Abstract
Revision anterior cruciate ligament (ACL) procedures are increasing in incidence and possess markedly inferior clinical outcomes (76% satisfaction) and return-to-sports (57%) rates than their primary counterparts. Given their complexity, a universal language is required to identify and communicate the technical challenges faced with revision procedures and guide treatment strategies. The proposed REVISE ACL Classification can serve as foundation for this universal language that is feasible and practical with acceptable inter-rater agreement. A focus group of sports medicine fellowship-trained orthopaedic surgeons was assembled to develop a classification to assess femoral/tibial tunnel “usability” (placement, widening, overlap) and guide the revision reconstruction strategy (one- versus two-stage) post-failed ACL reconstruction. Twelve board-certified sports medicine orthopaedic surgeons independently applied the classification to the de-identified computed tomography (CT) scan data of ten patients, randomly selected, who failed ACL reconstruction. An Inter-class Correlation Coefficient (ICC) was calculated (with 95% Confidence Intervals) to assess agreement amongst reviewers concerning the three major classifications of the proposed system. Across surgeons, and on an individual patient-basis, there was high internal validity and observed agreement on treatment strategy (one- versus two-stage revision). Reliability testing of the classification using CT scan data demonstrated an ICC [95% CI] of 0.92 [0.80, 0.98] suggesting “substantial” agreement between the surgeons across all patients for all elements of the classification. The proposed REVISE ACL Classification, which employs CT scan analysis to both identify technical issues and guide revision ACL treatment strategy (one- or two-stage) constitutes a feasible and practical system with high internal validity, high observed agreement and substantial inter-rater agreement. Adoption of this classification, both clinically and in research, will help provide a universal language for orthopaedic surgeons to discuss these complex clinical presentations and help standardize an approach to diagnosis and treatment to improve patient outcomes.
Level of Evidence:
3.
INTRODUCTION:
Failures of ACL reconstruction are multi-factorial and are influenced, in part, by such factors as: patient demographics (age, gender, body mass index, sport(s) played, level of competition, presence of missed and/or concomitant injuries to cartilage, cruciate/collateral ligaments, and menisci); technical issues (graft type/size/fixation/tension, tunnel drilling/preparation); and post-operative course (compliance with rehabilitation, complications)1. In addition, there is increased attention on the influence of bony morphology on failures of ACL reconstruction; in particular, increased tibial slope2. In broad terms, a recent study by the Multicenter ACL Revision Study (MARS) Group categorized failures as a result of traumatic re-injury (32%), technical errors (24%), or failures of biology (7%) – though often, a combination of factors (37%) exists3,4. Preoperative planning for revision ACL reconstruction requires a careful analysis to identify the contributing factor(s) – an analysis developed via a thorough history and physical examination and supplemented by a variety of diagnostic imaging modalities including but not limited to: plain radiographs (including a full length standing hip-ankle radiograph and standing monopedal lateral view), magnetic resonance imaging (MRI), computed tomography (CT), and the arthroscopic evaluation5. Further complicating the issue, revision procedures classically perform inferiorly to primary reconstruction across a variety of patient-reported and objective outcomes measures6. In fact, a recent systematic review of revision ACL patients reported that 57% did not return to pre-injury levels of sports7, and patient satisfaction remains as low as 76%8.
As an understanding of the nuances of ACL reconstruction continues to develop, it is possible that previous data underestimate the relative contribution of surgical technique to outcomes. Over 70% of primary ACL reconstructions are proposed to fail mainly as a result of technical factors9, specifically anterior femoral tunnel malposition10. Not only does each revision procedure present a unique set of challenges – be it handling bone loss/tunnel defects, retained hardware, malalignment, or incorrect tunnel placement5; but the ultimate revision strategy appears to be influenced in large part by surgeon preference3. As such, the potential inability for surgeons to reach consensus on contributing factors to non-ideal outcomes exists3 – the ramifications of which, include poor communication and limited literature interpretation. In orthopaedics, particularly in the knee, there exist classifications to identify and guide issues with chondral11 and meniscal pathology12, including root tears13. However, given both the heterogeneity across many parameters of the ACL reconstruction technique and a continual evolution of the surgical technique to improve results, there remains a need to establish a universal language in the revision scenario that surgeons can employ to communicate core decision-making elements. This is especially important in light of the potential relative annual infrequency that revision procedures are performed on an individual per surgeon basis. Thus, the purpose of this study is to propose and assess the feasibility of applying a revision ACL classification system for identifying technical problems with the index procedure and guiding treatment strategies (one- vs. two-stage) that can establish standards to inform clinical practice and better ascertain outcomes in this setting. The goal of this proposed classification system is not to identify a correct way to perform revision ACL reconstruction, but to develop a common language that surgeons and researchers can use to appropriately classify revision ACL reconstruction so that more meaningful research and data can be gleamed from an otherwise heterogenous population.
METHODS:
This study received Institutional Research Ethics Board approval (ID: PRO18020202; PRO18020185).
Study Development and Administration:
A focus group of North American board-certified orthopaedic surgeons with formal orthopaedic sports medicine fellowship training was assembled to identify the technical considerations important to revision ACL reconstruction. To develop a classification system that was easy to recall, simple to apply, and clinically-useful, meetings were held where hypothetical revision ACL scenarios were presented, classification schema applied, and revised appropriately to not only be all-encompassing, but to emphasize common clinical scenarios. A classification system that progressed in severity/complexity (one-stage to two-stage), and that presented modifiers for femoral-specific issues, tibial-specific issues, or both, in addition to malalignment was developed. The focus group performed both an extensive literature search for technical causes of failure, and in conjunction with prevalence data and expert polling, ultimately focused on tunnel malposition, widening / overlap, and malalignment issues, given their substantially higher influence as technical causes for failure amongst many3. Given that multiple methods exist in the literature to examine these parameters, with no established “gold standard”, the consensus amongst the focus group was to omit specific criteria/measurements for malposition or degree of tunnel widening to reflect and capture “surgeon gestalt.” This is supported by previous CT-based studies that have demonstrated high consistency and precision for both femoral and tibial tunnel location amongst surgeons performing single-bundle reconstructions through the anteromedial portal14. As well, it has been demonstrated that ACL surgeons are internally consistent with regards to their individual femoral and tibial tunnel locations, falling between 85% (femur) and 90% (tibia) of pre-established guidelines for ideal tunnel placement15. Moreover, though early literature attributed 15% of failed ACL reconstructions to missed associated ligament injuries16, the focus group felt this is likely an over-estimation given current improvements in injury understanding, physical examination, and sensitivity of diagnostic modalities minimizing this occurrence. In fact, missed/persistent posteromedial and posterolateral knee laxity, specifically, is attributable for 2% and 1% of ACL failures, respectively3. The focus group consensus remained that excluding these infrequent parameters additionally improved the applicability of the classification.
The final iteration of this classification (TABLE 1), with associated example images (FIGURES 1, 2, 3) follows. Type 1A is defined as a revision that requires no changes to the management (position or bone grafting) of both the index femoral and tibial tunnels; Type 1B refers to a revision that is performed as a one-stage, but that requires modifications to the femoral (F) and/or tibial (T) tunnels (1B, F; 1B, T; 1B, FT); Type 2 refers to a revision that is performed as a two-stage, due to significant tunnel widening/overlap, obvious malalignment, and infection. Type 2 also uses F, T, and I modifiers to specify tunnel location of tunnel widening/overlap (2F, 2T, and 2FT) as well as infection (2I). Previous understanding of revision ACL reconstruction show that approximately 34% of revisions follow the Type 1A classification and can be performed in one stage without change to previous tunnels, 50% of revisions follow Type 1B and require either one or both of the tunnels to re-drilled, and 15% of revisions follow Type 2 and are performed as two-stage procedures with significant tunnel widening/overlap.3,4,15 Combined, the proposed REVISE classification system is widely applicable and relevant for approximately 99% of all possible approaches to revision ACL reconstruction.
Table 1.
The REVision using Imaging to guide Staging and Evaluation (REVISE) in ACL Reconstruction Classification.
| Type 0 | NO CHANGES needed for either the femoral or tibial tunnels (i.e. one-stage) |
| Type 1 | One-stage revision, the femoral and/or tibial tunnels require new drilling |
| Type 1a | One-stage revision. Drill new femoral tunnel or OTT femur, keep tibial tunnel |
| Type 1b | One-stage revision. Drill new tibial tunnel, keep femoral tunnel |
| Type 1c | One-stage revision. Drill BOTH new femur or OTT AND new tibia |
| Type 2 | Two-stage revision is required for any or a combination of reasons (e.g. poorly placed tunnel(s), bone loss, infection, malalignment, etc.) |
| Type 2a | Two-stage revision. Any tunnel widening requiring bone grafting. |
| Type 2b | Two-stage revision. Other: Tunnel malalignment; Deficient secondary Restraints, etc.) |
OTT: Over-the-top approach
Figure 1.
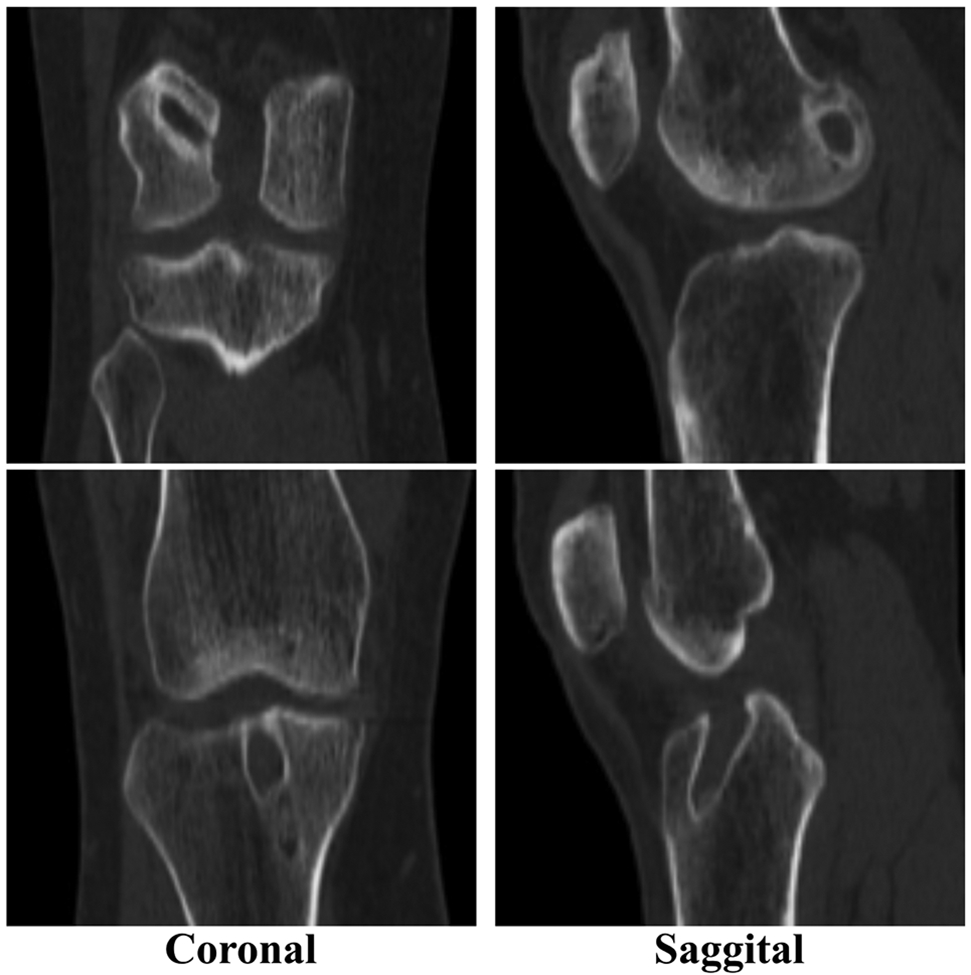
TYPE 1A: No change required to femoral or tibial index tunnels. Revision is one-stage, using same tunnels.
Figure 2.
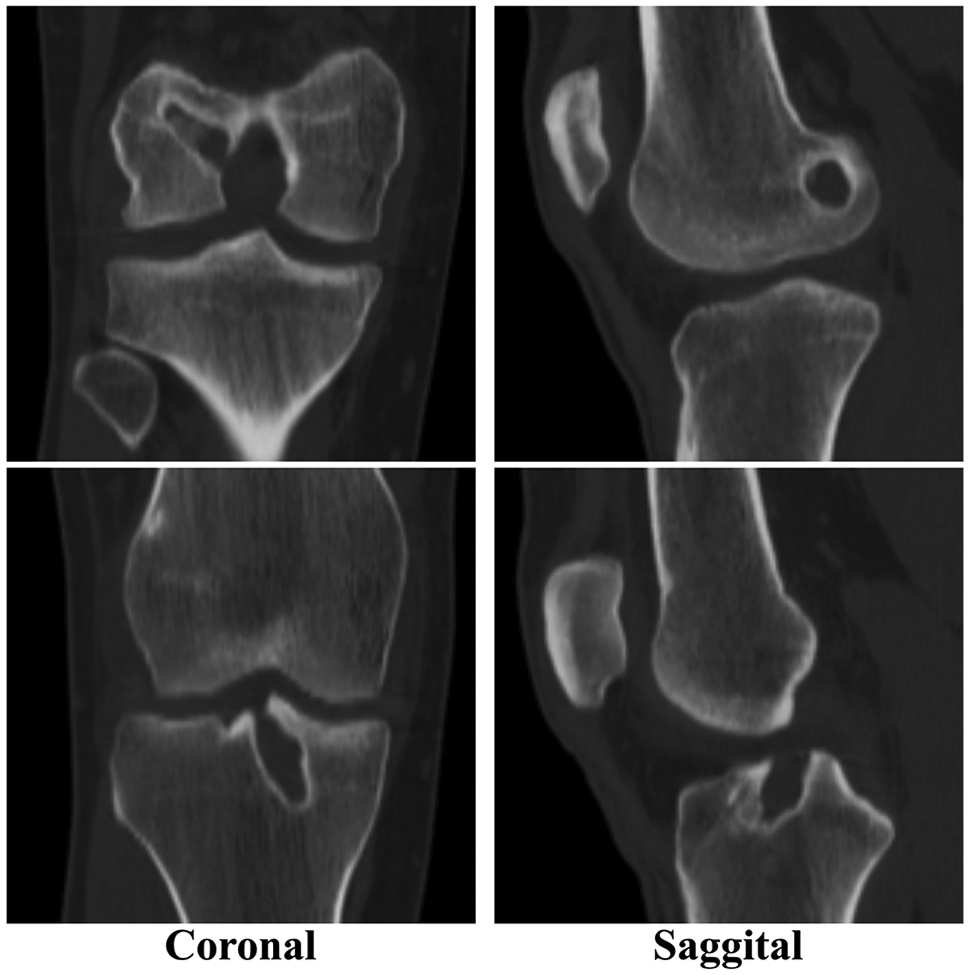
TYPE 1B, T: Tibial tunnel malposition. Femoral tunnel anatomic. Revision is one-stage, using new tibial tunnel and same femoral tunnel.
Figure 3.
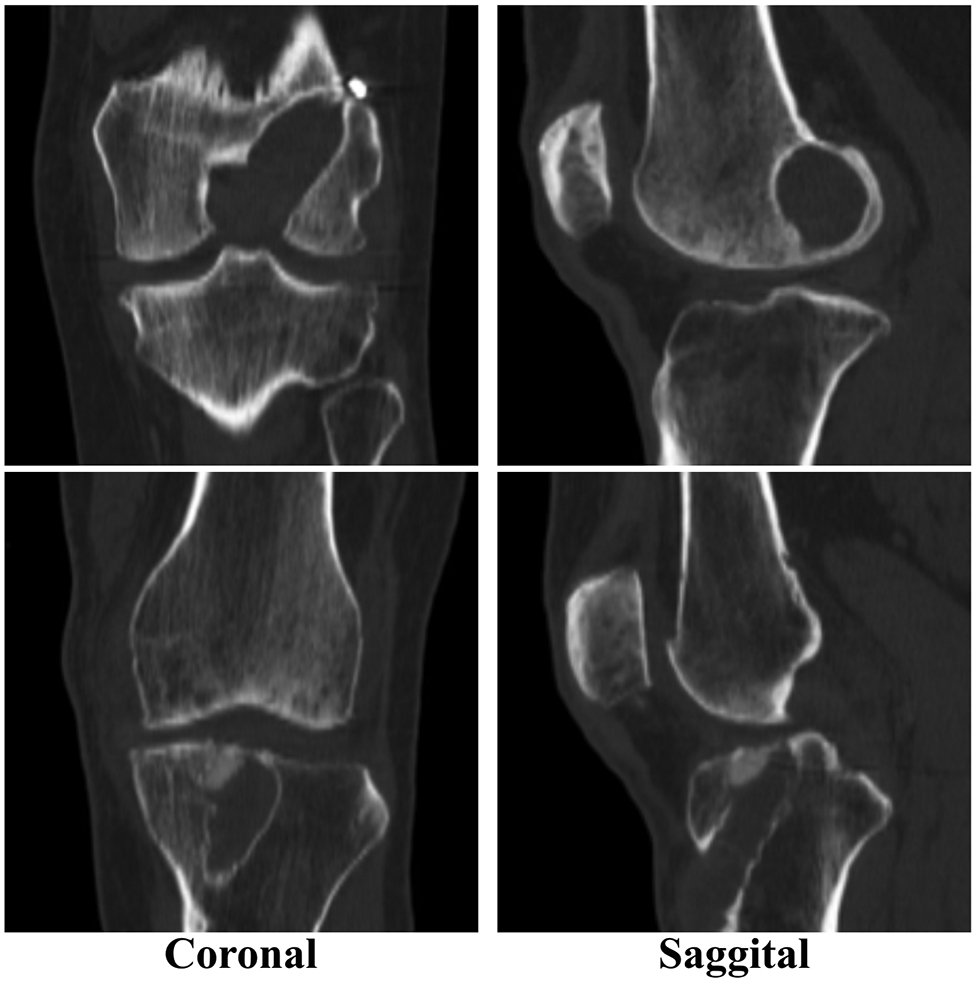
TYPE 2, FT: Both femoral and tibial tunnel widening. Revision is two-stage, requiring bone grafting of both tunnels as Stage 1.
The two-dimensional CT scan data of ten skeletally-mature patients independently presenting to the institution for consideration of revision ACL reconstruction were randomly selected by a member of the institutional research personnel, independent of the study team. These CT scan data were de-identified and separately uploaded as patient folders, accessible only to those with access to this secure link. Respondents only had access to the CT scan data, and were blinded to any patient history, physical examination, plain radiographic, magnetic resonance imaging, and arthroscopic data. Also included with access to this link, was a Microsoft Word document outlining the purpose of the study and the classification scheme, as well as links to download free versions of Digital Imaging and Communications in Medicine (DICOM) viewers for both Microsoft and Apple computer users. This allowed each respondent to independently view the de-identified patient scan images at their convenience, with a similar interface to what would be employed in their respective clinical environments.
A short survey was developed and administered to respondents, with the goal of capturing baseline demographic data including years in practice, number of primary and revision ACL procedures performed annually and clinical/technical preferences such as preferred technique(s) for ACL reconstruction, and diagnostic modalities employed for revision pre-operative planning. Answers to the brief survey and classification of each of the ten patients was entered electronically by each respondent into a secure database developed and administered by a member of the institutional research personnel, independent of the study team (Appendix 1). The database was established so that each respondent would be blinded to other respondent data and could only view and modify their personal entries. Each respondent was then personally contacted via electronic mail (e-mail) requesting to complete the survey using a unique identifier number. To increase response rate, reminder e-mails were sent at two week intervals17.
Statistical Analysis:
The Inter-class Correlation Coefficient (ICC) was used for multi-rater, inter-rater agreement to assess the level of agreement among the twelve reviewers concerning the classifications of the proposed system18. The REVISE Classification, which contains categorical data, used this statistical measure given its reported equivalence to weighted kappa analysis in this scenario18,19. Reliability analysis using IBM SPSS 25 was used to calculate the value and 95% confidence interval of the ICC for all twelve reviewers. The level of agreement was categorized prior to the beginning of the literature search using the Altman modification20 to the Landis and Koch21 ranges for ICC criteria: 0.00-0.20 indicating “poor”; 0.21-0.40 indicating “fair”; 0.41-0.60 indicating “moderate”; 0.61-0.80 indicating “good”; and 0.81-1.00 indicating “substantial”21. Within each individual patient case, statistical measures of agreement were not appropriate and agreement between reviewers was described descriptively for the classifications of the proposed system. Within each patient case, agreement and internal validity was further described within each subclass, as unknown to all study respondents, 60% of patient cases were performed by a single respondent surgeon.
RESULTS:
Respondent Demographics:
Twelve orthopaedic surgeons independently applied the classification to the CT scan data of ten patients presenting for revision ACL reconstruction. The respondents were in practice a mean 8.8 (range 6-18) years and reported annually performing a mean 78.5 (range 30-130) and 17.3 (range 5-30) primary and revision ACL reconstructions, respectively. The preferred technique for ACL reconstruction was anteromedial portal femoral tunnel drilling, selected by all respondents. With regards to preferred method(s) to assess technical errors with failed ACL reconstruction, plain radiographs (83.3%) and non-contrast MRI (75%) were the most preferred modalities, with 2D CT and contrast MRI occurring at frequencies of 41.7% and 8.3%, respectively. Interestingly, 66.7% of respondents used CT scans with 3D reconstruction images for pre-operative revision ACL planning and 0% of respondents used any 3D modeling modality for the review of study cases.
Inter-rater reliability:
Overall, the classification demonstrated an ICC [95% CI] of 0.92 [0.80, 0.98] suggesting “substantial” agreement between the twelve reviewers across all ten patients using all classification grades.
Observed Agreement:
Table 2 outlines the observed agreement between all twelve respondents on an individual case-by-case basis, as it pertains to both identifying the technical issue(s) requiring addressing in the revision, and the preferred strategy to manage it (one- or two-stage).
Table 2.
Comparison of the Observed Agreement Amongst Reviewers on a Case-by-Case Basis to Operative Data.
| CASE | % Agreement (Stage) |
% Agreement (Type) |
% Agreement (Sub-Type) |
|---|---|---|---|
| 1 |
One: 91.7 Two: 8.3 |
0: 75.0 1: 16.7 2: 8.3 |
1a: 50 1b: 50 2a: 100 |
| 2 | One: 0 Two: 100 |
0: 0 1: 0 2: 100 |
2a: 100 |
| 3 |
One: 50
Two: 50 |
0: 0 1: 50 2: 50 |
1a: 83.4 1c: 6.6 2a: 100 |
| 4 |
One: 83.3 Two: 6.7 |
0: 16.7 1: 66.7 2: 16.7 |
1a: 25.0 1b: 12.4 1c: 62.6 2a: 100 |
| 5 |
One: 91.7 Two: 8.3 |
0: 25 1: 66.7 2: 8.3 |
1a: 12.5 1b: 37.5 1c: 50.0 2b: 100 |
| 6 |
One: 75 Two: 25 |
0: 50 1: 25 2: 25 |
1a: 33.2 1b: 66.8 2a: 100 |
| 7 |
One: 91.7 Two: 8.3 |
0: 41.7 1: 50 2: 8.3 |
1a: 83.4 1b: 16.6 2a: 100 |
| 8 |
One: 91.7 Two: 8.3 |
0: 8.3 1: 83.3 2: 8.3 |
1c: 100 2b: 100 |
| 9 | One: 8.3 Two: 91.7 |
0: 0 1: 8.3 2: 91.7 |
1c: 100 2a: 100 |
| 10 |
One: 83.3 Two: 16.7 |
0: 75 1: 8.3 2: 16.7 |
1a: 100 2a: 100 |
Internal Validity:
Though unknown to all study respondents, 60% of the revision cases were treated by one of the study respondents to ascertain internal validity – that is, how closely the pre-operative classification agreed with the intra-operative decision. Interestingly, the treating surgeon’s intra-operative decision mirrored the assigned pre-operative REVISE Classification in five of six cases (83.3%); with the one differing case changing from a Type 1B, FT pre-operatively to Type 2 intra-operatively, after too significant tunnel osteolysis requiring a staged bone grafting procedure was determined post-diagnostic arthroscopic evaluation.
DISCUSSION:
The key findings of this study are that on a case-by-case basis, there exists high internal validity, and a high observed agreement across sports medicine fellowship-trained orthopaedic surgeons regarding how to manage previous ACL tunnels and whether to stage a revision ACL procedure. Across all revision ACL patients, the inter-rater agreement is “substantial” at 0.92 [0.80, 0.98] [95% CI], further suggesting that, despite different training backgrounds and revision philosophies22, the REVISE ACL Classification is useful and feasible for: identifying the technical issue causing failure; unifying surgeons on how to best manage the technical factor; and offering guidance on the optimal approach (one- or two-stage) for the revision procedure.
Revision ACL reconstruction poses many challenges, and is additionally complicated by outcomes that are consistently inferior compared to the index scenario9,23-25. Though several exhaustive definitions for what constitutes an ACL “failure” exist26,27, there remains no universally accepted definition8. From a technical standpoint, which arguably assumes the greatest responsibility (22-79%)3 for unsatisfactory outcomes post-index procedure, outcomes may be influenced by numerous factors, including but not limited to: tunnel position; tunnel widening and/or overlap; graft choice; graft fixation; coronal malalignment; increased posterior tibial slope; retained hardware; anterolateral complex injury; and concomitant/missed cruciate/collateral injury to name a few9. Therefore, identifying and understanding the relative contribution of each of these factors, to each individual patient, is of paramount importance to improve revision outcomes. To this end, REVISE focuses on those factors that are attributable to the majority of technical flaws in primary ACL reconstruction, namely tunnel position (70-80%)23,28 and widening5, and incorporates bone grafting as a two-stage option, given that it is nearly three times more commonly employed as a staged procedure for both the femur (8% versus 3%) and tibia (9% versus 3%)3.
It is important to note that, despite many published manuscripts on the ACL, there exists no evidence-based treatment algorithm for the primary or revision scenario. Nevertheless, in an era of increasing revision ACL procedures with no standardized method for grading, the REVISE ACL Classification represents the first attempt to identify the technical concerns requiring attention in revision ACL reconstruction, with suggested treatment guidance. Currently, the goal of ACL reconstruction is to perform one that is anatomic29 and individualized30, as has been the trend in recent years31,32. Though conceptually simple to understand, what constitutes “anatomic” is highly controversial, with some surgeons referring to direct visualization of native ligament insertion sites33; others to bony and/or soft tissue landmarks34; and still others to the number of bundles involved in reconstruction, the technique for femoral tunnel drilling, or some combination thereof. Moreover, the pre-operative imaging assessment of “anatomic” tunnel placement and “anatomic” tunnel [and inclination] angles35 varies widely, and has been described with reference to: radiographic quadrants36; Blumensatt’s line36; and/or a clock-face37, amongst others. Despite both these nuances of the “anatomic” term and its modifiers (semi-anatomic), and the fact that these guidelines are more difficult to appreciate in the revision setting, the REVISE ACL Classification still enabled primarily non-treating surgeons to substantially agree on whether or not femoral and/or tibial tunnel malposition existed. Therefore, the REVISE ACL Classification facilitates a more standardized revision ACL approach whilst remaining cognizant of important individual case differences.
REVISE has significant merit in that it allows for individual surgeon practice preferences, and still provides a novel system that going forwards, can categorize ACL revision procedures so that future outcomes studies can be analyzed with less heterogeneity. Interestingly, the literature suggests that the clinical results of revision Over-the-top (OTT) reconstructions, at least as measured by Lysholm scores, Lachman/pivot shift testing, and quantitative translation/rotational laxity; are “almost equivalent” to anatomical, single-bundle techniques38. While neither approach is necessarily incorrect, the literature does recommend a two-stage approach in cases where significant femoral tunnel widening and/or overlap exists8. Therefore, the additional value of the REVISE ACL Classification is that going forward, surgeons can communicate and standardize the “type” of revision procedure performed, so that, for example, patients who had non-anatomic OTT reconstructions are not pooled for analysis with those who used the original tunnels, even if performed as a one-stage, given the inherent differences in biomechanics and technique. The value of such standardization that REVISE further affords is illustrated Case 3, where 100% of the surveyed surgeons reported that the tibial tunnel was too wide, with 50% preferring to address the revision in one-stage using an Achilles tendon allograft with bone block, while the remaining half preferred to perform the revision in two-stages, with the first stage encompassing ACL graft debridement and bone grafting of the tunnel. Again, neither approach is necessarily incorrect, with the literature recommending a two-stage bone grafting procedure for unacceptable tunnels either due to overlap and/or widening greater than 16 mm wide5 or more than 100%35. However, no differences exist between one- and two-stage revision ACL procedures across the 12-item Short Form Health Survey (SF-12) Mental and Physical Component Summaries, Western Ontario and McMaster Universities Arthritis Index (WOMAC), Lysholm and Tegner active scale cores, or failure rates39. Though one-stage approaches are presumably the result a of a shared decision-making approach with the patient to limit operative time, and both the rehabilitation interval and risks of two surgical procedures, the fact that no difference exists between the staged approaches questions whether the risks of two separate procedures are more theoretical rather than a real clinical concern. Thus, in the absence of a “gold-standard” revision operation, REVISE respects this variability whilst still guiding practice.
For a classification to be useful, it is fundamental that it be feasible, and both valid and reliable40. Though REVISE has established feasibility, validity in this instance, represents the accuracy of the classification to describe the true pathologic process, often determined by comparison to a “gold-standard”40. In this case, the “gold-standard” involves the intra-operative arthroscopic evaluation. However, measuring validity in this instance is impractical, not only because of the difficulty in having all reviewers present to perform intra-operative assessments on a given patient (or view the arthroscopic video of the diagnostic evaluation); but also because those applying the classification herein were not necessarily the surgeon on record performing the revision procedure. Thus, in the absence of validity, reliability then becomes all the more important40. In addition, variability in the clinician, patient, and procedure can affect the reliability of a classification40. Though respondents were, by design, not provided with patient clinical data or specifics of the arthroscopic evaluation and/or final revision procedure to minimize the influence of the latter two factors, the REVISE ACL Classification still performed with substantial inter-rater reliability, despite the slight clinical variability.
It has not escaped notice that most classifications in orthopaedics are of low inter-rater reliability, and based on statistical analysis alone, deemed unacceptable40. REVISE, having feasibility tested on surgeons in academic and community settings, is generalizable as well. It is simple, easy to remember, and practical to communicate common challenges in revision ACL reconstruction that can be applied to clinical studies and research/epidemiological studies – the operative word being “common”. For example, REVISE is strengthened by excluding highly controversial revision ACL elements such as graft choice3, graft fixation41-43, infection3, “biologic” failures3, and when to consider the anterolateral structures44. Additional strengths include that it was tested using full CT scan data, not select cuts, and in doing so, improves upon the position-related limitations in assessing tunnel position and widening that can occur with plain radiograph use45,46, and is more encompassing and informative than previous femoral-side focused CT classifications47. This study also tests feasibility using CT modalities, given that it is the most accurate of methods, and one that is also more efficient and clinically appropriate35,48,49.
Limitations
In addition to a potential expertise bias that is introduced with having all respondents fellowship-trained, the main limitation of this classification, and any classification that aims to assess decision-making, remains in reconciling the potential difference in what a given surgeon states they would prefer to do, from what they do operatively. Moreover, there is a potential to underestimate the value of performing a re-alignment osteotomy in the revision setting, as CT scans are not the preferred modality for assessing coronal/sagittal limb malalignment. Lastly, it may be possible to perform bone grafting of tunnels as a one-stage procedure, using pre-made bone dowels, auto- or allograft bone chips, and/or a graft option with a large bone block, for example50. This was not included as a separate subsection in REVISE, given the focus group consensus to stage bone grafting based on literature3. As well, implied in a one-stage bone grafting procedure is the re-drilling of a new tunnel, which currently fits within the proposed schema. Statistically, the current study is a preliminary evaluation of the REVISE classification using a random sample of revision cases presenting to our institution and future studies will include increased numbers of patient cases to increase the power of future studies and external validity of the classification system. Nevertheless, future efforts encompass: epidemiological studies aimed at classifying all revision ACL procedures performed at this institution (and other registries) into appropriate categories to better understand the true prevalence of each ACL revision strategy and assess outcomes with less heterogeneity (i.e. investigating outcomes in Type 1A or 1B revision patients versus Type 2 for example, to better ascertain how an OTT revision compares to two-stage revision ACL procedures). Additional efforts will also aim to assess feasibility across other diagnostic modalities, such as MRI, 3D-MRI51, arthroscopic examination videos, and 3D printed models. This will be important going forwards to ascertain the need for CT in this classification based on its performance with other modalities, given the risks of radiation it entails. REVISE can also be applied prospectively to ascertain how the pre-operative classification correlates with the intra-operative decision (internal validity); in essence, investigating whether certain technical errors favor certain revision approaches. Lastly, though currently tested across orthopaedic surgeons, the hope is that this classification truly serves as a universal language, utilized by other medical specialties as well. To this end, future studies assessing REVISE’s inter-rater reliability amongst radiologists and across the aforementioned diagnostic modalities are planned. Having demonstrated feasibility, the authors anticipate that the REVISE ACL Classification will have wide applicability in the revision setting and lead to an enhanced understanding, both prospectively and retrospectively, of revision ACL challenges. REVISE does not function to establish a correct way to perform revision ACL reconstructions, but provides a common language that surgeons and researchers can use to appropriately classify revision ACL reconstruction to improve the consistency and external validity of future studies.
CONCLUSION:
The proposed REVISE ACL Classification, which employs CT scan analysis to both identify technical issues and guide revision ACL treatment strategy (one- or two-stage) constitutes a feasible and practical system with high internal validity, high observed agreement and substantial inter-rater agreement. Adoption of this classification, both clinically and in research, will help provide a universal language for orthopaedic surgeons to discuss these complex clinical presentations and help standardize an approach to diagnosis and treatment to improve patient outcomes.
LIST OF ABBREVIATIONS
- ACL
Anterior Cruciate Ligament
- CT
Computed Tomography
- ICC
Inter-class Correlation Coefficient
- MARS
Multicenter ACL Revision Study
- MRI
Magnetic Resonance Imaging
- DICOM
Digital Imaging and Communications in Medicine
- CI
Confidence Interval
- OTT
Over-the-top
- SF-12
Short Form Health Survey
- WOMAC
Western Ontario and McMaster Universities Arthritis Index
APPENDICES:
Appendix 1:
The REVision using Imaging to guide Staging and Evaluation (REVISE) in ACL Reconstruction Classification.
| Survey: | |
| DATE: | |
| 1. Sports-Medicine Fellowship Trained? | YES / NO |
| 2. Years in Independent Clinical Practice: | __________ |
| 3. Estimate of Number of Primary ACL Surgeries performed per year: | __________ |
4. Preferred Primary ACL Reconstruction Technique (check all that apply):
| |
| 5. Estimate of Number of Revision ACL Surgeries performed per year: | __________ |
6. Preferred Diagnostic Modality to Assess Technical Errors in ACL Reconstruction (check all that apply):
| |
| Classification: | |
| Type 1A – both femoral and tibial tunnels can be used in the revision as is; revision is one-stage | |
| Type 1B –the femoral and/or tibial tunnels require new drilling; revision is one-stage | |
| Type 1B, F: | One-stage revision. Drill new femoral tunnel/OTT femur, keep tibial tunnel |
| Type 1B, T: | One-stage revision. Drill new tibial tunnel, keep femoral tunnel |
| Type 1B, FT: | One-stage revision. Drill BOTH new femur/OTT AND new tibia |
| Type 2 – a two-stage revision is required for poorly placed tunnel(s), bone loss, infection, and obvious malalignment. | |
| Type 2, F: | Two-stage revision, Drill new femoral tunnel, keep tibial tunnel |
| Type 2, T: | Two-stage revision, Drill new tibial tunnel, keep femoral tunnel |
| Type 2, FT: | Two-stage revision, Drill BOTH new femoral and tibial tunnel. |
| Type 2, I: | Two-stage revision, complicated by infection. |
OTT: Over-the-top approach
REFERENCES:
- 1.Yabroudi MA, Björnsson H, Lynch AD, et al. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop. J. Sports Med 2016;4(9):2325967116666039. doi: 10.1177/2325967116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL. Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am. J. Sports Med 2015;43(10):2510–2514. doi: 10.1177/0363546515597664. [DOI] [PubMed] [Google Scholar]
- 3.MARS Group, Wright RW, Huston LJ, et al. Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am. J. Sports Med 2010;38(10):1979–1986. doi: 10.1177/0363546510378645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller MD, Thompson SR. Anterior Cruciate Ligament Injuries (Including Revision). In: DeLee & Drez’s Orthopaedic Sports Medicine. 4, revised ed. Elsevier Health Sciences; 2014:1149–1164. [Google Scholar]
- 5.Burnham JM, Herbst E, Pauyo T, et al. Technical considerations in revision anterior cruciate ligament (ACL) reconstruction for operative techniques in orthopaedics. Oper. Tech. Orthop 2017;27(1):63–69. doi: 10.1053/j.oto.2017.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gifstad T, Drogset JO, Viset A, Grøntvedt T, Hortemo GS. Inferior results after revision ACL reconstructions: a comparison with primary ACL reconstructions. Knee Surg. Sports Traumatol. Arthrosc 2013;21(9):2011–2018. doi: 10.1007/s00167-012-2336-4. [DOI] [PubMed] [Google Scholar]
- 7.Andriolo L, Filardo G, Kon E, et al. Revision anterior cruciate ligament reconstruction: clinical outcome and evidence for return to sport. Knee Surg. Sports Traumatol. Arthrosc 2015;23(10):2825–2845. doi: 10.1007/s00167-015-3702-9. [DOI] [PubMed] [Google Scholar]
- 8.Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of anterior cruciate ligament reconstruction. Arch Bone Jt Surg 2015;3(4):220–240. [PMC free article] [PubMed] [Google Scholar]
- 9.George MS, Dunn WR, Spindler KP. Current concepts review: revision anterior cruciate ligament reconstruction. Am. J. Sports Med 2006;34(12):2026–2037. doi: 10.1177/0363546506295026. [DOI] [PubMed] [Google Scholar]
- 10.Trojani C, Sbihi A, Djian P, et al. Causes for failure of ACL reconstruction and influence of meniscectomies after revision. Knee Surg. Sports Traumatol. Arthrosc 2011;19(2):196–201. doi: 10.1007/s00167-010-1201-6. [DOI] [PubMed] [Google Scholar]
- 11.Slattery C, Kweon CY. Classifications in brief: outerbridge classification of chondral lesions. Clin. Orthop. Relat. Res 2018. doi: 10.1007/s11999.0000000000000255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen JC, De Smet AA, Graf BK, Rosas HG. MR imaging-based diagnosis and classification of meniscal tears. Radiographics 2014;34(4):981–999. doi: 10.1148/rg.344125202. [DOI] [PubMed] [Google Scholar]
- 13.LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: a classification system based on tear morphology. Am. J. Sports Med 2015;43(2):363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 14.Buscayret F, Temponi EF, Saithna A, Thaunat M, Sonnery-Cottet B. Three-Dimensional CT Evaluation of Tunnel Positioning in ACL Reconstruction Using the Single Anteromedial Bundle Biological Augmentation (SAMBBA) Technique. Orthop. J. Sports Med 2017;5(5):2325967117706511. doi: 10.1177/2325967117706511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolf BR, Ramme AJ, Wright RW, et al. Variability in ACL tunnel placement: observational clinical study of surgeon ACL tunnel variability. Am. J. Sports Med 2013;41(6):1265–1273. doi: 10.1177/0363546513483271. [DOI] [PubMed] [Google Scholar]
- 16.Getelman MH, Schepsis AA, Zimmer J. Revision ACL Reconstruction: Autograft versus Allograft [abstract]. Arthroscopy 1995;11:378. [Google Scholar]
- 17.Sprague S, Quigley L, Bhandari M. Survey design in orthopaedic surgery: getting surgeons to respond. J. Bone Joint Surg. Am 2009;91 Suppl 3:27–34. doi: 10.2106/JBJS.H.01574. [DOI] [PubMed] [Google Scholar]
- 18.Fleiss JL, Cohen J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas 1973;33(3):613–619. doi: 10.1177/001316447303300309. [DOI] [Google Scholar]
- 19.Carey JL, Wall EJ, Grimm NL, et al. Novel arthroscopic classification of osteochondritis dissecans of the knee: A multicenter reliability study. Am. J. Sports Med 2016;44(7):1694–1698. doi: 10.1177/0363546516637175. [DOI] [PubMed] [Google Scholar]
- 20.Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall; 1991. [Google Scholar]
- 21.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- 22.Noyes FR, Barber-Westin SD. Anterior cruciate ligament revision reconstruction: results using a quadriceps tendon-patellar bone autograft. Am. J. Sports Med 2006;34(4):553–564. doi: 10.1177/0363546505281812. [DOI] [PubMed] [Google Scholar]
- 23.Kamath GV, Redfern JC, Greis PE, Burks RT. Revision anterior cruciate ligament reconstruction. Am. J. Sports Med 2011;39(1):199–217. doi: 10.1177/0363546510370929. [DOI] [PubMed] [Google Scholar]
- 24.Wright RW, Dunn WR, Amendola A, et al. Anterior cruciate ligament revision reconstruction: two-year results from the MOON cohort. J. Knee Surg 2007;20(4):308–311. [DOI] [PubMed] [Google Scholar]
- 25.Wright RW, Gill CS, Chen L, et al. Outcome of revision anterior cruciate ligament reconstruction: a systematic review. J. Bone Joint Surg. Am 2012;94(6):531–536. doi: 10.2106/JBJS.K.00733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Noyes FR, Barber-Westin SD. Revision anterior cruciate surgery with use of bone-patellar tendon-bone autogenous grafts. J. Bone Joint Surg. Am 2001;83-A(8):1131–1143. [DOI] [PubMed] [Google Scholar]
- 27.Alford JW, Bach BR. Arthrometric aspects of anterior cruciate ligamentsurgery before and after reconstruction with patellar tendon grafts. Tech Orthop 2005;20(4):421–438. [Google Scholar]
- 28.Garofalo R, Djahangiri A, Siegrist O. Revision anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. Arthroscopy 2006;22(2):205–214. doi: 10.1016/j.arthro.2005.08.045. [DOI] [PubMed] [Google Scholar]
- 29.Fu FH, van Eck CF, Tashman S, Irrgang JJ, Moreland MS. Anatomic anterior cruciate ligament reconstruction: a changing paradigm. Knee Surg. Sports Traumatol. Arthrosc 2015;23(3):640–648. doi: 10.1007/s00167-014-3209-9. [DOI] [PubMed] [Google Scholar]
- 30.van Eck CF, Widhalm H, Murawski C, Fu FH. Individualized anatomic anterior cruciate ligament reconstruction. Phys. Sportsmed 2015;43(1):87–92. doi: 10.1080/00913847.2015.1005545. [DOI] [PubMed] [Google Scholar]
- 31.Fu FH, Shen W, Starman JS, Okeke N, Irrgang JJ. Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am. J. Sports Med 2008;36(7):1263–1274. doi: 10.1177/0363546508314428. [DOI] [PubMed] [Google Scholar]
- 32.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am. J. Sports Med 2007;35(2):223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 33.van Eck CF, Schreiber VM, Mejia HA, et al. “Anatomic” anterior cruciate ligament reconstruction: a systematic review of surgical techniques and reporting of surgical data. Arthroscopy 2010;26(9 Suppl):S2–12. doi: 10.1016/j.arthro.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Ferretti M, Doca D, Ingham SM, Cohen M, Fu FH. Bony and soft tissue landmarks of the ACL tibial insertion site: an anatomical study. Knee Surg. Sports Traumatol. Arthrosc 2012;20(1):62–68. doi: 10.1007/s00167-011-1592-z. [DOI] [PubMed] [Google Scholar]
- 35.Illingworth KD, Hensler D, Working ZM, Macalena JA, Tashman S, Fu FH. A simple evaluation of anterior cruciate ligament femoral tunnel position: the inclination angle and femoral tunnel angle. Am. J. Sports Med 2011;39(12):2611–2618. doi: 10.1177/0363546511420128. [DOI] [PubMed] [Google Scholar]
- 36.Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. Am. J. Knee Surg 1997;10(1):14–21; discussion 21. [PubMed] [Google Scholar]
- 37.Amis AA, Beynnon B, Blankevoort L, et al. Proceedings of the ESSKA scientific workshop on reconstruction of the anterior and posterior cruciate ligaments. Knee Surg. Sports Traumatol. Arthrosc 1994;2(3):124–132. [DOI] [PubMed] [Google Scholar]
- 38.Usman MA, Kamei G, Adachi N, Deie M, Nakamae A, Ochi M. Revision single-bundle anterior cruciate ligament reconstruction with over-the-top route procedure. Orthop. Traumatol. Surg. Res 2015;101(1):71–75. doi: 10.1016/j.otsr.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 39.Mitchell JJ, Chahla J, Dean CS, Cinque M, Matheny LM, LaPrade RF. Outcomes After 1-Stage Versus 2-Stage Revision Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med 2017;45(8):1790–1798. doi: 10.1177/0363546517698684. [DOI] [PubMed] [Google Scholar]
- 40.Garbuz DS, Masri BA, Esdaile J, Duncan CP. Classification systems in orthopaedics. J Am Acad Orthop Surg 2002;10(4):290–297. [DOI] [PubMed] [Google Scholar]
- 41.Watson JN, McQueen P, Kim W, Hutchinson MR. Bioabsorbable interference screw failure in anterior cruciate ligament reconstruction: A case series and review of the literature. Knee 2015;22(3):256–261. doi: 10.1016/j.knee.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 42.Mayr R, Heinrichs CH, Eichinger M, Coppola C, Schmoelz W, Attal R. Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am. J. Sports Med 2015;43(6):1380–1385. doi: 10.1177/0363546515574062. [DOI] [PubMed] [Google Scholar]
- 43.Papalia R, Vasta S, D’Adamio S, Giacalone A, Maffulli N, Denaro V. Metallic or bioabsorbable interference screw for graft fixation in anterior cruciate ligament (ACL) reconstruction? Br Med Bull 2014;109:19–29. doi: 10.1093/bmb/ldt038. [DOI] [PubMed] [Google Scholar]
- 44.Musahl V, Getgood A, Neyret P, et al. Contributions of the anterolateral complex and the anterolateral ligament to rotatory knee stability in the setting of ACL Injury: a roundtable discussion. Knee Surg. Sports Traumatol. Arthrosc 2017;25(4):997–1008. doi: 10.1007/s00167-017-4436-7. [DOI] [PubMed] [Google Scholar]
- 45.Mahajan PS, Chandra P, Ahamad N, Hussein SA. Effects of extremity positioning on radiographic evaluation of femoral tunnel location with digitally reconstructed femoral lateral radiographs after anterior cruciate ligament reconstruction. BMC Med. Imaging 2015;15:47. doi: 10.1186/s12880-015-0093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Eck CF, Wong AK, Irrgang JJ, Fu FH, Tashman S. The effects of limb alignment on anterior cruciate ligament graft tunnel positions estimated from plain radiographs. Knee Surg. Sports Traumatol. Arthrosc 2012;20(5):979–985. doi: 10.1007/s00167-011-1683-x. [DOI] [PubMed] [Google Scholar]
- 47.Magnussen RA, Debieux P, Benjamin B, et al. A CT-based classification of prior ACL femoral tunnel location for planning revision ACL surgery. Knee Surg. Sports Traumatol. Arthrosc 2012;20(7):1298–1306. doi: 10.1007/s00167-011-1814-4. [DOI] [PubMed] [Google Scholar]
- 48.Forsythe B, Kopf S, Wong AK, et al. The location of femoral and tibial tunnels in anatomic double-bundle anterior cruciate ligament reconstruction analyzed by three-dimensional computed tomography models. J. Bone Joint Surg. Am 2010;92(6):1418–1426. doi: 10.2106/JBJS.I.00654. [DOI] [PubMed] [Google Scholar]
- 49.Amis AA, Jakob RP. Anterior cruciate ligament graft positioning, tensioning and twisting. Knee Surg. Sports Traumatol. Arthrosc 1998;6 Suppl 1:S2–12. doi: 10.1007/s001670050215. [DOI] [PubMed] [Google Scholar]
- 50.Werner BC, Gilmore CJ, Hamann JC, et al. Revision Anterior Cruciate Ligament Reconstruction: Results of a Single-stage Approach Using Allograft Dowel Bone Grafting for Femoral Defects. J Am Acad Orthop Surg 2016;24(8):581–587. doi: 10.5435/JAAOS-D-15-00572. [DOI] [PubMed] [Google Scholar]
- 51.Hart A, Sivakumaran T, Burman M, Powell T, Martineau PA. A Prospective Evaluation of Femoral Tunnel Placement for Anatomic Anterior Cruciate Ligament Reconstruction Using 3-Dimensional Magnetic Resonance Imaging. Am. J. Sports Med 2018;46(1):192–199. doi: 10.1177/0363546517730577. [DOI] [PubMed] [Google Scholar]


