Abstract
Objectives
COVID-19 has varied clinical manifestations, from asymptomatic to severe cases, and conjunctivitis is one of them, but sometimes a lone initial symptom is found to be present. The aim of this study was to identify the prevalence of conjunctivitis as the first symptom in COVID-19 patients in a primary healthcare unit.
Methodology
A retrospective study was conducted, analyzing the presenting complains/symptoms and results of COVID-19-confirmatory tests.
Results
Out of the 672 cases that were sent for RT-PCR testing, only 121 (18%) were found to be positive. Among these, 2.67% patients had both conjunctivitis and COVID-19, 77.77% patients had unilateral eye affected, while 22.22% had bilateral conjunctivitis of varying degrees. Fifteen patients diagnosed to have both acute conjunctivitis and COVID-19 presented other symptoms associated with COVID-19 infection. Three patients had only acute conjunctivitis during their entire course of COVID-19.
Conclusions
Conjunctivitis is a symptom of COVID-19 and may be the first sign of the infection, until the onset of the classical manifestations; such patients may continue to be a viral reservoir. Physicians should not miss unilateral conjunctivitis as it can be the only presenting complaint of COVID-19 during the initial phase, which might worsen if undetected and can aid in the spread of the contagion.
Keywords: Corona virus disease-2019, Conjunctivitis, Prevalence
Highlights of the Study
Conjunctivitis can be a lone feature of COVID-19 and can be easily missed by healthcare professionals.
This study could help physicians check for the presence of COVID-19 in patients presenting with conjunctivitis.
Early detection of asymptomatic spreaders of COVID-19 is quite important to control the spread.
Introduction
The World Health Organization (WHO) declared a global pandemic on March 11, 2020, and named the new disease “Corona Virus Disease 2019” (COVID-19) and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Positive cases went on surging high, reaching as many as 113,076,707, in a short timeframe (December 2019–February 2020) as reported by the WHO; India reported 11,079,979 positive cases (9.79% of the world total) [1].
A wide range of clinical manifestations have been documented from severe respiratory dysfunction, gastrointestinal, neurological, and dermatological affections to a mild ocular involvement [2, 3]. The most frequent symptom reported is the presence of fever in approximately 97% of the cases, followed by other major clinical manifestations such as dry cough, dyspnea, headache, pneumonia, malaise, and myalgia. The severe form of SARS-CoV-2 disease is characterized by a hypercoagulation state, pneumonia, and acute respiratory distress syndrome, due to which elective surgical procedures are postponed [4, 5]. Olfactory and taste alterations, such as anosmia and ageusia, were reported in many clinical studies [6] and were used by many to get an idea of whether they are infected or not as testing is quite expensive in many countries, especially in the absence of specific symptoms.
Ocular involvement was mentioned by several studies, while some studies reported acute conjunctivitis being the first and lone ocular symptom found in a few of the entirely asymptomatic positive COVID-19 cases [7, 8, 9, 10]. Among the travelers of the Diamond Princess ship found to be positive with this devastating virus, 1 patient was reported to have ocular involvement along with lymph node enlargement at the periauricular and submaxillary region [11]. Similarly, a case report from Argentina stated that conjunctivitis was the initial symptom, and within hours, other systemic symptoms appeared in this patient [12].
Conjunctivitis is not considered among the common symptoms as its prevalence ranges between 0.8 and 31.6% of positive cases [8]. Increased incidence of conjunctivitis was noted by Wu et al. [8]. The symptoms frequently seen in COVID-19-related conjunctivitis patients were conjunctival hyperemia, epiphora, and photophobia. Conjunctivitis may be explained by virus entering the tears from small, contaminated air droplets and reaching the conjunctival surface. Two elements were observed to be involved in the infection, angiotensin-converting enzyme 2 (ACE2) receptors and the serine protease TMPRSS2. One study showed that SARS-CoV-2 binds to the human ACE2 receptors using the serine protease TMPRSS2 in order to enter the respiratory epithelium [13]. Current studies report the existence of ACE2 receptors in the normal conjunctiva, but none of them confirm the presence of serine protease [14]. From the ocular surface, the virus passes through the nasolacrimal duct into the nose, entering the respiratory and gastrointestinal tract [15]. Lai et al. [13] reported that during viremia, coronavirus could be secreted in tears via the eccrine glands. The aim of this study was to identify the prevalence of conjunctivitis in COVID-19 patients and to detect its incidence as the first lone symptom related to SARS-CoV-2 infection, which might help in early detection of the virus, prior to the development of the serious complications of the disease.
Methodology
Subjects
A retrospective study was conducted on the records of patients who presented for a wide variety of issues (health problems, regular follow-ups, fitness certificates, etc.) during the period May 2020–February 2021, at Shreeji Clinic, India. During this period, 2,037 cases were reported out of which 672 (32.98%) cases were sent for nasopharyngeal swab RT-PCR testing for detecting a possible COVID-19 infection. A majority of these were asymptomatic but had to undergo testing in order to get fitness certificates for jobs/school/travel purposes and hence presented to the clinic for being tested on request. Around one-third of the patients (N = 229, 34.07%) presented to the clinic due to mild to moderate symptoms (e.g., fever, loss of smell and taste, diarrhea, sore throat, coughing, arthralgia, myalgia, etc.), which might be suggestive of a possible SARS-CoV-2 infection or prior to getting hospitalized for different planned surgeries/delivery/pathologies unrelated to COVID-19, to prove negative for acceptance in hospitals. These 672 persons included those presenting with ophthalmological problems suggestive of conjunctivitis, keeping in mind the possibility of COVID-19 virus being the causative agent. Diagnosis of conjunctivitis was made clinically. Signs and symptoms suggesting unilateral or bilateral conjunctivitis were pink discoloration or redness of the sclera, swelling of the conjunctiva/eyelids, crusting of the eyelids or lashes − especially in the morning, and watery or thick discharge − teary eye, foreign body sensation, itching, irritation, and burning sensation. All previously diagnosed/cured patients of SARS-CoV-2 infection or of conjunctivitis were excluded from the study and hence including only the new cases for this case-control study. As a part of routine procedure, informed written consent forms stating that the data can be used for future medical research purpose were signed by each patient at the time of presentation to the clinic.
Statistical Analysis
Medical data were extracted from the patients' medical records, and their information on symptoms, test results, clinical outcomes, treatment, and recovery details were analyzed statistically to draw results. Statistical analysis was performed using R software version 3.6.2 [16]. Means and standard deviations were computed. The statistical difference between the 2 study groups was tested using the unpaired t test for continuous variables. For categorical data, contingency tables and χ2 were used. Odds ratios were computed to quantify the risk. Logistic regression analysis was performed to model the presence of conjunctivitis as the first symptom in COVID-19-positive patients according to age, gender, need for hospitalization, and severity of COVID-19 infection, taking as reference asymptomatic COVID-19 patients.
Patients diagnosed positive for coronavirus were placed on 14 days' home quarantine, and their medical follow-up was performed over the phone/Zoom. Patients presenting moderate to severe symptoms of SARS-CoV-2 infection were transferred to hospital by state ambulance services having onboard medical staff wearing personal protective equipment.
Results
Out of the 672 persons who were referred by the clinic for RT-PCR testing for COVID-19, 121 (18%) cases were found to be positive. A total of 27 (4.01%) patients had findings (conjunctival hyperemia, epiphora, foreign body sensation, and inferior palpebral conjunctival follicles, for which they had presented to the clinic) suggesting acute conjunctivitis, from which 18 (14.87%) cases were from the COVID-19-positive group of patients, while remaining 9 (1.63%) cases having acute conjunctivitis, tested negative, as per the RT-PCR test results obtained, as shown in Tables 1 and 2.
Table 1.
Demographic and clinical characteristics for the patients in the 2 study groups
| Variables | COVID-19 with conjunctivitis as the initial symptom, % | COVID-19 without conjunctivitis as the initial symptom, % | p value | OR crude (0.95 CI) |
|---|---|---|---|---|
| Age, years | ||||
| Mean ± SD | 40.56±10.25 | 40.08±13.2 | 0.89 | |
| (Range) | (22–63) | (19–78) | ||
| Gender (male/female) | 12/6 | 57/46 | 0.52 | 1.59 (0.56–4.97) |
| COVID-19 severity | ||||
| Asymptomatic | 3 | 31 | 0.38 | 0.48 (0.1–1.62) |
| Mild | 7 | 42 | 0.99 | 0.93 (0.31–2.57) |
| Moderate | 6 | 22 | 0.42 | 1.85 (0.58–5.43) |
| Severe | 2 | 8 | 0.99 | 1.55 (0.2–7.12) |
| Hospitalization (yes/no) | 2/16 | 15/88 | 0.98 | 0.77 (0.1–3.18) |
OR, odds ratio; SD, standard deviation.
Table 2.
The result of logistic regression to model the probability of conjunctivitis as the initial symptom in COVID-19 patients using as predictors: age, gender, severity of COVID-19 infection, and need for hospitalization
| Characteristic | Estimate sth | Error | Z value | Pr(>|z|) |
|---|---|---|---|---|
| Intercept | −19.17 | 1,483 | −0.013 | 0.9897 |
| Age | −0.0073 | 0.0271 | −0.271 | 0.7866 |
| Gender (female) | 0.6303 | 0.5618 | 1.122 | 0.2619 |
| Mild COVID-19 infection | 0.6452 | 0.7534 | 0.856 | 0.3918 |
| Moderate COVID-19 infection | 1.567 | 0.8317 | 1.884 | 0.0596 |
| Severe COVID-19 infection | 17.79 | 1,483 | 0.012 | 0.9904 |
| Hospitalization | 16.65 | 1,483 | 0.011 | 0.9910 |
We used male gender and asymptomatic COVID-19 infection as the reference.
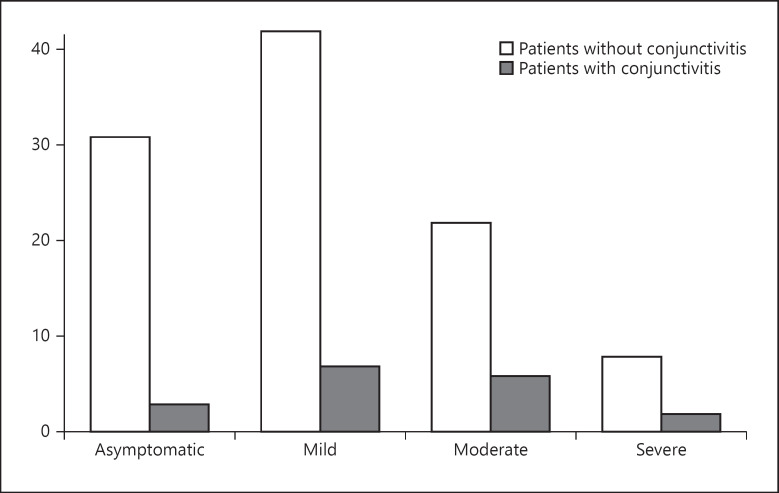
Among the patients who had both conjunctivitis and COVID-19 (N = 18, 14.88%), 12 (66.6%) were males and 6 (33.3%) females. Fourteen (77.77%) patients had unilateral eye affected, while 4 (22.22%) suffered from bilateral conjunctivitis of varying degrees. Only 2 (13.33%) patients presented with slight discoloration of the toes with mild discomfort along with conjunctivitis and COVID-19 infection. During the 14-day home quarantine period, the general medical condition of 2 patients (13.33%) deteriorated, and they were transferred to the hospital, while other 16 (88.88%) cases recovered well at home as shown in Figures 1 and 2. Among the 9 (1.33%) non-COVID-19 patients who had conjunctivitis, 8 had the bacterial form of conjunctivitis, while 1 patient had the viral form not related to the COVID-19 contagion.
Fig. 1.
The comparision of levels of severity of COVID-19 symptoms among the patients with or without conjunctivitis.
Fig. 2.
Flow-chart showing evolution of patients consulted in the clinic..
Palpable preauricular lymph nodes were identified in 3 (16.66%) patients and palpebral edema in 2 (11.11%) of the 18 COVID-19-positive patients. The onset of conjunctivitis was 1–2 days before presenting to the clinic. None of the patients presented decreased visual acuity, involvement of the cornea, or anterior chamber inflammation. Two of the 18 (11.1%) COVID-19-positive patients with mild conjunctivitis had refractive errors and were wearing permanent glasses. The other 16 (88.88%) patients had a best-corrected visual acuity of 6/6 as documented in their previous health records. Sixteen of the 18 (88.88%) patients presented mild to moderate acute conjunctivitis, except 2, who had severe form of conjunctivitis right since the beginning, when they presented to the clinic. A total of 15 patients (83.33%) presented with other symptoms associated with COVID-19 infection in the latter course of their disease, while 3 (16.66%) had solely conjunctivitis, which proves the fact that conjunctivitis can be the lone presenting feature of SARS-CoV-2 infection. Two patients (13.33%) with severe conjunctivitis and COVID-19-positive, after 6–8 days from the initial medical examination, required hospitalization due the development of severe systemic symptoms such as high fever, decreased oxygen saturation, and myalgia.
The demographic and clinical characteristics for the patients in the 2 study groups are shown in Table 1. There was no significant statistical difference concerning age, gender, and severity of COVID-19 infection between the patients presenting conjunctivitis as the initial symptom and the control group. The logistic regression confirmed these observations since none of these variables was found to be statistically significant.
The 18 patients with conjunctivitis received local treatment with antiviral eye drops (in most cases Ribavirin eye drops) 4 times per day for 7–14 days, depending on the progression of conjunctivitis. Artificial tears were recommended in order to increase ocular comfort, but due to financial issues, only 1 patient was able to afford them. After the 2 weeks of quarantine, 4 (22.2%) of the patients were still presenting conjunctival hyperemia with no other symptoms but were found to be COVID-19-negative on getting retested. The remaining 14 (77.7%) patients had no more symptoms after 8–10 days of local treatment.
Two male patients (11.1%), both having moderate conjunctivitis, aged 22 and 35 years, presented slight discoloration of the toes with mild discomfort. None of these 2 patients reported history of local trauma, foot and skin problems, exposure to extreme temperature, allergies, intake of medication, smoking history, or systemic diseases. The toes manifestations appeared after 4–6 days from the onset of conjunctivitis, and it was self-limiting in nature, having complete disappearance in approximately 6–8 days, without any local treatment. Neither of the 2 patients underwent examination by a dermatologist or an ophthalmologist due to the lack of resources (both financial and medical professional staff in the vicinity). Some ophthalmological consultations were arranged for few patients, by the clinic via telemedicine, which unfortunately cannot be considered to be as efficient as regular physical eye examinations. As all of the patients complained only of the conjunctivitis symptoms, with no alteration of the visual acuity, ophthalmoscopy exam was not considered as mandatory, especially in the pandemic era. Among the RT-PCR-positive patients, only 3 developed acute conjunctivitis later in the course of their disease; this indicates that conjunctivitis can appear even in the later phase, and initially, the typical symptoms might be witnessed.
Discussion
This study focused on ascertaining the prevalence of SARS-CoV-2 infection in patients suffering from conjunctivitis. A similar larger cohort study concluded that conjunctivitis may be diagnosed in 1 of 10 patients with SARS-CoV-2 infection being in female an early symptom of the disease [17]. A Japanese study reported that 30% of the COVID-19-positive persons were asymptomatic, which can increase the transmissibility rates immensely, if undetected [18]. Due to the high transmissibility index, through small droplets reaching the conjunctival layer of eyes, the use of gloves, eye glasses, and face shields are made mandatory in medical units worldwide, especially when consulting COVID-19-nontested individuals [19]. Proper protective equipment have become mandatory in hospitals for all staff members coming in contact to the positive cases, which provide adequate protection also for the eyes.
In our study, out of 27 patients with conjunctivitis, 18 (66.6%) were confirmed positive for COVID-19. Among the 18 patients, 12 (66.6%) were males and 6 (33.3%) females. Fourteen from the 18 (77.7%) patients presented with unilateral conjunctivitis. The clinical manifestations consisted in conjunctival hyperemia, epiphora, foreign body sensation, and inferior palpebral conjunctival follicles present in all 18 patients. A study performed in Hubei Province, China, on 38 patients with clinically confirmed SARS-CoV-2 infection reported 12 cases of conjunctivitis (31.6%) of which 2 (16.7%) were positive for COVID-19 RT-PCR from nasopharyngeal and conjunctival swabs. One of the 12 patients described epiphora as the first manifestation of SARS-CoV-2 disease [8]. Due to financial limitations none of the patients in our study were sent for conjunctival swab testing, which might have thrown more light to the existing details and can be considered as one of the limitations of this study. In another study, 35 of 301 patients (11.6%) with the RT-PCR test from nasopharyngeal swab for SARS-CoV-2 were diagnosed with acute conjunctivitis. Conjunctivitis was unilateral in 19 of the 35 cases (54.29%) unlike other viral conjunctivitis which usually is found to be bilateral [17]. Bilateral acute follicular conjunctivitis was reported in young males on day 13 from the first symptom of COVID-19 confirmed by positive conjunctival swabs RT-PCR for SARS-CoV-2. Conjunctival swab RT-PCR tests became negative after topical treatment with ribavirin four times per day for less than a week. Another study observed that conjunctivitis was diagnosed more frequently in males with moderate COVID-19 symptoms and in females with mild clinical manifestations. The same study underlined the case of a couple, both COVID-19-positive, with similar clinical severity scale, but with conjunctivitis being diagnosed only in the female, questioning the appearance of the ocular symptom depending on the host characteristics or mechanism of inoculation.
Wu et al. [8] reported conjunctival manifestations such as chemosis, epiphora, and local hyperemia in one-third of the COVID-19 patients, mostly in severe systemic disease [20]. In another study, conjunctival hyperemia was mild in 28 (80%) of the cases and moderate to severe in 7 (20%). Fifteen of the patients (42.8%) claimed tearing and 12 (34.2%) foreign body sensation. Moderate mucopurulent discharge was reported in 18 (54.5%) of the patients [17]. Contrary to this observation, in our study, no mucopurulent discharge was observed nor subconjunctival hemorrhages, membranes, and pseudo membranes were seen. Similar results were reported by a study after 72 h of medical follow-up [8, 17]. Pseudomembranous and hemorrhagic conjunctivitis were reported in the medical literature at 19 days after the onset of COVID-19 symptoms with improvement of the ocular manifestation from day 21 to day 26 [21]. None of the 18 patients included in our study presented decrease of the visual acuity or involvement of the cornea. Kerato-conjunctivitis was reported as initial clinical manifestation of a patient with COVID-19 [22].
A meta-analysis of 1167 COVID-19 patients reported that the severe form of COVID-19 might be associated with conjunctivitis [23]. A study from Italy reported that one female and four middle-aged males were diagnosed with viral conjunctivitis. Due to their recent travel history to Lombardy, known for high rates of COVID-19 infection, a nasopharyngeal swab was performed. RT-PCR confirmed the SARS-CoV-2 virus infection. During the 2-week self-quarantine, none of the 5 patients presented other symptoms such as fever, respiratory difficulties, or general malaise [24]. In our study, among the 18 patients with conjunctivitis, two presented severe manifestations requiring hospitalization.
During the 14-day quarantine, two of our 18 patients, aged 22 and 35 years, reported slight discoloration of the toes with mild discomfort. No treatment was required. Chilblains were observed in adolescents and young adults with no or mild COVID-19. The same study performed tests as anti-SARS-CoV/SARS CoV-2 immunostaining on skin biopsy that confirmed the presence of the virus [25]. The presence of chilblains could be a local cutaneous expression of type 1 interferon that induces early viral control. According to researchers, the presence of type 1 interferon would explain the association of conjunctivitis, COVID toe, and mild COVID-19 severity scale [26, 27]. An Italian study observed cutaneous manifestations in 18 of the 88 hospitalized COVID-19 patients. A female case from Ciudad Real, confined home for 2 weeks, observed red-violet lesions on the foot. Several days later, the patient experienced COVID-19 symptoms and tested positive. In addition to the classic clinical manifestation of COVID-19, the patient complained of dry eyes and pain in the feet [28].
Our study has several limitations such as the absence of a detailed ophthalmic examination, the patients being evaluated by primary care physicians, and guidance was provided via telemedicine by an ophthalmologist in only some cases. Second, RT-PCR was not performed on the tears and conjunctival secretions; thus, there was no direct confirmation of association between conjunctivitis and COVID-19. Studies have reported that in some cases, COVID-19 patients with conjunctivitis have negative RT-PCR results from conjunctival sac swabs, while positive SARS-CoV-2 nucleic acid tests are found in subjects with no ocular manifestation [15].
In other cases, an extremely low rate of positive SARS-CoV-2 RT-PCR is reported in tears and conjunctival secretions from patients confirmed with COVID-19 infection [8]. These findings suggest an underestimated prevalence of conjunctivitis, probably due to false-negative laboratory test results. A study reported the comparison of the viral load found in the plasma and in the tracheal aspirate of COVID-19-positive patients [29]. Eye manifestations can either be due to a direct infection or as a manifestation of systemic inflammatory disease in case COVID-19, as stated by L. Chen et al., in his study [29].
An Indian medical report presented 2 cases of unilateral conjunctivitis, associated in one of them with both nasopharyngeal and conjunctival swabs positive for SARS-CoV-2 RT-PCR tests. This medical report was the first to mention a positive conjunctival swabs test in the absence of other COVID-19 symptoms in India [30]. The lack of systemic COVID-19 symptoms may increase the spread of the virus from the patients with lone conjunctivitis if undiagnosed. A limitation of the present study is also the relatively low number of patients.
Conclusions
The aim of the study was to highlight the incidence rate of SARS-CoV-2 in conjunctivitis cases, in order not to underestimate the prevalence of COVID-19 in an area with restrictive measures and lack of ophthalmological consultations. Conjunctivitis can be the first symptom of COVID-19 infection. It can constitute a unique clinical manifestation or can be associated with other symptoms appearing within the 1-week period. Therefore, in cases of acute conjunctivitis, it is important to perform a SARS-CoV-2 RT-PCR test, for an early detection of infection. Due to the high transmissibility through small droplets reaching the conjunctiva, the use of gloves, eye glasses, and face shields should be highly be encouraged and made mandatory in medical units, where the exposure rates are immensely high. Conjunctivitis should never be neglected as it might be an early or lone symptom of a possible COVID-19 infection, which if left undiagnosed can aid in increasing the spread of the virus. Local authorities should ensure that lockdown measures and quarantine regulations are being strictly followed.
Statement of Ethics
The study was approved by the Central Ethical Committee of the Shreeji Clinic (approval no. 11/ABN/2021) in accordance with the Helsinki Declaration (recommendations guiding the medical doctor in biomedical research involving human subjects).
Conflict of Interest Statement
The authors declare that there is no conflict of interest.
Funding Sources
This retrospective study received no grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
V.M.: study design, data analysis, and drawing conclusion; D.B.: data collection and analysis and consent formalities; A.S.: manuscript draft and study validation; C.B.: protocol establishment; C.I.R.: data analysis; M.S.: protocol establishment; S.B.: data collection and quality check; L.M.H.: result validation; L.K.: study supervision; N.R.K.: manuscript revision and cross-checking; F.-R.H.: statistical analysis; and R.H.: prepared tables and figures and statistical analysis.
Data Availability Statement
The data will be made available on request.
References
- 1. https://covid19.who.int/table .
- 2.Chen L, Liu M, Zhang Z, Qiao K, Huang T, Chen M, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. 2020;104((6)):748–51. doi: 10.1136/bjophthalmol-2020-316304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colavita F, Lapa D, Carletti F, Lalle E, Bordi L, Marsella P, et al. SARS-CoV-2 isolation from ocular secretions of a patient with COVID-19 in Italy with prolonged viral RNA detection. Ann Intern Med. 2020;173((3)):242–3. doi: 10.7326/M20-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Violi F, Pastori D, Cangemi R, Pignatelli P, Loffredo L. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost. 2020;120((6)):949–56. doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tunescu M, Christodorescu R, Sharma A, Barsac CR, Rogobete AF, Crisan DC, et al. The preoperative evaluation of post-COVID-19 patients scheduled for elective surgery: what is important not to miss. Eur Rev Med Pharmacol Sci. 2021;25((23)):7607–15. doi: 10.26355/eurrev_202112_27459. [DOI] [PubMed] [Google Scholar]
- 6.Douglas KAA, Douglas VP, Moschos MM. Ocular manifestations of COVID-19 (SARS-CoV-2): a critical review of current literature. In Vivo. 2020;34((3 Suppl)):1619–28. doi: 10.21873/invivo.11952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. 2020;92((6)):589–94. doi: 10.1002/jmv.25725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with Coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138((5)):575–8. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawrenson JG, Buckley RJ. COVID-19 and the eye. Ophthalmic Physiol Opt. 2020;40((4)):383–8. doi: 10.1111/opo.12708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadhu S, Agrawal R, Pyare R, Pavesio C, Zierhut M, Khatri A, et al. COVID-19: limiting the risks for eye care professionals. Ocul Immunol Inflamm. 2020;28((5)):714–20. doi: 10.1080/09273948.2020.1755442. [DOI] [PubMed] [Google Scholar]
- 11.Salducci M, La Torre G. COVID-19 emergency in the cruiseʼs ship: a case report of conjunctivitis. Clin Ter. 2020;171((3)):e189–91. doi: 10.7417/CT.2020.2212. [DOI] [PubMed] [Google Scholar]
- 12.Daruich A, Martin D, Bremond-Gignac D. Unilateral conjunctivitis as first presentation of Coronavirus disease 2019 (COVID-19): a telemedicine diagnosis. J Fr Ophtalmol. 2020;43((5)):e167–8. doi: 10.1016/j.jfo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020;258((5)):1049–55. doi: 10.1007/s00417-020-04641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma D, Chen CB, Jhanji V, Xu C, Yuan XL, Liang JJ, et al. Expression of SARS-CoV-2 receptor ACE2 and TMPRSS2 in human primary conjunctival and pterygium cell lines and in mouse cornea. Eye. 2020;34((7)):1212–9. doi: 10.1038/s41433-020-0939-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qing H, Li Z, Yang Z, Shi M, Huang Z, Song J, et al. The possibility of COVID-19 transmission from eye to nose. Acta Ophthalmol. 2020;98((3)):e388. doi: 10.1111/aos.14412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. https://www.R-project.org .
- 17.Güemes-Villahoz N, Burgos-Blasco B, García-Feijoó J, Sáenz-Francés F, Arriola-Villalobos P, Martinez-de-la-Casa JM, et al. Conjunctivitis in COVID-19 patients: frequency and clinical presentation. Graefes Arch Clin Exp Ophthalmol. 2020;258((11)):2501–7. doi: 10.1007/s00417-020-04916-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishiura H, Kobayashi T, Miyama T, Suzuki A, Jung SM, Hayashi K, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–5. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Scalinci SZ, Trovato Battagliola E. Conjunctivitis can be the only presenting sign and symptom of COVID-19. IDCases. 2020;20:e00774. doi: 10.1016/j.idcr.2020.e00774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Llitjos JF, Leclerc M, Chochois C, Monsallier JM, Ramakers M, Auvray M, et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18((7)):1743–6. doi: 10.1111/jth.14869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dinkin M. Gao V, Kahan J, Bobker S, Simonetto M, Wechsler P, et al. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020;95((5)):221–3. doi: 10.1212/WNL.0000000000009700. [DOI] [PubMed] [Google Scholar]
- 22.Cheema M, Aghazadeh H, Nazarali S, Ting A, Hodges J, McFarlane A, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19) Can J Ophthalmol. 2020;55((4)):e125–9. doi: 10.1016/j.jcjo.2020.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Loffredo L, Pacella F, Pacella E, Tiscione G, Oliva A, Violi F. Conjunctivitis and COVID-19: a meta-analysis. J Med Virol. 2020;92((9)):1413–4. doi: 10.1002/jmv.25938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.La Distia Nora R, Putera I, Khalisha DF, Septiana I, Ridwan AS, Sitompul R. Are eyes the windows to COVID-19? Systematic review and meta-analysis. BMJ Open Ophthalmol. 2020;5((1)):e000563. doi: 10.1136/bmjophth-2020-000563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Colmenero I, Santonja C, Alonso-Riaño M, Noguera-Morel L, Hernández-Martín A, Andina D, et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br J Dermatol. 2020;183((4)):729–37. doi: 10.1111/bjd.19327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Damsky W, Peterson D, King B. When interferon tiptoes through COVID-19: pernio-like lesions and their prognostic implications during SARS-CoV-2 infection. J Am Acad Dermatol. 2020;83((3)):e269–70. doi: 10.1016/j.jaad.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Battesti G, El Khalifa J, Abdelhedi N, Ferre V, Bouscarat F, Picard-Dahan C, et al. New insights in COVID-19-associated chilblains: a comparative study with chilblain lupus erythematosus. J Am Acad Dermatol. 2020;83((4)):1219–22. doi: 10.1016/j.jaad.2020.06.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nirenberg MS, Del Mar Ruiz Herrera M. Foot manifestations in a COVID-19 positive patient: a Case Study. J Am Podiatr Med Assoc. 2020 doi: 10.7547/20-088. [DOI] [PubMed] [Google Scholar]
- 29.Olea B, Albert E, Torres I, Gozalbo-Rovira R, Carbonell N, Ferreres J, et al. Lower respiratory tract and plasma SARS-CoV-2 RNA load in critically ill adult COVID-19 patients: relationship with biomarkers of disease severity. J Infect. 2021;83((3)):381–412. doi: 10.1016/j.jinf.2021.05.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goel R, Arora R, Chhabra M, Kumar S. Viral shedding in tears of COVID-19 cases presenting as conjunctivitis. Indian J Ophthalmol. 2020;68((10)):2308. doi: 10.4103/ijo.IJO_2567_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data will be made available on request.