Abstract
Background
Although energy devices and botulinum toxin A (BTX-A) can alleviate age-related laxity, ptosis, and platysmal bands, they have limited efficacy on horizontal neck lines.
Objectives
The purpose of this study was to investigate the efficacy, safety, and subject satisfaction of a combined treatment of non–cross-linked hyaluronic acid (HA) compound filling plus mesotherapy for the correction of horizontal neck lines, in comparison with BTX-A.
Methods
This multicenter, randomized, evaluator-blinded, prospective study enrolled female patients with moderate-to-severe horizontal neck lines corrected with either 2 or 3 sessions of of non–cross-linked HA compound filling plus mesotherapy or 1 session of BTX-A injection. Improvement of the neck lines grades, Global Aesthetic Improvement Scale (GAIS), patient satisfaction, and adverse events (AEs) were evaluated and compared at 1, 3, 6, and 10 months after the final treatment.
Results
Twenty-five patients received HA filling plus mesotherapy and 23 received BTX-A injection. Compared with BTX-A, the HA compound filling plus mesotherapy significantly improved the horizontal neck lines grades on all follow-up visits (P = 0.000). Cases of different baseline grades (2, 2.5, and 3) demonstrated similar outcomes. The GAIS and patients’ satisfaction ratings were significantly higher for the HA filling plus mesotherapy treatment group (P = 0.000). Significantly higher pain ratings, higher incidence, and longer recovery of AEs (erythema, edema, and ecchymosis) were noticed in the combined treatment group (P < 0.001). No serious AEs occurred.
Conclusions
Compared with BTX-A, combined treatment with HA compound filling plus mesotherapy significantly improved moderate-to-severe horizontal neck lines and achieved a high level of patient satisfaction.
Level of Evidence: 4

See the Commentary on this article here.
Generally unclothed and visible, the neck can be regarded as both the anatomic and aesthetic continuation of the face. Fat accumulation, sagging, skin laxity and ptosis, and platysma bands are associated with the aging process. Nevertheless, horizontal neck lines are increasingly observed in relatively young people, even those without extensive facial or neck photodamage. Intrinsic factors including race and genetic factors, as well as external factors including smoking and alcohol consumption, are believed to be involved in the pathogenesis of these lines. The head-down posture related to work on mobile telephones and computers, together with regular twisting motions, have increased horizontal neck lines. Therefore, horizontal neck lines cannot simply be ascribed to age-related neck degeneration.1,2
Current noninvasive approaches for neck rejuvenation include fillers,2-8 energy devices,9,10 cosmetic products,11 and combined regimens.12-15 There is a degree of consensus recommending botulinum toxin A (BTX-A) as the first-line early aesthetic intervention for the neck area.16 Clinical studies have demonstrated that BTX-A injection is able to markedly improve the platysmal bands,17-19 and recontour and sharpen the jawline with the “Nefertiti lift.” 19 The microbotox technique has been documented to improve skin texture and sheen, proving mainly effective in treating neck and lower-face soft tissue ptosis.20,21 However, the effects of BTX-A on the horizontal neck lines remained limited, with the patient improvement rate and satisfaction level not exceeding 50%.22 High-intensity focused ultrasound, radiofrequency, and microfocused ultrasound can tighten and lift the skin, and reshape the cervicomental angle, but have limited effect on reducing neck lines.9,10
Although dermal fillers have not been the mainstay treatment for the aging neck, a few publications have reported positive results with commercially available or autologous filler injection for the correction of horizontal neck lines.3,5-8 With its lack of sebaceous glands and moisture, the cervical skin is prone to the loss of dermal matrix and atrophy of connective tissue, which makes the horizontal neck lines an appropriate indication for filler treatment. Significantly, the dryness and fine lines make mesotherapy a potentially beneficial complement for filler treatment. The direct multiple transepidermal transport of pharmaceutically active substances into the dermis or deeper layers might contribute to the maintenance of filler treatment outcomes and/or recovery of a rejuvenated cervical skin with a firm, bright, and moisturized texture.23
To date, no research on a combination of hyaluronic acid (HA) filler injection and mesotherapy treatment for neck lines has been reported. In this study, we aimed to investigate the efficacy and safety of a combined treatment of non–cross-linked HA compound filling and mesotherapy for horizontal neck lines, in comparison with BTX-A injection.
METHODS
Patients
From February 2020 to July 2020, this multicenter, randomized, evaluator-blinded, prospective study recruited Chinese female patients aged over 18 with a baseline presence of moderate to severe horizontal neck lines. Patients were excluded if they had a bleeding tendency or coagulation disorder, severe diabetes, hypertension, or other systematic diseases. Patients who were prone to scarring, were pregnant or lactating, or had received laser, chemical peeling, soft tissue filling, mesotherapy, BTX-A injection, or other surgeries of the neck and/or submandibular areas within 6 months of screening were also excluded. The exclusion criteria also included excessive trepidation, unrealistic expectations, possibility of being allergic to the treatment medication and local anesthesia, infection, dermatitis, or skin abnormality around the injection site. The study was approved by the Sichuan FreSkin Hospital Institutional Ethics Committee and was conducted in compliance with the 1975 Declaration of Helsinki. All patients provided written informed consent prior to enrollment. The patients were randomly assigned to either the HA compound filling plus mesotherapy combined treatment group or the BTX-A injection group.
Treatment and Follow-up
HA Compound Filling and Mesotherapy Combined Treatment
The HA compound filling plus mesotherapy combined treatment comprised delivery of a non–cross-linked HA compound (sodium hyaluronate 5.00 mg/mL, l-carnosine 2.00 mg/mL, proline 0.20 mg/mL, glycine 0.10 mg/mL, alanine 0.10 mg/mL, and vitamin B2 0.005 mg/mL) package (Hearty, Imeik Inc. Ltd, Beijing, China), which contained one 1.5-mL HA (molecular weight, 1200 kDa) compound syringe for filling and one 2.5-mL HA (molecular weight, 600 kDa) compound syringe for mesotherapy (Figure 1A). The patient was placed in Fowler’s position, and the cervical area was cleansed with povidone iodine solution 5% and alcohol swab. Compound lidocaine 5% cream (Tongfang Pharmaceutical Ltd, Beijing, China) was then topically applied for 30 to 40 minutes prior to treatment. After the topical anesthesia was removed, the HA compound filler was injected horizontally by the linear threading technique. Briefly, a 34G BD needle (Becton, Dickinson and Company, Franklin Lakes, NJ) was inserted right into the horizontal neck lines with the bevel up, at an angle of 10° to 15° to the skin surface. The plane of injection was the deep dermis and each injection was spaced about 0.3 to 0.4 cm apart. The HA was deposited as the needle receded. Subcisions could be performed underneath neck lines with the beveled needle to loosen up the tissue before HA injection. A single injection delivered 0.02 to 0.04 mL HA over a distance of 0.3 to 0.4 cm. In total, 1.0 to 3.0 mL HA compound deposition was achieved through serial punctures in a linear threading pattern around the neck, based upon the length and depth of the neck lines (Video 1, available online at www.aestheticsurgeryjournal.com). Immediately following the filler treatment, the HA mesotherapy was performed with Derma Shine (Interlims, Beijing, China) hydrolifting apparatus. The parameters were 0.8 mm depth and 0.0313 mL/shot; 2.5 mL HA compound was delivered to the cervical area in 70 to 85 shots (Video 2, available online at www.aestheticsurgeryjournal.com).
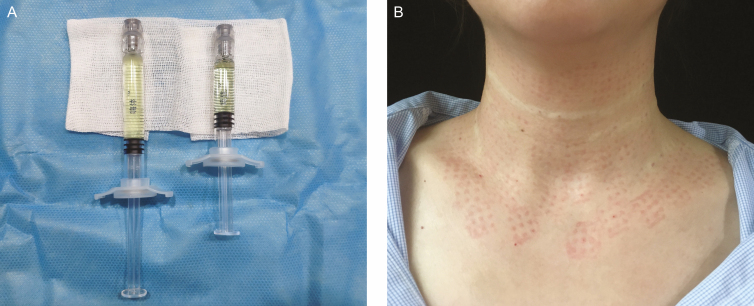
Figure 1.
Non–cross-linked HA compound package and the cervical area immediately after the treatment of this 38-year-old female patient. (A) (right) The 1.5-mL HA compound syringe for filling treatment and (left) the 2.5-mL HA compound syringe for mesotherapy. (B) The cervical area immediately after the treatment. Neck lines baseline grade: 2.5; procedure: 1.5 mL HA compound filling, followed by 2.5 mL HA compound mesotherapy. HA, hyaluronic acid.
Linear and punctate lumps and mild to moderate swelling could be observed after treatment (Figure 1B). Posttreatment care included immediate administration of one piece of neck membrane, together with ice packs for 20 minutes. The patients received 2 to 3 treatment sessions at 4-week intervals, based upon their baseline conditions.
BTX-A Treatment
The patient was placed in Fowler’s position, and disinfection and anesthetic were applied as above. A 100-U vial of onabotulinum toxin A (Botox, Allergan) was diluted with 5 mL normal saline to prepare a 2 U/0.1 mL solution. Injections were performed intradermally at points 1 to 1.5 cm apart in a zigzag pattern along the horizontal lines, placing 1 to 2 U BTX-A into each injection point with a 31G BD needle. Extreme care was taken to penetrate the needle as superficially as possible into the skin. The total maximum dose of BTX-A was 10 to 20 U per horizontal neck line. In cases of horizontal neck wrinkles with prominent vertical platysmal bands, BTX-A was injected at points of intersection between horizontal lines and vertical bands, and additionally along the bands. Less than 50 U of BTX-A was injected to avoid complications such as dysphagia or vocal cord movement abnormality.
Patients in both groups were instructed to avoid water and refrain from putting make-up on the treated area for the next 48 hours. Additional topical medication or treatment for neck lines were strictly forbidden throughout the follow-up period.
Follow-up
Standardized digital photographs of the treated region were taken at baseline and at 1, 3, 6, and 10 months after the final treatment procedure. Touch-ups were not allowed for both groups during follow-up visits.
Evaluation
Investigator-Evaluated Outcomes
The primary outcome measure was the overall improvement of horizontal neck lines, graded by the 2 evaluators (1 dermatologist and 1 plastic surgeon) blinded to the study. The evaluators graded the neck lines by analyzing the standardized digital photographs, based upon the Allergan Transverse Neck Lines Scale.24 In order to evaluate the outcomes more precisely, we modified the scale by supplementing a half grade between 2 whole-number grades. For instance, grade 2.5 represented a neck line condition worse than grade 2, but better than grade 3. The composite score was based on an average of the 2 independent assessments. Scores that had a greater than 20% discrepancy were discarded and reassessed.
The secondary outcome measure was the 6-point Global Aesthetic Improvement Scale (GAIS) of the treated region.11 The GAIS was used to objectively evaluate overall clinical outcomes, including the severity of horizontal neck lines, cervical skin texture, and the severity of platysmal bands (if applicable). The evaluators graded the treated region as “worse than before” (score –1), “clinically unchanged” (score 0), “slightly improved” (score 1), “moderately improved” (score 2), “markedly improved” (score 3), and “near totally improved” (score 4).
Patient-Evaluated Outcomes
Patients’ satisfaction with the treatment results was evaluated on a 7-point scale questionnaire (–3 = very dissatisfied, –2 = dissatisfied, –1 = slightly dissatisfied, 0 = neutral, 1 = slightly satisfied, 2 = satisfied, 3 = very satisfied) at 1, 3, 6, and 10 months after the final treatment. The anonymous questionnaire (Appendix, available online at www.aestheticsurgeryjournal.com) was conducted on paper. A nurse distributed the survey to the subjects when they came to complete the follow-up visits. In addition, the patients were allowed to state any comments and/or concerns they might have during the study. Patients were also given the opportunity to report any possible adverse events (AEs) they experienced during the study.
Safety
Immediately after each treatment session, the patients indicated their degree of pain on a visual analog scale (VAS) from 0 (no pain at all) to 10 (unbearable pain). AEs were recorded throughout the study.
Statistical Analysis
All quantitative data are expressed as mean [standard deviation]. All categoric data are presented as frequencies or percentages. Analysis was conducted with SPSS 23 (SPSS, Inc., Chicago, IL). An independent t test was used to compare continuous variables. The chi-square test or Fisher’s exact test was used for comparison of the ratios. A value of P < 0.05 was considered statistically significant.
RESULTS
Baseline Demographics
In total, 49 out of 52 Chinese female patients graded between 2 and 3 based upon the adapted Allergan Transverse Neck Lines Scale were enrolled in the study; 48 patients completed all treatments and follow-up visits. The average age of the HA compound filling plus mesotherapy combined treatment group was 37.7 [3.1] years (range, 31-42 years). The average age of the BTX-A treatment group was 36.8 [2.9] years (range, 32-42 years). Three patients were excluded for the following reasons: not meeting the inclusion criteria (n = 1), recent BTX-A injection (n = 1), and declined to participate (n = 1). The average follow-up time was 10 months. One patient dropped out due to low compliance. The patients’ baseline characteristics are listed in Table 1.
Table 1.
Patients’ Baseline Demographics
| Characteristics | HA filling plus mesotherapy combined treatment group | BTX-A treatment group | P value |
|---|---|---|---|
| Gender | |||
| Female | 25 (100) | 23 (100) | — |
| Age (years) | 37.7 [3.1] | 36.8 [2.9] | 0.306 |
| Fitzpatrick skin phototype, n (%) | |||
| III | 14 (56) | 10 (43.5) | — |
| IV | 11 (44) | 13 (56.5) | — |
| Grade of horizontal neck lines, n (%) | |||
| 2 | 2 (8) | 3 (13) | — |
| 2.5 | 10 (40) | 8 (34.8) | — |
| 3 | 13 (52) | 12 (52.2) | — |
Values are n (%) or mean [standard deviation]. BTX-A, botulinum toxin A; HA, hyaluronic acid.
Clinical Outcomes
Improvement of Horizontal Neck Lines and Treated Area
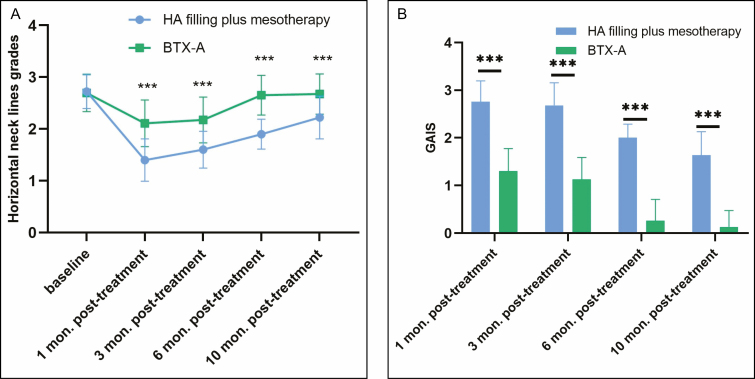
There was no significant difference in the neck line baseline grades between the 2 groups. Overall, for the HA compound filling plus mesotherapy combined treatment group, the grade decreased from 2.72 [0.33] at baseline to 1.4 [0.41], 1.6 [0.35], 1.9 [0.29], and 2.2 [0.41] at the 1-, 3-, 6-, and 10-month follow-ups, respectively. For the BTX-A treatment group, the grade decreased from 2.70 [0.36] at baseline to 2.11 [0.45], 2.15 [0.41], 2.65 [0.38] and 2.67 [0.39] at the 1-, 3-, 6-, and 10-month follow-ups, respectively. A statistically significant difference was observed between the 2 groups at the 1-, 3-, 6-, and 10-month follow-ups (P = 0.000) (Figures 2, 3, 4A).
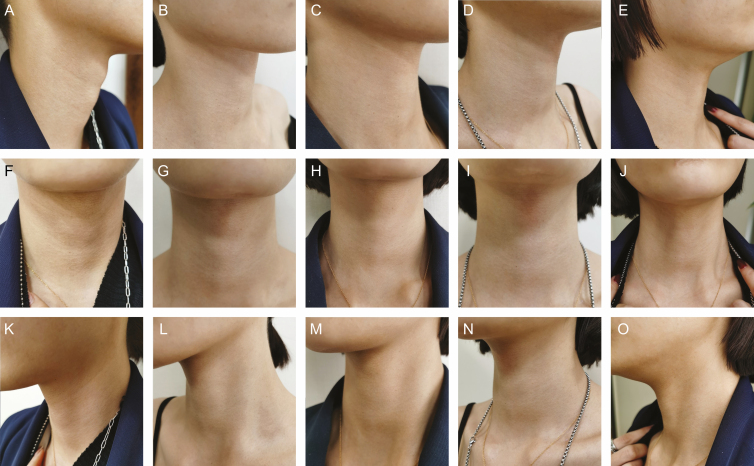
Figure 2.
This 35-year-old female patient was from the HA compound filling and mesotherapy combined treatment group at (A, F, K) baseline, (B, G, L) 1 month after the final treatment, (C, H, M) 3 months after the final treatment, (D, I, N) 6 months after the final treatment, and (E, J, O) 10 months after the final treatment. Neck line baseline grade: 2; procedure: 1.5 mL HA compound filling plus 2.5 mL HA compound mesotherapy, 2 treatment sessions. HA, hyaluronic acid.
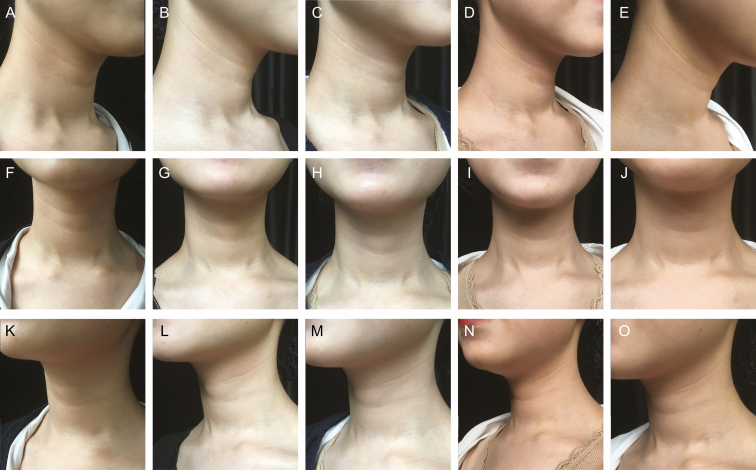
Figure 3.
This female 32-year-old patient was from the botulinum toxin A treatment group at (A, F, K) baseline, (B, G, L) 1 month after the treatment, (C, H, M) 3 months after the treatment, (D, I, N) 6 months after the treatment, and (E, J, O) 10 months after the treatment. Neck line baseline grade: 2.5; procedure: botulinum toxin A 36-U injection, 1 treatment session.
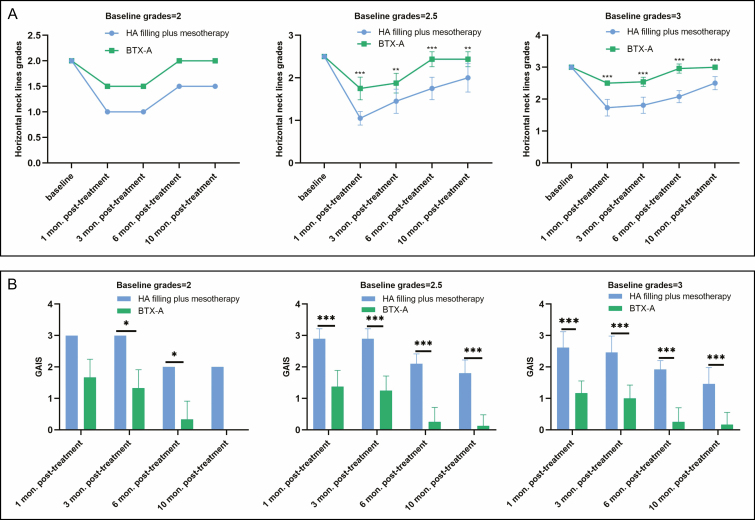
Figure 4.
(A) Neck line grades and (B) Global Aesthetic Improvement Scale scores for the 2 groups. ***P < 0.001.
For the HA compound filling plus mesotherapy combined treatment group, the GAIS scores were 2.8 [0.41], 2.68 [0.48], 2.0 [0.2], and 1.64 [0.49] at the 1-, 3-, 6-, and 10-month follow-ups, respectively. For the BTX-A treatment group, the GAIS scores were 1.30 [0.47], 1.13 [0.46], 0.26 [0.44] and 0.13 [0.34] at the 1-, 3-, 6-, and 10-month follow-ups, respectively. A statistically significant difference was observed between the 2 groups (P = 0.000) (Figure 4B). The improvement and GAIS scores for cases of different baseline grades (2, 2.5, and 3) are shown in Figure 5.
Figure 5.
(A) Improvement and (B) Global Aesthetic Improvement Scale scores for cases of baseline grades 2, 2.5, and 3. *P < 0.05; **P < 0.01; ***P < 0.001.
Patients’ Satisfaction Scores and Comments
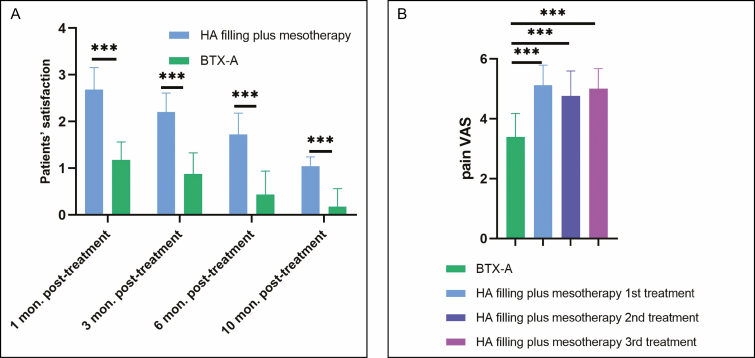
For the HA compound filling plus mesotherapy combined treatment, the patients’ satisfaction ratings were 2.68 [0.48], 2.2 [0.41], 1.72 [0.46], and 1.04 [0.2] at the 1-, 3-, 6-, and 10-month follow-ups respectively, compared with 1.17 [0.39], 0.87 [0.46], 0.43 [0.51], and 0.17 [0.39] for the BTX-A treatment (P = 0.000) (Figure 6A).
Figure 6.
(A) Patients’ satisfaction ratings and (B) pain visual analog scale score for the 2 groups. ***P < 0.001.
Notably, according to the patients’ questionnaire, 16 (64%) patients reported “improvement of topical hyperpigmentation” in the HA filling plus mesotherapy combined treatment group, compared with 4 (17.4%) patients in BTX-A treatment group (P = 0.001). Twenty (80%) patients mentioned “improvement on skin texture, smoother skin” in the HA filling plus mesotherapy combined treatment group, compared with 9 patients (39.1%) in BTX-A treatment group (P = 0.004). In addition, 16 (64%) patients mentioned “long recovery time” for the combined treatment (Table 2).
Table 2.
Patients’ Comments
| Comments | HA filling plus mesotherapy combined treatment group, n (%) | BTX-A treatment group, n (%) | P value |
|---|---|---|---|
| Improvement of topical hyperpigmentation | 16 (64) | 4 (17.4) | 0.001 |
| Obvious pain | 14 (56) | 3 (13) | 0.002 |
| Long recovery time | 16 (64) | 2 (8.7) | 0.000 |
| Nonsustainable efficacy | 9 (36) | 19 (82.6) | 0.001 |
| Too many treatment sessions | 13 (52) | — | — |
| Poor efficacy | 4 (16) | 17 (73.9) | 0.000 |
| Improvement on skin texture and smoother skin | 20 (80) | 9 (39.1) | 0.004 |
BTX-A, botulinum toxin A; HA, hyaluronic acid.
Adverse Events
The HA compound filling plus mesotherapy combined treatment was rated as moderately painful on the VAS. In comparison, the BTX-A treatment was rated as mildly painful (P = 0.000, Figure 6B).
The treatment-associated AEs in both groups are listed in Table 3. Twenty-five cases (100%) experienced erythema in the HA filling plus mesotherapy combined treatment group, compared with 22 (95.7%) in the BTX-A treatment group (P = 0.479). Twenty-five cases (100%) experienced topical edema in the HA filling plus mesotherapy combined treatment group, compared with 2 (8.7%) in the BTX-A treatment group (P = 0.000). Fourteen cases (56%) experienced ecchymosis in the HA filling plus mesotherapy combined treatment group, compared with 7 (30.4%) in the BTX-A treatment group (P = 0.074). Lumps (n = 2, 8%), Tyndall effect (n = 2, 8%), and rashes/itchiness (n = 3, 12%) were observed only in the HA filling plus mesotherapy combined treatment group. Trachyphonia (n = 1, 4.3%) presented only in the BTX-A treatment group. Recovery from erythema, edema, and ecchymosis was significantly shorter in the BTX-A treatment group (P < 0.001) (Table 4). Generally, the AEs were mild/moderate and managed conservatively. Dysphagia, neck weakness, postinflammatory hyperpigmentation, hypopigmentation, infection, and scarring were not observed during the study.
Table 3.
Treatment-Associated AEs and Incidence
| Treatment-associated AEs | HA filling plus mesotherapy combined treatment group, n (%) | BTX-A treatment group, n (%) | P value |
|---|---|---|---|
| Lumps | 2 (8) | — | — |
| Erythema | 25 (100) | 22 (95.7) | 0.479 |
| Topical edema and swelling | 25 (100) | 2 (8.7) | 0.000 |
| Ecchymosis | 14 (56) | 7 (30.4) | 0.074 |
| Tyndall effect | 2 (8) | — | — |
| Trachyphonia | — | 1 (4.3) | — |
| Rashes and itchiness | 3 (12) | — | — |
AE, adverse event; BTX-A, botulinum toxin A; HA, hyaluronic acid.
Table 4.
Duration of Treatment-Associated AEs
| Treatment-associated AEs | Duration, HA filling plus mesotherapy combined treatment group (days) | Duration, BTX-A treatment group (days) | P value |
|---|---|---|---|
| Lumps | 99 [14.1] | — | — |
| Erythema | 10.9 [1.7] | 4.4 [0.9] | 0.000 |
| Topical edema and swelling | 10.7 [1.3] | 2.5 [0.7] | 0.000 |
| Ecchymosis | 12.2 [1.1] | 10.3 [0.8] | 0.001 |
| Tyndall effect | 102.5 [9.2] | — | — |
| Trachyphonia | — | 35 | — |
| Rashes and itchiness | 12.7 [2.1] | — | — |
Values are mean [standard deviation]. AE, adverse event; BTX-A, botulinum toxin A; HA, hyaluronic acid.
Discussion
Distinct from the other signs of age-related neck degeneration, horizontal neck lines are not necessarily the results of photoaging or intrinsic aging.2 Reducing the “age gap” between the facial area and wrinkled cervical area is requested by increasing numbers of beauty seekers. Skin thickness and fat accumulation patterns differ in many respects between Asians and Caucasians. Thicker skin and less severe laxity problems make Asians good candidates for nonsurgical neck rejuvenation approaches.13
Energy devices have demonstrated a major benefit when treating skin laxity as a standalone treatment or as a complement to fat removal procedures. Thermally controlled laser-assisted energy subcutaneously leads to reorganization of the reticular dermis and generation of new collagen, and hence improvement in skin surface, texture, and laxity. However, significant delays in re-epithelization, the relative paucity of adnexal structures, and the superficial vascular network of the neck increase the risks associated with aggressive laser resurfacing.25,26 Other nonablative photoelectromagnetic manipulations, fractionated devices, and heated radiofrequency sessions may tighten the skin, with little effect on lessening rhytides.9,27
Horizontal neck lines have been found to be significantly associated with the attachment of the superficial musculoaponeurotic system to the skin, and injection of neuromodulators into platysmal bands has been shown to soften horizontal neck lines without any additional treatments in relatively young cases with minimal skin laxity.12,16,28 Similar to previous research,7 our study demonstrated that BTX-A treatment produced a marginal “wrinkle-softening” effect, presumably by weakening the superficial fibers of the platysma muscle and allowing the skin to conform to the underlying neck silhouette. In addition, the effect of smoothening the cervical skin was observed in some patients, mostly due to toxin intradermal effects targeting the sebaceous glands, the sweat glands, and the superficial muscular fibers.7 Although the efficacy of a single BTX-A treatment session gradually decreased within 4 to 6 months, better and longer-lasting results might be expected with repeated applications. We speculate that BTX-A treatment could be deemed a safe and effective therapeutic modality for young patients with mild horizontal neck lines (eg, baseline grade 1 or 1.5), but who at the same time want to avoid recuperation time or are unwilling to undertake the potential risks associated with other procedures.
To our knowledge, this is the first study employing a combined treatment of non–cross-linked HA compound filling plus mesotherapy for the correction of cervical horizontal lines. Theoretically, like furrows on the face, neck lines are often best corrected with dermal fillers, which play a more important role than neuromodulators and should be used first to provide structural support.2 Ma and co-workers proved that the effect and maintenance time of autologous keratin and fibroblast filler for neck wrinkles were better than the HA control.6 Lu and co-workers corrected horizontal neck lines using stromal vascular fraction gel and achieved a better and longer improvement compared with BTX-A injection.7 Nevertheless, preparation of autologous fillers requires laboratory apparatus and a series of procedures. In addition, the patients need to go through multiple procedures including local or general anesthesia, adipose tissue suction, blood collection, and skin tissue collection. Presumably, autologous fillers are not acceptable for patients who prefer to alleviate their neck lines by a lunch-break aesthetic treatment, given both mechanical processing of lipoaspirates and primary cell culture are time consuming. Commercially available ready-to-use fillers would be more applicable in this scenario. Currently the State Food and Drug Administration–approved indication for most commercially available HA dermal fillers is for the treatment of nasolabial folds. These cross-linked HA dermal fillers are not ideal candidates for neck line treatment, because the risk of lumps is high. Similarly, we did not consider cross-linked and expensive collagen fillers as suitable candidates. The non–cross-linked HA compound used in our study is the only product that has been approved for the correction of horizontal neck lines. The non–cross-linked characteristics made the combined treatment of filling plus mesotherapy clinically feasible. Additionally, an ideal filler should be affordable for most patients, given repeated treatments are needed.
The unique structure of the intervening superficial platysma muscle with minimal fat between the skin and fascia makes it difficult to perform HA filler injection in the neck and the results might be unpredictable. Thus, selection of the appropriate dermal filler is paramount. These cases demonstrated that effacement of the transverse neck lines could be achieved with injection of a dermal filler with the appropriate rheologic properties. HA fillers with low viscosity and elasticity are frequently employed due to their soft and easily molded properties.2 Additionally, the low-viscosity nature facilitated a comfortable injection and reduced the potential of nodules and the Tyndall effect. The non–cross-linked HA in the compound formula achieved the immediate volume-adding and furrow-supporting effect for the first 2 to 3 weeks. A previous study demonstrated that a formulation of HA enriched with amino acids inhibited fibroblast senescence induced by oxidative stress both in vitro and in vivo. 29l-Carnosine, proline, glycine, alanine, and vitamin B2 provided fundamental active substances for the subsequent dermal matrix neogenesis, collagen synthesis, and antioxidation.30, 31 According to our study, the results of the combined treatment of HA filling plus mesotherapy lasted for 6 to 8 months. The cases in our study received 2 or 3 treatment sessions in total. More sustained efficacy longer than 6 to 8 months could be expected if repeated treatments were performed.
This was also the first research utilizing mesotherapy for the neck area. Although mesotherapy has been reported for treatment of a variety of medical and cosmetic conditions of the face and scalp,32-35 until now its usage in the cervical area has been confined to the management of chronic neck pain in spondylarthrosis.36 Transdermal microinjections of the therapeutic substances mentioned above into the superficial papillary dermis contributed to maintenance and/or recovery of a youthful cervical skin texture. Theoretically, the multicomponent filling plus mesotherapy helps to maintain fibroblast function and improve extracellular matrix component biosynthesis, as well as to reverse the degeneration of elastin and the continuous transepidermal water loss, all of which occur during the aging process.23 Based upon our study, the combination of HA filling and mesotherapy seemed to achieve synergistic effects by targeting multiple pathogenetic factors involved in horizontal neck lines. It was worth noting that our “filling plus mesotherapy” represents a treatment regimen, rather than just a method. In addition to the commercially available HA product used in our study, more options such as platelet-rich plasma, platelet-rich fibrin, and even stem cell products could be taken into consideration as well. According to the laws of China, stem cell therapy can only be conducted in teaching hospitals for research purposes. Platelet-rich plasma and platelet-rich fibrin treatment can only be performed legally in hospitals incorporating a department of hematology. Most private medical aesthetic hospitals or clinics are not entitled to deploy these 2 treatments.
A few technical points should be noted. First, to avoid overcorrection and lumpiness, we advise placement of the bevel upward during the injection and not to inject too superficially. The injection depth might be regarded as appropriate when the shape of the needle, rather than its color, can be observed. Second, we recommend a 34G needle for injection, because a 32G needle might cause hemorrhage and bruising, and a 35G needle might lead to less smooth bolus. Third, we recommend 2.5 mL of HA compound for mesotherapy delivered by a hydrolifting apparatus to achieve a homogeneous local bioavailability, although it could be multipoint injected into the dermis as well. Fourth, no radiofrequency or laser treatment should be administered within the following 4 to 6 weeks to avoid accelerated HA compound degradation.
Patient selection was fundamental to guarantee a predictable and satisfactory outcome. The mean age of the patients in the HA compound filling plus mesotherapy treatment group was 37.7 [3.1] years with 18 patients (72%) in their 30s, which we deemed relatively young. For most Asian patients in their 30s and early 40s, the predominant cervical concerns are neck lines and local hyperpigmentation, rather than sagging, jowls, and platysmal bands. Although significant improvement in the horizontal neck lines was observed in our study, the efficacy of HA compound filling plus mesotherapy treatment could not simply be generalized to the population who presented a more complicated baseline condition. For instance, this regimen could not correct skin laxity or submental fat pads, and patients with baseline grade 4 (extreme, noneffaceable transverse neck furrows with redundant skin 24) would not be appropriate candidates either. Multimodal approaches incorporating surgery, energy devices, filling, and BTX-A might be more applicable for these cases, which need to be tailored individually based upon each case’s specific conditions.
The patients’ comments revealed several major concerns about the filling plus mesotherapy combined treatment: pain, recovery time, treatment frequency, and duration of efficacy. Pain management might be fulfilled by optimizing the local anesthesia modality and/or the physicochemical properties of the HA compound. Developing novel filler compounds might contribute to reducing the recovery time and number of treatment sessions. Additionally, given that de-nerving the muscle would lessen local tension, and hence possible filler translocation and degeneration, further investigation including neuromodulators would be necessary. Theoretically, less toxin dosage might be needed as compared to toxin monotherapy.
There are several limitations to the present study worthy of further exploration. For instance, skin biopsy was not performed due to cosmetic concerns. In addition, the patients received 2 or 3 treatment sessions in total, and therefore further studies are required to determine the efficacy and safety of repeated treatments.
Conclusions
This prospective, randomized study has demonstrated that compared with BTX-A injection, a combined treatment of HA compound filling plus mesotherapy significantly improved moderate-to-severe horizontal neck lines and achieved a high level of patient satisfaction.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The work was supported by the following projects and organizations: Science and Technology Department of Sichuan Province project (No. 2020YJ0058); Post-Doctor Research Project, West China Hospital, Sichuan University (No. 2020HXBH050) (Chengdu, Sichuan, China); China Postdoctoral Science Foundation (No. 2021M692292); National Natural Science Foundation of China (No. 82103753) (Beijing, China). The funding was used to pay the study subjects’ transport costs and publication open access charges.
References
- 1. Qiu H, Jiang Y, Chen C, Wu K, Wang H. The effect of different diameters of fat converters on adipose tissue and its cellular components: selection for preparation of nanofat. Aesthet Surg J. 2021;41(11):NP1734-NP1744. [DOI] [PubMed] [Google Scholar]
- 2. Lee SK, Kim HS. Correction of horizontal neck lines: our preliminary experience with hyaluronic acid fillers. J Cosmet Dermatol. 2018;17(4):590-595. [DOI] [PubMed] [Google Scholar]
- 3. Minokadeh A, Black JM, Jones DH. Effacement of transverse neck lines with VYC-15L and cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2018;44 Suppl 1:S53-S56. [DOI] [PubMed] [Google Scholar]
- 4. Calisti A, Elattar A. Three-dimensional vision: circumferential nonsurgical neck rejuvenation. Dermatol Surg. 2017;43(9):1186-1189. [DOI] [PubMed] [Google Scholar]
- 5. Chao YY, Chiu HH, Howell DJ. A novel injection technique for horizontal neck lines correction using calcium hydroxylapatite. Dermatol Surg. 2011;37(10):1542-1545. [DOI] [PubMed] [Google Scholar]
- 6. Wang Y, Wang B, Zhang Q, Ma J. New soft tissue filler derived from autologous keratin and fibroblast for neck wrinkles. J Cosmet Dermatol. 2018;17(4):600-605. [DOI] [PubMed] [Google Scholar]
- 7. Cai J, Wang J, Hu W, Lu F. Mechanical micronization of lipoaspirates for the treatment of horizontal neck lines. Plast Reconstr Surg. 2020;145(2):345-353. [DOI] [PubMed] [Google Scholar]
- 8. Tseng F, Yu H. Treatment of horizontal neck wrinkles with hyaluronic acid filler: a retrospective case series. Plast Reconstr Surg Glob Open. 2019;7(8):e2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Azuelos A, SidAhmed-Mezi M, La Padula S, Aboud C, Meningaud JP, Hersant B. High-intensity focused ultrasound: a satisfactory noninvasive procedure for neck rejuvenation. Aesthet Surg J. 2019;39(8):NP343-NP351. [DOI] [PubMed] [Google Scholar]
- 10. Jones IT, Guiha I, Goldman MP, Wu DC. A randomized evaluator-blinded trial comparing subsurface monopolar radiofrequency with microfocused ultrasound for lifting and tightening of the neck. Dermatol Surg. 2017;43(12):1441-1447. [DOI] [PubMed] [Google Scholar]
- 11. Boen M, Alhaddad M, Wu DC, Goldman MP. A prospective double-blind, placebo-controlled clinical trial evaluating the efficacy of a novel combination of hyaluronic acid serum and antioxidant cream for rejuvenation of the aging neck. J Clin Aesthet Dermatol. 2020;13(11):13-18. [PMC free article] [PubMed] [Google Scholar]
- 12. Jeon H, Kim T, Kim H, Cho SB. Multimodal approach for treating horizontal neck wrinkles using intensity focused ultrasound, cohesive polydensified matrix hyaluronic acid, and IncobotulinumtoxinA. Dermatol Surg. 2018;44(3):421-431. [DOI] [PubMed] [Google Scholar]
- 13. Doh EJ, Kim J, Lee DH, Park JY. Neck rejuvenation using a multimodal approach in Asians. J Dermatolog Treat. 2018;29(4):400-404. [DOI] [PubMed] [Google Scholar]
- 14. Paganelli A, Mandel VD, Pellacani G, Rossi E. Synergic effect of plasma exeresis and non-cross-linked low and high molecular weight hyaluronic acid to improve neck skin laxities. J Cosmet Dermatol. 2020;19(1):55-60. [DOI] [PubMed] [Google Scholar]
- 15. Casabona G, Nogueira Teixeira D. Microfocused ultrasound in combination with diluted calcium hydroxylapatite for improving skin laxity and the appearance of lines in the neck and décolletage. J Cosmet Dermatol. 2018;17(1):66-72. [DOI] [PubMed] [Google Scholar]
- 16. Fabi SG, Burgess C, Carruthers A, et al. Consensus recommendations for combined aesthetic interventions using botulinum toxin, fillers, and microfocused ultrasound in the neck, décolletage, hands, and other areas of the body. Dermatol Surg. 2016;42(10):1199-1208. [DOI] [PubMed] [Google Scholar]
- 17. Jabbour SF, Kechichian EG, Awaida CJ, Tomb RR, Nasr MW. Botulinum toxin for neck rejuvenation: assessing efficacy and redefining patient selection. Plast Reconstr Surg. 2017;140(1):9e-17e. [DOI] [PubMed] [Google Scholar]
- 18. Prager W, Bee EK, Havermann I, Zschocke I. IncobotulinumtoxinA for the treatment of platysmal bands: a single-arm, prospective proof-of-concept clinical study. Dermatol Surg. 2015;41 Suppl 1:S88-S92. [DOI] [PubMed] [Google Scholar]
- 19. Levy PM. Neurotoxins: current concepts in cosmetic use on the face and neck—jawline contouring/platysma bands/necklace lines. Plast Reconstr Surg. 2015;136(5 Suppl):80S-83S. [DOI] [PubMed] [Google Scholar]
- 20. Awaida CJ, Jabbour SF, Rayess YA, El Khoury JS, Kechichian EG, Nasr MW. Evaluation of the microbotox technique: an algorithmic approach for lower face and neck rejuvenation and a crossover clinical trial. Plast Reconstr Surg. 2018;142(3):640-649. [DOI] [PubMed] [Google Scholar]
- 21. Steinsapir KD. Microbotox of the lower face and neck: evolution of a personal technique and its clinical effects. Plast Reconstr Surg. 2016;138(6):1072e-1073e. [DOI] [PubMed] [Google Scholar]
- 22. Lee JH, Park YG, Park ES. A prospective observational study of the effectiveness and safety of botulinum toxin in the horizontal neck lines. Aesthetic Plast Surg. 2018;42(5):1370-1378. [DOI] [PubMed] [Google Scholar]
- 23. Plachouri KM, Georgiou S. Mesotherapy: safety profile and management of complications. J Cosmet Dermatol. 2019;18(6):1601-1605. [DOI] [PubMed] [Google Scholar]
- 24. Jones D, Carruthers A, Hardas B, et al. Development and validation of a photonumeric scale for evaluation of transverse neck lines. Dermatol Surg. 2016;42 Suppl 1:S235-S242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. DiBernardo GA, DiBernardo BE. Prediction of treatment outcomes for neck rejuvenation utilizing a unique classification system of treatment approach using a 1440-nm side-firing laser. Aesthet Surg J. 2018;38(Supplement_2):S43-S51. [DOI] [PubMed] [Google Scholar]
- 26. Han TY, Lee JW, Lee JH, et al. Subdermal minimal surgery with hyaluronic acid as an effective treatment for neck wrinkles. Dermatol Surg. 2011;37(9):1291-1296. [DOI] [PubMed] [Google Scholar]
- 27. de Oliveira TC, Rocha SF, Ramos DG, Ramos CG, Carvalho MV, Ramos MG. Effects of multipolar radiofrequency and pulsed electromagnetic field treatment for face and neck rejuvenation. Dermatol Res Pract. 2017;2017:4146391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Vanaman M, Fabi SG, Cox SE. Neck rejuvenation using a combination approach: our experience and a review of the literature. Dermatol Surg. 2016;42 Suppl 2:S94-S100. [DOI] [PubMed] [Google Scholar]
- 29. Cirillo N, Vicidomini A, McCullough M, et al. A hyaluronic acid-based compound inhibits fibroblast senescence induced by oxidative stress in vitro and prevents oral mucositis in vivo. J Cell Physiol. 2015;230(7):1421-1429. [DOI] [PubMed] [Google Scholar]
- 30. Bingül İ, Yılmaz Z, Aydın AF, Çoban J, Doğru-Abbasoğlu S, Uysal M. Antiglycation and anti-oxidant efficiency of carnosine in the plasma and liver of aged rats. Geriatr Gerontol Int. 2017;17(12):2610-2614. [DOI] [PubMed] [Google Scholar]
- 31. Solano F. Metabolism and functions of amino acids in the skin. Adv Exp Med Biol. 2020;1265:187-199. [DOI] [PubMed] [Google Scholar]
- 32. Lee JC, Daniels MA, Roth MZ. Mesotherapy, microneedling, and chemical peels. Clin Plast Surg. 2016;43(3):583-595. [DOI] [PubMed] [Google Scholar]
- 33. Melo DF, de Mattos Barreto T, Plata GT, Araujo LR, Tortelly VD. Excellent response to mesotherapy as adjunctive treatment in male androgenetic alopecia. J Cosmet Dermatol. 2020;19(1):75-77. [DOI] [PubMed] [Google Scholar]
- 34. Brandi C, Cuomo R, Nisi G, Grimaldi L, D’Aniello C. Face rejuvenation: a new combinated protocol for biorevitalization. Acta Biomed. 2018;89(3):400-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. D’Aloiso CM, Senzolo M. Efficacy of dermal redensification in chronoaged face: quantitative volumetric assessment. J Cosmet Dermatol. 2020;19(1):199-204. [DOI] [PubMed] [Google Scholar]
- 36. Ferrara PE, Nigito C, Maccauro G, Ferriero G, Foti C, Ronconi G. Efficacy of diclofenac mesotherapy for the treatment of chronic neck pain in spondylartrosis. Minerva Med. 2019;110(3):262-264. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.