Introduction
Chronic renal failure, progressing to the irreversible condition of ESKD, requires efficient RRT, typically dialysis or kidney transplantation (1). Compared with dialysis, kidney transplantation significantly benefits the survival and quality of life of ESKD patients and carries less of a burden. This minireview summarizes the development of kidney transplantation in China in recent years. In addition, we briefly introduce the human organ sharing system in China, which helps achieve justifiable, fair, and transparent organ allocation.
History of Kidney Transplantation in China
Organ transplantation is one of the most outstanding medical achievements in the last century. In China, the first kidney transplant was performed in Beijing in 1960. In 1972, the first living-related donor kidney transplant succeeded in Guangzhou. In recent years, with the development of transplantation technology and immunosuppressive protocols, we have continued to carry out complicated operations, such as pancreas–kidney combined transplantation, ABO-incompatible living-related donor kidney transplantation, and combined partial auxiliary liver and kidney transplantation.
Organ Donation and Allocation
We have established an ethical organ donation and transplantation system under the World Health Organization principles. Only deceased donors and living-related kidney transplants are performed in China; there have been no living-unrelated donors. For pre-emptive transplantation, a small number of trials have been carried out, but no protocols have been developed. Donation and allocation activities are firmly monitored and regulated under national laws. Informed voluntary organ donation by citizens is the only source of organ transplantation in China. The donated organs are allocated by a computer system called the China Organ Transplant Response System (COTRS) in an autonomous way (2,3). The quality of every kidney transplant program across mainland China is supervised and inspected by the kidney transplantation quality control center, and outcomes that are based on the original transplant recipient’s clinical data are monitored.
Epidemiology of Kidney Transplantation
According to the China Kidney Disease Network (CK-NET), there are approximately 132.3 million people in China with chronic kidney disease and 2.8 million people receiving RRT for ESKD (4,5).
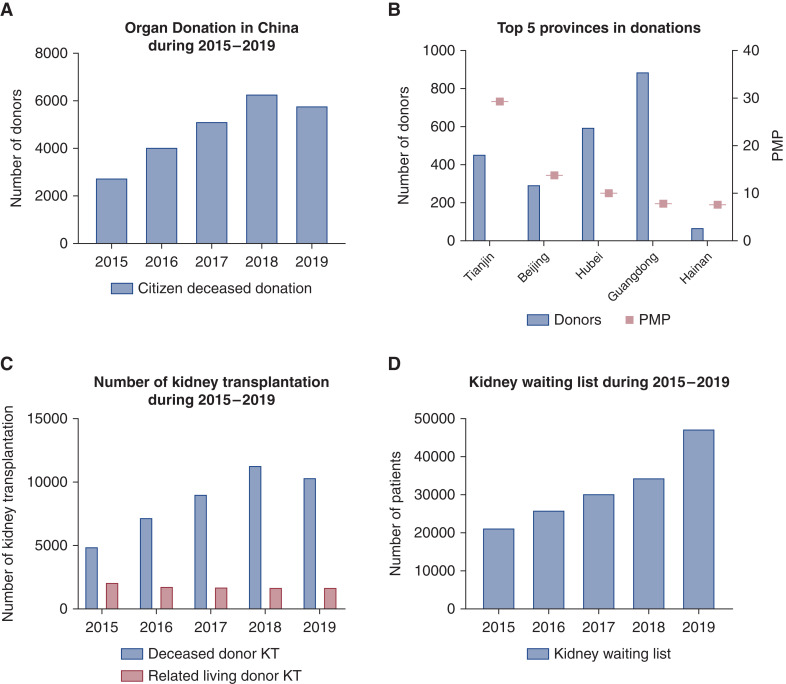
Kidney transplantation is the most efficient RRT for ESKD patients. The number of organ transplant operations and organ donations reached second place globally in 2019. During the period 2015–2019, China completed 2766 (2.01 per million people, [PMP]), 4080 (2.98 PMP), 5146 (23.72 PMP), 6302 (4.53 PMP), and 5818 (4.16 PMP) cases, respectively, of deceased organ donation (Figure 1A). The national target exceeds 15,000 donors per year. Twelve provinces exceeded the national level of PMP (Figure 1B). Cerebrovascular accidents and trauma were the two top causes of donor death, accounting for 45.30% and 41.52%, respectively. We also performed 4931, 7224, 9040, 11,302, and 10,389 cases of deceased donor (DD) kidney transplantation and 2109, 1795, 1753, 1727, and 1735 cases of living-related donor kidney transplantation in the past 5 years, respectively (Figure 1C). In 2019, there were 224 cases of kidney-related multiple-organ transplantations in China. Sixty-eight underwent combined liver–kidney transplantation, 149 were combined pancreas–kidney transplantations, and seven were combined heart–kidney transplantations, which increased 45.5% compared with the number in 2018 (3).
Figure 1.
The epidemiology of kidney transplantation in China. (A) The citizen deceased donations in China during the period 2015–2019. (B) The top five provinces in donations per million population. (C) The number of deceased donors and living-related donor kidney transplantations during the period 2015– 2019. (D) The numbers of patients on the kidney waiting list during the period 2015–2019.
The number of kidney transplantation candidates has increased every year. By the end of 2019, 47,382 (33.89 PMP) patients were waiting for kidney transplantation (Figure 1D). Factors contributing to the small percentage of dialysis patients in China waitlisted for transplant include patients disinterested in a transplant due to a fear of surgery or a lack of adequate financial resources. The prioritized receivers include immediate family members of deceased donors, volunteers who have been registered to donate for more than 3 years, living-related organ donors, children under 18 years old, and highly sensitized patients (panel reactive antibodies [PRA] ≥80%).
Quality and Safety of Kidney Transplantation
With improved kidney transplant surgery technology, immunosuppressive programs, and perioperative management, the kidney transplantation survival rate and 1-year complications in China have reached advanced international levels. The basic information on kidney transplantation in 2019 is shown in Table 1. From 2015 to 2019, there were 52,005 cases of kidney transplantation in China. A survival analysis for DD kidney transplantation indicated that the 1-year survival rate after operation was 97.8% (recipient)/95.7% (graft kidney) and that the 3-year survival rate was 96.9% (recipient)/93.3% (graft kidney). In addition, living-related kidney donor transplantation had a better survival rate, which was 99.4% (recipient)/98.8% (graft kidney) at 1 year and 98.9% (recipient)/97.0% (graft kidney) at 3 years (Table 1) (3). Graft loss included primary nonfunction 3 months or more after surgery and resumed dialysis 1 month or more after surgery. Among them, the 1- and 3-year survival rates of DD kidney transplantation were better than the international average for the same period (less than 90% and approximately 86%) (6). However, the long-term survival rate still needs more years of data accumulation.
Table 1.
Quality and safety of kidney transplantation
| Item | Value |
|---|---|
| General information | |
| Recipient age, yr | 40.1±12.1 |
| Dialysis time, mo | 25.7±29.2 |
| Recipient blood type, proportion (%) | |
| A | 30.0 |
| B | 26.8 |
| AB | 9.0 |
| O | 34.2 |
| Gender, proportion (%) | |
| Male | 70.6 |
| Female | 29.4 |
| Survival Rate | 1 Year | 3 Years | ||
|---|---|---|---|---|
| Recipient, % | Allograft, % | Recipient, % | Allograft, % | |
| Deceased donor | 97.8 | 95.7 | 96.9 | 93.3 |
| Living-related donor | 99.4 | 98.8 | 98.9 | 97.0 |
| Deceased Donor | Living-Related Donor | |
|---|---|---|
| Complications, 1 yr | ||
| DGF, % | 8.7 | 1.3 |
| Acute rejection, % | 3.1 | 3.2 |
| Infection, % | 5.9 | 3.7 |
| Graft loss, % | 4.3 | 1.2 |
| Ischemia time | ||
| Warm ischemia time, min | 8.7±7.4 | 3.7±3.3 |
| Cold ischemia time, h | 5.8±3.8 | 1.9±1.3 |
The information on the quality and safety of kidney transplantation in China is listed in the table. The recipient age, dialysis time, and the ischemia time are recorded by mean ± SD. The four most frequent complications are shown in the following table. The survival rate data were analyzed from 2015 to 2019, and the long-term survival rate still needs more years of data accumulation.
Kidney transplantation surgery in China is mostly performed by urologists or transplant surgeons. In some transplant centers, surgery is performed by a nephrologist. To obtain a more complete understanding of the patient's condition, most transplant surgeons provide post-transplant care, but in some centers, postoperative care is transferred to a transplant nephrologist.
The main complications after kidney transplantation include delayed graft function (DGF), acute rejection, and severe infection. DGF was defined as the recipient receiving dialysis treatment within 1 week post transplantation or failing to decline less than 400 µmol/L within 1 week after surgery. Our retrospective analysis of complications was conducted in 2019 and indicated that kidneys from donors who suffered brain death or circulatory death have a higher DGF rate than kidneys from living-related donors (8.7% to 1.3%); there was no significant difference between acute rejection or severe infection.
Ischemia-reperfusion injury is one of the main factors affecting the allograft function and survival time of transplanted kidneys. The cold/warm ischemia time is an important indicator of kidney transplantation success. Reducing the ischemic time of the living-related donor kidney is relatively easy, and problems can be solved by optimizing the surgical technique and the connection between the donor and recipient surgeries. For the deceased donor, the donation management center has established a “green channel” for organ transport to prioritize allocated organs and improve transport efficiency, successfully reducing the cold ischemia time of organs. Briefly, the green channel is a systemic coordination, including tests for human leukocyte antigen phenotype, pairing local suitable patients (in the order of the same hospital, the organ procurement organization, joint hospitals, province, and country). Also, the vehicles and flights transporting organs have priority.
In 2019, the warm/cold ischemia times of deceased donors were 8.7±7.4 minutes and 5.8±3.8 hours, respectively, while the 98.5% cold ischemia time of the kidney was less than 24 hours (3).
The Kidney Transplantation Quality Control Center of the Chinese National Health Commission was set up to monitor and promote national kidney transplantation-associated medical quality. Through scientifically assessing and monitoring the medical quality of each kidney transplantation program and introducing evidence-based practice guidelines and norms, this program aimed to promote kidney transplantation quality throughout China in a sustained way.
Perioperative Care
Routine preoperative preparations and preoperative examinations for kidney transplantation are the same as general surgery, but additional immunosuppressants are required. In most centers, widely used triple immunosuppression and induction protocols are followed. Commonly used immune induction medications are anti-lymphocyte immunoglobulin (for sensitized recipients) or CD25 monoclonal antibodies. Currently, we rarely perform kidney transplantation without antibody induction for safety purposes, except for some special patients, such as those who received a splenectomy for other reasons. Postoperative maintenance immunosuppressants typically involve the use of calcineurin inhibitors combined with mycophenolic acid and glucocorticoids (7). Some centers are trying new immunosuppressive programs, such as rituximab (8). Some experimental methods, such as gut microbiota, are also undergoing preclinical research (9).
The hospital stay of kidney transplantation patients can vary from 1 week to more than 1 month, mainly depending on complications. Generally, patients with no complications can be discharged 10 days after surgery because the risk of acute rejection has gradually decreased. Patients with DGF may stay more than 1 month until the recovery of kidney function without dialysis. A study involving 303 kidney transplant recipients showed that hospital stays of 7–14 days in the hospital accounted for 33%, with a median of 16 days. In cases of complications such as DGF or acute rejection, the stay date may increase to more than 1 month until the recipient stops dialysis. Recently, enhanced recovery after surgery has also shortened hospital stays by approximately 2–4 days.
Financing and Medical Insurance Policies
RRT is a long-term and expensive treatment. Taking Guangzhou as an example, the first-year cost of kidney transplantation is approximately US$21,027 (95% confidence interval [95% CI], US$17,427 to 23,519), including surgery, medication, and other charges, while for the second year it is approximately US$14,241 (95% CI, US$9344 to 15,592). These costs still carry a considerable burden for some patients. So, the Urban Employee-based Basic Medical Insurance and Urban Resident-based Basic Medical Insurance, the national social insurance programs that cover over 90% of citizens in some cities, can pay for part of the treatment costs including the surgery and lifelong immunosuppressants (as in Guangzhou). In these cities, the out-of-pocket expenses are approximately 20% of total costs (10).
Future Challenges
The shortage of donors is a global problem in transplantation. Improving organ donation and the utilization of donated organs is a primary goal of transplantation. In addition, transplant complications such as infection and rejection have severely affected the long-term survival of allografts and recipients. Therefore, attention should be given to the research of hotspots for kidney transplantation and the reinforcement of basic research into organ protection and immunology. Promoting kidney donation and transplantation while focusing on expanding the quantity of surgeries is necessary to achieve a high-quality, efficient transplant program.
Disclosures
All authors have nothing to disclose.
Funding
Z. Zhang received support from the National Natural Science Foundation of China (NSFC) grant number 82000711.
Acknowledgments
The clinical and epidemiological data in this review is partly quoted from the “Report on Organ Transplantation Development in China (2019)”. We would like to express our highest gratitude to the editor-in-chief of this book, Professor Huang Jiefu, and the editorial committee, China Organ Transplantation Development Foundation.
The content of this article reflects the personal experience and views of the author(s) and should not be considered medical advice or recommendation. The content does not reflect the views or opinions of the American Society of Nephrology (ASN) or Kidney360. Responsibility for the information and views expressed herein lies entirely with the author(s).
Author Contributions
Z. Zhang and Z. Liu wrote the original draft. Z. Zhang and B. Shi reviewed and edited the manuscript.
References
- 1.Ison MG, Grossi P; AST Infectious Diseases Community of Practice : Donor-derived infections in solid organ transplantation. Am J Transplant 13: 22–30, 2013. 10.1111/ajt.12095 [DOI] [PubMed] [Google Scholar]
- 2.Shi BY, Liu ZJ, Yu T: Development of the organ donation and transplantation system in China. Chin Med J (Engl) 133: 760–765, 2020. 10.1097/CM9.0000000000000779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang JF: Report on Organ Transplantation Development in China (2019), Beijing, China, Tsinghua University Press, 2020 [Google Scholar]
- 4.GBD Chronic Kidney Disease Collaboration : Global, regional, and national burden of chronic kidney disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 395: 709–733, 2020. 10.1016/S0140-6736(20)30045-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang C, Gao B, Zhao X, Su Z, Sun X, Wang HY, Zhang P, Wang R, Liu J, Tang W, Zhang D, Chu H, Wang J, Wang F, Wang S, Zuo L, Wang Y, Yu F, Wang H, Zhang L, Zhang H, Yang L, Chen J, Zhao MH: Executive summary for China Kidney Disease Network (CK-NET) 2016 Annual Data Report. Kidney Int 98: 1419–1423, 2020. 10.1016/j.kint.2020.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, Castro S, Foutz J, Wainright JL, Snyder JJ, Kasiske BL, Israni AK: OPTN/SRTR 2018 Annual Data Report: Kidney. Am J Transplant 20: 20–130, 2020. 10.1111/ajt.15672 [DOI] [PubMed] [Google Scholar]
- 7.Fu Q, Zhang H, Nie W, Deng R, Li J, Xiong Y, Dai Y, Liu L, Yuan X, He X, Wang C: Risk factors for acute rejection after deceased donor kidney transplantation in China. Transplant Proc 50: 2465–2468, 2018. 10.1016/j.transproceed.2018.03.063 [DOI] [PubMed] [Google Scholar]
- 8.Cen M, Wang R, Kong W, Deng H, Lei W, Chen J: ABO-incompatible living kidney transplantation. Clin Transplant 34: e14050, 2020. 10.1111/ctr.14050 [DOI] [PubMed] [Google Scholar]
- 9.Zhang Z, Liu L, Tang H, Jiao W, Zeng S, Xu Y, Zhang Q, Sun Z, Mukherjee A, Zhang X, Hu X: Immunosuppressive effect of the gut microbiome altered by high-dose tacrolimus in mice. Am J Transplant 18: 1646–1656, 2018. 10.1111/ajt.14661 [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Zhang C, Zhu S, Ye H, Zhang D: Direct medical costs of end-stage kidney disease and renal replacement therapy: A cohort study in Guangzhou City, southern China. BMC Health Serv Res 20: 122, 2020. 10.1186/s12913-020-4960-x [DOI] [PMC free article] [PubMed] [Google Scholar]