Abstract
Developing individuals and their families benefit from a warm and supportive relationship that fosters the development of good self-regulatory skills in the child needed for a host of positive developmental outcomes. Children and parents face special challenges to self-regulation when faced with a child’s chronic illness. A developmental model is presented that traces how positive parental involvement is coordinated with a child’s self-regulation skills (regulation of cognition, emotion, and behavior) that are essential for positive health management. This involves different temporal patterns of coordination of child and parent (and other close relationships) that lead to accumulating regulatory developments that afford benefits for managing illness. This process begins early in infancy through attachment and develops into childhood and adolescence to involve the coordination of parental monitoring and child disclosure that serves as a training ground for the expansion of social relationships beyond the family during emerging adulthood. The specific case of families dealing with type 1 diabetes is used to illustrate the transactional and dynamic nature of parent-child coordination across development. We conclude that a developmental model of parent-child coordination holds promise for understanding positive health outcomes and offers new methodological and statistical tools for the examination of development of both child and parent.
Keywords: Self-regulation, parent-child relationships, coordination, diabetes management, adolescence
The ability to effectively regulate one’s cognitions, behaviors, and emotions (i.e., self-regulation) is key to competent functioning across a broad array of indicators such as academic performance, social competence, psychological adjustment, and health (Eisenberg, Spinrad, & Eggum, 2010; Moffitt et al., 2011; Repetti, Taylor, & Seeman, 2002; Tangney, Baumeister, & Boone, 2004). Parents serve as an important resource for the development and maintenance of effective self-regulation (Belsky & Beaver, 2011), such that those who are warm and sensitive to children’s needs and monitor children’s activities provide a family context that models effective self-regulation and provides a scaffold for children’s developing cognitive and emotional abilities (Lengua, Honorado, & Bush, 2007; Morris, Silk, Steinberg, Myers, & Robinson, 2007). Self-regulatory skills developed in the family context (impulse control, emotion regulation) allow individuals to successfully navigate an expanding set of challenging contexts (e.g., drinking alcohol and driving, risky sexual practices) during late adolescence and early adulthood that increasingly lie outside of the purview of parents.
Developing individuals and their families may face especially difficult challenges to regulation when faced with chronic illness (e.g., diabetes, asthma, cancer; Compas, Jaser, Dunn, & Rodriguez, 2012; Modi et al., 2012). Nonnormative events such as chronic illness can be viewed as “experiments of nature” (Bronfenbrenner, 1977) that afford the opportunity to examine regulation under conditions of paramount adaptive significance and high stress for families. For example, the management of type 1 diabetes requires a complicated and intensive daily regimen of behaviors including repeated glucose testing and insulin injections. These behaviors must be managed in the face of daily negative emotions (Fortenberry et al., 2009) and cognitions such as perceptions of low self-efficacy and control that are offset by greater parental involvement (Berg et al., 2013; Berg et al., 2011; King, Berg, Butner, Butler, & Wiebe, 2014).
Although it is clear that parental involvement is beneficial for chronic illness management, the literature is somewhat fragmented with research focusing on different (albeit related) facets of parental involvement (e.g., support, parental monitoring, criticism) that facilitate or hinder a wide array of child self-regulatory characteristics (adherence behaviors, self-efficacy, self-control, emotion regulation, coping) relevant to health outcomes. Many of these child characteristics can be viewed as reflective of effective self-regulation (see Lansing & Berg, 2014). Further, this literature focuses on a specific direction of effects such that parental involvement presumably leads to enhanced chronic illness management through youth self-regulation skills. However, recent longitudinal research is supportive of the view that facets of parental involvement co-occur (e.g., high parental support co-occurs with low criticism), as do child self-regulation skills (e.g., high self-efficacy co-occurs with high adherence), and that these patterns of parental involvement and child characteristics are coordinated together (Helgeson et al., 2010; King et al., 2012; Luyckx & Seiffge-Krenke, 2009; Wiebe et al., 2014). That is, parents’ involvement changes together with youths’ self-regulation skills and illness management, mutually influencing each other across time.
In this article we present a developmental model of the coordinative process that exists between parents and children, a coordination that begins early in infancy and extends across the adult life span. Coordination is defined as the emergent temporal patterns between child and parent as they move together throughout time. This model draws on recent developmental theory that highlights the bi-directional nature of relationships between parents and children, whereby parenting not only affects the developing regulatory skills in the child, but these regulatory skills alter subsequent parenting as well (Hipwell et al., 2008; Pardini, Fite, & Burke, 2008). Our model captures these time-dependent relationships between child and parent as different forms of coordination.
In this paper, we highlight aspects of our model using type 1 diabetes as an example, as it is an illness that has daily regulatory challenges where parental involvement is beneficial. We first review the literature on parental involvement and illness management to demonstrate that there is existing evidence for the connection between positive facets of parental involvement (accepting relationship, monitoring, and behavioral involvement) and good adolescent self-regulation that facilitates management behaviors. Second, utilizing the broader developmental literature, we trace how this coordinative process begins early in infancy through attachment processes and develops across childhood, adolescence, and emerging adulthood. We also show that the coordinative process between parents and children serves as an important foundation for the development of new coordinations with close relationships outside of the family (Smetana, Campione-Barr, & Metzger, 2006). During adolescence especially, other relationships such as friends and romantic partners may enter into this coordinative process, as individuals solicit the instrumental and emotional support needed to manage chronic illness during young adulthood. Third, we illustrate how this model can identify forms of coordination across development and reduce the number of variables that are used to characterize these coordinative patterns. Finally, we conclude by noting the implications of the model for a life-span approach to chronic illness management, interventions for families, and the generalizability of our model beyond chronic illness into multiple domains of youth functioning. The model holds promise for a dynamic life-span perspective of the development of self-regulation skills within close relationships that views the parent-child relationship as setting the stage for the successful development of a larger coordinated system involving romantic partners and close friends as well as parents (Berg & Upchurch, 2007; Dinero, Conger, Shaver, Widaman, & Larsen-Rife, 2008; Nosko, Tieu, Lawford, & Pratt, 2011).
Developmental Model of Parent-Child Coordination for Self-Regulation Skills for Type 1 Diabetes Management
The Context of Type 1 Diabetes
We utilize the chronic illness of type 1 diabetes to illustrate the developmental model of parent-child coordination for illness management. Type 1 diabetes is a prevalent chronic illness affecting some 1 in 400 children (Mayer-Davis et al., 2009), caused by an autoimmune mediated deficiency of insulin secretion (Kaufman, 2012) by the pancreas. It is a serious illness that is associated with substantial decreases in longevity for those diagnosed during childhood (Pambianco et al., 2006). The goal of treatment is to achieve glycemic control that avoids both hypo- and hyper-glycemia. This is accomplished through adjusting the amount and timing of insulin together with multiple daily blood glucose tests (typically a minimum of 4 per day) as well as the timing and amount of food intake and the frequency and intensity of physical activity. Diabetes management, including adherence to this daily and demanding regimen, is crucial as it promotes better glycemic control, which substantially decreases potential long-term complications of the disease such as kidney problems, retinopathy, and cardiovascular disease (Hood, Peterson, Rohan, & Drotar, 2009; Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group, 2003). For example, maintaining good blood glucose control reduces long-term health complications such that a one percentage drop in HbA1c (a metric of how well blood glucose has been controlled over the past 3-4 months with higher numbers reflecting poorer control, e.g., 9%-8%) is associated with a 40% risk reduction of developing retinopathy (Hood, et al., 2009; Lachin, Genuth, Nathan, Zinman, & Rutledge, 2008).
To illustrate the daily self-regulation skills required of type 1 diabetes management for children and the coordination between children and parents, imagine a day in the life of an adolescent and his or her parents. The adolescent needs to test blood glucose at school, which involves adolescents’ self-regulation in planning to bring test supplies to school, dealing with negative emotions of feeling different because of one’s diabetes, and maintaining self-efficacy in the face of high blood glucose readings. The test may reveal a high blood glucose value, which then requires a calculation of the amount of insulin needed, depending on dietary information, and decisions as to whether to retest. Adolescents’ self-regulation skills are likely coordinated with numerous aspects of parental involvement. Parents’ knowledge and monitoring of their adolescents’ diabetes management may facilitate adolescents’ self-regulation: parents may remind their youth to take test supplies to school or bolster the adolescent’s efficacy that he or she can perform diabetes tasks at school. The manner in which adolescents’ and parents’ behaviors are coordinated may affect whether youth disclose, thereby affecting parents’ knowledge about such problems. For instance, parent-youth dyads or triads where parental negative affect is in direct relation with youth’s experience of problems may experience a pattern of low adolescent disclosure as adolescents begin to anticipate the negative repercussions of disclosing problems to their parents (Tilton-Weaver et al., 2010). Such blood glucose testing and adjustments in insulin and dietary intake take place multiple times each and every day for the person with diabetes and their parents.
Successful management behaviors (Modi, et al., 2012) such as checking blood glucose and adjusting insulin in response are especially difficult to maintain during adolescence (Bryden et al., 2001; Johnson et al., 1992; Morris et al., 1997; Rausch et al., 2012), but can be facilitated by parents’ greater involvement (Berg, et al., 2011; Ellis et al., 2007). A key tenant of our model is that facets of parental involvement (e.g., warmth, support) are coordinated with self-regulatory skills in the child together with illness management. Although the available body of literature in diabetes is only beginning to examine parent-child relationships as coordinative patterns (Butner, Berg, Baucom & Wiebe, 2014; Butner et al., in press), we use the literature to demonstrate linkages between multiple facets of parental involvement, adolescents’ self-regulatory skills and diabetes management.
Dynamic Approach to Self-Regulation and Parental Involvement
Better illness management (including adherence and metabolic control) during childhood and adolescence has been associated with a broad array of parental involvement measures including support, monitoring, criticism, behavioral involvement. We focus in this review (see Table 1) on three facets of parental involvement that have guided the study of parent-child interactions more broadly in developmental psychology (Beveridge & Berg, 2007; Dishion & McMahon, 1998) and diabetes more specifically (Palmer et al., 2011): high quality accepting parent-child relationships, which involve an accepting relationship characterized by parental responsiveness, warm communication and encouragement of autonomy (Miller-Johnson, et al., 1994; Skinner, John, & Hampson, 2000), monitoring, which involves regular contact with children regarding their daily activities, knowledge and supervision of those activities, and children disclosing to their parents so that they can be knowledgeable (Ellis et al., 2007; Stattin & Kerr, 2000), and behavioral involvement, which involves parents taking responsibility for diabetes management tasks (Anderson, Ho, Brackett, Finkelstein, & Laffel, 1997; Palmer et al., 2009; Wysocki & Gavin, 2006). The focus of research on parental involvement has largely been on mothers with a growing literature noting the important (and sometimes different) role played by fathers (Berg et al., 2013; Queen et al., 2016; Wysocki & Gavin, 2006). We highlight throughout the review aspects of parental involvement that may be different for mothers and fathers.
Table 1:
Studies of Parental Involvement, Self-Regulation, and Diabetes Management
| Authors | Sample | Design | Parental Involvement | Regulation of Behavior, Emotion, and Cognition |
Primary Findings |
|---|---|---|---|---|---|
| Anderson et al. (2002) | 104 youth (ages 8-17) with “short-duration” D (.5 to 6 years) and P | Cross-sectional | D responsibility; D-specific family conflict | Adherence Behaviors | P responsibility was [+] associated with adherence to BGM. Conflict was [−] associated with adherence to BGM and [+] with HbA1c. |
| Armstrong, Mackey, & Streisand (2011) | 84 youth (ages 9-11; M = 10.8, SD = .75) | Cross-sectional | Critical or negative (low quality) | Depressive symptoms (A), Self-efficacy (A) Adherence Behaviors |
Critical parenting was [+] associated with depression and [−] to self-efficacy, but not adherence or HbA1c . Depressive symptoms were [−] associated with self-efficacy and adherence, but not HbA1c . Self-efficacy mediated relationship between depressive symptoms and adherence. |
| Berg et al. (2011) | 252 youth with D (ages 10-14, M age=12.5) | Cross-sectional | M and F monitoring; parent-child relationship quality; P behavioral involvement in D management | Self-efficacy (A), Internalizing and externalizing behaviors (A) |
Relationship quality and monitoring related to adherence [+], HbA1c [−], self-efficacy [+], externalizing and internalizing [−]. Relationship quality→self-efficacy→ adherence. |
| Berg et al. (2013) | 180 youth (ages 10.50-15.58; M age = 12.87, SD = 1.53) and M (n=176) and F (n=139) |
Longitudinal (daily assessments across 14 days) | Parental persuasive strategies (e.g., “How much did you remind your child of the things he or she needs to do to manage his or her diabetes?”) | P confidence in adolescent’s ability to manage D | M persuasive strategies [−] associated with next day BG. M persuasive strategies [−] associated with next day confidence for A with high self-efficacy, [+] associated with next day confidence for A with low self-efficacy. |
| Berg et al. (2017) | 236 late adolescents (M age=17.76) | Cross-sectional Daily Diary |
Acceptance, Monitoring, Disclosure (A) | Adherence Behaviors Self-regulation failures |
Disclosure to M but not F associated with better daily adherence and fewer self-regulation failures. |
| Botello-Harbaum et al. (2008) | 69 youth (ages 11-16, M age = 13.3, SD = 1.7) |
Longitudinal (baseline, 12-month follow-up) | Authoritative parenting style (low quality): demandingness, responsiveness; D responsibility; D conflict. | Quality of Life | P responsiveness [+] associated with QOL at baseline and 12 months. D responsibility, D conflict, and demandingness not associated with QOL at either time point. |
| Butler, Skinner, Gelfand, Berg, & Wiebe (2007) | 78 youth (ages 11.58 – 17.42; M age = 14.21) and M | Cross-sectional | M psychological control, firm control, and acceptance | Depressive symptoms, Self-efficacy Adherence Behaviors |
Psychological control was [+] associated with A depression. A report of firm control was associated with A self-efficacy [+] and depressive symptoms [−] among older A. A report of M acceptance was associated with [−] depression and [+] with self-efficacy. M report of acceptance [+] associated with adherence. |
| Chisholm et al. (2011) | 40 youth (ages 2-8, M age = 6.57, SD = 1.63) | Cross-sectional | Quality of communication (combination of cohesion, expressiveness, and conflict); Behavioral control: a) commands, b) assigns responsibility | Internalizing and Externalizing Behaviors | Assign responsibility was associated [−] with % energy intake from sugars (NMES). When NMES consumption >10%, M quality of communication associated [−] to HbA1c. Command statements [+] correlated with externalizing symptoms. Assign responsibility statements [−] correlated with internalizing symptoms. |
| Davis et al. (2001) | 55 youth (ages 4-10; M age = 7.5, SD = 1.9) and a P |
Cross-sectional | Parenting style: a) warmth, b) restrictiveness, c) amount of control, d) physical punishment | Adherence Behaviors | Warmth alone was [+] associated with better adherence. No P measures were associated with HbA1c. |
| Drew et al. (2010) | 252 youth with D (ages 10-14; M age = 12.5) | Cross-sectional | Relationship quality | Extreme peer orientation (i.e., prioritizing peers over D management) Adherence Behaviors |
Relationship quality related to adherence [+], HbA1c [−], and extreme peer orientation [−]. Relationship quality →peer orientation→adherence, HbA1c. |
| Ellis et al. (2007) | 103 youth (ages 12-18; M = 14.8, SD = 1.7) |
Cross-sectional | Affective support for D; D and general monitoring | Adherence Behaviors | Monitoring (latent factor) was [+] associated with adherence, and indirectly [−] associated with HbA1c. |
| Hanna et al. (2011) | 118 late adolescents (range age 17-19) | Longitudinal | D Responsibility | Self-efficacy Worry about hypoglycaemia |
Greater youth D responsibility associated (+) with self-efficacy for those living independently, but (−) for those not living independently. |
| Hansen, Weissbrod, Schwartz, & Taylor (2012) | Parents (82 M and 43 F) of youth withD (ages 7-14) | Cross-sectional | P frequency and helpfulness of support for D management | Adherence Behaviors | F helpfulness associated with adherence [+]. |
| Helgeson et al. (2014a) | 112 youth with type 1 diabetes (M age=12) followed for 6 years | Longitudinal | P support and control | Adherence Behaviors Depressive Symptoms |
P control associated with lower depressive symptoms among those with type 1 diabetes. |
| Helgeson et al. (2014b) | 117 youth with type 1 diabetes and 122 without (M age=18.15 years) | Longitudinal | P support and control | Adherence Behaviors | P support associated with positive changes in adherence; parent control related to increases in depressive symptoms. Friend support buffered the negative effects of parent control on adherence |
| Helgeson, Reynolds, Siminerio, Escobar, Becker (2008) | 132 youth ages 10.73 – 14.21; M = 12.10) and a P | Longitudinal, across 3 time points (some cross-sectional results also reported) | D responsibility: a) % parent responsibility, b) % child responsibility, c) % shared responsibility | Depression, anxiety, anger, social competence, global self-worth, D self-efficacy | Shared responsibility (P-report) [+] associated with adherence. Shared responsibility (A-report) associated with HbA1c [−], self-efficacy [+], depressive symptoms [−], anger [−]. P responsibility (A-report) [+] associated with adherence. Child responsibility (A-report) associated with HbA1c [+], global self-worth [−], self-efficacy [−], and anger [+]. |
| Helgeson, Siminerio, Escobar, & Becker (2009) | 132 youth (ages 10.73-14.21; M = 12.10) | Longitudinal, across 4 time points, some cross-sectional findings reported | General relationship quality between P and A; P D-specific support | Depressive symptoms | Relationship quality [−] associated with HbA1c for girls only (Cross-Sectional). Depressive symptoms associated with HbA1c over time [+], but this association dissipated over time. |
| Helgeson, Snyder, Seltman, Escobar, Becker, & Siminerio (2009) | 132 youth (ages 10.73-14.21; M = 12.10) | Longitudinal across 5 years | Quality of parent relationship with M and F and emotional and instrumental support, friend support and conflict | Depressive symptoms, global self-worth | Deteriorating metabolic control trajectory associated [+] peer conflict and [+] poorer well-being. |
| Herzer, Vesco, Ingerski, Dolan, & Hood (2011) | 147 youth (ages 13-18; M age = 15.5, SD = 1.4 |
Longitudinal, across 3 time points | D-specific family conflict | Anxiety, Depressive symptoms | Conflict at baseline [+] associated with HbA1c at 9 months, Conflict →anxiety→HbA1c. |
| Hilliard et al. (2011) | 136 youth (ages 9-12; M = 10.5, SD = .9) | Cross-sectional | F “involvement (frequency and helpfulness of D- supportive behaviors) | Adherence Behaviors | F involvement [−] associated with HbA1c, but not with adherence. |
| Hilliard et al. (2012) | 257 youth (ages 11-14; M age = 12.8, SD = 1.2), P |
Cross-sectional | D monitoring, D-specific conflict, general family conflict | Adherence Behaviors | Monitoring [+] and conflict [−] associated with adherence, and (indirectly) with HbA1c . |
| Hilliard, Holmes et al. (2013) | 257 youth (ages 11-14, M age=12.8) | Cross-sectional | D monitoring and conflict | Adherence Behaviors | Conflict (+) and monitoring (−) independently associated with HbA1 through adherence behaviors. |
| Hilliard, Wu et al. (2013) | 150 youth (ages 13-18; M = 15.5, SD = 1.4) | Cross-sectional | D-specific family conflict | Depressive symptoms, Negative Affect (NA) related to BGM | Identified 3 trajectories of HbA1c, one trajectory representing those meeting their HbA1c treatment target, and others with HbA1c values exceeding recommended levels. Higher family conflict, depressive symptoms, and NA associated [−] to BGM and predicted poorer HbA1c trajectories. |
| Hilliard et al., (2014) | 136 families (M age=10.5) | Longitudinal | F involvement from M and F report. | Adherence Behaviors | Lower adherence was associated with increasing F involvement across time and higher F involvement associated with slower declines in adherence over time. |
| Hood, et al. (2007) | 202 youth (ages 8.2 – 18.7; M = 13.3, SD = 2.4, and P |
Cross-sectional | D family conflict | Negative affect (NA) responses to BGM results (A, P) | Conflict [+] associated with HbA1c. Conflict (A-report) associated with youth NA around BGM [+]. |
| Hsin, La Greca, Valenzuela, Moine, & Delamater (2010) | 111 youth (ages 10-17; M = 13.33, SD = 2.82) and a primary caregiver |
Cross-sectional | D responsibility, D “support” (i.e., frequency of supportive behavior x helpfulness of behavior) | Adherence Behaviors | Family support [+] associated with adherence. |
| Ingerski, Anderson, Dolan, & Hood (2010) | 147 youth (ages 13-18; M age = 15.5, SD = 1.4) |
Longitudinal | D responsibility, D conflict | Depressive symptoms, anxiety BGM frequency |
BGM frequency associated with P responsibility [+], D conflict [−]. P-reported child trait anxiety was [−] associated with BGM. Conflict [+] associated with HbA1c. |
| Iskander et al. (2015) | 217 youth (9-11 years) | Longitudinal | P negative and positive communication in interactions. | Adherence Behaviors | M positive communication predicted (+) adherence 3 years later. Changes in communication did not predict changes in HbA1c or adherence. |
| Jaser & Grey (2010) | 30 youth (ages 10-16; M = 12.6, SD = 1.6) and M | Cross-sectional | Ratings of a) hostility, b) parental influence, c) sensitive/child-centered, d) positive reinforcement during P-A interactions. | Depressive Symptoms | HbA1c associated with child-centered parenting [−], positive reinforcement [−], hostility [+], and parental influence [+]. M hostility associated with A depressive symptoms [+] and HbA1c [+]. Parental influence associated with child depression [+]. |
| King et al. (2012) | 252 youth (ages 10-14, M = 12.49, SD = 1.52) |
Longitudinal | M and F acceptance (relationship quality), D monitoring, and frequency of help | Behavioral self-control Externalizing Behaviors |
Better trajectories of HbA1c over time were associated with F monitoring [+], F frequency of help, behavioral self-control [+], extreme peer orientation [−], and externalizing behavior [−]. |
| King et al. (2013) | 252 youth (ages 10-14, M = 12.49, SD = 1.52) and 252 M and 188 F | Longitudinal |
M and F relationship quality, D monitoring, and behavioral involvement |
D Self-efficacy Adherence Behaviors |
M and F D monitoring and acceptance at baseline associated with less declines in adherence. Declines in M and F monitoring and acceptance predict declines in adherence. Tests of mediation indicated declines in M acceptance → less increase in self-efficacy → greater declines in adherence (A-report). Also, declines in maternal acceptance → less increase in self-efficacy → greater declines in adherence (A and M reports) |
| La Greca & Bearman (2002) | 74 youth (ages 11-18; M = 14.2, SD = 2.3) | Cross-sectional | D-specific support (frequency x helpfulness) | Adherence Behaviors | D-specific family support (frequency x helpfulness) was [+] associated with adherence, after controlling for family cohesion. |
| La Greca, Follansbee, & Skyler, 1990 | 40 youth w/ D (ages 7-17; M “Preadolescents” = 9.5; M “Adolescents” = 13.0) and M |
Cross-sectional | Transfer of responsibility from P to A Knowledge (Monitoring) of Diabetes |
Adherence Behaviors | Earlier transfer of responsibility [+] associated with HbA1c. M knowledge of D [+] associated with adherence of younger A. |
| Law et al. (2013) | 203 youth (M age=14.5 years) | Cross-sectional | Discrepancies in D responsibility | Perceived Consequences Dietary Self-efficacy |
HbA1c (+) associated with disagreements about responsibility and (−) with self-efficacy. |
| Lewandowski & Drotar (2007) | 51 youth (ages 13-18; M = 14.67, SD = 1.24) and M | Cross-sectional | M-A D conflict | Adherence Behaviors (A and M) | D conflict was [−] associated with adherence. |
| Luyckx et al. (2013) | 109 youth (M age=13.17 at baseline) | Longitudinal | P conflict | Internalizing and externalizing behaviors Adherence Behaviors |
Conflict with M and F associated with (−) adherence through (+) externalizing behaviors. |
| Main et al. (2014) | 118 youth (M age=12.74) | Cross-sectional | P acceptance and conflict | Depressive Symptoms Adherence Behaviors |
M and F acceptance associated (+) with adherence and conflict (−) with adherence and M conflict (+) with depressive symptoms. Conflict and adherence stronger associations among Caucasian rather than Latinos. |
| Main et al. (2015) | 247 late adolescents (M age=17.76) | Cross sectional | P monitoring, acceptance, disclosure, secrecy. | Externalizing Behaviors Adherence Behaviors |
M and F acceptance, monitoring, disclosure, (+) associated with adherence (−) to externalizing behaviors; secrecy associated (−) to adherence and (+) to externalizing behaviors. Externalizing behaviors (−) associated with adherence. |
| Miller & Drotar (2007) | 63 youth with D (ages 11-17, M = 13.3) and P | Cross-sectional | P-A communication and conflict | Adherence Behaviors | Parent-adolescent communication [+] associated with adherence. |
| Monaghan et al. (2015) | 134 children (ages=1 to 6) | Cross-sectional | P mealtime behaviors | Child’s problematic mealtime behaviors | More child problematic mealtime behaviors (+) associated with HbA1c. |
| Nansel, T., Rovner, A. J., Hayne, D., Iannottie, R. J., Simons-Morton, B., Wysocki, T., Anderson, B., Weissberg-Benchell, & Laffel, L. (2009) | 122 youth (M age=12) | Cross-sectional | Collaboration Parent Responsiveness and Demandingness, D Responsibility |
Adherence Quality of Life |
Collaboration was [+] associated with responsiveness, adherence, and quality of life. |
| Oris et al. (2015) | 228 youth (M age=13.9 years) | Longitudinal | P support | Internalizing Symptoms |
P support associated (−) internalizing symptoms and HbA1c. HbA1c and depressive symptoms especially high when low P support is combined with low friend support. |
| Ott et al. (2000) | 161 youth with D (ages 11-18, M = 13.97) | Cross sectional | P supportive and non-supportive behaviors | Self-efficacy for D management | Non-supportive behaviors→[−] Self-efficacy and [+] A non-adherence to BGM. |
| Palmer et al. (2004) | 127 youth with D (ages 10-15; M = 12.85) | Cross-sectional | M involvement in D care | Autonomy | HbA1c higher when parental involvement was low among adolescents with low autonomy. |
| Palmer et al. (2009) | 185 adolescents with D (ages 10-14, M=12.52), and 185 M and 145 F | Cross-sectional | P involvement in D care | Self-efficacy | P involvement [−] associated with self-efficacy. HbA1c higher when parental involvement was low among adolescents with low self-efficacy. |
| Patton, Piazza-Waggoner, Modi, Dolan, & Powers (2009) | 35 families of Youth with D (M = 5.6 years) | Cross sectional | Family functioning during mealtimes: Task Accomplishment and Behavioral Control | Affect management | Children’s dietary adherence [−] correlated with task accomplishment and behavioral control. Affect management [+] correlated with percentage of above-normal blood glucose levels. |
| Robinson et al. (2016) | 257 youth (ages 11-14) | Cross-sectional | Authoritative parenting, monitoring | Adherence Behaviors | More authoritative parenting and more monitoring were associated (+) with adherence. |
| Ronan et al. (2014) | 239 youth (ages 9-11) | Longitudinal | Family conflict | Executive Functioning, Adherence, Blood glucose monitoring | Higher family conflict and lower frequency of blood glucose monitoring associated with groups at elevated and high risk for poor HbA1c. |
| Skinner, et al. (2000) | 52 youth with D (ages 12-18; M = 15.2) | Longitudinal | General and D -specific family support | “Personal model” of D care | Family support [+] associated with adherence. Beliefs about effectiveness of D treatment regimens was [+] associated with dietary self-care. |
| Sweenie et al. (2014) | 86 youth (M =10.8 years) | Cross-sectional | Critical parenting | Child behavior problems | Critical parenting associated (+) with behavior problems and with HbA1c |
| Vesco et al. (2010) | 261 adolescents (13-18 years) | Cross-sectional | D responsibility | BGM frequency | Greater parental responsibility associated with higher BGM frequency |
| Weissberg-Benchell et al. (2009) | 121 youth with D (M age=12.1) | Cross-sectional | P responsiveness and demandingness, conflict, collaboration, positive and negative communication observed interactions | Quality of Life | Conflict and negative communication associated [−] quality of life, collaboration [+] associated with quality of life |
| Wiebe et al (2005) | 127 youth with D (ages 10-15 years) | Cross-sectional | M involvement in D | Adherence Behaviors |
M uninvolvement was [−] associated with adherence. Collaboration was associated with adherence [+] and HbA1c [−]. Collaboration and HbA1c was partially mediated by adherence. Control was [−] associated with adherence only among older youth. |
| Wiebe et al. (2014) | 252 youth, M, and F (M = 12.49 at baseline) | Longitudinal | P involvement | Adherence Behaviors Self-Efficacy |
Longitudinal declines in parental involvement especially linked to declines in adherence when adolescents did not report growth in self-efficacy. |
| Wysocki et al. (2009) | 309 youth (age range 9-14.5 years) | Cross-sectional | M and F collaborative involvement | Depressive Symptoms Self-Efficacy |
Depressive symptoms and self-efficacy poor when both primary and secondary caregiver were low in collaboration. |
A=Adolescent, BGM=blood glucose monitoring D=Diabetes, F=Father, M=Mother, P=Parent
This research is beginning to show evidence that parents’ involvement may be beneficial for diabetes management by facilitating the development and execution of many self-regulation skills including regulation of affect (Fortenberry, et al., 2009), active coping strategies and cognitive restructuring (Band & Weisz, 1990; Grey et al., 2009; Jaser & White, 2011), self-efficacy (Berg, et al., 2011; Iannotti et al., 2006; King, et al., 2014; Wiebe, et al., 2014), and goal-directed behavior (J. M. Butler et al., 2011; Helgeson & Takeda, 2009). In this review we adopt Baumeister’s framework (Baumeister, Vohs, & Tice, 2007) of self-regulation that defines self-regulation as an ongoing process of regulating one’s behaviors, cognitions, and emotions, in the service of goals relevant to diabetes management. Utilizing this approach to self-regulation, we will focus our review on constructs that relate to regulation of behavior (e.g., adherence behaviors including BG testing), cognitions (e.g., self-efficacy, beliefs about diabetes, planning), and emotions (negative affect including the persistent experience of negative affect as represented by elevated depressive symptoms or low quality of life).
Our approach highlights that diverse elements of parental involvement and the developing child’s self-regulation skills are coordinated, moving through time together in important ways along with illness management (see Figure 1), rather than guided by a particular direction of effects. Ongoing transactions among facets of parental involvement, self-regulation skills, and illness management occur in a dynamic system, with these elements moving together over time but also constraining one another, creating a coordinated system. Consistent with a dynamic systems approach, variables are assumed to be part of a multidirectional causal system (Butner, Amazeen, & Mulvey, 2005), represented in Figure 1 by springs rather than arrows (as relationships are transactional). That is, facets of parental regulation (e.g., parental monitoring) may push for greater coordination among a child’s facets of self-regulation. Relatedly, a child’s greater adherence behaviors (one facet of self-regulation) may push for low levels of parental behavioral involvement. Further, within self-regulation and parental involvement, some facets may serve to drive the coordination of the other aspects. For instance, within self-regulation fewer self-regulatory failures may serve to coordinate a system of lower negative affect and better adherence across time. Our approach is consistent with other developmental systems approaches (Fogel, 2011; Lewis, 2011; Smith & Thelen, 2003), that link aspects of parent-child relationships through a coordinative process.
Figure 1:
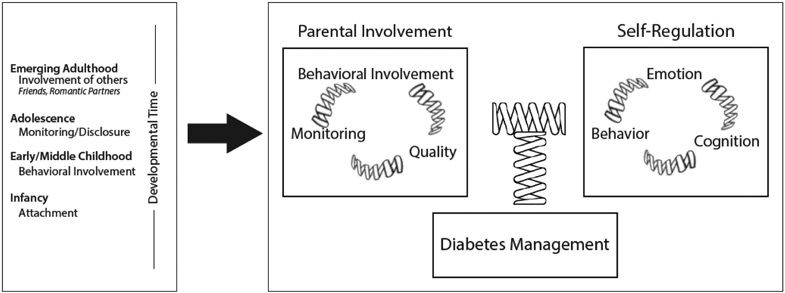
Developmental Model of Parent-Child Coordination for Self-Regulation in Type 1 Diabetes Management
Across developmental time, the specific manifestation of parental involvement important as inputs to this system may vary (depicted in the box on the left in Figure 1). During infancy, relationship quality may be key as attachment processes provide the foundation for the parent-child relationship. During early and middle-childhood, behavioral involvement may be most important in driving parental involvement as parent and child begin to negotiate new forms of relating as the child takes on more responsibility for diabetes management. During adolescence, parental monitoring may take on increasing importance as a driver of parental involvement as parents make adjustments to monitor their adolescent’s diabetes management behaviors as adolescents disclose relevant information to their parents. These foundations of parental involvement provide the basis for new relationships with friends and romantic partners to develop in adolescence and emerging adulthood, supplementing and even replacing the involvement that parents have provided.
A large literature in developmental psychology supports this transactional view of the parent-child relationship, whereby children are simultaneously affected by their parents, while also affecting their parents (Sameroff, 2009). That is, parental involvement not only affects youths’ self-regulation skills, but youths’ regulation skills affect parental involvement and parental development as well. For instance, a child’s ability to regulate emotions and cope with problems affects parents’ regulatory skills involved in parenting (Dix, 1991; Pettit, Keiley, Laird, Bates, & Dodge, 2007). Thus, children and parents are developing together across time in an interdependent fashion (Bell, 1968; Kim, Conger, Lorenz, & Elder, 2001; Nicholson, Deboeck, Farris, Boker, & Borkowski, 2011; Yates, Obradovic, & Egeland, 2010). Management of chronic illnesses such as diabetes is difficult and can engender family conflict (Anderson, et al., 2009; Hilliard, Harris, & Weissberg-Benchell, 2012), which may subsequently hinder effective parenting. Some evidence of the detrimental effect of adolescents’ daily problems with diabetes on subsequent parental daily mood has been found (Queen, Butner, Wiebe, & Berg, 2016). These parent-child coordinations can become self-organizing systems that are associated with positive regulatory skills or negative skills (Patterson, Debaryshe, & Ramsey, 1989; Repetti, et al., 2002).
There is a view in the literature that coordination between parents and children may change in nature across time, especially in terms of symmetries of influence, although the empirical support for this view is scarce. The coordination may be stronger earlier in development than later, with asymmetries such that parents may have a greater influence on children early in development with bidirectional effects between parents and youth strengthening over time (Pardini et al., 2008). In fact, adolescence may be a time during development when greater variability in aspects of the parent-child relationship may allow for these shifts in influence to occur (Granic, Hollenstein, Dishion, & Patterson, 2003).
Evidence for Coordination Between Self-Regulation and Parental Involvement for Diabetes Management
Both cross-sectional and longitudinal research provide evidence for relationships among parental involvement, chronic illness management, and some aspects of children’s self-regulatory skills (see Table 1). A large body of cross-sectional research demonstrates that parental warmth, acceptance, and emotional support are associated with better illness management during childhood and adolescence (Berg, et al., 2011; Davis et al., 2001; Eckshtain, Ellis, Kolmodin, & Naar-King, 2010; Miller-Johnson, et al., 1994; Skinner, et al., 2000). In addition, high quality parent-child relationships appear linked with good diabetes management through self-regulatory skills of adolescents such as self-efficacy (Berg, et al., 2011; Ott, Greening, Palardy, Holderby, & DeBell, 2000), being able to prioritize diabetes over peer influence (Drew, Berg, & Wiebe, 2010), and developing cognitive beliefs regarding how treatment may be effective (Skinner, et al., 2000). Parental support has also been associated with monitoring (i.e., what parents know about adolescents’ diabetes such as what their blood glucose readings are as well as what adolescents disclose to their parents and how frequently parents solicit information), and with better adherence and metabolic control (Ellis et al., 2007; Osborn, Berg, Hughes, Pham, & Wiebe, 2013).
The absence of positive aspects of high quality parental involvement (e.g., low support, low warmth) typically co-occur with the presence of more negative aspects of parental involvement (Anderson et al., 2002; J. M. Butler, Skinner, Gelfand, Berg, & Wiebe, 2007) such as hostility, criticism, control, and nagging, which have been associated with poorer adherence during adolescence (Armstrong, Mackey, & Streisand, 2011; Chisholm, et al., 2011; Grabill, et al., 2010; Jaser & Grey, 2010; Wiebe, et al., 2005). Further, such poor-quality relationships are also associated with self-regulatory challenges involved in emotion regulation such as increased parent-adolescent conflict (Anderson, et al., 2009; Herzer, Vesco, Ingerski, Dolan, & Hood, 2011; Hilliard, Wu, Rausch, Dolan, & Hood, 2013; Hood, Butler, Anderson, & Laffel, 2007) and negative emotions (Berg, et al., 2007). Critical parenting is also associated with lower self-efficacy (Armstrong, et al., 2011) and more depressive symptoms (Jaser & Grey, 2010). Conflict has been associated with greater depressive symptoms for adolescents (Barzel & Reid, 2011), greater parent and child negative affect surrounding blood glucose monitoring, a key metric of management (Hood, et al., 2007) and reduced levels of blood glucose monitoring (Ingerski, Anderson, Dolan, & Hood, 2010).
A number of recent longitudinal studies on developmental trajectories of diabetes management (Helgeson, et al., 2010; Hilliard, Wu et al., 2013; King, et al., 2014; King, et al., 2012; Luyckx & Seiffge-Krenke, 2009) provide further support for the idea that parental involvement, self-regulatory skills and illness management are coordinated across time. In one study, adherence deteriorated across adolescence in tandem with declines in maternal and paternal acceptance and monitoring (King, et al., 2014). Further, longitudinal associations between maternal acceptance and diabetes monitoring and subsequent adolescent adherence were mediated by changes in adolescents’ self-efficacy, an important self-regulatory skill (King, et al., 2014).
Longitudinal studies are also beginning to identify typologies of families characterized by patterns of family involvement and adolescent regulatory skills that support parent-child coordination. Research has identified at least two different trajectories of diabetes outcomes among adolescents: a group that begins adolescence in good or moderate metabolic control (Hilliard, Harris, & Weissberg-Benchell, 2012; King, et al., 2012; Luyckx & Seiffge-Krenke, 2009) and deteriorates modestly across adolescence, and a group that begins adolescence with quite poor metabolic control and deteriorates rapidly across adolescence (Helgeson, et al., 2010; Hilliard, et al., 2012; King, et al., 2012). Consistent with the idea that various elements of parental involvement are coordinated with child regulatory skills and diabetes management, King et al. (2012) found that adolescents with a better metabolic control trajectory reported greater paternal monitoring and scored higher on measures of self-control and autonomy. Hilliard et al. (2012) found that those with better metabolic control reported less family conflict, less depressive symptoms, and less negative affect regarding blood glucose monitoring and Helgeson et al. (2010) found similarly that a better metabolic control trajectory was associated with less negative emotions.
The cross-sectional and longitudinal research reviewed above points to consistent relationships among elements of parental involvement, youth self-regulation, and good illness management. Although few studies have included multiple facets of parental involvement, youth self-regulation skills and illness management (see Berg, et al., 2011; Ellis et al., 2007) or multiple directions of effects, taken as a whole the literature is consistent with the type of relationships depicted in Figure 1. That is, a broad array of parental involvement measures move together through time with self-regulation skills of the child and illness management outcomes. Further, the research is supportive of the idea of a bi-directional system of influence, whereby children and parents (and others) influence each other through time by pushing and pulling each other at different times across childhood and adolescence. Such coordinative patterns may be stable or labile at various times, and asymmetric or symmetric. The parent-child coordinations found during adolescence may derive from earlier foundations of effective coordinations between parents and children (attachment) that inform adolescents’ and emerging adults’ relationships with high quality friend, romantic, and health care relationships. We now describe this developmental coordinative process and provide evidence from the developmental literature for its emergence.
Developmental Perspective on Parent-Child Coordination
Our perspective characterizes the developmental progression of chronic illness management as moving from the highly interdependent relationship with parents that occurs early in development, where parents are integral in the coordination process, to one that remains interdependent but begins to involve other relationships (such as peers and romantic partners) in the coordination later in development. This is in contrast to the position frequently portrayed in the literature that the adolescent moves toward independent chronic illness management as they emerge into adulthood (Weissberg-Benchell, Wolpert, & Anderson, 2007). Thus, this model links to adult life-span models of dyadic coping in couples (Berg & Upchurch, 2007; Revenson, Kayser, & Bodenmann, 2005), which view adults dealing with chronic illness as interdependent within close relationships.
We illustrate developmental changes in the coordinative process that facilitate diabetes management in conjunction with other close relationships using the metaphor of a child riding a bicycle. During infancy, the parent has primary responsibility for management, much as when riding a bicycle the parent may do the work of pedaling and steering with the infant positioned in a seat carrier. Even during this early development period, however, the parent-infant relationship is characterized as involving a coordinative system (Biringen & Easterbrooks, 2012). That is, although the parent has primary responsibility for diabetes management, parental involvement may be affected by temperamental characteristics of the infant, much as slight shifts in the position of the infant on a bicycle affect the balance of the parent and vice versa. During childhood, as the child gains skills, the child begins to perform diabetes tasks independently, much as a child is taught to ride a tricycle and then a bicycle with extensive assistance from parents. Parental involvement is crucial during this phase, as premature autonomy granting can be detrimental (poor metabolic control for aspects of diabetes management, (Wysocki, et al., 1996); cut knees and broken bones in the case of bicycle riding). Parental involvement can help to foster self-regulatory skills such as emotion regulation (Morris, et al., 2007) and self-efficacy (Berg, et al., 2011; King, et al., 2014) that allow for greater adolescent independence in management behaviors. The success of the child’s growing independent attempts may affect parental well-being (Berg, et al., 2013) and parents’ subsequent parental involvement. During adolescence, the child manages diabetes sometimes independently from parents (as when riding their own bicycle on separate trips), sometimes in parallel (as when riding a bicycle at the same time, but separately) and sometimes with still extensive coordination (as when riding a tandem bicycle together). A key component of successful coordination that results in good diabetes outcomes requires a skillful dance between parent and adolescent in fitting the level of parental involvement to the competence of the developing child (Palmer, et al., 2009; Palmer, et al., 2004; Wiebe et al., 2014). It is during this time that additional close relationships may play an important role in the coordinative process (e.g., the adolescent rides a bicycle alongside a friend or adult healthcare provider or in tandem with a relationship partner). These additional relationships may produce changes in how parent and child relate to each other (e.g., the parent may no longer have the same opportunity to ride alongside the adolescent or emerging adult), with parents’ involvement still important (King, et al., 2014), especially when stressors or problems arise (Berg, et al., 2013).
Our model highlights the fact that this coordinative process of parent and child begins in infancy and provides a foundation for the emergence of later forms of coordination. We now highlight that across development, the specific components of parental involvement that may drive coordination may vary (see Figure 1) with features such as the high quality of the relationship (i.e., through attachment processes) being especially important in infancy, behavioral involvement important during early childhood, and monitoring and the adolescent’s ability to engage their social network through disclosure increasingly important across adolescence. However, at each point in time, there is evidence that parental involvement is linked to self-regulation of the child in ways that are associated with diabetes management. These coordinations provide the basis for how new relationships (friends, romantic partners, health care providers) enter this system and are coordinated and potentially move the system to new stable patterns throughout time. We now describe these coordinations that have been identified in the developmental literature on parent-child relationships and self-regulation and link these findings to the diabetes literature when possible.
Attachment as a Foundation for Parent-child Coordination
During infancy parental involvement has been captured via attachment processes that have themselves been characterized as a coordinated system (Coleman & Watson, 2000). Attachment processes serve as a foundation for numerous facets of an infant’s self-regulation and create a potential developmental cascade (Masten et al., 2005) involving progressive and more diffuse effects on a large number of other elements in the system. Thus, the high quality warm and accepting relationships that are important for effective diabetes management during adolescence likely have their foundation in secure attachment relationships that were formed well before adolescence, during infancy, and contribute to adolescents’ effective regulation skills (Allen et al., 2003). Support for this idea in the diabetes literature comes from Korbel (personal communication) who found that adolescents’ perceptions of mothers as warm and accepting were associated with greater attachment security. Greater evidence for this idea is available in the developmental literature that finds that maternal support and warmth during adolescence is associated with reports of early attachment security (Allen, et al., 2003; Kerns, Brumariu, and Seibert, 2011).
According to theorists, attachment behaviors to parents are formed during infancy through parent-child interactions that are key for early emotional development (e.g., Bowlby, 1969; Calkins & Leerkes, 2011; Main, Kaplan, & Cassidy, 1985; Main & Solomon, 1990). Children’s repeated experiences of communicating to their caregivers that they are in distress together with caregivers’ consistent responses to these distress signals establish in the child a set of internal working models (Bowlby, 1969, 1989) of the cognitions and behaviors to engage in and expect in others. When these sensitive responses occur, children develop a sense of self-confidence in their ability to clearly and accurately communicate physical and emotional needs without either exaggerating or minimizing their intensity (Bretherton, 1987; Sroufe, 1996). However, when parents are not able to sensitively and appropriately respond to their children’s distress signals, by reacting in ways that are either unresponsive (e.g., withdraw) or inappropriate (frightened/frightening behavior, intrusive/over-stimulating) (Ainsworth, 1991; Etzion-Carasso & Oppenheim, 2000), children are unable to develop secure attachments. Children with insecure attachments either minimize their expression of needs to their caregiver and withhold the desire for closeness within interpersonal relationships (anxious avoidant attachment) or foster a communication style with others characterized by exaggerated emotional expression and communication (anxious-ambivalent) (Carlson & Sroufe, 1995; Cassidy & Kobak, 1988).
The available research base, albeit small, is supportive of the idea that diabetes management during childhood and adolescence is associated with these early attachment relationships. Attachment security to mother has been associated with lower levels of depressive symptoms (Korbel, 2009) and better metabolic control among adolescents with type 1 diabetes (Rosenberg & Shields, 2009; note only maternal reports of attachment were associated with metabolic control). Further, attachment insecurity in the form of anxiety and avoidance has been associated with greater depressive symptoms and marginally with poorer adherence, and anxious attachment has been associated with poorer metabolic control in adolescents (Korbel, 2009). A larger literature on adult attachment style and diabetes management (both type 1 and type 2 diabetes) exists that is supportive of the relationships between insecure attachments and diabetes outcomes (Ciechanowski, Hirsch, & Katon, 2002; Ciechanowski, Katon, Russo, & Walker, 2001; Ciechanowski et al., 2004; Turan, Osar, Turan, Ilkova, & Damci, 2003). Adults who classified themselves as exhibiting a dismissing style characterized by high attachment avoidance showed poorer adherence and metabolic control as compared to those with other attachment organizations (Ciechanowski, et al., 2001; Ciechanowski, et al., 2004) (see discussion below in section on Coordination with Parents and Health Care Providers Across Development for further detail).
Parental Involvement in Young Children
The central role of attachment in the system of parent-child coordinations during young childhood can be seen in the far reaching effects of attachment on emotion regulation, social competence, and health during early and middle-childhood as well as adolescence (Calkins & Leerkes, 2011; Diamond & Fagundes, 2010). A secure attachment relationship has been associated with better emotion regulation skills during young childhood (Calkins & Leerkes, 2011). Of particular relevance to families dealing with a young child with type 1 diabetes who may find adherence behaviors demanding, secure attachments in infancy have been associated with the young child’s ability to engage in attention shifting strategies especially during times of frustration (Gilliom, Shaw, Beck, Schonberg, & Lukon, 2002). A secure attachment relationship is also associated with greater parental knowledge of children’s activities and greater cooperation by children in monitoring situations during middle childhood (Kerns, Aspelmeier, Gentzler, & Grabill, 2011).
The links between aspects of parental involvement and self-regulation in young children with type 1 diabetes have been much understudied, potentially as the incidence of type 1 diabetes is lower in this age group than during adolescence (Liese et al., 2006). The literature depicts mothers of young children with diabetes as experiencing high stress, anxiety, and depression (Monaghan et al., 2009; Streisand, Swift, Wickmark, Chen, & Holmes, 2005), especially among those mothers whose children have been newly diagnosed. Greater distress associated with diabetes management among parents has been associated with their lower self-efficacy surrounding diabetes care activities (Streisand et al., 2008) and their reports of greater child behavior problems (Hilliard, Monaghan, Cogen, & Streisand, 2010). Further, greater parental stress has been associated with greater parental fears of hypoglycemia (Streisand et al., 2005), with such fears associated with poorer blood glucose control (Patton et al., 2007). Fathers report lower distress than do mothers and their distress shows weaker associations with the child’s diabetes management, potentially due to their lower involvement in the day to day tasks of diabetes management (Mitchell, Hilliard, Mednick, Henderson, Cogen, & Streisand, 2009). Supporting coordination between a child’s self-regulation and parents, greater child’s self-control has been associated with lower parent distress (Monaghan, Clary, Stern, Hilliard, & Streisand, 2015). Although links between parenting distress and poor blood glucose control have been found, the specific elements of parental involvement affected by high distress have yet to be uncovered.
Some links between parental involvement and aspects of the young child’s regulation have been examined in the context of parent-child mealtime behaviors. From the perspective of parent-child coordination, mealtime behaviors provide an ideal setting in which to examine both the child’s self-regulation (especially emotional regulation) together with parental involvement in a context that involves key aspects of diabetes management (e.g., blood glucose testing, insulin administration, selection of foods). Parents of young children with type 1 diabetes report more concerns about feeding issues and mealtime behavior than parents of healthy children (Patton, Dolan, Mitchell, Byars, Standiford, & Powers, 2004). Parents’ poorer psychosocial functioning has also been associated with greater parental reports of their own as well as their child’s problematic mealtime behaviors (Monaghan et al., 2015). The kinds of behaviors examined in these interactions do not map well onto the components of parental involvement examined in our model. However, parents’ use of ineffective mealtime strategies (e.g., high control and frequent reminders for the child to eat) have been associated with poorer adherence to dietary recommendations (Patton, Piazza-Waggoner, Modi, Dolan, & Powers, 2009). In addition, having to deal with emotional issues surrounding food intake during mealtimes has been associated with poorer glycemic control (Patton et al., 2009), suggesting that emotion regulation in the developing child is an important component to effective diabetes management.
Recent interventions to help assist parents with their distress surrounding diabetes are suggestive of the coordination that may take place between parental involvement and children’s self-regulation. For instance, a parent-based educational intervention aimed at changing mealtime behaviors decreased both parent and child problematic mealtime behaviors as well as lowered blood glucose levels (Patton, Odar, Midyett, & Clements, 2014). Much more research is needed as to the specific components of parental involvement that may be associated with children’s self-regulation in the context of diabetes management and factors that may be key in this coordination.
Coordination of Parental Monitoring and Adolescent Disclosure
A high quality parent-child relationship laid down in infancy and early childhood allows for the emergence of new patterns of relating between parents and children during adolescence that facilitate self-regulatory skills of adolescents relevant to diabetes management. Positive aspects of maternal involvement co-occur together. Specifically, maternal warmth is associated with greater maternal knowledge during early adolescence (Grundy, Gondoli, & Salafia, 2010). The parent-child relationship during adolescence undergoes significant changes as individuals try to balance autonomy and connectedness (Allen, Porter, McFarland, McElhaney, & Marsh, 2007; Smetana et al., 2006). Parents and children who have developed a warm and trusting relationship in which the parent has operated as an effective secure base are at an advantage for developing effective partnerships during adolescence (Scott, Briskman, Woolgar, Humayun, & O’Connor, 2011; Waters, Kondo-Ikemura, Posada, & Richters, 1991), whereas those with insecure attachments are at greater risk during adolescence (Kochanska & Kim, 2012).
During adolescence, this partnership involves a transaction whereby parents monitor adolescents’ behavior together with adolescents disclosing information to their parents (Stattin & Kerr, 2000). Parental knowledge may become increasingly dependent on adolescent disclosure, that is, the way in which adolescents communicate and manage the flow of information about their lives with their parents, and how parents themselves use different strategies to gain knowledge about their child (Allen & Manning, 2007; Branstetter, Furman, & Cottrell, 2009; Wampler & Downs, 2010; Wilkinson, 2004). As adolescents spend more time away from their parents, they are uniquely positioned to influence how much parents know about their lives by using strategies such as self-disclosure, secret keeping, and lying (Almas, Grusec, & Tackett, 2011; Frijns, Keijsers, Branje, & Meeus, 2010). Adolescent outcomes like delinquency and risky health behaviors have been linked to lower levels of adolescent voluntary disclosure of information (e.g., Darling, Cumsille, Caldwell, & Dowdy, 2006; Kerr, Stattin, & Burk, 2010; Smetana, Villalobos, Tasopoulos-Chan, Gettman, & Campione-Barr, 2009; Stattin & Kerr, 2000), higher levels of secret-keeping (e.g., Bumpus & Hill, 2008; Cumsille, Darling, & Martinez, 2010; Frijns, et al., 2010), and more lying (e.g., Marshall, Tilton-Weaver, & Bosdet, 2005).
A growing literature indicates that adolescents’ willingness to disclose personal information to a parent and parental knowledge occurs through a transactional and dynamic process based in warm, trusting, and responsive parent-adolescent relationships (Hamza & Willoughby, 2011). Adolescents share more information with parents when parents are more warm and responsive and employ less psychological control (e.g., intrusive parenting) (e.g., Fletcher, Steinberg, & Williams-Wheeler, 2004; Soenens, et al., 2006). As evidence of the coordination between adolescents’ regulatory capacities underlying disclosure and parents’ emotion regulation skills, when the risk of disclosure may be associated with parental anger (Almas, et al., 2011) or disapproval (Darling, et al., 2006), secrecy or lying rather than disclosure may result. Further, longitudinal analyses reveal that adolescent disclosure contributes to better psychological functioning (lower depressive symptoms) through increasing parents’ knowledge; simultaneously, depressive symptoms limit subsequent parental knowledge and adolescent disclosure over time (Hamza & Willoughby, 2011).
As indicated above, the current literature on diabetes management clearly points to the importance of a high quality relationship, where parents monitor and are behaviorally involved in diabetes management (Berg, et al., 2008; Ellis, Podolski, et al., 2007; Main et al., 2014), despite the fact that parental involvement declines across adolescence (King et al., 2014; Wiebe et al., 2014). Consistent with the broader developmental literature (Racz & McMahon, 2011; Stattin & Kerr, 2000), the diabetes literature is beginning to acknowledge that effective parental monitoring involves not only active attempts by parents to solicit information from adolescents, but also adolescents’ willingness to disclose information to their parents (Berg et al., 2017; Ellis, Templin, Naar-King, & Frey, 2008; Osborn, et al., 2013) as well as to avoid keeping information secret (Main et al., 2015; Osborn, et al., 2013). Although parental monitoring of diabetes in the form of parents having knowledge of their adolescents’ diabetes management is associated with features of accepting and supportive parent-child relationships (Berg, et al., 2008; Ellis et al., 2007), longitudinal data are not available during early and middle childhood to trace whether effective monitoring and disclosure of diabetes information during adolescence emerges from earlier high-quality relationships during early childhood. However, the larger developmental literature does seem supportive of these links (Racz & McMahon, 2011).
A growing literature indicates that the level and nature of mothers’ and fathers’ involvement may vary for diabetes management. In general, mothers are more behaviorally involved, monitor more their adolescents’ diabetes, solicit more information and have adolescents disclose more information to them than do fathers (Berg et al., 2017; King et al., 2014). When comparing mothers’ and fathers’ daily involvement and links to diabetes management, mothers’ involvement has been somewhat more consistently associated with changes in daily blood glucose and adherence (Berg et al., 2013; Berg et al., 2016). However, despite their lesser involvement in diabetes management, greater paternal monitoring especially has been associated with better adherence (Hilliard, Rohan, Rausch, Delamater, Pendley, and Drotar, 2014; King et al., 2014) and HbA1c (Berg et al., 2011; Hilliard et al., 2014).
In sum, the high quality parent-adolescent relationship that is found to be important in fostering good regulatory skills necessary for effective diabetes management likely emerges from early attachment relationships that foster effective emotion regulation skills that allow young children and their parents to deal with the challenges of managing a chronic illness. The foundation of a high quality relationship allows for the emergence of a transactional relationship during adolescence whereby adolescents disclose to their parents problematic aspects of their diabetes management, thereby providing parents with the knowledge of the adolescent’s behavior. Such disclosure and knowledge is important in fostering effective diabetes management during late adolescence and emerging adulthood, when other relationships such as friends and romantic partners are incorporated into this coordination.
The Addition of Others in the Coordinative Process (Parents+)
Coordination with parents, peers, and romantic partners across development.
From the developmental literature we know that early parent-child relationships lay the foundation for the formation of relationships with friends and romantic partners that serve increasingly important roles across adolescence (De Goede, Branje, Delsing, & Meeus, 2009). These changing relationships introduce new elements into the coordinated system between parents and children (see Figure 1) that may spark new organizations of the system as adolescents seek acceptance and belonging with peers and potentially receive support from their peers for illness management. The capacity to utilize peers as a source of support is likely to be quite important for maintaining or strengthening self-regulation skills such as emotional competence (Laible, 2007) and mastery (Conger, Williams, Little, Masyn, & Shebloski, 2009) during adolescence. Consistent with these ideas, Beyers and Seiffge-Krenke (2007) found that adolescents who experienced trajectories in family relationships characterized by sustained connection and increases in mutual respect for individual decision-making across adolescence displayed greater support and lower negativity in friendships in late adolescence. Importantly, these peer relationships in late adolescence were associated with self-regulation skills such as lower internalizing symptoms in young adulthood.
Family and peer relationships form the staging ground for romantic relationships (Collins, Welsh, & Furman, 2009; Seiffge-Krenke, Overbeek, & Vermulst, 2010), and peer and romantic relationships become increasingly integrated and influential in this coordinative system as adolescents emerge into early adulthood (Collins, et al., 2009; Seiffge-Krenke, et al., 2010). By late adolescence, interactions with romantic partners are more frequent than with parents or friends, and provide as much support as relations with mothers (Smetana, Campione-Barr, et al., 2006). Although parents continue to be important elements of this coordinative system, their role changes and influence wanes as peers and then partners become increasingly important. Surjadi, Lorenz, Wickrama, and Conger (2011) demonstrated that parental support was associated with higher mastery in middle adolescence, and with greater partner support across the subsequent transition to adulthood. Partner support, but not parental support, was associated with increases in mastery during the transition to adulthood.
These changes in the social context provide the opportunity for new patterns of coordination among parents, adolescents, and friends surrounding diabetes management during adolescence and emerging adulthood. As in the general developmental literature, peers become increasingly influential sources of support for diabetes management during adolescence (see Burroughs, Harris, Pontious, & Santiago, 1997; Gallant, 2003; La Greca, Bearman, & Moore, 2002; Palladino & Helgeson, 2012 for reviews).This developmental shift is evident in several ways. Friends are more commonly cited as a source of support for diabetes by adolescents than by children (Shroff-Pendley et al., 2002) and while peer support for diabetes remains stable across adolescence, family support declines (Bearman & La Greca, 2002; Carcone, Ellis, Weisz, & Naar-King, 2011; Skinner, et al., 2000). Support from family also appears to serve different functions than support from friends during adolescence, with families providing more instrumental support for diabetes (e.g., help with insulin dose) and friends providing emotional support and companionship (Bearman & La Greca, 2002; La Greca et al., 1995). Skinner and Hampson (1998) found that family support (but not friend support) was associated with better diabetes adherence, while friend support (but not family support) was associated with lower adolescent depression.
The literature is beginning to note the important interplay between parents and friends in the developing adolescents’ self-regulation skills and chronic illness management. Wallander and Varni (1989) demonstrated that the presence of both family and peer support was necessary for optimal adjustment among adolescents dealing with type 1 diabetes or other chronic conditions. Support from friends can compensate for negative aspects of parental involvement such as control (Helgeson et al., 2014; Herzer, Umfress, Ajadeff, Ghai, & Zakowski, 2009) and parental support can compensate for conflict with friends in diabetes management. When the links between parents, children, and friends, however, are not coordinated well with the self-regulatory skills of the child, disruptions in illness management may take place. For instance, declines in parental involvement across adolescence (King, et al., 2014) occur at a time when friends’ involvement increases, which may be detrimental if such changes are not accompanied by the effective self-regulatory skills of the child.
When peers are not supportive, they can present tension and conflict that tax adolescents’ regulatory capabilities and have a negative effect on the coordinative system in managing diabetes. Storch et al. (2006) found adolescents may be bullied because of their diabetes, and that diabetes- related bullying was associated with poorer adherence and metabolic control via higher depressive symptoms. Similarly, adolescents’ reports of conflict with friends predict poorer adherence and metabolic control (Helgeson, Lopez, & Kamarck, 2009; Helgeson, et al., 2010), and rejection by friends is associated with poorer psychosocial well-being (Helgeson et al., 2009). Even positive peer relationships have been associated with poorer metabolic control among adolescents with diabetes (Hains et al., 2007; Helgeson et al., 2010), potentially because adolescents often expect friends to react negatively when they follow their diabetes regimen (Hains, et al., 2007), and may neglect their diabetes in order to socialize with peers (Delamater, Smith, Kurtz, & White, 1988; Drew, et al., 2010; Thomas, Peterson, & Goldstein, 1997). Taken together, such findings reveal that early parent-child relationships that are warm and accepting co-occur with positive and supportive peer relationships that further foster good self-regulatory skills into late adolescence as they increasingly manage their illness in social contexts away from parents.
In our model, we argue that these self-regulatory skills oriented toward the regulation of the interpersonal context develop out of adolescents’ relational history with parents, and some data exist to support this hypothesis in the context of diabetes management. Adolescents who report higher family support for diabetes also report higher peer support for diabetes (Bearman & La Greca, 2002; Carcone, et al., 2011; Skinner, et al., 2000), and adolescents who feel rejected by their parents also report higher rejection from peers (Herzer et al., 2009). In a more direct test of this hypothesis, Drew and colleagues (2010) found that adolescents who reported high quality relationships with parents (i.e., warmth and acceptance) achieved better diabetes management through being less likely to choose to socialize with peers at the expense of their diabetes management.
Minimal research has examined the role of romantic partners for supporting diabetes management during adolescence and emerging adulthood. The challenges of managing an illness such as type 1 diabetes may alter the development of intimate friendships and romantic relationships during adolescence and beyond. Seiffge-Krenke (2000) found that late adolescents with diabetes were less likely to have romantic partners than those without diabetes. However, those who had romantic partners were more satisfied with the relationship compared to those without diabetes, and the partners served different roles by providing more instrumental support. Qualitative research suggests that close friends and romantic partners gain a more prominent role in supporting diabetes management during emerging adulthood, although parents continue to be a trusted resource (Hanna, Weaver, Stump, Guthrie, & Oruche, 2014) providing guidance regarding diabetes management to their adult child as well as to their child’s friends and partners (Sparud-Lundin, Öhrn, & Danielson, 2010).
Coordination with parents and health care providers across development.
An additional relationship that has been infrequently examined in the coordinative system is the relationship with the physician and other health care providers. Diabetes management is improved when patients and parents are able to develop collaborative partnerships with health care providers (Drotar, 2009). These collaborative relationships involve many of the same key facets of relationships found in parental involvement. That is, a collaborative relationship with one’s health care provider is one that is warm and accepting, where there is active exchange of information so that providers are knowledgeable, and provide the context for shared decision-making among patient, parent and provider. Not surprisingly, positive patient-provider relationships are associated with higher patient satisfaction, better adherence and self-care, and better illness outcomes across a range of conditions, including type 1 diabetes (Drotar, 2009; Naar-King, Podolski, Ellis, Frey, & Templin, 2006). Such positive patient-provider relationships may relate to higher adherence to the diabetes regimen through heightened perceptions of the adolescent’s competence in diabetes management (Croom et al., 2010). In addition to empowering adolescents to manage their diabetes, physicians may be positioned to provide feedback to the family about developmentally appropriate shifts in parental involvement to ensure that there is a fit between child’s capabilities and the parent’s involvement (Wiebe et al., 2008).
Parents’ and children‘s relationships with health care providers change across development in a manner that reflects the growing regulatory capacities of the developing child (see De Civita & Dobkin, 2004 for review). Because pediatric conditions are managed primarily by parents during infancy and early childhood, parents’ relationship with the provider is initially a primary focus and children are rarely involved in medical decisions (Cahill & Papageorgiou, 2007; Coyne, 2008). As older children and adolescents assume increasing responsibilities for managing diabetes, potentially because older youth have a greater capacity to develop a treatment alliance with physicians (Gavin, Wamboldt, Sorokin, Levy, & Wamboldt, 1999), more time is spent on relationship building in interactions with providers (Cox, Smith, Brown, & Fitzpatrick, 2009). This increasing prominence of the adolescent-provider relationship is likely to provide an important training ground for the adolescent as he or she prepares to leave the pediatric setting and transition to adult care, a setting that is likely to pose new regulatory challenges for the young adult (Weissberg-Benchell, et al., 2007).
The ability to develop positive and collaborative partnerships with physicians and to navigate the health care system efficiently and effectively may develop out of positive relationships with parents. Ciechanowski and colleagues (2004) demonstrated that adults with diabetes who had secure attachment relationships with early caregivers reported more satisfaction with their relationship with their physician than those with insecure attachments, and that more satisfying doctor-patient relationship mediated associations between attachment security and better diabetes self-care. Secure attachments with early caregivers have also been associated with patients’ greater ability to trust providers and to value their relationship with providers (Ciechanowski & Katon, 2006), missing fewer scheduled clinic appointments (Ciechanowski et al., 2006), and having lower subsequent mortality (Ciechanowski et al., 2010).
Given the somewhat infrequent contact that adolescents have with their healthcare provider, it may be difficult to establish whether adolescents are in fact coordinated in important ways with their physician. Recent e-health technologies that offer the opportunity for those with chronic illness to be in more regular contact with health care professionals may, in fact, provide a greater opportunity for coordination to occur (Froisland, Olsen, Robinson, & Mandleco, 2012).
Summary
The broader developmental literature is consistent with the view that the coordinations between parents’ involvement and children’s regulatory skills found during adolescence have their foundations earlier in development in the formation of the parent-child relationship. Further, the positive facets of parental involvement together with developing regulatory skills allow for the emergence of new relationships with peers, romantic partners, and health care providers that emerging adults can draw on to facilitate diabetes management. This coordinated system begins early in development and may be maintained across time through psychosocial and biological processes (Lansing & Berg, 2014). However, such coordinations are not static or predetermined from early childhood, but rather move as new elements enter into the system (e.g., peers, healthcare providers). We now provide a specific illustration of how such coordinations can be modeled across time and the potential of our model as an effective data reduction technique.
Modeling Parent-Child Coordination in Diabetes Management
Forms of Coordination
The notion that development emerges from coordinations among elements of a child’s and parent’s functioning has much support in the developmental literature from infancy through adolescence (Evans & Porter, 2009; Fogel, 1993, 2011; Granic & Patterson, 2006; Lewis, 2000; A. J. Sameroff & Mackenzie, 2003; H. Steenbeek & van Geert, 2005; Thelen & Smith, 1994). Of particular relevance to our framework, specific modeling of elements of a child’s self-regulation (emotional functioning, social interactions) and parental involvement (e.g., coercion, warmth) from a coordination perspective have been undertaken (Granic, 2000; Hollenstein, Granic, Stoolmiller, & Snyder, 2004; Lichtwarck-Aschoff, Hasselman, Cox, Pepler, & Granic, 2012). Mathematical models are used to capture these coordinations and how elements change together over time through principles of self-organization (e.g. Lewis, 2000; Smith, 2005; Thelen & Smith, 1994). In addition, coordinations among elements have been modeled using coupled equations (e.g. H. Steenbeek & van Geert, 2008; H. W. Steenbeek & van Geert, 2007). In the dyadic interaction literature, such coupled equation approaches (Boker & Laurenceau, 2006; Hamaker, Zhang, & van der Maas, 2009; Steele & Ferrer, 2011; H. W. Steenbeek & van Geert, 2007) generate one-to-one synchronous behaviors, which is only one of many coordinations that could be modeled in parent-child relationships across childhood, adolescence, and emerging adulthood.
Coordination can be viewed as a more general framework for characterizing patterns of how elements such as parents and children move together (E. A. Butler, 2011), with coordination varying along a continuum (Beek & Beek, 1988; Turvey, 1990). At one end of the continuum is a lack of coordination that can also be called asynchrony, such that two or more elements are completely independent of one another through time. Although it may be difficult to imagine how parents and children may be completely independent when dealing with type 1 diabetes, a recent example demonstrates that it may be possible. Berg et al. (2013) reported a lack of relationship between adolescents’ daily blood glucose and fathers’ efforts to persuade them to better manage their diabetes. This asynchrony may have resulted from fathers’ lack of knowledge about adolescents’ blood glucose levels. At the other end of the continuum is synchrony where there is a direct relationship between elements of the system moving together through time. Synchrony can occur in a one to one relationship (e.g., ingestion of carbohydrates together with change in blood glucose) or a different scaling relationship (Stewart & Golubitsky, 1992; Treffner & Turvey, 1993).
Between asynchrony and synchrony is an area commonly known as entrainment where elements have periods of moving together with periods of asynchrony (Bernieri, Reznick, & Rosenthal, 1988; Butner, Diamond, & Hicks, 2007). In the case of chronic illness management, this may characterize the period of preadolescence through late adolescence, as parental involvement declines across time, but not always in tune with adolescents’ competencies (Palmer, et al., 2009; Wiebe et al., 2014; Wysocki, et al., 1996). Across adolescence parental involvement may decline due to normative changes in parental involvement and adolescent autonomy needs, but not their competencies. Problematic episodes, such as severe hypo- or hyper-glycemia may signal to parents that they need to increase their involvement. Thus, at times across development parent involvement may not be coordinated with adolescents’ competences, but such problematic episodes may be key in getting this coordination between parental involvement and the child’s developing skills back on track.
Recent analyses of coordination have begun to identify how two or more elements become linked in a stable pattern of relationship through time. For instance, adolescents’ daily problems in diabetes management are associated with increases in parents’ worry and decreases in parents’ views of adolescents’ self-efficacy, and these patterns of association occur repeatedly in the daily lives of families managing diabetes (Berg et al., 2013). These same sorts of coordinations have been identified in dyadic interactions more generally regarding influence and appraisal among child peers (Steenbeek & van Geert, 2008; Steenbeek & van Geert, 2007), couples’ affect (Butner, et al., 2007; Steele & Ferrer, 2011), and couples’ intimacy and disclosure (Boker & Laurenceau, 2006). In essence, coordination describes the stable pattern of relationship between two or more elements through time.
Current approaches for modeling coordination and testing bidirectional relationships allow us to identify both a coupling relationship that pulls elements together through time (known in early work as the magnet effect) and, independent of this coupling relationship, the intrinsic pattern of change in each element involved in the coordination (known in early works as the maintenance tendency) (Von Holst, 1939, 1973). For example, individuals are fairly stable in their relative position in metabolic control (HbA1c) across time (King, et al., 2014), which would be considered the natural (maintenance) tendency for HbA1c. However, there are mean level increases in HbA1c (indicating deterioration) across adolescence, likely pulled in that direction by changes in physiology associated with puberty, increased influence of the peer context, and reduced influence of parents (Drew, et al., 2010; Helgeson, et al., 2010; King, et al., 2012). Thus, an analysis of change patterns in the elements in our model (parental involvement, diabetes management, and self-regulation) would examine not only natural tendencies in each of these elements, but also their coordination.
Approaches for identifying these natural tendencies and coupling relationships are plentiful. In structural equation modeling alone techniques include, but are not limited to dynamic factor models (Molenaar, 1985), latent differential equation modeling (Boker et al., 2011), continuous time models (Oud, 2007), and latent change score modeling (McArdle & Hamagami, 2001). Such models are also conducive to multilevel modeling techniques (J. Butner, Amazeen, & Mulvey, 2005) and time series approaches more generally (see Guastello & Gregson, 2011). Each circumstance characterizes the time evolution of two or more outcomes and the linkages between them. Primarily, the techniques vary on their treatment of time (continuous or discrete), the assumption underlying natural tendency (e.g. trajectory-like or oscillatory), and their treatment of additional variability (e.g. models of error and perturbations).
We have recently applied these techniques to aspects of self-regulation and parental involvement in late adolescents with type 1 diabetes (Butner, Berg, Wiebe, Lansing, Munion, & Turner, in press). Dynamic systems modeling, via Structural Equation Modeling, was conducted examining the relationship between changes in a number of facets of self-regulation (adherence, daily diabetes problems, self-regulatory failures, positive and negative affect, self-confidence) and parental involvement (parents’ knowledge of diabetes, adolescents’ disclosure to parents, and perceived helpfulness of parents) separately from mothers and fathers over a 14-day diary period. Coordination in changes in these variables was then captured through the identification of latent factors of these changes. Coupling relationships were captured through predicting these latent coordination factors as a function of the current variables, and the stability information captured by how the variable predicted its own change, controlling for the coordination factor.
The results revealed that self-regulation functioned as one coordinative structure whereby self-regulation involved changes toward increased adherence, efficacy, and positive affect, and decreases in negative affect, self-regulatory failures, as well as daily problems. Parental involvement was separate from self-regulation, and mothers’ and fathers’ involvement were coordinated separately from each other. The coordinative structure for both mothers’ and fathers’ involvement consisted of changes toward greater knowledge of their adolescents’ diabetes behavior, greater disclosure from the adolescent to the parent, and greater helpfulness. The connection between parental involvement and adolescent self-regulation was most clear for mothers’ perceived helpfulness as it served as a key variable in returning adolescents’ self-regulation back to homeostasis. Fathers’ involvement did not move adolescents’ self-regulation across the 14 days.
These results are very consistent with our model of parent-child coordinations and hold promise for how we might utilize coordination as a way to understand parental involvement, self-regulation, and illness management. Within a developmental framework, coordination is the mechanism by which we observe stable trajectories over time. The developmental trajectories emerge from the combination of the maintenance tendencies of each element (i.e., the trajectory each would naturally traverse over time), and the inherent perturbations of the other elements that are constantly affecting one another.
Coordination as a Data Reduction Technique
A coordination model such as that described above may result in effective data reduction. When several variables are coordinated through time, they inherently display some concordance as they pull and push one another repeatedly. Thus, providing a good description of the temporal patterning of one variable will invariably depict the properties of other variables that are coordinated through time. For instance, in our above example, multiple facets of self-regulation (self-regulation failures, self-efficacy, adherence, positive and negative affect, and diabetes problems) were all coordinated throughout time. Thus, understanding the temporal patterning of one variable such as self-regulation failures may depict the properties of the system across time. Coordination involves a model of data reduction in process throughout time in much the way that factor analysis involves data reduction in actual values at a single point in time.
Coordination models also highlight variables that are not coordinated, but have the ability to alter how coordination works. For example a variable that has the ability to strengthen the connections between variables or divorce them from one another has the potential to greatly alter trajectories in time. In contrast, a variable that is part of the coordination itself can potentially change behavior, but will likely be pulled back to the old state after some period of time because each part of the coordination process helps stabilize the observed pattern.
Summary
Coordination captures a variety of ways of depicting the emergent patterns in which elements move together through time. Such patterns can involve synchrony of varying degrees or periods of synchrony-like behavior with periods of asynchrony. Models of coordination do not require equal influence, but allow for asymmetries in the influences between elements. As a set, these models can depict the changing transactional relationships (parental involvement, self-regulation, diabetes management) for our developmental model through advanced statistical approaches for the study of change. These techniques articulate that when many elements are coordinated, the dance depicted through time can often be described by a single element. Thus, coordination is an argument for data reduction at the level of change processes through time rather than at the level of any moment in time.
Implications of Developmental Model of Parent-Child Coordination
The developmental model of parent-child coordination described here has numerous implications for work in chronic illness management behaviors as well as other domains of functioning (e.g., academic, social, and health risk behaviors) for families across development. This model holds a new perspective on the development of children as they develop management behaviors, noting the inextricable connection that developing individuals have with their parents and subsequently peers and romantic relationships. These connections form early in infancy and provide a foundation for the emergence of other relationships. The coordinative process is dynamic as new relationships enter the process and self-regulatory skills change. Both parent and child are active agents in this coordinative process and elements of their regulatory skills may push and pull the system throughout time. We now provide the implications of this model for future research in chronic illness management, interventions to improve management, and the generalizability of the model beyond the domain of chronic illness management.
A Developmental Approach to Research on Chronic Illness Management
The Developmental Model of Parent-Child Coordination highlights the importance of taking a developmental perspective to the examination of management across time. The importance of both longitudinal research as well as intensive measurements such as daily diary and experience sampling methodologies will allow for modeling the coordinative process across time. There is a need for the measurement of multiple constructs in order to understand which variables may act as magnet effects, that push and pull the system, as well as variables that are redundant with elements of parental involvement and self-regulatory skills of the child.
In addition to the inclusion of children’s self-regulatory skills and parents’ involvement, our model points to the importance of examining regulatory skills of the parent as well as of other close relationships (e.g., peers, romantic partners). For instance, the increased incidence of depressive symptoms in parents with chronic illnesses such as type 1 diabetes (Frank, Hagglund & Schopp, 1998; Jaser, et al., 2009) together with the disruptions that depressive symptoms may have on parental involvement in diabetes management (Wiebe, et al., 2011) is suggestive of the role of parental depressive symptoms in impairing parents’ skills. Depressive symptoms may undermine numerous parental self-regulatory skills essential for good parental involvement (e.g., reducing attention to child input and parental self-efficacy, increasing negative appraisals of children, activating low positive and high negative emotion) (J. M. Butler, et al., 2009; Dix & Meunier, 2009).
A developmental perspective also highlights that the time point in development when the family experiences the diagnosis of diabetes will hold implications for the development of regulatory skills and parenting skills. Type 1 diabetes is most frequently diagnosed during adolescence with the peak occurring around ages 10-14 years and an earlier peak at 4-6 years. A child diagnosed early in life will not have yet developed cognitive and emotional capacities that allow for certain coping responses (e.g., cognitive restructuring or secondary control strategies, see Compas, et al., 2012) or emotion regulation strategies (e.g., delay of gratification, inhibitory control) (see Eisenberg, et al., 2010). Thus, such capacities develop within the context of coping with a chronic illness rather than applying such capacities to the new context of chronic illness. When diagnosis occurs during adolescence, however, individuals may be able to apply well-developed emotional and cognitive regulatory skills to the new context of chronic illness (Masten & Cicchetti, 2010). For instance, Lansing et al. (2016) reported that adolescents’ performance in school was an excellent predictor of adherence to the diabetes regimen, suggesting that adolescents’ abilities to regulate a difficult task such as school work may be generalizable to the context of diabetes management. Furthermore, the dysregulating effects of hyper or hypoglycemia affect executive function abilities that are essential for the development of future regulatory skills (Gaudieri, Chen, Greer, & Holmes, 2008).
The timing of the diagnosis of illness may also affect the development of high quality parent-child relationships. The elevations in distress and depressive symptoms that many parents experience (Cline, Schwartz, Axelrad, & Anderson, 2011; Streisand et al., 2008) may affect their ability to parent in an effective manner, contributing to their inability to develop high quality relationships with their young child (Hammen, 2009) or make fine-tuned adjustments in parental involvement in response to increasing demands during adolescence (Wiebe, et al., 2011).
The developmental model outlined in this paper bridges the pediatric and adult literatures which depict disparate views of how individuals adapt to chronic illness in the context of the family. The literature during childhood has focused on how children manage their illness together with their parents, with the focus being on how adolescents gain independence so that they can emerge during adulthood with the competence to manage their illness independently of their parents (Weissberg-Benchell, et al., 2007). However, the adult literature characterizes individuals as being connected with other close relationships (most especially the spouse) such that dyadic appraisal and coping are important elements of dealing with chronic illnesses throughout adulthood (Berg & Upchurch, 2007; Bodenmann, 2005; Revenson, et al., 2005). The current model bridges this gap by noting how the parent-child relationship serves as a training ground for the development of peer and romantic relationships that adolescents and emerging adults utilize as they develop long term relationships that they can draw on for coordination across adulthood. This model is embedded within a life-span perspective as to how individuals seek and receive support across development (Uchino, 2009) and as such traces the early relational history that may be important for understanding dyadic coping across the adult life span (see also Donato, Iafrate, Bradbury, & Scabini, 2012; Repetti, et al., 2002; Wiebe, Helgeson, & Berg, 2016).
A New Perspective on Interventions
Based upon this developmental model of parent-child coordination for the emergence of regulatory skills, there are multiple implications for psychosocial interventions. First, our model asserts that the emergence of clinical problems associated with disrupted self-regulation is attributable to patterns of coordination across parents and children over time. For example, a common clinical presentation in a child with diabetes who is non-adherent includes a child with less effective self-regulatory skills and a family higher in conflict and stress (Ellis et al., 2005). Second, our model also suggests that the changes underlying effective interventions are, in fact, the re-organizations of initial patterns of coordination linked with non-adherence (e.g., poor self-regulatory skills and impaired family functioning) into new patterns of coordination. These new patterns of coordination contribute to the emergence of improved self-regulation and decreased clinical problems. For example, if a multicomponent intervention for adolescents with poor adherence effectively targets both youth self-regulation and parent monitoring to improve adherence, the changes in coordination patterns among those characteristics would be evidenced in two key ways: (1) initial destabilization of the problematic pattern of coordination (caused by the intervention) and (2) restabilization of a new pattern of coordination resulting in the emergence of improved self-regulation, more parental monitoring and better adherence, with step 2 being the key for identifying a durable intervention effect.
These notions imply multiple future directions for clinical research, as we seek to identify new interventions or assess change mechanisms in current interventions. Clinical researchers will need to identify patterns of coordination that contribute to the presenting clinical problem, and identify patterns of coordination that contribute to stable and long-term improvements. This would include research on how to effect re-organization in patterns of coordination into patterns that contribute to the emergence of long-term stability and improvements in the clinical problem (see Granic, O'Hara, Pepler, & Lewis, 2007). To this end, we must identify which variables hinder re-organization of initial patterns of coordination by stabilizing and maintaining those patterns. Also, we must research which variables - when modified by intervention - contribute to the de-stabilization of the initial pattern of coordination and support re-organization into a new pattern that is associated with stable and long-term change.
For example, some interventions to improve diabetes management in adolescence have had stable effects in increasing adherence behaviors, but not in improving metabolic control (Ellis et al., 2007), or only improving metabolic control for particular groups (e.g., middle adolescents; Nansel, et al., 2009). This would suggest that the new pattern of coordination resulting from the intervention was unstable and not maintained over-time, or was a stable pattern that did not contribute to the emergence of long-term changes in metabolic control. The efficacy of such interventions would improve by identifying variables that are most highly influential to re-organizing patterns of coordination into stable patterns that contribute to the emergence of good metabolic control. It is important to note that these key variables may not necessarily be those variables that are most predictive of the outcome, but are those that contribute most to the stability of the desired pattern of coordination. Also, these key variables may be unique in different periods of the development of the child and the parent, and within particular patterns of coordination occurring within families. This may explain group or individual differences in intervention efficacy.
Finally, many existing interventions may already be accomplishing the task of re-organizing patterns of coordination, but we simply have not studied this notion within those interventions. Evidence based-interventions that modify variables within the child, the parent and the family will remain essential to treatment (Ellis, Templin, et al., 2007; Wysocki, Harris, et al., 2008). Our model provides a new way of conceptualizing the mechanisms underlying effective change in clinical interventions in that they are examined as creating different patterns of coordination over time. Our model also points to additional ways to understand and address interventions that are relatively ineffective.
Generalizability To Other Domains of Family Functioning and Child Development
The Developmental Model of Parent-Child Coordination for Self-Regulation described in this paper was situated in the context of families where a child has type 1 diabetes. We chose this context as type 1 diabetes is a chronic illness that poses daily regulatory challenges for parents and children and a large literature exists demonstrating the importance of parental involvement. However, we expect that the major principles and benefits of this developmental approach will extend to other pediatric chronic illnesses (e.g., asthma, spina bifida, pediatric cancer). For instance, adherence to the regimen for spina bifida is best when children’s low self-regulatory skills are matched with high parental involvement (O'Hara & Holmbeck, 2013). Similar results have been theorized for the case of pediatric cancer as well (Peterson & Drotar, 2006). Links between family functioning, child self-regulation, and illness management have also been found for asthma (Rhee et al., 2010). Such links between parental involvement and children’s self-regulatory skills also eventuate in different trajectories (e.g., risky family trajectory) with respect to physical health for those without a specific chronic illness condition (Repetti, et al., 2002).
Given the ubiquity of effective parental involvement and self-regulation in broad domains outside of the context of chronic illness (Moffitt, et al., 2011), we also expect that this model will readily generalize to other domains of parent and child coordinations. A sizable literature has examined bi-directional relationships between parental involvement and child psychopathology, with some research noting the importance of rigidity in parent-child interactions as a pattern consistent with externalizing problems (Hollenstein, et al., 2004). Relatedly, Granic and Patterson (2006) have reconceptualized the pattern of family coercion and related adolescent cognitions such as the hostile attribution bias from a dynamic systems perspective, noting that this recurrent pattern becomes stabilized in the system. Belsky, Pasco Fearon, and Bell (2007) found that early maternal sensitivity was associated with fewer child externalizing behaviors through better child attention control, which was also associated with enhanced parenting over time. The crucial role of early parent-child coordinations for maintaining children on trajectories of psychopathology and conduct disorders (Belsky, et al., 2007; Masten & Cicchetti, 2010; Pardini, et al., 2008) is consistent with our approach and this literature has been used extensively throughout this paper.
Further, a large body of research has examined parental involvement and self-regulation as important in academic performance (Blair & Diamond, 2008; Bowers et al., 2011; Grolnick, Benjet, Kurowski, & Apostoleris, 1997). Transactions between children’s academic performance and parents’ intrusive support have been found such that children’s low academic achievement may elicit maladaptive maternal involvement, which may be associated with at least short-term gains in performance (Pomerantz & Eaton, 2001). Such coordinations are also being explored between parents and adolescents as two interrelated identity systems in the emergence of identity development during adolescence and young adulthood (Koepke & Denissen, 2012).
Summary and Conclusions
In sum, the developmental model of parent-child coordination for self-regulation in type 1 diabetes integrates and extends the literature in important ways by noting the inextricable ties between parents and children that are initiated in infancy, extend into adolescence, and are transformed as new relationships enter the coordinative system. This systems perspective to parental involvement, children’s self-regulatory skill, and illness management offers new ways of viewing the development of parent and child across development that highlights the mutual influence between parent and child rather than a particular direction of causality. The perspective also presents a life-span perspective to illness management that highlights how self-regulation and illness management are embedded in a rich and changing landscape of interpersonal relationships across development.
Acknowledgments
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (Grant Numbers R01DK092939 and R01DK063044). Amy Hughes Lansing is now in the Department of Psychology at the University of Nevada at Reno. Jorie Butler is at the Veterans Administration at Salt Lake City.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ainsworth MDS (1991). Attachments and other affectional bonds across the life cycle. In Parkes CM, Stevenson-Hinde J & Marris P (Eds.), Attachment across the life cycle (pp. 33–51). New York, NY: Tavistock/Routledge. [Google Scholar]
- Allen JP, & Manning N (2007). From safety to affect regulation: Attachment from the vantage point of adolescence. New Directions for Child and Adolescent Development (117), 23–39. doi: 10.1002/cd.192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP, McElhaney KB, Land DJ, Kuperminc GP, Moore CW, O'Beirne-Kelly H, & Kilmer SL (2003). A secure base in adolescence: Markers of attachment security in the mother-adolescent relationship. Child Development, 74(1), 292–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP, Porter M, McFarland C, McElhaney KB, & Marsh P (2007). The relation of attachment security to adolescents' paternal and peer relationships, depression, and externalizing behavior. Child Development, 78(4), 1222–1239. doi: 10.1111/j.1467-8624.2007.01062.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almas AN, Grusec JE, & Tackett JL (2011). Children's disclosure and secrecy: Links to maternal parenting characteristics and children's coping skills. Social Development, 20(3), 624–643. doi: 10.1111/j.1467-9507.2010.00602.x [DOI] [Google Scholar]
- Anderson BJ, Auslander WF, Jung KC, Miller JP, & Santiago JV (1990). Assessing family sharing of diabetes responsibilities. Journal of Pediatric Psychology, 15, 477–492. [DOI] [PubMed] [Google Scholar]
- Anderson BJ, Ho J, Brackett J, Finkelstein D, & Laffel L (1997). Parent involvement in diabetes management tasks: Relationships to blood glucose monitoring adherence and metabolic control in young adolescents with insulin-dependent diabetes mellitus. The Journal of Pediatrics, 130(2), 257–265. [DOI] [PubMed] [Google Scholar]
- Anderson BJ, Holmbeck G, Iannotti RJ, McKay SV, Lochrie A, Volkening LK, & Laffel L (2009). Dyadic measures of the parent-child relationship during the transition to adolescence and glycemic control in children with type 1 diabetes. Families, Systems, & Health, 27(2), 141–152. doi: 10.1037/a0015759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson BJ, Vangness L, Connell A, Butler D, Goebel-Fabbri A, & Laffel LM (2002). Family conflict, adherence, and glycaemic control in youth with short duration type 1 diabetes. Diabetic Medicine, 19(8), 635–642. [DOI] [PubMed] [Google Scholar]
- Armstrong B, Mackey ER, & Streisand R (2011). Parenting behavior, child functioning, and health behaviors in preadolescents with type 1 diabetes. Journal of Pediatric Psychology, 36(9), 1052–1061. doi: 10.1093/jpepsy/jsr039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Band EB, & Weisz JR (1990). Developmental differences in primary and secondary control coping and adjustment to juvenile diabetes. Journal of Clinical Child Psychology, 19(2), 150–158. doi: 10.1207/s15374424jccp1902_7 [DOI] [Google Scholar]
- Barzel M, & Reid GJ (2011). Coparenting in relation to children's psychosocial and diabetes-specific adjustment. Journal of Pediatric Psychology, 36(5), 618–629. doi: 10.1093/jpepsy/jsr022 [DOI] [PubMed] [Google Scholar]
- Baumeister RF, Vohs KD, & Tice DM (2007) The strength model of self-control. Current Directions in Psychological Science, 16, 351–355. [Google Scholar]
- Bearman KJ, & La Greca AM (2002). Assessing friend support of adolescents' diabetes care: The diabetes social support questionnaire-friends version. Journal of Pediatric Psychology, 27(5), 417–428. [DOI] [PubMed] [Google Scholar]
- Beek PJ, & Beek WJ (1988). Tools for constructing dynamical models of rhythmic movement. Human Movement Science, 7, 301–342. doi: 10.1016/0167-9457(88)90015-2. [DOI] [Google Scholar]
- Bell RQ (1968). A reinterpretation of the direction of effects in studies of socialization. Psychological Review, 75(2), 81–95. doi: 10.1037/h0025583 [DOI] [PubMed] [Google Scholar]
- Belsky J, & Beaver KM (2011). Cumulative-genetic plasticity, parenting and adolescent self-regulation. Journal of Child Psychology and Psychiatry, 52(5), 619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J, Pasco Fearon RM, & Bell B (2007). Parenting, attention and externalizing problems: Testing mediation longitudinally, repeatedly and reciprocally. Journal of Child Psychology and Psychiatry, 48(12), 1233–1242. doi: 10.1111/j.1469-7610.2007.01807.x [DOI] [PubMed] [Google Scholar]
- Berg CA, Butler JM, Osborn P, King G, Palmer DL, Butner J, … Wiebe DJ (2008). Role of parental monitoring in understanding the benefits of parental acceptance on adolescent adherence and metabolic control of type 1 diabetes. Diabetes Care, 31(4), 678–683. doi: 10.2337/dc07-1678 [DOI] [PubMed] [Google Scholar]
- Berg CA, Butner JE, Butler JM, King PS, Hughes AE, & Wiebe DJ (2013). Parental persuasive strategies in the face of daily problems in adolescent type 1 diabetes management. Health Psychology, 32(7), 719–728. doi: 10.1037/a0029427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Butner JE, Turner SL, Lansing AH, King P, & Wiebe DJ (2016) Adolescents’, mothers’, and fathers’ reports of adherence across adolescence and their relation to diabetes management. Journal of Behavioral Medicine, 39, 1009–1019. [DOI] [PubMed] [Google Scholar]
- Berg CA, King PS, Butler JM, Pham P, Palmer D, & Wiebe DJ (2011). Parental involvement and adolescents' diabetes management: the mediating role of self-efficacy and externalizing and internalizing behaviors. Journal of Pediatric Psychology, 36(3), 329–339. doi: 10.1093/jpepsy/jsq088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, Queen TL, Butner JE, Turner SL, & Lansing AH, Main A, Anderson J, Thoma B, Winnick J, & Wiebe DJ, (2017). Adolescent disclosure to parents and daily management of type 1 diabetes. Journal of Pediatric Psychology, 42, 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg CA, & Upchurch R (2007). A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin, 133(6), 920–954. doi: 10.1037/0033-2909.133.6.920 [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Beveridge RM, Palmer DL, Korbel CD, Upchurch R, … Donaldson DL (2007). Mother child appraised involvement in coping with diabetes stressors and emotional adjustment. Journal of Pediatric Psychology, 32(8), 995–1005. doi: 10.1093/jpepsy/jsm043 [DOI] [PubMed] [Google Scholar]
- Bernieri F, Reznick JS, & Rosenthal R (1988). Synchrony, pseudosynchrony, and dissynchrony: Measuring the entrainments process in mother-infant interactions. Journal of Personality and Social Psychology, 54, 243–253. [Google Scholar]
- Beveridge RM, & Berg CA (2007). Parent–adolescent collaboration: An interpersonal model for understanding optimal interactions. Clinical Child and Family Psychology Review, 10(1), 25–52. doi: 10.1007/s10567-006-0015-z [DOI] [PubMed] [Google Scholar]
- Beyers W, & Seiffge-Krenke I (2007). Are friends and romantic partners the 'best medicine?' How the quality of other close relations mediates the impact of changing family relationships on adjustment. International Journal of Behavioral Development, 31(6), 559–568. doi: 10.1177/0165025407080583 [DOI] [Google Scholar]
- Biringen Z, & Easterbrooks MA (2012). A developmental psychopathology perspective on emotional availability research. Development and Psychopathology, 24, 1–8. doi: 10.1017/S0954579411000617 [DOI] [PubMed] [Google Scholar]
- Blair C, & Diamond A (2008). Biological processes in prevention and intervention: The promotion of self-regulation as a means of preventing school failure. Development and Psychopathology, 20(03), 899–911. doi: 10.1017/s0954579408000436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenmann G (2005). Dyadic coping and its significance for marital functioning. In Revenson TA, Kayser K & Bodenmann G (Eds.), Couples coping with stress: Emerging perspectives on dyadic coping (pp. 33–50). Washington, DC: American Psychological Association. [Google Scholar]
- Boker SM, & Laurenceau J-P (2006). Dynamical systems modeling: An application to the regulation of intimacy and disclosure in marriage. In Walls TA & Schafer JL (Eds.), Models for intensive longitudinal data (pp. 195–218). New York: Oxford University Press. [Google Scholar]
- Boker SM, Neale M, Maes H, Wilde M, Spiegel M, Brick T, … Fox J (2011). OpenMx: An open source extended structural equation modeling framework. Psychometrika, 76(2), 306–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botello-Harbaum M, Nansel T, Haynie DL, Iannotti RJ, & Simons-Morton B (2008). Responsive parenting is associated with improved type 1 diabetes-related quality of life. Child: Care, Health and Development, 34(5), 675–681. doi: 10.1111/j.1365-2214.2008.00855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers EP, Gestsdottir S, Geldhof GJ, Nikitin J, von Eye A, & Lerner RM (2011). Developmental trajectories of intentional self regulation in adolescence: The role of parenting and implications for positive and problematic outcomes among diverse youth. Journal of Adolescence, 34(6), 1193–1206. doi: 10.1016/j.adolescence.2011.07.006 [DOI] [PubMed] [Google Scholar]
- Bowlby J (1969). Attachment and loss: Volume I: Attachment (Vol. 1). London, UK: The Hogarth Press and The Institute of Psycho-Analysis. [Google Scholar]
- Bowlby J (1989). The role of attachment in personality development and psychopathology. In Greenspan SI & Pollock GH (Eds.), The course of life. Vol. 1: Infancy (pp. 229–270). Madison, CT: International Universities Press, Inc. [Google Scholar]
- Branstetter SA, Furman W, & Cottrell L (2009). The influence of representations of attachment, maternal-adolescent relationship quality, and maternal monitoring on adolescent substance use: A 2-year longitudinal examination. Child Development, 80(5), 1448–1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bretherton I (1987). New perspectives on attachment relations: Security, communication, and internal working models. In Osofsky JD (Ed.), Handbook of infant development (2nd ed., pp. 1061–1100). Oxford, England: John Wiley & Sons. [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. doi: 10.1037/0003-066x.32.7.513 [DOI] [Google Scholar]
- Bryden KS, Peveler RC, Stein A, Neil A, Mayou RA, & Dunger DB (2001). Clinical and psychological course of diabetes from adolescence to young adulthood. Diabetes Care, 24(9), 1536–1540. [DOI] [PubMed] [Google Scholar]
- Bumpus MF, & Hill LG (2008). Secrecy and parent-child communication during middle childhood: Associations with parental knowledge and child adjustment. Parenting: Science and Practice, 8(2), 93–116. doi: 10.1080/15295190802058868 [DOI] [Google Scholar]
- Burroughs TE, Harris MA, Pontious SL, & Santiago JV . (1997). Research on social support in adolescents with IDDM: A critical review. The Diabetes Educator, 23(4), 438–448. doi: 10.1177/014572179702300409 [DOI] [PubMed] [Google Scholar]
- Butler EA (2011). Temporal interpersonal emotion systems: the "TIES" that form relationships. Personality and Social Psychology Review, 15(4), 367–393. doi: 10.1177/1088868311411164 [DOI] [PubMed] [Google Scholar]
- Butler JM, Berg CA, King P, Gelfand D, Fortenberry K, Foster C, & Wiebe D (2009). Parental negative affect and adolescent efficacy for diabetes management. Journal of Family Psychology, 23(4), 611–614. doi: 10.1037/a0016141 [DOI] [PubMed] [Google Scholar]
- Butler JM, Fortenberry KT, Berg CA, McCabe J, Blakemore T, & Wiebe DJ (2011). Early adolescents' goals and mothers' accuracy in predicting adolescent goals in the context of type 1 diabetes. Children's Health Care, 40(2), 155–169. doi: 10.1080/02739615.2011.564940 [DOI] [Google Scholar]
- Butler JM, Skinner M, Gelfand D, Berg CA, & Wiebe DJ (2007). Maternal parenting style and adjustment in adolescents with type I diabetes. Journal of Pediatric Psychology, 32(10), 1227–1237. doi: 10.1093/jpepsy/jsm065 [DOI] [PubMed] [Google Scholar]
- Butner J, Amazeen P, & Mulvey G (2005). Growth modeling of two cyclical processes: Extending differential structural equation modeling to coupled systems. Psychological Methods, 10 (2), 159–177. [DOI] [PubMed] [Google Scholar]
- Butner JE, Berg CA, Baucom B, & Wiebe DJ (2014). Modeling coordination in multiple simultaneous latent difference scores. Multivariate Behavioral Research, 49, 554–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butner J, Berg CA, Wiebe DA, Lansing AH, Munion A & Turner S (in press). Coordination of self and social regulation surrounding type 1 diabetes management in late adolescence. Annals of Behavioral Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butner J, Diamond LM, & Hicks AM (2007). Attachment style and two forms of affect coregulation between romantic partners. Personal Relationships, 14, 431–455. [Google Scholar]
- Cahill P, & Papageorgiou A (2007). Triadic communication in the primary care pediatric consultation: A review of the literature. British Journal of General Practice, 904–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, & Leerkes EM (2011). Early attachment processes and the development of emotional self-regulation. In Vohs KD & Baumeister RF (Eds.), Handbook of self-regulation: Research, theory, and applications (2nd ed., pp. 355–373). New York, NY: Guilford Press. [Google Scholar]
- Carcone AI, Ellis DA, Weisz A, & Naar-King S (2011). Social support for diabetes illness management: Supporting adolescents and caregivers. Journal of Developmental and Behavioral Pediatrics, 32(8), 581–590. doi: 10.1097/DBP.0b013e31822c1a27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson EA, & Sroufe LA (1995). Contribution of attachment theory to developmental psychopathology. In Cicchetti D & Cohen DJ (Eds.), Developmental Psychopathology, Vol. 1: Theory and Methods (pp. 581–617). Oxford, England: John Wiley & Sons. [Google Scholar]
- Cassidy J, & Kobak RR (1988). Avoidance and its relation to other defensive processes. In Belsky J & Nezworski T (Eds.), Clinical implications of attachment (pp. 300–323). Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Chisholm V, Atkinson L, Donaldson C, Noyes K, Payne A, & Kelnar C (2011). Maternal communication style, problem-solving and dietary adherence in young children with type 1 diabetes. Clinical Child Psychology and Psychiatry, 16(3), 443–458. doi: 10.1177/1359104510373312 [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Hirsch IB, & Katon WJ (2002). Interpersonal predictors of HbA1C in patients with type 1 diabetes. Diabetes Care, 25(4), 731–736. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, & Katon WJ (2006). The interpersonal experience of health care through the eyes of patients with diabetes. Social Science & Medicine, 63(12), 3067–3079. doi: 10.1016/j.socscimed.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Katon WJ, Russo JE, & Walker EA (2001). The patient-provider relationship: Attachment theory and adherence to treatment in diabetes. The American Journal of Psychiatry, 158(1), 29–35. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Russo J, Katon W, Lin EHB, Ludman E, Heckbert S, … Young BA (2010). Relationship styles and mortality in patients with diabetes. Diabetes Care, 33(3), 539–544. doi: 10.2337/dc09-1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciechanowski P, Russo J, Katon W, Simon G, Ludman E, Von Korff M, … Lin E (2006). Where is the patient? The association of psychosocial factors and missed primary care appointments in patients with diabetes. General Hospital Psychiatry, 28(1), 9–17. doi: 10.1016/j.genhosppsych.2005.07.004 [DOI] [PubMed] [Google Scholar]
- Ciechanowski P, Russo J, Katon W, Von Korff M, Ludman E, Lin E, … Bush (2004). Influence of patient attachment style on self-care and outcomes in diabetes. Psychosomatic Medicine, 66(5), 720–728. doi: 10.1097/01.psy.0000138125.59122.23 [DOI] [PubMed] [Google Scholar]
- Cline GD, Schwartz DD, Axelrad ME, & Anderson B (2011). A pilot study of acute stress symptoms in parents and youth following diagnosis of type I diabetes. Journal of Clinical Psychology in Medical Settings, 18(4), 416–422. doi: 10.1007/s10880-011-9266-z [DOI] [PubMed] [Google Scholar]
- Cohen DM, Lumley MA, Naar-King S, Partridge T, & Cakan N (2004). Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: A prospective study. Journal of Pediatric Psychology, 29, 171–184. [DOI] [PubMed] [Google Scholar]
- Coleman PK, & Watson A (2000). A reply to commentaries on ‘Infant attachment as a dynamic system.’ Human Development, 43, 327–331. [Google Scholar]
- Collins WA, Welsh DP, & Furman W (2009). Adolescent romantic relationships. Annual Review of Psychology, 60(1), 631–652. doi: 10.1146/annurev.psych.60.110707.163459 [DOI] [PubMed] [Google Scholar]
- Compas BE, Jaser SS, Dunn MJ, & Rodriguez EM (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8(1), 455–480. doi: 10.1146/annurev-clinpsy-032511-143108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger KJ, Williams ST, Little WM, Masyn KE, & Shebloski B (2009). Development of mastery during adolescence: The role of family problem-solving. Journal of Health and Social Behavior, 50(1), 99–114. doi: 10.1177/002214650905000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox ED, Smith MA, Brown RL, & Fitzpatrick MA (2009). Learning to participate: Effect of child age and parental education on participation in pediatric visits. Health Communication, 24(3), 249–258. doi: 10.1080/10410230902804141 [DOI] [PubMed] [Google Scholar]
- Coyne I (2008). Children's participation in consultations and decision-making at health service level: A review of the literature. International Journal of Nursing Studies, 45(11), 1682–1689. doi: 10.1016/j.ijnurstu.2008.05.002 [DOI] [PubMed] [Google Scholar]
- Croom A, Wiebe DJ, Berg CA, Lindsay R, Donaldson D, Foster C, … Swinyard MT (2010). Adolescent and parent perceptions of patient-centered communication while managing type 1 diabetes. Journal of Pediatric Psychology, 36(2), 206–215. doi: 10.1093/jpepsy/jsq072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumsille P, Darling N, & Martinez ML (2010). Shading the truth: The patterning of adolescents' decisions to avoid issues, disclose, or lie to parents. Journal of Adolescence, 33(2), 285–296. [DOI] [PubMed] [Google Scholar]
- Darling N, Cumsille P, Caldwell LL, & Dowdy B (2006). Predictors of adolescents' disclosure to parents and perceived parental knowledge: Between- and within-person differences. Journal of Youth and Adolescence, 35(4), 659–670. [Google Scholar]
- Davis CL, Delamater AM, Shaw KH, La Greca AM, Eidson MS, Perez-Rodriguez JE, & Nemery R (2001). Parenting styles, regimen adherence, and glycemic control in 4- to 10- year-old children with diabetes. Journal of Pediatric Psychology, 26(2), 123–129. [DOI] [PubMed] [Google Scholar]
- De Civita M, & Dobkin PL (2004). Pediatric adherence as a multidimensional and dynamic construct, involving a triadic partnership. Journal of Pediatric Psychology, 29(3), 157–169. [DOI] [PubMed] [Google Scholar]
- De Goede IHA, Branje SJT, Delsing MJMH, & Meeus WHJ (2009). Linkages over time between adolescents' relationships with parents and friends. Journal of Youth and Adolescence, 38(10), 1304–1315. doi: 10.1007/s10964-009-9403-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delamater AM, Smith JA, Kurtz SM, & White NH (1988). Dietary skills and adherence in children with type I diabetes mellitus. The Diabetes Educator, 14(1), 33–36. [DOI] [PubMed] [Google Scholar]
- Diamond LM, & Fagundes CP (2010). Psychobiological research on attachment. Journal of Social and Personal Relationships, 27(2), 218–225. doi: 10.1177/0265407509360906 [DOI] [Google Scholar]
- Dinero RE, Conger RD, Shaver PR, Widaman KF, & Larsen-Rife D (2008). Influence of family of origin and adult romantic partners on romantic attachment security. Journal of Family Psychology, 22(4), 622–632. doi: 10.1037/a0012506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, & McMahon RJ (1998). Parental monitoring and the prevention of child and adolescent problem behavior: A conceptual and empirical formulation. Clinical Child and Family Psychology Review, 1(1), 61–75. [DOI] [PubMed] [Google Scholar]
- Dix T (1991). The affective organization of parenting: Adaptive and maladaptive processes. Psychological Bulletin, 110(1), 3–25. [DOI] [PubMed] [Google Scholar]
- Dix T, & Meunier LN (2009). Depressive symptoms and parenting competence: An analysis of 13 regulatory processes. Developmental Review, 29(1), 45–68. doi: 10.1016/j.dr.2008.11.002 [DOI] [Google Scholar]
- Donato S, Iafrate R, Bradbury TN, & Scabini E (2012). Acquiring dyadic coping: Parents and partners as models. Personal Relationships, 19(2), 386–400. doi: 10.1111/j.1475-6811.2011.01368.x [DOI] [Google Scholar]
- Drew LM, Berg CA, & Wiebe DJ (2010). The mediating role of extreme peer orientation in the relationships between adolescent–parent relationship and diabetes management. Journal of Family Psychology, 24(3), 299–306. doi: 10.1037/a0019352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drotar D (2009). Physician behavior in the care of pediatric chronic illness: Association with health outcomes and treatment adherence. Journal of Developmental and Behavioral Pediatrics, 30(3), 246–254. [DOI] [PubMed] [Google Scholar]
- Eckshtain D, Ellis DA, Kolmodin K, & Naar-King S (2010). The effects of parental depression and parenting practices on depressive symptoms and metabolic control in urban youth with insulin dependent diabetes. Journal of Pediatric Psychology, 35(4), 426–435. doi: 10.1093/jpepsy/jsp068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, & Eggum ND (2010). Emotion-related self-regulation and its relation to children's maladjustment. Annual Review of Clinical Psychology, 6(1), 495–525. doi: 10.1146/annurev.clinpsy.121208.131208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DA, Frey MA, Naar-King S, Templin T, Cunningham PB, & Cakan N . (2005). The effects of multisystemic therapy on diabetes stress among adolescents with chronically poorly controlled type 1 diabetes: findings from a randomized, controlled trial. Pediatrics, 116(6), e826–e832. [DOI] [PubMed] [Google Scholar]
- Ellis DA, Podolski CL, Frey M, Naar-King S, Wang B, & Moltz K (2007). The role of parental monitoring in adolescent health outcomes: Impact on regimen adherence in youth with type 1 diabetes. Journal of Pediatric Psychology, 32(8), 907–917. doi: 10.1093/jpepsy/jsm009 [DOI] [PubMed] [Google Scholar]
- Ellis DA, Templin TN, Naar-King S, & Frey MA (2008). Toward conceptual clarity in a critical parenting construct: Parental monitoring in youth with chronic illness. Journal of Pediatric Psychology, 33(8), 799–808. doi: 10.1093/jpepsy/jsn044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis DA, Templin T, Naar-King S, Frey MA, Cunningham PB, Podolski C, & Cakan N (2007). Multisystemic therapy for adolescents with poorly controlled type I diabetes: Stability of treatment effects in a randomized controlled trial. Journal of Consulting and Clinical Psychology, 75(1), 168–174. doi: 10.1037/0022-006x.75.1.168 [DOI] [PubMed] [Google Scholar]
- Etzion-Carasso A, & Oppenheim D (2000). Open mother–pre-schooler communication: Relations with early secure attachment. Attachment & Human Development, 2(3), 347–370. doi: 10.1080/14616730010007914 [DOI] [PubMed] [Google Scholar]
- Evans CA, & Porter CL (2009). The emergence of mother- infant co-regulation during the first year: Links to infants’ developmental status and attachment. Infant Behavior and Development, 32, 147–158. doi: 10.1016/j.infbeh.2008.12.005 [DOI] [PubMed] [Google Scholar]
- Fletcher AC, Steinberg L, & Williams-Wheeler M (2004). Parental influences on adolescent problem behavior: Revisiting Stattin and Kerr. Child Development, 75(3), 781–796. doi: 10.1111/j.1467-8624.2004.00706.x [DOI] [PubMed] [Google Scholar]
- Fogel A (1993). Developing through relationships: Origins of communications, self, and culture. Chicago: The University of Chicago Press. [Google Scholar]
- Fogel A (2011). Theoretical and applied dynamic systems research in developmental science. Child Development Perspectives, 5(4), 267–272. doi: 10.1111/j.1750-8606.2011.00174.x [DOI] [Google Scholar]
- Fortenberry KT, Butler JM, Butner J, Berg CA, Upchurch R, & Wiebe DJ (2009). Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine, 37(1), 1–9. doi: 10.1007/s12160-009-9086-7 [DOI] [PubMed] [Google Scholar]
- Frank RG, Hagglund KJ, & Schopp LH (1998). Disease and family contributors to adaptation in juvenile rheumatoid arthritis and juvenile diabetes. Arthritis Care and Research, 11, 166–176. [DOI] [PubMed] [Google Scholar]
- Frijns T, Keijsers L, Branje S, & Meeus W (2010). What parents don't know and how it may affect their children: Qualifying the disclosure-adjustment link. Journal of Adolescence, 33(2), 261–270. [DOI] [PubMed] [Google Scholar]
- Froisland DH, Olsen SF, Robinson CC, & Mandleco BL . (2012). Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones: mixed-methods study. Journal of Medical Internet Research, 14(4), e111. doi: 10.2196/jmir.2155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallant MP (2003). The influence of social support on chronic illness self-management: A review and directions for research. . Health Education & Behavior, 30(2), 170–195. [DOI] [PubMed] [Google Scholar]
- Gaudieri PA, Chen R, Greer TF, & Holmes CS (2008). Cognitive function in children with type 1 diabetes: A meta-analysis. Diabetes Care, 31(9), 1892–1897. doi: 10.2337/dc07-2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavin LA, Wamboldt MZ, Sorokin N, Levy SY, & Wamboldt FS (1999). Treatment alliance and its association with family functioning, adherence, and medical outcome in adolescents with severe, chronic asthma. Journal of Pediatric Psychology, 24(4), 355–365. doi: 10.1093/jpepsy/24.4.355 [DOI] [PubMed] [Google Scholar]
- Gilliom M, Shaw D, Beck JE, Schonberg MA, & Lukon JL (2002). Anger regulation in disadvantaged preschool boys: Strategies, antecedents, and the development of self-control. Developmental Psychology, 38, 222–235. [DOI] [PubMed] [Google Scholar]
- Grabill K, Geffken GR, Duke DC, Lewin AB, Williams LB, Storch EA, & Silverstein JH (2010). Family functioning and adherence in youth with type 1 diabetes: A latent growth model of glycemic control. Children's Health Care, 39(4), 279–295. doi: 10.1080/02739615.2010.515930 [DOI] [Google Scholar]
- Granic I (2000). The self-organization of parent-child relations: Beyond bidirectional models. In Lewis MA & Granic I (Eds.), Emotion, development, and self-organization: Dynamic systems approaches to emotional development (pp. 267–297.). New York, NY: Cambridge University Press. [Google Scholar]
- Granic I, Hollenstein T, Dishion TJ, & Patterson GR (2003). Longitudinal analysis of flexibility and reorganization in early adolescence: A dynamic systems study of family interactions. Developmental Psychology, 39(3), 606–617. [DOI] [PubMed] [Google Scholar]
- Granic I, O'Hara A, Pepler D, & Lewis MD (2007). A dynamic systems analysis of parent-child changes associated with successful 'real-world' interventions for aggressive children. Journal of Abnormal Child Psychology, 35, 845–857. [DOI] [PubMed] [Google Scholar]
- Granic I, & Patterson GR (2006). Toward a comprehensive model of antisocial development: A dynamic systems approach. Psychological Review, 113(1), 101–131. doi: 10.1037/0033-295X.113.1.101 [DOI] [PubMed] [Google Scholar]
- Grey M, Whittemore R, Jaser S, Ambrosino J, Lindemann E, Liberti L, … Dziura J (2009). Effects of coping skills training in school-age children with type 1 diabetes. Research in Nursing & Health, 32(4), 405–418. doi: 10.1002/nur.20336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grolnick WS, Benjet C, Kurowski CO, & Apostoleris NH (1997). Predictors of parent involvement in children's schooling. Journal of Educational Psychology, 89(3), 538–548. doi: 10.1037/0022-0663.89.3.538 [DOI] [Google Scholar]
- Grundy AM, Gondoli DM, & Salafia EHB (2010). Maternal knowledge and maternal behavior control as predictors of preadolescent behavioral competence. The Journal of Early Adolescence, 30(3), 410–431. doi: 10.1177/0272431609333302 [DOI] [Google Scholar]
- Guastello SJ, & Gregson RAM (Eds.). (2011). Nonlinear dynamical systems analysis for the behavioral sciences using real data. Boca Raton, FL: C R C Press/Taylor & Francis. [Google Scholar]
- Hains AA, Berlin KS, Davies WH, Sato AF, Smothers MK, Clifford LC, & Alemzadeh R (2007). Attributions of teacher reactions to diabetes self-care behaviors. Journal of Pediatric Psychology, 34(1), 97–107. doi: 10.1093/jpepsy/jsn041 [DOI] [PubMed] [Google Scholar]
- Hamaker EL, Zhang Z, & van der Maas HLJ (2009). Dyads as dynamic systems: Using threshold autoregressive models to study dyadic interactions. Psychometrika, 74(4), 727–745. [Google Scholar]
- Hammen CL (2009). Children of depressed parents. Handbook of depression, 2, 275–297. [Google Scholar]
- Hamza CA, & Willoughby T (2011). Perceived parental monitoring, adolescent disclosure, and adolescent depressive symptoms: A longitudinal examination. Journal of Youth and Adolescence, 40(7), 902–915. [DOI] [PubMed] [Google Scholar]
- Hanna KM, Weaver MT, Stump TE, DiMeglio LA, Miller AR, Crowder S, & Fortenberry JD (2011). Initial findings: primary diabetes care responsibility among emerging adults with type 1 diabetes post high school and move out of parental home. Child: Care, Health, and Development, 39, 61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna KM, Weaver MT, & Stump TE, Guthrie D, & Oruche UM (2014). Emerging adults with type 1 diabetes during the first year post-high school: Perceptions of parental behaviors. Emerging Adulthood, 2, 128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen JA, Weissbrod C, Schwartz DD, & Taylor WP (2012). Paternal involvement in pediatric Type 1 diabetes: fathers' and mothers' psychological functioning and disease management. Fam Syst Health, 30(1), 47–59. doi: 10.1037/a0027519 [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Lopez LC, & Kamarck T (2009). Peer relationships and diabetes: Retrospective and ecological momentary assessment approaches. Health Psychology, 28(3), 273–282. doi: 10.1037/a0013784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Palladino DK, Reynolds KA, Becker D, Escobar O, Siminerio L (2014). Early adolescent relationship predictors of emerging adult outcomes: Youth with and without type 1 diabetes. Annals of Behavioral Medicine, 47, 270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Palladino DK, Reynolds KA, Becker DJ, Oscobar O, & Siminerio L (2014). Relationships and health among emerging adult with and without type 1 diabetes. Health Psychology, 33, 1125–1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Siminerio L, Escobar O, & Becker D (2008). Parent and adolescent distribution of responsibility for diabetes self-care: Links to health outcomes. Journal of Pediatric Psychology, 33(5), 497–508. doi: 10.1093/jpepsy/jsm081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Siminerio L, Escobar O, & Becker D (2009). Predictors of metabolic control among adolescents with diabetes: A 4-year longitudinal study. Journal of Pediatric Psychology, 34(3), 254–270. doi: 10.1093/jpepsy/jsn079i [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Snyder PR, Seltman H, Escobar O, Becker D, & Siminerio L (2010). Brief report: Trajectories of glycemic control over early to middle adolescence. Journal of Pediatric Psychology, 35(10), 1161–1167. doi: 10.1093/jpepsy/jsq011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, & Takeda A (2009). Brief report: Nature and implications of personal projects among adolescents with and without diabetes. Journal of Pediatric Psychology, 34(9), 1019–1024. doi: 10.1093/jpepsy/jsp024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzer M, Umfress K, Ajadeff G, Ghai K, & Zakowski SG (2009). Interactions with parents and friends among chronically ill children: Examining social networks. Journal of Developmental and Behavioral Pediatrics, 30(6), 499–508. [DOI] [PubMed] [Google Scholar]
- Herzer M, Vesco A, Ingerski LM, Dolan LM, & Hood KK (2011). Explaining the family conflict-glycemic control link through psychological variables in adolescents with type 1 diabetes. Journal of Behavioral Medicine, 34(4), 268–274. doi: 10.1007/s10865-010-9307-3 [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Harris MA, & Weissberg-Benchell J (2012). Diabetes resilience: a model of risk and protection in type 1 diabetes. Current diabetes reports, 12(6), 739–748. doi: 10.1007/s11892-012-0314-3 [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Holmes CS, Chen R, Maher K, Robinson E, & Streisand R (2013). Disentangling the roles of parental monitoring and family conflict in adolescents' management of type 1 diabetes. Health Psychology, 32(4), 388–396. doi: 10.1037/a0027811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Monaghan M, Cogen FR, & Streisand R (2010). Parent stress and child behavior among young children with type 1 diabetes. Child: Care, Health, and Development, 37, 224–232. [DOI] [PubMed] [Google Scholar]
- Hilliard ME, Rohan JM, Carle AC, Pendley JS, Delamater A, & Drotar D (2011). Fathers' Involvement in Preadolescents' Diabetes Adherence and Glycemic Control. Journal Of Pediatric Psychology, 36(8), 911–922. doi: 10.1093/jpepsy/jsr020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Rohan JM, Rausch JR, Delamater A, Pendley JS, & Drotar D (2014). Patterns and predictors of paternal involvement in adolescents’ type 1 diabets management over 3 years. J of Pediatric Psychology, 39, 74–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilliard ME, Wu YP, Rausch JR, Dolan LM, & Hood KK (2013). Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. Journal of Adolescent Health, 52(1), 28–34. doi: 10.1016/j.jadohealth.2012.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell A, Keenan K, Kasza K, Loeber R, Stouthamer-Loeber M, & Bean T (2008). Reciprocal influences between girls’ conduct problems and depression, and parental punishment and warmth: A six year prospective analysis. Journal of Abnormal Child Psychology, 36(5), 663–677. doi: 10.1007/s10802-007-9206-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollenstein T, Granic I, Stoolmiller M, & Snyder J (2004). Rigidity in parent-child interactions and the development of externalizing and internalizing behavior in early childhood. Journal of Abnormal Child Psychology, 32, 595–607. [DOI] [PubMed] [Google Scholar]
- Hood KK, Butler DA, Anderson BJ, & Laffel LMB (2007). Updated and revised diabetes family conflict scale. Diabetes Care, 30(7), 1764–1769. doi: 10.2337/dc06-2358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood KK, Peterson CM, Rohan JM, & Drotar D (2009). Association between adherence and glycemic control in pediatric type 1 diabetes: A meta-analysis. Pediatrics, 124(6). doi: 10.1542/peds.2009-0207 [DOI] [PubMed] [Google Scholar]
- Hsin O, La Greca AM, Valenzuela J, Moine CT, & Delamater A (2010). Adherence and glycemic control among Hispanic youth with type 1 diabetes: role of family involvement and acculturation. Journal of Pediatric Psychology, 35(2), 156–166. doi: 10.1093/jpepsy/jsp045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iannotti R, Schneider S, Nansel T, Haynie DL, Plotnick LP, Clark L, & Sobel DO (2006). Self-efficacy, outcome expectations, and diabetes self-mamangement in adolescents with type 1 diabetes. Developmental and Behavioral Pediatrics, 27(2), 98–105. [DOI] [PubMed] [Google Scholar]
- Ingerski LM, Anderson BJ, Dolan LM, & Hood KK (2010). Blood glucose monitoring and glycemic control in adolescence: contribution of diabetes-specific responsibility and family conflict. Journal of Adolescent Health, 47(2), 191–197. doi: 10.1016/j.jadohealth.2010.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iskander JM, Rohan JM, Pendley JS, Delameter A, & Drotar D (2015). A 3-year prospective study of parent-child communication in early adolescents with type 1 diabetes: Relationship to adherence and glycemic control. Journal of Pediatric Psychology, 40, 109–120. Doi: 10.1093/jpepsy/jsu027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, & Grey M (2010). A pilot study of observed parenting and adjustment in adolescents with type 1 diabetes and their mothers. Journal of Pediatric Psychology, 35(7), 738–747. doi: 10.1093/jpepsy/jsp098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaser SS, & White LE (2011). Coping and resilience in adolescents with type 1 diabetes. Child: care, health and development, 37(3), 335–342. doi: 10.1111/j.1365-2214.2010.01184.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SB, Kelly M, Henretta JC, Cunningham WR, Tomer A, & Silverstein JH (1992). A longitudinal analysis of adherence and health status in childhood diabetes. Journal of Pediatric Psychology, 17(5), 537–553. [DOI] [PubMed] [Google Scholar]
- Kaufman FR (Ed.). (2012). Medical management of type 1 diabetes (6th ed.). Alexandria, VA: American Diabetes Association. [Google Scholar]
- Kerns KA, Aspelmeier JE, Gentzler AL, & Grabill CM (2001). Parent-child attachment and monitoring in middle childhood. Journal of Family Psychology, 15(1), 69–81. [DOI] [PubMed] [Google Scholar]
- Kerns KA, Brumariu LE, & Seibert A (2011). Multi-method assessment of mother-child attachment: links to parenting and child depressive symptoms in middle childhood. Attachment & Human Development, 13(4), 315–333. doi: 10.1080/14616734.2011.584398 [DOI] [PubMed] [Google Scholar]
- Kerr M, Stattin H, & Burk WJ (2010). A reinterpretation of parental monitoring in longitudinal perspective. Journal of Research on Adolescence, 20(1), 39–64. [Google Scholar]
- Kim KJ, Conger RD, Lorenz FO, & Elder GH (2001). Parent-adolescent reciprocity in negative affect and its relation to early adult social development. Developmental Psychology, 37, 775–790. [PubMed] [Google Scholar]
- King PS, Berg CA, Butner J, Butler JM, & Wiebe DJ (2014). Longitudinal trajectories of parental involvement in type 1 diabetes and adolescents' adherence. Health Psychology, 33, 424–432. doi: 10.1037/a0032804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King PS, Berg CA, Butner J, Drew LM, Foster C, Donaldson D, … Wiebe DJ (2012). Longitudinal trajectories of metabolic control across adolescence: Associations with parental involvement, adolescents' psychosocial maturity, and health care utilization. Journal of Adolescent Health, 50(5), 491–496. doi: 10.1016/j.jadohealth.2011.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochanska G, & Kim S (2012). Toward a new understanding of legacy of early attachments for future antisocial trajectories: evidence from two longitudinal studies. Development and Psychopathology, 24(3), 783–806. doi: 10.1017/S0954579412000375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koepke S, & Denissen JJA (2012). Dynamics of identity development and separation-individuation in parent-child relaitonships during adolescence and emerging adulthood-- A conceptual integration. Developmental Review, 32, 67–88. [Google Scholar]
- Korbel CD (2009). Maternal attachment: Associations with diabetes and psychosocial adjustment during adolescence. Doctoral Disseration, Department of Psychology, University of Utah. ProQuest LLC database. (002944685) [Google Scholar]
- La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB Jr., & Santiago JV (1995). I get by with a little help from my family and friends: adolescents' support for diabetes care. Journal of Pediatric Psychology, 20(4), 449–476. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Bearman KJ, & Moore H (2002). Peer relations of youth with pediatric conditions and health risks: Promoting social support and healthy lifestyles. Developmental and Behavioral Pediatrics, 23(4), 271–280. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Follansbee D, & Skyler JS (1990). Developmental and behavioral aspects of diabetes management in youngsters. Children's Health Care, 19(3), 132–139. doi: 10.1207/s15326888chc1903_1 [DOI] [Google Scholar]
- Lachin JM, Genuth S, Nathan DM, Zinman B, & Rutledge BN (2008). Effect of glycemic exposure on the risk of microvascular complications in the diabetes control and complications trial - revisited. Diabetes, 57(4), 995–1001. [DOI] [PubMed] [Google Scholar]
- Laible D (2007). Attachment with parents and peers in late adolescence: Links with emotional competence and social behavior. Personality and Individual Differences, 43(5), 1185–1197. doi: 10.1016/j.paid.2007.03.010 [DOI] [Google Scholar]
- Lansing AE, & Berg CA (2014). Adolescent self-regulation as a foundation for chronic illness self-management. Journal of Pediatric Psychology, 39, 1091–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansing AH, Turner S, Osborn P, Winnick JB, Taheri K, Murray M, … Berg CA (2016). Academic achievement and metabolic control in adolescents with type 1 diabetes. Under review. [Google Scholar]
- Law GU, Walsh J., Queralt V, & Nouwen A (2013). Adolescent and parent diabetes distress in type 1 diabetes: The role of self-efficacy, perceived consequences, family responsibility, and adolescent-parent discrepancies. Journal of Psychosomatic Research, 74, 334–339. [DOI] [PubMed] [Google Scholar]
- Lengua LJ, Honorado E, & Bush NR (2007). Contextual risk and parenting as predictors of effortful control and social competence in preschool children. Journal of Applied Developmental Psychology, 28(1), 40–55. doi: 10.1016/j.appdev.2006.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowski A, & Drotar D (2007). The Relationship between Parent-Reported Social Support and Adherence to Medical Treatment in Families of Adolescents with Type 1 Diabetes. Journal Of Pediatric Psychology, 32(4), 427–436. doi: 10.1093/jpepsy/jsl037 [DOI] [PubMed] [Google Scholar]
- Lewis MD (2000). The promise of dynamic systems approaches for an integrated account of human development. Child Development, 71(1), 36–43. doi: 10.1111/1467-8624.00116 [DOI] [PubMed] [Google Scholar]
- Lewis MD (2011). Dynamic systems approaches: Cool enough? Hot enough? Child Development Perspectives, 5(4), 279–285. doi: 10.1111/j.1750-8606.2011.00190 [DOI] [Google Scholar]
- Lewis MD, Lamey AV, & Douglas L (1999). A new dynamic systems method for the analysis of early socioemotional development. Developmental Science, 2(4), 457–475. doi: 10.1111/1467-7687.00090 [DOI] [Google Scholar]
- Lichtwarck-Aschoff A, Hasselman F, Cox R, Pepler D, & Granic I (2012). A characteristic destabilization profile of parent-child interactions associated with treatment efficacy for aggressive children. Nonlinear dynamics, psychology, and life sciences., 16, 353–379. [PubMed] [Google Scholar]
- Leise, (2006). The burden of diabetes mellitus among US Youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics, 118, 1510. [DOI] [PubMed] [Google Scholar]
- Luyckx K, & Seiffge-Krenke I (2009). Continuity and change in glycemic control trajectories from adolescence to emerging adulthood: Relationships with family climate and self-concept in type 1 diabetes. Diabetes Care, 32(5), 797–801. doi: 10.2337/dc08-1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyckx K, Seiffge-Krenke I, Missotten L, Rassart J, Casteels K, & Goethals K (2013). Parent-adolescent conflict, treatment adherence and glycemic control in type 1 diabetes: The importance of adolescent externalizing symptoms. Psychology and Health, 28, 1082–1097. [DOI] [PubMed] [Google Scholar]
- Main A, Wiebe DJ, Croom AR, Sardone K, Godbey E, Tucker C, & White PC (2014). Associations of parent-adolescent relationship quality with type 1 diabetes management and depressive symptoms in Latino and Causcasian Youth. Journal of Pediatric Psychology, 39, 1104–1114. Doi: 10.1093/jpepsy/jsu062. [DOI] [PubMed] [Google Scholar]
- Main A, Wiebe DJ, Bogart KV, Turner SL, Tucker C, & Berg CA (2015). Secrecy from parents and Associations with Type 1 Diabetes Management in Late Adolescence. Journal of Pediatric Psychology, 40, 1075–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main M, Kaplan N, & Cassidy J (1985). Security in infancy, childhood, and adulthood: A move to the level of representation. Monographs of the Society for Research in Child Development, 50(1-2), 66–104. doi: 10.2307/3333827 [DOI] [Google Scholar]
- Main M, & Solomon J (1990). Procedures for identifying infants as disorganized/disoriented during the Ainsworth Strange Situation. In Greenberg MT, Cicchetti D & Cummings EM (Eds.), Attachment in the preschool years: Theory, research, and intervention (pp. 121–160). Chicago, IL: University of Chicago Press. [Google Scholar]
- Marshall SK, Tilton-Weaver LC, & Bosdet L (2005). Information management: Considering adolescents’ regulation of parental knowledge. Journal of Adolescence, 28(5), 633–647. doi: 10.1016/j.adolescence.2005.08.008 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Cicchetti D (2010). Developmental cascades. Development and Psychopathology, 22(3), 491–495. doi: 10.1017/S0954579410000222 [DOI] [PubMed] [Google Scholar]
- Masten AS, Roisman GI, Long JD, Burt KB, Obradović J, Riley JR, … Tellegen A (2005). Developmental cascades: Linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology, 41(5), 733–746. doi: 10.1037/0012-1649.41.5.733 [DOI] [PubMed] [Google Scholar]
- Mayer-Davis EJ, Bell RA, Dabelea D, D'Agostino R, Imperatore G, Lawrence JM, … Marcovina S (2009). The many faces of diabetes in American youth: Type 1 and type 2 diabetes in five race and ethnic populations: The SEARCH for diabetes in youth study. Diabetes Care, 32(Supplement_2), S99–S101. doi: 10.2337/dc09-S201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle JJ, & Hamagami F (2001). Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In Collins LM & Sayer AG (Eds.), New methods for the analysis of change (pp. 137–176). Washington, DC: American Psychological Association. [Google Scholar]
- Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Lovinger R, & Martin M (1994). Parent-child relationships and the management of insulin-dependent diabetes mellitus. Journal of Consulting & Clinical Psychology, 62(3), 603–610. [DOI] [PubMed] [Google Scholar]
- Mitchell SJ, Hilliard ME, Mednick L, Henderson C, Cogen F, & Streisand R (2009). Stress among fathers of young children with type 1 diabetes. Families, Systems, and Health, 27, 314–324. DOI: 10.1037/a0018191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modi AC, Pai AL, Hommel KA, Hood KK, Cortina S, Hilliard ME, … Drotar D (2012). Pediatric self-management: A framework for research, practice, and policy. Pediatrics, 129(2), e473–e485. doi: 10.1542/peds.2011-1635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, … Caspi A (2011). A gradient of childhood self-control predicts health, wealth, and public safety. Proceedings of the National Academy of Sciences, 108(7), 2693–2698. doi: 10.1073/pnas.1010076108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molenaar PCM (1985). A dynamic factor analysis model for the analysis of multivariate time series. Multivariate Behavioral Research, 22, 329–353. [DOI] [PubMed] [Google Scholar]
- Monaghan M, Hilliard ME, Cogen, & Streisand R (2011). Supporting parents of very young children with type 1 diabetes: Results from a pilot study. Patient Education and Counseling, 82, 271–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan M, Clary L, Stern A, Hilliard ME, & Streisand R (2015). Protective factors in young children with type 1 diabetes. Journal of Pediatric Psychology, 40, 878–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan M, Herbert LJ, Wang J, Holmes C, Cogen R, & Streisand R (2015). Mealtime behavior and diabetes-specific parent functioning in young children with type 1 diabetes. Health Psychology, 34, 794–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris AD, Boyle DI, McMahon AD, Greene SA, MacDonald TM, & Newton RW (1997). Adherence to insulin treatment glycaemic control, and ketoacidosis in insulin-dependent diabetes mellitus. The Lancet, 350(9090), 1505–1510. [DOI] [PubMed] [Google Scholar]
- Morris AD, Silk JS, Steinberg L, Myers SS, & Robinson LR (2007). The role of the family context in the development of emotion regulation. Social Development, 16(2), 361–388. doi: 10.1111/j.1467-9507.2007.00389.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naar-King S, Podolski C, Ellis DA, Frey MA, & Templin T (2006). Social ecological model of illness management in high-risk youths with type 1 diabetes. Journal of Consulting and Clinical Psychology, 74(4), 785–789. doi: 10.1037/0022-006x.74.4.785 [DOI] [PubMed] [Google Scholar]
- Nansel TR, Rovner AJ, Haynie D, Iannotti RJ, Simons-Morton B, Wysocki T, … Laffel L (2009). Development and validation of the collaborative parent involvement scale for youths with type 1 diabetes. Journal of Pediatric Psychology, 34(1), 30–40. doi: 10.1093/jpepsy/jsn058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholson JS, Deboeck PR, Farris JR, Boker SM, & Borkowski JG (2011). Maternal depressive symptomatology and child behavior: Transactional relationship with simultaneous bidirectional coupling. Developmental Psychology, 47(5), 1312–1323. doi: 10.1037/a0023912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosko A, Tieu T, Lawford H, & Pratt MW (2011). How do I love thee? Let me count the ways: Parenting during adolescence, attachment styles, and romantic narratives in emerging adulthood. Developmental Psychology, 47(3), 645–657. [DOI] [PubMed] [Google Scholar]
- O'Hara LK, & Holmbeck GN (2013). Executive functions and parenting behaviors in association with medical adherence and autonomy among youth with spina bifida. Journal of pediatric psychology, 38(6), 675–687. doi: 10.1093/jpepsy/jst007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oris L, Seiffge-Krenke I, Moons P, Goubert L, Rassart J, Goossens E, & Luyckx K (2016). Parental and peer support in adolescents with a chronic conditions: a typological approach and developmental implications. Journal of Behavioral Medicine, 39, 107–119. [DOI] [PubMed] [Google Scholar]
- Osborn P, Berg CA, Hughes AE, Pham P, & Wiebe DJ (2013). What mom and dad don't know can hurt you: adolescent disclosure to and secrecy from parents about type 1 diabetes. Journal of Pediatric psychology, 38(2), 141–150. doi: 10.1093/jpepsy/jss102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott J, Greening L, Palardy N, Holderby A, & DeBell W (2000). Self-efficacy as a mediator variable for adolescents' adherence to treatment for insulin-dependent diabetes mellitus. Children’s Health Care, 29(1), 47–63. [Google Scholar]
- Oud JHL (2007). Continuous time modeling of reciprocal relationships in the cross- lagged panel design. In Boker SM & Wenger MJ (Eds.), Data analytic techniques for dynamical systems (pp. 87–129). Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Palladino DK, & Helgeson VS (2012). Friends or foes? A review of peer influence on self-care and glycemic control in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 37(5), 591–603. doi: 10.1093/jpepsy/jss009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer DL, Berg CA, Butler J, Fortenberry K, Murray M, Lindsay R, … Wiebe DJ (2009). Mothers', fathers', and children's perceptions of parental diabetes responsibility in adolescence: Examining the roles of age, pubertal status, and efficacy. Journal of Pediatric Psychology, 34(2), 195–204. doi: 10.1093/jpepsy/jsn073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer DL, Berg CA, Wiebe DJ, Beveridge R, Korbel CD, Upchurch R, … Donaldson D (2004). The role of autonomy and pubertal status in understanding age difference in maternal involvement in diabetes responsibility across adolescence. Journal of Pediatric Psychology, 29(1), 35–46. [DOI] [PubMed] [Google Scholar]
- Palmer DL, Osborn P, King PS, Berg CA, Butler J, Butner J, … Wiebe DJ (2011). The structure of parental involvement and relations to disease management for youth with type 1 diabetes. Journal of Pediatric Psychology, 36(5), 596–605. doi: 10.1093/jpepsy/jsq019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pambianco G, Costacou T, Ellis D, Becker DJ, Klein R, & Orchard TJ (2006). The 30-year natural history of type 1 diabetes complications: The Pittsburgh Epidemiology of Diabetes Complications Study experience. Diabetes, 55(5), 1463–1469. [DOI] [PubMed] [Google Scholar]
- Pardini DA (2008). Novel Insights into Longstanding Theories of Bidirectional Parent–Child Influences: Introduction to the Special Section. Journal of Abnormal Child Psychology, 36(5), 627–631. doi: 10.1007/s10802-008-9231-y [DOI] [PubMed] [Google Scholar]
- Pardini DA, Fite PJ, & Burke JD (2008). Bidirectional associations between parenting practices and conduct problems in boys from childhood to adolescence: The moderating effect of age and African-American ethnicity. Journal of Abnormal Child Psychology, 36(5), 647–662. doi: 10.1007/s10802-007-9162-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson GR, Debaryshe BD, & Ramsey E (1989). A developmental perspective on antisocial behavior. . American Psychologist, 44, 329–355. [DOI] [PubMed] [Google Scholar]
- Patton SR, Dolan LM, Mitchell MJ, Byars KC, Standiford D, & Power SW (2004). Mealtime interactions in families of pre-schoolers with type 1 diabetes. Pediatric Diabetes, 5, 190–198. [DOI] [PubMed] [Google Scholar]
- Patton SR, Odar C, Midyett LK, & Clements MA (2014). Pilot study results for a novel behavior plus nutrition intervention for caregivers of young children with type 1 diabetes. J Nutrition Education Behavior, 46, 429–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton SR, Piazza-Waggoner C, Modi AC, Dolan LM, & Powers SW (2009). Family functioning at meals relates to adherence in young children with type 1 diabetes. Journal of Paediatrics and Child Health, 45(12), 736–741. doi: 10.1111/j.1440-1754.2009.01604.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson CC, & Drotar D (2006). Family impact of neurodevelopmental late effects in survivors of pediatric cancer: review of research, clinical evidence, and future directions. Clinical child psychology and psychiatry, 11(3), 349–366. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Keiley MK, Laird RD, Bates JE, & Dodge KA (2007). Predicting the developmental course of mother-reported monitoring across childhood and adolescence from early proactive parenting, child temperament, and parents' worries. Journal of Family Psychology, 21(2), 206–217. doi: 10.1037/0893-3200.21.2.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz EM, & Eaton MM (2001). Maternal intrusive support in the academic context: Transactional socialization processes. Developmental Psychology, 37(2), 174–186. doi: 10.1037//0012-1649.37.2.174 [DOI] [PubMed] [Google Scholar]
- Queen TL, Butner JE, Wiebe DJ, & Berg CA (2016). A Micro-Developmental View of Parental Well-being in Families Coping with Chronic Illness. Journal of Family Psychology, 30, 843–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racz SJ, & McMahon RJ (2011). The relationship between parental knowledge and monitoring and child and adolescent conduct problems: A 10-year update. Clinical Child and Family Psychology Review, 14(4), 377–398. doi: 10.1007/s10567-011-0099-y [DOI] [PubMed] [Google Scholar]
- Rausch JR, Hood KK, Delamater A, Shroff Pendley J, Rohan JM, Reeves G, … Drotar D (2012). Changes in Treatment Adherence and Glycemic Control During the Transition to Adolescence in Type 1 Diabetes. Diabetes Care, 35(6), 1219–1224. doi: 10.2337/dc11-2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repetti RL, Taylor SE, & Seeman TE (2002). Risky families: Family social environments and the mental and physical health of offspring. Psychological Bulletin, 128(2), 330–366. [PubMed] [Google Scholar]
- Revenson TA, Kayser K, & Bodenmann G (2005). Couples coping with stress: Emerging perspectives on dyadic coping. Washington, DC: American Psychological Association. [Google Scholar]
- Rhee H, Belyea MJ, & Brasch J (2010). Family support and asthma outcomes in adolescents: barriers to adherence as a mediator. The Journal of Adolescent Health, 47(5), 472–478. doi: 10.1016/j.jadohealth.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson EM, Weaver P, Chen R, Streisand R, & Holmes CS (2016). A model of parental distress and factors that mediate its links with parental monitoring of youth diabetes care, adherence, and glycemic control. Health Psychology, 35, 1373–1382. Doi: 10.1037/hea0000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogoff B (1998). Cognition as a collaborative process. In Damon W (Ed.), Handbook of child psychology: Vol. 2, Cognition, perception, and language (pp. 679–744). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Ronan JM, Rausch JR, Pendley JS, Delamater AM, Dolan L, Reeves G, & Drotar D (2015). Identification and prediction of group-based glycemic control trajectories during the transition to adolescence. Health Psychology, 33, 1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg T, & Shields CG (2009). The role of parent-adolescent attachment in the glycemic control of adolescents with type 1 diabetes: A pilot study. Families, Systems, & Health, 27(3), 237–248. [DOI] [PubMed] [Google Scholar]
- Sameroff A (2009). Designs for transactional research. In Sameroff A (Ed.), The transactional model of development: How children and contexts shape each other (pp. 23–32). Washington, DC: American Psychological Association. [Google Scholar]
- Sameroff AJ, & Mackenzie MJ (2003). Research strategies for capturing transactional models of development: The limits of the possible. Developmental Psychopathology, 15(3), 613–640. doi: 10.1017/S0954579403000312 [DOI] [PubMed] [Google Scholar]
- Scarr S, & McCartney K (1983). How people make their own environments: A theory of genotype (leading to) environment effects. [Opinion Papers]. Child Development, 54(2), 424–435. [DOI] [PubMed] [Google Scholar]
- Scott S, Briskman J, Woolgar M, Humayun S, & O’Connor TG (2011). Attachment in adolescence: Overlap with parenting and unique prediction of behavioural adjustment. Journal of Child Psychology and Psychiatry, 52(10), 1052–1062. doi: 10.1111/j.1469-7610.2011.02453.x [DOI] [PubMed] [Google Scholar]
- Seiffge-Krenke I (2000). Diversity in romantic relations of adolescents with varying health status: Links to intimacy in close relationships. Journal of Adolescent Research, 15(6), 611–636. [Google Scholar]
- Seiffge-Krenke I, Overbeek G, & Vermulst A (2010). Parent–child relationship trajectories during adolescence: Longitudinal associations with romantic outcomes in emerging adulthood. Journal of Adolescence, 33(1), 159–171. doi: 10.1016/j.adolescence.2009.04.001 [DOI] [PubMed] [Google Scholar]
- Shroff-Pendley J, Kasmen LJ, Miller DL, Donze J, Swenson C, & Reeves G (2002). Peer and family support in children and adolescents with type 1 diabetes. Journal of Pediatric Psychology, 27(5), 429–438. [DOI] [PubMed] [Google Scholar]
- Skinner TC, & Hampson SE (1998). Social support and personal models of diabetes in relation to self-care and well-being inadolescents with type I diabetes mellitus. Journal of Adolescence, 21(6), 703–715. doi: 10.1006/jado.1998.0190 [DOI] [PubMed] [Google Scholar]
- Skinner TC, John M, & Hampson SE (2000). Social support and personal models of diabetes as predictors of self-care and well-being: A longitudinal study of adolescents with diabetes. Journal of Pediatric Psychology, 25(4), 257–267. [DOI] [PubMed] [Google Scholar]
- Smetana JG, Campione-Barr N, & Metzger A (2006). Adolescent development in interpersonal and societal contexts. Annual Review of Psychology, 57, 255–284. doi: 10.1146/annurev.psych.57.102904.190124 [DOI] [PubMed] [Google Scholar]
- Smetana JG, Villalobos M, Tasopoulos-Chan M, Gettman DC, & Campione-Barr N (2009). Early and middle adolescents' disclosure to parents about activities in different domains. Journal of Adolescence, 32(3), 693–713. doi: 10.1016/j.adolescence.2008.06.010 [DOI] [PubMed] [Google Scholar]
- Smith LB (2005). Cognition as a dynamic system: principles from embodiment. Developmental Review, 25(3-4), 278–298. doi: 10.1016/j.dr.2005.11.001 [DOI] [Google Scholar]
- Smith LB, & Thelen E (2003). Development as a dynamic system. Trends in cogntiive sciences, 7(8), 343–348. [DOI] [PubMed] [Google Scholar]
- Soenens B, Vansteenkiste M, Luyckx K, & Goossens L (2006). Parenting and adolescent problem behavior: An integrated model with adolescent self-disclosure and perceived parental knowledge as intervening variables. Developmental Psychology, 42(2), 305–318. doi: 10.1037/0012-1649.42.2.305 [DOI] [PubMed] [Google Scholar]
- Sparud-Lundin C, Öhrn I, & Danielson E (2010). Redefining relationships and identity in young adults with type 1 diabetes. Journal of Advanced Nursing, 66(1), 128–138. doi: 10.1111/j.1365-2648.2009.05166.x [DOI] [PubMed] [Google Scholar]
- Sroufe LA (1996). Emotional development: The organization of emotional life in the early years. New York, NY: Cambridge University Press. [Google Scholar]
- Stattin H, & Kerr M (2000). Parental monitoring: A reinterpretation. Child Development, 71(4), 1072–1085. [DOI] [PubMed] [Google Scholar]
- Steele J, & Ferrer E (2011). Latent differential equation modeling of self-regulatory and coregulatory affective processes. Multivariate Behavioral Research, 46, 956–984. doi: 10.1080/00273171.2011.625305 [DOI] [PubMed] [Google Scholar]
- Steenbeek H, & van Geert P (2005). A dynamic systems model of dyadic interactions during play of two children. European Journal of Developmental Psychology, 2, 105–145. doi: 10.1080/17405620544000020 [DOI] [Google Scholar]
- Steenbeek H, & van Geert P (2008). An empirical validation of a dynamic systems model of interaction: do children of different sociometric statuses differ in their dyadic play? Developmental Science, 11(2), 253–281. doi: 10.1111/j.1467-7687.2007.00655.x [DOI] [PubMed] [Google Scholar]
- Steenbeek HW, & van Geert PLC (2007). A theory and dynamic model of dyadic interaction: Concerns, appraisals, and contagiousness in a developmental context. Developmental Review, 27(1), 1–40. doi: 10.1016/j.dr.2006.06.002 [DOI] [Google Scholar]
- Steinberg L, & Monahan KC (2007). Age differences in resistance to peer influence. Developmental Psychology, 43(6), 1531–1543. doi: 10.1037/0012-1649.43.6.1531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart I, & Golubitsky M (1992). Fearful symmetry: Is god a geometer? : Blackwell Publishers, Oxford. [Google Scholar]
- Storch EA, Heidgerken AD, Geffken GR, Lewin AB, Ohleyer V, Freddo M, & Silverstein JH (2006). Bullying, regimen self-management, and metabolic control in youth with type I diabetes. The Journal of Pediatrics, 148(6), 784–787. doi: 10.1016/j.jpeds.2006.01.007 [DOI] [PubMed] [Google Scholar]
- Streisand R, Swift E, Wickmark T, Chen R, & Holmes CS (2005). Pediatric parenting stress among parents of children with type 1 diabetes: The role of self-efficacy, responsibility, and fear. Journal of Pediatric Psychology, 30, 513–521. [DOI] [PubMed] [Google Scholar]
- Streisand R, Mackey ER, Elliot BM, Mednick L, Slaughter IM, Turek J, & Austin A (2008). Parental anxiety and depression associated with caring for a child newly diagnosed with type 1 diabetes: Opportunities for education and counseling. Patient Education and Counseling, 73(2), 333–338. doi: 10.1016/j.pec.2008.06.014 [DOI] [PubMed] [Google Scholar]
- Surjadi FF, Lorenz FO, Wickrama KAS, & Conger RD (2011). Parental support, partner support, and the trajectories of mastery from adolescence to early adulthood. Journal of Adolescence, 34(4), 619–628. doi: 10.1016/j.adolescence.2010.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweenie R, Mackey ER, & Streisand R (2014). Parent-child relationships in type 1 diabetes: Associations among child behavior, parenting behavior, and pediatric parenting stress. Families, Systems, and Health, 32, 31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Baumeister RF, & Boone AL (2004). High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality, 72(2), 271–322. [DOI] [PubMed] [Google Scholar]
- Thelen E, & Smith LB (1994). A dynamic systems approach to the development of cognition and action. Cambridge, MA: Bradford/MIT Press. [Google Scholar]
- Thomas AM, Peterson L, & Goldstein D (1997). Problem solving and diabetes regimen adherence by children and adolescents with iddm in social pressure situations: A reflection of normal development. Journal of Pediatric Psychology, 22(4), 541–561. [DOI] [PubMed] [Google Scholar]
- Tilton-Weaver LC, Kerr M, Pakalniskeine V, Tokic A, Salihovic S, & Stattin H (2010). Open up or close down: How do parental reactions affect youth information management? Journal of Adolescence, 33(2), 333–346. doi: 10.1016/j.adolescence.2009.07.011 [DOI] [PubMed] [Google Scholar]
- Treffner PJ, & Turvey MT (1993). Symmetry, broken symmetry, and handedness in bimanual coordination dynamics. Experimental Brain Research, 107(3), 3. doi: 10.1007/BF00230426 [DOI] [PubMed] [Google Scholar]
- Turan B, Osar Z, Turan JM, Ilkova H, & Damci T (2003). Dismissing attachment and outcome in diabetes: The mediating role of coping. Journal of Social and Clinical Psychology, 22(6), 607–626. doi: 10.1521/jscp.22.6.607.22933 [DOI] [Google Scholar]
- Turvey MT (1990). Coordination. The American Psychologist, 45(8), 938–953. [DOI] [PubMed] [Google Scholar]
- Uchino BN (2009). Understanding the links between social support and physical health: A life-span perspective with emphasis on the separability of perceived and received support. Perspectives on Psychological Science, 4(3), 236–255. doi: 10.1111/j.1745-6924.2009.01122.x [DOI] [PubMed] [Google Scholar]
- Vesco A, Anderson BJ, Laffel L, Dolan LM, Ingerski LM, & Hood KK (2010). Responsibility sharing between adolescents with type 1 diabetes and their caregivers: Importance of adolescent perceptions on diabetes management and control. J of Pediatric Psychology, 35, 1168–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Holst E (1939, 1973). On the nature of order in the central nervous system. In Martin R (Ed.), The collected papers of Erich von Holst, vol. 1. The behavioral physiology of animal and man. Coral Gables, FL: University of Miami Press. [Google Scholar]
- Wallander JL, & Varni JW (1989). Social support and adjustment in chronically ill and handicapped children. American Journal of Community Psychology, 17(2), 185–201. [DOI] [PubMed] [Google Scholar]
- Wampler RS, & Downs AB (2010). Parent and peer attachment in minority males at high risk for delinquency. Clinical Social Work Journal, 38(1), 107–119. doi: 10.1007/s10615-009-0239-8 [DOI] [Google Scholar]
- Waters E, Kondo-Ikemura K, Posada G, & Richters JE (1991). Learning to love: Mechanisms and milestones. In Gunnar MR & Sroufe LA (Eds.), Self processes and development. (Vol. 23, pp. 217–255). Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc. [Google Scholar]
- Weissberg-Benchell J, Wolpert H, & Anderson BJ (2007). Transitioning from pediatric to adult care: A new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care, 30(10), 2441–2446. doi: 10.2337/dc07-1249 [DOI] [PubMed] [Google Scholar]
- Weissberg-Benchell J, Nansel T, Holmbeck G, Chen R, Anderson B, Wysocki T, Laffel L (2009). Generic and diabetes-specific parent-child behaviors and quality of life among youth with type 1 diabetes. Journal of Pediatric Psychology, 34, 977–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Fortenberry KT, Sirstins J, Lindsay R, Donaldson D, & Murray M (2008). Physician recommendations about maternal involvement in adolescent diabetes management. Diabetes Care, 31(4), 690–692. doi: 10.2337/dc07-1618 [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Palmer D, Korbel C, Beveridge R, Swinyard M, & Donaldson D (2005). Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology, 30(2), 167–178. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Chow CM, Palmer DL, Butner J, & Osborn P, Berg CA (2014). Developmental factors associated with longitudinal declines in parental responsibility and adherence to type 1 diabetes management across adolescent. Journal of Pediatric Psychology, 39(5), 532–541. doi: 10.1093/jpepsy/jsu006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Gelfand D, Butler JM, Korbel C, Fortenberry KT, McCabe JE, & Berg CA (2011). Longitudinal associations of maternal depressive symptoms, maternal involvement, and diabetes management across adolescence. Journal of Pediatric Psychology, 36(7), 837–846. doi: 10.1093/jpepsy/jsr002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiebe DJ, Helgeson VS, & Berg CA (2016). The social context of managing diabetes across the life span. American Psychologist, 71, 526–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson RB (2004). The role of parental and peer attachment in the psychological health and self-esteem of adolescents. Journal of Youth and Adolescence, 33(6), 479. [Google Scholar]
- Writing Team for the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Research Group. (2003). Sustained effect of intensive treatment of type 1 diabetes mellitus on development and progression of diabetic nephropathy: the Epidemiology of Diabetes Interventions and Complications (EDIC) study. Journal of the American Medical Association, 290(16), 2159–2167. doi: 10.1001/jama.290.16.2159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, & Gavin L (2006). Paternal involvement in the management of pediatric chronic diseases: Associations with adherence, quality of life, and health status. Journal of Pediatric Psychology, 31(5), 501–511. [DOI] [PubMed] [Google Scholar]
- Wysocki T, Harris MA, Buckloh LM, Mertlich D, Lochrie AS, Taylor A, … White NH (2008). Randomized, controlled trial of behavioral family systems therapy for diabetes: Maintenance and generalization of effects on parent-adolescent communication. Behavior Therapy, 39(1), 33–46. doi: 10.1016/j.beth.2007.04.001 [DOI] [PubMed] [Google Scholar]
- Wysocki T, Nansel TR, Holmbeck GN, Chen R, Laffel L, Anderson BJ, & Weissberg-Benchell J (2009). Collaborative involvement of primary and secondary caregivers: Associations with youths' diabetes outcomes. Journal of Pediatric Psychology, 34(8), 869–881. doi: 10.1093/jpepsy/jsn136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wysocki T, Taylor A, Hough BS, Linscheid TR, Yeates KO, & Naglieri JA (1996). Deviation from developmentally appropriate self-care autonomy: Association with diabetes outcomes. Diabetes Care, 19(2), 119–125. doi: 10.2337/diacare.19.2.119 [DOI] [PubMed] [Google Scholar]
- Yates TM, Obradovic J, & Egeland B (2010). Transactional relations across contextual strain, parenting quality, and early childhood regulation and adaptation in a high-risk sample. Development and Psychopathology, 22(3), 539–555. doi: 10.1017/S095457941000026X [DOI] [PubMed] [Google Scholar]


