Abstract
Eukaryotic cells possess a plethora of regulatory mechanisms to maintain homeostasis and ensure proper biochemical functionality. Autophagy, a central, conserved self-consuming process of the cell, ensures the timely degradation of damaged cellular components. Several studies have demonstrated the important roles of autophagy activation in mitigating neurodegenerative diseases, especially Alzheimer’s disease (AD). However, surprisingly, activation of macroautophagy has not shown clinical efficacy. Hence, alternative strategies are urgently needed for AD therapy. In recent years, selective autophagy has been reported to be involved in AD pathology, and different subtypes have been identified, such as aggrephagy, mitophagy, reticulophagy, lipophagy, pexophagy, nucleophagy, lysophagy and ribophagy. By clarifying the underlying mechanisms governing these various subtypes, we may come to understand how to control autophagy to treat AD. In this review, we summarize the latest findings concerning the role of selective autophagy in the pathogenesis of AD. The evidence overwhelmingly suggests that selective autophagy is an active mechanism in AD pathology, and that regulating selective autophagy would be an effective strategy for controlling this pathogenesis.
Keywords: Alzheimer’s disease, selective autophagy, aggrephagy, mitophagy, reticulophagy, lipophagy, pexophagy, nucleophagy, ribophagy, lysophagy
1. Introduction
Alzheimer’s disease (AD) is the most prevalent progressive neurologic disorder affecting aged people worldwide. Clinically, the primary manifestation of AD is memory impairment, followed by deficits in cognitive and adaptive functioning as the disease progresses [1,2,3]. On the basis of several factors, AD can be broadly categorized as familial and sporadic AD. Familial AD, also known as early onset AD, is often associated with genetic mutations, such as mutations in amyloid precursor protein (APP), presenilin 1 (PSEN1), and presenilin 2 (PSEN2). Sporadic AD is often caused by environmental and complex genetic factors such as the presence of the epsilon4 allele in apolipoprotein E (APOE) [4]. Pathologically, AD is characterized by the accumulation of tau-enriched neurofibrillary tangles (NFTs) and β-amyloid (Aβ) toxic aggregates in the hippocampus and cerebral cortex of the brain [5], which are the major pathological markers of AD [6,7]. According to previous studies, an accumulation of NFTs leads to synaptic dysfunction, which further causes a decline in memory and cognitive functions. Moreover, Aβ oligomers disrupt calcium homeostasis by binding to receptors, activating calcineurin and caspases [8]. In AD patients, a large number of aggregated toxic proteins interfere with the normal function of autophagy, further aggravating the pathogenesis of AD. Increasing evidence has suggested that autophagy, through which damaged organelles and misfolded proteins are degraded and then recycled to maintain proteostasis, plays a major role in AD. The mammalian nervous system, especially the neurons, is largely dependent on autophagy to clear large amounts of insoluble protein aggregates to maintain protein homeostasis [9]. Initially, autophagosomes and autolysosomes were found to accumulate in AD brains [10]. Early studies demonstrated that Beclin-1, a core subunit of the vacuolar protein-sorting 34 (VPS34) complex, decreases as AD progresses [11,12,13]. Interestingly, phosphatidylinositol 3-phosphate (PI3P) production, mediated by the VPS34 complex, is also downregulated in AD patients’ brains [14]. Autophagy is a protective mechanism in response to stress in the early stages of AD, but autophagic flux is reduced in the late stages of AD [15]. In our previous studies, we found that many Chinese herbs, formulas and compounds have neuroprotective effects and can promote the clearance of Aβ and tau proteins through enhancing autophagy and rescuing memory and cognitive impairment in AD mouse models [16,17,18,19,20]. Mounting evidence is leading to the conclusion that dysfunctional autophagy is strongly linked to AD pathogenesis.
In neurodegenerative diseases, especially AD, activating autophagy can promote cell survival by removing damaged organelles and protein deposits. Autophagy thereby provides additional energy, and dictates the fate and function of various cellular organelles [21]. According to the different pathways by which the cargo can be degraded in lysosomes, autophagy can be divided into three types: macroautophagy, microautophagy, and molecular chaperone-mediated autophagy (CMA). In macroautophagy, the double-membrane autophagosome wraps the cargo to be degraded, fuses with the lysosome, and degrades in the lysosome; this is the most common form of autophagy [22]. In conditions of nutrient imbalance, autophagy is generally a nonselective cellular degradation process. However, damaged and excess cellular organelles such as mitochondria, ER, lysosomes, and protein aggregates can also be degraded in a highly selective manner through selective autophagy [23]. For this type of autophagy, some autophagy-related proteins are required to ensure specific recognition and degradation of the cargo [21]. For example, the autophagy-related protein 8 (Atg8) family proteins on autophagosomes can target specific proteins for degradation. Microautophagy refers to the transport of cargo into lysosomes through lysosomal membrane invagination for degradation [24]. CMA refers to the process in which the cargo to be degraded binds to molecular chaperones and directly targets the lysosomes for degradation [25]. Heat shock cognate protein 70 (Hsc70) transports the target protein to the lysosomal receptor for degradation [26]. Ubiquitination is a marker of targeted protein degradation [27]. A variety of selective autophagy processes have been discovered and named according to their cellular targets, such as mitophagy (mitochondria), reticulophagy (the ER), lipophagy (lipid droplets), pexophagy (the peroxisome), nucleophagy (the nucleus), ribophagy (the ribosome), and lysophagy (the lysosome). All of the abovementioned selective autophagy subtypes are essential for maintaining proper cellular homeostasis [28].
Selective autophagy dysfunction is correlated with AD pathogenesis [29,30]. Aggrephagy and mitophagy dysfunction have been shown in the clearance of aggregated proteins and damage mitochondrial in AD patients [31]. There is some research on the link between AD and reticulophagy, which indicates that reticulon 3 (RTN3) aggregation, interferes with reticulophagy, and increases Aβ levels in elderly people [32]. Moreover, the presence of large amounts of lipid droplets (LDs), such as cholesteryl esters in the neurons, reduces the activity of the proteasomes, thereby promoting the accumulation of p-tau protein, further contributing to the pathogenesis of AD [33]. Therefore, clarifying the mechanism of selective autophagy in the pathogenesis of AD may lead us to a strategy for the prevention and treatment of AD. In this review, we summarize the current knowledge on the mechanisms of the various subtypes of selective autophagy in AD pathogenesis.
2. Aggrephagy
Generally, toxic aggregates cause neuronal membrane permeability damage, calcium homeostasis dysfunction, inflammation, neurotoxicity, and physiological abnormalities [34,35,36]. Aggrephagy is a subtype of selective autophagy that clears toxic protein aggregates [37]; in that sense, it reduces AD pathology. Aggregates are moved into double-membrane autophagosomes, where they are degraded in the acidic lysosomal lumen. The receptor SQSTM1-p62 (p62), the neighbor of BRCA1 gene 1 (NBR1), and the large junction protein ALFY are important in aggrephagy. A deficiency of ALFY or p62 is associated with neurodegeneration [38,39]. Autophagic receptors such as NBR1 and p62 directly bind to Atg8 homologs on autophagosomes for the degradation of protein aggregates [40,41,42,43,44]. Furthermore, CMA and the ubiquitin–proteasome system (UPS) prevent increases in soluble and insoluble protein aggregation [45]. Heat shock proteins such as Hsp40, Hsp60, Hsp70, and Hsp90 bind to the misfolded protein, neutralize hydrophobic areas exposed by the misfolded proteins, and prevent aggregation [46]. In CMA, Hsc70 binds to the KFERQ motif of the misfolded protein and is delivered to lysosomes for degradation by LAMP2a [47]. Ubiquitination of aggregates is critical for degradation in UPS and classical autophagy systems [48]. Existing studies have shown that ubiquitin interacts with seven lysine residues (K6, K11, K27, K29, K33, K48, and K63) [49]. These seven lysine residues bind with aggregates covalently, forming polyubiquitin chains for degradation [50].
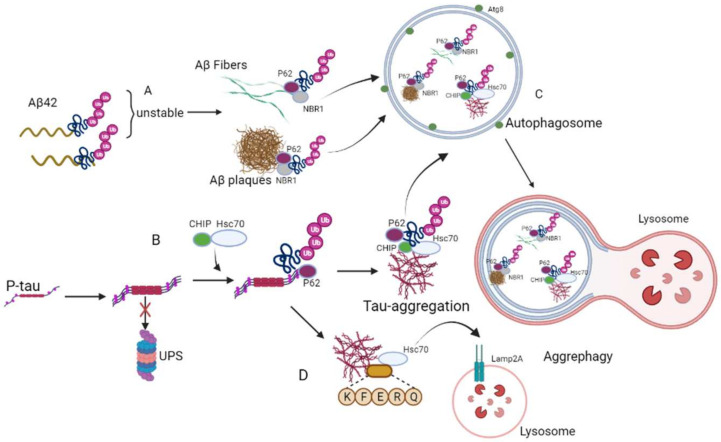
AD is a proteinopathy, with the aggregation of Aβ and P-tau protein in the brain leading to memory deficits and neurodegeneration. The elevated Aβ-42 monomers gradually assemble into aggregates within the perinuclear space [51]. Normally, ubiquitin protein binds with Aβ for UPS degradation [52]. However, these polyubiquitin chains are unstable when bound with Aβ. Therefore, they cannot fold properly, and Aβ folding dysfunction changes their physicochemical properties and promotes the formation of Aβ fibers and plaques. Overall, due to polyubiquitination, Aβ is unfolded, causing the unfolded Aβ aggregates to develop into insoluble Aβ fibers. During aggregation, some polyubiquitin Aβ peptides are degraded normally by autophagy. Other polyubiquitin Aβ fibers and plaques bind to the UBA domains of p62 and NBR1 selectively, initiating degradation by aggrephagy [53].
Clinically, in the brains of AD patients, an enormous amount of extracellular Aβ and intracellular neurofibrillary tangles can be found [54]. NFTs are formed by abnormal aggregation and hyperphosphorylation of tau into paired helical filaments (PHFs) [55]. P-tau is transported to the nucleus to form aggregates for lysosomal degradation [56]. When proteasomal aggregation degradation is inhibited, Hsc70 interacts with CHIP to regulate tau ubiquitination [57]. Ubiquitinated P-tau is recruited by the aggregation receptor p62 [56,58]. HDAC6 binds with p62 and enhances retrograde transport of the P-tau and p62 complex to form tau aggregates [59]. Furthermore, HDAC6 has been reported to respond to the protease imbalance induced by proteasome inhibition and recombine with the cytoskeletal actin network to induce the formation of tau aggregates [60]. It has been reported that the ubiquitin carboxyl-terminal hydrolase L1 (UCHL1) enzyme also affects the formation of tau protein aggregates. UCHL1 is a deubiquitinating enzyme that is abundantly expressed in the brain [61]. UCHL1 inhibition leads to hyperphosphorylation of tau protein and tau microtubule-stabilizing dysfunction [62]. In addition, UCHL1 can regulate the activity of HDAC6 and affect the formation of tau protein aggregates. Inhibition of UCHL1 impairs the interaction between P-tau and HDAC6, inhibiting the formation of tau aggregates [63]. Undoubtedly, specific aggregate degradation is required to prevent AD progression. Figure 1 illustrates the toxic protein aggregates degraded by the mechanism of aggrephagy in AD.
Figure 1.
Mechanism of aggrephagy during the occurrence of AD. (A) Polyubiquitinated Aβ plaques and fibers binds to p62 and NBR1 specifically, and initiate degradation through aggrephagy. (B) Hsc70 interacts with CHIP to regulate tau ubiquitination and then is recruited by p62. (C) All these aggregate proteins are wrapped by autophagosomes for degradation. (D) KFERQ binds with tau aggregates and is transferred to the lysosome by the Lamp2A receptor for degradation.
3. Mitophagy
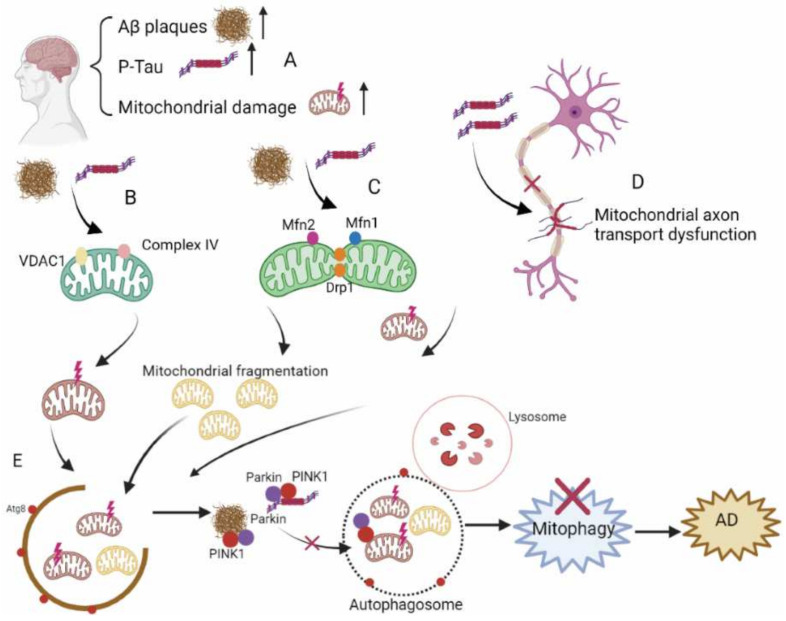
Mitochondria are critical for synaptic transmission, synaptic plasticity, calcium homeostasis, and neuronal survival [64,65]. Damaged mitochondria are degraded through mitophagy [66,67]. Impaired mitophagy is associated with a variety of neurodegenerative diseases, including AD [28]. Mitochondrial dysfunction appears with age, but it is exacerbated in AD [68,69,70,71]. Mitochondria are key targets of autophagy in AD patient brains [72,73]. In AD models, mitochondrial swelling, abnormal morphology, and the accumulation of large numbers of damaged mitochondria have been found [74,75,76]. For example, when the mitochondria are damaged, the membrane potential decreases, which stabilizes PINK1 to the outer membrane. PINK1 phosphorylates and recruits the E3 ubiquitin ligase Parkin to the mitochondria, and mediates the ubiquitination of mitochondrial outer membrane proteins to mark impaired mitochondria for degradation through mitophagy [77]. Increased PINK1, Parkin, and mitochondrial protein ubiquitination were detected in an AD mouse model, suggesting that the mitophagy process is activated but stalled [78]. This may be due to an insufficient capacity to remove many damaged mitochondria, thereby resulting in the accumulation of impaired mitochondria and disturbance of mitochondrial homeostasis. In addition, corresponding to the age-related increase in AD incidence, mitochondrial dysfunction and mitophagy also increase with age [79].
Impairment of the mitochondria occurs in the early stages of AD, and this impairment can even appear before Aβ and NTFs are formed [80,81,82,83]. Decreases in oxidative phosphorylation, an increase in ROS production, and downregulation of the tricarboxylic acid cycle (TCA) have been reported [84,85]. Studies have found that the energy metabolism in AD patients’ brains is lower than normal, which may be due to mitochondrial dysfunction [86]. PGC-1-alpha, a major regulator of mitochondrial biogenesis, is decreased in AD patients’ brains, indicating mitochondrial dysfunction [87,88]. In addition, the accumulation of damaged mitochondria has been confirmed in the neurons of AD brains. This may be due to severe impairment of the clearance of damaged mitochondria (such as through mitophagy) [89,90]. Mitophagy dysfunction can cause the accumulation of autophagic vacuoles (AVs) in neuronal cell bodies. AVs contain a large number of Aβ polypeptides, and they are a location where Aβ easily forms aggregates [91]. In AD patients, we found that Parkin and PINK1 are reduced, which decreases the occurrence of mitophagy, and the damaged mitochondria cannot be cleared [92], causing a dysfunction of mitochondrial transport, hyperphosphorylation of tau protein, and synaptic dysfunction [93].
Aβ/tau is also involved in mitochondrial dysfunction in AD. Overexpression of APP in the neurons leads to mitochondrial dysfunction [89]. Aβ and P-tau can directly interact with mitochondrial components, such as VDAC1 and Complex IV, and interfere with their function [94,95,96]. Mitochondrial dysfunction has been found in AD patients and mouse models; specifically, mitochondrial membrane potential is decreased, ROS production is increased, and mitochondrial swelling occurs [97,98,99]. In an AD cell model, mitofusin 1/2 (MFN1/2) decreased and Aβ oligomers induced mitochondrial fragmentation. Further studies have shown that Aβ oligomer mediates the activation of dynamin-related protein 1 (Drp1); this mitochondrial division proteins cause mitochondrial fragmentation and cell death in AD patients [100]. In addition, extracytoplasmic calcium is harmful to neurons and its presence may lead to neuronal death [101]. The endoplasmic reticulum and mitochondria are the main locations where intracellular calcium is stored, and they play a key role in intracellular calcium homeostasis [102,103]. It has been reported that Aβ oligomers disrupt intracellular calcium homeostasis. Aβ enhances glutamate neurotransmission and increases tau phosphorylation through n-methyl-D-aspartate receptors (NM-DARs), resulting in impaired mitochondrial function [104,105,106]. Tau pathology is also involved in AD mitochondrial dysfunction [107,108,109,110,111,112,113,114]. Studies have reported that P-tau leads to downregulation of Optic Atrophy 1 (Opa1) and Drp1. In addition, P-tau may cause an increase in mitochondrial membrane potential, thereby preventing the mitochondrial recruitment of Parkin by PINK1 [107,115,116,117]. In AD, hyperphosphorylation of tau can influence tau’s ability to bind to microtubules and can disrupt mitochondrial axon transport [118,119]. Mitochondrial fusion gene mutations have been shown to lead to mitochondrial fragmentation and AD pathology [120]. In addition, an inhibitor of mitochondrial Complex I induced tau protein pathology in rats [121,122]. Studies have shown that oxidative stress increases γ-secretase activity [123]. Similarly, excessive ROS promotes P-tau aggregation through phospholipid peroxidation [124,125]. Therefore, the accumulation of Aβ and p-tau proteins can aggravate mitochondrial dysfunction, and mitochondrial dysfunction can also aggravate tau phosphorylation and Aβ aggregation. In fact, there may be a vicious cycle between mitochondrial dysfunction and AD pathology. Figure 2 illustrates the key events in mitophagy as it relates to AD.
Figure 2.
Mitophagy in the pathogenesis of AD. (A) Impairment of the mitochondria occurs in the early stages of AD, and Aβ and P-tau are increased. (B) Aβ and P-tau interact with VDAC1 and Complex IV, and interfere with mitochondrial function. (C) Aβ and P-tau induce mitochondrial fragmentation by reducing MFN1/2 and activating Drp1. (D) Hyperphosphorylation of tau blocks the binding of tau with microtubules, disrupting mitochondrial axon transport. (E) Aβ and P-tau disturb the recruitment of PINK1 and Parkin, causing mitophagy dysfunction.
4. Reticulophagy
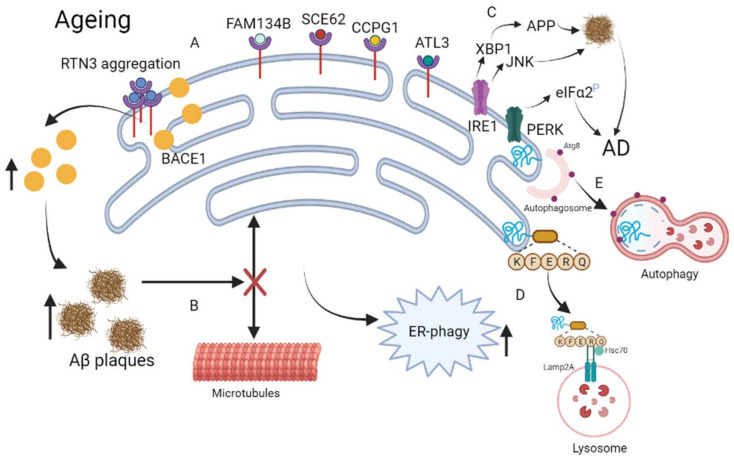
The endoplasmic reticulum (ER) is a network that is responsible for lipid and protein biosynthesis, and the modification and folding of secreted proteins. There are two vital quality control mechanisms in the cell, namely the unfolded protein response (UPR) and the ER-associated degradation pathways (ERAD) [126,127]. Activation of UPR has been reported to induce the formation of ER-associated autophagosomes, which can specifically wrap the ER and then fuse with the lysosome for degradation [128,129]. Reticulophagy seems to coexist with the downstream signaling pathways of ER stress, balancing the expansion of the ER [130,131,132]. Studies have shown that a PS1 mutation inhibits IRE1 signaling. IRE1 is an ER stress sensor serine/threonine kinase involved in AD pathogenesis, in which the IRE1α/JKN pathway may predispose a subject towards amyloid deposition and the process of AD [133,134]. Transcription factor XBP1 can bind to the promoter region of γ-secretase complex (Psen1 and Ncstn), which play an important role in Aβ synthesis [135]. Studies have shown that phospho-PERK increased in AD patients and that PS1 mutants inhibited PERK signaling [133,136]. Several receptors of reticulophagy have been discovered: FAM134, SEC62, RTN3, and CCPG1. RTN3 is involved in the development of neurodegenerative diseases [32]. RTN3 has several cleavage isoforms, the longest of which has six LIR domains that can bind with LC3/GABARAP and enhance the segmentation of ER tubules, inducing reticulophagy. In fact, RTN3 mainly initiates reticulophagy under conditions of deficient energy or hypoxia. RTN3 is a protein containing RHD that is located in the ER tubules, and its main function is to promote the formation of more ER tubules [137]. RTN3 was initially identified as a negative regulator of BACE1. BACE1 is an enzyme that cleaves APP to release beta-amyloid peptides. Increased RTN3 monomer expression affects the intracellular transport of BACE1, resulting in more BACE1 being retained in the ER, where the cleavage capacity of BACE1 for APP is attenuated. Interestingly, RTN3 can form aggregates, and an increase in the number of aggregates of RTN3 appears to be related to the formation of RTN3 immunoreactive dystrophic neurites in AD patients’ brains. Therefore, RTN3 aggregation counteracts the normal function of RTN3, by negatively regulating the RTN3 monomer-mediated BACE1 activity [32].
Growing evidence has suggested that UPR activation markers are increased in AD patients’ brains and animal models [136,138]. Studies have shown that the deposition of Aβ attenuates the interaction of the ER and microtubules in the hippocampal neurons, leading to the activation of reticulophagy [139]. In addition, chemicals that interfere with the cholesterol metabolism in the ER have been reported to increase the clearance of Aβ42, further suggesting that ER dysfunction is closely related to AD [140]. In addition, ER stress triggers autophagy, greatly decreasing APP and amyloid beta precursor-like protein 1 (APLP1). The inhibition of autophagy contributes to the deposition of APP and APLP1 [29]. Furthermore, tau has contributed to our understanding of the relationship between ER and autophagy. A study found that ER stress induces autophagy to reduce the deleterious effects of tau [141]. Therefore, the relationship between reticulophagy and AD needs further exploration. Figure 3 depicts the mechanism by which reticulophagy appears to be involved in aging and AD.
Figure 3.
Reticulophagy in the pathogenesis of AD. (A) RTN3 aggregation counteracts the negative regulation of BACE1 activity by RTN3, causing Aβ to increase in the aging brain. (B) Deposition of Aβ inhibits the interaction of the ER and microtubules, inducing reticulophagy. (C) ER stress/AD factors increase misfolded proteins through the IRE1 and PERK pathway. (D) KFERQ binds with impaired ER for CMA degradation. (E) Autophagosomes wrap the impaired ER for degradation.
5. Lipophagys
Lipid droplets (LDs) are organelles that store lipid. Mitochondria and the ER respond to ER stress and provide mitochondrial energy [142]. Lipophagy is a subtype of selective autophagy that targets LDs for degradation and plays a role in regulating lipid storage. In lipophagy, LC3-positive phagocytes engulf LDs and gradually form autophagosomes, fusing with lysosomes and degrading to glycerol and free fatty acids. Different LD-resident proteins participate in targeting LDs to undergo lipophagy, including the molecular chaperones, the Rab molecular switch family, and the UPS system [143]. In addition, adipose triglyceride lipase (ATGL) has been demonstrated to regulate lipophagy by interacting with LC3 [144]. LDs can be directly targeted for degradation by lysosomes. Furthermore, the LD-associated protein perilipins can be degraded by CMA, making LDs more susceptible to lipophagy and lipolytic degradation [145].
Many studies have shown that there is a relationship between AD and autophagy. The accumulation of LDs has been detected in mouse models of AD and the human brain [146]. There is ample evidence that LD accumulation is correlated with the pathology and severity of AD. When neurons are overactive or undergo oxidative stress, LDs accumulate in the neurons and are then transported to the astrocytes for degradation [147]. Interestingly, LD accumulation in the astrocytes has been shown to reduce the impact of ROS, thereby providing an antioxidant defense mechanism [148]. Similarly, the increased ROS production caused by neuronal dysfunction promotes the accumulation of LD in the microglia [149]. Although LDs in the microglia were initially thought to have a protective effect, it has been shown that an accumulation of LDs in the microglia can induce oxidative stress in mouse models [150]. Providing further evidence for the destructive role of LD accumulation in AD, studies have shown that cholesteryl esters in LDs reduce proteasome activity, therefore promoting the accumulation of P-tau [33]. Furthermore, studies have shown that the accumulation of LDs in AD mouse models inhibits the regenerative and homeostatic functions of neural stem cells [146]. There are a large number of LDs in neurons, and the normal metabolism of these lipids is essential for maintaining healthy neuronal function. Several studies have shown that a reduction in the cholesterol content of neurons greatly affects neuronal activity and neurotransmission, resulting in progressive degeneration of dendritic spines and synapses, which is the main characteristic of AD pathogenesis [151,152,153]. Furthermore, sphingomyelinase has been shown to increase neuronal apoptosis by producing the pro-apoptotic molecule ceramide [154,155,156]. Therefore, given the critical role of LD accumulation in AD pathology, lipophagy may represent a novel therapeutic strategy. Indeed, choline supplementation has been explored as a novel AD therapy [157]. Given this evidence, further investigation of the relationship between lipophagy and AD is warranted.
6. Pexophagy
Peroxisome dysfunction appears to be associated with many neurodegenerative diseases, including AD and Parkinson’s disease (PD) [158]. Peroxisomes include enzymes such as catalase (which can break down ROS), glutathione peroxidase (which breaks down hydrogen peroxide), and superoxide dismutase (which breaks down superoxide) [159]. Furthermore, they have been implicated in adipogenesis and ROS signaling in the heart and gut [160,161]. In particular, peroxisomes synthesize the lipids that make up myelin sheaths, cell membranes, and other phospholipids in the neurons. Peroxisome dysfunction impairs neuronal migration and cell membrane synthesis [162,163,164,165].
Pexophagy refers to selective degradation of the peroxisomes by autophagy. Thus, it controls the quality of the peroxisomes [166]. However, pexophagy-specific receptors have not been well studied in mammalian cells. Pexophagy mainly relies on the ubiquitination of peroxisomal proteins in mammals [167,168]. Studies have shown that overexpression of NBR1 and p62 induces peroxisome clustering and degradation. P62 is indispensable for pexophagy, whereas NBR1 overexpression manifests as hyperactivation of pexophagy. p62-NBR1 binding increases the efficiency of NBR1-mediated pexophagy [167]. Studies have shown that peroxisomal biogenesis factor 5 (PEX5) must be ubiquitinated by peroxisomal biogenesis factor (PEX2), an E3 ubiquitin ligase, to initiate mammalian pexophagy. However, a recent study suggested that increased cytoplasmic ROS can stimulate ubiquitination, allowing PEX5 to act as a ROS sensor, subsequently causing pexophagy [168,169,170]. After PEX5 is ubiquitinated, it is recognized by NBR1 or p62, which binds to the autophagosome, and pexophagy occurs [43,167,171].
In certain neurodegenerative diseases, the number and function of peroxisomes may be impaired. In AD, Aβ and tau proteins aggregate in the neurons, and the peroxisomes may be affected. One study has shown that treatment with a peroxisome proliferator, Wy-14.463, in an Aβ overexpressing rat hippocampus, increased peroxidase numbers and catalase activity, reduced ROS production, and produced the denaturing effects of beta-amyloid [172]. In a clinical study, plasma glycogen decreased in postmortem brain samples from AD patients, indicating reduced peroxisome activity or a shortened half-life of plasmalogens [173]. Abnormally reactive peroxisomes lead to excess ROS production, which, in turn, leads to activation of ATM kinase, which promotes phosphorylation and subsequent autoubiquitination of PEX5 to initiate pexophagy [169]. Therefore, as an important mechanism of neurodegenerative diseases, pexophagy may be beneficial in neurodegenerative diseases. However, there is no direct evidence that pexophagy and AD are related. Another gap in the literature is that there are no sex- or age-related studies on peroxisomes in neurological disorders. For example, there are studies on sex differences in response to cerebral ischemia or ischemic stroke, but it is unclear how these sex-related differences specifically affect peroxisomes [174,175,176]. Considering the effects of the peroxisome in the brain, future research on age-related neurological changes should investigate how the peroxisome pathways are affected, particularly in AD.
7. Nucleophagy
Nucleophagy refers to the selective removal of nuclear components by autophagy [177,178]. Mutations in Lamin A/C and Emerin lead to the formation of giant autophagosomes for the clearance of damaged nuclear material, thereby causing envelopathy [179]. The degradation of LMNB1 (Lamin B1) and chromatin during oncogene-induced human cell senescence is mediated by autophagy directly interacting with MAP1LC3B, suggesting the existence of a protective mechanism against tumors [180]. Although there is no evidence of a link between nucleophagy and AD, studies have found that LMNB1 mutation causes human degenerative disease and adult demyelinating leukodystrophy, and that LMNB1 and MAP1LC3B must interact for nucleophagy to occur [180,181,182]. Activation of LMNB1 can significantly delay cell senescence and alleviate degenerative diseases, suggesting that LMNB1-induced nucleophagy may have a protective effect [183,184,185].
8. Lysophagy
Lysophagy refers to damaged lysosomes being encapsulated by autophagosomes and fused with healthy lysosomes through autophagy. At the same time, β-galactoside is released from the damaged lysosome and is sensed by LGALS3/GAL3 (galectin 3), a key marker of lysosomal phagocytosis [186]. In addition, TRIM16, the E3 ligase of the TRIM family, is recruited to LGALS3 and localized to the damaged lysosomes, where it is further ubiquitinated to initiate autophagy, thereby removing the damaged lysosomes [187,188]. Similar to other types of organelle-selective autophagy, it relies on the degradation of p62-MAP1LC3B ubiquitination [186,189]. A novel ubiquitinated glycoprotein, FBXO27, also regulates impaired lysosomal recruitment [190]. In AD models, when lysophagy is damaged, the accumulated proteins cannot be cleared in a timely manner, which aggravates the symptoms of AD. It has been found that Aβ promotes the activation of NLRP3 inflammasomes by inducing lysosomal leakage; this indicates that lysosomal abnormalities in AD lead to inflammatory responses [191]. Moreover, lysosomal dysfunction can lead to neurodegeneration, and some lysosome-related gene mutations, such as valosin-containing protein (VCP), p62, OPTN, or TBK1, can cause lysosomal damage. These mutations have also been confirmed to be involved in the pathogenesis of neurodegenerative diseases [192,193,194]. Therefore, quality control of the lysosomes is crucial in neurodegenerative diseases.
9. Ribophagy
Ribosomes are the main organelles responsible for protein synthesis and translation; hence, they are crucial to cell homeostasis [195]. Generally, ribosome turnover in the cell is controlled by a selective autophagy process, known as ribophagy. Studies have shown that, in yeast, the ubiquitin protease ubiquitin carboxyl-terminal hydrolase 3 (UBP3) and its cofactor, UBP3-associated protein BRE5 (Bre5), participate in this process, which mainly targets the 60S subunit but does not affect the 40S subunit [196]. The recent discovery that USP10 and G3BP1 are homologous genes of UBP3 and Bre5 in mammals suggests that ribophagy is evolutionarily conserved [197]. There is increasing evidence that in mammalian cells, ribosomes are consumed by autophagosomes. Ribosomes are also involved in neurodegeneration, indicating that ribophagy plays a key role in cell function and vitality [198]. Studies have shown that during nutrient starvation, NUFIP1, an LIR motif-containing ribosome receptor, binds to LC3B on autophagosomes, mediates ribosome turnover, and promotes cell survival.
10. Therapeutic Strategies for AD Based on Selective Autophagy
Although the detailed mechanism(s) of selective autophagy in AD remains to be elucidated, enhancing autophagy by genetic manipulation or pharmacological approaches has been beneficial in different AD models. Overexpression of PINK1 restores mitochondrial function, reduces Aβ production and amyloid pathology, and attenuates synaptic and cognitive function by activating mitophagy signaling in APP transgenic mice [199]. In addition, AD is an aging-related disease and aging damages organelles, especially the mitochondria, causing the accumulation of abnormal proteins that damage the quality control of organelles. This undoubtedly plays a great role in the survival and function of neurons, and the clearance of these damaged organelles and proteins will benefit neuron homeostasis. PPAR/PPARα is a transcription factor that regulates neural autophagy in the system, and its mediated autophagy can affect AD. In one study, its agonist, Wy14643, was found to activate autophagy, reduce Aβ protein levels, and treat cognitive impairment in AD mice [200]. In this process, PPAR/PPARα is a peroxisome-related receptor, but it can regulate lipid metabolism-related genes, thereby regulating autophagy in the nervous system, which indicates that in cells, there is a crosslink between different organelles. In AD mice and nematode models, mitochondrial stimuli, such as NAD+ supplementation, urolithin A, and actinonin, increased PINK1 and Parkin-dependent mitophagy and alleviated AD pathology, suggesting that the removal of damaged mitochondria can act as a potential therapeutic strategy [201]. Furthermore, studies have found that microRNA can treat AD by enhancing autophagy and improving synaptic function [202]. However, it is not clear whether these microRNA participate in selective autophagy. Moreover, in the latest research, it was found that damage to the lysosome can cause synaptic dysfunction, which can cause nervous system-related diseases [203]. Lysosomes are the most critical degradation centers for all kinds of autophagy, so clearing damaged lysosomes and maintain healthy lysophagy quality will play an important role in AD treatment. A study found that impaired CMA caused neuronal dysfunction, increased protein toxicity, and neurological disorders, while chemical enhancement of CMA delayed the onset of AD in mice model [204]. This also implies that we can analyze its structure and function according to the CMA-specific receptors, find specific targets, conduct drug development, and specifically enhance the function of the CMA, which is a strategy for treating AD.
11. Discussion
Current studies have indicated that multiple autophagies may together contribute to the pathogenesis of AD. An increase in aggregating proteins will cause cytotoxicity and damage mitophagy, while damage to the mitochondria will aggravate the pathology of AD, forming a vicious cycle and causing damage to the body. Impaired mitochondrial function can also lead to changes in other organelles, such as reduced energy synthesis, reduced endoplasmic reticulum protein processing, and decreased synthesis of degrading enzymes, resulting in the accumulation of damaged proteins [205]. Studies have found that reticulophagy may play a protective role in AD patients, and the accumulation of toxic proteins can lead to positive feedback regulation of the ER, which degrades the damaged ER and misfolded proteins through macroautophagy and CMA.
In the subtypes of selective autophagy, the identification of AD-related specific receptors is a big challenge. For aggrephagy, several receptors have been confirmed, such as p62, NBR1, ALFY, and OPTN [206]. However, we need to further determine whether the degradation of Aβ and PHF-tau aggregates, and TNF are receptor-specific. If so, drugs that target specific receptors can be discovered and studied to promote degradation, which would then become a viable strategy for treating AD. For mitophagy, post-translational modifications (PTMs) are regarded as a key mechanism [207]. In addition, PINK1, BNIP3L, BNIP3, FUNDC1, NIPSNAP1, NIPSNAP2, BCL2L13, prohibitin 2, MCL-1, OPTN, and FKBP prolyl isomerase 8 (FKBP8) [208,209] have been identified as receptors. However, only a few receptors have been reported to be involved in the pathogenesis of AD. Are there other mitophagy receptors that mediate the clearance of damaged mitochondria in AD? With regard to reticulophagy and lipophagy, while there is very little evidence of their involvement in the pathogenesis of AD, ER stress, ER injury, and mutations in the reticulophagy-related receptor RTN3 have been demonstrated to be associated with AD pathogenesis [210]. Enhanced lipophagy can reduce the accumulation of lipid droplets and thereby reduce the neuronal neurodegeneration caused by an accumulation of dihydroceramide desaturase [211]. Therefore, more evidence is needed to support the involvement of reticulophagy and lipophagy in the pathogenesis of AD. Overall, the discovery of specific clearance mechanisms for these damaged organelles will provide new targets for the treatment of AD. Here, we have listed the related receptors in selective autophagy in AD (Table 1).
Table 1.
List of selective autophagy receptors in the pathogenesis of AD.
| Selective Autophagy | Receptor | References | AD-Related Receptor |
|---|---|---|---|
| Aggrephagy | P62; NBR1; ALFY Hsc70; CHIP OPTN; TOLLIP TAX1 binding protein 1 |
[38,39] [57] [212,213] [214] |
P62; NBR1; ALFY Hsc70; CHIP |
| Mitophagy | PINK1/Parkin VDAC; RHOT1 MFN1/2; BNIP3L FUNDC1; BNIP3 AMBRA1; BCL2LI3 FKBP8; CHDHD ISC1; PHB2 Cardiolipin; NIPSNAP1/2 NDP52; OPTN MCL-1; P62 |
[201,215] [216,217] [218,219] [208,220] [221,222] [223,224] [225,226] [227,228] [229,230] [231,232] |
PINK1/Parkin MCL-1; DISC1 |
| Reticulophagy | FAM134B.; SEC62 CCPG1; RTN3 ATL3 |
[233,234] [32,210,235] [236] |
RTN3 |
| Lipophagy | ATGL | [144] | - |
| Pexophagy | NBR1; P62; ABCD3 |
[167] [237] |
- |
| Nucleophagy | Atg39 | [238] | - |
| Lysophagy | Galectin 3 | [186] | - |
| Ribophagy | NUFIP1 | [239] | - |
In macroautophagy, substrates are recognized by different receptors in different selective autophagy pathways for degradation. Furthermore, at least 30% of the protein degradation process is through CMA, which is also lysosome-dependent and highly selective. The misfolded protein is further identified by Hsc70 by attaching a KFERQ motif, and is degraded by the lysosomal receptor Lamp2A. How does the cell recognize and maintain its specificity? This needs to be studied further, but it gives us a new way to focus on the receptor. Is it the structure of the receptor that determines this process and is there a propensity to degrade the damaged protein under certain conditions? In one recent study, APP protein was found to be the receptor of CMA [240], and APP could conduct both macroautophagy and CMA. However, how to conduct macroautophagy and CMA, and whether there is a priority between the two are problems to be solved in the future.
Finding the specific receptors will be the key point for promoting selective autophagy in AD. Therefore, further studies to find other autophagy-related receptors, develop specific drugs, or discover crosslinks between different subtypes of selective autophagy should provide new approaches for the treatment of AD.
Acknowledgments
We would like to thank Carol Chu for her enormous support in ordering reagents and managing our lab needs. We would also like to thank Martha Dahlen for English editing. Figures were created with BioRender (https://biorender.com, accessed on 20 March 2022).
Abbreviations
| AD | Alzheimer’s disease |
| Aβ | amyloid β-protein |
| APP | amyloid precursor protein |
| Atg8 | autophagy-related protein 8 |
| AVs | autophagic vacuoles |
| APLP1 | amyloid beta precursor-like protein 1 |
| Atg39 | autophagy-related protein 39 |
| ALFY | WD repeat and FYVE domain containing 3 |
| ATGL | adipose triglyceride lipase |
| ATM | ataxia-telangiectasia mutated |
| BNIP3 | E1B 19 kDa protein-interacting protein 3 |
| BNIP3L | adenovirus E1B 19kDa interacting protein 3-like |
| Bre5 | UBP3-associated protein BRE5 |
| BACE1 | beta-site APP-cleaving enzyme 1 |
| CMA | chaperone-mediated autophagy |
| CHIP | C-terminus of Hsc70-interacting protein |
| CCPG1 | cell cycle progression protein 1 |
| ER | endoplasmic reticulum |
| ERAD | ER-associated degradation |
| FIP200 | focal adhesion kinase family-interacting protein of 200 kDa |
| FBXO27 | F-box protein |
| FKBP8 | FKBP prolyl isomerase 8 |
| G3BP1 | G3BP stress granule assembly factor 1 |
| Galectin 3 | LGALS3/GAL3 |
| TRIM16 | tripartite motif containing 16 |
| HDAC6 | histone deacetylase 6 |
| Hsc70 | heat shock cognate protein 70 |
| HSP60 | heat shock cognate protein 60 |
| HSP90 | heat shock cognate protein 90 |
| HSPs | heat shock proteins |
| LDs | lipid droplets |
| LMNB1 | lamin B1 protein |
| LC3 | microtubule-associated proteins light chain 3 |
| MFN1/2 | mitofusin 1 and 2 |
| Drp1 | dynamin-related protein 1 |
| NUFIP1 | nuclear fragile X mental retardation-interacting protein 1 |
| NM-DARS | n-methyl-D-aspartate receptors |
| NFTs | neurofibrillary tangles |
| Nvj1 | nucleus–vacuole junction protein 1 |
| NBR1 | neighbor of BRCA1 gene 1 |
| NLRP3 | NLR family pyrin domain containing 3 |
| Opa1 | optic atrophy 1 |
| PHFs | paired helical filaments |
| PINK1 | PTEN-induced kinase 1 |
| PGC-1-alpha | peroxisome proliferator-activated receptor gamma coactivator 1 |
| PTMs | post-translational modifications |
| PEX5 | peroxisomal biogenesis factor 5 |
| PEX2 | peroxisomal biogenesis factor 2 |
| PD | Parkinson’s disease |
| PPAR/PPARα | peroxisome proliferator activated receptor alpha |
| PI3P | phosphatidylinositol 3-phosphate |
| P-tau | phosphorylated tau |
| ROS | reactive oxygen species |
| RTN3 | reticulon 3 |
| P62 | SQSTM1-p62 |
| SEC62 | preprotein translocation factor |
| RB1CC1 | RB1-inducible coiled-coil 1 |
| TBK1 | serine/threonine protein kinase |
| TCA | tricarboxylic acid cycle |
| UPS | ubiquitin–proteasome system |
| UBA | ubiquitin-associated domains |
| UCHL1 | ubiquitin carboxyl-terminal hydrolase L1 |
| ULK1 | Unc-51-like autophagy activating kinase 1 |
| UBP3 | ubiquitin carboxyl-terminal hydrolase 3 |
| USP10 | ubiquitin-specific protease 10 |
| UPR | unfolding protein response |
| VDAC1 | voltage-dependent anion-selective channel 1 |
| VPS34 | vacuolar protein sorting 34 |
| Vac8 | vacuole related 8 |
| VCP | valosin-containing protein. |
Author Contributions
The research study was conceived and conceptualized, and funding was obtained by K.-H.C., M.L. and J.T.; manuscript drafting, literature collection, and manuscript editing: X.G., A.I., S.G.S. and C.S. Z.Z., J.L. (Jia Liu), Y.K., A.I. and S.G.S. helped organize the manuscript and provided technical support. Manuscript review and editing: A.I., S.G.S., J.L. (Jiahong Lu), J.T. and M.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Shenzhen Science and Technology Innovation Commission, grant number (JCYJ20180302174028790, JCYJ20180507184656626); the Hong Kong Baptist University, grant number (HKBU/RC-IRCs/17-18/03, IRCMS/19-20/H02); the National Natural Science Foundation of China, grant number (81703487, 81773926); the Hong Kong Health and Medical Research Fund, grant number (HMRF17182541, HMRF17182551, HMRF 19200721); the National Natural Science Foundation of China, grant number (82171258); the Department of Science and Technology of Hunan Province, grant number (the Innovative Team Program 2019RS1010); Central South University, grant number (the Innovation-Driven Team Project 2020CX016); Hong Kong General Research Fund, grant number (GRF/HKBU12100618).
Conflicts of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moreira P.I., Santos R.X., Zhu X., Lee H.G., Smith M.A., Casadesus G., Perry G. Autophagy in Alzheimer’s disease. Expert Rev. Neurother. 2010;10:1209–1218. doi: 10.1586/ern.10.84. [DOI] [PubMed] [Google Scholar]
- 2.Querfurth H.W., LaFerla F.M. Alzheimer’s disease. N. Engl. J. Med. 2010;362:329–344. doi: 10.1056/NEJMra0909142. [DOI] [PubMed] [Google Scholar]
- 3.Selkoe D.J., Hardy J. The amyloid hypothesis of Alzheimer’s disease at 25 years. EMBO Mol. Med. 2016;8:595–608. doi: 10.15252/emmm.201606210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorszewska J., Prendecki M., Oczkowska A., Dezor M., Kozubski W. Molecular Basis of Familial and Sporadic Alzheimer’s Disease. Curr. Alzheimer Res. 2016;13:952–963. doi: 10.2174/1567205013666160314150501. [DOI] [PubMed] [Google Scholar]
- 5.Kelley B.J., Petersen R.C. Alzheimer’s disease and mild cognitive impairment. Neurol. Clin. 2007;25:577–609. doi: 10.1016/j.ncl.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thinakaran G., Koo E.H. Amyloid precursor protein trafficking, processing, and function. J. Biol. Chem. 2008;283:29615–29619. doi: 10.1074/jbc.R800019200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schindowski K., Bretteville A., Leroy K., Begard S., Brion J.P., Hamdane M., Buee L. Alzheimer’s disease-like tau neuropathology leads to memory deficits and loss of functional synapses in a novel mutated tau transgenic mouse without any motor deficits. Am. J. Pathol. 2006;169:599–616. doi: 10.2353/ajpath.2006.060002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yin X., Qiu Y., Zhao C., Zhou Z., Bao J., Qian W. The Role of Amyloid-Beta and Tau in the Early Pathogenesis of Alzheimer’s Disease. Med. Sci. Monit. 2021;27:e933084. doi: 10.12659/MSM.933084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malampati S., Song J.X., Chun-Kit Tong B., Nalluri A., Yang C.B., Wang Z., Gopalkrishnashetty Sreenivasmurthy S., Zhu Z., Liu J., Su C., et al. Targeting Aggrephagy for the Treatment of Alzheimer’s Disease. Cells. 2020;9:311. doi: 10.3390/cells9020311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nixon R.A., Wegiel J., Kumar A., Yu W.H., Peterhoff C., Cataldo A., Cuervo A.M. Extensive involvement of autophagy in Alzheimer disease: An immuno-electron microscopy study. J. Neuropathol. Exp. Neurol. 2005;64:113–122. doi: 10.1093/jnen/64.2.113. [DOI] [PubMed] [Google Scholar]
- 11.Lucin K.M., O’Brien C.E., Bieri G., Czirr E., Mosher K.I., Abbey R.J., Mastroeni D.F., Rogers J., Spencer B., Masliah E., et al. Microglial beclin 1 regulates retromer trafficking and phagocytosis and is impaired in Alzheimer’s disease. Neuron. 2013;79:873–886. doi: 10.1016/j.neuron.2013.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pickford F., Masliah E., Britschgi M., Lucin K., Narasimhan R., Jaeger P.A., Small S., Spencer B., Rockenstein E., Levine B., et al. The autophagy-related protein beclin 1 shows reduced expression in early Alzheimer disease and regulates amyloid beta accumulation in mice. J. Clin. Investig. 2008;118:2190–2199. doi: 10.1172/JCI33585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rohn T.T., Wirawan E., Brown R.J., Harris J.R., Masliah E., Vandenabeele P. Depletion of Beclin-1 due to proteolytic cleavage by caspases in the Alzheimer’s disease brain. Neurobiol. Dis. 2011;43:68–78. doi: 10.1016/j.nbd.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morel E., Chamoun Z., Lasiecka Z.M., Chan R.B., Williamson R.L., Vetanovetz C., Dall’Armi C., Simoes S., Point Du Jour K.S., McCabe B.D., et al. Phosphatidylinositol-3-phosphate regulates sorting and processing of amyloid precursor protein through the endosomal system. Nat. Commun. 2013;4:2250. doi: 10.1038/ncomms3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chung K.M., Hernandez N., Sproul A.A., Yu W.H. Alzheimer’s disease and the autophagic-lysosomal system. Neurosci. Lett. 2019;697:49–58. doi: 10.1016/j.neulet.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 16.Song J.X., Malampati S., Zeng Y., Durairajan S.S.K., Yang C.B., Tong B.C., Iyaswamy A., Shang W.B., Sreenivasmurthy S.G., Zhu Z., et al. A small molecule transcription factor EB activator ameliorates beta-amyloid precursor protein and Tau pathology in Alzheimer’s disease models. Aging Cell. 2020;19:e13069. doi: 10.1111/acel.13069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iyaswamy A., Krishnamoorthi S.K., Zhang H., Sreenivasmurthy S.G., Zhu Z., Liu J., Su C.F., Guan X.J., Wang Z.Y., Cheung K.H., et al. Qingyangshen mitigates amyloid-beta and Tau aggregate defects involving PPARalpha-TFEB activation in transgenic mice of Alzheimer’s disease. Phytomedicine. 2021;91:153648. doi: 10.1016/j.phymed.2021.153648. [DOI] [PubMed] [Google Scholar]
- 18.Iyaswamy A., Krishnamoorthi S.K., Song J.X., Yang C.B., Kaliyamoorthy V., Zhang H., Sreenivasmurthy S.G., Malampati S., Wang Z.Y., Zhu Z., et al. NeuroDefend, a novel Chinese medicine, attenuates amyloid-beta and tau pathology in experimental Alzheimer’s disease models. J. Food Drug Anal. 2020;28:132–146. doi: 10.1016/j.jfda.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Sreenivasmurthy S.G., Iyaswamy A., Krishnamoorthi S., Senapati S., Malampati S., Zhu Z., Su C.F., Liu J., Guan X.J., Tong B.C., et al. Protopine promotes the proteasomal degradation of pathological tau in Alzheimer’s disease models via HDAC6 inhibition. Phytomedicine. 2022;96:153887. doi: 10.1016/j.phymed.2021.153887. [DOI] [PubMed] [Google Scholar]
- 20.Iyaswamy A., Krishnamoorthi S.K., Liu Y.W., Song J.X., Kammala A.K., Sreenivasmurthy S.G., Malampati S., Tong B.C.K., Selvarasu K., Cheung K.H., et al. Yuan-Hu Zhi Tong Prescription Mitigates Tau Pathology and Alleviates Memory Deficiency in the Preclinical Models of Alzheimer’s Disease. Front. Pharmacol. 2020;11:584770. doi: 10.3389/fphar.2020.584770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yao R.Q., Ren C., Xia Z.F., Yao Y.M. Organelle-specific autophagy in inflammatory diseases: A potential therapeutic target underlying the quality control of multiple organelles. Autophagy. 2021;17:385–401. doi: 10.1080/15548627.2020.1725377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Settembre C., Fraldi A., Medina D.L., Ballabio A. Signals from the lysosome: A control centre for cellular clearance and energy metabolism. Nat. Rev. Mol. Cell Biol. 2013;14:283–296. doi: 10.1038/nrm3565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jin M., Liu X., Klionsky D.J. SnapShot: Selective autophagy. Cell. 2013;152:368. doi: 10.1016/j.cell.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marzella L., Ahlberg J., Glaumann H. Autophagy, heterophagy, microautophagy and crinophagy as the means for intracellular degradation. Virchows Arch. B Cell Pathol. Incl. Mol. Pathol. 1981;36:219–234. doi: 10.1007/BF02912068. [DOI] [PubMed] [Google Scholar]
- 25.Kaushik S., Cuervo A.M. Chaperone-mediated autophagy: A unique way to enter the lysosome world. Trends Cell Biol. 2012;22:407–417. doi: 10.1016/j.tcb.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scrivo A., Bourdenx M., Pampliega O., Cuervo A.M. Selective autophagy as a potential therapeutic target for neurodegenerative disorders. Lancet Neurol. 2018;17:802–815. doi: 10.1016/S1474-4422(18)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun-Wang J.L., Yarritu-Gallego A., Ivanova S., Zorzano A. The ubiquitin-proteasome system and autophagy: Self-digestion for metabolic health. Trends Endocrinol. Metab. 2021;32:594–608. doi: 10.1016/j.tem.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 28.Reddy P.H., Oliver D.M. Amyloid Beta and Phosphorylated Tau-Induced Defective Autophagy and Mitophagy in Alzheimer’s Disease. Cells. 2019;8:488. doi: 10.3390/cells8050488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou F., van Laar T., Huang H., Zhang L. APP and APLP1 are degraded through autophagy in response to proteasome inhibition in neuronal cells. Protein Cell. 2011;2:377–383. doi: 10.1007/s13238-011-1047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fang E.F. Mitophagy and NAD(+) inhibit Alzheimer disease. Autophagy. 2019;15:1112–1114. doi: 10.1080/15548627.2019.1596497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakashima A., Shima T., Tsuda S., Aoki A., Kawaguchi M., Furuta A., Yasuda I., Yoneda S., Yamaki-Ushijima A., Cheng S.B., et al. Aggrephagy Deficiency in the Placenta: A New Pathogenesis of Preeclampsia. Int. J. Mol. Sci. 2021;22:2432. doi: 10.3390/ijms22052432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi Q., Prior M., He W., Tang X., Hu X., Yan R. Reduced amyloid deposition in mice overexpressing RTN3 is adversely affected by preformed dystrophic neurites. J. Neurosci. 2009;29:9163–9173. doi: 10.1523/JNEUROSCI.5741-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van der Kant R., Langness V.F., Herrera C.M., Williams D.A., Fong L.K., Leestemaker Y., Steenvoorden E., Rynearson K.D., Brouwers J.F., Helms J.B., et al. Cholesterol Metabolism Is a Druggable Axis that Independently Regulates Tau and Amyloid-beta in iPSC-Derived Alzheimer’s Disease Neurons. Cell Stem Cell. 2019;24:363–375. doi: 10.1016/j.stem.2018.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shankar G.M., Li S., Mehta T.H., Garcia-Munoz A., Shepardson N.E., Smith I., Brett F.M., Farrell M.A., Rowan M.J., Lemere C.A., et al. Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat. Med. 2008;14:837–842. doi: 10.1038/nm1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De S., Wirthensohn D.C., Flagmeier P., Hughes C., Aprile F.A., Ruggeri F.S., Whiten D.R., Emin D., Xia Z., Varela J.A., et al. Different soluble aggregates of Abeta42 can give rise to cellular toxicity through different mechanisms. Nat. Commun. 2019;10:1541. doi: 10.1038/s41467-019-09477-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fusco G., Chen S.W., Williamson P.T.F., Cascella R., Perni M., Jarvis J.A., Cecchi C., Vendruscolo M., Chiti F., Cremades N., et al. Structural basis of membrane disruption and cellular toxicity by alpha-synuclein oligomers. Science. 2017;358:1440–1443. doi: 10.1126/science.aan6160. [DOI] [PubMed] [Google Scholar]
- 37.Gatica D., Lahiri V., Klionsky D.J. Cargo recognition and degradation by selective autophagy. Nat. Cell Biol. 2018;20:233–242. doi: 10.1038/s41556-018-0037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Finley K.D., Edeen P.T., Cumming R.C., Mardahl-Dumesnil M.D., Taylor B.J., Rodriguez M.H., Hwang C.E., Benedetti M., McKeown M. blue cheese mutations define a novel, conserved gene involved in progressive neural degeneration. J. Neurosci. 2003;23:1254–1264. doi: 10.1523/JNEUROSCI.23-04-01254.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramesh Babu J., Lamar Seibenhener M., Peng J., Strom A.L., Kemppainen R., Cox N., Zhu H., Wooten M.C., Diaz-Meco M.T., Moscat J., et al. Genetic inactivation of p62 leads to accumulation of hyperphosphorylated tau and neurodegeneration. J. Neurochem. 2008;106:107–120. doi: 10.1111/j.1471-4159.2008.05340.x. [DOI] [PubMed] [Google Scholar]
- 40.Johansen T., Lamark T. Selective autophagy mediated by autophagic adapter proteins. Autophagy. 2011;7:279–296. doi: 10.4161/auto.7.3.14487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bjorkoy G., Lamark T., Brech A., Outzen H., Perander M., Overvatn A., Stenmark H., Johansen T. p62/SQSTM1 forms protein aggregates degraded by autophagy and has a protective effect on huntingtin-induced cell death. J. Cell Biol. 2005;171:603–614. doi: 10.1083/jcb.200507002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ichimura Y., Kumanomidou T., Sou Y.S., Mizushima T., Ezaki J., Ueno T., Kominami E., Yamane T., Tanaka K., Komatsu M. Structural basis for sorting mechanism of p62 in selective autophagy. J. Biol Chem. 2008;283:22847–22857. doi: 10.1074/jbc.M802182200. [DOI] [PubMed] [Google Scholar]
- 43.Kirkin V., Lamark T., Sou Y.S., Bjorkoy G., Nunn J.L., Bruun J.A., Shvets E., McEwan D.G., Clausen T.H., Wild P., et al. A role for NBR1 in autophagosomal degradation of ubiquitinated substrates. Mol. Cell. 2009;33:505–516. doi: 10.1016/j.molcel.2009.01.020. [DOI] [PubMed] [Google Scholar]
- 44.Pankiv S., Clausen T.H., Lamark T., Brech A., Bruun J.A., Outzen H., Overvatn A., Bjorkoy G., Johansen T. p62/SQSTM1 binds directly to Atg8/LC3 to facilitate degradation of ubiquitinated protein aggregates by autophagy. J. Biol. Chem. 2007;282:24131–24145. doi: 10.1074/jbc.M702824200. [DOI] [PubMed] [Google Scholar]
- 45.Ciechanover A. Intracellular protein degradation: From a vague idea thru the lysosome and the ubiquitin-proteasome system and onto human diseases and drug targeting. Best Pract. Res. Clin. Haematol. 2017;30:341–355. doi: 10.1016/j.beha.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 46.Mogk A., Bukau B. Role of sHsps in organizing cytosolic protein aggregation and disaggregation. Cell Stress Chaperones. 2017;22:493–502. doi: 10.1007/s12192-017-0762-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ungelenk S., Moayed F., Ho C.T., Grousl T., Scharf A., Mashaghi A., Tans S., Mayer M.P., Mogk A., Bukau B. Small heat shock proteins sequester misfolding proteins in near-native conformation for cellular protection and efficient refolding. Nat. Commun. 2016;7:13673. doi: 10.1038/ncomms13673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grumati P., Dikic I. Ubiquitin signaling and autophagy. J. Biol. Chem. 2018;293:5404–5413. doi: 10.1074/jbc.TM117.000117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Peng J., Schwartz D., Elias J.E., Thoreen C.C., Cheng D., Marsischky G., Roelofs J., Finley D., Gygi S.P. A proteomics approach to understanding protein ubiquitination. Nat. Biotechnol. 2003;21:921–926. doi: 10.1038/nbt849. [DOI] [PubMed] [Google Scholar]
- 50.Ikeda F., Dikic I. Atypical ubiquitin chains: New molecular signals. ‘Protein Modifications: Beyond the Usual Suspects’ review series. EMBO Rep. 2008;9:536–542. doi: 10.1038/embor.2008.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu M., Williamson N., Mishra A., Michel C.H., Kaminski C.F., Tunnacliffe A., Kaminski Schierle G.S. Structural progression of amyloid-beta Arctic mutant aggregation in cells revealed by multiparametric imaging. J. Biol. Chem. 2019;294:1478–1487. doi: 10.1074/jbc.RA118.004511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hong L., Huang H.C., Jiang Z.F. Relationship between amyloid-beta and the ubiquitin-proteasome system in Alzheimer’s disease. Neurol. Res. 2014;36:276–282. doi: 10.1179/1743132813Y.0000000288. [DOI] [PubMed] [Google Scholar]
- 53.Morimoto D., Walinda E., Fukada H., Sou Y.S., Kageyama S., Hoshino M., Fujii T., Tsuchiya H., Saeki Y., Arita K., et al. The unexpected role of polyubiquitin chains in the formation of fibrillar aggregates. Nat. Commun. 2015;6:6116. doi: 10.1038/ncomms7116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Iqbal K., Alonso A.C., Gong C.X., Khatoon S., Pei J.J., Wang J.Z., Grundke-Iqbal I. Mechanisms of neurofibrillary degeneration and the formation of neurofibrillary tangles. J. Neural. Transm. Suppl. 1998;53:169–180. doi: 10.1007/978-3-7091-6467-9_15. [DOI] [PubMed] [Google Scholar]
- 55.Brunden K.R., Trojanowski J.Q., Lee V.M. Advances in tau-focused drug discovery for Alzheimer’s disease and related tauopathies. Nat. Rev. Drug Discov. 2009;8:783–793. doi: 10.1038/nrd2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guo J.L., Buist A., Soares A., Callaerts K., Calafate S., Stevenaert F., Daniels J.P., Zoll B.E., Crowe A., Brunden K.R., et al. The Dynamics and Turnover of Tau Aggregates in Cultured Cells: Insights into Therapies for Tauopathies. J. Biol. Chem. 2016;291:13175–13193. doi: 10.1074/jbc.M115.712083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hatakeyama S., Matsumoto M., Kamura T., Murayama M., Chui D.H., Planel E., Takahashi R., Nakayama K.I., Takashima A. U-box protein carboxyl terminus of Hsc70-interacting protein (CHIP) mediates poly-ubiquitylation preferentially on four-repeat Tau and is involved in neurodegeneration of tauopathy. J. Neurochem. 2004;91:299–307. doi: 10.1111/j.1471-4159.2004.02713.x. [DOI] [PubMed] [Google Scholar]
- 58.Demishtein A., Fraiberg M., Berko D., Tirosh B., Elazar Z., Navon A. SQSTM1/p62-mediated autophagy compensates for loss of proteasome polyubiquitin recruiting capacity. Autophagy. 2017;13:1697–1708. doi: 10.1080/15548627.2017.1356549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Guthrie C.R., Kraemer B.C. Proteasome inhibition drives HDAC6-dependent recruitment of tau to aggresomes. J. Mol. Neurosci. 2011;45:32–41. doi: 10.1007/s12031-011-9502-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leyk J., Goldbaum O., Noack M., Richter-Landsberg C. Inhibition of HDAC6 modifies tau inclusion body formation and impairs autophagic clearance. J. Mol. Neurosci. 2015;55:1031–1046. doi: 10.1007/s12031-014-0460-y. [DOI] [PubMed] [Google Scholar]
- 61.Bishop P., Rocca D., Henley J.M. Ubiquitin C-terminal hydrolase L1 (UCH-L1): Structure, distribution and roles in brain function and dysfunction. Biochem. J. 2016;473:2453–2462. doi: 10.1042/BCJ20160082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xie M., Han Y., Yu Q., Wang X., Wang S., Liao X. UCH-L1 Inhibition Decreases the Microtubule-Binding Function of Tau Protein. J. Alzheimers Dis. 2016;49:353–363. doi: 10.3233/JAD-150032. [DOI] [PubMed] [Google Scholar]
- 63.Yu Q., Zhang H., Li Y., Liu C., Wang S., Liao X. UCH-L1 Inhibition Suppresses tau Aggresome Formation during Proteasomal Impairment. Mol. Neurobiol. 2018;55:3812–3821. doi: 10.1007/s12035-017-0558-7. [DOI] [PubMed] [Google Scholar]
- 64.Mattson M.P., Gleichmann M., Cheng A. Mitochondria in Neuroplasticity and Neurological Disorders. Neuron. 2008;60:748–766. doi: 10.1016/j.neuron.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stockburger C., Eckert S., Eckert G.P., Friedland K., Muller W.E. Mitochondrial Function, Dynamics, and Permeability Transition: A Complex Love Triangle as A Possible Target for the Treatment of Brain Aging and Alzheimer’s Disease. J. Alzheimers Dis. 2018;64:S455–S467. doi: 10.3233/JAD-179915. [DOI] [PubMed] [Google Scholar]
- 66.Green D.R., Van Houten B. SnapShot: Mitochondrial Quality Control. Cell. 2011;147:950. doi: 10.1016/j.cell.2011.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Anzell A.R., Maizy R., Przyklenk K., Sanderson T.H. Mitochondrial Quality Control and Disease: Insights into Ischemia-Reperfusion Injury. Mol. Neurobiol. 2018;55:2547–2564. doi: 10.1007/s12035-017-0503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Reddy P.H., Tripathi R., Troung Q., Tirumala K., Reddy T.P., Anekonda V., Shirendeb U.P., Calkins M.J., Reddy A.P., Mao P., et al. Abnormal mitochondrial dynamics and synaptic degeneration as early events in Alzheimer’s disease: Implications to mitochondria-targeted antioxidant therapeutics. Biochim. Biophys. Acta. 2012;1822:639–649. doi: 10.1016/j.bbadis.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Santos R.X., Correia S.C., Wang X., Perry G., Smith M.A., Moreira P.I., Zhu X. A synergistic dysfunction of mitochondrial fission/fusion dynamics and mitophagy in Alzheimer’s disease. J. Alzheimers Dis. 2010;20((Suppl. S2)):S401–S412. doi: 10.3233/JAD-2010-100666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Swerdlow R.H., Khan S.M. A “mitochondrial cascade hypothesis” for sporadic Alzheimer’s disease. Med. Hypotheses. 2004;63:8–20. doi: 10.1016/j.mehy.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 71.Swerdlow R.H., Burns J.M., Khan S.M. The Alzheimer’s disease mitochondrial cascade hypothesis: Progress and perspectives. Biochim. Biophys. Acta. 2014;1842:1219–1231. doi: 10.1016/j.bbadis.2013.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Moreira P.I., Siedlak S.L., Wang X., Santos M.S., Oliveira C.R., Tabaton M., Nunomura A., Szweda L.I., Aliev G., Smith M.A., et al. Autophagocytosis of mitochondria is prominent in Alzheimer disease. J. Neuropathol. Exp. Neurol. 2007;66:525–532. doi: 10.1097/01.jnen.0000240476.73532.b0. [DOI] [PubMed] [Google Scholar]
- 73.Moreira P.I., Siedlak S.L., Wang X., Santos M.S., Oliveira C.R., Tabaton M., Nunomura A., Szweda L.I., Aliev G., Smith M.A., et al. Increased autophagic degradation of mitochondria in Alzheimer disease. Autophagy. 2007;3:614–615. doi: 10.4161/auto.4872. [DOI] [PubMed] [Google Scholar]
- 74.Hirai K., Aliev G., Nunomura A., Fujioka H., Russell R.L., Atwood C.S., Johnson A.B., Kress Y., Vinters H.V., Tabaton M., et al. Mitochondrial abnormalities in Alzheimer’s disease. J. Neurosci. 2001;21:3017–3023. doi: 10.1523/JNEUROSCI.21-09-03017.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang W., Yin J., Ma X., Zhao F., Siedlak S.L., Wang Z., Torres S., Fujioka H., Xu Y., Perry G., et al. Inhibition of mitochondrial fragmentation protects against Alzheimer’s disease in rodent model. Hum. Mol. Genet. 2017;26:4118–4131. doi: 10.1093/hmg/ddx299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Martin-Maestro P., Gargini R., Perry G., Avila J., Garcia-Escudero V. PARK2 enhancement is able to compensate mitophagy alterations found in sporadic Alzheimer’s disease. Hum. Mol. Genet. 2016;25:792–806. doi: 10.1093/hmg/ddv616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nguyen T.N., Padman B.S., Lazarou M. Deciphering the Molecular Signals of PINK1/Parkin Mitophagy. Trends Cell Biol. 2016;26:733–744. doi: 10.1016/j.tcb.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 78.Medala V.K., Gollapelli B., Dewanjee S., Ogunmokun G., Kandimalla R., Vallamkondu J. Mitochondrial dysfunction, mitophagy, and role of dynamin-related protein 1 in Alzheimer’s disease. J. Neurosci. Res. 2021;99:1120–1135. doi: 10.1002/jnr.24781. [DOI] [PubMed] [Google Scholar]
- 79.Kerr J.S., Adriaanse B.A., Greig N.H., Mattson M.P., Cader M.Z., Bohr V.A., Fang E.F. Mitophagy and Alzheimer’s Disease: Cellular and Molecular Mechanisms. Trends Neurosci. 2017;40:151–166. doi: 10.1016/j.tins.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wimo A., Jonsson L., Bond J., Prince M., Winblad B., Alzheimer Disease I. The worldwide economic impact of dementia 2010. Alzheimers Dement. 2013;9:1–11. doi: 10.1016/j.jalz.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 81.Lopez O.L., Becker J.T., Sweet R.A., Klunk W., Kaufer D.I., Saxton J., Habeych M., DeKosky S.T. Psychiatric symptoms vary with the severity of dementia in probable Alzheimer’s disease. J. Neuropsychiatry Clin. Neurosci. 2003;15:346–353. doi: 10.1176/jnp.15.3.346. [DOI] [PubMed] [Google Scholar]
- 82.van der Flier W.M., Scheltens P. Epidemiology and risk factors of dementia. J. Neurol. Neurosurg. Psychiatry. 2005;76((Suppl. S5)):v2–v7. doi: 10.1136/jnnp.2005.082867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Reitz C., Brayne C., Mayeux R. Epidemiology of Alzheimer disease. Nat. Rev. Neurol. 2011;7:137–152. doi: 10.1038/nrneurol.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kapogiannis D., Mattson M.P. Disrupted energy metabolism and neuronal circuit dysfunction in cognitive impairment and Alzheimer’s disease. Lancet Neurol. 2011;10:187–198. doi: 10.1016/S1474-4422(10)70277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dong Y., Brewer G.J. Global Metabolic Shifts in Age and Alzheimer’s Disease Mouse Brains Pivot at NAD+/NADH Redox Sites. J. Alzheimers Dis. 2019;71:119–140. doi: 10.3233/JAD-190408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.The Canadian Study of Health and Aging: Risk factors for Alzheimer’s disease in Canada. Neurology. 1994;44:2073–2080. doi: 10.1212/WNL.44.11.2073. [DOI] [PubMed] [Google Scholar]
- 87.Rona-Voros K., Weydt P. The role of PGC-1alpha in the pathogenesis of neurodegenerative disorders. Curr. Drug Targets. 2010;11:1262–1269. doi: 10.2174/1389450111007011262. [DOI] [PubMed] [Google Scholar]
- 88.Cenini G., Voos W. Mitochondria as Potential Targets in Alzheimer Disease Therapy: An Update. Front. Pharmacol. 2019;10:902. doi: 10.3389/fphar.2019.00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fratiglioni L., De Ronchi D., Aguero-Torres H. Worldwide prevalence and incidence of dementia. Drugs Aging. 1999;15:365–375. doi: 10.2165/00002512-199915050-00004. [DOI] [PubMed] [Google Scholar]
- 90.Lindsay J., Hebert R., Rockwood K. The Canadian Study of Health and Aging: Risk factors for vascular dementia. Stroke. 1997;28:526–530. doi: 10.1161/01.STR.28.3.526. [DOI] [PubMed] [Google Scholar]
- 91.Hebert R., Lindsay J., Verreault R., Rockwood K., Hill G., Dubois M.F. Vascular dementia: Incidence and risk factors in the Canadian study of health and aging. Stroke. 2000;31:1487–1493. doi: 10.1161/01.STR.31.7.1487. [DOI] [PubMed] [Google Scholar]
- 92.Ye X., Sun X., Starovoytov V., Cai Q. Parkin-mediated mitophagy in mutant hAPP neurons and Alzheimer’s disease patient brains. Hum. Mol. Genet. 2015;24:2938–2951. doi: 10.1093/hmg/ddv056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pradeepkiran J.A., Reddy P.H. Defective mitophagy in Alzheimer’s disease. Ageing Res. Rev. 2020;64:101191. doi: 10.1016/j.arr.2020.101191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Donix M., Ercoli L.M., Siddarth P., Brown J.A., Martin-Harris L., Burggren A.C., Miller K.J., Small G.W., Bookheimer S.Y. Influence of Alzheimer disease family history and genetic risk on cognitive performance in healthy middle-aged and older people. Am. J. Geriatr. Psychiatry. 2012;20:565–573. doi: 10.1097/JGP.0b013e3182107e6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Pizzonia J.H., Ransom B.R., Pappas C.A. Characterization of Na+/H+ exchange activity in cultured rat hippocampal astrocytes. J. Neurosci. Res. 1996;44:191–198. doi: 10.1002/(SICI)1097-4547(19960415)44:2<191::AID-JNR12>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- 96.Tiraboschi P., Hansen L.A., Masliah E., Alford M., Thal L.J., Corey-Bloom J. Impact of APOE genotype on neuropathologic and neurochemical markers of Alzheimer disease. Neurology. 2004;62:1977–1983. doi: 10.1212/01.WNL.0000128091.92139.0F. [DOI] [PubMed] [Google Scholar]
- 97.Picone P., Nuzzo D., Caruana L., Scafidi V., Di Carlo M. Mitochondrial dysfunction: Different routes to Alzheimer’s disease therapy. Oxid Med. Cell Longev. 2014;2014:780179. doi: 10.1155/2014/780179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Du H., Yan S.S. Mitochondrial permeability transition pore in Alzheimer’s disease: Cyclophilin D and amyloid beta. Biochim. Biophys. Acta. 2010;1802:198–204. doi: 10.1016/j.bbadis.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rao V.K., Carlson E.A., Yan S.S. Mitochondrial permeability transition pore is a potential drug target for neurodegeneration. Biochim. Biophys. Acta. 2014;1842:1267–1272. doi: 10.1016/j.bbadis.2013.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kim D.I., Lee K.H., Gabr A.A., Choi G.E., Kim J.S., Ko S.H., Han H.J. Abeta-Induced Drp1 phosphorylation through Akt activation promotes excessive mitochondrial fission leading to neuronal apoptosis. Biochim. Biophys. Acta. 2016;1863:2820–2834. doi: 10.1016/j.bbamcr.2016.09.003. [DOI] [PubMed] [Google Scholar]
- 101.Orrenius S., Gogvadze V., Zhivotovsky B. Calcium and mitochondria in the regulation of cell death. Biochem. Biophys. Res. Commun. 2015;460:72–81. doi: 10.1016/j.bbrc.2015.01.137. [DOI] [PubMed] [Google Scholar]
- 102.Gandhi S., Wood-Kaczmar A., Yao Z., Plun-Favreau H., Deas E., Klupsch K., Downward J., Latchman D.S., Tabrizi S.J., Wood N.W., et al. PINK1-associated Parkinson’s disease is caused by neuronal vulnerability to calcium-induced cell death. Mol. Cell. 2009;33:627–638. doi: 10.1016/j.molcel.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Area-Gomez E., de Groof A., Bonilla E., Montesinos J., Tanji K., Boldogh I., Pon L., Schon E.A. A key role for MAM in mediating mitochondrial dysfunction in Alzheimer disease. Cell Death Dis. 2018;9:335. doi: 10.1038/s41419-017-0215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cheng J., Liao Y., Dong Y., Hu H., Yang N., Kong X., Li S., Li X., Guo J., Qin L., et al. Microglial autophagy defect causes parkinson disease-like symptoms by accelerating inflammasome activation in mice. Autophagy. 2020;16:2193–2205. doi: 10.1080/15548627.2020.1719723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zheng W.H., Bastianetto S., Mennicken F., Ma W., Kar S. Amyloid beta peptide induces tau phosphorylation and loss of cholinergic neurons in rat primary septal cultures. Neuroscience. 2002;115:201–211. doi: 10.1016/S0306-4522(02)00404-9. [DOI] [PubMed] [Google Scholar]
- 106.Garwood C.J., Pooler A.M., Atherton J., Hanger D.P., Noble W. Astrocytes are important mediators of Abeta-induced neurotoxicity and tau phosphorylation in primary culture. Cell Death Dis. 2011;2:e167. doi: 10.1038/cddis.2011.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Perez M.J., Jara C., Quintanilla R.A. Contribution of Tau Pathology to Mitochondrial Impairment in Neurodegeneration. Front. Neurosci. 2018;12:441. doi: 10.3389/fnins.2018.00441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Manczak M., Reddy P.H. Abnormal interaction between the mitochondrial fission protein Drp1 and hyperphosphorylated tau in Alzheimer’s disease neurons: Implications for mitochondrial dysfunction and neuronal damage. Hum. Mol. Genet. 2012;21:2538–2547. doi: 10.1093/hmg/dds072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ittner L.M., Fath T., Ke Y.D., Bi M., van Eersel J., Li K.M., Gunning P., Gotz J. Parkinsonism and impaired axonal transport in a mouse model of frontotemporal dementia. Proc. Natl. Acad. Sci. USA. 2008;105:15997–16002. doi: 10.1073/pnas.0808084105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mandelkow E.M., Mandelkow E. Biochemistry and cell biology of tau protein in neurofibrillary degeneration. Cold Spring Harb. Perspect. Med. 2012;2:a006247. doi: 10.1101/cshperspect.a006247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kopeikina K.J., Carlson G.A., Pitstick R., Ludvigson A.E., Peters A., Luebke J.I., Koffie R.M., Frosch M.P., Hyman B.T., Spires-Jones T.L. Tau accumulation causes mitochondrial distribution deficits in neurons in a mouse model of tauopathy and in human Alzheimer’s disease brain. Am. J. Pathol. 2011;179:2071–2082. doi: 10.1016/j.ajpath.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Andreadis A. Tau gene alternative splicing: Expression patterns, regulation and modulation of function in normal brain and neurodegenerative diseases. Biochim. Biophys. Acta. 2005;1739:91–103. doi: 10.1016/j.bbadis.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 113.Leon-Espinosa G., Garcia E., Garcia-Escudero V., Hernandez F., Defelipe J., Avila J. Changes in tau phosphorylation in hibernating rodents. J. Neurosci. Res. 2013;91:954–962. doi: 10.1002/jnr.23220. [DOI] [PubMed] [Google Scholar]
- 114.Amadoro G., Corsetti V., Stringaro A., Colone M., D’Aguanno S., Meli G., Ciotti M., Sancesario G., Cattaneo A., Bussani R., et al. A NH2 tau fragment targets neuronal mitochondria at AD synapses: Possible implications for neurodegeneration. J. Alzheimers Dis. 2010;21:445–470. doi: 10.3233/JAD-2010-100120. [DOI] [PubMed] [Google Scholar]
- 115.Li X.C., Hu Y., Wang Z.H., Luo Y., Zhang Y., Liu X.P., Feng Q., Wang Q., Ye K., Liu G.P., et al. Human wild-type full-length tau accumulation disrupts mitochondrial dynamics and the functions via increasing mitofusins. Sci. Rep. 2016;6:24756. doi: 10.1038/srep24756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.DuBoff B., Gotz J., Feany M.B. Tau promotes neurodegeneration via DRP1 mislocalization in vivo. Neuron. 2012;75:618–632. doi: 10.1016/j.neuron.2012.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Itoh K., Nakamura K., Iijima M., Sesaki H. Mitochondrial dynamics in neurodegeneration. Trends Cell Biol. 2013;23:64–71. doi: 10.1016/j.tcb.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Crespo-Biel N., Theunis C., Van Leuven F. Protein tau: Prime cause of synaptic and neuronal degeneration in Alzheimer’s disease. Int. J. Alzheimers Dis. 2012;2012:251426. doi: 10.1155/2012/251426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kolarova M., Garcia-Sierra F., Bartos A., Ricny J., Ripova D. Structure and pathology of tau protein in Alzheimer disease. Int. J. Alzheimers Dis. 2012;2012:731526. doi: 10.1155/2012/731526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Knott A.B., Bossy-Wetzel E. Impairing the mitochondrial fission and fusion balance: A new mechanism of neurodegeneration. Ann. N. Y. Acad. Sci. 2008;1147:283–292. doi: 10.1196/annals.1427.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Hoglinger G.U., Lannuzel A., Khondiker M.E., Michel P.P., Duyckaerts C., Feger J., Champy P., Prigent A., Medja F., Lombes A., et al. The mitochondrial complex I inhibitor rotenone triggers a cerebral tauopathy. J. Neurochem. 2005;95:930–939. doi: 10.1111/j.1471-4159.2005.03493.x. [DOI] [PubMed] [Google Scholar]
- 122.Yoo S.M., Park J., Kim S.H., Jung Y.K. Emerging perspectives on mitochondrial dysfunction and inflammation in Alzheimer’s disease. BMB Rep. 2020;53:35–46. doi: 10.5483/BMBRep.2020.53.1.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Guo L., Tian J., Du H. Mitochondrial Dysfunction and Synaptic Transmission Failure in Alzheimer’s Disease. J. Alzheimers Dis. 2017;57:1071–1086. doi: 10.3233/JAD-160702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Cheng Y., Bai F. The Association of Tau With Mitochondrial Dysfunction in Alzheimer’s Disease. Front. Neurosci. 2018;12:163. doi: 10.3389/fnins.2018.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Agnihotri A., Aruoma O.I. Alzheimer’s Disease and Parkinson’s Disease: A Nutritional Toxicology Perspective of the Impact of Oxidative Stress, Mitochondrial Dysfunction, Nutrigenomics and Environmental Chemicals. J. Am. Coll Nutr. 2020;39:16–27. doi: 10.1080/07315724.2019.1683379. [DOI] [PubMed] [Google Scholar]
- 126.Wang S., Kaufman R.J. The impact of the unfolded protein response on human disease. J. Cell Biol. 2012;197:857–867. doi: 10.1083/jcb.201110131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hwang J., Qi L. Quality Control in the Endoplasmic Reticulum: Crosstalk between ERAD and UPR pathways. Trends Biochem. Sci. 2018;43:593–605. doi: 10.1016/j.tibs.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Bernales S., Schuck S., Walter P. ER-phagy: Selective autophagy of the endoplasmic reticulum. Autophagy. 2007;3:285–287. doi: 10.4161/auto.3930. [DOI] [PubMed] [Google Scholar]
- 129.Khaminets A., Heinrich T., Mari M., Grumati P., Huebner A.K., Akutsu M., Liebmann L., Stolz A., Nietzsche S., Koch N., et al. Regulation of endoplasmic reticulum turnover by selective autophagy. Nature. 2015;522:354–358. doi: 10.1038/nature14498. [DOI] [PubMed] [Google Scholar]
- 130.Bernales S., McDonald K.L., Walter P. Autophagy counterbalances endoplasmic reticulum expansion during the unfolded protein response. PLoS Biol. 2006;4:e423. doi: 10.1371/journal.pbio.0040423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Schuck S., Gallagher C.M., Walter P. ER-phagy mediates selective degradation of endoplasmic reticulum independently of the core autophagy machinery. J. Cell Sci. 2014;127:4078–4088. doi: 10.1242/jcs.154716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Moretti J., Roy S., Bozec D., Martinez J., Chapman J.R., Ueberheide B., Lamming D.W., Chen Z.J., Horng T., Yeretssian G., et al. STING Senses Microbial Viability to Orchestrate Stress-Mediated Autophagy of the Endoplasmic Reticulum. Cell. 2017;171:809–823. doi: 10.1016/j.cell.2017.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Katayama T., Imaizumi K., Honda A., Yoneda T., Kudo T., Takeda M., Mori K., Rozmahel R., Fraser P., George-Hyslop P.S., et al. Disturbed activation of endoplasmic reticulum stress transducers by familial Alzheimer’s disease-linked presenilin-1 mutations. J. Biol. Chem. 2001;276:43446–43454. doi: 10.1074/jbc.M104096200. [DOI] [PubMed] [Google Scholar]
- 134.Duran-Aniotz C., Martinez G., Hetz C. Memory loss in Alzheimer’s disease: Are the alterations in the UPR network involved in the cognitive impairment? Front. Aging Neurosci. 2014;6:8. doi: 10.3389/fnagi.2014.00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Acosta-Alvear D., Zhou Y., Blais A., Tsikitis M., Lents N.H., Arias C., Lennon C.J., Kluger Y., Dynlacht B.D. XBP1 controls diverse cell type- and condition-specific transcriptional regulatory networks. Mol. Cell. 2007;27:53–66. doi: 10.1016/j.molcel.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 136.Hoozemans J.J., van Haastert E.S., Nijholt D.A., Rozemuller A.J., Eikelenboom P., Scheper W. The unfolded protein response is activated in pretangle neurons in Alzheimer’s disease hippocampus. Am. J. Pathol. 2009;174:1241–1251. doi: 10.2353/ajpath.2009.080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Voeltz G.K., Prinz W.A., Shibata Y., Rist J.M., Rapoport T.A. A class of membrane proteins shaping the tubular endoplasmic reticulum. Cell. 2006;124:573–586. doi: 10.1016/j.cell.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 138.Hoozemans J.J., van Haastert E.S., Nijholt D.A., Rozemuller A.J., Scheper W. Activation of the unfolded protein response is an early event in Alzheimer’s and Parkinson’s disease. Neurodegener. Dis. 2012;10:212–215. doi: 10.1159/000334536. [DOI] [PubMed] [Google Scholar]
- 139.Lai C.S., Preisler J., Baum L., Lee D.H., Ng H.K., Hugon J., So K.F., Chang R.C. Low molecular weight Abeta induces collapse of endoplasmic reticulum. Mol. Cell Neurosci. 2009;41:32–43. doi: 10.1016/j.mcn.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 140.Shibuya Y., Chang C.C., Huang L.H., Bryleva E.Y., Chang T.Y. Inhibiting ACAT1/SOAT1 in microglia stimulates autophagy-mediated lysosomal proteolysis and increases Abeta1-42 clearance. J. Neurosci. 2014;34:14484–14501. doi: 10.1523/JNEUROSCI.2567-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Loewen C.A., Feany M.B. The unfolded protein response protects from tau neurotoxicity in vivo. PLoS ONE. 2010;5:e13084. doi: 10.1371/journal.pone.0013084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Cohen S. Lipid Droplets as Organelles. Int. Rev. Cell Mol. Biol. 2018;337:83–110. doi: 10.1016/bs.ircmb.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Robichaud S., Fairman G., Vijithakumar V., Mak E., Cook D.P., Pelletier A.R., Huard S., Vanderhyden B.C., Figeys D., Lavallee-Adam M., et al. Identification of novel lipid droplet factors that regulate lipophagy and cholesterol efflux in macrophage foam cells. Autophagy. 2021;17:3671–3689. doi: 10.1080/15548627.2021.1886839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Martinez-Lopez N., Garcia-Macia M., Sahu S., Athonvarangkul D., Liebling E., Merlo P., Cecconi F., Schwartz G.J., Singh R. Autophagy in the CNS and Periphery Coordinate Lipophagy and Lipolysis in the Brown Adipose Tissue and Liver. Cell Metab. 2016;23:113–127. doi: 10.1016/j.cmet.2015.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Haidar M., Loix M., Bogie J.F.J., Hendriks J.J.A. Lipophagy: A new player in CNS disorders. Trends Endocrinol. Metab. 2021;32:941–951. doi: 10.1016/j.tem.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 146.Hamilton L.K., Dufresne M., Joppe S.E., Petryszyn S., Aumont A., Calon F., Barnabe-Heider F., Furtos A., Parent M., Chaurand P., et al. Aberrant Lipid Metabolism in the Forebrain Niche Suppresses Adult Neural Stem Cell Proliferation in an Animal Model of Alzheimer’s Disease. Cell Stem Cell. 2015;17:397–411. doi: 10.1016/j.stem.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 147.Ioannou M.S., Jackson J., Sheu S.H., Chang C.L., Weigel A.V., Liu H., Pasolli H.A., Xu C.S., Pang S., Matthies D., et al. Neuron-Astrocyte Metabolic Coupling Protects against Activity-Induced Fatty Acid Toxicity. Cell. 2019;177:1522–1535. doi: 10.1016/j.cell.2019.04.001. [DOI] [PubMed] [Google Scholar]
- 148.Islam A., Kagawa Y., Miyazaki H., Shil S.K., Umaru B.A., Yasumoto Y., Yamamoto Y., Owada Y. FABP7 Protects Astrocytes Against ROS Toxicity via Lipid Droplet Formation. Mol. Neurobiol. 2019;56:5763–5779. doi: 10.1007/s12035-019-1489-2. [DOI] [PubMed] [Google Scholar]
- 149.Moreau K., Fleming A., Imarisio S., Lopez Ramirez A., Mercer J.L., Jimenez-Sanchez M., Bento C.F., Puri C., Zavodszky E., Siddiqi F., et al. PICALM modulates autophagy activity and tau accumulation. Nat. Commun. 2014;5:4998. doi: 10.1038/ncomms5998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Alzheimer A., Stelzmann R.A., Schnitzlein H.N., Murtagh F.R. An English translation of Alzheimer’s 1907 paper, “Uber eine eigenartige Erkankung der Hirnrinde”. Clin. Anat. 1995;8:429–431. doi: 10.1002/ca.980080612. [DOI] [PubMed] [Google Scholar]
- 151.Liu Q., Trotter J., Zhang J., Peters M.M., Cheng H., Bao J., Han X., Weeber E.J., Bu G. Neuronal LRP1 knockout in adult mice leads to impaired brain lipid metabolism and progressive, age-dependent synapse loss and neurodegeneration. J. Neurosci. 2010;30:17068–17078. doi: 10.1523/JNEUROSCI.4067-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Liu Q., Zerbinatti C.V., Zhang J., Hoe H.S., Wang B., Cole S.L., Herz J., Muglia L., Bu G. Amyloid precursor protein regulates brain apolipoprotein E and cholesterol metabolism through lipoprotein receptor LRP1. Neuron. 2007;56:66–78. doi: 10.1016/j.neuron.2007.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Linetti A., Fratangeli A., Taverna E., Valnegri P., Francolini M., Cappello V., Matteoli M., Passafaro M., Rosa P. Cholesterol reduction impairs exocytosis of synaptic vesicles. J. Cell Sci. 2010;123:595–605. doi: 10.1242/jcs.060681. [DOI] [PubMed] [Google Scholar]
- 154.Jana A., Pahan K. Fibrillar amyloid-beta-activated human astroglia kill primary human neurons via neutral sphingomyelinase: Implications for Alzheimer’s disease. J. Neurosci. 2010;30:12676–12689. doi: 10.1523/JNEUROSCI.1243-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Sanchez-Mejia R.O., Newman J.W., Toh S., Yu G.Q., Zhou Y., Halabisky B., Cisse M., Scearce-Levie K., Cheng I.H., Gan L., et al. Phospholipase A2 reduction ameliorates cognitive deficits in a mouse model of Alzheimer’s disease. Nat. Neurosci. 2008;11:1311–1318. doi: 10.1038/nn.2213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Esposito G., Giovacchini G., Liow J.S., Bhattacharjee A.K., Greenstein D., Schapiro M., Hallett M., Herscovitch P., Eckelman W.C., Carson R.E., et al. Imaging neuroinflammation in Alzheimer’s disease with radiolabeled arachidonic acid and PET. J. Nucl. Med. 2008;49:1414–1421. doi: 10.2967/jnumed.107.049619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Sienski G., Narayan P., Bonner J.M., Kory N., Boland S., Arczewska A.A., Ralvenius W.T., Akay L., Lockshin E., He L., et al. APOE4 disrupts intracellular lipid homeostasis in human iPSC-derived glia. Sci. Transl. Med. 2021;13:eaaz4564. doi: 10.1126/scitranslmed.aaz4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Cipolla C.M., Lodhi I.J. Peroxisomal Dysfunction in Age-Related Diseases. Trends Endocrinol. Metab. 2017;28:297–308. doi: 10.1016/j.tem.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Nordgren M., Fransen M. Peroxisomal metabolism and oxidative stress. Biochimie. 2014;98:56–62. doi: 10.1016/j.biochi.2013.07.026. [DOI] [PubMed] [Google Scholar]
- 160.Colasante C., Chen J., Ahlemeyer B., Baumgart-Vogt E. Peroxisomes in cardiomyocytes and the peroxisome / peroxisome proliferator-activated receptor-loop. Thromb. Haemost. 2015;113:452–463. doi: 10.1160/TH14-06-0497. [DOI] [PubMed] [Google Scholar]
- 161.Morvay P.L., Baes M., Van Veldhoven P.P. Differential activities of peroxisomes along the mouse intestinal epithelium. Cell Biochem. Funct. 2017;35:144–155. doi: 10.1002/cbf.3255. [DOI] [PubMed] [Google Scholar]
- 162.Farooqui A.A., Horrocks L.A. Plasmalogens: Workhorse lipids of membranes in normal and injured neurons and glia. Neuroscientist. 2001;7:232–245. doi: 10.1177/107385840100700308. [DOI] [PubMed] [Google Scholar]
- 163.Powers J.M. Normal and defective neuronal membranes: Structure and function: Neuronal lesions in peroxisomal disorders. J. Mol. Neurosci. 2001;16:285–287. doi: 10.1385/JMN:16:2-3:285. discussion 317–321. [DOI] [PubMed] [Google Scholar]
- 164.Bottelbergs A., Verheijden S., Hulshagen L., Gutmann D.H., Goebbels S., Nave K.A., Kassmann C., Baes M. Axonal integrity in the absence of functional peroxisomes from projection neurons and astrocytes. Glia. 2010;58:1532–1543. doi: 10.1002/glia.21027. [DOI] [PubMed] [Google Scholar]
- 165.Kassmann C.M. Myelin peroxisomes—Essential organelles for the maintenance of white matter in the nervous system. Biochimie. 2014;98:111–118. doi: 10.1016/j.biochi.2013.09.020. [DOI] [PubMed] [Google Scholar]
- 166.Zientara-Rytter K., Subramani S. Autophagic degradation of peroxisomes in mammals. Biochem. Soc. Trans. 2016;44:431–440. doi: 10.1042/BST20150268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Deosaran E., Larsen K.B., Hua R., Sargent G., Wang Y., Kim S., Lamark T., Jauregui M., Law K., Lippincott-Schwartz J., et al. NBR1 acts as an autophagy receptor for peroxisomes. J. Cell Sci. 2013;126:939–952. doi: 10.1242/jcs.114819. [DOI] [PubMed] [Google Scholar]
- 168.Kim P.K., Hailey D.W., Mullen R.T., Lippincott-Schwartz J. Ubiquitin signals autophagic degradation of cytosolic proteins and peroxisomes. Proc. Natl. Acad. Sci. USA. 2008;105:20567–20574. doi: 10.1073/pnas.0810611105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Zhang J., Tripathi D.N., Jing J., Alexander A., Kim J., Powell R.T., Dere R., Tait-Mulder J., Lee J.H., Paull T.T., et al. ATM functions at the peroxisome to induce pexophagy in response to ROS. Nat. Cell Biol. 2015;17:1259–1269. doi: 10.1038/ncb3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Walton P.A., Brees C., Lismont C., Apanasets O., Fransen M. The peroxisomal import receptor PEX5 functions as a stress sensor, retaining catalase in the cytosol in times of oxidative stress. Biochim. Biophys. Acta Mol. Cell Res. 2017;1864:1833–1843. doi: 10.1016/j.bbamcr.2017.07.013. [DOI] [PubMed] [Google Scholar]
- 171.Kabeya Y., Mizushima N., Ueno T., Yamamoto A., Kirisako T., Noda T., Kominami E., Ohsumi Y., Yoshimori T. LC3, a mammalian homologue of yeast Apg8p, is localized in autophagosome membranes after processing. EMBO J. 2000;19:5720–5728. doi: 10.1093/emboj/19.21.5720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Santos M.J., Quintanilla R.A., Toro A., Grandy R., Dinamarca M.C., Godoy J.A., Inestrosa N.C. Peroxisomal proliferation protects from beta-amyloid neurodegeneration. J. Biol. Chem. 2005;280:41057–41068. doi: 10.1074/jbc.M505160200. [DOI] [PubMed] [Google Scholar]
- 173.Goodenowe D.B., Senanayake V. Relation of Serum Plasmalogens and APOE Genotype to Cognition and Dementia in Older Persons in a Cross-Sectional Study. Brain. Sci. 2019;9:92. doi: 10.3390/brainsci9040092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Siegel C.S., McCullough L.D. NAD+ and nicotinamide: Sex differences in cerebral ischemia. Neuroscience. 2013;237:223–231. doi: 10.1016/j.neuroscience.2013.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Mirza M.A., Ritzel R., Xu Y., McCullough L.D., Liu F. Sexually dimorphic outcomes and inflammatory responses in hypoxic-ischemic encephalopathy. J. Neuroinflammation. 2015;12:32. doi: 10.1186/s12974-015-0251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Ritzel R.M., Patel A.R., Spychala M., Verma R., Crapser J., Koellhoffer E.C., Schrecengost A., Jellison E.R., Zhu L., Venna V.R., et al. Multiparity improves outcomes after cerebral ischemia in female mice despite features of increased metabovascular risk. Proc. Natl. Acad. Sci. USA. 2017;114:E5673–E5682. doi: 10.1073/pnas.1607002114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kvam E., Goldfarb D.S. Nucleus-vacuole junctions and piecemeal microautophagy of the nucleus in S. cerevisiae. Autophagy. 2007;3:85–92. doi: 10.4161/auto.3586. [DOI] [PubMed] [Google Scholar]
- 178.Kraft C., Reggiori F., Peter M. Selective types of autophagy in yeast. Biochim. Biophys. Acta. 2009;1793:1404–1412. doi: 10.1016/j.bbamcr.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 179.Park Y.E., Hayashi Y.K., Bonne G., Arimura T., Noguchi S., Nonaka I., Nishino I. Autophagic degradation of nuclear components in mammalian cells. Autophagy. 2009;5:795–804. doi: 10.4161/auto.8901. [DOI] [PubMed] [Google Scholar]
- 180.Dou Z., Xu C., Donahue G., Shimi T., Pan J.A., Zhu J., Ivanov A., Capell B.C., Drake A.M., Shah P.P., et al. Autophagy mediates degradation of nuclear lamina. Nature. 2015;527:105–109. doi: 10.1038/nature15548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Salama R., Sadaie M., Hoare M., Narita M. Cellular senescence and its effector programs. Genes Dev. 2014;28:99–114. doi: 10.1101/gad.235184.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Dobrzynska A., Gonzalo S., Shanahan C., Askjaer P. The nuclear lamina in health and disease. Nucleus. 2016;7:233–248. doi: 10.1080/19491034.2016.1183848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Shimi T., Butin-Israeli V., Adam S.A., Hamanaka R.B., Goldman A.E., Lucas C.A., Shumaker D.K., Kosak S.T., Chandel N.S., Goldman R.D. The role of nuclear lamin B1 in cell proliferation and senescence. Genes Dev. 2011;25:2579–2593. doi: 10.1101/gad.179515.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Shah P.P., Donahue G., Otte G.L., Capell B.C., Nelson D.M., Cao K., Aggarwala V., Cruickshanks H.A., Rai T.S., McBryan T., et al. Lamin B1 depletion in senescent cells triggers large-scale changes in gene expression and the chromatin landscape. Genes Dev. 2013;27:1787–1799. doi: 10.1101/gad.223834.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Lukasova E., Kovarik A., Bacikova A., Falk M., Kozubek S. Loss of lamin B receptor is necessary to induce cellular senescence. Biochem. J. 2017;474:281–300. doi: 10.1042/BCJ20160459. [DOI] [PubMed] [Google Scholar]
- 186.Maejima I., Takahashi A., Omori H., Kimura T., Takabatake Y., Saitoh T., Yamamoto A., Hamasaki M., Noda T., Isaka Y., et al. Autophagy sequesters damaged lysosomes to control lysosomal biogenesis and kidney injury. EMBO J. 2013;32:2336–2347. doi: 10.1038/emboj.2013.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Chauhan S., Kumar S., Jain A., Ponpuak M., Mudd M.H., Kimura T., Choi S.W., Peters R., Mandell M., Bruun J.A., et al. TRIMs and Galectins Globally Cooperate and TRIM16 and Galectin-3 Co-direct Autophagy in Endomembrane Damage Homeostasis. Dev. Cell. 2016;39:13–27. doi: 10.1016/j.devcel.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Fraiberg M., Elazar Z. A TRIM16-Galactin3 Complex Mediates Autophagy of Damaged Endomembranes. Dev. Cell. 2016;39:1–2. doi: 10.1016/j.devcel.2016.09.025. [DOI] [PubMed] [Google Scholar]
- 189.Hung Y.H., Chen L.M., Yang J.Y., Yang W.Y. Spatiotemporally controlled induction of autophagy-mediated lysosome turnover. Nat. Commun. 2013;4:2111. doi: 10.1038/ncomms3111. [DOI] [PubMed] [Google Scholar]
- 190.Yoshida Y., Yasuda S., Fujita T., Hamasaki M., Murakami A., Kawawaki J., Iwai K., Saeki Y., Yoshimori T., Matsuda N., et al. Ubiquitination of exposed glycoproteins by SCF(FBXO27) directs damaged lysosomes for autophagy. Proc. Natl. Acad. Sci. USA. 2017;114:8574–8579. doi: 10.1073/pnas.1702615114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Heneka M.T., Kummer M.P., Stutz A., Delekate A., Schwartz S., Vieira-Saecker A., Griep A., Axt D., Remus A., Tzeng T.C., et al. NLRP3 is activated in Alzheimer’s disease and contributes to pathology in APP/PS1 mice. Nature. 2013;493:674–678. doi: 10.1038/nature11729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Teyssou E., Takeda T., Lebon V., Boillee S., Doukoure B., Bataillon G., Sazdovitch V., Cazeneuve C., Meininger V., LeGuern E., et al. Mutations in SQSTM1 encoding p62 in amyotrophic lateral sclerosis: Genetics and neuropathology. Acta Neuropathol. 2013;125:511–522. doi: 10.1007/s00401-013-1090-0. [DOI] [PubMed] [Google Scholar]
- 193.Maruyama H., Morino H., Ito H., Izumi Y., Kato H., Watanabe Y., Kinoshita Y., Kamada M., Nodera H., Suzuki H., et al. Mutations of optineurin in amyotrophic lateral sclerosis. Nature. 2010;465:223–226. doi: 10.1038/nature08971. [DOI] [PubMed] [Google Scholar]
- 194.Freischmidt A., Wieland T., Richter B., Ruf W., Schaeffer V., Muller K., Marroquin N., Nordin F., Hubers A., Weydt P., et al. Haploinsufficiency of TBK1 causes familial ALS and fronto-temporal dementia. Nat. Neurosci. 2015;18:631–636. doi: 10.1038/nn.4000. [DOI] [PubMed] [Google Scholar]
- 195.Warner J.R. The economics of ribosome biosynthesis in yeast. Trends Biochem. Sci. 1999;24:437–440. doi: 10.1016/S0968-0004(99)01460-7. [DOI] [PubMed] [Google Scholar]
- 196.Kraft C., Deplazes A., Sohrmann M., Peter M. Mature ribosomes are selectively degraded upon starvation by an autophagy pathway requiring the Ubp3p/Bre5p ubiquitin protease. Nat. Cell Biol. 2008;10:602–610. doi: 10.1038/ncb1723. [DOI] [PubMed] [Google Scholar]
- 197.Soncini C., Berdo I., Draetta G. Ras-GAP SH3 domain binding protein (G3BP) is a modulator of USP10, a novel human ubiquitin specific protease. Oncogene. 2001;20:3869–3879. doi: 10.1038/sj.onc.1204553. [DOI] [PubMed] [Google Scholar]
- 198.Baltanas F.C., Casafont I., Weruaga E., Alonso J.R., Berciano M.T., Lafarga M. Nucleolar disruption and cajal body disassembly are nuclear hallmarks of DNA damage-induced neurodegeneration in purkinje cells. Brain Pathol. 2011;21:374–388. doi: 10.1111/j.1750-3639.2010.00461.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Du F., Yu Q., Yan S., Hu G., Lue L.F., Walker D.G., Wu L., Yan S.F., Tieu K., Yan S.S. PINK1 signalling rescues amyloid pathology and mitochondrial dysfunction in Alzheimer’s disease. Brain. 2017;140:3233–3251. doi: 10.1093/brain/awx258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Luo R., Su L.Y., Li G., Yang J., Liu Q., Yang L.X., Zhang D.F., Zhou H., Xu M., Fan Y., et al. Activation of PPARA-mediated autophagy reduces Alzheimer disease-like pathology and cognitive decline in a murine model. Autophagy. 2020;16:52–69. doi: 10.1080/15548627.2019.1596488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Fang E.F., Hou Y., Palikaras K., Adriaanse B.A., Kerr J.S., Yang B., Lautrup S., Hasan-Olive M.M., Caponio D., Dan X., et al. Mitophagy inhibits amyloid-beta and tau pathology and reverses cognitive deficits in models of Alzheimer’s disease. Nat. Neurosci. 2019;22:401–412. doi: 10.1038/s41593-018-0332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Chen M.L., Hong C.G., Yue T., Li H.M., Duan R., Hu W.B., Cao J., Wang Z.X., Chen C.Y., Hu X.K., et al. Inhibition of miR-331-3p and miR-9-5p ameliorates Alzheimer’s disease by enhancing autophagy. Theranostics. 2021;11:2395–2409. doi: 10.7150/thno.47408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zhang X., Wei M., Fan J., Yan W., Zha X., Song H., Wan R., Yin Y., Wang W. Ischemia-induced upregulation of autophagy preludes dysfunctional lysosomal storage and associated synaptic impairments in neurons. Autophagy. 2021;17:1519–1542. doi: 10.1080/15548627.2020.1840796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bourdenx M., Martin-Segura A., Scrivo A., Rodriguez-Navarro J.A., Kaushik S., Tasset I., Diaz A., Storm N.J., Xin Q., Juste Y.R., et al. Chaperone-mediated autophagy prevents collapse of the neuronal metastable proteome. Cell. 2021;184:2696–2714.e2625. doi: 10.1016/j.cell.2021.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Martinez J., Marmisolle I., Tarallo D., Quijano C. Mitochondrial Bioenergetics and Dynamics in Secretion Processes. Front. Endocrinol. 2020;11:319. doi: 10.3389/fendo.2020.00319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Zellner S., Schifferer M., Behrends C. Systematically defining selective autophagy receptor-specific cargo using autophagosome content profiling. Mol. Cell. 2021;81:1337–1354 e1338. doi: 10.1016/j.molcel.2021.01.009. [DOI] [PubMed] [Google Scholar]
- 207.Wang L., Qi H., Tang Y., Shen H.M. Post-translational Modifications of Key Machinery in the Control of Mitophagy. Trends Biochem. Sci. 2020;45:58–75. doi: 10.1016/j.tibs.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 208.Liu L., Feng D., Chen G., Chen M., Zheng Q., Song P., Ma Q., Zhu C., Wang R., Qi W., et al. Mitochondrial outer-membrane protein FUNDC1 mediates hypoxia-induced mitophagy in mammalian cells. Nat. Cell Biol. 2012;14:177–185. doi: 10.1038/ncb2422. [DOI] [PubMed] [Google Scholar]
- 209.Xie Y., Liu J., Kang R., Tang D. Mitophagy Receptors in Tumor Biology. Front. Cell Dev. Biol. 2020;8:594203. doi: 10.3389/fcell.2020.594203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zou Y., He W., Wang K., Han H., Xiao T., Chen X., Zhou B., Tan J., Xia K., Tang B., et al. Identification of rare RTN3 variants in Alzheimer’s disease in Han Chinese. Hum. Genet. 2018;137:141–150. doi: 10.1007/s00439-018-1868-1. [DOI] [PubMed] [Google Scholar]
- 211.Jung W.H., Liu C.C., Yu Y.L., Chang Y.C., Lien W.Y., Chao H.C., Huang S.Y., Kuo C.H., Ho H.C., Chan C.C. Lipophagy prevents activity-dependent neurodegeneration due to dihydroceramide accumulation in vivo. EMBO Rep. 2017;18:1150–1165. doi: 10.15252/embr.201643480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Heo J.M., Ordureau A., Paulo J.A., Rinehart J., Harper J.W. The PINK1-PARKIN Mitochondrial Ubiquitylation Pathway Drives a Program of OPTN/NDP52 Recruitment and TBK1 Activation to Promote Mitophagy. Mol. Cell. 2015;60:7–20. doi: 10.1016/j.molcel.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Lu K., Psakhye I., Jentsch S. Autophagic clearance of polyQ proteins mediated by ubiquitin-Atg8 adaptors of the conserved CUET protein family. Cell. 2014;158:549–563. doi: 10.1016/j.cell.2014.05.048. [DOI] [PubMed] [Google Scholar]
- 214.Lamark T., Johansen T. Aggrephagy: Selective disposal of protein aggregates by macroautophagy. Int. J. Cell Biol. 2012;2012:736905. doi: 10.1155/2012/736905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yang X., Zhang M., Dai Y., Sun Y., Aman Y., Xu Y., Yu P., Zheng Y., Yang J., Zhu X. Spermidine inhibits neurodegeneration and delays aging via the PINK1-PDR1-dependent mitophagy pathway in C. elegans. Aging. 2020;12:16852–16866. doi: 10.18632/aging.103578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Geisler S., Holmstrom K.M., Skujat D., Fiesel F.C., Rothfuss O.C., Kahle P.J., Springer W. PINK1/Parkin-mediated mitophagy is dependent on VDAC1 and p62/SQSTM1. Nat. Cell Biol. 2010;12:119–131. doi: 10.1038/ncb2012. [DOI] [PubMed] [Google Scholar]
- 217.Lahiri V., Klionsky D.J. Functional impairment in RHOT1/Miro1 degradation and mitophagy is a shared feature in familial and sporadic Parkinson disease. Autophagy. 2017;13:1259–1261. doi: 10.1080/15548627.2017.1327512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Chen Y., Dorn G.W., 2nd PINK1-phosphorylated mitofusin 2 is a Parkin receptor for culling damaged mitochondria. Science. 2013;340:471–475. doi: 10.1126/science.1231031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Gao F., Chen D., Si J., Hu Q., Qin Z., Fang M., Wang G. The mitochondrial protein BNIP3L is the substrate of PARK2 and mediates mitophagy in PINK1/PARK2 pathway. Hum. Mol. Genet. 2015;24:2528–2538. doi: 10.1093/hmg/ddv017. [DOI] [PubMed] [Google Scholar]
- 220.Tang C., Han H., Liu Z., Liu Y., Yin L., Cai J., He L., Liu Y., Chen G., Zhang Z., et al. Activation of BNIP3-mediated mitophagy protects against renal ischemia-reperfusion injury. Cell Death Dis. 2019;10:677. doi: 10.1038/s41419-019-1899-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Strappazzon F., Nazio F., Corrado M., Cianfanelli V., Romagnoli A., Fimia G.M., Campello S., Nardacci R., Piacentini M., Campanella M., et al. AMBRA1 is able to induce mitophagy via LC3 binding, regardless of PARKIN and p62/SQSTM1. Cell Death Differ. 2015;22:419–432. doi: 10.1038/cdd.2014.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Murakawa T., Yamaguchi O., Hashimoto A., Hikoso S., Takeda T., Oka T., Yasui H., Ueda H., Akazawa Y., Nakayama H., et al. Bcl-2-like protein 13 is a mammalian Atg32 homologue that mediates mitophagy and mitochondrial fragmentation. Nat. Commun. 2015;6:7527. doi: 10.1038/ncomms8527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bhujabal Z., Birgisdottir A.B., Sjottem E., Brenne H.B., Overvatn A., Habisov S., Kirkin V., Lamark T., Johansen T. FKBP8 recruits LC3A to mediate Parkin-independent mitophagy. EMBO Rep. 2017;18:947–961. doi: 10.15252/embr.201643147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Park S., Choi S.G., Yoo S.M., Son J.H., Jung Y.K. Choline dehydrogenase interacts with SQSTM1/p62 to recruit LC3 and stimulate mitophagy. Autophagy. 2014;10:1906–1920. doi: 10.4161/auto.32177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wang Z.T., Lu M.H., Zhang Y., Ji W.L., Lei L., Wang W., Fang L.P., Wang L.W., Yu F., Wang J., et al. Disrupted-in-schizophrenia-1 protects synaptic plasticity in a transgenic mouse model of Alzheimer’s disease as a mitophagy receptor. Aging Cell. 2019;18:e12860. doi: 10.1111/acel.12860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Wei Y., Chiang W.C., Sumpter R., Jr., Mishra P., Levine B. Prohibitin 2 Is an Inner Mitochondrial Membrane Mitophagy Receptor. Cell. 2017;168:224–238 e210. doi: 10.1016/j.cell.2016.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Chu C.T., Ji J., Dagda R.K., Jiang J.F., Tyurina Y.Y., Kapralov A.A., Tyurin V.A., Yanamala N., Shrivastava I.H., Mohammadyani D., et al. Cardiolipin externalization to the outer mitochondrial membrane acts as an elimination signal for mitophagy in neuronal cells. Nat. Cell Biol. 2013;15:1197–1205. doi: 10.1038/ncb2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Princely Abudu Y., Pankiv S., Mathai B.J., Hakon Lystad A., Bindesboll C., Brenne H.B., Yoke Wui Ng M., Thiede B., Yamamoto A., Mutugi Nthiga T., et al. NIPSNAP1 and NIPSNAP2 Act as “Eat Me” Signals for Mitophagy. Dev. Cell. 2019;49:509–525 e512. doi: 10.1016/j.devcel.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 229.Lazarou M., Sliter D.A., Kane L.A., Sarraf S.A., Wang C., Burman J.L., Sideris D.P., Fogel A.I., Youle R.J. The ubiquitin kinase PINK1 recruits autophagy receptors to induce mitophagy. Nature. 2015;524:309–314. doi: 10.1038/nature14893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Cao L.L., Guan P.P., Zhang S.Q., Yang Y., Huang X.S., Wang P. Downregulating expression of OPTN elevates neuroinflammation via AIM2 inflammasome- and RIPK1-activating mechanisms in APP/PS1 transgenic mice. J. Neuroinflamm. 2021;18:281. doi: 10.1186/s12974-021-02327-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Cen X., Chen Y., Xu X., Wu R., He F., Zhao Q., Sun Q., Yi C., Wu J., Najafov A., et al. Pharmacological targeting of MCL-1 promotes mitophagy and improves disease pathologies in an Alzheimer’s disease mouse model. Nat. Commun. 2020;11:5731. doi: 10.1038/s41467-020-19547-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Yamada T., Dawson T.M., Yanagawa T., Iijima M., Sesaki H. SQSTM1/p62 promotes mitochondrial ubiquitination independently of PINK1 and PRKN/parkin in mitophagy. Autophagy. 2019;15:2012–2018. doi: 10.1080/15548627.2019.1643185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Cinque L., De Leonibus C., Iavazzo M., Krahmer N., Intartaglia D., Salierno F.G., De Cegli R., Di Malta C., Svelto M., Lanzara C., et al. MiT/TFE factors control ER-phagy via transcriptional regulation of FAM134B. EMBO J. 2020;39:e105696. doi: 10.15252/embj.2020105696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Fumagalli F., Noack J., Bergmann T.J., Cebollero E., Pisoni G.B., Fasana E., Fregno I., Galli C., Loi M., Solda T., et al. Translocon component Sec62 acts in endoplasmic reticulum turnover during stress recovery. Nat. Cell Biol. 2016;18:1173–1184. doi: 10.1038/ncb3423. [DOI] [PubMed] [Google Scholar]
- 235.Smith M.D., Harley M.E., Kemp A.J., Wills J., Lee M., Arends M., von Kriegsheim A., Behrends C., Wilkinson S. CCPG1 Is a Non-canonical Autophagy Cargo Receptor Essential for ER-Phagy and Pancreatic ER Proteostasis. Dev. Cell. 2018;44:217–232 e211. doi: 10.1016/j.devcel.2017.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Chen Q., Teng J., Chen J. ATL3, a cargo receptor for reticulophagy. Autophagy. 2019;15:1465–1466. doi: 10.1080/15548627.2019.1609862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zheng J., Chen X., Liu Q., Zhong G., Zhuang M. Ubiquitin ligase MARCH5 localizes to peroxisomes to regulate pexophagy. J. Cell Biol. 2022;221:e202103156. doi: 10.1083/jcb.202103156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Mochida K., Oikawa Y., Kimura Y., Kirisako H., Hirano H., Ohsumi Y., Nakatogawa H. Receptor-mediated selective autophagy degrades the endoplasmic reticulum and the nucleus. Nature. 2015;522:359–362. doi: 10.1038/nature14506. [DOI] [PubMed] [Google Scholar]
- 239.Wyant G.A., Abu-Remaileh M., Frenkel E.M., Laqtom N.N., Dharamdasani V., Lewis C.A., Chan S.H., Heinze I., Ori A., Sabatini D.M. NUFIP1 is a ribosome receptor for starvation-induced ribophagy. Science. 2018;360:751–758. doi: 10.1126/science.aar2663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Xu X., Sun Y., Cen X., Shan B., Zhao Q., Xie T., Wang Z., Hou T., Xue Y., Zhang M., et al. Metformin activates chaperone-mediated autophagy and improves disease pathologies in an Alzheimer disease mouse model. Protein Cell. 2021;12:769–787. doi: 10.1007/s13238-021-00858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]