Abstract
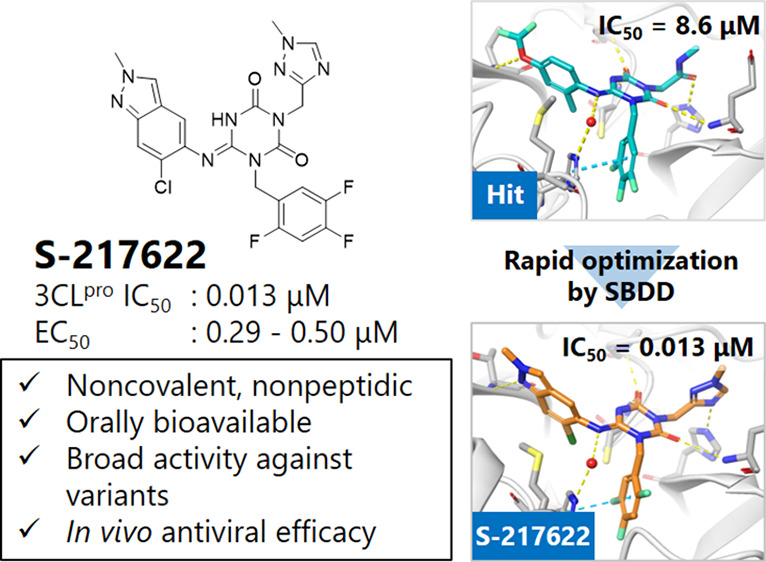
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has resulted in millions of deaths and threatens public health and safety. Despite the rapid global spread of COVID-19 vaccines, effective oral antiviral drugs are urgently needed. Here, we describe the discovery of S-217622, the first oral noncovalent, nonpeptidic SARS-CoV-2 3CL protease inhibitor clinical candidate. S-217622 was discovered via virtual screening followed by biological screening of an in-house compound library, and optimization of the hit compound using a structure-based drug design strategy. S-217622 exhibited antiviral activity in vitro against current outbreaking SARS-CoV-2 variants and showed favorable pharmacokinetic profiles in vivo for once-daily oral dosing. Furthermore, S-217622 dose-dependently inhibited intrapulmonary replication of SARS-CoV-2 in mice, indicating that this novel noncovalent inhibitor could be a potential oral agent for treating COVID-19.
Introduction
The global coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to spread worldwide; more than 440 million people have been infected, and 6.0 million have died as of March 2022.1 Because therapeutic options remain limited, oral COVID-19 therapeutics are urgently needed, especially for nonhospitalized patients, to prevent hospitalization and death.2
SARS-CoV-2 is highly pathogenic to older adults and persons with high-risk factors and can develop into severe, life-threatening acute respiratory distress syndrome. SARS-CoV-2 is an enveloped positive-sense single-stranded RNA virus that is a member of the genus Betacoronavirus.3 SARS-CoV-2 enters host cells by binding its spike glycoprotein to angiotensin-converting enzyme 2 (ACE2) and releases its viral RNA genome into the cytoplasm after uncoating. After entry, the viral RNA genome subjects the cell to translation of two large polyproteins, pp1a and pp1ab, which are processed into individual nonstructural proteins. Nsp5, also known as 3C-like protease (3CLpro) or the main protease, is a cysteine protease responsible for cleaving 11 distinct sites of the polyproteins to transform into mature functional proteins. 3CLpro plays a critical role in viral replication, and its inhibition prevents the formation of replication-essential enzymes, such as RNA-dependent RNA polymerase, thus inhibiting viral replication.4 Viral proteases are well-validated drug targets for treating human immunodeficiency virus and hepatitis C virus and have been used in various approved oral drugs.5 Additionally, the antiviral efficacy of the 3CLpro inhibitor would likely be unaffected by and not induce mutations of the spike protein, which often occur in SARS-CoV-2 variants, because the 3CLpro and spike protein are distinct proteins encoded in different regions of the viral genome. Thus, 3CLpro is an attractive target for small-molecule oral therapeutics for treating COVID-19. Recent reports have revealed that peptidelike 3CLpro inhibitors with reactive “warheads” show potent antiviral activities in vitro, and some of these drugs reduced viral loads in vivo in SARS-CoV-2-infected human ACE2 transgenic mouse models.6,7 Recently, Pfizer reported good results from a clinical study of the peptidic, covalent oral 3CLpro inhibitor, PF-07321332, which is dosed with ritonavir as a pharmacokinetic (PK) booster.8 However, challenges remain for improving the target selectivity and PK profiles of peptidelike covalent inhibitors owing to the intrinsic nature of the reactivity, low membrane permeability, and low metabolic stability.9−11 Hence, nonpeptidic, noncovalent small-molecule inhibitors have attracted much attention; however, their potency and PK profiles must be further optimized.12−16
Here, we describe the discovery of S-217622, the first nonpeptidic, noncovalent SARS-CoV-2 3CLpro inhibitor clinical candidate for treating COVID-19, and its preclinical characterization. S-217622 displayed antiviral activity in vitro toward a range of SARS-CoV-2 variants and coronavirus families, favorable drug metabolism and pharmacokinetic (DMPK) profiles for the oral agents, and dose-dependent antiviral efficacy in vivo, indicating its potential for once-daily oral treatment of COVID-19.
Results and Discussions
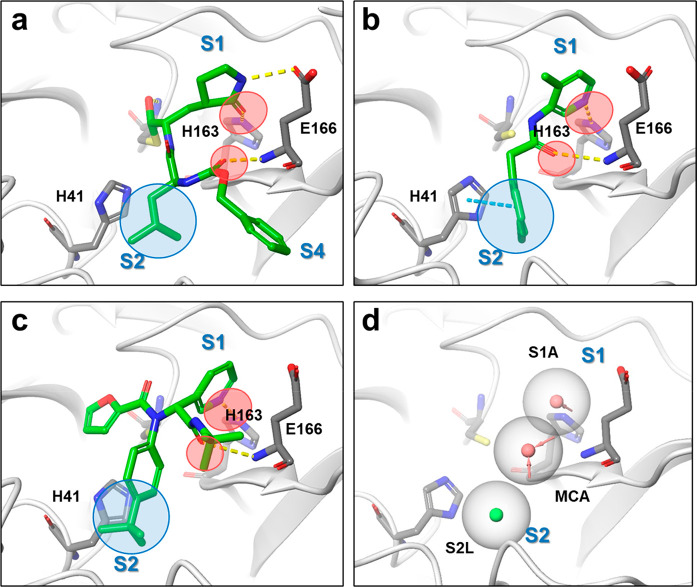
To rapidly obtain the noncovalent SARS-CoV-2 3CLpro inhibitor clinical candidate to combat the pandemic, we used a structure-based drug design (SBDD) strategy, starting with docking-based virtual screening followed by biological screening using an in-house compound library (Figure 1). First, we investigated pharmacophores in the binding site of 3CLpro based on the interactions of known inhibitors because applying the pharmacophore filter to the docking screening helps enrich the virtual-screening hit rate.17 3CLpro is a cysteine protease with a Cys145-His41 catalytic dyad in its active site, which recognizes P1 Gln and P2 Leu/Met/Phe/Val as its substrates.6 These substratelike substructures are shared with the potent peptidelike inhibitors GC-3767 and N3,18 a Gln-mimic lactam moiety in the S1 pocket and Leu-mimic hydrophobic moiety in the S2 pocket (Figure 2a). Noncovalent small-molecule inhibitors, such as ML188,12 ML300,13,14 and the 3-aminopyridine-like compound of the Postera COVID moonshot project,15,16 exhibit similar binding interactions, which form a hydrogen bond with the side-chain NH donor of His163 in the S1 pocket and have fitted lipophilic moieties in the S2 pocket (Figure 2b,c). Additionally, the hydrogen bond with the Glu166 main-chain NH recognizes the P2 main-chain carbonyl of the substrate and is conserved in the known inhibitors. Given these interactions, we hypothesized that these three pharmacophore elements, that is, the acceptor site with the side-chain NH donor of His163 in the S1 pocket, the lipophilic site in the S2 pocket, and the acceptor site with the Glu166 main-chain NH, play critical roles in small-molecule binding (Figure 2d).
Figure 1.
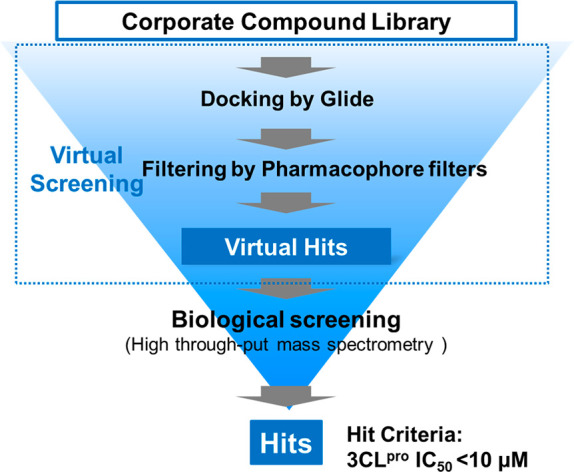
Schematic flow of the screening campaign.
Figure 2.
Binding modes of 3CLpro inhibitors, their interactions, and defined pharmacophore filters for virtual screening. (a) Crystal structures of GC376 (PDB code: 6WTT), (b) 3-aminopyridine-like compound of the Postera COVID moonshot project (PDB code: 5RH2), and (c) ML188 (PDB code: 7L0D). The common H-bond acceptors are circled in red; the common hydrophobic features are circled in blue. (d) Common pharmacophore shared with inhibitors A–C. Red and green spheres represent H-bond acceptors and lipophilic features, respectively.
We performed docking-based virtual screening using the crystal structures of the 3CLpro and ML188-like noncovalent small molecules (Protein Data Bank [PDB] code: 6W63).19 There were a limited number of cocrystal structures of SARS-CoV-2 3CLpro available especially for noncovalent inhibitors at the time we planned the virtual screening. Among the available structures, we selected 6W63 because of its relatively high resolution (2.10 Å) and clear electron density of compound and active site residues. In the virtual screening, hundreds of thousands of compounds from the in-house library were docked, then the pharmacophore filters described above were applied to each docking pose, and the 300 top-scoring compounds were evaluated via enzymatic assays using mass spectrometry to avoid the false positives that frequently occur in fluorescence-based assays, giving some hit compounds with IC50 < 10 μM.
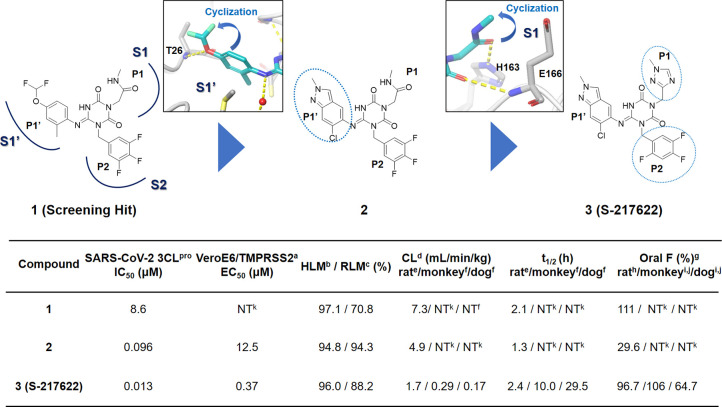
Optimization of the PK profile is a common challenge in drug discovery and usually takes time to overcome. Therefore, if possible, potency optimization of a hit compound with favorable PK profiles is likely the most straightforward way to meet the urgent need for an oral 3CLpro inhibitor. Further profiling of hit compounds revealed that one of the hit compounds, 1, could be a potential lead for this project because it displayed potent enzymatic inhibitory activity and favorable PK profiles with oral bioavailability (Figure 3). An enzymatic inhibition assay revealed that the IC50 value of 1 was 8.6 μM, and the in vitro metabolic stabilities of 1, measured after 30 min of incubation in human and rat microsomes, were 97% and 71%, respectively. An in vivo PK study in rats demonstrated that 1 had a favorable profile for the oral agent, oral bioavailability (F) of 111%, and a low clearance of 7.3 mL/min/kg.
Figure 3.
Structure-based optimization of the hit compound 1 and the profile of compounds. (a) Cytopathic effect (CPE) inhibition assay with Vero E6 cells expressing human transmembrane protease serine2 (VeroE6/TMPRSS2). (b) Percentage remaining in human liver microsomes (HLM) after 30 min. (c) Percentage remaining in rat liver microsomes (RLM) after 30 min. (d) Total clearance, (e) intravenously administered, 0.5 μmol/mL/kg (n = 2) in the nonfasted condition, (f) intravenously administered, 0.1 mg/0.2 mL/kg (n = 2) in the nonfasted condition, and (g) oral bioavailabiity. (h) Oral administration was carried out at 1 μmol/5 mL/kg (n = 2) under the nonfasted condition. (i) Oral administration was carried out at 3 mg/2 mL/kg (n = 3) under the nonfasted condition. (j) Evaluated as S-217622 fumaric acid. (k) Not tested.
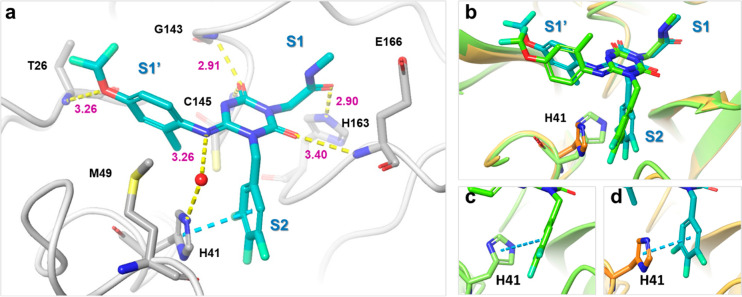
We resolved the X-ray complex structure of 1 with the protease (Figure 4a). As expected, the binding mode of 1 in the X-ray structure was similar to that obtained in the docking (Figure 4b). The S1 and S2 pockets were filled with the methyl-amide and 3,4,5-trifluorobenzene moieties, respectively. The 4-difluoromethoxy-2-methylbenzene subunit was placed in the S1′ pocket. The 2-carbonyl oxygen of the center triazine moiety formed a hydrogen bond with the main-chain NH of Glu166. The other side of the 4-carbonyl oxygen was bound in the oxyanion hole of the protease, which formed two hydrogen bonds with the main-chain NHs of Gly143 and Cys145. The methyl-amide moiety was placed in the S1 pocket, of which the carbonyl oxygen interacted with the side-chain NH of His163. The protease exhibited an interesting conformational change in the S2 pocket; the side chain of the catalytic His41 was rotated and formed a face-to-face π interaction with the 3,4,5-trifluorobenzene moiety of 1, whereas the docking pose predicted an edge-to-face π interaction (Figure 4c,d). Along with the side-chain flip of His41, the 4-difluoromethoxy-2-methylbenzene fragment was placed in a slightly different site compared to that of the docking pose, in which the ether oxygen of the P1′ ligand formed a hydrogen bond with the main-chain NH of Thr26. An imine linker formed a water-mediated hydrogen bond with the His41 side chain, indicating its contribution to the affinity.
Figure 4.
X-ray costructure of hit compound 1 and 3CLpro (PDB code: 7VTH). (a) Close-up view of 1 (cyan) in the binding pocket. Water molecules are shown as red spheres. Hydrogen bonds are indicated as yellow dashed lines; π–π stacking is indicated as a cyan dashed line. (b–d) Comparison of a docking pose and X-ray crystal structure of 1. Near the S2 pocket, the side chain of His41 was rotated to form a face-to-face π interaction with the 3,4,5-trifluorobenzene moiety of 1. Docked structure is in lime green, and the X-ray structure is in cyan (1) and orange (protein residues).
Keeping the hydrogen bonds confirmed by the X-ray complex structure, we achieved straightforward multiparameter optimization starting from hit compound 1 (Figure 3, Table S1). First, for a better fit with the S1′ pocket, we optimized the P1′ ligand while keeping the hydrogen bond with Thr26. As a result, compound 2, having 6-chloro-2-methyl-2H-indazole as a P1′ ligand, displayed a 90-fold improvement in enzymatic inhibitory activity while maintaining the favorable DMPK profile. Next, the P1 methyl-amide moiety was replaced with a range of heterocyclic compounds, thus yielding compound 3, which eventually became the clinical candidate S-217622. S-217622 showed a biochemical activity of IC50 = 0.013 μM, an antiviral activity of EC50 = 0.37 μM, and preferable DMPK profiles for oral dosing, such as high metabolic stability (96% and 88% in human and rat liver microsomes, respectively), high oral absorption (97%), and low clearance (1.70 mL/min/kg) in rats (Figure 3, Tables S2–S4). Furthermore, S-217622 showed even better DMPK profiles in monkeys and dogs than in rats, with low clearance, long elimination half-lives (t1/2) of approximately 10 and 30 h in monkeys and dogs, respectively, and high oral bioavailability for all animals tested, suggesting its potential use for once-daily treatment of COVID-19 without requiring a PK booster such as ritonavir.
Figure 5 shows the X-ray cocrystal structure of 3CLpro complexed with S-217622. In the S1 site, the 1-methyl-1H-1,2,4-triazole unit fit to the S1 pocket, forming a hydrogen bond with the side-chain NH of His163. The distinctive His41 flip observed in 1 was maintained in the S-217622 complex, and the 2,4,5-trifluorobenzylic moiety occupied the hydrophobic S2 pocket and stacked with the side chain of His41. The P1′ ligand, 6-chloro-2-methyl-2H-indazole moiety, held hydrogen bonding with the Thr26 main-chain NH and hydrophobic contact with Met49 as seen in the cocrystal structure of 1.
Figure 5.
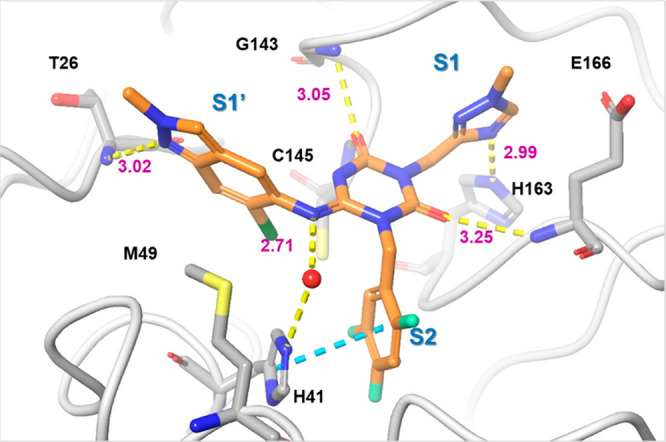
X-ray costructure of S-217622 (3) and 3CLpro (PDB code: 7VU6). 3 is colored in orange and the protein is colored in gray. Water molecules are shown as red spheres. Hydrogen bonds are indicated as yellow dashed lines; π–π stacking is indicated as a cyan dashed line.
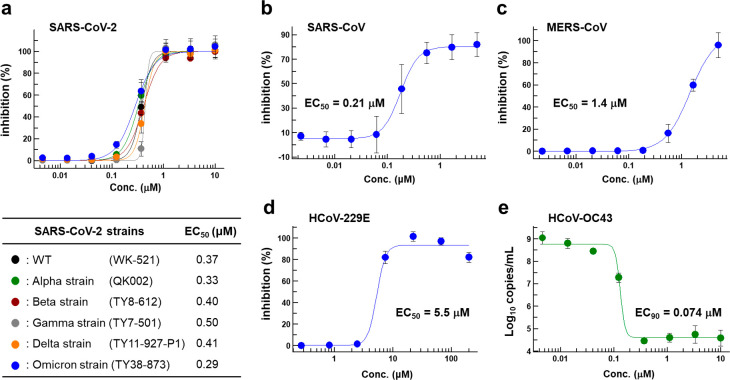
Figure 6 summarizes the in vitro antiviral activities of S-217622 against several clinically isolated SARS-CoV-2 variants and the family of coronaviruses. The antiviral activities were evaluated as per their inhibitory ability of the cytopathic effects elicited in SARS-CoV-2-infected VeroE6/TMPRSS2 cells. S-217622 exhibited similar antiviral activities against all tested SARS-CoV-2 variants, including the Omicron strain, which is responsible for the current wave of the pandemic, indicating its potential broad usability as a therapeutic agent for treating COVID-19 (half-maximal effective concentration [EC50] = 0.29–0.50 μM; Figure 6a, Tables S3 and S4). Because no significant mutations have been reported near the catalytic center of 3CLpro in these variants of concern, orthosteric 3CLpro inhibitors should be effective against all strains known to date. Antiviral activity of S-217622 against SARS-CoV (EC50 = 0.21 μM, Figure 6b) was also comparable to that against SARS-CoV-2, where the sequence homology of 3CLpro between SARS-CoV-2 and SARS-CoV was well-conserved. S-217622 also exhibited potent antiviral activity against MERS-CoV (EC50 = 1.4 μM, Figure 6c), HCoV-OC43 (EC90 = 0.074 μM, Figure 6e), and HCoV-229E (EC50 = 5.5 μM, Figure 6d). As described above, S-217622 displayed broad antiviral activities against a range of coronaviruses (Figure 6, Table S5), suggesting possible applications of this compound or its derivatives for the next pandemic caused by future emerging coronaviruses. S-217622 showed no inhibitory activity against host-cell proteases, such as caspase-2, chymotrypsin, cathepsin B/D/G/L, and thrombin at up to 100 μM, suggesting its high selectivity for coronavirus proteases (Table 1). S-217622 exhibited no safety concerns in vitro in studies involving ether-a-go-go-related gene inhibition, mutagenicity/clastogenicity, and phototoxicity (Table S6).
Figure 6.
In vitro cellular activity of S-217622. Antiviral activity of S-217622 against (a) various SARS-CoV-2 strains, (b) SARS-CoV, and (c) MERS-CoV in a cytopathic effect (CPE) inhibition assay using VeroE6/TMPRSS2 cells. Antiviral activity of S-217622 against (d) HCoV-229E (Alphacoronavirus) in a CPE inhibition assay with MRC-5 cells and (e) HCoV-OC43 (Betacoronavirus) in a real-time quantitative reverse transcription polymerase chain reaction (RT-qPCR) assay with MRC-5 cells. Data are the means ± standard deviation; n = 3 biological replicates for SARS-CoV-2 strains, MERS-CoV, HCoV-229E, and HCoV-OC43 and n = 4 for SARS-CoV.
Table 1. Enzymatic Inhibitory Activity of S-217622 against Human Host Proteases and an HIV-1 Proteasea.
| protease | IC50 (μM) |
|---|---|
| caspase 2 | >100 |
| chymotrypsin | >100 |
| chathepsin B | >100 |
| chathepsin D | >100 |
| chathepsin G | >100 |
| chathepsin L | >100 |
| thorombin | >100 |
| HIV-1 protease | >100 |
Inhibitory activities were <50% at 100 μM.
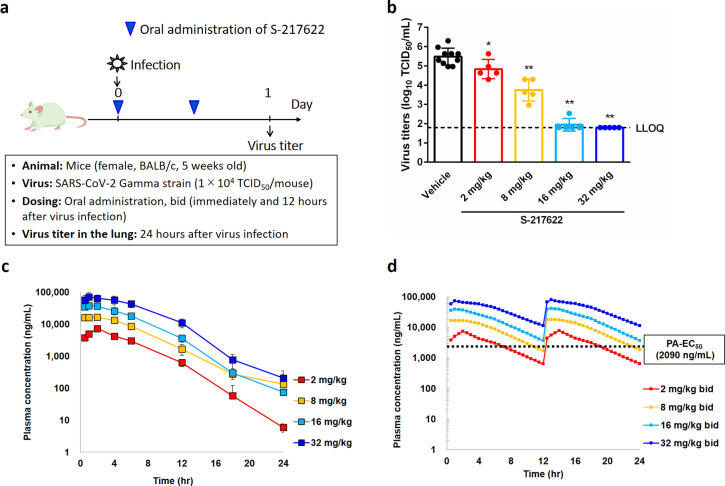
We evaluated the antiviral efficacy of S-217622in vivo in mice infected with SARS-CoV-2 Gamma strain (Figure 7). K417T, E484 K, and N501Y mutations at the receptor-binding domain of the Spike protein in SARS-CoV-2 gamma strain promote interactions with mouse ACE2.20 Five-week-old BALB/c mice were intranasally inoculated with SARS-CoV-2 Gamma strain (hCoV-19/Japan/TY7-501/2021), and S-217622 was administered orally as a 0.5% methylcellulose suspension immediately and 12 hours after infection (Figure 7a). Twenty-four hours after viral infection, the mice were euthanized, and the viral titers in their lung homogenates were measured. S-217622 treatment reduced the intrapulmonary viral titers dose-dependently (Figure 7b). The mean viral titer was significantly lower in the S-217622 treatment groups than in the vehicle treatment group (2 mg/kg vs vehicle, p = 0.0289; 8, 16, and 32 mg/kg vs vehicle, p < 0.0001). Viral titers reached near the lower limit of quantification (1.80 – log10 50% tissue culture infectious dose [TCID50]/mL) at 16 and 32 mg/kg in the S-217622 treatment group. The plasma concentration increased dose-dependently between 2 and 32 mg/kg in the infected mice (Figure 7c), and at doses of ≥16 mg/kg, the plasma concentration was estimated to be above the protein-adjusted-EC50 (PA-EC50) value (extrapolated to 100% mouse serum, 3.93 μmol/L = 2090 ng/mL) over time, indicating the importance of the free plasma concentration for in vivo efficacy (Figure 7d). Although we applied twice-daily treatment in this mouse model, a once-daily treatment model could be applicable in clinical treatment because S-217622 showed a much lower clearance and longer elimination half-lives in nonrodents than in rodents (Figure 3).
Figure 7.
Dose-dependent in vivo antiviral efficacy of S-217622 in mice infected with SARS-CoV-2. (a) Protocol for the in vivo study. bid = twice a day. (b) Effect of S-217622 (administered as S-217622 fumaric acid) treatment on lung viral titers in SARS-CoV-2 gamma strain (hCoV-19/Japan/TY7-501/2021)-infected mice. TCID50 = 50% tissue culture infectious dose; each point represents an individual viral titer (n = 5–10). The broken line represents the lower limit of quantification (1.80 log10 TCID50/mL). The following p-values were calculated using Dunnett’s test: *p < 0.05 and **p < 0.0001 vs vehicle. (c) S-217622 plasma concentration in the infected mice (n = 4). (d) Simulated S-217622 plasma concentrations after repeated oral administration of S-217622 (administered as S-217622 fumaric acid) twice daily in infected mice as per nonparametric superposition. PA-EC50 = protein-adjusted EC50 extrapolated to 100% mouse serum.
Chemistry
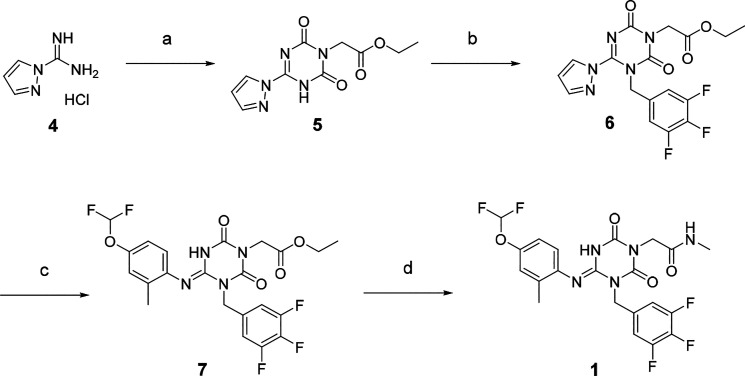
The synthetic scheme for compound 1 is described in Scheme 1. Starting from the pyrazole derivative 4, cyclization with ethyl isocyanatoacetate and CDI was conducted, giving 5 in 90% yield, and then an alkylation with 5-(bromomethyl)-1,2,3-trifluorobenzene followed by introduction of a 4-difluoromethoxy-2-methylaniline unit, to give 7 (40% in 2 steps). The ester group in 7 was hydrolyzed and then amidated with methylamine, yielding 1 (58% in two steps). Compound 2 was synthesized similarly, as shown in Scheme 2.
Scheme 1. Synthesis of Compound 1.
Reagents and conditions: (a) Ethyl isocyanato-acetate, DBU, CDI, DMA, −10 °C to rt, 90%; (b) 5-(bromomethyl)-1,2,3-trifluorobenzene, N,N-diisopropylethylamine, DMA, 60 °C; (c) 4-difluoromethoxy-2-methylaniline, tert-butanol, 100 °C, 40% in two steps; (d) (i) NaOH aq., THF/MeOH, rt; (ii) methylamine, HATU, N,N-diisopropylethylamine, THF, rt, 58% in two steps.
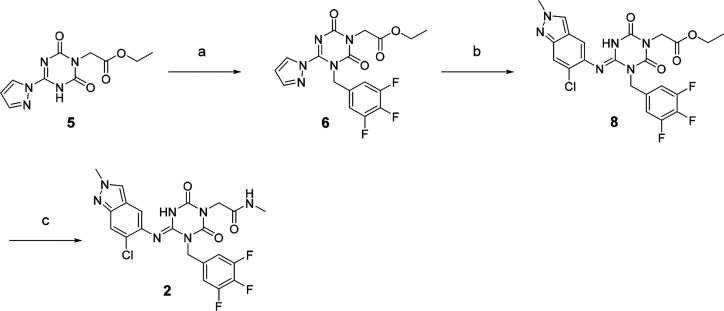
Scheme 2. Synthesis of Compound 2.
Reagents and conditions: (a) 5-(Bromomethyl)-1,2,3-trifluorobenzene, N,N-diisopropylethylamine, DMA, 60 °C; (b) 6-chloro-2-methyl-2H-indazol-5-amine,22tert-amyl alcohol, 100 °C, 44% in two steps from 5; (c) (i) NaOH aq., THF/MeOH, rt; (ii) methylamine, HATU, N,N-diisopropylethylamine, THF, rt, 29% in two steps.
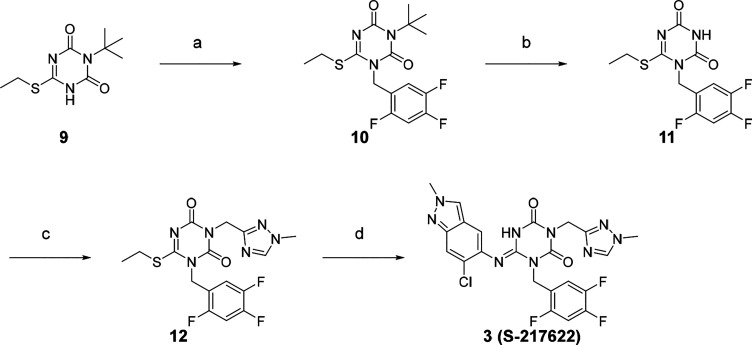
S-217622 (3) was synthesized, as described in Scheme 3. Starting from known compound 9,21 an alkylation with 1-(bromomethyl)-2,4,5-trifluorobenzene gave 10 in 93% yield. Then the 3-t-Bu group was removed, the triazole unit was introduced, and the substitution of the SEt moiety with the indazole unit finally gave S-217622 (3).
Scheme 3. Synthesis of Compound 3 (S-217622).
Reagents and conditions: (a) 1-(Bromomethyl)-2,4,5-trifluorobenzene, K2CO3, MeCN, 80 °C, 93%; (b) TFA, rt, 97%; (c) 3-(chloromethyl)-1-methyl-1H-1,2,4-triazole hydrochloride, K2CO3, DMF, 60 °C, 45%; (d) 6-chloro-2-methyl-2H-indazol-5-amine, LHMDS, THF, 0 °C to rt, 25%.
Conclusions
Here, we described the discovery of S-217622, the first nonpeptidic, noncovalent, oral 3CLpro inhibitor clinical candidate for treating COVID-19. When we started this discovery program, most of the known inhibitors were peptide substrate mimetics with covalent warheads that bound covalently to Cys145 in the active site of 3CLpro. We assumed that these peptidic and reactive structural features would cause problems in the DMPK profile, such as low oral bioavailability due to low cell permeability, low metabolic stability, and low stability in the blood. Thus, we began the de novo search for nonpeptidic 3CLpro inhibitors using the SBDD strategy to combat the current SARS-CoV-2 pandemic. Virtual screening followed by biological screening yielded several hit compounds with IC50 values <10 μM, and one of these hit compounds, compound 1, showed a favorable DMPK profile for an oral agent. With use of the X-ray costructure, SBDD-based structural optimization enabled >600-fold activity improvement while maintaining a good DMPK profile; this ultimately yielded the drug candidate S-217622 (3). S-217622 exhibited a favorable preclinical profile as a once-daily oral therapeutic agent for COVID-19 with promising antiviral activities to known variants of concern, a long elimination half-life in vivo, especially in monkeys and dogs, excellent oral bioavailability, and steep efficacy in an in vivo mouse model infected with SARS-CoV-2. These favorable profiles prompted us to progress S-217622 to clinical trials, and studies are ongoing.
Experimental Section
General Chemistry
All commercial reagents and solvents were used as-received without further purification. Reactions were monitored via thin-layer chromatography performed on Merck silica gel plates (60 F254) or analytical liquid chromatography/mass spectroscopy (LC/MS) performed on a Shimadzu Shim-pack XR-ODS (C18, 2.2 μm, 3.0 × 50 mm, linear gradient from 10% to 100% B over 3 min, then 100% B for 1 min [A = water + 0.1% formic acid, B = MeCN + 0.1% formic acid], flow rate: 1.6 mL/min) using a Shimadzu UFLC system equipped with a LCMS-2020 mass spectrometer, LC-20AD binary gradient module, SPD-M20A photodiode array detector (detection at 254 nm), and SIL-20AC sample manager. All compounds used in the bioassay are >95% pure as determined by HPLC analysis. Flash column chromatography was performed on an automated purification system using Fuji Silysia prepacked silica gel columns. 1H and 13C NMR spectra were recorded on a Bruker Advance at 400 and 100 MHz, respectively. Spectral data are reported as follows: chemical shift (as ppm referenced to tetramethylsilane), integration value, multiplicity (s = singlet, d = doublet, t = triplet, q = quartet, m = multiplet, br = broad), and coupling constant. High-resolution mass spectra were recorded on a Thermo Fisher Scientific LTQ Orbitrap using electrospray positive ionization.
Ethyl 2-[2,6-Dioxo-4-(1H-pyrazol-1-yl)-3,6-dihydro-1,3,5-triazin-1(2H)-yl]acetate (5)
To a stirred solution of 1H-pyrazole-1-carboximidamide hydrochloride 4 (53.5 g, 365 mmol) in DMA (214 mL) were added ethyl isocyanatoacetate (49.5 g, 383 mmol) and DBU (57.8 mL, 383 mmol) below −10 °C. The reaction mixture was allowed to warm to 0 °C and stirred for 30 min at the same temperature. CDI (89.0 g, 548 mmol) and DBU (85.0 mL, 566 mmol) were added to the mixture below 10 °C. After being stirred at room temperature overnight, the reaction mixture was quenched with aqueous 2 M HCl (1000 mL). The solid was filtered and washed with H2O to afford 5 (86.8 g, 90%) as a white solid. 1H NMR (400 MHz, DMSO-d6) δ 1.21 (3H, t, J = 7.1 Hz), 4.15 (2H, q, J = 7.1 Hz), 4.52 (2H, s), 6.74 (1H, dd, J = 2.9, 1.5 Hz), 8.08 (1H, d, J = 1.0 Hz), 8.59 (1H, dd, J = 2.9 Hz). 13C NMR (100 MHz, DMSO-d6) δ 14.03, 42.19, 61.24, 111.38, 130.47, 145.82, 151.32, 152.12, 167.64. HRMS-ESI (m/z): [M + H]+ calcd for [C10H12N5O4]+ 266.0877; found 266.0884; purity, 100% (LCMS).
Ethyl (4E)-2-(4-{[4-(difluoromethoxy)-2-methylphenyl]imino}-2,6-dioxo-3-(3,4,5-trifluorobenzyl)-1,3,5-triazinan-1-yl)acetate (7)
A mixture of 5 (1.06 g, 4.00 mmol), N,N-diisopropylethylamine (0.907 mL, 5.20 mmol), and 5-(bromomethyl)-1,2,3-trifluorobenzene (0.631 mL, 4.80 mmol) in DMA (10 mL) was stirred at 60 °C for 5 h. Then the reaction mixture was cooled to room temperature and diluted with H2O and EtOAc. The aqueous layer was extracted with EtOAc. The organic layer was washed with H2O and brine, dried over MgSO4, and concentrated under reduced pressure to afford a crude product of 6 (1.65 g). After a mixture of 6 (268 mg, ≤0.665 mmol) and 4-(difluoromethoxy)-2-methylaniline (0.094 mL, 0.665 mmol) in tert-butanol (2.7 mL) was stirred at 100 °C for 30 min, the reaction mixture was allowed to cool to room temperature. The mixture was concentrated under reduced pressure. The residue was purified by silica gel column chromatography (n-hexane/EtOAc, gradient, 15–33% EtOAc) to afford 7 (134 mg, 40% over two steps) as a white solid. 1H NMR (400 MHz, CDCl3) δ 1.31 (3H, t, J = 7.2 Hz), 2.01 (3H, s), 4.26 (2H, q, J = 7.2 Hz), 4.57 (2H, s), 5.17 (2H, s), 6.48 (1H, t, J = 74.0 Hz), 6.72 (1H, d, J = 8.5 Hz), 6.98 (1H, dd, J = 8.5, 2.4 Hz), 7.03 (1H, d, J = 2.4 Hz), 7.19 (2H, t, J = 7.3 Hz), 7.40 (1H, br s). 13C NMR (100 MHz, CDCl3) δ 14.11, 17.92, 42.71, 44.95, 62.16, 113.36 (dd, J = 16.1, 5.9 Hz), 115.95 (t, J = 260 Hz), 118.88, 121.78, 122.97, 132.09, 132.03–132.23 (m), 136.80, 139.52 (dt, J = 251.9, 15.2 Hz), 140.50, 147.13, 147.80 (t, J = 2.9 Hz), 149.46, 151.07 (ddd, J = 250.2, 9.5, 3.7 Hz), 167.35. HRMS-ESI (m/z): [M + H]+ calcd for [C22H20F5N4O5]+ 515.1359; found 515.1348; purity, 100% (LCMS).
(4E)-2-(4-{[4-(Difluoromethoxy)-2-methylphenyl]imino}-2,6-dioxo-3-(3,4,5-trifluorobenzyl)-1,3,5-triazinan-1-yl)-N-methylacetamide (1)
To a stirred solution of 7 (100 mg, 0.194 mmol) in THF/MeOH (2 mL, v/v = 1/1) was added NaOH (1 M aqueous solution, 1.37 mL, 1.37 mmol) at room temperature. After being stirred at room temperature for 2 h, the reaction mixture was quenched with 1 M aqueous HCl solution. The aqueous layer was extracted with EtOAc. The organic layer was washed with H2O and brine, dried over MgSO4, and concentrated under reduced pressure to afford a crude residue (71.1 mg). To the residue (71.1 mg, ≤0.146 mmol) in THF (0.6 mL) were added methylamine (2 M in THF, 0.110 mL, 0.219 mmol), N,N-diisopropylethylamine (0.077 mL, 0.439 mmol), and HATU (83.0 mg, 0.219 mmol). After being stirred at room temperature overnight, the reaction mixture was diluted with H2O and EtOAc. The aqueous layer was extracted with EtOAc. The organic layer was washed with H2O and brine, dried over MgSO4, and concentrated under reduced pressure. The residue was purified by silica gel column chromatography (CHCl3/MeOH, gradient, 0–10% MeOH). The collected fraction was recrystallized from n-hexane/EtOAc to afford 1 (60.7 mg, 58% over two steps) as a white solid. 1H NMR (400 MHz, CDCl3) δ 1.97 (3H, s), 2.86 (3H, d, J = 4.8 Hz), 4.33 (2H, s), 5.13 (2H, s), 5.76 (1H, d, J = 4.8 Hz), 6.47 (1H, t, J = 74.2 Hz), 6.68 (1H, d, J = 8.3 Hz), 6.92 (1H, dd, J = 8.3, 2.4 Hz), 6.97 (1H, d, J = 2.4 Hz), 7.16 (2H, t, J = 7.4 Hz), 8.15 (1H, br s). 13C NMR (100 MHz, CDCl3) δ 17.93, 26.49, 43.67, 44.96, 113.27 (dd, J = 16.1, 5.9 Hz), 116.18 (t, J = 259.7 Hz), 118.59, 122.03, 122.56, 122.9, 132.21, 132.21–132.39 (m), 136.83, 139.44 (dt, J = 252.4, 15.0 Hz), 140.87, 147.56 (t, J = 2.9 Hz), 147.84, 149.68, 151.02 (ddd, J = 250.2, 10.3, 3.7 Hz), 166.40. HRMS-ESI (m/z): [M + H]+ calcd for [C21H19F5N5O4]+ 500.1352; found 500.1348; purity, 100% (LCMS).
Ethyl (4E)-2-{4-[(6-Chloro-2-methyl-2H-indazol-5-yl)imino]-2,6-dioxo-3-(3,4,5-trifluorobenzyl)-1,3,5-triazinan-1-yl}acetate (8)
A mixture of 6 (291 mg, ≤0.711 mmol) and 6-chloro-2-methyl-2H-indazol-5-amine22 (129 mg, 0.711 mmol) in tert-amyl alcohol (3 mL) was stirred at 100 °C for 2 h. The reaction mixture was cooled to room temperature and then concentrated under reduced pressure. The residue was triturated with EtOAc, and the solid was filtered and washed with EtOAc to afford 8 (160 mg, 44% over two steps) as a white solid. 1H NMR (400 MHz, DMSO-d6, DCl in D2O) δ 1.18 (3H, t, J = 7.2 Hz), 4.12 (2H, q, J = 7.2 Hz), 4.15 (3H, s), 4.47 (2H, s), 5.28 (2H, s), 7.37 (2H, dd, J = 8.8, 7.0 Hz), 7.47 (1H, s), 7.74 (1H, s), 8.37 (1H, s). 13C NMR (100 MHz, DMSO-d6, DCl in D2O) δ 14.04, 40.20, 42.78, 44.44, 61.25, 79.33, 111.93 (dd, J = 16.1, 5.1 Hz), 116.84, 120.66, 125.43, 127.92, 128.65, 131.63, 133.46–133.65 (m), 137.98 (dt, J = 248.2, 15.4 Hz), 146.39, 150.22 (ddd, J = 247.0, 10.1, 3.9 Hz), 150.39, 150.52, 168.00. HRMS-ESI (m/z): [M + H]+ calcd for [C22H19ClF3N6O4]+ 523.1103; found 523.1104; purity, 99% (LCMS).
(4E)-2-{4-[(6-Chloro-2-methyl-2H-indazol-5-yl)imino]-2,6-dioxo-3-(3,4,5-trifluorobenzyl)-1,3,5-triazinan-1-yl)-N-methylacetamide (2)
To a stirred solution of 8 (445 mg, 0.851 mmol) in THF/MeOH (4.5 mL, v/v = 1/1) was added aqueous NaOH (1 M solution, 2.55 mL, 2.55 mmol) at room temperature. After being stirred at room temperature for 70 min, the reaction mixture was diluted with EtOAc and then quenched with aqueous 2 M HCl solution. The aqueous layer was extracted with EtOAc. The organic layer was washed with H2O and brine, dried over Na2SO4, and concentrated under reduced pressure. The residue was triturated with diisopropylether, and the solid was filtered and washed with diisopropylether to afford a crude residue (467 mg). To the crude residue (100 mg, ≤0.202 mmol) in THF (2 mL) were added methylamine (2 M in THF, 0.152 mL, 0.303 mmol), N,N-diisopropylethylamine (0.106 mL, 0.606 mmol), and HATU (115 mg, 0.303 mmol). After being stirred at room temperature overnight, the reaction mixture was diluted with H2O and EtOAc. The aqueous layer was extracted with EtOAc. The organic layer was washed with H2O and brine, dried over MgSO4, and concentrated under reduced pressure. The residue was purified by silica gel column chromatography (CHCl3/MeOH, gradient, 0–2% MeOH). The collected fraction was recrystallized from n-hexane/EtOAc to afford 2 (26.6 mg, 29% over two steps) as a white solid. 1H NMR (400 MHz, DMSO-d6, DCl in D2O) δ 2.57 (3H, s), 4.15 (3H, s), 4.27 (2H, s), 5.24 (2H, s), 7.38 (1H, s), 7.41 (2H, dd, J = 8.7, 7.2 Hz), 7.73 (1H, s), 8.36 (1H, s). 13C NMR (100 MHz, DMSO-d6, DCl in D2O) δ 25.47, 40.19, 43.99, 44.47, 79.37, 111.98 (dd, J = 16.9, 5.1 Hz), 115.78, 116.77, 120.81, 125.39, 128.64, 132.87, 133.78–133.97 (m), 137.91 (dt, J = 248.0, 15.4 Hz), 145.57, 146.14, 150.22 (ddd, J = 246.7, 9.9, 4.0 Hz), 150.30, 150.51, 166.97. HRMS-ESI (m/z): [M + H]+ calcd for [C21H18ClF3N7O3]+ 508.1106; found 508.1106; purity, 100% (LCMS).
3-(tert-Butyl)-6-(ethylthio)-1,3,5-triazine-2,4-(1H,3H)-dione (9)
Compound 9 was prepared according to the reported procedure.211H NMR (400 MHz, CDCl3) δ 1.36 (3H, t, J = 7.4 Hz), 1.66 (9H, s), 3.14 (2H, q, J = 7.4 Hz). 13C NMR (100 MHz, CDCl3) δ 14.35, 25.22, 29.20, 61.55, 152.26, 154.19, 165.96. HRMS-ESI (m/z): [M + H]+ calcd for [C9H16N3O2S]+ 230.0958; found 230.0952; purity, 97% (LCMS).
3-(tert-Butyl)-6-(ethylthio)-1-(2,4,5-trifluorobenzyl)-1,3,5-triazine-2,4-(1H,3H)-dione (10)
A mixture of 9 (100 mg, 0.436 mmol), potassium carbonate (78.0 mg, 0.567 mmol), and 1-(bromomethyl)-2,4,5-trifluorobenzene (0.063 mL, 0.480 mmol) in MeCN (0.8 mL) was stirred at 80 °C for 2 h. The reaction mixture was cooled to room temperature, and then the mixture was diluted with EtOAc. The precipitate was filtered, and the filtrate was concentrated under reduced pressure. The residue was purified by silica gel column chromatography (n-hexane/EtOAc gradient, 0–30% EtOAc) to afford 10 (151 mg, 93%) as a colorless oil. 1H NMR (400 MHz, CDCl3) δ 1.33 (3H, t, J = 7.4 Hz), 1.65 (9H, s), 3.15 (2H, q, J = 7.4 Hz), 5.03 (2H, s), 6.91–7.01 (2H, m). 13C NMR (100 MHz, CDCl3) δ 13.73, 26.88, 28.88, 41.05 (d, J = 4.4 Hz), 61.59, 105.92 (dd, J = 27.5, 20.9 Hz), 116.24 (ddd, J = 20.5, 5.1, 1.5 Hz), 118.65 (td, J = 10.5, 5.4 Hz), 147.03 (ddd, J = 246.1, 12.8, 3.7 Hz), 149.72 (ddd, J = 252.4, 13.9, 12.5 Hz), 150.36, 152.98, 155.24 (ddd, J = 246.5, 9.5, 2.9 Hz), 166.69. HRMS-ESI (m/z): [M + H]+ calcd for [C16H19F3N3O2S]+ 374.1145; found 374.1142; purity, 100% (LCMS).
6-(Ethylthio)-1-(2,4,5-trifluorobenzyl)-1,3,5-triazine-2,4-(1H,3H)-dione (11)
A mixture of 10 (4.88 g, 13.08 mmol) in TFA (9.8 mL) was stirred at room temperature for 4 h and then was left to stand at the same temperature overnight. After concentration under reduced pressure, the residue was azeotroped with toluene and triturated with diisopropylether to afford 11 (4.01 g, 97%) as a white solid. 1H NMR (400 MHz, CDCl3) δ 1.37 (3H, t, J = 7.4 Hz), 3.23 (2H, q, J = 7.4 Hz), 5.15 (2H, s), 6.95–7.09 (2H, m), 8.23 (1H, br s). 13C NMR (100 MHz, DMSO-d6) δ 13.73, 26.40, 40.66 (d, J = 3.7 Hz), 106.13 (dd, J = 28.2, 21.6 Hz), 116.51 (dd, J = 20.9, 4.8 Hz), 119.52 (dq, J = 16.1, 3.2 Hz), 145.05–149.96, 150.08, 152.42, 154.70 (ddd, J = 244.5, 10.1, 2.4 Hz), 169.98. HRMS-ESI (m/z): [M + H]+ calcd for [C12H11FN3O2S]+ 318.0519; found 318.0516; purity, 100% (LCMS).
6-(Ethylthio)-3-[(1-methyl-1H-1,2,4-triazol-3-yl)methyl]-1-(2,4,5-trifluorobenzyl)-1,3,5-triazine-2,4-(1H,3H)-dione (12)
A mixture of 11 (2.50 g, 7.88 mmol), 3-(chloromethyl)-1-methyl-1H-1,2,4-triazole hydrochloride (1.99 g, 11.8 mmol), and potassium carbonate (3.27 g, 23.6 mmol) in DMF (23 mL) was stirred at 60 °C for 3.5 h. The reaction mixture was allowed to cool to room temperature and diluted with aqueous NH4Cl solution. The precipitate was filtered and washed with H2O. The solid was purified by silica gel column chromatography (n-hexane/EtOAc gradient, 30–60% EtOAc) to afford 12 (1.47 g, 45%) as a white solid. 1H NMR (400 MHz, CDCl3) δ 1.34 (3H, t, J = 7.4 Hz), 3.20 (2H, q, J = 7.4 Hz), 3.84 (3H, s), 5.16 (2H, s), 5.23 (2H, s), 6.92–6.98 (1H, m), 7.10–7.17 (1H, m), 7.93 (1H, s). 13C NMR (100 MHz, CDCl3) δ 13.55, 27.31, 36.13, 39.92, 41.11 (d, J = 3.7 Hz), 105.80 (dd, J = 27.5, 20.9 Hz), 116.20 (dd, J = 20.5, 3.7 Hz), 118.11 (td, J = 11.0, 4.9 Hz), 144.33, 145.87–151.14, 150.57, 151.68, 155.18 (ddd, J = 246.5, 9.5, 2.9 Hz), 159.29, 169.56. HRMS-ESI (m/z): [M + H]+ calcd for [C16H16F3N6O2S]+ 413.1002; found 413.0998; purity, 100% (LCMS).
(6E)-6-[(6-Chloro-2-methyl-2H-indazol-5-yl)imino]-3-[(1-methyl-1H-1,2,4-triazol-3-yl)methyl]-1-(2,4,5-trifluorobenzyl)-1,3,5-triazinane-2,4-dione (3, S-217622)
To a solution of 12 (300 mg, 0.727 mmol) and 6-chloro-2-methyl-2H-indazol-5-amine22 (172 mg, 0.946 mmol) in THF (6 mL) was added LHMDS (1 M in THF; 1.46 mL, 1.46 mmol) dropwise at 0 °C. The reaction mixture was stirred at 0 °C for 2.5 h and then at rt for 40 min. The reaction was quenched with aqueous NH4Cl solution, and the aqueous layer was extracted with EtOAc. The organic layer was washed with brine, dried over MgSO4, and concentrated under reduced pressure. The residue was purified by silica gel column chromatography (CHCl3/MeOH gradient, 0–20% MeOH). The solid was solidized from acetone/H2O to afford 3 (S-217622) (95.3 mg, 25%) as a pale brown solid. 1H NMR (400 MHz, DMSO-d6, DCl in D2O) δ 3.90 (3H, s), 4.15 (3H, s), 5.04 (2H, s), 5.26 (2H, s), 7.44 (1H, m), 7.52–7.65 (2H, m), 7.73 (1H, s), 8.40 (1H, s), 9.31 (1H, s). 13C NMR (100 MHz, DMSO-d6, DCl in D2O) δ 37.34, 38.04, 40.06, 40.29, 106.16 (dd, J = 28.2, 21.6 Hz), 116.46–116.70, 116.70, 120.54–120.76, 120.76, 125.93, 129.10, 132.35, 143.84, 145.98, 146.38 (ddd, J = 241.4, 12.5, 3.7 Hz), 146.60, 148.52 (td, J = 247.7, 13.6 Hz), 150.43, 150.50, 155.22 (ddd, J = 244.3, 10.3, 2.2 Hz), 155.58. HRMS-ESI (m/z): [M + H]+ calcd for [C22H18 F3ClN9O2]+ 532.1219; found 532.1221; purity, 100% (LCMS).
Preparation of Compound 3 (S-217622) Fumaric Acid: (6E)-6-[(6-Chloro-2-methyl-2H-indazol-5-yl)imino]-3-[(1-methyl-1H-1,2,4-triazol-3-yl)methyl]-1-(2,4,5-trifluorobenzyl)-1,3,5-triazinane-2,4-dione Fumaric Acid (1:1)
A mixture of 3(S-217622) (1.17 g, 2.2 mmol) and fumaric acid (278 mg, 2.4 mmol) in EtOAc (5.9 mL) was stirred at room temperature for 45 min. The suspension was filtrated to afford 3 (S-217622) fumaric acid (1.37 g, 95%) as a white solid. 1H NMR (400 MHz, pyridine-d5) δ 3.64 (s, 3H), 3.99 (s, 3H), 5.56 (s, 2H), 5.61 (s, 2H), 7.16–7.25 (m, 2H), 7.44 (s, 2H), 7.81 (s, 1H), 7.89 (s, 1H), 7.89–7.97 (m, 1H), 8.32 (s, 1H); purity, 98.2% (HPLC).
Cells and Viruses
Remdesivir was purchased from MedChemExpress. VeroE6/TMPRSS2 cells from the National Institutes of Biomedical Innovation (Tokyo, Japan) were used to evaluate the antiviral activity against SARS-CoV-2. Those prepared by Hokkaido University as previously reported23 were used to evaluate the antiviral activities against SARS-CoV and MERS-CoV. MRC-5 cells (CCL-171) were purchased from American Type Culture Collection (ATCC; Manassas, VA, USA). Cells were maintained in Dulbecco’s modified Eagle’s medium (Thermo Fisher Scientific) supplemented with 10% heat-inactivated fetal bovine serum (FBS) (Sigma-Aldrich Co., Ltd.) at 37 °C with 5% CO2.
SARS-CoV-2 clinical isolates were obtained from the National Institute of Infectious Diseases (NIID; Tokyo, Japan): hCoV-19/Japan/TY/WK-521/2020 (Pango Lineage: A), hCoV-19/Japan/QK002/2020 (Alpha, B.1.1.7), hCoV-19/Japan/QHN001/2020 (Alpha, B.1.1.7), hCoV-19/Japan/QHN002/2020 (Alpha, B.1.1.7), hCoV-19/Japan/TY7-501/2021 (Gamma, P.1), hCoV-19/Japan/TY7-503/2021 (Gamma, P.1), hCoV-19/Japan/TY8-612/2021 (Beta, B.1.351), hCoV-19/Japan/TY11-927-P1/2021 (Delta, B.1.617.2), and hCoV-19/Japan/TY38-873/2021 (Omicron, B.1.1.529). All SARS-CoV-2 strains were propagated in VeroE6/TMPRSS2 cells, and infectious titers were determined by standard tissue culture infectious dose (TCID)50 in VeroE6/TMPRSS2 cells. SARS-CoV (Hanoi strain) was provided by Dr. Koichi Morita of Nagasaki University.24 MERS-CoV (EMC/2012) was provided by Dr. Bart L. Haagmans, Erasmus University Medical Center.25 VeroE6 cells (ATCC) were used to propagate SARS-CoV; VeroE6/TMPRSS2 cells were used to propagate MERS-CoV. HCoV-OC43 and HCoV-229E were obtained from ATCC.
3CL Protease Inhibition Assay
The 3CL protease inhibition assay was conducted in 384-well plates (Corning 3702). The substance solution (10 mM dimethyl sulfoxide [DMSO] solution) was diluted to 250 μmol/L stepwise with a threefold dilution with DMSO. Finally, the solutions were mixed with 20 mmol/L Tris-HCl (pH 7.5) as a compound solution. Ten microliters of compound solution was added manually to each well, and then 5 μL of 16 μM substrate in inhibition buffer (2 mM EDTA, 20 mM DTT, 0.02% BSA, and 20 mM Tris-HCl, pH 7.5) was added. The reaction was initiated by adding 5 μL of 12 nM 3CL protease (R&D Systems, Inc.) in an inhibition buffer and incubated at room temperature for 3 h. The following operations were the same as those described in the Biological Screening.
Biological Screening
The compound screening assay was performed in 384-well plates (Corning 3702 or Greiner 781280). Testing compound (159 nL) at various concentrations was added to each well by an ECHO 555 dispenser (Labcyte Inc.). Next, 7.5 μL of 8 μM substrate (Dabcyl-KTSAVLQSGFRKME [Edans]-NH2, 3249-v, Peptide Institute, Inc.) in assay buffer (100 mM NaCl, 1 mM ethylenediaminetetraacetic acid [EDTA], 10 mM dl-dithiothreitol (DTT), 0.01% bovine serum albumin [BSA], and 20 mM Tris-HCl, pH 7.5) was dispensed using Multidrop Combi (Thermo Scientific). The reaction was initiated by adding 7.5 μL of 6 or 0.6 nM 3CL protease (R&D Systems, Inc.) in assay buffer and incubated at room temperature for 3 h. After incubation, the reaction was stopped by adding 45 μL of water solution containing 0.1% formic acid, 10% acetonitrile, and 0.05 μmol/L Internal Standard (IS) peptide (Dabcyl-KTSAVLeu [13C6,15N]-Q, custom-synthesized by Peptide Institute, Inc.). The reactions were analyzed with MS using a RapidFire 360 high-throughput sampling robot (Agilent Technologies) connected to an iFunnel Agilent 6550 accurate mass quadrupole time-of-flight mass spectrometer using electrospray. Peak areas were acquired and analyzed using a RapidFire Integrator (Agilent Technologies). Reaction product peak areas were acquired from m/z 499.27; IS peak areas were acquired from m/z 502.78. IC50 values were determined by plotting the compound concentration versus inhibition and fitting data with a four-parameter logistical fit (Model 205, XLfit).
Cellular Antiviral Activity
Antiviral activity against SARS-CoV-2, SARS-CoV, MERS-CoV, and HCoV-229E was assessed by monitoring the cell viability; that against HCoV-OC43 was assessed by monitoring viral RNA in a cell suspension. EC50 values were determined by plotting the compound concentration versus inhibition and fitting data with a four-parameter logistical fit (Model 205, XLfit). EC90 values against HCoV-OC43 were determined from the resulting dose–response curves and calculated with the two-point method.
Antiviral activities against SARS-CoV-2 were evaluated using VeroE6/TMPRSS2 cells. VeroE6/TMPRSS2 cells (1.5 × 104/well) suspended in minimum essential medium (MEM) (Thermo Fisher Scientific) supplemented with heat-inactivated 2% FBS were seeded into 96-well plates with diluted compounds in each well. Cells were infected with each SARS-CoV-2 at 30–3000 TCID50/well and cultured at 37 °C with 5% CO2 for 3 days or 4 days. Cell viability was assessed using a CellTiter-Glo 2.0 assay (Promega). The CC50 was assessed in the absence of viruses after being cultured for 3 days.
Antiviral activities against SARS-CoV and MERS-CoV were evaluated at Hokkaido University using VeroE6/TMPRSS2 cells as previously reported.23 VeroE6/TMPRSS2 cells (1.5 × 104/well) suspended in 2% FBS-containing MEM were seeded into 96-well plates with diluted compounds in each well. Cells were infected with each SARS-CoV at 1000 TCID50/well or MERS-CoV 2500 TCID50/well and cultured at 37 °C with 5% CO2 for 3 days. Cell viability was assessed via (3-[4,5-dimethyl-2-thiazolyl]-2,5-diphenyl-2H-tetrazolium bromide (MTT) assay (Nacalai Tesque) as previously described.26
Antiviral activity against HCoV-229E was evaluated using MRC-5 cells. MRC-5 cells (2.0 × 104/well) suspended in 2% FBS-containing MEM were seeded into 96-well plates and incubated at 37 °C with 5% CO2 overnight. The next day, the cells were infected with HCoV-229E at 1000 TCID50/well and incubated at 37 °C with 5% CO2 for 1 h, followed by removal of the inoculum and addition of 2% FBS-containing MEM with the diluted compounds. Cells infected with HCoV-229E were incubated at 37 °C with 5% CO2 for 3 days. Cell viability was assessed using a CellTiter-Glo 2.0 assay.
Antiviral activity against HCoV-OC43 was evaluated using MRC-5 cells. MRC-5 cells (2.0 × 104/well) suspended in 2% FBS-containing MEM were seeded into 96-well plates and incubated at 37 °C with 5% CO2 overnight. The next day, the cells were infected with HCoV-OC43 at 100 TCID50/well and incubated at 37 °C with 5% CO2 for 1 h, followed by removal of the inoculum and addition of 2% FBS-containing MEM with the diluted compounds. Cells infected with HCoV-OC43 were incubated at 37 °C with 5% CO2 for 42 h, and viral RNA was extracted from the supernatants using a Quick-RNA Viral Kit (Zymo Research, #R1041). Viral RNA was quantified via real-time PCR (Applied Biosystems, QuantStudio 3) with specific primers and probes for HCoV-OC43 detection.27
Cellular Antiviral Activity in the Presence of Mouse Serum
Antiviral activity against SARS-CoV-2 in the presence of mouse serum was assessed by monitoring cell viability. S-217622 was diluted with 3.125%, 6.25%, 12.5%, and 25% mouse serum in MEM supplemented with heat-inactivated 2% FBS. One hundred microliters of serially diluted compound solutions was added to a 96-well plate and incubated at room temperature for approximately 1 h. Each 50 μL/well of VeroE6/TMPRSS2 cells was adjusted to 3.0 × 105 cells/mL with MEM supplemented with heat-inactivated 2% FBS and dispensed on the plate. Each 50 μL/well of SARS-CoV-2 was added at 10000 TCID50/well and cultured at 37 °C with 5% CO2 for 3 days. Cell viability was assessed using a CellTiter-Glo 2.0 assay, followed by the determination of the EC50 value from the cell viability. PA-EC50 extrapolated to 100% serum was calculated by linear regression using the EC50 value of each serum concentration. PS extrapolated to 100% serum was calculated by dividing the PA-EC50 (extrapolated value of 100% mouse serum) by EC50 (in the presence of mouse serum).
Human Protease Enzyme Assay
Selectivity tests against a variety of host protease activity were conducted by Eurofins Panlabs Discovery Services Taiwan, Ltd., on behalf of Shionogi Co. & Ltd. as per established protocols. S-217622 was tested on a set of seven proteases (caspase-2, chymotrypsin, cathepsin B/D/G/L, and thrombin) at 100 μM.
In Vivo SARS-CoV-2 Infection and Treatment Studies
In vivo SARS-CoV-2 infection experiments were conducted in accordance with the guidelines of the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC). The animal study protocol was approved by the director of the institute based on the report of the Institutional Animal Care and Use Committee of Shionogi Research Laboratories.
Mouse in vivo SARS-CoV-2 infection studies were done at Shionogi Pharmaceutical Research Center (Osaka, Japan). Five-week-old female BALB/cAJcl mice (CLEA Japan, Inc.; n = 5 or 10 per group) were intranasally inoculated with SARS-CoV-2 Gamma strain (hCoV-19/Japan/TY7-501/2021) (10000 TCID50/mouse) under anesthesia. Immediately after infection, the mice were orally administered S-217622 fumaric acid (2, 8, 16, or 32 mg/kg q12h; n = 5 per group) or vehicle (0.5 w/v% methyl cellulose in aqueous solution q12h; n = 10 per group) for 1 day. Twenty-four hours postinfection, the mice were euthanized via cervical dislocation under anesthesia; their lungs were removed, and the viral titers in the lung homogenates were determined using VeroE6/TMPRSS2 cells. Viral titers are expressed as log10 TCID50/mL.
PK Study in Infected Mice
PK experiments in infected mice were conducted in accordance with the guidelines provided by AAALAC and were approved by IACUC of Shionogi Research Laboratories.
Mouse PK studies were done at Shionogi Pharmaceutical Research Center (Osaka, Japan). BALB/cAJcl mice were intranasally inoculated with SARS-CoV-2 Gamma strain (hCoV-19/Japan/TY7-501/2021) (10000 TCID50/mouse) and orally administered with S-217622 fumaric acid (2, 8, 16, or 32 mg/kg) immediately after infection. Blood was taken at 0.5, 1, 2, 4, 6, 12, 18, and 24 h after dosing (n = 4 per group per time point), and plasma concentrations of S-217622 were determined by LC/MS/MS. LC/MS/MS analysis was performed using a Vanquish Binary Flex system equipped with TSQ Altis (Thermo Fisher Scientific). The plasma concentrations of all dosing groups in the in vivo SARS-CoV-2 infection and treatment studies were simulated by nonparametric analysis from plasma concentration data obtained in the PK study using Phoenix WinNonlin (Ver. 8.1, Certara, L.P.).
Metabolic Stability Studies
Rat liver microsomes (pool of 5, male) were purchased from the Jackson Laboratory Japan, Inc. (Yokohama, Japan) or Charles River Japan, Inc. (Yokohama, Japan). Human liver microsomes (HLM, pool of 15, male and female) were purchased from Sekisui XenoTech (Kansas City, KS). Metabolic stabilities of the test compounds in rat and human liver microsomes were determined at 0.5 μM. The compounds were incubated with 0.5 mg protein/mL in suspension in buffer (50 mM Tris-HCl buffer, pH 7.4, 150 mM KCl, 10 mM MgCl2, 1 mM NADPH) at 37 °C. Microsomal incubations were initiated by adding a 100-fold concentrated solution of the compounds. Incubations were terminated by adding a 2-fold volume of organic solvent (MeCN/MeOH = 1:1) after 0 and 30 min of incubation at 37 °C. The precipitation protein was removed by centrifugation. The supernatants were analyzed by liquid chromatography tandem mass spectrometry (LC/MS/MS). LC/MS/MS was performed using LCMS-8060 (Shimadzu Corporation, Kyoto). All incubations were conducted in duplicate, and the percentage of compound remaining at the end of the incubation was determined from the LC/MS/MS peak area ratio.
Rat PK Studies
The animal study protocol was approved by the director of the institute after reviewing the protocol by the Institutional Animal Care and Use Committee in terms of the 3R (Replacement/Reduction/Refinement) principles.
Rat PK studies were done at Shionogi Pharmaceutical Research Center (Osaka, Japan). Eight-week-old male Sprague–Dawley rats were purchased from Charles River Laboratories. For oral administration, the dosing vehicle was dimethyl sulfoxide/0.5% methylcellulose (400 cP) = 1:4. The compound was orally administered at 1–2 μmol/5 mL/kg (n = 2) under nonfasted conditions. Blood samples (0.2 mL) were collected with 1 mL syringes containing anticoagulants (EDTA-2K and heparin) at 0.5, 1, 2, 4, 8, and 24 h after dosing. For intravenous administration, compounds were formulated as solutions in dimethyl sulfoxide/propylene glycol (1:1, v/v) and intravenously administered via the tail vein at 0.5–1.0 μmol/mL/kg (n = 2) under isoflurane anesthesia under nonfasted conditions. Blood samples (0.2 mL) were collected with 1 mL syringes containing anticoagulants (EDTA-2K and heparin) at 3, 10, 30, 60, 120, 240, and 360 min after dosing. Blood samples were centrifuged to obtain plasma samples, which were transferred to each tube and stored in a freezer until analysis. Plasma concentrations were determined by LC/MS/MS after protein precipitation with MeOH or MeCN. LC/MS/MS analysis was performed using a SCIEX Triple Quad 5500 or SCIEX API5000 or SCIEX Triple Quad 5500 (Sciex, Framingham, MA). PK parameters were calculated by noncompartmental analysis.
Dog/Monkey PK Studies
PK experiments in dogs and monkeys were conducted in accordance with the guidelines provided by AAALAC. The animal study protocol was approved by the director of the institute after reviewing the protocol by the Institutional Animal Care and Use Committee in terms of the 3R (Replacement/Reduction/Refinement) principles.
Dog and Monkey PK studies were done at Shionogi Aburahi Research Center (Shiga, Japan). Male beagles were purchased from Marshall BioResources. Female cynomolgus monkeys were purchased from Shin Nippon Biomedical Laboratories, Ltd. or Hamri Co., Ltd. For oral administration, dosing vehicles were 0.5% methylcellulose (400 cP). The compound was orally administered at 3 mg/2 mL/kg (n = 3) under nonfasted conditions. Blood samples (0.3 mL) were collected with 1 mL syringes containing anticoagulants (EDTA-2K and heparin) at 0.25, 0.5, 1, 2, 4, 8, and 24 h after dosing. For intravenous administration, compounds were formulated as solutions in dimethyl acetamide/ethanol/20% HP-β-CD in carbonate buffer (pH 9.0) (2:3:5, by volume) and intravenously administered via a forelimb or hind limb vein at 0.1 mg/0.2 mL/kg (n = 2) under nonfasted conditions. Blood samples (0.2 mL) were collected with 1 mL syringes containing anticoagulants (EDTA-2K and heparin) at 2, 5, 15, 30, 60, 120, 240, 480, and 1440 min after dosing. Blood samples were centrifuged to obtain plasma samples, which were transferred to each tube and stored in a freezer until analysis. Plasma concentrations were determined by LC/MS/MS after protein precipitation with MeOH or MeCN. LC/MS/MS analysis was performed using a SCIEX API5000 or SCIEX Triple Quad 6500 or Triple Quad 6500+ (Sciex, Framingham, MA). PK parameters were calculated by noncompartmental analysis.
Virtual Screening
As a target structure for virtual screening, we retrieved the crystal structure of the SARS-CoV-2 3CLpro in a complex with a noncovalent inhibitor, X77 (PDB code: 6W63),19 from PDB. First, the structure was prepared using Protein Preparation Wizard.28 Missing atoms and side chains were added, and the ionization states of the amino acids were calculated using Epic.29,30 Hydrogen bond networks were optimized, and the energy was minimized with a heavy atom restraint of 0.3 Å. All water molecules were removed from the crystal structure, and the docking grid was set to the center of the bound ligand of X77. An in-house compound library was preprocessed by Ligprep31 before docking. Virtual screening was performed via Glide32,33 in SP mode. The generated docking poses were filtered by the predefined pharmacophores using Phase.34,35 The pharmacophores were set as the acceptor sites with the side-chain NH donor of His163 in the S1 pocket, the lipophilic site in the S2 pocket, and the acceptor site with the Glu166 main-chain NH. Finally, the 300 top-scoring compounds that matched all pharmacophores were selected for enzymatic assays. These procedures were conducted using Schrödinger Drug Discovery Suite 2019-4.
Expression and Purification of SARS-CoV-2 3CLpro Protein
The SARS-CoV-2 3CLpro (1-306) containing an N-terminal 10-histidine tag followed by a thrombin cleavage site and the SARS-CoV-2 3CLpro (1-306) containing a thrombin cleavage site followed by a C-terminal 10-histidine tag were cloned into pET15b vectors. Two 3CLpro constructs were expressed and purified in the same manner as below. E. coli strain BL21 Star (DE3) (Thermo Fisher Scientific) was transformed by the expression plasmid and then precultivated in a LB medium containing 100 μg/mL ampicillin sodium salt. Six milliliters of preculture was inoculated into 600 mL of fresh TB medium supplemented by 100 μg/mL ampicillin sodium salt in a 2-L flask with baffles. After vigorous shaking at 37 °C, 1 mM IPTG was added for the induction when the optical density (OD)600 reached 1.0. After induction for 16 h at 16 °C, the cells were harvested by centrifugation.
Cells expressing SARS-CoV-2 3CLpro were resuspended and sonicated. The clarified lysate was subjected to HisTrap FF 5 mL (Cytiva) equilibrated with 20 mM Tris-HCl (pH 8.0), 300 mM NaCl, 1 mM DTT, and 20 mM imidazole, and the proteins were eluted with a linear concentration gradient of imidazole (20–500 mM). Fractions containing SARS-CoV-2 3CLpro were collected and mixed with thrombin at 4 °C overnight to remove the N- or C-terminus His-tag. Thrombin-treated SARS-CoV-2 3CLpro was applied to HisTrap FF 5 mL (Cytiva) to remove proteins with uncleaved His-tags. The flow-through fraction was applied to a HiLoad 16/60 Superdex 200 prep grade (Cytiva) equilibrated with 20 mM HEPES (pH 7.5), 150 mM NaCl, and 1 mM DTT, and the fraction containing the major peak was collected.
Co-crystallization of SARS-CoV-2 3CLpro with Compounds 1 and 3 (S-217622), Diffraction Data Collection, and Structure Determination
C-terminal His-tag free SARS-CoV-2 3CLpro protein (4.4 mg/mL) was incubated with 500 μM compound 1 for 1 h at room temperature, and the complexes were crystallized by sitting-drop vapor diffusion at 20 °C. The crystal of the compound 1 complex was grown with buffer containing 0.2 M ammonium citrate tribasic, pH 7.0, with 20% (w/v) PEG 3350.
N-terminal His-tag-free SARS-CoV-2 3CLpro protein (4.6 mg/mL) was incubated with 500 μM S-217622 for 1 h at room temperature, and the complexes were crystallized by sitting-drop vapor diffusion at 20 °C. The S-217622 complex crystal was grown with buffer containing 0.1 M Bis-Tris, pH 6.5, with 2.0 M ammonium sulfate.
X-ray diffraction data were collected using a Rigaku HyPix6000C detector mounted on a Rigaku FR-X rotating anode generator. Data were processed by CrysAlis Pro.36 The structures were determined by molecular replacement using MOLREP37 with the SARS-CoV-2 3CLpro-inhibitor complex (PDB code: 6LU7) as a search model.38 Iterative model-building cycles were performed with COOT39 and refined using REFMAC.40 The data collection and structure refinement statistics are summarized in Table S7.
Acknowledgments
We thank all participants and investigator teams in the clinical study. We acknowledge the National Institute of Infectious Diseases (NIID), Dr. Kouichi Morita (Nagasaki University), and Dr. Bart Haagmans (Erasmus University Medical Center) for providing the SARS-CoV-2 strains, SARS-CoV, and MERS-CoV, respectively. We are also grateful to all our colleagues who participated in the COVID-19 antiviral program at Shionogi: Yasushi Hasegawa, Masahiro Masuda, Rina Yasui, Misato Kitamura, Keisuke Mizote, Kotaro Nagatani, Shomitsu Maeno, Tatsuya Tanaka, Azusa Okano, Akinari Sumita, Masayuki Takamatsu, Manabu Kato, Hiroyuki Meichin, Yu Takahashi, Shinya Hisakawa, Yoshihide Sugata, Takao Oyama, Shinichiro Hara, Atsuhiro Iimuro, and Eiichi Kojima, for the compound synthesis; Tetsuya Miyano for the physicochemical studies; Masayoshi Ogawa for structural analysis of the compounds; Akira Kugimiya, Akira Ino, and Kenji Yamawaki for scientific discussion and advice; Takao Shishido, Keita Fukao, Takayuki Kuroda, Masaaki Nakashima, Ryuichi Yano, Yoko Kajiwara, Keiichi Taniguchi, Masaaki Izawa, Shinji Kusakabe, Sachi Takahara, Keiko Baba, and Shigeru Miki for the pharmacological studies; Junji Yamane for X-ray crystallography analysis; Shinpei Yoshida, Yukari Tanaka, Ryoko Oka, and all members of Drug Metabolism & Pharmacokinetics 1&2 group for the DMPK studies; and Yoko Nishimura, Keigo Matsuyama, Sho Hasegawa, Chinami Nekomoto, and Kayoko Kanasaki for the safety studies. We also thank Shionogi Technoadvance Research Co., Ltd. for the compound supplies and technical support in the pharmacological studies. We thank Traci Raley, MS, ELS, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Glossary
Abbreviations Used
- CDI
N,N′-carbonyldiimidazole
- DBU
1,8-diazabicyclo[5.4.0]-7-undecene
- DMA
N,N-dimethylacetamide
- DMEM
Dulbecco’s modified Eagle medium
- DMSO
dimethyl sulfoxide
- DTT
1,4-dithiothreitol
- ESI
electrospray ionization
- EtOAc
ethyl acetate
- HATU
1-[bis(dimethylamino)methylene]-1H-1,2,3-triazolo[4,5-b]pyridinium 3-oxide hexafluorophosphate
- LCMS
liquid chromatography mass spectrometry
- LHMDS
lithium bis(trimethylsilyl)amide
- HRMS
high-resolution mass spectrometry
- MeCN
acetonitrile
- TFA
trifluoroacetic acid
- THF
tetrahydrofuran.
Supporting Information Available
The Supporting Information is available free of charge at https://pubs.acs.org/doi/10.1021/acs.jmedchem.2c00117.
Supporting tables for SAR studies, in vitro antiviral activities, in vitro safety experiments, and crystallography data collection and refinement statistics; synthesis and characterization for compounds 13–21; 1H NMR and 13C NMR spectra of synthetic compounds; HPLC traces of final compounds; experimental procedures for in vitro safety (PDF)
Molecular formula strings (CSV)
PDB coordinates for the docking model of 1 with SARS-CoV-2 3CLpro (PDB)
PDB validation reports for 7VTH (PDF)
PDB validation reports for 7VU6 (PDF)
Accession Codes
The coordinates and structural factors of SARS-CoV-2 3CLpro in a complex with 1 and 3 (S-217622) have been deposited into PDB with accession numbers 7VTH and 7VU6, respectively. Authors will release the atomic coordinates and experimental data upon article publication.
Author Contributions
# Y.U., S.U., and K.N. contributed equally to this work. Conceptualization: T.K., Y.T. Methodology: S.Y., H.N., Y.Y., S.T. Formal analysis: S.U., K.N., H.N.,Y.Y., S.Y., S.K., T.M., T.K., Y.T. Investigation: Y.U., S.U., K.N., H.N., Y.Y., S.Y., Y.M., Y.Taoda, K.K., T.S., K.K., A.N., S.K., T.S., S.T., K.U., S.A., A.S. Resources: M.S., Y.O., H.S. Writing—original draft preparation: Y.U., S.U., K.N., H.N., Y.T. writing—review and editing: Y.U., S.U., K.N., H.N., T.S., M.S., Y.O., H.S., T.S., T.K., Y.T.. Visualization: Y.U., S.U., H.N., Y.M., S.K., Y.T. Project administration: Y.U., S.U., K.N., J.N., Y.Y., S.Y., Y.M., T.M., S.A.,.T.S., T.K., Y.T. Supervision: T.K., Y.T.
The authors declare the following competing financial interest(s): SHIONOGI has applied for a patent covering 1, 2, and 3 (S-217622). Y.U., S.U., K.N., H.N., Y.Y., S.Y., Y.M., Y.T., K.K., T.S., K.K., A.N., S.K., T.S., S.T., K.U., T.M., S.A., A.S., T.S., T.K., and Y.T. are employees of SHIONOGI & Co., Ltd. S.U., K.N., H.N., Y.M., Y.T., K.K., T.S., K.K., S.K., TS, S.T., K.U., T.S., and T.K. are shareholders in SHIONOGI & Co., Ltd. M.S., Y.O., and H.S. are financially supported by the joint research fund from SHIONOGI & Co., Ltd.
Supplementary Material
References
- WHO . Coronavirus (COVID-19) Dashboard. https://covid19.who.int (accessed 2022-03-07).
- WHO . Target Product Profiles for COVID-19 Therapeutics for non-hospitalized patients. https://www.who.int/publications/m/item/who-target-product-profiles-for-covid-19-therapeutics-for-non-hospitalized-patients (accessed 2022-01-12).
- Hu B.; Guo H.; Zhou P.; Shi Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullrich S.; Nitsche C. The SARS-CoV-2 main protease as drug target. Bioorg. Med. Chem. Lett. 2020, 30, 127377. 10.1016/j.bmcl.2020.127377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agbowuro A. A.; Huston W. M.; Gamble A. B.; Tyndall J. D. A. Proteases and protease inhibitors in infectious diseases. Med. Res. Rev. 2018, 38, 1295–1331. 10.1002/med.21475. [DOI] [PubMed] [Google Scholar]
- Qiao J.; Li Y.-S.; Zeng R.; Liu F.-L.; Luo R.-H.; Huang C.; Wang Y.-F.; Zhang J.; Quan B.; Shen C.; Mao X.; Liu X.; Sun W.; Yang W.; Ni X.; Wang K.; Xu L.; Duan Z.-L.; Zou Q.-C.; Zhang H.-L.; Qu W.; Long Y.-H.-P.; Li M.-H.; Yang R.-C.; Liu X.; You J.; Zhou Y.; Yao R.; Li W.-P.; Liu J.-M.; Chen P.; Liu Y.; Lin G.-F.; Yang X.; Zou J.; Li L.; Hu Y.; Lu G.-W.; Li W.-M.; Wei Y.-Q.; Zheng Y.-T.; Lei J.; Yang S. SARS-CoV-2 Mpro inhibitors with antiviral activity in a transgenic mouse model. Science 2021, 371, 1374–1378. 10.1126/science.abf1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dampalla C. S.; Zheng J.; Perera K. D.; Wong L. Y. R.; Meyerholz D. K.; Nguyen H. N.; Kashipathy M. M.; Battaile K. P.; Lovell S.; Kim Y.; Perlman S.; Groutas W. C.; Chang K.-O. Postinfection treatment with a protease inhibitor increases survival of mice with a fatal SARS-CoV-2 infection. Proc. Natl. Acad. Sci. U.S.A. 2021, 118, e2101555118. 10.1073/pnas.2101555118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen D. R.; Allerton C. M. N.; Anderson A. S.; Aschenbrenner L.; Avery M.; Berritt S.; Boras B.; Cardin R. D.; Carlo A.; Coffman K. J.; Dantonio A.; Di L.; Eng H.; Ferre R.; Gajiwala K. S.; Gibson S. A.; Greasley S. E.; Hurst B. L.; Kadar E. P.; Kalgutkar A. S.; Lee J. C.; Lee J.; Liu W.; Mason S. W.; Noell S.; Novak J. J.; Obach R. S.; Ogilvie K.; Patel N. C.; Pettersson M.; Rai D. K.; Reese M. R.; Sammons M. F.; Sathish J. G.; Singh R. P.; Steppan C. M.; Stewart A. E.; Tuttle J. B.; Updyke L.; Verhoest P. R.; Wei L.; Yang Q.; Zhu Y. An oral SARS-CoV-2 Mpro inhibitor clinical candidate for the treatment of COVID-19. Science 2021, 374, 1586–1593. 10.1126/science.abl4784. [DOI] [PubMed] [Google Scholar]
- Pelly S.; Liotta D. Potent SARS-CoV-2 Direct-acting antivirals provide an important complement to COVID-19 vaccines. ACS Cent. Sci. 2021, 7, 396–399. 10.1021/acscentsci.1c00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L.; Lin D.; Sun X.; Curth U.; Drosten C.; Sauerhering L.; Becker S.; Rox K.; Hilgenfeld R. Crystal structure of SARS-CoV-2 main protease provides a basis for design of improved α-ketoamide inhibitors. Science (Washington, DC, U. S.) 2020, 368, 409–412. 10.1126/science.abb3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengist H. M.; Mekonnen D.; Mohammed A.; Shi R.; Jin T. Potency, safety, and pharmacokinetic profiles of potential inhibitors targeting SARS-CoV-2 main protease. Front. Pharmacol. 2021, 11, 630500. 10.3389/fphar.2020.630500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs J.; Grum-Tokars V.; Zhou Y.; Turlington M.; Saldanha S. A.; Chase P.; Eggler A.; Dawson E. S.; Baez-Santos Y. M.; Tomar S.; Mielech A. M.; Baker S. C.; Lindsley C. W.; Hodder P.; Mesecar A.; Stauffer S. R. Discovery, synthesis, and structure-based optimization of a series of N-(tert-butyl)-2-(N-arylamido)-2-(pyridin-3-yl) acetamides (ML188) as potent noncovalent small molecule inhibitors of the severe acute respiratory syndrome coronavirus (SARS-CoV) 3CL protease. J. Med. Chem. 2013, 56, 534–546. 10.1021/jm301580n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turlington M.; Chun A.; Tomar S.; Eggler A.; Grum-Tokars V.; Jacobs J.; Daniels J. S.; Dawson E.; Saldanha A.; Chase P.; Baez-Santos Y. M.; Lindsley C. W.; Hodder P.; Mesecar A. D.; Stauffer S. R. Discovery of N-(benzo[1,2,3]triazol-1-yl)-N-(benzyl)acetamido)phenyl) carboxamides as severe acute respiratory syndrome coronavirus (SARS-CoV) 3CLpro inhibitors: identification of ML300 and noncovalentnanomolar inhibitors with an induced-fit binding. Bioorg. Med. Chem. Lett. 2013, 23, 6172–6177. 10.1016/j.bmcl.2013.08.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han S. H.; Goins C. M.; Arya T.; Shin W. J.; Maw J.; Hooper A.; Sonawane D. P.; Porter M. R.; Bannister B. E.; Crouch R. D.; Lindsey A. A.; Lakatos G.; Martinez S. R.; Alvarado J.; Akers W. S.; Wang N. S.; Jung J. U.; Macdonald J. D.; Stauffer S. R. Structure-based optimization of ML300-derived, noncovalent inhibitors targeting the severe acute respiratory syndrome coronavirus 3CL protease (SARS-CoV-2 3CLpro). J. Med. Chem. 2022, 65, 2880. 10.1021/acs.jmedchem.1c00598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douangamath A.; Fearon D.; Gehrtz P.; Krojer T.; Lukacik P.; Owen C. D.; Resnick E.; Strain-Damerell C.; Aimon A.; Ábrányi-Balogh P.; Brandão-Neto J.; Carbery A.; Davison G.; Dias A.; Downes T. D.; Dunnett L.; Fairhead M.; Firth J. D.; Jones S. P.; Keeley A.; Keserü G. M.; Klein H. F.; Martin M. P.; Noble M. E. M.; O’Brien P.; Powell A.; Reddi R. N.; Skyner R.; Snee M.; Waring M. J.; Wild C.; London N.; von Delft F.; Walsh M. A. Crystallographic and electrophilic fragment screening of the SARS-CoV-2 main protease. Nat. Commun. 2020, 11, 5047. 10.1038/s41467-020-18709-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The COVID Moonshot Consortium . Achdout H.; Aimon A.; Bar-David E.; Barr H.; Ben-Shmuel A.; Bennett J.; Bobby M. L.; Borden B.; Bowman G. R.; Brun J.; BVNBS S.; Calmiano M.; Carbery A.; Cattermole E.; Chernyshenko E.; Chodera J. D.; Clyde A.; Coffland J. E.; Cohen G.; Cole J.; Contini A.; Cox L.; Cvitkovic M.; Dias A.; Donckers K.; Dosten D. L.; Douangamath A.; Duberstein S.; Dudgeon T.; Dunnett L.; Eastman P. K.; Erez N.; Eyermann C. J.; Fairhead M.; Fate G.; Fearon D.; Fedorov O.; Ferla M.; Fernandes R. S.; Ferrins L.; Foster R.; Foster H.; Gabizon R.; Garcia-Sastre A.; Gawriljuk V. O.; Gehrtz P.; Gileadi C.; Giroud C.; Glass W. G.; Glen R.; Glinert I.; Godoy A. S.; Gorichko M.; Gorrie-Stone T.; Griffen E. J.; Hart S. H.; Heer J.; Henry M.; Hill M.; Horrell S.; Hurley M. F. D.; Israely T.; Jajack A.; Jnoff E.; Jochmans D.; John T.; Jonghe S. D.; Kantsadi A. L.; Kenny P. W.; Kiappes J. L.; Koekemoer L.; Kovar B.; Krojer T.; Lee A. A.; Lefker B. A.; Levy H.; London N.; Lukacik P.; Macdonald H. B.; MacLean B.; Malla T. R.; Matviiuk T.; McCorkindale W.; MacGovern B. L.; Melamed S.; Michurin O.; Mikolajek H.; Milne B. F.; Morris A.; Morris G. M.; Morwitzer M. J.; Moustakas D.; Nakamura A. M.; Neto J. B.; Neyts J.; Nguyen L.; Noske G. D.; Oleinikovas V.; Olivia G.; Overheul G. J.; Owen D.; Psenak V.; Pai R.; Pan J.; Paran N.; Perry B.; Pingle M.; Pinjari J.; Politi B.; Powell A.; Puni R.; Rangel V. L.; Reddi R. N.; Reid S. P.; Resnick, Ripika E. G.; Robinson M. C.; Robinson R. P.; Rodriguez-Guerra J.; Rosales R.; Rufa D.; Schofield C.; Shafeev M.; Shaikh A.; Shi J.; Shurrush K.; Singh S.; Sittner A.; Skyner R.; Smalley A.; Smilova M. D.; Solmesky J.; Spencer J.; Strain-Damerell C.; Swamy V.; Tamir H.; Tennant R.; Thompson A.; Thompson W.; Tomasio S.; Tumber A.; Vakonakis I.; van Rij R. P.; Vangeel L.; Varghese F. S.; Vaschetto M.; Vitner E. B.; Voelz V.; Volkamer A.; von Delft A.; von Delft F.; Walsh M.; Ward W.; Weatherall C.; Weiss S.; White K. M.; Wild C. F.; Wittmann M.; Wright N.; Yahalom-Ronen Y.; Zaidmann D.; Zidane H.; Zitzmann N.. Open science discovery of oral non-covalent SARS-CoV-2 main protease inhibitor therapeutics. bioRxiv 2020, 10.29.339317, 10.1101/2020.10.29.339317v2 (accessed 2022-01-21). [DOI] [Google Scholar]
- Peach M. L.; Nicklaus M. C. Combining docking with pharmacophore filtering for improved virtual screening. J. Cheminformatics 2009, 1, 6. 10.1186/1758-2946-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H.; Xie W.; Xue X.; Yang K.; Ma J.; Liang W.; Zhao Q.; Zhou Z.; Pei D.; Ziebuhr J.; Hilgenfeld R.; Yuen K. Y.; Wong L.; Gao G.; Chen S.; Chen Z.; Ma D.; Bartlam M.; Rao Z. Design of wide-spectrum inhibitors targeting coronavirus main proteases. PLoS Biol. 2005, 3, e324. 10.1371/journal.pbio.0030324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mesecar A. D.6W63: Structure of COVID-19 main protease bound to potent broad-spectrum non-covalent inhibitor X77. Deposited 2020-03-16. DOI: 10.2210/pdb6w63/pdb.
- Wang R.; Zhang Q.; Ge J.; Ren W.; Zhang R.; Lan J.; Ju B.; Su B.; Yu F.; Chen P.; Liao H.; Feng Y.; Li X.; Shi X.; Zhang Z.; Zhang F.; Ding Q.; Zhang T.; Wang X.; Zhang L. Analysis of SARS-CoV-2 variant mutations reveals neutralization escape mechanisms and the ability to use ACE2 receptors from additional species. Immunity 2021, 54, 1611. 10.1016/j.immuni.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kai H.; Kameyama T.; Horiguchi T.; Asahi K.; Endoh T.; Fujii Y.; Shintani T.; Nakamura K.; Matsumoto S.; Hasegawa T.; Oohara M.; Tada Y.; Maki T.; Iida A.. Preparation of triazine derivatives and pharmaceutical compound that contains same and exhibits analgesic activity. WO 2012020749 A1, Feb 16, 2012.
- Al-Awar R.; Isaac M.; Chau A. M.; Mamai A.; Watson I.; Poda G.; Subramanian P.; Wilson B.; Uehling D.; Prakesch M.; Joseph B.; Morin J. A.. Preparation of substituted pyrrolopyrimidinylacetamides as inhibitors of the BCL6 BTB domain protein-protein interaction and uses thereof. WO 2019153080 A1, Aug 15, 2019.
- Sasaki M.; Uemura K.; Sato A.; Toba S.; Sanaki T.; Maenaka K.; Hall W. W.; Orba Y.; Sawa H. SARS-CoV-2 variants with mutations at the S1/S2 cleavage site are generated in vitro during propagation in TMPRSS2-deficient cells. PLoS Pathog. 2021, 17, e1009233. 10.1371/journal.ppat.1009233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thai H. T. C.; Le M. Q.; Vuong C. D.; Parida M.; Minekawa H.; Notomi T.; Hasebe F.; Morita K. Development and evaluation of a novel loop-mediated isothermal amplification method for rapid detection of severe acute respiratory syndrome coronavirus. J. Clin. Microbiol. 2004, 42, 1956–1961. 10.1128/JCM.42.5.1956-1961.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raj V. S.; Mou H.; Smits S. L.; Dekkers D. H. W.; Müller M. A.; Dijkman R.; Muth D.; Demmers J. A. A.; Zaki A.; Fouchier R. A. M.; Thiel V.; Drosten C.; Rottier P. J. M.; Osterhaus A. D. M. E.; Bosch B. J.; Haagmans B. L. Dipeptidyl peptidase 4 is a functional receptor for the emerging human coronavirus-EMC. Nature 2013, 495, 251–254. 10.1038/nature12005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauwels R.; Balzarini J.; Baba M.; Snoeck R.; Schols D.; Herdewijn P.; Desmyter J.; De Clercq E. Rapid and automated tetrazolium-based colorimetric assay for the detection of anti-HIV compounds. J. Virol. Methods 1988, 20, 309–321. 10.1016/0166-0934(88)90134-6. [DOI] [PubMed] [Google Scholar]
- Vijgen L.; Keyaerts E.; Moes E.; Maes P.; Duson G.; Van Ranst M. Development of one-step, real-time, quantitative reverse transcriptase PCR assays for absolute quantitation of human coronaviruses OC43 and 229E. J. Clin. Microbiol. 2005, 43, 5452–5456. 10.1128/JCM.43.11.5452-5456.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madhavi Sastry G.; Adzhigirey M.; Day T.; Annabhimoju R.; Sherman W. Protein and ligand preparation: parameters, protocols, and influence on virtual screening enrichments. J. Comput. Aided Mol. Des. 2013, 27, 221–234. 10.1007/s10822-013-9644-8. [DOI] [PubMed] [Google Scholar]
- Greenwood J. R.; Calkins D.; Sullivan A. P.; Shelley J. C. Towards the comprehensive, rapid, and accurate prediction of the favorable tautomeric states of drug-like molecules in aqueous solution. J. Comput. Aided Mol. Des 2010, 24, 591–604. 10.1007/s10822-010-9349-1. [DOI] [PubMed] [Google Scholar]
- Shelley J. C.; Cholleti A.; Frye L.; Greenwood J. R.; Timlin M. R.; Uchimaya M. Epik: a software program for pKa prediction and protonation state generation for drug-like molecules. J. Comput. Aided Mol. Des 2007, 21, 681–691. 10.1007/s10822-007-9133-z. [DOI] [PubMed] [Google Scholar]
- Schrödinger Release 2019–4: LigPrep. Schrödinger, LLC: New York, 2021. [Google Scholar]
- Halgren T. A.; Murphy R. B.; Friesner R. A.; Beard H. S.; Frye L. L.; Pollard W. T.; Banks J. L. Glide: a new approach for rapid, accurate docking and scoring. 2. Enrichment factors in database screening. J. Med. Chem. 2004, 47, 1750–1759. 10.1021/jm030644s. [DOI] [PubMed] [Google Scholar]
- Friesner R. A.; Banks J. L.; Murphy R. B.; Halgren T. A.; Klicic J. J.; Mainz D. T.; Repasky M. P.; Knoll E. H.; Shelley M.; Perry J. K.; Shaw D. E.; Francis P.; Shenkin P. S. Glide: a new approach for rapid, accurate docking and scoring. 1. Method and assessment of docking accuracy. J. Med. Chem. 2004, 47, 1739–1749. 10.1021/jm0306430. [DOI] [PubMed] [Google Scholar]
- Dixon S. L.; Smondyrev A. M.; Knoll E. H.; Rao S. N.; Shaw D. E.; Friesner R. A. PHASE: a new engine for pharmacophore perception, 3D QSAR model development, and 3D database screening. 1. Methodology and preliminary results. J. Comput. Aided Mol. Des. 2006, 20, 647–671. 10.1007/s10822-006-9087-6. [DOI] [PubMed] [Google Scholar]
- Dixon S. L.; Smondyrev A. M.; Rao S. N. PHASE: a novel approach to pharmacophore modeling and 3D database searching. Chem. Biol. Drug Des. 2006, 67, 370–372. 10.1111/j.1747-0285.2006.00384.x. [DOI] [PubMed] [Google Scholar]
- Matsumoto T.; Yamano A.; Sato T.; Ferrara J. D.; White F. J.; Meyer M. ″What is this?″ A structure analysis tool for rapid and automated solution of small molecule structures. J. Chem. Crystallogr. 2021, 51, 438–450. 10.1007/s10870-020-00867-w. [DOI] [Google Scholar]
- Vagin A.; Teplyakov A. MOLREP: an automated program for molecular replacement. J. Appl. Crystallogr. 1997, 30, 1022–1025. 10.1107/S0021889897006766. [DOI] [Google Scholar]
- Jin Z.; Du X.; Xu Y.; Deng Y.; Liu M.; Zhao Y.; Zhang B.; Li X.; Zhang L.; Peng C.; Duan Y.; Yu J.; Wang L.; Yang K.; Liu F.; Jiang R.; Yang X.; You T.; Liu X.; Yang X.; Bai F.; Liu H.; Liu X.; Guddat L. W.; Xu W.; Xiao G.; Qin C.; Shi Z.; Jiang H.; Rao Z.; Yang H. Structure of Mpro from SARS-CoV-2 and discovery of its inhibitors. Nature 2020, 582, 289–293. 10.1038/s41586-020-2223-y. [DOI] [PubMed] [Google Scholar]
- Emsley P.; Lohkamp B.; Scott W. G.; Cowtan K. Features and development of Coot. Acta Crystallogr. 2010, D66, 486–501. 10.1107/S0907444910007493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murshudov G. N.; Vagin A. A.; Dodson E. J. Refinement of macromolecular structures by the maximum-likelihood method. Acta Crystallogr. 1997, D53, 240–255. 10.1107/S0907444996012255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.