Abstract
Background
Firearm sales in the United States (U.S.) markedly increased during the COVID-19 pandemic. Our objective was to determine if firearm injuries in children were associated with stay-at-home orders (SHO) during the COVID-19 pandemic. We hypothesized there would be an increase in pediatric firearm injuries during SHO.
Methods
This was a multi institutional, retrospective study of institutional trauma registries. Patients <18 years with traumatic injuries meeting National Trauma Data Bank (NTDB) criteria were included. A “COVID” cohort, defined as time from initiation of state SHO through September 30, 2020 was compared to “Historical” controls from an averaged period of corresponding dates in 2016–2019. An interrupted time series analysis (ITSA) was utilized to evaluate the association of the U.S. declaration of a national state of emergency with pediatric firearm injuries.
Results
Nine Level I pediatric trauma centers were included, contributing 48,111 pediatric trauma patients, of which 1,090 patients (2.3%) suffered firearm injuries. There was a significant increase in the proportion of firearm injuries in the COVID cohort (COVID 3.04% vs. Historical 1.83%; p < 0.001). There was an increased cumulative burden of firearm injuries in 2020 compared to a historical average. ITSA showed an 87% increase in the observed rate of firearm injuries above expected after the declaration of a nationwide emergency (p < 0.001).
Conclusion
The proportion of firearm injuries affecting children increased during the COVID-19 pandemic. The pandemic was associated with an increase in pediatric firearm injuries above expected rates based on historical patterns.
Keywords: Pediatric trauma, Firearm violence, COVID-19, Pandemic, Gun violence, 2020
Abbreviations: WHO, World Health Organization; CDC, disease control and prevention; UNESCO, United Nations Educational, Scientific, and Cultural Organization; MWPSC, Midwest Pediatric Surgery Consortium; SHO, stay-at-home orders; NTDB, national trauma data bank; SVI, social vulnerability index; ITSA, interrupted time series analysis; ISS, injury severity score; SRS, simple random sampling
1. Introduction
With the spread of the SARS-CoV2 virus (COVID-19) causing a worldwide pandemic, there have been unprecedented alterations in daily living. Following World Health Organization (WHO) recommendations for social distancing, more people began working from home, unemployment increased, and both public and private schools transitioned to temporary closure and remote education. The United Nations Educational, Scientific, and Cultural Organization (UNESCO) reported that 1.37 billion school-aged children worldwide were at one point out of school [1]. Simultaneously, as children were forced to stay at home, families experienced job loss and increased financial strain. According to the United States (U.S.) Bureau of Labor Statistics, the United States reached an unemployment rate of almost 15% at its peak [2] .
During this time, Americans began to purchase firearms at an extraordinary rate. In the first four months of the pandemic, 4.3 million more firearms were purchased in the U.S than expected based on historical trends, an 85% increase [3]. In addition, the United States experienced heightened racial tensions in 2020 with several high-profile police shootings. Many of these events occurred within the Midwest region, where there was heightened awareness that children were increasingly becoming victims of firearm injuries [4], [5], [6].
The objectives of this study were to determine the association of the start of the COVID-19 pandemic with firearm injuries and to explore the change in predictors of firearm injuries and outcomes before and after SHO. We hypothesized that the COVID-19 pandemic would be associated with an increase in firearm injuries among children.
2. Methods
2.1. Study design and population
In this multi institutional study, nine Level I pediatric trauma centers from the Midwest Pediatric Surgery Consortium (www.mwpsc.org) contributed local trauma registry data from January 1, 2016 to September 30, 2020. Study inclusion criteria comprised injured children <18 years old who met National Trauma Data Bank (NTDB) standards, such as those admitted, transferred, and/or died. A complete list of inclusion criteria can be found on the American College of Surgeons’ NTDB website [7]. Institutional review board approval was obtained at each site with a waiver of consent.
The primary aim of the study was to evaluate the association of the COVID-19 pandemic with changes in pediatric firearm injuries. The primary outcome of interest was change in the volume of pediatric firearm-related injuries. Secondary outcomes included mortality, hospital length of stay (LOS), and hospital disposition. Intensive care unit (ICU) stay and days on mechanical ventilation were analyzed only for those patients who had an ICU LOS or ventilator days ≥ 1 day, respectively.
The study population was divided into two cohorts. The first was the “COVID” cohort, which was defined as patients who were injured from the date of the SHO to September 30, 2020. Each site's individual SHO orders were defined based on local and state ordinances. A “Historical” cohort was used as the comparator. Patients from corresponding SHO dates to September 30 from 2016 to 2019 were averaged in order to minimize outlying effects from any one year. In addition, a sensitivity analysis comparing the COVID cohort to patients evaluated over the same period in 2019 alone was completed to account for temporal changes in care (e.g., population changes, catchment area re distribution, triage pattern changes including centralization or decentralization). Demographics, injury characteristics, and outcomes were compared between cohorts. Using the U.S. Department of Agriculture's definition of rural counties, a crosswalk was used to code resident zip codes into urban or rural categories [8]. Rural was defined as open countryside, towns with <2500 people, and cities with 2500–49,999 people not part of a larger metropolitan area. Specific injuries were categorized by body region using the International Classification of Disease 10th revision (ICD-10) diagnosis codes to obtain a more granular description of the firearm injuries. Location External Cause Codes were used to categorize those injuries that occurred inside or outside a home. Data for this variable were only available from 7 of the 9 sites, and only those sites were included in this specific analysis.
Predictors of pediatric firearm violence were explored. The year 2020, following SHO dates, was the exposure period of interest. With known associations between social determinants of health and firearm violence [9], we set out to determine the association between firearm violence and social vulnerability. The CDC's Social Vulnerability Index (SVI) ranks each census tract on 15 social factors compromising 4 domains: socioeconomic status, household composition and disability, minority status and language, and housing and transportation. An SVI of 0 indicates the population of lowest level of vulnerability and 1 the highest vulnerability. SVI as a predictor of pediatric firearm violence was examined.
2.2. Statistical analysis
The Pearson Chi Square was used to compare categorical variables, while Student's t-test and Wilcoxon rank-sum were used to compare normally distributed continuous variables and non parametric continuous variables, respectively. If missing data comprised >5% then it would be presented in the results section. Significance was set at p < 0.05. Using a LOESS smoothing technique, month-to-month variations in gun violence were graphed for the two cohorts, COVID vs. Historical. We considered both the average number of firearm injuries per month and the cumulative burden of firearm injuries throughout the year.
Among all injured patients, logistic regression was used to assess a child's odds of firearm injury post COVID-19 pandemic in 2020 compared to the Historical cohort, controlling for age, sex, race, SVI. To minimize any regional confounders, clustering by site was also included in the model. Simple random sampling (SRS) of the non firearm injuries was compared to firearm injuries owing to the imbalance in population sizes. The SRS model was bootstrapped 1000 times to limit any potential rare event bias.
An interrupted time series analysis (ITSA), using a Poisson distribution, was used to determine the difference in expected and observed rates of firearm injuries in a longitudinal fashion, while still controlling for the known temporal variations of traumatic injuries. An “interruption” of March 13, 2020 was used as this was the date of declaration of a state of emergency in the U.S in response to the COVID-19 pandemic. Local and regional SHO went into effect shortly following this announcement. Variations between expected versus observed rates of firearm injuries per month were compared. All analyses were performed using R statistical software (RStudio, version 1.4.1717 © 2009–2021 RStudio, PBC) [10].
3. Results
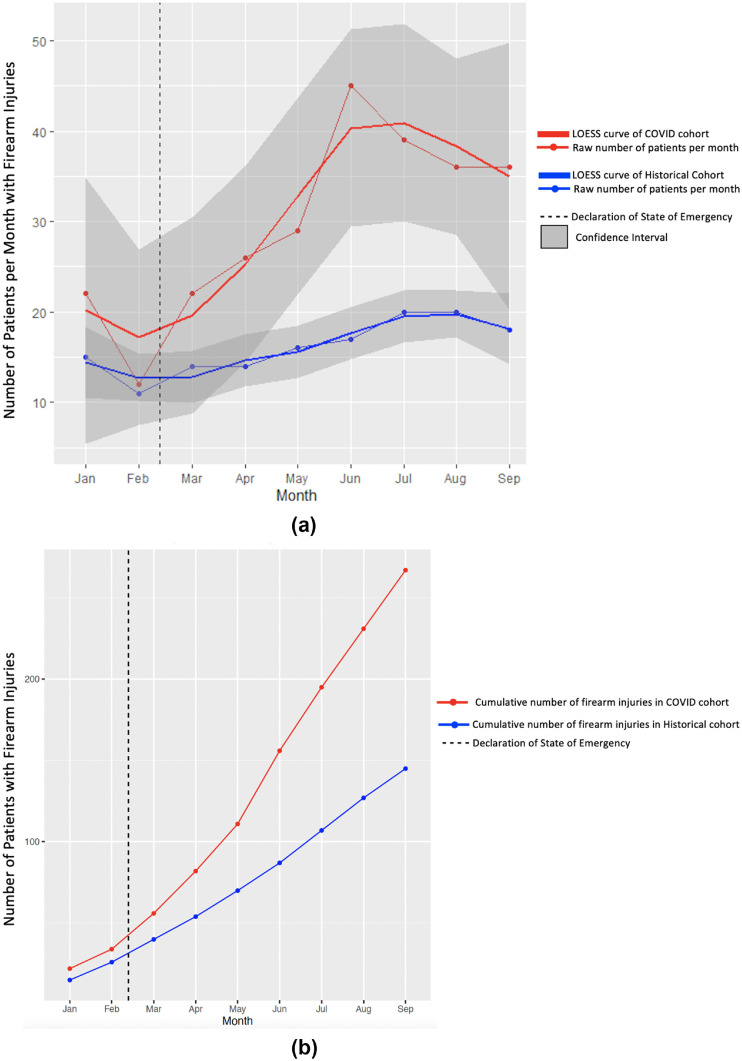
From January 1, 2016 to September 30, 2020, a total of 47,385 pediatric trauma patients met inclusion criteria. Of this population, 1,062 children (2.2%) sustained firearm injuries. Overall, the COVID cohort experienced significantly more firearm injuries than the averaged Historical cohort (COVID 215 patients (3.04%) vs. Historical 108 patients (1.83%); p < 0.001). This was consistent in the sensitivity analysis using just 2019 data (COVID 215 patients (3.04%) vs. Historical 109 patients (1.79%); p < 0.001). The number of firearm injuries observed each month significantly increased in March through September 2020 relative to the Historical cohort (p = 0.006, Fig. 1 a) with an increased cumulative burden of firearm injuries in 2020 when compared with prior years (Fig. 1b).
Fig. 1.
(a) Frequency of firearm injuries by month across all sites with a LOESS smoothing line; (b) Cumulative firearm injuries by month across all sites.
There were no significant differences in baseline characteristics of sex, age, SVI, or Injury Severity Score (ISS). There was a significant difference in ethnicity across cohorts (Table 1 ); however, this was driven by a decrease in “unknowns” in the COVID cohort. There were no significant differences in the intent of firearm injuries and the proportion of injuries that occurred in the home (Table 1). The sensitivity analysis using 2019 as a recent historical control did not vary greatly from the averaged Historical cohort in terms of demographics or outcomes (Supplement Tables 1 and 2). There was no significant change in the COVID cohort with respect to the specific types of injuries resulting from firearms when compared to the Historical cohort (Supplement 3). In addition, there were no significant differences in the mortality, hospital or ICU length of stay, ventilator days, or hospital disposition between cohorts (Table 2 ).
Table 1.
Demographic and injury characteristics; Number (%).
| Historical average 2016–2019 Total N = 431 Averaged N = 108 |
COVID 2020 N = 215 |
p-value | ||
|---|---|---|---|---|
| Male | 82 (76.6) | 164 (76.3) | 0.696 | |
| Age, years | 0.948 | |||
| <1 | 2 (1.9) | 3 (1.4) | ||
| 1–4 | 12 (11.1) | 26 (12.1) | ||
| 5–9 | 13 (12.0) | 20 (9.3) | ||
| 10–14 | 31 (28.7) | 64 (29.8) | ||
| 15–17 | 50 (46.3) | 102 (47.4) | ||
| Mean age, years (SD) | 12.3 (4.8) | 12.5 (4.8) | 0.55 | |
| Race | 0.464 | |||
| White | 23 (21.3) | 39 (18.1) | ||
| African American | 76 (70.4) | 149 (69.3) | ||
| Other | 9 (8.3) | 27 (12.6) | ||
| Ethnicity | <0.001 | |||
| Hispanic | 4 (3.7) | 17 (7.9) | ||
| Non-Hispanic | 79 (73.8) | 187 (87.0) | ||
| Unknown | 24 (22.4) | 11 (5.1) | ||
| Residence | 1.0 | |||
| Rural | 6 (5.6) | 11 (5.1) | ||
| Urban | 101 (94.4) | 203 (94.9) | ||
| Social Vulnerability Index, quartiles | 0.277 | |||
| 1st Quartile, least vulnerable | 8 (7.5) | 7 (3.3) | ||
| 2nd Quartile | 19 (17.8) | 48 (22.3) | ||
| 3rd Quartile | 38 (35.5) | 69 (32.1) | ||
| 4th Quartile, most vulnerable | 42 (39.3) | 91 (42.3) | ||
| Weighted Mean SVI (SD) | 0.64 (0.21) | 0.66 (0.20) | 0.3 | |
| Median Household Income | 0.201 | |||
| 1st Quintile | 53 (49.1) | 105 (48.8) | ||
| 2nd Quintile | 23 (21.3) | 49 (22.8) | ||
| 3rd Quintile | 14 (13.0) | 28 (13.0) | ||
| 4th Quintile | 9 (8.3) | 27 (12.6) | ||
| 5th Quintile | 9 (8.3) | 6 (2.8) | ||
| Payor | 0.289 | |||
| No Insurance | 9 (8.4) | 22 (10.2) | ||
| Private | 19 (17.8) | 26 (12.1) | ||
| Public | 77 (72.0) | 156 (72.6) | ||
| Unknown/Missing | 2 (1.9) | 11 (5.1) | ||
| Injury Severity Score (ISS) | 0.779 | |||
| 0–15 | 44 (41.5) | 97 (45.1) | ||
| 16–24 | 14 (13.2) | 24 (11.2) | ||
| 25+ | 48 (45.3) | 94 (43.7) | ||
| Injury Intent | 0.299 | |||
| Unintentional | 29 (26.9) | 52 (24.2) | ||
| Assault | 64 (59.3) | 136 (63.3) | ||
| Suicide | 5 (4.6) | 3 (1.4) | ||
| Other | 10 (9.3) | 24 (11.2) | ||
| Location of Injury* | 0.93 | |||
| Home | 31 (40.8) | 60 (40.5) | ||
| Other | 44 (57.9) | 85 (57.4) | ||
Includes 7 of the 9 sites.
Table 2.
Outcomes after firearm injury; Number (%).
| Historical average 2016–2019 Total N = 431 Averaged N = 108 |
COVID 2020 N = 215 |
p-value | |
|---|---|---|---|
| Overall mortality | 9 | 15 | 0.999 |
| Death in ED | 4 (44.4%) | 8 (53.3) | |
| Inpatient death | 5 (55.6) | 7 (46.7) | |
| ED Disposition | 0.731 | ||
| Floor/Observation | 45 (41.7) | 90 (41.9) | |
| ICU | 17 (15.7) | 24 (11.2) | |
| Operating Room | 26 (24.1) | 46 (21.4) | |
| Transfer Out | 2 (1.9) | 7 (3.3) | |
| Morgue | 4 (3.7) | 8 (3.7) | |
| Home | 10 (9.3) | 32 (14.9) | |
| Unknown | 4 (3.7) | 8 (3.7) | |
| Hospital Disposition | 0.457 | ||
| Morgue | 5 (5.4) | 7 (4.3) | |
| Home & Home Services | 72 (77.4) | 133 (81.1) | |
| Other Facility | 9 (9.7) | 14 (8.5) | |
| Jail or Against Medical Advice | 3 (3.2) | 2 (1.2) | |
| Unknown | 4 (4.3) | 8 (6.9) | |
| Median vent days [IQR]^ | 2.5 [1], [2], [3], [4], [5], [6], [7] | 4 [1], [2], [3], [4], [5] | 0.64 |
| Median LOS, ICU [IQR]^ | 3 [2–6.5] | 3 [2], [3], [4], [5] | 0.95 |
| Median LOS, hospital [IQR] | 2 [1], [2], [3], [4], [5], [6], [7] | 2 [1], [2], [3], [4], [5], [6] | 0.98 |
Of patients that had vent or ICU LOS ≥1day.
In univariate analyses, age, sex, race and SVI were associated with increased odds of pediatric firearm injury (Table 3 ) and were thus included in the multivariate model. In adjusted analysis, injured children were at almost 80% increased odds of suffering a firearm injury post SHO in 2020 compared to prior years (adjusted odds ratio (aOR) 1.78, 95% CI 1.45–2.12, p < 0.001; Table 4 ). In the sensitivity analysis using bootstrapped SRS, a similar effect size was demonstrated, with children at 63% higher odds of sustaining a firearm injury in 2020 (aOR 1.63, 95% CI 1.17–2.27, p = 0.018; Supplement Table 4).
Table 3.
Univariate regression for the association with firearm injuries compared to any other type of injury.
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Age, years | |||
| < 1 | 0.49 | 0.25–0.89 | 0.030 |
| 1–4 | 1.55 | 1.11–2.14 | 0.009 |
| 5–9 | Ref | – | – |
| 10–14 | 3.30 | 2.52- 4.36 | <0.001 |
| 15–17 | 10.38 | 8.06–13.56 | <0.001 |
| Sex (Male) | 2.06 | 1.72–2.48 | <0.001 |
| Race | |||
| Caucasian | Ref | – | – |
| African American | 15.91 | 13.11–19.44 | <0.001 |
| Minority, other | 4.25 | 2.90–6.24 | <0.001 |
| Other | 3.93 | 2.51–5.82 | <0.001 |
| Social Vulnerability Index (SVI), Quartile | |||
| 1st, most resourced | Ref | – | – |
| 2nd | 1.9 | 1.34–2.75 | <0.001 |
| 3rd | 3.631 | 2.62–5.16 | <0.001 |
| 4th least resourced | 12.81 | 9.27–18.18 | <0.001 |
Table 4.
Multivariate regression with aggregate population measuring the association of the COVID pandemic (2020) and firearm injury, accounting for demographic factors.
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| Historical Control | Ref | – | – |
| COVID Cohort | 1.78 | 1.45–2.12 | <0.001 |
| Age, years | |||
| < 1 | 0.37 | 0.18- 0.69 | 0.002 |
| 1–4 | 1.31 | 0.94–1.82 | 0.108 |
| 5–9 | Ref | – | – |
| 10–14 | 2.89 | 2.20–3.85 | <0.001 |
| 15–17 | 8.41 | 6.47–11.06 | <0.001 |
| Gender (Male) | 1.65 | 1.37–2.01 | <0.001 |
| Race | |||
| Caucasian | Ref | – | – |
| African American | 10.65 | 8.61–13.25 | <0.001 |
| Minority, other | 4.24 | 2.83–6.18 | <0.001 |
| Other | 3.39 | 2.23–5.17 | <0.001 |
| Social Vulnerability Index (SVI), Quartile | |||
| 1st, most resourced | Ref | – | – |
| 2nd | 1.57 | 1.10–2.29 | 0.015 |
| 3rd | 2.30 | 1.64–3.3 | <0.001 |
| 4th least resourced | 3.63 | 2.56–5.27 | <0.001 |
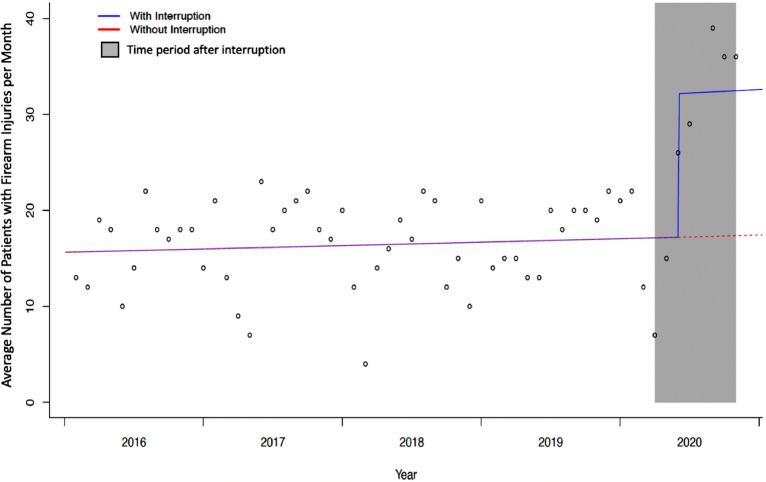
After the declaration of a state of emergency, there was an increase in observed firearm injuries over the expected rate (Fig. 2 ). This difference was statistically significant within the Poisson model, which calculated 87% higher odds of injured children suffering firearm injuries during the COVID-19 pandemic following SHO (OR 1.87, 95% CI 1.54–2.28, p < 0.001).
Fig. 2.
Interrupted time series with the interruption point representing the declaration of state of emergency in the U.S. (March 13, 2020).
4. Discussion
This study found that during the COVID-19 pandemic, there was a significant change in the volume of pediatric firearm injuries. There was an increased cumulative burden of firearm injuries in 2020 compared to a historical average. After controlling for multiple risk factors, injured children were at higher odds of sustaining a firearm injury in 2020 compared to prior years. Furthermore, there was an increase in the observed rate of firearm injuries above that of the expected rate after the onset of the COVID-19 pandemic. Although our study group found that occupancy motor vehicle collisions decreased during the pandemic, there was an increase in falls and injuries from bicycles and ATVs, leading to a net increase in overall trauma [11]. Thus, the rise in the proportion of firearm injuries is not fully explained by an overall decrease in other mechanisms of injury.
To date, there have been two other studies published evaluating rates of pediatric firearm injuries during the COVID-19 pandemic. Cohen et al. queried the Gun Violence Archive for patients <12 years old and found that from March to August 2020, firearm injuries both suffered and perpetrated by children increased when compared to historical controls [12]. Although our study also included adolescents, similar trends were observed. Gastineau et al. probed the Pediatric Health Information System and reported an almost 40% increase in firearm-related encounters in 2020 when compared to 2017–2019, although there was no change in patient demographics between time points [13]. We observed increased firearm injury rates during the COVID-19 pandemic, supporting the findings of these studies. Our study uniquely found that the least resourced children, measured by those in the 4th SVI quartile, were at the greatest risk during this time.
In adults, analogous findings have been observed. Several single and multi institutional studies have shown that firearm injuries in adults increased after SHO when compared to previous years [14], [15], [16], [17]. There may be a regional effect on the change in frequency in firearm injuries, with Midwest and urban areas experiencing a greater increase in firearm injuries compared to Western states and rural areas [16,18]. Our study confirms that the increase in firearm injuries after SHO in the Midwest also affected children with an increased cumulative burden of firearm injuries and a significant increase in the odds of an injured child sustaining a firearm injury compared to prior years.
The downstream consequences of the COVID-19 pandemic and SHO have yet to be completely understood; however, as fear, mistrust, and uncertainty increased, many individuals obtained firearms for protection [19,20]. There was an unprecedented surge in US gun and ammunition sales in 2020, often by first-time buyers who may also be less likely to know how to safely use, secure and store weapons [3,19,21]. Additionally, some parents reported that fear of protests, home invasion, or the unknown caused them to make firearms more accessible to their adolescent children [20].
There were several limitations to our study. First, this was a retrospective study with its inherent limitations, including an inability to determine causation rather than association between events. We chose to use institutional trauma registry data and therefore were limited to evaluating patients whose injuries met NTDB inclusion criteria, thus excluding patients who were discharged directly home from the ED or who died before hospital arrival. Implementation of SHO orders varied between different regions and states, which may have caused some site variations in its effects. Despite the large catchment areas of the included trauma centers, this study was not a population-based assessment and thus generalizability may be limited.
5. Conclusions
The proportion of firearm injuries affecting children increased during the COVID-19 pandemic. After controlling for significant demographics, injured children were at higher odds of sustaining a firearm injury in 2020 compared to previous years. The pandemic was associated with an increase in pediatric firearm injuries above expected rates based on historical patterns. Future work must determine if this increase was a transient shift during the acute phase of the pandemic or rather a sustained level of increased violence. This work will help direct resources toward firearm injury prevention should the trend continue.
Level of evidence: III.
Declaration of Competing Interest
The authors have no financial disclosures. The study had no source of funding.
Acknowledgments
We would like to thank the research coordinators and trauma registrars at each of the participating sites for their help in obtaining institutional data, including Sarah Fox, Jill Jaeger, Kristin Braun, Jane Riebe-Rodgers, Suzanne Moody, Taunya Kessler, Jessica Johnson, Carley Lutz, Michelle Bainter, Jodi Raymond, Pete Muenks, Elizabeth McClure, Jennifer Seay, Linda Cherney, Benjamin Eithun, Loran Zwiefelhofer, Connor Fairfax, and Amanda Truelove. A special thanks to Sarah Fox, the MWPSC Project Manager, for her efforts in helping the MWPSC to run smoothly and efficiently.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpedsurg.2022.03.034.
Appendix. Supplementary materials
References
- 1.UNESCO . UNESCO; 2021. 1.37 Billion students now home as COVID-19 school closures expand, ministers scale up multimedia approaches to ensure learning continuity.en.unesco.org/news/137-billion-students-now-home-covid-19-school-closures-expand-ministers-scale-multimedia 5 May. [Google Scholar]
- 2.“Employment Situation News Release.” U.S. Bureau of Labor Statistics, U.S. Bureau of Labor Statistics, 3 Sept. 2021, www.bls.gov/news.release/empsit.htm.
- 3.Schleimer J.P., McCort C.D., Shev A.B., et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a cross-sectional study. Inj Epidemiol. 2021;8(1):43. doi: 10.1186/s40621-021-00339-5. Published 2021 Jul 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kravitz-Wirtz N., Aubel A., Schleimer J., Pallin R., Wintemute G. Public concern about violence, firearms, and the COVID-19 pandemic in California. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.33484. Published 2021 Jan 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cluver L., Lachman J.M., Sherr L., et al. Parenting in a time of COVID-19. Lancet. 2020;395(10231):e64. doi: 10.1016/S0140-6736(20)30736-4. [published correction appears in Lancet. 2020 Apr 11;395(10231):1194] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sanford E.L., Zagory J., Blackwell J.M., et al. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg. 2021;56(5):918–922. doi: 10.1016/j.jpedsurg.2021.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.“National Trauma Data Standard (NTDS).” American College of Surgeons, https://www.facs.org/quality-programs/trauma/tqp/center-programs/ntdb/ntds.
- 8.Cromartie, J. “Overview: rural classifications.” USDA economic research service, United States Department of Agriculture, 17 June 2021, https://www.ers.usda.gov/topics/rural-economy-population/rural-classifications/.
- 9.Phelos H.M., Deeb A.P., Brown J.B. Can social vulnerability indices predict county trauma fatality rates? J Trauma Acute Care Surg. 2021;91(2):399–405. doi: 10.1097/TA.0000000000003228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.R Core Team (2021). R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
- 11.Katherine T F.O.B., Amelia T C., Farazi M., et al. Pediatric injury trends and relationships with social vulnerability during the COVID-19 pandemic: a multi-institutional analysis. J Trauma Acute Care Surg. 2022 doi: 10.1097/TA.0000000000003687. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen J.S., Donnelly K., Patel S.J., et al. Firearms injuries involving young children in the United States during the COVID-19 pandemic. Pediatrics. 2021;148(1) doi: 10.1542/peds.2020-042697. [DOI] [PubMed] [Google Scholar]
- 13.Gastineau K.A.B., Williams D.J., Hall M., et al. Pediatric firearm-related hospital encounters during the SARS-CoV-2 pandemic. Pediatrics. 2021;148(2) doi: 10.1542/peds.2021-050223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdallah H.O., Zhao C., Kaufman E., et al. Increased firearm injury during the COVID-19 pandemic: a hidden urban burden. J Am Coll Surg. 2021;232(2):159–168. doi: 10.1016/j.jamcollsurg.2020.09.028. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chodos M., Sarani B., Sparks A., et al. Impact of COVID-19 pandemic on injury prevalence and pattern in the Washington, DC Metropolitan Region: a multicenter study by the American College of Surgeons Committee on Trauma, Washington, DC. Trauma Surg Acute Care Open. 2021;6(1) doi: 10.1136/tsaco-2020-000659. Published 2021 Jan 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Donnelly M.R., Grigorian A., Inaba K., et al. A dual pandemic: the influence of Coronavirus disease 2019 on trends and types of firearm violence in California, Ohio, and the United States. J Surg Res. 2021;263:24–33. doi: 10.1016/j.jss.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim D.Y., Phillips S.W. When COVID-19 and guns meet: a rise in shootings. J Crim Justice. 2021;73 doi: 10.1016/j.jcrimjus.2021.101783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salottolo K., Caiafa R., Mueller J., et al. Multicenter study of US trauma centers examining the effect of the COVID-19 pandemic on injury causes, diagnoses and procedures. Trauma Surg Acute Care Open. 2021;6(1) doi: 10.1136/tsaco-2020-000655. Published 2021 Apr 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons V.H., Haviland M.J., Azrael D., et al. Firearm purchasing and storage during the COVID-19 pandemic. Inj Prev. 2021;27(1):87–92. doi: 10.1136/injuryprev-2020-043872. [DOI] [PubMed] [Google Scholar]
- 20.Sokol R.L., Marineau L., Zimmerman M.A., Rupp L.A., Cunningham R.M., Carter P.M. Why some parents made firearms more accessible during the beginning of the COVID-19 pandemic: results from a national study [published online ahead of print, 2021 Jul 23] J Behav Med. 2021:1–7. doi: 10.1007/s10865-021-00243-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Donnelly M.R., Barie P.S., Grigorian A., et al. New York State and the Nation: trends in firearm purchases and firearm violence during the COVID-19 pandemic. Am Surg. 2021;87(5):690–697. doi: 10.1177/0003134820954827. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.