Abstract
The burden of temperature-associated mortality and hospital visits is significant, but temperature’s effects on non-emergency health outcomes is less clear. This burden is potentially greater in low-income households unable to afford efficient heating and cooling. We examined short-term associations between indoor temperatures and cognitive function and daytime sleepiness in low-income residents of Detroit, Michigan. Apparent temperature (AT, based on temperature and humidity) was recorded hourly in 34 participant homes between July 2019-March 2020. Between July-October 2019, 18 participants were administered word list immediate (WLL) and delayed (WLD) recall tests (10-point scales) and the Epworth Sleepiness Scale (24-point scale) 2–4 times. We applied longitudinal models with nonlinear distributed lags of temperature up to 7 days prior to testing. Indoor temperatures ranged 8–34° C overall and 15–34 C on survey days. We observed a 0.4 (95% CI: 0.0, 0.7) point increase in WLL and 0.4 (95% CI: 0.0, 0.9) point increase in WLD scores per 2 C increase in AT. Results suggested decreasing sleepiness scores with decreasing nighttime AT below 22 C. Low-income Detroit residents experience uncomfortably high and low indoor temperatures. Indoor temperature may influence cognitive function and sleepiness, although we did not observe deleterious effects of higher temperatures.
Keywords: climate change, weather, indoor temperature, socioeconomic, cognition, sleepiness
INTRODUCTION
Due to climate change, extreme weather events are increasing, and extreme heat days are expected to warm by 3 C in the mid-latitudes by mid-century (Intergovernmental Panel on Climate Change (IPCC) 2018). The impacts of extreme weather events, e.g., temperatures or precipitation amounts that were observed less than 1% of the time in a historical period, such as 1981–2010 (Field et al. 2012), disproportionately fall on vulnerable communities. These vulnerable communities include persons of color, who are more likely to live in lower quality homes and neighborhoods with fewer resources due to racially discriminatory mortgage lending practices, and individuals with low incomes, who often lack extreme temperature mitigation methods or may limit energy usage to minimize utility costs (Jessel et al. 2019). Of U.S. cities, Detroit, Michigan may be particularly vulnerable. This city of 670,000 people (American Community Survey (ACS) 2021) lies in the Koppen climate classification group ”hot summer continental climate.” (Peel et al. 2007). In the 1981–2010 climatological period, 8.9 days per year had maximum temperatures exceeding 32 C, 114.5 days per year had minimum temperatures below 0 C (Great Lakes Integrated Sciences and Assessments (GLISA) 2017), and the relative humidity level was 69% (Climate-Data.org). In the Detroit region, 7.4% of deaths annually are attributed to ambient hot or cold temperatures (Gasparrini et al. 2015). According to the 2019 American Community Survey, 79% of Detroit’s residents identify as Black or African American, 8% identify as Hispanic or Latino, and 31% live below the poverty level (ACS 2021). Furthermore, in the 2019 American Housing Survey, 15% of Detroit households reported uncomfortably cold home temperatures for 24 hours or longer for reasons such as equipment breakdowns, utility interruptions, and inadequate insulation (U.S. Census Bureau 2020). Utility disconnections for non-payment are of particular concern for uncomfortable or unsafe indoor air temperatures. DTE Energy, which provides both natural gas and electricity service to Detroit residents, performed over 70,000 disconnections between September 2020 and September 2021 amidst ongoing pandemic conditions (Michigan Public Service Commission, 2021). In an analysis of energy inefficiency in Detroit, energy inefficiency correlated with the percentage of African American or Latino households in a census tract, likely due to inadequate weatherization of the homes in these neighborhoods (Bednar et al. 2017). To inform policies related to healthcare subsidies, housing subsidies, and environmental and energy justice, it is particularly important to understand the health impacts of indoor temperatures among those more likely to have inadequate housing and therefore exposure to a wide range of indoor temperatures.
Both hot and cold temperatures have been shown to increase emergency health events, and these associations have been used to estimate annual attributable mortality, hospitalizations, emergency department visits, and health costs (Gasparrini et al. 2015; Gronlund et al. 2019; Liu et al. 2019). However, associations between non-emergency events and temperature, particularly in community settings, are less well characterized. With respect to one such non-emergency health event, short-term cognitive function change, there is compelling evidence from a wide range of disciplines (education, psychology, health and medicine, ergonomics, building science, neuroscience, and gerontology) that cognitive function is impacted by temperature extremes in laboratory conditions, schools, and the workplace (Pilcher et al. 2002; Taylor et al. 2016; Xiong et al. 2018; Zhang et al. 2019). For example, in classroom settings, higher temperatures negatively affected students’ learning, performance on standardized tests, focus, attention, and task completion (Goodman et al. 2018; Barbic et al. 2019). Considering residential settings, a study of older men in Boston found inverse associations between indoor temperature and cognitive function (Dai et al. 2016). Among young adults in non-air conditioned buildings, cognitive function was reduced during a heat wave (Laurent et al. 2018). However, among older adults or in low-socioeconomic households, these associations are not well characterized.
The effects of the sleep environment have received much attention to better understand the factors contributing to restful sleep and daytime sleepiness, although findings have been mixed with regard to optimal sleeping temperatures (Lan et al. 2017). Furthermore, few studies have examined sleep-temperature associations in community-based samples, where individuals might have more control over indoor temperature via a thermostat or may be exposed to wider temperature ranges given that older or unemployed individuals in the community are less likely to be in school or workplace environments during the day. Among Hong Kong students sleeping in dormitory rooms, Zhang et al. (2018) found a slight U-shaped association between reported sleeping thermal environment satisfaction and room temperature, with optimal satisfaction at 24.2 °C. Another study found sleep to be more disrupted among low-income residents in Boston as summer temperatures increased (Williams et al. 2019). Furthermore, cognition is directly impacted by sleep quality (McCoy & Strecker 2011, Scullin et al. 2015), and may therefore be impacted both directly and indirectly by indoor temperature. These findings as a whole suggest associations between indoor temperature and the specific health outcomes of cognitive function and sleep. However, community-based research on indoor temperature as well as its association with both outcomes is sparse.
In the current study, we characterized indoor temperature exposures in 34 low-income Detroit residences between July 2019-March 2020. For 18 of the participants, we then estimated associations of indoor temperatures with cognitive function and daytime sleepiness, and we characterized the time course (how long the exposure effects last) of temperature-associated cognition and sleepiness. We administered a phone survey on 2–4 occasions and measured indoor temperatures in the hours and nights prior to the survey. We hypothesized that cognitive processes—specifically working memory and auditory attention-- and sleepiness would increase with increasing temperatures above 22 C, decreasing temperatures below 22 C, and increasing temperature variability. We hypothesized that temperature exposures immediately prior to the survey or in the night prior to the survey would have stronger effects than temperatures occurring 24 hours or more earlier.
METHODS
Recruitment
The Detroit Communities Reducing Energy and Water (D-CREW) is a community-based participatory research project to examine the feasibility of an integrated, neighborhood-based, case-management approach to increasing household access to existing residential energy and water assistance programs to inform broader city-wide programs and planning. The cognition and temperature study was part of the larger study seeking to understand the potential health benefits of an energy efficiency program by reducing the barriers to assistance program utilization for low-income Detroit residents. Participants, adults with low-to-moderate household incomes residing in Detroit, were recruited using community flyers in an East Detroit public housing complex and Lower East Side neighborhood and consented in person. Of the 41 consented and enrolled participants, 18 consented to this optional cognition and temperature sub-study and responded to at least 2 phone surveys. Seven of the 41 participants completed only one phone survey. We excluded these 7 participants from the cognition and sleepiness analyses so that we could focus our analysis on within-participant associations between temperature and cognition and sleepiness and control for individual non-time-varying characteristics by design (see Statistical Analysis below). In an initial face-to-face survey of all participants, demographic and housing information were collected.
Cognitive and Sleepiness Phone Surveys
Participants were called between July and November 2019, between 11:00 and 18:00, and phone calls lasted approximately ten minutes. The assessments included three previously validated measures of daytime sleepiness and cognition. These tests were chosen for their speed and ease of administration by phone.
The Epworth Sleepiness Scale (Johns 1994) was used to measure sleepiness. Participants were asked to rate (scale of 0–3) how likely they were to doze or fall asleep given the following situations: sitting and reading, watching television, sitting inactive in a public place (e.g a theater or a meeting), as a passenger in a car for an hour without a break, lying down to rest in the afternoon when circumstances permit, sitting and talking to someone, sitting quietly after a lunch without alcohol, and in a car stopped for a few moments in traffic. The sum of the 8-item scale can range from 0 to 24, with higher scores indicating more sleepiness.
The immediate, single trial word list learning (WLL) and the five-minute delay word list delayed (WLD) tests of nonassociated verbal material from the Health and Retirement Study (HRS) were used to measure cognition (Ofstedal et al 2005). These cognitive tests are associated with frontally-mediated performance in attention and working memory (WLL) and temporally-mediated performance in episodic memory (WLL and WLD; Lezak et al. 2012). Previous studies have demonstrated negative associations between the cognitive distraction of physical discomfort, such as thermal discomfort, and frontally-mediated tasks.(Legrain et al. 2013, Lan et al. 2014). In the WLL test, participants heard 10 words in a row, two seconds apart, and were asked to repeat the words they remembered at the completion of the list. For the WLD task the participants were asked to recall as many words as they could remember from the initial list after a five minute delay. More words remembered indicated better performance on that test. Each of the four phone calls included a different list of words from the HRS. WLD was administered at the end of the phone survey as that was timed to be approximately five minutes after the WLD. We created four distinct word lists—one for each phone survey—and we randomly assigned, within each individual, the survey order of the word lists. The Epworth Sleepiness Scale was administered during the delay between the WLL and the WLD. The survey end time was used as the reference time in linking environmental information. We attempted to contact each participant on at least 4 occasions with the goal of completing 4 surveys per participant.
Outdoor Temperature
Outdoor temperature values were obtained from the Detroit City Airport (DET) hourly values from the Integrated Surface Hourly Database (NCEI 2019). DET is approximately 3 km from the East Side housing complex and 7 km from the Lower East Side neighborhood. Missing values (< 0.01% of values) were replaced with Detroit Metropolitan Airport (DTW) values. DTW is 36 km from DET and DET temperature values were well-predicted (R2 = 0.68) by those from DTW. These data were imported using the rnoaa package in R (Chamberlain 2020), converted to local time, and linearly interpolated to create a value for each hour on the hour.
Indoor Temperature
Each participant was given a UX100–011 HOBO logger (Onset Corp.), which recorded indoor temperatures and humidity at hourly intervals. Participants were asked to mount the HOBO at eye level on an interior bedroom wall away from direct sunlight and air vents. Missing indoor data were imputed (see below). Apparent temperature (AT) is a measure of temperature incremented upwards at higher humidity values to better reflect perceived temperature (Steadman 1979). We chose this metric given the synergistic effects of humidity and temperature on sleep quality (Okomato-Mizuno 1999). We calculated AT as AT = –2.653 + (0.994 × temperature) + 0.0153 × (dew point)2 for both indoor and outdoor environments (Zanobetti et al. 2002).
Statistical Analysis
AT exposure, both indoor and outdoor, was characterized in 5 distinct ways. 1) First, for each participant and cognitive exam, we converted AT, one value for each of the prior 24 hours, to a distributed lag nonlinear crossbasis (Gasparrini et al. 2010) using R’s dlnm package. A distributed lag nonlinear crossbasis is a two-dimensional spline of AT. We used a piecewise linear spline with one inflection point (knot) at the median AT of 22 C in the exposure dimension and a natural cubic spline with one knot at 12 hours in the lag dimension. This allowed us to characterize nonlinear associations between AT and cognition (e.g., potential negative associations both at very low and very high temperatures) as well as a nonlinear lag effect (e.g., a potentially stronger effect at immediate vs. much longer lags). We chose a piecewise linear spline in the exposure dimension due to a priori beliefs that effects would be minimized at room temperature (22 C) but be adverse both at colder and hotter temperatures (Zhang et al. 2019). In sensitivity analyses, we moved the knot to other moderate room temperatures: 20 C and 24 C. In the lag dimension, we chose a natural cubic spline, which has an additional degree of freedom, due to a lack of a priori beliefs about the point in time at which effects would begin to diminish. 2) We also characterized nighttime AT as a piecewise linear spline of the average of hourly AT from 22:00 to 06:00 on the night before the exam (lag night 0). 3) To characterize temperature variability at night, we calculated the standard deviation (SD), rather than the average, of nighttime hourly AT in the prior night (lag night 0) as a natural cubic spline with a knot at 1 C. 4) Nighttime AT over the prior 7 nights (lag nights 0–6) was also converted to a crossbasis, again as a piecewise linear spline in the exposure dimension with a knot at 22 C and a natural cubic spline in the lag dimension with a knot at 2 days. 5) We characterized nighttime AT SD over lag days 0–6 as a natural cubic spline crossbasis with a knot at 1 C and lag day 2. If the association modeled using a spline appeared linear, we additionally characterized the temperature metric as a single continuous variable in a separate model.
Taking advantage of the moderate correlation between indoor and outdoor temperature in this population, (Larsen et al. In progress) we performed multiple imputations using chained equations (MICE) using the R package mice (van Buuren and Groothuis-Oudshoorn 2010) to impute missing AT crossbasis values using available values and crossbases formed from 24 lags of airport AT. We imputed the crossbases rather than the raw AT values given that, unlike raw lags of AT, the components of the crossbases are assumed to be linearly associated with the outcome and are not highly multicollinear. We used predictive mean matching and performed 5 imputations with 50 iterations each. Because the mice package only outputs the square root of the diagonal of the covariance matrix rather than the full covariance matrix, which is needed to calculate predictions at given temperature and lag values using model output and the dlnm package above, we calculated the covariance matrix using Rubin’s Rules (Barnard and Rubin 1999) as follows. Step 1: We calculated the multiple imputation point estimate as the mean of the five imputed estimates. Step 2: We calculated the “within” variance, or the mean of the variances. Step 3: We calculated the “between” variance, or mean of the squared differences of each imputation estimate from the multiply-imputed point estimate. Step 4: We calculated total variance as (Step 2) + (Step 3) + (Step 3)/(number of imputations). We confirmed our calculations by verifying that the square root of the diagonal of the resulting covariance matrix was identical to the coefficients’ standard errors calculated for the model output by the mice package, which also used Rubin’s Rules.
We employed repeated measures fixed effects analyses (Wooldridge 2011) in which we included a dummy variable for each participant in a linear regression of temperature on cognitive outcome. This controls for non-time-varying confounding (e.g., age, race, gender, etc.) and instead estimates the change in outcome for a change in time-varying exposure. This is equivalent to modeling the association between the difference between cognitive or sleepiness score and the within-person mean score and the difference between temperature exposure and the within-person mean of that temperature exposure.
| Eq 1 |
where yij is the health effect (WLL, WLD, or sleepiness score) for person i at time point j; α1 through αn are dummy variables for n individuals, vector Tij is either 1) the 24-hour crossbasis for AT, 2) the piecewise linear spline basis for nighttime average AT, 3) the natural cubic spline basis for nighttime AT SD, 4) the 7-day crossbasis for nighttime average AT, or 5) the 7-day crossbasis for nighttime AT SD.
Descriptive statistics, including means, medians, and percentiles were calculated for both the exposures and outcomes as well as for the within-person differences between the values and the within-person means. Pearson’s correlation coefficients were calculated among certain exposure metrics. Descriptive statistics were also calculated over the entire time the temperature and humidity monitors were in the residences: from July 2019 through March 2020.
RESULTS
Participant Characteristics
Due to in-person research restrictions related to the COVID-19 pandemic, we were not able to retrieve the monitors in-person, but most participants returned the monitors by mail or at a drop-off location. Two monitors were mis-programmed and the data were not usable. In total, we acquired hourly indoor temperature and humidity data for 15 of the 18 phone survey participants and 34 of the 41 overall study participants. Of the 18 phone survey participants, indoor temperature and humidity data were imputed for 10 surveys among 3 participants. A total of 64 participant-days were available for analysis, with one participant completing 2 surveys, 6 participants completing 3 surveys, and 11 completing all 4 surveys.
Of the 18 survey participants, most (89%) were women, and 89% identified as African American. Given that we had selected low-income residents, most (83%) of the respondents had annual household incomes less than $20,000 (Table 1), which was lower than the Detroit 2019 median household income of $31,000 (ACS 2021) and well below the national 2019 median household income of $68,700 (Semega et al. 2020). Participant ages ranged from 28–77 years with a median of 58 years.
Table 1.
Counts and percents by race, gender (only male and female reported), and income categories among 18 Detroit, Michigan participants surveyed on 2–4 occasions, July-November, 2019.
| Characteristic | N (Percent) |
|---|---|
| Race | |
| African American | 16 (89%) |
| White | 1 (5%) |
| Other | 1 (5%) |
| Female | 16 (89%) |
| Income categories | |
| $0–19,999 | 15 (83%) |
| $20,000–34,999 | 0 (0%) |
| $35,000–49,999 | 1 (5%) |
| $50,000-$74,999 | 1 (5%) |
| No Answer | 1 (5%) |
Indoor AT and Response Characteristics on the Survey Day
For the days participants were surveyed, hourly AT values in the prior 24 hours ranged from 15.0 C to 32.4 C. Means of AT values over the prior 24-hour periods ranged from 16.7 C to 30.1 C, but nighttime (22:00–06:00) mean AT values were slightly higher and ranged from 17.3 C to 30.8 C. None of the indoor temperature measures exceeded plausible values during the survey period (Table 2). Indoor AT range also varied within person, with the majority of 24-average measurements being at least ±1 to ±6.5 C from the within-person mean (Supplemental Information Table S1). When indoor AT was cooler, indoor AT variability also increased (Pearson correlation coefficient r = −0.38 for AT < 22 C vs. AT SD). WLL and WLD scores ranged from 2 to 10 and 1 to 10, respectively, on these 10-point scales. On the Epworth sleepiness scale, 11 is the threshold above which a respondent is considered to have mild excessive daytime sleepiness. Fifty percent of the reported scores were 6 or less, so most of our responses did not indicate excessive daytime sleepiness (Table 2). WLL, WLD, and sleepiness scores exhibited within-person variability, with the majority of responses being at least ±0.8, ±0.8, and ±1.4 points from the within-person mean, respectively (Supplemental Information Table S1).
Table 2.
Distributions of age, apparent temperature (AT) exposure, cognition (word list and delayed word list learning scores), and sleepiness scores among 18 Detroit, Michigan participants surveyed on 2–4 occasions, July-November, 2019.
| Characteristic | Mean | Min | Median | Max |
|---|---|---|---|---|
| Age (years, N = 14) | 56 | 28 | 58 | 77 |
| Word list learning score (WLL) | 6.4 | 2.0 | 6.0 | 10.0 |
| Delayed word list learning score (WLD) | 4.9 | 1.0 | 4.5 | 10.0 |
| Epworth Sleepiness Scale score | 6.8 | 0.0 | 6.0 | 18.0 |
| AT (C), minimum of lags 0–23 hours† | 22.1 | 15.0 | 22.0 | 28.4 |
| AT (C), maximum of lags 0–23 hours† | 25.5 | 19.1 | 25.6 | 32.4 |
| AT (C), mean of lags 0–23 hours† | 23.6 | 16.7 | 23.2 | 30.1 |
| AT (C), mean of prior night†‡ | 23.9 | 17.3 | 23.6 | 30.8 |
| Meant AT standard deviation (C), prior night†‡ | 0.6 | 0.1 | 0.5 | 3.1 |
N = 15 participants with complete (non-imputed) data representing 54 participant days
Night = 22:00–06:00
Indoor AT on a Warm Day
Indoor AT varied through the day and varied between participants. For example, on the warm day of August 21, 2019, when the outdoor AT ranged from 24.0 to 32.7 C, the hourly median indoor AT across participants ranged within a somewhat comfortable 24.0–27.0 C over the course of the day, with the highest temperatures in the evening. However, hourly maximum indoor AT ranged from 31.1–34.0 C. On that day, participant-specific medians ranged from 21.7–32.2 C, while participant-specific maxima ranged from 23.0–34.0 C, and one participant never experienced indoor ATs below 31 C. Additionally, 3 of the participants experienced indoor ATs greater than 30 C at some point during that day (Supplemental Information Figure S1).
Indoor AT July 2019-March 2020
In examining the range of temperatures experienced throughout the entire larger study period (July 2019-March 2020), including several months after the end of this phone survey period, the first through third quartiles of daily indoor AT remained between 19 C and 28 C (Supplemental Information Figure S2A). However, indoor AT was as low as 8.0 C and as high as 43.5 C. The highest and somewhat implausible values may have resulted from inappropriate placement of a monitor, e.g., near an appliance or in the sun. Nevertheless, even after excluding participant 10, values were as high as 33.8 C. Of the 34 participants, 5 and 22 experienced indoor ATs below 10 C and above 30 C, respectively, and 3 participants experienced both extremes (Supplemental Information Figure S2B).
Associations of Cognitive Changes and Sleepiness with AT
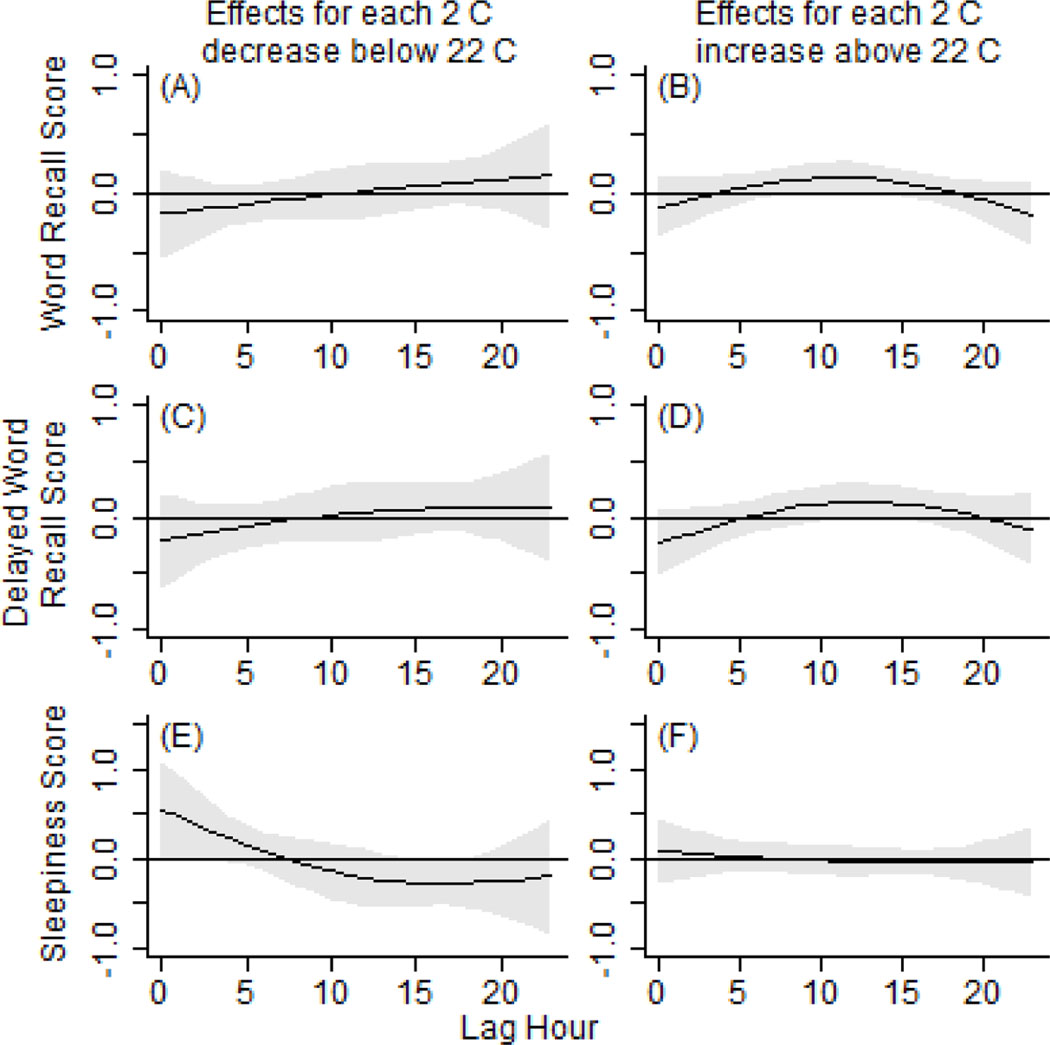
For indoor AT below 22 C, we did not see associations between cognitive changes and AT in the 24 hours preceding the phone survey (Figures 1A, 1C). However, we did see an increase in sleepiness score for low AT in the hour of the survey: for a 2 C decrease in AT below 22 C, we observed a 0.5 (95% CI: −0.0, 1.1, p = 0.05) point increase. In the directions opposite to those hypothesized, we additionally observed a decline in sleepiness score in the 10–20 hours prior to the survey such that, e.g., for a 2 C decrease in AT below 22 C, sleepiness scores decreased by −0.3 (95% CI: −0.5, −0.0, p = 0.03) points in lag hour 17 (Figure 1E). Most of the surveys were administered in the afternoon and evening, so this 10–20 lag hour time period corresponds to the prior evening and night during which individuals might have been trying to sleep. Similarly, with increasing indoor AT above 22 C in this time period of 10–15 hours prior to the survey, results were suggestive of improvements in WLL and WLD scores (Figures 1B, 1D). Specifically, we observed a 0.1 (95% CI: 0.0, 0.3, p = 0.06) point increase in WLL score for each 2 C increase in AT above 22 C at lag hour 12 and a 0.1 (95% CI: 0.0, 0.3, p = 0.09) point increase in WLD score.
Figure 1.
Time course of associations for hourly indoor apparent temperatures prior to the hour of the phone survey (lag hours), the differences between the word recall (A, B), delayed word recall (C, D), and sleepiness (E, F) scores and the scores at 22 C. The left column (A, C, E) are the effects above 22 C and the right column (B, D, F) are the effects below 22 C. The gray shaded areas represent 95% confidence intervals.
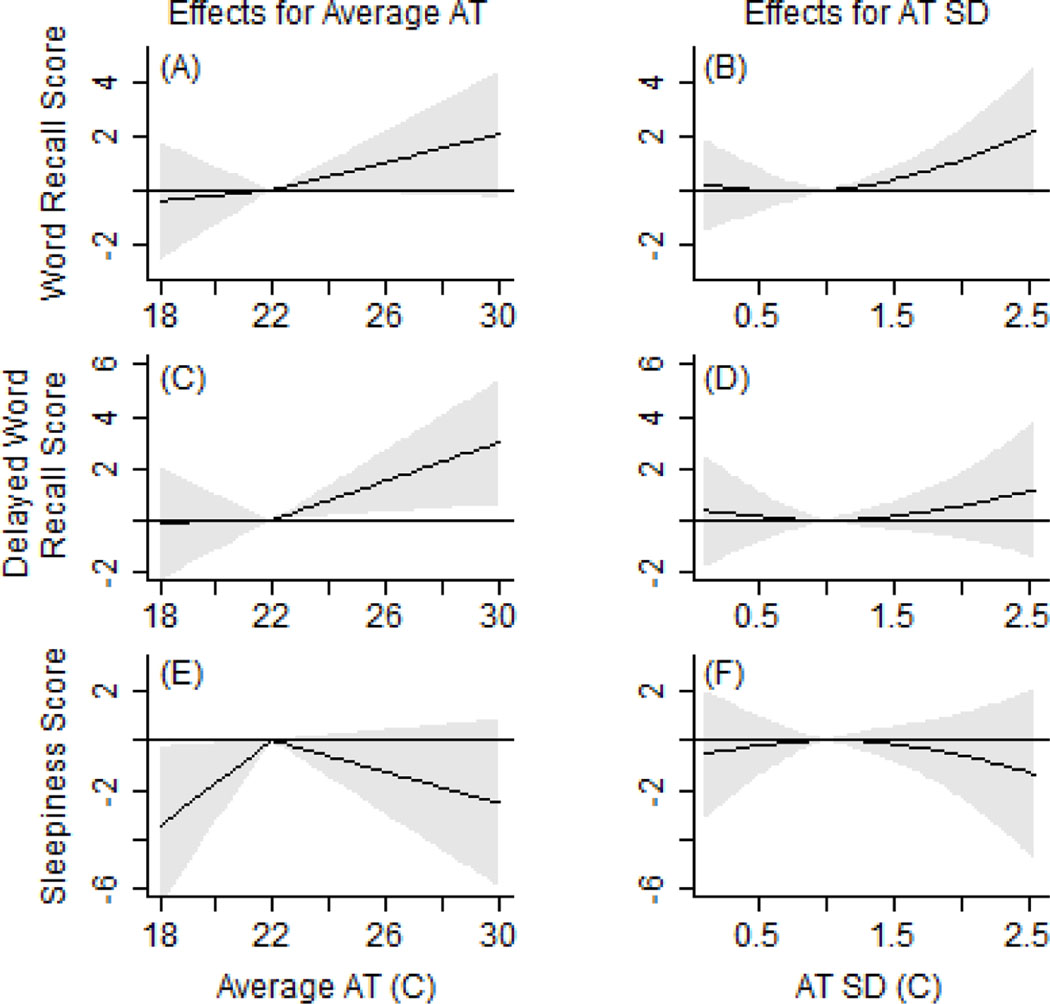
When examining average night time AT in isolation from the other time periods, we found positive associations with WLD, WLL, and sleepiness, which were again contrary to our hypotheses. Specifically, for WLD, we found a 0.7 (95% CI: 0.1, 1.4, p = 0.02) point increase in score for each 2 C increase in average night time AT above 22 C. In fact, neither WLL or WLD exhibited non-linear associations with AT within the observed AT range (Figures 2A and 2C). In a model with AT represented as a single, linear term rather than a spline, we observed a 0.4 (95% CI: 0.0, 0.7) point increase in WLL and 0.4 (95% CI: 0.0, 0.9) point increase in WLD scores for each 2 C increase in AT. At cooler temperatures, we found a −1.7 (95% CI: −3.3, −0.1, p = 0.03) point decrease in sleepiness score for each 2 C decrease in average night time AT below 22 C. When considering the night time AT variability (SD) instead of the average, we observed results suggestive of an increase in WLL score with increasing night time AT SD. However, the AT SD results were not statistically significant and may also have been confounded by cooler average AT given the moderate correlation (r = −0.38) between average night time AT and night time AT SD at AT below 22 C. In sensitivity analyses of average night time AT in which we assigned the cold-hot inflection point at 20 C or 24 C rather than 22 C, results were qualitatively similar for WLL, WLD, and sleepiness, although the positive association between sleepiness and AT at lower temperatures became non-significant (Supplemental Information, Figure S3A-F).
Figure 2.
Associations between nighttime (22:00–06:00) average indoor apparent temperatures (AT) and AT standard deviations (SD) and next-day cognition and sleepiness, or the differences between the word recall (A, B), delayed word recall (C, D), and sleepiness (E, F) scores and the scores at 22 C or an SD of 1 C. The left column (A, C, E) are the effects for average AT and the right column (B, D, F) are the effects for AT SD. The gray shaded areas represent 95% confidence intervals.
In models of 7 prior nights of AT exposure, we did not find significant associations between either average night time AT or night time AT SD and the cognitive or sleepiness scores for any of the lag nights (Supplemental Information, Figures S4A-F and S5A-F).
DISCUSSION
This community-based participatory research study recruited low-income residents of Detroit and estimated associations between indoor temperatures and the participants’ cognitive function and daytime sleepiness during 2019. Although findings were mixed and inconsistent with some prior literature, our work adds to the limited body of knowledge about how temperature may influence indicators of health and quality of life, and not only deaths and urgent health effects requiring hospital visits. This research is an important area of inquiry in the context of climate change and the well-documented disparities in weather-related health outcomes, and may also inform efforts to reduce energy insecurity among lower-income populations and enhance environmental justice. We next discuss our findings in more detail and in the context of previous findings from the literature, discuss strengths and limitations, and suggest areas for future research building upon this work.
Cognition and AT
Multiple domains of indoor environmental quality, including thermal environment, lighting, noise, and air pollution, have been found to influence cognitive performance (reviewed in Wang et al. 2021). Cold temperature exposure has been shown to impact memory, vigilance, and reaction time as well as changes in dopamine, epinephrine, and norepinephrine levels (reviewed in Taylor et al. 2016). Cognitive deficits related to temperature may also be due to a distracting effect of thermal discomfort or poor sleep the prior night (Lan et al. 2017, Alhola & Polo-Kantola 2007, Johnson et al. 2017). However, many of our findings, particularly for the warm temperatures, did not agree with these prior findings or support our hypotheses that working and episodic memory and auditory attention cognitive domains would show an inverse-V-shaped association with AT within the range of observed ATs (18–30 C) and with an inflection point of 20–24 C. Rather, we observed an increase in these domains of cognitive performance with increasing ATs, which supports the hypothesis of a protective effect of increasing AT, but not the hypothesis that the upper threshold for this effect is 22 C. Our survey period started mid-summer and ended in mid-autumn, prior to the much colder outdoor and indoor temperatures experienced by some of our participants and after the hottest day of the summer (maximum AT of 39.9 C). Therefore, our participants may not have experienced indoor temperatures above or below the threshold at which temperature has deleterious effects on these cognitive domains. In contrast to field studies that did capture more extreme temperatures, attention/processing speed and working memory were reduced in young adults in non-air conditioned buildings during a heat wave (Laurent et al. 2018), and the odds of having a low mini-mental status score was minimized at daily mean outdoor temperatures of 10–15 C in older male veterans, with the daily mean outdoor temperature ranging from −5 C to 25 C (Dai et al. 2016). In a meta-analysis of cognition and temperature studies, where cognition included office productivity and learning, Seppanen et al. (2006) found a 10% decline in normalized performance for indoor temperatures at 30 C vs. 23 C.
These and other studies are consistent with the idea that a U- or V-model, with a single inflection point, is too restrictive (Zhang et al. 2019). Instead, the “extended-U” model (Hancock and Warm 2003) may be more appropriate in allowing for a wider range of temperatures over which cognition is only slightly or not at all affected by temperature and therefore allowing for significantly increasing or decreasing associations at only the extreme ends of the temperature range. Support for the extended-U model with regards to memory was found in a recent qualitative meta analysis of studies of college students (Wang et al. 2021). Additional support for an extended-U model was provided by a quantitative meta-analysis of laboratory studies of temperature and cognitive function, incorporating studies using a wide variety of cognitive performance measures.,In this meta analysis, effects in the experimental groups vs. the control groups did not change substantially when temperature rose to 5 C above the control group room temperatures. However, 5% decreases in overall cognitive function were observed for a 6 C decrease in temperature or a 9 C increase in temperature, and cognitive function declined by as much as 8% at extreme hot and cold temperatures. As expected, heterogeneity in study findings was considerable given different levels of acclimatization, physical fitness, thermal comfort, and clothing between studies (Yeganeh et al. 2018). With respect to thermal comfort and acclimatization, military and sports medicine studies have demonstrated physiological adaptation to warm temperatures (Garrett et al. 2011). Specific to cognition, a chamber study of tropically-acclimated and temperate-climate-acclimated men showed greater decrement in mental arithmetic performance in the temperate-climate acclimated men (Wijayanto et al. 2017). In occupational settings, thermal comfort preferences vary across individuals and countries, and this variation may be due in part to differences in acclimatization (Hwang & Cheng 2007). These studies further support the idea that our temperature ranges were not sufficiently wide to detect decreases in cognitive function in a U-shaped model, particularly for hot temperatures. Additionally, studies of mortality and temperature have found a strong effect of timing in year such that the first wave of high temperatures in spring or early summer has the most substantial deleterious effects, and then subsequent days or nights of high temperature in mid- or late-summer are less impactful as subjects have likely become either acclimated to or, rarely, expired from high temperatures (Gasparrini et al. 2016). Therefore, future research on indoor temperatures and cognition should study warm-temperature effects early in and throughout the summer and should also study cold temperature effects during the coldest months. Future studies should also include a higher number of participants to provide the statistical power needed for an extended-U model, or more flexible regression splines that could account for a potentially wide range of ideal indoor AT values.
Sleep and AT
In support of one hypothesis, we did observe an increase in sleepiness when AT was below 22 C in the hour of the phone survey. However, when considering a longer time course of exposure, our results did not support our hypothesis of a V-shaped association between AT and sleepiness within the range of observed ATs (18–30 C) and an inflection point of 20–24 C. However, we did see significantly reduced daytime sleepiness at lower bedroom temperatures the night before, suggesting that sleep quality was maximized at these lower nighttime bedroom temperatures. Our results are consistent with those from a study of 8 older men in Japan with average bedroom temperatures ranging from 20–28 C. In that study, increasing air temperature and humidity were correlated with earlier wake-up times and decreased sleep efficiency (Tsuzuki et al. 2015). However, our findings conflict with those from studies of Hong Kong students in their dormitory rooms, in which sleeping thermal environment satisfaction was maximized at 24.2 C with satisfaction slightly diminished at both lower and higher temperatures (Zhang et al. 2018), and sleep quality was higher among students reporting thermal satisfaction vs. those reporting feeling too hot or cold (Tsang et al. 2021). Also, perhaps because our participants did not experience extreme-heat conditions, our findings did not concur with those of a Massachusetts study (Williams et al. 2019), in which sleep was disrupted in low-income housing residents during a heat wave. Our results also conflict with a review of sleep and thermal environment studies finding that heat exposure, but not mild cold exposure, impacts sleep stages in community-based settings where bedding and clothing can be altered by the participants (Okamoto-Mizuno K & Mizuno 2012).
In general, minimum wintertime recommended indoor temperatures for sleeping range from 17–20 C and maximum summertime indoor temperatures range from 23–26 C (Jackson & Gaston 2019). In community settings, thermal comfort during sleep has been optimized at temperatures as high as 24 C (Lin & Deng 2008). These wide ranges in comfortable sleeping temperatures are likely due in part to the strong influences of bedding and bed clothing on optimal ambient sleeping temperature (Irshad et al. 2019, Pan et al. 2012, Lin & Deng 2008, Zhang et al. 2018, Wang et al. 2015). If bedding and bed clothing remained consistent within our participants during each participant’s survey period, then our study would have controlled for bedding and clothing effects by examining only within-person changes in sleepiness with within-person changes in temperature. However, individuals in our study may have altered their bedding and clothing based on ambient bedroom temperature in ways that were not consistent from one individual to the next.
Study Strengths
In contrast to most temperature and cognition or temperature and sleep research, our indoor temperature measurements were acquired in a community setting, among adults, including retirees, in their own homes. We also employed a community-based participatory research approach, whereby community partners participated in and enhanced the quality of the study design, played a critical role in recruitment and retention, and participated in analysis and dissemination. Our long observation period across multiple months allowed for indoor temperature characterization in 3 seasons and longitudinal, within-person comparisons of temperature with short-term changes in sleep and cognition to fully control for non-time-varying confounding.
Furthermore, although air conditioning is often proposed as an easy mitigation method, for many low-income families, such as those included in our study, the cost of mechanical cooling is likely prohibitive. Heating and cooling costs in the Midwestern U.S. can strain household resources, where 1 in 5 residents reported reducing or forgoing food or medicine to pay energy costs in the 2015 Residential Energy Consumption Survey (EIA 2018). Therefore, low-income subjects are potentially most greatly impacted by indoor temperature and temperature variability due to fewer household resources to control the indoor environment.
Study Limitations and Avenues for Future Research
We did not control for indoor air pollutants, which may be associated with cognitive function and correlate with indoor temperatures (Du et al. 2020). Furthermore, the Epworth Sleepiness Scale includes questions about riding in cars, which may not be appropriate for our low-income, urban population. We chose the WLL and WLD tests given their validated use over the phone and in racially diverse populations (e.g., Howard et al. 2005). Simple task decrement in the heat has been reported in a small number of studies, but there is evidence that more complex tasks are more sensitive to heat (Wang et al. 2021). We also did not ask about pajama type or coverage or bedding materials. We assumed that individuals would select the combination of each that would maximize their comfort given ambient bedroom temperatures, but preferences could be influenced by other factors and vary seasonally. We also did not verify that participants had properly sited the monitors prior to phone survey administration. Without a clear decision rule on what would be an impossible indoor temperature value, we did not drop or impute high values. However, an overestimate of the change in exposures from one time period to the next might have biased our results. Higher sample size, in addition to allowing us to fit an extended-U model as discussed above, would allow us to examine differences by sex and age, which may be important for generalizing our findings. Notably, prior research suggests that men have been found to prefer cooler sleeping environments due perhaps to higher basal metabolic rates (Irshad et al. 2019, Pan et al. 2012), and it is plausible that women’s temperature preferences vary across the life course, including during pregnancy and perimenopause. Our participants ranged in age from 28–77 years old, and prior research has shown that age impacts cognitive performance and sleep (e.g., Mander et al. 2017, Murman 2015). Additionally, sleep disparities by race have been observed (Johnson et al. 2019), and a better understanding of the determinants of sleep quality and subsequent daytime sleepiness in low-income households and people of color is critical to eliminating these disparities.
Higher sample sizes would permit us to consider interactions between duration and intensity of exposure, with the idea that habituation to the temperatures occur or, conversely, that long durations of mild temperatures may be as impactful as short durations of intense exposure. The surveys were also administered from late morning through the evening, which may have introduced chronobiological bias, considering the circadian patterns of cognitive performance and sleepiness (e;g., Blatter & Cajochen 2007, Schmidt & Bao 2017). Finally, little is known about precisely which domains of cognition are impacted by temperature in a non-occupational setting. We chose to study domains that were measured by tests easily administered in a short amount of time over the phone. Future studies should examine a more comprehensive range of cognitive domains, including complex cognitive tasks such as arithmetic given that complex cognitive tasks may be more susceptible to temperature (Zhang et al. 2019).
Conclusions
Our results were suggestive of short-term associations of AT with sleepiness and cognition, such that sleepiness increased when AT was below 22 C in the hour of the testing and cognition declined for each 2 C decrease in average nighttime AT below 30 C. Protective effects of cool (18–22 C) nighttime AT on daytime sleepiness were also observed. The association between cognition and AT was linear, rather than V-shaped as hypothesized. Future research should expand sample size, seasons of testing, and number of tests per person to allow for a potentially more complex functional form, i.e., an “extended-U” shape, of cognition and sleepiness with temperature. These advancements would enable the characterization of cognition and sleepiness over the wide range of indoor temperatures experienced by this and other low-income populations.
Supplementary Material
Practical Implications (up to 5 sentences):
Climate adaptation strategies should account for non-emergency health problems related to indoor temperature rather than just the mortality and emergencies related to temperature. Even in late summer and autumn, short-term changes in temperature weree associated with short-term changes in sleepiness and cognitive function. We did not see deleterious effects at high temperatures as hypothesized, but this may be due to insufficient sampling on extreme heat days. Further research on indoor temperatures and health is warranted to inform low-income energy efficiency assistance policies.
Acknowledgments:
We thank the Climate Hazards, Housing, and Health Community-Academic Partnership and the Detroit Communities Reducing Energy and Water (D-CREW) participants.
Funding Statement: This work was funded by grants R00ES026198 and P30 ES017885 from the National Institute for Environmental Health Sciences, grant T42 OH008455-09 from the National Institute for Occupational Safety and Health, grant 1520803 from the National Science Foundation, and grants from the University of Michigan Poverty Solutions and M-Cubed programs.
Data availability statement: The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Ethics approval statement: This study was approved and exempted from annual review by the Institutional Review Board of the University of Michigan (study number HUM00166674).
Footnotes
Conflict of interest disclosure: The authors have no conflicts of interest to declare.
Patient consent statement: All participants provided informed consent.
Permission to reproduce material from other sources: Not applicable.
REFERENCES
- American Community Survey (ACS). 2021. 2019 American Community Survey 1-Year Estimates. [Google Scholar]
- Barbic F, Minonzio M, Cairo B, Shiffer D, Dipasquale A, Cerina L, et al. 2019. Effects of different classroom temperatures on cardiac autonomic control and cognitive performances in undergraduate students. Physiol Meas 40:054005; doi: 10.1088/1361-6579/ab1816. [DOI] [PubMed] [Google Scholar]
- Barnard J, Rubin DB. 1999. Small-sample degrees of freedom with multiple imputation. Biometrika 86: 948–955. [Google Scholar]
- Bednar DJ, Reames TG, Keoleian GA. 2017. The intersection of energy and justice: Modeling the spatial, racial/ethnic and socioeconomic patterns of urban residential heating consumption and efficiency in Detroit, Michigan. Energy Build 143:25–34; doi: 10.1016/j.enbuild.2017.03.028. [DOI] [Google Scholar]
- Blatter K, Cajochen C. 2007. Circadian rhythms in cognitive performance: Methodological constraints, protocols, theoretical underpinnings. Physiology & Behavior 90:196–208. doi: 10.1016/j.physbeh.2006.09.009. [DOI] [PubMed] [Google Scholar]
- Chamberlain S. 2020. rnoaa: “NOAA” Weather Data from R. R package version 0.9.6. [Google Scholar]
- Climate-Data.org. Available: https://en.climate-data.org/north-america/united-states-of-america/michigan/detroit-59/
- Cui W, Cao G, Park JH, Ouyang Q, Zhu Y. 2013. Influence of indoor air temperature on human thermal comfort, motivation and performance. Build Environ 68:114–122. doi: 10.1016/j.buildenv.2013.06.012. [DOI] [Google Scholar]
- Dai LZ, Kloog I, Coull BA, Sparrow D, Spiro A, Vokonas PS, et al. 2016. Cognitive function and short-term exposure to residential air temperature: A repeated measures study based on spatiotemporal estimates of temperature. Environ Res 150:446–451; doi: 10.1016/j.envres.2016.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du B, Tandoc MC, Mack ML, Siegel JA. 2020. Indoor CO2 concentrations and cognitive function: A critical review. Indoor Air Nov;30(6):1067–1082. doi: 10.1111/ina.12706. [DOI] [PubMed] [Google Scholar]
- Energy Information Administration (EIA). 2018. U.S. Residential Energy Consumption Survey Table HC11.1 Household Energy Insecurity, 2015. Available: https://www.eia.gov/consumption/residential/data/2015/hc/php/hc11.1.php [accessed Feb 24 2021].
- Field CB, Barros V, Stocker TF, Dahe Q. 2012. Managing the risks of extreme events and disasters to advance climate change adaptation: Special report of the intergovernmental panel on climate change (ipcc). Cambridge, UK, and New York, NY, USA:Cambridge University Press. [Google Scholar]
- Garrett AT, Rehrer NJ, Patterson MJ. 2011. Induction and decay of short-term heat acclimation in moderately and highly trained athletes. Sports medicine (Auckland, NZ) 41:757–771. doi: 10.2165/11587320-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2010. Distributed lag non-linear models. Stat Med 29:2224–34; doi: 10.1002/sim.3940 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Hashizume M, Lavigne E, Zanobetti A, Schwartz J, et al. 2015. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386:369–75; doi: 10.1016/s0140-6736(14)62114-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo YM, Hashizume M, Lavigne E, Tobias A, Zanobetti A, et al. 2016. Changes in susceptibility to heat during the summer: A multicountry analysis. American Journal of Epidemiology 183:1027–1036. doi: 10.1093/aje/kwv260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman J, Hurwitz M, Park J, Smith J. 2018. Heat and Learning. Natl Bur Econ Res Working Paper No. 24639. [Google Scholar]
- Great Lakes Integrated Sciences and Assessments (GLISA). 2017. Historical climatology: Detroit, michigan. Detroit, Michigan:Detroit Climate Action Collaborative. [Google Scholar]
- Gronlund CJ, Cameron L, Shea C, O’Neill MS. 2019. Assessing the magnitude and uncertainties of the burden of selected diseases attributable to extreme heat and extreme precipitation under a climate change scenario in Michigan for the period 2041–2070. Env Health 18; doi: 10.1186/s12940-019-0483-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock PA, Warm JS. 2003. A dynamic model of stress and sustained attention. Journal of Human Performance in Extreme Environments 7:4. [DOI] [PubMed] [Google Scholar]
- Health and Retirement Study. 2018. HRS 2018 Questionnaires, Section D: Cognition. [Google Scholar]
- Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, et al. 2005. The reasons for geographic and racial differences in stroke study: Objectives and design. Neuroepidemiology 25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- Hwang RL, Cheng M-J. 2007. Field survey on human thermal comfort reports in air-conditioned offices in taiwan. The open construction and building technology journal 1. [Google Scholar]
- Intergovernmental Panel on Climate Change (IPCC). 2018. Summary for Policymakers. Masson-Delmotte Zhai V,P, Pörtner HO, Roberts D, Skea J, Shukla PR, Pirani A, Moufouma-Okia W, Péan C, Pidcock R, Connors S, Matthews JBR, Chen Y, Zhou X, Gomis MI, Lonnoy E, Maycock T, Tignor M. and Waterfield T, eds. Glob Warm 15°C IPCC Spec Rep Impacts Glob Warm 15°C Pre-Ind Levels Relat Glob Greenh Gas Emiss Pathw Context Strength Glob Response Threat Clim Change Sustain Dev Efforts Eradicate Poverty 32. [Google Scholar]
- Irshad K, Algarni S, Jamil B, Ahmad MT, Khand MA. 2019. Effect of gender difference on sleeping comfort and building energy utilization: Field study on test chamber with thermoelectric air-cooling system. Build Environ 152:214–227. doi: 10.1016/j.buildenv.2019.01.058. [DOI] [Google Scholar]
- Jackson CL, Gaston SA. 2019. Ch. 8 - The impact of environmental exposures on sleep. Sleep and Health. 10.1016/B978-0-12-815373-4.00008-3. [DOI] [Google Scholar]
- Jessel S, Sawyer S, Hernández D. 2019. Energy, Poverty, and Health in Climate Change: A Comprehensive Review of an Emerging Literature. Front Public Health 7:357; doi: 10.3389/fpubh.2019.00357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MW. 1994. Sleepiness in Different Situations Measured by the Epworth Sleepiness Scale. Sleep 17:703–710; doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- Johnson DA, Jackson CL, Williams NJ, Alcántara C. 2019. Are sleep patterns influenced by race/ethnicity - a marker of relative advantage or disadvantage? Evidence to date. Nature and Science of Sleep 11:79–95. doi: 10.2147/nss.S169312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan L, Wargocki P, Lian Z. 2014. Thermal effects on human performance in office environment measured by integrating task speed and accuracy. Applied ergonomics 45:490–495. [DOI] [PubMed] [Google Scholar]
- Larsen L, Gronlund CJ, Berrocal V, O’Neill MO, Stone B. In progress. Modification of outdoor-indoor temperature associations by housing and neighborhood characteristics in Detroit, MI. [Google Scholar]
- Laurent JGC, Williams A, Oulhote Y, Zanobetti A, Allen JG, Spengler JD. 2018. Reduced cognitive function during a heat wave among residents of non-air-conditioned buildings: An observational study of young adults in the summer of 2016. Plos Med 15:20; doi: 10.1371/journal.pmed.1002605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legrain V, Crombez G, Plaghki L, Mouraux A. 2013. Shielding cognition from nociception with working memory. Cortex 49:1922–1934. [DOI] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Bigler ED, & Tranel D. (2012). Neuropsychological assessment. Oxford University Press, USA. [Google Scholar]
- Liu Y, Saha S, Hoppe BO, Convertino M. 2019. Degrees and dollars - Health costs associated with suboptimal ambient temperature exposure. Sci Total Environ 678:702–711; doi: 10.1016/j.scitotenv.2019.04.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mander BA, Winer JR, Walker MP. 2017. Sleep and human aging. Neuron 94:19–36. doi: 10.1016/j.neuron.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy JG, Strecker RE. 2011. The cognitive cost of sleep lost. Neurobiology of Learning and Memory 96:564–582. doi: 10.1016/j.nlm.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michigan Public Service Commission (MPSC). 2021. Utility Customer Data. Compiled from monthly reports: https://www.michigan.gov/mpsc/0,9535,7-395-93309_93438_93459-561128--,00.html
- Murman D. The impact of age on cognition. In: Proceedings of the Seminars in Hearing, 2015, Vol. 36, 111–121. 10.1055/s-0035-1555115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy PJ, Campbell SS. 1997. Nighttime drop in body temperature: A physiological trigger for sleep onset? Sleep 20:505–511. doi: 10.1093/sleep/20.7.505. [DOI] [PubMed] [Google Scholar]
- National Centers for Environmental Information (NCEI). 2019. Integrated Surface Hourly Database. [Google Scholar]
- Ofstedal MB, Fisher GG, Herzog AR. 2005. Documentation of cognitive functioning measures in the health and retirement study. HRS/AHEAD Documentation Report DR- 006. Available through the Survey Research Center at the Institute for Social Research, University of Michigan. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-006.pdf [Google Scholar]
- Okamoto-Mizuno K, Mizuno K, Michie S, Maeda A, Lizuka S. 1999. Effects of humid heat exposure on human sleep stages and body temperature. Sleep 22:767–773. [PubMed] [Google Scholar]
- Okamoto-Mizuno K, Mizuno K. 2012. Effects of thermal environment on sleep and circadian rhythm. J Physiol Anthropol 31:9. doi: 10.1186/1880-6805-31-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan L, Lian Z, Lan L. 2012. Investigation of gender differences in sleeping comfort at different environmental temperatures. Indoor and Built Environment 21:811–820. doi: 10.1177/1420326X11425967. [DOI] [Google Scholar]
- Peel MC, Finlayson BL, McMahon TA. 2007. Updated world map of the Köppen-Geiger climate classification. Hydrol Earth Syst Sci 11:1633–1644. doi: 10.5194/hess-11-1633-2007. [DOI] [Google Scholar]
- Pilcher JJ, Nadler E, Busch C. 2002. Effects of hot and cold temperature exposure on performance: a meta-analytic review. Ergonomics 45:682–698; doi: 10.1080/00140130210158419. [DOI] [PubMed] [Google Scholar]
- Schmidt C, Bao Y. 2017. Chronobiological research for cognitive science: A multifaceted view. PsyCh Journal 6:249–252. doi: 10.1002/pchj.203. [DOI] [PubMed] [Google Scholar]
- Scullin MK & Bliwise DL. 2015. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspectives on Psychological Science, 10(1), 97–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semega J, Kollar M, Shrider EA, Creamer J. 2020. Income and Poverty in the United States: 2019. [Google Scholar]
- Sörös P, Marmurek J, Tam F, Baker N, Staines WR, Graham SJ. 2007. Functional MRI of working memory and selective attention in vibrotactile frequency discrimination. BMC neuroscience 8:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steadman RG. 1979. The assessment of sultriness, part I: A temperature humidity index based on human physiology and clothing science. J Appl Meteor 18:861–873. [Google Scholar]
- Taylor L, Watkins SL, Marshall H, Dascombe BJ, Foster J. 2016. The Impact of Different Environmental Conditions on Cognitive Function: A Focused Review. Front Physiol 6; doi: 10.3389/fphys.2015.00372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuzuki K, Mori I, Sakoi T, Kurokawa Y. 2015. Effects of seasonal illumination and thermal environments on sleep in elderly men. Build Environ 88:82–88. [Google Scholar]
- Census Bureau US. 2020. 2019 American Housing Survey. [Google Scholar]
- van Buuren S, Groothuis-Oudshoorn K. 2010. mice: Multivariate imputation by chained equations in R. J Stat Softw 1–68. [Google Scholar]
- Wang C, Zhang F, Wang J, Doyle JK, Hancock PA, Mak CM, et al. 2021. How indoor environmental quality affects occupants’ cognitive functions: A systematic review. Build Environ:107647. doi: 10.1016/j.buildenv.2021.107647. [DOI] [Google Scholar]
- Wang Y, Liu Y, Song C, Liu J. 2015. Appropriate indoor operative temperature and bedding micro climate temperature that satisfies the requirements of sleep thermal comfort. Build Environ 92:20–29. doi: 10.1016/j.buildenv.2015.04.015. [DOI] [Google Scholar]
- Wijayanto T, Toramoto S, Maeda Y, Son S-Y, Umezaki S, Tochihara Y. 2017. Cognitive performance during passive heat exposure in japanese males and tropical asian males from southeast asian living in japan. J Physiol Anthropol 36:8. doi: 10.1186/s40101-016-0124-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AA, Spengler JD, Catalano P, Allen JG, Cedeno-Laurent JG. 2019. Building vulnerability in a changing climate: Indoor temperature exposures and health outcomes in older adults living in public housing during an extreme heat event in cambridge, ma. International Journal of Environmental Research and Public Health 16:15. doi: 10.3390/ijerph16132373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge JM. 2011. Econometric Analysis of Cross Section and Panel Data (2nd Edition). [Google Scholar]
- Xiong LL, Huang X, Li J, Mao P, Wang X, Wang RB, et al. 2018. Impact of Indoor Physical Environment on Learning Efficiency in Different Types of Tasks: A 3 × 4 × 3 Full Factorial Design Analysis. Int J Environ Res Public Health 15; doi: 10.3390/ijerph15061256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Lan L, Lian ZW, De Dear R. 2020. Associations of bedroom temperature and ventilation with sleep quality. Science and Technology for the Built Environment 26:1274–1284. doi: 10.1080/23744731.2020.1756664. [DOI] [Google Scholar]
- Yeganeh AJ, Reichard G, McCoy AP, Bulbul T, Jazizadeh F. 2018. Correlation of ambient air temperature and cognitive performance: A systematic review and meta-analysis. Build Environ 143:701–716. doi: 10.1016/j.buildenv.2018.07.002. [DOI] [Google Scholar]
- Zanobetti A, Schwartz J, Samoli E, Gryparis A, Touloumi G, Atkinson R, et al. 2002. The temporal pattern of mortality responses to air pollution: A multicity assessment of mortality displacement. Epidemiology 13:87–93; doi: 10.1097/00001648-200201000-00014. [DOI] [PubMed] [Google Scholar]
- Zhang N, Cao B, Zhu Y. 2018. Indoor environment and sleep quality: A research based on online survey and field study. Build Environ 137:198–207. doi: 10.1016/j.buildenv.2018.04.007 [DOI] [Google Scholar]
- Zhang F, de Dear R, Hancock P. 2019. Effects of moderate thermal environments on cognitive performance: A multidisciplinary review. Appl Energy 236:760–777; doi: 10.1016/j.apenergy.2018.12.005. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.