Abstract
Background
Electronic health record (EHR) system users devise workarounds to cope with mismatches between workflows designed in the EHR and preferred workflows in practice. Although workarounds appear beneficial at first sight, they frequently jeopardize patient safety, the quality of care, and the efficiency of care.
Objective
This review aims to aid in identifying, analyzing, and resolving EHR workarounds; the Sociotechnical EHR Workaround Analysis (SEWA) framework was published in 2019. Although the framework was based on a large case study, the framework still required theoretical validation, refinement, and enrichment.
Methods
A scoping literature review was performed on studies related to EHR workarounds published between 2010 and 2021 in the MEDLINE, Embase, CINAHL, Cochrane, or IEEE databases. A total of 737 studies were retrieved, of which 62 (8.4%) were included in the final analysis. Using an analytic framework, the included studies were investigated to uncover the rationales that EHR users have for workarounds, attributes characterizing workarounds, possible scopes, and types of perceived impacts of workarounds.
Results
The SEWA framework was theoretically validated and extended based on the scoping review. Extensive support for the pre-existing rationales, attributes, possible scopes, and types of impact was found in the included studies. Moreover, 7 new rationales, 4 new attributes, and 3 new types of impact were incorporated. Similarly, the descriptions of multiple pre-existing rationales for workarounds were refined to describe each rationale more accurately.
Conclusions
SEWA is now grounded in the existing body of peer-reviewed empirical evidence on EHR workarounds and, as such, provides a theoretically validated and more complete synthesis of EHR workaround rationales, attributes, possible scopes, and types of impact. The revised SEWA framework can aid researchers and practitioners in a wider range of health care settings to identify, analyze, and resolve workarounds. This will improve user-centered EHR design and redesign, ultimately leading to improved patient safety, quality of care, and efficiency of care.
Keywords: electronic health records, electronic medical records, framework, patient safety, unintended consequences, usability, workarounds, workflow
Introduction
Electronic health record (EHR) systems are the backbone of modern health care organizations. This is in pursuit of promising gains in patient safety, quality of care, efficiency, and control of spiraling costs by enabling value-based reimbursements. However, realizing these expected benefits is far from a given value. Over the years, an overwhelming number of studies have reported that EHRs have led to a multitude of unintended consequences. Examples include potential patient harm resulting from bad EHR usability [1,2]; increased odds of burnout of health care professionals [3,4]; physicians experiencing stress [5]; users spending an equal amount of time on desktop medicine as they spend on having face-to-face interaction with patients [6,7]; extensive copy and paste practices of patient notes leading to note bloating, internal inconsistencies, and errors [8]; and the unavailability of complete clinical information at the point of care [9].
Many causes of unintended consequences of EHR use can be traced back to discrepancies between the behavior, intentions, and expectations of EHR users and the workflows dictated by EHRs [10-15]. When EHR users experience workflow mismatches, they often create workarounds [16]. Workarounds are practices that handle exceptions to normal workflow [17] and do not follow the rules, assumptions, workflow regulations, or intentions of systems designers [18]. Although workarounds allow EHR users to proceed in accomplishing tasks in their preferred way (with or without the EHR), research shows that workarounds frequently jeopardize the safety, quality, and efficiency of care [19]. Given their common adverse effects, workarounds are valuable points of departure for improving the EHR design and redesign.
Blijleven et al [20] developed the Sociotechnical EHR Workaround Analysis (SEWA) framework for identifying, analyzing, and subsequently resolving EHR workarounds. The framework was inspired by the Systems Engineering Initiative for Patient Safety (SEIPS) framework [21]. The SEWA framework incorporates four angles: the different rationales EHR users have for creating workarounds (eg, memory aid and required data entry option missing), the stakeholders affected by a workaround (eg, patient and health care professional), the impact of a workaround (eg, on safety and efficiency), and inherent attributes of workarounds (eg, unavoidable, repetitive, and cascading).
The SEWA framework [20] was based on approximately 200 hours of audiovisual material of user–EHR interaction and semistructured follow-up interviews in a single large case study in an academic hospital setting [19,22]. However, the authors argued that the applicability of the framework in other contexts might be limited, such as in nonacademic hospitals or in hospitals where paper-based workarounds (eg, for ordering drugs) are still allowed. Therefore, they recommended validation, refinement, and enrichment of the framework by incorporating workarounds and related rationales, attributes, possible scopes, and types of consequences identified in other EHR workaround–related research and clinical contexts.
To address these shortcomings, a scoping literature review was performed to identify and map the available evidence on EHR workarounds [23]. This paper presents a revised version of the SEWA framework, with rationales, attributes, possible scopes, and types of impact described in workaround-related studies in the EHR, electronic medical record, and computerized physician order entry domains in primary, secondary, and tertiary care contexts published between 2010 and 2021.
Methods
Search Strategy
The MEDLINE, Embase, CINAHL, Cochrane, and IEEE databases were searched for relevant studies. We included original, full papers of research with empirical data and conference papers if there were no full papers published in the same study. Gray literature, such as books, was not considered. The search queries included the keywords EHR, electronic health record, and workaround(s) and their synonyms. As the aim was to identify new rationales, attributes, consequences, and scopes of EHR workarounds for the enrichment of the SEWA framework, we defined the searches as broad as possible. Pilot literature searches were conducted to check the appropriateness of the queries. During the pilot searches, the term workflow was used as a possible synonym for workarounds. The inclusion of this term led to a much larger pool of possible studies. However, most of these studies were focused on care processes that have no relation with EHR use and were thus, out of scope. Therefore, this term was excluded from search queries. Furthermore, to include the complete spectrum of possible EHRs, a combination of the terms health/medical/patient/health care/clinical record and electronic/digital/online was used. The results of this pilot evaluation were used to adjust the queries. The used queries are shown in Table 1.
Table 1.
Search queries used for the scoping review.
| Date of search | Database | Query |
| April 9, 2021 | MEDLINE | ([([([(((((health record*) OR medical record*) OR patient record*) OR health care record*) OR clinical record*) AND electronic] OR digital) OR digitized] OR online) OR online] OR [([Electronic Health Records (MeSH Terms)] OR electronic health record*) OR EHR] OR [([Medical Records Systems, Computerized (MeSH Terms)] OR computerized patient record) OR computerised patient record]) AND ([(workaround*) OR work around*] OR workaround*) |
| April 9, 2021 | Embase |
(workaround OR workaround* OR workaround OR workaround*) AND
([(health record* OR medical record* OR patient record* OR health care record* OR clinical record*) AND (electronic OR digital OR online OR online OR digitized OR digitised)] OR [electronic health record* OR ehr OR electronic medical record* OR emr] OR [computerized patient record OR computerised patient record]) |
| April 9, 2021 | CINAHL | (workaround OR work around OR workarounds) AND ([(health record OR medical record OR patient record OR health care record OR clinical record) AND (electronic OR digital OR [online OR online] OR [digitized OR digitised])] OR [electronic health record* OR EHR OR electronic medical record* OR EMR] OR [computerized patient record OR computerised patient record]) |
| April 9, 2021 | IEEE | ([([([(workaround*) OR work around*] OR workaround*)])] AND [([health record OR medical record OR patient record OR health care record OR clinical record] AND [electronic OR digital OR (online OR online) OR (digitized OR digitised)]) OR (electronic health record* OR EHR OR electronic medical record* OR EMR) OR (computerized patient record OR computerised patient record)]) |
| April 9, 2021 | Cochrane | (workaround*): ti, ab,kw OR (work-around*): ti, ab, kw OR (work around*): ti, ab, kw AND ([(electronic health record*): ti, ab, kw OR (health record*): ti, ab, kw OR (medical record*): ti, ab, kw OR (patient record*): ti, ab, kw OR (health care record): ti, ab, kw OR (EHR): ti, ab, kw OR (EMR):ti, ab, kw OR (clinical record):ti, ab, kw OR ([computerized patient record]: ti, ab, kw OR [computerized patient record]: ti, ab, kw)] AND [electronic]: ti, ab, kw OR [digital]: ti, ab, kw OR [online]: ti, ab, kw OR [online]: ti, ab, kw OR [digitized]: ti, ab, kw OR [digitised]: ti, ab, kw) |
Selection Criteria
The inclusion and exclusion criteria were chosen through discussions among the reviewers (FH, VB, and MJ). As the focus of this scoping review was on workarounds in EHR use, it was decided to exclude studies focused on barcode medication administration systems as these systems serve only 1 purpose and cover only a small part of the medication process. Furthermore, the choice was made to exclude research focused on EHR functionalities other than those aimed at supporting the clinical process. To ensure data quality, a study was excluded if the research methods were not reported or in case the study had not been peer reviewed. Furthermore, research published before 2010 was excluded as EHRs have undergone significant changes and improvements over the years. Finally, the inclusion and exclusion criteria were chosen.
The study inclusion criteria were as follows:
The health care setting of the study must be either ≥1 of primary, secondary, or tertiary care.
Workarounds were studied or reported in the context of EHR use.
The article was published between 2010 and 2021.
Studies were excluded if they met any of the following criteria:
The research focused on EHR functionalities other than those aimed at supporting within the clinical process.
The research focused on a barcode administration functionality.
The article was not written in English.
There was no access to the full-text article.
The article was not peer reviewed.
The research methods were not reported.
Article Selection
A literature search was conducted in April 2021. A total of 737 potentially relevant studies were retrieved from our initial search of electronic databases, more specifically MEDLINE (263/737, 35.7%), Embase (121/737, 16.4%), CINAHL (89/737, 12.1%), IEEE (58/737, 7.9%), and Cochrane (206/737, 27.9%). The results of the study selection process are shown in the PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analyses) flowchart in Figure 1.
Figure 1.
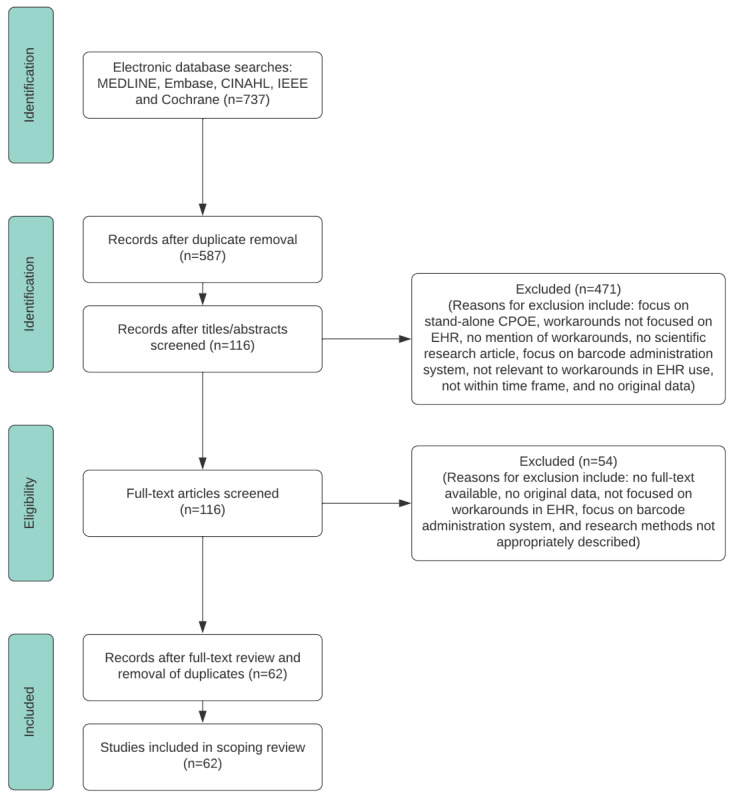
PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analyses) flowchart of the study selection process. CPOE: computerized physician order entry; EHR: electronic health record.
The retrieved 737 studies were uploaded to EndNoteX9 (Clarivate), in which duplicates were first removed by both using EndNoteX9 and by performing a manual check (Figure 1). This led to 79.6% (587/737) of unique studies. These studies were reviewed by two independent reviewers (FH and VB). The 2 reviewers first independently screened the titles and abstracts of the eligible papers to evaluate whether they met the inclusion criteria. Of the 587 studies, 116 (19.8%) studies met the inclusion criteria, and 471 (60.2%) studies were excluded (because of, for example, workarounds not being focused on the EHR, not being a scientific research article, and no workarounds mentioned). Afterward, the reviewers independently screened the full texts of these 116 studies, leading to 62 (53.4%) included studies and 54 (46.6%) excluded studies (eg, no full-text available and methods inappropriately described). After each screening phase, the two reviewers (FH and VB) discussed their findings. The next screening phase was conducted only if a consensus was reached between the 2 independent reviewers. If a disagreement between the 2 reviewers could not be resolved by discussion, a third independent reviewer (MJ) was involved. After consensus was reached, interrater reliability was reported by calculating the Cohen κ. The interrater agreement was also calculated to show the extent to which the reviewers were able to reconcile through discussion [24]. For the first round (title and abstract screening), the Cohen κ value was 0.958, and the interrater agreement value was 0.985. For the second round (full-text screening), the Cohen κ value was 0.930, and the interrater agreement value was 0.966.
Data Analysis of Included Articles
Descriptive data from the included articles, such as title, authors, year of publication, study setting, functionalities of EHR studied, and research methods used, were captured in a generic overview per study (Multimedia Appendix 1). Workaround-related data from the included articles, such as workaround rationales, attributes, consequences, and scope, were captured in an analytic frame per study (Multimedia Appendix 2).
The data extracted from the included articles were compared with the SEWA framework on a study-by-study basis. In doing so, SEWA was supplemented with new rationales, attributes, possible scopes, and types of impact of EHR workarounds that were not previously included. After the analysis was completed, an updated (graphical) version of the SEWA framework was created.
Results
General Characteristics
The general characteristics of the 62 studies are shown in Table 2. There was an approximately even split in studies published between 2010 and 2015 and between 2016 and 2021. The study settings were almost equally distributed, with most (23/62, 37%) being set in tertiary care, such as academic hospitals and special care units. The largest group of studies (28/62, 45%) focused their research on the EHR overall. Of the 62 studies, 17 (27%) studied medication-related functionalities or EHR-integrated systems, such as computerized physician order entries. Approximately half (28/62, 45%) used or included a combination of physicians, nurses, and other staff such as pharmacists and administrative personnel as participants. Of the 62 studies, 26 (42%) used a combination of methods such as observations, interviews, and questionnaires, 15 (24%) used interviews as the sole method, 5 (8%) solely used questionnaires, 7 (11%) solely used observational methods, and 9 (15%) used other methods such as think-aloud protocols and documentation analysis.
Table 2.
General characteristics of the included studies (N=62).
| Study characteristics | Values, n (%) | |
| Year of publication | ||
|
|
2010-2015 | 30 (48) |
|
|
2016-2021 | 32 (52) |
| Study setting | ||
|
|
Primary care | 18 (29) |
|
|
Secondary care | 21 (34) |
|
|
Tertiary care | 23 (37) |
| Functionalities of EHRa studied | ||
|
|
Medication-related (eg, prescribing and CPOEb) | 17 (27) |
|
|
Documentation | 8 (13) |
|
|
Overall EHR | 28 (45) |
|
|
Others (eg, alert systems and authentication process) | 9 (15) |
| Type of population | ||
|
|
Physicians | 9 (15) |
|
|
Nurses | 13 (21) |
|
|
Others (eg, pharmacists or administrative staff such as managers, assistants, secretary, or not mentioned) |
12 (19) |
|
|
Combination of users | 28 (45) |
| Methods | ||
|
|
Observations | 7 (11) |
|
|
Interviews | 15 (24) |
|
|
Questionnaires | 5 (8) |
|
|
Others (eg, think-aloud and documentation analysis) | 9 (15) |
|
|
Combination of ≥1 observation, interview, questionnaire, or other | 26 (42) |
aEHR: electronic health record.
bCPOE: computerized physician order entry.
Validation, Refinement, and Enrichment of the SEWA Framework
Overview
Evidence for the work system components, rationales, attributes, type of impact, and possible scopes contained in the original SEWA framework was found in the included studies. Moreover, we refined and enriched the original framework with 7 rationales, 4 attributes, and 3 types of impact. The following subsections elaborate on the work system components, rationales, attributes, possible scopes, and types of impact.
Work System Components
Support for all 5 work system components was found in the included studies, as shown in Table 3. No new work system components were identified. However, we made 1 change to the work system component EHR system, which we renamed to EHR system and related technology. The latter was incorporated to also cover workarounds stemming from the use of technology other than the EHR but used in parallel with the EHR, such as scanners [25].
Table 3.
Overview of work system components and related included studies.
| Work components | Description | Studies |
| Person(s) | Health care professionals developing and using EHRa workarounds | [20,26-28] |
| EHR system and related technology | The EHR and related information technology used by health care professionals | [20,25-27,29-31] |
| Organization | Organizational conditions (eg, care directives and hospital policies) under which clinical tasks and EHR use are performed | [20,27,28,30,31] |
| Physical environment | The environment (eg, outpatient examination room and inpatient ward) and its conditions (eg, lighting and noise) in which clinical tasks are conducted by health care professionals | [20,26,27] |
| Task(s) | Clinical tasks performed by health care professionals | [20,26,28,30-32] |
aEHR: electronic health record.
Rationales
The rationales for workarounds contained in the original SEWA framework were confirmed in many studies. In addition, 7 new rationales were identified.
Under the work system component person(s), one rationale was added: trust (Table 4). Multiple studies reported that users created workarounds because of insufficient trust in the (new) system or its capabilities while frequently maintaining trust in older systems (replaced by the EHR). The related causes of a lack of trust are a lack of perceived usefulness of the (new) system and insufficient confidence in (completeness) of the data available in the EHR [33-39]. The description of the rationale awareness has been refined to also cover awareness of the information needs of patients and not just of colleagues [40]. Likewise, the description of the rationale social norms has been refined to make cultural [30,41] and collaborative [27,42] aspects more explicit.
Table 4.
Overview of rationales for the work system component person(s) and related included studies.
| Rationales | Description | Studies |
| Declarative knowledge | Not knowing how to use (a part of) the EHRa to accomplish a task | [20,33,34,39,43,44] |
| Procedural knowledge | Knowing how but not being proficient enough to use a part of the EHR to accomplish a task | [20,28,34,39,44] |
| Memory aid | Writing patient data down on paper (eg, keywords) or adding visual elements to parts of text in a progress note (eg, boldfacing, italicizing, or underlining) to remind oneself | [20,34,39,43,45-47] |
| Awareness | Storing patient data that are perceived important by the EHR user for other colleagues or patients to be noticed (frequently in a data field other than the intended field in the EHR) | [20,39,40,48] |
| Social norms | Formal or informal, collaborative, and cultural understandings among health care professionals leading to the creation and dissemination of workarounds (eg, mimicking workarounds devised by colleagues to accomplish a task or working around the system upon as friendly requested or enforced by a fellow clinician) | [20,29-31,45,49,50] |
| Trust (new) | Having insufficient trust in the (new) EHR system or its capabilities, lack of perceived usefulness, or insufficient confidence in the (completeness) of data | [20,33-39] |
aEHR: electronic health record.
Although extensive support in the included studies was found for all rationales under the work system component EHR system and related technology, except patient data specificity, four additional rationales were identified: data integration, enforced actions, data quality, and interoperability (Table 5). The description of the pre-existing rationale technical issues has been refined to cover technical issues related to ancillary technology used in conjunction with the EHR.
Table 5.
Overview of rationales for the work system component EHRa system and related technology and related included studies.
| Rationales | Description | Studies |
| Usability | High behavioral user cost in accomplishing a task | [20,25,28,29,31,41,42,45,46,50-56] |
| Technical issues | (A part of the) EHR or ancillary technology halting, crashing, or slowing down, hampering the EHR user in accomplishing a task | [20,25,28,31-33,43,44,51-53,55-61] |
| Data presentation | Preferring a different data view (eg, visualization by means of charts or graphs rather than plain text) | [20,55,62] |
| Patient data specificity | Needing to enter or request patient data with greater or lesser specificity than offered or enforced by the EHR | [20] |
| Data integration (new) | EHR not providing or supporting the integration of patient data necessary for care delivery | [42,45] |
| Enforced actions (new) | Avoiding or overriding actions enforced by the EHR (eg, bypassing the approval process of prescribing medication or using a different user account) | [29,43,48,54,63] |
| Data quality (new) | Unavailability of data, disparity in data formats (eg, the same data being stored in multiple different formats in the EHR), lack of standardization, and information gaps in the EHR | [31,34-36,39,41,42,44,50,57,64-67] |
| Interoperability (new) | Data not able to be exchanged between health care systems or institutions (eg, causing data to be unavailable at the right moment and time) | [44,50,54,56,64,65] |
aEHR: electronic health record.
Multiple studies provide support for all rationales under the work system component organization except for the rationale data migration policy (Table 6). No new rationales were identified.
Table 6.
Overview of rationales for the work system component organization and related included studies.
| Rationales | Description | Studies |
| Efficiency | Using an alternative way of accomplishing a task that improves actual efficiency | [20,29,31,34,35,37,43,46,47,55,68-70] |
| Data migration policy | Not having (direct) access to required historical data because of data not having been imported from previously used systems to the current EHRa | [20] |
| Enforced data entry | EHR enforcing user to enter patient data of which neither the user nor the patient has knowledge of | [20,71,72] |
| Required data entry option missing | EHR not offering the required data entry option (eg, 3.75 mg rather than the available options 2.5 mg or 5 mg) | [20,32,71] |
aEHR: electronic health record.
Although support was found for the pre-existing rationales under task(s), one rationale was added: task complexity (Table 7). Approximately 3% (2/62) of studies described that the EHR does not always sufficiently support the execution of a complex task at hand [34-39]. Therefore, health care professionals resort to workarounds to make their workflow more digestible.
Table 7.
Overview of rationales for the work system component task(s) and related included studies.
| Rationales | Description | Studies |
| Task interference | Inability to perform multiple tasks at once (eg, simultaneously treating a patient on the treatment table as well as entering patient data into the EHRa) | [20,61] |
| Commitment to patient interaction | Valuing patient interaction over computer interaction (ie, writing things down on paper and afterward entering this into the EHR) | [20,34,37,41,44,55,61,73] |
| Task complexity (new) | The high complexity of the tasks needing to be conducted | [34,39] |
aEHR: electronic health record.
Finally, the SEIPS work system component physical environment was incorporated into the original SEWA framework without any rationale. However, Dudding et al [25] mentioned that a busy, fast-paced environment where interruptions are constant, such as the neonatal intensive care unit, gives rise to EHR workarounds. The rationale here is “fast-paced environment” and is described as “devising workarounds to cope with the inability to, for example, update the documentation in fast-paced care environments where interruptions are constant” [25].
Attributes
Although several studies confirmed the previously defined attributes in SEWA, several included studies also mentioned a total of 4 new attributes (Table 8). These are concerned with whether the user is aware of using a workaround [49] (awareness), whether the workaround is an individual or shared practice across users [49] (shared), on what medium the workaround is conducted (eg, paper or computer) [34,41] (medium), and whether the workaround is a formal or informal practice (eg, part of a defined process or approved or promoted by management or not) [56] (formality).
Table 8.
Overview of workaround attributes and related included studies.
| Attributes | Description | Source |
| Cascadedness | Whether the workaround initiates the creation of 1 or multiple additional workarounds or is an isolated occurrence | [20] |
| Avoidability | Whether the workaround is required to proceed with one’s workflow or optional | [20,32,66,74] |
| Anticipatedness | Whether the workaround is used at known moments in time (ie, the situation in which the workaround is used is known beforehand) or used unexpectedly | [20,74] |
| Repetitiveness | Whether the workaround is ingrained into the workflow (ie, becomes part of daily routines) or used temporarily to overcome workflow constraints | [20,56,74] |
| Awareness (new) | Whether the user is aware of using the workaround | [49] |
| Shared (new) | Whether the workaround is a shared practice across multiple other users of the EHRa or limited to 1 user | [49] |
| Medium (new) | On what medium the workaround is conducted (eg, paper, computer, verbal, or a combination) | [34,41] |
| Formality (new) | Whether the use of the workaround is approved by management and part of a defined process | [56] |
aEHR: electronic health record.
Types of Impact
The previously defined types of impact in the SEWA framework were confirmed by many included studies. Multiple additional types of impact were also identified: privacy/security, data quality, employee perception of EHR, financial, law/regulations, and workload (Table 9). Privacy/security relates not only to the impact a workaround has on the security and privacy of the data but also to the patient and organization itself. Data quality concerns the impact on, for example, loss of data, or a lower data quality because of spelling or formatting mistakes in the data. Moreover, workarounds can have a positive or negative financial impact [58], may jeopardize laws and regulations [63,75], and have a positive or negative impact on the workload of the user [43].
Table 9.
Overview of types of impact and related included studies.
| Impact | Description | Source |
| Patient safety | The impact on the safety (physical and mental) of the patient | [20,28,29,41,43,46,48,53,54,58,59,67,75-77] |
| Effectiveness of care | The effectiveness and quality of the care process performed | [20,28,43,46,54,58,59,67] |
| Efficiency of care | The impact on the efficiency of the care process in terms of time and resources expended | [20,33,55,60,64,72,76] |
| Privacy and security (new) | Impact on the security and privacy of data related to the patient or organization | [32,39,51,52,56,63,68,75] |
| Data quality (new) | Impact of workarounds on data quality (eg, loss of data or decreased data quality) | [32,33,35,39,41,46,51,52,56,59,69,76] |
| Financial (new) | Financial implications because of the workaround | [58] |
| Laws and regulations (new) | Legal conflicts resulting from the use of a workaround | [63,75] |
| Workload (new) | An increase or decrease in workload of the EHRa user resulting from the use of a workaround | [43] |
aEHR: electronic health record.
Possible Scopes
Only a few studies explicitly discussed possible scopes (ie, entities impacted) of workarounds and resonated with those in the SEWA framework [41,43,53,77] (Table 10). No new possible scopes were identified.
Table 10.
Overview of possible scopes and related included studies.
| Scope | Description | Source |
| Patient | The workaround affects the patients in the care process | [20,43,77] |
| Health care professional | The workaround affects the health care professionals such as physicians, nurses, and pharmacists | [20] |
| Organization | The workaround affects the whole organization, including the supporting departments such as finance or legal | [20,41,53] |
Revised Version of the SEWA Framework
On the basis on the foregoing results, the original SEWA framework [20] was revised to incorporate new rationales, attributes, types of impact, and possible scopes identified in the included studies (Figure 2). The revised SEWA framework still comprises 2 major parts. The first part concerns the work system and its components (inspired by the SEIPS framework), [21] constituting the context in which EHR workarounds are created. The work system components now include 22 rationales (previously 15) for workaround creation, and EHR workarounds are now defined by 8 attributes (previously 4). The second part concerns the possible scope of workarounds in terms of types and number of entities affected (still 3), as well as their impact on patient safety, the effectiveness of care, the efficiency of care, and 5 newly introduced types of impact. All new items in the framework are marked with asterisks.
Figure 2.
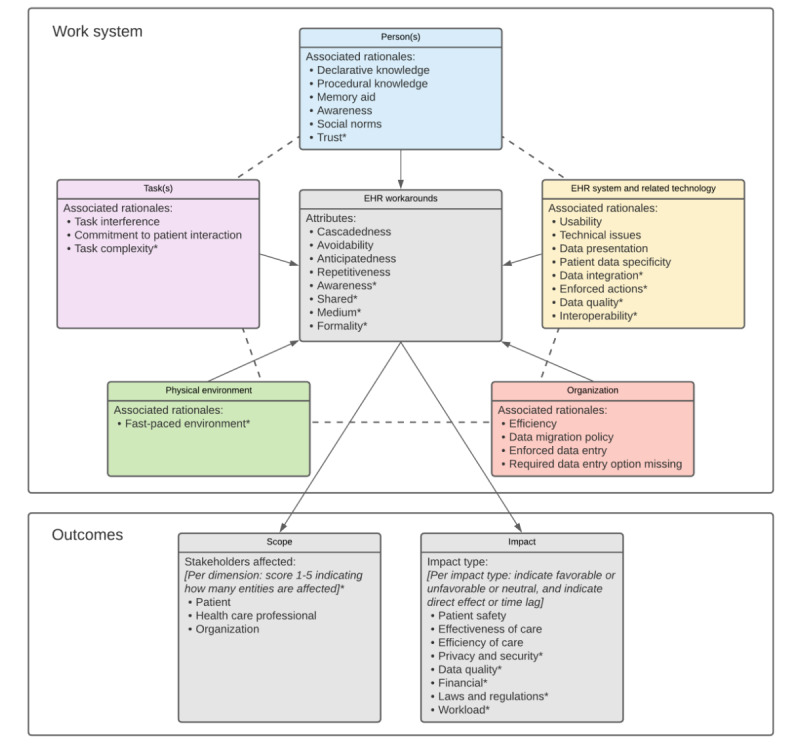
Revised SEWA framework with incorporated rationales, attributes, types of impact, and possible scopes identified in included studies. EHR: electronic health record; SEWA: Sociotechnical Electronic Health Record Workaround Analysis.
The recommendations [20] for using a scoring mechanism to indicate whether the impact per workaround is favorable, unfavorable, or neutral, as well as to indicate whether the impact is immediate or only observable after a certain period (direct/time lag) remain. However, we also recommend the inclusion of a scoring mechanism to indicate the number of patients and health care professionals and organizational units affected per applicable scope. This is in line with Carayon et al [53], who distinguished between workarounds having an impact at an individual or team level (eg, an entire team of nurses in a certain hospital ward). Applying a scoring mechanism allows for a more substantiated view when analyzing and prioritizing various identified workarounds for resolution.
Discussion
Principal Findings
A scoping review was performed to theoretically validate the SEWA framework [20] and refine and enrich it with newly identified rationales, attributes, types of impact, and possible scopes of EHR workarounds. The scoping review retrieved 737 studies, of which 62 (8.4%) were included. The included studies provided extensive support for nearly all the items included in the original SEWA framework. SEWA was revised and enriched with 7 new rationales, 4 attributes, and 5 types of impact of EHR workarounds mentioned in the included studies. The definitions of several existing rationales were also refined. As a result, SEWA is now grounded in the existing body of peer-reviewed empirical evidence on EHR workarounds published between 2010 and 2021. In addition, this revised version is likely also applicable in a wider range of health care settings as input for the original SEWA framework that came from a single comprehensive case study on EHR workarounds in an academic hospital.
Comparison With the Literature
The results of this scoping review are in line with prior research and reviews of EHR workarounds. In an integrative review, Fraczkowski et al [78] examined nurse workarounds in EHR use. The categories defined in the review by Fraczkowski et al [78] are similar to the work system components defined in SEWA, with the exception of usability being a separate rationale in the SEWA framework under the work system component EHR system and related technology [20]. The patient category in the review by Fraczkowski et al [78] is defined as an impact and scope category in SEWA [20]. Finally, Fraczkowski et al [78], similar to Koppel et al [18], did not include a work system component for person(s) (the users of the EHR) as a category. Our scoping review is one of the few studies that investigated the entire spectrum of EHR users. On the one hand, we included studies of all types of health care professionals in primary, secondary, and tertiary care who make use of an EHR in their clinical practice, whereas other reviews merely focused on a specific population such as physicians, nurses, or secretary personnel [78]. On the other hand, we excluded studies researching workarounds in the use of barcode medication administration systems, whereas other reviews did not [78].
Strengths and Limitations
To maximize the capture of relevant information on EHR workarounds, comprehensive and structured searches were conducted in MEDLINE, Embase, CINAHL, Cochrane, and IEEE databases. Data charting templates and analytic frames were used to extract relevant information from the reviewed studies and compare with pre-existing items in the SEWA framework.
A total of 2 research team members participated in the review process for both the title and abstract and full-text review phases, with a Cohen κ value of >0.9. This indicates an adequate interrater agreement. Despite this, our scoping review is at risk for selection bias, as we did not identify all available data, such as gray literature on EHR workarounds. There is a chance that relevant but nonincluded studies may use terminology other than the terms included in the search queries.
The broad scope of the retrieved information on EHR workarounds and the different types of studies reporting a particular issue made using a formal meta-analytic method to quantitatively assess the quality of the studies and evidence of retrieved information difficult. However, given the purpose of the scoping review to theoretically validate and refine the SEWA framework, we do not consider this limitation.
Implications for Practice and Future Research
Multidisciplinary teams (comprising, for example, physicians, nurses, management, and EHR developers) can use the revised SEWA framework to identify, analyze, prioritize, and resolve workarounds related to EHR use more accurately. Similarly, the consequences of current and future configurations of the work system (health care professionals’ work processes and activities in relation to their EHR use) can be assessed and discussed in greater detail to determine how a design and redesign of the work system would positively or negatively affect the interaction between work system components. Finally, as workarounds are subject to gradual change (eg, personal changes in experience with the EHR, system updates to the EHR, and hospital policies), more detailed snapshots of the work system using SEWA can be taken over time and compared so as to gain valuable insights into how EHR workarounds evolve over time.
Concerning future research, EHR systems are continuously subject to technological evolution by developments in, for example, artificial intelligence, machine learning, and telemedicine. This may lead to the creation of hitherto unidentified rationales, attributes, possible scopes, and types of impact of workarounds on users, patients, and health care organizations. Similarly, more studies on EHR workarounds will continue to emerge that may report novel insights not incorporated into the revised SEWA framework. Therefore, we expect that SEWA needs a continuous process of refinement over time. This could be done by repeating the scoping review using the described search strategy, search queries, and inclusion and exclusion criteria.
In addition, although the revised SEWA framework is now theoretically validated, refined, and enriched, practical validation is still required. The same holds true when investigating its practicality. The firsthand experience from the application of SEWA in practice could yield suggestions for further improvement. A related suggestion is that although the framework helps in identifying and analyzing workarounds, a prioritization method for handling these issues is likely required, as workarounds are generally abundant in any organization, and resources to resolve them are finite. Therefore, the framework could benefit from being extended with prioritization mechanisms and weighting factors for deciding which workarounds require priority. Similarly, the framework could be translated into a practical tool such as a scoring matrix to facilitate use by practitioners.
Finally, the applicability of the SEWA framework could be explored for systems other than EHRs (eg, enterprise resource planning, customer relationship management, and content management) and in other settings (eg, nonacademic hospitals and general practitioner practices) and even in other industries (eg, financial services and manufacturing) after appropriate validation. Although SEWA has an explicit focus on EHRs used in health care, we expect many of the described workaround rationales and attributes to be applicable to other systems, settings, and industries.
Abbreviations
- EHR
electronic health record
- PRISMA
Preferred Reporting Item for Systematic Reviews and Meta-Analyses
- SEIPS
Systems Engineering Initiative for Patient Safety
- SEWA
Sociotechnical Electronic Health Record Workaround Analysis
Descriptive data template that was captured per included study.
Analytic frame with workaround-related data captured per study.
Footnotes
Authors' Contributions: VB, FH, and MJ conceived and designed the study. FH collected the data. VB and FH analyzed the data and wrote the manuscript. VB and MJ edited the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest: None declared.
References
- 1.Howe JL, Adams KT, Hettinger AZ, Ratwani RM. Electronic health record usability issues and potential contribution to patient harm. J Am Med Assoc. 2018 Mar 27;319(12):1276–8. doi: 10.1001/jama.2018.1171. http://europepmc.org/abstract/MED/29584833 .2676098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ratwani RM, Savage E, Will A, Fong A, Karavite D, Muthu N, Rivera AJ, Gibson C, Asmonga D, Moscovitch B, Grundmeier R, Rising J. Identifying electronic health record usability and safety challenges in pediatric settings. Health Aff (Millwood) 2018 Nov;37(11):1752–9. doi: 10.1377/hlthaff.2018.0699. [DOI] [PubMed] [Google Scholar]
- 3.Melnick ER, Dyrbye LN, Sinsky CA, Trockel M, West CP, Nedelec L, Tutty MA, Shanafelt T. The association between perceived electronic health record usability and professional burnout among US physicians. Mayo Clin Proc. 2020 Mar;95(3):476–87. doi: 10.1016/j.mayocp.2019.09.024. https://linkinghub.elsevier.com/retrieve/pii/S0025-6196(19)30836-5 .S0025-6196(19)30836-5 [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Dyrbye LN, West CP. Addressing physician burnout: the way forward. J Am Med Assoc. 2017 Mar 07;317(9):901–2. doi: 10.1001/jama.2017.0076.2603408 [DOI] [PubMed] [Google Scholar]
- 5.Akbar F, Mark G, Prausnitz S, Warton EM, East JA, Moeller MF, Reed ME, Lieu TA. Physician stress during electronic health record inbox work: in situ measurement with wearable sensors. JMIR Med Inform. 2021 Apr 28;9(4):e24014. doi: 10.2196/24014. https://medinform.jmir.org/2021/4/e24014/ v9i4e24014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tai-Seale M, Olson CW, Li J, Chan AS, Morikawa C, Durbin M, Wang W, Luft HS. Electronic health record logs indicate that physicians split time evenly between seeing patients and desktop medicine. Health Aff (Millwood) 2017 Apr 01;36(4):655–62. doi: 10.1377/hlthaff.2016.0811. http://europepmc.org/abstract/MED/28373331 .36/4/655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinsky C, Colligan L, Li L, Prgomet M, Reynolds S, Goeders L, Westbrook J, Tutty M, Blike G. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med. 2016 Sep 06;165(11):753. doi: 10.7326/m16-0961. [DOI] [PubMed] [Google Scholar]
- 8.Tsou A, Lehmann C, Michel J, Solomon R, Possanza L, Gandhi T. Safe practices for copy and paste in the EHR: systematic review, recommendations, and novel model for health IT collaboration. Appl Clin Inform. 2017 Dec 20;26(01):12–34. doi: 10.4338/aci-2016-09-r-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sittig DF, Wright A, Ash J, Singh H. New unintended adverse consequences of electronic health records. Yearb Med Inform. 2018 Mar 06;25(01):7–12. doi: 10.15265/iy-2016-023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH. Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2006 Sep 01;13(5):547–56. doi: 10.1197/jamia.m2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 2007 Jun;76 Suppl 1:21–7. doi: 10.1016/j.ijmedinf.2006.05.017.S1386-5056(06)00138-9 [DOI] [PubMed] [Google Scholar]
- 12.Ash JS, Sittig DF, Poon EG, Guappone K, Campbell E, Dykstra RH. The extent and importance of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc. 2007 Jul 01;14(4):415–23. doi: 10.1197/jamia.m2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell EM, Guappone KP, Sittig DF, Dykstra RH, Ash JS. Computerized provider order entry adoption: implications for clinical workflow. J Gen Intern Med. 2009 Jan 20;24(1):21–6. doi: 10.1007/s11606-008-0857-9. http://europepmc.org/abstract/MED/19020942 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greenhalgh T, Potts H, Wong G, Bark P, Swinglehurst D. Tensions and paradoxes in electronic patient record research: a systematic literature review using the meta-narrative method. Milbank Q. 2009 Dec;87(4):729–88. doi: 10.1111/j.1468-0009.2009.00578.x. http://europepmc.org/abstract/MED/20021585 .MILQ578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blijleven V, Koelemeijer K, Jaspers M. Identifying and eliminating inefficiencies in information system usage: a lean perspective. Int J Med Inform. 2017 Nov;107:40–7. doi: 10.1016/j.ijmedinf.2017.08.005.S1386-5056(17)30204-6 [DOI] [PubMed] [Google Scholar]
- 16.Halbesleben J, Wakefield D, Wakefield B. Work-arounds in health care settings: literature review and research agenda. Health Care Manage Rev. 2008;33(1):2–12. doi: 10.1097/01.HMR.0000304495.95522.ca.00004010-200801000-00002 [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi M, Fussell S, Xiao Y, Seagull F. Work coordination, workflow, and workarounds in a medical context. Proceedings of the CHI '05 Extended Abstracts on Human Factors in Computing Systems; CHI05: CHI 2005 Conference on Human Factors in Computing Systems; April 2 - 7, 2005; Portland OR USA. 2005. pp. 1561–4. [DOI] [Google Scholar]
- 18.Koppel R, Wetterneck T, Telles JL, Karsh B. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc. 2008 Jul 01;15(4):408–23. doi: 10.1197/jamia.m2616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blijleven V, Koelemeijer K, Wetzels M, Jaspers M. Workarounds emerging from electronic health record system usage: consequences for patient safety, effectiveness of care, and efficiency of care. JMIR Hum Factors. 2017 Oct 05;4(4):e27. doi: 10.2196/humanfactors.7978. https://humanfactors.jmir.org/2017/4/e27/ v4i4e27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blijleven V, Koelemeijer K, Jaspers M. SEWA: a framework for sociotechnical analysis of electronic health record system workarounds. Int J Med Inform. 2019 May;125:71–8. doi: 10.1016/j.ijmedinf.2019.02.012.S1386-5056(18)30460-X [DOI] [PubMed] [Google Scholar]
- 21.Holden RJ, Carayon P, Gurses AP, Hoonakker P, Hundt AS, Ozok AA, Rivera-Rodriguez AJ. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013 Nov;56(11):1669–86. doi: 10.1080/00140139.2013.838643. http://europepmc.org/abstract/MED/24088063 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Blijleven V, Koelemeijer K, Jaspers M. Exploring workarounds related to electronic health record system usage: a study protocol. JMIR Res Protoc. 2017 Apr 28;6(4):e72. doi: 10.2196/resprot.6766. https://www.researchprotocols.org/2017/4/e72/ v6i4e72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018 Nov 19;18(1):143. doi: 10.1186/s12874-018-0611-x. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-018-0611-x .10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociolog Methods Res. 2013 Aug 21;42(3):294–320. doi: 10.1177/0049124113500475. [DOI] [Google Scholar]
- 25.Dudding K, Gephart S, Carrington J. Neonatal nurses experience unintended consequences and risks to patient safety with electronic health records. Comput Inform Nurs. 2018 Apr;36(4):167–76. doi: 10.1097/CIN.0000000000000406. [DOI] [PubMed] [Google Scholar]
- 26.Niazkhani Z, Pirnejad H, van der Sijs H, Aarts J. Evaluating the medication process in the context of CPOE use: the significance of working around the system. Int J Med Inform. 2011 Jul;80(7):490–506. doi: 10.1016/j.ijmedinf.2011.03.009.S1386-5056(11)00075-X [DOI] [PubMed] [Google Scholar]
- 27.Holden RJ. What stands in the way of technology-mediated patient safety improvements?: a study of facilitators and barriers to physicians' use of electronic health records. J Patient Saf. 2011 Dec;7(4):193–203. doi: 10.1097/PTS.0b013e3182388cfa. http://europepmc.org/abstract/MED/22064624 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Salahuddin L, Ismail Z, Abd Ghani MK, Aboobaider BM, Hasan Basari AS. Exploring the contributing factors to workarounds to the hospital information system in Malaysian hospitals. J Eval Clin Pract. 2020 Oct 20;26(5):1416–24. doi: 10.1111/jep.13326. [DOI] [PubMed] [Google Scholar]
- 29.Baysari M, Gigante JD, Moran M, Sandaradura I, Li L, Richardson K, Sandhu A, Lehnbom E, Westbrook J, Day R. Redesign of computerized decision support to improve antimicrobial prescribing. Appl Clin Inform. 2017 Dec 20;08(03):949–63. doi: 10.4338/aci2017040069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ser G, Robertson A, Sheikh A. A qualitative exploration of workarounds related to the implementation of national electronic health records in early adopter mental health hospitals. PLoS One. 2014;9(1):e77669. doi: 10.1371/journal.pone.0077669. http://dx.plos.org/10.1371/journal.pone.0077669 .PONE-D-12-12587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stevenson JE, Israelsson J, Petersson G, Bath PA. Factors influencing the quality of vital sign data in electronic health records: a qualitative study. J Clin Nurs. 2018 Mar 08;27(5-6):1276–86. doi: 10.1111/jocn.14174. [DOI] [PubMed] [Google Scholar]
- 32.Ali M, Cornford T, Klecun E. Exploring control in health information systems implementation. Stud Health Technol Inform. 2010;160(Pt 1):681–5. [PubMed] [Google Scholar]
- 33.Crosson JC, Etz RS, Wu S, Straus SG, Eisenman D, Bell DS. Meaningful use of electronic prescribing in 5 exemplar primary care practices. Ann Fam Med. 2011 Sep 12;9(5):392–7. doi: 10.1370/afm.1261. http://www.annfammed.org/cgi/pmidlookup?view=long&pmid=21911757 .9/5/392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Flanagan ME, Saleem JJ, Millitello LG, Russ AL, Doebbeling BN. Paper- and computer-based workarounds to electronic health record use at three benchmark institutions. J Am Med Inform Assoc. 2013 Jun 01;20(e1):59–66. doi: 10.1136/amiajnl-2012-000982. http://europepmc.org/abstract/MED/23492593 .amiajnl-2012-000982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horsky J, Drucker E, Ramelson H. Higher accuracy of complex medication reconciliation through improved design of electronic tools. J Am Med Inform Assoc. 2018 May 01;25(5):465–75. doi: 10.1093/jamia/ocx127. http://europepmc.org/abstract/MED/29121197 .4601882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Djalali S, Ursprung N, Rosemann T, Senn O, Tandjung R. Undirected health IT implementation in ambulatory care favors paper-based workarounds and limits health data exchange. Int J Med Inform. 2015 Nov;84(11):920–32. doi: 10.1016/j.ijmedinf.2015.08.001.S1386-5056(15)30025-3 [DOI] [PubMed] [Google Scholar]
- 37.Watson A, Skipper C, Steury R, Walsh H, Levin A. Inpatient nursing care and early warning scores: a workflow mismatch. J Nurs Care Qual. 2014;29(3):215–22. doi: 10.1097/NCQ.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 38.Hysong SJ, Sawhney MK, Wilson L, Sittig DF, Espadas D, Davis T, Singh H. Provider management strategies of abnormal test result alerts: a cognitive task analysis. J Am Med Inform Assoc. 2010 Jan 01;17(1):71–7. doi: 10.1197/jamia.m3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saleem JJ, Russ AL, Neddo A, Blades PT, Doebbeling BN, Foresman BH. Paper persistence, workarounds, and communication breakdowns in computerized consultation management. Int J Med Inform. 2011 Jul;80(7):466–79. doi: 10.1016/j.ijmedinf.2011.03.016.S1386-5056(11)00092-X [DOI] [PubMed] [Google Scholar]
- 40.Ihlebæk HM. Lost in translation - Silent reporting and electronic patient records in nursing handovers: an ethnographic study. Int J Nurs Stud. 2020 Sep;109:103636. doi: 10.1016/j.ijnurstu.2020.103636. https://linkinghub.elsevier.com/retrieve/pii/S0020-7489(20)30120-6 .S0020-7489(20)30120-6 [DOI] [PubMed] [Google Scholar]
- 41.Stevenson JE, Israelsson J, Nilsson G, Petersson G, Bath PA. Vital sign documentation in electronic records: the development of workarounds. Health Informatics J. 2016 Aug 19;:206–15. doi: 10.1177/1460458216663024.1460458216663024 [DOI] [PubMed] [Google Scholar]
- 42.Carrington J, Effken J. Strengths and limitations of the electronic health record for documenting clinical events. Comput Inform Nurs. 2011 Jun;29(6):360–7. doi: 10.1097/NCN.0b013e3181fc4139. [DOI] [PubMed] [Google Scholar]
- 43.Lee S, Lee M. Nurses' electronic medical record workarounds in a tertiary teaching hospital. Comput Inform Nurs. 2021 Mar 08;39(7):367–74. doi: 10.1097/CIN.0000000000000692.00024665-202107000-00006 [DOI] [PubMed] [Google Scholar]
- 44.Rathert C, Porter TH, Mittler JN, Fleig-Palmer M. Seven years after meaningful use: physicians’ and nurses’ experiences with electronic health records. Health Care Manage Rev. 2019;44(1):30–40. doi: 10.1097/hmr.0000000000000168. [DOI] [PubMed] [Google Scholar]
- 45.Assis-Hassid S, Grosz BJ, Zimlichman E, Rozenblum R, Bates DW. Assessing EHR use during hospital morning rounds: a multi-faceted study. PLoS One. 2019 Feb 25;14(2):e0212816. doi: 10.1371/journal.pone.0212816. https://dx.plos.org/10.1371/journal.pone.0212816 .PONE-D-18-33695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cresswell KM, Worth A, Sheikh A. Integration of a nationally procured electronic health record system into user work practices. BMC Med Inform Decis Mak. 2012 Mar 08;12(1):15. doi: 10.1186/1472-6947-12-15. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-12-15 .1472-6947-12-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Menon S, Murphy D, Singh H, Meyer AN, Sittig D. Workarounds and test results follow-up in electronic health record-based primary care. Appl Clin Inform. 2017 Dec 16;07(02):543–59. doi: 10.4338/aci-2015-10-ra-0135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Der Sijs H, Rootjes I, Aarts J. The shift in workarounds upon implementation of computerized physician order entry. Stud Health Technol Inform. 2011;169:290–4. [PubMed] [Google Scholar]
- 49.Barrett AK, Stephens KK. Making Electronic Health Records (EHRs) work: informal talk and workarounds in healthcare organizations. Health Commun. 2017 Aug 27;32(8):1004–13. doi: 10.1080/10410236.2016.1196422. [DOI] [PubMed] [Google Scholar]
- 50.O'Malley AS, Grossman JM, Cohen GR, Kemper NM, Pham HH. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010 Mar 22;25(3):177–85. doi: 10.1007/s11606-009-1195-2. http://europepmc.org/abstract/MED/20033621 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bowen JL, O'Brien BC, Ilgen JS, Irby DM, Cate OT. Chart stalking, list making, and physicians' efforts to track patients' outcomes after transitioning responsibility. Med Educ. 2018 Apr 30;52(4):404–13. doi: 10.1111/medu.13509. [DOI] [PubMed] [Google Scholar]
- 52.Bristol A, Nibbelink C, Gephart S, Carrington J. Nurses' use of positive deviance when encountering electronic health records-related unintended consequences. Nurs Adm Q. 2018;42(1):1–11. doi: 10.1097/NAQ.0000000000000264.00006216-201801000-00014 [DOI] [PubMed] [Google Scholar]
- 53.Carayon P, Hundt AS, Hoonakker P. Technology barriers and strategies in coordinating care for chronically ill patients. Appl Ergon. 2019 Jul;78:240–7. doi: 10.1016/j.apergo.2019.03.009. http://europepmc.org/abstract/MED/31046955 .S0003-6870(19)30061-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schiff GD, Amato MG, Eguale T, Boehne JJ, Wright A, Koppel R, Rashidee AH, Elson RB, Whitney DL, Thach T, Bates DW, Seger AC. Computerised physician order entry-related medication errors: analysis of reported errors and vulnerability testing of current systems. BMJ Qual Saf. 2015 Apr 16;24(4):264–71. doi: 10.1136/bmjqs-2014-003555. http://qualitysafety.bmj.com/lookup/pmidlookup?view=long&pmid=25595599 .bmjqs-2014-003555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Staggers N, Jennings BM, Lasome CE. A usability assessment of AHLTA in ambulatory clinics at a military medical center. Mil Med. 2010 Jul;175(7):518–24. doi: 10.7205/milmed-d-09-00285. [DOI] [PubMed] [Google Scholar]
- 56.Cresswell KM, Mozaffar H, Lee L, Williams R, Sheikh A. Workarounds to hospital electronic prescribing systems: a qualitative study in English hospitals. BMJ Qual Saf. 2017 Jul;26(7):542–51. doi: 10.1136/bmjqs-2015-005149.bmjqs-2015-005149 [DOI] [PubMed] [Google Scholar]
- 57.Bhattacharjee S, Murcko AC, Fair MK, Warholak TL. Medication prior authorization from the providers perspective: a prospective observational study. Res Social Adm Pharm. 2019 Sep;15(9):1138–44. doi: 10.1016/j.sapharm.2018.09.019.S1551-7411(18)30154-2 [DOI] [PubMed] [Google Scholar]
- 58.Samaras EA, Real SD, Curtis AM, Meunier TS. Recognizing nurse stakeholder dissonance as a critical determinant of patient safety in new healthcare information technologies. Work. 2012;41 Suppl 1:1904–10. doi: 10.3233/WOR-2012-0406-1904.2271K3M825770883 [DOI] [PubMed] [Google Scholar]
- 59.Yeung M, Lapinsky S, Granton J, Doran D, Cafazzo J. Examining nursing vital signs documentation workflow: barriers and opportunities in general internal medicine units. J Clin Nurs. 2012 Apr;21(7-8):975–82. doi: 10.1111/j.1365-2702.2011.03937.x. [DOI] [PubMed] [Google Scholar]
- 60.Naughton BD. Medicine authentication technology: a quantitative study of incorrect quarantine, average response times and offline issues in a hospital setting. BMJ Open. 2019 Feb 19;9(2):e026619. doi: 10.1136/bmjopen-2018-026619. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=30782947 .bmjopen-2018-026619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sockolow P, Bass EJ, Eberle CL, Bowles KH. Homecare nurses' decision-making during admission care planning. Stud Health Technol Inform. 2016;225:28–32. [PubMed] [Google Scholar]
- 62.Slight S, Eguale T, Amato M, Seger AC, Whitney DL, Bates DW, Schiff GD. The vulnerabilities of computerized physician order entry systems: a qualitative study. J Am Med Inform Assoc. 2016 Mar;23(2):311–6. doi: 10.1093/jamia/ocv135.ocv135 [DOI] [PubMed] [Google Scholar]
- 63.Balka E, Tolar M. Everyday ethical dilemmas arising with electronic record use in primary care. Stud Health Technol Inform. 2011;169:285–9. [PubMed] [Google Scholar]
- 64.Vest J, Issel LM, Lee S. Experience of using information systems in public health practice: findings from a qualitative study. Online J Public Health Inform. 2014 Feb 05;5(3):227. doi: 10.5210/ojphi.v5i3.4847. http://europepmc.org/abstract/MED/24678380 .ojphi-05-e227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Steele Gray C, Barnsley J, Gagnon D, Belzile L, Kenealy T, Shaw J, Sheridan N, Wodchis WP. Using information communication technology in models of integrated community-based primary health care: exploring ICT in the iCOACH study. Int J Integr Care. 2017 Oct 17;17(5):144. doi: 10.5334/ijic.3452. [DOI] [Google Scholar]
- 66.Østensen E, Bragstad LK, Hardiker NR, Hellesø R. Nurses' information practice in municipal health care-A web-like landscape. J Clin Nurs. 2019 Jul 23;28(13-14):2706–16. doi: 10.1111/jocn.14873. [DOI] [PubMed] [Google Scholar]
- 67.Remen VM, Grimsmo A. Closing information gaps with shared electronic patient summaries: how much will it matter? Int J Med Inform. 2011 Nov;80(11):775–81. doi: 10.1016/j.ijmedinf.2011.08.008.S1386-5056(11)00172-9 [DOI] [PubMed] [Google Scholar]
- 68.Eikey EV, Murphy AR, Reddy MC, Xu H. Designing for privacy management in hospitals: understanding the gap between user activities and IT staff's understandings. Int J Med Inform. 2015 Dec;84(12):1065–75. doi: 10.1016/j.ijmedinf.2015.09.006.S1386-5056(15)30041-1 [DOI] [PubMed] [Google Scholar]
- 69.Shemilt K, Morecroft CW, Ford JL, Mackridge AJ, Green C. Inpatient prescribing systems used in NHS Acute Trusts across England: a managerial perspective. Eur J Hosp Pharm. 2017 Jul 30;24(4):213–7. doi: 10.1136/ejhpharm-2016-000905. https://ejhp.bmj.com/lookup/pmidlookup?view=long&pmid=31156943 .ejhpharm-2016-000905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mamykina L, Vawdrey DK, Stetson PD, Zheng K, Hripcsak G. Clinical documentation: composition or synthesis? J Am Med Inform Assoc. 2012 Nov 01;19(6):1025–31. doi: 10.1136/amiajnl-2012-000901. http://europepmc.org/abstract/MED/22813762 .amiajnl-2012-000901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Collins SA, Fred M, Wilcox L, Vawdrey DK. Workarounds used by nurses to overcome design constraints of electronic health records. Proceedings of the 11th International Congress on Nursing Informatics; International Congress in Nursing Informatics; June 23-27, 2012; Montreal, Canada. 2012. http://europepmc.org/abstract/MED/24199061 . [PMC free article] [PubMed] [Google Scholar]
- 72.Stanhope V, Matthews EB. Delivering person-centered care with an electronic health record. BMC Med Inform Decis Mak. 2019 Aug 22;19(1):168. doi: 10.1186/s12911-019-0897-6. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-019-0897-6 .10.1186/s12911-019-0897-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Swinglehurst D, Greenhalgh T. Caring for the patient, caring for the record: an ethnographic study of 'back office' work in upholding quality of care in general practice. BMC Health Serv Res. 2015 Apr 23;15(1):177. doi: 10.1186/s12913-015-0774-7. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0774-7 .10.1186/s12913-015-0774-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Friedman A, Crosson JC, Howard J, Clark EC, Pellerano M, Karsh B, Crabtree B, Jaén CR, Cohen DJ. A typology of electronic health record workarounds in small-to-medium size primary care practices. J Am Med Inform Assoc. 2014 Feb 01;21(e1):78–83. doi: 10.1136/amiajnl-2013-001686. http://europepmc.org/abstract/MED/23904322 .amiajnl-2013-001686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Campbell AN, McCarty D, Rieckmann T, McNeely J, Rotrosen J, Wu L, Bart G. Interpretation and integration of the federal substance use privacy protection rule in integrated health systems: a qualitative analysis. J Subst Abuse Treat. 2019 Feb;97:41–6. doi: 10.1016/j.jsat.2018.11.005. http://europepmc.org/abstract/MED/30577898 .S0740-5472(18)30216-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bramble JD, Abbott AA, Fuji KT, Paschal KA, Siracuse MV, Galt K. Patient safety perspectives of providers and nurses: the experience of a rural ambulatory care practice using an EHR with E-prescribing. J Rural Health. 2013 Mar 12;29(4):383–91. doi: 10.1111/jrh.12015. [DOI] [PubMed] [Google Scholar]
- 77.Kandaswamy S, Hettinger A, Hoffman D, Ratwani R, Marquard J. Communication through the electronic health record: frequency and implications of free text orders. JAMIA Open. 2020 Jul;3(2):154–9. doi: 10.1093/jamiaopen/ooaa020. http://europepmc.org/abstract/MED/32734153 .ooaa020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fraczkowski D, Matson J, Lopez KD. Nurse workarounds in the electronic health record: an integrative review. J Am Med Inform Assoc. 2020 Jul 01;27(7):1149–65. doi: 10.1093/jamia/ocaa050. http://europepmc.org/abstract/MED/32651588 .5870050 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Descriptive data template that was captured per included study.
Analytic frame with workaround-related data captured per study.


