Abstract
Purpose
Psychometric validity/reliability of 10-item and 2-item abbreviations of the Connor–Davidson Resilience Scale (CD-RISC-10; CD-RISC-2) was investigated via item response theory and classic approaches.
Methods
We sampled 5023 adult American participants in a June/July 2020 survey on the COVID-19 pandemic’s psychological effects. Our questionnaire incorporated the CD-RISC-10 with other validated measures. CD-RISC-10 items were ranked on item-to-scale correlations, loadings on a one-factor confirmatory factor analysis model, and item slope/threshold parameters plus information curves from a unidimensional graded response model. Concurrent validity of the highest ranked item pair was evaluated vis-à-vis the CD-RISC-10 and CD-RISC−2. Internal consistency, based on average variance extracted (AVE) and multiple reliability coefficients, was also compared. Convergent/divergent validity was tested by correlating anxiety, depression, fear of COVID-19, anxiety sensitivity, coping, and personality measures with both scales and the highest ranked item pair. Binary agreement/classification indexes assessed inter-rater reliability.
Results
Items 2 and 9 from CD-RISC-10 ranked the highest. Reliability coefficients were > 0.93, > 0.72, and > 0.82 for the CD-RISC-10, CD-RISC-2, vs summation of items 2 and 9. AVEs were 0.66, 0.67, and 0.77. CD-RISC abbreviations and the summation of items 2 and 9 correlated negatively with anxiety (> − 0.43), depression (> − 0.42), and fear of COVID-19 (> − 0.34); positively with emotional stability (> 0.53) and conscientiousness (> 0.40). Compared to the CD-RISC-2, summative scores of items 2 and 9 more efficiently classified/discriminated high resilience on the CD-RISC-10.
Conclusion
We confirmed construct validity/reliability of copyrighted CD-RISC abbreviations. The CD-RISC-10’s items 2 and 9 were psychometrically more salient than the CD-RISC−2.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11136-022-03125-y.
Keywords: COVID-19 pandemic, CD-RISC-10, CD-RISC-2, Resilience, Item response theory, Graded response model
Plain English summary
Two abbreviated Connor-Davidson Resilience Scales (CD-RISC-10; CD-RISC-2) have been validated for measuring resilience, namely the ability to adapt to, bounce back from, and even thrive after adversity. Experts disagree on which of many published resilience measures is the best one. Most studies show that the CD-RISC-10 captures resilience as a single, overall ability. Some recent studies, applying newer methods, find the CD-RISC-10 to represent more than one facet of resilience. Thus, further research, using modern approaches, is needed. We re-evaluated CD-RISC-10 and CD-RISC-2 scales via item response theory. We studied the extent to which the CD-RISC-10 captures “overall” resilience versus multiple domains, and whether the CD-RISC-2 contains the strongest pair out of all CD-RISC-10 items. Our intention was to contribute towards improved resilience measures. We sampled 5023 adult Americans facing the COVID-19 pandemic. Our findings confirmed that the CD-RISC-10 accurately measures “overall” resilience. Study participants rated another item pair (CD-RISC-10 items 2 and 9) as superior to the CD-RISC-2 in capturing resilience towards the surging pandemic. The scales inefficiently captured high resilience. This calls for new measures that more efficiently capture high-end resilience plus the varying flavors of resilience utilized in adapting to different adversities.
Introduction
There is growing interest in resilience, broadly defined an individual’s capacity to adapt, bounce back and potentially even thrive after experiencing adversity [1–4]. Research frequently shows that resilience directly or indirectly influences individual and social well-being indicators [5, 6], hence the increased focus on this construct. Resilience is a vital component in the optimal functioning of healthcare professionals [7, 8], corporate leaders [9], military personnel [10], first responders [11], educationists [12], and the general community at large [13]. This is especially the case following stressful events such as the global 2019 coronavirus disease (COVID-19) pandemic caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) [14–17].
Metrics of resilience in the literature include the Connor–Davidson Resilience Scale (CD-RISC), Resilience Scale for Adults, Brief Resilience Scale, and Five-by-Five Resilience Scale [18–21]. There is no “gold standard” measure of individual resilience [19]. Lack of consensus on the most suitable resilience measure limits deeper research into factors influencing depletion, gain/regain, conservation, and/or growth/cultivation of resilience. Of the existing measures, the CD-RISC ranks among the most validated [18–20]. It was developed as a multi-factorial scale comprising five dimensions: (i) personal competence, high standards and tenacity; (ii) trust in one’s intuition, tolerance of negative affect and strengthening effects of stress; (iii) positive acceptance of change and secure relationships; (iv) control; and (v) spirituality [22]. Subsequent studies failed to replicate this five-factor structure [23–27], and its conceptual validity was weakened by items representing qualities that foster resilience but are not part of the core construct [28]. The 25-item scale (CD-RISC-25) was also initially validated [22] via outmoded methods (e.g., Kaiser-Guttman factor retention criterion, orthogonal rotation) [29]. The 10-item abbreviation (CD-RISC-10), developed by deleting items with tenuous conceptual validity and weak item-to-scale correlations [23], is mostly shown as uni- rather than multi-factorial [23, 25, 30–34]. However, some studies find a two-factor model superior to the single-factor model [35–37], suggesting further investigation of the scale is warranted. Moreover, validations of the CD-RISC-10 rarely exploit advantages of item response theory (IRT) [38–41] over classical test theory (CTT).1 Two Rasch analyses of the CD-RISC-25 yielded 21- and 22- item revisions with good data fit but with ceiling effects that indicated poor capture of high resilience [42, 43]. Ehrich et al. (2017)’s Rasch partial credit model study of the CD-RISC-10 among Australian university students (N = 288), found evidence of multiple factors and misfitting items not detected by CTT, leading authors to propose a shorter, 8-item abbreviation [44]. In contrast, Rasch analyses by Pulido-Martos et al. (2020) on a sample of Spanish citizens (N = 1011) confirmed CD-RISC-10’s unifactorial structure [45]. Nevertheless, Heritage et al. (2021)’s Rasch rating scale model study among Canadian/Australian nursing students (N = 708) did not support a unifactorial model, leading authors to propose a 7-item abbreviation [46]. Despite extant literature suggesting the graded response model (GRM) [47, 48] is a superior approach for Likert scales [49, 50], most IRT analyses of the CD-RISC-10 apply Rasch models. Heritage et al. (2021) advocated for using the GRM in future studies [46]. Lim et al. (2019)’s GRM study among older adults awaiting knee replacement surgery for osteoarthritis (N = 700) supported the CD-RISC-10’s unifactorial structure but their report provided scanty details [51].
The present study primarily aimed to investigate the validity/reliability of unidimensional 10- [23], and 2-item abbreviations [52] of the Connor–Davidson Resilience scale (CD-RISC-10, and CD-RISC-2) [32, 33] using a GRM-based analysis to augment CTT findings. Secondly, we examined whether the copyrighted CD-RISC 2 comprises the most valid and reliable pair out of the ten CD-RISC-10 items. Thirdly, if any pair of items ranked higher than the CD-RISC-2’s contents, we aimed to test their concurrent validity and inter-rater reliability versus the traditional two-item scale. The purpose of this item validity, reliability, and calibration study of CD-RISC abbreviations was to contribute evidence towards eventual consensus regarding quantitative measurement of resilience. We intentionally did not focus on modifying the copyrighted scales. We hypothesized that the study would confirm the CD-RISC-10’s unifactorial model and prove the CD-RISC-2’s contents as the item duo with the strongest concurrent validity and inter-rater reliability. We further hypothesized that the CD-RISC-10 and CD-RISC-2 would exhibit robust convergent and divergent validity plus measurement invariance.
Methods
Study design
This was an in-depth psychometric validation and recalibration study nested within a prospective, observational study of a nationwide cohort of Americans responding to the COVID-19 pandemic. The parent project was approved by the Institutional Review Board (IRB) at Baylor Scott and White Research Institute (protocol # 020-035). The IRB determined that, owing to the anonymous/de-identified nature of the survey, the study presented only minimal risk to participants and qualified for a waiver of the written informed consent requirement. Prospective participants first read a cover letter describing the study, the privacy/confidentiality of survey responses, and the free option not to respond if one did not consent to participating in the study. Informed consent was indicated by opting to answer the survey and to submit one’s responses.
Participants and recruitment procedure
Participants were English-speaking adult Americans (aged ≥ 18 years) who responded to an online survey-questionnaire distributed via the Qualtrics™ platform (Qualtrics, Inc.; Seattle, WA) across all states of the country from June 22 to July 5, 2020 [53]. The questionnaire assessed participants’ psychological responses to the first surge of the COVID-19 pandemic. A total of 5023 participants were sampled. The Qualtrics platform eliminated invalid/incoherent responses. Questionnaires with incomplete responses (≈ 2.03%) were excluded from analysis.
Study measures
Reference scale The CD-RISC-10 was our referent based on its superior validity/reliability among published CD-RISC versions [31, 45, 54]. It includes items 1, 4, 6, 7, 8, 11, 14, 16, 17, and 19 from the CD-RISC-25 [23]. Most studies find the CD-RISC-10 to have a unifactorial model [23, 25, 30–34] different from the 5-factor structure in the initial CD-RISC-25 validation [22]. Respondents rate, on a 5-point Likert spectrum from 0 (“not true at all”) to 4 (“true nearly all the time”), how frequently they achieve each of ten abilities (e.g., “able to adapt when changes occur”). Summating all items yields scale scores, with higher totals (minimum = 0, maximum = 40) implying greater resilience. We evaluated continuous CD-RISC-10 scores and binary dummy variables of “high” resilience. The “high resilience” threshold was one standard deviation above the sample’s mean CD-RISC-10 score rounded to the nearest whole number (i.e., scores ≥ 36).
Index scale The CD-RISC-2 [52] was our index scale. It incorporates two items (“able to adapt when changes occur” and “tend to bounce back after… hardships”) [52], which are items 1 and 5 of the CD-RISC-10 [23]. Their inclusion in CD-RISC-2 was based on a subjective judgment that they best represent “adaptability” and “bouncing back”, the two concepts deemed most essential to defining resilience [52]. For the purposes of this study, we ranked CD-RISC-10 items on (a) item-to-scale correlations, (b) item difficulty indices, and (c) item information functions from a unidimensional GRM [47, 48]. Concurrent validity and inter-rater reliability of a summated score of the two highest ranking items was tested against the CD-RISC-10 and CD-RISC−2.
Convergent and divergent validity Polychoric correlations of abbreviated CD-RISC scales with subscales of the Brief COPE Inventory [55], and the Ten-Item Personality Inventory (TIPI)’s five subscales [56] were used to test convergent validity. Correlations of abbreviated CD-RISC scales with the seven-item Generalized Anxiety Disorder (GAD-7) scale [57], eight-item patient health questionnaire (PHQ-8) scale [58], seven-item Fear of COVID-19 (FCV-19) scale [59], and the Anxiety Sensitivity Index-3 (ASI-3) subscales [60], were used to demonstrate discriminant validity. Previous studies found resilience to be positively correlated with adaptive coping styles [61] and conscientious/extraverted personality [61] but negatively correlated with anxiety [31–33], depression [31–33, 62], anxiety sensitivity [63], and COVID-19 fear [64, 65].
Internal consistency reliability was assessed using ordinal coefficients alpha (α) and theta (θ) [66, 67], Cronbach’s coefficient alpha (α) [68], McDonald’s omega (ω) coefficient [69, 70], the Spearman-Brown formula [71, 72], and average variance extracted (AVE) [73]. AVEs ≥ 0.50 indicated adequate convergence between items. Reliability coefficients ≥|0.70| indicated high internal consistency [74].
Sample characteristics and other contextual variables The questionnaire included these demographics: gender, age, race/ethnicity, marital status, education level, occupation/profession, income, and years of experience in occupation/profession. Geographic variables were: residential zip code, metropolitan status of neighborhood, state of residence, and census region. Clinical information included prior medical/mental health history, comorbidities, and personal/family experience(s) of the COVID-19 pandemic (e.g., whether a participant had tested positive for the SARS-Cov-2 virus, knew someone with COVID-19, or had cared for patients with COVID-19).
Statistical analysis strategy
The study dataset was randomly and equitably split 50:50 into derivation and validation subsamples (N = 2512 and 2511, respectively) to enable a split-sample internal validation strategy [75]. Demographics, geographic locales, personality traits, physical/mental health histories, and COVID-19 experiences were compared between derivation and validation subsamples. Lack of significant differences (p > 0.05) in inter-subsample distributions of these variables was taken to confirm successful random partitioning. Bartlett’s test of sphericity [76] and the Kaiser–Meyer–Olkin (KMO) test [77] assessed adequacy of the data as a source of factor-analytic correlation matrices.
We tested the assumption that the CD-RISC-10 measures only one dominant latent ability (i.e., unidimensionality) via inter-item correlations, parallel analysis [78], Velicer’s minimum average partial (MAP) test [79], and confirmatory factor analysis (CFA)[74, 80]. The comparative fit index (CFI), Tucker-Lewis index (TLI) [81], and standardized root mean square of approximation (SRMR) [82] assessed CFA models’ global fit to the data. Per Shi et al. (2020) [83], the SRMR was preferred over the root mean square error of approximation (RMSEA). Meeting a combined cutoff threshold of CFI ≥ 0.95, TLI ≥ 0.95, SRMR ≤ 0.08 [80], and standardized factor loadings >|0.400| [74] suggested that a scale’s constituent items were “good” indicators of the latent trait. CFAs were based on polychoric correlations [84]. Robust maximum likelihood (MLR), means- and variance-adjusted weighted least square (WLSMV), and means- and variance-adjusted unweighted least squares (ULSMV) estimators were compared [85] to find the method yielding the best data fit. CD-RISC-10 items were ranked on CFA factor loadings, item-to-scale correlations, and item reliabilities.
A GRM was fitted to the CD-RISC-10 to derive item discriminant/difficulty indices plus Eigenvalues and to plot response option characteristic curves (OCCs) plus information function curves for scales/items. The GRM was the preferred IRT model due to the polytomous, ordered categorical nature of the scale/items. For each scale item, 1 slope (discrimination, α) and 4 threshold (b) parameters were estimated. Steeper α parameters indicate which items more efficiently discriminate between respondents’ resilience levels. α values from 0.65–1.34 indicate “moderate”, 1.35–1.75 “high”, and > 1.76 “very high” discrimination [86]. Item b parameters assessed the point on the resilience continuum at which a respondent was most likely to select each response option. Higher b values indicate more “difficult” options. Item response OCCs and item information function (IIF) plots visually illustrate how much psychometric information each item/scale captures. The generalized S-∑2 index assessed item goodness-of-fit in the GRM [87]. Significance for the S-∑2 index was set at p < 0.0001 as scales were short [88]. Standardized local-dependence (LD) ∑2 statistics for item pairs test the assumption that each item contributes uniquely to the latent trait (resilience) measured (i.e., local item independence) [89]. LD statistics <|5| are small/inconsequential, |5| to |10| moderate/questionable, and >|10| large (i.e., indicating excessive residual covariance between ≥ 2 items not captured by the GRM). The assumption that probability of selecting higher response options rises with greater resilience (i.e., monotonicity) was tested via Mokken’s H scalability coefficient [90] for each item/scale. Item scalability (Hi) coefficients ≥ 0.3 and scale-level scalability (Ht) coefficients ≥ 0.5 confirm monotonicity [91].
Mixed-effects logistic regressions of high resilience per the CD-RISC-10 scale (scores ≥ 36) on continuous 2-item scale scores were fitted to yield receiver operating characteristic (ROC) curves. ROC plots visually depicted the optimal cut-off thresholds on index scales that provide the best sensitivity in discriminating high CD-RISC-10 scores while maintaining high specificity. We employed these thresholds to delineate “high” resilience on index scales. Inter-rater reliability was assessed via percent agreement, kappa coefficients, Gwet’s AC1 coefficient, Krippendorf’s alpha, Brennann-Prediger coefficient [92], accuracy, sensitivity, specificity, positive predictive value, negative predictive value, plus areas under the ROC and precision-recall curves (PRCs) [93]. Measurement invariance of the CD-RISC-10 scale across subgroups of the sample was assessed via global fit indices of multi-group CFAs [94]. Statistical analyses were conducted using SAS® version 9.4 (SAS Inc, Cary, NC), R® version 3.6.0 (R Development Core Team, Vienna, Austria), and Mplus® version 8.6 (Muthén & Muthén, Los Angeles, CA).
Results
Participants sampled
A total of 5023 out of 6461 initial respondents (77.74%) provided complete responses for the baseline survey [53]. As shown in Table 1, there were no significant differences in the distribution of sociodemographic, geographic, personality, and clinical attributes or COVID-related experiences between the overall sample and the two analysis sub-samples. Participants were predominantly (59%) female, white (74%), married or partnered (56%), educated up to college or beyond (59%), urbanized (89%), members of the general public (62%) (i.e., neither healthcare practitioners nor essential workers), and earning $60,000 or more annually (57%). The median (± interquartile range) age was 52 (38, 61) years. Just over 1% of respondents had personally tested positive for SARS-Cov− 2. Almost one of eight (12% of) participants had cared for patients with COVID-19, and 40% knew someone who had been infected with the disease.
Table 1.
Characteristics of the Study Sample
| Respondent attribute | verall Study Sample (N = 5023) |
Derivation Subsample (n = 2512) |
Validation Subsample (n = 2511) |
Significance (p) |
|---|---|---|---|---|
| Gender, n (%) | ||||
| Female | 2,960 (58.9) | 1,482 (59.0) | 1,478 (58.9) | 0.9730a |
| Male | 2,042 (40.7) | 1,020 (40.6) | 1,022 (40.7) | |
| Undisclosed | 21 (0.4) | 10 (0.4) | 11 (0.4) | |
| Age in years | ||||
| median (Q1, Q3) | 52 (38, 61) | 52 (38, 61) | 51 (38, 62) | 0.5057b |
| Marital status, n (%) | ||||
| Married/partnered | 2806 (55.86) | 1433 (57.05) | 1373 (54.68) | 0.5387a |
| Single | 1547 (30.80) | 745 (29.66) | 802 (31.94) | |
| Divorced/separated | 630 (12.54) | 318 (12.66) | 312 (12.43) | |
| Undisclosed | 40 (0.80) | 16 (0.64) | 24 (0.96) | |
| Race/ethnicity, n (%) | ||||
| White/Non-Hispanic | 3,724 (74.14) | 1,882 (74.92) | 1842 (73.36) | 0.4782a |
| Black | 392 (7.80) | 184 (7.32) | 208 (8.28) | |
| Hispanic | 376 (7.49) | 180 (7.17) | 196 (7.81) | |
| Asian | 359 (7.15) | 185 (7.36) | 174 (6.93) | |
| Other | 172 (3.42) | 81 (3.22) | 91 (3.62) | |
| Education level, n (%) | ||||
| ≤ 8th Grade | 6 (0.12) | 2 (0.08) | 4 (0.16) | 0.9147a |
| 9th – 11th Grade | 34 (0.68) | 16 (0.64) | 18 (0.72) | |
| High school/GED® | 615 (12.24) | 318 (12.66) | 297 (11.83) | |
| Vocational/technical | 249 (4.96) | 113 (4.50) | 136 (5.42) | |
| Associate degree | 1152 (22.93) | 561 (22.33) | 591 (23.54) | |
| Bachelor’s degree | 1648 (32.81) | 849 (33.80) | 799 (31.82) | |
| Advanced degree | 1299 (25.86) | 644 (25.64) | 655 (26.09) | |
| Other | 14 (0.28) | 8 (0.32) | 6 (0.24) | |
| Undisclosed | 6 (0.12) | 1 (0.04) | 5 (0.20) | |
| Income level, n (%) | ||||
| < 30,000 $ | 792 (15.77) | 406 (16.16) | 386 (15.37) | 0.1194a |
| 30,000 to < 60,000 $ | 1,166 (23.21) | 554 (22.05) | 612 (24.37) | |
| 60,000 to < 100,000 $ | 1,259 (25.06) | 657 (26.15) | 602 (23.97) | |
| ≥ 100,000 $ | 1,580 (31.46) | 785 (31.25) | 795 (31.66) | |
| Undisclosed | 226 (4.50) | 110 (4.38) | 116 (4.62) | |
| Occupation type, n (%) | ||||
| Healthcare practitioner | 1,419 (28.25) | 699 (27.83) | 720 (28.67) | 0.3670a |
| Essential worker | 501 (9.97) | 265 (10.55) | 236 (9.40) | |
| General public | 3,103 (61.78) | 1,548 (61.62) | 1,555 (61.93) | |
| RUCA category, n (%) | ||||
| Large metropolitan area | 4457 (88.89) | 2221 (88.59) | 2236 (89.19) | 0.8178a |
| Suburban area | 337 (6.72) | 167 (6.66) | 170 (6.78) | |
| Small town/rural area | 220 (4.39) | 119 (4.75 | 101 (4.03) | |
| Census region, n (%) | ||||
| South | 1,787 (35.58) | 875 (34.83) | 912 (36.32) | 0.9219a |
| North East | 1,143 (22.76) | 576 (22.93) | 567 (22.58) | |
| West | 1,070 (21.30) | 556 (22.13) | 514 (20.47) | |
| Midwest | 993 (19.77) | 489 (19.47) | 504 (20.07) | |
| Puerto Rico & Islands | 21 (0.42) | 11 (0.44) | 10 (0.40) | |
| Undisclosed | 9 (0.18) | 5 (0.20) | 4 (0.16) | |
| TIPI, median (Q1, Q3) | ||||
| Agreeableness | 5.5 (4.5, 6.5) | 5.5 (4.5, 6.5) | 5.5 (4.5, 6.5) | 0.2529b |
| Conscientiousness | 6 (5, 7) | 6 (5, 7) | 6 (5, 7) | 0.4069b |
| Extraversion | 4 (2.5, 5) | 4 (2.5, 5) | 4 (2.5, 5) | 0.4087b |
| Neuroticism | 5 (4, 6.5) | 5 (4, 6.5) | 5 (4, 6.5) | 0.4917b |
| Openness | 4.5 (4, 5.5) | 4.5 (4, 5.5) | 4.5 (4, 5.5) | 0.5851b |
| H/o mental illness, n (%) | ||||
| Depression | 502 (9.99) | 236 (9.39) | 266 (10.59) | 0.9646a |
| Bipolar Disorder/Mania | 113 (2.25) | 61 (2.43) | 52 (2.07) | 0.9857a |
| Generalized anxiety | 428 (8.52) | 198 (7.88) | 230 (9.16) | 0.9531a |
| PTSD | 158 (3.15) | 77 (3.07) | 81 (3.23) | 0.9980a |
| OCD | 72 (1.43) | 31 (1.23) | 41 (1.63) | 0.9724a |
| Psychotic Disorder | 29 (0.58) | 20 (0.80) | 9 (0.36) | 0.9199a |
| Any phobia | 59 (1.17) | 22 (0.88) | 37 (1.47) | 0.9285a |
| Other | 72 (1.45) | 19 (0.76) | 31 (1.23) | 0.8973a |
| H/o medical illness, n (%) | ||||
| Asthma/emphysema/COPD | 308 (6.13) | 148 (5.89) | 160 (6.37) | 0.9906a |
| Diabetes Mellitus | 315 (6.27) | 149 (5.93) | 166 (6.61) | 0.9817a |
| CVD/hypertension/CHF | 685 (13.64) | 334 (13.30) | 351 (13.98) | 0.9916a |
| Chronic kidney disease | 36 (0.70) | 18 (0.72) | 18 (0.72) | 0.9998a |
| Liver disease | 35 (0.70) | 16 (0.64) | 19 (0.76) | 0.9949a |
| Cancer(s) | 127 (2.53) | 64 (2.55) | 63 (2.51) | 0.9998a |
| Exposure to COVID, n (%) | ||||
| Tested Positive for COVID | 67 (1.33) | 37 (1.47) | 30 (1.19) | 0.6156a |
| Cared for COVID Patients | 619 (12.32) | 305 (12.14) | 314 (12.50) | 0.6587a |
| Knew Person with COVID | 2,009 (40.00) | 1,023 (40.72) | 986 (39.27) | 0.0867a |
CHF chronic heart failure, COPD chronic obstructive pulmonary disorder, COVID 2019 Coronavirus Infectious Disease, CVD cardiovascular disease, GED® general educational development tests, H/o history of;,OCD obsessive compulsive disorder, PTSD posttraumatic stress disorder, Q1 first quartile; Q3 third quartile,RUCA rural–urban commuting areas, TIPI Ten-Item Personality Inventory
Key: adenotes a p-value for Chi-square test; bdenotes a p-value for Kruskal–Wallis or Wilcoxon test
Sample adequacy and number of extractable resilience factors
Bartlett’s test of sphericity on CD-RISC-10 items within the derivation subsample was significant (Chi-square = 15.785; p < 0.0001), indicating support for a single underlying latent factor. The KMO value for the CD-RISC-10 scale was 0.950, and values for all items (from 0.925 for item 2 to 0.963 for item 8) exceeded the 0.800 threshold of sampling adequacy for factor analysis. In Velicer’s MAP test on derivation data, the Eigenvalue of a first component (14.712) accounted for almost 100% of total variance. Parallel analysis also supported the CD-RISC-10 items being summarized with a single domain (i.e., unidimensionality).
Item score distribution and item-level reliability
Table 2 illustrates the CD-RISC-10-item score distributions and correlations within the derivation subsample. Mean (± standard deviation) item scores ranged from a low of 2.57 (1.10) on item 8 to a high of 3.02 (0.98) on item 5. Appendix B in the supplement lists the frequencies with which respondents endorsed various response options on the CD-RISC-10 items. As tests for normality (e.g., Kolmogorov-Smirnoff D test, Anderson–Darling test, and Shapiro–Wilk W test) were all significant (p < 0.05), we reject the null hypothesis of normal distribution of item scores within the study sample. Inter-item polychoric correlations ranged from a low of 0.51 (SE 0.20) between items 3 and 8 to a high of 0.82 (SE 0.01) between items 1 (“able to adapt”) and 2 (“can deal with whatever comes”). Item 3 (“try to see humorous side”) was least correlated with other items. The two CD-RISC-10 items with the highest item-to-scale polychoric correlations were items 2 (ρ = 0.88, SE = 0.01) and 9 (ρ = 0.88, SE = 0.01). Among CD-RISC-10 items, deletion of items 2 (“can deal with whatever comes”) and 9 (“think of myself as strong person”) causes the largest decrease(s) in the scale’s Cronbach’s alpha coefficient. Despite similar floor (1.20 vs 1.30%) and ceiling effects (25.0 vs 24.7%), a summated score of items 2 and 9 is more correlated (ρ = 0.936, SE = 0.003) than the CD-RISC-2 (ρ = 0.908, SE = 0.004) with the CD-RISC-10 scale.
Table 2.
Score dispersion and inter-item correlations of the abbreviated Connor–Davidson resilience scale in the derivation subsample
| CD-RISC-10© Scale Item |
Item Score Dispersion | Inter-item Polychoric Correlation, ρ (SE) | Cronbach’s alpha if the item is deleted | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (± SD) | Skewness | Kurtosis | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |||
| 1 | “able to adapt when changes occur” | 2.974 (.983) | − 0.887 | 0.545 | 1.000 | 0.925 | |||||||||
| 2 | “can deal with whatever comes” | 2.975 (.944) | − 0.758 | 0.318 | 0.823 (.009) | 1.000 | 0.922 | ||||||||
| 3 | “try to see humorous side of things” | 2.665 (1.071) | − 0.488 | − 0.358 | 0.545 (.017) | 0.601 (.016) | 1.000 | 0.931 | |||||||
| 4 | “…stress can make me stronger” | 2.652 (1.014) | − 0.433 | − 0.252 | 0.605 (.016) | 0.641 (.015) | 0.615 (.015) | 1.000 | 0.926 | ||||||
| 5 | “tend to bounce back after… hardships” | 3.022 (.979) | − 0.932 | 0.590 | 0.659 (.014) | 0.723 (.013) | 0.567 (.016) | 0.676 (.014) | 1.000 | 0.924 | |||||
| 6 | “can achieve… goals, even if…obstacles” | 2.986 (.953) | − 0.813 | 0.397 | 0.650 (.015) | 0.690 (.014) | 0.530 (.017) | 0.639 (.015) | 0.717 (.013) | 1.000 | 0.923 | ||||
| 7 | “Under pressure, I stay focused…” | 2.807 (.988) | − 0.650 | 0.093 | 0.672 (.014) | 0.719 (.012) | 0.517 (.017) | 0.611 (.015) | 0.660 (.014) | 0.719 (.012) | 1.000 | 0.923 | |||
| 8 | “not easily discouraged by failure” | 2.570 (1.102) | − 0.456 | − 0.432 | 0.568 (.016) | 0.624 (.015) | 0.505 (.017) | 0.570 (.016) | 0.616 (.015) | 0.650 (.014) | 0.687 (.013) | 1.000 | 0.927 | ||
| 9 | “strong… when dealing with challenges” | 2.978 (1.022) | − 0.857 | 0.236 | 0.661 (.014) | 0.721 (.013) | 0.544 (.017) | 0.627 (.015) | 0.716 (.013) | 0.754 (.011) | 0.736 (.012) | 0.696 (.013) | 1.000 | 0.922 | |
| 10 | “able to handle unpleasant or painful feelings” | 2.835 (1.032) | − 0.734 | 0.121 | 0.642 (.015) | 0.695 (.013) | 0.525 (.017) | 0.605 (.015) | 0.686 (.013) | 0.674 (.014) | 0.680 (.013) | 0.656 (.014) | 0.772 (.011) | 1.000 | 0.924 |
| Scale | Scale Score Dispersion | Item-to-Scale Polychoric Correlation, ρ (SE) | Polychoric correlation, ρ (SE), with CDRISC-10 | ||||||||||||
| Mean (± SD) | Percent Floor | Percent Ceiling | |||||||||||||
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||||||
| CDRISC-10 | 28.463 (7.926) | 0.70 | 6.60 | 0.831 (.008) | 0.881 (.006) | 0.737 (.010) | 0.809 (.008) | 0.853 (.007) | 0.851 (.007) | 0.852 (.007) | 0.810 (.008) | 0.878 (.006) | 0.843 (.007) | 1.000 | |
| CDRISC-2 | 5.996 (1.745) | 1.30 | 24.70 | 0.943 (.004) | – | – | – | 0.935 (.004) | – | – | – | – | – | 0.908 (.004) | |
| Summation of Items 2 and 9 | 5.953 (1.785) | 1.20 | 25.00 | – | 0.949 (.003) | – | – | – | – | – | – | 0.959 (.003) | – | 0.936 (.003) | |
Key: CD-RISC-10 = Ten-item abbreviation of the Connor–Davidson resilience scale; SD = standard deviation; SE = standard error; © As the CD-RISC-10 is a proprietary scale protected by copyright, the brief phrases here do not reveal the entire framing of items
CFAs of the CD-RISC-10 based on the ULSMV estimator provided the best fit to the derivation data (SRMR = 0.024; CFI = 0.976; TLI = 0.969). The good fit of a one-factor ten-item CFA model supports unidimensionality. Standardized loadings (λstandardized) for all items exceeded 0.700 (p < 0.001). Items 2 and 9 had the highest and second highest factor loadings (λstandardized = 0.866 and 0.865) plus proportions of variance in item scores (R2 = 0.750 and 0.748) accounted for by the single factor. Appendix C reports findings from multi-group CFAs of the CD-RISC-10 within the derivation subsample. The ULSMV-estimated CFA model showed good overall fit to the data (SRMR ≤ 0.800, CFI ≥ 0.950; TLI ≥ 0.950) among the subpopulations tested. Indices of global fit to the derivation data were weakest among rural/small town respondents (CFI = 0.949; TLI = 0.934) and strongest for micro-urban areas (CFI = 0.986; TLI = 0.983).
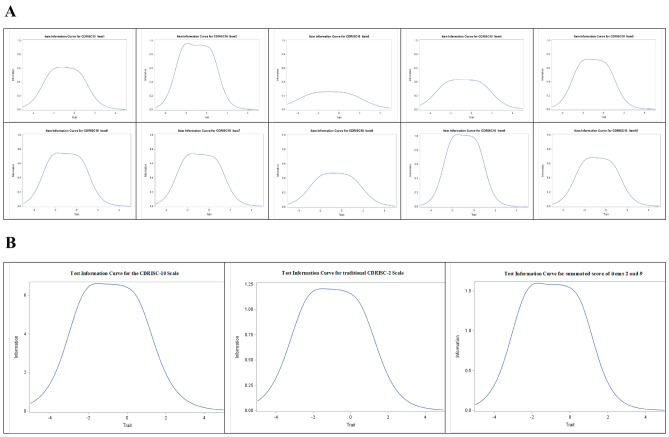
Calibration with the unidimensional graded response model
Examination of item response OCCs (cf. Fig. 1) confirms that CD-RISC-10 items validly capture respondents’ resilience. Item 3 had the flattest OCCs (lowest endorsements) for response options 1, 2, and 3. Respondents endorsed a wide spread of responses (from 0 to 4) on the other 9 items. As resilience (x axis) rises, probability (y axis) of endorsing higher options (3 or 4) increases but that of selecting lower options (0 or 1) decreases, supporting monotonicity. Parameter estimates from the unidimensional GRM of CD-RISC-10 in the derivation subsample are listed in Table 3. Monotonicity was confirmed by item scalability coefficients ranging from Hi = 0.529 for item 3 to Hi = 0.662 for item 2, and a Mokken scalability (Hs) coefficient (95% CI) of 0.617 (0.597 – 0.638) for the entire CD-RISC-10. Item 3 had a “high” slope (α = 1.35–1.75). The other 9 items had “very high” slopes (α ≥ 1.70). Item 9 had the steepest slope (α = 3.387) followed by item 2 (α = 3.208). Thus, these were the two most efficient items at discriminating between respondents’ self-rated resilience on the CD-RISC-10. Response category thresholds ranged from − 2.679 for Ь1 on item 3 to 0.927 for Ь4 on item 3. Local independence is supported by absence of extremely high slope parameters (> 4), and by the very small/inconsequential standardized LD ∑2 statistics for all item pairs (from |0.074| for items 2 and 7 to |0.217| for items 1 and 2). The S-∑2 index showed good overall fit (p ≥ 0.001) for most CD-RISC-10 items, with only items 8 and 2 showing weak fit (p < 0.001). Figure 2A shows the information function curves for the CD-RISC-10 items. The plots reveal that items 2 and 9 captured the highest amount of psychometric information on resilience across the entire breadth of its variability. In contrast, item 3 displayed the flattest information curve. Figure 2B compares test information curves for the CD-RISC-10 scale, the CD-RISC-2 scale, and a summated score of items 2 and 9. A summation of items and 9 captures more psychometric information than the CD-RISC-2, despite the latter’s good performance.
Fig. 1.
Response option characteristic curves for the ten items of the abbreviated Connor–Davidson Resilience Scale
Table 3.
Unidimensional Graded Response Model of the Ten-Item Abbreviated Connor–Davidson Resilience Scale in the Derivation Subsample – Item Scalability, Slope (Discrimination), and Response Category Threshold (Difficulty) Parameters
| CD-RISC-10© Scale Item | Monotonicity | Slope ʃ | Response Category Thresholds ʃ | Item Goodness of Fit | |||||
|---|---|---|---|---|---|---|---|---|---|
| Hi (SE) | α (SE) | Ƅ1 (SE) | Ƅ2 (SE) | Ƅ3 (SE) | Ƅ4 (SE) | S-Σ2 Index | p | ||
| 1 | “able to adapt when changes occur” | 0.604 (0.014) | 2.587 (.047) | − 2.360 (.071) | − 1.819 (.055) | − 0.687 (.034) | 0.431 (.033) | 105.997 | 0.004 |
| 2 | “can deal with whatever comes” | 0.662 (0.011) | 3.208 (.061) | − 2.458 (.075) | − 1.770 (.051) | − 0.621 (.031) | 0.448 (.030) | 110.430 | < 0.001 |
| 3 | “try to see humorous side of things” | 0.529 (0.015) | 1.630 (.032) | − 2.679 (.097) | − 1.604 (.063) | − 0.285 (.038) | 0.927 (.048) | 120.611 | 0.014 |
| 4 | “…stress can make me stronger” | 0.605 (0.013) | 2.132 (.039) | − 2.501 (.081) | − 1.522 (.053) | − 0.226 (.033) | 0.923 (.041) | 80.227 | 0.112 |
| 5 | “tend to bounce back after… hardships” | 0.634 (0.012) | 2.796 (.051) | − 2.365 (.072) | − 1.773 (.054) | − 0.717 (.033) | 0.341 (.031) | 86.718 | 0.053 |
| 6 | “can achieve… goals, even if…obstacles” | 0.635 (0.012) | 2.856 (.052) | − 2.456 (.079) | − 1.769 (.054) | − 0.650 (.032) | 0.425 (.031) | 81.090 | 0.062 |
| 7 | “Under pressure, I stay focused…” | 0.639 (0.012) | 2.836 (.050) | − 2.316 (.071) | − 1.537 (.048) | − 0.449 (.031) | 0.696 (.034) | 102.67 | 0.003 |
| 8 | “not easily discouraged by failure” | 0.593 (0.014) | 2.310 (.040) | − 2.062 (.066) | − 1.245 (.045) | − 0.196 (.032) | 0.883 (.041) | 135.391 | < 0.001 |
| 9 | “strong… when dealing with challenges” | 0.657 (0.012) | 3.387 (.062) | − 2.194 (.066) | − 1.524 (.045) | − 0.589 (.030) | 0.326 (.029) | 73.082 | 0.138 |
| 10 | “able to handle unpleasant or painful feelings” | 0.624 (0.013) | 2.792 (.048) | − 2.176 (.067) | − 1.513 (.048) | − 0.497 (.031) | 0.572 (.033) | 99.400 | 0.005 |
Key α is the item slope (discrimination) parameter; Ƅ1 to Ƅ4 are item response category threshold (difficulty, location) parameters;
Hi is the scalability index of monotonicity; SE = standard error; ʃ indicates that p < 0.0001 for all the slope (α) and threshold (Ƅ) parameters, S- Σ2 is the generalized item-level goodness-of-fit index (calculated on 2460 observations with complete data); p is significance level for the S- Σ2 index
© As the CD-RISC-10 is a proprietary scale protected by copyright, the brief phrases here do not reveal the entire framing of items
Fig. 2.
A Item information curves for the ten items of the abbreviated Connor–Davidson Resilience Scale. B Test information curves for ten-item and two-item abbreviations of the Connor–Davidson Resilience Scale
Concurrent validity and reliability of the CD-RISC-2 versus a summation of items 2 and 9
Figure 3 shows the ROC and PRC plots of how well high resilience on the CD-RISC-10 scale (score ≥ 36) is predicted by continuous scores on the conventional CD-RISC-2 scale versus the summated score of items 2 and 9. For both item pairs, a combined score of 8 represents the optimum threshold corresponding with high resilience (≥ 36) on the CD-RISC-10. Despite the good predictive validity of the CD-RISC-2, summation of items 2 and 9 slightly but consistently outperforms it in discriminating high CD-RISC-10 scores (area under the ROC = 0.940 vs 0.928, p < 0.001; area under the PRC = 0.701 vs 0.687, p = 0.050; respectively). Table 4 lists internal consistency reliability indices for the CD-RISC-10, the CD-RISC-2 and summation of items 2 and 9 from CD-RISC-10. AVE was > 0.500 and other reliability coefficients were > 0.700 for all three item combinations, supporting internal consistency. The summation of items 2 and 9 has higher internal consistency than the CD-RISC− 2. Negative correlations > 0.300 with anxiety, depression, anxiety sensitivity, COVID fear, and 2 avoidant (behavioral disengagement, self-blame) coping orientations (cf. Table 5) support discriminant validity for the CD-RISC-10, CD-RISC-2, and summation of items 2 and 9. Positive correlations > 0.300 with ‘emotionally stable’, ‘conscientious’, and ‘open to experience’ personalities plus > 0.250 with 1 approach (acceptance) coping orientation (cf. Table 5) support convergent validity. Kruskal–Wallis nonparametric analyses of variance found that COVID-related experiences (testing positive for SARS-Cov-2, caring for COVID-19 patients, or knowing someone with COVID) had no significant association (p > 0.05) with scores on the CD-RISC-10, CD-RISC-2, or summation of items 2 and 9. Table 6 compares inter-rater reliability for CD-RISC-10, CD-RISC-2, and summated score of items 2 and 9 in discriminating high resilience in the validation subsample. Agreement coefficients and binary/prediction indexes with the CD-RISC-10 were consistently higher for the summation of items 2 and 9 versus the CD-RISC− 2.
Fig. 3.
Receiver operating characteristic and Precision-recall curve plots of CD-RISC-2 scale’s ability to discriminate high CD-RISC-10 scale scores in the derivation subsample
Table 4.
Internal Consistency Reliability Indices of the Abbreviated Connor–Davidson Resilience Scales in the Validation Subsample
| Index of Scale Reliability | CDRISC-10 Scale | CDRISC-2 Scale | Summated Score of Items 2 and 9 |
|---|---|---|---|
| Ordinal alpha (α) coefficient | 0.950 | 0.794 | 0.856 |
| Ordinal theta (θ) coefficient | 0.951 | 0.794 | 0.856 |
| Cronbach's alpha (α) coefficient (standardized) | 0.934 | 0.726 | 0.804 |
| Cronbach's alpha (α) coefficient (raw) | 0.933 | 0.726 | 0.801 |
| Spearman-Brown coefficient | 0.945 | 0.726 | 0.804 |
| McDonald’s omega (ω) coefficient of composite reliability | 0.950 | 0.791 | 0.855 |
| Average variance extracted (AVE) | 0.657 | 0.665 | 0.767 |
Table 5.
Convergent and Discriminant Validity of the Abbreviated Connor–Davidson Resilience Scales in the Validation Subsample
| Type of Criterion Validity | Construct | Measurement Scale or Subscale | CD-RISC-10 | CD-RISC-2 | Summation of |
|---|---|---|---|---|---|
| Scale | Scale | Items 2 and 9 | |||
| ρ (SE) | ρ (SE) | ρ (SE) | |||
| Divergent validity | Anxiety | GAD-7 Scale | − 0.450 (.018) | − 0.437 (.018) | − 0.435 (.019) |
| Depression | PHQ-8 Scale | − 0.460 (.017) | − 0.424 (.018) | − 0.448 (.018) | |
| Anxiety Sensitivity | ASI-3 physical concerns | − 0.354 (.019) | − 0.332 (.019) | − 0.349 (.019) | |
| ASI-3 cognitive concerns | − 0.400 (.019) | − 0.374 (.019) | − 0.404 (.019) | ||
| ASI-3 social concerns | − 0.259 (.019) | − 0.247 (.020) | − 0.259 (.020) | ||
| COVID Fear | FCV-19 Scale | − 0.357 (.026) | − 0.342 (.027) | − 0.371 (.027) | |
| Convergent validity | Personality Traits | TIPI – agreeableness | 0.308 (.019) | 0.275 (.019) | 0.302 (.020) |
| TIPI – conscientiousness | 0.453 (.017) | 0.404 (.018) | 0.480 (.017) | ||
| TIPI – emotional stability | 0.588 (.014) | 0.539 (.015) | 0.578 (.015) | ||
| TIPI – extraversion | 0.302 (.019) | 0.275 (.019) | 0.295 (.020) | ||
| TIPI – openness to experience | 0.330 (.018) | 0.306 (.019) | 0.313 (.019) | ||
| Coping Orientation | Brief COPE – acceptance | 0.254 (.020) | 0.278 (.021) | 0.258 (.021) | |
| Brief COPE – positive reframing | 0.223 (.020) | 0.185 (.021) | 0.190 (.021) | ||
| Brief COPE – active coping | 0.213 (.020) | 0.174 (.020) | 0.189 (.020) | ||
| Brief COPE – religion | 0.122 (.022) | 0.076 (.023) | 0.103 (.023) | ||
| Brief COPE – planning/strategizing | 0.088 (.021) | 0.072 (.022) | 0.077 (.022) | ||
| Brief COPE – use of humor | 0.077 (.022) | 0.044 (.023) | 0.026 (.023) | ||
| Brief COPE – emotional support | 0.042 (.022) | 0.018 (.022) | 0.041 (.022) | ||
| Divergent validity | Brief COPE – behavioral disengagement | − 0.378 (.022) | − 0.399 (.022) | − 0.402 (.022) | |
| Brief COPE – self-blame | − 0.384 (.021) | − 0.372 (.021) | − 0.396 (.021) | ||
| Brief COPE – substance abuse | − 0.246 (.025) | − 0.268 (.025) | − 0.271 (.025) | ||
| Brief COPE – denial of reality | − 0.222 (.024) | − 0.250 (.024) | − 0.255 (.024) | ||
| Brief COPE – venting | − 0.121 (.021) | − 0.109 (.022) | − 0.141 (.022) | ||
| Brief COPE – self distraction | − 0.046 (.021) | − 0.039 (.022) | − 0.047 (.022) | ||
| Brief COPE – instrumental support | − 0.043 (.022) | − 0.079 (.023) | − 0.076 (.023) |
KEY ASI-3 = Anxiety Sensitivity Index-3; Brief COPE = Coping Orientation to Problems Experienced Inventory; CD-RISC-10 = Ten-item abbreviation of the Connor–Davidson Resilience Scale; CD-RISC-2 = Two-item abbreviation of the Connor–Davidson Resilience Scale; FCV-19 = Seven-item Fear of COVID-19 Scale; GAD-7 = Seven-item Generalized Anxiety Disorder Scale; PHQ-8 = Eight-item Patient Health Questionnaire; ρ = polychoric correlation coefficient; SE = standard error of correlation coefficient; TIPI = Ten-item Personality Inventory;
Table 6.
Inter-rater Reliability of the Abbreviated Connor–Davidson Resilience Scales in the Validation Subsample
| CD-RISC-2 Scale vs CD-RISC-10 Scale | Summation of Items 2 and 9 vs CD-RISC-10 Scale | CD-RISC-2 Scale vs Summation of Items 2 and 9 | |
|---|---|---|---|
| Coefficients of agreement | |||
| Percent agreement | 88.875 | 90.805 | 86.172 |
| Cohen's kappa statistic (κc) | 0.692 | 0.750 | 0.638 |
| Conger’s kappa statistic | 0.692 | 0.746 | 0.617 |
| Fleiss' kappa statistic (κf) | 0.692 | 0.749 | 0.639 |
| Gwet's AC1 coefficient | 0.826 | 0.855 | 0.776 |
| Brennan‐Prediger coefficient (κ3) | 0.778 | 0.816 | 0.723 |
| Krippendorff's alpha (α) coefficient | 0.692 | 0.750 | 0.638 |
| Discrimination and classification indices | |||
| Accuracy | 0.889 | 0.908 | – |
| Misclassification (Error) rate | 0.111 | 0.092 | – |
| Sensitivity/Recall (True positive probability) | 0.819 | 0.890 | – |
| Specificity (True negative probability) | 0.908 | 0.913 | – |
| Positive predictive value/Precision | 0.717 | 0.743 | – |
| Negative predictive value | 0.947 | 0.967 | – |
| False negative probability | 0.181 | 0.110 | – |
| False positive probability (1 – Specificity) | 0.092 | 0.087 | – |
| Area under the ROC curve | 0.934 | 0.952 | – |
| Area under the PRC curve | 0.624 | 0.688 | – |
| Matthews correlation coefficient (ϕ) | 0.695 | 0.755 | – |
| F1-score | 0.765 | 0.810 | – |
Key: CDRISC-10 = Ten-item abbreviation of the Connor–Davidson Resilience Scale; CDRISC-2 = Two-item abbreviation of the Connor–Davidson Resilience Scale; ROC = receiver operating characteristic; PRC = precision recall characteristic
Discussion
An in-depth investigation of the validity and reliability of abbreviated CD-RISC scales was conducted using both CTT- and IRT-based methods among a nationwide sample of Americans responding to the COVID-19 pandemic. This psychometric validation study aimed to augment previous research by adducing evidence based on modern measurement theory to contribute towards eventual consensus on effective ways of tracking personal resilience. In correspondence with past studies, our findings confirm the construct validity, reliability, internal consistency, unidimensionality, and monotonicity of the CD-RISC-10 scale. However, study data did not support our hypothesis that, among CD-RISC-10 items, CD-RISC-2 items would be the most valid/reliable item duo. A summation of CD-RISC-10 items 2 and 9 slightly but significantly outperforms the CD-RISC-2 on concurrent validity and inter-rater reliability indices.
The mean (± SD) CD-RISC-10 score of 28.46 (7.93) in our sample is comparable to that in the initial validation study [23], lower than reported for U.S. community samples in previous years [95, 96] but identical to findings in populations responding to the COVID-19 pandemic [97] or similar crises [98]. Compared to validations in U.S. [23, 52, 95] and other settings [31–33], we observed higher internal consistency for the CD-RISC-10 and CD-RISC-2 (cf. Table 4). In concurrence with prior studies [31–33], the CD-RISC-10 had greater internal consistency in our sample than the CD-RISC−2. This could be partially due to how the CD-RISC-2 scale was originated more on subjective than empirical criteria [52].
In convergent/divergent validity analyses, both the CD-RISC-2 and summation of items 2 and 9 correlated with measures of depression, anxiety, COVID-19 fear, and coping styles to the same degree and in the same direction as the CD-RISC-10 (cf. Table 5). Thus, two-item and ten-item CD-RISC abbreviations show identical convergent/divergent validity. Compared to previous reports [32, 33, 62, 64], larger correlations of CD-RISC-2 and CD-RISC-10 scales with depression, anxiety, and fear of COVID-19 measures were observed in the present study. Prior studies used Pearson and Spearman, instead of polychoric, correlation coefficients in convergent/divergent validity analyses [32, 33, 64], despite the ordinal nature of Likert scales such as the CD-RISC-10/-2, PHQ-8/-9, GAD-7, and FCV-19. Unlike polychoric correlations, Pearson/Spearman correlations under-estimate associations between ordinal scales [84]. Higher correlations with anxiety and depression were reported in a study using the Hospital Anxiety and Depression Scale (HADS) [31] instead of the PHQ-9 [32, 33, 62] and GAD-7 [32, 33] employed in aforementioned studies. Of the five personality traits, emotional stability was most correlated with abbreviated CD-RISC scales, followed by conscientiousness, findings that concur with Zager Kojcan et al. [99].
The present study supports the psychometric quality and utility of the CD-RISC-10 and CD-RISC-2 scales. We also found evidence, based on CTT and IRT methods, that a summation of items 2 and 9 of the CD-RISC-10 slightly but consistently outperforms the CD-RISC-2 on multiple validity/reliability indices. Summated scores of items 2 and 9 correlated better than the CD-RISC-2 with the CD-RISC-10, and manifested superior agreement and inter-rater reliability. Some previous studies also found items 2 and 9 to have the highest factor loadings among CD-RISC-10 items [25, 37]. However, we know of no prior study that conducted GRM-based item diagnostics to test the CD-RISC-2’s concurrent validity and reliability against alternative item pairings from the CD-RISC-10. This study is not intended to modify the CD-RISC-2, a copyright-protected proprietary scale. Rather, the study yields evidence that, contrary to the CD-RISC-2’s emphasis on adaptability and bouncing back, Americans facing a surging COVID-19 pandemic rated their ability to cope with adversity and mental strength as more salient pillars of resilience. Thus, the salience of different flavors of resilience rises or falls based on variation in adaptation demands arising from the evolution of adverse stimuli across time and context [3]. Future studies should utilize IRT-based item-level diagnostics of old and new resilience measures to test varying salience of different flavors of resilience among persons responding to one adversity versus another. High ceiling effects reported in past studies such as Heritage et al. [46], now corroborated by our findings, call for fresh, innovative measures incorporating items that conceptually reflect and psychometrically capture the sentiments of highly resilient persons more efficiently than CD-RISC scales do.
Limitations of the present study are worth noting. The cross-sectional sample precluded test–retest reliability assessment. The U.S. English context limits generalizability/transferability to non-U.S. geographic/cultural contexts without further evidence. Multi-group CFAs revealed scalar variance [94] by the metropolitan status of respondents’ residential areas. The survey did not include another single-factor resilience measure (e.g., the Brief Resilience Scale [100]) against which to test the relative performance of CD-RISC scales. The self-administered, self-report, subjective scales were not validated against external observer ratings (e.g., situational judgment tests [20, 101]), nor objective metrics (e.g., genetic markers [102], stress hormones [103]). We also did not assess the extent of acquiescence response bias. The large, nationwide sample; diverse range of validity/reliability inferential tests reported compared to the few indices in past studies; and the split-sample internal validation strategy to minimize overfitting were notable strengths. The study’s timing, in the midst of a surging COVID-19 pandemic, was a further strength. Past resilience research has predominantly focused on responses to violent events [13], natural disasters [104], or wartime combat [26]. The COVID-19 surge allowed us to expand the evidence base by investigating resilience within the context of a pervasive, escalating stressor.
Conclusion
In an extensive psychometric validation study that employed both classic and modern approaches, we adduced sufficient evidence to confirm our hypothesis that the CD-RISC-10 and CD-RISC-2 exhibit good construct validity, internal consistency, and inter-rater reliability, in addition to unidimensionality, monotonicity, and local independence. However, the data failed to support our hypothesis that the CD-RISC-2’s constituent items represented the most empirically robust pairing out of the ten CD-RISC-10 items. Summative scores of items 2 and 9 (instead of items 1 and 5) from the CD-RISC-10 slightly but consistently outperformed the CD-RISC-2 on all empirical indices of validity and reliability. This study adds new psychometric evidence from a rigorous GRM-based evaluation of the abbreviated CD-RISC scales.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Study concept and design – ACW, BMB, MMB, DCM, AMW. Acquisition of data – AMW, MMB. Analysis and interpretation of data – ACW, JRP, MCM, RDB, DCM. Drafting of manuscript – ACW, BMB, JRP, DCM. Critical revision of the manuscript for intellectual content – All authors. Final approval of version to be published – All authors. Accountable for all aspects of the work – ACW.
Funding
The authors gratefully acknowledge financial support from the Baylor Scott and White Foundation and the W. W. Caruth, Jr. Fund at Communities Foundation of Texas.
Data availability
Data from this study are strictly protected by privacy and confidentiality agreements specified in the study protocol that was approved by the institutional review board.
Code availability
Samples of the kind of software syntax that was utilized in the quantitative analyses can be requested from the corresponding author. All requests will be subject to vetting by the institutional review board prior to dissemination.
Declarations
Conflict of interest
The authors have no conflicting interests to declare.
Ethical approval
The Institutional Review Board (IRB) at Baylor Scott and White Research Institute approved the parent project under protocol # 020-035.
Footnotes
References
- 1.Coutu DL. How resilience works. Harvard Business Review. 2002;80(5):46–50. [PubMed] [Google Scholar]
- 2.Luthans F, Vogelgesang GR, Lester PB. Developing the psychological capital of resiliency. Human Resource Development Review. 2006;5(1):25–44. doi: 10.1177/1534484305285335. [DOI] [Google Scholar]
- 3.Fletcher D, Sarkar M. Psychological resilience: A review and critique of definitions, concepts and theory. European Psychologist. 2013;18(1):12–23. doi: 10.1027/1016-9040/a000124. [DOI] [Google Scholar]
- 4.Neenan M. Developing resilience: A cognitive-behavioural approach. 2. New York: Routledge; 2018. [Google Scholar]
- 5.Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology. 2004;86(2):320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waddimba AC, Scribani M, Hasbrouck MA, Krupa N, Jenkins P, May JJ. Resilience among employed physicians and mid-level practitioners in upstate New York. Health Services Research. 2016;51(5):1706–1734. doi: 10.1111/1475-6773.12499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Waddimba AC, Bennett MM, Fresnedo M, Ledbetter TG, Warren AM. Resilience, well-being, and empathy among private practice physicians and advanced practice providers in Texas: A structural equation model study. Mayo Clinic Proceedings: Innovation, Quality and Outcomes. 2021;5(5):928–945. doi: 10.1016/j.mayocpiqo.2021.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kermott CA, Johnson RE, Sood R, Jenkins SM, Sood A. Is higher resilience predictive of lower stress and better mental health among corporate executives? PLoS ONE. 2019;14(6):e0218092. doi: 10.1371/journal.pone.0218092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dragonetti JD, Gifford TW, Yang MS. The process of developing a unit-based army resilience program. Current Psychiatry Reports. 2020;22(9):48. doi: 10.1007/s11920-020-01169-w. [DOI] [PubMed] [Google Scholar]
- 11.Crane MF, Falon SL, Kho M, Moss A, Adler AB. Developing resilience in first responders: strategies for enhancing psychoeducational service delivery. Psychological Services. 2021 doi: 10.1037/ser0000439. [DOI] [PubMed] [Google Scholar]
- 12.Zadok-Gurman T, Jakobovich R, Dvash E, Zafrani K, Rolnik B, Ganz AB, Lev-Ari S. Effect of Inquiry-Based Stress Reduction (IBSR) intervention on well-being, resilience and burnout of teachers during the COVID-19 pandemic. International Journal of Environmental Research and Public Health. 2021;18(7):3689. doi: 10.3390/ijerph18073689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Butler LD, Koopman C, Azarow J, Blasey CM, Magdalene JC, DiMiceli S, Seagraves DA, Hastings TA, Chen X-H, Garlan RW, Kraemer HC, Spiegel D. Psychosocial predictors of resilience after the September 11, 2001 terrorist attacks. Journal of Nervous and Mental Disease. 2009;197(4):266–273. doi: 10.1097/NMD.0b013e31819d9334. [DOI] [PubMed] [Google Scholar]
- 14.Román-Mata SS, Zurita-Ortega F, Puertas-Molero P, Badicu G, González-Valero G. A predictive study of resilience and its relationship with academic and work dimensions during the COVID-19 pandemic. Journal of Clinical Medicine. 2020;9(10):3258. doi: 10.3390/jcm9103258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.PeConga EK, Gauthier GM, Holloway A, Walker RSW, Rosencrans PL, Zoellner LA, Bedard-Gilligan M. Resilience is spreading: Mental health within the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice and Policy. 2020;12(S1):S47–S48. doi: 10.1037/tra0000874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Killgore WDS, Taylor EC, Cloonan SA, Dailey NS. Psychological resilience during the COVID-19 lockdown. Psychiatry Research. 2020;291:113216. doi: 10.1016/j.psychres.2020.113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rotărescu VS, Matei DB, Mircea IA, Mirescu AM, Nedelescu BG, Nedelea DG, Raluca Neagu AN, Necşulescu AG, Oteşanu GA, Tudor LC. How anxious did you feel during lockdown? The roles resilience, living environment, and gender play on the level of anxiety state during pandemic isolation. Research in Psychotherapy. 2021;23(496):231–238. doi: 10.4081/ripppo.2020.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahern NR, Kiehl EM, Sole ML, Byers J. A review of instruments measuring resilience. Issues in Comprehensive Pediatric Nursing. 2006;29(2):103–125. doi: 10.1080/01460860600677643. [DOI] [PubMed] [Google Scholar]
- 19.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and Quality of Life Outcomes. 2011;9(1):1–8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pangallo A, Zibarras L, Lewis R, Flaxman P. Resilience through the lens of interactionism: a systematic review. Psychological Assessment. 2015;27(1):1–20. doi: 10.1037/pas0000024. [DOI] [PubMed] [Google Scholar]
- 21.DeSimone JA, Harms PD, Vanhove AJ, Herian MN. Development and validation of the five-by-five resilience scale. Assessment. 2017;24(6):778–797. doi: 10.1177/1073191115625803. [DOI] [PubMed] [Google Scholar]
- 22.Connor KM, Davidson JR. Development of a New Resilience Scale: The Connor–Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 23.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor–Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- 24.Burns RA, Anstey KJ. The Connor–Davidson Resilience Scale (CD-RISC): Testing the invariance of a uni-dimensional resilience measure that is independent of positive and negative affect. Personality and Individual Differences. 2010;48(5):527–531. doi: 10.1016/j.paid.2009.11.026. [DOI] [Google Scholar]
- 25.Gucciardi DF, Jackson B, Coulter TJ, Mallett CJ. The Connor–Davidson Resilience Scale (CD-RISC): Dimensionality and age-related measurement invariance with Australian Cricketers. Psychology of Sport and Exercise. 2011;12(4):423–433. doi: 10.1016/j.psychsport.2011.02.005. [DOI] [Google Scholar]
- 26.Green KT, Hayward LC, Williams AM, Dennis PA, Bryan BC, Taber KH, Davidson JR, Beckham JC, Calhoun PS. Examining the Factor Structure of the Connor–Davidson Resilience Scale (CD-RISC) in a Post-9/11 U.S. Military Veteran Sample. Assessment. 2014;21(4):443–451. doi: 10.1177/1073191114524014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fernandez AC, Fehon DC, Treloar H, Ng R, Sledge WH. Resilience in organ transplantation: An application of the Connor–Davidson Resilience Scale (CD-RISC) with liver transplant candidates. Journal of Personality Assessment. 2015;97(5):487–493. doi: 10.1080/00223891.2015.1029620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sarkar M, Fletcher D. How should we measure psychological resilience in sport performers? Measurement in Physical Education and Exercise Science. 2013;17(4):264–280. doi: 10.1080/1091367X.2013.805141. [DOI] [Google Scholar]
- 29.Preacher KJ, MacCallum RC. Repairing Tom Swift's electric factor analysis machine. Understanding Statistics. 2003;2(1):13–43. doi: 10.1207/S15328031US0201_02. [DOI] [Google Scholar]
- 30.Notario-Pacheco B, Solera-Martínez M, Serrano-Parra MD, Bartolomé-Gutiérrez R, García-Campayo J, Martínez-Vizcaíno V. Reliability and Validity of the Spanish Version of the 10-item Connor–Davidson Resilience Scale (10-item CD-RISC) in Young Adults. Health and Quality of Life Outcomes. 2011 doi: 10.1186/1477-7525-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuiper H, van Leeuwen CCM, Stolwijk-Swüste JM, Post MWM. Measuring Resilience with the Connor–Davidson Resilience Scale (CD-RISC): Which version to choose? Spinal Cord. 2019;57(5):360–366. doi: 10.1038/s41393-019-0240-1. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, Mo Y, Yan C, Li Y, Li H. Psychometric properties of two abbreviated Connor–Davidson Resilience Scales in Chinese infertile couples. Quality of Life Research. 2021;30(8):2405–2414. doi: 10.1007/s11136-021-02820-6. [DOI] [PubMed] [Google Scholar]
- 33.Wollny AI, Jacobs I. Validity and reliability of the German versions of the CD-RISC-10 and CD-RISC-2. Current Psychology. 2021 doi: 10.1007/s12144-021-01670-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kavčič T, Zager Kocjan G, Dolenc P. Measurement invariance of the CD-RISC-10 across gender, age, and education: A study with Slovenian adults. Current Psychology. 2021 doi: 10.1007/s12144-021-01564-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aloba O, Olabisi O, Aloba T. The 10-item Connor–Davidson Resilience Scale: Factorial structure, reliability, validity, and correlates among student nurses in southwestern Nigeria. Journal of the American Psychiatric Nurses Association. 2016;22(1):43–51. doi: 10.1177/1078390316629971. [DOI] [PubMed] [Google Scholar]
- 36.Smith KJ, Emerson DJ, Schuldt MA. A demographic and psychometric assessment of the Connor–Davidson resilience Scale 10 (CD-RISC 10) with a US Public Accounting Sample. Journal of Accounting & Organizational Change. 2018;14(4):513–534. doi: 10.1108/JAOC-12-2016-0085. [DOI] [Google Scholar]
- 37.Smith KJ, Emerson DJ, Haight TD, Mauldin S, Wood BG. An examination of the psychometric properties of the Connor–Davidson Resilience Scale-10 (CD-RISC10) among accounting and business students. Journal of Accounting Education. 2019;47:48–62. doi: 10.1016/j.jaccedu.2019.01.002. [DOI] [Google Scholar]
- 38.Hambleton RK, Swaminathan H, Rogers HJ. Fundamentals of Item Response Theory. Fundamentals of item response theory. Thousand Oaks: Sage; 1991. [Google Scholar]
- 39.Embretson SE, Reise SP. Item response theory for psychologists. Item response theory for psychologists. Mahwah: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- 40.de Ayala RJ. The theory and practice of item response theory. 1. New York: Guilford Press; 2009. [Google Scholar]
- 41.Millsap RE. Statistical approaches to measurement invariance. New York: Taylor and Francis Group; 2011. Item Response Theory: Models, estimation, fit evaluation; pp. 147–189. [Google Scholar]
- 42.Arias González VB, Crespo Sierra MT, Arias Martínez B, Martínez-Molina A, Ponce FP. An in-depth psychometric analysis of the Connor–Davidson Resilience Scale: Calibration with Rasch-Andrich Model. Health and Quality of Life Outcomes. 2015 doi: 10.1186/s12955-015-0345-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Papini N, Kang M, Ryu S, Griese E, Wingert T, Herrmann S. Rasch calibration of the 25-item Connor–Davidson Resilience Scale. Journal of Health Psychology. 2020 doi: 10.1177/1359105320904769. [DOI] [PubMed] [Google Scholar]
- 44.Ehrich J, Mornane A, Powern T. Psychometric validation of the 10-item Connor–Davidson Resilience Scale. Journal of Applied Measurement. 2017;18(2):122–136. [PubMed] [Google Scholar]
- 45.Pulido-Martos M, Fernández-Sánchez MD, Lopez-Zafra E. Measurement invariance across gender and age in the Connor–Davidson Resilience Scale (CD-RISC) in a Spanish general population. Quality of Life Research. 2020;29(5):1373–1384. doi: 10.1007/s11136-019-02389-1. [DOI] [PubMed] [Google Scholar]
- 46.Heritage B, Al Asadi AA, Hegney DG. Examination of the Connor–Davidson Resilience Scale 10 (CD-RISC-10) using the polytomous Rasch model. Psychological Assessment. 2021;33(7):672–684. doi: 10.1037/pas0001011. [DOI] [PubMed] [Google Scholar]
- 47.Samejima F. The general graded response model. In: Nering ML, Ostini R, editors. Handbook of polytomous item response theory models. 1. New York: Taylor & Francis; 2010. pp. 77–107. [Google Scholar]
- 48.Samejima F. Graded response models. In: van der Linden WJ, editor. Handbook of Item Response Theory, Volume One: Models. Boca Raton, FL: Chapman & Hall; 2016. pp. 95–108. [Google Scholar]
- 49.de Ayala RJ, Dodd BG, Koch WR. A comparison of the partial credit and graded response models in computerized adaptive testing. Applied Measurement in Education. 1992;5(1):17–34. doi: 10.1207/s15324818ame0501_2. [DOI] [Google Scholar]
- 50.Baker JG, Rounds JB, Zevon MA. A comparison of graded response and Rasch partial credit models with subjective well-being. Journal of Educational and Behavioral Statistics. 2000;25(3):253–270. doi: 10.2307/1165205. [DOI] [Google Scholar]
- 51.Lim KK, Kwan YH, Yeo SJ, Yeo W, Thumboo J, Matchar D, Leung YY. AB1324 measurement properties of the 10-item Connor–Davidson resilience scale among patients with total knee replacement based on item response theory. Annals of the Rheumatic Diseases. 2019;78(Supplement 2):2125–2126. doi: 10.1136/annrheumdis-2019-eular.1014. [DOI] [Google Scholar]
- 52.Vaishnavi S, Connor K, Davidson JR. An abbreviated version of the Connor–Davidson Resilience Scale (CD-RISC), the CD-RISC2: Psychometric properties and applications in psychopharmacological trials. Psychiatry Research. 2007;152(2–3):293–297. doi: 10.1016/j.psychres.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Warren AM, Zolfaghari K, Fresnedo M, Bennett MM, Pogue JR, Waddimba AC, Zvolensky M, Carlbring P, Powers MB. Anxiety sensitivity, COVID-19 fear, and mental health: Results from a United States Population Sample. Cognitive Behavior Therapy. 2021;50(3):204–216. doi: 10.1080/16506073.2021.1874505. [DOI] [PubMed] [Google Scholar]
- 54.Gonzalez SP, Moore EWG, Newton M, Galli NA. Validity and reliability of the Connor–Davidson Resilience Scale (CD-RISC) in competitive sport. Psychology of Sport and Exercise. 2016;23:31–39. doi: 10.1016/j.psychsport.2015.10.005. [DOI] [Google Scholar]
- 55.Carver CS. You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 56.Gosling SD, Rentfrow PJ, Swann WB. A very brief measure of the big-five personality domains. Journal of Research in Personality. 2003;37(6):504–528. doi: 10.1016/S0092-6566(03)00046-1. [DOI] [Google Scholar]
- 57.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 58.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 59.Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 Scale: Development and initial validation. International Journal of Mental Health and Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Abramowitz JS, Holaway RM, Sandin B, Stewart SH, Coles M, Eng W, Daly ES, Arrindell WA, Bouvard M, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the anxiety sensitivity index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- 61.Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience to personality, coping, and psychiatric symptoms in young adults. Behaviour Research and Therapy. 2006;44(4):585–599. doi: 10.1016/j.brat.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 62.Ni MY, Li TK, Yu NX, Pang H, Chan BHY, Leung GM, Stewart SM. Normative data and psychometric properties of the Connor–Davidson Resilience Scale (CD-RISC) and the abbreviated version (CD-RISC2) among the general population in Hong Kong. Quality of Life Research. 2016;25(1):111–116. doi: 10.1007/s11136-015-1072-x. [DOI] [PubMed] [Google Scholar]
- 63.Ruiz-Párraga GT, López-Martínez AE, Esteve R, Ramírez-Maestre C, Wagnild G. A confirmatory factor analysis of the resilience scale adapted to chronic pain (RS-18): New empirical evidence of the protective role of resilience on pain adjustment. Quality of Life Research. 2015;24(5):1245–1253. doi: 10.1007/s11136-014-0852-z. [DOI] [PubMed] [Google Scholar]
- 64.Chi X, Chen S, Chen Y, Chen D, Yu Q, Guo T, Cao Q, Zheng X, Huang S, Hossain MM, Stubbs B, Yeung A, Zou L. Psychometric evaluation of the fear of COVID-19 scale among Chinese population. International Journal of Mental Health and Addiction. 2021 doi: 10.1007/s11469-020-00441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nazari N, Zekiy AO, Feng LS, Griffiths MD. Psychometric validation of the Persian version of the Covid-19-related psychological distress scale and association with Covid-19 fear, Covid-19 anxiety, optimism, and lack of resilience. International Journal of Mental Health and Addiction. 2021 doi: 10.1007/s11469-021-00540-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zumbo B, Gadermann A, Zeisser C. Ordinal versions of coefficients alpha and theta for Likert rating scales. Journal of Modern Applied Statistical Methods. 2007;6(1):21–29. doi: 10.22237/jmasm/1177992180. [DOI] [Google Scholar]
- 67.Gadermann A, Guhn M, Zumbo B. Estimating ordinal reliability for Likert-type and ordinal item response data: A conceptual, empirical, and practical guide. Practical Assessment, Research & Evaluation. 2012;17(3):1–13. doi: 10.7275/n560-j767. [DOI] [Google Scholar]
- 68.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. doi: 10.1007/BF02310555. [DOI] [Google Scholar]
- 69.McDonald RP. Test theory: A unified treatment. 1. Hillsdale: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- 70.Hayes AF, Coutts JJ. Use omega rather than cronbach’s alpha for estimating reliability. But…. Communication Methods and Measures. 2020;14(1):1–24. doi: 10.1080/19312458.2020.1718629. [DOI] [Google Scholar]
- 71.Eisinga R, Grotenhuis MT, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? International Journal of Public Health. 2013;58(4):637–642. doi: 10.1007/s00038-012-0416-3. [DOI] [PubMed] [Google Scholar]
- 72.de Vet HCW, Mokkink LB, Mosmuller DG, Terwee CB. Spearman-Brown prophecy formula and Cronbach's alpha: Different faces of reliability and opportunities for new applications. Journal of Clinical Epidemiology. 2017;85:45–49. doi: 10.1016/j.jclinepi.2017.01.013. [DOI] [PubMed] [Google Scholar]
- 73.Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research. 1981;18(1):39–50. doi: 10.1177/002224378101800104. [DOI] [Google Scholar]
- 74.Hair JF, Jr, Black WC, Babin BJ, Anderson RE. Multivariate data analysis. 8. Hampshire: Cengage Learning EMEA; 2019. [Google Scholar]
- 75.Picard RR, Berk KN. Data splitting. American Statistician. 1990;44(2):140–147. doi: 10.2307/2684155. [DOI] [Google Scholar]
- 76.Bartlett MS. A note on the multiplying factors for various χ2 approximations. Journal of the Royal Statistical Society Series B (Methodological) 1954;16(2):296–298. doi: 10.1111/j.2517-6161.1954.tb00174.x. [DOI] [Google Scholar]
- 77.Cerny BA, Kaiser HF. A study of a measure of sampling adequacy for factor-analytic correlation matrices. Multivariate Behavioral Research. 1977;12(1):43–47. doi: 10.1207/s15327906mbr1201_3. [DOI] [PubMed] [Google Scholar]
- 78.Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30(2):179–185. doi: 10.1007/bf02289447. [DOI] [PubMed] [Google Scholar]
- 79.Zwick WR, Velicer WF. Comparison of five rules for determining the number of components to retain. Psychological Bulletin. 1986;99(3):432–442. doi: 10.1037/0033-2909.99.3.432. [DOI] [Google Scholar]
- 80.Brown TA. Confirmatory factor analysis for applied research. 2. New York: Guilford; 2015. [Google Scholar]
- 81.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 82.Maydeu-Olivares A. Assessing the size of model misfit in structural equation models. Psychometrika. 2017;82(3):533–558. doi: 10.1007/s11336-016-9552-7. [DOI] [PubMed] [Google Scholar]
- 83.Shi D, Maydeu-Olivares A, Rosseel Y. Assessing fit in ordinal factor analysis models: SRMR vs RMSEA. Structural Equation Modeling. 2020;27(1):1–15. doi: 10.1080/10705511.2019.1611434. [DOI] [Google Scholar]
- 84.Holgado-Tello FP, Chacón-Moscoso S, Barbero-García I, Vila-Abad E. Polychoric versus Pearson correlations in exploratory and confirmatory factor analysis of ordinal variables. Quality & Quantity. 2010;44(1):153–166. doi: 10.1007/s11135-008-9190-y. [DOI] [Google Scholar]
- 85.Holgado-Tello FP, Morata-Ramírez MÁ, Barbero-García MI. Confirmatory factor analysis of ordinal variables: A simulation study comparing the main estimation methods. Avances en Psicología Latinoamericana. 2018;36(3):601–617. doi: 10.12804/revistas.urosario.edu.co/apl/a.4932. [DOI] [Google Scholar]
- 86.Baker FB. The basics of item response theory. 2. College Park: ERIC Clearinghouse on Assessment and Evaluation; 2001. [Google Scholar]
- 87.Kang T, Chen TT. Performance of the generalized S-X2 item fit index for the graded response model. Asia Pacific Education Review. 2011;12(1):89–96. doi: 10.1007/s12564-010-9082-4. [DOI] [Google Scholar]
- 88.Stone CA, Zhang B. Assessing goodness of fit of item response theory models: A comparison of traditional and alternative procedures. Journal of Educational Measurement. 2003;40(4):331–352. doi: 10.1111/j.1745-3984.2003.tb01150.x. [DOI] [Google Scholar]
- 89.Chen W-H, Thissen D. Local dependence indexes for item pairs using item response theory. Journal of Educational and Behavioral Statistics. 1997;22(3):265–289. doi: 10.3102/10769986022003265. [DOI] [Google Scholar]
- 90.van der Ark LA. Mokken scale analysis in R. Journal of Statistical Software. 2007;20(11):1–19. doi: 10.18637/jss.v020.i11. [DOI] [Google Scholar]
- 91.Mokken RJ. A theory and procedure of scale analysis: With applications in political research. Reprint. New York: De Gruyter Mouton; 2011. [Google Scholar]
- 92.Gwet KL. Handbook of inter-rater reliability: The definitive guide to measuring the extent of agreement among raters. 4. Gaithersburg: Advanced Analytics, LLC; 2014. [Google Scholar]
- 93.Kuhn M, Johnson K, Modeling AP. Applied predictive modeling. New York: Springer; 2013. [Google Scholar]
- 94.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9(2):233–255. doi: 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- 95.Campbell-Sills L, Forde DR, Stein MB. Demographic and childhood environmental predictors of resilience in a community sample. Journal of Psychiatric Research. 2009;43(12):1007–1012. doi: 10.1016/j.jpsychires.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 96.Jeste DV, Savla GN, Thompson WK, Vahia IV, Glorioso DK, Martin AS, Palmer BW, Rock D, Golshan S, Kraemer HC, Depp CA. Association between older age and more successful aging: Critical role of resilience and depression. American Journal of Psychiatry. 2013;170(2):188–196. doi: 10.1176/appi.ajp.2012.12030386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Seifer DB, Petok WD, Agrawal A, Glenn TL, Bayer AH, Witt BR, Burgin BD, Lieman HJ. Psychological experience and coping strategies of patients in the Northeast U.S. delaying care for infertility during the COVID-19 pandemic. Reproductive Biology and Endocrinology. 2021 doi: 10.1186/s12958-021-00721-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dale S, Cohen M, Weber K, Cruise R, Kelso G, Brody L. Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS Patient Care and STDS. 2014;28(3):136–143. doi: 10.1089/apc.2013.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zager Kocjan G, Kavčič T, Avsec A. Resilience matters: Explaining the association between personality and psychological functioning during the COVID-19 pandemic. International Journal of Clinical and Health Psychology. 2021;21(1):100198–100198. doi: 10.1016/j.ijchp.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: Assessing the ability to bounce back. International Journal of Behavioral Medicine. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 101.Teng Y, Brannick MT, Borman WC. Capturing resilience in context: development and validation of a situational judgment test of resilience. Human Performance. 2020;33(2–3):74–103. doi: 10.1080/08959285.2019.1709069. [DOI] [Google Scholar]
- 102.Stein MB, Campbell-Sills L, Gelernter J. Genetic variation in 5HTTLPR is associated with emotional resilience. American Journal of Medical Genetics Part B - Neuropsychiatrics Genetics. 2009;150B(7):900–906. doi: 10.1002/ajmg.b.30916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Davidson RJ, McEwen BS. Social influences on neuroplasticity: Stress and interventions to promote well-being. Nature Neuroscience. 2012;15(5):689–695. doi: 10.1038/nn.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.McCanlies EC, Mnatsakanova A, Andrew ME, Burchfiel CM, Violanti JM. Positive psychological factors are associated with lower PTSD symptoms among police officers: Post Hurricane Katrina. Stress and Health. 2014;30(5):405–415. doi: 10.1002/smi.2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data from this study are strictly protected by privacy and confidentiality agreements specified in the study protocol that was approved by the institutional review board.
Samples of the kind of software syntax that was utilized in the quantitative analyses can be requested from the corresponding author. All requests will be subject to vetting by the institutional review board prior to dissemination.