Sanchez TH, Zlotorzynska M, Sullivan PS. Adverse childhood experiences and sexual health outcomes and risk behaviors among a nationwide sample of men who have sex with men. Child Abuse Negl. 2020;107:104627. doi: 10.1016/j.chiabu.2020.104627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Craig SL, Austin A, Levenson J, Leung VWY, Eaton AD, D’Souza SA. Frequencies and patterns of adverse childhood events in LGBTQ+ youth. Child Abuse Negl. 2020;107:104623. doi: 10.1016/j.chiabu.2020.104623. [DOI] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. BRFSS survey data and documentation 2019. 2020. https://www.cdc.gov/brfss/annual_data/annual_2019.html
- 17.Ford DC, Merrick MT, Parks SE, et al. Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychol Violence. 2014;4(4):432–444. doi: 10.1037/a0037723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dimock M.2021. https://www.pewresearch.org/fact-tank/2019/01/17/where-millennials-end-and-generation-z-begins
- 19.Reuben A, Moffitt TE, Caspi A, et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry. 2016;57(10):1103–1112. doi: 10.1111/jcpp.12621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Choi C, Mersky JP, Janczewski CE, Plummer Lee C-T, Davies WH, Lang AC. Validity of an expanded assessment of adverse childhood experiences: a replication study. Child Youth Serv Rev. 2020;117:105216. doi: 10.1016/j.childyouth.2020.105216. [DOI] [Google Scholar]
- 21.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185–199. doi: 10.1037/abn0000410. [DOI] [PubMed] [Google Scholar]
- 22.Zheng H, Echave P. Are recent cohorts getting worse? Trends in US adult physiological status, mental health, and health behaviors across a century of birth cohorts. Am J Epidemiol. 2021;190(11):2242–2255. doi: 10.1093/aje/kwab076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.DePew R, Gonzales G. Differences in health outcomes between millennials and Generation X in the USA: evidence from the National Health Interview Survey. Popul Res Policy Rev. 2020;39(3):605–616. doi: 10.1007/s11113-019-09563-w. [DOI] [Google Scholar]
- 24.Harless C, Nanney M, Johnson A, Polanski A, Beach-Ferrara J. The Report of the 2019 Southern LGBTQ Health Survey. Asheville, NC: Campaign for Southern Equality; 2019. [Google Scholar]
- 25.Williams ND, Fish JN. The availability of LGBT‐specific mental health and substance abuse treatment in the United States. Health Serv Res. 2020;55(6):932–943. doi: 10.1111/1475-6773.13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Biglan A, Van Ryzin MJ, Hawkins JD. Evolving a more nurturing society to prevent adverse childhood experiences. Acad Pediatr. 2017;17(7 suppl):S150–S157. doi: 10.1016/j.acap.2017.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Asmussen K, McBride T, Waddell S. The potential of early intervention for preventing and reducing ACE-related trauma. Soc Policy Soc. 2019;18(3):425–434. doi: 10.1017/S1474746419000071. [DOI] [Google Scholar]
- 28.Bellazaire A. Preventing and Mitigating the Effects of Adverse Childhood Experiences. National Conference of State Legislatures; 2018. p. 14.https://www.ncsl.org/Portals/1/HTML_LargeReports/ACEs_2018_32691.pdf [Google Scholar]
- 29.Fortson BL, Klevens J, Merrick MT, Gilbert LK, Alexander SP. Preventing child abuse and neglect: a technical package for policy, norm, and programmatic activities. Atlanta, GA: National Center for Injury Prevention and Control, Division of Violence Prevention; 2016. [DOI] [Google Scholar]
- 30.Richards TN, Tillyer MS, Wright EM. Intimate partner violence and the overlap of perpetration and victimization: considering the influence of physical, sexual, and emotional abuse in childhood. Child Abuse Negl. 2017;67:240–248. doi: 10.1016/j.chiabu.2017.02.037. [DOI] [PubMed] [Google Scholar]
- 31.Andrilla CHA, Garberson LA, Patterson DG, Quigley TF, Larson EH. Comparing the health workforce provider mix and the distance travelled for mental health services by rural and urban Medicare beneficiaries. J Rural Health. 2020;37(4):692–699. doi: 10.1111/jrh.12504. [DOI] [PubMed] [Google Scholar]
- 32.Mojtabai R. US health care reform and enduring barriers to mental health care among low-income adults with psychological distress. Psychiatr Serv. 2021;72(3):338–342. doi: 10.1176/appi.ps.202000194. [DOI] [PubMed] [Google Scholar]
- 33.Beletsky L, Davis CS. Today’s fentanyl crisis: Prohibition’s Iron Law, revisited. Int J Drug Policy. 2017;46:156–159. doi: 10.1016/j.drugpo.2017.05.050. [DOI] [PubMed] [Google Scholar]
- 34.Chaudoir SR, Wang K, Pachankis JE. What reduces sexual minority stress? A review of the intervention “toolkit”: sexual minority stress-reduction interventions. J Soc Issues. 2017;73(3):586–617. doi: 10.1111/josi.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]