Abstract
Emotional regulation is important for mental health and behavioral regulation. A relevant precursor to emotional regulation may involve identification of one’s emotions. Here, we propose a model of seven components that may provide a foundation for emotion identification. These factors include baseline mood, monitoring, physiological responses, interoception, past personal experiences regarding emotions/metacognition, context, and labeling. We additionally examine how deficits in different components may contribute to the concept of alexithymia, which is defined by difficulty identifying and describing one’s own emotions. Ultimately, we explore how the model may support a relationship between specific psychiatric disorders and alexithymia. The proposed model may help explain emotional identification impairment in multiple psychiatric disorders and guide future research and treatment development efforts.
Keywords: Emotions, emotional intelligence, alexithymia, emotional identification, emotional regulation
Introduction
Developing an understanding of one’s emotions is important in current definitions of mental health (Galderisi et al., 2015). Emotional intelligence is a key component of resilience (Salovey, 1990), and understanding of one’s own emotions (intrapersonal emotional intelligence) contributes to overall well-being and effective emotional regulation (Mayer, 2004).
To begin, we offer definitions for some terms we will use in this manuscript. We define emotion identification as the ability or tendency to recognize feelings. The goal of the proposed model is to provide a comprehensive account of the different processes by which an individual arrives at the realization of which emotions they are feeling. This is similar to, but distinct from, the previously examined concept of emotion categorization, which is the process by which an individual may discriminate and classify one feeling from another. Identification in the context of this review specifically refers to recognition of the emotion one is currently feeling in the moment, and may be independent of comparisons to other emotions. Another concept is emotion perception, which we define as the ability or tendency to recognize and identify the subjective feelings of others. In this article, we focus specifically on the ability or tendency to identify one’s own emotions, although future work may determine if emotional identification is necessary for accurate emotional perception. Emotional understanding refers to a grasp of the potential causes, natures, and control of feelings (Viana et al., 2020), and may be informed by intact identification of one’s own emotions. Further, emotional intelligence refers to a general understanding of one’s own feelings and how to manage them (Mayer, 1997), which we assert is influenced by emotion identification. Additionally, we assert that emotion identification is separate from emotional regulation, and occurs before steps related to emotional regulation. Emotional regulation is the process by which individuals may control their own feelings (Gross, 2015), and different strategies may be utilized by individuals to do so, including emotional reappraisal and emotional suppression (Gross and John, 2003). Emotional reappraisal involves changing the way one thinks about feelings, and emotional suppression involves actively inhibiting one’s responses. In our model, both processes may occur after an emotion is initially identified, making correct emotional identification necessary for proper emotional regulation.
We emphasize the importance of emotional identification as we assert that identification is important for proper emotional regulation. Considerable work has focused on understanding emotion-regulation strategies with an eye toward developing more effective treatments for mental illnesses. Cognitive behavioral therapy (CBT), an empirically validated treatment for multiple psychiatric disorders (Butler et al., 2006), teaches individuals to re-frame thinking about negative emotions and experiences as a strategy for emotion regulation. Similarly, emotional intelligence has been proposed to consist of four major components within an ability model of emotional intelligence: emotion perception, regulation, understanding, and utilization (Ciarrochi et al., 2000; Mayer, 1997). Emotional intelligence is measurable in the laboratory (Mayer et al., 2003) and associated with success in different areas of one’s life (Brackett, 2011). It is also associated with resilience to mental illness (Armstrong et al., 2011). Taken together, the previously cited work emphasizes the importance of understanding and regulating one’s own emotions. However, successful regulation of emotion may optimally begin with accurate identification of emotions (Morie et al., 2020; Sheppes et al., 2015).
Individuals who have significant difficulties identifying or naming emotions they are feeling may experience more confusion, and ultimately distress, upon feeling negative emotions. Difficulties identifying emotions or that one’s physiological responses may be related to emotions and not to health or external factors may increase distress and preclude individuals from applying beneficial emotional regulation strategies. Incorrect identification of an emotion may influence individuals to use maladaptive regulation strategies, such as suppressing (Goldin et al., 2008) or avoiding emotions (Venta et al., 2013) rather than reappraising emotion in a healthier manner. In addition, many therapies, including CBT, rely on individuals reappraising emotions, or discussing how they feel with therapists (Gaudiano, 2006). If individuals cannot identify their emotions or accurately label them, treatment may be more difficult and less efficacious. This notion is supported by poorer treatment outcomes of individuals with alexithymia, a major factor of which is difficulties identifying emotions (Grabe et al., 2008). Independent of treatment, if individuals cannot identify their feelings, then emotional regulation may become more difficult (Pandey, 2011). In this manuscript, we explore the concept of emotional identification, develop a model of how it may operate in a step-wise fashion, and consider how difficulties in emotional identification may operate transdiagnostically in major mental illnesses. We focus on alexithymia as a clinical example of how emotional identification may fail and how the proposed model may contribute to difficulties experienced by individuals with alexithymia.
Developing understanding of one’s emotions relies on identification of those emotions and may be a necessary step before emotional regulation can be enacted. We begin this review and exploration of a proposed model of emotional identification by considering previous models that have addressed the definition of emotions, including related processes of emotional categorization. We identify some commonalities across these models. We then propose a model, which outlines the processes by which individuals may identify their emotions, building upon prior work. From there, we explore how lapses in elements of the model may impact emotion identification and ultimately mental health, framing considerations with respect to alexithymia.
Definitions of emotion
Different theories include various conceptualizations of emotion. One set of theories proposes emotions as discrete, measurable concepts with a neurophysiological basis, that can exist independently of context or experience with that emotion. Emotions like joy, sadness, and fear are often examples used, with a definition of these emotions as a type of “natural kind” of emotion with specific neural and physiological correlates (Charland, 1995). Other theories describe emotions as emotional schemas which are biologically based and cannot be learned but heavily influence all forms of cognition and behavior when they are “activated” (Izard, 2007; Izard et al., 1993).
However, more recent theories concerning emotional experiences have arguably moved away from this view of discrete emotions and emotion schemas, considering other influences. These theories have examined the understanding of emotions as being dependent on cognition and context. Appraisal theories (Ellsworth, 2003; Scherer, 2000) emphasize the importance of how one interprets one’s feelings to arrive at an emotion, describing emotions as “patterns of perception, and interpretation, and their correlates in the peripheral and nervous system.” Appraisal theories stand in apparent contrast to theories of discrete emotion, that posit the existence of established, measurable, and predictable emotional responses. Appraisal theories, on the other hand, posit that emotions are continuous and constantly changing, with updates dependent upon behavioral responses and consequences of those responses (Moors et al., 2013).
A model by Lisa Barrett extends the appraisal theory, positing that emotions do not exist on their own, but rather only exist when categorized or identified by the person experiencing that emotion. In this model, individuals categorize their emotions using core affect, valuation, conceptual knowledge of emotion, context, internal models of emotion, and language (Barrett, 2006). Emotion is proposed to be a concept that should be understood holistically (Barrett, 2017). This model puts forth the idea that perception of emotion can be influenced by the social reality and culture in which a person was raised, with emotional concepts built from an individual’s cultural experiences (Gendron et al., 2014). This model emphasizes that the reality of an emotion is how the person experiencing the emotion perceives it, and is heavily influenced by the social context surrounding that emotion.
The importance of perception of emotion suggests that regulation of emotion may play a role in the ultimate emotional experience. Models exist that seem to consider emotion identification as part of emotional regulation. James Gross (Gross, 2015) described an emotion-regulation model containing three major stages: identification of the emotion, selection of the strategy to regulate the emotion, and implementation of that strategy (perception, valuation, and action steps). Some previous models suggest that emotions may be categorized differently on the basis of emotional regulation; that is, regulation may operate before an emotion is identified and influence how an individual identifies that emotion (Frijda, 2009; Scherer, 2019). However, the proposed model focuses expressly on emotion identification, a step prior to regulation in the Gross model. While affect may exist as a starting point for the eventual emotion to be identified, with mood contributing or influencing, and emotions may be frequently changing and identification of one may rely on identification of another, the proposed model focuses upon identification of an emotion given its proximal temporal location with respect to ultimate regulation. The theory of mentalized affectivity described by Jurist (Greenberg et al., 2017), one that encompasses emotional identification, processing of emotion, and emotion expression, suggests that emotion identification is an important aspect of emotional regulation. Here, we suggest that initial identification of what an individual is feeling is an important first step before beneficial emotional regulation may begin. While some theories, such as those cited above, may assert that elements of regulation contribute before complete emotion identification occurs, our assertion is that strategies that may operate before emotion identification is complete would consist of maladaptive strategies such as suppression or avoidance. For beneficial strategies such as cognitive reappraisal, intact emotional identification is important, and the proposed model focuses upon steps leading to identification of an emotion (Barrett, 2006; Greenberg et al., 2017; Gross, 2015). Questions raised from this background and seeming consensus in the literature that emotions are dependent on individual perception are thus twofold. What steps, tendencies and abilities do individuals use to perceive their emotions? And further, what sort of troubles arise when certain steps fail? Although this model is similar to previous models, and has similar aspects to models including use of physiological states as found in discrete models of emotion and has much in common with the Barrett model of constructed emotion, there are unique aspects. The steps in the model are independent yet interacting, and consist of both automatic and cognitive processes. The model asserts that identification is necessary before proper regulation can occur, which differs from other models (Greenberg et al., 2017; Gross, 2015) that tend to use regulation as part of the emotional experience. Our model asserts that proper use of the steps in the model can result in more accurate emotion identification, that emotions can be identified more accurately and that this accuracy can contribute to more beneficial regulation strategies, and thus emotion identification can be considered an aspect of emotional intelligence. The model additionally implements monitoring and interoception as key steps, which are not explored in some other models (Barrett, 2006), processes that we assert are important for emotional identification. Further, we assert that difficulties or deficiencies in these steps have ramifications for alexithymia and mental health in predictable, testable ways.
Alexithymia
Difficulties in emotion identification are reflected in alexithymia. Alexithymia, which translates to “no words for emotions” (Taylor, 1984), is characterized by difficulties identifying and describing emotions and an externalized coping style (Parker, 2003). Alexithymia is theorized as a potential personality dimension (Luminet et al., 2021b) with potential repercussions for all stages of emotional regulation (Luminet et al., 2021a), though here we focus upon its interaction with emotion identification and ramifications for mental illnesses.
Alexithymia is associated with multiple mental illnesses, including depression (Wise et al., 1990), anxiety disorders (Karukivi et al., 2010), substance use disorders (Bruce et al., 2012; Cecero and Holmstrom, 1997; de Haan et al., 2014; de Timary et al., 2008; Pombo, 2014) gambling disorder (Lumley and Roby, 1995), eating disorders (Taylor et al., 1996), psychosomatic disorders (Lundh and Simonsson-Sarnecki, 2001), and autism (Poquerusse et al., 2018; Szatmari et al., 2008). Impairments in particular components of the proposed model may not only underlie different aspects of alexithymia, but also have ramifications for different mental illnesses.
Three factors of alexithymia have been identified with the Toronto Alexithymia Scale (TAS-20), the most commonly used measure of alexithymia (Parker, 2003). These factors are difficulty identifying emotion, difficulty describing emotion, and an externalizing coping style. Difficulty with particular stages in the emotional identification model we present may result in alexithymia through different processes and may relate to each identified factor of alexithymia.
Here, we propose a model of the processes that lead to identification of emotions. We first present the model, which contains seven components. We then expand upon each stage, linking each to existing literature on emotion. We then discuss the model’s ramifications for the concept of alexithymia. Finally, we suggest future directions for research using the model. This model aims to establish how emotion identification may be achieved, providing an enhanced framework for the development of therapies that may target alexithymia in order to improve treatment efficacy.
Components of the emotion identification model
We propose seven components of the model for identifying and labeling emotions. Some of these concepts have been introduced in previous models, and we further elaborate on these and how they may interact with other steps we propose as individuals arrive at the labels for their current emotion. We introduce each concept in brief before expanding upon them.
We propose a first component of baseline mood. The definition of mood in this context is different than emotion, which is the perception of a feeling, and is similar to the concept of core affect in the Barrett model (Barrett, 2017). The second component is monitoring. This involves a stimulus that may or may not elicit the emotion and may be internally or externally generated. This stimulus may result in a feedback response that is different from the ongoing mood, the detection of which is dependent on monitoring tendencies or abilities. This concept of monitoring is somewhat similar to the previously introduced concept of valuation, which takes into account the “badness or goodness” of a stimulus. The monitoring we propose here encompasses the negative or positive valence of the stimulus, and is reliant on intact cognitive control. The third concept introduced into the proposed model is the physiological response, referring to the physical manifestation of emotional responses, as theories of discrete emotion have suggested these may be predictable responses. Physiological response would next be interpreted using the fourth concept of the proposed model, which is interoception, the active recognition and analysis of the physiological state. The fifth concept is metacognitive processing of the perceived physical state, comparing these sensations to previous experiences of these sensations, which we designate as metacognition. This is similar to the conceptual knowledge of emotion and the internal models of emotion described previously (Agnes Moors, 2013; Ellsworth, 2003; Moors et al., 2013; Scherer, 2005, 2019). Individuals also use context to identify what they are feeling, where information is used from the current experience to frame emotion. Finally, an individual may then use all of these factors to label their emotional experience, which is the final component and is dependent on naming approaches and abilities.
The model here expands upon the Barrett model (Barrett, 2017). The Barrett model encompasses some similar steps, although it does not include the important aspects of monitoring capability/tendencies and interoception, which we assert are important aspects of emotion identification. The Barrett model describes emotions as reliant on individual experiences, and experiences inform concepts of emotions. Here, we seek to expand upon the steps individuals use to determine how to emotionally label those experiences and investigate the processes by which individuals form these concepts. We further expand upon some of the concepts introduced in the Barrett Model, such as valuation, context and internal models of emotion, and additionally explore concepts related to emotional awareness such as physiological responses and interoception. Finally, we make predictions related to mental illnesses based upon components of the model, constructing testable hypotheses for future work related to mental health that may ultimately inform clinical care. Many evidence-based mental health treatments, such as CBT, offer training in how to change one’s thoughts and address one’s emotions. Understanding individuals’ emotional intelligence, and further understanding what may be limiting or influencing how individuals may be identifying their emotions, could potentially inform patient-specific care, help with the development of different therapies such as emotional awareness therapy (Burger et al., 2016) and improve treatments of different mental illnesses. Understanding how each component relates to alexithymia may also help to explain how alexithymia contributes to mental illnesses. From here, we explore each proposed component that underlies emotion identification in more detail. We then consider how each component may contribute to the process of emotion identification and mental health, and how deficits in specific components may contribute to alexithymia.
The components in our model are presented as independent, yet interacting processes, all of which combined may be used to arrive at an emotional label. Three of them are considered sensory-related or automatic processes, while the four remaining are considered cognitive processes. More or less weight placed on each component may result in different emotional labels, and poor abilities or tendencies to properly use one or more of them may result in alexithymic symptoms that may worsen mental health.
Mood (Automatic/sensory process)
Mood in this model refers to the present feeling an individual experiences. It is the baseline from which an emotion is derived once an internally or externally generated emotional stimulus occurs. Of course, mood is intrinsically theoretically intertwined with emotion. Mood may be influenced by one’s experiences and previous contexts (a frustrating day as opposed to a more relaxing one) and mental disorders, among other factors. Mood has genetic contributions (Luciano et al., 2012). Most people generally present with a relatively neutral mood, and mood may influence decision-making (Mayer et al., 1992). Mood itself may be influenced by awareness of one’s mood (Swinkels and Giuliano, 1995), linking it with emotion identification. A prime example is the influence of ruminating on negative mood, which may lead to further worsening depression and negative affect (Nolen-Hoeksema et al., 2008). Both emotion and mood may inform each other. Successive experiences of emotions and the future labeling of those emotions may circle back and inform individuals’ understandings of their own mood states. In turn, individuals’ mood states may influence emotions by serving as baselines by which emotions are measured. In this context, moods may be conceptualized as baseline states with which individuals approach situations. If individuals’ moods are highly positive, stimuli may more readily elicit positive emotions, whereas if individuals’ moods are negative, positive emotions may be harder to elicit. When a stimulus occurs, it may then trigger the next aspect of the proposed model.
Findings on alexithymia and mood mostly center around the well-known comorbidity of alexithymia and mood disorders, such as depression and anxiety (Hendryx et al., 1991; Honkalampi et al., 2000). Consistent failures to identify emotions accurately may trigger anxious moods, as a failure to recognize emotions continuously may circle back and influence persistent uncertainty. With depression, persistent avoidance of emotion due to alexithymia may contribute to anhedonia and depressed mood due to avoidance of positive reinforcers (Leventhal, 2008). As mood serves as the baseline in our model and is also influenced by labeling, alexithymia may create consistent uncertainty or perseverative mood cycles that are hard to escape.
Monitoring (Automatic/sensory process)
Monitoring in the proposed model refers to detection of changes relating to a stimulus eliciting a difference from the baseline mood. This detection may be achieved via “automatic” feedback processing systems that code violations or confirmations of heuristics and expectations (Bellebaum et al., 2010). This monitoring system operates in both emotional and non-emotional contexts in order to form predictions and monitor outcomes related to daily life and behaviors (Zubarev and Parkkonen, 2018). In the context of the model, when a stimulus occurs, monitoring is the capability or tendency by which a person recognizes that something has occurred that either is consistent with predictions or violates predictions, and is an important step in ultimately determining which emotion may best fit the prediction or prediction violation.
Electrophysiology studies in primates have indicated that dopamine neurons within the midbrain increase activity during reward receipt, whereas aversive feedback results in short-term inhibition of dopamine signaling (Schultz et al., 1997). In humans, electroencephalography (EEG) studies have implicated this system for feedback processing (Holroyd and Coles, 2002). This midbrain dopaminergic signaling indicates when an expectation is violated, perpetuating reward-based learning. When reward is received and midbrain dopaminergic signaling increases, an experience may be coded as positive or rewarding, whereas when dopaminergic signaling is decreased, it may be perceived as negative or punishing (Hajcak et al., 2006). When a stimulus occurs that generates a deviation from expectation, either positive or negative, feedback systems may detect it within a few hundred milliseconds, as can be seen via EEG (Hajcak et al., 2006; Hauser et al., 2014). During reward processing, sharp deviations from a baseline may underlie a perceived loss of reward (Cohen et al., 2007). Such signals may also indicate internally generated mistakes, as mistakes may indicate performance beneath expectations (Luu et al., 2003). Clinical studies suggest such events may rely on information about the stimulus, including timing and magnitude (van Noordt and Segalowitz, 2012). Responses may also rely on cognitive control (Ridderinkhof et al., 2004), processes served by prefrontal and orbitofrontal brain regions (MacDonald et al., 2000). Relevant to the proposed model, data suggest these processes are influenced by/ linked to mood states, even in non-emotional contexts. Individuals with depression show enhanced responses to negative feedback and to their own mistakes during performance of a monitoring task, even in non-emotional contexts (Tucker et al., 2003), and negative mood states (including in healthy individuals) have been associated with increased feedback responses (Santesso et al., 2012). Similar findings have been observed in relation to anxiety (Gu et al., 2010; Olvet and Hajcak, 2008).
In the proposed model, the direction of the deviation elicited by a stimulus, positive or negative, may help determine how someone may label an emotion the stimulus engenders. The magnitude of this deviation may also set the stage for the intensity of the emotion. A sharp, deep negative deviation in the setting of significant positive expectation may have long-lasting, intense emotional repercussions, as may the reverse. This would be consistent with findings related to hedonic contrast, which purports that preference for a positive stimulus is enhanced if such a stimulus is preceded by a less positive stimulus, or vice versa (Voichek and Novemsky, 2021; Zellner et al., 2003). In our model, positive stimuli would be perceived as more positive as the prediction violation would be greater in the case of negative prediction followed by positive feedback (or vice versa). This is consistent with findings related to automatic error detection in feedback-processing paradigms (Hauser et al., 2014), and demonstrates how mood states may influence monitoring capability (Maier et al., 2016; Olvet and Hajcak, 2009). Future studies that focus upon feedback processing and how it relates to mood, and if severe deviations may lead to longer-lasting mood states, will further inform understanding of these processes.
Uncertainty or poorer monitoring capabilities or tendencies may impair emotional identification. A reduced deviation, either due to ambiguous stimuli (e.g., being called to a meeting with a teacher/supervisor but not knowing why) or poorer monitoring tendencies or capabilities (e.g., having difficulties appreciating errors when they are made) may lead to greater uncertainty when applying emotional labels to experiences. In the latter case, poor monitoring may lead to individuals experiencing emotions without knowing why they are feeling the ways they are, as they may not be aware of the initial stimuli or changes that elicited those emotions. Intact self-monitoring capabilities have been associated with less stress and more effective emotional regulation (Bono and Vey, 2007). Future studies that focus upon feedback processing and how it relates to mood, and if severe deviations may lead to longer-lasting mood states, may further inform understanding of these processes. The proposed model would predict that monitoring deficits may contribute to alexithymia, but the literature on alexithymia and monitoring capabilities/tendencies is scarce. One study has examined if alexithymia contributes to monitoring during performance of emotional tasks, using an EEG task that utilized the error-related negativity (ERN), which is a marker of error monitoring. In non-alexithymic individuals, the ERN was enhanced in individuals during the emotional task, but not in those with alexithymia, potentially indicating difficulty using monitoring capabilities during emotional contexts in this group (Maier et al., 2016). More work in this vein is needed, and future work remains to be done on monitoring capability in non-emotional contexts in those with alexithymia.
Physiological state (Automatic/sensory process)
Another nearly instantaneous reaction to a stimulus, beginning just after the initial deviation, is the physiological response, which encompasses the physiological state piece of the proposed model. In 1884, William James said, “bodily changes follow directly the perception of the exciting fact, and that our feelings of the same changes as they occur IS the emotion” (Cannon, 1987). Physiological responses are arguably what most people consider when they try to define emotion. These physiological responses may be largely innate (Hariri et al., 2002) and may vary in intensity depending on factors such as family history of mood disorders (Waugh et al., 2012) or gender (Stoney et al., 1987).
The literature is mixed regarding which physiological states may link to specific emotions. Emotional classification theories have typically focused on how many emotions may be classified as different from another, and often rely on considerations regarding arousal (intensity) and valence (positive or negative). For example, the circumplex model of affect (Remmington et al., 2000) suggests that emotion may be represented by a physiological state that depends on arousal and valence. Few models explicitly link emotion classifications to physical states. However, Lovheim’s model (Lovheim, 2012) discusses the role of monoamine neurotransmitters (serotonin, dopamine, and norepinephrine) and how they may contribute to the classification of what may be considered eight basic emotions (anger, excitement, distress, surprise, fear, enjoyment, shame, contempt). Differences relating to the presence, location, concentration and other factors relating to these neurotransmitters may code for these emotions and their identification. Although the model has yet to be empirically tested, physiological states of an emotion may depend on specific neurotransmitters. Dopamine may code valence of an emotion, as described above, with additional dopamine release encoding the precursor to positive emotion and pauses in dopamine signaling encoding negative states. Norepinephrine and epinephrine, part of the hypothalamic-pituitary-adrenal (HPA) axis, may contribute significantly to intense emotional responses, and an “adrenaline rush” may be classified as being exciting (Slanger and Rudestam, 1997) or frightening (van Zijderveld et al., 1999). Evidence exists that certain physiological responses or hormone levels, such as cortisol, relate to emotional intelligence (Liu et al., 2019) and even emotional regulation (Langer et al., 2021). If physiological states are identical or similar for some emotions, then more information may be necessary for labeling them (Langer et al., 2021; Liu et al., 2019). Of course, for proper emotional identification, physiological states also need to be perceived by the individual experiencing them.
Alexithymia has been tested with respect to physiological states, and the literature has thus far been somewhat inconsistent. When examining physiological responses to odors, individuals with higher alexithymia showed altered physiological responses than did those with lower alexithymia (Cecchetto et al., 2017). In another study, those with alexithymia showed lower heart rates toward frightening images (Peasley-Miklus et al., 2016). However, other work examining anxiety and self-consciousness in those with alexithymia revealed that while physiological responses were indistinguishable, those with alexithymia reported more self-consciousness during a social stress task involving giving an impromptu speech (Eastabrook, 2013). Other work has also revealed no differences in physiological responses to emotional stimuli in those with alexithymia compared to those without (Stone and Nielson, 2001). These seemingly inconsistent findings may be explained in our model, as different pathways that underlie alexithymia may involve more cognitively-driven factors in identifying emotions in some individuals versus more physiologically-driven factors in others.
Interoception (Cognitive process)
Accurate awareness of physiological responses may constitute a vital aspect of identifying emotions. Perception of internal states involves interoception, which has been associated with emotional awareness (Craig, 2002) and insular function (Craig, 2009; Critchley et al., 2004). Interoception is also a key feature of the theory of constructed emotion (Barrett et al, 2017). One measure of interoceptive awareness is the heartbeat counting task (Wiens et al., 2000). Poor performance on this task is associated with depression (Terhaar et al., 2012) and anxiety (Domschke et al., 2010), and other disorders marked by interpersonal difficulties, such as autism (Garfinkel et al., 2016). The proposed model predicts that if people are not aware of their own physiological states, they may have limited insight into an important aspect of emotion identification. Poor awareness of the nuances of physiological responses complicates emotional labeling. This aspect of the proposed model resonates somewhat with the somatic marker theory, which postulates that individuals use bodily states as clues to the emotions they are feeling, such as interpreting a pounding heart as anxiety (Xu et al., 2020). Anti-anxiety medications such as beta-blockers may reduce anxiety by reducing the pounding heart sensation in individuals with panic disorder (Bachmann et al., 2011). In our model, however, we assert that proper interoception requires accurate interpretation of one’s own physiological responses, and an ideal amount of reliance on internal states. Over-reliance on physiological features may predispose to negative emotions, such as the aforementioned anxiety, while poor interoception may complicate identification and potentially predispose to anhedonia or flat affect common in depression.
Additional investigations of interoception have linked impairments in interoception to alexithymia. One prominent recent model of alexithymia involves a failure of interoception (Brewer et al., 2016; Murphy et al., 2018a). There is evidence linking alexithymia to interoception in different domains, including with a heartbeat counting task (Borhani et al., 2017; Murphy et al., 2018b). A poor ability to identify one’s physiological state would complicate identifying one’s emotion, as individuals with poor interoception may lack information gleaned from their physiological states. In the proposed model, alexithymia related to interoception would lead to an increased reliance on other components of the model.
Metacognition (Cognitive process)
History of one’s experience with different physiological states may highly inform emotional labels applied to such states. Once a label is applied to a physiological state and the same state is experienced again, this experience may lead to the emotion being labeled similarly. Metacognition is relevant to the proposed model as it influences recognition of one’s current state and comparison with previous experiences. Metacognition has been linked to emotional intelligence (Salovey, 1995). Mindfulness, the process of becoming aware of one’s emotions, is also linked to greater emotional well-being (Brown and Ryan, 2003). Other models of emotional perception also incorporate similar components, including the idea of concepts in the theory of constructed emotion, which are knowledge of emotional concepts derived from one’s experiences and culture (Barrett et al, 2017).
Metacognition is arguably less immediately relevant for individuals who have very little history with emotions, such as children and adolescents. They will likely have less history with certain states and thus may be less able to generate an informed emotional label based on experience. In addition, limited experience with physiological states and proper labels to apply to them may lead to greater uncertainty with regard to labeling emotions. This uncertainty may lead to emotions being more distressing and likely to be labeled as fear or anxiety. Consider, for example, how very young children more often react to uncertain or new experiences with fear and anxiety, such as in the strange situation task (Muris et al., 2001; Smith et al., 2016). In this context, they may rely on parents, caregivers and peers to give additional context with which to frame their emotions, emphasizing the importance of attachment (Chae et al., 2018). In addition, children will use social referencing, relying on their parent’s facial expressions to give context to situations, as early as 8–10 months of age (Walden and Ogan, 1988). Different instructional styles may have long-term consequences for how such experiences are framed and managed prospectively. The proposed model predicts that relative to adults, younger children and adolescents will have more difficulty accurately identifying their emotions. Impairment in metacognition related to emotion may lead to difficulties developing emotional intelligence related to emotional states, contributing to alexithymia. Indeed, among people who use substances, metacognitive difficulties have predicted alexithymic tendencies (Babaei et al., 2015). Alexithymic individuals have demonstrated difficulties in labeling emotions when presented with emotional faces (Rocha, 2016) and poorer memory for emotion (Donges and Suslow, 2015), suggesting that those who have poor knowledge of emotion histories present with alexithymia.
Context (Cognitive process)
Another important factor of the proposed model involves context. The details of stimuli, and situations surrounding stimuli, may frame how an individual identifies their emotion given a certain stimulus or scenario. Two physiological states involving crying may be identical on a behavioral level, but different contexts (e.g., funeral versus wedding) may influence the identified emotion related to that behavior (e.g., sadness versus happiness). We assert that while context relates in a cognitive manner to identification in our model, context does not refer to reappraisal or regulation processes, but instead to proper recognition of the external aspects of the emotional stimuli. This can occur very early in emotional processing. The importance of context has been demonstrated in laboratory settings when observers are asked to label an emotional expression (Hassin et al., 2013). Faces showing an identical expression may be labeled differently depending on context, and eye-movement data suggest this may happen at very early stages of processing (Aviezer et al., 2008). Work using EEG and the N170 evoked response potential (ERP) component, generated in the visual cortex even before recognition of the face has occurred (Eimer, 2000), has also suggested that responses to emotional faces are influenced by the contexts in the scenes in which they are presented (Righart and de Gelder, 2008). An ambiguous situation may also influence individuals’ identification of their own emotions, and context is one of multiple factors that may influence individuals’ labeling of emotions, as evidenced by use of context helping to resolve emotionally ambiguous faces (Bublatzky et al., 2020). Individuals with mental illness, such as depression, may not show typical reactions to emotional contexts that may be expected, such as showing limited happiness during a recounting of happy experiences (Rottenberg et al., 2005). This also emphasizes the importance of the baseline mood state, and illustrates how each of these components within the proposed model informs the other.
Alexithymia is often marked by a tendency to externalize focus or use an externally oriented coping style. Indeed, alexithymic individuals with externally oriented coping styles may focus intently on contexts in order to inform their emotions. They may describe what is happening in an emotional scene rather than focus on emotive components, as evidenced in a study in which individuals with alexithymia described a scene from an emotional movie using fewer emotional words (Luminet et al., 2004). Increased reliance on context may predispose individuals to alexithymia.
Labeling (Cognitive process)
A final proposed stage involves applying an emotional label. This final stage is a cognitive process that uses the application of verbal knowledge, which may also depend on metacognition, and benefits from a vocabulary for naming emotional states. Individuals with poor verbal intelligence tend to show poorer emotional identification perhaps by virtue of not having the correct words to apply. Individuals may have intact monitoring, interoceptive, and metacognitive abilities to inform the previous stages, but difficulties in applying proper labels due to poor naming ability may make discussion of emotions difficult, including within therapeutic settings. This stage is important in the development of emotional intelligence in children, where the label given by the child’s caregivers may frame their labeling of similar experiences in the future, and poor verbal or cognitive development may have ramifications for future identification and regulation of emotions (Karukivi et al., 2012). These findings relate importantly to alexithymia (Hobson et al., 2018; Lamberty and Holt, 1995). The very term alexithymia implies a deficit in describing and choosing words for emotions. Considering that difficulty identifying emotions may also influence abilities or tendencies to describe them, and these phenomena are often correlated, these relationships may also apply to the final stage, labeling. Labeling may relate to experiences and skills in naming that may reflect verbal abilities or tendencies. Individuals testing lower on verbal testing tend to score higher on alexithymia (Lamberty and Holt, 1995). Poor verbal testing in childhood may predict alexithymia later in life (Karukivi et al., 2012). Damage to language centers of the brain, including the temporal lobe and inferior frontal gyrus, may predict acquired alexithymia (Hobson et al., 2018). Alexithymia is also correlated negatively with verbal testing results in patients with traumatic brain injuries (Wood and Williams, 2007). A relationship between poorer verbal performance and alexithymia may not be surprising, but it underscores the importance of labeling in the proposed model. Intriguingly, when verbal intelligence was controlled, no difference was found in emotion recognition between those with high and low alexithymia (Montebarocci et al., 2011). It is possible that some individuals may present with alexithymia due to poor verbal ability but may in fact have intact ability to use other components of the model. Where labeling may become particularly problematic may be in communication with others. Such concerns may make therapy more difficult, suggesting that individuals, particularly those with alexithymia, may benefit from testing of verbal intelligence.
The Model
The proposed model of how components may interact during emotion identification is presented schematically (Figure 2).
Figure 2.
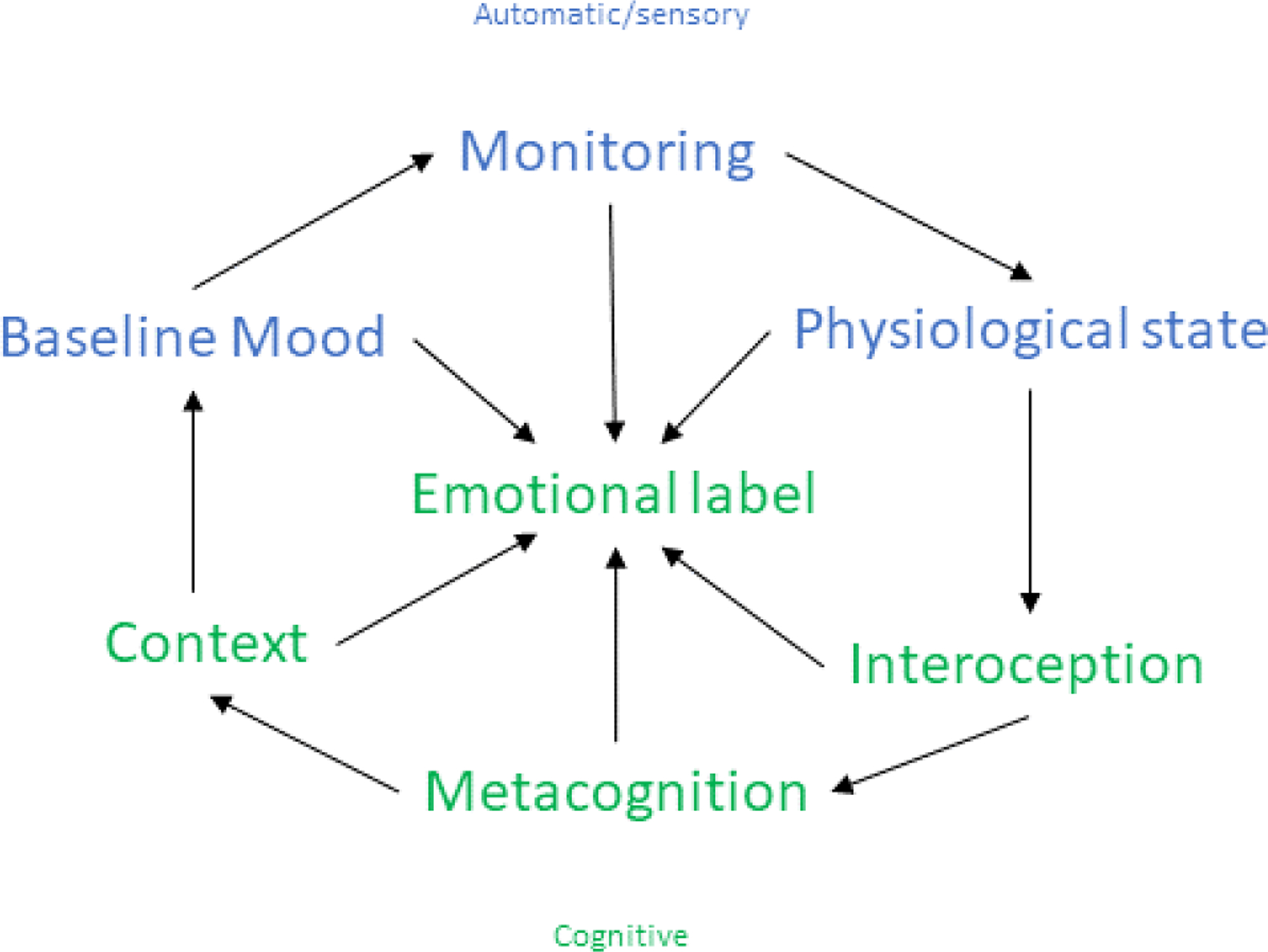
Schematic diagram of proposed components involved in labeling emotions.
Here we consider general and specific examples relating to operation of the proposed model. Individuals present with baseline moods that may have been influenced by histories with specific moods and prior emotional experiences. A stimulus is experienced that may result in an instantaneous or rapid deviation from that mood. Interpretation of that deviation depends on individuals’ monitoring tendencies, influenced by monitoring systems that may involve neurotransmitters like dopamine. A physiological state may evolve as a result of the previous components and additional reactivity, involving interoceptive processes. Individuals use information about their history with the physiological state and context to frame their emotional responses, and ultimately use history with emotional labels to apply labels. The process of emotional identification and labeling may ultimately inform both current mood states and histories of experiencing emotions.
For example, consider a person coming home from work who encounters people leaping out and yelling “surprise” when they arrive. Their physiological state may involve a pounding heart relating to adrenaline release, and this may result in a sharp deviation from a more neutral or relaxed mood they had been experiencing previously. Past experience with this feeling may be ambiguous, particularly if the individual is not often anxious. The immediate framing—surprise in the setting of this party—may result in the physiological feelings being coded as ones of excitement and surprise.
On the other hand, a person presenting with high reactivity due to anxiety may enter into the same situation with different reactions. The resulting physiological state, just like the non-anxious person, may involve a pounding heart and a release of adrenaline, but this may accentuate an already heightened anxious mood. From past experiences, the individual may recognize this state as unpleasant. The context may not be enough for the individual to identify the intense experience as pleasurable, and the sensations in the setting of an anxious mood state may continue to be unpleasant and be coded as dread or panic. A label may then be applied for the person to communicate with others about his or her feelings.
Every factor in the model contributes to determining the label of emotions. The proposed model has utility in exploring alexithymia, as described below.
Predictions
Now we turn to some specific disorders commonly seen among individuals with alexithymia, and explore how particular failures in the model may explain these associated links. Improper weighting of different components of the model may result in alexithymia through different mechanisms, and may primarily present as various mental health concerns. We present here a predictive model illustrating some of the potential ways this may occur. Hypotheses generated here specify that certain deficits may contribute to alexithymia in the indicated mental health disorders.
While not entirely accounting for every aspect of mental illnesses, specific deficits in utilizing skills outlined in this model may contribute to alexithymia in different ways that both increase severity of these illnesses and complicate their treatment. We briefly review how deficits in stages of the model may contribute to specific psychological disorders.
Somatic symptom disorder
Somatic symptom disorder manifests as reports of physical pain or illness that are not a result of illness or injury or a result of substance use (Nijenhuis et al., 1997). In addition, individuals with this condition report preoccupation with their symptoms that is out of proportion to the symptom severity (Garcia-Campayo et al., 2009).These disorders have long been associated with alexithymia (Lundh and Simonsson-Sarnecki, 2001), and heightened interoception combined with difficulties correctly taking context into account may underlie this relationship. With increased focus on one’s physiological states, a person may believe that their physiological states are worse or more intense than they are. They may then focus disproportionately on physical symptoms their emotions may elicit rather than the emotional experience given the context. Overreliance on interoception may also contribute to increased distress from pain experiences, as evidenced by heightened distress and alexithymia experienced by individuals with chronic pain who received methadone (Morie et al., 2021).
Eating disorders
Eating disorders have significant morbidity and can manifest as anorexia nervosa, binge-eating disorder, or bulimia (Sim et al., 2010). Alexithymia is common in people with eating disorders (Nowakowski et al., 2013), and utilization of our model may help to explain their co-occurrence. Overreliance on monitoring and poor interoception may contribute to alexithymia in eating disorders such as anorexia nervosa, enabled by tendencies to purposefully ignore or not properly process bodily sensations related to hunger (Westwood et al., 2017). Other forms of eating disorders, such as binge-eating disorder, may stem from failure to process interoceptive feelings of fullness (Sysko et al., 2007). Tendencies to ignore physical sensations related to over-eating, or not eating enough, coupled with overly strict self-monitoring of intake and perception of body shape may contribute to difficulties experienced in people with eating disorders.
Anxiety
Anxiety disorders, including generalized anxiety, obsessive-compulsive, panic, post-traumatic stress, and social phobia disorders (Fajkowska et al., 2017), are frequently experienced in community samples (Jones et al., 2020; Preti et al., 2021). Intact interoception with poor monitoring capability may lead to failures in identifying physiological states as being related to emotions, in turn increasing anxiety and further worsening physiological states and perpetuating a cycle of anxiety that may be difficult to break. Difficulties managing personal ruminations that trigger anxiety and recognition of physiological symptoms of anxiety may worsen this cycle. This process may explain the high prevalence of anxiety in individuals with alexithymia (Karukivi et al., 2010; Troisi et al., 2000), and emphasizes that recognizing anxiety is an important step toward treatment (Coles et al., 2014). In addition, history of frightening experiences may also contribute to tendencies to label arousal as frightening, which may also be seen in depressive disorders.
Depression
Affective disorders are also important to consider within the framework of the proposed model. Depression is common among individuals with alexithymia (Serafini et al., 2016), and this may reflect a focus on mood states, limited metacognition and potentially inappropriate responses to context. One route to depression that stems from alexithymia may involve early life trauma. Similar considerations exist for anxiety disorders. Anxious parents may instill anxiety in a child, observable in the laboratory at very young ages (de Rosnay et al., 2006). More severe examples may include frequent uncertainty in the environment, making it difficult to properly label one’s emotional responses (inconsistent parenting and neglect) or constant negative events that repeatedly instill sadness and fear (abuse), and these events may have repercussions on emotional processing at multiple developmental stages including throughout adulthood (Morie, 2020; Young and Widom, 2014). Once a particular situation or physiological state has been labeled a certain way, it may be difficult to re-label. In addition, the proposed model suggests that repeated emotions labeled negatively may set a low baseline mood, suggesting that individual differences in trauma exposure are important to consider in the mechanisms underlying experiencing and labeling emotions. Uncertainty in future emotional contexts, in situations in which an individual relies more on their history to label an emotion, may be strongly influenced by positive (stable attachment) or negative (neglect or abuse) histories. In the latter case, potentially positive things, such as meeting a new person or starting a new relationship, may be perceived as frightening rather than exciting or joyful, and this may lead to experiential and emotional avoidance (Gratz et al., 2007). A history of abuse and neglect may skew emotion identification in the proposed model and lead to poorer functioning and a cycle of negative affect that may be difficult to break.
Addictive disorders
Executive dysfunction and difficulties in monitoring as well as blunted physiological responses may explain links between alexithymia and addictive disorders (Pinard et al., 1996). According to the proposed model, poor monitoring may result in failures to properly respond emotionally to stimuli. A commonly observed tendency in individuals with addictive disorders relates to processing of negative feedback suggestive of poorer error processing (Castelluccio et al., 2014; Franken et al., 2007; Morie et al., 2014) and reflected in real-world continued engagement in addictive behaviors despite negative consequences. Similarly, reductions in physiological responses, notably reward, may influence individuals to seek substances of abuse, and anhedonia and reward deficits in addictive disorders are well characterized (Leventhal et al., 2010). Alexithymia has been related to decision-making, with poorer feedback monitoring capabilities seen in alexithymic individuals during a gambling task (Ferguson et al., 2009).
Conditions involving frontal cortical dysfunction
Executive dysfunction is commonly seen in individuals with alexithymia (Koven and Thomas, 2010), with a noted deficit in emotional monitoring. Alexithymic features are seen in individuals with traumatic brain injuries to frontal regions (Henry et al., 2006) as well as illnesses associated with frontal regions, such as human immunodeficiency virus (HIV) infection (Bogdanova et al., 2010; McIntosh et al., 2014), and Parkinson’s disease (Bogdanova and Cronin-Golomb, 2013).
Future work can test these components of the model in individuals with different mental illnesses. Specific treatments may then be developed and employed to address specific patterns of deficits that may accompany alexithymia in each case.
Conclusions
We have proposed a model of emotion identification to provide a framework for how people may identify their feelings. We have described how the model may relate to alexithymia and to different mental illnesses commonly seen in individuals with alexithymia. The model presents seven steps, including baseline mood, monitoring, physiological responses, interoception, contexts, metacognition, and labeling. These steps are independent, interconnected abilities/tendencies required for people to most accurately identify their emotions, which is required in order to regulate emotion in an optimal fashion. The proposed model is informed by the current literature and uniquely explores the idea that emotion identification is necessary for intact emotional regulation. The model provides testable hypotheses surrounding deficits in different abilities or tendencies that contribute to alexithymia and mental illnesses. Like every model, it deserves rigorous testing of these hypotheses. Future work should examine each element of the model to test the possibilities described above.
This model may also have ramifications for emotional intelligence, including empathy and perceiving emotions in others, and emotional regulation. Once an emotion is understood and labeled, regulating that emotion may become easier, and the emotion may be perceived as less threatening. Additional insight into behavior, such as through mindfulness, may be beneficial for well-being.
Ultimately, increasing understanding of how individuals arrive at emotions they experience could have significant impacts on psychiatric treatments. Therapies designed around increasing awareness of emotions may be helpful transdiagnostically (Lumley et al., 2021). Further, treatment providers who investigate how patients identify emotions and form concepts of emotions may be able to tailor treatments more readily. For example, treatments for individuals with trauma histories who may need practice applying new schemas to their emotions may differ from treatments for individuals with poor cognitive control who may need assistance developing abilities or tendencies to monitor what actions may influence their own emotions or from individuals who lack interoceptive capabilities or tendencies. In sum, the model we present seeks to inform the literature on potential ways to understand how individuals identify their emotions and the importance of intact emotion identification, and emphasizes the importance of patient-centered psychiatric care.
Figure 1:
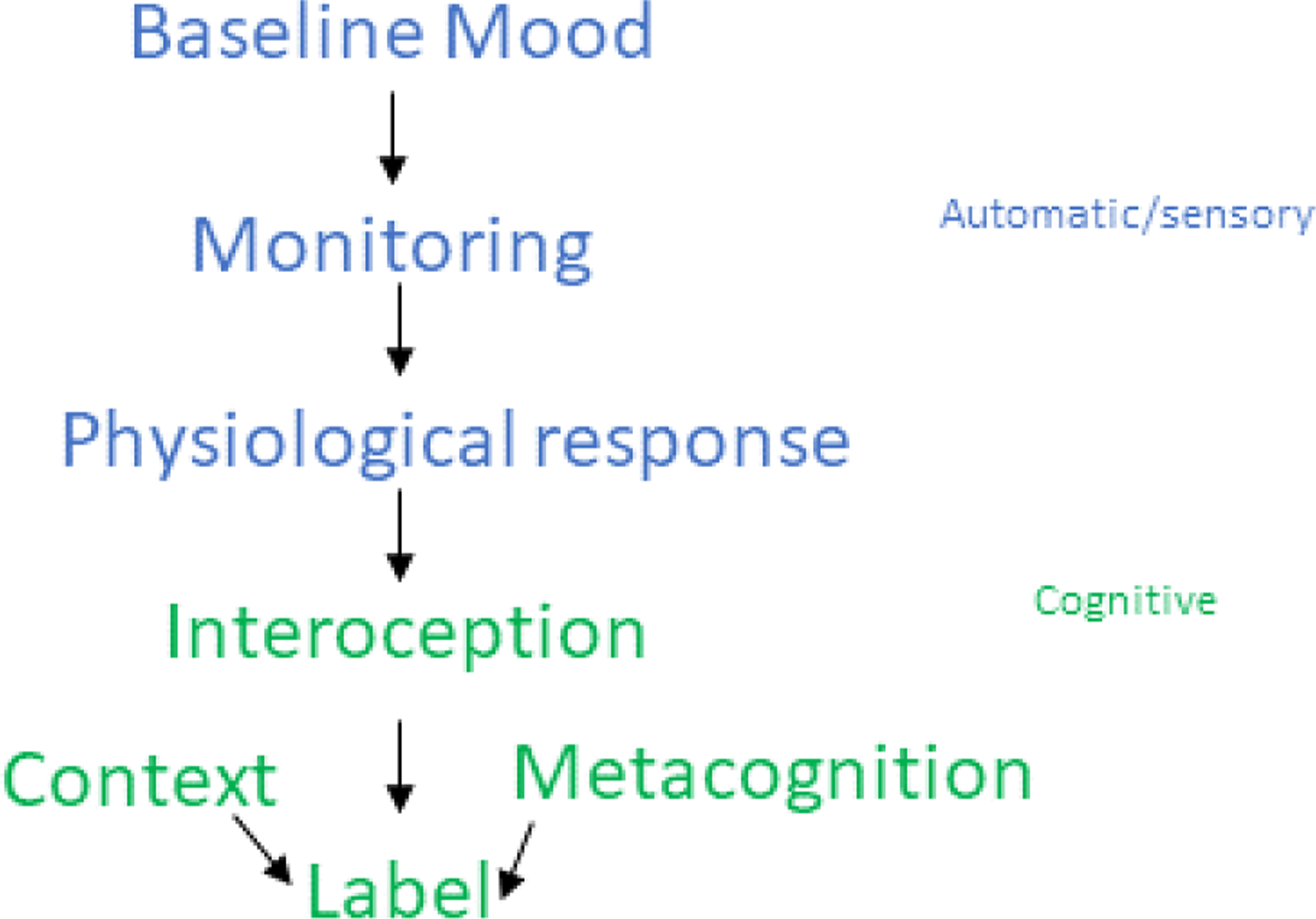
Schematic illustrating the proposed steps involved in emotional identification and the order in which they occur. Context and metacognition are not time-dependent and may influence previous steps, as well as the ultimate label.
Figure 3:
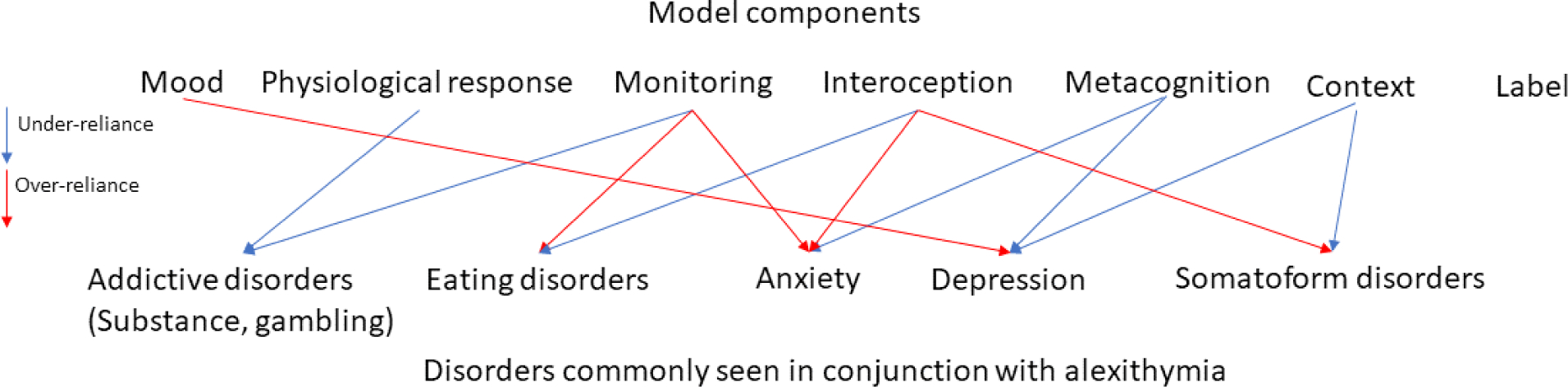
Deficits in processes related to the emotional model and potential associations with mental illnesses common in alexithymia.
Role of the Funding Source
KPM receives support from MH018268-31 and from K01DA042937. MNP receives support from the Connecticut Council on Problem Gambling and from RF1 MH128614, R01 DK121551 and R01 AA029611. Beyond funding, the funding agencies had no further role in the writing of the report or in the decision to submit the paper for publication.
Footnotes
Conflicts of Interest
The authors report no conflict of interest with respect to the content of this manuscript.
The authors report no conflicts of interest with respect to the content of this manuscript. Dr. Potenza has the following financial disclosures. He has consulted for and advised Opiant Pharmaceuticals, Idorsia Pharmaceuticals, AXA, Game Day Data, and the Addiction Policy Forum; has been involved in a patent application with Yale University and Novartis; has received research support from the Mohegan Sun Casino, the Connecticut Council on Problem Gambling, and the National Center for Responsible Gaming; has participated in surveys, mailings or telephone consultations related to drug addiction, impulse control disorders or other health topics; and has consulted for law offices and gambling entities on issues related to impulse control or addictive disorders. Other authors report no disclosures. The other authors report no financial relationships with commercial interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agnes Moors PCE, Scherer Klaus R., Frijda Nico H., 2013. Moors Agnes, Ellsworth Phoebe C., Scherer Klaus R., Frijda Nico H.. Emot Rev 5. [Google Scholar]
- Armstrong AR, Galligan RF, Critchley CR, 2011. Emotional intelligence and psychological resilience to negative life events. Personality and Individual Differences 51, 331–336. [Google Scholar]
- Aviezer H, Hassin RR, Ryan J, Grady C, Susskind J, Anderson A, Moscovitch M, Bentin S, 2008. Angry, disgusted, or afraid? Studies on the malleability of emotion perception. Psychological science 19, 724–732. [DOI] [PubMed] [Google Scholar]
- Babaei S, Gharechahi M, Hatami Z, Ranjbar Varandi S, 2015. Metacognition and Body Image in Predicting Alexithymia in Substance Abusers. Int J High Risk Behav Addict 4, e25775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachmann S, Muller-Werdan U, Huber M, Kasel M, Werdan K, Schmidt H, 2011. Positive impact of the beta-blocker celiprolol on panic, anxiety, and cardiovascular parameters in patients with mitral valve prolapse syndrome. J Clin Psychopharmacol 31, 783–785. [DOI] [PubMed] [Google Scholar]
- Barrett LF, 2006. Solving the emotion paradox: categorization and the experience of emotion. Pers Soc Psychol Rev 10, 20–46. [DOI] [PubMed] [Google Scholar]
- Barrett LF, 2017. The theory of constructed emotion: an active inference account of interoception and categorization. Soc Cogn Affect Neurosci 12, 1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellebaum C, Polezzi D, Daum I, 2010. It is less than you expected: The feedback-related negativity reflects violations of reward magnitude expectations. Neuropsychologia 48, 3343–3350. [DOI] [PubMed] [Google Scholar]
- Bogdanova Y, Cronin-Golomb A, 2013. Alexithymia and apathy in Parkinson’s disease: Neurocognitive correlates. Behav Neurol 27, 535–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogdanova Y, Diaz-Santos M, Cronin-Golomb A, 2010. Neurocognitive correlates of alexithymia in asymptomatic individuals with HIV. Neuropsychologia 48, 1295–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bono JE, Vey MA, 2007. Personality and emotional performance: extraversion, neuroticism, and self-monitoring. J Occup Health Psychol 12, 177–192. [DOI] [PubMed] [Google Scholar]
- Borhani K, Ladavas E, Fotopoulou A, Haggard P, 2017. “Lacking warmth”: Alexithymia trait is related to warm-specific thermal somatosensory processing. Biol Psychol 128, 132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brackett MA, Rivers SE, Salovey P, 2011. Emotional Intelligence: Implications for Personal, Social, Academic, and Workplace Success. Social and Personality Psychology Compass. [Google Scholar]
- Brewer R, Cook R, Bird G, 2016. Alexithymia: a general deficit of interoception. Roy Soc Open Sci 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, 2003. The benefits of being present: Mindfulness and its role in psychological well-being. J Pers Soc Psychol 84, 822–848. [DOI] [PubMed] [Google Scholar]
- Bruce G, Curren C, Williams L, 2012. Alexithymia and alcohol consumption: the mediating effects of drinking motives. Addictive behaviors 37, 350–352. [DOI] [PubMed] [Google Scholar]
- Bublatzky F, Kavcioglu F, Guerra P, Doll S, Junghofer M, 2020. Contextual information resolves uncertainty about ambiguous facial emotions: Behavioral and magnetoencephalographic correlates. NeuroImage 215, 116814. [DOI] [PubMed] [Google Scholar]
- Burger AJ, Lumley MA, Carty JN, Latsch DV, Thakur ER, Hyde-Nolan ME, Hijazi AM, Schubiner H, 2016. The effects of a novel psychological attribution and emotional awareness and expression therapy for chronic musculoskeletal pain: A preliminary, uncontrolled trial. Journal of psychosomatic research 81, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT, 2006. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clin Psychol Rev 26, 17–31. [DOI] [PubMed] [Google Scholar]
- Cannon WB, 1987. The James-Lange theory of emotions: a critical examination and an alternative theory. By Walter B. Cannon, 1927. Am J Psychol 100, 567–586. [PubMed] [Google Scholar]
- Castelluccio BC, Meda SA, Muska CE, Stevens MC, Pearlson GD, 2014. Error processing in current and former cocaine users. Brain Imaging Behav 8, 87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecchetto C, Rumiati RI, Aiello M, 2017. Alexithymia and emotional reactions to odors. Sci Rep 7, 14097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecero JJ, Holmstrom RW, 1997. Alexithymia and affect pathology among adult male alcoholics. J Clin Psychol 53, 201–208. [DOI] [PubMed] [Google Scholar]
- Chae Y, Goodman M, Goodman GS, Troxel N, McWilliams K, Thompson RA, Shaver PR, Widaman KF, 2018. How children remember the Strange Situation: The role of attachment. J Exp Child Psychol 166, 360–379. [DOI] [PubMed] [Google Scholar]
- Charland LC, 1995. Emotion as a Natural Kind - Towards a Computational Foundation for Emotion Theory. Philos Psychol 8, 59–84. [Google Scholar]
- Ciarrochi JV, Chan AYC, Caputi P, 2000. A critical evaluation of the emotional intelligence construct. Personality and Individual Differences 28, 539–561. [Google Scholar]
- Cohen MX, Elger CE, Ranganath C, 2007. Reward expectation modulates feedback-related negativity and EEG spectra. NeuroImage 35, 968–978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles ME, Schubert JR, Heimberg RG, Weiss BD, 2014. Disseminating treatment for anxiety disorders: step 1: recognizing the problem as a precursor to seeking help. J Anxiety Disord 28, 737–740. [DOI] [PubMed] [Google Scholar]
- Craig AD, 2002. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neurosci 3, 655–666. [DOI] [PubMed] [Google Scholar]
- Craig AD, 2009. How do you feel - now? The anterior insula and human awareness. Nat Rev Neurosci 10, 59–70. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Wiens S, Rotshtein P, Ohman A, Dolan RJ, 2004. Neural systems supporting interoceptive awareness. Nat Neurosci 7, 189–195. [DOI] [PubMed] [Google Scholar]
- de Haan HA, van der Palen J, Wijdeveld TG, Buitelaar JK, De Jong CA, 2014. Alexithymia in patients with substance use disorders: state or trait? Psychiatry research 216, 137–145. [DOI] [PubMed] [Google Scholar]
- de Rosnay M, Cooper PJ, Tsigaras N, Murray L, 2006. Transmission of social anxiety from mother to infant: An experimental study using a social referencing paradigm. Behaviour research and therapy 44, 1165–1175. [DOI] [PubMed] [Google Scholar]
- de Timary P, Luts A, Hers D, Luminet O, 2008. Absolute and relative stability of alexithymia in alcoholic inpatients undergoing alcohol withdrawal: relationship to depression and anxiety. Psychiatry research 157, 105–113. [DOI] [PubMed] [Google Scholar]
- Domschke K, Stevens S, Pfleiderer B, Gerlach AL, 2010. Interoceptive sensitivity in anxiety and anxiety disorders: an overview and integration of neurobiological findings. Clin Psychol Rev 30, 1–11. [DOI] [PubMed] [Google Scholar]
- Donges US, Suslow T, 2015. Alexithymia and Memory for Facial Emotions. Univ Psychol 14, 103–110. [Google Scholar]
- Eastabrook JM, Lanteigne DM, Hollenstein T, 2013. Decoupling between physiological, self-reported, and expressed emotional responses in alexithymia. Personality and Individual Differences 55. [Google Scholar]
- Eimer M, 2000. The face-specific N170 component reflects late stages in the structural encoding of faces. Neuroreport 11, 2319–2324. [DOI] [PubMed] [Google Scholar]
- Ellsworth PC, & Scherer KR, 2003. Appraisal processes in emotion. In: Davidson RJ, K.R.S., & Goldsmith HH (Ed.), Series in affective science Handbook of affective sciences. Oxford University Press. pp. 572–595. [Google Scholar]
- Fajkowska M, Domaradzka E, Wytykowska A, 2017. Types of Anxiety and Depression: Theoretical Assumptions and Development of the Anxiety and Depression Questionnaire. Front Psychol 8, 2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson E, Bibby PA, Rosamond S, O’Grady C, Parcell A, Amos C, McCutcheon C, O’Carroll R, 2009. Alexithymia, cumulative feedback, and differential response patterns on the Iowa Gambling Task. Journal of personality 77, 883–902. [DOI] [PubMed] [Google Scholar]
- Franken IH, van Strien JW, Franzek EJ, van de Wetering BJ, 2007. Error-processing deficits in patients with cocaine dependence. Biol Psychol 75, 45–51. [DOI] [PubMed] [Google Scholar]
- Frijda NH, 2009. Emotion Experience and its Varieties. Emot Rev 1, 264–271. [Google Scholar]
- Galderisi S, Heinz A, Kastrup M, Beezhold J, Sartorius N, 2015. Toward a new definition of mental health. World Psychiatry 14, 231–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Campayo J, Fayed N, Serrano-Blanco A, Roca M, 2009. Brain dysfunction behind functional symptoms: neuroimaging and somatoform, conversive, and dissociative disorders. Curr Opin Psychiatry 22, 224–231. [DOI] [PubMed] [Google Scholar]
- Garfinkel SN, Tiley C, O’Keeffe S, Harrison NA, Seth AK, Critchley HD, 2016. Discrepancies between dimensions of interoception in autism: Implications for emotion and anxiety. Biol Psychol 114, 117–126. [DOI] [PubMed] [Google Scholar]
- Gaudiano BA, 2006. Review: cognitive behavioural therapy is an effective treatment for depression, panic disorder, and generalised anxiety disorder, but may be less effective in severe cases. Evid Based Ment Health 9, 80. [DOI] [PubMed] [Google Scholar]
- Gendron M, Roberson D, van der Vyver JM, Barrett LF, 2014. Perceptions of emotion from facial expressions are not culturally universal: evidence from a remote culture. Emotion 14, 251–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, McRae K, Ramel W, Gross JJ, 2008. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry 63, 577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grabe HJ, Frommer J, Ankerhold A, Ulrich C, Groger R, Franke GH, Barnow S, Freyberger HJ, Spitzer C, 2008. Alexithymia and outcome in psychotherapy. Psychother Psychosom 77, 189–194. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Bornovalova MA, Delany-Brumsey A, Nick B, Lejuez CW, 2007. A laboratory-based study of the relationship between childhood abuse and experiential avoidance among inner-city substance users: The role of emotional nonacceptance. Behav Ther 38, 256–268. [DOI] [PubMed] [Google Scholar]
- Greenberg DM, Kolasi J, Hegsted CP, Berkowitz Y, Jurist EL, 2017. Mentalized affectivity: A new model and assessment of emotion regulation. PloS one 12, e0185264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ, 2015. Emotion Regulation: Current Status and Future Prospects. Psychol Inq 26, 1–26. [Google Scholar]
- Gu R, Huang YX, Luo YJ, 2010. Anxiety and feedback negativity. Psychophysiology 47, 961–967. [DOI] [PubMed] [Google Scholar]
- Hajcak G, Moser JS, Holroyd CB, Simons RF, 2006. The feedback-related negativity reflects the binary evaluation of good versus bad outcomes. Biol Psychol 71, 148–154. [DOI] [PubMed] [Google Scholar]
- Hariri AR, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D, Egan MF, Weinberger DR, 2002. Serotonin transporter genetic variation and the response of the human amygdala. Science 297, 400–403. [DOI] [PubMed] [Google Scholar]
- Hassin RR, Aviezer H, Bentin S, 2013. Inherently Ambiguous: Facial Expressions of Emotions, in Context. Emot Rev 5, 60–65. [Google Scholar]
- Hauser TU, Iannaccone R, Stampfli P, Drechsler R, Brandeis D, Walitza S, Brem S, 2014. The feedback-related negativity (FRN) revisited: New insights into the localization, meaning and network organization. NeuroImage 84, 159–168. [DOI] [PubMed] [Google Scholar]
- Hendryx MS, Haviland MG, Shaw DG, 1991. Dimensions of alexithymia and their relationships to anxiety and depression. J Pers Assess 56, 227–237. [DOI] [PubMed] [Google Scholar]
- Henry JD, Phillips LH, Crawford JR, Theodorou G, Summers F, 2006. Cognitive and psychosocial correlates of alexithymia following traumatic brain injury. Neuropsychologia 44, 62–72. [DOI] [PubMed] [Google Scholar]
- Hobson H, Hogeveen J, Brewer R, Catmur C, Gordon B, Krueger F, Chau A, Bird G, Grafman J, 2018. Language and alexithymia: Evidence for the role of the inferior frontal gyrus in acquired alexithymia. Neuropsychologia 111, 229–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holroyd CB, Coles MG, 2002. The neural basis of human error processing: reinforcement learning, dopamine, and the error-related negativity. Psychological review 109, 679–709. [DOI] [PubMed] [Google Scholar]
- Honkalampi K, Hintikka J, Tanskanen A, Lehtonen J, Viinamaki H, 2000. Depression is strongly associated with alexithymia in the general population. J Psychosom Res 48, 99–104. [DOI] [PubMed] [Google Scholar]
- Izard CE, 2007. Basic Emotions, Natural Kinds, Emotion Schemas, and a New Paradigm. Perspect Psychol Sci 2, 260–280. [DOI] [PubMed] [Google Scholar]
- Izard CE, Libero DZ, Putnam P, Haynes OM, 1993. Stability of Emotion Experiences and Their Relations to Traits of Personality. J Pers Soc Psychol 64, 847–860. [DOI] [PubMed] [Google Scholar]
- Jones AL, Cochran SD, Rafferty J, Taylor RJ, Mays VM, 2020. Lifetime and Twelve-Month Prevalence, Persistence, and Unmet Treatment Needs of Mood, Anxiety, and Substance Use Disorders in African American and U.S. versus Foreign-Born Caribbean Women. Int J Environ Res Public Health 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karukivi M, Hautala L, Kaleva O, Haapasalo-Pesu KM, Liuksila PR, Joukamaa M, Saarijarvi S, 2010. Alexithymia is associated with anxiety among adolescents. J Affect Disorders 125, 383–387. [DOI] [PubMed] [Google Scholar]
- Karukivi M, Joukamaa M, Hautala L, Kaleva O, Haapasalo-Pesu KM, Liuksila PR, Saarijarvi S, 2012. Deficit in speech development at the age of 5 years predicts alexithymia in late-adolescent males. Compr Psychiat 53, 54–62. [DOI] [PubMed] [Google Scholar]
- Koven NS, Thomas W, 2010. Mapping facets of alexithymia to executive dysfunction in daily life. Personality and Individual Differences 49, 24–28. [Google Scholar]
- Lamberty GJ, Holt CS, 1995. Evidence for a verbal deficit in alexithymia. J Neuropsychiatry Clin Neurosci 7, 320–324. [DOI] [PubMed] [Google Scholar]
- Langer K, Jentsch VL, Wolf OT, 2021. Cortisol promotes the cognitive regulation of high intensive emotions independent of timing. The European journal of neuroscience. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, 2008. Sadness, depression, and avoidance behavior. Behavior modification 32, 759–779. [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Brightman M, Ameringer KJ, Greenberg J, Mickens L, Ray LA, Sun P, Sussman S, 2010. Anhedonia Associated With Stimulant Use and Dependence in a Population-Based Sample of American Adults. Exp Clin Psychopharm 18, 562–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T, Li D, Shangguan F, Shi J, 2019. The Relationships Among Testosterone, Cortisol, and Cognitive Control of Emotion as Underlying Mechanisms of Emotional Intelligence of 10- to 11-Year-Old Children. Front Behav Neurosci 13, 273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovheim H, 2012. A new three-dimensional model for emotions and monoamine neurotransmitters. Med Hypotheses 78, 341–348. [DOI] [PubMed] [Google Scholar]
- Luciano M, Huffman JE, Arias-Vasquez A, Vinkhuyzen AA, Middeldorp CM, Giegling I, Payton A, Davies G, Zgaga L, Janzing J, Ke X, Galesloot T, Hartmann AM, Ollier W, Tenesa A, Hayward C, Verhagen M, Montgomery GW, Hottenga JJ, Konte B, Starr JM, Vitart V, Vos PE, Madden PA, Willemsen G, Konnerth H, Horan MA, Porteous DJ, Campbell H, Vermeulen SH, Heath AC, Wright A, Polasek O, Kovacevic SB, Hastie ND, Franke B, Boomsma DI, Martin NG, Rujescu D, Wilson JF, Buitelaar J, Pendleton N, Rudan I, Deary IJ, 2012. Genome-wide association uncovers shared genetic effects among personality traits and mood states. Am J Med Genet B Neuropsychiatr Genet 159B, 684–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luminet O, Nielson KA, Ridout N, 2021a. Cognitive-emotional processing in alexithymia: an integrative review. Cogn Emot 35, 449–487. [DOI] [PubMed] [Google Scholar]
- Luminet O, Nielson KA, Ridout N, 2021b. Having no words for feelings: alexithymia as a fundamental personality dimension at the interface of cognition and emotion. Cogn Emot 35, 435–448. [DOI] [PubMed] [Google Scholar]
- Luminet O, Rime B, Bagby RM, Taylor GJ, 2004. A multimodal investigation of emotional responding in alexithymia. Cognition Emotion 18, 741–766. [Google Scholar]
- Lumley MA, Krohner S, Marshall LM, Kitts TC, Schubiner H, Yarns BC, 2021. Emotional awareness and other emotional processes: implications for the assessment and treatment of chronic pain. Pain Manag 11, 325–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley MA, Roby KJ, 1995. Alexithymia and pathological gambling. Psychother Psychosom 63, 201–206. [DOI] [PubMed] [Google Scholar]
- Lundh LG, Simonsson-Sarnecki M, 2001. Alexithymia, emotion, and somatic complaints. Journal of personality 69, 483–510. [DOI] [PubMed] [Google Scholar]
- Luu P, Tucker DM, Derryberry D, Reed M, Poulsen C, 2003. Electrophysiological responses to errors and feedback in the process of action regulation. Psychological science 14, 47–53. [DOI] [PubMed] [Google Scholar]
- MacDonald AW 3rd, Cohen JD, Stenger VA, Carter CS, 2000. Dissociating the role of the dorsolateral prefrontal and anterior cingulate cortex in cognitive control. Science 288, 1835–1838. [DOI] [PubMed] [Google Scholar]
- Maier ME, Scarpazza C, Starita F, Filogamo R, Ladavas E, 2016. Error monitoring is related to processing internal affective states. Cogn Affect Behav Neurosci 16, 1050–1062. [DOI] [PubMed] [Google Scholar]
- Mayer JD, & Salovey P, 1997. What is emotional intelligence?. In: Sluyter PSDJ (Ed.), Emotional Development and Emotional Intelligence: Educational Implications Basic Books, Inc., New York, NY. [Google Scholar]
- Mayer JD, Gaschke YN, Braverman DL, Evans TW, 1992. Mood-Congruent Judgment Is a General Effect. J Pers Soc Psychol 63, 119–132. [Google Scholar]
- Mayer JD, Salovey P, Caruso DR, Sitarenios G, 2003. Measuring Emotional Intelligence With the MSCEIT V2.0. Emotion 3, 97–105. [DOI] [PubMed] [Google Scholar]
- Mayer JD, Salovey P, & Caruso DR, 2004. Emotional intelligence: Theory, findings, and implications. Psychological Inquiry 15, 197–215. [Google Scholar]
- McIntosh RC, Ironson G, Antoni M, Kumar M, Fletcher MA, Schneiderman N, 2014. Alexithymia is linked to neurocognitive, psychological, neuroendocrine, and immune dysfunction in persons living with HIV. Brain Behav Immun 36, 165–175. [DOI] [PubMed] [Google Scholar]
- Montebarocci O, Surcinelli P, Rossi N, Baldaro B, 2011. Alexithymia, verbal ability and emotion recognition. The Psychiatric quarterly 82, 245–252. [DOI] [PubMed] [Google Scholar]
- Moors A, Ellsworth PC, Scherer KR, Frijda NH, 2013. Appraisal Theories of Emotion: State of the Art and Future Development. Emot Rev 5, 119–124. [Google Scholar]
- Morie K, Zhai ZW, Potenza MN, Mayes LC, 2020. Alexithymia, emotion-regulation strategies, and traumatic experiences in prenatally cocaine-exposed young adults. Am J Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morie KP, De Sanctis P, Garavan H, Foxe JJ, 2014. Executive dysfunction and reward dysregulation: a high-density electrical mapping study in cocaine abusers. Neuropharmacology 85, 397–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morie KP, Potenza MN, Beitel M, Oberleitner LM, Roos CR, Yip SW, Oberleitner DE, Gaeta M, Barry DT, 2021. Alexithymia and pain experience among patients using methadone-maintenance therapy. Drug and alcohol dependence 218, 108387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morie KP, Zhai ZW, Potenza MN, Mayes LC, 2020. Alexithymia, Emotion-Regulation Strategies, and Traumatic Experiences in Prenatally Cocaine-Exposed Young Adults. Am J Addict. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Ollendick TH, King NJ, Bogie N, 2001. Children’s nighttime fears: parent-child ratings of frequency, content, origins, coping behaviors and severity. Behaviour research and therapy 39, 13–28. [DOI] [PubMed] [Google Scholar]
- Murphy J, Brewer R, Hobson H, Catmur C, Bird G, 2018a. Is alexithymia characterised by impaired interoception? Further evidence, the importance of control variables, and the problems with the Heartbeat Counting Task. Biol Psychol. [DOI] [PubMed] [Google Scholar]
- Murphy J, Catmur C, Bird G, 2018b. Alexithymia Is Associated With a Multidomain, Multidimensional Failure of Interoception: Evidence From Novel Tests. J Exp Psychol Gen 147, 398–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nijenhuis ER, Spinhoven P, van Dyck R, van der Hart O, Vanderlinden J, 1997. The development of the somatoform dissociation questionnaire (SDQ-5) as a screening instrument for dissociative disorders. Acta Psychiatr Scand 96, 311–318. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S, 2008. Rethinking Rumination. Perspect Psychol Sci 3, 400–424. [DOI] [PubMed] [Google Scholar]
- Nowakowski ME, McFarlane T, Cassin S, 2013. Alexithymia and eating disorders: a critical review of the literature. J Eat Disord 1, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvet DM, Hajcak G, 2008. The error-related negativity (ERN) and psychopathology: Toward an endophenotype. Clin Psychol Rev 28, 1343–1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvet DM, Hajcak G, 2009. The effect of trial-to-trial feedback on the error-related negativity and its relationship with anxiety. Cogn Affect Behav Neurosci 9, 427–433. [DOI] [PubMed] [Google Scholar]
- Pandey R, Saxena P, Dubey A, 2011. Emotion regulation difficulties in alexithymia and mental health. Europe’s journal of psychology 7. [Google Scholar]
- Parker JD, Taylor GJ, Bagby M, 2003. The 20-Item Toronto Alexithymia Scale III. Reliability and factorial validity in a community population. J Psychosom Res 55, 269–275. [DOI] [PubMed] [Google Scholar]
- Peasley-Miklus CE, Panayiotou G, Vrana SR, 2016. Alexithymia predicts arousal-based processing deficits and discordance between emotion response systems during emotional imagery. Emotion 16, 164–174. [DOI] [PubMed] [Google Scholar]
- Pinard L, Negrete JC, Annable L, Audet N, 1996. Alexithymia in substance abusers - Persistence and correlates of variance. Am J Addiction 5, 32–39. [Google Scholar]
- Pombo S, Felix da Costa Nuno, Ismail Fatima, Jose M. Neves Cardoso, Maria Luisa Figueira, 2014. Alexithymia and alcohol dependence: Do different subtypes manifest different emotion regulations? Addiction Research and Theory Ahead of print, 1–9. [Google Scholar]
- Poquerusse J, Pastore L, Dellantonio S, Esposito G, 2018. Alexithymia and Autism Spectrum Disorder: A Complex Relationship. Front Psychol 9, 1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti A, Demontis R, Cossu G, Kalcev G, Cabras F, Moro MF, Romano F, Balestrieri M, Caraci F, Dell’Osso L, Di Sciascio G, Drago F, Hardoy MC, Roncone R, Faravelli C, Gonzalez CIA, Angermayer M, Carta MG, 2021. The lifetime prevalence and impact of generalized anxiety disorders in an epidemiologic Italian National Survey carried out by clinicians by means of semi-structured interviews. BMC Psychiatry 21, 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remmington NA, Fabrigar LR, Visser PS, 2000. Reexamining the circumplex model of affect. J Pers Soc Psychol 79, 286–300. [DOI] [PubMed] [Google Scholar]
- Ridderinkhof KR, van den Wildenberg WP, Segalowitz SJ, Carter CS, 2004. Neurocognitive mechanisms of cognitive control: the role of prefrontal cortex in action selection, response inhibition, performance monitoring, and reward-based learning. Brain and cognition 56, 129–140. [DOI] [PubMed] [Google Scholar]
- Righart R, de Gelder B, 2008. Rapid influence of emotional scenes on encoding of facial expressions: an ERP study. Soc Cogn Affect Neurosci 3, 270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha M, Soares S, Silva S, Madeira N, Silva C, 2016. The effects of alexithymia in the recognition of dynamic emotional faces. European Psychiatry 33. [Google Scholar]
- Rottenberg J, Gross JJ, Gotlib IH, 2005. Emotion context insensitivity in major depressive disorder. Journal of abnormal psychology 114, 627–639. [DOI] [PubMed] [Google Scholar]
- Salovey P, Mayer JD, 1990. Emotional Intelligence. Imagination, Cognition and Personality 9, 185–211. [Google Scholar]
- Santesso DL, Bogdan R, Birk JL, Goetz EL, Holmes AJ, Pizzagalli DA, 2012. Neural responses to negative feedback are related to negative emotionality in healthy adults. Soc Cogn Affect Neurosci 7, 794–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer KR, 2000. Appraisal processes in emotion: Theories and research. Int J Psychol 35, 400–401. [Google Scholar]
- Scherer KR, 2005. What are emotions? And how can they be measured? Soc Sci Inform 44, 695–729. [Google Scholar]
- Scherer KR, 2019. Studying appraisal-driven emotion processes: taking stock and moving to the future. Cogn Emot 33, 31–40. [DOI] [PubMed] [Google Scholar]
- Schultz W, Dayan P, Montague PR, 1997. A neural substrate of prediction and reward. Science 275, 1593–1599. [DOI] [PubMed] [Google Scholar]
- Serafini G, Engel-Yeger B, Gonda X, Costi S, Pompili M, Rihmer Z, Girardi P, Amore M, 2016. Sensory processing patterns and their relation with impulsivity, alexithymia, depression, and hopelessness in major affective disorders. Eur Neuropsychopharm 26, S485–S486. [Google Scholar]
- Sheppes G, Suri G, Gross JJ, 2015. Emotion regulation and psychopathology. Annu Rev Clin Psychol 11, 379–405. [DOI] [PubMed] [Google Scholar]
- Sim LA, McAlpine DE, Grothe KB, Himes SM, Cockerill RG, Clark MM, 2010. Identification and treatment of eating disorders in the primary care setting. Mayo Clin Proc 85, 746–751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slanger E, Rudestam KE, 1997. Motivation and disinhibition in high risk sports: Sensation seeking and self-efficacy. J Res Pers 31, 355–374. [Google Scholar]
- Smith JD, Woodhouse SS, Clark CA, Skowron EA, 2016. Attachment status and mother-preschooler parasympathetic response to the strange situation procedure. Biol Psychol 114, 39–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone LA, Nielson KA, 2001. Intact physiological response to arousal with impaired emotional recognition in alexithymia. Psychother Psychosom 70, 92–102. [DOI] [PubMed] [Google Scholar]
- Stoney CM, Davis MC, Matthews KA, 1987. Sex differences in physiological responses to stress and in coronary heart disease: a causal link? Psychophysiology 24, 127–131. [DOI] [PubMed] [Google Scholar]
- Swinkels A, Giuliano TA, 1995. The Measurement and Conceptualization of Mood Awareness - Monitoring and Labeling Ones Mood States. Pers Soc Psychol B 21, 934–949. [Google Scholar]
- Sysko R, Devlin MJ, Walsh BT, Zimmerli E, Kissileff HR, 2007. Satiety and test meal intake among women with binge eating disorder. Int J Eat Disord 40, 554–561. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Georgiades S, Duku E, Zwaigenbaum L, Goldberg J, Bennett T, 2008. Alexithymia in parents of children with autism spectrum disorder. J Autism Dev Disord 38, 1859–1865. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, 1984. Alexithymia: concept, measurement, and implications for treatment. Am J Psychiatry 141, 725–732. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, Parker JDA, Bagby RM, Bourke MP, 1996. Relationships between alexithymia and psychological characteristics associated with eating disorders. J Psychosom Res 41, 561–568. [DOI] [PubMed] [Google Scholar]
- Terhaar J, Viola FC, Bar KJ, Debener S, 2012. Heartbeat evoked potentials mirror altered body perception in depressed patients. Clin Neurophysiol 123, 1950–1957. [DOI] [PubMed] [Google Scholar]
- Troisi A, Belsanti S, Bucci AR, Mosco C, Sinti F, Verucci M, 2000. Affect regulation in alexithymia: an ethological study of displacement behavior during psychiatric interviews. The Journal of nervous and mental disease 188, 13–18. [DOI] [PubMed] [Google Scholar]
- Tucker DM, Luu P, Frishkoff G, Quiring J, Poulsen C, 2003. Frontolimbic response to negative feedback in clinical depression. Journal of abnormal psychology 112, 667–678. [DOI] [PubMed] [Google Scholar]
- van Noordt SJR, Segalowitz SJ, 2012. Performance monitoring and the medial prefrontal cortex: a review of individual differences and context effects as a window on self-regulation. Frontiers in human neuroscience 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Zijderveld GA, Veltman DJ, van Dyck R, van Doornen LJ, 1999. Epinephrine-induced panic attacks and hyperventilation. J Psychiatr Res 33, 73–78. [DOI] [PubMed] [Google Scholar]
- Venta A, Hart J, Sharp C, 2013. The relation between experiential avoidance, alexithymia and emotion regulation in inpatient adolescents. Clin Child Psychol P 18, 398–410. [DOI] [PubMed] [Google Scholar]
- Voichek G, Novemsky N, 2021. Asymmetric Hedonic Contrast: Pain Is More Contrast Dependent Than Pleasure. Psychological science 32, 1038–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walden TA, Ogan TA, 1988. The development of social referencing. Child Dev 59, 1230–1240. [DOI] [PubMed] [Google Scholar]
- Waugh CE, Muhtadie L, Thompson RJ, Joormann J, Gotlib IH, 2012. Affective and physiological responses to stress in girls at elevated risk for depression. Dev Psychopathol 24, 661–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westwood H, Kerr-Gaffney J, Stahl D, Tchanturia K, 2017. Alexithymia in eating disorders: Systematic review and meta-analyses of studies using the Toronto Alexithymia Scale. Journal of psychosomatic research 99, 66–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiens S, Mezzacappa E, Katkin E, 2000. Heartbeat detection and the experience of emotions. Cognition and Emotion 14, 417–427. [Google Scholar]
- Wise TN, Mann LS, Hill B, 1990. Alexithymia and depressed mood in the psychiatric patient. Psychother Psychosom 54, 26–31. [DOI] [PubMed] [Google Scholar]
- Wood RL, Williams C, 2007. Neuropsychological correlates of organic alexithymia. J Int Neuropsychol Soc 13, 471–479. [DOI] [PubMed] [Google Scholar]
- Xu F, Xiang P, Huang L, 2020. Bridging Ecological Rationality, Embodied Emotion, and Neuroeconomics: Insights From the Somatic Marker Hypothesis. Front Psychol 11, 1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JC, Widom CS, 2014. Long-term effects of child abuse and neglect on emotion processing in adulthood. Child Abuse Negl 38, 1369–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zellner DA, Rohm EA, Bassetti TL, Parker S, 2003. Compared to what? Effects of categorization on hedonic contrast. Psychon Bull Rev 10, 468–473. [DOI] [PubMed] [Google Scholar]
- Zubarev I, Parkkonen L, 2018. Evidence for a general performance-monitoring system in the human brain. Human brain mapping 39, 4322–4333. [DOI] [PMC free article] [PubMed] [Google Scholar]


