Abstract
Objectives
Healthcare workers (HCWs) are the front lines during the COVID-19 pandemic. They are more exposed to COVID-19 than other professions. Studies from other countries have shown that the mental health and health-related quality of life (HRQoL) of HCWs were affected during this pandemic. However, studies on mental health in Indonesia remain scarce and no study has evaluated the HRQoL among HCWs. Thus, this study was designed to explore the mental health status and HRQoL among HCWs in Indonesia.
Design
This was a cross-sectional study.
Setting
This was an open online survey in Indonesia conducted from December 2020 to February 2021.
Participants
This study involved HCWs who worked during the COVID-19 pandemic. Of the 502 respondents who accessed the online questionnaire, 392 were included in the analysis.
Outcomes
Mental health status was measured using the 21-item Depression, Anxiety and Stress Scale and HRQoL was measured using the second version of the 12-item Short-Form Health Survey (SF12v2).
Results
The prevalence of depression, anxiety and stress among HCWs was 29.4%, 44.9% and 31.8%, respectively. Using the SF12v2 questionnaire, 354 (90.3%) HCWs were found to have impaired physical component and 156 (39.8%) HCWs have impaired mental component.
Conclusion
The prevalence of mental health problems among HCWs was high in Indonesia. HRQoL, particularly the physical component, was affected in most HCWs. Thus, policymakers should give more attention to the mental health and HRQoL of HCWs during the COVID-19 pandemic.
Keywords: COVID-19, MENTAL HEALTH, PUBLIC HEALTH, EPIDEMIOLOGY
Strengths and limitations of this study.
This study assessed the prevalence of and determinants for mental health problems and impaired health-related quality of life (HRQoL) among healthcare workers (HCWs) during the COVID-19 pandemic in Indonesia.
We performed univariate logistic regression analysis, followed by multivariate logistic regression analysis using backward selection, to determine the determinants for mental health problems and impaired HRQoL.
The cross-sectional nature of this study could not identify temporal relationships between the course of the COVID-19 pandemic and mental health problems and HRQoL impairment.
Because of the non-probability purposive sampling method, generalisation of this study’s findings to all HCWs in Indonesia should be done cautiously.
Background
COVID-19, caused by SARS-CoV-2, emerged in December 2019 in Wuhan, Hubei Province of China.1 This virus is related to SARS-CoV-1, which was the cause of SARS in 2002 and Middle East respiratory syndrome in 2012.2 As of 11 March 2020, the WHO characterised COVID-19 as a pandemic.3 To this date, over 428 million were affected by this disease with over 5 million of deaths worldwide.4 In Indonesia, the first official case of COVID-19 was on 2 March 2020.5 After that, the number of reported cases in Indonesia has been exponentially increasing. Currently, over 3.9 million individuals are positive for the disease with more than 121 000 deaths.6
Healthcare workers (HCWs) are the front lines during the COVID-19 pandemic and thus are more exposed to COVID-19 than other professions. Worldwide, the total number of deaths among HCWs is over 155 000.7 In Indonesia, the total number of deaths among HCWs is 2066 to this date.8 Although the reported mortality rate among HCWs is lower than that in the general population,9 10 higher levels of mental health problems are found among HCWs.11 Heavy workload and lack of personal protective equipment (PPE) are highlighted as profession-related contributing risk factors.12
A recently published systematic review has revealed that the prevalence of depression and anxiety among HCWs during the COVID-19 pandemic was 37% and 40%, respectively.13 This prevalence was higher than that observed in non-pandemic situations, where the prevalence of depression and anxiety was 11.3% and 17.3%, respectively.14 However, no study from Indonesia was included in this meta-analysis.13 15 To this date, studies on mental health among HCWs in Indonesia remain scarce and are either focusing on a certain HCW profession or conducted only in one part of the country.16–20 Other than that, all studies have adopted a cross-sectional study design, thus only illustrating a particular moment of the pandemic. Nonetheless, no study has been conducted during the later stage of the COVID-19 pandemic in Indonesia when the number of cases and deaths was increasing.21
Besides mental health problems, health-related quality of life (HRQoL) is also affected during the COVID-19 pandemic.22 Currently, few published studies have evaluated the HRQoL of HCWs during the COVID-19 pandemic23–31; however, no such studies have been conducted in Indonesia. Thus, this study was designed to explore the mental health status and HRQoL among HCWs in Indonesia and identify the determining factors.
Methods
Study design
This study was a cross-sectional study using an open online questionnaire. SurveyMonkey was used as the survey platform. Using this survey platform, each respondent can only participate in the questionnaire once because the Internet Protocol address was used to identify potential duplicate entries from the same respondent. The questionnaire link was distributed through social media, that is, WhatsApp and Instagram, the most popular and accessible social media platforms in Indonesia.
Participants
The study participants were HCWs in Indonesia and were recruited using a non-probability purposive snowball sampling technique. The inclusion criteria were as follows: HCWs who were actively working during the COVID-19 pandemic and agreed to participate in this study. The HCWs aimed to be included in this study were doctor, dentist, midwife, pharmacist, nutritionist, physiotherapist, laboratory analyst, acupuncturist, health educator and hospital administrator.32 Informed consent was obtained from each respondent prior to their participation in the study. Data collection was conducted from December 2020 to February 2021. The minimum required sample size was calculated using EpiInfo.33 According to the Indonesia National Disaster Management Agency, the total number of HCWs in Indonesia was 528 714 on September 2020.34 Using an expected frequency of 50%, acceptable margin of error of 5%, and design effect of 1.0, a minimum of 384 samples were needed to obtain sufficient statistical power, assuming 95% CIs.
Instruments
The questionnaire contained 60 questions, separated into four pages. The time needed to complete the questionnaire was 15–20 min. All questions were mandatory to answer, and respondents could not move to the next page if all questions on the previous page had not been answered. Before submitting the questionnaire, the respondents could review and change their answers.
The background and demographic characteristics of each respondent were obtained using a questionnaire that contained questions on the respondent’s gender, age, marital status, specific job, workplace setting during the pandemic, workplace location, working experience as an HCW before the COVID-19 pandemic, working hours per week, monthly income, history of COVID-19 infection, comorbidities, availability of PPE in the workplace, verbal or physical intimidation in the workplace, intimidation from the society outside the workplace, support from the workplace if there is any intimidation, willingness to work during the COVID-19 pandemic and reason for working during the COVID-19 pandemic.
Mental health was measured using the Indonesian version of 21-item Depression, Anxiety and Stress Scale (DASS-21).35 This questionnaire has been adapted to Bahasa Indonesia previously and showed good validity and reliability.36 The DASS-21 is a self-administered questionnaire consisting of depression, anxiety and stress subscales, each composed of 7 items. Every item could have a score ranging from 0, indicating a lack of symptoms in the past week, to 3, indicating the presence of symptoms for almost every day in the past week. To calculate the final score of each subscale, the score was multiplied by 2. The minimum final score was 0 and the maximum score was 42 for each subscale. Based on the total score, mental health can be categorised into normal or mild, moderate, severe or extremely impaired (table 1).35
Table 1.
Cut-off score for mental health status categorisation35
| Normal | Mild | Moderate | Severe | Extremely impaired | |
| Depression | 0–9 | 10–12 | 13–20 | 21–27 | 28–42 |
| Anxiety | 0–6 | 7–9 | 10–14 | 15–19 | 20–42 |
| Stress | 0–10 | 11–18 | 19–26 | 27–34 | 25–42 |
Lovibond and Lovibond.35
HRQoL was evaluated using the second version of the 12-item Short-Form Health Survey (SF12v2) (license number: QM054173).37 The use of SF12v2 to evaluate HRQoL was based on the consideration that it can be used in non-patient populations and has fewer questions than other HRQoL questionnaires. The SF12v2 has been adapted to Bahasa Indonesia previously and showed good validity and reliability.38 This questionnaire measures both the physical and mental health components, which are divided into eight health domain scales, that is, physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE) and mental health (MH). PF, RP, BP and GH have the greatest physical component among the health domains, whereas VT, SF, RE and MH have the greatest mental component.37 The explanations of each domain scale have been described elsewhere.38 The SF12v2 was scored using Optum PRO CoRE software (Optum PROCoRE 1.3 Smart Measurement System, Optum, USA). The software will generate the score for each health domain and the summary scores of the physical and mental components. Scores of less than 47 indicate significant impairment in the associated health domain.37
Data analysis
Only completed questionnaires were included in the data analysis. Acquired data were analysed using IBM SPSS Statistics for Windows V.25.0 (IBM Corp., Armonk, New York, USA). Differences with p values <0.05 were considered statistically significant. The one-sample Kolmogorov-Smirnov test was used to evaluate the data distribution. Normally distributed data were presented as mean±SD, skewed data were presented as median (IQR) and nominal data were presented as frequency (%). To discover the determinants of mental health and HRQoL, multiple logistic regression analysis using backward selection was used. Data analysis was conducted in two phases. In the first phase, univariate logistic regression was used to identify independent variables associated with mental health status and HRQoL. Variables with p values <0.1 were included in the next phase. In the second phase, multivariate logistic regression using backward selection was used. Variables with p values <0.05 from multivariate regression analysis were considered as the determinants.39 During the analysis to determine the determinants, mental health variables were recategorised into dichotomous (normal or not) variables with the cut-off as follows: 9 for depression, 6 for anxiety and 10 for stress.35
Patient and public involvement
Patients and the public were not involved in this study.
Results
Of the 502 HCWs who accessed the online questionnaire, 392 were included for the analysis. The total response rate for this study was 78% (figure 1). The detailed sociodemographic characteristics of the respondents are summarised in table 2.
Figure 1.
Flow diagram of study participants. HCWs, healthcare workers.
Table 2.
Sociodemographic characteristics of the respondents (n=392)
| Variables | n (%) |
| Age in years, mean±SD | 33.5±9.4 |
| Sex | |
| Male | 127 (32.4) |
| Female | 265 (67.6) |
| Marital status | |
| Single | 146 (37.2) |
| Married | 128 (32.7) |
| Married with children | 118 (30.1) |
| Job | |
| Nurse | 52 (13.3) |
| Midwife | 19 (4.9) |
| Doctor | 227 (57.9) |
| Dentist | 26 (6.6) |
| Pharmacist | 20 (5.1) |
| Others (nutritionist, physiotherapist, laboratory analyst, acupuncturist, health educator and hospital administrator) | 48 (12.2) |
| Workplace setting | |
| COVID-19 hospital or COVID-19 referral hospital | 160 (40.8) |
| Non-COVID-19 hospital | 76 (19.4) |
| Primary care facilities | 138 (35.2) |
| Other healthcare facilities | 18 (4.6) |
| Workplace island | |
| Java Island | 296 (75.5) |
| Outside Java Island | 96 (24.5) |
| Working period during the COVID-19 pandemic | |
| Since the beginning of the pandemic (March–April 2020) | 310 (79.1) |
| In the middle of the pandemic (May 2020 or later) | 82 (20.9) |
| Working experience before the COVID-19 pandemic | |
| Not working | 36 (9.2) |
| <1 year | 67 (17.1) |
| 1–3 years | 92 (23.5) |
| >3 years | 197 (50.2) |
| Income during the COVID-19 pandemic | |
| <3 million rupiah/month | 77 (19.7) |
| 3–5 million rupiah/month | 107 (27.3) |
| 5–10 million rupiah/month | 111 (28.3) |
| 10–20 million rupiah/month | 51 (13.0) |
| >20 million rupiah/month | 46 (11.7) |
| Working hours per week during the COVID-19 pandemic | |
| <40 hours/week | 180 (45.9) |
| 40–60 hours/week | 181 (46.2) |
| >60 hours/week | 31 (7.9) |
| History of COVID-19 infection | |
| Yes | 57 (14.5) |
| No | 335 (85.5) |
| History of COVID-19 infection in the family | |
| Yes | 118 (30.1) |
| No | 274 (69.9) |
| Any family member died because of COVID-19 | |
| Yes | 25 (6.4) |
| No | 367 (93.6) |
| Having one or more comorbidities | |
| Yes | 276 (70.4) |
| No | 116 (29.6) |
| PPE availability in the workplace | |
| Not available or not according to standard | 134 (34.2) |
| Available and according to standard | 258 (65.8) |
| Free routine COVID-19 PCR swab test for HCWs | |
| No | 177 (45.1) |
| Only if there are any symptoms | 194 (49.5) |
| Routinely 1–3 times a month | 20 (5.1) |
| At least once a week | 1 (0.3) |
| Verbal intimidation in the workplace | |
| Never | 243 (62.0) |
| Less than once a month | 84 (21.4) |
| 1–4 times a month | 49 (12.5) |
| More than once a week | 16 (4.1) |
| Physical intimidation in the workplace | |
| Never | 379 (96.7) |
| Less than once a month | 8 (2.0) |
| 1–4 times a month | 3 (0.8) |
| More than once a week | 2 (0.5) |
| Intimidation from the society outside the workplace | |
| Never | 285 (72.7) |
| Less than once a month | 77 (19.7) |
| 1–4 times a month | 26 (6.6) |
| More than once a week | 4 (1.0) |
| Workplace support from intimidation | |
| Yes | 322 (82.1) |
| No | 70 (17.9) |
| How the workplace treats HCWs with COVID-19 symptoms | |
| Do not know | 21 (5.3) |
| HCWs are not allowed to come to work until the test result came out | 306 (78.1) |
| HCWs still come to work until the test result came out | 65 (16.6) |
| HCWs’ salary if they are infected with COVID-19 | |
| Do not know | 136 (34.7) |
| Reduced by the number of the absence | 67 (17.1) |
| Full payment | 189 (48.2) |
| Willingness to work during the COVID-19 pandemic | |
| Yes | 330 (84.2) |
| No | 62 (15.8) |
| Reason for HCWs to work during the COVID-19 pandemic | |
| Feeling responsible | 285 (72.7) |
| Financial matters | 88 (22.4) |
| Already bound to work contracts | 36 (9.2) |
HCWs, healthcare workers; PPE, personal protective equipment.
Mental health
The median scores of the depression, anxiety and stress subscales were 6 (2–10), 6 (2–12) and 10 (4–10), respectively. Of the 392 respondents, 119 (29.4%) experienced depression, 176 (44.9%) experienced anxiety and 164 (31.8%) experienced stress (figure 2). Stratified by gender, the prevalence of depression, anxiety and stress among male HCWs was 27 (21.3%), 42 (33.1%) and 45 (35.4%), respectively, whereas the prevalence of depression, anxiety and stress among female HCWs was 92 (34.7%), 134 (50.6%) and 119 (44.9%), respectively (online supplemental figures 1 and 2).
Figure 2.
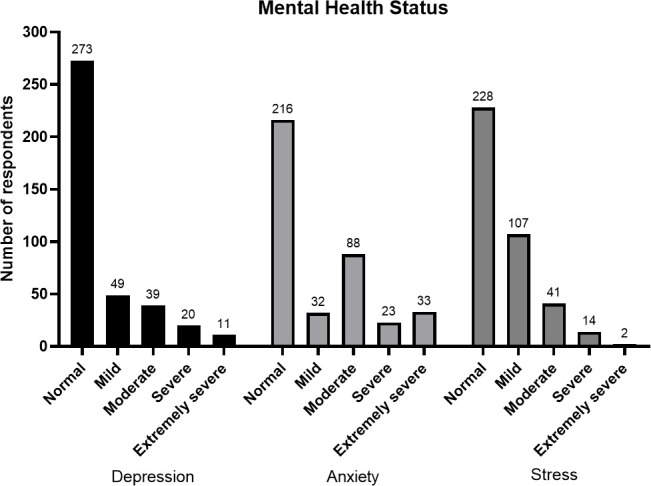
Prevalence of depression, anxiety and stress among healthcare workers in each severity level according to 21-item Depression, Anxiety and Stress Scale scores.
bmjopen-2021-057963supp001.pdf (600.8KB, pdf)
To find the determinants of depression among HCWs, multivariate logistic regression analysis was performed by including all variables that had a p value of <0.1 in the univariate analysis (online supplemental table 1). Female HCWs, HCWs who did not receive support from the workplace when intimidated by the patients or patients’ family members because of COVID-19-related issues, and HCWs that worked during the pandemic because they were bound by working contracts were more likely to be depressed. Meanwhile, HCWs with working experience of more than 3 years in healthcare facilities were less likely to be depressed (table 3).
Table 3.
Determinants of depression among healthcare workers (n=392)
| Variables | P value | aOR | 95% CI |
| Sex | |||
| Male (ref) | – | – | – |
| Female | 0.033 | 1.777 | 1.048 to 3.013 |
| Working experience before the COVID-19 pandemic | |||
| Not working (ref) | – | – | – |
| <1 year | 0.801 | 0.893 | 0.369 to 2.162 |
| 1–3 years | 0.56 | 1.283 | 0.554 to 2.969 |
| >3 years | 0.008 | 0.333 | 0.147 to 0.753 |
| Workplace support from intimidation | |||
| Yes (ref) | – | – | – |
| No | 0.002 | 2.493 | 1.383 to 4.494 |
| Work during the COVID-19 pandemic because already bound to working contracts | |||
| Yes | 0.015 | 2.578 | 1.198 to 5.547 |
| No (ref) | – | – | – |
P values <0.05 were considered statistically significant.
aOR, adjusted OR.
To find the determinants of anxiety among HCWs, multivariate logistic regression analysis was performed by including all variables that had a p value of <0.1 in the univariate analysis (online supplemental table 2). Female HCWs, HCWs who did not receive support from the workplace when intimidated by the patients or patients’ family members, and HCWs who were not willing to work during the COVID-19 pandemic were more likely to be anxious. Meanwhile, older HCWs and HCWs who worked in healthcare facilities other than COVID-19 hospitals or referral hospitals for COVID-19 were less likely to be anxious (table 4).
Table 4.
Determinants of anxiety among healthcare workers (n=392)
| Variables | P value | aOR | 95% CI |
| Age | <0.001 | 0.938 | 0.913 to 0.964 |
| Sex | |||
| Male (ref) | – | – | – |
| Female | 0.01 | 1.874 | 1.163 to 3.021 |
| Workplace setting | |||
| COVID-19 hospital or referral hospital (ref) | – | – | – |
| Non-COVID-19 hospital | 0.001 | 0.356 | 0.189 to 0.669 |
| Primary care or other healthcare facilities | 0.029 | 0.574 | 0.348 to 0.946 |
| Workplace support from intimidation | |||
| Yes (ref) | – | – | – |
| No | 0.017 | 2.099 | 1.143 to 3.854 |
| Willingness to work during the COVID-19 pandemic | |||
| Yes (ref) | – | – | – |
| No | 0.016 | 2.154 | 1.157 to 4.012 |
P values <0.05 were considered statistically significant.
aOR, adjusted OR.
To find the determinants of stress among HCWs, multivariate logistic regression analysis was performed by including all variables that had a p value of <0.1 in the univariate analysis (online supplemental table 3). HCWs who did not receive support from the workplace when intimidated by the patients or patients’ family members, HCWs who are not willing to work during the COVID-19 pandemic, and HCWs who worked during the pandemic because of financial matters or because they were bound by working contracts were more likely to be stressed. Meanwhile, older HCWs were less likely to be stressed (table 5).
Table 5.
Determinants of stress among healthcare workers (n=392)
| Variables | P value | aOR | 95% CI |
| Age | 0.001 | 0.956 | 0.930 to 0.983 |
| Workplace support from intimidation | |||
| Yes (ref) | – | – | – |
| No | 0.014 | 2.043 | 1.154 to 3.616 |
| Willingness to work during COVID-19 pandemic | |||
| Yes (ref) | – | – | – |
| No | 0.014 | 2.169 | 1.168 to 4.027 |
| Work during COVID-19 pandemic because of financial matters | |||
| Yes | 0.014 | 3.575 | 1.293 to 9.885 |
| No (ref) | – | – | – |
| Work during COVID-19 pandemic because already bound to working contract | |||
| Yes | 0.014 | 4.352 | 1.340 to 14.137 |
| No (ref) | – | – | – |
P values <0.05 were considered statistically significant.
aOR, adjusted OR.
Health-related quality of life
The median score of the physical component summary (PCS) was 41.80 (39.15–44.14) and the median score of the mental component summary (MCS) was 49.81 (43.25–55.95). The detailed scores of the PCS, MCS and each health domain scale are summarised in figure 3. Of the 392 HCWs, 354 (90.3%) had an impairment in the physical component and 156 (39.8%) had an impairment in the mental component (figure 4).
Figure 3.
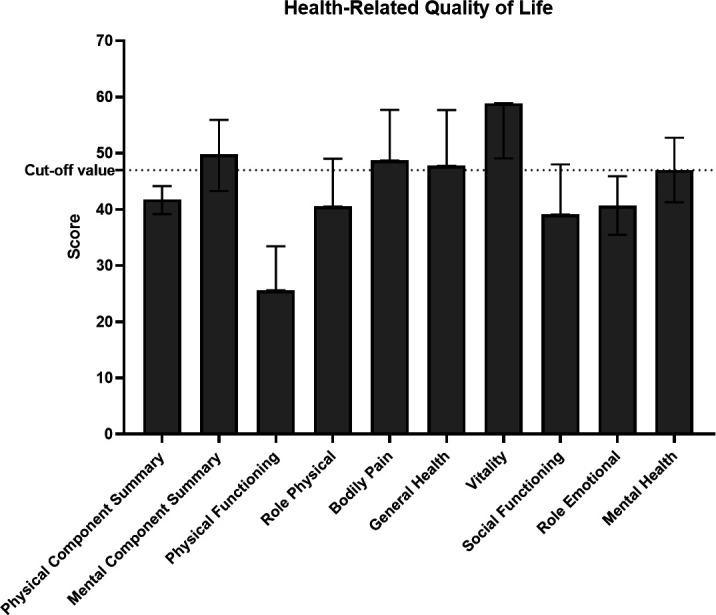
The median (IQR) norm-based T-score of summary scores and each health domain scale.
Figure 4.
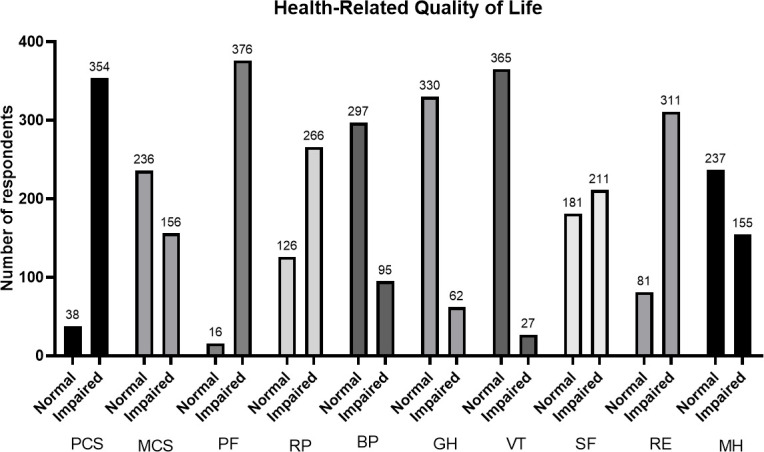
The prevalence of impairment in physical and mental components in general and each health domain scale among healthcare workers. BP, bodily pain; GH, general health; MCS, mental component summary; MH, mental health; PCS, physical component summary; PF, physical function; RE, role emotional; RP, role physical; SF, social functioning; VT, vitality.
To find the determinants of impaired physical and mental health components among HCWs, multivariate logistic regression analysis was performed by including all variables that had a p value of <0.1 in the univariate analysis (online supplemental tables 4 and 5). However, no determinants were found in the multivariate analysis.
Discussion
The results of this study provided additional information on the mental health conditions and HRQoL among Indonesian HCWs. Moreover, this study identified several significant determinants of stress, anxiety, and depression among HCWs. This may also act as a guide for relevant actions that can be taken by relevant authorities to provide preventive efforts regarding mental health matters.
Mental health
The prevalence of depression, anxiety and stress observed in this study was 29.4%, 44.9% and 31.8%, respectively, which were higher than that reported in previous studies from Indonesia that also used the DASS-21 as the study instrument, wherein the prevalence was 2.4%–13.2% for depression, 6.8%–20.6% for anxiety and 5.7%–11% for stress.16 17 19 The discrepancy between this study and previous studies might be attributed to the time difference in data collection. In this study, data collection was performed in the later time of the pandemic, whereas in previous studies, data collection was performed at the beginning of the pandemic.
Indeed, a recent systematic review and meta-analysis of longitudinal studies has shown that the prevalence of mental health problems was higher only at the beginning of the pandemic and continuously declined after 2 months.40 In HCWs, the high prevalence of mental health problems at the beginning of the pandemic may be because of the sudden escalation of the workload and lack of understanding of the disease. At the later stage, as there are more information about the disease and HCWs have adapted to the new workload, the prevalence of mental health problems decreased.41 However, note that most studies included in that review were from countries where the peak of the first wave occurred at the beginning of the pandemic and that there is a lack of studies conducted in the later period of the pandemic when the number of cases surged again.40 41 In a single-centre longitudinal study in Italy, the prevalence of anxiety and stress remained high even during the third wave, whereas the prevalence of depression increased from the first wave to the third wave.42 As the number of cases increases, the workload of the HCWs also increases. This will negatively affect their mental health condition.43 44 In Indonesia, the peak of the first wave occurred not at the beginning of the pandemic but during the data collection of this study, that is, from December 2020 to February 2021.21 This explained the higher prevalence of mental health problems in this study than in previous studies.
Several studies were conducted during the same period as this study. Ménard et al have shown that the prevalence of depression, anxiety and stress among Canadian HCWs was 14.4%, 21.8% and 13.5%, respectively.45 The lower prevalence in Canada might be explained by the difference in the healthcare systems. Different healthcare systems across countries can lead to differences in the prevalence of mental health problems among HCWs.46 Unlike Canada, the capacity of the current Indonesia’s healthcare system to respond to the COVID-19 pandemic is far from adequate.47 Another study from Italia has revealed that the prevalence of depression, anxiety and stress was 63%, 31% and 80%, respectively.42 The higher prevalence in that study might be explained by the difference in the study population where that study only included frontline HCWs (intensivist) caring exclusively for patients with COVID-19, whereas the HCWs in this study also treat non-COVID-19 patients and some of them were not frontline HCWs. It has been shown previously that frontline HCWs and those who worked in the intensive care unit during the COVID-19 pandemic were more likely to develop mental health problems.48 49
In this study, the prevalence of depression, anxiety and stress was higher in female HCWs than that in male HCWs (online supplemental figures 1 and 2). Moreover, the female sex was an independent risk factor for depression and anxiety (tables 3 and 4). Similarly, other studies have also reported gender differences in mental health problems among HCWs during the COVID-19 pandemic, where it is more prevalent in female HCWs.50 51 This can be because females have higher rates of mood and anxiety disorders due to a higher mean level of internalising and potentially by the influence of sex hormones.52 53
A previous study in Indonesia among nurses who worked during the COVID-19 pandemic has shown that rejection from family and/or neighbours is a risk factor for depression, anxiety and stress.17 We also found a similar finding where intimidation from society was a risk factor for depression, anxiety and stress in the univariate analysis (online supplemental tables 1-3). However, this variable lost its significance in the multivariate analysis, whereas workplace support towards potential intimidation was shown to lower the risk of depression, anxiety and stress. This indicates that the workplace environment plays a more substantial role in mental health. Havaei et al have found that negative ratings of workplace conditions such as workplace relations, workplace safety, organisational support and preparedness were associated with poor mental health outcomes during the COVID-19 pandemic.54 A narrative review focusing on the mental health of HCWs during the COVID-19 pandemic has also stated that intrinsic high-risk professional, organisational factors such as lack of workplace support, and vulnerable workers such as frontline HCWs are at a higher risk of mental issues during the pandemic.55
Health-related quality of life
To this date, many established questionnaires can be used to assess HRQoL. In previously published studies on HRQoL among HCWs during the COVID-19 pandemic, several HRQoL questionnaires were used, that is, WHOQOL-BREF,23 27 29 EQ-5D,30 31 SF3624 and SF12.28 Since we used the SF12v2 to evaluate HRQoL in this study, we argue that comparing our findings with those of previous studies that have used either the SF12 or SF36 is essential. The PCS and MCS scores in previous studies were higher than those in this study,24 28 indicating that HRQoL in previous studies was better. Moreover, we found that 39.8% of the HCWs included in this study had an impairment in the mental component and 90.3% had an impairment in the physical component. However, we cannot compare our findings with those of previous studies since they did not present the prevalence of HCWs with impaired physical and mental health components.24 28
The worse HRQoL in this study might be caused by the time difference of the study period where previous studies were conducted at the beginning of the pandemic and this study was conducted in the later time of the pandemic.24 28 Similar to the mental health status, we would argue that the HRQoL of HCWs at the beginning of the pandemic was not as affected as that at the later period. The number of patients with COVID-19 at the later period was significantly higher than at the beginning of the pandemic.6 This increased number of patients will increase the workload of HCWs, even if the working hour is not prolonged. Over time, increasing workload will lead to physical exhaustion of HCWs. Moreover, the number of deaths of patients with COVID-19 increases over time. Constant exposure to dealing with dying and death, in addition to the high workload, is considered as an occupational stressor.56 57
Study limitations
This study has some limitations to consider. First, the study design was cross-sectional study, whereas the prevalence of mental health problems during the COVID-19 pandemic is dynamic. Second, as the sampling technique used in this study was non-probability purposive snowball sampling and that only those who had internet access and spare time can enrol in this study, this study was prone to selection bias. Furthermore, although the number of respondents in this study had surpassed the minimum required number of samples, the number of respondents was small compared with the total number of HCWs in Indonesia. Therefore, generalisation of this study’s findings to all HCWs in Indonesia should be done cautiously. Third, the respondents were not only frontline HCWs but also second-line HCWs, and they worked not only in COVID-19 hospitals but also in other healthcare sectors. This may underestimate the prevalence of mental health problems. Fourth, the diagnosis of depression, anxiety, stress and HRQoL impairment in this study was based on self-reported questionnaires. This may also underestimate the prevalence of mental health problems. Fifth, 78 (16%) respondents accessed the online questionnaire but did not finish it. The possible explanation for this high loss is because it takes quite a long time (approximately 15–20 min) to complete the questionnaire.
Conclusion
This is the first study that evaluated the prevalence of and determinants for both mental health status and HRQoL during the COVID-19 pandemic in Indonesia. The prevalence of depression, anxiety and stress among HCWs was 29.4%, 44.9% and 31.8%, respectively, whereas the prevalence of impaired HRQoL was 90.3% for PCS and 39.8% for MCS. The results of this study suggest that the workplace environment is where interventions to prevent and mitigate mental issues are most needed. Additionally, more attention is also needed for female HCWs, since female HCWs are at a higher risk of developing mental health issues. Based on our findings, we recommend that more attention towards HCWs should be given by the policymakers in Indonesia. This can be done by providing psychological support and also by assigning sufficient number of security guards or policies in healthcare facilities in order to provide a safer workplace. Studies with larger sample sizes and periodical evaluation may further contribute to adequately monitor the mental health and HRQoL of HCWs throughout this pandemic and develop corresponding support and interventions.
Supplementary Material
Acknowledgments
The authors would like to thank QualityMetric Incorporated, LLC for giving a free SF12v2 licensing package for this study.
Footnotes
ATS and SS contributed equally.
Contributors: ATS, SS, FFA, MK, MP, FP and BA were involved in the conceptualisation and the design of the study. ATS, SS, FFA, YEP, MK, AK and BA carried out the data collection. SS, FFA and AI conducted the analysis, and FP and BA were the main consultants in the data interpretation. ATS, SS, FFA and AI drafted the manuscript, and all the authors revised it. All authors read and approved the final manuscript to be submitted.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MP received grants and honoraria from various pharmaceutical companies, all fully unrelated to this research. Other authors have no conflict of interest to declare.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants. This study was performed according to the principles of the Declaration of Helsinki and was approved by Faculty of Medicine Universitas Airlangga (251/EC/KEPK/FKUA/2020). Participants gave informed consent to participate in the study before taking part.
References
- 1.Khan S, Siddique R, Bai Q, et al. Coronaviruses disease 2019 (COVID-19): causative agent, mental health concerns, and potential management options. J Infect Public Health 2020;13:1840–4. 10.1016/j.jiph.2020.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fauci AS, Lane HC, Redfield RR. Covid-19 - Navigating the Uncharted. N Engl J Med 2020;382:1268–9. 10.1056/NEJMe2002387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . Rolling updates on coronavirus disease (COVID-19), 2020. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen [Accessed 12 Sep 2021].
- 4.World Health Organization . WHO coronavirus (COVID-19) Dashboard, 2022. Available: https://covid19.who.int/ [Accessed 25 Feb 2022].
- 5.World Health Organization Indonesia . Coronavirus Disease 2019 (COVID-19) Situation Report - 1, 2020. Available: https://www.who.int/indonesia/news/novel-coronavirus/situation-reports [Accessed 12 Sep 2021].
- 6.World Health Organization Indonesia . Coronavirus Disease 2019 (COVID-19) Situation Report - 87, 2022. Available: https://www.who.int/indonesia/news/novel-coronavirus/situation-reports [Accessed 25 Feb 2022].
- 7.World Health Organization . Director-General’s opening remarks at the World Health Assembly, 2021. Available: https://www.who.int/director-general/speeches/detail/director-general-s-opening-remarks-at-the-world-health-assembly-24-may-2021 [Accessed 12 Sep 2021].
- 8.Lapor Covid-19. Pusara digital Tenaga Kesehatan Indonesia, 2022. Available: https://nakes.laporcovid19.org/ [Accessed 25 Feb 2022].
- 9.Bandyopadhyay S, Baticulon RE, Kadhum M, et al. Infection and mortality of healthcare workers worldwide from COVID-19: a systematic review. BMJ Glob Health 2020;5:e003097. 10.1136/bmjgh-2020-003097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Díez-Manglano J, Solís-Marquínez MN, Álvarez García A, et al. Healthcare workers hospitalized due to COVID-19 have no higher risk of death than general population. data from the Spanish SEMI-COVID-19 registry. PLoS One 2021;16:e0247422. 10.1371/journal.pone.0247422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun 2020;89:531–42. 10.1016/j.bbi.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De Kock JH, Latham HA, Leslie SJ, et al. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health 2021;21:104. 10.1186/s12889-020-10070-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud 2021;121:104002. 10.1016/j.ijnurstu.2021.104002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weaver MD, Vetter C, Rajaratnam SMW, et al. Sleep disorders, depression and anxiety are associated with adverse safety outcomes in healthcare workers: a prospective cohort study. J Sleep Res 2018;27:e12722. 10.1111/jsr.12722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salari N, Khazaie H, Hosseinian-Far A, et al. The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: a systematic review and meta-regression. Hum Resour Health 2020;18:100. 10.1186/s12960-020-00544-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chew NWS, Ngiam JN, Tan BY-Q, et al. Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. BJPsych Open 2020;6:e116. 10.1192/bjo.2020.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marthoenis M, Fathiariani L, Nassimbwa J. Investigating the burden of mental distress among nurses at a provincial COVID-19 referral hospital in Indonesia: a cross-sectional study. BMC Nurs 2021;20:76. 10.1186/s12912-021-00596-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Setiawati Y, Wahyuhadi J, Joestandari F, et al. Anxiety and resilience of healthcare workers during COVID-19 pandemic in Indonesia. J Multidiscip Healthc 2021;14:1–8. 10.2147/JMDH.S276655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sitanggang FP, Wirawan GBS, Wirawan IMA, et al. Determinants of mental health and practice behaviors of general practitioners during COVID-19 pandemic in Bali, Indonesia: a cross-sectional study. Risk Manag Healthc Policy 2021;14:2055–64. 10.2147/RMHP.S305373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sunjaya DK, Herawati DMD, Siregar AYM. Depressive, anxiety, and burnout symptoms on health care personnel at a month after COVID-19 outbreak in Indonesia. BMC Public Health 2021;21. 10.1186/s12889-021-10299-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization Indonesia . Coronavirus Disease 2019 (COVID-19) Situation Report - 86, 2022. Available: https://cdn.who.int/media/docs/default-source/searo/indonesia/covid19/external-situation-report-86_19-january-2022.pdf?sfvrsn=7db37ea6_5 [Accessed 11 Feb 2022].
- 22.Melo-Oliveira ME, Sá-Caputo D, Bachur JA, et al. Reported quality of life in countries with cases of COVID19: a systematic review. Expert Rev Respir Med 2021;15:213–20. 10.1080/17476348.2021.1826315 [DOI] [PubMed] [Google Scholar]
- 23.Woon LS-C, Mansor NS, Mohamad MA, et al. Quality of life and its predictive factors among healthcare workers after the end of a movement Lockdown: the salient roles of COVID-19 stressors, psychological experience, and social support. Front Psychol 2021;12:652326. 10.3389/fpsyg.2021.652326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stojanov J, Malobabic M, Stanojevic G, et al. Quality of sleep and health-related quality of life among health care professionals treating patients with coronavirus disease-19. Int J Soc Psychiatry 2021;67:175-181. 10.1177/0020764020942800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Çelmeçe N, Menekay M. The effect of stress, anxiety and burnout levels of healthcare professionals caring for COVID-19 patients on their quality of life. Front Psychol 2020;11:597624. 10.3389/fpsyg.2020.597624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suryavanshi N, Kadam A, Dhumal G, et al. Mental health and quality of life among healthcare professionals during the COVID-19 pandemic in India. Brain Behav 2020;10:e01837. 10.1002/brb3.1837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.da Costa Matos RA, Akutsu RdeCCdeA, Zandonadi RP, et al. Quality of life prior and in the course of the COVID-19 pandemic: a nationwide cross-sectional study with Brazilian dietitians. Int J Environ Res Public Health 2021;18. 10.3390/ijerph18052712. [Epub ahead of print: 08 03 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amerio A, Bianchi D, Santi F, et al. Covid-19 pandemic impact on mental health: a web-based cross-sectional survey on a sample of Italian general practitioners. Acta Biomed 2020;91:83–8. 10.23750/abm.v91i2.9619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.An Y, Yang Y, Wang A, et al. Prevalence of depression and its impact on quality of life among frontline nurses in emergency departments during the COVID-19 outbreak. J Affect Disord 2020;276:312–5. 10.1016/j.jad.2020.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manh Than H, Minh Nong V, Trung Nguyen C, et al. Mental health and health-related quality-of-life outcomes among frontline health workers during the peak of COVID-19 outbreak in Vietnam: a cross-sectional study. Risk Manag Healthc Policy 2020;13:2927–36. 10.2147/RMHP.S280749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martín J, Padierna Ángel, Villanueva A, et al. Evaluation of the mental health of health professionals in the COVID‐19 era. what mental health conditions are our health care workers facing in the new wave of coronavirus? Int J Clin Pract 2021;75. 10.1111/ijcp.14607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laws of the Republic of Indonesia on healthcare workers 2014;36. [Google Scholar]
- 33.Dean AG, Arner TG, Sunki GG. Epi Info™, a database and statistics program for public health professionals. Atlanta, GA: CDC, 2011. [Google Scholar]
- 34.Badan Nasional Penanggulangan Bencana (National Disaster Management Agency) . Peta Jumlah Tenaga Medis per 100,000 Penduduk Indonesia, 2020. Available: https://bnpb-inacovid19.hub.arcgis.com/app/f881fb2a91584fa5b96871a6bc2eb2e6 [Accessed 20 Sep 2020].
- 35.Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. 2nd ed. Sydney, Australia: Psychology Foundation, 1995. [Google Scholar]
- 36.EL-Matury HJ, Lestari F,Besral . Depression, anxiety and stress among undergraduate students in Jakarta: examining scores of the depression anxiety and stress scale according to origin and residency. Indian J Public Health Res Dev 2018;9:290–5. 10.5958/0976-5506.2018.00135.3 [DOI] [Google Scholar]
- 37.Maruish ME. User’s manual for the SF-12v2 Health Survey. 3rd ed. Lincoln, RI: QualityMetric Incorporated, 2012. [Google Scholar]
- 38.Wicaksana AL, Maharani E, Hertanti NS. The Indonesian version of the Medical Outcome Survey - Short Form 12 version 2 among patients with cardiovascular diseases. Int J Nurs Pract 2020;26:e12804. 10.1111/ijn.12804 [DOI] [PubMed] [Google Scholar]
- 39.Flynn J, Alkaff FF, Sukmajaya WP, et al. Comparison of who growth standard and national Indonesian growth reference in determining prevalence and determinants of stunting and underweight in children under five: a cross-sectional study from Musi sub-district. F1000Res 2020;9:324. 10.12688/f1000research.23156.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Robinson E, Sutin AR, Daly M, et al. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J Affect Disord 2022;296:567–76. 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu X, Zhu M, Zhang R, et al. Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence. Transl Psychiatry 2021;11:384. 10.1038/s41398-021-01501-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Magnavita N, Soave PM, Antonelli M. A one-year prospective study of work-related mental health in the Intensivists of a COVID-19 hub Hospital. Int J Environ Res Public Health 2021;18:9888. 10.3390/ijerph18189888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Peng R, Zhou W, Zhou D, et al. The mediating role of fatigue between mental health and its associated factors: evidence from Chinese healthcare workers during the COVID-19 pandemic. Front Psychiatry 2021;12:665992. 10.3389/fpsyt.2021.665992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tiete J, Guatteri M, Lachaux A, et al. Mental health outcomes in healthcare workers in COVID-19 and Non-COVID-19 care units: a cross-sectional survey in Belgium. Front Psychol 2020;11:612241. 10.3389/fpsyg.2020.612241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ménard AD, Soucie K, Freeman LA, et al. "My problems aren't severe enough to seek help": Stress levels and use of mental health supports by Canadian hospital employees during the COVID-19 pandemic. Health Policy 2022;126:106–11. 10.1016/j.healthpol.2022.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Uphoff EP, Lombardo C, Johnston G, et al. Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: a rapid systematic review. PLoS One 2021;16:e0254821. 10.1371/journal.pone.0254821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mahendradhata Y, Andayani NLPE, Hasri ET, et al. The capacity of the Indonesian healthcare system to respond to COVID-19. Front Public Health 2021;9:649819. 10.3389/fpubh.2021.649819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wozniak H, Benzakour L, Moullec G, et al. Mental health outcomes of ICU and non-ICU healthcare workers during the COVID-19 outbreak: a cross-sectional study. Ann Intensive Care 2021;11:106. 10.1186/s13613-021-00900-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hao Q, Wang D, Xie M, et al. Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry 2021;12:567381. 10.3389/fpsyt.2021.567381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu S, Yang L, Zhang C, et al. Gender differences in mental health problems of healthcare workers during the coronavirus disease 2019 outbreak. J Psychiatr Res 2021;137:393–400. 10.1016/j.jpsychires.2021.03.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.De Sio S, Buomprisco G, La Torre G, et al. The impact of COVID-19 on doctors' well-being: results of a web survey during the lockdown in Italy. Eur Rev Med Pharmacol Sci 2020;24:7869–79. 10.26355/eurrev_202007_22292 [DOI] [PubMed] [Google Scholar]
- 52.Eaton NR, Keyes KM, Krueger RF, et al. An invariant dimensional liability model of gender differences in mental disorder prevalence: evidence from a national sample. J Abnorm Psychol 2012;121:282–8. 10.1037/a0024780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Li SH, Graham BM. Why are women so vulnerable to anxiety, trauma-related and stress-related disorders? the potential role of sex hormones. Lancet Psychiatry 2017;4:73–82. 10.1016/S2215-0366(16)30358-3 [DOI] [PubMed] [Google Scholar]
- 54.Havaei F, Ma A, Staempfli S, et al. Nurses' workplace conditions impacting their mental health during COVID-19: a cross-sectional survey study. Healthcare 2021;9. 10.3390/healthcare9010084. [Epub ahead of print: 16 01 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Giorgi G, Lecca LI, Alessio F, et al. COVID-19-Related mental health effects in the workplace: a narrative review. Int J Environ Res Public Health 2020;17. 10.3390/ijerph17217857. [Epub ahead of print: 27 10 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gray-Toft P, Anderson JG. The nursing stress scale: development of an instrument. J Behav Assess 1981;3:11–23. 10.1007/BF01321348 [DOI] [Google Scholar]
- 57.Sjöberg A, Pettersson-Strömbäck A, Sahlén K-G, et al. The burden of high workload on the health-related quality of life among home care workers in northern Sweden. Int Arch Occup Environ Health 2020;93:747–64. 10.1007/s00420-020-01530-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-057963supp001.pdf (600.8KB, pdf)
Data Availability Statement
Data are available upon reasonable request.