Telehealth in Chronic Liver Disease:
Telehealth has allowed for the safe, continued delivery of liver-related care during the coronavirus disease-19 (COVID-19) pandemic.1 Gastroenterology and hepatology practices rapidly increased their use of telehealth visits, reaching rates as high as 94%.2 Satisfaction is high among patients and providers who complete telehealth visits3 and there are encouraging results showing similar post-liver transplantation clinical outcomes, including patient and graft survival and readmissions.4
Telehealth visits exist predominantly in two forms, an audio-only telephone visit and an audio-visual video visit. In contrast to a telephone visit, a video visit allows for a modified physical examination, exchange of non-verbal cues, insight into the patient’s living environment, and potential maintenance of a more interpersonal patient-provider relationship. Telehealth is hoped by many to endure beyond the pandemic.5 However, there are hidden complexities in the conduct of telehealth, particularly video visits, that may result in widening disparities across geography, age, socioeconomics, and race.6 Data are lacking regarding the rates of and reasons for not accepting or completing a video visit. Understanding and overcoming the barriers for those who fail to connect to a video visit is essential to the success, maintenance, and equity of telemedicine.7 Herein, we provide a framework for optimizing video visit uptake informed by our local single-center experience with hepatology care. We present our findings, identified barriers,(Figure 1) and healthcare system and patient-centered solutions within the broader context of telehepatology research and organized around selected principles of technology acceptance and implementation.8–10
Figure 1:
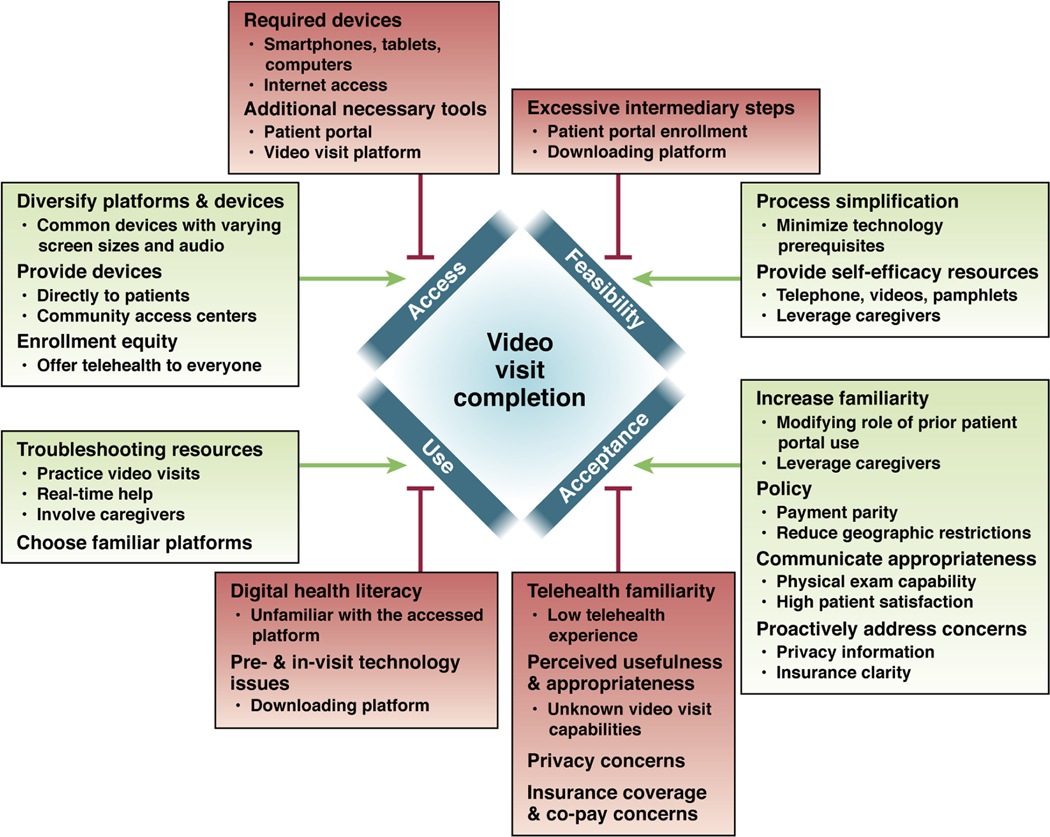
Barriers and Facilitators to Video Visit Use
A Local Experience with Telehealth Visits
Telehealth visits (video visit or, if a patient declined, a telephone visit) were offered to all patients with a scheduled hepatology appointment during April 2020 unless an in-person evaluation was required. Overall, 244 patients completed a telehealth visit with median age 59 years (IQR 48–66), 80% were Caucasian, 50% were female, and 62% had cirrhosis. 197 (78.7%) completed their visit by telephone and 47 (19.3%) by video. Five video visits were converted to a telephone visit for technical reasons. We sent a survey evaluating opinions about telehealth and technology use(Supplemental Table 1) to all patients with a valid email address who completed a telehealth visit (174 of 244). We received survey responses from 51 (29.0%) patients. Lastly, we reviewed patient satisfaction survey comments completed by patients who performed a video visit in the hepatology clinic during April/May 2020.
Barriers to Video Visit Use
Access
Devices, Connectivity, and Downstream Requirements:
The most proximal barrier to engagement in a video visit is access to prerequisite tools. Basic requirements include ownership of a smartphone, laptop, or tablet device with a functioning camera and reliable internet access. Depending on the facility and platform, potential users may also need to enroll in the patient portal and download a compatible mobile application. These steps constitute the structural barriers to successful video visit implementation and result in the gradual attrition of potential users. During our study period, these were the requirements to participate in a video visit and highlight access barriers. Smartphone ownership and internet access exceeded 92% in our surveyed population; conversely, this represents an immediate exclusion of 8% of persons unable to participate in a video visit. Notably, smartphone ownership is less frequent in the general population (81%)11 and other liver transplant centers with more socioeconomically diverse patient populations (76%).12 Multiple additional requirements increasingly impeded use. Nearly 30% of our participants did not have access to the patient portal and at least as many also did not have the video visit application available for use on their devices.
Feasibility
The Burden of Intermediary Steps:
Each technological requirement necessary to engage in the video visit platform presents a barrier to feasibility as they require completion of often complicated steps. Enrollment in the patient portal itself is a challenging multistep process. Potential enrollees must first provide an email address, receive the invitation token, and complete the enrollment process. Subsequently, the institution’s video visit platform needs to be downloaded - a process barrier for the 28.6% of our surveyed participants who did not know how to download a smartphone application. Others may know how to download the application but run into an additional barrier of not being able to recall or locate their log-in information.7
Acceptance
Unfamiliarity and Unrecognized Benefits:
Technology acceptance is influenced by its perceived usefulness, ease-of-use, prior experience, and general comfort with technology.7,8 We identified three main barriers to video visit acceptance. First, limited familiarity with video communication influenced the perceived usefulness and appropriateness of receiving care using this method.
Forty-two percent of surveyed participants rarely or never communicated with others by video and an additional 14% only did so no more than once per month. Low familiarity led many to view a video visit as too impersonal and as a reason for declining a video visit. Furthermore, a lack of prior experience decreased the perceived appropriateness of care provided by video as the interactive capabilities of these platforms may have been less understood (physical exam, shared facial cues and reactions) and incorrectly equated to a telephone visit. This may explain why 71% of patients 50–80 years of age have concerns about the lack of a physical exam with a virtual visit.13
Privacy and Insurance:
Second, privacy concerns were another barrier to video visit acceptance. Ensuring privacy extends beyond platform privacy protections. Patients also need to feel confident that they can create, and have access to, an environment with audio-visual privacy to conduct the video visit.14 Third, we found that perceptions of insurance coverage limitations influenced the decision to not accept a video visit. Non-private insurance (including Medicare) is independently associated with completing a telephone visit instead of a video visit for chronic liver disease.15 Patients may elect to complete a telephone visit if the out-of-pocket cost is perceived to be lower compared to a video visit.
Video Visit Uptake
Digital Health Literacy:
Low digital health literacy is the most important barrier to video visit use. Several patient-related risk factors that impact digital health literacy and video visit use in the general population such as older age2,3 and cognitive dysfunction16 (hepatic encephalopathy, cognitive frailty), may be more prevalent in persons with chronic liver disease. These factors can impede their ability to adequately interact with the platform and complete the video visit.17 This was reflected in our study cohort where 10% of patients had a failed video visit encounter, a fifth of surveyed participants agreed to but did not complete a video visit, and overall peak video visit use in the hepatology clinic between April and July 2020 was 28%. This rate of video visit use is lower than that seen by Serper et al. at another large academic gastroenterology/hepatology outpatient practice early during pandemic where video visit use was 47% after four weeks.3 A similar percentage (53%) was observed elsewhere.2 However our rate of video visit use in the hepatology clinic was comparable to that seen at another advanced liver disease and liver transplantation clinic (16%−37%) during a similar time period.18 This suggests the potential presence of key digital health literacy challenges present in those with chronic liver disease that need to be explored further.
Navigating New Technology:
A majority of surveyed patients in our study attributed non-use of an accepted video visit to technical issues and believed they would have been able to complete the video visit if a different platform was offered. Patient satisfaction surveys expanded on this finding. Multiple respondents described video-related issues leading to either an audio-only use of the platform or defaulting to a telephone visit. Additionally, patients described alternative platforms that they believed could have improved the completion of their virtual visit.
Expanding Video Visit Use
Improving Access
Providing Access to Devices:
Accessibility solutions must be tailored to each center’s unique infrastructure and patient populations. Video visit implementation methods in the Veterans Health Affairs provide an exemplary healthcare system-centered approach to improving accessibility. By conducting video visits at local primary care facilities, wait-times for transplant evaluations are significantly reduced for patients living long distances from a liver transplant center.19 A similarly successful community-based video visit delivery strategy for persons with chronic liver disease has been developed in a non-centralized healthcare system; however, it is limited by unequal insurance reimbursement practices and state and federal regulatory issues.20 Nonetheless, these solutions highlight a method of eliminating patient-centered barriers related to device access and process feasibility.
Providing devices to patients can eliminate barriers to telehealth visits and address disparities. In a randomized clinical trial of liver transplant recipients, those receiving a tablet with video communication functionality for remote patient monitoring experienced less 90-day readmissions and had improved patient-reported outcomes.21 This highlights the potential cost-effectiveness of a telehealth model that is able to ensure device access. Providing telehealth devices preloaded with the necessary software may be the most efficient method to connect patients to care. This method may not be practical to broad patient populations. Solutions, therefore, should focus on reducing patient-related barriers by expanding entry points of use.
Diversifying Devices and Eliminating Disparities:
The tools necessary to engage in a video visit should be widely available. This includes platforms that can facilitate a video visit on smartphones, tablets, laptops, and desktops. A variety of compatible devices ensures accessibility for those with visual (screen size) and auditory difficulties (speakers). Additionally, healthcare systems must strive to improve telehealth equity. There are racial and socioeconomic disparities existing in who is even offered portal enrollment.22 Addressing these disparities starts with ensuring everyone is given the opportunity to engage in telehealth.
Increasing Process Feasibility
Process Simplification:
Reducing and removing intermediary steps is key to video visit completion. Video visit platforms should minimize usage prerequisites that are multistep or that depend on prior enrollment and use of another telehealth tool, such as the patient portal. Not only is a lack of patient portal use associated with less acceptance of a video visit,6 there are pre-existing racial/ethnic and socioeconomic disparities in the use of patient portals that could widen video visit use disparities if it is a prerequisite.22
Resources to Improve Self-Efficacy:
Feasibility of the set-up process can also be modified through the provision of real-time technology assistance from healthcare centers to their patients. This should be adjusted to match the complexity of the telehealth tool enrollment process. As the study by Lee et al. in post-transplantation patients further highlights, successful implementation of a telehealth tool requires patient navigation.21 This includes basic training to modify digital health literacy and providing troubleshooting support in multiple settings – in-clinic, by telephone, or in-home by trained staff.21 Self-efficacy in the set-up process can also be modified by leveraging caregivers. Caregivers are present in a majority of patients with chronic liver disease12 and their presence can potentially improve the patient’s perceived technological capability to navigate through the enrollment process.7,16
Fostering Video Visit Acceptance
Encouraging Familiarity Through Experience and Social Network:
Modifying patient familiarity, comfort, and acceptance of technology is challenging but achievable. For example, while the patient portal as a prerequisite represents an access barrier, its use is associated with increased video visit uptake.6 The patient portal likely represents an incremental prior telehealth exposure that can be leveraged to improve self-efficacy and acceptance of an additional telehealth tool.8 Similar to improving a patient’s perceived ability to set-up a video visit, caregivers can also provide patients with the confidence to accept an unfamiliar method of communication.
Proactively Address Concerns:
Methods to increase patient acceptance of a video visit requires proactive patient education during the scheduling process that addresses concerns related to cost, privacy, and appropriateness of virtual care. Centers can address this by standardizing the process of scheduling a video visit. Billing differences, or lack thereof, of either telehealth visit method must be transparent.2 Concerns about the privacy of the visit should be addressed, including environmental techniques to maintain privacy (i.e., headphones, quiet location free from potential disturbances).14 Furthermore, insight into the appropriateness and utility of a video visit over a telephone visit can be outlined. Patients should be informed in a scripted fashion that their provider has identified their care as appropriate for a video visit and of the additional ability to perform a modified physical exam to address their health concerns. Finally, advertising clinic-specific patient satisfaction rates with video visits may help potential users recognize that appropriate care can be, and has been, received using these platforms.9 Consistent with high patient satisfaction rates described across multiple diverse gastroenterology and hepatology centers,3,20,23 more than 90% of our surveyed participants would complete a video visit again in the future. Centers should be proud of these high patient-reported experiences and advertise them to hesitant patients.
Policy Advocacy:
The expanded access to and benefits of video visits will require healthcare systems to continue advocating for the maintenance of policies allowing for payment parity and reduced geographic barriers.5 Locally, institutions can advocate for their patients by requiring the creators of telehealth platforms to refine their tools to match the needs of the local population.24
Successful Video Visit Use
Available Technology Assistance:
Building a healthcare system infrastructure capable of providing video visit platform assistance is essential for ensuring successful use. First, similar to providing technology assistance for the intermediary telehealth visit enrollment steps, implementation of real-time staff-guided practice visits with the platform can increase telehealth visit completion rates by more than 30%.25 This can be combined with traditional aides such as how-to videos and detailed pictorial step-by-step pamphlets specifically related to the use of the video visit application.17
Leverage Familiarity:
Second, centers should integrate platforms already familiar to patients in order to improve usability. This can reduce the risk of technology issues directly related to the use of a novel video communication platform, and many institutions like ours have switched to more widely used platforms. Lastly, encouraging patients to involve caregivers and family members in the actual visit may also increase successful completion by improving video visit technology navigation and in-use troubleshooting.16
The Way Forward for Telehealth Visits
The advantages of a video visit in the management of liver disease are quantifiable. Benefits include decreased travel time and geographic barriers to receiving specialist care,19,20 comparable clinical outcomes4, and high satisfaction rates.3,18,20 However, little attention has been paid in prior studies to those who declined or were unable to complete a video visit. Such ‘per-protocol’ analyses may obscure how efforts to implement telemedicine could inadvertently widen healthcare disparities.24 Our single-center experience, although limited by sample size and selection-bias, highlights key factors that modify video visit use. Over time, the acceptance of telehealth by patients and institutions has grown to benefit many. Still, barriers persist. Action is needed to avoid further entrenching disparities.
It is important to understand the barriers and facilitators of effective video visit use in order promote its appropriate and equitable use.(Figure 1):
The telehealth visit enrollment process must be simplified and accessible via a range of devices.
Relying on one video visit platform through a patient portal may result in a high rate of default to telephone visits.
Avoiding multistep processes in favor of one-step connections from smartphones, tablets, or computers will improve feasibility and telehealth acceptance.
Patient concerns and presumptions regarding insurance coverage, privacy, and appropriateness of a video visit must be addressed.
The visit type must match the digital literacy and healthcare needs of the patient; if discordant, dissatisfaction in the care received increases.18
Varying levels of digital health literacy necessitate an enrollment and use process with diverse technology support at each step and involvement of caregivers.
Conclusion
Telehealth visits are here to stay. Purposeful actions are necessary to ensure a more successful, but more importantly equitable, use of video visits in the care of persons with liver disease.
Supplementary Material
Acknowledgments
Disclosure:
1. Roles
a. Concept: Louissaint, Tapper, Lok
b. Data Acquisition: Louissaint, Gibbs
c. Analysis: Louissaint
d. Writing: Louissaint
e. Revision: Tapper, Lok, Gibbs
2. Financial support: Dr. Louissaint was supported by T32DK062708. Dr. Tapper is supported by NIDDK K23 DK117055.
Footnotes
Conflicts: Dr. Tapper has served on advisory boards for Mallinckrodt, Kaleido, Rebiotix, Novo Nordisk and Bausch Health, consulted for Allergan, Novartis, and has received unrestricted research grants from Valeant, Gilead.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Tapper EB, Asrani SK. The COVID-19 pandemic will have a long-lasting impact on the quality of cirrhosis care. J Hepatol 2020;73:441–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kochar B, Ufere NN, Nipp R, et al. Video-Based Telehealth Visits Decrease With Increasing Age. Am J Gastroenterol 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serper M, Nunes F, Ahmad N, et al. Positive Early Patient and Clinician Experience with Telemedicine in an Academic Gastroenterology Practice During the COVID-19 Pandemic. Gastroenterology 2020;159:1589–1591.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delman AM, Turner KM, Jones CR, et al. Keeping the lights on: Telehealth, testing, and 6-month outcomes for orthotopic liver transplantation during the COVID-19 pandemic. Surgery 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehrotra A, Bhatia RS, Snoswell CL. Paying for Telemedicine After the Pandemic. JAMA 2021;325:431–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez JA, Betancourt JR, Sequist TD, et al. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care 2021;27:21–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Louissaint J, Lok AS, Fortune BE, et al. Acceptance and use of a smartphone application in cirrhosis. Liver Int 2020;40:1556–1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkatesh V, Bala H. Technology Acceptance Model 3 and a Research Agenda on Interventions. Decision Sciences 2008;39:273–315. [Google Scholar]
- 9.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011;38:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varsi C, Solberg Nes L, Kristjansdottir OB, et al. Implementation Strategies to Enhance the Implementation of eHealth Programs for Patients With Chronic Illnesses: Realist Systematic Review. J Med Internet Res 2019;21:e14255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pew Research Center. Mobile Fact Sheet. Pew Research Center: Internet, Science & Tech. Available at: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/ [Accessed January 20, 2021]. [Google Scholar]
- 12.Bloom PP, Marx M, Wang TJ, et al. Attitudes towards digital health tools for outpatient cirrhosis management in patients with decompensated cirrhosis. BMJ Innovations 2020;6. Available at: https://innovations.bmj.com/content/6/1/18 [Accessed November 19, 2020]. [Google Scholar]
- 13.Kurlander J, Kullgren J, Singer D, Solway E, Malani P, Kirch M, Saini S. Virtual Visits: Telehealth and Older Adults. University of Michigan National Poll on Healthy Aging. October 2019. Available at: http://hdl.handle.net/2027.42/151376. [Google Scholar]
- 14.Powell RE, Henstenburg JM, Cooper G, et al. Patient Perceptions of Telehealth Primary Care Video Visits. Ann Fam Med 2017;15:225–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wegermann K, Wilder JM, Parish A, et al. Racial and Socioeconomic Disparities in Utilization of Telehealth in Patients with Liver Disease During COVID-19. Dig Dis Sci 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lam K, Lu AD, Shi Y, et al. Assessing Telemedicine Unreadiness Among Older Adults in the United States During the COVID-19 Pandemic. JAMA Intern Med 2020;180:1389–1391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nouri S, Khoong EC, Lyles CR, et al. Addressing Equity in Telemedicine for Chronic Disease Management During the Covid-19 Pandemic. NEJM Catal Innov Care Deliv 2020. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7371279/ [Accessed February 16, 2021]. [Google Scholar]
- 18.Serper M, Shaked A, Olthoff KM, et al. A local response to COVID-19 for advanced liver disease: Current model of care, challenges and opportunities. J Hepatol 2020;73:708–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.John BV, Love E, Dahman B, et al. Use of Telehealth Expedites Evaluation and Listing of Patients Referred for Liver Transplantation. Clin Gastroenterol Hepatol 2020;18:1822–1830.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.erper M, Cubell AW, Deleener ME, et al. Telemedicine in Liver Disease and Beyond: Can the COVID-19 Crisis Lead to Action? Hepatology 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee TC, Kaiser TE, Alloway R, et al. Telemedicine Based Remote Home Monitoring After Liver Transplantation: Results of a Randomized Prospective Trial. Ann Surg 2019;270:564–572. [DOI] [PubMed] [Google Scholar]
- 22.Anthony DL, Campos-Castillo C, Lim PS. Who Isn’t Using Patient Portals And Why? Evidence And Implications From A National Sample Of US Adults. Health Aff (Millwood) 2018;37:1948–1954. [DOI] [PubMed] [Google Scholar]
- 23.Le LB, Rahal HK, Viramontes MR, et al. Patient Satisfaction and Healthcare Utilization Using Telemedicine in Liver Transplant Recipients. Dig Dis Sci 2019;64:1150–1157. [DOI] [PubMed] [Google Scholar]
- 24.Rodriguez JA, Clark CR, Bates DW. Digital Health Equity as a Necessity in the 21st Century Cures Act Era. JAMA 2020;323:2381–2382. [DOI] [PubMed] [Google Scholar]
- 25.Hollander JE, Sites FD. The Transition from Reimagining to Recreating Health Care Is Now. NEJM Catal Innov Care Deliv 2020. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7373098/ [Accessed February 16, 2021]. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


