Abstract
COVID-19 has affected the health and well-being of almost every American. The aim of this study was to examine the sustained impacts of COVID-19 prevention measures on the diet and exercise habits, risk for food insecurity, and quality of life among adults in the U.S. We conducted a longitudinal study using a convenience sample of participants recruited via Amazon's Mechanical Turk (MTurk) platform between March 30 and April 7, 2020, and 8 months into the outbreak, from November 2 to November 21, 2020. We compared self-reported diet and exercise habits and risk for food insecurity shortly after the pandemic began, in April, to those reported in November. We also measured changes in quality-of-life using the PROMIS-29 + 2 (PROPr) scale. A total of 636 respondents completed both surveys. Compared to reports in April, respondents ate lunch and dinner out more frequently in November and consumed more take-out and fast food. Weekly frequencies of consuming frozen food and the number of daily meals were slightly lower in November than they were in April. 54% of respondents screened positively for being at risk for food insecurity in April, reducing to 41% by November. In April, survey respondents were found to have lower quality-of-life relative to U.S. population norms, but by November levels of depression and cognitive function had improved. Our findings underscore how the initial effects of the pandemic on diet, exercise, risk for food insecurity, and quality of life have evolved. As U.S. states re-open, continued efforts to encourage healthy eating and support mental health, especially to reduce feelings of anxiety and social isolation, remain important to mitigate the potential long-term effects of the pandemic.
Keywords: COVID-19, Coronavirus, Diet, Exercise, Food insecurity, Quality of life
1. Introduction
On January 20, 2020, the first case of the novel coronavirus (COVID-19) was identified in the United States (U.S.) and by March 17, all 50 states reported at least one person with the virus (Feuer, 2020; Harcourt et al., 2020). By the end of March 2020, 30 U.S. states had issued state-wide stay-at-home orders to curb its spread, a number that quickly increased to 42 states by mid-April (Executive Department State of California, 2020; Florida Office of the Governor, 2020; Mervosh et al., 2020). During this time, an AP-NORC poll reported that 94% of respondents were avoiding large gatherings and 86% were avoiding other people as much as possible (AP-NORC, 2020). As the outbreak evolved, and economic and political pressures emerged, local officials began loosening restrictions. By mid-November 2020, nearly all states, except New Mexico and parts of California, no longer had orders to stay at home, relying largely on mask mandates, curfews, and the encouragement of social distancing to keep the outbreak at bay (U.S. Coronavirus Restrictions, 2020; New Mexico Department of Health, 2020; Chokshi, 2020). Nevertheless, COVID-19, and the measures necessary to prevent its spread, dramatically changed the daily lives of those living in the U.S. (Haleem et al., 2020).
COVID-19 prevention measures have affected people's eating and exercise routines, access to healthy food, and overall quality of life. A majority (52%) of respondents to the AP-NORC poll in March reported stocking up on food, much of which was likely processed and calorie-dense, lacking in nutritional quality (AP-NORC, 2020; Buckland et al., 2021; Skerritt et al., 2020). Maintaining exercise regimens amid COVID-19 also poses a challenge, as many states have mandated that community centers and gyms restrict capacity or remain closed. Numerous studies documented unhealthy changes in physical activity and eating behaviors shortly after the pandemic began (Ammar et al., 2020; Cherikh et al., 2020; E. Robinson et al., 2021; Rolland et al., 2020; Scarmozzino & Visioli, 2020; Sidor & Rzymski, 2020). These changes are of particular concern as healthy diet and exercise habits are important to preserve a strong immune system and reduce the risk of developing metabolic disease, both of which are important for the prevention of severe COVID-19 and the promotion of long-term health (Iddir et al., 2020; Martinez-Ferran et al., 2020). However, many of these early studies have relied on retrospectively reported data to determine behaviors before the pandemic, introducing significant recall bias. Longitudinal studies are needed to eliminate the biases that are inherent to such cross-sectional designs.
Furthermore, demand at food banks sky-rocketed at the beginning of the pandemic and continued to grow throughout the year (Kulish, 2020; Luhby, 2020; Reiley, 2020). In November, Feeding America reported that more than 80% of food banks were serving more people than they had one year prior (Morello, 2020). Several studies completed in March and April found a drastic increase in food insecurity in the U.S. compared to before the outbreak, especially among racial and ethnic minorities and low-income households (Lauren et al., 2021; Mayasari et al., 2020; Niles et al., 2020; Wolfson & Leung, 2020). In addition to the rapidly changing food environment, economic hardships and feelings of anxiety, stress, and isolation due to social distancing have negatively influenced mental health and well-being (Brooks et al., 2020; Saladino et al., 2020). These feelings have also been linked to unhealthy eating behaviors (Yau & Potenza, 2013; Groesz et al., 2012; Cummings et al., 2021). While the early impacts of the pandemic on health have been widely documented, little longitudinal data exist on how these lifestyle changes continued to affect Americans as the pandemic and local responses evolved. To this end, we surveyed a convenience sample of adults in the U.S. directly after and 8 months following the outbreak to examine how COVID-19 prevention measures affected the diet and exercise patterns, as well as the risk for food insecurity and overall quality of life, over time among adults in the United States.
2. Methods
2.1. Study design
We performed a longitudinal study of American adults through Amazon's Mechanical Turk (MTurk) platform, an online labor market of over 225,000 U.S. workers who complete online tasks and surveys (J. Robinson et al., 2019). Participants were recruited using convenience sampling. MTurk workers were invited to take part in an online survey, administered using Qualtrics, that included questions regarding demographics and social distancing, as well as items assessing their diet, exercise habits, risk for food insecurity, and quality of life before, 1 month after, and 8 months after the COVID-19 outbreak in the U.S. Workers who completed the first survey in April were recruited again in November to complete the same survey as a follow-up. Participants were compensated with $0.50 for completing the survey each time, which took 10–15 min to complete. All study procedures were approved by Columbia University Irving Medical Center's Institutional Review Board (Protocol AAAS9665). Informed consent was not required because the data were analyzed anonymously. However, we included an information sheet that contains information similar to a consent form prior to beginning the survey. A complete transcript of the information sheet and survey is provided in the Supplementary Files.
2.2. Materials and measures
2.2.1. Demographics
Demographic questions included age, gender, race/ethnicity, income, postal code, relationship status, employment status, and whether participants lived with children under age 18. We also included questions assessing self and community practice of social distancing measures.
2.2.2. Diet and exercise
Questions about meals were derived from the Diet Behavior and Nutrition questionnaire of the National Health and Nutrition Examination Survey (NHANES) (Centers for Disease Control and Prevention (CDC), 2017). These included a 9-item scale about the weekly frequencies of exercising, eating frozen meals, eating fast food or other meals prepared outside the home, drinking soda or sugar-sweetened beverages, and drinking alcohol, as well as a 5-item scale about the daily consumption of different food groups, such as meat, fruit, and vegetables. For each item in the April survey, participants reported their habits before and after the outbreak. In the November survey, participants reported only their current habits.
2.2.3. Risk for food insecurity
We included a validated two-item screen for household risk for food insecurity (Hager et al., 2010). Participants were considered at risk for food insecurity if they responded “Sometimes true” or “Often true” to either or both items. Again, participants reported answers to each of these questions for both before and after the COVID-19 outbreak in April and for their current situations in November. An in-depth report of the predictors of becoming at risk for food insecurity after the outbreak has been published (Lauren et al., 2021).
2.2.4. Quality of life
We used the PROMIS-29 + 2 (PROPr) scale to assess quality of life (Dewitt et al., 2018). This validated questionnaire is used to assess quality of life along 8 domains: physical function, anxiety, depressive symptoms, fatigue, sleep disturbance, ability to participate in social roles and activities, pain interference, and cognitive function. It also includes a single-item measure of pain intensity.
2.3. Analysis
Descriptive statistics were calculated for all baseline subject characteristics. Subsequent analyses were focused on the change in participant responses for reported habits 1 month after the outbreak, in April, and 8 months after, in November. To assess changes in diet and exercise, we conducted paired Wilcoxon sign rank tests comparing patterns in diet and exercise in April to those reported in November. A McNemar test compared the proportion of participants who screened positive for being at risk for food insecurity 1 month and 8 months after the outbreak. Finally, PROPr scores standardized relative to general population values (T-Scores) were calculated using the NIH's HealthMeasures Assessment Center website. We assessed quality of life by comparing PROPr T-Scores at each time point to general population means using one-sample t-tests for all 8 PROPr domains. All tests were performed in Python (Version 3.9.0) and considered p-values less than 0.05 to be statistically significant.
3. Results
We received a total of 1965 responses from across the United States in April, 636 of whom responded to the follow-up survey in November, for an overall response rate of 32%. Those lost to follow-up were younger (aged 18–35) (55%) and more male (49%) than those who completed the study (26% and 43%, respectively), but had similar demographics otherwise. Individual responses across the times points were matched by unique survey codes and Worker IDs. Among the total respondents who answered both surveys, 17 responses were unable to be matched across the timepoints due to missing or incorrect survey codes. The responses of 619 were matched and subsequent analyses were based on this subset of the population.
3.1. Demographics
Demographically, 55% of respondents were female, 43% were male, and <1% were non-binary or other. The majority (68%) were between the ages of 25 and 55 years old and 73% were white. Furthermore, 81% made below $100,000 annually, with 40% earning an income below $50,000. Unemployment was reported by 17% of respondents, 40% of whom were unemployed only after the COVID-19 outbreak. See complete details in Table 1 .
Table 1.
Baseline Characteristics of Survey Participants, n = 619.
| Age, n (%) | |
|---|---|
| 18–24 | 33 (5) |
| 25–34 | 133 (21) |
| 35–44 | 177 (29) |
| 45–54 | 112 (18) |
| 55–64 | 108 (17) |
| 65–74 | 49 (8) |
| 75 or older | 7 (1) |
| No response | 0 (0) |
| Gender, n(%) | |
| Woman | 342 (55) |
| Man | 264 (43) |
| Non-binary or another gender not listed | 3 (<1) |
| No response | 10 (2) |
| Race | |
| White | 450 (73) |
| Asian or Asian-American | 63 (10) |
| Black or African-American | 47 (8) |
| Hispanic or Latino | 24 (4) |
| Biracial or multiracial | 30 (5) |
| American Indian or Alaska Native | 0 (0) |
| Native Hawaiian or Other Pacific Islander | 2 (<1) |
| Another race not listed | 3 (<1) |
| No response | 0 (0) |
| Employment Status, n(%) | |
| Employed full-time | 399 (64) |
| Unemployed | 108 (17) |
| Employed part-time | 103 (17) |
| Student | 7 (1) |
| No response | 2 (<1) |
| Unemployed Before COVID-19, n(%) | |
| Yes | 65 (60) |
| No | 43 (40) |
| No response | 0 (0) |
| Relationship Status | |
| Married or cohabitating | 345 (56) |
| Casually dating or single | 144 (23) |
| Committed relationship | 42 (7) |
| Divorced, separated, or widowed | 84 (14) |
| No response | 4 (<1) |
| Income, n(%) | |
| Less than $20,000 | 68 (11) |
| $20,000 - $49,999 | 177 (29) |
| $50,000 - $99,999 | 251 (41) |
| $100,000 - $149,999 | 78 (13) |
| More than $150,000 | 42 (7) |
| No response | 2 (<1) |
| Region of Residence (United States), n(%) | |
| South | 239 (39) |
| West | 153 (25) |
| Midwest | 115 (19) |
| Northeast | 108 (17) |
| No response | 4 (<1) |
3.2. Social distancing measures
Participants were also asked to self-report the social distancing measures they practice as well as those that they perceive people in their community to practice (Table 2 ). In April, the vast majority of participants reported practicing multiple social distancing measures, while the proportions in November were much lower. These differences were greatest for community practices. 77% of people in April reported that those in their community were traveling only for essential functions versus 17% in November. Around 90% of respondents in April reported that their community's schools were closed and restaurants were take-out only, compared to about 33% in November. While 65% of respondents were under shelter-in-place orders in April, only 13% were by November. In November, only 58% of people reported leaving their home only for essentials, declining from 90% in April. Some measures participants reported practicing themselves varied less between the two time points, including 71% still avoiding bars and restaurants, 77% avoiding rec. venues, and 61% not taking public transportation in November (84%, 81%, and 64%, respectively, in April).
Table 2.
Change in self-reported personal and community-level social distancing measures.
| Social Distancing Measures | April |
November |
|---|---|---|
| No. (%) | No. (%) | |
| Practiced by the Participant's Community (Selected all that applied) | ||
| Schools closed | 554 (90) | 199 (33) |
| Restaurants take-out only | 561 (91) | 210 (34) |
| Rec. venues are closed | 538 (87) | 267 (43) |
| Companies encouraging WFH | 515 (83) | 422 (68) |
| Essential travel only | 478 (77) | 107 (17) |
| Shelter in place | 400 (65) | 79 (13) |
| Public transit disrupted | 268 (43) | 128 (21) |
| Other measures | 24 (4) | 72 (12) |
| Practiced by the Participant (Selected all that applied) | ||
| Leaving home only for essentials | 556 (90) | 356 (58) |
| Avoiding bars and restaurants | 521 (84) | 439 (71) |
| Avoiding rec. venues | 499 (81) | 476 (77) |
| Work or learn from home | 415 (67) | 327 (53) |
| Not taking public transit | 394 (64) | 379 (61) |
| Not sending kids to school | 206 (33) | 99 (16) |
| Other measures | 28 (5) | 42 (7) |
3.3. Diet, exercise, and food insecurity
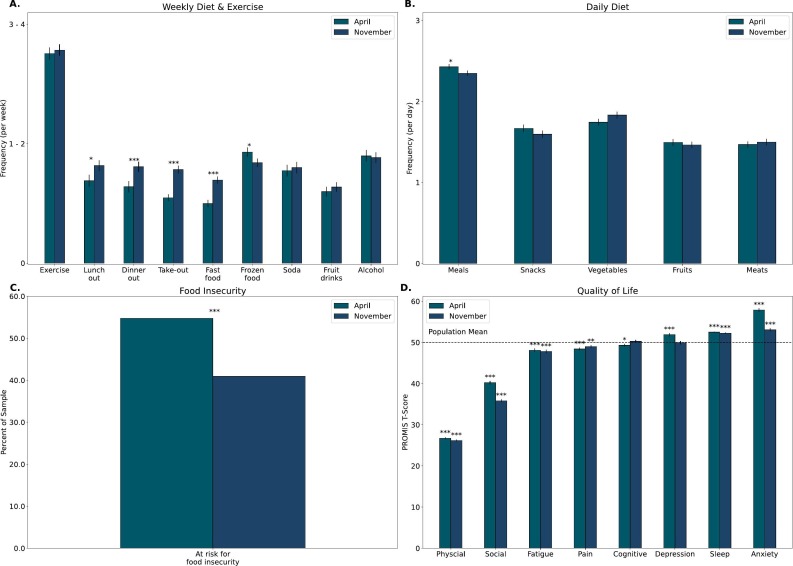
Fig. 1A–C and Table 3 present reported changes in diet, exercise, and risk for food insecurity 1 month after (April) and 8 months after (November) the COVID-19 outbreak in the U.S. Fig. 1A illustrates average weekly dietary and exercise habits. Between the two time points, exercise habits and beverage consumption (soda, fruit drinks, and alcohol) remained similar. By November, there was a significant increase in the number of participants that reported eating lunch and dinner outside of the home (29% and 30%, respectively). Additionally, 27% of respondents reported more often eating take-out and 29% reported more frequently eating fast food in November, while 26% reported a decrease in frequency of frozen food consumption. Fig. 1B illustrates average daily dietary habits during the COVID-19 outbreak. Participants on average reported a statistically significant decline in the number of daily meals consumed from April to November. Lastly, as seen in Fig. 1C, significantly less participants screened positively for being at risk for food insecurity 8 months after the start of the pandemic, declining from 54% in April to 41% in November.
Fig. 1.
Diet, Exercise, Food Insecurity, and Quality-of-Life Results. (A) Average weekly dietary and exercise habits among respondents 1 month after the COVID-19 outbreak (April) and 8 months after (November). (B) Average daily dietary habits among respondents in April and November 2020 (C) Proportion of participants screening positive for being at risk for food insecurity in April and November 2020. (D) Average quality-of-life scores of respondents at time of the two surveys compared to population means. (***p < 0.001; **p < 0.01; *p < 0.05).
Table 3.
Change in diet, exercise, and food security after COVID-19 outbreak, n = 619.
| Variable | Change April to November | No. (%1) | Statistic |
|---|---|---|---|
| Average week | Wilcoxon Sign Rank Test | ||
| Exercise | No change | 291 (47) | Z = 23465 p = 0.603 |
| Decreased | 148 (24) | ||
| Increased | 163 (26) | ||
| No response | 17 (3) | ||
| Eating lunch outside home | No change | 324 (52) | Z = 16600.5 p = 0.016 |
| Decreased | 101 (16) | ||
| Increased | 180 (29) | ||
| No response | 14 (2) | ||
| Eating dinner outside home | No change | 331 (53) | Z = 13941 p < 0.001 |
| Decreased | 86 (14) | ||
| Increased | 184 (30) | ||
| No response | 18 (3) | ||
| Eating take out/delivery | No change | 343 (55) | Z = 9441 p < 0.001 |
| Decreased | 78 (13) | ||
| Increased | 182 (29) | ||
| No response | 16 (3) | ||
| Eating fast food | No change | 367 (59) | Z = 7960.5 p < 0.001 |
| Decreased | 65 (11) | ||
| Increased | 168 (27) | ||
| No Response | 19 (3) | ||
| Eating frozen food | No change | 324 (52) | Z = 16322.5 p = 0.020 |
| Decreased | 162 (26) | ||
| Increased | 115 (19) | ||
| No Response | 18 (3) | ||
| Drinking soda | No change | 390 (63) | Z = 10115 p = 0.434 |
| Decreased | 99 (16) | ||
| Increased | 108 (17) | ||
| No Response | 22 (4) | ||
| Drinking fruit-flavored beverages | No change | 368 (59) | Z = 13402 p = 0.491 |
| Decreased | 111 (18) | ||
| Increased | 126 (20) | ||
| No Response | 14 (2) | ||
| Drinking alcohol | No change | 410 (66) | Z = 9242.5 p = 0.679 |
| Decreased | 95 (15) | ||
| Increased | 100 (16) | ||
| No Response | 14 (2) | ||
| Average day | |||
| Meals | No change | 343 (55) | Z = 15462 p = 0.042 |
| Decreased | 150 (24) | ||
| Increased | 117 (19) | ||
| No Response | 9 (1) | ||
| Snacks | No change | 242 (39) | Z = 24093.5 p = 0.168 |
| Decreased | 176 (28) | ||
| Increased | 148 (24) | ||
| No Response | 53 (9) | ||
| Vegetables | No change | 293 (47) | Z = 21696 p = 0.076 |
| Decreased | 138 (22) | ||
| Increased | 174 (28) | ||
| No Response | 14 (2) | ||
| Fruit | No change | 282 (46) | Z = 25030 p = 0.474 |
| Decreased | 167 (27) | ||
| Increased | 156 (25) | ||
| No Response | 14 (2) | ||
| Meat | No change | 341 (55) | Z = 16862 p = 0.456 |
| Decreased | 121 (20) | ||
| Increased | 145 (23) | ||
| No Response | 12 (2) | ||
| Food insecurity screen | McNemar Exact Test | ||
| Positive in April | 334 (54) | X2 (1, N = 600) = 48 p < 0.001 | |
| Positive in November | 252 (41) |
3.4. Quality of life
Fig. 1D and Table 4 show average participant scores for the 8 dimensions of the PROMIS-29 + 2 (PROPr) quality-of-life scale. In April, participants reported significantly higher than average levels of anxiety, sleep disturbance, and depression. In addition, participants reported significantly lower than average levels of cognitive function, pain interference, fatigue, physical function, and ability to participate in social roles and activities. Respondents reported improved levels of cognitive function and depression by November. Levels of physical function, fatigue, pain interference, and sleep disturbance in November had little to no change from those reported in April and remained significantly worse than population means. Additionally, while anxiety levels reduced slightly between April and November, they remained significantly higher than population means. Respondents also reported even greater reduction in their ability to participate in social roles and activities in November.
Table 4.
Average quality of life (PROPr) scores among participants at time of survey, compared to general population means.
| April | November | |||||
| Quality of life (PROPr) | Average T-Score (SD) | T-Test (Sample vs. Population Mean) | Average T-Score (SD) | T-Test (Sample vs. Population Mean) | ||
| Physical Function | 26.75 (6.37) | t(617) = −90.61 | 26.19 (6.00) | t(618) = −98.64 | ||
| p = 0 | p = 0 | |||||
| Social Role Participation | 40.25 (10.35) | t(619) = −23.43 | 35.82 (8.88) | t(618) = −39.71 | ||
| p < 0.001 | p < 0.001 | |||||
| Fatigue | 48.13 (11.49) | t(618) = −4.06 | 47.82 (11.58) | t(618) = −4.67 | ||
| p < 0.001 | p < 0.001 | |||||
| Pain Interference | 48.43 (9.00) | t(616) = −4.34 | 49.01 (9.16) | t (618) = −2.69 | ||
| p < 0.001 | p = 0.007 | |||||
| Cognitive Function | 49.32 (8.14) | t(617) = −2.08 | 50.30 (8.62) | t(618) = 0.88 | ||
| p = 0.037 | p = 0.381 | |||||
| Depression/Sadness | 51.91 (10.21) | t(617) = 4.66 | 49.96 (10.01) | t(617) = −0.09 | ||
| p < 0.001 | p = 0.927 | |||||
| Sleep Disturbance | 52.50 (3.48) | t (619) = 17.88 | 52.27 (3.88) | t (618) = 14.51 | ||
| p < 0.001 | p < 0.001 | |||||
| Anxiety/Fear | 57.89 (10.44) | t(617) = 18.76 | 53.08 (10.87) | t(618) = 7.02 | ||
| p < 0.001 | p < 0.001 | |||||
4. Discussion
Our findings underscore how the initial consequences of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life have persisted over time. Many of the acute impacts found in April by previous studies have continued long after the initial shock of the outbreak. Other changes, however, have improved since April, likely due to the loosening of local COVID-19 restrictions and people's adaption to a new way of living.
By November, respondents' frequency of exercise had not changed from levels in April. Although resources for at home exercise may have become more widely available as the fitness industry adapted to gym and studio closures, peoples' exercise habits did not evolve (Benveniste, 2020). Frequency of ordering take out, on the other hand, increased since April. The economic pressures of the pandemic on communities spurred many campaigns to support local restaurants through take-out and delivery. Additionally, as we learned more about the virus’ transmission, take-out was identified by the CDC as the food service option with the lowest risk of transmission (Centers for Disease Control and Prevention, 2020). Despite many communities resuming in-person dining by November, the vast majority of respondents still reported avoiding restaurants. This finding suggests that individual-level responses to the pandemic might differ from local guidelines and perceived community practices. Promoting take-out may continue to be an important strategy for restaurants, even as dining restrictions loosen.
Concerning diet-related behaviors have also persisted. Fruit and vegetable consumption remained the same as that at the beginning of the pandemic, which is of concern given the wide documentation of the early negative effects of the pandemic on diet quality (Mattioli et al., 2020; E. Robinson et al., 2021; Scarmozzino & Visioli, 2020; Sidor & Rzymski, 2020). Interestingly, however, one longitudinal study found positive changes in diet after the pandemic, including improved Healthy Eating Index score and less consumption of added sugar (Lamarche et al., 2021). The need for longitudinal studies done in the U.S., like the present one, that don't contain the limitations of retrospective self-reporting are important.
Additionally, while depression and cognitive function improved by November, all other quality of life measures remained significantly worse than population means. The improvement in depression levels is a positive change seen in the cohort, while the persistence of anxiety scores across the time points is of concern. The cohort's high levels of anxiety are consistent with previous studies documenting the effects of COVID-19 restrictions on mental health and well-being (Saladino et al., 2020). Additionally, the decline in the cohort's reported ability to participate in social roles raises concerns for increased isolation despite limitations on social gatherings loosening. These findings reflect the negative influence of stress, anxiety, and isolation on diet-related behaviors and underscore their persistence throughout the pandemic (Cummings et al., 2021; Groesz et al., 2012; Yau & Potenza, 2013).
Food insecurity also remains a significant consequence of the outbreak. Although risk for food insecurity decreased in the study population between April and November, it remained nearly 4 times higher than national levels reported before the pandemic (Coleman-Jensen et al., 2020). The economic fallout of COVID-19 has affected food supply across the country and many food banks have struggled to meet unprecedented demand. Thus, it is not surprising that participants in our sample reported greater concern regarding food availability. The reduction in those at risk by November may point to the early successes of relief efforts, while also indicating that there is still a significant portion of the population in need.
Our study has limitations. Firstly, the use of the two-item screener to identify food insecurity risk rather than the 18-item U.S. Household Food Security Module limited our ability to definitively classify household food insecurity. This may partly explain the differences in food insecurity rates at the beginning of the pandemic in our sample (54%) compared to rates reported in other studies at this time (44%) (Wolfson & Leung, 2020). An additional reason for these differences could be that the final study population was older and included more women, who are likely more vulnerable for becoming food insecure, than those who did not complete the study. For the total sample who completed the survey in April, the food insecurity rate was 41%, which much closely resembles the levels reported in previous analyses (Lauren et al., 2021). Participants’ responses to the screening questions could have also been influenced by the uncertainty of the situation, especially in the early months of the pandemic. Nevertheless, using the screener allowed us to quickly identify those at risk for food insecurity during a rapidly evolving situation.
Additionally, the diet and exercise scales were not based on a validated study and relied on participant recall of weekly and daily activities. The scales were based on frequency rather than amount consumed, making it difficult to compare diets against national nutrition guidelines (U.S. Department of Agriculture, 2020). The items were, however, derived from the NHANES’ widely accepted tool used to explore eating behaviors, which were the focus of this study. Lastly, the convenience sample of MTurk workers limits the generalizability of our results. Previous analyses suggest that relative to the general U.S. population, MTurk workers are less likely to report excellent or very good health (Mortensen et al., 2018). They are also younger, have higher educational attainment, and are disproportionately white (Walters et al., 2018). As a result, our sample included proportionally fewer Black and Hispanic individuals (8% vs 13% and 4% vs 18%, respectively) than the larger U.S. population, two groups that have been disproportionally impacted by the pandemic (U.S. Census Bureau, 2019). Despite these limitations, a recent review supports the use of MTurk as a cost-effective way to quickly gather data from a convenience sample (Mortensen & Hughes, 2018). Given the rapidly evolving situation surrounding COVID-19, we prioritized quick responses from a large sample of the U.S. population. Future work with population-based rather than convenience sampling is necessary to corroborate these findings in a more representative context.
Our study documents how the initial effects of COVID-19 and the measures necessary to prevent its spread have changed since the beginning of the pandemic. Improvements in depression and food insecurity rates since April may point to the early successes of interventions and the rapidly changing landscape of the food environment in the U.S. These findings also demonstrate the resiliency of Americans to adapt to unprecedented circumstances. However, our results suggest that people in the U.S. are still struggling despite loosening COVID-19 restrictions. Efforts to encourage healthy eating and support mental health, especially to reduce feelings of anxiety and social isolation, remain important to mitigate the lasting impacts of the COVID-19 pandemic. As states re-open, the needs of Americans will continue to evolve and future studies documenting these changes will be essential to shaping appropriate responses.
Ethical statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by Columbia University Irving Medical Center's Institutional Review Board (Protocol AAAS9665 approved March 25, 2020). Electronic informed agreement to participate was obtained from all subjects involved in the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Author contributions
Conceptualization, A.M.R., B.N.L., and C.H.; methodology, A.M.R., B.N.L., J.A.W.B., E.M.O., and C.H.; formal analysis, A.M.R. and B.N.L.; investigation, A.M.R.; resources, A.M.R.; data curation, A.M.R.; writing—original draft, A.M.R. and B.N.L.; writing—review and editing, J.A.W.B., E.M.O., and C.H.; visualization, A.M.R. and B.N.L.; supervision, C.H.; project administration, A.M.R. All authors have read and agreed to the published version of the manuscript.
Declaration of competing interest
None.
Acknowledgements
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.appet.2021.105639.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Ammar A., Brach M., Trabelsi K., Chtourou H., Boukhris O., Masmoudi L., Bouaziz B., Bentlage E., How D., Ahmed M., Müller P., Müller N., Aloui A., Hammouda O., Paineiras-Domingos L.L., Braakman-Jansen A., Wrede C., Bastoni S., Pernambuco C.S., on behalf of the ECLB-COVID19 consortium on behalf of the ECLB-COVID19 consortium Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benveniste A. CNN; 2020, April 1. The $94 billion fitness industry is reinventing itself as Covid-19 spreads.https://www.cnn.com/2020/04/01/business/fitness-studios-coronavirus/index.html [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckland N.J., Swinnerton L.F., Ng K., Price M., Wilkinson L.L., Myers A., Dalton M. Susceptibility to increased high energy dense sweet and savoury food intake in response to the COVID-19 lockdown: The role of craving control and acceptance coping strategies. Appetite. 2021;158 doi: 10.1016/j.appet.2020.105017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2020, February 11. Community, work, and school.https://www.cdc.gov/coronavirus/2019-ncov/community/organizations/business-employers/bars-restaurants.html [Google Scholar]
- Centers for Disease Control and Prevention (CDC) U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2017. National health and nutrition examination survey questionnaire.https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/questionnaires.aspx?Cycle=2017-2018 [Google Scholar]
- Cherikh F., Frey S., Bel C., Attanasi G., Alifano M., Iannelli A. Behavioral food addiction during lockdown: Time for awareness, time to prepare the aftermath. Obesity Surgery. 2020;30(9):3585–3587. doi: 10.1007/s11695-020-04649-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chokshi N. The New York Times; 2020, November 11. As U.S. Breaks hospitalization records, N.Y. And other states add restrictions.https://www.nytimes.com/live/2020/11/11/world/covid-19-coronavirus-live-updates [Google Scholar]
- Coleman-Jensen A., Rabbitt M.P., Gregory C.A., Singh A. U.S. Department of Agriculture, Economic Research Service; 2020. Household food Security in the united States in 2019 (ERR-275) [Google Scholar]
- Cummings J.R., Ackerman J.M., Wolfson J.A., Gearhardt A.N. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite. 2021;162:105163. doi: 10.1016/j.appet.2021.105163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewitt B., Feeny D., Fischhoff B., Cella D., Hays R.D., Hess R., Pilkonis P.A., Revicki D.A., Roberts M.S., Tsevat J., Yu L., Hanmer J. Estimation of a preference-based summary score for the patient-reported outcomes measurement information system: The PROMIS ® -preference (PROPr) scoring system. Medical Decision Making. 2018;38(6):683–698. doi: 10.1177/0272989X18776637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Executive Department State of California . 2020, March 19. Executive order N-33-20.https://covid19.ca.gov/img/Executive-Order-N-33-20.pdf [Google Scholar]
- Feuer W. 2020, March 17. Coronavirus has now spread to all 50 states and DC, US death toll passes 100.https://www.cnbc.com/2020/03/17/coronavirus-has-now-spread-to-all-50-states-us-death-toll-passes-100.html CNBC. [Google Scholar]
- Florida Office of the governor . 2020, April 1. Executive Order Number 20-91 (Essential Services And Activities During The Covid-19 Emergency)https://www.flgov.com/wp-content/uploads/orders/2020/EO_20-91.pdf [Google Scholar]
- Groesz L.M., McCoy S., Carl J., Saslow L., Stewart J., Adler N., Laraia B., Epel E. What is eating you? Stress and the drive to eat. Appetite. 2012;58(2):717–721. doi: 10.1016/j.appet.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hager E.R., Quigg A.M., Black M.M., Coleman S.M., Heeren T., Rose-Jacobs R., Cook J.T., Cuba S. A. E. de, Casey P.H., Chilton M., Cutts D.B., Meyers A.F., Frank D.A. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- Haleem A., Javaid M., Vaishya R. Effects of COVID-19 pandemic in daily life. Current Medicine Research and Practice. 2020;10(2) doi: 10.1016/j.cmrp.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harcourt J., Tamin A., Lu X., Kamili S., Sakthivel S.K., Murray J., Queen K., Tao Y., Paden C.R., Zhang J., Li Y., Uehara A., Wang H., Goldsmith C., Bullock H.A., Wang L., Whitaker B., Lynch B., Gautam R., Thornburg N.J. Severe acute respiratory syndrome coronavirus 2 from patient with coronavirus disease. United States. 2020;26(6):1266–1273. doi: 10.3201/eid2606.200516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iddir M., Brito A., Dingeo G., Fernandez Del Campo S.S., Samouda H., La Frano M.R., Bohn T. Strengthening the immune system and reducing inflammation and oxidative stress through diet and nutrition: Considerations during the COVID-19 crisis. Nutrients. 2020;12(6) doi: 10.3390/nu12061562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulish N. ‘Never seen anything like it’: Cars line up for miles at food banks. The New York Times. 2020, April 8 https://www.nytimes.com/2020/04/08/business/economy/coronavirus-food-banks.html [Google Scholar]
- Lamarche B., Brassard D., Lapointe A., Laramée C., Kearney M., Côté M., Bélanger-Gravel A., Desroches S., Lemieux S., Plante C. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: Results from NutriQuébec. American Journal of Clinical Nutrition. 2021;113(4):984–992. doi: 10.1093/ajcn/nqaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauren B.N., Silver E.R., Faye A.S., Rogers A.M., Woo Baidal J.A., Ozanne E.M., Hur C. Predictors of households at risk for food insecurity in the United States during the COVID-19 pandemic. Public Health Nutrition. 2021;1–19 doi: 10.1017/S1368980021000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luhby T. 2020, April 3. Food banks struggle as demand explodes.https://www.cnn.com/2020/03/31/politics/food-banks-supplies-groceries-coronavirus/index.html [Google Scholar]
- Martinez-Ferran M., de la Guía-Galipienso F., Sanchis-Gomar F., Pareja-Galeano H. Metabolic impacts of confinement during the COVID-19 pandemic due to modified diet and physical activity habits. Nutrients. 2020;12(6) doi: 10.3390/nu12061549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattioli A.V., Sciomer S., Cocchi C., Maffei S., Gallina S. Quarantine during COVID-19 outbreak: Changes in diet and physical activity increase the risk of cardiovascular disease. Nutrition, metabolism, and cardiovascular diseases: Nmcd. 2020 doi: 10.1016/j.numecd.2020.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayasari N.R., Ho D.K.N., Lundy D.J., Skalny A.V., Tinkov A.A., Teng I.-C., Wu M.-C., Faradina A., Mohammed A.Z.M., Park J.M., Ngu Y.J., Aliné S., Shofia N.M., Chang J.-S. Impacts of the COVID-19 pandemic on food security and diet-related lifestyle behaviors: An analytical study of google trends-based query volumes. Nutrients. 2020;12(10):3103. doi: 10.3390/nu12103103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh S., Lu D., Swales V. 2020, March. See which states and cities have told residents to stay at home. the new york times.https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html [Google Scholar]
- Morello P. Feeding America; 2020, November 25. The food bank response to COVID, by the numbers.https://www.feedingamerica.org/hunger-blog/food-bank-response-covid-numbers [Google Scholar]
- Mortensen K., Alcalá M.G., French M.T., Hu T. Self-reported health status differs for Amazon's mechanical Turk respondents compared with nationally representative surveys. Medical Care. 2018;56(3):211–215. doi: 10.1097/MLR.0000000000000871. [DOI] [PubMed] [Google Scholar]
- Mortensen K., Hughes T.L. Comparing Amazon's mechanical Turk platform to conventional data collection methods in the health and medical research literature. Journal of General Internal Medicine. 2018;33(4):533–538. doi: 10.1007/s11606-017-4246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Mexico Department of Health . 2020, November 16. Public health order clarifying that current guidance documents, advisories, and emergency public health orders remain in effect; and amending prior public health emeregency orders to provide additional temporary restrictions due to COVID-19.https://cv.nmhealth.org/wp-content/uploads/2020/11/111620-PHO.pdf [Google Scholar]
- Niles M.T., Bertmann F., Belarmino E.H., Wentworth T., Biehl E., Neff R. The early food insecurity impacts of COVID-19. Nutrients. 2020;12(7):2096. doi: 10.3390/nu12072096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NORC A.P.- 2020. Personal impacts of the coronavirus outbreak.https://apnorc.org/projects/personal-impacts-of-the-coronavirus-outbreak/ [Google Scholar]
- Reiley L. 2020, March. Food banks are seeing volunteers disappear and supplies evaporate as coronavirus fears mount.https://www.washingtonpost.com/business/2020/03/16/food-banks-are-seeing-volunteers-disappear-food-supply-evaporate-coronavirus-fears-mount/ Washington Post. [Google Scholar]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., Mead B.R., Noonan R., Hardman C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson J., Rosenzweig C., Moss A.J., Litman L. Tapped out or barely tapped? Recommendations for how to harness the vast and largely unused potential of the mechanical Turk participant pool. PloS One. 2019;14(12) doi: 10.1371/journal.pone.0226394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global changes and factors of increase in caloric/salty food intake, screen use, and substance use during the early COVID-19 containment phase in the general population in France: Survey study. JMIR Public Health and Surveillance. 2020;6(3) doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saladino V., Algeri D., Auriemma V. The psychological and social impact of covid-19: New perspectives of well-being. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.577684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scarmozzino F., Visioli F. Covid-19 and the subsequent lockdown modified dietary habits of almost half the population in an Italian sample. Foods. 2020;9(5) doi: 10.3390/foods9050675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- See Coronavirus Restrictions and Mask Mandates for All 50 States . 2020, April 25. The New York times.https://www.nytimes.com/interactive/2020/us/states-reopen-map-coronavirus.html [Google Scholar]
- Sidor A., Rzymski P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients. 2020;12(6) doi: 10.3390/nu12061657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skerritt J., Mulvany L., Almeida I. Bloomberg.Com; 2020. Americans drop kale and quinoa to lock down with chips and oreos.https://www.bloomberg.com/news/articles/2020-03-21/americans-drop-kale-and-quinoa-to-lock-down-with-chips-and-oreos [Google Scholar]
- U.S. Census Bureau . 2019. Annual estimates of the resident population by sex, race, and hispanic origin.https://www.census.gov/data/tables/time-series/demo/popest/2010s-national-detail.html April 1, 2010 to July 1, 2019. [Google Scholar]
- U.S. Department of Agriculture . 2020, December. Dietary guidelines for Americans; pp. 2020–2025.https://www.dietaryguidelines.gov/ [Google Scholar]
- Walters K., Christakis D.A., Wright D.R. Are Mechanical Turk worker samples representative of health status and health behaviors in the U.S.? PloS One. 2018;13(6) doi: 10.1371/journal.pone.0198835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Leung C.W. Food insecurity and COVID-19: Disparities in early effects for US adults. Nutrients. 2020;12(6):1648. doi: 10.3390/nu12061648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yau Y.H.C., Potenza M.N. Stress and eating behaviors. Minerva Endocrinologica. 2013;38(3):255–267. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.