Abstract
Background and Purpose.
Patient care-seeking has likely changed during the COVID-19 pandemic. In stroke, delayed or avoided care may translate to substantial morbidity. We sought to determine the effect of the pandemic on patterns of stroke patient presentation and quality of care.
Methods.
We analyzed data from 25 New England hospitals: one urban, academic comprehensive stroke center (CSC) and telestroke hub, and 24 spoke hospitals in the telestroke network. We included all telestroke consultations from the 24 spokes, and all stroke admissions to the CSC hub from 11/1/2019 through 4/30/20220. We compared rates of presentation, timeliness presentation, and quality of care pre- vs. post-3/1/2020. We examined trends in patient demographics, stroke severity, timeliness, diagnoses including large vessel occlusion (LVO), alteplase use, and endovascular thrombectomy among eligible subjects. We compared proportions and bivariate comparisons to examine for changes pre- vs. post-3/1/2020, and used linear regression to examine trends over time.
Results.
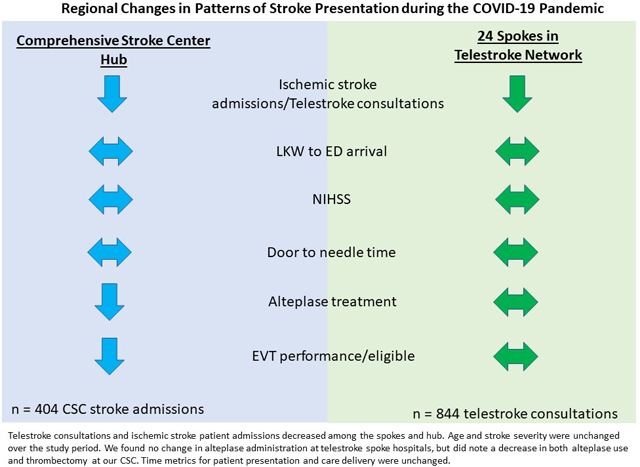
Among 1248 patient presentations (844 telestroke consultations, 404 CSC admissions), telestroke consultations and ischemic stroke patient admissions decreased among the spokes and hub. Age and stroke severity were unchanged over the study period. We found no change in alteplase administration at telestroke spoke hospitals, but did note a decrease in both alteplase use and thrombectomy at our CSC. Time metrics for patient presentation and care delivery were unchanged, however, rates of adherence for the quality measures dysphagia screening, early antithrombotic initiation, and early venous thromboembolism prophylaxis were reduced during the pandemic.
Conclusions.
In this regional analysis, we found decreasing telestroke consultations and ischemic stroke admissions, and reduced performance on stroke quality of care measures during the COVID-19 pandemic. Contrary to prior reports, we did not find an increase in thrombectomy nor decrease in clinical severity that might be expected if patients with milder symptoms avoided hospitalization.
Graphical Abstract
INTRODUCTION
The management of patients with acute ischemic stroke is predicated on the timely delivery of acute stroke care.1 With the current outbreak of coronavirus disease 2019 (COVID-19) and its impact on the medical system, there is significant concern regarding the potential ramifications of this pandemic on acute stroke care.2 Many physicians and healthcare leaders have expressed concern about the potential consequences of delayed care for time-critical diagnoses like stroke and acute myocardial infarction.2–4 Understanding the influence of the COVID-19 pandemic on stroke patient presentation, and systems and quality of care, holds potential to improve stroke care moving forward.
Recent reports from areas afflicted by COVID-19 at earlier stages of the pandemic have suggested a potential impact on both the volume and timeliness of stroke/TIA hospital presentation.5–7 In China, at the early epicenter of the COVID-19 pandemic, an analysis of survey results from greater than 200 national stroke centers observed a 25% decrease in rates of thrombolysis and thrombectomy cases at designated COVID-19 hospitals.5 However, the generalizability of these results internationally is limited as this was a survey-based investigation of a single country where >70% of hospitals reported at least a partial reduction in emergency stroke capacity. Another small, single-site investigation of patients presenting to a stroke center in Hong Kong during COVID-19 showed an approximate 1 hour delay in time from stroke onset to emergency department arrival as well as a reduction in admissions for transient ischemic attack (TIA).6 These findings are also provocative, however, as this was a relatively small study of a single center, the impact of the COVID-19 pandemic on other countries like the United States is less clear.
Regarding the impact of the COVID-19 pandemic on stroke case in the United States, a small study from a New Jersey comprehensive stroke center reported a nearly 40% reduction in new stroke diagnoses but no difference in stroke severity or times of stroke onset to emergency department arrival, or door-to-needle.8 Importantly, this was another relatively small and early investigation of the effect of COVID-19 in a single state at a single institution with no analysis of telestroke quality measures. A small case series of five COVID-19 patients in New York also suggested increased prevalence of stroke in the young secondary to large-vessel occlusion.9 These findings suggest that the COVID-19 outbreak may have impacted stroke patient presentation and systems of care in the United States but warrant further investigation in a larger stroke network.
To better understand the impact of COVID-19 on stroke presentation, systems, and quality of care, we used data from our academic hub-and-spoke telestroke network to examine patterns of telestroke consultations and stroke patient presentations from 25 urban and rural hospitals across New England during the course of the pandemic. We hypothesized that the volume of patients presenting during the pandemic would be decreased, that there would be delays in patient presentation, and that median stroke severity might increase if patients with more severe stroke symptoms would still present early but those with minor symptoms would delay or avoid seeking care. We also hypothesized that door to thrombolysis and thrombectomy might increase due to more onerous infection control protocols, delayed activation of the stroke team, and increased burden of high-acuity patients in emergency departments during the surge. Finally, we assessed the impact of COVID-19-related process changes on acute and inpatient quality of stroke care.
METHODS
Setting and Population
The Partners TeleNeurology Network consists of two academic hub hospitals and 24 urban, suburban, and rural spoke hospitals across 3 New England states that function at a level equivalent to acute stroke ready or primary stroke center hospitals. Spoke hospitals are encouraged to call telestroke consultations for all potential alteplase or thrombectomy cases, or for complex stroke cases requiring comprehensive stroke center (CSC) intervention. Details of the network have been previously described.10 Consultations include phone and video; time metrics and National Institutes of Health Stroke Scale (NIHSS) are recorded for video consultations. Performance of NIHSS by neurologists via telestroke has been shown to have high-fidelity with in-person exam.11 All consultations are documented in a secure online TeleHealth Portal using structured data fields with embedded logic checks. The dataset includes all patients for whom a telestroke was called whether from the emergency department or inpatient setting.
In addition to the telestroke data from patients presenting to the 24 spoke hospitals, we also analyzed data from the main telestroke hub, which supports these spokes. This urban, academic CSC hub hospital uses the Get with the Guidelines – Stroke (GWTG-S) registry as the CSC stroke database and all data were extracted from this source.12 GWTG-S is a national stroke quality improvement registry developed by the American Heart Association and includes information on patients’ demographics, medical history, and hospital treatment characteristics and outcomes for all patients with a diagnosis of stroke. This includes both emergency department and inpatient strokes. Hospital personnel are trained in data abstraction and collect data on consecutively admitted stroke patients.
We used data from the telestroke portal and CSC hospital registry from November 1, 2019 through April 30, 2020. In Massachusetts, March 1st immediately preceded the first reported cases of community transmission,13 and the peak of reported cases occurred on April 29.14 Thus our analysis included 4 months of pre-pandemic and 2 months of intra-pandemic data. The study was approved by the local IRB, and requirement for informed consent was waived. A fully deidentified version of the data that support the findings of this study are available from the corresponding author upon reasonable request.
Clinical Variables
Details of patient age, gender, and stroke severity (NIHSS) were extracted from the TeleHealth Portal. We also collected the details of the acute stroke presentation including last known well (LKW), time of emergency department arrival, consult request, and alteplase treatment. Treatment rates for intravenous alteplase and transfer for endovascular thrombectomy (EVT) consideration were recorded. Final diagnosis after telestroke consultation was recorded by the neurologist performing the teleconsultation, and included acute ischemic stroke (defined as less than 9 hours from LKW), subacute ischemic stroke (greater than 9 hours from LKW), TIA, or “other”.
GWTG-S is a national stroke quality improvement registry developed by the American Heart Association and includes information on patients’ demographics, medical history, and hospital treatment characteristics and outcomes. Hospital personnel are trained in data abstraction and collect data on consecutively admitted stroke patients. Quality measures collected included rates of adherence to evidence-based measures in the acute, subacute, and discharge phases of care as follows: acute (door to CT less than 25 minutes, patients treated with alteplase that arrive within 2 hours and treated with 3 hours or 3.5 hours and treated within 4.5 hours, door to alteplase within 60 minutes of arrival, dysphagia screen prior to oral feeding); subacute (antithrombotics initiated by hospital day 2 and venous thromboembolism prophylaxis initiated by hospital day 2); and by the time of discharge (anticoagulation for stroke patients with atrial fibrillation/flutter, antithrombotics, statin therapy, evaluation for rehabilitation services, smoking cessation counseling, and stroke education).
Statistical Analysis
We performed analyses separately for telestroke consultations and for CSC stroke patient admissions. The telestroke and CSC datasets were cross-analyzed to remove any patient overlap. The telestroke consult documentation includes a data field indicating whether the patient was transferred, and the name of the destination hospital. Among the consults included we identified the number for which transfer to our CSC was indicated as the transfer destination in order to identify potential overlap between the two groups.
We used the TeleHealth Portal to identify all telestroke consultations from November 1, 2019 through April 30, 2020. We excluded consultations with missing age or age less than 18 years, and with unknown consult request time (n=18). All other consultations during this period were included in the analysis and treated as independent observations.
We used our institutional GWTG-S registry to identify all CSC stroke patient admissions from November 1, 2019 through April 30, 2020. We excluded patients with unknown or non-stroke related diagnoses. All stroke and TIA admissions during this period were included in the analysis, however, the registry has incomplete capture of TIA cases that are not admitted (i.e., observation stays or emergency department discharges).
Analyses were performed separately for telestroke consultations and for CSC stroke patient admissions with the observations grouped by week. Comparison of the clinical and quality outcomes of interest pre-versus post-March 1st were performed using chi-square test, Mann-Whitney U test, and Poisson regression as appropriate. Given the small sample size for chi-square testing, we also performed a Monte Carlo version as a robustness check and report significance tests from this version. We used Poisson regression analyses to study stroke incidence over time in all patients and stratified by diagnosis subtype (acute ischemic stroke, transient ischemic attack [TIA], and hemorrhagic stroke). We also examined trends over time in (1) telestroke consultations transferred for thrombectomy, (2) LVO strokes at our CSC, (3) stroke severity by NIHSS score and (4) age.
Next, in response to reports of increased LVO stroke among the young related to COVID, we were interested in examining whether this phenomenon was occurring in our own region. We identified the subgroup of young stroke patients (defined as less than 50 years of age) among telestroke consultations transferred for thrombectomy and CSC stroke admissions with LVO stroke, and used simple descriptive statistics to examine the proportion of patients presenting before versus after March 1, 2020.
This study was approved by the Partners Institutional Review Board.
RESULTS
Overall, 1248 patients were included in our analysis over the six-month study period; 844 telestroke consultations from 24 spoke hospitals and 404 stroke patient admissions to our CSC hospital. There were 125 telestroke consultations with documentation of plan to transfer, and 65 (52%) indicated a plan to transfer to our CSC, reflecting a maximum of 16% (65/404) overlap in cases between the two cohorts. Patient characteristics are outlined in Table 1.
Table 1.
Patient Characteristics
| Telestroke Consultations n = 844 | CSC Stroke Admissions n = 404 | |
|---|---|---|
|
| ||
| Median age (IQR) | 72 (62 – 82) | 70 (58 – 81) |
|
| ||
| Female, n (%) | 440 (52.1%) | 201 (49.8%) |
|
| ||
| Month of presentation, n (%) | ||
| November | 155 (18.4%) | 72 (17.8%) |
| December | 174 (20.6%) | 84 (20.8%) |
| January | 148 (17.5%) | 73 (18.1%) |
| February | 113 (13.4%) | 57 (14.1%) |
| March | 120 (14.2%) | 68 (16.8%) |
| April | 134 (15.9%) | 50 (12.4%) |
|
| ||
| Mode of Arrival, n (%) | ||
| EMS from home/scene | Not collected | 123 (30.4%) |
| Private transport from home/scene | 72 (17.8%) | |
| Transfer from other hospital | 191 (47.3%) | |
| Missing | 18 (4.5%) | |
|
| ||
| Mean NIHSS (SD) | 7.2 (7.2) | 7.2 (8.0) |
| Median NIHSS (IQR) | 5 (1.0 – 12.0) | 4 (1.0 – 11.0) |
| Missing NIHSS, n (%) | 645 (76.4%) | 58 (14.4%) |
|
| ||
| Diagnosis, n (%) | ||
| TIA | 77 (9.1%) | 5 (1.2%) |
| Ischemic stroke | 509 (60.3%) | 322 (79.7%) |
| Hemorrhagic stroke | 15 (1.8%) | 77 (19.1%) |
| Other | 243 (28.8%) | 0 (0%) |
|
| ||
| Alteplase given, n (%) | 85 (10.1%) | 22 (5.4%) |
|
| ||
| Large vessel occlusion suspected, n (%) | Not collected | 84 (20.8%) |
|
| ||
| EVT eligible, n (%) | 84 (20.8%) | Not collected |
|
| ||
| Transfer for EVT, n (%) | 66 (7.8%) | Not applicable |
|
| ||
| EVT performed, n (%) | Not collected | 50 (12.8%) |
|
| ||
| Telestroke consultation disposition, n (%) | ||
| Transfer | 125 (14.8%) | Not applicable |
| Remain at spoke hospital | 678 (80.3%) | |
| Unable to determine | 41 (4.9%) | |
Abbreviations. CSC: Comprehensive Stroke Center; EMS: Emergency Medical Services; EVT: endovascular thrombectomy; IQR: Interquartile Range presented as 25th to 75th percentile; NIHSS: National Institutes of Health Stroke Scale; SD: standard deviation; TIA: transient ischemic attack.
Trends in Telestroke Consultation Volumes from 24 New England Hospitals
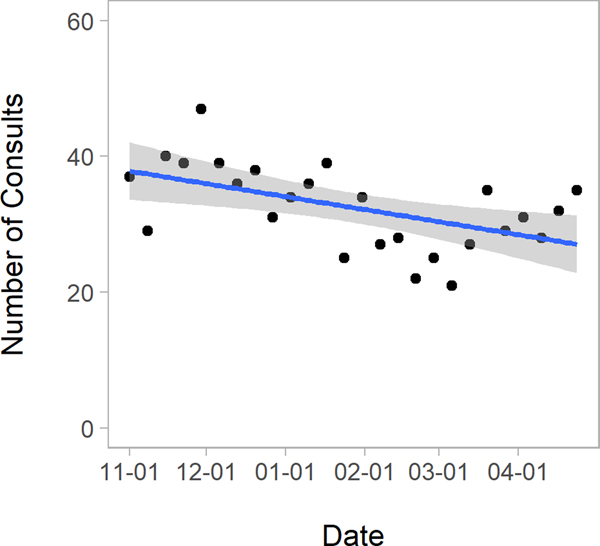
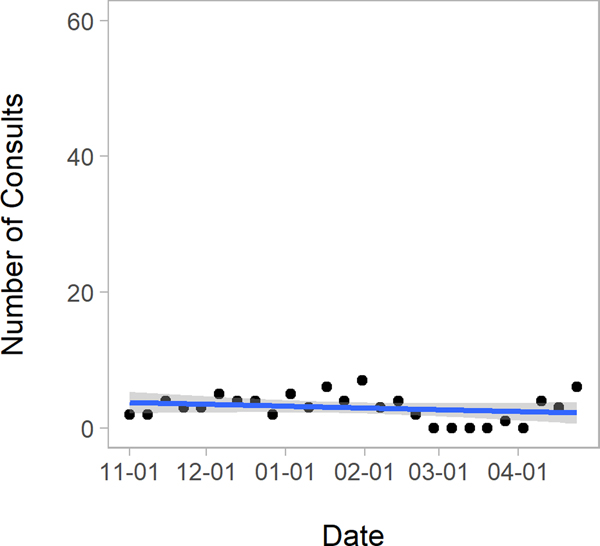
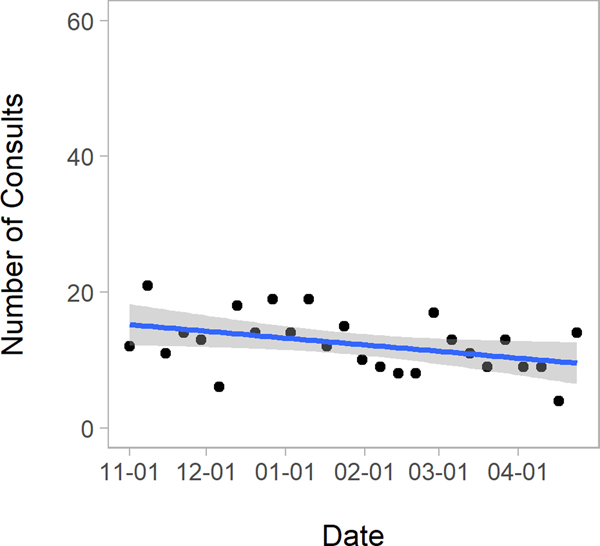
Among acute telestroke consultations, there were decreasing number of consultations per week over the entire study period as illustrated in Figure 1 (1.32% fewer consults per week, p=0.004), but no difference in the mean number of consultations per week pre- vs. post-March 1st (33.7 vs. 29.8 respectively, p=0.11). When examining telestroke consultations with a final diagnosis of ischemic stroke, there was a decrease over the study period (decrease by 1.24% in cases per week, p=0.02, Figure 1), and a decrease in the number of TIA cases per week pre- vs. post-March 1st (3.5 vs. 1.8 respectively, p=0.02, Figure 1) but no difference in the mean number of stroke cases per week pre- vs. post-March 1st (stroke: 23.9 vs. 21.2 respectively, p=0.20). TIA made up a smaller proportion of telestroke consultations after March 1st versus before (10.5% before vs 5.4% after, p=0.02).
Figure 1. Trends in Telestroke Consultations Overall, Consultations with a Stroke Diagnosis, and Consultations with TIA: November 2019 through April 2020.
TIA: Transient Ischemic Attack; Figures present scatterplots in which each data point represents the number of consults performed during a week of the study period. The blue line gives the fitted regression line and the grey area denotes 95% confidence intervals.
Trends in Stroke Admission Volumes from a Large, Urban, Academic CSC
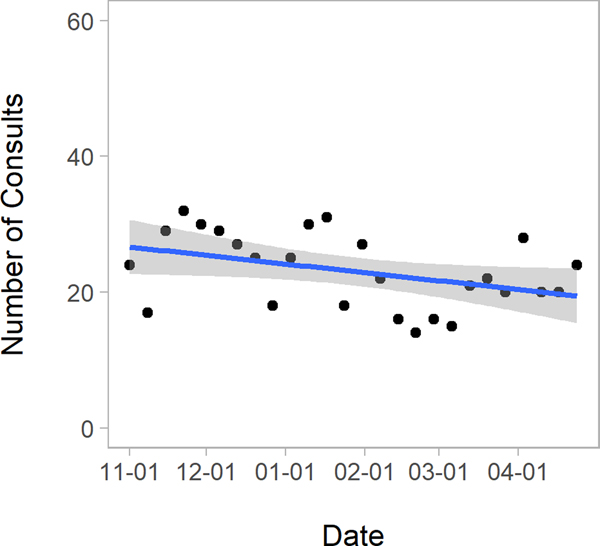
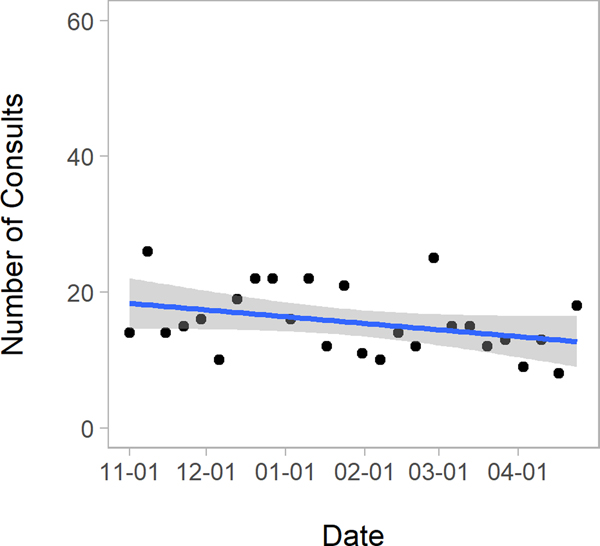
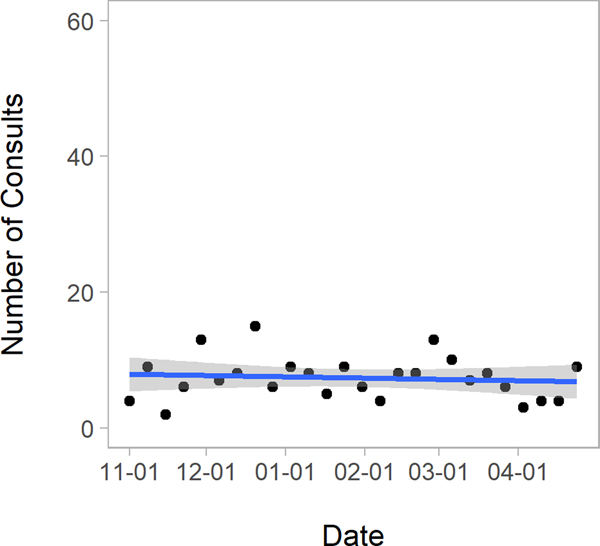
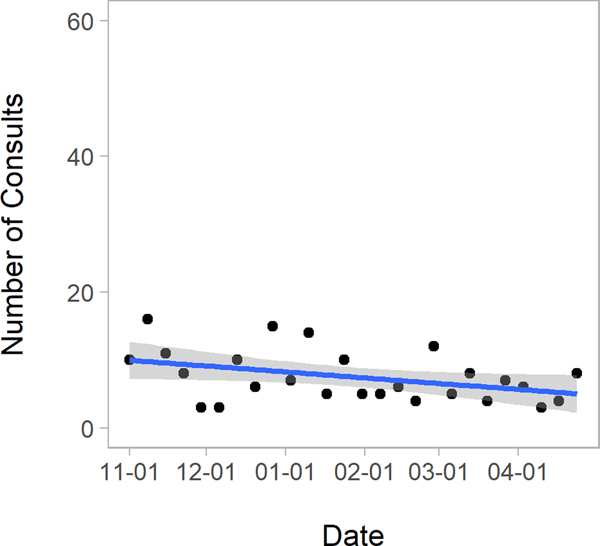
Among all stroke admissions to our CSC, we noted decrease in all stroke admissions and in ischemic stroke admissions from pre- to post-March 1st (all strokes 16.7 vs. 12.9 patients per week, respectively, p=0.02; ischemic strokes 13.3 vs. 10.3 patients per week respectively, p=0.04) (Figure 2). While there was not a significant change in the number of patients received in transfer, we did experience a decrease in the number of patients presenting directly to our institution (mean of 8.3 per week pre- vs. 5.6 per week post-March 1st, p=0.02).
Figure 2. Trends in Comprehensive Stroke Center Patient Admissions: November 2019 – April 2020.
CSC Comprehensive Stroke Center.
Figures present scatterplots of the number of stroke patients during each week of the study period. The blue line gives the fitted regression line and the grey area denotes 95% confidence intervals.
Trends in Alteplase Administration
We found no significant change in the number of patients treated with alteplase among telestroke consultations during the study period (3.2 per week prior to March 1st and 3.4 per week after, p=0.84), or among CSC admissions (0.9 per week prior to March 1st and 0.6 per week after, p=0.42).
Trends in Stroke due to Large Vessel Occlusion
Among telestroke consultations, we found no significant change in the number of cases eligible for endovascular thrombectomy over the study period (trend line non-significant; 2.9 cases per week prior to March 1st and 2.6 cases per week after, p=0.66),
Among our institutional stroke admissions, we found no significant change in the number of patients with large vessel occlusion overall, nor when stratified by transfer versus front-door admission. However, we did note a decrease in the performance of endovascular thrombectomy over the study period (4.26% fewer cases per week, p=0.03). The average number of cases per week prior to March 1st was 2.1 and after March 1st was 1.6 (p=0.47).
Trends in Age and Stroke Severity
Both age and median NIHSS scores for telestroke consultations and among stroke admissions at our CSC were stable over the study period (overall median age = 70 years, median NIHSS = 4; p=ns for changes in both over the period). There were no significant changes over the six-month period (Supplemental Material).
There were 16 patients over the study period who were less than 50 years old with presumed large vessel occlusion. This included 5 telestroke consultations and 11 patients in our own institution. Of the 5 telestroke consultations, none (0%) presented after March 1st, and of the 11 young patients with large vessel occlusion in our CSC, 3 (27.2%) presented after March 1st.
Timeliness of Presentation and Care
Among both telestroke consultations and CSC stroke admissions, we found no difference in time from LKW to presentation or time from symptom discovery to presentation (Table 2). Care at telestroke sites did not significantly change after March 1st, with stable time from arrival to telestroke consultation call, and stable time from arrival to alteplase administration. Likewise, CSC time metrics were stable with respect to time from arrival to alteplase administration and to groin puncture for thrombectomy (Table 2).
Table 2.
Timeliness of Patient Presentation and Stroke Care Delivery Before and During COVID-19 at a Comprehensive Stroke Center and its 24 Telestroke Network Spoke Hospitals
| Nov 1, 2019 – Feb 29, 2020 | March 1 – April 30, 2020 | p-value for comparison | |
|---|---|---|---|
| Median (IQR) time from LKW to ED presentation (min)* Telestroke consultations (n=154) CSC stroke admissions (n=363) |
68.5 (42.0 – 127.0) 686.5 (198.0 – 2095.5) |
65.0 (38.0 – 97.2) 704.0 (226.0 – 1689.5) |
0.44 0.87 |
| Median time (IQR) from symptom discovery to ED presentation (min)* Telestroke consultations (n=153) CSC admissions (n=383) |
51.0 (35.0 – 85.0) 299.0 (110.0 – 936.0) |
55.5 (36.8 – 76.2) 272.0 (138.2 – 795.5) |
0.98 0.99 |
| Median (IQR) time from ED arrival to telestroke consult (min) Telestroke consultations (n=151) |
35.0 (19.8 – 55.8) | 35.0 (23.0 – 52.0) | 0.83 |
| Median (IQR) time from ED arrival to alteplase (min) Telestroke consultations (n=75) CSC admissions (n=22) |
64.5 (49.8 – 81.8) 42.0 (28.0 – 64.0) |
70.0 (59.5 – 104.5) 43.0 (39.0 – 51.0) |
0.25 0.56 |
| Median (IQR) time from CSC ED arrival to groin puncture for thrombectomy (min) CSC admissions (n=48) |
67.5 (21.5 – 107.2) | 64.5 (33.8 – 129.5) | 0.78 |
Abbreviations. CSC: Comprehensive Stroke Center; ED: emergency department; LKW: last known well. IQR: Interquartile Range presented as 25th to 75th percentile.
Among telestroke consultations, median times from LKW and symptom discovery to ED presentation are primarily collected among patients who may be potential candidates for alteplase or thrombectomy. Among CSC patients, these fields are recorded for all stroke and TIA admissions.
Evaluation of the measures of stroke quality care at the CSC, however, demonstrated reduced rates of alteplase administration for patients arriving within 3.5 hours of LKW and treated by 4.5 hours during COVID (Table 3). In addition, rates of compliance with acute interventions beyond alteplase such as dysphagia screening, early antithrombotic initiation, and early venous thromboembolism prophylaxis were reduced during COVID (Table 3). No difference was observed in rates of prescription of a statin or antithrombotic on discharge or anticoagulation for stroke patients with atrial fibrillation or flutter, or evaluation for rehabilitation services. The rate of stroke education was also reduced (Table 3).
Table 3.
Stroke Quality of Care at a CSC Hub
| Variable, % (n) | Nov 1, 2019 – Feb 29, 2020 | March 1 – April 30, 2020 | p-value |
|---|---|---|---|
| Door to CT ≤ 25 minutes | 15.6 (19) | 15 (9) | 1.0 |
| Alteplase: arrive by 2 hours, treat by 3 hours LKW | 100 (10) | 83.3 (5) | 0.38 |
| Alteplase: arrive by 3.5 hours, treat by 4.5 hours LKW | 100 (15) | 55.6 (5) | 0.01 |
| DTN ≤ 60 min | 100 (11) | 100 (4) | 1.0 |
| Dysphagia screen | 94.6 (210) | 66.7 (94) | <0.001 |
| Antithrombotics by end of hospital day 2 | 100 (134) | 70.4 (50) | <0.001 |
| VTE prophylaxis by end of hospital day 2 | 99.6 (242) | 70.9 (90) | <0.001 |
| Anticoagulation for atrial fibrillation/flutter | 100 (39) | 94.7 (18) | 0.33 |
| Antithrombotic at discharge | 100 (178) | 100 (88) | 1.0 |
| Statin on discharge | 100 (142) | 98.5 (66) | 0.33 |
| Evaluated for Rehabilitation Services | 100 (235) | 85.8 (109) | 0.32 |
| Smoking Cessation Counseling | 100 (37) | 100 (20) | 1.0 |
| Stroke Education | 98.3 (114) | 87.0 (60) | 0.002 |
Abbreviations. CT: Computed Tomography; DTN: Door To Needle; LKW: Last Known Well.
DISCUSSION
In this analysis of a large urban and rural telestroke network and large, urban CSC in the Northeastern United States during the COVID-19 pandemic, we found decreasing rates of telestroke consultations and, as others have reported, decreasing ischemic stroke patient admissions.5,6,8 We also observed no delays in patient presentation or in timeliness of in-hospital stroke evaluation and treatment. Lastly, we observed an impact of the COVID pandemic on several measures of stroke quality of care.
While we may have lacked statistical power for a definitive conclusion, we did not find any change in age or in stroke severity among telestroke consultations nor among our institutional stroke patients over time. Our findings stand in contrast to a small case series from Mt. Sinai Hospital in New York, in which Oxley and colleagues described an association between large-vessel stroke and COVID-19 in five young stroke patients.9 We also failed to find any examples of large-vessel occlusion stroke in patients less than 50 years during the height of the pandemic in our region. While we have not experienced the COVID-19 pandemic to the extent of our colleagues in New York, at the time of this submission, the state of Massachusetts was third only to New York and New Jersey for state COVID-19 cases per capita and remained as one of the states with the highest number of COVID-19 cases per capita to date.14,15 Nevertheless, it remains possible that the number of cases in our sample was too low to have detected the association.
Our findings of decreasing proportion of telestroke consultations with TIA during the pandemic are worrisome from a public health perspective and warrant further investigation. Stroke after TIA is of high likelihood, especially in the short-term period, which is why urgent medical evaluation is recommended.1,16,17 The results from our large, regional telestroke network are in agreement with those reported from a single Hong Kong stroke center, which also observed overall delays in stroke care during COVID-19.6 These findings suggest that during the COVID-19 outbreak patients with TIAs and minor strokes may have deferred seeking medical attention in contrast to those patients with more severe stroke syndromes. In support of this hypothesis, analysis of patient mode of presentation from a New Jersey CSC observed reduced rates of private vehicle/walk-in as the arrival mode.8 Furthermore, the Chinese national survey results observed high rates of response for delays in stroke care due to patients and families fear of presenting to the hospital during the pandemic.5 In contrast, a study of ambulance calls for stroke and acute myocardial infarction in the United Kingdom observed no change during COVID suggesting decreased likelihood of delay for more severe strokes.18 Along these lines, the results of the French national registry analysis of LVO patients that underwent EVT showed no difference in time from symptom onset to imaging during the pandemic.7 Assimilating the results of these multinational studies supports the hypothesis that the COVID-19 pandemic contributed to decreased rates of presentation for non-disabling strokes or TIAs. For these reasons, a continued emphasis on public health campaigns for stroke and TIA awareness is necessary.
Reassuringly, this large-scale analysis of telestroke consultations and CSC stroke admissions demonstrates that stroke severity and the timeliness of delivery of stroke care were similar during COVID-19. In the aforementioned French study of patients that underwent EVT, the observed 21% reduction in EVT rates during the pandemic was probably influenced, at least in part, by the observed increase in time from imaging to groin puncture during the pandemic, especially in those individuals requiring transfer (mean difference +29 minutes).7 In the United States, a small study from a New Jersey CSC also reported no difference in stroke severity or times of LKW to emergency department arrival, or door-to-needle.8 We did observe, however, that several measures of stroke quality of care were affected during the COVID pandemic with reduced rates of dysphagia screening, early antithrombotic initiation and venous thromboembolism prophylaxis, and stroke education. Our institutional response to the COVID-19 pandemic was to convert our designated stroke unit to an intensive care unit for patients with COVID, resulting in stroke patients being distributed throughout the hospital. As a result, these observations likely reflect this restructuring of stroke patient flow to hospital units not previously designated as stroke units and underscore the importance of stroke unit care for stroke patients. These findings suggest that the United States made great strides to adequately prepare its stroke systems of care for the impending COVID-19 outbreak but continued efforts on delivery of high-quality care are necessary.
Our findings are limited as this was a retrospective analysis of 25 hospitals in the Northeast United States that have worked closely together in a telestroke network relationship for many years and may not be generalizable to other settings. We do not have additional details on patient demographics, radiographic features, stroke subtypes, and total ischemic stroke admission volumes for our telestroke spoke hospitals, nor do we know basic information about patients presenting to the spoke hospitals for which telestroke consultations were not requested. These gaps preclude a population level estimate of stroke admissions or changes in presentation. However, it is our experience that spoke hospitals routinely use the platform for the vast majority of acutely presenting patients with suspected stroke. In addition, we do not have reason to believe that this would have changed in response to the pandemic, as most of our spokes have no alternative stroke consultants. Similarly, the nature of these data also do not enable us to definitively distinguish between secular trends and pandemic-related influences on referral patterns and patient behaviors. However, we suspect these potential factors did not contribute significantly as our telestroke volumes have previously increased annually10 and we did not observe a significant reduction in our CSC transfer volume. Additionally, the observed trend prior to February did not suggest a decrease; it is possible that there were changes in patient and physician behavior that preceded March 1st (the date when Massachusetts had its first reported case of community transmission). In addition, our discussion of stroke care quality metrics was limited to a single CSC and may not be generalizable to other settings. Nevertheless, as one of the first reports to include an evaluation of changes in stroke care delivery at a large-volume CSC during the pandemic, we believe these data serve as a useful starting point for recognizing the impact of this pandemic on stroke care quality measures. Finally, we may not have had adequate power to identify significant changes in trends over time, however this analysis of 1248 patients from 25 hospitals is one of the larger regional analyses of this topic to date and adds substantial information to our current understanding of trends in stroke care in relation to the pandemic.
Conclusion
In this analysis of stroke patient presentations to 25 New England hospitals, we found decreasing frequency of patient presentation in relation to the pandemic. We did not replicate the previously reported findings of increased presentation of young patients with large vessel occlusion stroke, nor did we identify increased stroke severity or delays in presentation that would be expected if patients with mild strokes avoided or delayed presenting acutely to the hospital. We also found that timeliness of stroke care delivery was stable but that several measures of stroke quality of care were reduced during the pandemic. These findings suggest that the reorganization efforts of stroke systems of care in preparation for the COVID-19 surge were successful in mitigating the potential impact on delays in acute stroke treatment but that continued emphasis on optimizing stroke quality care is essential. For the purposes of population awareness and recognition of stroke and TIA symptoms, a continued national emphasis will be important for stroke prevention and public health.
Supplementary Material
Acknowledgements
We thank Ms. Joyce McIntyre and Ms. Kiera Macdonald for their assistance in providing data from our GWTG-S database and Telestroke portals.
Funding: Agency for Healthcare Research and Quality (Zachrison, K08 HS024561)
Disclosures
KSZ reports grants from NIH-NINDS, CRICO, and the American College of Emergency Physicians, as well as personal fees from Portola Pharmaceuticals outside of the submitted work. MB received unrelated funding from the Société Française de Neuroradiologie, Société Française de Radiologie and Fondation ISITE-ULNE. AV reports grants from NIH, personal fees from Alynylam Pharmaceuticals, and personal fees from Biogen outside the submitted work. ABS reports grants from NIH-NINDS during the conduct of the study; other from UpToDate (Wolters Kluwer Health, Inc.), other from Medlink, Inc, personal fees from Omniox. Inc, personal fees from Deck Therapeutics, Inc, personal fees from Biogen, other from American Academy of Neurology, and personal fees from Expert Testimony outside the submitted work. LHS reports the following relationships relevant to research grants or companies that manufacture products for telemedicine, thrombolysis or thrombectomy: scientific consultant regarding trial design and conduct on late window thrombolysis and member of steering committee for Genentech (TIMELESS NCT03785678); user interface design and usability to LifeImage (privately held teleradiology company); stroke systems of care to the Massachusetts Dept of Public Health; member of a Data Safety Monitoring Board (DSMB) for Penumbra (MIND NCT03342664); Diffusion Pharma PHAST-TSC NCT03763929); PI, multicenter trial of stroke prevention for Medtronic (Stroke AF NCT02700945); PI, late window thrombolysis trial, NINDS (P50NS051343, MR WITNESS NCT01282242); PI, StrokeNet Network NINDS (New England Regional Coordinating Center U24NS107243, CURENT); Co-I, The Impact of Telestroke on Patterns of Care and Long-Term Outcomes, NINDS (R01NS111952); Co-I, REACH-PC tele-palliative care trial, PCORI (NCT03375489)
Non-standard Abbreviations and Acronyms
- COVID-19
coronavirus disease 2019
- TIA
transient ischemic attack
- CSC
comprehensive stroke center
- NIHSS
National Institutes of Health Stroke Scale
- GWTG-S
Get with the Guidelines – Stroke
- LKW
last known well
- EVT
endovascular thrombectomy
- CT
computed tomography
- LVO
large vessel occlusion
- EMS
emergency medical services
- IQR
interquartile range
- SD
standard deviation
- ED
emergency department
Footnotes
MRE, ZY, LS, and JE have no conflicts of interest to disclose.
REFERENCES
- 1.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50:E344–E418. [DOI] [PubMed] [Google Scholar]
- 2.Lyden P, AHA/ASA Stroke Council Leadership. Temporary Emergency Guidance to US Stroke Centers During the COVID-19 Pandemic. Stroke. 2020;epub ahead. [DOI] [PubMed] [Google Scholar]
- 3.Mahmud E, Dauerman HL, Welt FG, Messenger JC, Rao SV., Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, et al. Management of Acute Myocardial Infarction During the COVID-19 Pandemic. J. Am. Coll. Cardiol. [Internet]. 2020. [cited 2020 Apr 30]; Available from: https://linkinghub.elsevier.com/retrieve/pii/S0735109720350269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsieh P. Do Not Delay Urgent Medical Care Due To The COVID-19 Coronavirus Pandemic [Internet]. Forbes. 2020. [cited 2020 Apr 30]; Available from: https://www.forbes.com/sites/paulhsieh/2020/04/20/do-not-delay-urgent-medical-care-due-to-the-covid-19-coronavirus-pandemic/#2e9c34a763ea [Google Scholar]
- 5.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 Epidemic on Stroke Care and Potential Solutions. Stroke [Internet]. 2020. [cited 2020 May 21]; STROKEAHA120030225. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32432997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teo K-C, Leung WCY, Wong Y-K, Liu RKC, Chan AHY, Choi OMY, Kwok W-M, Leung K-K, Tse M-Y, Cheung RTF, et al. Delays in Stroke Onset to Hospital Arrival Time During COVID-19. Stroke [Internet]. 2020. [cited 2020 May 21]; STROKEAHA120030105. Available from: http://www.ncbi.nlm.nih.gov/pubmed/32432998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kerleroux B, Fabacher T, Bricout N, Moïse M, Testud B, Vingadassalom S, Ifergan H, Janot K, Consoli A, Ben Hassen W, et al. Mechanical Thrombectomy for Acute Ischemic Stroke Amid the COVID-19 Outbreak. Stroke [Internet]. 2020. [cited 2020 May 21]; Available from: 10.1161/STROKEAHA.120.030373 [DOI] [PubMed] [Google Scholar]
- 8.Siegler JE, Heslin ME, Thau L, Smith A, Jovin TG. Falling stroke rates during COVID-19 pandemic at a Comprehensive Stroke Center: Cover title: Falling stroke rates during COVID-19. J. Stroke Cerebrovasc. Dis. 2020;104953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oxley TJ, Mocco J, Majidi S, Kellner CP, Shoirah H, Singh IP, De Leacy RA, Shigematsu T, Ladner TR, Yaeger KA, et al. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N. Engl. J. Med. [Internet]. 2020. [cited 2020 May 12]; e60. Available from: 10.1056/NEJMc2009787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma R, Zachrison KS, Viswanathan A, Matiello M, Estrada J, Anderson CD, Etherton M, Silverman S, Rost NS, Feske SK, et al. Trends in Telestroke Care Delivery: A 15-Year Experience of an Academic Hub and Its Network of Spokes. Circ. Cardiovasc. Qual. Outcomes [Internet]. 2020. [cited 2020 Apr 30]; 13:e005903. Available from: 10.1161/CIRCOUTCOMES.119.005903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang S, Lee SB, Pardue C, Ramsingh D, Waller J, Gross H, Nichols FT, Hess DC, Adams RJ. Remote Evaluation of Acute Ischemic Stroke. Stroke. 2003;34:e188–91. [DOI] [PubMed] [Google Scholar]
- 12.Zachrison KS, Leslie-Mazwi TM, Boulouis G, Goldstein JN, Regenhardt RW, Viswanathan A, Lauer A, Siddiqui KA, Charidimou A, Rost N, et al. Frequency of early rapid improvement in stroke severity during interfacility transfer. Neurol. Clin. Pract. 2019;9:373–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mapping COVID-19 - Dartmouth Atlas of Health Care [Internet]. [cited 2020 May 21]; Available from: https://www.dartmouthatlas.org/covid-19/hrr-mapping/
- 14.CDC COVID Data Tracker [Internet]. [cited 2020 Jul 13]; Available from: https://www.cdc.gov/covid-data-tracker/#cases
- 15.State Data and Policy Actions to Address Coronavirus | The Henry J. Kaiser Family Foundation [Internet]. [cited 2020 May 12]; Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/state-data-and-policy-actions-to-address-coronavirus/
- 16.Hill MD, Yiannakoulias N, Jeerakathil T, Tu JV., Svenson LW, Schopflocher DP. The high risk of stroke immediately after transient ischemic attack: A population-based study. Neurology. 2004;62:2015–2020. [DOI] [PubMed] [Google Scholar]
- 17.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. J. Am. Med. Assoc. 2000;284:2901–2906. [DOI] [PubMed] [Google Scholar]
- 18.Holmes JL, Brake S, Docherty M, Lilford R, Watson S. Emergency ambulance services for heart attack and stroke during UK’s COVID-19 lockdown. Lancet. 2020;395:e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.