Abstract
Objective
Social distancing is one of the main non-pharmaceutical interventions used in the control of the COVID-19 pandemic. This scoping review aims to synthesise research findings on the effectiveness of different types and levels of social distancing measures in the earlier stage of COVID-19 pandemic without the confounding effect of mass vaccination.
Design
Scoping review.
Data sources
MEDLINE, Embase, Global Health and four other databases were searched for eligible studies on social distancing for COVID-19 published from inception of the databases to 30 September 2020.
Study selection and data extraction
Effectiveness studies on social distancing between individuals, school closures, workplace/business closures, public transport restrictions and partial/full lockdown were included. Non-English articles, studies in healthcare settings or not based on empirical data were excluded.
Results
After screening 1638 abstracts and 8 additional articles from other sources, 41 studies were included for synthesis of findings. The review found that the outcomes of social distancing measures were mainly indicated by changes in Rt, incidence and mortality, along with indirect indicators such as daily contact frequency and travel distance. There was adequate empirical evidence for the effect of social distancing at the individual level, and for partial or full lockdown at the community level. However, at the level of social settings, the evidence was moderate for school closure, and was limited for workplace/business closures as single targeted interventions. There was no evidence for a separate effect of public transport restriction.
Conclusions
In the community setting, there was stronger evidence for the combined effect of different social distancing interventions than for a single intervention. As fatigue of preventive behaviours is an issue in public health agenda, future studies should analyse the risks in specific settings such as eateries and entertainment to implement and evaluate measures which are proportionate to the risk.
Keywords: COVID-19, EPIDEMIOLOGY, Infection control, Public health
Strengths and limitations of this study.
First scoping review to synthesise findings on the effectiveness of social distancing measures for COVID-19 at individual, community and national levels and social settings assessed by different outcome parameters.
This review analyses the level of evidence for different types and levels of social distancing measures.
Findings in varied outcome parameters could not be compared directly.
Non-English literature was excluded from this review.
Introduction
Social distancing is one of the main non-pharmaceutical interventions (NPIs) to control the outbreak of COVID-19 worldwide. Social distancing, also known as physical distancing, is based on the premise that the rate of transmission of infectious diseases will decrease if people in communities stay at home from work or school, avoid large gatherings and refrain from having physical contact with each other. WHO guidelines describe social distancing measures at the individual level (eg, keeping at least one metre from each other) and the community level including stay-at-home recommendation/ordinances and measures in specific socioeconomic settings (eg, workplace, schools, eateries, entertainment and parties).1 2 At the national or regional levels, lockdown (also called ‘community quarantine’ to restrict movement of population groups) may be imposed as an extreme form of social distancing,3 4 where it can be a total or partial lockdown to restrict key socioeconomic activities.5
Despite the fact that social distancing measures have become a crucial strategy globally in mitigating COVID-19 pandemic, the evidence for their effectiveness is just slowly accruing. Earlier studies applied mathematical modelling to predict effectiveness of social distancing measures.6–9 Recent studies evaluated the outcomes retrospectively using empirical data and reported the outcomes within specific parameters. A study which analysed data from 149 countries suggested that implementation of different social distancing interventions was associated with an overall reduction in COVID-19 incidence of 13% (incident rate ratio, IRR 0.87, 95% CI 0.85 to 0.89).10 It concluded that data from 11 countries indicated similar overall effectiveness (pooled IRR 0.85, 95% CI 0.81 to 0.89) when school closures, workplace closures and restrictions on mass gatherings were in place.10 The European Centre for Disease Prevention and Control (ECDC) also estimated the effectiveness of different types of social distancing in Europe. While most were based on prediction modelling, some retrospective analyses showed that lockdown reduced Rt from around 2.7 to 0.6 in the UK.11 Given different types, variations and combinations of social distancing measures were implemented at different levels in different jurisdictions and pandemic contexts, it is important to study what parameters and methods were used and what outcomes were measured in various research studies. This is critical in a protracted pandemic after continuing restrictions to individual movement and socioeconomic life, which have led to fatigue in preventive behaviours. In this context, targeted measures which have been evaluated to be proportionate to the risks should motivate continuing preventive behaviours.
This study aims to synthesise research findings on the effectiveness of different types and levels of social distancing measures during earlier stage of the COVID-19 pandemic. The study was conducted as a scoping review to include a broad range of outcome parameters and study designs. This enables a better understanding of the effectiveness of the spectrum of social distancing measures in controlling the COVID-19 pandemic.
Methods
The scoping review method was applied to include a range of parameters relating to effectiveness of social distancing measures during the COVID-19 pandemic. In contrast to a systematic review which answers a specific and narrow question, a scoping review aims to explore a set of emerging and diverse themes to synthesise the current evidence, clarify conceptual parameters and identify gaps for further research.12–14
Eligibility criteria
Inclusion criteria for this review were studies that described: (1) effectiveness or outcomes of social distancing measures targeting the general public; (2) social distancing measures including those between individuals; targeted measures including closures of schools, workplaces, restaurants, bars and other social settings; stay-at-home recommendation/ ordinances, community quarantine and lockdown; and (3) quantitative research, secondary data analysis, modelling studies based on empirical data and review articles.
Exclusion criteria were: (1) qualitative studies, commentaries, mini-reviews without search strategies, editorials, conference presentations, dissertations and book chapters); (2) non-English articles; (3) studies in healthcare settings, such as those on healthcare workers, hospital patients and elderly nursing homes; (4) studies on the impact of social distancing measures on non-COVID-19 disease management and psychosocial health of the public and (5) hypothetical/stimulation models predicting future trends of incidence.
Search strategies and study selection
Seven electronic databases including AMED, Embase, Global Health, MEDLINE, Ovid Nursing Database, APA PsycINFO, Social Work Abstracts were searched by an experienced team member in scoping and systematic reviews. The search period was from the inception of the databases to 30 September 2020. To enhance sensitivity, syntax of “COVID*“.m_titl. AND social distan*.ab and “COVID*".m_titl. AND physical distan*.ab were used as search strategies to cover both terms of social distancing and physical distancing. Additional syntax of “SARS-CoV-2*".m_titl. and (social distan* or physical distan*).ab. were used to search for articles using the keyword ‘SARS-CoV-2’. Details are shown in the online supplemental file 1. Furthermore, backward searches from the reference lists of the articles were conducted to locate additional articles and reports. The search and selection process followed the Joanna Briggs Institute Methods Manual for scoping reviews, and the reporting was guided by Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Extension for Scoping Reviews (PRISMA-ScR).15 Two reviewers independently screened the titles and abstracts to assess their eligibility. Full texts of potential citations were retrieved for detailed examination. Selection discrepancies were settled through discussions between these two reviewers. Any outstanding disagreements were resolved by consulting the third member. We did not conduct risk of bias assessment, which is consistent with recommendations from the Joanna Briggs Institute Scoping Review Methods Manual and PRISMA-ScR,15 as different from a systematic review, a scoping review aims to provide an overview of the existing evidence comprehensively, regardless of risk of bias of included studies.15
bmjopen-2021-053938supp001.pdf (28.6KB, pdf)
Data extraction and synthesis
For each study included, texts under the headings of ‘results’ or ‘findings’ were extracted and analysed by two reviewers. The analysis was performed by one reviewer and verified by a second reviewer. The two reviewers reached consensus on the outcomes reported and their classification to corresponding types of social distancing and effectiveness indicators.
Patient and public involvement statement
It was not appropriate or possible to involve patients or the public in the design, or conduct, or reporting, or dissemination plans of our research.
Results
Study selection and characteristics
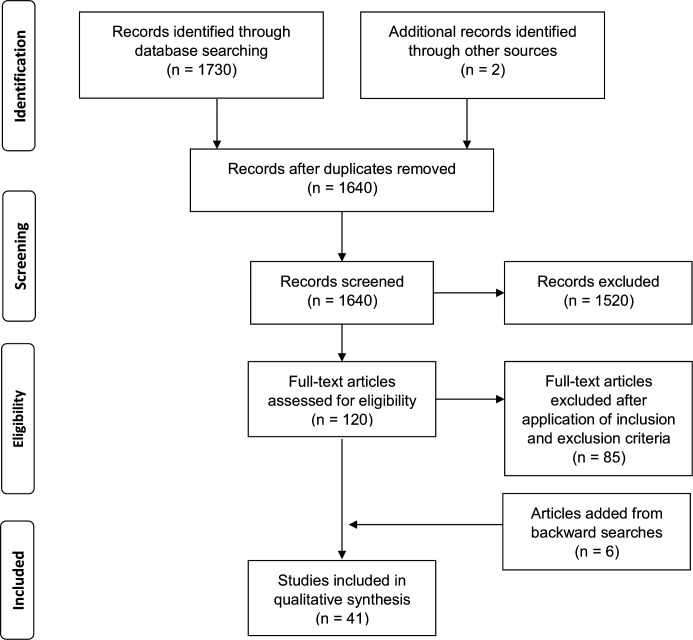
We screened 1638 abstracts from our electronic search on the databases with 2 additional research reports identified from governmental websites. Of the 120 full texts retrieved for further assessment, 35 articles fulfilled our eligibility criteria. In addition, 6 relevant studies were identified from the reference lists of the articles through backward searches. Hence, in total, 41 studies were included in this review. Figure 1 presents results of the literature search and classification flow, and table 1 provides detailed characteristics of the selected articles.
Figure 1.
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses - Extension for Scoping Reviews) flow diagram of literature search and selection.
Table 1.
Article characteristics (n=41)
| Count (%) | |
| Countries/cities by geographic region | |
| Asia | 13 (27.7) |
| Australia and New Zealand | 2 (4.3) |
| Europe | 12 (25.5) |
| North America | 14 (29.8) |
| South America | 3 (6.4) |
| Global studies | 3 (6.4) |
| Country economy* | |
| High income | 33 (63.5) |
| Middle income | 16 (30.8) |
| Low income | 3 (5.8) |
| Article type | |
| Research article | 38 (92.7) |
| Review article | 3 (7.3) |
*Country economy level according to The World Bank’s classification.
There were 38 research studies and 3 reviews. Fourteen studies reported data from North America, another 13 from Asia, 12 from Europe, 3 from South America and 2 from Australia. There were also 3 global studies which reported data from over 50 countries in multiple regions. According to the classification by World Bank, 63.5% of the studies were from high-income countries/regions; 30.8% and 5.8% were from middle-income and low-income countries/regions, respectively.
Table 2 summarises the key findings based on the following effectiveness indicators: (1) Infectivity: Rt, effective reduction number; (2) Incidence: infection incidence, ratio of incidence rate, attack rate or bed occupancy rate; (3) Mortality or fatality rate; (4) Effect time: action and effect duration, time of reaching peak; (5) Attendance percentage of location, daily vehicles miles, daily contact frequency, mobility of leaving home, or travel distance. A description of each type of intervention is also given. A tick “✓” is put if no detailed elaboration was provided in the reviewed articles.
Table 2.
Effectiveness and outcomes of social distancing measures
| Article and study characteristics | Type of social distancing measures | Effectiveness indicators | ||||||
| Authors; article type; study period/ publication date; study design | Country/ region; economy level | Social distancing between individuals | School measure/closure | Workplace measure/closure | Public transport restriction | Stay-at-home recommendation/ordinances | Others | Infectivity: Rt, effective reduction number Incidence: Incidence, incidence rate, attack rate, bed occupancy rate Mortality: Mortality or fatality rate Effect time: Action and effect duration, time of reaching peak Attendance: Attendance % of location, daily vehicles miles, daily contact frequency, mobility of leaving home, travel distance |
| Auger et al Research article; 9/3/2020-7/5/2020; Population–based observational study of changes in incidence and mortality24 |
The US; High |
Statewide closure of primary and secondary schools | (Incidence and mortality): Primary and secondary school closure in the USA between March and May 2020 was associated with decreased COVID-19 incidence (adjusted relative change per week, −62%) and mortality (−58%). States that closed schools earlier, when cumulative incidence of COVID-19 was low, had the largest relative reduction in incidence and mortality, although there might be confounding effects from other interventions. | |||||
| Brauner et al Research article; 22/1/2020-30/5/2020; Modelling study based on national case and death counts17 |
Members of the EU countries; High |
Limiting size of gathering | Closing most of non-essential businesses and high-risk businesses, for example, bars and restaurants | (Infectivity): 41 countries-pooled data showed Rt reduction of 36% when gatherings were limited to 10 people or below; 28% when 100 or below and 13% when 1000 or below. A 29% Rt reduction came with closing most of non-essential businesses while 20% was found when closing high risk businesses, for example, bars and restaurants. | ||||
| Castaneda-Babarro et al; Research article; 23/3/2020-1/4/2020; Cross-sectional survey on 800 general public for walking time46 |
Spain; High |
✓ | Forced e-learning | Restricted travel | Country lockdown with stay-at-home measures | (Attendance): Self-reported walking time decreased by 58.2% during confinement. | ||
| Clipman et al; Research article; 17–28/6/2020 Cross-sectional survey on 1030 general public for infection history and social distancing behaviours20 |
Maryland, the US; High |
✓ | (Incidence): Multivariable analysis found that history of SARS-CoV-2 infection was significantly less common among those who always practiced social distancing (aOR for indoor social distancing, 0.32(95% CI 0.10 to 0.99); aOR for outdoor social distancing, 0.10 (95% CI 0.03 to 0.33). | |||||
| Cruz; Research article; 15/3 to 5/4/2020; Time series analysis of death counts40 |
São Paulo City, Brazil; Middle |
✓ | Mandatory closure | Work-from-home and mandatory closure of non-essential businesses | (Mortality): Correlating daily death number with Social Distancing Index (SDI) was derived from government websites. SDI was between 52% and 56%, crossing the break-even point of death number (from 0.82 to −0.4). SDI larger than 55% is needed to reduce death number. | |||
| Courtemanche et al Research article; 1/3 – 27/4/2020; Analysis of growth rate of cases37 |
The US; High |
Ban on large social gathering with a limit of 50 people | Public school closure | Closing entertainment businesses | Shelter-in-place order (last policy) |
(Incidence): Growth rate of daily confirmed cases reduced by 5.4% after 1–5 days, 6.8% after 6–10 days, 8.2% after 11–15 days, 9.1% after 16–20 days. The number of confirmed cases was 10 times greater without shelter-in-place order and 35 times greater without 4 types of social distancing measures. | ||
| Du et al; Research article; 1/1 - 15/2/2020; Analysis of case data from online reports31 |
58 cities of China; Middle |
Ban on public gathering | ✓ | Closing shopping malls, restaurants and entertainment businesses | Suspension of intracity and intercity public transport | ✓ | Testing | (Infectivity):
Rt declined by an average of 54.3% (±17.6%) during the containment period. (Effect time): The mean time until successful containment was 21 days after the first reported case and 8 days following the initiation of interventions. During the period of containment, the Rt declined by an average of 54.3%. A delay of 1 day in implementing the first intervention is expected to prolong an outbreak by 2.41 days (95% CI 0.96 to 3.86) |
| Ehrhardt et al; Research letter; 25/5/20-25/8/20 Analysis of COVID- 19 cases aged 0–19 years who attended schools / childcare facilities27 |
Germany; High |
50% class size reduction, cancelling physical education lesson, physical distancing between children | Enhance ventilation of rooms, policy for sick students to stay at home, facemask wearing, suspension of singing or use of wind instruments during music lesson, promoting hand hygiene, cough etiquette, cleaning of contact surfaces | (Incidence): The infection for children aged 0–19 was 3.3% among all settings, suggesting child-to-child transmission in schools and childcare facilities was uncommon and not the primary cause of SARS-CoV-2 infection in children. It might be partially due to the infection control measures initiated after school/child-care-facility reopening. | ||||
| Otte et al; Research letter; 28/1/20 – 31/8/20 Analysis of COVID-19 data on school outbreaks using national surveillance system26 |
Germany; High |
Opening school for specific grades, staggering timetables, alternating between remote and on-site teaching, restricting class size, keeping distance between students | Policies for sick students and staff to stay home, enhanced hand hygiene, wearing face masks, ventilation of rooms, respiratory etiquette | (Incidence): The average number of outbreaks and of cases per outbreak was smaller after reopening of schools (2.2 outbreaks/week and 4 cases/ outbreak) than before school closure (3.3 outbreaks/week and 6 cases/outbreak). | ||||
| Huynh; Research article; 16/2 - 29/3/2020; Analysis of data from community mobility reports41 |
58 countries; Low to high |
Social distancing in:
3.parks
|
(Attendance): Attendance in percentage change of specific locations was reported. Countries with higher Uncertainty Avoidance Index (UAI) predicted lower proportion of people gathering in public such as retail and recreation, grocery and pharmacy, parks, transit stations, workplaces. Northern Europe (Finland, Sweden and Norway) with lower UAI was unlikely to commit to social distancing. The cultural determinants played an important role in controlling infection behaviour. | |||||
| Islam et al; Research article; 1/1– 30/5/2020; Natural experiment with interrupted time series analysis10 |
149 countries; Low to High |
Restriction of mass gathering and public events | School closure | Workplace closure | Public transport closure | Movement Lockdown | (Incidence): Overall, with any intervention, there was 13% reduction in incidence. Data suggested similar effectiveness when school closures, workplace closures, and restrictions on mass gatherings were in place. Earlier lockdown was associated with a larger reduction compared with a delay after other interventions were in place. A combination of 4 measures including restrictions on mass gatherings, school closures, workplace closures, and lockdowns in 32 countries was associated with decreasing incidence of COVID-19 (pooled incident rate ratio, IRR 0.87, 95% CI 0.84 to 0.91). | |
| Jarvis et al; Research article; 24/3-27/3/2020; Cohort survey on 1356 general public to report daily number of contacts47 |
The UK; High |
School closure | Limiting time at work, having work closed and/or not visiting work | Quarantine and isolation isolate | (Attendance): A 74% reduction in the average daily number of contacts was observed per participant (from 10.8 to 2.8). It was expected to be sufficient to reduce R0 from 2.6 before the lockdown to 0.62 (95% CI 0.37 to 0.89) after the lockdown, based on all types of contact and 0.37 (95% CI 0.22 to 0.53) for physical contacts only. |
|||
| Lemaitre et al Research article; 24/2/2020-24/4/2020 Modelling study using data on hospitalisations and deaths21 |
Switzerland; High |
Ban on gathering | School closure | Closure of nonessential activities | (Infectivity): Strong support for changes in R0 following the mobility decline which happened before school closure (national-level mean probability across activities 0.70, cantonal range 0.55–0.99), High correlation between changes in R0 and changes in mobility were found, with the strongest associations shown in mobility to work, transit stations, retail and recreation, and residential (cross-correlations >0.9 in all cantons and nationally). |
|||
| Jüni et al; Research article; 7– 13/3/2020; Prospective cohort study for incidence48 |
144 countries; Low to High |
Gathering of any size | ✓ | Closing restaurants, bars, or non-grocery stores | (Incidence): A rate ratio comparing the cumulative count of confirmed COVID-19 cases with that of previous week was reported. There was strong association of epidemic growth with mass gathering (RRR 0.65, 95% CI 0.53 to 0.79), school closure (RRR 0.63, 95% CI 0.57 to 0.78), business closure (RRR 0.62, 95% CI 0.45 to 0.85). | |||
| Khanna et al; Review; Published on 10 April 202049; |
China, HK, Singapore, South Korea, USA, Italy, Spain, Iran and India; Middle to High |
All transports in and out of Hubei were prohibited, with each citizen being allowed to go out for 30 min every 2 days | 3 weeks lockdown in Hubei | Quarantine of mild and asymptomatic cases for China Travellers | (Infectivity): China Rt reduced from 2.35 to 1.05 during the period of 16/1/2020–30/1/2020. (Effect time): China slowed the dispersal of infection to other cities by 2.91 days and increased the doubling time from 2 to 4 days. Other Chinese cities implementing preventive control measures earlier were reported 33.3% fewer cases in the first week of their outbreaks compared with that of cities starting the control later. |
|||
| Koh et al; Research report; 1/1/2020-28/5/2020 Analysis of effect of measures indicated by Rt36 |
142 countries; Low to High |
Cancellation of public events, restrictions on size of gatherings, | ✓ | Closure of workplace | Closures of public transport | Stay-at-home order | Restrictions on internal movements/ international travel | (Infectivity): Following the 100th case, it was found effective that complete travel bans and all forms of lockdown-type measures reduced average Rt over the 14 days. Stay-at-home recommendation and partial lockdowns were as effective as complete lockdowns when controlling the outbreaks. However, these measures were effective when it could be implemented early. |
| Macartney et al; Research article; 25/1/20-10/4/20. Analysis of confirmed cases in children and staff who attended schools or early childhood education and care settings28 |
Australia; High |
Reduced face-to-face attendance | (Incidence): Although the attack rate of secondary cases was 0.5% in schools, it was unable to assess the effect on transmission regarding hygiene or physical distancing used in educational settings | |||||
| Lai et al; Research article; 23/1 – 1/3/2020; Epidemiological study analysing government information of the confirmed cases50 |
Hong Kong; High |
✓ | Work from home | Border Control
(18/1-7/2)
(8-29/2) Mandatory quarantine for China travellers in phase 4 |
(Infectivity): Median Rt dropped from 1.07 to 0.75 with border control in phase 4 (8–29/2/2020). | |||
| Lam et al; Research article; 1/1 – 31/5/2020; Epidemiological study analysing the changes in daily number of confirmed cases39 |
Hong Kong; High |
Cancellation of large-scale events | School suspension from phases 1–4 | Work from home for civil servants in phases 1 and 2 | Entry restriction / quarantine for inbound travellers and asymptomatic testing | (Mortality): Case fatality ratio (0.4%) was much lower than global ones during the same period in WHO (6.1%). | ||
| Lasry et al; Research article; 26/2 – 1/4/2020 Descriptive analysis using types and timing of mitigation interventions, cumulative number of reported cases, percentage change in confirmed cases and community mobility51 |
4 US metropolitan areas: San Francisco, Seattle; New Orleans, and New York City; High |
Ban on gathering of certain size | School closure | Restrictions on businesses | Stay-at-home orders (last policy) |
States of Emergency (first policy) |
(Attendance): Mobility of leaving home was reported. In four localities, the percentage leaving home was close to 80% on February 26, and decreased to 42% in New York City, 47% in San Francisco, 52% in Seattle, and 61% in New Orleans on April 1. Mobility did not decline following the state of emergency alone but a combination of policies such as gathering restrictions or school closures and further decreased after stay-at-home orders. (Incidence): 3 day average percentage change in cumulative case count showed a decreasing trend by the last 2 weeks of March after a set of policies implemented. |
|
| Lino et al; Research article; 1-31/5/2020 Observational study on bed occupation rates in a hospital following lockdown4 |
Fortaleza (state capital city), Ceará, Brazil; Middle |
✓ | Suspension of commercial activities | Restricted daytime movements and interruption of intercity trips | City lockdown, night curfews | (Incidence) Bed occupancy rates in a tertiary hospital for referred COVID-19 cases were higher than 100% before the lockdown and reached nearly 140% 2 days after. The rate decreased to below 100% 14 days after the lockdown (viral incubation period) and dropped to about 85% 23 days after the lockdown onset. | ||
| Lim et al; Research article; 15/2/20-9/5/20. Analysis of COVID-19 case counts from each Southeast Asian country collected from open web source34 |
9 Southeast countries including Cambodia, Indonesia, Laos, Malaysia, Myanmar, the Philippines, Singapore, Thailand and Viet Nam; Middle to High |
No social gathering or with people limit, 1–2 m physical distance in public place |
Close schools | Close of non-essential business, work from home | No or limited capacity of public transport, healthcare declaration forms required, no interstate transportation | Stay-at-home order, curfew from 10pm to 4am | Broader closure, mandatory masking in public place | (Incidence): Average daily incidence declined gradually for all countries except the Philippines and Laos. (Infectivity): A large variation in Rt reduction, with the biggest decrease in Malaysia from 3.68 (95% CrI 3.47–3.91) to 1.53 (1.44–1.61) and the smallest decrease in Laos from 1.55 (1.04–2.08) to 1.20 (0.84–1.56). |
| Marschner; Research article; 25/1 – 8/5/2020 Back-projection study analysing the probability distribution of the time between infection and diagnosis35 |
Australia; High |
Stage 2: limiting gathering of 2 people (26–31 March) |
Stage 1: prohibited face-to-face meeting and entertainment activities (23 March) | Stage 3: prohibited leaving home (26–31 March) | Border control (20 March) |
(Effect time): It was estimated that 1 week delay in control measures would lead to an almost fivefold increase in total infections but 1 week earlier control would reduce total infections of similar magnitude. | ||
| Munayco et al; Research article; 23/1– 9/5/2020 Modelling study using the daily number of confirmed cases by date of symptoms onset52 |
Peru; Middle |
Ban on gathering of larger than 300 people on 12 March | School measure since 11/3 | Closing country border, National Emergency Declaration on 16 March | (Incidence): Before the implementation of social distancing measures in Lima, the mean scaling of growth parameter, p, was estimated at 0.9 and the reproduction number at 2.3. School closures and other social distancing interventions slowed down the spread of the novel coronavirus, shifting the exponential growth trend to an approximately linear growth trend, with the scaling of growth parameter being reduced to 0.53. | |||
| Pan et al; Research article; 8/12/2019– 8/3/2020 Cohort study on data of 32 583 patients33 |
China Wuhan; Middle |
Social distancing | Traffic restriction | Cordons sanitaire | Universal symptom survey, home and centralised quarantine | (Infectivity): A reduction of Rt from larger than three in January to less than 1.0 on February six and then less than 0.3 in March after implementation of measures by different phases. | ||
| Patel P et al; Research article; 30/1– 4/5/2020 Epidemiology study using the growth rate of confirmed cases53 |
India; Middle |
✓ | ✓ | ✓ | Lockdown since 25 March | progressive travel restriction, health promotion and enhanced testing | (infectivity): A decline in Rt following NPIs implementation was observed, with a reduction from 2.51 to 1.83 at the end of lockdown phase. Although the sub-exponential growth confirmed mitigation of epidemic, Rt larger than one still indicated ongoing disease transmission. | |
| Randhawa et al; Research letter; 1/3/20-16/4/20. Analysis of the positivity rates for SARS-CoV-2 in outpatient settings In Washington State and in emergency departments in Seattle29 |
The US High |
Statewide gathering limits | Statewide shut down of bars and restaurants | Washington State’s stay-home order | (Incidence): The positivity rate was 17.6% in the outpatient clinics and 14.3% in emergency departments at the peak period and 3.8% and 9.8%, respectively, at the end of the analysis period. | |||
| Rivkees et al; Brief report; 1/3/2020-31/5/202023 |
Florida, US High |
✓ | Closures of elementary schools, high schools, and universities for in-person classes | Restricted access to bars and restaurants, limited commerce to essential businesses | ✓ | Statewide stay-at-home order | (Attendance) Assessment of movement within the state using Google mobility and Unacast mobility analytics based on cell phone data showed that closing schools resulted in a 40%–55% reduction in average distance travelled compared with pre-outbreak levels. The stay-at-home order was associated with a further reduction in average distance travelled. During the period under stay-at-home order, the density of in-person encounters fell by 74%–82%, visits to nonessential venues by 55%, and overall distance travelled by 45%. Average distance travelled within the state decreased by 25%–40%. | |
| Rubin et al Research article; 25/2/2020- 23/4/2020 Cohort study using publicly de-identified data19 |
The US; High |
✓ | Reduce visits to nonessential businesses | (Infectivity): In multivariable analysis, a 50% decline in visits to nonessential businesses was associated with a 45% decline in Rt (95% CI, 43% to 49%). With a 70% decrease in visits to nonessential business, a fall below a threshold Rt of 1.0 was estimated in 202 counties (95.7%), including 17 of 21 counties (81.0%) in the top density decile and 52 of 53 counties (98.1%) in the lowest density quartile. | ||||
| Saez et al Research report; 17/1/2020-5/4/2020 Time series analysis on the new daily cases54 |
Spain High |
Reducing travel, avoiding crowded places, using non-contact greetings | ✓ | Closure of workplaces, stadiums, cinemas, theatres and restaurants | ✓ | Quarantines, travel restrictions | After implementing the measures for 1 day, the variation rate of accumulated cases decreased daily by 3.059 percentage points on average (95% credibility interval: −5.371 to –0.879) and the decline was greater when time passed and reached 5.11 percentage points on the last day of data collection. Despite not entering the decrease phase, the measures taken by the Spanish Government on March 14, 2020 managed to flatten the curve. | |
| Siedner et al; Research article; 10/3/2020- 26/5/2020 Longitudinal pretest–posttest comparison study of incidence and mortality25 |
All 50 states of the US, High |
Statewide social distancing measures with cancellation of public events | ✓ | ✓ | Restrictions on internal movement and closure of state borders | (Incidence) The mean daily COVID-19 case growth rate dropped by 0.9% per day, starting 4 days after implementation of the first statewide social distancing measures. (Mortality) After implementing social distancing for 7 days, the COVID-19-attributed mortality growth rate fell by 2.0% per day, although this decline was no longer statistically significant by 10 days. |
||
| Thu et al; Research article; 11/1 – 2/5/2020 Time-series analysis based on daily cases38 |
ten countries: the US, Spain, Italy, UK, France, Germany, Russia, Turkey, Iran and China; Middle to High |
Cancellation of public events | ✓ | Work from home, cancellation of non-essential events | Domestic transportation restriction | By region and, by nationwide, by different phases | Entry restrictions to those from highly infected areas | (Incidence): Growth rates of daily confirmed cases in the UK and the USA were the most severe, at 99.9%, followed by Spain at 99.2%, France at 96.2%, Italy at 95.4%, Germany at 85%, Russia at 72.2%, Turkey at 70.7% and Iran at 62.8%. Countries with high growth rate showed lower decline rate, showing longer time needed for those countries to control the epidemic by social distancing measures. |
| Vokó et al; Research article; 1/2/2020-18/4/2020 Modelling study using daily new cases55 |
28 European countries; High | Social distancing with public event ban | ✓ | ✓ | ✓ | ✓ | (Incidence) Incidence of new COVID-19 cases grew by 24% per day on average before the changepoint. From the changepoint observed, the growth rate was reduced to 0.9%, 0.3% increase, and to 0.7% and 1.7% decrease by increasing social distancing quartiles based on SDI calculated based on Google Community Mobility Reports. | |
| Wan et al; Research article; 20/1/2020-3/3/2020 Modelling study using incidence data, with death and recovery cases30 |
Mainland of China excluding Hubei; Middle |
Social distancing and self-isolation | ✓ | Close contact tracing, body temperature measurement | (Infectivity)Rt has dropped sharply from 3.34 on 20 January 2020 to 0.89 on 31 January 2020, after integrated control strategies were implemented. | |||
| Weill et al; Research article; 1/1/2020-21/4/2020 Event study design on behaviour subsequent to state emergency orders18 |
The US; High |
✓ | business closures | Safer-at-home orders | (Attendance): Median distance travelled, retail and recreation, locations visited by a mobile device per day showed a sharp decrease in March after the implementation of social distancing measures, with the wealthier areas decreasing mobility more significantly than poorer areas. However, the trend shifted reversely after March regarding completely staying at home. People from wealthier areas shifted from the lowest before March to the most likely to completely stay at home after March, vice versa for those in poorer countries. | |||
| Wilasang et al; Research article; From the date of 100 cases to 7/4/2020 Analysis on the number of daily new cases and the distribution of the serial interval56 |
ten countries: Belgium, China, France, Germany, Iran, South Korea, Spain, Thailand, US and UK; Middle to High |
✓ | ✓ | Active case finding | (Infectivity): After 3 weeks control measures, only China and South Korea were successful in controlling the disease (Rt <1), while the others were unsuccessful. The study observed that countries with active case-finding and prompt isolation could have a reduction in the reproduction number more rapidly. | |||
| Yehya et al; Research article; 21/1-29/42020 Ecological study using secondary data to analyse relationship between timing of interventions and mortality57 |
The US; High |
School closure | Declaration of Emergency | (Mortality): Each day of delay of either intervention increased mortality risk by 5%–6%. | ||||
| Zhang et al; Research article; 24 – 30/12/2019 as baseline and 1-10/2/2020 as outbreak period Analysis on contact survey data reported by 1193 study participants32 |
Wuhan and Shanghai; Middle |
✓ | ✓ | (Attendance): Daily contact frequency in Wuhan showed a reduction from 14.6 to 2.0 while Shanghai from 18.8 to 2.3. The trend was consistent with mobility data of an 86.9% and a 74.5% drop in Wuhan and Shanghai respectively. | ||||
| Zhang et al; Research article; 23/1– 9/5/2020 Analysis of the changes in incidence58 |
Wuhan (China), Italy and the US; Middle to High |
✓ | Stay-at-home | Face mask | (Incidence): Daily new infection in New York decreased with a slope of 106 cases per day (decreasing rate at around 3%) after face mask-on policy, while USA (excluding New York) increased with a slope of 70 cases per day (increasing rate at around 0.3%). The decreasing rate in the daily new infections in New York with face covering mandate was proportionately higher than that in the United States with only social distancing and stay-at-home order, illustrating the importance of face covering on stemming the virus spread. With mask-on policy, Italy showed an infection reduction by over 75 000 from April six to May 9. |
|||
| 58th SAGE meeting summary; Review22 |
The UK; High |
Lockdown, short stay-at-home order | (Infectivity): Lockdown was very impactful and reduced Rt from 2.7 to 0.6. 2–3 week short stay-at-home order had moderate impact on reducing Rt to less than 1. Both showed high confidence correlation. | |||||
| Decreasing contact between households, closure of worship/ community centres, restriction on outdoor gatherings | (Infectivity): Moderate impact was found by stopping contacts among different households, reducing Rt by around 0.1–0.2. Low to moderate impact was shown following closure of worship/ community centres, with a potential reduction in Rt up to 0.1. Low impact came with the restriction on outdoor gatherings, with Rt being reduced to less than 0.05, considering the frailty of SARS-CoV2 under well-ventilated environment. | |||||||
| Local 5 mile travel restriction, use of public transport restricted to key workers | (Infectivity): The impact of 5 mile travel restriction was considered as low to moderate, with limited benefit especially when local outbreak was widespread. Restricted use of public transport to key workers might have low impact due to low level of crowding, mandated face-mask policy and inconclusive evidence of the transmission risk in public transport. |
|||||||
| Mass / reactive school closure, closure of class with infection, alterative school schedules with half class sizes, closure of further/ high education or childcare | (Infectivity): Moderate impact of closing all schools was found, with a reduction in Rt of 0.2~0.5 while closing secondary schools was considered to be more effective, with a Rt drop of 0.35. Reactive school closure might have a moderate impact on the reduction in Rt of 0.12~0.45 whereas low to moderate impact was estimated for reactive closure of class with infection. Alternative school schedules with reduced class size were suggested to have moderate to low impact. Closure of further / higher education associated with moderate impact while closure of childcare might have low to moderate impact. |
|||||||
| Work from home, alternate work, closure of bars/ pubs/ cafes/ restaurants, closure of gym/ leisure centres, non-essential retail, personal services, adherence to “COVID-19 security” arrangement in workplaces | (Infectivity): Moderate impact of work from home was evaluated with a Rt reduction of 0.2–0.4 if all people followed while low to moderate impact with a Rt drop up to 0.1 was estimated for alternate work. Moderate impact with potential reduction in Rt of 0.1–0.2 was predicted for the closure of bars/pub/restaurants. Closure of gym/ leisure centres associated with low to moderate impact, with potential reduction in Rt of up to 0.1. Impact of closure of non-essential retail and personal services was estimated to be limited. Adherence to ‘COVID-19 security’ in workplaces such as improved hand/ surface hygiene and added barrier setting was also considered as low impact. |
|||||||
| ECDC; Review; Published on 24 Sept 202011 |
Members of the EU countries; High |
Stay-at-home | (Infectivity): Rt reduced by 18% (ranging from 4% to 31%). | |||||
| Physical distance between 1–2 m | (Infectivity): Physical distancing of 1 m or more was linked to an approximately fivefold reduction of the transmission risk, with the protective effect being doubled for every extra metre added. | |||||||
| Domestic travel restrictions: a cordon sanitaire or public transportation closure | (Infectivity): There were contradictory results on Rt among the studies. Modelling showed strong association while other studies showed no impact unless other NPI was put in place, for example, physical distancing. It was difficult to relate observed changes in transmission dynamics to a single measure. | |||||||
| School closure | (Incidence): Observational data suggested that reopening schools has not been associated with significant increases in community transmission. | |||||||
| Work from home, flexible working time and social distancing measures, closure of non-essential businesses | (Infectivity): There was a 40% Rt reduction by closing most of non-essential businesses while 31% by closing high risk businesses, for example, restaurant/bars/nightclub/cinemas/gym. | |||||||
ECDC, European Centre for Disease Prevention and Control; NPIs, non-pharmaceutical interventions; SAGE, Scientific Advisory Group for Emergencies.
Social distancing at individual level
Social distancing was usually achieved by prohibition of mass gathering in public areas and/ or maintaining certain physical distance between people. Most studies reported a relationship between the transmission risk and the level of social distancing. A meta-analysis including seven studies on COVID-19 concluded that physical distancing of 1 m or more was effective in reducing the transmission risk by five times and the protective impact was double for every extra metre.16 Similarly, based on the chronological data on interventions in 41 countries between January and May 2020, Brauner et al17 estimated that Rt reduced by 36%, 28% and 12% when gatherings were limited to 10, 100 and 1000 people, respectively. Furthermore, studies found how mobility changed according to different social distancing measures. A study by Weill et al18 in the US.Afound that median distance travelled, retail and recreation locations visited by a mobile device per day showed a sharp decrease in March 2020 after implementation of social distancing measures in the country, with the percentage of the population completely staying at home doubled. Similar results showed that a decline in visits to non-essential businesses following the implementation of social distancing was associated with a reduction in estimated Rt.19 In the analysis of 211 US counties, visits to nonessential businesses reduced by 50% and 70% contributed to a 45% decline in Rt and a drop of Rt to a threshold of 1.0, respectively, indicating that the larger the drop in nonessential business visits, the more significance in the reduction of a Rt.19 Another US study by Clipman et al,20 in Maryland, found that a history of COVID-19 infection was significantly less likely among the public who always practised social distancing (adjusted OR for indoor social distancing, 0.32 (95% CI 0.10 to 0.99]; adjusted OR for outdoor social distancing, 0.10 (95% CI 0.03 to 0.33)), giving indications of the effect of mobility on the pandemic. It was consistent with the inference by Lemaitre et al21 who found a strong support for changes in R0 following the mobility decline before implementation of school closure, underlining the importance of behaviour changes on the reductions in transmission. However, social distancing in different settings may have different impact. The UK Scientific Advisory Group for Emergencies (SAGE) meeting report22 suggested that stopping contact from different households would provide moderate impact by reducing Rt of 0.1–0.2 but the impact of physical distancing on outdoor gathering was minimal (Rt reduction <0.05) since good ventilation was usually observed.
Social distancing at level of community settings
School closure
School closure may have benefits during the pandemic, but the effectiveness was mixed when considering level of closures and the unexpected link between school closure and reopening. Rivkees’s23 study in Florida of the USA found that closing schools resulted in a 40%–55% reduction in average distance travelled compared with preoutbreak levels. Moreover, Auger et al24 found that the primary and secondary school closure in the USA between March and May 2020 was associated with decreased COVID-19 incidence (adjusted relative change per week, −62%) and mortality (−58%). On the other hand, the SAGE report22 suggested that closing secondary schools and further education could have greater impact, even though a moderate Rt drop of 0.1–0.5 was associated with mass school closure, as mature students worked in daytime and linked up infection pathways between workplace and households. It was also observed that states closing schools earlier, when cumulative incidence of COVID-19 was low, had the largest relative reduction in incidence and mortality, although there might be confounding effects from other interventions.25 Contrary to expected impacts of school closures, observational data in ECDC review suggested that reopening schools had not been associated with significant increases of community transmission.11 In other studies26 27 that focused on the various measures used in educational and children care centre settings after reopening, the results showed a low incidence rate in these settings. There was a decreasing trend of both the average outbreak numbers and the cases per outbreak by school measures and might be partially due to the extensive measures. However, the specific impact of reduction of face-to-face attendance in classrooms was not assessed.28
Workplace measures
Workplace measures include work-from-home arrangement, measures in working environment and closure of businesses. The SAGE report22 suggested a moderate impact of work from home measure, with a reduction of Rt between 0.2 and 0.4. Brauner et al17 estimated that a 29% Rt reduction was likely to follow with closing most of non-essential businesses, while closing high risk businesses, for example, bars and restaurants would be associated with a Rt decline of 20%. Although there was limited empirical data on the impact of closure of businesses, reduced visits to nonessential businesses in the USA was associated with a drop in Rt.19
Public transport restriction
Public transport restriction refers to suspension/limitation of intracity or intercity public transportation. The SAGE report22 suggested a low to moderate impact following the 5 mile travel restriction, especially when local outbreak was widespread. It might be because crowding in public transport was low and mandated face mask policy had already been implemented. However, Islam’s study10 showed no difference in reduction with or without the suspension of public transportation. On the other hand, ECDC review showed contradictory results, with a modelling study indicating a strong association with reduction of Rt while other studies did not show any impact unless introduced with other NPIs such as social distancing and behavioural changes.11 Therefore, it is difficult to relate observed changes in transmission dynamics to this single measure of public transport restriction.
Social distancing at national/regional level
Combination of interventions: partial lockdown
While the studies mentioned above focused on the effect of single type of intervention, many studies showed the effect of a combination of interventions, which could be regarded as a partial lockdown. A study by Siedner et al25 in the USA found that the mean daily COVID-19 case growth rate fell by 0.9% per day, starting 4 days after implementation of the first statewide social distancing measures including cancellation of public events, travel restriction, school and workplace closures. In a study by Randhawa et al,29 the SARS-CoV-2 positivity rate in Seattle-area outpatient clinics and emergency departments declined from the peak range of 14.3%–17.6% to 3.8%–3.9% after statewide physical distancing measures, such as shutdown of bars/restaurants, implementation of social gathering limits and stay-home orders. A drop of 2% in daily COVID-19-attributed mortality growth rate was also observed 7 days after the measures were implemented. Similarly, a study by Wan et al30 in Mainland China excluding Hubei (province of Wuhan) found that Rt had dropped sharply from 3.34 on 20 January 2020 to 0.89 on 31 January 2020 after implementing integrated control strategies. In Du’s study31 of 58 cities in China, also with a remarkable Rt reduction, at 54.3%, demonstrated the effectiveness after the implementation of multiple types of interventions.
Full lockdown
A full lockdown can be viewed as a combination of all measures. Islam et al10 reported a combination of 4 measures, including restrictions on mass gatherings, school closures, workplace closures, and lockdowns in 32 countries, were associated with decreasing incidence of COVID-19 (pooled IRR 0.87, 95% CI 0.84 to 0.91). Similar declining incidence was observed when public transport closure was added (pooled IRR 0.85, 95% CI 0.82 to 0.88; n=72 countries). Other than incidence reduction, bed occupancy could also be benefited from lockdown measures. In Lino’s study,4 before the lockdown, the bed occupancy rate for referred COVID-19 cases in a tertiary hospital in Fortaleza of Brazil was over 100% in the beginning of May and reached nearly 140% after 10 days. The rates decreased to below 100% and 85% at 14 and 23 days, respectively, after the lockdown.
There was more evidence showing the effect of lockdown with various indicators. Zhang et al32 found that an average daily number of contacts per survey participant significantly dropped from 14.6 to 2 and 18.8 to 2.3 in Wuhan and Shanghai, respectively, during the lockdown period, consistent with the respective trends of mobility data declining at 86.9% and 74.5%. Pan et al33 analysed data from Wuhan and found that the Rt gradually reduced from greater than 3 in January 2020 to less than 1 in February 2020 and fell further to less than 0.3 in March 2020 after the city lockdown. Lim et al34 studied 9 Southeast Asian countries found a large variation in social distancing policies across countries, leading to marked differences in the reduction in Rt, with the biggest decrease in Malaysia from 3.68 to 1.53 and the smallest decrease in Laos from 1.55 to 1.20. Similarly, a brief report from Rivkees and Roberson23 showed that the stay-at-home order in Florida of the USA, after the first month of implementation, resulted in a 74%–82% reduction in person-to-person encounters, 55% in visits to non-essential venues and 45% in overall distance travelled. After 2 months of implementing stay-at-home order, the average distance travelled within the state was also found to decrease by 25%–40%. Further, a modelling study of Brauner et al17 gathering data of 41 countries using NPIs estimated that stay-at-home orders (with exemptions) reduced the mean percentage of Rt by 10%. Moreover, in a SAGE report,22 it was suggested that country lockdown was impactful and could reduce Rt from 2.7 to 0.6 while 2–3 week short stay-at-home order had moderate impact in reducing Rt to below 1. As with all other measures, the earlier the stay-at-home order was implemented, the higher the impact.
Implementation timing and impact on the pandemic curve
Nearly all findings found that a timely implementation of measures could reduce the transmission risk significantly. The relationships between the timing and the change in rates of daily confirmed cases were analysed in a time series. Marschner35 used Australia data to back-project that there would be a fivefold increase in total infections if social distancing measures were delayed by 1 week. Consistently, in Du et al’s study,31 a 1-day delay in implementing the first intervention was expected to prolong an outbreak by 2.41 days. However, earlier lockdown, simulated by Islam et al,10 showed a larger reduction in COVID-19 incidence compared with a delayed one after other social distancing interventions were initiated. Another empirical study based on the Oxford COVID-19 Government Response Tracker36 tracked Rt temporally for 2 weeks following the 100th reported case in 140 countries and observed the median timing of implementation of measures across countries. The study found that lockdown measures and travel bans can be considered early if they were implemented around 2 weeks before the 100th case and a week before detecting the first case, respectively.36
In addition, social distancing measures had a progressive control impact on the growth rates of daily confirmed cases, with Courtemanche et al37 showing reductions of 5.4%, 6.8%, 8.2% and 9.1% after 1–5 days, 6–10 days, 11–15 days and 16–20 days, respectively, following the roll-out of the measures. The timing effect was further illustrated by Thu et al38 that social distancing interventions took 1–4 weeks to have an effect on the decline in number of infected cases among the 10 countries studied. Countries with higher growth rates at the beginning might have greater difficulties in controlling the transmission, and vice versa for those countries with initial lower growth rates. For example, China, Iran and Turkey, promulgating the most stringent level of social distancing measures, with initial infection growth rates apparently lower at around 60%–70%, had the highest decline rates at 71%, 51.8% and 50.8%, respectively, while the USA and the UK, having the highest initial growth rates (99.9%), experienced significantly lower decline rates of 14.8% and 25.9%, respectively. The result suggested that social distancing measures could be more effective when introduced earlier under situations with low growth rates.
Discussion
This scoping review covered a board range of social distancing interventions and outcome indicators. A comparison of the key findings of different levels of measures is shown in table 3. Outcomes were mainly indicated by changes in Rt, incidence and mortality, along with indirect indicators such as daily contact frequency and travel distance. Based on changes in Rt, incidence and mortality, there was adequate empirical evidence for the effect of social distancing at the individual level, and for partial or full lockdown at the community level. However, for targeted measures in social settings, the evidence was moderate and inconsistent for school closure, and limited for workplace/business closures. There was no evidence for the effect of public transport restriction alone.
Table 3.
Comparison of the major outcomes of different types/levels of social distancing
| Social distancing between individuals | School closure | Workplace measures | Public transport restriction | Partial lockdown | Full lockdown | |
| Relative frequency and consistency of evidence* | Adequate | Moderate | Limited | No | Adequate | Adequate |
| (Infectivity): Rt, effective reduction number |
Physical distancing of 1 m or more could reduce the transmission risk by five times and the protective impact was double for every extra metre.16 Estimated Rt reduced by 36%, 28% and 12% when gatherings were limited to 10, 100 and 1000 people, respectively.17 |
Estimated 29% Rt reduction by closing most of non-essential businesses while 20% by closing high risk businesses.17 In the USA, a 50% decline in visits to nonessential businesses was associated with a 45% decline in Rt (95% CI 43% to 49%).19 |
No difference in reduction in Rt.10 | In Mainland China excluding Hubei (province of Wuhan), Rt dropped from 3.34 to 0.89.30 In 58 cities of China, Rt dropped by 54.3%.31 |
From data of 41 countries, estimated Rt reduced by 10% by stay-at-home orders (−2%–22%).17 UK estimation suggested that country lockdown could reduce Rt from 2.7 to 0.6 while 2–3 weeks short stay-at-home order had moderate impact by reducing Rt to below 1.22 China Rt reduced from 2.35 to 1.05 during the lockdown.49 |
|
| (Incidence): Infection incidence/ratio of incidence rate ratio/attack rate/bed occupancy rate | In the USA, COVID-19 infection was less likely among the public who always practiced social distancing (aOR for indoor social distancing, 0.32 (95% CI 0.10 to 0.99); aOR for outdoor social distancing, 0.10(95% CI 0.03 to 0.33).20 | In the US, school closure decreased COVID-19 incidence (adjusted relative change per week, −62%).24 Observational data from a number of the EU countries suggested that reopening of schools was not associated with increase of community transmission.11 |
In the USA, mean daily COVID-19 case growth rate decreased by 0.9% per day 4 days after lockdown.25 | Data from 32 countries showed decreased incidence of COVID-19 (pooled incident rate ratio, IRR 0.87, 95% CI 0.84 to 0.91).10 Growth rate of daily confirmed cases reduced by 5.4% after 1–5 days, 6.8% after 6–10 days, 8.2% after 11–15 days, 9.1% after 16–20 days.37 |
||
| (Mortality): Mortality/fatality rate | In the USA, school closure decreased COVID-19-related mortality (−58%).24 | In the USA, COVID-19-attributed mortality growth rate decreased by 2% per day 7 days after lockdown.25 | ||||
| (Effect time): Action and effect duration/time of reaching peak | In 58 cities of China, mean time until successful containment was 8 days.31 | |||||
| (Attendance): Attendance % of location/daily vehicles miles/daily contact frequency/mobility of leaving home/distance travel | In Florida, the USA found that closing of schools resulted in a 40%–55% reduction in average distance travelled.23 | In Spain, self-reported walking time decreased by 58.2%.46 | In Wuhan and Shanghai, the average daily number of contacts dropped from 14.6 to 2 and 18.8 to 2.3, respectively, during lockdown. Mobility dropped 86.9% and 74.5% in respective areas.32 Stay-at- home order in Florida of the USA resulted in a reduction of in-person encounters by 74%–82%, visits to nonessential venues by 55%, and overall distance travelled by 45%.23 |
*Relative frequency and consistency of evidence based on the studies reviewed, without risk of bias assessment.
Many studies reported the combined effects of different social distancing interventions which were usually implemented as a package of 3–5 measures. Observed impact of a single measure in a social setting was scarcely reported or only demonstrated with modelling. For example, Islam et al10 reported that among 149 countries studied, 118 countries implemented 5 measures while 29 countries used 3 to 4 interventions, with only one country introducing 2 measures and the remaining one implementing a single measure. In addition, even though the lockdown, in this review, was shown to have the highest reduction in Rt, it had been implemented as multiple measures.
Apart from types of interventions, the relationship between implementation time points and the effect were also investigated. Lam et al39 observed an early public health measure promulgation was able to contain the epidemic in Hong Kong, without initiating extreme measures such as a city-wide lockdown. Other studies suggested that the effect time variation might be due to the different times and levels of promulgating the social distancing measures, making the effectiveness apparently different.38 It could be demonstrated in the comparison between countries that the stronger the level of social distancing, the faster it took to reduce the number of daily confirmed cases.38 Furthermore, high initial infection incidence due to late implementation of measures would reduce the effectiveness of measures.38 All these results indicated a need for a rapid response and stringent measures to win the battle.
Contextual factors
In addition to the types, levels and timing of social distancing measures highlighted in this review, the effectiveness of measures was also affected by contextual factors such as compliance, social belief and cultural factors. Low public compliance may be a key explanation when interventions showed no sign of flattening of the epidemic curve. The compliance issue was further supported by Cruz’s study40 in examining the Social Distancing Index, a social distancing adoption index used by the Brazilian government found that it needed to be larger than 55% to reduce the daily death number. Moreover, social belief such as awareness of disease information might cultivate a sense of self-imposed initiation of handwashing, wearing protectives, keeping a distance from people and reducing outdoor activities. Cultural factors may also have an influence on public gatherings, although it was too complicated for a quantitative evaluation of the timing, magnitudes and processes that were prevalent in a region. Cultural factors were studied in Huynh’s study41 illustrating that countries with higher Uncertainty Avoidance Index (UAI) predicted a smaller proportion of people gathering in public such as in grocery and retail stores, pharmacies stores, recreation areas, public transport and workplaces, whereas countries in the northern European such as Finland, Sweden and Norway with lower UAI people were unlikely to follow social distancing measures. Furthermore, Islam’s study10 observed greater case reduction associated with those countries with a higher gross domestic product (GDP) per capita, a higher proportion of population aged 65 years or above, and stronger preparedness for the pandemic measured by the country health security index. Therefore, cultural determinants are likely to play an important role in compliance with preventive behaviours.
Knowledge gap for future research
Due to the heterogeneity of the outcomes adopted in the studies, it is difficult to render direct comparison of the changes in Rt and incidence. Consistent inclusion of these outcomes in studies of similar kinds may allow systematic review and meta-analysis in further studies.
Few studies have investigated the effect of closure of entertainment and eatery settings. The SAGE report22 suggested that closures of gyms, bars and restaurants were useful since there were environmental risks linked to higher probability of touch surfaces, higher aerosol generation and breathing rates due to aerobic activities. Specifically, the risk in bars and pubs was likely to be higher than many other indoor settings due to close proximity of people, long exposure duration, no wearing of face coverings and talking loudly. Some venues were poorly ventilated, especially in winter. In addition, consumption of alcohol impacts on customers’ behaviours. More empirical evidence focusing on the dynamic interaction of the environment, customer behaviours and transmission risks would be beneficial.
Some researchers proposed strategies need to be demonstrated by empirical evidence. A circuit breaker, proposed in the SAGE report,22 referring to as the 2–3 weeks short-time lockdown, could put the epidemic curve back by about 28 days or more. Based on historical evidence from the 1918 influenza pandemic, Correia et al42 argued that regions taking earlier and aggressive social distancing measures grew faster economically in the postpandemic period although there were adverse effects on the economy during the pandemic. Thus, predicting the recovery in an economy or a community based on the effectiveness of each intervention would be a continuing concern.
Fatigue of pandemic prevention was seen everywhere during the course of COVID-19 pandemic which may exacerbate the peaks and resurgence following the relaxation of measures and undermine the public acceptance to the advice from authorities. Governments with good risk communication with the public, hinging on engagement, communication and feedback, would be essential to help individuals assess and reduce their own risks appropriately. Abel et al43 reported that social distancing might lead to depression and anxiety in some people, which in turn would have an impact on social stability. Psychological impacts were not only observed on patients, healthcare workers but also on the overall population. However, Kim and Su44 suggested we should routinely provide psychological support instead of stopping social distancing measures. Future studies should explore the longer-term strategies for risk communication and risk analysis in specific settings to minimise public fatigue in compliance with social distancing mandates. Response measures should be proportional to the risk in different settings.
Our search period was up to 30 September 2020 when vaccine was not available for population use. For mass vaccination programmes which were implemented in most countries after December 2020.45 The reported number of cases per population was under 2.3% across countries. Including unreported asymptomatic cases, population immunity should still be insignificant during this period. However, this study period may have an advantage in excluding the confounding effect of population immunity and mass vaccination on the effects of social distancing measures. Future studies should explore whether the effect of social distancing declines as the degree of population immunity increases.
Limitations
Although a lot of information on the measures taken was collected from government websites, measures implemented in small localities or regional areas were not widely publicised or difficult to access, resulting in relevant studies being limited. Moreover, there was a wide variation of testing accessibility and for the criteria who should be tested, in different countries. Similarly, the points of time of promulgation and severity level of interventions were different among countries. Therefore, the cumulative confirmed cases might not reflect the actual situation in the population and were not accurate for comparisons. Using a time series analysis referencing to the date of death but not to the date of testing might be under a possible variation of case reporting and might delay the reporting process for as long as 15 days. Another concern is that some studies used mobile devices for imputing people attendance changes in specific times and locations. The drawback was the characteristics of those persons using mobile devices such as age and gender were unknown. The data only tracked mobile devices but not persons, who might have multiple devices (eg, a phone and a tablet), or might not take their devices when they left home. Hence, the results might not reflect the actual mobility patterns. Finally, our review excluded non-English literature. The English literature of COVID-19 might be biased towards countries with good research capacity and interests in publishing their findings for an international audience.
Conclusions
Our review showed that the outcomes of social distancing measures were mainly measured by changes in Rt, incidence and mortality. There was empirical evidence for the effect of social distancing between individuals, and for partial or full lockdowns. However, the evidence was moderate for the separate effect of school closure and limited for workplace/business closures. There was no evidence for the separate effect of public transport restriction. In the community setting, there was more evidence for the combined effect of different social distancing interventions than for a single intervention. Apart from the effectiveness of the interventions, public compliance is another important issue. COVID-19 has been changing our lives and a new norm may emerge as we have to live with new variants of the virus, which may develop to a situation similar to that of the seasonal influenza, where a total elimination is not the goal. Fatigue of preventive behaviours is on the top of the public health agenda. Community compliance with social distancing measures is related to the population’s attitude to government policies, access/awareness of trustful sources of information, the initiations and maintenance of self-protective measures. Therefore, risk communication and risk analysis continue to be of cornerstone of public health measures and to address research gaps for implementing effective measures which are targeted and proportionate to the risk in different settings.
Supplementary Material
Acknowledgments
The Centre for Health Systems and Policy Research funded by The Tung Foundation is acknowledged for the support throughout the conduct of this study.
Footnotes
Contributors: EKY designed the study, applied for the grant and made major contributions to writing the manuscript. VCHC, EKY, KSS and CTH managed the review methodology. TSML, KSS and YSL conducted the review and data synthesis. TSML, KSS, EKY, CHKY and CTH wrote the first draft of the manuscript. All authors read, revised and approved the final manuscript. EKY is responsible for the overall content as guarantor.
Funding: This study was funded by Commissioned Research on the Novel Coronavirus Disease (Ref.: COVID190105) of the Health and Medical Research Fund, Food and Health Bureau, Hong Kong SAR Government.
Disclaimer: The funder had no role in the study design, collection, analysis, and interpretation of data, or in writing the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Ethical approval was obtained from the Survey and Behavioural Research Ethics Committee of the Chinese University of Hong Kong (Ref no. SBRE-19-595).
References
- 1.WHO . Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza. Geneva, 2019. [Google Scholar]
- 2.WHO . COVID-19: physical distancing, 2020. Available: https://www.who.int/westernpacific/emergencies/covid-19/information/physical-distancing
- 3.Chowdhury R, Luhar S, Khan N, et al. Long-term strategies to control COVID-19 in low and middle-income countries: an options overview of community-based, non-pharmacological interventions. Eur J Epidemiol 2020;35:743–8. 10.1007/s10654-020-00660-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lino DODC, Barreto R, Souza FDD, et al. Impact of lockdown on bed occupancy rate in a referral hospital during the COVID-19 pandemic in northeast Brazil. Brazilian Journal of Infectious Diseases 2020;24:466–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pépin JL, Bruno RM, Yang R-Y, et al. Wearable activity Trackers for monitoring adherence to home confinement during the COVID-19 pandemic worldwide: data aggregation and analysis. J Med Internet Res 2020;22:e19787. 10.2196/19787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Viner RM, Russell SJ, Croker H, et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health 2020;4:397–404. 10.1016/S2352-4642(20)30095-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chowdhury R, Heng K, Shawon MSR, et al. Dynamic interventions to control COVID-19 pandemic: a multivariate prediction modelling study comparing 16 worldwide countries. Eur J Epidemiol 2020;35:389–99. 10.1007/s10654-020-00649-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature 2020;585:410–3. 10.1038/s41586-020-2293-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev 2020;4:CD013574. 10.1002/14651858.CD013574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Islam N, Sharp SJ, Chowell G, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ 2020;370:m2743. 10.1136/bmj.m2743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.ECDC . Guidelines for non-pharmaceutical interventions to reduce the impact of COVID-19 in the EU/EEA and the UK. Stockholm, 2020. [Google Scholar]
- 12.Meyer J, Paré G, Impacts T. Telepathology impacts and implementation challenges: a scoping review. Arch Pathol Lab Med 2015;139:1550–7. 10.5858/arpa.2014-0606-RA [DOI] [PubMed] [Google Scholar]
- 13.Tricco AC, Zarin W, Rios P, et al. Engaging policy-makers, health system managers, and policy analysts in the knowledge synthesis process: a scoping review. Implement Sci 2018;13:31. 10.1186/s13012-018-0717-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lockwood C, Tricco AC. Preparing scoping reviews for publication using methodological guides and reporting standards. Nurs Health Sci 2020;22:1–4. 10.1111/nhs.12673 [DOI] [PubMed] [Google Scholar]
- 15.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 16.Chu DK, Akl EA, Duda S, et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet 2020;395:1973–87. 10.1016/S0140-6736(20)31142-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brauner JM, Mindermann S, Sharma M. The effectiveness of eight nonpharmaceutical interventions against COVID-19 in 41 countries. medRxiv 2020. [Google Scholar]
- 18.Weill JA, Stigler M, Deschenes O, et al. Social distancing responses to COVID-19 emergency declarations strongly differentiated by income. Proc Natl Acad Sci U S A 2020;117:19658–60. 10.1073/pnas.2009412117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubin D, Huang J, Fisher BT, et al. Association of social distancing, population density, and temperature with the instantaneous reproduction number of SARS-CoV-2 in counties across the United States. JAMA Netw Open 2020;3:e2016099. 10.1001/jamanetworkopen.2020.16099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clipman SJ, Wesolowski AP, Gibson DG, et al. Rapid real-time tracking of non-pharmaceutical interventions and their association with SARS-CoV-2 positivity: the COVID-19 pandemic pulse study. medRxiv 2020;02. 10.1101/2020.07.29.20164665. [Epub ahead of print: 11 Aug 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lemaitre JC, Perez-Saez J, Azman AS, et al. Assessing the impact of non-pharmaceutical interventions on SARS-CoV-2 transmission in Switzerland. Swiss Med Wkly 2020;150:w20295. 10.4414/smw.2020.20295 [DOI] [PubMed] [Google Scholar]
- 22.SAGE . The effectiveness and harms of non-pharmaceutical interventions 2020.
- 23.Rivkees SA, Roberson S. The Florida department of health steps public health approach: the COVID-19 response plan and outcomes through may 31, 2020. Public Health Rep 2020;135:560–4. 10.1177/0033354920946785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Auger KA, Shah SS, Richardson T, et al. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA 2020;324:859–70. 10.1001/jama.2020.14348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Siedner MJ, Harling G, Reynolds Z, et al. Social distancing to slow the US COVID-19 epidemic: longitudinal pretest-posttest comparison group study. PLoS Med 2020;17:e1003244. 10.1371/journal.pmed.1003244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Otte Im Kampe E, Lehfeld A-S, Buda S, et al. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.38.2001645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ehrhardt J, Ekinci A, Krehl H, et al. Transmission of SARS-CoV-2 in children aged 0 to 19 years in childcare facilities and schools after their reopening in May 2020, Baden-Württemberg, Germany. Euro Surveill 2020;25. 10.2807/1560-7917.ES.2020.25.36.2001587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macartney K, Quinn HE, Pillsbury AJ, et al. Transmission of SARS-CoV-2 in Australian educational settings: a prospective cohort study. Lancet Child Adolesc Health 2020;4:807–16. 10.1016/S2352-4642(20)30251-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Randhawa AK, Fisher LH, Greninger AL, et al. Changes in SARS-CoV-2 positivity rate in outpatients in Seattle and Washington state, March 1-April 16, 2020. JAMA 2020;323:2334–6. 10.1001/jama.2020.8097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wan H, Cui J-A, Yang G-J. Risk estimation and prediction of the transmission of coronavirus disease-2019 (COVID-19) in the mainland of China excluding Hubei Province. Infect Dis Poverty 2020;9:116. 10.1186/s40249-020-00683-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Du Z, Xu X, Wang L, et al. Effects of proactive social distancing on COVID-19 outbreaks in 58 cities, China. Emerg Infect Dis 2020;26. doi: 10.3201/eid2609.201932. [Epub ahead of print: 09 06 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang J, Litvinova M, Liang Y, et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2020;368:1481–6. 10.1126/science.abb8001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pan A, Liu L, Wang C, et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA 2020;323:1915–23. 10.1001/jama.2020.6130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lim JT, Dickens BSL, Choo ELW, et al. Revealing regional disparities in the transmission potential of SARS-CoV-2 from interventions in Southeast Asia. Proc Biol Sci 2020;287:20201173. 10.1098/rspb.2020.1173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marschner IC. Back-projection of COVID-19 diagnosis counts to assess infection incidence and control measures: analysis of Australian data. Epidemiol Infect 2020;148:e97. 10.1017/S0950268820001065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koh WC, Naing L, Wong J. Estimating the impact of physical distancing measures in containing COVID-19: an empirical analysis. Int J Infect Dis 2020;100:42–9. 10.1016/j.ijid.2020.08.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Courtemanche C, Garuccio J, Le A, et al. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff 2020;39:1237–46. 10.1377/hlthaff.2020.00608 [DOI] [PubMed] [Google Scholar]
- 38.Thu TPB, Ngoc PNH, Hai NM, et al. Effect of the social distancing measures on the spread of COVID-19 in 10 highly infected countries. Sci Total Environ 2020;742:140430. 10.1016/j.scitotenv.2020.140430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lam HY, Lam TS, Wong CH, et al. The epidemiology of COVID-19 cases and the successful containment strategy in Hong Kong-January to may 2020. Int J Infect Dis 2020;98:51–8. 10.1016/j.ijid.2020.06.057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cruz CHdeB. Social distancing in São Paulo state: demonstrating the reduction in cases using time series analysis of deaths due to COVID-19. Rev Bras Epidemiol 2020;23:e200056. 10.1590/1980-549720200056 [DOI] [PubMed] [Google Scholar]
- 41.Huynh TLD. Does culture matter social distancing under the COVID-19 pandemic? Saf Sci 2020;130:104872. 10.1016/j.ssci.2020.104872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Correia S, Luck S, Verner E. Pandemics depress the economy, public health interventions do not: evidence from the 1918 flu. SSRN Electronic Journal 2020;131. 10.2139/ssrn.3561560 [DOI] [Google Scholar]
- 43.Abel T, McQueen D. The COVID-19 pandemic calls for spatial distancing and social closeness: not for social distancing! Int J Public Health 2020;65:231. 10.1007/s00038-020-01366-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kim S-W, Su K-P,. Using psychoneuroimmunity against COVID-19. Brain Behav Immun 2020;87:4–5. 10.1016/j.bbi.2020.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Our World in Data . Coronavirus (COVID-19) vaccinations. Available: https://ourworldindata.org/covid-vaccinations
- 46.Castaneda-Babarro A, Coca A, Arbillaga-Etxarri A, et al. Physical activity change during COVID-19 confinement. International Journal of Environmental Research and Public Health 2020;17:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jarvis CI, Van Zandvoort K, Gimma A, et al. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med 2020;18:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jüni P, Rothenbühler M, Bobos P, et al. Impact of climate and public health interventions on the COVID-19 pandemic: a prospective cohort study. CMAJ 2020;192:E566–73. 10.1503/cmaj.200920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Khanna RC, Cicinelli MV, Gilbert SS, et al. COVID-19 pandemic: lessons learned and future directions. Indian J Ophthalmol 2020;68:703–10. 10.4103/ijo.IJO_843_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lai CKC, Ng RWY, Wong MCS, et al. Epidemiological characteristics of the first 100 cases of coronavirus disease 2019 (COVID-19) in Hong Kong special administrative region, China, a City with a stringent containment policy. Int J Epidemiol 2020;49:1096–105. 10.1093/ije/dyaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lasry A, Kidder D, Hast M, et al. Timing of community mitigation and changes in reported COVID-19 and community mobility - four U.S. metropolitan areas, February 26-April 1, 2020. MMWR Morb Mortal Wkly Rep 2020;69:451–7. 10.15585/mmwr.mm6915e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Munayco CV, Tariq A, Rothenberg R, et al. Early transmission dynamics of COVID-19 in a southern hemisphere setting: Lima-Peru: February 29th-March 30th, 2020. Infect Dis Model 2020;5:338–45. 10.1016/j.idm.2020.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Patel P, Athotra A, Vaisakh TP, et al. Impact of nonpharmacological interventions on COVID-19 transmission dynamics in India. Indian J Public Health 2020;64:S142–6. 10.4103/ijph.IJPH_510_20 [DOI] [PubMed] [Google Scholar]
- 54.Saez M, Tobias A, Varga D, et al. Effectiveness of the measures to flatten the epidemic curve of COVID-19. The case of Spain. Sci Total Environ 2020;727:138761. 10.1016/j.scitotenv.2020.138761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vokó Z, Pitter JG. The effect of social distance measures on COVID-19 epidemics in Europe: an interrupted time series analysis. Geroscience 2020;42:1075–82. 10.1007/s11357-020-00205-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wilasang C, Sararat C, Jitsuk NC, et al. Reduction in effective reproduction number of COVID-19 is higher in countries employing active case detection with prompt isolation. J Travel Med 2020;27:taaa095. 10.1093/jtm/taaa095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yehya N, Venkataramani A, Harhay MO. Statewide interventions and coronavirus disease 2019 mortality in the United States: an observational study. Clin Infect Dis 2021;73:e1863–9. 10.1093/cid/ciaa923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang R, Li Y, Zhang AL, et al. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci U S A 2020;117:14857–63. 10.1073/pnas.2009637117 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-053938supp001.pdf (28.6KB, pdf)
Data Availability Statement
Data are available on reasonable request. The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.