Abstract
E-cigarette usage (also known as e-cigarettes or vaping products) has increasingly been recognized as a global public health problem. One challenge in particular involves their marketing to minors (teenagers and children) and the rising prevalence of use in this population. E-cigarettes unnecessarily expose minors to health risks, these include respiratory health problems, such as exacerbations of asthma, bronchitis, and respiratory-tract irritation. Nicotine, commonly found in e-cigarettes, is also associated with cognitive impairment and neurodevelopmental problems. E-cigarettes are also risk factors for downstream substance use, including cigarettes and cannabis initiation (the gateway hypothesis), which compounds health risks in dual users. Current public health preventative and intervention studies are limited, and there is a clear need for more interventions that may prevent usage and assist with cessation in this vulnerable population. Physician education and screening uptake should also be enhanced. Stricter public health policy and protection measures are also needed on a global scale to limit e-cigarette exposure in minors.
Subject terms: Epidemiology, Respiratory signs and symptoms, Epidemiology, Health policy, Disease prevention
Introduction
The use of electronic cigarettes (also known as e-cigarettes, e-cigs, or vaping products) has increasingly been recognized as a global public health problem1. Vaping consists of inhaling a smoke-free aerosol through a mouthpiece, which is produced through the heating of a liquid such as glycol or glycerin in an electronic device2,3. Most e-cigarettes have the shape of a pen, but others are more discrete-looking such as JUUL, which resembles a USB drive and is popular among teenagers4. Common terminology for e-cigarettes is summarized in Table 1. E-cigarettes have often been used by smokers as a harm-reduction intervention aimed to assist with cigarette-smoking cessation5. A meta-analysis found that e-cigarette users (who received free e-cigarettes in trials) were 1.5 times more likely to quit smoking than the control group6. Thus, they may play a role in smoking cessation in adult smokers and the benefits of use may outweigh the risks from a public health-harm reduction perspective as they are a safer alternative7. However, e-cigarettes are increasingly initiated by teenagers, some of whom have never previously smoked8 and who are exposed to unnecessary health risks associated with e-cigarette use, making them a public health issue9.
Table 1.
| Term | Meaning |
|---|---|
| Electronic cigarettes | A battery operated device, which heats a liquid, commonly containing glycerol, glycol, nicotine, flavorings, and other additives, producing an aerosol, which the user inhales with the mouthpiece. The cartridge is either refillable or disposable. |
| E-cigarettes/E-cigs | Short terminology for electronic cigarettes |
| Vape pens | Another term for e-cigarettes that are shaped like or resemble pens |
| Pods | Another term for e-cigarettes |
| Vape products | A term which broadly includes all forms of electronic cigarettes made by different manufacturers including nicotine free e- cigarettes and ones with nicotine along with other chemical additives |
| Vaping | The act of (verb) using electronic cigarettes/ vape products by inhalation of the smoke free aerosol that is generated from the device |
| Juice | The liquid that is added to electronic cigarettes, which is heated for inhalation by the user. It can include nicotine, cannabis oil, flavorings, and other chemical additives. |
| JUUL | A discrete looking electronic cigarette device which resembles a USB drive and has a high content of nicotine |
| EVALI | Electronic Cigarette of Vaping Related Lung Injury resulting from the inhalation of vitamin E acetate and cannabis using electronic cigarettes |
Some of the reported reasons for e-cigarette use in teenagers and young adults include their flavoring10,11, discreteness12, easy accessibility10, desire to experiment10, perceptions that they are safer10, and advertising as well as marketing that directly targets young people13. Research on flavoring found that sweet flavors (e.g., fruity or candy flavored) were more often selected by teenagers over tobacco or minty flavored (conventional) e-cigarettes14.
Here, we review of the epidemiology of e-cigarette use in teenagers and young adults and associated health risks, theoretical mechanisms, and management, including prevention as well as interventions and policies. The overarching aim is to provide an in-depth overview of e-cigarette usage in teenagers and young adults from a public health perspective and to provide insight into emerging trends as well as opportunities for health promotion.
Methods
A review of PubMed (Medline) and Google Scholar was undertaken in September 2021. We broadly included all up-to-date studies that were related to teenage-vaping epidemiology, mechanisms, and global policies published in the English language. Primary studies that were not undertaken in teenager ages 13–18 or young-adult ages 19–24 were excluded. Systematic reviews and meta-analyses were only included if they were related to global policies or epidemiological updated findings related to our study population or highly applicable to it. Studies on youth perceptions of e-cigarettes were only included if the papers addressed policy.
We used broad search terms that included word variations for “e-cigarettes” or “vaping”, “teenagers”, “respiratory health effects”, and “vaping policies”. MESH terminology and free text was used in the search. A medical librarian assisted with the search strategy. Manual hand and primary government-database searches were also undertaken. The details of the Medline search-strategy example are summarized in Table 2.
Table 2.
PubMed/Medline search strategy.
| Topic | Keywords |
| Population |
“adolescent”[MeSH Terms] OR “adolescen*”[All Fields] OR “youth”[tiab] OR “youths”[tiab] OR “teen”[tiab] OR pubescen*[tiab] OR puberty[tiab] OR minor[tiab] OR minors[tiab] OR underage*[tiab] OR “under age*”[tiab] OR “young adult”[mesh] OR young adult*[tiab] OR “high school*”[tiab] OR student*[tiab] AND |
| Intervention |
(“Counseling”[Mesh] OR counsel*[tiab]) OR (((reduc*[ti] OR decreas*[ti]) AND (use[tiab] OR utilization[tiab]))) OR (“harm reduction*”[tiab] OR “Mass Screening”[Mesh] OR “screen*”[tiab] OR “routine testing”[tiab] OR experiment*[tiab] OR intervention*[tiab] OR study[tiab] OR studies[tiab] OR trial*[tiab] OR RCT[tiab] OR random*[tiab] OR “secondary prevention”[mesh] OR “tertiary prevention”[mesh] OR quit*[tiab] OR stop[ti] OR stopped[ti] OR stopping[ti] OR stops[ti]) OR (“Health campaign*”[tiab] OR “education campaign*”[tiab] OR “educational campaign*”[tiab] OR “media campaign*”[tiab]) OR (((Public health[ti] OR regulat*[ti]) AND (effect*[tiab] OR impact*[tiab] OR strateg*[tiab] OR campaign*[tiab] OR policy[tiab] OR policies[tiab] OR program*[tiab]))) OR (Taper*[tiab] OR “Behavioral support*”[tiab] OR “behavioral support*”[tiab] OR “Behavioral therap*”[tiab] OR “Behavioral therap*”[tiab] OR manag*[ti] OR control*[ti]) OR (((“flavoring agents”[mesh] OR flavor*[tiab] OR flavor*[tiab]) AND (restrict*[tiab] OR limit*[tiab] OR decreas*[tiab]))) OR (“reduced risk”[tiab] OR “risk reduction”[tiab] OR “vaping cessation”[tiab] OR “cessation therap*” OR “cessation treatment*”[tiab]) OR ((increas*[tiab] AND price[tiab])) OR (“smoke free law”[tiab] OR “smoke free laws”[tiab] OR “population health standard*”[tiab] OR “warning label*”[tiab] OR tax[tiab] OR taxation[tiab] OR taxed[tiab] OR taxes[tiab] OR taxing[tiab] OR tax[tiab] OR taxation[tiab] OR taxed[tiab] OR taxes[tiab] OR taxing[tiab] OR “Commerce”[Mesh]) OR (((“Flavoring Agents”[Mesh] OR flavor*[tiab] OR flavor*[tiab]) AND (restricted[tiab] OR restriction[tiab] OR limit*[tiab] OR decreas*[tiab]) OR (increas*[tiab] AND price[tiab]))) OR (((reduc*[tiab] OR decreas*[tiab]) AND (use[tiab] OR utilization[tiab]))) OR (“Government Regulation”[Mesh] OR “Public Policy”[Mesh] OR “legislation and jurisprudence”[MeSH Subheading]) OR (“prevention and control”[sh] OR “public health”[mesh:noexp] OR “consumer product safety”[mesh] OR “public health practice”[mesh]) AND |
| Outcome |
“adverse effects” OR “Lung injury” OR “EVALI” OR “toxicity”[Subheading] OR “poisoning” OR “irritation” OR “inflammation” OR “pneumonia” OR “allergy” OR intoxication OR “respiratory effect” OR “cardiovascular” OR “health effect*” OR “case report*” OR “adverse effects”[Subheading] OR “lung injury”[MeSH Terms] OR “poisoning”[MeSH Terms] OR “poisoning”[Subheading] OR “poisons”[MeSH Terms] OR “poisons”[All Fields] OR “irritants”[MeSH Terms] OR “inflammation”[MeSH Terms] OR “pneumonia”[MeSH Terms] OR “hypersensitivity”[MeSH Terms] OR “allergy and immunology”[MeSH Terms] OR “cardiovascular system”[MeSH Terms] OR casereports[Filter] Combined into one large search string |
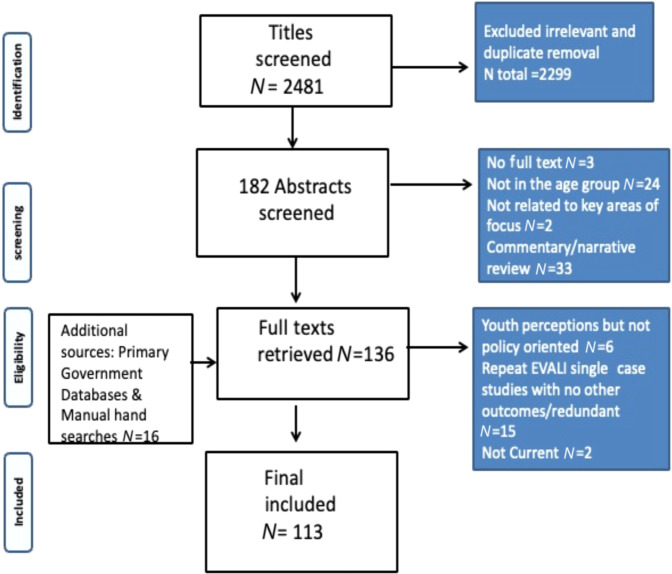
After screening 2481 titles against the inclusion and exclusion criteria, followed by abstract screening and full-text retrieval, 113 studies were included in the final review. Figure 1 illustrates the search process (PRISMA flow chart)15.
Fig. 1.
Prisma flow chart.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Results
Epidemiology
The uptake of e-cigarettes has markedly increased in recent years across the globe16. A systematic review found that e-cigarette usage in teenagers increased by over 19% between 2011 and 2018 in the United States12. Studies have also reported an increase in the prevalence of use in Canada and the United Kingdom9. According to the report from the Canadian Student Tobacco, Alcohol, and Drugs Survey, the prevalence of e-cigarette usage in teens (grades 7–12) within the past 30 days was 20 percent in 2018–2019, a doubling of the prevalence in the previous year’s report17. A total of 90% had consumed products containing nicotine17. Between 2010 and 2014, there was a 24.4% rise in e-cigarette use among teens in Eastern and Central Europe18. The study had also found that a large proportion of students (43.7%) had previously tried e-cigarettes18, highlighting that many young adults have previously experimented with e-cigarettes.
Prevalence of ever use of e-cigarettes appears to be lower in Asian countries such as Japan, where 3.5% reported past use, and South Korea, where 10.1% reported previous experimentation with e-cigarettes19,20. One study in China reported a low prevalence of past 30-day use of 1.2%, though the study was undertaken in middle-school students instead of high-school students, which could have underestimated teenage e-cigarette use21. However, more studies are needed in this region to better ascertain the prevalence of use and changes over time. Data from South America are further limited, but older studies in Brazil (2015) indicate that 2.1% had ever tried e-cigarettes22. Additionally, there was a reported rise in prevalence of teenage e-cigarette usage in Argentina between 2014 and 2015 of 5.2%23. There are fewer studies in low-income countries, in particular in Africa and India24, where the prevalence of e-cigarette use in teenagers is underreported. There is a gap in the literature in low-income countries, highlighting that the topic of e-cigarette use in teenagers remains relatively unexplored and more research is needed in this area.
Figure 2 compares reported proportions of “ever use” of e-cigarettes in teenagers across high-income countries, including Canada, the United States, Great Britain, and Europe between 2015–2017 and 2018–201925–28. Figure 3. compares trends in past 30-day prevalence of e-cigarettes from 2015 to 2020 in North America. Overall, the trends indicate a rise in prevalence and past use of e-cigarettes across countries9,27,29–33, though prevalence of use declined in 2020 during the pandemic according to data from Canada and the United States27,31.
Fig. 2. History of “Ever Use” of e-cigarettes in teenagers by country and period9,18,25–27,30,33.
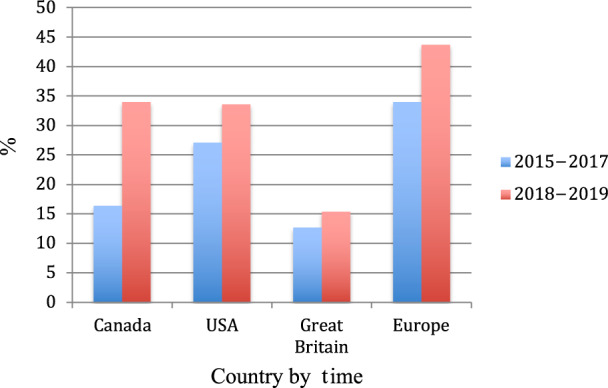
History of “ever use” of e-cigarettes in Canada, the United States, Great Britain, and the rest of Europe between 2015–2017 and 2018–20199,18,25–27,30,33. If countries reported history of past use within any of these time periods, they were included. Please note that the 2015–2017 prevalence of ever use is for the following European countries: Belgium, Finland, Germany, Ireland, Italy, the Netherlands, and Portugal28. The 2018–2019 report in Europe collected data from Central and Eastern Europe, including the following countries: Poland, Lithuania, Belarus, Slovakia, and Russia18. It should be noted that while the report by Hammond et al9 reported a prevalence of “ever use” in the United Kingdom of 32.7% (2018), the Action and Smoking on Health Report in England25 produced a significantly lower prevalence of 16.4% for the same period in Great Britain. It could be that Northern Ireland has a higher prevalence of ever use and was omitted from the report.
Fig. 3. Prevalence of e-cigarette use (past 30 days) in teenagers in North America over a five year period (between 2015 and 2020)9,27,29–33.
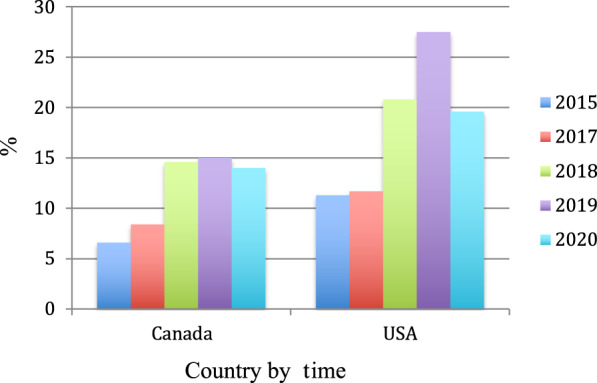
Past 30-day prevalence of e-cigarette use from 2015 to 2020 in North America (comparisons between Canada and the United States) in teenagers (grades 7 through 12). Reported prevalence declined in 2020 during the COVID-19 pandemic. The Canadian Tobacco and Nicotine Surveys were used for 2015, 2019, and 2020 surveys, respectively27,29. The 2018–2019 surveys for Canada were obtained from the International Tobacco Control Policy Evaluation Project (ITC) Youth Tobacco and Vaping Survey, in Hammond et al9. The NYTS30 (in the Surgeon’s Report on E-Cigarette Usage), CDC, and FDA data from reports31,32 between 2015 and 2020 were also used. It should be noted that there is a slight discrepancy in reported past 30-day prevalence of use in Canada between a Canadian report in 201733 and the ITC survey report9 (6.6% versus 8.4%) as well as between the FDA USA32 report and the ITC in 20199 (20.8 versus 16.2%).
Health effects and associated risks
Although e-cigarettes appear to be a safer alternative than smoking cigarettes over the short term7, they are not without risks, especially when used on a regular basis34. The potential benefits and risks of e-cigarettes are summarized in Table 3. Previous reviews have linked e-cigarettes with asthma and chronic obstructive pulmonary disease34. A systematic review found that e-cigarettes were associated with myriad respiratory health effects such as exacerbations of asthma, eosinophilic pneumonia, epiglottitis, bronchitis, and acute respiratory distress35. Other notable symptoms in regular teenage vapers have included headaches, generalized coughing, insomnia, weakness, and pain in the chest area36.
Table 3.
| Exposure | Potential benefits | Potential risks |
|---|---|---|
| E-Cigarettes |
• May assist with smoking cessation • Potential harm reduction intervention for cigarette smokers as a form of nicotine replacement (also mimics smoking hand to mouth behaviors) • Safer alternative than smoking cigarettes • Less toxic chemicals and in lower doses than in conventional cigarettes |
• Exposure of e-cigarettes to minors (children and teenagers) and previous nonsmokers • Potential gateway to smoking and initiation of other substances in teenagers • Dual smoking and e-cigarette use compounds public health risks • May increase the risk of respiratory health problems • May increase the risk deficits in cognition, brain development, effort-reward imbalances in the brain in children and teenagers • Long-term effects on health are unknown |
The FDA had issued a warning in 2019, after a series of cases (N = > 1000 of E-cigarette and vaping use associated lung injury (EVALI))37, which were later confirmed to have been caused by the addition of THC and vitamin-E acetate to vape products38–40. The specific effects of e-cigarettes on lung injury in teenagers (seven case series) included tachycardia, shortness of breath, and coughing41. Six out of the seven cases required ventilator support and were hospitalized41.The odds of getting COVID were also five times greater in teenage vapers relative to their nonvaping counterparts (OR = 5.0; 95% CI = 1.8–14.0)42. A total of 25.8% of participants who reported previous vaping had symptoms of COVID when compared with nonvapers (13.5%)42. It should be noted, however, that the long-term effects of e-cigarettes on respiratory health cannot yet be ascertained43.
There is some emerging research, which suggests that e-cigarettes may have cardiovascular effects in teenagers. A study found a rise in arterial blood pressure and heart rate in young adult vapers using JUUL, but not in e-cigarettes without nicotine44. Cardiopulmonary risk is also compounded in dual e-cigarette and cigarette smokers45.
In addition to this, nicotine use has been documented to have adverse effects on cognition and the developing adolescent brain46–48, as well as fetal brain development46. Research in teenagers suggests that it is associated with memory problems and troubles with concentrating and focusing on tasks, with increased impulsive behaviors as adults48,49. A review also found that nicotine use was associated with imbalances in brain development, whereby teens exposed to nicotine had less-developed regions in the prefrontal cortex responsible for inhibitory control, while the part of the brain responsible for the reward system (dopamine pathway)50 had been well matured as indicated on functional MRIs, highlighting the imbalance in reward and control regions in the brain47. Nicotine use during adolescence has also been linked with an increased risk of mental health problems later in life47,48.
Furthermore, e-cigarette use is a risk factor for subsequent cigarette smoking. A systematic review and meta-analysis found that e-cigarette users had a 30% chance of initiating cigarette smoking when compared with never-users (7.9%)51. The odds of smoking were 3.5-times higher (95% CI = 2.4–5.2) in e-cigarette users when compared with never-users (23.2% of previous e-cigarette users reported smoking versus 7.2% of never-users)51. Research in young adults found that 82.6% of e-cigarette consumers concurrently used additional nicotine products such as conventional cigarettes. Prevalence of nicotine dependence in this young population was 68%52. Another study found that nearly half of teenage vapers smoked a cigarette two years later when compared with their nonvaping counterparts53. A qualitative study in teens found that many identified e-cigarettes as a gateway to cigarette smoking54.
E-cigarettes are also associated with downstream substance use. Research has found that teenagers who use e-cigarettes are also more likely to use cannabis when compared with non-e-cigarette users and that it is commonly added to vaping products52,55. Cannabis vaping has been linked with bronchitis in youth as well56.
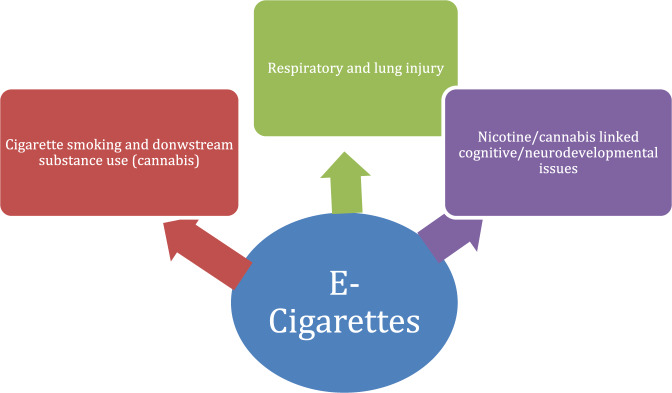
Finally, there have been incidents of ingestion and intoxication associated with e-cigarettes in preteens57. Figure 4 illustrates the health risks associated with vaping.
Fig. 4. The health risks associated with vaping37,46–48,51,52,55.
The following figure illustrates the relationship between e-cigarette exposure and potential health effects in teenagers, which primarily affect the respiratory system, neurodevelopment/cognition, and may increase the risk of dual smoking and addiction to other drugs.
Mechanisms
Nicotine is a well-established respiratory irritant58, but other chemicals in e-cigarettes (e.g., diacetyl59, propylene glycol, carbon monoxide, and formaldehyde60) also have detrimental effects for lung function including respiratory volume61. E-cigarettes also contain trace amounts of toxic chemicals such as polycyclic aromatic compounds in tandem with heavy metals, aldehydes, and nicotine derivatives62. However, it should be noted that exposure to potentially toxic chemicals is lower in e-cigarettes than in conventional cigarettes63. E-cigarettes also irritate mucous membranes and trigger the release of inflammatory markers64. Additionally, the sweet-flavoring additives (e.g., candy or fruity flavored) have also been reported to be hazardous to the lung65. The cinnamon-flavoring cinnamaldehyde has been identified as being one of the main constituents capable of damaging immune cells in the lungs (macrophage-phagocytosis impairment) even without nicotine as a co-additive65. Furthermore, the sweet Crème Brulee flavoring was linked with increased tumor-necrosis factor, interleukin levels, and oxidative stress associated with DNA changes66. In terms of e-cigarette or vaping use-associated lung injury (EVALI), vitamin E acetate along with cannabis oil were identified as being the primary causative agents38,39.
In addition to this, nicotine is a risk factor for cardiovascular disease through its well-known effects on endothelial function and stimulation of inflammatory markers such as C-reactive protein67,68. Studies in youth have identified a possible mechanism for cardiovascular effects resulting from activation of the splenocardiac axis from inhaled toxins in e-cigarettes69.
Nicotine additionally affects the developing brain through its effect on cerebral cortex as well as in the hippocampus49. All types of e-cigarettes, including non-nicotine ones, have been reported to induce oxidative stress, thereby increasing the risk of cognitive-related impairment in teenagers70. Research also suggests that nicotine can bind to N-acetylcholine receptors, thereby impacting signaling in the prefrontal cortex47. Nicotine also has been documented to have an effect on serotonin receptors (5HT1 and 5HT2), which subsequently affects the body’s response to serotonin, supporting the link between exposure to nicotine in adolescence and risk of mood disorders later in life47,48.
Furthermore, e-cigarettes are thought to increase dual smoking and downstream substance use through the gateway hypothesis, whereby exposure to nicotine products further puts individuals at risk of initiating other substances by stimulating neurotransmitters associated with the reward system4,55,71–73. This feedback loop creates a pathway for substance abuse and dependence72.
There is some evidence of second-hand exposure effects, but the exposure dose is much smaller than in conventional cigarettes74. However, a study found that teenagers presenting with an asthma attack over a 12-month period were 27% times more likely to be exposed to e-cigarette second-hand smoke relative to their counterparts75. Thus, second-hand exposure may be related to respiratory health in youth, including asthma and generalized wheezing75,76.
Screening, prevention, and management
Research indicates that screening patients for e-cigarette usage in primary practice is not frequently undertaken by medical practitioners77. One study found a low prevalence of screening for e-cigarettes in primary-care practice relative to smoking screening (14% versus 86%) in a sample of 776 practitioners across the United States77. This low uptake is concerning, given the serious health risks of e-cigarettes. A qualitative study in the United States further confirmed that there is insufficient knowledge of e-cigarettes among physicians, including both the potential benefits and health risks78. A study in US college students found that most students did not receive any form of counseling about risks from medical practitioners, including dental hygienists79. More research is needed to learn about the global screening prevalence of e-cigarette use in primary care. Studies have also shown that there is a need for stronger education on e-cigarettes in medical curricula, which will allow physicians to begin addressing e-cigarette use in teenagers80.
Presently, there is little information on primary-care interventions for e-cigarette use in teenagers and young adults. A case study of a 23-year-old e-cigarette user shows promising results for tapering e-cigarette use with the assistance of a pharmacist81, which suggests that different healthcare practitioners may play a role helping patients with gradually tapering off e-cigarettes. A randomized controlled trial of asthmatic teenagers who attended one of four clinics found that physicians discussed smoking during 38.2% of thee visits, but vaping was never brought up as a topic82. This emphasizes that physicians should discuss both smoking and vaping during appointments82, in particular in youth presenting with asthma75.
Medical curricula should stress that concurrent smoking and vaping screening and management interventions should be undertaken in the primary-care setting. This way, many cases will not be missed given the high prevalence of dual use51. Family physicians should aim to identify youth at risk of vaping through screening questionnaires and aim to increase awareness of vaping for prevention purposes. This could include handing out brochures to patients and their families about the health risks associated with vaping and therapies that are available, which can assist with gradual tapering of nicotine from e-cigarettes. Family physicians have previously recommended open discussions with youth about risks during appointments83, as well as educating families through public health educational campaigns84.
It may also be strategic for medical, public health practitioners, and researchers to target particular groups and populations of teenagers that are most vulnerable to using e-cigarettes. A longitudinal study in the United Kingdom found an association between socioeconomic disadvantage and e-cigarette use in teenagers and young adults85. A systematic review also found that older teenagers from more affluent homes, of white ethnicity, and with higher levels of education had higher levels of knowledge and awareness of e-cigarette use, highlighting a possible need to educate younger teenagers with less education, ethnic minorities, and from lower-income neighborhoods86. It should be noted that one study found conflicting results with regard to the relationship between SES and e-cigarettes, whereby young adults from wealthier families were more likely to use e-cigarette, though the comparison groups were all in the affluent state of Connecticut87.
Education was also found to be inversely associated with e-cigarette use in another study, but it had the greatest association in whites when compared with black young adults88. Vocational training, without higher education, was found to also be associated with e-cigarette use in youth in Europe89. Thus, public health campaigns and medical doctors could potentially target individuals with lower levels of education, lower SES, and racially diverse groups to minimize any potential inequities in health.
Gender differences in e-cigarette use have also been noted in North America as well as Europe, whereby males were more likely to use them89–91. Additionally, since research indicates that females use e-cigarettes for mostly weight and stress management92, interventions could focus on assisting them with stress along with making healthy lifestyle choices associated with weight.
Other particularly vulnerable groups have also included teenagers with impulsivity as well as those with mental health problems93–95. A study that explored EVALI cases found that mental health problems were prevalent in this population95. Thus, physicians and public health researchers may also consider screening and targeting individuals with mental health problems.
To date, there have been limited community-based and public health intervention trials to assist with e-cigarette prevention. “Catch my breath” was a prevention intervention in 12 middle schools across the United States. The intervention focused on increasing knowledge on the harms associated with e-cigarette use96. The study authors found statistically significant differences in e-cigarette use prevalence in schools that had implemented the program when compared with control schools. They also found increased knowledge of e-cigarettes and the risks associated with their use96.
Similarly, public health interventions targeting existing teenage users are in their infancy. There is a current text messaging intervention for e-cigarette cessation in teens in the United States97. The intervention provides users with educational content on e-cigarettes, focuses on fostering self-efficacy, assists with resilience building, and provides users with support and encouragement. The study had a very high enrollment after about one month of recruitment, with over 27,000 teenagers and young adults enrolled97. This indicates that this form of intervention is feasible, given the willingness for e-cigarette users to enroll97. Previous studies have found that text messaging for smoking cessation is effective and acceptable for this population98–101, indicating that it could be used for vaping.
Additionally, there are very few commercially available e-cigarette cessation apps that can help teenagers and young adults quit. A systematic review of apps in the Google Play Store found that most apps encouraged e-cigarette use and that only 2 out of 79 were vaping cessation apps102. There is a need to develop an app that can be readily available and accessible to teenagers wanting to quit as well as an educational prevention app.
Policies
Strict policies to limit e-cigarette accessibility and exposure play an important role in preventing use. Research indicates that children and teenagers are exposed to e-cigarette marketing103. A study in the United Kingdom found that most e-cigarette advertisements were near children’s stores and in areas that were less affluent103, indicating that social health inequalities may exist, but more research is needed in this area. A review of 124 e-cigarette marketing publications revealed that companies have increased expenditures on social media campaigns and that they are often marketed as an alternative to cigarette smoking104. This is especially concerning given how social media may influence the decisions of teenagers and young adults. A randomized controlled trial found that by exposing youth without prior smoking history (N = 417) to e-cigarette advertising (four advertisements), they were more likely to select e-cigarettes and have positive attitudes toward them relative to controls not exposed to this advertising13. Research had found that many e-cigarette advertisements on social media had used cartoons on packages to promote vaping in youth along with hashtags for vaping (#ejuice and #eliquid)105. The study authors also found that over 20% of advertisements had used a cartoon (66% of which were promotional posts), indicating that youth are often the targets of these ads across the globally accessible Instagram platform. They recommend similar policies to the ones for smoking including the Historical Master Settlement Agreement that banned advertising to youth105. Studies have also found that teenagers require multiple warnings in the forms of messages and ads to reduce their positive interest and susceptibility to e-cigarettes106 and that perceptions of safety are related to environmental policy restrictions on vaping107.
Research also indicates that patterns of e-cigarette use changed markedly in teenagers and young adults during the COVID-19 pandemic108. Changes in substance use behavioral patterns included ordering from alternative sellers, buying vaping products online, quitting vaping, and switching to cannabis or other products, resulting from the inherent challenges with making purchases at local vendors108. This emphasizes how the availability of vaping products including their placement and immediate accessibility influences e-cigarette behavioral patterns, including quitting108.
Besides restricting marketing and advertisements, limiting the availability of e-cigarettes and accessibility to teenagers is greatly needed. A policy review on bans on the sale of e-cigarettes to minors across the United States found that e-cigarette use decreased along with smoking traditional cigarettes109. A qualitative study of adult vapers found that many agree with bans on advertising to minors to protect them110.
A review of global vaping policies found that 68 countries regulate e-cigarettes and that the most frequent cross-national governmental policies include age limits (over 18 years of age), restricting advertisements, and placing bans on vaping in public places, while e-cigarette taxes are not commonly used111. The review found that Australia, the Czech Republic, and Malaysia classified e-cigarettes as toxic and poisonous substances111. Countries that have enacted child safety policies to protect children include Canada (banned flavoring and marketing to children)112, Australia (available by prescription only with a child safety seal)113, New Zealand (banned vaping near schools)114, the United Kingdom111, the United States (some states have banned JUUL)115, Finland, Germany, Ireland, Italy, Lithuania, Malta, Netherlands, and the Philippines111. Some countries with vape-free restrictions that were also identified include France, Germany, Greece, Jamaica, Nepal, Portugal, Slovakia, Spain, Turkey, Venezuela, and Vietnam111. Countries with taxes on e-cigarettes include Italy, Latvia, Portugal, Republic of Korea, Togo, and the United Kingdom111. Asian countries that have banned e-cigarettes include Singapore and Thailand, and Japan has banned the use of nicotine-containing e-cigarettes but not e-cigarettes without nicotine116. Vaping products are also prohibited in the United Arab Emirates116. Switzerland had banned the sale of vaping products until 2018, but now they are available on the market117.
In developing countries, where resources are depleted and there is less regulatory oversight118, concerns are raised about efforts to protect minors. Although data in India are limited, protective measures have nonetheless have been put into place in 2019, when e-cigarettes were banned to protect minors119. Concern has been raised in Guatemala over the lack of regulatory control over flavored e-cigarettes that are enticing for teenagers120. While little is known about Africa, South Africa is planning on placing restrictions on e-cigarettes in 2021121, but there has been strong opposition from the Tobacco Industry122.
Discussion
Recommendations
Without stricter interventions and policies, teenagers and young adult vapers will continue to be at risk of multiple health problems associated with e-cigarettes.
The following are a set of recommendations:
Strengthen global policies to restrict marketing, use of enticing flavoring, accessibility, and exposure to e-cigarettes in the environment
Increase physician education on screening and nicotine tapering in the primary-care setting.
Increase public health education campaigns and develop evidence-based interventions.
Develop collaborations between physicians and public health researchers through joint efforts in education, screening, and referral.
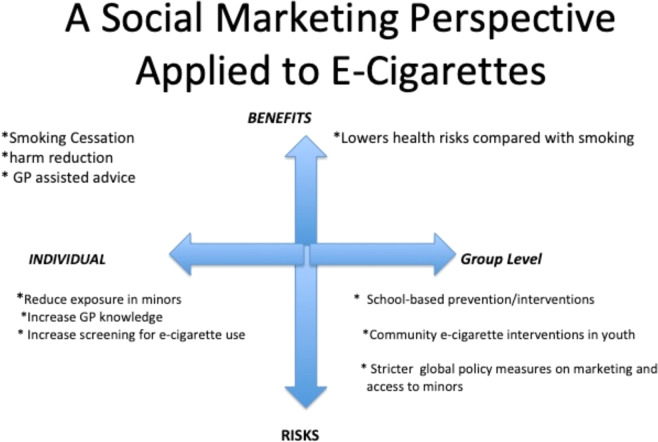
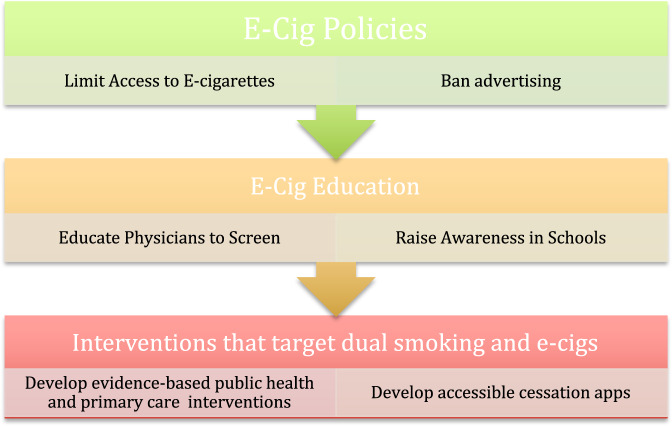
Figure 5 illustrates strategies that may be applied from a social-marketing perspective123 to e-cigarettes by emphasizing that the health risks41,46,51 should be reduced by restricting their access to children and teenagers9, while the benefits of their use may be maximized when safely used in adult smokers attempting to quit7. It illustrates that screening, prevention, and intervention can take place in primary-care settings and through public health interventions. Figure 6 illustrates a three-tiered approach to screening, education, prevention, and interventions for e-cigarettes in youth.
Fig. 5. Strategies to reduce the harm and maximize the benefits associated with e-cigarettes at the individual and group levels82,96,97,123.
The North Axis represents the benefits of e-cigarettes for smokers and the South axis represents the risks, while the East and West axes represent the strategies that may be adopted at an individual level and community/population level. By maximizing the benefits in select adult smokers through harm reduction and minimizing the risks of exposure in minors, e-cigarettes may be safely used.
Fig. 6. A three-tiered approach to managing e-cigarette use in minors126.
The following figure illustrates a three-tiered approach to managing e-cigarette use in minors, which includes policy changes, awareness, and prevention campaigns, and finally public health interventions that target existing teenage users.
Conclusion
In summary, e-cigarettes pose a health threat to teenagers and young adults, given the rise in the prevalence of use. While e-cigarettes are a safer alternative than smoking cigarettes and may be used as a harm-reduction strategy in existing smokers, measures need to be urgently put into place to protect children and teenagers from unnecessary use and potential dual smoking and e-cigarette uptake. The outlook depends on whether sufficient primary care and public health strategies will be implemented to protect minors and young adults. As the long-term effects are unknown62, it is especially prudent to limit unnecessary exposure. There is an urgent need to develop evidence-based primary-care intervention and public health interventions that target vulnerable groups. Furthermore, there is need for stronger public health protection policies and bans to protect youth.
Supplementary information
Acknowledgements
The corresponding author LNL would like to thank her friend medical librarian, Lars Eriksson at the University of Queensland for his advice with the searches. LNL would also like to thank Distinguished Professor Robert Hogg at SFU for his mentorship during COVID-19.
Author contributions
The corresponding author, Dr. Lynnette Lyzwinski (LNL) led the paper, including its conceptualization, methodology, writing, paper drafting, review and editing. Dr John Naslund (JN) offered thorough review and editing of the paper. He contributed to the policy and epidemiology sections. Dr Chris J Miller (CJM) provided thorough review and editing of the paper. He also contributed to the management section. Dr Mark Eisenberg (ME) inspired LNL to write about e-cigarettes as a topic of interest and supported her ideas throughout. He also offered general review and editing suggestions.
Data availability
No datasets were generated nor analyzed from this study. Source data for Figs. 2–3 are detailed in the paper (i.e., data on vaping prevalence are available on the CDC and FDA websites).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41533-022-00277-9.
References
- 1.Besaratinia A, Tommasi S. Vaping: a growing global health concern. EClinicalMedicine. 2019;17:100208. doi: 10.1016/j.eclinm.2019.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korfei M. The underestimated danger of E-cigarettes - also in the absence of nicotine. Respir. Res. 2018;19:159. doi: 10.1186/s12931-018-0870-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Long GA. Comparison of select analytes in exhaled aerosol from e-cigarettes with exhaled smoke from a conventional cigarette and exhaled breaths. Int. J. Environ. Res. Public Health. 2014;11:11177–11191. doi: 10.3390/ijerph111111177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hammond D, Wackowski OA, Reid JL, O’Connor RJ. Use of JUUL e-cigarettes among youth in the United States. Nicotine Tob. Res. 2020;22:827–832. doi: 10.1093/ntr/nty237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahman MA, Hann N, Wilson A, Mnatzaganian G, Worrall-Carter L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS ONE. 2015;10:e0122544. doi: 10.1371/journal.pone.0122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang RJ, Bhadriraju S, Glantz SA. E-cigarette use and adult cigarette smoking cessation: a meta-analysis. Am. J. public health. 2021;111:230–246. doi: 10.2105/AJPH.2020.305999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farsalinos KE, Polosa R. Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review. Ther. Adv. Drug Saf. 2014;5:67–86. doi: 10.1177/2042098614524430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrington-Trimis, J. L. et al. E-cigarettes, cigarettes, and the prevalence of adolescent tobacco use. Pediatrics, 10.1542/peds.2015-3983 (2016). [DOI] [PMC free article] [PubMed]
- 9.Hammond D, et al. Prevalence of vaping and smoking among adolescents in Canada, England, and the United States: repeat national cross sectional surveys. BMJ. 2019;365:l2219. doi: 10.1136/bmj.l2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob. Res. 2015;17:847–854. doi: 10.1093/ntr/ntu257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morean ME, et al. Preferring more e-cigarette flavors is associated with e-cigarette use frequency among adolescents but not adults. PLoS ONE. 2018;13:e0189015. doi: 10.1371/journal.pone.0189015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fadus MC, Smith TT, Squeglia LM. The rise of e-cigarettes, pod mod devices, and JUUL among youth: Factors influencing use, health implications, and downstream effects. Drug Alcohol Depend. 2019;201:85–93. doi: 10.1016/j.drugalcdep.2019.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Padon AA, Lochbuehler K, Maloney EK, Cappella JN. A randomized trial of the effect of youth appealing e-cigarette advertising on susceptibility to use e-cigarettes among youth. Nicotine Tob. Res. 2018;20:954–961. doi: 10.1093/ntr/ntx155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soneji SS, Knutzen KE, Villanti AC. Use of flavored e-cigarettes among adolescents, young adults, and older adults: findings from the population assessment for tobacco and health study. Public Health Rep. 2019;134:282–292. doi: 10.1177/0033354919830967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perikleous EP, Steiropoulos P, Paraskakis E, Constantinidis TC, Nena E. E-cigarette use among adolescents: an overview of the literature and future perspectives. Front. Public Health. 2018;6:86. doi: 10.3389/fpubh.2018.00086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Government of Canada. Summary of results for the Canadian Student Tobacco, Alcohol and Drugs Survey 2018–19. https://www.canada.ca/en/health-canada/services/canadian-student-tobacco-alcohol-drugs-survey/2018-2019-summary.html (2018).
- 18.Brożek, G. M. et al. The prevalence of cigarette and e-cigarette smoking among students in Central and Eastern Europe-results of the YUPESS study. Int. J. Environ. Res. Public Health, 10.3390/ijerph16132297 (2019). [DOI] [PMC free article] [PubMed]
- 19.Kuwabara Y, et al. Heat-not-burn tobacco, electronic cigarettes, and combustible cigarette use among Japanese adolescents: a nationwide population survey 2017. BMC Public Health. 2020;20:741. doi: 10.1186/s12889-020-08916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee, J. A., Lee, S. & Cho, H. J. The relation between frequency of e-cigarette use and frequency and intensity of cigarette smoking among South Korean adolescents. Int. J. Environ. Res. Public Health14, 10.3390/ijerph14030305 (2017). [DOI] [PMC free article] [PubMed]
- 21.Xiao L, Parascandola M, Wang C, Jiang Y. Perception and current use of e-cigarettes among youth in China. Nicotine Tob. Res. 2019;21:1401–1407. doi: 10.1093/ntr/nty145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oliveira WJC, et al. Electronic cigarette awareness and use among students at the Federal University of Mato Grosso, Brazil. J. Bras. Pneumol. 2018;44:367–369. doi: 10.1590/S1806-37562017000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morello, P. et al. Prevalence and predictors of e-cigarette trial among adolescents in Argentina. Tob. Prev. Cessat., 10.18332/tpc/66950 (2016). [DOI] [PMC free article] [PubMed]
- 24.Bhave SY, Chadi N. E-cigarettes and vaping: a global risk for adolescents. Indian Pediatrics. 2021;58:315–319. [PubMed] [Google Scholar]
- 25.Action on Smoking and Health. Use of e-cigarettes among young people in Great Britain. https://ash.org.uk/wp-content/uploads/2021/02/YouthEcig2020pdf (2021).
- 26.Statistics Canada. Canadian Tobacco and Nicotine Survey 2018–2019. https://www150.statcan.gc.ca/n1/daily-quotidien/210317/dq210317b-eng.htm (2019).
- 27.Statistics Canada. Canadian Tobacco and Nicotine Survey 2018–2019. https://www150.statcan.gc.ca/n1/daily-quotidien/210317/dq210317b-eng.htm (2020).
- 28.Kinnunen JM, et al. Electronic cigarette use among 14- to 17-year-olds in Europe. Eur. J. Public Health. 2021;31:402–408. doi: 10.1093/eurpub/ckaa145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Canadian Tobacco and Nicoitne Survey. Canadian Tobacco and Nicotine Survey, 2019. https://www150.statcan.gc.ca/n1/daily-quotidien/200305/dq200305a-eng.htm (2019).
- 30.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. E-cigarette use among youth and young adults: a report of the surgeon general [Internet]. Atlanta (GA). Centers for Disease Control and Prevention (US); 2016. https://www.ncbi.nlm.nih.gov/books/NBK538680/ (2016). [PubMed]
- 31.CDC. E-cigarette Use Among Middle and High School Students — United States, 2020. https://www.cdc.gov/mmwr/volumes/69/wr/mm6937e1.htm (2020). [DOI] [PMC free article] [PubMed]
- 32.FDA. 2018 NYTS Data: A Startling Rise in Youth E-cigarette Use. https://www.fda.gov/tobacco-products/youth-and-tobacco/2018-nyts-data-startling-rise-youth-e-cigarette-use (2018).
- 33.Waterloo, U. O. Tobacco Use in Canada. https://uwaterloo.ca/tobacco-use-canada/e-cigarette-use-canada/prevalence-e-cigarette-use/e-cigarette-prevalence-age (2021).
- 34.Kaur, G., Pinkston, R., McLemore, B., Dorsey, W. C. & Batra, S. Immunological and toxicological risk assessment of e-cigarettes. Eur. Respir. Rev., 10.1183/16000617.0119-2017 (2018). [DOI] [PMC free article] [PubMed]
- 35.Tzortzi, A., Kapetanstrataki, M., Evangelopoulou, V. & Beghrakis, P. A systematic literature review of e-cigarette-related illness and injury: not just for the respirologist. Int. J. Environ. Res. Public Health, 10.3390/ijerph17072248 (2020). [DOI] [PMC free article] [PubMed]
- 36.Benyo SE, et al. Risk factors and medical symptoms associated with electronic vapor product use among adolescents and young adults. Clin. Pediatr. 2021;60:279–289. doi: 10.1177/00099228211009681. [DOI] [PubMed] [Google Scholar]
- 37.Sun, T. W. P. L. H. Vaping lung injuries top 1000 cases as deaths rise to 18. Hundreds more people in the U.S. have been sickened by a mysterious vaping-related lung disease, and the death toll has risen to 18, according to federal health data released Thursday. (2019).
- 38.Blount BC, et al. Vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N. Engl. J. Med. 2020;382:697–705. doi: 10.1056/NEJMoa1916433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abeles M, et al. Vaping-associated lung injury caused by inhalation of cannabis oil. Pediatr. Pulmonol. 2020;55:226–228. doi: 10.1002/ppul.24579. [DOI] [PubMed] [Google Scholar]
- 40.Boudi FB, Patel S, Boudi A, Chan C. Vitamin E acetate as a plausible cause of acute vaping-related Illness. Cureus. 2019;11:e6350. doi: 10.7759/cureus.6350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khan A, Parlette K, Kuntz HM. E-cigarettes and vaping, product-use associated lung injury: a case series of adolescents. Clin. Pract. Cases Emerg. Med. 2021;5:11–16. doi: 10.5811/cpcem.2020.10.48707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gaiha SM, Cheng J, Halpern-Felsher B. Association between youth smoking, electronic cigarette use, and COVID-19. J. Adolesc. Health. 2020;67:519–523. doi: 10.1016/j.jadohealth.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gotts JE, Jordt SE, McConnell R, Tarran R. What are the respiratory effects of e-cigarettes? BMJ. 2019;366:l5275. doi: 10.1136/bmj.l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gonzalez JE, Cooke WH. Acute effects of electronic cigarettes on arterial pressure and peripheral sympathetic activity in young nonsmokers. Am. J. Physiol. Heart Circ. Physiol. 2021;320:H248–h255. doi: 10.1152/ajpheart.00448.2020. [DOI] [PubMed] [Google Scholar]
- 45.Wang JB, et al. Cigarette and e-cigarette dual use and risk of cardiopulmonary symptoms in the Health eHeart Study. PLoS ONE. 2018;13:e0198681. doi: 10.1371/journal.pone.0198681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.England LJ, Bunnell RE, Pechacek TF, Tong VT, McAfee TA. Nicotine and the developing human: a neglected element in the electronic cigarette debate. Am. J. Prev. Med. 2015;49:286–293. doi: 10.1016/j.amepre.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goriounova NA, Mansvelder HD. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2012;2:a012120. doi: 10.1101/cshperspect.a012120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J. Physiol. 2015;593:3397–3412. doi: 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.England LJ, et al. Developmental toxicity of nicotine: a transdisciplinary synthesis and implications for emerging tobacco products. Neurosci. Biobehav. Rev. 2017;72:176–189. doi: 10.1016/j.neubiorev.2016.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim SI. Neuroscientific model of motivational process. Front. Psychol. 2013;4:98. doi: 10.3389/fpsyg.2013.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Soneji S, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatrics. 2017;171:788–797. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dugas EN, Sylvestre MP, O’Loughlin J. Type of e-liquid vaped, poly-nicotine use and nicotine dependence symptoms in young adult e-cigarette users: a descriptive study. BMC Public Health. 2020;20:922. doi: 10.1186/s12889-020-09056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Aleyan S, Cole A, Qian W, Leatherdale ST. Risky business: a longitudinal study examining cigarette smoking initiation among susceptible and non-susceptible e-cigarette users in Canada. BMJ Open. 2018;8:e021080. doi: 10.1136/bmjopen-2017-021080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Akre C, Suris JC. Adolescents and young adults’ perceptions of electronic cigarettes as a gateway to smoking: a qualitative study in Switzerland. Health Educ. Res. 2017;32:448–454. doi: 10.1093/her/cyx054. [DOI] [PubMed] [Google Scholar]
- 55.Dai, H., Catley, D., Richter, K. P., Goggin, K. & Ellerbeck, E. F. Electronic cigarettes and future marijuana use: a longitudinal study. Pediatrics, 10.1542/peds.2017-3787 (2018). [DOI] [PubMed]
- 56.Braymiller JL, et al. Assessment of nicotine and cannabis vaping and respiratory symptoms in young adults. JAMA Netw. Open. 2020;3:e2030189. doi: 10.1001/jamanetworkopen.2020.30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Noble MJ, Longstreet B, Hendrickson RG, Gerona R. Unintentional pediatric ingestion of electronic cigarette nicotine refill liquid necessitating intubation. Ann. Emerg. Med. 2017;69:94–97. doi: 10.1016/j.annemergmed.2016.08.448. [DOI] [PubMed] [Google Scholar]
- 58.Lee LY, et al. Airway irritation and cough evoked by inhaled cigarette smoke: role of neuronal nicotinic acetylcholine receptors. Pulm. Pharmacol. Ther. 2007;20:355–364. doi: 10.1016/j.pupt.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 59.Vas CA, Porter A, McAdam K. Acetoin is a precursor to diacetyl in e-cigarette liquids. Food Chem. Toxicol. 2019;133:110727. doi: 10.1016/j.fct.2019.110727. [DOI] [PubMed] [Google Scholar]
- 60.Son, Y., Bhattarai, C., Samburova, V. & Khlystov, A. Carbonyls and carbon monoxide emissions from electronic cigarettes affected by device type and use patterns. Int. J. Environ. Res. Public Health, 10.3390/ijerph17082767 (2020). [DOI] [PMC free article] [PubMed]
- 61.Meo SA, et al. Electronic cigarettes: impact on lung function and fractional exhaled nitric oxide among healthy adults. Am. J. Mens Health. 2019;13:1557988318806073. doi: 10.1177/1557988318806073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bracken-Clarke D, et al. Vaping and lung cancer - a review of current data and recommendations. Lung Cancer. 2021;153:11–20. doi: 10.1016/j.lungcan.2020.12.030. [DOI] [PubMed] [Google Scholar]
- 63.Drummond MB, Upson D. Electronic cigarettes. Potential harms and benefits. Ann. Am. Thorac. Soc. 2014;11:236–242. doi: 10.1513/AnnalsATS.201311-391FR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Meo SA, Al Asiri SA. Effects of electronic cigarette smoking on human health. Eur. Rev. Med. Pharmacol. Sci. 2014;18:3315–3319. [PubMed] [Google Scholar]
- 65.Clapp PW, et al. Flavored e-cigarette liquids and cinnamaldehyde impair respiratory innate immune cell function. Am. J. Physiol. Lung Cell. Mol. Physiol. 2017;313:L278–l292. doi: 10.1152/ajplung.00452.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Muthumalage T, Lamb T, Friedman MR, Rahman I. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci. Rep. 2019;9:19035. doi: 10.1038/s41598-019-51643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.O’Loughlin J, et al. Association between cigarette smoking and C-reactive protein in a representative, population-based sample of adolescents. Nicotine Tob. Res. 2008;10:525–532. doi: 10.1080/14622200801901997. [DOI] [PubMed] [Google Scholar]
- 68.Golbidi S, Edvinsson L, Laher I. Smoking and endothelial dysfunction. Curr. Vasc. Pharmacol. 2020;18:1–11. doi: 10.2174/1573403X14666180913120015. [DOI] [PubMed] [Google Scholar]
- 69.Boas, Z. et al. Activation of the “Splenocardiac Axis” by electronic and tobacco cigarettes in otherwise healthy young adults. Physiol. Rep., 10.14814/phy2.13393 (2017). [DOI] [PMC free article] [PubMed]
- 70.Tobore TO. On the potential harmful effects of E-Cigarettes (EC) on the developing brain: the relationship between vaping-induced oxidative stress and adolescent/young adults social maladjustment. J. Adolesc. 2019;76:202–209. doi: 10.1016/j.adolescence.2019.09.004. [DOI] [PubMed] [Google Scholar]
- 71.Dai H, Hao J. Electronic cigarette and marijuana use among youth in the United States. Addict. Behav. 2017;66:48–54. doi: 10.1016/j.addbeh.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 72.Ren M, Lotfipour S. Nicotine gateway effects on adolescent substance use. West. J. Emerg. Med. 2019;20:696–709. doi: 10.5811/westjem.2019.7.41661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wong DN, Fan W. Ethnic and sex differences in E-cigarette use and relation to alcohol use in California adolescents: the California Health Interview Survey. Public Health. 2018;157:147–152. doi: 10.1016/j.puhe.2018.01.019. [DOI] [PubMed] [Google Scholar]
- 74.National Academies of Sciences. Public Health Consequences of E-Cigarettes (National Academies Press, 2018). [PubMed]
- 75.Bayly JE, Bernat D, Porter L, Choi K. Secondhand exposure to aerosols from electronic nicotine delivery systems and asthma exacerbations among youth with asthma. Chest. 2019;155:88–93. doi: 10.1016/j.chest.2018.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Alnajem A, et al. Use of electronic cigarettes and secondhand exposure to their aerosols are associated with asthma symptoms among adolescents: a cross-sectional study. Respir. Res. 2020;21:300. doi: 10.1186/s12931-020-01569-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pepper JK, Gilkey MB, Brewer NT. Physicians’ counseling of adolescents regarding e-cigarette use. J. Adolesc. Health. 2015;57:580–586. doi: 10.1016/j.jadohealth.2015.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.El-Shahawy, O., Brown, R. & Elston Lafata, J. Primary care physicians’ beliefs and practices regarding e-cigarette use by patients who smoke: a qualitative assessment. Int. J. Environ. Res. Public Health, 10.3390/ijerph13050445 (2016). [DOI] [PMC free article] [PubMed]
- 79.Abadi S, Couch ET, Chaffee BW, Walsh MM. Perceptions related to use of electronic cigarettes among california college students. J. Dent. Hyg. 2017;91:35–43. [PubMed] [Google Scholar]
- 80.Geletko KW, et al. Medical residents’ and practicing physicians’ e-cigarette knowledge and patient screening activities: do they differ? Health Serv. Res. Manag. Epidemiol. 2016;3:2333392816678493. doi: 10.1177/2333392816678493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sahr M, Kelsh SE, Blower N. Pharmacist assisted vape taper and behavioral support for cessation of electronic nicotine delivery system use. Clin. Case Rep. 2020;8:100–103. doi: 10.1002/ccr3.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Beznos B, et al. Communication about adolescent and caregiver smoking and vaping during pediatric asthma visits: implications for providers. J. Pediatr. Health Care. 2021;35:401–407. doi: 10.1016/j.pedhc.2021.02.004. [DOI] [PubMed] [Google Scholar]
- 83.Arane K, Goldman RD. Electronic cigarettes and adolescents. Can. Fam. Physician. 2016;62:897–898. [PMC free article] [PubMed] [Google Scholar]
- 84.Alexander JP, Williams P, Lee YO. Youth who use e-cigarettes regularly: a qualitative study of behavior, attitudes, and familial norms. Prev. Med Rep. 2019;13:93–97. doi: 10.1016/j.pmedr.2018.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Green MJ, Gray L, Sweeting H, Benzeval M. Socioeconomic patterning of vaping by smoking status among UK adults and youth. BMC Public Health. 2020;20:183. doi: 10.1186/s12889-020-8270-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hartwell G, Thomas S, Egan M, Gilmore A, Petticrew M. E-cigarettes and equity: a systematic review of differences in awareness and use between sociodemographic groups. Tob. Control. 2017;26:e85–e91. doi: 10.1136/tobaccocontrol-2016-053222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Simon P, et al. Socioeconomic status and adolescent e-cigarette use: the mediating role of e-cigarette advertisement exposure. Prev. Med. 2018;112:193–198. doi: 10.1016/j.ypmed.2018.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Assari, S., Mistry, R. & Bazargan, M. Race, Educational Attainment, and E-Cigarette Use. J. Med. Res. Innov., 10.32892/jmri.185 (2020). [DOI] [PMC free article] [PubMed]
- 89.Surís JC, Berchtold A, Akre C. Reasons to use e-cigarettes and associations with other substances among adolescents in Switzerland. Drug Alcohol Depend. 2015;153:140–144. doi: 10.1016/j.drugalcdep.2015.05.034. [DOI] [PubMed] [Google Scholar]
- 90.Cooper M, Case KR, Loukas A, Creamer MR, Perry CL. E-cigarette dual users, exclusive users and perceptions of tobacco products. Am. J. Health Behav. 2016;40:108–116. doi: 10.5993/AJHB.40.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hanewinkel R, Isensee B. Risk factors for e-cigarette, conventional cigarette, and dual use in German adolescents: a cohort study. Prev. Med. 2015;74:59–62. doi: 10.1016/j.ypmed.2015.03.006. [DOI] [PubMed] [Google Scholar]
- 92.Piñeiro B, et al. Gender differences in use and expectancies of e-cigarettes: online survey results. Addict. Behav. 2016;52:91–97. doi: 10.1016/j.addbeh.2015.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bold KW, et al. Early age of e-cigarette use onset mediates the association between impulsivity and e-cigarette use frequency in youth. Drug Alcohol Depend. 2017;181:146–151. doi: 10.1016/j.drugalcdep.2017.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Alanazi, A. M. M. et al. Mental Health and the Association between Asthma and E-cigarette Use among Young Adults in The United States: A Mediation Analysis. Int. J. Environ. Res. Public Health, 10.3390/ijerph17238799 (2020). [DOI] [PMC free article] [PubMed]
- 95.Adkins SH, et al. Demographics, substance use behaviors, and clinical characteristics of adolescents with e-cigarette, or vaping, product use-associated lung injury (EVALI) in the United States in 2019. JAMA Pediatrics. 2020;174:e200756. doi: 10.1001/jamapediatrics.2020.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kelder SH, et al. A middle school program to prevent e-cigarette use: a pilot study of “CATCH My Breath”. Public Health Rep. 2020;135:220–229. doi: 10.1177/0033354919900887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Graham AL, Jacobs MA, Amato MS. Engagement and 3-month outcomes from a digital e-cigarette cessation program in a cohort of 27000 teens and young adults. Nicotine Tob. Res. 2020;22:859–860. doi: 10.1093/ntr/ntz097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Haug S, Schaub MP, Venzin V, Meyer C, John U. Efficacy of a text message-based smoking cessation intervention for young people: a cluster randomized controlled trial. J. Med. Internet Res. 2013;15:e171. doi: 10.2196/jmir.2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.McClure E, Baker N, Carpenter MJ, Treiber FA, Gray K. Attitudes and interest in technology-based treatment and the remote monitoring of smoking among adolescents and emerging adults. J. Smok. Cessat. 2017;12:88–98. doi: 10.1017/jsc.2015.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Müssener U, Bendtsen M, McCambridge J, Bendtsen P. User satisfaction with the structure and content of the NEXit intervention, a text messaging-based smoking cessation programme. BMC Public Health. 2016;16:1179. doi: 10.1186/s12889-016-3848-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Müssener U, et al. Effectiveness of short message service text-based smoking cessation intervention among university students: a randomized clinical trial. JAMA Intern. Med. 2016;176:321–328. doi: 10.1001/jamainternmed.2015.8260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Meacham MC, Vogel EA, Thrul J. Vaping-related mobile apps available in the google play store after the apple ban: content review. J. Med. Internet Res. 2020;22:e20009. doi: 10.2196/20009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Eadie D, et al. E-cigarette marketing in UK stores: an observational audit and retailers’ views. BMJ Open. 2015;5:e008547. doi: 10.1136/bmjopen-2015-008547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Collins L, Glasser AM, Abudayyeh H, Pearson JL, Villanti AC. E-cigarette marketing and communication: how e-cigarette companies market e-cigarettes and the public engages with e-cigarette information. Nicotine Tob. Res. 2019;21:14–24. doi: 10.1093/ntr/ntx284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Allem JP, et al. Return of cartoon to market e-cigarette-related products. Tob. Control. 2019;28:555–557. doi: 10.1136/tobaccocontrol-2018-054437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Andrews JC, Mays D, Netemeyer RG, Burton S, Kees J. Effects of E-Cigarette Health Warnings and Modified Risk Ad Claims on Adolescent E-Cigarette Craving and Susceptibility. Nicotine Tob. Res. 2019;21:792–798. doi: 10.1093/ntr/nty076. [DOI] [PubMed] [Google Scholar]
- 107.Agaku IT, Perks SN, Odani S, Glover-Kudon R. Associations between public e-cigarette use and tobacco-related social norms among youth. Tob. Control. 2020;29:332–340. doi: 10.1136/tobaccocontrol-2018-054728. [DOI] [PubMed] [Google Scholar]
- 108.Gaiha SM, Lempert LK, Halpern-Felsher B. Underage youth and young adult e-cigarette use and access before and during the coronavirus disease 2019 pandemic. JAMA Netw. Open. 2020;3:e2027572. doi: 10.1001/jamanetworkopen.2020.27572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Abouk R, Adams S. Bans on electronic cigarette sales to minors and smoking among high school students. J. Health Econ. 2017;54:17–24. doi: 10.1016/j.jhealeco.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 110.Farrimond H. E-cigarette regulation and policy: UK vapers’ perspectives. Addiction. 2016;111:1077–1083. doi: 10.1111/add.13322. [DOI] [PubMed] [Google Scholar]
- 111.Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob. Control. 2017;26:440–445. doi: 10.1136/tobaccocontrol-2016-053179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Government of Canada. Vaping Products – New limits on nicotine concentration and consultation on flavour restrictions. https://www.canada.ca/en/health-canada/news/2021/06/backgrounder-vaping-products-new-limits-on-nicotine-concentration-and-consultation-on-flavour-restrictions.html (2021).
- 113.Advisory, T. G. Nicotine e-cigarettes laws are changing. https://www.tga.gov.au/blogs/tga-topics/nicotine-e-cigarettes-laws-are-changing (2021).
- 114.Ministry of Health New Zealand. Regulation of vaping and smokeless tobacco products. https://www.health.govt.nz/our-work/regulation-health-and-disability-system/regulation-vaping-and-smokeless-tobacco-products (2021).
- 115.Ducharme, J. As the number of vaping-related deaths climbs, these states have implemented e-cigarette bans. Timehttps://time.com/5685936/state-vaping-bans/ (2019).
- 116.Doan TTT, et al. Evaluating smoking control policies in the e-cigarette era: a modelling study. Tob. Control. 2020;29:522–530. doi: 10.1136/tobaccocontrol-2019-054951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Swiss Info. Swiss court overturns ban on vaping products. https://www.swissinfo.ch/eng/immediate-effect_court-overturns-swiss-ban-on-e-cigarettes/44082174 (2018).
- 118.Otañez MG, Mamudu HM, Glantz SA. Tobacco companies’ use of developing countries’ economic reliance on tobacco to lobby against global tobacco control: the case of Malawi. Am. J. Public Health. 2009;99:1759–1771. doi: 10.2105/AJPH.2008.146217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Chakma JK, Kumar H, Bhargava S, Khanna T. The e-cigarettes ban in India: an important public health decision. Lancet Public Health. 2020;5:e426. doi: 10.1016/S2468-2667(20)30063-3. [DOI] [PubMed] [Google Scholar]
- 120.Monzón J, Islam F, Mus S, Thrasher JF, Barnoya J. Effects of tobacco product type and characteristics on appeal and perceived harm: results from a discrete choice experiment among Guatemalan adolescents. Prev. Med. 2021;148:106590. doi: 10.1016/j.ypmed.2021.106590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.BusinessTech. Push for new e-cigarette and smoking laws in South Africa. BusinessTech.https://businesstech.co.za/news/lifestyle/472460/push-for-new-e-cigarette-and-smoking-laws-in-south-africa/ (2021).
- 122.BusinessTech. Tobacco industry pushes back against new smoking and vaping laws for South Africa. BusinessTech.https://businesstech.co.za/news/lifestyle/491565/tobacco-industry-pushes-back-against-new-smoking-and-vaping-laws-for-south-africa/ (2021).
- 123.Centre, T. N. S. M. Social Marketing Benchmark Criteria. NSMChttps://www.thensmc.com/sites/default/files/benchmark-criteria-090910.pdf (2009).
- 124.Johns Hopkins Medicine. Vape Flavours and Vape juice: What you need to know. Hopkins Medicine. Rhttps://www.hopkinsmedicine.org/health/wellness-and-prevention/vape-flavors-and-vape-juice-what-you-need-to-know/ (2021).
- 125.CDC. E-cigarettes, Or Vaping Products Visual Dictionary. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/pdfs/ecigarette-or-vaping-products-visual-dictionary-508.pdf /(2021).
- 126.Lyzwinski, L., Eisenber, M. In Handbook of Substance Misuse and Addictions: From Biology to Public Health (eds. Patel, V. B. & Preedy, V. R.) (Nature Springer, 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated nor analyzed from this study. Source data for Figs. 2–3 are detailed in the paper (i.e., data on vaping prevalence are available on the CDC and FDA websites).