Abstract
OBJECTIVE:
Although many studies have identified risk factors for adolescent pregnancy, much less is known about factors that support pregnant adolescents’ psychological wellbeing and offspring outcomes. This study drew on strength-based frameworks to investigate family and neighborhood factors linked to social connectedness that predict psychological wellbeing during adolescent pregnancy and offspring outcomes.
METHOD:
Participants included 135 adolescent mothers (ages 14–21; 90% Black American) assessed annually since childhood as part of a longitudinal study. During preadolescence (ages 11–13), data on contextual stressors and neighborhood support were gathered from participants’ caregivers; participants also rated their perceived trust/attachment with caregivers before and during pregnancy. To assess changes in psychological wellbeing, adolescents reported positive and depressed mood before and during pregnancy. A path analysis model tested the prospective associations between family and neighborhood factors, psychological wellbeing during pregnancy, and offspring outcomes (birth outcomes; observed infant positive/negative emotions at age 3-months).
RESULTS:
Positive mood decreased from pre-pregnancy to pregnancy, whereas depressed mood remained stable. Adjusting for pre-pregnancy mood, perceived caregiver trust/attachment during pregnancy was associated with prenatal positive mood. Prenatal positive mood, in turn, reduced risk of preterm birth and indirectly predicted positive infant emotions via birth outcomes. Neighborhood support in preadolescence predicted lower prenatal depressed mood, but depressed mood did not predict infant outcomes beyond positive mood. Contextual life stress was not associated with prenatal mood after adjusting for family and neighborhood support.
CONCLUSIONS:
Findings highlight changes in positive-valence emotions during adolescent pregnancy that may have unique associations with birth outcomes and offspring emotions.
Keywords: adolescent mothers, prenatal mental health, psychological wellbeing, birth outcomes, infant emotion
Although adolescent pregnancy has decreased in recent years, the United States continues to have one of the highest rates among industrialized countries (Sedgh et al., 2015), with 171,674 live births reported to 15–19-year old mothers in 2019 (16.7 per 1,000) (Martin et al., 2021). Childbirth before age 20 is associated with multiple psychological, biological, and social consequences for young mothers and their offspring, outcomes that are compounded by adolescent mothers’ disproportionate exposure to contextual life stressors (Logsdon et al., 2016). Indeed, adolescent mothers are more likely than mothers of other age groups to grow up in under-resourced communities and have a history of family exposure to contextual life stressors, including financial and housing difficulties and exposure to violence (Uzun et al., 2013). These effects are further heightened for young Black women who systematically experience greater exposure to these contextual life stressors due to discrimination and institutional racism, which contributes to health inequities during the sensitive pregnancy period (Gee et al., 2012; Orchard & Price, 2017; Pearl et al., 2018). Indeed, rates of low birth weight and preterm birth among Black American women are approximately twice that of non-Hispanic White women (Martin et al., 2021). These racial disparities in birth outcomes are linked to systematic differences in exposure to life stressors that often begin before conception (Almeida et al., 2018; Kramer et al., 2011).
According to the developmental origins of health and disease theory and related lifespan models of pregnancy health (Barker, 2004; Lu & Halfon, 2003; Misra et al., 2003), frequent maternal exposure to life stressors before and during pregnancy increases risk for adverse birth outcomes in part by heightening mothers’ psychological distress during pregnancy (Hodgkinson et al., 2014; Siegel & Brandon, 2014). High levels of psychological distress during pregnancy, in turn, have been linked to increased risk for adverse birth outcomes (e.g., prematurity, low birthweight; Marvin-Dowle & Soltani, 2020) as well as heightened infant negative emotionality (Nolvi et al., 2016), both of which are linked to a broad range of emotional and behavioral difficulties across the lifespan (Beauchaine & Cicchetti, 2019). Thus, frequent exposure to contextual life stressors is theorized to be a major pathway through which stress-related disparities in health are transmitted across generations (Pearl et al., 2018). This cycle of risk systematically impacts young Black mothers living in under-resourced contexts whose experiences of life stress are magnified due to the intersection of systemic racism with the unique psychosocial stressors associated with adolescent pregnancy. Identifying modifiable factors that promote psychological health during pregnancy specifically for adolescent mothers is an important step to informing preventative interventions to improve birth outcomes for the children of young mothers.
Psychological Wellbeing During Adolescent Pregnancy
To date, most studies of adolescent mothers, and of young Black mothers in particular, have used a ‘deficit lens’ to investigate risk factors linked to maternal and offspring outcomes (Brand et al., 2014; Savio Beers, 2012). However, many young mothers have positive birth outcomes and emotionally healthy infants despite disproportionate exposure to contextual life stressors (Hodgkinson et al., 2014); these resilient pathways have received less empirical attention. Importantly, leading scholars in Black Psychology have long pushed for strength-based perspectives (Bethea, 2020). Dr. Joseph White, a pioneer in the field of Black Psychology, emphasized the importance of expanding beyond risk factors to investigate psychological strengths (White, 1984). These psychological strengths are conceptualized as resilience resources that are necessary for Black Americans to sustain wellbeing in the face of adversity, oppression, and social inequities (Myers et al., 2018; White, 1984). The emphasis on psychological strengths and wellbeing is also reflected in the emergence of Positive Psychology theories that focus on factors that enable humans to thrive (Seligman & Csikszentmihalyi, 2000). For example, in line with the resilience framework in theories from Black Psychology, the broaden-and-build theory of positive emotions posits that increases in positive emotions can buffer life stress and promote restoration of health by broadening the scope of attention, enhancing cognitive processing of information, and buffering autonomic arousal generated by negative emotions (Fredrickson, 2001). Indeed, positive emotions such as joy, pride, and self-assurance have been linked to faster cardiovascular recovery following negative mood inductions (Tugade & Fredrickson, 2004). In a sample of Black, Latinx, and Asian American young adults, positive affect also buffered psychological reactivity to racism (Ong & Edwards, 2008), results that support the need to take a strength-based perspective to interrupt developmental pathways of stress transmission for young mothers of color.
Drawing from these strength-based frameworks, the goal of this study is to expand on existing research on adolescent pregnancy by focusing on factors that predict prenatal psychological wellbeing and positive birth outcomes. In particular, we focus on subjective levels of psychological wellbeing including positive emotions such as joy, pride, and feelings of calm as well as the absence of self-reported distress such as depressed mood. Although most work on prenatal mental health has focused on psychological distress (e.g., depression), emerging research from adult samples suggests that psychological wellbeing during pregnancy, such as positive mood, can have unique protective effects on birth outcomes and infant emotional health (Voellmin et al., 2013). Given that positive emotions are known to have beneficial effects on neuroendocrine, autonomic, and immune system functioning and subsequent health outcomes (Dockray & Steptoe, 2010), positive emotions during pregnancy may play an important role in promoting positive birth and offspring outcomes among pregnant adolescents exposed to frequent life stressors, a hypothesis that has yet to be tested. One study of 41 adult pregnant women showed that positive mood, but not depressed mood, was uniquely associated with lower cortisol awakening response (Cheng & Pickler, 2010). These findings suggest that positive moods may have unique effects on stress regulation during adolescent pregnancy, which could have important implications for strength-based approaches to supporting positive birth outcomes for young pregnant women living with contextual life stress.
Patterns of psychological wellbeing among pregnant adolescents likely differ from those of adult women because of the unique social circumstances of adolescent pregnancy. For young Black mothers, this can be further exacerbated by racism-related stressors (e.g., heightened experiences of stigma driven by negative racial stereotypes). From a developmental perspective, most pregnancies during adolescence are unintended and many girls who become pregnant report increased feelings of depression and social isolation (Kirisits & Kirchengast, 2013; Logsdon et al., 2016), although few studies have measured these emotions prospectively across time. One example is a study of first-time, Black adolescent mothers living with low income recruited from urban hospitals and followed for two years. Significant individual differences in postpartum depressed mood were observed across the postpartum period (Ramos-Marcuse et al., 2010), suggesting that changes in emotional wellbeing during adolescent pregnancy cannot be generally characterized as suboptimal. Moreover, few studies measure emotional health prior to childbirth or include positive emotions, despite their potentially unique effects on offspring outcomes. Studies with longitudinal data collected prior to pregnancy are needed to understand how changes in positive and negative mood during the transition to adolescent pregnancy influence birth outcomes and infant emotional health.
Family and Neighborhood Connectedness as Predictors of Psychological Wellbeing During Pregnancy
Whereas many contextual factors have been shown to increase the likelihood of becoming pregnant during adolescence, much less is known about factors that support adolescent mothers and their infants to thrive (Savio Beers, 2012). Drawing from a strength-based framework, we improve upon prior prenatal research by investigating a range of malleable contextual factors linked to psychological wellbeing during pregnancy. In addition to contextual life stressors measured before pregnancy that have been implicated in racial disparities in birth outcomes (Almeida et al., 2018), we include strength-based factors in the home and neighborhood settings. We focus on factors linked to a sense of social connectedness, including interpersonal relationships in the family context and community collectivism/collective efficacy in the neighborhood context. These family and neighborhood strengths in connectedness are psychosocial resources, linked to an Afrocentric worldview, that have been theorized as critical to building resilience in the face of oppression for Black Americans (Bethea, 2020; White, 1984). Thus, we designed this study based on a conceptual framework that, for pregnant adolescents with a history of contextual life stress, a strong sense of connectedness and support in the home and community setting may serve as critical psychosocial strengths for building psychological resilience to stress during the transition to early motherhood.
First, to measure connectedness in the home context, we focus on adolescent mothers’ trust and attachment with their own mothers. Pregnant adolescents are unique from adult women in their typical family context, such that most adolescent mothers are still living with their own caregiver(s) when they become pregnant. Because these young women are developing adolescents themselves, caregivers can play a critical role in facilitating adolescents’ psychological responses to pregnancy and childbirth. For example, perceived family support is linked to lower risk for postpartum depression (Brown et al., 2012; Logsdon et al., 2005). Similarly, one study of 395 pregnant adolescents found that negative expectations of how pregnancy would impact life led to increased prenatal depression, which contributed to lower perceived quality of life during pregnancy; however, this association was attenuated by adolescents’ satisfaction with the level of social support received from their own mothers (Pires et al., 2014). These findings suggest that a strong sense of connectedness with a caregiver may help to buffer the negative impact of pregnancy-related stress on adolescent psychological wellbeing during pregnancy. Importantly, pregnancy itself can have a significant impact on the relationship between an adolescent and her mother, and perceived trust and attachment can vary depending on the nature of their relationship before pregnancy (Bojczyk et al., 2010). Qualitative studies of Black and Latinx adolescent mothers living in under-resourced neighborhoods suggest that while some adolescents report increased family conflict, others experience increased closeness and improved communication with their mothers during this transition to motherhood (Lloyd, 2004; Paskiewicz, 2001). To our knowledge, no quantitative studies have examined how a sense of connectedness, trust, and attachment with a caregiver impacts adolescent mothers’ psychological wellbeing during pregnancy and her offspring’s developmental outcomes.
The second psychosocial factor we examined that is linked to the strength of connectedness is the family’s perception of neighborhood support or collective efficacy, a sociocultural resource that reflects a strength of community collectivism. Prior studies suggest that community-level stress and violence may elevate adolescents’ risk for emotional distress during pregnancy (Tzilos et al., 2012; Willie et al., 2016). However, neighborhoods also vary widely in their responses to community stressors depending on their level of collective efficacy, such as the likelihood that neighbors intervene or protect others who experience a problem or threat (Bellair & Browning, 2010; Sampson et al., 1997). Growing up in a community with a strong sense of neighborhood support is associated with psychological wellbeing and academic outcomes among children and adolescents (Prince et al., 2019; Rose et al., 2019; Tan et al., 2017). In addition, neighborhood collective efficacy is associated with greater life satisfaction and has been shown to buffer the association between race-related stressors and life satisfaction among Black Americans (Driscoll et al., 2015). Few studies have examined neighborhood support/collective efficacy in relation to pregnancy health and birth outcomes. In one sample of adult women, perceived support from neighbors was linked to higher offspring birthweight; however, this association was only significant for White (vs. Black) women after accounting for economic disparities (Buka et al., 2003). Although no studies to our knowledge have examined these associations among adolescent mothers, growing up with high levels of support and collective efficacy in the neighborhood context may be a particularly relevant sociocultural resource for young Black mothers living in under-resourced neighborhoods given their systematically elevated exposure to contextual life stressors (Mitchell et al., 2010).
The Present Study
The present study used a strength-based framework embedded in a prospective longitudinal study to achieve three aims. First, in a sample of predominantly Black adolescent mothers interviewed annually since childhood, we characterized changes in psychological wellbeing (positive and depressive mood) from two years pre-pregnancy to year of pregnancy. Next, we identified family and neighborhood factors that predicted adolescent psychological wellbeing during pregnancy, including a history of contextual life stressors (e.g., family financial and housing difficulties, neighborhood violence), as well as positive resources linked to social connectedness (i.e., having a trusting and close relationship with a caregiver and perceived support from neighbors). Finally, we examined the associations between psychological wellbeing during pregnancy and birth outcomes and infant emotional health.
We expected psychological wellbeing to show stability in the years prior to pregnancy but decrease during the year of adolescent pregnancy, reflecting the heightened stress experienced by young mothers – particularly young Black mothers – during adolescent pregnancy. We hypothesized that greater history of exposure to contextual life stressors would predict higher depressed mood and lower positive moods during pregnancy, whereas a history of neighborhood support and greater perceived trust/attachment with a caregiver during the transition to pregnancy would predict more positive psychological adjustment to pregnancy. Adolescents with higher positive mood and lower depressed mood during pregnancy, in turn, were hypothesized to have offspring with positive birth outcomes (higher birthweight, later gestational age at birth) and higher positive and lower negative infant emotions observed at 3-months of age.
Methods
Participants and Procedure
Participants were drawn from the Pittsburgh Girls Study (Hipwell et al., 2002; Keenan et al., 2010), a racially diverse sample of 2,450 girls initially recruited in childhood based on a stratified, random sampling of 103,238 households that oversampled low-income neighborhoods. Participants have been assessed annually over the past 20 years with high retention (range: 97% to 86%). Starting at age 11, annual assessments included questions about pregnancy and childbirth. Pregnant participants were then approached for recruitment into one of two sub-studies with parallel assessment batteries: Teen-Mother study (< age 18) or Mother-Baby study (age 18+). Adolescents who agreed to participate in a sub-study reported on birth outcomes and completed a postnatal assessment when their infant was 3-months old, including a mother-infant interaction task in the laboratory (described below). All procedures were approved by the University of Pittsburgh’s Institutional Review Board (IRB). We obtained written informed consent from caregivers and verbal assent from girls through age 17; participants provided written informed consent from age 18 onwards.
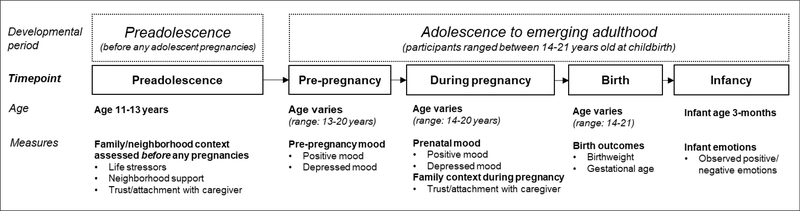
The present analysis included 135 first-time adolescent mothers who completed an annual interview during pregnancy and participated in one of the postnatal sub-studies with their infant at 3-months of age (Figure 1). Participants ranged in age from 14–21 years of age (mean = 18.32 years old). Almost all participants (90%) identified as Black or Black and another race, and 10% identified as White. At age 11 (the first timepoint of data for the current analyses), 50% of families were receiving public assistance (e.g., WIC, food stamps, welfare), 57% of adolescents were living in a single parent household, and 24% of adolescents’ caregivers reported less than 12 years of education. Measures collected during preadolescence (age 11–13; before any adolescent pregnancies), the two years immediately before pregnancy (varying by age across participants), and during pregnancy (varying by age across participants) were drawn from data available from annual interviews in the larger longitudinal Pittsburgh Girls Study (see Supplemental Table S1). Birth outcome data and observationally coded measures of infant emotions were collected as part of the pregnancy sub-studies described above. Participants varied across trimester of pregnancy during their prenatal interview: 26.7% in their first trimester, 40.7% in second trimester, and 32.6% in third trimester. Ratings of positive and depressed mood did not differ by trimester of assessment (all p’s > .10). On average, the time elapsed between the pre-pregnancy and pregnancy time points was 0.96 years (range = 0.56–2.68 years). Differences in the timing of the pre-pregnancy interview was not correlated with any of the mood variables before or during pregnancy (all p’s > .10).
Figure 1.
Variables included across the study timepoints.
Note. Due to the assessment schedule of the original longitudinal study (see Supplemental Table S1), two of the contextual measures (life stressors and neighborhood support) were not available during pregnancy for most participants, and thus only trust/attachment with caregiver was able to be examined during pregnancy.
Measures
Positive mood before and during pregnancy.
During the two years before pregnancy and the year of pregnancy, adolescents completed an abbreviated version of the Positive and Negative Affect Schedule (PANAS; Crawford & Henry, 2004), including items about joviality (8 items; α range=.92-.93 across three time points; e.g., “happy,” “joyful”), self-assurance (6 items; α=.79-.82; e.g., “proud,” “confident”), and serenity (3 items; α=.76-.80; e.g., “calm,” “relaxed”). Items were rated on a 5-point Likert scale (0=not at all to 4=extremely). These positive affect subscales were correlated (r=.55-.75) and summed into a positive mood score in each year.
Depressed mood before and during pregnancy.
Depressed mood during the two years before pregnancy and year of pregnancy were assessed using the Adolescent Symptom Inventory-4 (ASI-4) transitioning to the Adult Self-Report Inventory (ASRI-4; Gadow et al., 2004) at age 18. Participants reported on the severity of 11 depression symptoms (0=never to 3=all the time). Items were summed into a depression severity score at each year (α=.74-.86 across timepoints).
Contextual life stressors.
The Difficult Life Circumstances scale (DLC; Barnard, 1988) was administered to adolescents’ primary caregiver during preadolescence (ages 11–13; prior to any adolescent pregnancies). The DLC includes a 28-item (α=.63-.64) checklist of stressors commonly experienced in under-resourced communities, including financial and housing difficulties, exposure to community violence/crime, and domestic violence or interpersonal conflicts. Items were summed and then averaged across ages 11–13.
Perceived trust and attachment with caregiver.
To measure adolescents’ sense of social connection in the home, adolescents’ perceived trust and attachment with their primary caregiver was measured using the Inventory of Parent and Peer Attachment-Revised (IPPA-R; Armsden & Greenberg, 1987) in preadolescence (ages 11–13) and during pregnancy. Participants used a Likert scale (1=never true, 3=always true) to complete 9-items (α=.85-.90 range across time points) about their relationship, including perceived trust and the extent to which the adolescent perceives that her caregiver respects her feelings, and accepts, listens, and understands her. Items were summed to represent a greater perceived sense of connection, specifically trust and attachment, with their caregiver.
Neighborhood support.
To measure the family’s sense of social connection and collective efficacy in the community setting, questions about neighborhood context (Sampson & Raudenbush, 1999) were administered to participants’ primary caregiver during the preadolescent years prior to adolescent pregnancy (ages 11–13), including 4-items (α=.92-.94) related to neighborhood support or collective efficacy (e.g., How likely is it that one of your neighbors would do something about it if: “someone was breaking into your house in plain sight?” or “there was a fight in front of your house and someone was being beaten?”). Items were rated on a Likert scale (1=very unlikely to 4=very likely) and then summed and averaged across ages 11–13 to represent neighborhood support in preadolescence.
Infant birth outcomes.
Participants reported on their infant’s birthweight and gestational age at birth. Birthweight ranged from 1,714 to 4,450 grams (8.5% low birthweight, i.e., < 2,500 grams) and gestational age at birth ranged from 34 to 41 weeks (9.3% premature status, i.e., < 37 weeks). Birth outcomes were analyzed as continuous variables.
Infant emotional health.
When infants were 3-months old, they completed a laboratory assessment: mother-infant dyads were filmed during a 2-minute warm-up task followed by a 3-minute toy play task. The frequency and intensity of infant positive and negative emotional expressions were coded by two independent observers using time-sampled global ratings (Hipwell et al., 2019). Positive emotion was defined as smiling and laughter and negative as distress and fussiness, both of which were coded on a 5-point scale (1=none to 5=frequent/severe). Inter-rater reliability was determined by intra-class coefficients (ICCs) on a random sample of 28 mother–infant pairs (positive emotions ICC=.91, negative emotions ICC=.94). The positive and negative emotion codes were averaged across warm-up and toy play; a ratio of positive to negative emotion, with higher scores representing a greater proportion of positive to negative emotion, was used for analysis.
Data Analytic Plan
Analyses were conducted in Stata 13.0. To examine changes in positive and depressive mood from pre-pregnancy to pregnancy, we conducted repeated measures analysis of covariance (ANCOVA) models across three time points: two years before pregnancy (T-2), one year before pregnancy (T-1), and during pregnancy (T0). Next, we tested a path analysis model using the sem command to examine direct and indirect associations between psychosocial factors (life stressors, attachment with caregiver, neighborhood support), psychological wellbeing during pregnancy (positive and depressed mood), and offspring outcomes (birthweight, gestational age at birth, and observed infant emotionality at 3-months of age). Several variables were evaluated as potential covariates, including adolescent age, infant sex, and pre-pregnancy positive and depressed mood. Variables correlated with prenatal psychological wellbeing or infant outcomes (i.e., adolescent age, pre-pregnancy mood variables) were included in predictive models as covariates to increase specificity of effects. We evaluated models using standard fit indices (chi-square, RMSEA, CFI, TFI).
Rates of missingness across variables ranged from 0% to 20.7% (mean = 2.6% missing). Little’s test showed that data were missing completely at random (MCAR; χ2=59.66, p=.07) (Li, 2013; Little, 1988). To account for missing data and reduce parameter biases associated with listwise deletion, we used multiple imputation with 10 iterations prior to conducting the ANCOVA models. Full information maximum likelihood estimation was used to account for missing data in the path analysis model.
Results
Descriptive Statistics
Descriptive statistics and bivariate correlations among study variables appear in Table 1. Positive mood and depressed mood were modestly, inversely correlated during pregnancy, highlighting their independence. Greater perceived trust/attachment with caregiver in preadolescence and during pregnancy were correlated with higher positive mood and lower depressed mood during pregnancy. Life stressors was inversely correlated with neighborhood support during preadolescence, and it was also correlated with positive and depressed mood during pregnancy in expected directions. Positive mood during pregnancy was positively correlated with gestational age at birth, whereas depressed mood during pregnancy was correlated with a lower ratio of positive to negative infant emotion at 3-months of age.
Table 1.
Descriptive statistics and bivariate correlations among demographic and study variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| M(SD) or %: | 18.32 (1.67) | 90% | 4.16 (2.59) | 12.59 (2.61) | 24.11 (2.91) | 23.91 (3.6) | 3.33 (0.77) | 3.32 (0.72) | 3.18 (0.7) | 8.23 (4.87) | 7.3 (4.93) | 7.73 (4.28) | 53% | 39.01 (1.61) | 6.97 (1.14) | 1.95 (1.1) |
|
| ||||||||||||||||
| 1. Age at childbirth (years) | – | |||||||||||||||
| 2. Race (1=Black, 0=White) | −.13 | – | ||||||||||||||
| 3. Life stressors in preadolescence | −.02 | −.19* | – | |||||||||||||
| 4. Neighborhood support in preadolescence | .06 | −.25** | −.26** | – | ||||||||||||
| 5. Caregiver attachment in preadolescence | −.09 | .01 | <.01 | −.09 | – | |||||||||||
| 6. Caregiver attachment during pregnancy | .13 | −.01 | −.16 | .02 | .39** | – | ||||||||||
| 7. Positive mood: 2 years before pregnancy | −.19* | .13 | −.16 | −.07 | .37** | .12 | – | |||||||||
| 8. Positive mood: 1 year before pregnancy | −.11 | .06 | −.11 | −.05 | .29** | .22* | .53** | – | ||||||||
| 9. Positive mood: during pregnancy | .04 | .03 | −.18* | −.06 | .27** | .35** | .43** | .58** | – | |||||||
| 10. Depressed mood: 2 years before pregnancy | −.03 | −.03 | .14 | .04 | −.24** | −.27** | −.30** | −.16 | −.16 | – | ||||||
| 11. Depressed mood: 1 year before pregnancy | −.25** | −.03 | .21* | −.04 | −.24** | −.21* | −.29** | −.31** | −.21* | .36** | – | |||||
| 12. Depressed mood: during pregnancy | −.25** | .03 | .20* | −.20* | −.24** | −.29** | −.16 | −.15 | −.30** | .34** | .49** | – | ||||
| 13. Infant biological sex (1=male, 0=female) | −.07 | −.03 | .01 | .02 | −.01 | −.04 | .15 | −.08 | .04 | .05 | −.02 | −.03 | – | |||
| 14. Infant gestational age at birth (weeks) | .03 | .11 | −.12 | −.13 | .06 | −.03 | .06 | .07 | .22* | −.05 | −.05 | −.10 | .12 | – | ||
| 15. Infant birthweight (grams) | .01 | −.10 | −.03 | .02 | −.05 | .03 | −.07 | −.07 | .09 | −.07 | .06 | −.02 | .14 | .58** | – | |
| 16. Infant emotional health (positive-to-negative ratio) | .20* | .10 | −.04 | −.10 | −.03 | .09 | .04 | .02 | .03 | −.11 | −.28** | −.22** | −.08 | .12 | .16 | – |
Note.
p<.05
p<.01.
Changes in Psychological Wellbeing
Adjusting for adolescent mothers’ age, a significant effect of time was observed on changes in positive mood from two years pre-pregnancy to pregnancy (F=3.60, ηp2 = .03, p=.03). Post-hoc contrasts that used Bonferroni corrections to adjust for multiple comparisons revealed that on average, positive mood remained stable across the two pre-pregnancy time points (MD<.01, SE=.06, p=.99), but significantly decreased during the year of pregnancy (MD=−.14, SE=.06, p=.04). The effect of time on changes in depression severity was marginal (F=3.12, ηp2 = .03, p=.05). Post hoc contrasts that adjusted for multiple comparisons revealed that depression severity showed stability across the pre-pregnancy years (MD=−.92, SE=.47, p=.15) as well as in the transition to pregnancy (MD=.41, SE=.40, p=.94).
Predicting Prenatal Psychological Wellbeing and Infant Outcomes
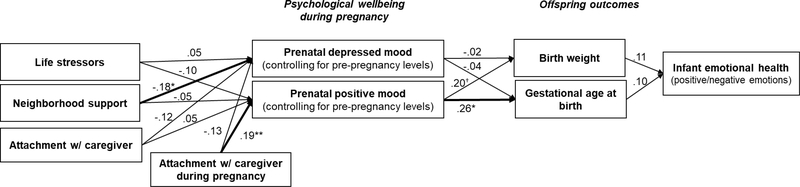
Figure 2 and Table 2 display the single path analysis model used to test associations between contextual factors, prenatal psychological wellbeing, and infant outcomes. Model fit was excellent (ꭓ2= 15.04, p=.38; RMSEA = .02, CFI = .99, TLI = .98). Controlling for pre-pregnancy mood variables, preadolescent attachment with caregiver was not associated with mood during pregnancy. However, attachment with caregiver during pregnancy was uniquely associated with higher levels of positive mood during pregnancy, above and beyond the effects of prior attachment in preadolescence, which highlights the specificity of these effects to the pregnancy period. Greater neighborhood support in preadolescence predicted lower depressed mood (but not positive mood) during pregnancy. Life stress during preadolescence was not associated with positive or depressed mood during pregnancy after accounting for caregiver attachment and neighborhood support.
Figure 2.
Path analysis model testing the direct and indirect associations between contextual factors, psychological wellbeing during pregnancy, and offspring outcomes. Model included adolescent age at childbirth and pre-pregnancy positive and depressed mood (measured the year before pregnancy) as covariates. Standardized coefficients of direct effects are shown. Significant effects are bolded for emphasis. †p<.10, *p<.05, **p<.01.
Table 2.
Primary direct and indirect associations tested in the path analysis model
| Variables | B (SE) | 95% CI | β | p |
|---|---|---|---|---|
|
| ||||
| Direct effects | ||||
| Life stressors in preadolescence → positive mood in pregnancy | −.03 (.02) | [−.02, .09] | −.10 | .15 |
| Neighborhood support in preadolescence → positive mood in pregnancy | −.01 (.02) | [−.05, .02] | −.05 | .43 |
| Caregiver trust/attachment in preadolescence → positive mood in pregnancy | .01 (.02) | [−.03, .05] | .05 | .55 |
| Caregiver trust/attachment in pregnancy → positive mood in pregnancy | .04 (.01) | [.01, .07] | .19 | .01 |
| Life stressors in preadolescence → depressed mood in pregnancy | .08 (.12) | [−.17, .32] | .05 | .54 |
| Neighborhood support in preadolescence → depressed mood in pregnancy | −.29 (.12) | [−.53, −.06] | −.18 | .02 |
| Caregiver attachment in preadolescence → depressed mood in pregnancy | −.18 (.12) | [−.41, .06] | −.12 | .14 |
| Caregiver attachment during pregnancy → depressed mood in pregnancy | −.15 (.09) | [−.34, .03] | −.13 | .10 |
| Positive mood in pregnancy → Infant gestational age at birth | .60 (.27) | [.08, 1.12] | .26 | .02 |
| Depressed mood in pregnancy → Infant gestational age at birth | −.01 (.04) | [−.10, .07] | −.04 | .72 |
| Positive mood in pregnancy → Infant birth weight | .33 (.18) | [−.03, .69] | .20 | .08 |
| Depressed mood in pregnancy → Infant birth weight | −.01 (.03) | [−.06, .05] | −.02 | .84 |
| Positive mood in pregnancy → Infant emotional health | −.13 (.17) | [−.46, .19] | −.08 | .43 |
| Depressed mood in pregnancy → Infant emotional health | −.02 (.02) | [−.07, .02] | −.09 | .34 |
| Infant gestational age at birth → Infant emotional health | .07 (.08) | [−.08, .22] | .10 | .36 |
| Infant birth weight → Infant emotional health | .11 (.10) | [−.09, .31] | .11 | .29 |
| Indirect effects | ||||
| Positive mood during pregnancy → infant emotional health (through birth outcomes: infant gestational age at birth and birth weight) |
.08 (.03) | [.01, .15] | .05 | .02 |
| Depressed mood during pregnancy → infant emotional health (through birth outcomes: infant gestational age at birth and birth weight) |
−.002 (.01) | [−.01, .01] | −.01 | .75 |
Note. B (SE) = unstandardized coefficient and standard error. 95% CI = 95% confidence interval for unstandardized coefficient. β = standardized coefficient. Significant effects (p < .05) are bolded for emphasis. All direct and indirect effects adjusted for adolescent age at childbirth and pre-pregnancy positive and depressed mood (measured the year before pregnancy) as covariates.
Adjusting for pre-pregnancy mood, positive mood during pregnancy predicted later gestational age at birth and marginally higher birthweight (Figure 2). Positive mood during pregnancy also demonstrated a small indirect effect on infant emotion via the total effects of the two birth outcomes (birthweight and gestational age) (B= −.078, SE=.034, p=.022, 95% CI [.011, .145]). However, neither birthweight nor gestational age had a specific direct effect (i.e., uniquely predicted) infant emotion. Adjusting for positive mood and other covariates, depressed mood during pregnancy did not predict birth outcomes or infant emotion, and the indirect association between prenatal depression and infant emotional health through birth outcomes was not significant (B=−.002, SE=.005, p=.751, 95% CI [−.012, .009]).
Discussion
In a longitudinal study of predominantly Black American adolescent mothers who have been prospectively interviewed since they were children, we investigated changes in psychological wellbeing prior to and during pregnancy. We also examined the prospective associations between adolescent mothers’ psychological wellbeing during pregnancy with subsequent birth outcomes and infant positive and negative emotions observationally coded at 3-months of age. Drawing from strength-based psychology theories that emphasize the importance of social connectedness and other psychosocial strengths for supporting resilience to adversity (White, 1984), we expanded on prior studies of adolescent mothers by investigating positive family and community factors as predictors of psychological wellbeing during pregnancy. Several findings emerged: First, on average, adolescents’ self-reported levels of positive emotion (e.g., joy, self-assurance) were stable during the two years prior to pregnancy and then significantly decreased during pregnancy, whereas depressed mood remained stable across all time points. These results suggest that the effects of adolescent pregnancy on emotional health may be more salient for positive than for negative valence systems. Second, an adolescent’s perceived sense of trust and attachment with her primary caregiver during pregnancy was uniquely associated with higher prenatal positive mood after controlling for these factors before pregnancy. Positive mood during pregnancy, in turn, predicted later gestational age at childbirth (and marginally higher infant birthweight), and also demonstrated a small indirect effect on infant emotional behavior at 3-months of age via these birth outcomes. Finally, greater perceived neighborhood support or collective efficacy in preadolescence (ages 11–13) predicted lower depressed mood during adolescent pregnancy, above and beyond the effect of life stressors and pre-pregnancy levels of depressed mood. However, depressed mood during pregnancy did not predict offspring outcomes after accounting for depressed mood the year before pregnancy and concurrent positive mood during pregnancy.
To date, most research on adolescent mothers has focused on prenatal depression and negative health outcomes; our findings highlight that there are also significant changes in positive emotion during this period that may be important targets for intervention. The decreases in positive mood specifically during the year of adolescent pregnancy is consistent with studies conceptualizing pregnancy as a developmentally-atypical stressful life event for adolescents (Logsdon et al., 2016). This is particularly important to consider for young Black mothers, who experience this transition in their lives in the context of a societal context characterized by significant discrimination and structural racism that exacerbates life stressors and contributes to racial disparities in birth outcomes (Rosenthal & Lobel, 2011). Indeed, racial stressors such as discrimination have been shown to increase specifically during pregnancy for Black women in part due to exposure to harmful negative stereotypes about Black girls and women regarding sexuality and motherhood (Rosenthal et al., 2014; Rosenthal & Lobel, 2016). Importantly, contextual life stress is often discussed in relation to negative valence emotions such as depressed mood, but there is also evidence that chronic forms of life stress including racism can blunt positive emotions over time (Priest et al., 2013). Given the unique role of positive emotions in coping processes and in buffering the effect of chronic stress on mental health (Folkman, 2008; Ong & Edwards, 2008), our findings highlight a need to better understand the correlates and patterns of changes in positive valence emotions during the transition to pregnancy, particularly among young Black mothers with a history of significant life stress.
Although we initially observed bivariate correlations between life stressors and both positive and depressed mood during pregnancy, these associations were no longer significant after accounting for positive family and neighborhood factors that reflect the psychosocial strength of social connectedness. These findings are consistent with strength-based theories from Black Psychology (White, 1984) as well as with Positive Psychology studies of positive emotions (Tugade & Fredrickson, 2004), which have highlighted the important role of positive emotions and social connectedness in family and community settings for promoting psychological wellbeing. For Black adolescents in particular, these psychological and psychosocial strengths have been framed as necessary resilience resources in the face of chronic oppression and racism (Bethea, 2020), but this conceptualization has not previously been extended to Black pregnant adolescents, despite their heightened experiences of stress during the perinatal period. Because our study drew from a larger longitudinal dataset that included adolescent mood and contextual measures collected prior to pregnancy, we were uniquely suited to investigate psychosocial factors measured in the pre-pregnancy period, which has implications for informing preventative care that aims to strengthen social connection in family and neighborhood contexts during pre-pregnancy periods (e.g., preadolescence). Interestingly, the types of contextual factors predicting positive mood during pregnancy differed from those predicting depressed mood. Specifically, neighborhood support in preadolescence predicted lower depressed mood during pregnancy, even after accounting for pre-pregnancy mood. Thus, a strong sense of collective efficacy and neighborhood support in the community setting may help to offset the effects of life stressors on depressed mood during adolescent pregnancy.
These findings align with studies demonstrating the inverse association between neighborhood support and depression symptoms among Black adolescents (Matlin et al., 2011). Our findings extend this work by demonstrating the high relevance of these early neighborhood-level sources of connection on young Black mothers’ depressed mood during the transition to pregnancy. These results also highlight the need studies of perinatal health to expand beyond the individual and family unit, given the potential protective effects of neighborhood-level support systems on prenatal mental health. Neighborhood cohesion and support have been linked to a greater sense of self-efficacy among Black adolescent girls, which may be partially mediated by a greater ability for parents and adults in the adolescent’s life to provide social support (Plybon et al., 2003). Future studies should test the extent to which neighborhood level protective factors influence family dynamics and pregnant adolescents’ sense of self-efficacy during the transition to motherhood. This work is particularly relevant for adolescent mothers, who disproportionately live in areas with high levels of community stress and may benefit from targeted neighborhood resources during the sensitive transitional pregnancy and postpartum periods.
Whereas neighborhood support was inversely associated with depressed mood during pregnancy, adolescents’ trust and attachment with their primary caregiver during pregnancy was uniquely associated with higher levels of positive valence emotions during pregnancy. These effects were significant beyond measures of caregiver attachment during preadolescence (age 11–13, i.e., developmental period before any pregnancies). Thus, our findings suggest that adolescents’ perceived feelings of trust and attachment with their caregiver specifically during the transitional pregnancy year may be associated with the maintenance of positive valence emotions during pregnancy, which has potential implications for offspring birth outcomes. Our results are consistent with meta-synthesis reviews of qualitative studies that highlight the importance of having a close and trusting relationship with a caregiver during pregnancy on adolescent mothers’ mental health outcomes (Clemmens, 2003). There is evidence that social support tailored to address racial discrimination is a more powerful buffer of racism-related stress for Black women then ‘general’ social support (Seawell et al., 2014). Given the unique forms of racialized and gendered stigma that Black women – particularly young Black mothers – can face, a strong feeling of social connectedness to family could help to buffer this stress. This may be particularly relevant for pregnant adolescent’s sense of connection with their own mothers, who may be uniquely placed to provide tailored support specific to the unique gendered and racialized experiences of young Black mothers. Importantly, our measure of caregiver trust/attachment was based on adolescent perceptions. Adolescents may vary in their disclosure about pregnancy with caregivers as well as how openly they discuss pregnancy-related topics in the family context. Thus, future studies are needed to investigate the different ways in which pregnant adolescents communicate with their caregivers about pregnancy during this transitional phase, which could mediate a positive sense of caregiver trust/attachment during pregnancy.
Consistent with emerging studies of adults, adolescents’ positive mood during pregnancy emerged as a unique predictor of birth outcomes, such that higher prenatal positive mood predicted later gestational age at birth and marginally higher birthweight, even after controlling for positive mood levels in the year before pregnancy. Prenatal positive mood (but not depressed mood) also indirectly predicted the ratio of positive-to-negative infant emotions at age 3-months via the total effect of the two birth outcomes. Note, however, that neither birthweight nor gestational age at birth had a significant independent effect on infant emotion, and the indirect effect of prenatal positive mood on infant emotional outcomes was relatively small. Thus, further investigation is needed to replicate this preliminary model with a larger sample and to explore a broader range of potential mechanisms that may help to explain potential indirect effects of positive mood during pregnancy on infant emotional health. Nevertheless, our findings are consistent with studies of adults highlighting the unique role of positive emotions during pregnancy on offspring birth outcomes (Voellmin et al., 2013). Importantly, because our study controlled for pre-pregnancy mood, our results suggest that it may specifically be within-person changes in positive mood from pre-pregnancy to pregnancy that contribute to birth outcomes rather than stable individual differences in positive emotions. Given that adolescent pregnancy can be considered a stressful life event, stability or increases in positive mood from pre-pregnancy to pregnancy could be conceptualized as more resilient responses to this life stressor. Indeed, positive emotions have been shown to have stress-buffering effects on neuroendocrine functioning (e.g., attenuated cortisol output; Dockray & Steptoe, 2010; Steptoe et al., 2005), physiological indices during pregnancy that can shape fetal development and early infant emotionality. Thus, positive mood during adolescent pregnancy may have protective downstream effects on offspring birth outcomes by helping to buffer fetal exposure to stress hormones, a hypothesis to be tested in future studies.
Although replication studies are needed, our findings add support to growing literature showing that maternal experiences of psychological wellbeing during pregnancy can have unique effects on birth outcomes and potentially indirectly shape the frequency of positive and negative emotions in infants. The implications of this work are particularly important for young Black mothers living in under-resourced contexts, given that their experiences of life stress during this transitional period are compounded by the additional effects of systemic racism and economic adversity. Studies of adolescent mothers – and young Black mothers in particular – have disproportionately centered on ‘deficit’ narratives. Our findings highlight the need for more strength-based approaches to informing mental health prevention and care during the pre-pregnancy, pregnancy, and postpartum periods. There are several ways in which strength-based frameworks can be integrated into existing prenatal care. For example, standard prenatal screenings and preventative mental health interventions often focus exclusively on prenatal depression or anxiety (Declercq et al., 2021; Kroenke, 2021). However, our findings suggest that it may be equally important to monitor the lack of or sudden decrease in positive emotions, as well as the availability of emotional support and connection in family and community settings. Particularly in the context of chronic exposure to racism and discrimination, the maintenance of positive valence emotions such as joy, relaxation, and pride and the maintenance of psychosocial strengths such as family and neighborhood connectedness may play an essential role in promoting stress resilience during the transitional perinatal period. Screening positive emotions and sources of emotional connection in family/neighborhood contexts as a standard part of prenatal care is an important first step to proactively increasing support and improving psychological wellbeing during pregnancy.
There are only a few strength-based prenatal intervention programs, several of which were adapted from broader Positive Psychology Interventions (Corno, Espinoza, et al., 2019). These interventions, which can be delivered in a modular online format to increase accessibility, aim to improve mental health wellbeing during the perinatal period by increasing positive emotions (e.g., gratitude, optimism) and social connectedness and support. Preliminary findings from pilot studies are promising, with evidence that strength-based interventions can have direct effects on both self-reported stress and physiological stress (e.g., cortisol) during pregnancy (Corno, Espinoza, et al., 2019; Corno, Molinari, et al., 2019; Matvienko-Sikar & Dockray, 2017). When designing prenatal interventions specifically for young Black mothers, it is important to intentionally attend to intersectional experiences such as gendered anti-Black discrimination and unique forms of stigma and stereotypes experienced by young Black mothers, which can impact psychological wellbeing and influence help-seeking behaviors (Belgrave et al., 2000; Nelson et al., 2020). As strength-based prenatal interventions continue to develop, there is a need to directly integrate culturally relevant strengths, such as positive racial and gender identity, culturally affirming socialization of Black girls and women, and Afrocentric cultural strengths such as communalism and spirituality, which could provide unique protective effects for young Black mothers during the prenatal and postpartum periods.
These results should be interpreted in the context of our study’s methodological limitations. First, although we improved upon prior cross-sectional studies by using a longitudinal design that included repeated measures of mood across time as well as measures prospectively collected prior to pregnancy, our study did not use experimental methods, thus precluding assertions about causality. Second, due to the availability of measures in the larger longitudinal study (Table S1), trust/attachment with caregiver was the only psychosocial factor that was able to be assessed both before and during pregnancy. Future studies that measure neighborhood support and life stress during pregnancy are needed to elucidate the precise timing effects of these variables. Third, our life stress measure was designed to provide an overview of overall contextual stressors commonly experienced by families living in under-resourced communities. Follow-up studies are needed to further investigate variability in the severity, duration, and type of stressors on psychological wellbeing during pregnancy. These studies would also be benefit from directly including race-based stressors, such as experiences of discrimination and microaggressions, particularly given that these specific forms of stress have been shown to increase during pregnancy for Black American women (Rosenthal et al., 2014). Information about prior or current receipt of psychological services is also important to consider in future studies, given that inequities in service usage and access may partly account for differences in psychological wellbeing during adolescent pregnancy.
Finally, it is important to note that psychological wellbeing during pregnancy, birth outcomes, and early differences in infant emotional health are influenced by multiple developmental pathways and contexts. Although our study did not have measures of the infant’s father, father involvement needs to be incorporated into future studies given their influence on young mothers’ psychological wellbeing during pregnancy. In addition, infant emotions continue to be shaped by the postnatal family environment (Perry et al., 2017). This may be particularly relevant for adolescent mothers who often live with their caregivers after childbirth. For example, grandparent involvement has been shown to influence parenting stress for adolescent mothers, although findings have differed based on family race-ethnicity and whether or not the grandparent is co-residing in the home (Greenfield, 2011). Adolescent mothers’ relationship quality with their own mothers has also been shown to influence observed parenting behaviors during parent-infant interactions (Sellers et al., 2011). Thus, follow-up studies are needed to explore how continued grandparent involvement influences mother-infant interactions and infant emotional development across multiple stages of development starting from the prenatal period.
Conclusions
Our findings highlight pregnancy during adolescence as an important transitional period characterized by changes in psychological wellbeing that may uniquely predict birth outcomes and early differences in offspring emotional health. Positive factors linked to community connectedness, such as neighborhood support, may serve as a protective factor for depression during adolescent pregnancy, whereas adolescents’ feelings of connection, trust, and attachment with their own caregivers were associated concurrently with more positive emotions during pregnancy. Furthermore, positive mood during pregnancy uniquely predicted birth outcomes and had a small indirect effect on early infant emotional health via these birth outcomes. Our results support the need for more studies that incorporate positive health and resilience frameworks to investigate family and neighborhood factors linked to positive mental health outcomes for pregnant adolescents, particularly young Black mothers whose experiences of stress during this transitional period are magnified by additional race-based stressors such as discrimination and institutional racism. This research will help inform the development of strength-based interventions that address the unique developmental needs of pregnant adolescents and their infants.
Supplementary Material
Funding Details and Acknowledgements:
This research was supported by grants from the National Institute of Mental Health (MH071790, MH056630) and the National Institute of Child Health and Development (HD067185). IT was supported by a postdoctoral training grant from the National Institute on Alcohol Abuse and Alcoholism (T32AA007453) and an early career development award from the National Institute of Mental Health (MH123505). Special thanks to the families of the Pittsburgh Girls Study for their participation in this research and to our dedicated research team for their continued efforts.
Footnotes
Disclosure Statement: All authors declare no competing or potential conflicts of interest.
References
- Almeida J, Bécares L, Erbetta K, Bettegowda VR, & Ahluwalia IB (2018). Racial/ethnic inequities in low birth weight and preterm birth: The role of multiple forms of stress. Maternal and Child Health Journal, 22(8), 1154–1163. 10.1007/s10995-018-2500-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armsden GC, & Greenberg MT (1987). The Inventory of Parent and Peer Attachment: Individual differences and their relationship to psychological well-being in adolescence. Journal of Youth and Adolescence, 16(5), 427–454. 10.1007/BF02202939 [DOI] [PubMed] [Google Scholar]
- Barker DJP (2004). The developmental origins of adult disease. Journal of the American College of Nutrition, 23(sup6), 588S–595S. 10.1080/07315724.2004.10719428 [DOI] [PubMed] [Google Scholar]
- Barnard K (1988). Difficult Life Circumstances scale. University of Washington, Seattle. [Google Scholar]
- Beauchaine TP, & Cicchetti D (2019). Emotion dysregulation and emerging psychopathology: A transdiagnostic, transdisciplinary perspective. Development and Psychopathology, 31(3), 799–804. 10.1017/S0954579419000671 [DOI] [PubMed] [Google Scholar]
- Belgrave FZ, Chase-Vaughn G, Gray F, Addison JD, & Cherry VR (2000). The effectiveness of a culture and gender-specific intervention for increasing resiliency among African American preadolescent females. Journal of Black Psychology, 26(2), 133–147. 10.1177/0095798400026002001 [DOI] [Google Scholar]
- Bellair PE, & Browning CR (2010). Contemporary disorganization research: An assessment and further test of the systemic model of neighborhood crime. Journal of Research in Crime and Delinquency, 47(4), 496–521. 10.1177/0022427810375578 [DOI] [Google Scholar]
- Bethea A (2020). Black Psychology: A forerunner of Positive Psychology. Psychology from the Margins, 2(1). https://ideaexchange.uakron.edu/psychologyfromthemargins/vol2/iss1/5 [Google Scholar]
- Bojczyk KE, Lehan TJ, McWey LM, Melson GF, & Kaufman DR (2010). Mothers’ and their adult daughters’ perceptions of their relationship. Journal of Family Issues. 10.1177/0192513X10384073 [DOI] [Google Scholar]
- Brand G, Morrison P, & Down B (2014). How do health professionals support pregnant and young mothers in the community? A selective review of the research literature. Women and Birth: Journal of the Australian College of Midwives, 27(3), 174–178. 10.1016/j.wombi.2014.05.004 [DOI] [PubMed] [Google Scholar]
- Brown JD, Harris SK, Woods ER, Buman MP, & Cox JE (2012). Longitudinal study of depressive symptoms and social support in adolescent mothers. Maternal and Child Health Journal, 16(4), 894–901. 10.1007/s10995-011-0814-9 [DOI] [PubMed] [Google Scholar]
- Buka SL, Brennan RT, Rich-Edwards JW, Raudenbush SW, & Earls F (2003). Neighborhood support and the birth weight of urban infants. American Journal of Epidemiology, 157(1), 1–8. 10.1093/aje/kwf170 [DOI] [PubMed] [Google Scholar]
- Cheng C-Y, & Pickler RH (2010). Maternal psychological well-being and salivary cortisol in late pregnancy and early post-partum. Stress and Health, 26(3), 215–224. 10.1002/smi.1285 [DOI] [Google Scholar]
- Clemmens D (2003). Adolescent motherhood: A meta-synthesis of qualitative studies. MCN: The American Journal of Maternal/Child Nursing, 28(2), 93–99. [DOI] [PubMed] [Google Scholar]
- Corno G, Espinoza M, & Maria Baños R (2019). A narrative review of positive psychology interventions for women during the perinatal period. Journal of Obstetrics and Gynaecology, 39(7), 889–895. 10.1080/01443615.2019.1581735 [DOI] [PubMed] [Google Scholar]
- Corno G, Molinari G, Espinoza M, Etchemendy E, Herrero R, Carrillo A, & Baños RM (2019). Applying Positive Psychology to prenatal care among women from different cultures: A web-based Positive Psychology intervention. In Van Zyl LE & Rothmann S Sr. (Eds.), Evidence-Based Positive Psychological Interventions in Multi-Cultural Contexts (pp. 269–287). Springer International Publishing. 10.1007/978-3-030-20311-5_12 [DOI] [Google Scholar]
- Crawford JR, & Henry JD (2004). The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. The British Journal of Clinical Psychology; Leicester, 43, 245–265. [DOI] [PubMed] [Google Scholar]
- Declercq E, Feinberg E, & Belanoff C (2021). Racial inequities in the course of treating perinatal mental health challenges: Results from listening to mothers in California. Birth (Berkeley, Calif.). 10.1111/birt.12584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dockray S, & Steptoe A (2010). Positive affect and psychobiological processes. Neuroscience & Biobehavioral Reviews, 35(1), 69–75. 10.1016/j.neubiorev.2010.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Driscoll MW, Reynolds JR, & Todman LC (2015). Dimensions of race-related stress and African American life satisfaction: A test of the protective role of collective efficacy. Journal of Black Psychology, 41(5), 462–486. 10.1177/0095798414543690 [DOI] [Google Scholar]
- Folkman S (2008). The case for positive emotions in the stress process. Anxiety, Stress, & Coping, 21(1), 3–14. 10.1080/10615800701740457 [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56(3), 218–226. 10.1037/0003-066X.56.3.218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J, & Weiss MD (2004). Adult Self-Report Inventory-4 Manual. Checkmate Plus. [Google Scholar]
- Gee GC, Walsemann KM, & Brondolo E (2012). A life course perspective on how racism may be related to health inequities. American Journal of Public Health, 102(5), 967–974. 10.2105/AJPH.2012.300666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA (2011). Grandparent involvement and parenting stress among nonmarried mothers of young children. Social Service Review, 85(1), 135–157. 10.1086/658395 [DOI] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, & Kroneman L (2002). Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health, 12(1), 99–118. 10.1002/cbm.489 [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Tung I, Northrup J, & Keenan K (2019). Transgenerational associations between maternal childhood stress exposure and profiles of infant emotional reactivity. Development and Psychopathology, 31(3), 887–898. 10.1017/S0954579419000324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgkinson S, Beers L, Southammakosane C, & Lewin A (2014). Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics, 133(1), 114–122. 10.1542/peds.2013-0927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, & McTigue K (2010). The Pittsburgh Girls Study: Overview and initial findings. Journal of Clinical Child and Adolescent Psychology, 39(4), 506–521. 10.1080/15374416.2010.486320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirisits K, & Kirchengast S (2013). Adolescent pregnancy outcome and the impact of social support—A pilot study from eastern Austria. Anthropologischer Anzeiger; Bericht Uber Die Biologisch-Anthropologische Literatur, 70(4), 439–453. 10.1127/0003-5548/2013/0349 [DOI] [PubMed] [Google Scholar]
- Kramer MR, Hogue CJ, Dunlop AL, & Menon R (2011). Preconceptional stress and racial disparities in preterm birth: An overview. Acta Obstetricia et Gynecologica Scandinavica, 90(12), 1307–1316. 10.1111/j.1600-0412.2011.01136.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K (2021). Two birds with one stone: Joint screening for perinatal depression and anxiety. Journal of Women’s Health (2002), 30(4), 455–456. 10.1089/jwh.2020.8643 [DOI] [PubMed] [Google Scholar]
- Li C (2013). Little’s test of missing completely at random. Stata Journal, 13(4), 795–809. [Google Scholar]
- Little RJA (1988). A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association, 83(404), 1198–1202. 10.1080/01621459.1988.10478722 [DOI] [Google Scholar]
- Lloyd SL (2004). Pregnant adolescent reflections of parental communication. Journal of Community Health Nursing, 21(4), 239–251. 10.1207/s15327655jchn2104_4 [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Birkimer JC, Simpson T, & Looney S (2005). Postpartum depression and social support in adolescents. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 34(1), 46–54. 10.1177/0884217504272802 [DOI] [PubMed] [Google Scholar]
- Logsdon MC, Monk C, & Hipwell AE (2016). Perinatal experiences of adolescent mothers. In The Oxford Handbook of Perinatal Psychology. Oxford University Press. http://www.oxfordhandbooks.com/view/10.1093/oxfordhb/9780199778072.001.0001/oxfordhb-9780199778072-e-008 [Google Scholar]
- Lu MC, & Halfon N (2003). Racial and ethnic disparities in birth outcomes: A life-course perspective. Maternal and Child Health Journal, 7(1), 13–30. 10.1023/A:1022537516969 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, & Driscoll AK (2021). Births: Final Data for 2019. National Vital Statistics Reports : From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 70(2), 1–51. [PubMed] [Google Scholar]
- Marvin-Dowle K, & Soltani H (2020). A comparison of neonatal outcomes between adolescent and adult mothers in developed countries: A systematic review and meta-analysis. European Journal of Obstetrics & Gynecology and Reproductive Biology: X, 6, 100109. 10.1016/j.eurox.2020.100109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matlin SL, Molock SD, & Tebes JK (2011). Suicidality and depression among African American adolescents: The role of family and peer support and community connectedness. The American Journal of Orthopsychiatry, 81(1), 108–117. 10.1111/j.1939-0025.2010.01078.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matvienko-Sikar K, & Dockray S (2017). Effects of a novel positive psychological intervention on prenatal stress and well-being: A pilot randomised controlled trial. Women and Birth, 30(2), e111–e118. 10.1016/j.wombi.2016.10.003 [DOI] [PubMed] [Google Scholar]
- Misra DP, Guyer B, & Allston A (2003). Integrated perinatal health framework: A multiple determinants model with a life span approach. American Journal of Preventive Medicine, 25(1), 65–75. 10.1016/S0749-3797(03)00090-4 [DOI] [PubMed] [Google Scholar]
- Mitchell SJ, Lewin A, Horn IB, Valentine D, Sanders-Phillips K, & Joseph JG (2010). How does violence exposure affect the psychological health and parenting of young African-American mothers? Social Science & Medicine (1982), 70(4), 526–533. 10.1016/j.socscimed.2009.10.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers LJ, Anderson M, Lodge T, Speight S, & Queener JE (2018). Optimal Theory’s contributions to understanding and surmounting global challenges to humanity. Journal of Black Psychology, 44(8), 747–771. 10.1177/0095798418813240 [DOI] [Google Scholar]
- Nelson T, Shahid NN, & Cardemil EV (2020). Do I really need to go and see somebody? Black women’s perceptions of help-seeking for depression. Journal of Black Psychology, 46(4), 263–286. 10.1177/0095798420931644 [DOI] [Google Scholar]
- Nolvi S, Karlsson L, Bridgett DJ, Korja R, Huizink AC, Kataja E-L, & Karlsson H (2016). Maternal prenatal stress and infant emotional reactivity six months postpartum. Journal of Affective Disorders, 199, 163–170. 10.1016/j.jad.2016.04.020 [DOI] [PubMed] [Google Scholar]
- Ong AD, & Edwards LM (2008). Positive affect and adjustment to perceived racism. Journal of Social and Clinical Psychology, 27(2), 105–126. 10.1521/jscp.2008.27.2.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orchard J, & Price J (2017). County-level racial prejudice and the black-white gap in infant health outcomes. Social Science & Medicine, 181, 191–198. 10.1016/j.socscimed.2017.03.036 [DOI] [PubMed] [Google Scholar]
- Paskiewicz LS (2001). Pregnant adolescents and their mothers. A shared experience of teen mothering. MCN. The American Journal of Maternal Child Nursing, 26(1), 33–38. 10.1097/00005721-200101000-00009 [DOI] [PubMed] [Google Scholar]
- Pearl M, Ahern J, Hubbard A, Laraia B, Shrimali BP, Poon V, & Kharrazi M (2018). Life-course neighbourhood opportunity and racial-ethnic disparities in risk of preterm birth. Paediatric and Perinatal Epidemiology, 32(5), 412–419. 10.1111/ppe.12482 [DOI] [PubMed] [Google Scholar]
- Perry RE, Blair C, & Sullivan RM (2017). Neurobiology of infant attachment: Attachment despite adversity and parental programming of emotionality. Current Opinion in Psychology, 17, 1–6. 10.1016/j.copsyc.2017.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pires R, Araújo-Pedrosa A, & Canavarro MC (2014). Examining the links between perceived impact of pregnancy, depressive symptoms, and quality of life during adolescent pregnancy: The buffering role of social support. Maternal and Child Health Journal, 18(4), 789–800. 10.1007/s10995-013-1303-0 [DOI] [PubMed] [Google Scholar]
- Plybon LE, Edwards L, Butler D, Belgrave FZ, & Allison KW (2003). Examining the link between neighborhood cohesion and school outcomes: The role of support coping among African American adolescent girls. Journal of Black Psychology, 29(4), 393–407. 10.1177/0095798403256892 [DOI] [Google Scholar]
- Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, & Kelly Y (2013). A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine, 95, 115–127. 10.1016/j.socscimed.2012.11.031 [DOI] [PubMed] [Google Scholar]
- Prince DM, Hohl B, Hunter BA, Thompson AB, Matlin SL, Hausman AJ, & Tebes JK (2019). Collective efficacy as a key context in neighborhood support for urban youth. American Journal of Community Psychology, 63(1–2), 179–189. 10.1002/ajcp.12311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Marcuse F, Oberlander SE, Papas MA, McNary SW, Hurley KM, & Black MM (2010). Stability of maternal depressive symptoms among urban, low-income, African American adolescent mothers. Journal of Affective Disorders, 122(1–2), 68–75. 10.1016/j.jad.2009.06.018 [DOI] [PubMed] [Google Scholar]
- Rose T, McDonald A, Von Mach T, Witherspoon DP, & Lambert S (2019). Patterns of social connectedness and psychosocial wellbeing among African American and Caribbean Black adolescents. Journal of Youth and Adolescence, 48(11), 2271–2291. 10.1007/s10964-019-01135-7 [DOI] [PubMed] [Google Scholar]
- Rosenthal L, Earnshaw VA, Lewis TT, Reid AE, Lewis JB, Stasko EC, Tobin JN, & Ickovics JR (2014). Changes in experiences with discrimination across pregnancy and postpartum: Age differences and consequences for mental health. American Journal of Public Health, 105(4), 686–693. 10.2105/AJPH.2014.301906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal L, & Lobel M (2011). Explaining racial disparities in adverse birth outcomes: Unique sources of stress for Black American women. Social Science & Medicine, 72(6), 977–983. 10.1016/j.socscimed.2011.01.013 [DOI] [PubMed] [Google Scholar]
- Rosenthal L, & Lobel M (2016). Stereotypes of Black American women related to sexuality and motherhood. Psychology of Women Quarterly, 40(3), 414–427. 10.1177/0361684315627459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson RJ, Raudenbush SW, & Earls F (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science, 277(5328), 918–924. 10.1126/science.277.5328.918 [DOI] [PubMed] [Google Scholar]
- Sampson R, & Raudenbush SW (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology. 10.1086/210356 [DOI] [Google Scholar]
- Savio Beers LA (2012). Through a different lens: Examining how we care for adolescent-headed families. American Journal of Public Health, 102(12), 2203–2205. 10.2105/AJPH.2012.300937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seawell AH, Cutrona CE, & Russell DW (2014). The effects of general social support and social support for racial discrimination on African American women’s well-being. Journal of Black Psychology, 40(1), 3–26. 10.1177/0095798412469227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedgh G, Finer LB, Bankole A, Eilers MA, & Singh S (2015). Adolescent pregnancy, birth, and abortion rates across countries: Levels and recent trends. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 56(2), 223–230. 10.1016/j.jadohealth.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman MEP, & Csikszentmihalyi M (2000). Positive Psychology: An introduction. American Psychologist, 55(1), 5–14. [DOI] [PubMed] [Google Scholar]
- Sellers K, Black MM, Boris NW, Oberlander SE, & Myers L (2011). Adolescent mothers’ relationships with their own mothers: Impact on parenting outcomes. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 25(1), 117–126. 10.1037/a0021877 [DOI] [PubMed] [Google Scholar]
- Siegel RS, & Brandon AR (2014). Adolescents, pregnancy, and mental health. Journal of Pediatric and Adolescent Gynecology, 27(3), 138–150. 10.1016/j.jpag.2013.09.008 [DOI] [PubMed] [Google Scholar]
- Steptoe A, Wardle J, & Marmot M (2005). Positive affect and health-related neuroendocrine, cardiovascular, and inflammatory processes. Proceedings of the National Academy of Sciences, 102(18), 6508–6512. 10.1073/pnas.0409174102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan TX, Wang Y, & Ruggerio AD (2017). Childhood adversity and children’s academic functioning: Roles of parenting stress and neighborhood support. Journal of Child and Family Studies, 26(10), 2742–2752. 10.1007/s10826-017-0775-8 [DOI] [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86(2), 320–333. 10.1037/0022-3514.86.2.320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzilos GK, Zlotnick C, Raker C, Kuo C, & Phipps MG (2012). Psychosocial factors associated with depression severity in pregnant adolescents. Archives of Women’s Mental Health, 15(5), 397–401. 10.1007/s00737-012-0296-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uzun AK, Orhon FS, Baskan S, & Ulukol B (2013). A comparison between adolescent mothers and adult mothers in terms of maternal and infant outcomes at follow-ups. The Journal of Maternal-Fetal & Neonatal Medicine: The Official Journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians, 26(5), 454–458. 10.3109/14767058.2012.733748 [DOI] [PubMed] [Google Scholar]
- Voellmin A, Entringer S, Moog N, Wadhwa PD, & Buss C (2013). Maternal positive affect over the course of pregnancy is associated with the length of gestation and reduced risk of preterm delivery. Journal of Psychosomatic Research, 75(4), 336–340. 10.1016/j.jpsychores.2013.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JL (1984). The psychology of Blacks: An Afro-American perspective. Prentice Hall. [Google Scholar]
- Willie TC, Powell A, & Kershaw T (2016). Stress in the city: Influence of urban social stress and violence on pregnancy and postpartum quality of life among adolescent and young mothers. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 93(1), 19–35. 10.1007/s11524-015-0021-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.