Abstract
Background
Anesthesiologists are at high risk of developing burnout, a condition which can lead to many deleterious effects for the physician, and far-reaching effects on their patients and hospital systems. The COVID-19 pandemic has presented new challenges that have further exacerbated the risk of burnout in anesthesiologists. It is critical to develop effective strategies to promote well-being and decrease burnout for physicians in this specialty. The purpose of this observational study was to evaluate the impact of a Physician Well-Being Initiative on distress and well-being in anesthesiologists. It was hypothesized that the wellness intervention would promote an improvement in well-being scores.
Methods
The Physician Well-Being Initiative was launched in August 2019 in the Department of Anesthesiology, Pain Management and Perioperative Medicine at Henry Ford Hospital in Detroit, Michigan. The Physician Well-Being Initiative was designed to address several of the key factors that improve physician wellness, including 1) a sense of autonomy; 2) positive view of leadership; and 3) flexible schedule opportunities. To assess the impact of the Physician Well-Being Initiative on the well-being and distress scores of participating anesthesiologists, the physicians were emailed the validated Well-Being Index survey at baseline and 3, 6 and 12 months. The Well-Being Index evaluates multiple items of distress in the healthcare setting. The sample size was limited to the 54 anesthesiologists at Henry Ford Hospital.
Results
Forty-four of the 54 anesthesiologists completed the baseline questionnaire. A total of 44 physicians answered the questionnaire at baseline, with more male than female physicians (35 males and 7 females) and the majority (17/44) in practice for 5-10 years. Thirty-two physicians completed the survey at 3 and 6 months, and 31 physicians at 12 months after the launch of the Physician Well-Being Initiative. Twenty-one physicians completed the questionnaire at all 4 time points. Although the COVID-19 pandemic started shortly after the 6-month surveys were submitted, results indicated that there was a 0.05 decrease in the Well-Being Index sum score for every 1-month of time (coefficient -0.05, 95% CI -0.01, -0.08, P = 0.013). This study shows that, with the wellness initiative in place, the department was able to maintain and potentially even reduce physician distress despite the concurrent onset of the pandemic.
Conclusions
Following the launch of a sustained wellness initiative, this study demonstrates that physician wellness improved with time. This suggests that it takes time for a wellness initiative to have an effect on well-being and distress in anesthesiologists.
Keywords: Physician wellness, burnout, resiliency, cultural change
1. Introduction
Anesthesiologists have emerged as essential healthcare workers on the frontlines of the COVID-19 pandemic, relying on their unique skills in airway management, resuscitation and critical care medicine. While burnout was already prevalent in 50% of anesthesiologists prior to the pandemic, the pandemic has resulted in increased rates of stress, depression and burnout amongst this specialty.1, 2, 3, 4 Numerous job-related risk factors increase the risk of burnout in anesthesiologists, including elevated levels of work-related stress, fatigue, production pressure, and complexity of clinical tasks, the solitary nature of patient care, frequency of adverse perioperative events, lack of reliable shift hours, high level of medical acuity, and the lack of stress management strategies.5 , 6 Recent literature suggests that lack of support at work and home are most strongly associated with burnout syndrome amonst anesthesiologists.2 , 3 This has contributed to higher substance use disorders at a rate 2.7 times that of other physicians,4 and higher rates of anxiety and depression, which are particularly well documented among anesthesia residents.7
Burnout is a state of emotional, physical, and mental exhaustion that entails a constellation of symptoms that can result in maladaptive behaviors such as relationship instability, substance misuse, depression, anxiety, and suicide.8 , 9 Burnout is not a function of personal resiliency, but rather a result of workplace demands and pressure that lead to a discord between employer expectations and physician career satisfaction. Physician burnout does not only impact physicians, it has far-reaching negative effects on patients and healthcare institutions, including increased staff turnover, poor workplace performance, inefficiency, and medical errors.8 , 10 Much of the literature regarding distress in anesthesiology focuses on the identification and diagnosis of burnout, as well as the effects of burnout on anesthesiologists. However, there is a paucity of data on effective interventions to decrease physician burnout, particularly for anesthesiologists.
Recognizing the need to promote physician wellness, the Department of Anesthesiology, Pain Management and Perioperative Medicine at Henry Ford Hospital in Detroit, MI, developed a Physician Well-Being Initiative. The Physician Well-Being Initiative is an evidence-based multidimensional approach that addresses several of the key factors that promote physician wellness, including a sense of autonomy, flexibility and control over time, a positive view of leadership, and social support in the workplace5, 16-18 (see Supplemental Digital Content, Appendix 1 for a description of the entire initiative).
The key purpose of this study is to evaluate the impact of the Physician Well-Being Initiative on distress and well-being in the department's anesthesiology providers. It was hypothesized that implementation of the wellness initiative would decrease physician distress and improve well-being.
2. Methods
This study evaluated the effects of the Physician Well-Being Initiative launched by the Department of Anesthesiology, Pain Management & Perioperative Medicine at Henry Ford Hospital in Detroit, MI. The Physician Well-Being Initiative was designed to promote wellness and decrease distress in anesthesiology providers (see Supplemental Digital Content, Appendix 1 for a description of the entire initiative). The Physician Well-Being Initiative was first introduced to the department in a 60-minute morning meeting lecture. During this lecture, the topic of physician wellness, engagement and distress was discussed, and the department Physician Well-Being Initiative was described. After receiving approval from the Henry Ford Health System Institutional Review Board, an email announcement outlining the study details was sent to all staff anesthesiologists and pain medicine physicians at Henry Ford Hospital. Formal informed consent was waived, and instead a consent script was included preceding the baseline survey that was distributed to the physicians via email. Completion of the survey served as agreement to participate in the study. In order to prevent bias, coercion, or other undue influence in survey responses, the emails and surveys were distributed using REDCap (Vanderbilt University, Nashville, TN) and responses were completely anonymous. The survey consisted of 11 questions about employment, demographics, work schedule, and the Well-Being Index. The Well-Being Index is a tool created by the Mayo Clinic that consists of 7 questions to evaluate professional stress and distress in the healthcare setting; it has been shown to be a valid measure of this construct in large samples of US physicians, residents, and medical students.11, 12, 13, 14 The baseline survey was distributed in August 2019. After baseline Well-Being Index scores were collected, the Physician Well-Being Initiative was launched. Physicians who completed the baseline questionnaire received emails containing links to take the survey again at 3 months, 6 months, and 12 months after the launch of the initiative. Well-Being Index scores were then compared to determine if the initiative had a significant effect on physician distress and well-being. The sample size was limited to 54, as this is the total number of staff anesthesiologists and pain medicine physicians employed at Henry Ford Hospital. The authors were included in the original sample size. As participation was voluntary, not all providers chose to participate in the study.
The Physician Well-Being Initiative utilized a multidimensional approach to address salient factors that promote physician wellness, including 1) a sense of autonomy; 2) positive view of leadership; and 3) sense of control of one's time/schedule.1 , 15 Physician autonomy, time, and control of one's schedule were addressed via several scheduling initiatives. A flextime system was introduced that provided various shifts to create more variability in weekly scheduling while still maintaining the same full-time employee's status. Additionally, enhanced night-time coverage was offered via a night-float system, wherein over-night calls were offered for 3 or 4 consecutive nights, with the respective amount of post-call days offered to allow time for recovery of circadian rhythm. Additionally, 12 protected hours were provided each year for participation in community service events, with the idea that incentivizing community engagement translates into increased meaning and purpose in one's work.16
To evaluate leadership, focus groups were conducted for each division within the department. Each focus group was conducted by the health system's Chief Wellness Officer (not a member of the Department of Anesthesiology). The results of each focus group were then summarized into a report and presented to each division head. The division head was then expected to create an action plan based on any identified barriers to physician wellness.
2.1. Statistical Analysis
Basic characteristics between those who responded and those who did not were compared using Fisher's exact test. The primary outcomes of this study were established a priori. Following collection of the baseline, 3-month, 6-month, and 12-month questionnaires, an analysis comparing baseline and post-Physician Well-Being Initiative scores was performed to evaluate if Well-Being Index scores were significantly changed following the Physician Well-Being Initiative. Numeric variables were summarized in mean and standard deviation, and categorical variables were summarized in frequency and proportion. Changes in response to individual yes/no items from baseline to each follow-up point was compared using McNemar's test for paired nominal data. A Well-Being Index sum score was created by summing up the number of “yes” in the Well-Being Index questionnaire. The repeated measures of Well-Being Index were correlated within each physician's own score. The generalized estimating equation (GEE) method was used with the R package “gee”17 to study the repeated measures of Well-Being Index sum scores across baseline and 3 follow-ups since GEE can consider the correlation of within-subject data. Variance in GEE models were estimated using the robust “sandwich” estimator. Further, GEE does not require follow-up data for all timepoints, so if subjects had at least one follow-up survey, their data was incorporated in the analysis. The association between time and Well-Being Index was evaluated graphically to determine if linearity was a reasonable assumption in the GEE model. Models were adjusted for the confounding variables of physician sex, years in practice, and time since the launch of the intervention. Underlying mechanisms of loss to follow-up missingness were assessed using Little's missing completely at random (MCAR) test18 while missing at random (MAR) was assessed by associating indicators of missingness at each time point with baseline Well-Being Index, sex, and years in practice (linear regression or Fisher's exact tests). To adjust for each of the 7 items in the Well-Being Index by all other Well-Being Index items, generalized estimating equations were used that took into account repeated subject measures, but instead of a continuous outcome (the WBI index, normal distribution), each individual item was treated as a binary outcome using a logistic link, and then the remaining 6 items were adjusted for. A p-value less than 0.05 was considered statistically significant. The sample size was limited to the 54 anesthesiologists and pain physicians in the department; therefore, a formal sample size calculation was not performed. All statistical analysis was performed using R Statistical Software (version 4.0; R Foundation, Vienna, Austria). The R package “ggplot2”19 was used for figure generation.
This manuscript adheres to the applicable STROBE guidelines for observational studies, and the study was approved by the Henry Ford Health System Institutional Review Board (IRB#13706). Written informed consent was waived. A consent script preceded the baseline survey and completion of the survey served as consent to participate in the study.
3. Results
Of the total 54 practicing anesthesiologists in practice at Henry Ford Hospital in Detroit, MI, 44 physicians answered the Well-Being Index questionnaire at baseline. Among them, 40 physicians completed at least one of the follow-up Well-Being Index questionnaires at 3 months, 6 months, or 12 months following launch of the Physician Well-Being Initiative, and 21 of the anesthesiologists completed the questionnaire at all time points. During the study time frame, 6 staff anesthesiologists left the department for a myriad of reasons, which contributed to attrition.
A few basic demographic items were asked at baseline: 93% (n = 41) of respondents were full-time anesthesiologists (compared to 83% of the entire department), 79% identified as male (compared to 76% of the entire department),16% were female and 5% did not disclose their sex (Table 1 ). The majority of respondents (39%, n = 17) were in practice between 5-10 years, while 32% (71% vs. 78% in practice 10 years or less among respondents and entire department, respectively; Table 1).
Table 1.
Characteristics of the physician population, comparing entire department to those who responded.
| Variable | Frequency- Respondents (%) | Frequency- Entire Department (%) | p-value1 |
|---|---|---|---|
| Full-time physician | 41/44 (93) | 48/54 (89) | 0.20 |
| Sex | 0.99 | ||
| Male | 35/44 (79) | 43/54 (79) | |
| Female | 7/44 (16) | 9/54 (17) | |
| Unknown | 2/44 (5) | 2/54 (4) | |
| Years in practice | 0.90 | ||
| <5 | 14/44 (32) | 17/54 (31) | |
| 5-10 | 17/44 (39) | 22/54 (41) | |
| 11-15 | 1/44 (2) | 1/54 (2) | |
| 16-20 | 3/44 (7) | 4/54 (7) | |
| >20 | 9/44 (20) | 10/54 (19) |
Comparison of anesthesiologists who responded versus those who did not, using Fisher's exact test.
Baseline data was collected at the study start of August 2019. Three-month follow-up data was collected in November 2019, 6-month follow-up data was collected in February 2020 and 12-month data was collected in August 2020. The 6-month follow-up data was collected just prior to the dramatic increase in COVID-19 cases in the United States, so there is a particular window of pre- and post-pandemic data that has been captured.
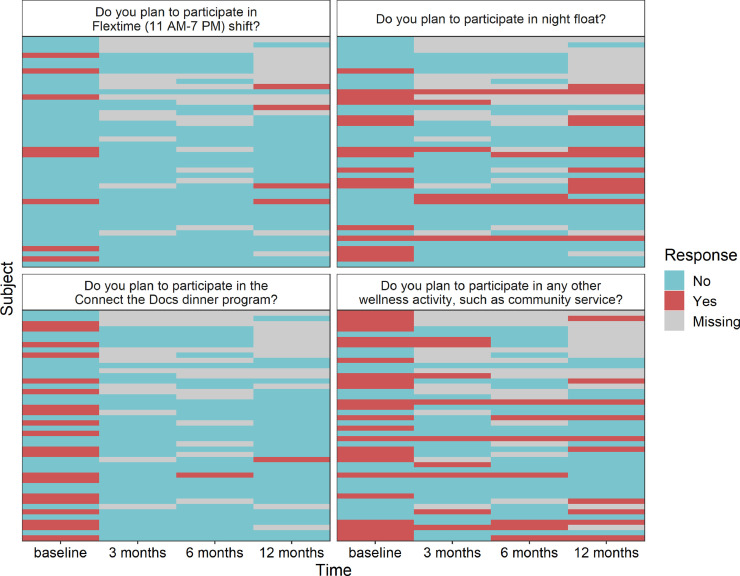
Comparing baseline and 12-month follow-up responses to the 7-items of the Well-Being Index, questions regarding falling asleep while driving (35.5% at baseline vs. 12.9% at 12 months; p=0.023) and work piling up too high (45.2% at baseline vs. 25.8% at 12 months; p=0.041) were both significantly improved from baseline responses (Table 2 ). These two items also exhibited significant reductions from baseline to 3 months (both p=0.041). The remaining five items of the Well-Being index did not exhibit a significant change from baseline to any of the follow-up time points (all p≥0.05). These trends are also graphically displayed in Supplemental Figure 1. Initial plans to participate in various components of the well-being initiative were significantly higher than the actual participation in three out of the four components evaluated (Table 2; Supplemental Figure 2). Specifically, plans to participate in flextime were 21.9% at baseline, compared to actual participation in flextime being 0% at 3-months (p=0.023); results were similar at 6-months (p=0.041). Similarly, the percentage of staff that planned to participate in the Connect the Docs dinner program was significantly higher than the percentage of staff that participated at all three follow-up times (p<0.001, p=0.001, p=0.001), and plans to participate in any other wellness activities were higher at baseline compared to the percentage who actually participated at both 3-months (p=0.027) and 6-months (p=0.003).
Table 2.
Change in survey results prior to and following launch of the physician well-being intervention.
| Question | Baseline (Aug 2019) vs. 3 Months (Nov 2019) |
Baseline (Aug 2019) vs. 6 Months (Feb 2020) |
Baseline (Aug 2019) vs. 12 Months (Aug 2020) |
|||
|---|---|---|---|---|---|---|
| Percentages1 | p-value2 | Percentages1 | p-value2 | Percentages1 | p-value2 | |
| Engagement in Physician Well-Being Initiative | ||||||
| Participation in Flextime (11 AM-7 PM) shift3 |
21.9% vs. 0% | 0.023 | 19.4% vs. 0% | 0.041 | 16.1% vs. 12.9% | 0.999 |
| Participation in night float3 | 40.6% vs. 18.8% | 0.070 | 25.8% vs. 16.1% | 0.450 | 38.7% vs. 38.7% | 0.999 |
| Participation in the Connect the Docs dinner program3 | 50% vs. 0% | <0.001 | 48.4% vs. 3.2% | 0.001 | 48.4% vs. 3.2% | 0.001 |
| Participation in any other wellness activity, such as community service?3 | 56.2% vs. 28.1% | 0.027 | 58.1% vs. 22.6% | 0.003 | 51.6% vs. 32.3% | 0.114 |
| Well-Being Index | ||||||
| Have you felt burned out from your work? | 56.2% vs. 53.1% | 0.999 | 54.8% vs. 41.9% | 0.343 | 61.3% vs. 41.9% | 0.077 |
| Have you worried that your work is hardening you emotionally? | 56.2% vs. 40.6% | 0.182 | 58.1% vs. 45.2% | 0.221 | 64.5% vs. 48.4% | 0.131 |
| Have you been bothered by feeling down, depressed, or hopeless? | 15.6% vs. 21.9% | 0.617 | 16.1% vs. 9.7% | 0.683 | 12.9% vs. 25.8% | 0.221 |
| Have you fallen asleep while stopped in traffic or driving? | 31.2% vs. 12.5% | 0.041 | 32.3% vs. 25.8% | 0.683 | 35.5% vs. 12.9% | 0.023 |
| Have you felt that all things you had to do were piling up so high that you could not overcome them? | 43.8% vs. 25% | 0.041 | 45.2% vs. 32.3% | 0.289 | 45.2% vs. 25.8% | 0.041 |
| Have you been bothered by emotional problems (such as feeling anxious, depressed, or irritable)? | 28.1% vs. 37.5% | 0.505 | 32.3% vs. 29% | 0.999 | 35.5% vs. 41.9% | 0.724 |
| Has your physical health interfered with your ability to do your daily work at home and/or away from home? | 9.4% vs. 6.2% | 0.999 | 9.7% vs. 16.1% | 0.480 | 9.7% vs. 9.7% | 0.999 |
Baseline percentages may shift as only participants who have data at both time points are included.
Calculated by McNemar's Test for paired nominal data.
Baseline survey was phrased “Do you plan to participate in [component of wellness intervention]?”, while 3 month, 6 month, and 12 month follow-up surveys were phrased “Have you participated in [component of wellness intervention]?”
As shown in Table 3 , when the composite Well-Being Index score was examined, the unadjusted generalized estimating equations model indicated that there was a significant effect of time, i.e., a 0.04 improvement in Well-Being Index sum score for every 1-month of time (p=0.012). This trend can be seen in Figure 1 , which demonstrates that linearity is a reasonable assumption for the time trend. The adjusted generalized estimating equations also gave similar results that there was a significant effect for time, i.e., with a 0.05 improvement in Well-Being Index sum score for every 1-month of time (p=0.013; Table 3). Though men on average had 0.62 lower Well-Being Index scores than women, this was non-significant (Table 3; p=0.397). When a time by sex interaction term was further added to this model to evaluate if the effect of the wellness initiative over time differs between men and women, we did not find a sex-specific effect (p=0.453).
Table 3.
Generalized estimating equations models for the change in Well-Being Index scores in the 12 months following the launch of the physician well-being initiative.
| Generalized estimating equations model | Coefficient | 95% CI | p-value |
|---|---|---|---|
| Unadjusted model | |||
| Time (Per Month) | -0.04 | (-0.08, -0.01) | 0.012 |
| Adjusted model | |||
| Time (Per Month) | -0.05 | (-0.08, -0.01) | 0.013 |
| Sex | |||
| Male (Ref: Female) | -0.62 | (-2.06, 0.82) | 0.397 |
| Years in Practice | |||
| 5-10 years (Ref: More than 10 years) | 0.26 | (-1.27, 1.79) | 0.738 |
| Less than 5 years (Ref: More than 10 years) | -0.60 | (-1.95, 0.76) | 0.388 |
Figure 1.
Spaghetti plot for the association between time and Well-Being Index Score. Thin grey lines are individual subjects, while the thick red line is the linear smooth line and the red dots are means at each time point.
As can be seen in Table 4 , when each of the 7 items in the Well-Being Index were adjusted for by all other Well-Being Index items, the adjusted model did not converge for 3 of the 7 measures (Table 4). Of the items that did converge, only falling asleep while driving remains significant, with each 1-month increase in time resulting in 0.89 lower odds of responding “yes” to this question (Table 4; p=0.028).
Table 4.
Generalized estimating equations models for the change in individual Well-Being Index items in the 12 months following the launch of the physician well-being initiative.
| Outcome | Unadjusted |
Adjusted1 |
||
|---|---|---|---|---|
| OR (95% CI)2 | p-value | OR (95% CI)2 | p-value | |
| Have you felt burned out from your work? | 0.95 (0.90, 1.01) | 0.060 | —3 | —3 |
| Have you worried that your work is hardening you emotionally? | 0.95 (0.91, 1.01) | 0.071 | 1.00 (0.94, 1.07) | 0.963 |
| Have you been bothered by feeling down, depressed, or hopeless? | 1.05 (0.96, 1.15) | 0.289 | 1.09 (0.95, 1.26) | 0.208 |
| Have you fallen asleep while stopped in traffic or driving? | 0.89 (0.81, 0.97) | 0.010 | 0.89 (0.81, 0.99) | 0.028 |
| Have you felt that all things you had to do were piling up so high that you could not overcome them? | 0.94 (0.89, 0.99) | 0.033 | 0.91 (0.82, 1.01) | 0.075 |
| Have you been bothered by emotional problems (such as feeling anxious, depressed, or irritable)? | 1.03 (0.98, 1.09) | 0.218 | —3 | —3 |
| Has your physical health interfered with your ability to do your daily work at home and/or away from home? | 1.05 (0.98, 1.12) | 0.171 | —3 | —3 |
Adjusted for all other well-being index items.
Interpreted as the change in odds of experiencing the outcome for each 1-month increase in time.
Model did not converge.
When the underlying mechanism for missingness due to loss to follow-up was examined, we could not reject the null hypothesis that data are missing completely at random (MCAR, p=0.55). When missing at random (MAR) was tested to see if baseline covariates could predict loss to follow-up, we did not find any associations between baseline Well-Being Index and loss to follow-up at any of the three time points (all linear regression p≥0.22). Additionally, both sex (all Fisher's exact p≥0.16) and years in practice (all Fisher's exact p≥0.30) did not associate with loss to follow-up.
4. Discussion
To our knowledge, this is the first study describing the impact of an intervention to reduce distress amongst attending anesthesiologists amid the COVID-19 pandemic. At the time of study conception and institutional review board approval, there was no knowledge of the impending COVID-19 pandemic, so the original study design was not intended to assess on the impact of COVID-19 on distress in our department. The results indicated that, despite the potentially devastating impact of the COVID-19 pandemic, intervention duration is a significant factor in the success of a wellness initiative. Our study shows that overall physician distress may have declined over time, suggesting that a 12-month initiative would be more effective than an intervention of shorter duration.
Looking at pre-COVID-19 responses (August 2019, November 2019, and February 2020), there were significant improvements between baseline and pre-COVID-19 responses for falling asleep while driving and feeling as though work was piling up too high and being bothered by emotional problems. While there are emerging data regarding the impact of COVID-19 on physician burnout,5 , 6 , 20 this study shows an improvement in both of these parameters of distress assessed by the Well-Being Index following the exponential increase in COVID-19 cases in the United Stated in March 2020. Overall, the study does show that, despite the distress epidemic and COVID-19 pandemic, the implementation of the Physician Well-Being Initiative was associated with improvement in composite wellness scores and reduced distress at the end of the 12-month study period.
Study participants self-selected to enroll, so there may be a selection bias to those who chose to participate in a study or in wellness activities in general. About one-third of the participants were lost to follow-up from baseline to the final questionnaire. In investigating reasons for missingness, we were unable to reject the null hypothesis of missing completely at random (MCAR) and we did not find evidence for missing at random (MAR). However, lack of response to the follow-up questionnaires could have been due to physician burnout or negative perceptions of the initiative (missing not at random, MNAR), increasing the risk for bias in the responses. During the study time frame, six staff anesthesiologists left the department for myriad reasons, which contributed to attrition. It should be noted that most anesthesiologists who left the department did so for non-job-stress related reasons, such as spouse relocation or to be closer to an ailing family member. While the WBI assesses for various parameters of well-being, we did not specifically ask questions about dependents and responsibilities at home. Asking about dependents and roles in the home could have provided more insight into these variables as possible contributors to decreased well-being. This was a single center study, so the results cannot be generalized to other anesthesiology departments. Additionally, because this is not a randomized controlled trial and therefore lacks a control group, strong inferences cannot necessarily be made regarding the causality of our intervention on the decrease in anesthesiologist distress.
This analysis was not designed to identify the individual impact of each facet within the wellness initiative (i.e. flexible scheduling or physician dinners) on distress and wellness. The impact was evaluated cumulatively, making it impossible to establish which aspects of the Well-Being Index may have been most impactful. However, these findings speak to the importance of cultural change within the Department of Anesthesiology at Henry Ford Hospital. The recognition by departmental leadership that physician wellness is a priority and should be integrated into the cultural fabric may be an important factor in the enhanced perception of improved workplace environment. Identifying various employer-related factors that contribute to physician distress is paramount to reducing burnout and promoting wellness. Including initiatives such as leadership evaluation, control of time/schedule, physician autonomy and team building are all important aspects of promoting departmental wellness. Future analysis is necessary to examine the specific factors of the work environment that could reduce burnout amongst anesthesiologists, and to evaluate if implementation of a Well-Being Index at institutions outside of Henry Ford Hospital can promote similar changes in distress and well-being scores.
5. Conclusion
The epidemic of physician distress is of growing national concern, compounded by the social and clinical impact of the COVID-19 pandemic. This was one of the first published initiatives to implement a departmental program to reduce distress amongst anesthesiologists. Additionally, more studies are needed to further characterize effective interventions to reduce burnout on the entire anesthesia-provider team, including certified registered nurse anesthetists, residents and fellows. While more studies are needed to elucidate which specific interventions mitigate burnout amongst anesthesiologists, the results of this study suggest that the presence of a 12-month initiative can reduce distress and promote wellness amongst anesthesiologists.
Author contributions
Lara Zador, MD: This author served as the principal investigator for the study, and came up with the study idea, developed the protocol, monitored data collection, and prepared the manuscript.
Katherine Nowak, PhD: This author helped develop the protocol, submitted and managed regulatory documents, assembled the study database, collected survey results, and assisted in preparing the manuscript.
Alexandra Sitarik, MS: This author performed some statistical analyses of data and contributed to writing the manuscript.
Lisa MacLean, MD: This author helped develop and implement the various aspects of the Physician Well-Being Initiative.
Xiaoxia Han, PhD: This author helped with study design, performed some statistical analyses of data, and contributed to writing the manuscript.
Mandip Kalsi, MD: This author helped with discussion of the results and contributed to the final manuscript.
Nicholas Yeldo, MD: This author helped with discussion of the results and contributed to the final manuscript.
Nabil Sibai, MD: This author helped with discussion of the results and contributed to the final manuscript.
Donald Penning, MD: This author helped with discussion of the results and contributed to the final manuscript.
Michael Lewis, MD: This author helped with encouragement of LZ to develop the project and contributed to the final manuscript.
Funding
No funding was received.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This study was funded internally by the Department of Anesthesiology, Pain Management, and Perioperative Medicine, Henry Ford Hospital.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.pcorm.2022.100251.
Appendix. Supplementary materials
References
- 1.Saadat H., Kain Z.N. Wellness interventions for anesthesiologists. Curr Opin Anaesthesiol. 2018;31(3):375–381. doi: 10.1097/ACO.0000000000000598. [DOI] [PubMed] [Google Scholar]
- 2.Afonso A.M., et al. Burnout rate and risk factors among anesthesiologists in the United States. Anesthesiology. 2021;134(5):683–696. doi: 10.1097/ALN.0000000000003722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hyman S.A., et al. Prevalence of burnout and its relationship to health status and social support in more than 1000 subspecialty anesthesiologists. Reg Anesth Pain Med. 2021;46(5):381–387. doi: 10.1136/rapm-2020-101520. [DOI] [PubMed] [Google Scholar]
- 4.Lefebvre L.G., Kaufmann I.M. The identification and management of substance use disorders in anesthesiologists. Can J Anaesth. 2017;64(2):211–218. doi: 10.1007/s12630-016-0775-y. [DOI] [PubMed] [Google Scholar]
- 5.Azoulay E., et al. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10(1):110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sasangohar F., et al. Provider burnout and fatigue during the COVID-19 pandemic: lessons learned from a high-volume intensive care unit. Anesth Analg. 2020;131(1):106–111. doi: 10.1213/ANE.0000000000004866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Oliveira G.S., Jr., et al. The prevalence of burnout and depression and their association with adherence to safety and practice standards: a survey of United States anesthesiology trainees. Anesth Analg. 2013;117(1):182–193. doi: 10.1213/ANE.0b013e3182917da9. [DOI] [PubMed] [Google Scholar]
- 8.Dewa C.S., et al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14(1):325. doi: 10.1186/1472-6963-14-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shanafelt T.D., et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 10.Lu D.W., et al. Impact of burnout on self-reported patient care among emergency physicians. West J Emerg Med. 2015;16(7):996–1001. doi: 10.5811/westjem.2015.9.27945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dyrbye L.N., Satele D., Shanafelt T. Ability of a 9-item well-being index to identify distress and stratify quality of life in US workers. J Occup Environ Med. 2016;58(8):810–817. doi: 10.1097/JOM.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 12.Dyrbye L.N., et al. Ability of the physician well-being index to identify residents in distress. J Grad Med Educ. 2014;6(1):78–84. doi: 10.4300/JGME-D-13-00117.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dyrbye L.N., et al. Utility of a brief screening tool to identify physicians in distress. J Gen Intern Med. 2013;28(3):421–427. doi: 10.1007/s11606-012-2252-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dyrbye L.N., et al. Development and preliminary psychometric properties of a well-being index for medical students. BMC medical education. 2010;10(1):1–9. doi: 10.1186/1472-6920-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shanafelt T.D., Noseworthy J.H. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129–146. doi: 10.1016/j.mayocp.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Shanafelt T.D., et al. Career fit and burnout among academic faculty. Arch Intern Med. 2009;169(10):990–995. doi: 10.1001/archinternmed.2009.70. [DOI] [PubMed] [Google Scholar]
- 17.Carey, V.J., gee: Generalized Estimation Equation Solver. R package version 4.13-20.https://CRAN.R-project.org/package=gee. 2019.
- 18.Little R.J. A test of missing completely at random for multivariate data with missing values. Journal of the American statistical Association. 1988;83(404):1198–1202. [Google Scholar]
- 19.Hadley W. Springer; 2016. Ggplot2: Elegrant graphics for data analysis. [Google Scholar]
- 20.Dinibutun S.R. Factors associated with burnout among physicians: an evaluation during a period of COVID-19 pandemic. J Healthc Leadersh. 2020;12:85–94. doi: 10.2147/JHL.S270440. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.