Abstract
Non-traumatic osteonecrosis of the femoral head is the main cause of disability in young individuals and incurs major health care expenditure. The lifestyle changes in recent years, especially increased use of hormones and alcohol consumption, has greatly increased the incidence of femoral head necrosis. The underlying causes and risk factors of osteonecrosis of the femoral head are increasingly being elucidated, which has led to the development of novel surgical and non-surgical treatment options. Although the main goal of any treatment method is prevention and delaying the progression of disease, there is no common consensus on the most suitable method of treatment. The present review discussed the latest developments in the etiology and treatment methods for femoral head necrosis.
Keywords: femoral head necrosis, platelet rich plasma, core decom-pression, bone-marrow stem cell transplantation, joint replacement
1. Introduction
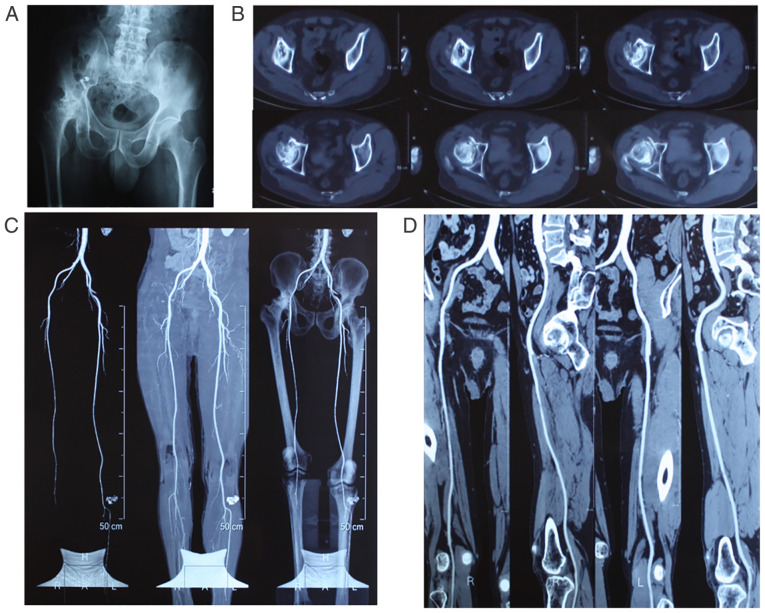
Non-traumatic osteonecrosis of the femoral head (NONFH) is the result of impaired blood supply to the femoral head and structural and functional disruption of local articular cartilage, subchondral bone and blood vessels (Fig. 1), which culminate in subchondral osteonecrosis, femoral head collapse and hip joint pain (1). Mont et al (2) estimate that the total number of patients with NONFH worldwide could reach >20 million in the next decade. The pain and limited hip joint mobility resulting from femoral head necrosis can seriously affect the quality of life of the patient.
Figure 1.
Imaging results of non-traumatic femoral head necrosis. (A) Representative X-ray showing lack of any joint space in the right hip joint and collapse of the acetabulum and femoral head, along with altered structure. (B) Representative computerized tomography image showing stenosis of the hip joint space, hollow femoral head and abnormal calcification. (C) Angiography of the lower extremities showing insufficient supply from blood vessels in the right femoral head. (D) Angiography of one side of the lower extremity showing properly functioning main blood vessels.
NONFH is a chronic disease with risk factors including long-term steroid use, excessive alcohol consumption and other underlying disease (3,4). Early diagnosis is difficult and there is currently no specific diagnostic standard or treatment that can reverse early-stage femoral head necrosis. Therefore, most patients with NONFH already show substantial necrosis at the time of diagnosis. The early-stage treatments are typically palliative and experimental, rather than preventive and curative. Given the personal and social burden of NONFH, the optimal treatment method is based on the individual needs of the patients. The most suitable course of action is to perform appropriate physical and minimally invasive surgery when first diagnosed. In case the symptoms are not sufficiently relieved within a reasonable period, hip replacement surgery needs to be performed. The present review examined recent developments regarding the treatment methods of NONFH and the underlying mechanisms.
2. Epidemiology
NONFH has a complex etiology and the most common causes are hormonal disturbances and excessive alcohol consumption. The risk of osteonecrosis is significantly higher in adolescents and adult compared with children (3,4). Every year in the United States alone ~10,000-20,000 new cases of ONFH are diagnosed; it is common in individuals aged between 20-50 years and 5-12% of the patients eventually undergo total hip replacement (5). In India, the mean age of onset of femoral head necrosis is 34.71 years and the male to female ratio is 5:1(3). More than one-third (37.3%) of patients with ONFH have a history of long-term steroid usage, whereas 21.3% of the cases are idiopathic and chronic alcoholism is the underlying cause in 20.1% of the patients (3). In Japan, the incidence of femoral head necrosis is relatively low in men aged 40-49 years and significantly higher in individuals aged >50 years. Among women, the incidence rate is lower in the 16-29 years age bracket and increases markedly in the 30-39 and 60-69 age groups (4). In addition, 48 and 35% of ONFH cases among males are respectively alcohol- and hormone-induced. By contrast, 70% of the cases among females have a hormonal basis (6). Studies have shown that high-dose corticosteroids (>40 mg/day) significantly increase the risk of NONFH (7,8) and every 10 mg increase in the dose increases the incidence rate by 3.6% (9).
3. Pathogenesis
Studies have shown that femoral head necrosis is associated with several underlying diseases (Table I), including trauma or surgery of the hip joint, excessive corticosteroid production, hyperlipidemia, abnormal blood pressure, autoimmune diseases, endotoxin poisoning, smoking, excessive alcohol consumption and blood hypercoagulability (10). All of these pathological changes can eventually lead to vascular damage, bone marrow infarction and avascular necrosis.
Table I.
Underlying causes of NONFH.
| NONFH type | Causes |
|---|---|
| Non-traumatic osteonecrosis | Antituberculosis III deficiency, lack of protein C or S, anti-activated protein C, deficiency of the plasminogen activator, research progress of plasminogen activator inhibitor, COVID-19 and severe acute respiratory syndrome |
| Secondary hypercoagulable state | Steroid intake, alcoholism, myelodysplastic syndrome, pregnancy, contraceptive use, hyperlipidemia, collagen disease and Eller-Danlos syndrome, Raynaud's disease, diabetes, and antiphospholipid antibodies |
| Blood diseases | Hemophilia, hemoglobin disease and Erythrocytosis |
| Metabolic diseases | Hyperparathyroidism, gout, Cushing's disease and Gaucher's disease |
| Digestive diseases | Pancreatin, ulcerative colitis and chronic diseases |
| Other risk factors | Smoking, decompression sickness, radiation and hemodialysis |
NONFH, non-traumatic osteonecrosis of the femoral head.
Hormones
Long-term steroid use is the most common cause of NONFH (11), as it can lead to microthrombosis and impede blood and oxygen supply to the femoral head, resulting in osteonecrosis (12). Kuroda et al (13) followed up 78 systemic lupus erythematosus (SLE) patients receiving high-dose prednisolone treatment and found that 21 patients developed ONFH three months after starting treatment and that the cholesterol and triglyceride levels of the patients increased significantly within 4 weeks of hormone therapy. Wu et al (14) identified several non-coding RNAs involved in the development and progression of hormonal ONFH. Yue et al (15) found that miR-132-3p and miR-335 probably serve an important role in hormone-induced ONFH by inducing apoptosis of endothelial cells via the Wnt, Foxo and Rap1 signaling pathways.
Alcohol
Alcohol abuse is one of the main risk factors of bone deterioration. Ethanol impairs the proliferation of human bone mesenchymal stem cells (hBMSCs) and induces their differentiation into adipocytes, which eventually leads to bone loss and structural damage (16,17). Recent studies have shown that abnormal bone metabolism in patients with alcoholic ONFH is associated with the inhibition of the Akt/GSK-3β/β-catenin pathway in bone mesenchymal stem cells (BMSCs), which is negatively affected by ethanol-induced increase in tensin homology phosphatase (18).
Other diseases
Sickle cell leukemia can lead to microthrombosis, resulting in osteonecrosis and occasionally osteomyelitis (19). Further aggravation can also lead to hemolysis, increased red blood cell activity and expansion of the bone marrow cavity (19). Femoral head necrosis in patients with HIV is associated with hyperlipidemia and drug treatment (20). A meta-analysis conducted by Matos et al (20) shows that protease inhibitors can cause hyperlipidemia and ultimately lead to osteonecrosis. Mazzotta et al (21) conducted a multi-center case-control study wherein the highly active antiretroviral therapy significantly increased the triglyceride and cholesterol levels of patients with HIV and altered the total IgE levels in the serum. In a study on 539 patients with severe acute respiratory syndrome who received different types of steroid therapy, 39.5% of the males and 19.3% of the females were diagnosed with ONFH. In addition, ONFH was more common in patients aged 20-49 years (25.9%) compared with that in the 50-59 years group (6.3%). The incidence of ONFH in patients receiving one steroid was 12.5% as opposed to 28.6 and 37.1% in patients treated respectively with two and three types of steroids (37.1%) (22). The COVID-19 patients are also at a higher risk of developing ONFH. The COVID-19 virus is more sensitive to ONFH and the cumulative dose of steroids is smaller (23).
4. Treatment strategies
The current treatments for NONFH can be classified into non-surgical and surgical methods (Fig. S1). The non-surgical approaches include protective weight bearing, physical therapy and drug therapy and examples of surgical intervention are non-vascular transplantation, osteotomy, core decompression, vascularized transplantation and joint replacement. Some therapeutic strategies developed in recent years for treating avascular necrosis of the femoral head are discussed in the following sections.
Protective load bearing
The patients are advised to lose weight, reduce the force exerted on the femoral head of the affected side, avoid mutual and reverse movement, use crutches for walking and avoid sitting or lying in bed for a long period of time (24). Studies show (21,24) that local non-weight bearing can reduce the occurrence of femoral head deformity following ischemic osteonecrosis by increasing revascularization and reducing bone resorption in the infarcted epiphysis, although it does not stimulate new bone formation. Nevertheless, it can optimize osteogenic therapies and the healing of necrotic femoral heads by controlling the rate of bone resorption (24). Therefore, weight bearing can prevent the occurrence and development of osteonecrosis, especially femoral head collapse, in subjects at the early stage of the disease [association research circulation osseous (ARCO Ia)] and with small lesions. However, this non-surgical intervention is ineffective for 80-90% of the patients with ONFH (25,26).
Pharmacological agents
Lipid-lowering agents, anticoagulants, vasoactive substances, statins and bisphosphonates have been used to prevent and treat femoral head necrosis at the early-stages. Bisphosphonates such as alendronate (trade name Fosamax) were originally prescribed to treat osteoporosis, They improve bone density by reducing osteoclast-mediated bone resorption (27-33). Animal studies and clinical trials have shown that bisphosphonates can accelerate the recovery of joint function, delay disease progression, reduce pain and lower the risk of femoral head collapse associated with ONFH without significant side effects (27-33). Nevertheless, the therapeutic effect of bisphosphonates against corticosteroid-induced ONFH is controversial (27) and there is no clear recommendation for the dose and duration of treatment. Overall, bisphosphonate drugs can be considered for treating femoral head necrosis caused due to metabolic disturbances.
Prostacyclin is a vasodilatory agent and an antagonist of thromboxane that improves blood flow by preventing platelet aggregation. While short-term use of prostacyclin is associated with significant improvements in the clinical and radiological indices of early-stage ONFH, the long-term efficacy is still being evaluated (34). One study showed that a combination of intravenous prostacyclin and core decompression can alleviate the symptoms of osteonecrosis (35). Iloprost is a synthetic analog of prostacyclin that is routinely used to treat pulmonary arterial hypertension and has proved to effective against bone marrow edema and ONFH (36,37). A prospective study on 30 cases of ONFH with coagulopathy showed that 53% of the patients did not progress to Ficat and Arlet stages I and II following treatment with the anticoagulant enoxaparin. In addition, the combination of enoxaparin, ginkgo biloba extract (vasodilators) and sildenafil improved femoral head perfusion in an animal model of steroid-induced ONFH (36,37).
Studies show that the development of ONFH in the hip joint is associated with an increase in the number and size of circulating fat cells (38,39). Therefore, the lipid-lowering statins that are used to treat steroid-related inflammatory disorders (38,39) can potentially be therapeutic against ONFH. Indeed, lovastatin decreases adipogenesis and bone death in a chicken model of steroid-induced ONFH and increases the expression of osteogenic genes in bone marrow cells (40). One study on patients receiving statins and high-dose steroids showed that after an mean follow-up period of 7.5 years, the incidence of ONFH was 1% at annual follow-up, as opposed to 3% usually reported by patients receiving high-dose steroids. Therefore, statins may prevent osteonecrosis in subjects with long-term steroid use (38).
Traditional Chinese medicine formulations have been used to treat osteonecrosis for decades. Ye et al (41) showed that the ginsenoside Rb1 inhibits steroid-induced avascular necrosis, osteonecrosis and the elevation of serum osteocalcin in a rat model of Steroid-induced avascular necrosis of the femoral head (SANFH) by blocking the vascular endothelial growth factor (VEGF)/runt-related transcription factor 2/bone morphogenetic protein 2 signaling pathway. In addition, Rb1 also reduces inflammation, oxidative stress, total cholesterol and low/high lipoprotein levels, alkaline phosphatase activity and bone calcium loss in the SANFH rats.
Extracorporeal shock wave therapy (ESWT)
High-energy ESWT is a non-invasive approach that has been used for treating ONFH since the end of the last century (42,43). Its potential mechanisms of action include restoration of tissue oxygenation, reduction of bone marrow edema and increased blood supply to focal lesions (42,43). ESWT is a promising alternative to the more invasive surgical methods currently used to treat ONFH at different stages. Ludwig et al (44) subjected 22 patients with ONFH to the shock wave treatment and assessed the visual analog scale (VAS) and HHS scores after one year follow-up. The VAS scores of the patients decreased from 8.5 points before surgery to 1.2 points and the HHS scores increased from 43.3 points to 92 points, indicating high efficacy of ESWT. Other studies have shown that ESWT is only effective against early-stage ONFH (45). Algarni and Al Moallem (46) treated 21 patients (33 hips) with early-stage ONFH using this approach and found that the VAS scores and HHS scores of 21 hip joints improved significantly after 8 months. After 5 years, 4 cases received THA treatment. Among them, 26 cases showed no significant progression from the first stage. Magnetic resonance imaging (MRI) results showed that in 23 cases, bone marrow edema was significantly reduced. Thus, ESWT significantly improved the quality of life of patients with ONFH, delayed the progression of disease and avoided the need for total hip arthroplasty (THA). Xie et al (43) retrospectively analyzed the data of 31 patients with ONFH (44 hips) who underwent ESWT and were followed up over an mean duration of 130.6 months. The imaging findings showed lack of disease progression in all stage I, 64.3% of stage II and 12.5% of stage III hips. Thus, ESWT is a suitable option for ARCO I and II patients.
Pulsed electromagnetic field
In 1974, Bassett et al (47) discovered that pulsed electromagnetic fields (PEMF) can promote fracture repair and subsequent studies have shown that PEMF can also control inflammation and repair articular cartilage in patients with osteoarthritis and joint surgery (48,49). Seber et al (50) reported the cases of two Ficat II patients with ONFH who were subjected to PEMF therapy daily for 10 h over a period of 6 months and exhibited a significant improvement in their condition. Massari et al (51) treated 66 patients with ONFH (76 hips) with PEMF as above and followed their progress for 28 months. While 94% of the patients at Ficat stages I and II showed improvement, most Ficat stage III patients deteriorated and finally had to receive THA treatment. Thus, PEMF may be an effective option for early-stage ONFH. However, only a few studies have reported the efficacy of PEMF in the treatment of ONFH, which therefore warrants further investigation. In summary, this method can be beneficial for patients with ARCO stage I and II ONFH.
Hyperbaric oxygen therapy (HBO)
HBO has proved to be highly effective against early stages of femoral head necrosis, particularly in Asian populations (52-55). In a recent study (56) on 19 patients with stage II ONFH, 12 (52.2%) underwent core decompression (CD) surgery and 11 (47.8%) received HBO treatment. Over the mean follow-up period of 34.2±18.4 months, 66.7% of patients in the CD group and 81.8% of patients in the HBO group showed satisfactory hip joint function. However, 8 patients (34.7%) progressed to a higher radiological stage during the first year of follow-up and the progression rate was similar in both groups. Studies have also shown that HBO therapy is as effective as CD for treating non-traumatic pre-collapsed femoral head AVN and therefore can be used a non-invasive alternative (52-56). The clinical efficacy of HBO depends on the synthesis of growth factors, which promote wound healing and reduce post-ischemia and post-inflammatory damage (57,58). In addition, the increase in hydrostatic pressure compresses all gas-filled spaces in the human body (Ball's law), which can reverse decompression-related diseases (59,60). HBO therapy reduces edema, increases tissue oxygenation and restores venous drainage in the affected bone area by inducing proliferation of endothelial progenitor cells, promoting neo-angiogenesis and improving local microcirculation (57,61-65). A 2017 systematic review found that HBO therapy is effective against early-stage ONFH and may reduce cellular ischemia by increasing the concentration of extracellular oxygen (66). In summary, HBO therapy can be considered for the prevention and treatment of early-stage femoral head necrosis.
The literature related to the non-surgical treatment methods for NONFH are summarized in Table II.
Table II.
Non-surgical treatment of NONFH.
| First author/s, year | Treatment method | Quantity (hip) | Follow-up time (month) | Indications | (Refs.) |
|---|---|---|---|---|---|
| Xie K, 2018 | ESWT | 44 | 130.6 | ARCO I-III | (43) |
| Algarni AD, 2018 | 33 | 8 | ARCO I-II | (46) | |
| Massari L, 2006 | PEMF | 76 | 28 | Ficat I-II | (51) |
| Moghamis I, 2021 | HBO | 11 | 34.2 | Steinberg II | (56) |
NONFH, non-traumatic osteonecrosis of the femoral head; ESWT, energy extracorporeal shock wave therapy; PEMF, pulsed electromagnetic fields; HBO, hyperbaric oxygen.
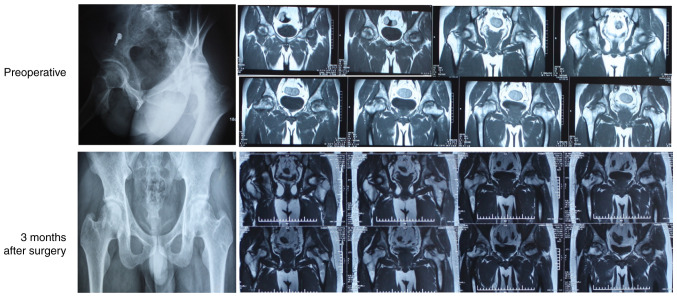
CD
CD is the commonest surgical procedure for early-stage osteonecrosis and is used to relieve pain and promote bone regeneration and repair (67,68). As shown in Fig. 2, pure CD can repair and delay the progression of NONFH (67) by reducing intramedullary pressure on the inside of the femoral head, accelerating bone regeneration, reversing femoral head necrosis and improving blood flow. However, the clinical results so far are inconclusive and indicate that CD may have an improved effect on early-stage ONFH (68).
Figure 2.
Typical imaging results of non-traumatic osteonecrosis of the femoral head after pure core decompression.
In one study, CD surgery prevented further deterioration of the hip joints of 87-90% of Ficat I patients with NONFH, whereas only 59-70% of stage IIa patients derived a clinical benefit from this procedure (69,70). CD surgery can also significantly reduce hip pain in patients with stage I and II a avascular necrosis of the femoral head and increase the range of motion of the hip joint (69,71). Simank et al (72) found that the therapeutic effect of CD can be weakened in case of corticosteroid usage, smoking, drinking and other risk factors. In addition, some studies report that CD can only exert a short-term therapeutic effect and the long-term curative effect is poor and does not preclude the need for total hip replacement (73-76). Multiple drilling cannot effectively reduce the rate of THA conversion in early-stage NONFH. In fact, the risk of conversion to THA is increased after multiple drilling in case of larger necrotic lesions, presence of bone marrow edema and higher postoperative workload (74,75). Furthermore, Sadile et al (76) report lower efficacy of CD against NONFH compared with that of other palliative surgical techniques in terms of clinical status, imaging characteristics and the need for total hip replacement.
Despite the inconsistencies regarding the therapeutic effects of CD alone, the combination of CD with other treatment methods has shown encouraging results. For instance, the HHS score, hip function recovery and imaging performance of patients with NONFH that received bone marrow mesenchymal stem cell therapy are superior compared with patients who underwent CD, although the combination treatment had the optimal effect. Tabatabaee et al (77) subjected 28 cases of early NONFH to CD or a combination of CD with concentrated bone marrow implantation and found that the VAS pain index and MRI results improved to a significant greater extent in the combination treatment group. In a recent study conducted on 52 hips (65%) with Ficat IIa and 28 hips (35%) with Ficat IIb ONFH, 46 hips (30 Ficat IIa and 16 Ficat IIb) received HBO therapy and 34 hips (22 Ficat IIa and 12 Ficat IIb) were treated with a combination of CD and HBO. Although the VAS and HHS scores improved in each group compared with the pre-treatment scores (P<0.001), the recovery was markedly higher in the CD + HBO group (P<0.001). Furthermore, the functional and pain scores as per the SF-36 scale (78) were also significantly different between the two groups (P<0.005). HBO treatment can reduce the degree of pain in Ficat II patients and increase their functional scores. The combination of CD and HBO treatment achieves greater pain reduction in stage IIa patients compared with stage IIb patients (78). The BMSCs-bone morphogenetic protein 2 (BMP-2) complex on the magnesium alloy rod was implanted into the metaphysis of the left femur of the rabbit to the femoral head, BMP-2 coated magnesium alloy can promote the expression of bone growth factor in rabbit bone marrow implants, thereby delaying femoral head necrosis and promoting repair (79).
Platelet-rich plasma (PRP)
PRP has 8-fold higher load of platelets compared with whole blood, along with high levels of regenerative cytokines such as platelet-derived growth factor, transforming growth factor β, basic fibroblast growth factor, endothelial growth factor, insulin-like growth factor and VEGF (80). Karakaplan et al (81) found that PRP alleviates the symptoms of early-stage hormonal ONFH in a rabbit model. Zhang et al (82) further showed that the fusion of PRP with tricalcium phosphate (TCP) promotes the formation of new bone and inhibited inflammation in the rabbit model of ONFH. In addition, the triple combination of CD surgery, PRP fusion and autologous granular bone transplantation relieves traumatic ONFH with a success rate of 80% (83). Houdek et al (84) treated 22 steroid-induced patients with ONFH (35 hips) with BMSCs and PRP and found that the mean HSS increased from 57 points pre-transplantation to 85 points over an mean follow-up duration of 3 years and 93% of the patients were stable without any disease progression or complications. Although PRP cannot reverse the pathophysiological process of ONFH, it can induce osteogenic activity and stimulate the differentiation of stem cells in ARCO stage I and II patients when used in conjunction with CD and stem cell transplantation or bone grafting (85).
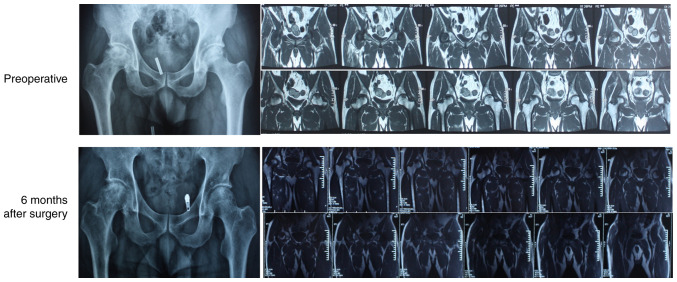
Previous studies (86,87) have shown that PRP can alleviate the symptoms of ONFH by the following mechanisms: i) Induction of angiogenesis and osteogenesis to promote bone healing, ii) inhibition of the inflammatory response in necrotic lesions, iii) prevention of GC-induced apoptosis and iv) activation of GC-induced osteogenesis and autophagy (87). While combination therapies incorporating PRP have achieved potent therapeutic effects (88), further prospective randomized clinical trials must be conducted to determine the optimal concentration of PRP and the proportion of stem cells (86). Platelet lysates can also treat femoral head necrosis by promoting the proliferation of osteoblasts and endothelial cells and reducing cell apoptosis and bone resorption (89). As shown in Fig. 3, CD combined with PRP therapy can accelerate the treatment of femoral head necrosis and promote healing of the decompression tunnel. Therefore, for patients with early-stage femoral head necrosis, a combination of PRP and CD is recommended.
Figure 3.
Imaging results of patients with non-traumatic osteonecrosis of the femoral head 6 months after the combination treatment of core decompression and platelets in platelet-rich plasma.
Stem cell therapy
Studies increasingly show that femoral head necrosis is associated with a weakened regenerative ability of the affected tissue, which can be attributed to the decrease in the number of BMSCs and lower osteogenic differentiation (90-92). Since BMSCs support angiogenesis, transplantation of bone marrow MSCs can potentially achieve clinical resolution of ONFH. However, there are several challenges in the practical application of stem cell therapy, such as patient selection, standardization of procedures, safety assessment and the fate of transplanted cells in vivo. Further studies are needed to identify ideal sources of cells, the appropriate transplantation methods, as well as the optimal number of cells (90-92).
Hernigou and Beaujean (93) performed CD and autologous bone marrow transplantation on 116 patients (189 hips) with NONFH and followed them up for 5-10 years. The treatment effect was evaluated using HHS score, imaging and the necessity for THA. Among the 145 early-stage hips, 136 achieved the desired results, whereas 25 out of the 44 hip joints with advanced femoral head collapse eventually underwent THA. Autologous bone marrow transplantation is a reliable method for treating NONFH and the therapeutic effect is proportional to the number of transplanted progenitor cells. The success rate of CD in combination with autologous bone marrow mononuclear cell transplantation is 79.7% in the patients with NONFH and this method can significantly relieve pain and stall femoral head necrosis in the early stages (94-96).
Mao et al (97) devised a technique for the directional delivery of autologous bone marrow mononuclear cells (BMMCs) enriched in MSCs through the medial femoral circumflex artery for the treatment of ONFH. They followed-up on 62 patients (78 hips) with ONFH for 5 years and found that the failure rate of the treatment was 3/68 for Ficat I-II hip joints and 3/10 in the stage III cases. Thus, targeted delivery of bone marrow cells can effectively delay the progression of ONFH, especially at the early-stage. Yoshioka et al (98) performed bone marrow transplantation on 9 patients with SLE complicated by ONFH, of which 8 did not require THA. During the follow-up period of ≤3 years, the patients reported significant pain relief and an improvement in HHS scores, indicating that this method is also effective for ONFH complicated by SLE. Autologous BMMC transplantation was also used to treat ONFH caused by sickle cell leukemia. At the last follow-up, the patients reported significant pain relief and improvement in HHS score and the quality of life. Imaging further showed a marked reduction in bone marrow edema around the necrotic area and the lesion area, indicating that BMMC implantation is a safe and effective treatment method (99,100).
Nandeesh et al (101) treated 48 patients with ONFH with autologous bone marrow stem cells combined with PRP-derived growth factor concentrate. During the 2-year follow-up, 93% of the patients had increased hip joint space and MRI results showed cartilage regeneration. The joint function of the patients also improved significantly and the overall satisfaction was high. Nevertheless, the findings need to be validated on a larger cohort. Emadedin et al (102) subjected 9 patients with ONFH to CD surgery and injected autologous bone marrow-derived CD133+ cells derived into the necrotic area of 9 patients in combination with CD therapy. During the 12-month follow-up, all patients recovered considerably and the necrotic area was significantly smaller. Due to the small number of patients however, further validation is required. Pak (103) treated two patients with ONFH by transplanting adipose tissue-derived stem cells and recorded a marked improvement in the VAS score, HHS score and MRI results, which coincided with regeneration of the medullary bone tissue in the femoral head. Mardones et al transplanted 5 patients with ONFH with hBMSCs expanded in vitro and observed significant recovery after 19 to 54 months (34).
Migration technology
Bone transplantation has been the mainstay of early NONFH treatment for more than 70 years (104). The common methods included simple bone transplantation, osteochondral transplantation and vascularized bone flap transplantation, all of which have exhibited good clinical effects.
Simple bone transplantation
Bone impaction grafting prevents the development of osteoarthritis by restoring the collapsed spherical head and remodeling the necrotic area using autologous bone tissue (105). Guo et al (106) performed allogeneic fibula transplantation in patients with early-stage femoral head necrosis and recorded rapid recovery of joint function, low level of trauma and significant improvement in clinical symptoms, indicating that this method is ideal for short-term management (107,108).
Bednarek et al (109) treated 63 patients with NONFH (72 hips) with autogenous or artificial bone transplantation. After 5 years of follow-up, 45 hips (63%) had less pain and did not exhibit any change in the shape of the femoral head. The degree of pain in 16 hips (22%) was lower, although the movement was still limited. X-ray images showed that the femoral head had collapsed significantly and this method created mechanical and biological conditions suitable for bone graft fusion and produced obvious long-term effects. Vahid Farahmandi et al (110) performed iliac crest auto-cortical bone grafting on 96 cases (132 hips) and followed the patients for an mean duration of 48.5 months. The shape of the femoral head did not change in 120 hips (90.9%) and the degree of pain was significantly lower and only 12 cases progressed to grade IV. Therefore, this method can treat patients with early-stage NONFH and prevent total hip replacement. However, some studies have shown that the efficacy of bone transplantation is not ideal. Bakx et al (111) performed tibial bone grafting on 16 patients (20 hips) with femoral head necrosis. During the 3-year follow-up, 15 cases reported improvement without any significant changes in the imaging characteristics. The treatment failed for 2 cases and further surgical intervention was required, indicating overall low efficacy of this method for NONFH.
Bone transplantation with blood vessels
Vascularized bone grafts have been developed to restore the blood supply to the necrotic femoral head and improve the ischemic state. Zhu and Zhou (112) subjected 6 patients with NONFH to vascularized iliac periosteum transplantation and detected significant recovery during the follow-up period of 3 to 7.5 years. The patients reported complete cessation of pain in the hip joint and were able to move freely. X-ray images showed that the shape of the femoral head was normal with a clear outline and the bone density was also restored. Thus, vascularized bone transplantation improves the blood supply of the femoral head, which is conducive to its revascularization and may reverse early-stage avascular necrosis of the femoral head (113).
For vascularized iliac bone transplantation with femoral head necrosis, medium and short-term therapeutic effects that can effectively delay the need for total hip replacement have been observed (114,115). Scully et al (116) compared the therapeutic effects of vascularized fibula transplantation and cord decompression in patients with ONFH at different stages. The combination of both treatments had a significant curative effect in the Ficat I patients. In patients at Ficat stages II and III, the success rate of vascularized fibula transplantation was 89 and 81% respectively compared with only 65 and 21% with CD, indicating that vascularized bone transplantation is superior to CD against both early and late stage ONFH. Heinrich and McBeath (117) used the gluteal muscle pedicle bone grafting technique to treat 16 patients (20 hips) with Ficat II-III NONFH. After an mean follow-up duration of 47 months, X-ray imaging showed recovery in 12 cases whereas no obvious progress was seen in 8 cases.
Cartilage transplantation
Cartilage transplantation, including autologous chondrocyte implantation, autologous osteochondral transplantation and allogeneic osteochondral transplantation (118), is widely used for treating talus osteochondral disease and knee cartilage injury (119,120). Gagala et al (121) treated 7 early stage patients with NONFH via osteochondral transplantation and 13 advanced-stage patients with a combination of autologous osteochondral and allogeneic bone transplantation. The mean follow-up duration was 46.14 months. At the final follow-up, the HHS scores of both groups had improved significantly, especially in patients with early-stage NONFH, indicating that osteochondral transplantation can significantly slow the progression of NONFH and delay the need for THA. However, due to lack of relevant research, the curative effect of cartilage transplantation is not completely clear.
Porous tantalum or other implants transplantation
A porous tantalum rod is a biocompatible material with an elastic modulus similar to the human fibula and can therefore provide structural support for the femoral head. Tantalum implants have been widely used for treating orthopedic diseases. Studies show that porous tantalum implants can effectively slow the progression of femoral head necrosis (122) and that its therapeutic effect on early-stage NONFH is superior to that of traditional bone transplantation (123). Nadeau et al (124) used porous tantalum implants for treating 15 patients with NONFH (18 hips), of which 3 cases were at Steinberg stage III and 15 cases were at stage IV. Most patients did not need further surgical treatment after 12 months and the success rate was 77.8%. The postoperative HHS score of the patients had improved significantly over an mean follow-up period of 23 months, which was indicative of good short-term effects. At the last follow-up however, the total success rate dropped to 44.5%, indicating that the long-term treatment effect requires further resolution. Liu et al (125) compared the postoperative hospital stay, number of days of PCA, HHS score and survival rate of the hip joint in patients who underwent traditional bone transplantation (control group) and patients who had received porous tantalum implants. The HHS score of the tantalum rod implantation group was significantly higher compared with the control group and the hip joint survival rate was 74.1% compared with only 49% in the bone-transplanted controls. Thus, implantation of tantalum rod can have a significant therapeutic effect in patients with NONFH without bone marrow edema and can delay or even avoid the need for THA. Likewise, Liu et al (126) found that whole tantalum rod implantation can effectively treat early-stage to mid-term NONFH. However, they observed high-density metal particles remnants in the femoral bone marrow cavity on X-ray images, which may be the cause of post-treatment pain and treatment failure.
The composite scaffold is expected to be a promising device for regulating the microenvironment of osteonecrosis and overcoming the challenges related to bone regeneration. A number of organic [for example, poly(lactide-co-glycolide) (PLGA), poly(ε-caprolactone), polylactide and chitosan], inorganic (for example, nano-hydroxyapatite, β-tricalcium phosphate and ceramics) and composite materials have attracted increasing attention as the matrix of bone tissue engineering scaffolds. This is due to their excellent biocompatibility, controllable degradation, easy processing, excellent mechanical properties, osteoconductivity and the ability to promote bone regeneration (127-130). The combined application of polymers and various other substances utilizes the advantages of various substances and the advantages of polymers to meet the needs of a wider range of osteonecrosis research. The addition of various substances improves the biological activity and mechanical support performance of the pure polymer. Various biologically active substances are added to polymers to produce functionalized polymers. The addition of stem cells, growth factors, small molecule drugs and metal ions in polymer bone substitute materials give the polymer bone-forming and vascular properties, which is conducive to repairing osteonecrosis (129-131). The research on functionalized polymer bone substitute materials has become a development trend and the production of various functionalized polymer biomaterials may improve the treatment of osteonecrosis (131).
Magnesium powder, PLGA and β-TCP are elements used to formulate novel porous PLGA/TCP/Mg (PTM) scaffolds using low temperature-rapid prototyping technology. The biological safety assessment from 0-12 weeks after implantation did not cause an increase in the serum magnesium ion concentration and the immune response and liver and kidney function parameters were at normal levels. These findings indicate that PTM scaffolds have osteogenic and angiogenic capabilities and they have a synergistic effect in enhancing the formation of new bone and enhancing the quality of newly formed bone in ONFH (132).
Osteotomy
Osteotomy can effectively delay the need for THA in patients with NONFH and the most common type is intertrochanteric valgus flexion osteotomy. The postoperative situation is related to the degree of the femoral head necrosis (133,134). Portigliatti Barbos et al (135) performed flexion osteotomy on 19 patients with avascular necrosis of the femoral head and followed them up for 8 years. Almost 85% of patients showed significant recovery, indicating that osteotomy is an ideal choice for treating NONFH (136). Mont et al (137) followed up 37 patients with Ficat II-III NONFH who underwent intertrochanteric osteotomy for an mean of 11.5 years and found that 28 showed good recovery with improved HHS score, while 9 had to undergo THA. Among the 17 patients with hormonal NONFH, the treatment failed in 6 cases, of which 5 had a necrosis angle exceeding 200 degrees. Thus, intertrochanteric osteotomy can be effective against Ficat II-III NONFH, but is not recommended for patients with long-term corticosteroid usage or excessive necrosis. Inao et al (138) and Masui and Hasegawa (139) performed transtrochanteric osteotomy on patients with NONFH and confirmed good recovery of the femoral heads during the mean follow-up of 13.2 years, with <2 mm collapse over 15 years after surgery.
Motomura et al (140) conducted a long-term follow-up study on 16 patients (25 hips) with SLE complicated by NONFH who had undergone transtrochanteric anterior rotation osteotomy. The hip survival rate was 73.7% on the 25th year post-surgery, indicating long-term therapeutic effect. However, osteotomy has certain disadvantages that preclude it as the first choice for NONFH treatment. Schneider et al (141) compared the therapeutic effects of different osteotomies, including flexion osteotomy, rotational osteotomy, variant osteotomy, intermediate osteotomy and extension osteotomy, on 106 patients that were followed-up for an mean of 69 months. Only flexion osteotomy achieved the desired effect, with the 5-year and 10-year hip survival rates reaching 89.2 and 60.7% respectively. The other groups, particularly rotary osteotomy, the success rate was very low and the frequency of complications was high. Thus, the current consensus is that flexion osteotomy is the only effective method for NONFH provided it is only applied when the necrotic area is small enough to guarantee a satisfactory therapeutic effect. Nevertheless, one study reported development of osteoarthritis 5 years after osteotomy and extremely poor long-term effect (142).
The adaptation period and therapeutic effects of non-traumatic NONFH with non-replacement surgery are summarized in Table III.
Table III.
Effectiveness of CD-based treatments for non-traumatic NONFH.
| First author/s, year | Treatment method | Quantity (hip) | Follow-up time (month) | Indications | Treatment effect (rate) | (Refs.) | |
|---|---|---|---|---|---|---|---|
| Leder K, 1993 | CD | CD-alone | 47 | ≥24 | Ficat I-II | Ⅰ 87.0% | (69) |
| Ⅱ 59.0% | |||||||
| Specchiulli F, 2000 | 20 | 60 | Ficat I-IIa | Ⅰ 90.0% | (70) | ||
| Ⅱa 70.0% | |||||||
| Etemadifar M, 2014 | 22 | 12 | Ficat I-IIa | / | (71) | ||
| Hernigou P, 2002 | Stem Cell | 189 | 84 | Ficat I-II | Ⅰ+Ⅱ 93.8% | (93) | |
| Ⅲ+Ⅳ 43.2% | |||||||
| Wang BL, 2010 | 59 | 27.6 | ARCO I-IIIA | 76.3% | (94) | ||
| Xian H, 2020 | PRP | 46 | 36 | ARCO II-III | 91.7% | (83) | |
| Houdek MT, 2018 | 35 | 36 | Pennsylvania Stage 1-2 | 93.0% | (84) | ||
| Tomaru Y, 2017 | Simple bone graft | 50 | 48.5 | ARCO II-III | 90.9% | (100) | |
| Bakx PA, 1991 | 20 | 36 | FICATⅡ-Ⅳ | 30.0% | (111) | ||
| Lau HW, 2021 | 50 | ≥60 | FICAT II-III | 56.0% | (115) | ||
| Zhang NF, 2003 | Vascular bone graft | 26 | 31.5 | ARCO I-II | 56.5% | (114) | |
| Scully SP, 1998 | 614 | 50 | FICAT II-III | 81.0% | (116) | ||
| Heinrich JT, 1995 | 20 | 47 | FICATⅡ-Ⅲ | 60.0% | (117) | ||
| Gagala J, 2013 | Cartilage transplantation | 7 | 46.14 | ARCO II | 61.5% | (121) | |
| Nadeau M, 2007 | Porous tantalum transplantation | 18 | 23 | Steinberg III-Ⅳ | 44.5% | (124) | |
| Liu Y, 2016 | 42 | 48 | SteinbergI-II | 84.6% | (125) |
NONFH, non-traumatic osteonecrosis of the femoral head; PRP, platelets in platelet-rich plasma.
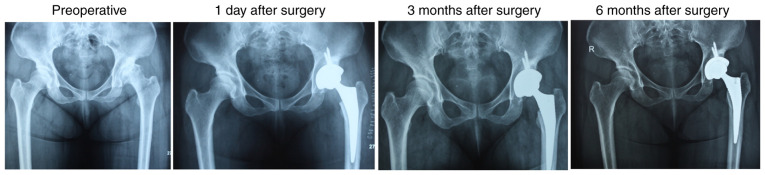
Joint replacement
For the Ficat stage III or IV patients with NONFH with femoral head depression measuring >2 mm and large lesions, it is frequently difficult to achieve the desired therapeutic effect using palliative surgery and the patients often require total hip replacement or hip resurfacing. The number of cases opting for THA is increasing, which can be attributed to the improvements in long-term efficacy. Furthermore, younger patients with ONFH are unwilling to undergo joint-sparing surgery that requires long-term hospitalization (143). Thus, joint replacement surgery is currently the most preferred treatment method for advanced NONFH.
Total hip replacement
Kirschenbaum et al (144) followed up 87 patients who underwent THA for a mean of 5.7 years. The respective scores of prosthesis loosening, revision and pain were <5 at the endpoints and survival rates were 0.61, 0.94 and 0.81 respectively. As of the revision study, there were no differences between men and women who were <50 years old, ≥50 years old, or patients weighing <185 pounds and patients weighing ≥185 pounds. Therefore, THA is a viable option for the treatment of NONFH.
Ritter et al (145) compared acetabular prosthesis loosening, femoral prosthesis loosening and revision rates of 115 patients with NONFH who underwent THA with that of 202 patients who had undergone THA due to osteoarthritis. Postoperative pain scores were similar in both groups, which further confirms the efficacy of THA against NONFH. Dong et al (146) performed cemented THA on 40 steroid-induced patients with NONFH (50 hips) and recorded significant improvement in HHS scores during the mean follow-up duration of 8.5 years. The revision rate was 2% after 4 years, while the renovation rate after 18 months was 18%. The authors holds the view that cemented THA is a suitable option for treating younger patients. Yuan et al (147) conducted a 7.6-year follow-up on 19 alcoholic patients with ONFH (24 hips) who underwent THA and detected significant improvements in the VAS and HHS scores. The 5-year and 10-year survival rate of the prosthesis was 96 and 64% respectively, which shows that THA is a reliable choice for alcoholic patients with ONFH as well. The study also found that chronic alcoholism can significantly increase the risk of revision.
Al-Mousawi et al (148) performed THA on 28 patients (35 hips) with ONFH secondary to sickle cell disease (SCD) and followed them up for an mean of 9.5 (5-15) years. One case developed infection and 6 cases developed aseptic loosening. SCD patients are at a higher risk during and post-THA. However, despite the higher failure rate in SCD patients, THA is still the most reliable option. As shown in Fig. 4, after 3 months of follow-up, THA led to significant recovery of ONFH.
Figure 4.
Representative image of total hip arthroplasty on a non-traumatic osteonecrosis of the femoral head patient.
The aforementioned studies underscore the influence of age on femoral head necrosis and that of various underlying diseases on joint function. The surgical approach of joint replacement has no significant impact on the lifespan of joint replacement and rather depends on individual differences (149-153).
Hip resurfacing
Compared to THA, hip resurfacing (HRA) can preserve more femoral bone mass and maintain normal biomechanics with similar outcomes (154,155). Therefore, HRA can be used as an alternative to total hip replacement. Beaulé et al (156) performed half-face replacement therapy on 37 patients with Ficat stage II, III or IV NONFH. The clinical, imaging and functional indices showed considerable improvement during the mean follow-up duration of 6.5 years and the 5-, 10- and 15-year survival rates were 79, 59 and 45% respectively. However, some studies have reported suboptimal outcomes of HRA. Calder et al (157) performed HRA on 12 patients with NONFH (15 hips; 1 stage Ⅱ, 9 stage III and 5 stage IV), of which 9 had to undergo revision surgery within two years during the mean follow-up period of 22.8 months. In addition, the overall results were not satisfactory. In addition, Hsieh et al (158) found that temperatures >50˚C prolonged bone cement polymerization during HRA, resulting in higher heat loss compared with normal bone. Therefore, more research is needed to determine the therapeutic efficacy of HRA. As summarized in Table IV, THA has a significantly lower revision rate compared with HRA.
Table IV.
Revision rates of total hip arthroplasty and hip resurfacing in patients with NONFH.
| First author/s, year | Treatment method | Quantity (hip) | Follow-up time (month) | Revision rate (%) | (Refs.) |
|---|---|---|---|---|---|
| Kirschenbaum IH, 1991 | Total hip replacement | 87 | 5.7 | 11.5 | (144) |
| Dong W, 1997 | 50 | 8.5 | 20.0 | (146) | |
| Al Mousawi F, 2002 | 35 | 9.5 | 20.0 | (148) | |
| Beaulé PE, 2001 | Hip resurfacing | 37 | 6.5 | 30.0 | (156) |
| Calder PR, 2004 | 15 | 1.9 | 60.0 | (157) |
5. Conclusion
Femoral head necrosis is a slow progressive disease that causes irreversible structural changes in the hip joint, leading to chronic pain and disability. However, there are no standard criteria for early screening and diagnosis, thus making early treatment less likely. Based on the current literature, the present review recommended CD combined with bone transplantation, PRP, HBO therapy, stem cell therapy, high-energy ESWT and PEMF for patients at ARCO stage Ⅰ or Ⅱ following the failure of non-surgical treatment. For patients at ARCO stage III, these methods may be effective, although there is currently lack of evidence. THA must be performed for the ARCO stage IV patients. However, this surgical plan does not consider patient age, comorbidities and other influencing factors. Therefore, an individualized plan based on the patient's condition and the mechanisms of the therapeutic strategy should be developed.
Supplementary Material
Acknowledgements
Not applicable.
Funding Statement
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
NL and QW collected images from clinical work. NL performed literature review and wrote the manuscript. CZ performed literature review of pathophysiology and diagnosis. QW edited the manuscript and figures. ZH designed the study and wrote the manuscript. NL and ZH confirm the authenticity of all raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Jin H, Li L, Yu W, Fu Y. The efficacy of acupuncture and moxibustion for early and middle-stage osteonecrosis of the femeral head: A systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2021;100(e26210) doi: 10.1097/MD.0000000000026210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mont MA, Zywiel MG, Marker DR, McGrath MS, Delanois RE. The natural history of untreated asymptomatic osteonecrosis of the femoral head: A systematic literature review. J Bone Joint Surg Am. 2010;92:2165–2170. doi: 10.2106/JBJS.I.00575. [DOI] [PubMed] [Google Scholar]
- 3.Vardhan H, Tripathy SK, Sen RK, Aggarwal S, Goyal T. Epidemiological profile of femoral head osteonecrosis in the North Indian population. Indian J Orthop. 2018;52:140–146. doi: 10.4103/ortho.IJOrtho_292_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomaru Y, Yoshioka T, Sugaya H, Shimizu Y, Aoto K, Wada H, Akaogi H, Yamazaki M, Mishima H. Mid-term results of concentrated autologous bone marrow aspirate transplantation for corticosteroid-associated osteonecrosis of the femoral head in systemic lupus erythematosus. Int Orthop. 2018;42:1623–1630. doi: 10.1007/s00264-018-3959-y. [DOI] [PubMed] [Google Scholar]
- 5.Gun BK, Frank RM, Gratton RW, Bader JO, Kusnezov N, Orr JD, Waterman BR. Non-modifiable risk factors associated with avascular necrosis in the US military. Mil Med. 2020;185:e178–e182. doi: 10.1093/milmed/usz128. [DOI] [PubMed] [Google Scholar]
- 6.Takahashi S, Fukushima W, Yamamoto T, Iwamoto Y, Kubo T, Sugano N, Hirota Y. Temporal trends in characteristics of newly diagnosed nontraumatic osteonecrosis of the femoral head from 1997 to 2011: A hospital-based sentinel monitoring system in Japan. J Epidemiol. 2015;25:437–444. doi: 10.2188/jea.JE20140162. Japanese Sentinel Monitoring Study Group for Idiopathic Osteonecrosis of the Femoral Head. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shigemura T, Nakamura J, Kishida S, Harada Y, Ohtori S, Kamikawa K, Ochiai N, Takahashi K. Incidence of osteonecrosis associated with corticosteroid therapy among different underlying diseases: Prospective MRI study. Rheumatology (Oxford) 2011;50:2023–2028. doi: 10.1093/rheumatology/ker277. [DOI] [PubMed] [Google Scholar]
- 8.Mont MA, Pivec R, Banerjee S, Issa K, Elmallah RK, Jones LC. High-dose corticosteroid use and risk of hip osteonecrosis: Meta-analysis and systematic literature review. J Arthroplasty. 2015;30:1506–1512.e5. doi: 10.1016/j.arth.2015.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gladman DD, Dhillon N, Su J, Urowitz MB. Osteonecrosis in SLE: Prevalence, patterns, outcomes and predictors. Lupus. 2018;27:76–81. doi: 10.1177/0961203317711012. [DOI] [PubMed] [Google Scholar]
- 10.Assouline-Dayan Y, Chang C, Greenspan A, Shoenfeld Y, Gershwin ME. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum. 2002;32:94–124. [PubMed] [Google Scholar]
- 11.Zhu Z, Li S, Yu H, Huang J, Tong P. Correlation between continuation of glucocorticoid treatment and risk of femoral head collapse: A retrospective cohort study of patients with glucocorticoid-induced osteonecrosis of femoral head after hip-preserving interventions. Orthopade. 2021;50:143–149. doi: 10.1007/s00132-019-03851-1. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Q, L VJ, Jin L. Role of coagulopathy in glucocorticoid-induced osteonecrosis of the femoral head. J Int Med Res. 2018;46:2141–2148. doi: 10.1177/0300060517700299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuroda T, Tanabe N, Wakamatsu A, Takai C, Sato H, Nakatsue T, Wada Y, Nakano M, Narita I. High triglyceride is a risk factor for silent osteonecrosis of the femoral head in systemic lupus erythematosus. Clin Rheumatol. 2015;34:2071–2077. doi: 10.1007/s10067-015-3075-y. [DOI] [PubMed] [Google Scholar]
- 14.Wu X, Sun W, Tan M. Noncoding RNAs in steroid-induced osteonecrosis of the femoral head. Biomed Res Int. 2019;2019(8140595) doi: 10.1155/2019/8140595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yue J, Wan F, Zhang Q, Wen P, Cheng L, Li P, Guo W. Effect of glucocorticoids on miRNA expression spectrum of rat femoral head microcirculation endothelial cells. Gene. 2018;651:126–133. doi: 10.1016/j.gene.2018.01.057. [DOI] [PubMed] [Google Scholar]
- 16.Tan B, Li W, Zeng P, Guo H, Huang Z, Fu F, Gao H, Wang R, Chen W. Epidemiological study based on China osteonecrosis of the femoral head database. Orthop Surg. 2021;13:153–160. doi: 10.1111/os.12857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoon BH, Jones LC, Chen CH, Cheng EY, Cui Q, Drescher W, Fukushima W, Gangji V, Goodman SB, Ha YC, et al. Etiologic classification criteria of ARCO on femoral head osteonecrosis part 2: Alcohol-associated osteonecrosis. J Arthroplasty. 2019;34:169–174.e1. doi: 10.1016/j.arth.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Chen YX, Zhu DY, Gao J, Xu ZL, Tao SC, Yin WJ, Zhang YL, Gao YS, Zhang CQ. Diminished membrane recruitment of Akt is instrumental in alcohol-associated osteopenia via the PTEN/Akt/GSK-3β/β-catenin axis. FEBS J. 2019;286:1101–1119. doi: 10.1111/febs.14754. [DOI] [PubMed] [Google Scholar]
- 19.Aguilar C, Vichinsky E, Neumayr L. Bone and joint disease in sickle cell disease. Hematol Oncol Clin North Am. 2005;19:929–941. doi: 10.1016/j.hoc.2005.07.001. viii. [DOI] [PubMed] [Google Scholar]
- 20.Matos MA, Alencar RW, Matos SS. Avascular necrosis of the femoral head in HIV infected patients. Braz J Infect Dis. 2007;11:31–34. doi: 10.1590/s1413-86702007000100009. [DOI] [PubMed] [Google Scholar]
- 21.Mazzotta E, Agostinone A, Rosso R, Di Biagio A, De Socio GV, Cappelletti A, Zicolella R, Polilli E, Bonfanti P, Di Matteo L, et al. Osteonecrosis in human immunodeficiency virus (HIV)-infected patients: A multicentric case-control study. J Bone Miner Metab. 2011;29:383–388. doi: 10.1007/s00774-010-0245-5. [DOI] [PubMed] [Google Scholar]
- 22.Guo KJ, Zhao FC, Guo Y, Li FL, Zhu L, Zheng W. The influence of age, gender and treatment with steroids on the incidence of osteonecrosis of the femoral head during the management of severe acute respiratory syndrome: A retrospective study. Bone Joint J. 2014;96-B:259–262. doi: 10.1302/0301-620X.96B2.31935. [DOI] [PubMed] [Google Scholar]
- 23.Agarwala SR, Vijayvargiya M, Pandey P. Avascular necrosis as a part of ‘long COVID-19’. BMJ Case Rep. 2021;14(e242101) doi: 10.1136/bcr-2021-242101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim HK, Aruwajoye O, Stetler J, Stall A. Effects of non-weight-bearing on the immature femoral head following ischemic osteonecrosis: An experimental investigation in immature pigs. J Bone Joint Surg Am. 2012;94:2228–2237. doi: 10.2106/JBJS.L.00300. [DOI] [PubMed] [Google Scholar]
- 25.Hungerford DS, Mont MA. Current options and approaches for blood management in orthopaedic surgery. J Bone Joint Surg Am. 1998;80A(765) [Google Scholar]
- 26.Arai R, Takahashi D, Inoue M, Irie T, Asano T, Konno T, Terkawi MA, Onodera T, Kondo E, Iwasaki N. Efficacy of teriparatide in the treatment of nontraumatic osteonecrosis of the femoral head: A retrospective comparative study with alendronate. BMC Musculoskelet Disord. 2017;18(24) doi: 10.1186/s12891-016-1379-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee YK, Ha YC, Cho YJ, Suh KT, Kim SY, Won YY, Min BW, Yoon TR, Kim HJ, Koo KH. Does zoledronate prevent femoral head collapse from osteonecrosis? A prospective, randomized, open-label, multicenter study. J Bone Joint Surg Am. 2015;97:1142–1148. doi: 10.2106/JBJS.N.01157. [DOI] [PubMed] [Google Scholar]
- 28.Yuan HF, Guo CA, Yan ZQ. The use of bisphosphonate in the treatment of osteonecrosis of the femoral head: A meta-analysis of randomized control trials. Osteoporos Int. 2016;27:295–299. doi: 10.1007/s00198-015-3317-5. [DOI] [PubMed] [Google Scholar]
- 29.Agarwala S, Banavali SD, Vijayvargiya M. Bisphosphonate combination therapy in the management of postchemotherapy avascular necrosis of the femoral head in adolescents and young adults: A retrospective study from India. J Glob Oncol. 2018;4:1–11. doi: 10.1200/JGO.17.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li D, Yang Z, Wei Z, Kang P. Efficacy of bisphosphonates in the treatment of femoral head osteonecrosis: A PRISMA-compliant meta-analysis of animal studies and clinical trials. Sci Rep. 2018;8(1450) doi: 10.1038/s41598-018-19884-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sheng H, Lao Y, Zhang S, Ding W, Lu D, Xu B. Combined pharmacotherapy with alendronate and desferoxamine regulate the bone resorption and bone regeneration for preventing glucocorticoids-induced osteonecrosis of the femoral head. Biomed Res Int. 2020;2020(3120458) doi: 10.1155/2020/3120458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roth A, Beckmann J, Bohndorf K, Heiß C, Jäger M, Landgraeber S, Maus U, Nöth U, Peters KM, Rader C, et al. Update of the German S3 guideline on atraumatic femoral head necrosis in adults. Orthopade. 2018;47:757–769. doi: 10.1007/s00132-018-3620-x. (In German) [DOI] [PubMed] [Google Scholar]
- 33.Agarwala S, Vijayvargiya M. Bisphosphonate combination therapy for non-femoral avascular necrosis. J Orthop Surg Res. 2019;14(112) doi: 10.1186/s13018-019-1152-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mardones R, Camacho D, Monsalvo F, Zulch N, Jofre C, Minguell JJ. Treatment of osteonecrosis of the femoral head by core decompression and implantation of fully functional ex vivo-expanded bone marrow-derived mesenchymal stem cells: A proof-of-concept study. Stem Cells Cloning. 2019;12:11–16. doi: 10.2147/SCCAA.S181883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Beckmann J, Schmidt T, Schaumburger J, Rath B, Lüring C, Tingart M, Grifka J. Infusion, core decompression, or infusion following core decompression in the treatment of bone edema syndrome and early avascular osteonecrosis of the femoral head. Rheumatol Int. 2013;33:1561–1565. doi: 10.1007/s00296-012-2597-8. [DOI] [PubMed] [Google Scholar]
- 36.Osmani F, Thakkar S, Vigdorchik J. The utility of conservative treatment modalities in the management of osteonecrosis. Bull Hosp Jt Dis (2013) 2017;75:186–192. [PubMed] [Google Scholar]
- 37.Song Q, Ni J, Jiang H, Shi Z. Sildenafil improves blood perfusion in steroid-induced avascular necrosis of femoral head in rabbits via a protein kinase G-dependent mechanism. Acta Orthop Traumatol Turc. 2017;51:398–403. doi: 10.1016/j.aott.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pritchett JW. Statin therapy decreases the risk of osteonecrosis in patients receiving steroids. Clin Orthop Relat Res. 2001:173–178. doi: 10.1097/00003086-200105000-00022. [DOI] [PubMed] [Google Scholar]
- 39.Jiang Y, Zhang Y, Zhang H, Zhu B, Li P, Lu C, Xu Y, Chen W, Lin N. Pravastatin prevents steroid-induced osteonecrosis in rats by suppressing PPARγ expression and activating Wnt signaling pathway. Exp Biol Med (Maywood) 2014;239:347–355. doi: 10.1177/1535370213519215. [DOI] [PubMed] [Google Scholar]
- 40.Pengde K, Fuxing P, Bin S, Jing Y, Jingqiu C. Lovastatin inhibits adipogenesis and prevents osteonecrosis in steroid-treated rabbits. Joint Bone Spine. 2008;75:696–701. doi: 10.1016/j.jbspin.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 41.Ye J, Wei D, Peng L, Chang T. Ginsenoside Rb1 prevents steroid-induced avascular necrosis of the femoral head through the bone morphogenetic protein-2 and vascular endothelial growth factor pathway. Mol Med Rep. 2019;20:3175–3181. doi: 10.3892/mmr.2019.10553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hao Y, Guo H, Xu Z, Qi H, Wang Y, Lu C, Liu J, Yuan P. Meta-analysis of the potential role of extracorporeal shockwave therapy in osteonecrosis of the femoral head. J Orthop Surg Res. 2018;13(166) doi: 10.1186/s13018-018-0861-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xie K, Mao Y, Qu X, Dai K, Jia Q, Zhu Z, Yan M. High-energy extracorporeal shock wave therapy for nontraumatic osteonecrosis of the femoral head. J Orthop Surg Res. 2018;13(25) doi: 10.1186/s13018-017-0705-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ludwig J, Lauber S, Lauber HJ, Dreisilker U, Raedel R, Hotzinger H. High-energy shock wave treatment of femoral head necrosis in adults. Clin Orthop Relat Res. 2001;137:119–126. doi: 10.1097/00003086-200106000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Russo S, Sadile F, Esposito R, Mosillo G, Aitanti E, Busco G, Wang CJ. Italian experience on use of E.S.W. therapy for avascular necrosis of femoral head. Int J Surg. 2015;24:188–190. doi: 10.1016/j.ijsu.2015.11.038. [DOI] [PubMed] [Google Scholar]
- 46.Algarni AD, Al Moallem HM. Clinical and radiological outcomes of extracorporeal shock wave therapy in early-stage femoral head osteonecrosis. Adv Orthop. 2018;2018(7410246) doi: 10.1155/2018/7410246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bassett CA, Pawluk RJ, Pilla AA. Augmentation of bone repair by inductively coupled electromagnetic fields. Science. 1974;184:575–577. doi: 10.1126/science.184.4136.575. [DOI] [PubMed] [Google Scholar]
- 48.Massari L, Benazzo F, Falez F, Perugia D, Pietrogrande L, Setti S, Osti R, Vaienti E, Ruosi C, Cadossi R. Biophysical stimulation of bone and cartilage: State of the art and future perspectives. Int Orthop. 2019;43:539–551. doi: 10.1007/s00264-018-4274-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Al-Jabri T, Tan JYQ, Tong GY, Shenoy R, Kayani B, Parratt T, Khan T. The role of electrical stimulation in the management of avascular necrosis of the femoral head in adults: a systematic review. BMC Musculoskelet Disord. 2017;18(319) doi: 10.1186/s12891-017-1663-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Seber S, Omeroğlu H, Cetinkanat H, Köse N. The efficacy of pulsed electromagnetic fields used alone in the treatment of femoral head osteonecrosis: A report of two cases. Acta Orthop Traumatol Turc. 2003;37:410–413. (In Turkish) [PubMed] [Google Scholar]
- 51.Massari L, Fini M, Cadossi R, Setti S, Traina GC. Biophysical stimulation with pulsed electromagnetic fields in osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88 (Suppl 3):S56–S60. doi: 10.2106/JBJS.F.00536. [DOI] [PubMed] [Google Scholar]
- 52.Paderno E, Zanon V, Vezzani G, Giacon TA, Bernasek TL, Camporesi EM, Bosco G. Evidence-supported HBO therapy in femoral head necrosis: A systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(2888) doi: 10.3390/ijerph18062888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li W, Ye Z, Wang W, Wang K, Li L, Zhao D. Clinical effect of hyperbaric oxygen therapy in the treatment of femoral head necrosis: A systematic review and meta-analysis. Orthopade. 2017;46:440–446. doi: 10.1007/s00132-016-3360-8. [DOI] [PubMed] [Google Scholar]
- 54.Chandrinou A, Korompeli A, Grammatopoulou E, Gaitanou K, Tsoumakas K, Fildissis G. Avascular necrosis of the femoral head: Evaluation of hyperbaric oxygen therapy and quality of life. Undersea Hyperb Med. 2020;47:561–569. doi: 10.22462/10.12.2020.5. [DOI] [PubMed] [Google Scholar]
- 55.Li H, Bai X, Pan S. Repetitive 1.6 ATA hyperbaric oxygen therapy for bilateral ARCO stage II steroid-associated osteonecrosis of the femoral head. Undersea Hyperb Med. 2020;47:625–633. doi: 10.22462/10.12.2020.12. [DOI] [PubMed] [Google Scholar]
- 56.Moghamis I, Alhammoud AA, Kokash O, Alhaneedi GA. The outcome of hyperbaric oxygen therapy versus core decompression in the non-traumatic avascular necrosis of the femoral head: Retrospective cohort study. Ann Med Surg (Lond) 2021;62:450–454. doi: 10.1016/j.amsu.2021.01.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Camporesi EM, Bosco G. Mechanisms of action of hyperbaric oxygen therapy. Undersea Hyperb Med. 2014;41:247–252. [PubMed] [Google Scholar]
- 58.Bennett M. Hyperbaric oxygen therapy improved both pain scores and range of motion in patients with early idiopathic femoral head necrosis (Ficat stage II) Diving Hyperb Med. 2011;41(105) [PubMed] [Google Scholar]
- 59.Camporesi E, Vezzani G, Zanon V, Manelli D, Enten G, Quartesan S, Bosco G. Review on hyperbaric oxygen treatment in femoral head necrosis. Undersea Hyperb Med. 2017;44:497–508. doi: 10.22462/11.12.2017.1. [DOI] [PubMed] [Google Scholar]
- 60.Vann RD, Butler FK, Mitchell SJ, Moon RE. Decompression illness. Lancet. 2011;377:153–164. doi: 10.1016/S0140-6736(10)61085-9. [DOI] [PubMed] [Google Scholar]
- 61.Thom SR. Hyperbaric oxygen: Its mechanisms and efficacy. Plast Reconstr Surg. 2011;127 (Suppl 1):131S–141S. doi: 10.1097/PRS.0b013e3181fbe2bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Al Hadi H, Smerdon GR, Fox SW. Hyperbaric oxygen therapy accelerates osteoblast differentiation and promotes bone formation. J Dent. 2015;43:382–388. doi: 10.1016/j.jdent.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 63.Al Hadi H, Smerdon GR, Fox SW. Hyperbaric oxygen therapy suppresses osteoclast formation and bone resorption. J Orthop Res. 2013;31:1839–1844. doi: 10.1002/jor.22443. [DOI] [PubMed] [Google Scholar]
- 64.Vezzani G, Iezzi M, Rizzato A, Quartesan S, Mangar D, Camporesi E, Paganini M, Bosco G. Effects of hyperbaric oxygen exposure on mobilization of endothelial progenitor cells in healthy volunteers. Acta Med Mediterr. 2017;33:801–805. [Google Scholar]
- 65.Bosco G, Vezzani G, Mrakic Sposta S, Rizzato A, Enten G, Abou-Samra A, Malacrida S, Quartesan S, Vezzoli A, Camporesi E. Hyperbaric oxygen therapy ameliorates osteonecrosis in patients by modulating inflammation and oxidative stress. J Enzyme Inhib Med Chem. 2018;33:1501–1505. doi: 10.1080/14756366.2018.1485149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Banerjee S, Issa K, Pivec R, Kapadia BH, Khanuja HS, Mont MA. Osteonecrosis of the hip: Treatment options and outcomes. Orthop Clin North Am. 2013;44:463–476. doi: 10.1016/j.ocl.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 67.Pakos EE, Megas P, Paschos NK, Syggelos SA, Kouzelis A, Georgiadis G, Xenakis TA. Modified porous tantalum rod technique for the treatment of femoral head osteonecrosis. World J Orthop. 2015;6:829–837. doi: 10.5312/wjo.v6.i10.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rajagopal M, Balch Samora J, Ellis TJ. Efficacy of core decompression as treatment for osteonecrosis of the hip: A systematic review. Hip Int. 2012;22:489–493. doi: 10.5301/HIP.2012.9748. [DOI] [PubMed] [Google Scholar]
- 69.Leder K, Knahr K. Results of medullary space decompression in the early stage of so-called idiopathic femur head necrosis. Z Orthop Ihre Grenzgeb. 1993;131:113–119. doi: 10.1055/s-2008-1039913. (In German) [DOI] [PubMed] [Google Scholar]
- 70.Specchiulli F. Core decompression in the treatment of necrosis of the femoral head. Long-term results. Chir Organi Mov. 2000;85:395–402. (In English, Italian) [PubMed] [Google Scholar]
- 71.Etemadifar M, Kooskzari M, Khalilollah N, Ali MK, Mahsa B. The results of core decompression treatment in patients with avascular necrosis of femoral head in patients at Isfahan City educational hospitals in 2010-2011. Adv Biomed Res. 2014;3(93) doi: 10.4103/2277-9175.129363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Simank HG, Brocai DR, Strauch K, Lukoschek M. Core decompression in osteonecrosis of the femoral head: Risk-factor-dependent outcome evaluation using survivorship analysis. Int Orthop. 1999;23:154–159. doi: 10.1007/s002640050335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Miyahara HS, Rosa BB, Hirata FY, Gurgel HMC, Ejnisman L, Vicente JRN. What is the role of core decompression in the early stages of osteonecrosis of the femoral head? Evaluation of the surgical result by functional score and radiological follow-up. Rev Bras Ortop. 2018;53:537–542. doi: 10.1016/j.rboe.2018.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu Z, Yang X, Li Y, Zeng WN, Zhao E, Zhou Z. Multiple drilling is not effective in reducing the rate of conversion to total hip Arthroplasty in early-stage nontraumatic osteonecrosis of the femoral head: A case-control comparative study with a natural course. BMC Musculoskelet Disord. 2021;22(535) doi: 10.1186/s12891-021-04418-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Moon JK, Yoon JY, Kim CH, Lee SH, Kekatpure AL, Lee JS, Yoon PW. Multiple drilling and multiple matchstick-like bone allografts for large osteonecrotic lesions in the femoral head: An average 3-year follow-up study. Arch Orthop Trauma Surg. 2020;140:1655–1663. doi: 10.1007/s00402-020-03364-z. [DOI] [PubMed] [Google Scholar]
- 76.Sadile F, Bernasconi A, Russo S, Maffulli N. Core decompression versus other joint preserving treatments for osteonecrosis of the femoral head: A meta-analysis. Br Med Bull. 2016;118:33–49. doi: 10.1093/bmb/ldw010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tabatabaee RM, Saberi S, Parvizi J, Mortazavi SM, Farzan M. Combining concentrated autologous bone marrow stem cells injection with core decompression improves outcome for patients with early-stage osteonecrosis of the femoral head: A comparative study. J Arthroplasty. 2015;30 (9 Suppl):S11–S15. doi: 10.1016/j.arth.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 78.Bozkurt I, Yalcin N, Uluyardimci E, Akgul EA. doi: 10.1177/11207000211003285. Combination of hyperbaric oxygen and core decompression therapies improve outcomes in the treatment of hip osteonecrosis. Hip Int: April 12, 2021 (Epub ahead of print). [DOI] [PubMed] [Google Scholar]
- 79.Katiella KA, Yanru Z, Hui Z. Magnesium alloy transfected BMSCs-BMP-2 composite in repair of femoral head necrosis with assessment of visceral organs. Springerplus. 2016;5(1857) doi: 10.1186/s40064-016-3472-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Eppley BL, Woodell JE, Higgins J. Platelet quantification and growth factor analysis from platelet-rich plasma: Implications for wound healing. Plast Reconstr Surg. 2004;114:1502–1508. doi: 10.1097/01.prs.0000138251.07040.51. [DOI] [PubMed] [Google Scholar]
- 81.Karakaplan M, Gülabi D, Topgül H, Elmalı N. Does platelet-rich plasma have a favorable effect in the early stages of steroid-associated femoral head osteonecrosis in a rabbit model? Eklem Hastalik Cerrahisi. 2017;28:107–113. doi: 10.5606/ehc.2017.54402. [DOI] [PubMed] [Google Scholar]
- 82.Zhang XL, Wang YM, Chu K, Wang ZH, Liu YH, Jiang LH, Chen X, Zhou ZY, Yin G. The application of PRP combined with TCP in repairing avascular necrosis of the femoral head after femoral neck fracture in rabbit. Eur Rev Med Pharmacol Sci. 2018;22:903–909. doi: 10.26355/eurrev_201802_14368. [DOI] [PubMed] [Google Scholar]
- 83.Xian H, Luo D, Wang L, Cheng W, Zhai W, Lian K, Lin D. Platelet-rich plasma-incorporated autologous granular bone grafts improve outcomes of post-traumatic osteonecrosis of the femoral head. J Arthroplasty. 2020;35:325–330. doi: 10.1016/j.arth.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 84.Houdek MT, Wyles CC, Collins MS, Howe BM, Terzic A, Behfar A, Sierra RJ. Stem cells combined with platelet-rich plasma effectively treat corticosteroid-induced osteonecrosis of the hip: A prospective study. Clin Orthop Relat Res. 2018;476:388–397. doi: 10.1007/s11999.0000000000000033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.D'Ambrosi R, Biancardi E, Massari G, Ragone V, Facchini RM. Survival analysis after core decompression in association with platelet-rich plasma, mesenchymal stem cells, and synthetic bone graft in patients with osteonecrosis of the femoral head. Joints. 2018;6:16–22. doi: 10.1055/s-0038-1626740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Han J, Gao F, Li Y, Ma J, Sun W, Shi L, Wu X, Li T. The use of platelet-rich plasma for the treatment of osteonecrosis of the femoral head: A systematic review. Biomed Res Int. 2020;2020(2642439) doi: 10.1155/2020/2642439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Huang Z, Wang Q, Zhang T, Fu Y, Wang W. Hyper-activated platelet lysates prevent glucocorticoid-associated femoral head necrosis by regulating autophagy. Biomed Pharmacother. 2021;139(111711) doi: 10.1016/j.biopha.2021.111711. [DOI] [PubMed] [Google Scholar]
- 88.Aggarwal AK, Poornalingam K, Jain A, Prakash M. Combining platelet-rich plasma instillation with core decompression improves functional outcome and delays progression in early-stage avascular necrosis of femoral head: A 4.5- to 6-year prospective randomized comparative study. J Arthroplasty. 2021;36:54–61. doi: 10.1016/j.arth.2020.07.010. [DOI] [PubMed] [Google Scholar]
- 89.Huang Z, Zhao Z, Lang J, Wang W, Fu Y, Wang W. Therapeutic study of thermosensitive hydrogel loaded with super-activated platelet lysate combined with core decompression technology for the treatment of femoral head necrosis. Stem Cells Int. 2021;2021(7951616) doi: 10.1155/2021/7951616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Xu Y, Jiang Y, Xia C, Wang Y, Zhao Z, Li T. Stem cell therapy for osteonecrosis of femoral head: Opportunities and challenges. Regen Ther. 2020;15:295–304. doi: 10.1016/j.reth.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Maruyama M, Nabeshima A, Pan CC, Behn AW, Thio T, Lin T, Pajarinen J, Kawai T, Takagi M, Goodman SB, Yang YP. The effects of a functionally-graded scaffold and bone marrow-derived mononuclear cells on steroid-induced femoral head osteonecrosis. Biomaterials. 2018;187:39–46. doi: 10.1016/j.biomaterials.2018.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tomaru Y, Yoshioka T, Sugaya H, Kumagai H, Hyodo K, Aoto K, Wada H, Akaogi H, Yamazaki M, Mishima H. Ten-year results of concentrated autologous bone marrow aspirate transplantation for osteonecrosis of the femoral head: A retrospective study. BMC Musculoskelet Disord. 2019;20(410) doi: 10.1186/s12891-019-2797-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002:14–23. doi: 10.1097/00003086-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 94.Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, Xu SQ, Lou JN, Li ZR. Treatment of nontraumatic osteonecrosis of the femoral head with the implantation of core decompression and concentrated autologous bone marrow containing mononuclear cells. Arch Orthop Trauma Surg. 2010;130:859–865. doi: 10.1007/s00402-009-0939-0. [DOI] [PubMed] [Google Scholar]
- 95.Rastogi S, Sankineani SR, Nag HL, Mohanty S, Shivanand G, Marimuthu K, Kumar R, Rijal L. Intralesional autologous mesenchymal stem cells in management of osteonecrosis of femur: A preliminary study. Musculoskelet Surg. 2013;97:223–228. doi: 10.1007/s12306-013-0273-0. [DOI] [PubMed] [Google Scholar]
- 96.Khan M, Abbas K, Ayling EA, Waqas Ilyas M, Dunlop DG. Autologous stem cell implantation with core decompression for avascular necrosis of the femoral head using a new device. Ann R Coll Surg Engl. 2021;103:508–513. doi: 10.1308/rcsann.2021.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Mao Q, Jin H, Liao F, Xiao L, Chen D, Tong P. The efficacy of targeted intraarterial delivery of concentrated autologous bone marrow containing mononuclear cells in the treatment of osteonecrosis of the femoral head: A five year follow-up study. Bone. 2013;57:509–516. doi: 10.1016/j.bone.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yoshioka T, Mishima H, Akaogi H, Sakai S, Li M, Ochiai N. Concentrated autologous bone marrow aspirate transplantation treatment for corticosteroid-induced osteonecrosis of the femoral head in systemic lupus erythematosus. Int Orthop. 2011;35:823–829. doi: 10.1007/s00264-010-1048-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Daltro GC, Fortuna V, de Souza ES, Salles MM, Carreira AC, Meyer R, Freire SM, Borojevic R. Efficacy of autologous stem cell-based therapy for osteonecrosis of the femoral head in sickle cell disease: A five-year follow-up study. Stem Cell Res Ther. 2015;6(110) doi: 10.1186/s13287-015-0105-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tomaru Y, Yoshioka T, Sugaya H, Aoto K, Wada H, Akaogi H, Yamazaki M, Mishima H. Hip preserving surgery with concentrated autologous bone marrow aspirate transplantation for the treatment of asymptomatic osteonecrosis of the femoral head: Retrospective review of clinical and radiological outcomes at 6 years postoperatively. BMC Musculoskelet Disord. 2017;18(292) doi: 10.1186/s12891-017-1652-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nandeesh NH, Janardhan K, Subramanian V, Ashtekar AB, Srikruthi N, Koka PS, Deb K. Treatment of AVN using autologous BM stem cells and activated platelet-derived growth factor concentrates. J Stem Cells. 2016;11:135–148. [PubMed] [Google Scholar]
- 102.Emadedin M, Karimi S, Karimi A, Labibzadeh N, Niknejadi M, Baharvand H, Aghdami N. Autologous bone marrow-derived CD133 cells with core decompression as a novel treatment method for femoral head osteonecrosis: A pilot study. Cytotherapy. 2019;21:107–112. doi: 10.1016/j.jcyt.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 103.Pak J. Autologous adipose tissue-derived stem cells induce persistent bone-like tissue in osteonecrotic femoral heads. Pain Physician. 2012;15:75–85. [PubMed] [Google Scholar]
- 104.Wu CT, Yen SH, Lin PC, Wang JW. Long-term outcomes of phemister bone grafting for patients with non-traumatic osteonecrosis of the femoral head. Int Orthop. 2019;43:579–587. doi: 10.1007/s00264-018-4013-9. [DOI] [PubMed] [Google Scholar]
- 105.Osawa Y, Seki T, Okura T, Takegami Y, Ishiguro N, Hasegawa Y. Long-term outcomes of curved intertrochanteric varus osteotomy combined with bone impaction grafting for non-traumatic osteonecrosis of the femoral head. Bone Joint J. 2021;103-B:665–671. doi: 10.1302/0301-620X.103B4.BJJ-2020-1107.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Guo X, Dou B, Zhou Y, Li Y. Surgical treatment of necrosis of the femoral head in early stages with core depression and allo-fibular grafting. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2005;19:697–699. (In Chinese) [PubMed] [Google Scholar]
- 107.Yue J, Gao H, Guo X, Wang R, Li B, Sun Q, Liu W, Chen J, Li Y. Fibula allograft propping as an effective treatment for early-stage osteonecrosis of the femoral head: A systematic review. J Orthop Surg Res. 2020;15(206) doi: 10.1186/s13018-020-01730-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Alam MT, Alam QS, Alam MK, Islam MA, Saha MK, Rahman MM, Hossain MZ, Roy MK, Islam MK, Hossain M, et al. Core decompression with non vascularized fibular graft as modern surgical treatment of early hip avascular necrosis. Mymensingh Med J. 2021;30:323–328. [PubMed] [Google Scholar]
- 109.Bednarek A, Atras A, Gągała J, Kozak Ł. Operative technique and results of core decompression and filling with bone grafts in the treatment of osteonecrosis of femoral head. Ortop Traumatol Rehabil. 2010;12:511–518. [PubMed] [Google Scholar]
- 110.Vahid Farahmandi M, Abbasian M, Safdari F, Emami Moghaddam Tehrani M. Midterm results of treating femoral head osteonecrosis with autogenous corticocancellous bone grafting. Trauma Mon. 2014;19(e17092) doi: 10.5812/traumamon.17092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bakx PA, van Biezen FC, van Linge B. Failure of tibial bone grafting for femoral head necrosis. Acta Orthop Scand. 1991;62:230–231. doi: 10.3109/17453679108993598. [DOI] [PubMed] [Google Scholar]
- 112.Zhu SX, Zhou MW. Iliac periosteal graft with vascular pedicle in the treatment of avascular necrosis of the femoral head. Experimental study and clinical application. Chin Med J (Engl) 1992;105:849–855. [PubMed] [Google Scholar]
- 113.Ligh CA, Nelson JA, Fischer JP, Kovach SJ, Levin LS. The effectiveness of free vascularized fibular flaps in osteonecrosis of the femoral head and neck: A systematic review. J Reconstr Microsurg. 2017;33:163–172. doi: 10.1055/s-0036-1594294. [DOI] [PubMed] [Google Scholar]
- 114.Zhang NF, Li ZR, Zhang XZ, Wang W. Vascularized iliac bone grafting for avascular necrosis of the femoral head. Zhonghua Wai Ke Za Zhi. 2003;41:125–129. (In Chinese) [PubMed] [Google Scholar]
- 115.Lau HW, Wong KC, Ho K, Chung KY, Chiu WK, Kumta SM. Long-term outcome of vascularized iliac bone grafting for osteonecrosis of femoral head: A retrospective study with 17-year follow-up. J Orthop Surg (Hong Kong) 2021;29(2309499021996842) doi: 10.1177/2309499021996842. [DOI] [PubMed] [Google Scholar]
- 116.Scully SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am. 1998;80:1270–1275. doi: 10.2106/00004623-199809000-00004. [DOI] [PubMed] [Google Scholar]
- 117.Heinrich JT, McBeath AA. The gluteus minimus muscle pedicle graft in the treatment of femoral head avascular necrosis. Am J Orthop (Belle Mead NJ) 1995;24:615–623. [PubMed] [Google Scholar]
- 118.Chahla J, LaPrade RF, Mardones R, Huard J, Philippon MJ, Nho S, Mei-Dan O, Pascual-Garrido C. Biological therapies for cartilage lesions in the hip: A new horizon. Orthopedics. 2016;39:e715–e723. doi: 10.3928/01477447-20160623-01. [DOI] [PubMed] [Google Scholar]
- 119.Seow D, Shimozono Y, Gianakos AL, Chiarello E, Mercer N, Hurley ET, Kennedy JG. Autologous osteochondral transplantation for osteochondral lesions of the talus: High rate of return to play in the athletic population. Knee Surg Sports Traumatol Arthrosc. 2021;29:1554–1561. doi: 10.1007/s00167-020-06216-w. [DOI] [PubMed] [Google Scholar]
- 120.Carey JL, Shea KG, Lindahl A, Vasiliadis HS, Lindahl C, Peterson L. Autologous chondrocyte implantation as treatment for unsalvageable osteochondritis dissecans: 10- to 25-year follow-up. Am J Sports Med. 2020;48:1134–1140. doi: 10.1177/0363546520908588. [DOI] [PubMed] [Google Scholar]
- 121.Gagala J, Tarczyńska M, Gawęda K. Clinical and radiological outcomes of treatment of avascular necrosis of the femoral head using autologous osteochondral transfer (mosaicplasty): Preliminary report. Int Orthop. 2013;37:1239–1244. doi: 10.1007/s00264-013-1893-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Tsao AK, Roberson JR, Christie MJ, Dore DD, Heck DA, Robertson DD, Poggie RA. Biomechanical and clinical evaluations of a porous tantalum implant for the treatment of early-stage osteonecrosis. J Bone Joint Surg Am. 2005;87 (Suppl 2):S22–S27. doi: 10.2106/JBJS.E.00490. [DOI] [PubMed] [Google Scholar]
- 123.Shuler MS, Rooks MD, Roberson JR. Porous tantalum implant in early osteonecrosis of the hip: Preliminary report on operative, survival, and outcomes results. J Arthroplasty. 2007;22:26–31. doi: 10.1016/j.arth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 124.Nadeau M, Séguin C, Theodoropoulos JS, Harvey EJ. Short term clinical outcome of a porous tantalum implant for the treatment of advanced osteonecrosis of the femoral head. Mcgill J Med. 2007;10:4–10. [PMC free article] [PubMed] [Google Scholar]
- 125.Liu Y, Yan L, Zhou S, Su X, Cao Y, Wang C, Liu S. Tantalum rod implantation for femoral head osteonecrosis: Survivorship analysis and determination of prognostic factors for total hip arthroplasty. Int Orthop. 2016;40:1397–1407. doi: 10.1007/s00264-015-2897-1. [DOI] [PubMed] [Google Scholar]
- 126.Liu G, Wang J, Yang S, Xu W, Ye S, Xia T. Effect of a porous tantalum rod on early and intermediate stages of necrosis of the femoral head. Biomed Mater. 2010;5(065003) doi: 10.1088/1748-6041/5/6/065003. [DOI] [PubMed] [Google Scholar]
- 127.Zhu T, Jiang M, Zhang M, Cui L, Yang X, Wang X, Liu G, Ding J, Chen X. Biofunctionalized composite scaffold to potentiate osteoconduction, angiogenesis, and favorable metabolic microenvironment for osteonecrosis therapy. Bioact Mater. 2021;9:446–460. doi: 10.1016/j.bioactmat.2021.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Benedini L, Laiuppa J, Santillán G, Baldini M, Messina P. Antibacterial alginate/nano-hydroxyapatite composites for bone tissue engineering: Assessment of their bioactivity, biocompatibility, and antibacterial activity. Mater Sci Eng C Mater Biol Appl. 2020;115(111101) doi: 10.1016/j.msec.2020.111101. [DOI] [PubMed] [Google Scholar]
- 129.Zhou H, Boys AJ, Harrod JB, Bonassar LJ, Estroff LA. Mineral distribution spatially patterns bone marrow stromal cell behavior on monolithic bone scaffolds. Acta Biomater. 2020;112:274–285. doi: 10.1016/j.actbio.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhao D, Zhu T, Li J, Cui L, Zhang Z, Zhuang X, Ding J. Poly(lactic-co-glycolic acid)-based composite bone-substitute materials. Bioact Mater. 2020;6:346–360. doi: 10.1016/j.bioactmat.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dong H, Zhu T, Zhang M, Wang D, Wang X, Huang G, Wang S, Zhang M. Polymer scaffolds-enhanced bone regeneration in osteonecrosis therapy. Front Bioeng Biotechnol. 2021;9(761302) doi: 10.3389/fbioe.2021.761302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lai Y, Li Y, Cao H, Long J, Wang X, Li L, Li C, Jia Q, Teng B, Tang T, et al. Osteogenic magnesium incorporated into PLGA/TCP porous scaffold by 3D printing for repairing challenging bone defect. Biomaterials. 2019;197:207–219. doi: 10.1016/j.biomaterials.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 133.Wagner H, Baur W, Wagner M. Joint-preserving osteotomy in segmental femur head necrosis. Orthopade. 1990;19:208–218. (In German) [PubMed] [Google Scholar]
- 134.Lee YK, Park CH, Ha YC, Kim DY, Lyu SH, Koo KH. Comparison of surgical parameters and results between curved varus osteotomy and rotational osteotomy for osteonecrosis of the femoral head. Clin Orthop Surg. 2017;9:160–168. doi: 10.4055/cios.2017.9.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Portigliatti Barbos M, Balbo C, Rossi P. Middle and long-term results of flexion osteotomy for avascular necrosis of the femoral head. Ital J Orthop Traumatol. 1992;18:53–61. [PubMed] [Google Scholar]
- 136.Xu YX, Ren YZ, Zhao ZP, Wang YZ, Wang T, Li T. Hip survival rate in the patients with avascular necrosis of femoral head after transtrochanteric rotational osteotomy: A systematic review and meta-analysis. Chin Med J (Engl) 2019;132:2960–2971. doi: 10.1097/CM9.0000000000000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mont MA, Fairbank AC, Krackow KA, Hungerford DS. Corrective osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Am. 1996;78:1032–1038. doi: 10.2106/00004623-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 138.Inao S, Ando M, Gotoh E, Matsuno T. Minimum 10-year results of Sugioka's osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res. 1999:141–148. [PubMed] [Google Scholar]
- 139.Masui T, Hasegawa Y. Curved intertrochanteric varus osteotomy. Clin Calcium. 2007;17:931–937. (In Japanese) [PubMed] [Google Scholar]
- 140.Motomura G, Yamamoto T, Suenaga K, Nakashima Y, Mawatari T, Ikemura S, Iwamoto Y. Long-term outcome of transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head in patients with systemic lupus erythematosus. Lupus. 2010;19:860–865. doi: 10.1177/0961203310361896. [DOI] [PubMed] [Google Scholar]
- 141.Schneider W, Aigner N, Knahr K. Intertrochanteric rotational osteotomies in idiopathic femur head necrosis-comparison of different procedures. Z Orthop Ihre Grenzgeb. 1998;136:147–153. doi: 10.1055/s-2008-1051297. (In German) [DOI] [PubMed] [Google Scholar]
- 142.Morita D, Hasegawa Y, Okura T, Osawa Y, Ishiguro N. Long-term outcomes of transtrochanteric rotational osteotomy for non-traumatic osteonecrosis of the femoral head. Bone Joint J. 2017;99-B:175–183. doi: 10.1302/0301-620X.99B2.BJJ-2016-0417.R2. [DOI] [PubMed] [Google Scholar]
- 143.Kuroda Y, Okuzu Y, Kawai T, Goto K, Matsuda S. Difference in therapeutic strategies for joint-preserving surgery for non-traumatic osteonecrosis of the femoral head between the United States and Japan: A review of the literature. Orthop Surg. 2021;13:742–748. doi: 10.1111/os.12979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kirschenbaum IH, Vernace JV, Booth RE Jr, Balderston RA, Rothman RH. Total hip arthroplasty for osteonecrosis. Semin Arthroplasty. 1991;2:234–240. [PubMed] [Google Scholar]
- 145.Ritter MA, Helphinstine J, Keating EM, Faris PM, Meding JB. Total hip arthroplasty in patients with osteonecrosis. The effect of cement techniques. Clin Orthop Relat Res. 1997:94–99. doi: 10.1097/00003086-199705000-00014. [DOI] [PubMed] [Google Scholar]
- 146.Dong W, Yu N, Bai B. Total hip replacement in patients with steroid-induced femoral head necrosis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 1997;11:161–163. (In Chinese) [PubMed] [Google Scholar]
- 147.Yuan B, Taunton MJ, Trousdale RT. Total hip arthroplasty for alcoholic osteonecrosis of the femoral head. Orthopedics. 2009;32(400) doi: 10.3928/01477447-20090511-06. [DOI] [PubMed] [Google Scholar]
- 148.Al-Mousawi F, Malki A, Al-Aradi A, Al-Bagali M, Al-Sadadi A, Booz MM. Total hip replacement in sickle cell disease. Int Orthop. 2002;26:157–161. doi: 10.1007/s00264-002-0337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Holzapfel BM, Rak D, Kreuzer S, Arnholdt J, Thaler M, Rudert M. Short stem hip arthroplasty via the minimally invasive direct anterior approach. Oper Orthop Traumatol. 2021;33:288–303. doi: 10.1007/s00064-021-00723-w. [DOI] [PubMed] [Google Scholar]
- 150.Anthony CA, Wasko MK, Pashos GE, Barrack RL, Nunley RM, Clohisy JC. Total hip arthroplasty in patients with osteoarthritis associated with legg-calve-perthes disease: Perioperative complications and patient-reported outcomes. J Arthroplasty. 2021;36:2518–2522. doi: 10.1016/j.arth.2021.02.031. [DOI] [PubMed] [Google Scholar]
- 151.Moschetti WE, Kunkel S, Keeney BJ, Jevsevar D. Do patients with higher preoperative functional outcome scores preferentially seek direct anterior approach total hip arthroplasty? Arthroplast Today. 2021;10:6–11. doi: 10.1016/j.artd.2021.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Bose VC, Kalaivanan K, Manohar M, Kumar A, Patil S, Suryanarayan P. Is the revision rate higher after hip arthroplasty in teenage patients? A prospective study with long-term follow-up of more than 10 years. Indian J Orthop. 2021;55:993–1002. doi: 10.1007/s43465-021-00370-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Agrawal Y, Kerry RM, Stockley I, Hamer AJ. Review of total hip arthroplasty in patients younger than 30 years: Mid- to long-term results. Hip Int. 2021;31:533–541. doi: 10.1177/1120700020901685. [DOI] [PubMed] [Google Scholar]
- 154.Mont MA, Rajadhyaksha AD, Hungerford DS. Outcomes of limited femoral resurfacing arthroplasty compared with total hip arthroplasty for osteonecrosis of the femoral head. J Arthroplasty. 2001;16 (8 Suppl 1):S134–S139. doi: 10.1054/arth.2001.28722. [DOI] [PubMed] [Google Scholar]
- 155.Dong T, Sun J, Qu Y, Wang Y. Resurfacing arthroplasty for treatment of avascular necrosis of femoral head in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2005;19:707–709. (In Chinese) [PubMed] [Google Scholar]
- 156.Beaulé PE, Schmalzried TP, Campbell P, Dorey F, Amstutz HC. Duration of symptoms and outcome of hemiresurfacing for hip osteonecrosis. Clin Orthop Relat Res. 2001:104–117. doi: 10.1097/00003086-200104000-00018. [DOI] [PubMed] [Google Scholar]
- 157.Calder PR, Hynes MC, Scott G. Short-term results of hemi-resurfacing for osteonecrosis of the femoral head. Hip Int. 2004;14:174–181. doi: 10.5301/HIP.2008.4533. [DOI] [PubMed] [Google Scholar]
- 158.Hsieh PH, Tai CL, Liaw JW, Chang YH. Thermal damage potential during hip resurfacing in osteonecrosis of the femoral head: An experimental study. J Orthop Res. 2008;26:1206–1209. doi: 10.1002/jor.20639. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.