Abstract
Objectives
Health conditions that limit work are associated with myriad socioeconomic disadvantages and around half of Americans could face a work limitation at some point in their working career. Our study examines the relationship between midlife work limitations and two aging outcomes: longevity and healthy aging.
Methods
Using longitudinal data from the Panel Study of Income Dynamics and restricted mortality data, multivariate logistic regressions estimate the odds of desirable aging outcomes around age 65 for individuals with various midlife work limitation histories in samples of around 2,000 individuals.
Results
Midlife work limitations are consistently linked with a lower likelihood of desirable aging outcomes. Temporary limitations are associated with 59% and 69% lower survival and healthy aging odds, respectively. Chronic limitations are associated with approximately 80% lower survival odds and 90% lower healthy aging odds at age 65.
Discussion
Even temporary work limitations can be highly disadvantageous for aging outcomes, emphasizing the need to understand different work limitation histories. Future research should identify underlying mechanisms linking midlife work limitations and less desirable aging outcomes.
Keywords: Disability, Healthy aging, Longevity, Work limitations
Health conditions that interfere with an individual’s ability to engage in the labor market are associated with myriad adverse circumstances. Around half of American workers experience such health conditions—or work limitations—at some point in their working-age career (Laditka & Laditka, 2018a; Meyer & Mok, 2019). On average, individuals reporting work limitations have lower educational attainment and are less likely to marry (Clarke & Latham, 2014), which may affect household financial resources. Household budgets may be further strained by higher medical expenses (Mitra et al., 2009). Although work limitations can be temporary, employment, earnings, and household income noticeably decline (Charles, 2003; Meyer & Mok, 2019). More chronic and severe conditions are linked with precipitous declines in income up to ten years after onset (Charles, 2003; Jolly, 2013; Meyer & Mok, 2019), and may pre-date a complete labor market exit (Meyer & Mok, 2019). More than two million American workers applied for Social Security Disability Insurance annually in recent years, and almost 10 million receive benefits (Social Security Administration, 2019).
Despite the documented challenges and prevalence of work limitations in the United States, we know relatively little regarding how a history of work limitations is associated with an individual’s aging experience. Previous research on aging coupled with knowledge of the deleterious implications of work limitations suggest such health conditions in midlife could be linked with differentiated aging patterns—both in terms of duration and quality of life. The duration of life is objectively measured by survival or longevity. Capturing quality of life in later years is complex. Some research focuses on healthy, successful, or optimal aging experiences to help understand quality of life in older adults. Without a universal definition though, one review found prevalence ranged widely from near zero to 95% (Depp & Jeste, 2006). Some common themes are present throughout various definitions, including the absence of chronic illness, high physical functioning, freedom from disability, and absence of cognitive impairments (Li et al., 2018; McLaughlin, 2017; McLaughlin et al., 2012; Rowe & Kahn, 1987).
McLaughlin et al. (2012) offer a useful conceptualization of healthy aging with four progressively restrictive partitions. Their most restrictive conceptualization of healthy aging—modeled on the traditional Rowe and Kahn (1987) aging model—requires the absence of chronic physical health conditions (arthritis, cancer, chronic lung disease, diabetes, heart disease, psychiatric illness, or stroke), “physiological risk factors” (i.e., obesity and hypertension), and limitations in activities of daily living or instrumental activities of daily living (ADL/IADL). It furthermore requires “high physical functioning”—defined as the absence of physical limitations in 10 of 11 tasks (e.g., picking up a dime or using stairs)—and “high cognitive functioning”—defined as scoring in the top half of cognitive assessments. Their Level I Healthy Aging adopts the requirements of this most restrictive definition, but does not require an absence of obesity and hypertension, and relaxes cognition requirements to the absence of cognitive impairment. Level II allows individuals with a history of asymptomatic chronic health conditions (i.e., those which do not require medication, therapy, treatment, and do not limit usual activities) to qualify as healthy agers, while Level III eliminates considering chronic health conditions all together (McLaughlin et al., 2012). Naturally, these progressively less restrictive definitions of Healthy Aging lead to increasing population prevalence from 3% to 36%, and the authors conclude that Levels II and III are perhaps the most useful based on the ability to specifically identify individuals most likely to experience mortality (McLaughlin et al., 2012). Our analysis follows their suggestion, as our main measure of healthy aging reflects their Level II. However, for completeness, we alternatively examine healthy aging definitions that reflect their Level I or Level III definitions.
Work limitations relate to poor health, lower socioeconomic status, and reduced work. These linkages suggest a history of work limitations could be associated with poorer aging outcomes. Clark and Latham (2014) found early midlife work limitations are associated with lower levels of self-rated health status later in life. Self-assessed poor health in midlife is also related to the development of both pre-frailty and frailty in old age (Huohvanainen et al., 2016), and may predict mortality (Idler & Angel, 1990; Woo & Zajacova, 2017). As highlighted above, work limitations are linked to protracted lower socioeconomic status (Brucker et al., 2015; Charles, 2003; Clarke & Latham, 2014; Jolly, 2013; Meyer & Mok, 2019), which, in turn, may be associated with poorer aging outcomes. Most strikingly, the life expectancy gap between the richest and poorest 1% in the United States is over 10 years (Chetty et al., 2016). Household wealth and higher educational attainment is positively correlated with the odds of healthy aging (McLaughlin, 2017; McLaughlin et al., 2012), and the education–life expectancy gap may be increasing over time (Meara et al., 2008; Montez et al., 2011). Case and Deaton (2020) report rising mortality rates uniquely affecting U.S. non-Hispanic Whites without a college degree due to “deaths of despair”—that is, accidental poisonings (drug overdoses), suicide, chronic liver disease, and cirrhosis—and they note an accompanying increased portion of that population reporting fair or poor health (Case & Deaton, 2020, p. 75–77). Work itself may directly grant mental health benefits that would be diminished or absent depending on the severity of work limitations. Jahoda (1981) theorized that apart from financial gain, work provides psychological benefits through five latent functions of work: time structure, social contacts, goals and purposes, status and identity, and regular activity. Zechmann and Paul (2019) support the theory, finding that unemployed individuals gaining employment experienced a decrease in psychological distress, and that many of the five latent functions of employment helped explain that change. Buttressing an argument linking work to long-term health, recent evidence from Caputo et al. (2020) found that women who worked consistently over 20 years at midlife lived longer and reported fewer depressive symptoms or functional limitations in late life. Additionally, unemployment is associated with increased mortality risk (Tapia Granados et al., 2014).
Because work limitations are typically self-reported, individual variation in reports may exist through perceptions of the interaction of health, work, and one’s environment. Poorer health is conceptually linked with work limitations as it is a key feature captured in a commonly used survey question: a health condition that limits work ability. Reports of pain, chronic health conditions, and obesity are also associated with work limitations (Kapteyn et al., 2008; Kreider, 1999; Sturm et al., 2004). Social context including social acceptability and awareness of disability benefit receipt within individual social networks could influence self-reports of work limitations (Kapteyn et al., 2007; Van Soest et al., 2011). Recessions and high unemployment can induce disability applications and increase the number of beneficiaries (Maestas et al., 2021), and disability benefits might incentivize labor market exits (Maestas et al., 2013)—which may lead to work limitation self-reports. Workplace environments also matter. Workers with accommodations or in accessible work environments may not report work limitations (Maestas & Mullen, 2019). Evidence from the Netherlands suggests that perceived access to flexible work arrangements and comfort in disclosure is associated with fewer self-reports of work limitations (Vanajan et al., 2020).
Conceptually, work limitations can be related to adverse aging outcomes such as decreased longevity and lower likelihoods of healthy aging through various pathways. A work limitation could cause poor aging outcomes if it has negative effects on health via income loss (Charles, 2003; Jolly, 2013; Meyer & Mok, 2019), social isolation, and/or mental health effects (Jahoda, 1981). At the same time, a work limitation could be due to health factors that also impact aging outcomes. Midlife work limitations could result from a pre-existing health condition, impairment, accident, or exposure to a health shock (e.g., pandemic) from birth or childhood that may also negatively impact aging outcomes (e.g., Almond, 2006; Almond & Mazumder, 2005; Laditka & Laditka, 2018b; Zablotsky et al., 2019). For instance, approximately one in six children experience a developmental disability including attention deficit/hyperactivity disorder, autism, hearing or vision loss, learning disabilities, and others (Zablotsky et al., 2019), which may limit the ability to work in midlife and may also impact longevity. Poor health and work limitations could also be a result of fewer resources in childhood (Case et al., 2002), lower educational attainment (Conti & Heckman, 2010), inadequate access to health insurance (Boudreaux et al., 2016; Lykens & Jargowsky, 2002; Miller & Wherry, 2019), workplace injury or illness, or living in poorly accessible environments (e.g., transportation or workplace barriers for persons with mobility limitations). Thus, the association of midlife work limitations with less desirable aging outcomes could reflect the impact of work limitations on health later in life as well as the impact of factors that influence both midlife work limitations and aging outcomes.
There is limited direct evidence to support adverse aging outcomes for individuals confronted with work limitations at midlife. Work limitations are sometimes used as an indicator of disability, and a few studies have found increased mortality risk for persons with disabilities (Forman-Hoffman et al., 2015; Rupp & Dushi, 2017; Verbrugge et al., 2017). A few studies in the U.S. population take into account work limitations in the aging experience by controlling for the characteristic when estimating mortality risk (Karraker et al., 2015; Rupp & Dushi, 2017; Tapia Granados et al., 2014). Although these studies provide suggestive evidence that work limitations are deleterious for longevity, these studies measure work limitations only once (Karraker et al., 2015; Rupp & Dushi, 2017) or have brief temporal follow-up (Tapia Granados et al., 2014). Because work limitation experiences and consequences vary widely (Charles, 2003; Meyer & Mok, 2019), previous studies do not adequately address the long-term aging outcomes for persons with various histories of work limitations. Outside the United States, poor levels of self-reported work ability in midlife were associated with increased mortality rates with 28 years of follow-up in a Finnish cohort of municipal employees (von Bonsdorff et al., 2011), and impairments from work injuries were associated with premature mortality after 19 years of follow-up in Canada (Scott-Marshall et al., 2014). While these studies again offer suggestive evidence of adverse aging outcomes for work-limited individuals, analyzing mortality patterns and quality of life in later years (i.e., healthy aging) in the U.S. population is also warranted. In particular, it is imperative to consider different experiences of midlife work limitations ranging from temporary to chronic and severe limitations.
Our study fills this void by examining the association of midlife work limitations with longevity and healthy aging. Both outcomes are informative on aging experiences as longevity can provide an objective measure, but it does not necessarily address quality of life. We hypothesize that: (a) midlife work limitations have a strong adverse association with longevity and healthy aging at age 65, and (b) chronic and/or severe limitations have the strongest negative relationship with aging outcomes. Our analysis bridges literatures concerning healthy aging and longevity by analyzing associations of midlife experiences for both outcomes. Using data that capture up to 20 annual reports of midlife experiences from age 40 to 59, our study can capture nuanced differences in midlife experiences of work limitations in terms of duration and severity. If certain midlife experiences are found to be associated with poorer aging outcomes, policymakers and practitioners can take steps to identify persons at greater risk in midlife and potentially mitigate the effects of those midlife experiences on subsequent aging outcomes. Our analysis corroborates the hypotheses above, presenting new evidence on the adverse association of midlife work limitations with longevity and healthy aging.
Method
Data
Data are from the Panel Study of Income Dynamics (PSID) and include restricted mortality data (PSID, 2018). PSID is an ideal data source for this analysis due to its panel structure spanning over 50 years. In contrast to other aging data sets (e.g., the Health and Retirement Study typically begins observing individuals who are over 50 years old biennially), the PSID can accommodate observing aging outcomes at age 65 and older as well as up to 20 years of reports from ages 40 to 59 to richly characterize midlife. There are two aging outcomes of interest: (a) survival and (b) healthy aging. We focus on outcomes around age 65 (i.e., 1933–1952 birth cohorts) to address the experience of older Americans of traditional full retirement age while also optimizing the sample size. Higher age thresholds are considered in sensitivity analyses (i.e., around ages 70 and 75), and results are robust. The two aging outcomes necessitate distinct samples of individuals (n = 2,156 and n = 2,041 for mortality and healthy aging, respectively), although there is significant overlap. Most individuals in the healthy aging sample are also in the survival sample, and the deceased of the survival sample are excluded from the healthy aging sample. Rare deviations can occur, however. For example, someone turning 65 in a calendar year (but aged 64 at the time of interview) can be included in the healthy aging sample but be deceased by their 65th birthday. All analyses are weighted and adjusted for PSID survey design using cross-sectional weights and all specifications use regional and quintile-binned birth cohort fixed effects. For age 65 analyses, the five birth cohort quintiles are (a) January 1933 to June 1939, (b) July 1939 to November 1944, (c) December 1944 to March 1948, (d) April 1948 to September 1950, and (e) October 1950 to December 1952. The Institutional Review Board of Fordham University approved this study (protocol #995).
The Samples and Dependent Variables
Each sample is dichotomously divided into individuals who experience success (survival or healthy aging), and those who do not (the deceased or non-healthy agers). Survival is observed at ages 65, 70, and 75 while healthy aging is observed among individuals turning 65–66 or 70–71 between 1999 and 2017. The main results use younger ages to optimize sample size, and older ages are examined in sensitivity checks. Analyses are conditioned on survival to 1997—the first year when cross-sectional weights are available. Longitudinal weights reduce the healthy aging sample size, but results are robust. PSID began observing characteristics of healthy aging (defined below) in 1999, which coincided with a switch to biennial surveys. This means that not everyone can be observed at age 65 (or 70) and some are observed at an adjacent age (i.e., age 66 or 71).
This study uses a comparable definition of healthy aging to Level II healthy aging from McLaughlin et al. (2012), although more and less restrictive partitions are also examined (a Level I definition is more restrictive by requiring the complete absence of chronic health conditions and a Level III definition is less restrictive by eliminating chronic health conditions from consideration; see Supplementary Table A2). Healthy aging is defined as the absence of: activity-limiting disease (arthritis, cancer, diabetes, heart conditions, lung conditions, or stroke that pose some limit to the individual’s normal daily activities), permanent memory loss, and ADL (i.e., bathing, dressing, eating, getting in and out of bed, toileting, and walking)/IADL (i.e., managing finances, preparing meals, running errands, and using the telephone—unobserved in 1999 and 2001) limitations. Respondents self-report each of these items separately in the PSID. Additional cognition elements are surveyed beginning in 2017; however, we include only permanent memory loss for consistency of the outcome across survey waves.
Characterizing Midlife Work Limitations
Midlife work limitations may capture pivotal experiences for later aging patterns and are the key independent variable in this analysis. With up to 20 midlife reports, there is a wide variety of work limitation experiences that the PSID can uniquely capture, including episodic or temporary limitations. We leverage responses to survey questions from waves when individuals are between ages 40 and 59 to categorize them into four mutually exclusive categories as in Meyer and Mok (2019). In order to be eligible for sample inclusion, individuals must be observed in at least 50% of survey waves during midlife. Each wave a respondent reports no “physical or nervous condition that limits the type of work or the amount of work [he/she] can do” is identified as a wave without a work-limiting condition. Respondents indicating the presence of a work-limiting condition are asked follow-up questions to gauge severity. Those reporting conditions that limit work “just a little” or “not at all” are deemed to have a mild condition, while those with conditions that interfere “somewhat” are classified with moderate conditions. Reports of conditions that limit work “a lot” or that the individual “can do nothing” are categorized as severe.
Following Meyer and Mok (2019), persons who never report a work limitation between the ages of 40 and 59 are categorized as non-limited. Due to the biannual survey structure in later years, we delineate temporary and chronic work limitations based on the percentage of waves observed rather than a nominal number of waves as in Meyer and Mok (2019). Those with a reported limiting condition less than 25% of the time are categorized with a temporary limitation, while those with a condition 25% of the time or more are classified as chronically limited. Chronic work limitations are disaggregated into severe and not-severe conditions based on the ratio of severe reports relative to positive reports. As in Meyer and Mok (2019), a severity ratio at or above 50% constitutes a severe chronic work-limiting condition, while a severity ratio below 50% is a non-severe chronic work-limiting condition (in sensitivity analyses—Supplementary Table A1, column 9 and Supplementary Table A2, column 7—we split “chronic, not severe” conditions into either “chronic, never severe” or “chronic, at least one severe report” conditions and results are robust). We do not explicitly parse out early versus late onset of work-limiting conditions in midlife. Because “chronic” conditions are present at least 25% of the time in midlife, and often longer, by construction they must begin relatively earlier in the life course. For example, consider an individual from the 1952 birth cohort. They are observed in midlife annually from 1992 to 1997 and biennially from 1999 to 2011. With at most 13 waves of midlife observations, at least four of these must have a positive work limitation report to classify as “chronic.” The latest possible onset for this hypothetical individual’s chronic work limitation would be age 53 (in 2005). In our healthy aging sample, 90% of identified chronic work limitations begin prior to age 50. Temporary work limitations then consist of a more heterogeneous group of episodic limitations—recovering either in midlife or beyond—and beginning spells of what will be chronic (and unobserved) work limitations into later life.
Covariates
We control for several characteristics known to be associated with aging outcomes including: sex (Chetty et al., 2016; McLaughlin, 2017; McLaughlin et al., 2012), race (McLaughlin et al., 2012; Singh & Siahpush, 2014), education (McLaughlin, 2017; McLaughlin et al., 2012; Meara et al., 2008; Montez et al., 2019), urbanicity (Singh & Siahpush, 2014), and smoking (Södergren, 2013). Sex is a binary indicator for female while race is a binary indicator for any racial or ethnic minority. Educational attainment is categorical: less than high school (reference), high school or General Equivalency Diploma, some college, or four-plus years of college. Current urban/rural residency is a binary indicator for living in a metropolitan area (i.e., areas with local population at or above 250,000), and smoking is a binary indicator for ever smoking.
Because our study examines the influence of midlife experiences on aging outcomes, we also control for marriage and poverty between the ages of 40 and 59. These characteristics may differentiate aging experiences (Chetty et al., 2016; Dupre et al., 2009; Li et al., 2018; McLaughlin, 2017; Tucker et al., 1996), and relate to midlife work limitations (Brucker et al., 2015; Charles, 2003; Clarke & Latham, 2014; Jolly, 2013; Meyer & Mok, 2019). Midlife marriage is the percent of waves an individual is married, while poverty captures duration and severity over midlife. Real family income as a ratio to the Federal Poverty Level (adjusted for family size and age of head of household in 2016 dollars) is calculated in each wave. The ratio is rescaled such that persons with income above 300% of this threshold are coded zero (for no material deprivation), and those with income at or below 100% of the threshold are coded one (representing full material deprivation). Midlife poverty is the average of this rescaled ratio, and ranges from zero to one.
Analysis
Due to potential collinearity of poverty with work limitations and education, there are four specifications, each represented by the general equation below.
In all specifications, represents individual characteristics including sex, race/ethnicity, education, metropolitan residence, and smoking history. represents the individual’s midlife marital status, poverty, and work limitations. All models include regional () and quintile-based birth cohort fixed effects (). Model 1 reports the full model with all covariates and is the preferred model. We include three additional models in the main results to address concerns surrounding the correlation of midlife work limitations with midlife poverty and/or education, which can exceed 30% in the healthy aging sample. Models 2 and 3 eliminate midlife poverty or work limitations, respectively, and Model 4 is without work limitations and education. Individuals with missing data were dropped from the analysis (N = 553 in the healthy aging sample, or 21.3%). The most common source of missing data is missing only midlife information (N = 361 in the healthy aging sample, or 65.3% of missing observations). The prevalence of healthy aging across individuals with complete or missing midlife data is similar.
Results
Descriptive Statistics
Table 1 shows that women are more prevalent among survivors yet less prevalent among healthy agers at age 65. Fewer minorities are found among both survivors and healthy agers around age 65. Individuals experiencing favorable aging outcomes tend to have more education, and in midlife were married longer and experienced less poverty. While around 60% of the sample reports previous smoking, a statistically lower proportion of smokers is found among the groups experiencing healthy aging and longevity.
Table 1.
Descriptive Statistics for Samples at Age 65
| S sample | S = 1 | S = 0 | HA sample | HA = 1 | HA = 0 | |
|---|---|---|---|---|---|---|
| Dependent variable | 0.915 | 0.581 | ||||
| (0.008) | (0.018) | |||||
| % Female | 0.535 | 0.546 | 0.418* | 0.545 | 0.516 | 0.585** |
| (0.008) | (0.009) | (0.046) | (0.01) | (0.011) | (0.02) | |
| % Other race/ethnicity (ref. non-Hispanic White) | 0.165 | 0.159 | 0.23* | 0.162 | 0.138 | 0.195** |
| (0.015) | (0.015) | (0.038) | (0.015) | (0.016) | (0.018) | |
| % <HS | 0.0882 | 0.0807 | 0.169** | 0.0801 | 0.0465 | 0.127*** |
| (0.008) | (0.008) | (0.028) | (0.008) | (0.006) | (0.014) | |
| % HS/GED | 0.319 | 0.312 | 0.4* | 0.313 | 0.301 | 0.328 |
| (0.016) | (0.015) | (0.038) | (0.015) | (0.019) | (0.016) | |
| % Some college | 0.254 | 0.259 | 0.208+ | 0.257 | 0.245 | 0.273 |
| (0.012) | (0.012) | (0.029) | (0.011) | (0.014) | (0.016) | |
| % 4+ years college | 0.338 | 0.349 | 0.224** | 0.35 | 0.407 | 0.272*** |
| (0.018) | (0.018) | (0.042) | (0.018) | (0.02) | (0.022) | |
| % Metro area | 0.648 | 0.651 | 0.621 | 0.656 | 0.671 | 0.634 |
| (0.02) | (0.019) | (0.051) | (0.019) | (0.024) | (0.022) | |
| % Ever smoked | 0.609 | 0.594 | 0.777*** | 0.595 | 0.561 | 0.642*** |
| (0.013) | (0.013) | (0.034) | (0.012) | (0.014) | (0.019) | |
| Midlife characteristics | ||||||
| Mean % time married | 0.78 | 0.787 | 0.705* | 0.785 | 0.828 | 0.725*** |
| (0.014) | (0.014) | (0.04) | (0.013) | (0.014) | (0.018) | |
| Mean Poverty index | 0.137 | 0.125 | 0.271*** | 0.127 | 0.0897 | 0.178*** |
| (0.008) | (0.007) | (0.034) | (0.007) | (0.006) | (0.011) | |
| % Never work limited | 0.524 | 0.551 | 0.229*** | 0.554 | 0.733 | 0.306*** |
| (0.019) | (0.019) | (0.035) | (0.018) | (0.018) | (0.02) | |
| % Temporary work limit | 0.236 | 0.236 | 0.232 | 0.23 | 0.198 | 0.276** |
| (0.012) | (0.014) | (0.039) | (0.013) | (0.015) | (0.022) | |
| % Chronic, not severe work limit | 0.163 | 0.146 | 0.346*** | 0.151 | 0.058 | 0.279*** |
| (0.01) | (0.01) | (0.039) | (0.01) | (0.008) | (0.019) | |
| % Chronic, severe work limit | 0.0778 | 0.067 | 0.194** | 0.0652 | 0.0118 | 0.139*** |
| (0.01) | (0.009) | (0.04) | (0.008) | (0.004) | (0.015) | |
| Observations | 2,156 | 1,940 | 216 | 2,041 | 1,147 | 894 |
Notes: Source: Authors’ calculations using PSID core data. GED is the General Education Development tests.
Columns (1) to (3) represent the Survival sample (S), while columns (4) to (6) represent the Healthy Aging (HA) sample. ***p < .001, **p < .01, *p < .05, + p < .1.
Importantly, the prevalence of midlife work limitations is significantly different for those who experience favorable aging outcomes relative to individuals with adverse aging outcomes. Only 23% of deceased individuals at age 65 never experienced work limitations in midlife while 55% of survivors were never work-limited. Similar patterns emerge with healthy aging: 73% of healthy agers never had work limitations in midlife compared to just 31% of non-healthy agers. Table 1 also highlights that midlife work limitations do not preclude healthy aging. More than a quarter of this sample’s healthy agers also experienced work limitations in midlife, although most of these limitations were temporary.
Survival
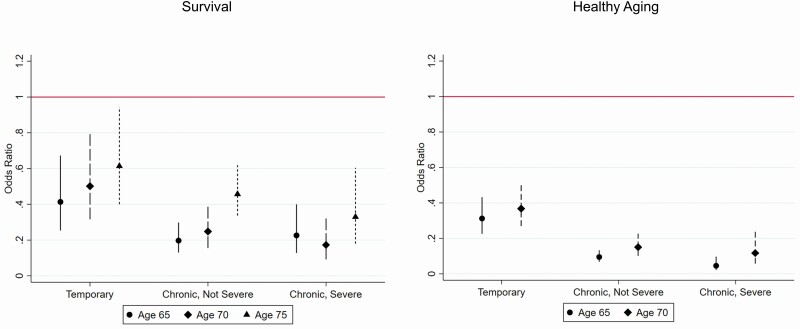
Results in Table 2 suggest that work limitations in midlife are particularly detrimental for longevity, net of other characteristics. Persons who experienced a temporary work limitation in midlife experience 59% lower adjusted odds of survival to age 65 relative to those who never experience a work limitation in midlife. Those experiencing chronic work limitations (regardless of severity) have an 80% reduction in adjusted survival odds to age 65. Midlife poverty may be correlated with midlife work limitations; however, removing the poverty index from the model’s control variables does not materially change the association of work limitations on survival (Model 2). Removing midlife work limitations and educational attainment from the model, however, reduces the odds ratio on the poverty index (Models 3 and 4). Midlife work limitations therefore are a key characteristic associated with survival to age 65 and Model 1 is preferred. The association of work limitations with survival at older ages is generally consistent (see left panel Figure 1 and Supplementary Table A1, columns 2–3); however, odds ratios tend to be slightly higher at each successive examined age. For example, by age 75, those who had experienced a temporary work limitation in midlife are only estimated to experience 39% lower odds of survival. By age 75, however, there appears to be more of a severity gradient for midlife work limitations among those with chronic limitations.
Table 2.
Correlates of Survival to Age 65 (odds ratios)
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Female (ref. Male) | 1.830** | 1.843** | 1.809* | 1.693* |
| (0.411) | (0.414) | (0.423) | (0.396) | |
| Other race/ethnicity (ref. non-Hispanic White) | 0.913 | 0.796 | 1.001 | 0.881 |
| (0.249) | (0.185) | (0.266) | (0.227) | |
| HS/GED (ref. <HS) | 1.040 | 1.233 | 1.202 | |
| (0.263) | (0.307) | (0.302) | ||
| Some college (ref. <HS) | 1.874** | 2.361*** | 1.968* | |
| (0.432) | (0.555) | (0.500) | ||
| 4+ years college (ref. <HS) | 1.918* | 2.534** | 2.309* | |
| (0.606) | (0.842) | (0.755) | ||
| Metro area | 1.046 | 1.110 | 0.993 | 1.070 |
| (0.225) | (0.235) | (0.203) | (0.224) | |
| Ever smoked (ref. never) | 0.565* | 0.588* | 0.513** | 0.475** |
| (0.138) | (0.145) | (0.114) | (0.105) | |
| Midlife characteristics | ||||
| % Time married | 1.086 | 1.397 | 1.234 | 1.053 |
| (0.318) | (0.371) | (0.350) | (0.321) | |
| Poverty Index | 0.361* | 0.200*** | 0.139*** | |
| (0.160) | (0.0844) | (0.0608) | ||
| Temporary work limit (ref. never) | 0.413*** | 0.392*** | ||
| (0.100) | (0.100) | |||
| Chronic, not severe work limit (ref. never) | 0.197*** | 0.182*** | ||
| (0.0405) | (0.0381) | |||
| Chronic, severe work limit (ref. never) | 0.226*** | 0.188*** | ||
| (0.0640) | (0.0543) | |||
| Constant | 5.058* | 2.814 | 2.709 | 6.089* |
| (4.022) | (1.921) | (1.994) | (4.285) | |
| Observations | 2,156 | 2,156 | 2,156 | 2,156 |
| F | 12.59 | 11.82 | 8.384 | 11.31 |
Notes: Source: Authors’ calculations using PSID core and restricted mortality data.
Exponentiated coefficients are from logistic regressions. Both coefficients and (standard errors) are adjusted for complex survey design. All models include a constant, regional and binned quintile birth cohort fixed effects. ***p < .001, **p < .01, *p < .05.
Figure 1.
Odds ratios of healthy aging and survival for midlife experiences with work limitations. Source: Authors’ calculations using PSID core and restricted mortality data. Notes: Coefficients are based on the preferred logistic model (Model 1) in all cases. Relevant odds ratios reported in Tables 2 and 3, column 1 and Supplementary Table A1, columns 2–3, Supplementary Table A2, column 2. PSID = Panel Study of Income Dynamics.
Stratified results in Supplementary Table A1 by sex and race/ethnicity suggest the association of midlife work limitations is consistent across these demographic groups (Supplementary Table A1, columns 5–8). In these stratifications, however, sample sizes are small, particularly for non-Hispanic Blacks, warranting considerable caution in interpretation. As an example, the sample of non-Hispanic Blacks is so small that it does not have sufficient observations to report estimates on education coefficients, although they are included in the model as controls. Splitting the “chronic, not severe” work limitation category into “never severe” and “sometimes severe” (i.e., at least one severe report, but less than 50%) suggests those with never severe work limitations, although chronic in nature, are more similar to persons with temporary limitations. Individuals with some severe reports, but less than half of reports, appear worst off (Supplementary Table A1, column 9).
Healthy Aging
It is also important to consider the quality of aging preceding mortality, which we examine as healthy aging. Table 3 presents results for the healthy aging sample at age 65. Relative to persons who never experience work limitations in midlife, those with a temporary limitation experience 69% lower adjusted odds of healthy aging at age 65, while those with a chronic limitation experience more than a 90% reduction in adjusted healthy aging odds. Removing midlife poverty as a control variable does not meaningfully alter the association of midlife work limitations with healthy aging (Model 2). However, removing work limitations from the model significantly alters the association of midlife poverty with healthy aging (Models 3 and 4). This suggests part of the poverty-healthy aging association may run through work limitations and it is important to include both experiences in the specification. The strong gradient between work limitations and healthy aging observed at age 65 persists at age 70 (right panel of Figure 1, Supplementary Table A2, column 2), although the odds ratios in each work limitation category are slightly higher.
Table 3.
Correlates of Healthy Aging to Age 65 (odds ratios)
| (1) | (2) | (3) | (4) | |
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| Female (ref. Male) | 0.829 | 0.830 | 0.821+ | 0.784* |
| (0.0988) | (0.0986) | (0.0867) | (0.0809) | |
| Other race/ethnicity (ref. non-Hispanic White) | 0.882 | 0.862 | 1.055 | 0.985 |
| (0.140) | (0.138) | (0.136) | (0.126) | |
| HS/GED (ref. <HS) | 1.639* | 1.693* | 1.863** | |
| (0.397) | (0.375) | (0.404) | ||
| Some college (ref. <HS) | 1.701* | 1.771* | 1.821** | |
| (0.431) | (0.393) | (0.404) | ||
| 4+ years college (ref. <HS) | 2.349** | 2.462*** | 2.743*** | |
| (0.636) | (0.564) | (0.672) | ||
| Metro area (ref. non-metro) | 1.195 | 1.205 | 1.049 | 1.083 |
| (0.180) | (0.181) | (0.144) | (0.144) | |
| Ever smoked (ref. never) | 0.850 | 0.850 | 0.762* | 0.725** |
| (0.107) | (0.106) | (0.0813) | (0.0764) | |
| Midlife characteristics | ||||
| Marriage history | 1.655* | 1.697* | 1.679** | 1.530* |
| (0.372) | (0.350) | (0.305) | (0.262) | |
| Poverty Index | 0.824 | 0.295*** | 0.193*** | |
| (0.292) | (0.0896) | (0.0505) | ||
| Temporary work limit (ref. none) | 0.312*** | 0.310*** | ||
| (0.0505) | (0.0501) | |||
| Chronic, not severe work limit (ref. none) | 0.0948*** | 0.0935*** | ||
| (0.0163) | (0.0161) | |||
| Chronic, severe work limit (ref. none) | 0.0454*** | 0.0444*** | ||
| (0.0171) | (0.0166) | |||
| Constant | 2.004 | 1.849 | 1.126 | 3.001*** |
| (0.978) | (0.801) | (0.468) | (0.834) | |
| Observations | 2,041 | 2,041 | 2,041 | 2,041 |
| F | 26.43 | 28.27 | 7.613 | 7.819 |
Notes: Source: Authors’ calculations using PSID core data.
Exponentiated coefficients are from logistic regressions. Both coefficients and (standard errors) are adjusted for complex survey design. Healthy aging binary is observed at age 65 or 66. All models include a constant, regional and binned quintile birth cohort fixed effects. ***p < .001, **p < .01, *p < .05, +p < .1.
Results in Supplementary Table A2 demonstrate that work limitations appear deleterious for healthy aging odds even with a more or less inclusive definition, similar to the level I and level III definitions from McLaughlin et al. (2012) (columns 9–10). Gender- and race/ethnicity-stratified models again reveal a similar gradient in midlife work limitations, although there is limited evidence supporting a stronger gradient for non-Hispanic Blacks (Supplementary Table A2, columns 3–6). Stratifications by sex and race/ethnicity, however, warrant considerable caution in interpretation due to small sample sizes. Splitting the “chronic, not severe” group in two, we find that chronic reports that are never severe in nature still have an 88% reduction in the odds of healthy aging (Supplementary Table A2, column 7).
Discussion
This study highlights the critical but overlooked association of midlife work limitations with aging outcomes. Work limitations affect nearly half of U.S. workers (Laditka & Laditka, 2018a; Meyer & Mok, 2019), although cross-sectional prevalence rates would suggest fewer than one in five might be affected (Meyer & Mok, 2019). Thus, to gain a better understanding of the association of a wide range of work limitation experiences with aging outcomes, it is imperative to richly capture midlife. Leveraging the unique intersection of up to 20 annual reports of work limitations and other midlife characteristics along with aging outcomes from the PSID, our study can address the association of nuanced midlife experiences on aging outcomes. Specifically, our study can distinguish the association of temporary work limitations—which are the most common—with aging outcomes, rather than assuming that work limitation experiences are homogeneous.
Supporting our first hypothesis, a work limitation of any length or severity in midlife has a strong negative association with longevity and healthy aging outcomes. Supporting the second hypothesis, chronic work limitations, defined as limitations present for 25% of midlife or more, appear to have the most disadvantageous outcomes, reducing the odds of healthy aging by more than 90% and reducing the odds of survival to age 65 by 80%. However, it is important that temporary limitations also have a strong link to poorer aging outcomes as well. Persons with temporary limitations, defined as limitations present for less than 25% of midlife, have nearly 70% reduced odds of healthy aging and 60% lower odds of survival to age 65. Results are stable to a variety of sensitivity analyses, including removing the Survey of Economic Opportunity sample that had some sampling irregularities at the time of survey design (Brown, 1996), focusing on a subset of birth cohorts (1941–1952) thought to have more consistent reports of work limitation by sex, and using probit or complementary log-log specifications (probit and complementary log-log specifications not shown).
Although midlife work limitations may have a strong conceptual relationship with healthy aging, as highlighted in Table 1, longevity and healthy aging are feasible despite midlife work limitations. However, our results point to this midlife experience—even when temporary in nature—being critically disadvantageous for favorable aging patterns. This is consistent with long-term follow-up studies in Finland (von Bonsdorff et al., 2011) and Canada (Scott-Marshall et al., 2014). Our results also support U.S. studies identifying increased mortality risk for persons experiencing work limitations (Karraker et al., 2015; Rupp & Dushi, 2017; Tapia Granados et al., 2014). Additionally, the results expand knowledge on long-term aging patterns given heterogeneous work limitations in midlife and specifically parsing out chronicity and severity.
We do not explicitly address the timing of work-limitation onset, although most chronic limitations begin before age 50. Therefore, our results of particularly disadvantageous aging outcomes for persons with chronic work limitations could alternatively reflect early onset relative to later onset. We also note that our analysis suggests the odds of positive aging outcomes for persons with work limitations in midlife are typically lower when outcomes are measured earlier in life (i.e., age 65 vs. age 70; Figure 1). Smaller sample sizes could have less precise estimation at later ages; however, initial disadvantage could also dissipate with time due to coping strategies or access to public retirement (Social Security) and health insurance (Medicare) benefits.
There are limitations to this study. Samples are small for some stratifications and the precision of some estimated controls is low. We also do not identify the pathways or mechanisms by which work limitations may precede poorer aging outcomes. Work limitations are linked with poorer health, economic security, and labor market participation—each being associated with poorer aging outcomes (e.g., Caputo et al., 2020; Chetty et al., 2016; Huohvanainen et al., 2016; Jahoda, 1981). In the case of the healthy aging analysis, a work limitation could also be a direct result of a physical health condition (e.g., stroke) that would preclude qualifying as a healthy ager. We leave pinning down mechanisms to future research. Importantly, we do not observe individuals’ characteristics prior to age 40. Earlier life events could affect development of work limitations in midlife. Individuals exposed to the 1918 pandemic in utero were more likely to develop work limitations and health issues (Almond, 2006; Almond & Mazumder, 2005) and adverse childhood circumstances are associated with functional difficulties later in life (Laditka & Laditka, 2018b). Furthermore, approximately one in six children experience a developmental disability (Zablotsky et al., 2019). Although children were not followed into adulthood, one may conjecture that some of these children may have work limitations as they age. Finally, there is a link between family income and childhood health (e.g., Case et al., 2002), and health shocks due to injury or illness can occur before age 40. Each of these could influence developing work limitations in midlife. The Bureau of Labor Statistics reports that there were nearly 3 million nonfatal workplace injuries in 2019, and nearly 1 million injuries necessitated at least a one-day absence (Bureau of Labor Statistics, 2020). Our results are unable to address determinants of work limitations that might also influence aging limitations. We conducted additional analyses excluding individuals with work limitations at the first midlife observation as these individuals could be more likely to have experienced adverse childhood circumstances or developmental disabilities that may have led to their work limitation in midlife: results are robust to excluding these individuals (Supplementary Table A1, column (10) and Supplementary Table A2, column (8)). Although this does not preclude the possibility that early-life circumstances influenced the development of work limitations in midlife, it does lessen concern with persistent childhood or early adult conditions being the driving force behind our results.
Another key limitation relates to the measurement of self-reported work limitations. Work limitation self-reports could reflect justification bias (Black et al., 2017) and/or may be influenced by unemployment, disability insurance benefit generosity, and relaxed definitions of disability (Autor & Duggan, 2003). At the same time, a self-reported work limitation at midlife captures a health problem or disability that is severe enough to impact work (Benítez-Silva et al., 2004) and economic outcomes (Meyer & Mok, 2019). Functional limitations or ADL limitations as alternative measures of disability are not available until later waves of the PSID. However, substituting self-reported health status for work limitations suggests persons in poorer midlife health also experience worse aging outcomes. Furthermore, work limitations reports are close to the definition of disability used to determine public disability insurance eligibility, pointing toward the need for further research on how these programs might affect aging outcomes.
Insights into the long-term implications of midlife work limitations may prove particularly helpful in understanding other observed aging patterns. Case and Deaton (2020) report a rising all-cause mortality trend among non-Hispanic Whites with less than a college degree. They hypothesize that the trend could be attributable to a combination of loss of resources, vocation, and social support in the population. The loss of vocation and social support in particular aligns well with the theorized latent functions of employment discussed by Jahoda (1981) that could be diminished or absent for persons with work limitations.
There is a strong link between poverty and work limitations (Brucker et al., 2015; She & Livermore, 2007) with evidence of decreasing financial resources shortly before the onset of work limitations (Charles, 2003; Jolly, 2013; Meyer & Mok, 2019). For individuals with work limitations who also experience poverty in midlife, there may be additional deprivations, not noted in the current study, that are associated with poorer aging outcomes. An inability to consistently access necessary food for a healthy, active midlife, for example, may impact aging outcomes. Similarly, housing deprivations such as instability, overcrowding, or unsafe conditions may have longer-term impacts. While there are public programs and policies in the United States which can boost income (e.g., Earned Income Tax Credit, Temporary Assistance for Needy Families) or increase resources (e.g., rental housing assistance vouchers, Supplemental Nutrition Assistance Program), little is known about how participation in these programs throughout the life span affects well-being and mortality for older Americans. Recent research, however, suggests that the U.S. disability insurance program may decrease mortality risk, particularly among low-income recipients (Gelber et al., 2018). Expansions of public health insurance availability for low-income populations, made possible by Medicaid expansions and the Affordable Care Act, could also decrease claims for means-tested disability income support (Supplemental Security Income) in some contexts, possibly owing in part to an improvement in health (Chatterji & Li, 2017). Our paper provides evidence supporting the need for further research along these lines on the impact of such programs on aging outcomes.
Although the pathways by which persons with midlife work limitations experience less-desirable aging outcomes are far from clear, a renewed commitment to workplace accommodations to prevent labor market detachment may be of interest. Vanajan et al. (2020) suggest employer flexible work arrangements may decrease reported work limitations. Employers must continue to adapt to retain employees who develop conditions that may limit their ability to work. Workplace accommodations, including assistive technology, flexible schedules, or modifications in work tasks, can extend the ability of people with disabilities to remain engaged in the workforce. To ensure that employees actively work with their employers to facilitate sustained employment, employees must not only be aware of their rights in requesting such accommodations but must also be confident that their workplace does not stigmatize persons with disabilities.
Supplementary Material
Funding
This project was funded by a National Institute on Aging grant P01 AG029409. Postdoctoral Trainee funding (K. M. Jajtner) under National Institute on Aging grant T32 AG00129 and support from the Center for Demography of Health and Aging (CDHA) at the University of Wisconsin-Madison under National Institute on Aging core grant P30 AG17266 is also acknowledged. Fordham University’s Alumni Dissertation Fellowship also provided financial support (K. M. Jajtner). Comments from participants of the 2021 Allied Social Sciences Association/Society of Government Economists and 2019 American Public Health Association poster session are appreciated. The collection of data used in this study was partly supported by the National Institutes of Health under grant number R01 HD069609 and R01 AG040213, and the National Science Foundation under award numbers SES 1157698 and 1623684.
Author Contributions
K. M. Jajtner was responsible for data analysis, interpretation, manuscript drafting, and editing. D. L. Brucker was responsible for data interpretation, manuscript drafting, and editing. S. Mitra was responsible for data interpretation, manuscript drafting, and editing.
Stata user-written programs: (Jann, 2014; Wada, 2005).
Conflict of Interest
None declared.
References
- Almond, D. (2006). Is the 1918 influenza pandemic over? Long-term effects of in utero influenza exposure in the post-1940 US population. Journal of Political Economy, 114(4), 672–712. doi: 10.1086/507154 [DOI] [Google Scholar]
- Almond, D., & Mazumder, B. (2005). The 1918 influenza pandemic and subsequent health outcomes: An analysis of SIPP data. The American Economic Review, 95(2), 258–262. doi: 10.1257/000282805774669943 [DOI] [PubMed] [Google Scholar]
- Autor, D. H., & Duggan, M. G. (2003). The rise in the disability rolls and the decline in unemployment. The Quarterly Journal of Economics, 118(1), 157–206. doi: 10.1162/00335530360535171 [DOI] [Google Scholar]
- Benítez-Silva, H., Buchinsky, M., Man Chan, H., Cheidvasser, S., & Rust, J. (2004). How large is the bias in self-reported disability? Journal of Applied Econometrics, 19(6), 649–670. doi: 10.1002/jae.797 [DOI] [Google Scholar]
- Black, N., Johnston, D. W., & Suziedelyte, A. (2017). Justification bias in self-reported disability: New evidence from panel data. Journal of Health Economics, 54, 124–134. doi: 10.1016/j.jhealeco.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Boudreaux, M. H., Golberstein, E., & McAlpine, D. D. (2016). The long-term impacts of Medicaid exposure in early childhood: Evidence from the program’s origin. Journal of Health Economics, 45, 161–175. doi: 10.1016/j.jhealeco.2015.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, C. (1996). Notes on the “SEO” or “Census” component of the PSID (Technical Series Paper #96-03). Panel Study of Income Dynamics. https://psidonline.isr.umich.edu/publications/Papers/tsp/1996-03_Notes_on_the_SEO_C_Brown.pdf
- Brucker, D. L., Mitra, S., Chaitoo, N., & Mauro, J. (2015). More likely to be poor whatever the measure: Working-age persons with disabilities in the United States. Social Science Quarterly, 96(1), 273–296. doi: 10.1111/ssqu.12098 [DOI] [Google Scholar]
- Bureau of Labor Statistics. (2020). Employer-reported workplace injuries and illnesses—2019 (USDL-20-2030).Bureau of Labor Statistics. https://www.bls.gov/news.release/pdf/osh.pdf [Google Scholar]
- Caputo, J., Pavalko, E. K., & Hardy, M. A. (2020). Midlife work and women’s long-term health and mortality. Demography, 57(1), 373–402. doi: 10.1007/s13524-019-00839-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case, A., & Deaton, A. (2020). Deaths of despair and the future of Capitalism. Princeton University Press. [Google Scholar]
- Case, A., Lubotsky, D., & Paxson, C. (2002). Economic status and health in childhood: The origins of the gradient. The American Economic Review, 92(5), 1308–1334. doi: 10.1257/000282802762024520 [DOI] [PubMed] [Google Scholar]
- Charles, K. K. (2003). The longitudinal structure of earnings losses among work-limited disabled workers. Journal of Human Resources, 38(3), 618–646. doi: 10.3368/jhr.XXXVIII.3.618 [DOI] [Google Scholar]
- Chatterji, P., & Li, Y. (2017). Early coverage expansions under the Affordable Care Act and Supplemental Security Income participation. The Journal of the Economics of Ageing, 10, 75–83. doi: 10.1016/j.jeoa.2017.10.001 [DOI] [Google Scholar]
- Chetty, R., Stepner, M., Abraham, S., Lin, S., Scuderi, B., Turner, N., Bergeron, A., & Cutler, D. (2016). The association between income and life expectancy in the United States, 2001-2014. JAMA, 315(16), 1750–1766. doi: 10.1001/jama.2016.4226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke, P., & Latham, K. (2014). Life course health and socioeconomic profiles of Americans aging with disability. Disability and Health Journal, 7(1 Suppl), S15–S23. doi: 10.1016/j.dhjo.2013.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conti, G., & Heckman, J. J. (2010). Understanding the early origins of the education–health gradient: A framework that can also be applied to analyze gene–environment interactions. Perspectives on Psychological Science, 5(5), 585–605. doi:10.1177%2F1745691610383502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depp, C. A., & Jeste, D. V. (2006). Definitions and predictors of successful aging: A comprehensive review of larger quantitative studies. The American Journal of Geriatric Psychiatry, 14(1), 6–20. doi: 10.1097/01.JGP.0000192501.03069.bc [DOI] [PubMed] [Google Scholar]
- Dupre, M. E., Beck, A. N., & Meadows, S. O. (2009). Marital trajectories and mortality among US adults. American Journal of Epidemiology, 170(5), 546–555. doi: 10.1093/aje/kwp194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman-Hoffman, V. L., Ault, K. L., Anderson, W. L., Weiner, J. M., Stevens, A., Campbell, V. A., & Armour, B. S. (2015). Disability status, mortality, and leading causes of death in the United States community population. Medical Care, 53(4), 346–354. doi: 10.1097/MLR.0000000000000321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelber, A., Moore, T., & Strand, A. (2018). Disability Insurance income saves lives. Stanford Institute for Economic Policy Research (SIEPR), Working Paper No. 18-005.https://siepr.stanford.edu/sites/default/files/publications/18-005.pdf
- Huohvanainen, E., Strandberg, A. Y., Stenholm, S., Pitkälä, K. H., Tilvis, R. S., & Strandberg, T. E. (2016). Association of self-rated health in midlife with mortality and old age frailty: A 26-year follow-up of initially healthy men. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 71(7), 923–928. doi: 10.1093/gerona/glv311 [DOI] [PubMed] [Google Scholar]
- Idler, E. L., & Angel, R. J. (1990). Self-rated health and mortality in the NHANES-I epidemiologic follow-up study. American Journal of Public Health, 80(4), 446–452. doi: 10.2105/ajph.80.4.446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahoda, M. (1981). Work, employment, and unemployment: Values, theories, and approaches in social research. American Psychologist, 36(2), 184. doi: 10.1037/0003-066X.36.2.184 [DOI] [Google Scholar]
- Jann, B. (2014). Plotting regression coefficients and other estimates. Stata Journal, 14(4), 708–737. doi:10.1177%2F1536867X1401400402 [Google Scholar]
- Jolly, N. A. (2013). The impact of work-limiting disabilities on earnings and income mobility. Applied Economics, 45(36), 5104–5118. doi: 10.1080/00036846.2013.818212 [DOI] [Google Scholar]
- Kapteyn, A., Smith, J. P., & Van Soest, A. (2007). Vignettes and self-reports of work disability in the United States and the Netherlands. American Economic Review, 97(1), 461–473. doi: 10.1257/aer.97.1.461 [DOI] [Google Scholar]
- Kapteyn, A., Smith, J. P., & van Soest, A. (2008). Dynamics of work disability and pain. Journal of Health Economics, 27(2), 496–509. doi: 10.1016/j.jhealeco.2007.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karraker, A., Schoeni, R. F., & Cornman, J. C. (2015). Psychological and cognitive determinants of mortality: Evidence from a nationally representative sample followed over thirty-five years. Social Science & Medicine (1982), 144, 69–78. doi: 10.1016/j.socscimed.2015.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreider, B. (1999). Latent work disability and reporting bias. Journal of Human Resources, 734–769. doi: 10.2307/146415 [DOI] [Google Scholar]
- Laditka, J. N., & Laditka, S. B. (2018a). Work disability in the United States, 1968–2015: Prevalence, duration, recovery, and trends. SSM—Population Health, 4, 126–134. doi: 10.1016/j.ssmph.2017.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laditka, J. N., & Laditka, S. B. (2018b). Adverse childhood circumstances and functional status throughout adult life. Journal of Aging and Health, 30(9), 1347–1368. doi: 10.1177/0898264317715976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S., Hagan, K., Grodstein, F., & VanderWeele, T. J. (2018). Social integration and healthy aging among U.S. women. Preventive Medicine Reports, 9, 144–148. doi: 10.1016/j.pmedr.2018.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lykens, K. A., & Jargowsky, P. A. (2002). Medicaid matters: Children’s health and Medicaid eligibility expansions. Journal of Policy Analysis and Management, 21(2), 219–238. doi: 10.1002/pam.10024 [DOI] [PubMed] [Google Scholar]
- Maestas, N., & Mullen, K. J. (2019). Unmet need for workplace accommodation. Journal of Policy Analysis and Management, 38(4), 1004–1027. doi: 10.1002/pam.22148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maestas, N., Mullen, K. J., & Strand, A. (2013). Does Disability Insurance receipt discourage work? Using examiner assignment to estimate causal effects of SSDI receipt. American Economic Review, 103(5), 1797–1829. doi: 10.1257/aer.103.5.1797 [DOI] [Google Scholar]
- Maestas, N., Mullen, K. J., & Strand, A. (2021). The effect of economic conditions on the disability insurance program: Evidence from the great recession. Journal of Public Economics, 199, 104410. doi: 10.1016/j.jpubeco.2021.104410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin, S. J. (2017). Healthy aging in the context of educational disadvantage: The role of “ordinary magic”. Journal of Aging and Health, 29(7), 1214–1234. doi: 10.1177/0898264316659994 [DOI] [PubMed] [Google Scholar]
- McLaughlin, S. J., Jette, A. M., & Connell, C. M. (2012). An examination of healthy aging across a conceptual continuum: Prevalence estimates, demographic patterns, and validity. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 67(7), 783–789. doi: 10.1093/gerona/glr234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meara, E. R., Richards, S., & Cutler, D. M. (2008). The gap gets bigger: Changes in mortality and life expectancy, by education, 1981–2000. Health Affairs, 27(2), 350–360. doi: 10.1377/hlthaff.27.2.350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, B. D., & Mok, W. K. C. (2019). Disability, earnings, income and consumption. Journal of Public Economics, 171, 51–69. doi: 10.1016/j.jpubeco.2018.06.011 [DOI] [Google Scholar]
- Miller, S., & Wherry, L. R. (2019). The long-term effects of early life Medicaid coverage. Journal of Human Resources, 54(3), 785–824. doi: 10.3368/jhr.54.3.0816.8173R1 [DOI] [Google Scholar]
- Mitra, S., Findley, P. A., & Sambamoorthi, U. (2009). Health care expenditures of living with a disability: Total expenditures, out-of-pocket expenses, and burden, 1996 to 2004. Archives of Physical Medicine and Rehabilitation, 90(9), 1532–1540. doi: 10.1016/j.apmr.2009.02.020 [DOI] [PubMed] [Google Scholar]
- Montez, J. K., Hummer, R. A., Hayward, M. D., Woo, H., & Rogers, R. G. (2011). Trends in the educational gradient of U.S. adult mortality from 1986 to 2006 by race, gender, and age group. Research on Aging, 33(2), 145–171. doi: 10.1177/0164027510392388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez, J. K., Zajacova, A., Hayward, M. D., Woolf, S. H., Chapman, D., & Beckfield, J. (2019). Educational disparities in adult mortality across U.S. states: How do they differ, and have they changed since the mid-1980s? Demography, 56(2), 1–24. doi: 10.1007/s13524-018-0750-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- PSID. (2018). Panel Study of Income Dynamics, restricted use dataset.https://psidonline.isr.umich.edu/
- Rowe, J. W., & Kahn, R. L. (1987). Human aging: Usual and successful. Science (New York, N.Y.), 237(4811), 143–149. doi: 10.1126/science.3299702 [DOI] [PubMed] [Google Scholar]
- Rupp, K., & Dushi, I. (2017). Accounting for the process of disablement and longitudinal outcomes among the near elderly and elderly. Research on Aging, 39(1), 190–221. doi: 10.1177/0164027516656141 [DOI] [PubMed] [Google Scholar]
- Scott-Marshall, H. K., Tompa, E., Wang, Y., & Liao, Q. (2014). Long-term mortality risk in individuals with permanent work-related impairment. Canadian Journal of Public Health = Revue canadienne de sante publique, 105(5), e330–e335. doi: 10.17269/cjph.105.4535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- She, P., & Livermore, G. A. (2007). Material hardship, poverty, and disability among working-age adults. Social Science Quarterly, 88(4), 970–989. doi: 10.1111/j.1540-6237.2007.00513.x [DOI] [Google Scholar]
- Singh, G. K., & Siahpush, M. (2014). Widening rural–urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health, 91(2), 272–292. doi: 10.1007/s11524-013-9847-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Security Administration. (2019). Annual statistical report on the Social Security Disability Insurance program, 2018 (No. 13-11826).Social Security Administration. https://www.ssa.gov/policy/docs/statcomps/di_asr/index.html [Google Scholar]
- Södergren, M. (2013). Lifestyle predictors of healthy ageing in men. Maturitas, 75(2), 113–117. doi: 10.1016/j.maturitas.2013.02.011 [DOI] [PubMed] [Google Scholar]
- Sturm, R., Ringel, J. S., & Andreyeva, T. (2004). Increasing obesity rates and disability trends. Health Affairs (Project Hope), 23(2), 199–205. doi: 10.1377/hlthaff.23.2.199 [DOI] [PubMed] [Google Scholar]
- Tapia Granados, J. A., House, J. S., Ionides, E. L., Burgard, S., & Schoeni, R. S. (2014). Individual joblessness, contextual unemployment, and mortality risk. American Journal of Epidemiology, 180(3), 280–287. doi: 10.1093/aje/kwu128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker, J. S., Friedman, H. S., Wingard, D. L., & Schwartz, J. E. (1996). Marital history at midlife as a predictor of longevity: Alternative explanations to the protective effect of marriage. Health Psychology, 15(2), 94–101. doi: 10.1037//0278-6133.15.2.94 [DOI] [PubMed] [Google Scholar]
- Van Soest, A., Andreyeva, T., Kapteyn, A., & Smith, J. P. (2011). Self-reported disability and reference groups. In Investigations in the economics of aging (pp. 237–264). University of Chicago Press. doi: 10.7208/9780226903163-009 [DOI] [Google Scholar]
- Vanajan, A., Bültmann, U., & Henkens, K. (2020). Health-related work limitations among older workers—the role of flexible work arrangements and organizational climate. The Gerontologist, 60(3), 450–459. doi: 10.1093/geront/gnz073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge, L. M., Latham, K., & Clarke, P. J. (2017). Aging with disability for midlife and older adults. Research on Aging, 39(6), 741–777. doi: 10.1177/0164027516681051 [DOI] [PubMed] [Google Scholar]
- von Bonsdorff, M. B., Seitsamo, J., Ilmarinen, J., Nygård, C. H., von Bonsdorff, M. E., & Rantanen, T. (2011). Work ability in midlife as a predictor of mortality and disability in later life: A 28-year prospective follow-up study. CMAJ, 183(4), E235–E242. doi: 10.1503/cmaj.100713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada, R. (2005). OUTREG2: Stata module to arrange regression outputs into an illustrative table. Statistical Software Components S456416, Boston College Department of Economics, Revised 17 Aug 2014. https://sociorepec.org/publication.xml?h=repec:boc:bocode:s456416&l=en
- Woo, H., & Zajacova, A. (2017). Predictive strength of self-rated health for mortality risk among older adults in the United States: Does it differ by race and ethnicity? Research on Aging, 39(7), 879–905. doi: 10.1177/0164027516637410 [DOI] [PubMed] [Google Scholar]
- Zablotsky, B., Black, L. I., Maenner, M. J., Schieve, L. A., Danielson, M. L., Bitsko, R. H., Blumberg, S. J., Kogan, M. D., & Boyle, C. A. (2019). Prevalence and trends of developmental disabilities among children in the United States: 2009–2017. Pediatrics, 144(4). doi: 10.1542/peds.2019-0811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zechmann, A., & Paul, K. I. (2019). Why do individuals suffer during unemployment? Analyzing the role of deprived psychological needs in a six-wave longitudinal study. Journal of Occupational Health Psychology, 24(6), 641–661. doi: 10.1037/ocp0000154 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.