Abstract
Emotional eating (EE) is food consumption in response to feelings rather than hunger. EE is related to unhealthy food intake and abdominal obesity (AO). However, little evidence exists about the association between EE and dietary patterns (DPs) and EE–AO interaction related to DPs. DPs allow describing food combinations that people usually eat. We analyzed the association of EE with DPs in adults (≥18 years) with AO (WC ≥ 80/90 cm in women/men, respectively; n = 494; 66.8% women;) or without AO (n = 269; 74.2% women) in a cross-sectional study. Principal component analysis allowed identifying four DPs from 40 food groups (validated with a semiquantitative food frequency questionnaire). Among the subjects presenting AO, being “emotional/very-emotional eater” (emotional eating questionnaire) was negatively associated with the “Healthy” DP (fruits, vegetables, olive oil, oilseeds, legumes, fish, seafood) (OR:0.53; 95% CI: 0.33, 0.88, p = 0.013) and positively with the “Snacks and fast food” DP (sweet bread, breakfast cereal, corn, potato, desserts, sweets, sugar, fast food) (OR:1.88; 95% CI: 1.17, 3.03, p = 0.010). Emotional eaters with AO have significantly lower fiber intake, folic acid, magnesium, potassium, vitamin B1, and vitamin C, while they had a higher intake of sodium, lipids, mono and polyunsaturated fatty acids, and saturated fats. In non-AO participants, EE was not associated with any DP (p > 0.05). In conclusion, EE is associated with unhealthy DPs in subjects with AO.
Keywords: emotional eating, dietary patterns, abdominal obesity, eating style, eating behavior
1. Introduction
Environmental and individual determinants influence food consumption [1,2]. Personal aspects include emotions, which can influence food intake [1,2,3,4]. Negative emotions produce a series of physiological reactions that naturally promote a lack of appetite or decreased food intake [3,5]. However, some people increase their food intake in response to negative emotions such as emotional stress, anxiety, frustration, sadness, anger, and loneliness [3]. This situation is known as “emotional eating” [3,5,6]. It has been evidenced that, on average, 30% of people increase and 48% decrease their appetite or food intake when facing a negative emotion, such as emotional stress [3].
Several studies have assessed the association of emotional eating with energy and macronutrient intake or particular food choices [3,7,8,9,10,11,12,13,14]. Emotional eating has been associated with fast food intake [10,12], salty snacks [9,10], sweet high-fat foods [3,7], or energy-dense foods [9] such as cakes, biscuits, pastries [7,8], ice cream, chocolate and its products, breakfast cereals [7], candies [11], and artificially sweetened beverages [7,9,11]. Furthermore, emotional eating has been positively associated with waist circumference (WC) [15,16], abdominal obesity (AO) by WC [17,18], body mass index (BMI) [15,16,19,20], obesity by BMI [6,12,17], obesity by percent body fat [18], bodyweight gain [6,21], and weight loss impairments [21]. Moreover, emotional eating has been shown to interact with the physiological and genetic characteristics of the individual for body weight loss effectiveness [22,23]. In addition, obesity and AO are more frequent among those subjects classified as emotional eaters than non-emotional ones [17].
Despite this relatively large number of studies, few studies have analyzed the potential association between emotional eating and specific dietary patterns (DPs) [15,24,25,26]. Only one study evaluated the interaction between emotional eating and obesity/abdominal obesity with specific DPs, with non-significant results [15]. Assessing DPs is interesting because it allows for the description of the complete diet, i.e., the food combinations people usually eat [27]. This diet description is close to reality since people do not typically consume individual foods or nutrients. On the other hand, considering that emotional eating is a risk factor for developing obesity [6,12,15,16,17,18,19,20], the interest arises to analyze whether emotional eating is associated with specific DPs in people with and without obesity.
While BMI is widely used as an index of obesity, it does not differentiate between body lean mass and body fat mass and does not reflect the location of body fat [28]. Instead, WC is an indicator of abdominal fat that has been associated with increased cardiometabolic risk [29,30]. Therefore, considering the advantage of measuring AO with WC vs. BMI, we analyzed if emotional eating relates to the DPs in people with and without AO.
Identifying the different DPs in people with and without AO and looking for potential connections with emotional eating is essential in designing strategies to improve adherence to a healthy DP and prevent and treat AO. We aimed to analyze the association of emotional eating with various DPs in adults with and without AO.
2. Materials and Methods
2.1. Characteristics of the Participants
The present article is part of the macro project entitled “Association of Diet Quality Index, emotions and chronotype with Body Mass Index in workers of the University of Guadalajara (CADICEM)” within this university’s “Organizational Health Program” framework. The University of Guadalajara has 15 University Centers spread throughout the state of Jalisco (78 thousand km2), Mexico: of those, 14 participated in this macro project. The university also has a virtual university system and a high school system: both were also asked to join at the end of 2019. The participants’ selection was non-random; all the workers were verbally invited during a visit to their workplace. This macro project included volunteers, men or women over 18 years of age, among workers of this public university in Mexico. Pregnant women were not involved in the study.
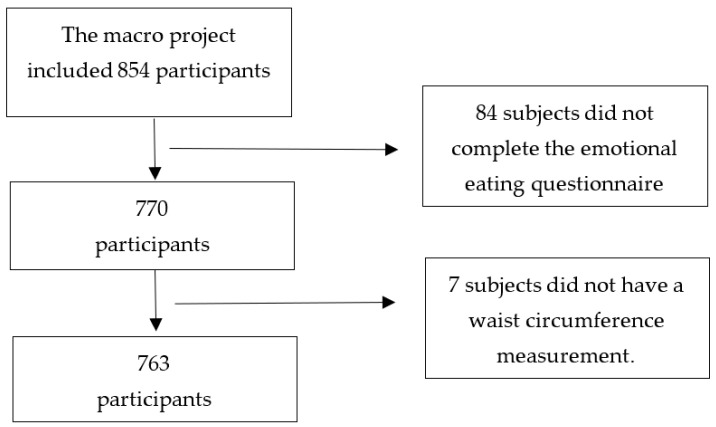
For the present study, all participants of the macro project with WC determination and who reported sociodemographic, dietary, and emotional eating characteristics were included. The variables analyzed for this study are described below. In this sense, the macro project had 854 participants; however, for the present study, we eliminated 84 subjects because they did not complete the emotional eating questionnaire, and 7 participants did not have their WC measurement. The 91 people excluded were female (64.8%), older than 31 years (71.4%), administrative workers (64.4%), sedentary (71.4%), and having AO (65.1%) (in those who had their WC measurement). The present study included 763 participants (Figure 1).
Figure 1.
Flow chart.
This project was approved by the Research Ethics, Research and Biosafety Committees of the Centro Universitario de Ciencias de la Salud, Universidad de Guadalajara (CI-02719) and was performed according to the last version of the Declaration of Helsinki [31]. After opening a dialogue to clarify doubts regarding their participation, all participants voluntarily signed an informed consent letter.
2.2. Sociodemographic Characteristics
Participants were asked about their age, sex, occupation (academic, managerial, operative, administrative) and perception of physical activity (sedentary, active, or very active) by employing an interview. Additionally, we recorded the University Center to which they were attached.
2.3. Anthropometric Measurements
Bodyweight (Tanita® BC-568 electric scale, precision 0.1 kg) and height (portable stadiometer Seca 213®, precision 0.1 cm) were measured by a nutritionist to calculate the BMI. Waist circumference was measured (fiberglass tape measure) at the midpoint between the edge of the lower costal (tenth rib) and the iliac crest, after one exhalation, following normal breathing [32]. Individuals were classified using WC into AO (≥80 cm in women and ≥90 cm in men) and non-AO groups (<80 cm in women and <90 cm in men) according to the specific cut-off points for the Central and South American population proposed by Alberti et al., 2009 [33].
2.4. Emotional Eating
Participants completed the self-reported emotional eating questionnaire (EEQ), validated in Spain in adults with obesity [34] and in university students with and without obesity [35]. This questionnaire contains ten questions, with four response options that have a specific score: never (0 points), sometimes (1 point), usually (2 points), and always (3 points). The total score (sum of each question score) allows the participants to be classified as non-emotional eaters (0–5 points), low emotional eaters (6 to 10 points), and emotional or very emotional eaters (11 to 30 points). For the current study, the EEQ was analyzed by academics and graduate students. They perceived it was adequately understood and did not find words not recognized in the Mexican lexicon. Therefore, we decided to apply it without any changes. We evaluated its reliability (internal consistency). Cronbach’s alpha for the entire instrument was 0.838 when including all participants, 0.851 when including only participants with AO, and 0.761 when including participants with non-AO. These Cronbach’s alpha values are interpreted as satisfactory [36].
2.5. Dietary Intake
A semiquantitative food frequency questionnaire (SFFQ) of 162 items, previously validated in the Mexican population, was used [37]. A trained nutritionist team applied it by interview, using a validated Mexican photo album as visual support [38]. Participants mentioned each food item’s frequency and regular consumption in the year before the survey. From this information, the nutritionist recorded the number of servings consumed of each food (each item has a standard serving), choosing from nine possible response options ranging from never or seldom to more than six servings per day.
From the number of servings consumed and the standard portion of each item, we calculated each participant’s daily nutrition intake of the 162 items. The daily intake of all items was then grouped into 40 food groups (Table 1) according to their nutritional characteristics (carbohydrate, protein, lipid, sugar, fiber, and alcohol content) and preparation (industrialized or home-prepared foods). Some foods were not grouped and formed a food group by themselves.
Table 1.
Description of the food groups.
| Food Group | Foods Considered in the Group |
|---|---|
| 1. Fish and Seafood | Oysters, squid, crustaceans, white fish, bluefish, salted fish, canned tuna (in oil or water), canned prepared tuna. |
| 2. Meat | Beef, pork, pork rinds, lamb, offal, and liver. |
| 3. Chicken | Chicken with and without skin. |
| 4. Egg | Egg. |
| 5. Semimature cheeses | Manchego, Gouda, Oaxaca and mozzarella cheeses. |
| 6. Fresh cheeses | Requesón (curd), cottage cheese, panela cheese, adobera cheese. |
| 7. Whole milk and yogurt | Whole milk, evaporated milk, Petit, whole yogurt, and smoothies. |
| 8. Skimmed milk | Skimmed milk. |
| 9. Processed meats | Ham and processed meats. |
| 10. Fast food | Hamburger, industrialized French fries, popcorn, sachet soups. |
| 11. Industrialized sauces and dressings | Mustard, hot sauce, ketchup, mayonnaise. |
| 12. Breakfast cereals | Breakfast cereals. |
| 13. Industrialized bakery | María type cookies, chocolate cookies, industrialized bread, vegetable shortening, and margarine. |
| 14. Sweets, sugar, and honey | Honey, jam, candies, fruit in syrup, ate (quince paste), cajeta (caramel sauce), condensed milk, sugar, and piloncillo (brown sugar). |
| 15. Desserts | Custard, chocolate, cocoa, ice cream. |
| 16. Industrialized sweetened beverages | Light soda, regular soda, canned juices, fermented-milk beverages (e.g., Yakult). |
| 17. Alcoholic beverages | Distilled spirits, liquor, beer, white wine, rosé wine, young red wine, and aged red wine. |
| 18. Oils (various) | Corn oil, soybean oil, sunflower oil, mixed oils, canola oil, safflower oil. |
| 19. Olive oil | Extra-virgin olive oil, olive oil, olives. |
| 20. Animal fats | Bacon, lard, cream, cream cheese, and butter. |
| 21. Corn products | Corn dough, corn tortilla, and toast. |
| 22. Pasta | Pasta: noodle, spaghetti, macaroni. |
| 23. Rice | Rice. |
| 24. White bread | Bolillo, white bread, and buns. |
| 25. Whole grain cereals | Whole grain cereals (oatmeal, granola), whole grain crackers, whole wheat bread. |
| 26. Non-industrialized sweet bread | Sweetbread, cake, homemade bread, mantecada (shortbread), doughnut, churro. |
| 27. Flour tortilla | Flour tortilla. |
| 28. Vegetables frequently consumed in Mexico | Onion, garlic, tomato, chili, bell pepper, poblano chili, lemon |
| 29. Vegetables | Green bean, cabbage, chard, asparagus, herbs, other vegetables, eggplant, chayote (squash) and jicama (yam bean), carrot and pumpkin flower, lettuce, peas, mushrooms, and nopales (prickly pear leaf). |
| 30. Fruits | Orange, kiwi, guava, lime, mango, pineapple, strawberry, plum, prune, tuna (prickly pear fruit), grape, peach, watermelon, melon, papaya, apple, raisins, tamarind, banana, dates, prune, natural fruit juices. |
| 31. Avocado | Avocado. |
| 32. Elote | Fresh corn. |
| 33. Potatoes | Potatoes prepared homemade. |
| 34. Nuts | Almonds, walnuts, and peanuts. |
| 35. Beans | Frijoles and alubias (beans and white beans). |
| 36. Leguminous plants | Lentils and chickpeas. |
| 37. Tea | Tea. |
| 38. Coffee | Coffee. |
| 39. Natural water | Natural water. |
| 40. Salt | Salt added. |
Some foods are written in italics because we used their Mexican Spanish name.
The responses recorded in the SFFQ were captured in the Nutricloud® software (https://www.nutricloud.mx/, accessed on 17 February 2022, software as a service, Guadalajara, Mexico) to determine energy and nutrient intake data. This software included Mexican food composition data [39] and the USDA [40].
2.6. Statistical Analysis
Qualitative variables were expressed as frequency and percentage, while quantitative variables were expressed as mean and standard deviation. We analyzed the association between qualitative variables with the Chi2 test. Student’s t-test was used to compare quantitative variables between those subjects with and without AO. We compared quantitative variables among the three groups of emotional eaters (non-emotional eaters, low emotional eaters, and emotional/very emotional eaters) with one-factor ANOVA and ANCOVA adjusted by energy intake. Bonferroni’s post hoc statistical tests were carried out between the groups of non-emotional with emotional/very emotional eaters, when they achieved significant differences. Those variables with non-normal distribution were log-transformed. However, the mean values are shown in the original variables.
We generated DPs using principal component analysis (PCA) from the 40 food groups in the total sample. Before performing this statistical approach, Kaiser-Meyer-Olkin analysis and Bartlett’s sphericity test were performed to define the feasibility of multivariate analysis with these variables. We interpreted the results of the Kaiser-Meyer-Olkin analysis (0.70) and the Bartlet sphericity test (p < 0.001) as acceptable; therefore, it was feasible to perform the multivariate analysis [41,42]. The first four components were selected and named “Snacks and fast food,” “Traditional Westernized”, “Healthy,” and “Animal products and cereals” (Supplementary Figure S1 and Supplementary Table S1). The number of DPs was defined with the help of the scree plot test [41,42,43]. We applied a Varimax rotation analysis to improve factor loadings interpretation and obtain uncorrelated components [41,42]. As part of a DP, a factor loading between each food group, equal or greater than 0.3 (positive or negative), was considered significant [43] and maintained in the model. When the factor loadings were between 0.25 to 0.3 (positive or negative), the food groups remained in the model because they were considered relevant in the conformation of the DP. If a food group had a factor loading ≥0.3 in more than one DP, this food group was considered part of more than one DP. Food groups that presented low factor loadings (≤0.25) in the four DP were eliminated from the PCA. For this reason, the PCA performed in the total sample did not include coffee, natural water, and skim milk.
We calculated the potential interaction between emotional eating and obesity (classified by BMI) with the four DPs identified, adjusted by WC, but no significant interaction was observed. Nevertheless, a significant interaction was observed between emotional eating and AO with the “Healthy” DP (p = 0.046), adjusted by BMI. Thus, we decided to generate DPs in participants with and without AO following the abovementioned process.
The results of the Kaiser-Meyer-Olkin analysis (0.67 in participants with non-AO, and 0.75 in participants with AO) and the Bartlet sphericity test (p < 0.001) were interpreted as acceptable [41,42]. The first four components were selected. The DPs in non-AO participants did not contain salt or skim milk, and the DPs in those with AO did not include natural water or coffee. Because these food groups presented low factor loadings (≤0.25) in the four DPs, we eliminated them from the PCA.
The factor scores for each DP were divided into two categories (50th percentile). The lower half (lower score) was interpreted as non-adherence to the DP, and the upper half (higher score) was interpreted as adherence to the DP. All the participants had a score in each of the DPs; hence, each subject could score high in more than one DP. We assessed the association of DPs (dependent variable) with the emotional eater classification (independent variable) with multivariate logistic regression analyses, adjusted for age, BMI, sex, energy intake, and physical activity. These associations were performed according to whether AO or non-AO was present. A value of p ≤ 0.05 was considered significant. We developed all analyses with IBM SPSS Statistics for Windows, version 28 (IBM Corp., Armonk, NY, USA).
3. Results
3.1. General Characteristics of the Participants
The present study included 494 participants with AO (64.7%) and 269 without AO (35.3%). Their characteristics are shown in Table 2. Compared to those with non-AO, those with AO were emotional or very emotional eaters in a higher frequency, were older, presented higher BMI, and were more sedentary (Table 2). Emotional eaters in the AO group had a higher BMI and were more sedentary than non-emotional eaters. Furthermore, within the AO and non-AO groups, a higher proportion of women were among the emotional or very emotional eaters (Table 2). We found no significant differences in the occupation between AO and non-AO subjects or across the different emotional eater categories.
Table 2.
Characteristics of the participants with and without abdominal obesity and according to the emotional eating classification.
| Total | Abdominal Obesity | Non-Abdominal Obesity | Abdominal Obesity | Non-Abdominal Obesity | |||||
|---|---|---|---|---|---|---|---|---|---|
| Non-EE | Low EE | EE or Very EE | Non-EE | Low-EE | EE or Very EE | ||||
| N (%) | 763 | 494 (64.7) | 269 (35.3) | 153 (31.0) | 159 (32.2) | 182 (36.8) *** | 114 (42.4) | 95 (35.3) | 60 (22.3) |
| Age (years) | 38 ± 11 | 40 ± 11 *** | 34 ± 9 | 42 ± 11 | 41 ± 11 | 38 ± 11 ●** | 36 ± 10 | 33 ± 9 | 32 ± 6 ●** |
| BMI (kg/m2) | 27.3 ± 5.2 | 29.8 ± 4.6 *** | 22.8 ± 2.4 | 28.7 ± 3.6 | 29.7 ± 4.4 | 30.8 ± 5.2 ●*** | 22.4 ± 2.5 | 23.1 ± 2.4 | 23.1 ± 2.2 |
| WC (cm) | 88.2 ± 13.4 | 95.1 ± 11 *** | 75.5 ± 6.1 | 94.4 ± 9.7 | 95.5 ± 11.5 | 95.4 ± 11.5 | 76 ± 6.5 | 75.6 ± 6.2 | 74.4 ± 4.7 |
| Sex | |||||||||
| Female | 530 (69.5) | 330 (66.8) * | 200 (74.3) | 85 (55.6) | 102 (64.2) | 143 (78.6) *** | 78 (68.4) | 68 (71.6) | 54 (90.0) ** |
| Occupation | |||||||||
| Academic | 74 (9.8) | 45 (9.3) | 29 (10.9) | 14 (9.3) | 14 (8.9) | 17 (9.6) | 10 (8.9) | 14 (14.9) | 5 (8.3) + |
| Managerial | 54 (7.2) | 35 (7.2) | 19 (7.1) | 15 (9.9) | 10 (6.4) | 10 (5.6) | 7 (6.3) | 8 (8.5) | 4 (6.7) |
| Administrative | 546 (72.6) | 348 (71.6) | 198 (74.4) | 97 (64.2) | 118 (75.2) | 133 (74.7) | 85 (75.9) | 65 (69.1) | 48 (80.0) |
| Operative | 37 (4.9) | 31 (6.4) | 6 (2.3) | 12 (7.9) | 8 (5.1) | 11 (6.2) | 3 (2.7) | 3 (3.2) | 0 (0) |
| Academic and other | 41 (5.5) | 27 (5.6) | 14 (5.3) | 13 (8.6) | 7 (4.5) | 7 (3.9) | 7 (6.3) | 4 (4.3) | 3 (5.0) |
| Physical activity | |||||||||
| Sedentary | 519 (68) | 353 (71.5) *** | 166 (61.7) | 104 (68.0) | 108 (67.9) | 141 (77.5) * | 67 (58.8) | 59 (62.1) | 40 (66.7) |
| Active | 151 (19.8) | 96 (19.4) | 55 (20.4) | 31 (20.3) | 33 (20.8) | 32 (17.6) | 26 (22.8) | 19 (20.0) | 10 (16.7) |
| Very active | 93 (12.2) | 45 (9.1) | 48 (17.8) | 18 (11.8) | 18 (11.3) | 9 (4.9) | 21 (18.4) | 17 (17.9) | 10 (16.7) |
EE: Emotional Eater; BMI: Body Mass Index; WC: Waist circumference. Other: administrative, managerial, operational. Data are presented as mean ± standard deviation and n (%). Differences between those with abdominal obesity and non-abdominal obesity were calculated by Student’s t-test. Differences between the three emotional eater categories were calculated by one-factor ANOVA. p < 0.05 was considered significant. * p < 0.05; ** p < 0.01; *** p < 0.001. Differences between the non-emotional eaters vs. emotional or very emotional eaters were calculated with Bonferroni’s post hoc statistical test, ● p < 0.05. Relationship between qualitative variables was evaluated with the Chi2 statistical test. + Not applicable Chi2 test, 40% have an expected frequency less than 5.
3.2. Description of the Dietary Patterns in Participants with and without Abdominal Obesity
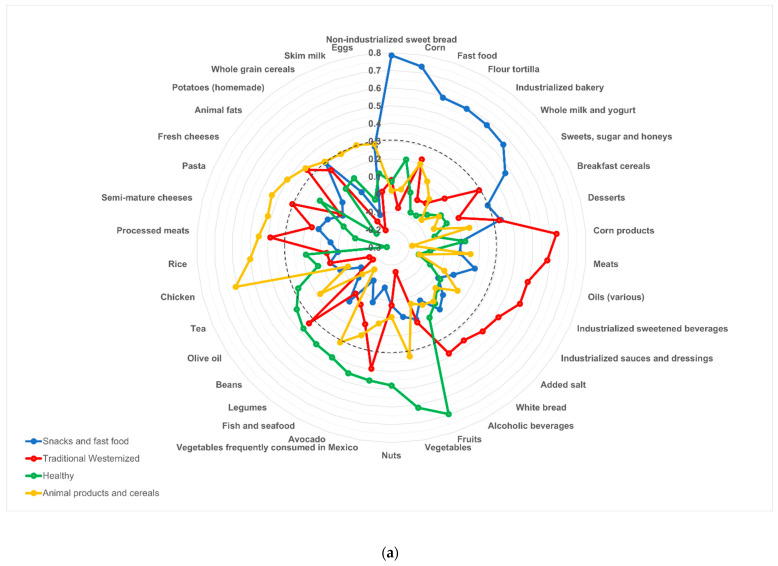
Figure 2 shows the four DPs identified in those with and without AO. In those who presented AO, the first DP, which explained the most significant percentage of the variance (12.5% of the total variance, Supplementary Table S1), was named “Snacks and fast food” because it was made up of non-industrialized sweet bread (with factor load of 0.785) followed by corn, fast food, flour tortilla, industrialized bakery, sweets and sugar, whole milk and yogurt, desserts, potato, and breakfast cereals. The second DP (7.06% of the total variance, Supplementary Table S1) was named “Traditional Westernized” because it was made up of food groups traditionally consumed in Mexico (corn products like tortilla, meat, oil, vegetables frequently consumed in Mexico, alcoholic beverages, white bread, animal fat, and beans), together with foods characteristic of western culture (industrialized sweetened beverages, industrialized sauces and dressings, added salt, processed meats, desserts, and pasta). The third DP (5.71% of the total variance, Supplementary Table S1) was named “Healthy” because it consisted of the following food groups: fruits (with factor load of 0.69) followed by vegetables, nuts, avocado, fish and seafood, legumes, beans, olive oil, and tea. Finally, the fourth DP (4.39% of the total variance, Supplementary Table S1) was named “Animal products and cereals” because it consisted of chicken (with factor load of 0.6) followed by rice, pasta, semimature cheeses, fresh cheeses, whole grain cereals, skim milk, and eggs (Figure 2a).
Figure 2.
Dietary patterns drawn from participants with and without abdominal obesity. This figure shows the dietary patterns (DPs) identified in participants with abdominal obesity (a), and those without abdominal obesity (b). The numbers expressed are the factor loads obtained by principal component analysis. DPs are only made up of food groups with a factor load equal to or greater than 0.3 or close to 0.3 (positive or negative). The dotted line indicates the factorial load equal to 0.3 to improve the interpretation of the graph. If a food group had a factor loading ≥0.3 on more than one DP, this food group was considered part of more than one DP. The food groups that make up the DP named “Traditional Westernized” are in red. The food groups that make up the DP named “Animal products and cereals” or “Animal products, cereals, and vegetables” are drawn in yellow. The green color shows the food groups that make up the DP named “Healthy”, and the blue color shows the food groups that make up the DP named “Snacks and fast food” or “Snacks” in the abdominal obesity group and the non-abdominal obesity, respectively.
In non-AO subjects, the first DP, which explained the most significant percentage of the variance (11.13%, Supplementary Table S1), was the “Traditional Westernized” DP. This pattern received this name (similar to the one for subjects with AO) because it was made up of food typical of the Mexican food culture (white bread, animal fat, beans, non-industrialized sweet bread, flour tortillas, oils, alcoholic beverages, and corn products), in combination with foods from the western culture (industrialized sauces and dressings, fast food, semimature cheeses, industrialized sweetened beverages, processed meats, pasta, whole milk, and yogurt). The second DP (8.53% of the total variance, Supplementary Table S1) included animal products (eggs, fish and seafood, fresh cheeses, chicken, meat), cereals (rice, whole grains), and vegetables (vegetables, avocado). Therefore, this DP was named “Animal products, cereals, and vegetables.” The third DP (5.75% of the total variance, Supplementary Table S1) was also called “Healthy” because it included vegetables, olive oil, tea, nuts, fish and seafood, legumes, and fruits with low whole milk and yogurt intake. Finally, the “Snacks” DP (4.82% of the total variance, Supplementary Table S1) included desserts, sweets and sugar, breakfast cereals, corn, fruits, potatoes, and industrialized bakery products with a low intake of natural water and coffee (Figure 2b).
Supplementary Table S1 shows the factorial loads of the food groups in each DP and the percentage of the total variance of each DP. Supplementary Tables S2 and S3 show energy and nutrient intake according to adherence to DPs in participants with and without AO, respectively.
Participants with/without AO (Table 3) who adhered to any DP consumed significantly more energy than the non-adherent ones. Similarly, those who stuck to the “Traditional Westernized” DP were characterized mainly as men. Among those who presented AO (Table 3), participants who adhered to the “Snacks and fast food” DP and “Animal products and cereals” DP were younger than those who did not adhere to these DPs. Mainly, those who adhered to the “Healthy” DP were older and more “active or very active” than those who did not comply with this DP. Notably, among subjects without AO (Table 3), those who adhered to the “Traditional Westernized” DP were younger than those who did not adhere to this DP. Likewise, those who stuck to the “Animal products, cereals, and vegetables” DP were characterized by being “very active” regarding physical activity, compared to those non-adherents.
Table 3.
Participant characteristics between subjects who adhere or do not adhere to each dietary pattern in participants with or without obesity.
| Abdominal Obesity (n = 494) | ||||||||
| Snacks and Fast Food | Traditional Westernized | Healthy | Animal Products and Cereals | |||||
| No Adherence | Adherence | No Adherence | Adherence | No Adherence | Adherence | No Adherence | Adherence | |
| Age (years) | 42 ± 11 | 38 ± 10 *** | 40 ± 11 | 40 ± 11 | 37 ± 10 | 43 ± 12 *** | 42 ± 11 | 39 ± 11 ** |
| BMI (kg/m2) | 29.7 ± 4.3 | 29.9 ± 4.9 | 29.3 ± 4.3 | 30.3 ± 4.8 * | 29.9 ± 4.8 | 29.8 ± 4.3 | 29.5 ± 4.4 | 30.1 ± 4.7 |
| WC (cm) | 94.9 ± 10.6 | 95.4 ± 11.3 | 92.9 ± 10.2 | 97.4 ± 11.2 *** | 94.7 ± 11.3 | 95.6 ± 10.7 | 95.0 ± 11.3 | 95.3 ± 10.7 |
| Energy intake | 2058 ± 758 | 2616 ± 1097 *** | 1920 ± 801 | 2754 ± 971 *** | 2104 ± 770 | 2571 ± 1110 *** | 2185 ± 954 | 2490 ± 989 *** |
| Sex | ||||||||
| Female | 163 (49.4) | 167 (50.6) | 192 (58.2) | 138 (41.8) *** | 165 (50.0) | 165 (50.0) | 163 (49.4) | 167 (50.6) |
| Male | 84 (51.2) | 80 (48.8) | 55 (33.5) | 109 (66.5) | 82 (50.0) | 82 (50.0) | 84 (51.2) | 80 (48.8) |
| Occupation | ||||||||
| Academic | 26 (57.8) | 19 (42.2) * | 22 (48.9) | 23 (51.1) | 22 (48.9) | 23 (51.1) | 23 (51.1) | 22 (48.9) |
| Managerial | 24 (68.6) | 11 (31.4) | 18 (51.4) | 17 (48.6) | 15 (42.9) | 20 (57.1) | 18 (51.4) | 17 (48.6) |
| Administrative | 163 (46.8) | 185 (53.2) | 183 (52.6) | 165 (47.4) | 177 (50.9) | 171 (49.1) | 177 (50.9) | 171 (49.1) |
| Operative | 13 (41.9) | 18 (58.1) | 8 (25.8) | 23 (74.2) | 15 (48.4) | 16 (51.6) | 17 (54.8) | 14 (45.2) |
| Academic and other | 17 (63.0) | 10 (37.0) | 12 (44.4) | 15 (55.6) | 16 (59.3) | 11 (40.7) | 10 (37.0) | 17 (63.0) |
| Physical activity | ||||||||
| Sedentary | 174 (49.3) | 179 (50.7) | 160 (45.3) | 193 (54.7) *** | 192 (54.4) | 161 (45.6) ** | 168 (47.6) | 185 (52.4) * |
| Active | 51 (53.1) | 45 (46.9) | 65 (67.7) | 31 (32.3) | 38 (39.6) | 58 (60.4) | 59 (61.5) | 37 (38.5) |
| Very active | 22 (48.9) | 23 (51.1) | 22 (48.9) | 23 (51.1) | 17 (37.8) | 28 (62.2) | 20 (44.4) | 25 (55.6) |
| Non-Abdominal Obesity (n = 269) | ||||||||
| Traditional Westernized | Animal Products, Cereals, and Vegetables | Healthy | Snacks | |||||
| No Adherence | Adherence | No Adherence | Adherence | No Adherence | Adherence | No Adherence | Adherence | |
| Age (years) | 36 ± 9 | 32 ± 8 *** | 34 ± 8 | 34 ± 10 | 34 ± 9 | 34 ± 9 | 34 ± 9 | 34 ± 9 |
| BMI (kg/m2) | 23.1 ± 2.4 | 22.5 ± 2.4 | 22.7 ± 2.4 | 22.9 ± 2.4 | 23.0 ± 2.5 | 22.7 ± 2.3 | 22.9 ± 2.4 | 22.7 ± 2.4 |
| WC (cm) | 75.1 ± 5.9 | 75.9 ± 6.2 | 75.6 ± 6.2 | 75.4 ± 5.9 | 76.0 ± 6.0 | 75.0 ± 6.1 | 75.9 ± 6.1 | 75.1 ± 6.0 |
| Energy intake | 1951 ± 647 | 2744 ± 848 *** | 2050 ± 786 | 2650 ± 811 *** | 2192 ± 801 | 2507 ± 875 *** | 2126 ± 819 | 2574 ± 827 *** |
| Sex | ||||||||
| Female | 112 (56.0) | 88 (44.0) *** | 105 (52.5) | 95 (47.5) | 99 (49.5) | 101 (50.5) | 97 (48.5) | 103 (51.5) |
| Male | 22 (31.9) | 47 (68.1) | 30 (43.5) | 39 (56.5) | 36 (52.2) | 33 (47.8) | 38 (55.1) | 31 (44.9) |
| Occupation | ||||||||
| Academic | 16 (55.2) | 13 (44.8) * | 15 (51.7) | 14 (48.3) | 14 (48.3) | 15 (51.7) | 17 (58.6) | 12 (41.4) ** |
| Managerial | 9 (47.4) | 10 (52.6) | 9 (47.4) | 10 (52.6) | 9 (47.4) | 10 (52.6) | 3 (15.8) | 16 (84.2) |
| Administrative | 95 (48.0) | 103 (52.0) | 100 (50.5) | 98 (49.5) | 101 (51.0) | 97 (49.0) | 99 (50.0) | 99 (50.0) |
| Operative | 1 (16.7) | 5 (83.3) | 3 (50.0) | 3 (50.0) | 2 (33.3) | 4 (66.7) | 3 (50.0) | 3 (50.0) |
| Academic and other | 12 (85.7) | 2 (14.3) | 5 (35.7) | 9 (64.3) | 8 (57.1) | 6 (42.9) | 11 (78.6) | 3 (21.4) |
| Physical activity | ||||||||
| Sedentary | 80 (48.2) | 86 (51.8) | 92 (55.4) | 74 (44.6) * | 88 (53.0) | 78 (47.0) | 80 (48.2) | 86 (51.8) |
| Active | 32 (58.2) | 23 (41.8) | 26 (47.3) | 29 (52.7) | 28 (50.9) | 27 (49.1) | 27 (49.1) | 28 (50.9) |
| Very active | 22 (45.8) | 26 (54.2) | 17 (35.4) | 31 (64.6) | 19 (39.6) | 29 (60.4) | 28 (58.3) | 20 (41.7) |
BMI: Body Mass Index; WC: Waist circumference. Other: administrative, managerial, operational. Data are presented as mean ± standard deviation and n (%). Differences in participant characteristics (those who adhere vs. those who do not adhere to each dietary pattern) were calculated by Student’s t-test. We calculated the log of energy for the statistical analysis; however, in the table, we show the original value of this variable. p < 0.05 was considered significant. * p < 0.05; ** p < 0.01; *** p < 0.001.
3.3. Adherence to Dietary Patterns According to the Emotional Eating Classification in Participants with and without Abdominal Obesity
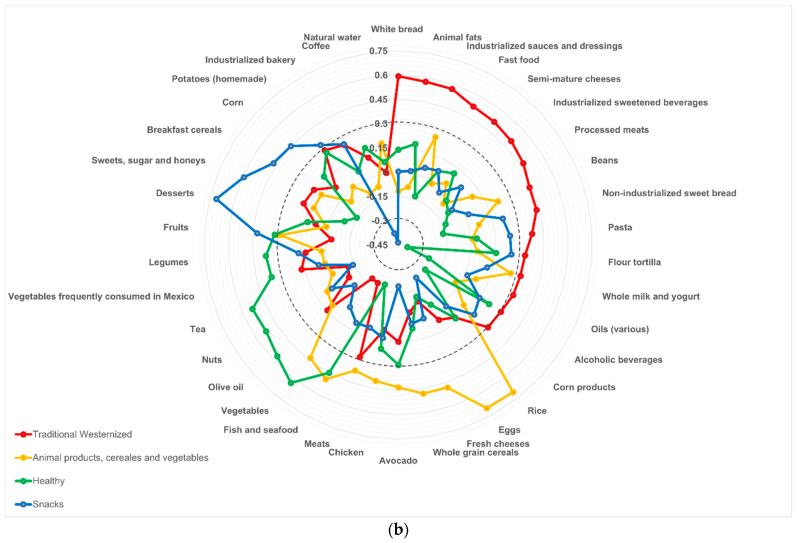
Importantly, subjects with AO who were emotional or very emotional eaters adhered more to the “Snacks and fast food” DP (p = 0.007) and less to the “Healthy” DP (p = 0.008) than those who were non-emotional or low emotional eaters (Figure 3a). In subjects with non-AO, significant differences were not found (Figure 3b).
Figure 3.
Adherence to dietary patterns according to the emotional eating classification in participants with and without abdominal obesity. This figure shows the adherence to dietary patterns according to the emotional eating classification in participants (a) with abdominal obesity or (b) without abdominal obesity. The emotional eating classification is presented in three categories: light gray for the non-emotional eaters, medium gray for the low emotional eaters, and dark gray for the emotional or very emotional eaters. The percentages expressed the proportion of subjects in the respective emotional category who adhered to each dietary pattern. It is important to notice that all subjects in a group (with abdominal obesity or without abdominal obesity) adhered or not to the four dietary patterns. * p < 0.05.
3.4. Association between Dietary Patterns and Emotional Eating Classification
After adjustment by age, sex, energy intake, physical activity, and BMI, in subjects with AO, being an emotional or very emotional eater (independent variable) was negatively associated with the “Healthy” DP (OR: 0.54; 95% CI: 0.33, 0.90) and positively associated with the “Snacks and fast food” DP (OR: 1.95; 95% CI: 1.19, 3.18) as opposed to being a non-emotional eater (Table 4). On the other hand, among non-AO subjects, no significant associations were observed between emotional eating and DPs (Table 4).
Table 4.
Association between emotional eating and dietary patterns in participants with and without abdominal obesity.
| Dietary Patterns | Abdominal Obesity (n = 494) | Non-Abdominal Obesity (n = 269) | |||||
|---|---|---|---|---|---|---|---|
| Non-EE (n = 153) |
Low EE (n = 159) |
Emotional or Very EE (n = 182) |
Dietary Patterns | Non-EE (n = 114) |
Low EE (n = 95) |
Emotional or Very EE (n = 60) |
|
| Snacks and fast food DP | Traditional Westernized DP | ||||||
| Crude | 1 | 1.27 (0.81, 1.99) | 1.98 (1.28, 3.07) * | Crude | 1 | 1.02 (0.59, 1.76) | 1.00 (0.53, 1.87) |
| Model I | 1 | 1.25 (0.79, 1.97) | 1.83 (1.17, 2.88) * | Model I | 1 | 0.87 (0.49, 1.58) | 1.02 (0.52, 1.98) |
| Model II | 1 | 1.37 (0.85, 2.22) | 1.88 (1.17, 3.03) * | Model II | 1 | 0.71 (0.36, 1.38) | 0.76 (0.35, 1.65) |
| Model III | 1 | 1.40 (0.86, 2.26) | 1.95 (1.19, 3.18) * | Model III | 1 | 0.77 (0.39, 1.51) | 0.86 (0.39, 1.9) |
| Traditional Westernized DP | Animal products, cereals and vegetables DP | ||||||
| Crude | 1 | 0.81 (0.52, 1.27) | 0.87 (0.56, 1.34) | Crude | 1 | 1.73 (1.00, 3.01) * | 1.68 (0.89, 3.15) |
| Model I | 1 | 0.88 (0.55, 1.39) | 1.08 (0.69, 1.71) | Model I | 1 | 1.79 (1.02, 3.15) * | 1.89 (0.98, 3.65) |
| Model II | 1 | 0.95 (0.56, 1.61) | 1.00 (0.59, 1.68) | Model II | 1 | 1.79 (0.98, 3.28) | 1.77 (0.88, 3.58) |
| Model III | 0.92 (0.54, 1.56) | 0.92 (0.54, 1.57) | Model III | 1 | 1.74 (0.94, 3.21) | 1.70 (0.83, 3.46) | |
| Healthy DP | Healthy DP | ||||||
| Crude | 1 | 0.73 (0.46, 1.14) | 0.50 (0.32, 0.78) * | Crude | 1 | 0.94 (0.55, 1.63) | 0.90 (0.48, 1.69) |
| Model I | 1 | 0.74 (0.47, 1.17) | 0.56 (0.35, 0.89) * | Model I | 1 | 0.97 (0.56, 1.68) | 0.91 (0.47, 1.73) |
| Model II | 1 | 0.75 (0.46, 1.23) | 0.53 (0.33, 0.88) * | Model II | 1 | 0.92 (0.52, 1.63) | 0.83 (0.42, 1.60) |
| Model III | 1 | 0.76 (0.46, 1.24) | 0.54 (0.33, 0.90) * | Model III | 1 | 0.95 (0.53, 1.69) | 0.86 (0.44, 1.69) |
| Animal products and cereals DP | Snacks DP | ||||||
| Crude | 1 | 0.95 (0.61, 1.48) | 1.08 (0.70, 1.66) | Crude | 1 | 1.32 (0.76, 2.27) | 1.61 (0.86, 3.03) |
| Model I | 1 | 0.92 (0.59, 1.44) | 0.96 (0.62, 1.51) | Model I | 1 | 1.34 (0.77, 2.33) | 1.59 (0.83, 3.05) |
| Model II | 1 | 0.95 (0.60, 1.51) | 0.96 (0.61, 1.52) | Model II | 1 | 1.28 (0.71, 2.31) | 1.47 (0.74, 2.92) |
| Model III | 1 | 0.92 (0.58, 1.46) | 0.89 (0.56, 1.420) | Model III | 1 | 1.33 (0.73, 2.41) | 1.54 (0.77, 3.10) |
DP: Dietary pattern; EE: Emotional Eater. Data were presented in Odds ratio (95% confidence interval). Adjusted Model I: adjusted for age and sex. Adjusted Model II: adjusted for age, sex, energy intake, and physical activity. Adjusted Model III: adjusted for age, sex, energy intake, physical activity, and body mass index. * The Odds ratio is significantly different from the reference (non-emotional eaters) p < 0.05.
These results complement and match nutrient intake among the different categories of emotional eaters within each population group. According to the emotional eater classification, in subjects without AO, no significant differences were observed in energy, macronutrients, vitamins, and minerals. Nevertheless, in participants with AO, the emotional eaters consumed significantly less fiber, magnesium, potassium, vitamin B1, vitamin C, and folate, and more lipids, saturated fatty acids, monounsaturated fatty acids, polyunsaturated fatty acids, and sodium than the non-emotional eaters (Table 5). Supplementary Table S4 shows the intake of energy and nutrients in people with and without AO.
Table 5.
Energy and nutrient intake according to emotional eater classification in participants with/without abdominal obesity.
| Abdominal Obesity (n = 494) | Non-Abdominal Obesity (n = 269) | |||||
|---|---|---|---|---|---|---|
| Non-EE | Low EE | EE or Very EE | Non-EE | Low EE | EE or Very EE | |
| Energy (Kcal) | 2400.5 ± 1096.7 | 2287.4 ± 1018.0 | 2328.0 ± 841.9 | 2290.6 ± 819.5 | 2397.8 ± 901.9 | 2382.7 ± 837.6 |
| CH (g) | 287.3 ± 132.4 | 268.5 ± 128.7 | 273.6 ± 108.2 | 268.0 ± 101.3 | 273.3 ± 105.8 | 280.0 ± 122.6 |
| Fiber (g) | 22.5 ± 9.9 | 20.3 ± 10.1 | 18.9 ± 8.8 ●*** | 20.8 ± 8.0 | 20.9 ± 8.4 | 21.2 ± 9.6 |
| Proteins (g) | 89.6 ± 42.3 | 84.6 ± 31.0 | 85.2 ± 33.0 | 85.2 ± 32.0 | 93.8 ± 39.5 | 92.2 ± 36.6 |
| Lipids (g) | 96.4 ± 50.8 | 95.5 ± 43.9 | 99.6 ± 39.5 ●*** | 95.3 ± 34.6 | 103.5 ± 48.8 | 99.8 ± 34.4 |
| SFA (g) | 26.3 ± 16.0 | 26.3 ± 11.6 | 28.4 ± 12.8 ●*** | 26.4 ± 11.7 | 29.7 ± 15.9 | 29.1 ± 10.8 |
| MFA (g) | 32.9 ± 16.9 | 33.4 ± 16.9 | 33.5 ± 13.7 ●* | 33.5 ± 13.5 | 36.4 ± 20.5 | 35.7 ± 13.7 |
| PUFA (g) | 20.8 ± 13.4 | 20.8 ± 13.3 | 22.5 ± 12.7 ●* | 20.4 ± 9.9 | 22.1 ± 13.5 | 19.7 ± 9.8 |
| Cholesterol (mg) | 364.2 ± 296.8 | 354.6 ± 220.0 | 376.4 ± 239.3 | 363.3 ± 234.7 | 441.1 ± 330.5 | 432.7 ± 255.1 |
| Ethanol (g) | 11.1 ± 28.5 | 8.3 ± 21.3 | 5.9 ± 11.4 | 9.0 ± 25.8 | 6.3 ± 9.6 | 6.5 ± 7.6 |
| Calcium (mg) | 881.8 ± 536.1 | 790.7 ± 307.4 | 818.5 ± 348.0 | 803.2 ± 348.7 | 902.0 ± 462.7 | 876.2 ± 340.7 |
| Phosphorus (mg) | 1433.6 ± 644.2 | 1345.4 ± 496.2 | 1346.7 ± 505.4 | 1368.7 ± 505.6 | 1517.3 ± 650.4 | 1452.3 ± 572.7 |
| Iron (mg) | 20.8 ± 9.4 | 19.3 ± 8.4 | 19.4 ± 8.8 | 20.2 ± 8.2 | 21.6 ± 10.1 | 20.9 ± 9.2 |
| Magnesium (mg) | 466.8 ± 189.3 | 423.5 ± 170.1 | 411.4 ± 155.6 ●** | 434.6 ± 150.7 | 450.0 ± 170.2 | 430.3 ± 172.1 |
| Sodium (mg) | 1841.3 ± 1227.3 | 1815.0 ± 982.9 | 1994.3 ± 1006.3 ●* | 1840.1 ± 956.4 | 1988.7 ± 1093.6 | 2009.3 ± 1047.2 |
| Potassium (mg) | 4084.6 ± 1728.0 | 3750.0 ± 1597.8 | 3591.6 ± 1426.3 ●** | 3840.6 ± 1285.5 | 3956.9 ± 1477.9 | 4000.2 ± 1545.3 |
| Zinc (mg) | 10.5 ± 4.9 | 10.0 ± 4.3 | 9.9 ± 4.1 | 10.0 ± 3.6 | 10.6 ± 4.6 | 10.4 ± 4.1 |
| Selenium (mcg) | 38.6 ± 16.2 | 36.3 ± 22.6 | 37.9 ± 25.7 | 38.6 ± 19.3 | 39.5 ± 21.0 | 43.9 ± 25.1 |
| Vitamin A (mcg) | 961.7 ± 647.2 | 849.6 ± 499.4 | 872.9 ± 447.0 | 871.6 ± 354.3 | 989.7 ± 544.6 | 1015.2 ± 607.9 |
| Vitamin B1 (mg) | 1.9 ± 0.8 | 1.8 ± 0.8 | 1.7 ± 0.6 ●* | 1.8 ± 0.6 | 1.8 ± 0.7 | 1.9 ± 0.7 |
| Vitamin B2 (mg) | 2.9 ± 2.1 | 2.8 ± 1.5 | 2.6 ± 1.4 | 2.9 ± 2.1 | 2.9 ± 1.5 | 3.4 ± 2.3 |
| Vitamin B3 (mg) | 22.5 ± 9.7 | 21.3 ± 9.8 | 20.7 ± 8.3 | 22.1 ± 8.4 | 22.6 ± 8.9 | 23.2 ± 9.8 |
| Vitamin B6 (mg) | 2.2 ± 1.0 | 2.0 ± 1.0 | 1.9 ± 0.8 | 2.1 ± 0.8 | 2.2 ± 0.9 | 2.2 ± 1.0 |
| Folate (mcg) | 266.8 ± 141.4 | 243.4 ± 141.6 | 227.6 ± 113.6 ●* | 252.4 ± 99.6 | 273.6 ± 131.8 | 264.6 ± 140.6 |
| Vitamin B12 (mcg) | 7.5 ± 5.4 | 7.0 ± 4.4 | 6.7 ± 3.8 | 6.6 ± 3.8 | 8.5 ± 8.0 | 8.1 ± 5.5 |
| Vitamin C (mg) | 346.7 ± 225.2 | 296.3 ± 205.2 | 268.8 ± 174.2 ●*** | 303.9 ± 160.9 | 279.5 ± 137.0 | 309.1 ± 164.2 |
| Vitamin E (mg) | 1.0 ± 1.1 | 1.0 ± 1.4 | 0.9 ± 1.1 | 0.8 ± 0.9 | 0.9 ± 1.1 | 1.0 ± 1.0 |
EE: Emotional Eater; CH: Carbohydrates; MFA: Monounsaturated Fatty Acids; PUFA: Polyunsaturated Fatty Acids; SFA: Saturated Fatty Acids. Data are presented as mean ± standard deviation. The log of all these variables was calculated for the statistical analysis; however, in this table we show the original value of the variables. Differences among the three emotional eater categories were calculated by ANCOVA with these transformed variables, adjusted by energy intake. * p < 0.05; ** p < 0.01; *** p < 0.001. Differences between the “non-emotional eaters” and the “emotional or very emotional eaters” groups were calculated with Bonferroni’s post hoc statistical test with these transformed variables. ● p < 0.05.
4. Discussion
The current study was the first to show a significant interaction between AO and emotional eating in relation to different DPs. Having AO and being an emotional or very emotional eater was positively associated with the “Snacks and fast food” DP and negatively with adherence to the “Healthy” DP. Among those non-AO subjects, no significant associations were observed between emotional eating and DPs.
To the best of our knowledge, few studies have described eating as DPs and have evidenced the association between emotional eating and specific DPs [15,24,25,26]. In these few studies, a positive association between emotional eating and DPs constituted by foods rich in sugar or fat was reported. Emotional eating was evaluated by different scales such as the three-factor eating questionnaire [15,25], the emotion-induced eating scale (EIES) [24], and the Dutch eating behavior questionnaire [26], while DPs were generated as in the present study, by principal component analysis. Thus, emotional eating was positively associated with several DPs such as “Energy-dense sweet foods”, “Energy-dense non-sweet foods” [15], “Unhealthy snacks, convenience foods”, “Sweets” [25], and with a DP named “Energy-rich” [26]. These DPs consisted mainly of the following foods: fast food (such as pizza and hamburger), snacks (such as potato chips, French fries, popcorn, ice cream, chocolate, sweets, cakes, pastries, biscuits, and bread), fried foods, and sweetened beverages.
From those studies, only one study showed a significant and negative correlation between the emotional eating score and a healthy DP. This DP was constituted mainly by whole grains, fresh vegetables, fruit, milk, soy products, pork/beef meat, and poultry [26]. In contrast, in two other studies, emotional eating was not significantly related, neither positively nor negatively, to a Mediterranean-type pattern [10,44].
According to the psychosomatic theory, the positive association observed between emotional eating and the “Snacks and fast food” DP and the negative association between emotional eating and the “Healthy” DP could be related to the fact that emotional eaters consume food to reduce the intensity of their negative emotion and to cope with emotions in the absence of another effective strategy [3,4,5]. Hence, it has been evidenced that the consumption of good-tasting foods (usually foods rich in sugar or fat) provides immediate pleasure and reward (positive affective responses) that can decrease the impact of stress [3,5]. In addition, foods induce emotions; therefore, the palatability of these foods, not their nutritional content (rich in carbohydrates or fat), is the main factor in regulating emotions [3,5]. Further, food consumption is considered to distract the person from the experience of the negative emotion [3,5]. Another reason for selecting this type of food in response to an emotional state may reflect food availability and accessibility. Mainly, in the context of the current study, many foods included in the “Snacks and fast food” DP are ready-to-eat and readily available. In contrast, healthy foods, such as fruits and vegetables, are less accessible [45].
We found that the associations between emotional eating and the DPs were significant among subjects with AO. In a study in adults, there was no evidence that a relationship between emotional eating and three DPs (“Sweet foods”, “Non-sweet foods”, and “Fruits and vegetables”) varied with BMI or waist circumference [15].
The obtained results may be related to changes in cortisol levels since cortisol is released in stressful situations (negative emotions). An excess of cortisol has been correlated with an increase in abdominal fat, independent of BMI [46,47,48,49]. Likewise, it has been observed that people with AO, mainly women, in stressful situations, have higher concentrations of cortisol (increased cortisol reactivity) compared to people without AO [47,50]. Furthermore, visceral fat accumulation provides increased intracellular glucocorticoids [47]. High levels of cortisol can increase appetite. Therefore, there could be an increase in caloric intake [47] with a preference for energy-dense foods [46,47,48], specifically foods rich in fat [46,48,51,52], saturated fat [51], and sugar [46,52]. Besides, cortisol levels and the effects of emotional intake (positive or negative) could also be associated with different physical activity patterns. We should explore this to obtain a complete multiparametric picture.
On the other hand, in this study sample, of those subjects who presented AO, 90.3% were overweight or obese as determined by BMI. The psychosomatic theory of obesity proposes that emotions influence food consumption in subjects with and without obesity. In obese subjects, emotions are more closely related to eating [4]. It was suggested that people with obesity have difficulties in differentiating hunger and satiety cues and do not differentiate hunger from other non-pleasurable emotional feelings [4]. In addition, this increased susceptibility may be due to the level of emotional intelligence. One study observed that people with obesity had reduced emotional intelligence, which means that they have difficulties in perceiving, understanding, regulating, and generating emotions for self-control, both in a self-reported way [53,54] and in an implicit way [55]. Thus, emotional intelligence has been negatively associated with emotional eating [56]. One approach that can be applied in interventions in overweight or obese populations to improve emotional eating is mindfulness-based interventions [57].
Among other results identified in the present study that complement the DP results, no significant differences in energy and macronutrient intake were observed between non-emotional eaters and emotional eaters. In this regard, there is no consistent evidence to claim an increase in food intake in emotional circumstances in individuals who score high on self-reported emotional eating [14]. Furthermore, in other studies, no significant associations between emotional eating and macronutrient intake were observed [7,8,13]. However, significant and positive associations between emotional eating and energy intake have been observed in women (with and without depressive symptoms) [7], in men [8], and in both sexes [10]. Nevertheless, in the current study, those subjects with AO who were emotional eaters consumed less fiber, magnesium, potassium, vitamin C, and folate, and more saturated fatty acids than non-emotional eaters. In addition, being an emotional eater and having AO was positively associated with commitment to the “Snacks and fast food” DP and negatively with adherence to the “Healthy” DP. The “Snacks and fast food” DP included foods rich in lipids and saturated fats, such as fast foods, industrialized bakery, and desserts, and was characterized by a lack of fruits, vegetables, legumes, whole grains, and nuts, which are the primary sources of fiber, magnesium, potassium, vitamin B1, vitamin C, and folate. The consumption of these nutrients, which are lacking in this DP, is essential for cardiovascular health. The Dietary Approaches to Stop Hypertension (DASH) promote the intake of fiber, magnesium, potassium, calcium, and vegetable proteins and suggests a lower intake of refined carbohydrates and saturated fat. This DASH diet was associated with systolic and diastolic blood pressure improvements and significant reductions in total cholesterol and LDL concentrations [58].
The present study contributed to scientific knowledge regarding the association of emotional eating and the selection and combination of foods habitually consumed by participants (DP) rather than consumption of individual foods or nutrients. Another strength is that dietary intake was assessed with a validated SFFQ [37]. In addition, this SFFQ was applied by trained nutritionists using visual support [38] to facilitate the transformation process of usual portion sizes consumed by the participants to the portion sizes presented in the SFFQ. This questionnaire refers to identification of food consumption during the year before the survey day; therefore, it allows the estimation of habitual food consumption. Nevertheless, the SFFQ has some limitations. Energy and macronutrient estimation is not as precise as with other methods such as dietary records, because the reported intake is limited to the foods included in the FFQ used. Besides, there may be errors in the estimation of the habitual portion size consumed since it depends on the respondent’s memory. In addition, participants may report dietary intake according to social desirability, which may result in overestimating certain foods and underestimating others [59]. Another limitation is that the information of supplements was not asked, so we may involuntarily underreport the consumption of vitamins and minerals.
One limitation of the present study was its cross-sectional design, so causality cannot be drawn. These results should be tested in study designs with a higher level of scientific evidence. Furthermore, this study was performed before COVID-19, new studies should be performed in the post-pandemic period in which emotions and DPs may dramatically change.
Future lines of research should explore the association between emotional eating, DPs, and psychological factors, such as emotional dysregulation [60], as these factors could become targets for intervention. In addition, other eating styles such as external eating, uncontrolled eating, and restrained eating, and positive emotions could be analyzed in future studies together with DPs due to the scarce evidence in this regard.
5. Conclusions
Being an emotional or very emotional eater and presenting AO is related to how we eat and impacts food and nutrient intake. Those subjects who were emotional eaters and had AO adhered more closely to a DP characterized by frequent snacking and fast food (sweet bread, industrialized bakery, flour tortillas, sweets, sugar and honey, breakfast cereals, and desserts) and adhered less to a healthy DP (fruits, vegetables, nuts, legumes and beans, olive oil, tea, chicken, and rice, among other food groups). This combination of DPs that characterizes emotional eaters, results in a low-quality diet with a lower intake of fiber, folic acid, magnesium, potassium, and vitamin C, and a higher intake of sodium and saturated fats.
This study was one of the few studies that analyzed the association of emotional eating with specific DPs. In addition, the current study was the first, to the best of our knowledge, to show a significant interaction between emotional eating and AO with different DPs.
Dietary pattern analyses allow describing the complete diet: the combination of foods habitually consumed by participants rather than independent foods or nutrients. Therefore, considering that emotional eating was associated with specific DPs, when implementing individualized interventions to promote adherence to a healthy DP, we suggest evaluating emotional eating mainly in people with AO. For this purpose, it is necessary to strengthen the nutritionist’s training in this area and to collaborate with other health professionals more specialized in these aspects.
Acknowledgments
We thank Sonia Briseño Montes de Oca and the university authorities for their support in carrying out this study to benefit our institution’s academic and administrative workers. We also thank the multidisciplinary team involved in the execution of the project and the area managers who provided us with all the facilities to carry out the evaluation. With these results and in addition to other analyses that are planned, we will suggest actions that will favor the health of our community. We also thank the surveyors who participated in the data collection processes: Silvia Viridiana Martínez-Rodríguez, Olga Lupita Villalpando-González, Jessica Griselda Castellanos-Rodríguez, Kenia Osornio-García, Andrea Elizabeth Álvarez-del-Río, María Elena Gutiérrez-Urzua, Verónica Michel González-Novoa, Juliana de Jesús Carrión-Ruelas, Wendy Yareni Campos-Pérez, Karina González-Becerra, Elisa María Barrón-Cabrera, and Alondra Guadalupe Mora-Jiménez. We want to thank Gabriela Macedo-Ojeda, a key participant in the training of the surveyors, who participates in other project products. We thank the Organizational Health Program participants for their interest in their health and contribution to a better understanding of how and why we eat. We are also grateful for the English review of the document by Alana Lenaghan and Emma Christine Frey Bell.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14071371/s1, Figure S1: Dietary patterns in the total sample; Table S1: Dietary patterns generated by principal component analysis in the total sample, in participants with non-abdominal obesity and in participants with abdominal obesity; Table S2: Energy and nutrient intake according to non-adherence and adherence to each dietary patterns in participants with abdominal obesity; Table S3: Energy and nutrient intake according to non-adherence and adherence to each dietary patterns in participants without abdominal obesity; Table S4: Energy and nutrient intake in participants with and without abdominal obesity.
Author Contributions
Conceptualization, B.V., E.M.-L., N.T.-C. and C.O.D.L.-R.; methodology, B.V., M.G., E.M.-L. and N.T.-C.; validation, N.T.-C.; formal analysis, A.B.-N., M.G., B.V., M.F.B.-O., and F.M.-S.; investigation, N.T.-C. and E.D.-B.; resources, B.V., E.M.-L. and C.O.D.L.-R.; data curation, N.T.-C. and A.B.-N.; writing—original draft preparation, A.B.-N. and B.V.; writing—review and editing, all the authors.; visualization, A.B.-N., M.G. and B.V.; supervision, B.V., E.M.-L. and C.O.D.L.-R.; project administration, C.O.D.L.-R.; funding acquisition, E.M.-L., C.O.D.L.-R. and B.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Programa para el Desarrollo Profesional Docente (PRODEP) grant awarded to A.B.-N. (UDG-PTC-1511), and by the Institutional Program for Strengthening Research, awarded for the 2019 and 2020 Institute of Nutrigenetics and Translational Nutrigenomics (Programa de Fortalecimiento de la Investigación, CUCS-2019 and CUCS-2020). Transportation of the evaluators was supported by the Organization Health Program of Universidad de Guadalajara (2019-POA). A.B.-N., B.V., N.T., E.M.-L., M.F.B.-O., F.M.-S., and C.O.D.L.-R., received support from the National System of Researchers (CVU number 484393, 22064, 590683, 121937, 176919, 280927, 346109, respectively). Grant PID2020-112768RB-I00 funded by MCIN/AEI/10.13039/501100011033. The Autonomous Community of the Region of Murcia through the Seneca Foundation (20795/PI/18) and NIDDK R01DK105072 granted to M.G.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics, Research and Biosafety Committees of the Centro Universitario de Ciencias de la Salud, Universidad de Guadalajara (protocol code CI-02719, date of approval 14 August 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data are not publicly available because when we created the research protocol, we did not think to include this point in the informed consent. We also want to propose improvements to the workers’ health care program and continue to explore analyses that will benefit this community and other potential beneficiaries. The data presented in this study are available on request, completely anonymously, from the corresponding authors.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Raine K.D. Determinants of healthy eating in Canada: An overview and synthesis. Can. J. Public Heal. 2005;96:S8–S15. doi: 10.1007/BF03405195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Leng G., Adan R.A.H., Belot M., Brunstrom J.M., De Graaf K., Dickson S.L., Hare T., Maier S., Menzies J., Preissl H., et al. The determinants of food choice. Proc. Nutr. Soc. 2017;76:316–327. doi: 10.1017/S002966511600286X. [DOI] [PubMed] [Google Scholar]
- 3.Macht M. How emotions affect eating: A five-way model. Appetite. 2008;50:1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Canetti L., Bachar E., Berry E.M. Food and emotion. Behav. Process. 2002;60:157–164. doi: 10.1016/S0376-6357(02)00082-7. [DOI] [PubMed] [Google Scholar]
- 5.Evers C., Marijn Stok F., de Ridder D.T.D. Feeding your feelings: Emotion regulation strategies and emotional eating. Pers. Soc. Psychol. Bull. 2010;36:792–804. doi: 10.1177/0146167210371383. [DOI] [PubMed] [Google Scholar]
- 6.van Strien T. Causes of Emotional Eating and Matched Treatment of Obesity. Curr. Diab. Rep. 2018;18:35. doi: 10.1007/s11892-018-1000-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camilleri G.M., Méjean C., Kesse-Guyot E., Andreeva V.A., Bellisle F., Hercberg S., Péneau S. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J. Nutr. 2014;144:1264–1273. doi: 10.3945/jn.114.193177. [DOI] [PubMed] [Google Scholar]
- 8.De Lauzon B., Romon M., Deschamps V., Lafay L., Borys J.M., Karlsson J., Ducimetière P., Charles M.A. The Three-Factor Eating Questionnaire-R18 is able to distinguish among different eating patterns in a general population. J. Nutr. 2004;134:2372–2380. doi: 10.1093/jn/134.9.2372. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen-Michel S.T., Unger J.B., Spruijt-Metz D. Dietary correlates of emotional eating in adolescence. Appetite. 2007;49:494–499. doi: 10.1016/j.appet.2007.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paans N.P.G., Gibson-Smith D., Bot M., van Strien T., Brouwer I.A., Visser M., Penninx B.W.J.H. Depression and eating styles are independently associated with dietary intake. Appetite. 2019;134:103–110. doi: 10.1016/j.appet.2018.12.030. [DOI] [PubMed] [Google Scholar]
- 11.Ling J., Zahry N.R. Relationships among perceived stress, emotional eating, and dietary intake in college students: Eating self-regulation as a mediator. Appetite. 2021;163:105215. doi: 10.1016/j.appet.2021.105215. [DOI] [PubMed] [Google Scholar]
- 12.Elran Barak R., Shuval K., Li Q., Oetjen R., Drope J., Yaroch A.L., Fennis B.M., Harding M. Emotional eating in adults: The role of sociodemographics, lifestyle behaviors, and self-regulation—findings from a U.S. National Study. Int. J. Environ. Res. Public Health. 2021;18:1744. doi: 10.3390/ijerph18041744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Anschutz D.J., Van Strien T., Van De Ven M.O.M., Engels R.C.M.E. Eating styles and energy intake in young women. Appetite. 2009;53:119–122. doi: 10.1016/j.appet.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 14.Bongers P., Jansen A. Emotional Eating Is Not What You Think It Is and Emotional Eating Scales Do Not Measure What You Think They Measure. Front. Psychol. 2016;7:1932. doi: 10.3389/fpsyg.2016.01932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Konttinen H., Männistö S., Sarlio-Lähteenkorva S., Silventoinen K., Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54:473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 16.Konttinen H., Van Strien T., Männistö S., Jousilahti P., Haukkala A. Depression, emotional eating and long-term weight changes: A population-based prospective study. Int. J. Behav. Nutr. Phys. Act. 2019;16:28. doi: 10.1186/s12966-019-0791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lopez-Cepero A., Frisard C.F., Lemon S.C., Rosal M.C. Association of Dysfunctional Eating Patterns and Metabolic Risk Factors for Cardiovascular Disease among Latinos. J. Acad. Nutr. Diet. 2018;118:849–856. doi: 10.1016/j.jand.2017.06.007. [DOI] [PubMed] [Google Scholar]
- 18.Pacheco L., Blanco E., Burrows R., Correa-Burrows P., Santos J., Gahagan S. Eating behavior and body composition in Chilean young adults. Appetite. 2021;156:104857. doi: 10.1016/j.appet.2020.104857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hunot-Alexander C., Arellano-Gómez L.P., Smith A.D., Kaufer-Horwitz M., Vásquez-Garibay E.M., Romero-Velarde E., Fildes A., Croker H., Llewellyn C.H., Beeken R.J. Examining the validity and consistency of the Adult Eating Behaviour Questionnaire-Español (AEBQ-Esp) and its relationship to BMI in a Mexican population. Eat. Weight Disord. 2022;27:651–663. doi: 10.1007/s40519-021-01201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lazarevich I., Irigoyen Camacho M.E., Velázquez-Alva M.d.C., Zepeda Zepeda M. Relationship among obesity, depression, and emotional eating in young adults. Appetite. 2016;107:639–644. doi: 10.1016/j.appet.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Frayn M., Knäuper B. Emotional Eating and Weight in Adults: A Review. Curr. Psychol. 2018;37:924–933. doi: 10.1007/s12144-017-9577-9. [DOI] [Google Scholar]
- 22.López-Guimerà G., Dashti H.S., Smith C.E., Sánchez-Carracedo D., Ordovas J.M., Garaulet M. CLOCK 3111 T/C SNP interacts with emotional eating behavior for weight-loss in a Mediterranean population. PLoS ONE. 2014;9:e99152. doi: 10.1371/JOURNAL.PONE.0099152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bonnet G., Gómez-Abellán P., Vera B., Sánchez-Romera J.F., Hernández-Martínez A.M., Sookoian S., Pirola C.J., Garaulet M. Serotonin-transporter promoter polymorphism modulates the ability to control food intake: Effect on total weight loss. Mol. Nutr. Food Res. 2017;61:1700494. doi: 10.1002/mnfr.201700494. [DOI] [PubMed] [Google Scholar]
- 24.Jalo E., Konttinen H., Vepsäläinen H., Chaput J.P., Hu G., Maher C., Maia J., Sarmiento O.L., Standage M., Tudor-Locke C., et al. Emotional eating, health behaviours, and obesity in children: A 12-country cross-sectional study. Nutrients. 2019;11:351. doi: 10.3390/nu11020351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pentikäinen S., Arvola A., Karhunen L., Pennanen K. Easy-going, rational, susceptible and struggling eaters: A segmentation study based on eating behaviour tendencies. Appetite. 2018;120:212–221. doi: 10.1016/j.appet.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 26.Lu Q., Tao F., Hou F., Zhang Z., Ren L.-L. Emotion regulation, emotional eating and the energy-rich dietary pattern. A population-based study in Chinese adolescents. Appetite. 2016;99:149–156. doi: 10.1016/j.appet.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 27.Hu F.B. Dietary pattern analysis: A new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Nuttall F.Q. Body Mass Index Obesity, BMI, and Health: A Critical Review. Nutr. Today. 2015;50:117–128. doi: 10.1097/NT.0000000000000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Després J., Lemieux I., Bergeron J., Pibarot P., Mathieu P., Larose E., Rodés-Cabau J., Bertrand O., Poirier P. Abdominal obesity and the metabolic syndrome: Contribution to global cardiometabolic risk. Arterioscler. Thromb. Vasc. Biol. 2008;28:1039–1049. doi: 10.1161/ATVBAHA.107.159228. [DOI] [PubMed] [Google Scholar]
- 30.Choi D., Choi S., Son J.S., Oh S.W., Park S.M. Impact of discrepancies in general and abdominal obesity on major adverse cardiac events. J. Am. Heart Assoc. 2019;8:e013471. doi: 10.1161/JAHA.119.013471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Medical Association World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 32.World Health Organization . Waist Circumference and Waist–Hip Ratio: Report of a WHO Expert Consultation. World Health Organization; Geneva, Switzerland: 2008. [Google Scholar]
- 33.Alberti K.G.M.M., Eckel R.H., Grundy S.M., Zimmet P.Z., Cleeman J.I., Donato K.A., Fruchart J.-C., James W.P.T., Loria C.M., Smith S.C. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 34.Garaulet M., Canteras M., Morales E., López-Guimera G., Sánchez-Carracedo D., Corbalán-Tutau M.D. Validation of a questionnaire on emotional eating for use in cases of obesity: The Emotional Eater Questionnaire (EEQ) Nutr. Hosp. 2012;27:645–651. doi: 10.1590/S0212-16112012000200043. [DOI] [PubMed] [Google Scholar]
- 35.Bernabéu E., Marchena C., Iglesias M.T. Factor structure and psychometric properties of emotional eater questionnaire (EEQ) in spanish colleges. Int. J. Environ. Res. Public Health. 2020;17:9090. doi: 10.3390/ijerph17239090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bland J.M., Altman D.G. Statistics notes: Cronbach’s alpha. BMJ. 1997;314:572. doi: 10.1136/bmj.314.7080.572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Macedo-Ojeda G., Vizmanos-Lamotte B., Márquez-Sandoval Y.F., Rodríguez-Rocha N.P., López-Uriarte P.J., Fernández-Ballart J.D. Validation of a semi-quantitative food frequency questionnaire to assess food groups and nutrient intake. Nutr. Hosp. 2013;28:2212–2220. doi: 10.3305/nutrhosp.v28in06.6887. [DOI] [PubMed] [Google Scholar]
- 38.Bernal-Orozco M., Vizmanos-Lamotte B., Rodríguez-Rocha N., Macedo-Ojeda G., Orozco-Valerio M., Rovillé-Sausse F., León-Estrada S., Márquez-Sandoval F., Fernández-Ballart J. Validation of a Mexican food photograph album as a tool to visually estimate food amounts in adolescents. Br. J. Nutr. 2013;109:944–952. doi: 10.1017/S0007114512002127. [DOI] [PubMed] [Google Scholar]
- 39.Ledesma Solano J., Chávez Villasana A., Pérez-Gil F., Mendoza Martínez E., Calvo Carrillo C. Composición de Alimentos Miriam Muñoz de Chávez. Valor Nutritivo de Los Alimentos de Mayor Consumo. McGraw-Hill, Ed.; Ciudad de México, México: 2010. [Google Scholar]
- 40.USDA National Nutrient Database for Standard Reference. Release 25. [(accessed on 24 January 2022)]; Available online: http://ndb.nal.usda.gov/ndb/search/list.
- 41.Taherdoost H., Sahibuddin S., Jalaliyoon N. Exploratory factor analysis; concepts and theory. Adv. Appl. Pure Math. 2014:375–382. [Google Scholar]
- 42.Williams B., Onsman A., Brown T. Exploratory factor analysis: A five-step guide for novices. [(accessed on 22 January 2022)];J. Emerg. Prim. Heal. Care. 2010 8:990399. doi: 10.33151/ajp.8.3.93. Available online: https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.475.8594&rep=rep1&type=pdf. [DOI] [Google Scholar]
- 43.Costello A., Osborne J. Best Practices in Exploratory Factor Analysis: Four Recommendations for Getting the Most From Your Analysis. Pract. Assess. Res. Eval. 2005;10:7. [Google Scholar]
- 44.Carlos M., Elena B., Teresa I.M. Are adherence to the mediterranean diet, emotional eating, alcohol intake, and anxiety related in university students in Spain? Nutrients. 2020;12:2224. doi: 10.3390/nu12082224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gastelum Strozzi V., Márquez-Sandoval Y.F. Disponibilidad y costo de alimentos ofertados dentro y fuera de los Centros Universitarios de la Universidad de Guadalajara de la Zona Metropolitana. [(accessed on 25 October 2021)]. Available online: https://hdl.handle.net/20.500.12104/83822.
- 46.van der Valk E., Savas M., van Rossum E. Stress and Obesity: Are There More Susceptible Individuals? Curr. Obes. Rep. 2018;7:193–203. doi: 10.1007/s13679-018-0306-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adam T., Epel E. Stress, eating and the reward system. Physiol. Behav. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 48.Vicennati V., Pasqui F., Cavazza C., Garelli S., Casadio E., di Dalmazi G., Pagotto U., Pasquali R. Cortisol, energy intake, and food frequency in overweight/obese women. Nutrition. 2011;27:677–680. doi: 10.1016/j.nut.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 49.Geiker N., Astrup A., Hjorth M., Sjödin A., Pijls L., Markus C. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes. Rev. 2018;19:81–97. doi: 10.1111/obr.12603. [DOI] [PubMed] [Google Scholar]
- 50.Incollingo Rodriguez A., Epel E., White M., Standen E., Seckl J., Tomiyama A. Hypothalamic-pituitary-adrenal axis dysregulation and cortisol activity in obesity: A systematic review. Psychoneuroendocrinology. 2015;62:301–318. doi: 10.1016/j.psyneuen.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 51.Laugero K., Falcon L., Tucker K. Relationship between perceived stress and dietary and activity patterns in older adults participating in the Boston Puerto Rican Health Study. Appetite. 2011;56:194–204. doi: 10.1016/j.appet.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hewagalamulage S., Lee T., Clarke I., Henry B. Stress, cortisol, and obesity: A role for cortisol responsiveness in identifying individuals prone to obesity. Domest. Anim. Endocrinol. 2016;56:S112–S120. doi: 10.1016/j.domaniend.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 53.Kass A.E., Wildes J.E., Coccaro E.F. Identification and regulation of emotions in adults of varying weight statuses. J. Health Psychol. 2019;24:941–952. doi: 10.1177/1359105316689604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Casagrande M., Boncompagni I., Forte G., Guarino A., Favieri F. Emotion and overeating behavior: Effects of alexithymia and emotional regulation on overweight and obesity. Eat. Weight Disord. 2020;25:1333–1345. doi: 10.1007/s40519-019-00767-9. [DOI] [PubMed] [Google Scholar]
- 55.Scarpina F., Varallo G., Castelnuovo G., Capodaglio P., Molinari E., Mauro A. Implicit facial emotion recognition of fear and anger in obesity. Eat. Weight Disord. 2021;26:1243–1251. doi: 10.1007/s40519-020-01010-6. [DOI] [PubMed] [Google Scholar]
- 56.Zysberg L., Rubanov A. Emotional intelligence and emotional eating patterns: A new insight into the antecedents of eating disorders? J. Nutr. Educ. Behav. 2010;42:345–348. doi: 10.1016/j.jneb.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 57.Warren J., Smith N., Ashwell M. A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: Effectiveness and associated potential mechanisms. Nutr. Res. Rev. 2017;30:272–283. doi: 10.1017/S0954422417000154. [DOI] [PubMed] [Google Scholar]
- 58.Siervo M., Lara J., Chowdhury S., Ashor A., Oggioni C., Mathers J.C. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br. J. Nutr. 2015;113:1–15. doi: 10.1017/S0007114514003341. [DOI] [PubMed] [Google Scholar]
- 59.Pérez Rodrigo C., Aranceta J., Salvador G., Varela-Moreiras G. Food frequency questionnaires. Nutr. Hosp. 2015;31:49–56. doi: 10.3305/nh.2015.31.sup3.8751. [DOI] [PubMed] [Google Scholar]
- 60.Usubini A.G., Cattivelli R., Varallo G., Castelnuovo G., Molinari E., Giusti E.M., Pietrabissa G., Manari T., Filosa M., Franceschini C., et al. The Relationship between Psychological Distress during the Second Wave Lockdown of COVID-19 and Emotional Eating in Italian Young Adults: The Mediating Role of Emotional Dysregulation. J. Pers. Med. 2021;11:569. doi: 10.3390/jpm11060569. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data are not publicly available because when we created the research protocol, we did not think to include this point in the informed consent. We also want to propose improvements to the workers’ health care program and continue to explore analyses that will benefit this community and other potential beneficiaries. The data presented in this study are available on request, completely anonymously, from the corresponding authors.