Abstract
PROBLEM:
Sleep and mood represent two important malleable opportunities for adolescent health. This study investigated the sleep–mood relationship in adolescent girls.
METHODS:
Short-term, longitudinal design. Latina adolescents (N = 19, mean age 15) completed ecological momentary assessments on sleep (perceived quality, self-report quantity) and mood (negative affect, positive affect, and positivity ratio).
FINDINGS:
Adolescents sent 1,598 texts on sleep and mood. Bidirectional sleep–mood relationships were in expected directions; negative affect and the positivity ratio affect predicted adolescents’ sleep quality.
CONCLUSIONS:
Interventions should encourage sleep–mood relationship awareness, and further research should identify significant differences to inform tailored interventions with adolescents.
Keywords: Adolescent, ecological momentary assessment, female, mental health, mHealth, sleep
The prevalence of mental health problems reported by adolescents in the United States is concerning, with one in five U.S. adolescents exhibiting a mental health problem (Schwarz, 2009). Disproportionately higher rates of poor mental health are demonstrated among non-White adolescents and females, with suicide being a leading cause of death (DHHS, 2001; Duarté-Vélez & Bernal, 2007; Lowry, Crosby, Brener, & Kann, 2013; Mulye, 2009). Adolescent mental health is receiving noteworthy attention because of both the immediate (i.e., depressive symptoms, anxiety, perceived stress, high-risk behaviors) and long-term (i.e., immune function, chronic disease, suicide, reduced education/employment success) consequences associated with poor mental health. Previous research has demonstrated associations between adolescent mental health and common risk and protective factors within youth themselves (i.e., coping behaviors, stress response, self-esteem, substance use) (Aldridge & Roesch, 2008a; Elkington, Bauermeister, & Zimmerman, 2010; Forster et al., 2013; Umaña-Taylor & Updegraff, 2007), their communities (i.e., family poverty, violence, school support) (Aldridge & Roesch, 2008b; Theokas, 2006), and the broader society (i.e., racism) (Berkel et al., 2010; Chavez & French, 2007). These studies reveal the complex interplay of intrinsic and extrinsic factors that influence adolescent mental health. Leading resiliency theorists recognize that all stressors cannot and should not be removed from an adolescent’s life, but rather, an adolescent’s unique makeup and subsequent interaction with these factors and stressors should be supported to yield a response (Carbonell, Reinherz, & Beardslee, 2005; Compas, ConnorSmith, Saltzman, Thomsen, & Wadsworth, 2001). More recently, attention has been given to specific individual-level factors that could be opportunities for strengthening adolescent resiliency, health, and mental health in particular; one of these is a basic need all humans have—the need for sleep (Carskadon, 2009).
Review of the Literature
Insufficient sleep levels among adolescents range from minimal to serious and chronic (i.e., behaviorally induced insufficient sleep syndrome; Pallesen et al., 2011) and have been documented via self-report and objective methods (Noland, Price, Dake, & Telljohann, 2009; Vallido, Peters, O’Brien, & Jackson, 2009). Adolescent sleep deprivation is in part the result of normative pubertal changes in sleep regulation, specifically homeostatic and circadian regulation systems (Dahl & Lewin, 2002; Hagenauer, Perryman, Lee, & Carskadon, 2009), but inadequate sleep is also a symptom associated with depression and suicidality (Lee, Cho, Cho, & Kim, 2012). Although there are biological explanations for insufficient sleep, attention toward minimizing sleep deprivation among adolescents is warranted because it is associated with numerous negative outcomes, including mental health (i.e., depression, mood disturbances, suicidality; Lee et al., 2012; McKnight-Eily et al., 2011), physical health (i.e., daytime sleepiness, immune system compromise, overweight, caffeine use, pedestrian safety; Davis, Avis, & Schwebel, 2013; James, Kristjánsson, & Sigfúsdóttir, 2011; Landis, Parker, & Dunbar, 2009; McKnight-Eily et al., 2011; Noland et al., 2009), academic behavior (i.e., inattention, behavior problems, poor grades, success; James et al., 2011), and other behavioral problems (i.e., substance use; James et al., 2011; McKnight-Eily et al., 2011), driving crashes, impulse control, delinquency, and violence (Danner & Phillips, 2008; McKnight-Eily et al., 2011; Peach & Gaultney, 2013). Sleep quality is another important dimension, having demonstrated negative associations with depressive symptoms and problem behaviors for both young males and females (Meijer, Reitz, Dekovi, van den Wittenboer, & Stoel, 2010; Yip, 2013). Among adolescent females, sleep quality predicted increased dream recall (Brand et al., 2011), which has been positively associated with health and well-being.
Statement of the Problem
No study to date has examined perceived sleep (sufficiency or quality) and mood specifically among Latino adolescent females (Latinas), despite their notably high rates of depressive symptoms and suicidal ideation (Garcia, Skay, Sieving, Naughton, & Bearinger, 2008; Minnesota Department of Health [MDE], 2007; Mulye, 2009; Zayas, Gulbas, Fedoravicius, & Cabassa, 2010) and reports of insufficient sleep (Eaton et al., 2010). Therefore, this study was conducted to examine adolescent sleep and mood relationship among Latina adolescents.
Furthermore, although research addressing adolescent sleep is maturing and expanding, including use of observed and self-report strategies for documenting actual and perceived sleep, only one research team to date has used ecological momentary assessment (EMA) to collect real-time sleep data (Rofey et al., 2010). EMA is a methodological technique that is characterized by real-time data collection, typically of behaviors or attitudes that are relatively dynamic rather than static (Armey, Crowther, & Miller, 2011; Shrier et al., 2012; Wenze & Miller, 2010; Rofey et al., 2010). EMA data in the sleep study were collected using a verbal phone interview (Eaton et al., 2010), which is not a typical EMA strategy; more common EMA approaches have involved use of automated probes to complete an electronic journal or short messaging service (SMS)-based text message questions that can be responded to directly. EMA offers methodological advantages to recall-based tools, including real-time reporting of mood, behavior, and environment (Forbes et al., 2012; Armey et al., 2011; Shrier et al., 2012; Wenze & Miller, 2010). EMA data are collected via cellular phone but historically collection involved sending automated surveys via handheld devices such as palm pilots (Collins, Kashdan, & Gollnisch, 2003; Shrier, Shih, Hacker, & de Moor, 2007). Adolescent cell phone ownership rates increase each year. With some adolescents sending over 4,000 text messages a month (note: no one texts more than 13- to 17-year-old females) (Nielsen, 2010), EMA via text messages is potentially a rich data collection tool for young people in the United States.
Aims of the Study
The goal of our study was to contribute to existing adolescent sleep-mood knowledge by examining Latina adolescents’ reports of their sleep and mood using EMA data collected via text messaging. Based on previous research with adolescents generally, as noted in the literature review above, we hypothesized that a bidirectional relationship exists between sleep and mood; specifically, higher levels of positive mood and lower levels of negative mood would be associated with better sleep outcomes and that higher levels of sleep quality and quantity would predict better mood.
Methods
A pilot longitudinal study was conducted to implement a newly developed EMA data collection system via text messaging with a community, school-based sample of Latina adolescents.
Participants
Participants were recruited from two high schools in an urban city within a Midwestern State. School records indicated that there were 100 eligible girls across the two schools; of these, 96 were contacted by a research team member about the study and invited to participate. There were four girls who did not have confirmed contact, because they were possibly not at school on the days recruitment occurred, and they did not respond to the mailed information about the study. A research team member actively recruited participants during school lunch periods and at outreach events for Latino parents. There were 27 adolescents who indicated interest; of these, 24 returned written parental consent forms, completed assent processes, and enrolled in the study. Human research ethics committees at both the university and school district reviewed and approved the study protocol. Participants received $20 per month for the cost of unlimited texting; to encourage texting responses, a drawing was held for an iTouch at each school at the conclusion of the study and participants had a certain number of entries in the drawing based on their texted response rate.
The 24 participants ranged in age from 14 to 17 years (mean age 15). Nineteen adolescents (79%) provided sleep data and are included in the analysis described in this article. The five participants who did not provide sleep data and are excluded from analysis were not statistically significantly different from the 19 participants on select demographics (i.e., age, free/reduced lunch status).
Study Protocol
Data were collected in a pilot study testing the feasibility of the Youth Ecological Momentary Assessment System (YEMAS), an automated SMS-based text messaging data collection system (Garcia et al., 2014). YEMAS was developed to collect automated texted self-report of daily activities, behaviors, and attitudes among adolescents. This system was also created to collect and transfer real-time data about individual- and social-level factors that influence physical, mental, emotional, and social well-being (Garcia et al., 2014). Enrolled participants confirmed cell phone ownership (four participants requested a cell phone that was provided with text messaging ability only). Each day, participants were sent SMS-based text messaging questions four times (morning, after school, late afternoon, evening). Each time, between 7 and 11 questions were texted (range: 28–44 questions per day), covering categories of health, mood, social network, and risk and protective behaviors. The research team determined the frequency of each question based on the nature of the question and with sensitivity to avoiding participant burden; the questions were then randomly distributed across times of day and days of week, with certain rules applied to the randomization (i.e., sleep questions asked in a morning survey rather than in the afternoon). The measures in the current study (i.e., sleep quantity, sleep quality, and mood) were limited to sleep data that were available from Monday, Tuesday, Thursday, Friday, and Sunday, and mood data that were available from Monday, Thursday, Saturday, and Sunday. In this way, temporal analysis of the sleep–mood relationship was possible (i.e., Sunday sleep data examined in relation to Monday mood data). With this temporal analysis limitation, texted sleep and mood data were obtained from participants on approximately 7 days (range 2–13 days).
Measures
Ecological Momentary Assessment
Latina adolescents responded to automated EMA text messages; each text was an individual question assessing variables such as sleep quantity, sleep quality, positive mood, and negative mood. Self-report was the only source of data for this study. Measures were derived from established surveys (i.e., Minnesota Student Survey (Minnesota Department of Education [MDE],2006) and validated instruments (i.e.,Positive and Negative Affect Schedule [PANAS]; Crawford & Henry, 2004) and were modestly adapted for texting purposes (e.g., “you” shortened to “u”). (Note that the PANAS instrument reports measures of “affect”; while we report our results in the original PANAS terms [e.g., positive affect (PA),negative affect (NA)],we have chosen to use “mood” in all other parts of this article because it is more representative of the traits being assessed. Furthermore, we refer to “mood” in the way in which an adolescent would describe her “mood,” not in the psychiatric or clinical sense of“mood.”) Each day the texted survey was delivered one question at a time; the adolescent received an initial text message indicating that it was time for a survey. When she responded to the first question, the next question was texted. If she was distracted or did not respond, the system would wait for a response before sending the next question. At the end of the day, every survey would close, whether completed or not, and a new survey would initiate the next day (Garcia et al., 2014). Table 1 shows the sleep and mood measures used in the current analysis, including response options and the number of texts received (range, mean, median) for each EMA measure. PA was measured by summing responses to texts assessing happy, relaxed, and excited mood states (4-point Likert scale, summed range 0–12). NA was measured by summing responses to texts assessing sad, mad, and nervous mood states. The PA to NA ratio (PA/NA; positivity ratio) was measured by dividing PA by NA (Crawford & Henry, 2004).
Table 1.
Quantity of Text Responses (Range, Mean, Median) by Measure, Overall, and in Analysis
| Number of text responses |
||||||
|---|---|---|---|---|---|---|
| Measure | Response options | Range | M | Median | Sum | Used for analysisa |
| Sleep | ||||||
| Sleep quantity | Open ended | 1–19 | 8.1 | 6.0 | 153 | 121 |
| “How many hours of sleep did u get last night?” | ||||||
| Sleep quality | Yes/No | 3–16 | 7.5 | 6.5 | 135 | 103 |
| “Do u feel u got enough sleep last night for ur body?” | ||||||
| Mood | ||||||
| Happy | Not at all A little Quite a bit Extremely | 17–48 | 29.3 | 28.0 | 557 | 240 |
| “How HAPPY were u feeling just before u got this txt?” | ||||||
| Excited | 9–46 | 27.6 | 27.0 | 524 | 269 | |
| “How EXCITED were u feeling just before u got this txt?” | ||||||
| Relaxed | 8–39 | 23.5 | 24.0 | 446 | 205 | |
| “How RELAXED were u feeling just before u got this txt?” | ||||||
| Mad | 6–36 | 20.7 | 21.0 | 394 | 231 | |
| “How MAD were u feeling just before u got this txt?” | ||||||
| Sad | 4–28 | 16.1 | 15.0 | 305 | 183 | |
| “How SAD were u feeling just before u got this txt?” | ||||||
| Nervous | 12–53 | 29.2 | 28.0 | 555 | 246 | |
| “How NERVOUS were u feeling just before u got this txt?” | ||||||
For sleep variable, Monday, Tuesday, Thursday, Friday, and Sunday data are used; for mood variable, Monday, Thursday, Saturday, and Sunday data are used.
Demographic data such as age, race, and subjective and objective socioeconomic status were collected in a separate online survey administered before the EMA texting data collection began.
Data Analysis
Descriptive statistics are expressed as frequencies (percent) or mean (SD) as appropriate. For the comparison of sleep hours between enough sleep and non-enough sleep groups (groups divided at the mean, 7 hr of sleep), the difference and p value were calculated using repeated measures analysis of variance (ANOVA). PA is calculated by sum of the average daily scores of happy, excited, and relaxed. NA is calculated by sum of the average of daily scores of mad, sad, and nervous, and PA/NA is their ratio. Linear mixed modeling was used for analyses with continuous outcomes (i.e., sleep hours) to account for the nesting of observations within each participant. For example, the night before sleep quantity or quality was used to predict the next day’s mood, and each day’s mood was used to predict the next night’s sleep quality or quantity. Logistic regression was used for the analysis with binary outcomes (i.e., sleep quality) with generalized estimating equations to account for within-subject correlations. All analyses were conducted using the Statistical Analysis System (SAS) (Crawford & Henry, 2004; SAS Institute, 2012). All p values are two tailed and .05 is considered statistically significant.
Findings
Sleep and Mood Descriptive Results
Nineteen Latina adolescents provided nearly 1,600 (1,598) texts on sleep and mood (see Table 1). The adolescents reported a range of 0–10 hr of sleep (121 texts in response to the sleep quantity question “how many hours of sleep did u get last night?”, M = 7.1 sleep hours, SD = 1.6). Girls reported slightly more sleep on weekends (7.7 hr; SD = 1.3, range 4–10) than weekdays (6.8 hr; SD = 1.6, range 0–10). When girls indicated they had enough sleep, they reported having slept between 5.5 and 10 hr the night before (M = 8.2 hr, SD = 1.1) whereas when girls said they did not have enough sleep, the number of hours slept ranged from 0 to 9 (M = 6.3 hr, SD = 1.6). The sleep hour difference between those reporting enough sleep and not enough sleep was statistically significant (mean difference = 1.9, SE = 0.31, p < .001).
The score for each mood included in the PA or NA score ranged from 1 to 4: 1 (not at all), 2 (a little), 3 (quite a bit), 4 (extremely). Girls reported slightly higher scores for positive moods than negative moods (see Table 2). PA is a little bit higher than NA (PA mean = 5.9 [a little] versus NA mean = 4.6 [not at all—a little]; the positivity ratio [PA/NA] was 1.52).
Table 2.
Texted Mood Responses: Mean and Median Scorea (N = 24)
| Mood | M (SD) | Median | |
|---|---|---|---|
| Positive affect | Happy | 2.13 (0.83) | 2 |
| Excited | 1.70 (0.82) | 2 | |
| Relax | 2.15 (0.85) | 2 | |
| Negative affect | Mad | 1.53 (0.80) | 1 |
| Sad | 1.48 (0.73) | 1 | |
| Nervous | 1.51 (0.79) | 1 |
Data are all texted responses from participants for these mood questions throughout the study.
Response options: 1 (not at all), 2 (a little), 3 (quite a bit), 4 (extremely).
In exploratory analyses, each of the affect variables (PA, NA, PA/NA) was associated with previous night sleep hours; the association followed a straight line with a change in the line’s slope at 7 hr of sleep the previous night. A similar association was observed between the sleep hour reported for the following night and each of the affect variables, with the slope change occurring at the mean of each affect variable. These changes were taken into account in the subsequent analyses.
Amount of Sleep From Previous Night as a Predictor for Next Day Affect
Participants who reported fewer than 7 hr of sleep had the following outcomes with every 1-hr increase in sleep: an average of 0.12 lower PA, a 0.03 higher NA, and a 0.08 lower positivity ratio. In contrast, for participants reporting greater than 7 hr of sleep, each extra hour of sleep resulted in 0.08 higher PA, 0.27 lower NA, and 0.09 higher positivity ratio. None of these results were statistically significant. Based on these data, sleep hour does not appear to predict PA, NA, or PA/NA.
Last Night Sleep Quality Predicting Next Day Affect
Participants who reported sufficient sleep had an average of 0.48 higher PA, a 0.19 lower NA, and a 0.04 higher positivity ratio than participants who reported insufficient sleep; however, these were not statistically significant.
Affect Predicting Following Night Sleep Quantity
A nonlinear relationship was observed between affect and sleep quantity. When PA is less than its mean, sleep hour increases 0.24 with one unit increase in PA (non-significance: ns); when PA is greater than or equal to its mean, sleep hour decreases 0.13 with one unit increase in PA (ns). Similarly, when NA is less than its mean, sleep hour decreases 0.50 with one unit increase in NA; when NA is greater than or equal to its mean, sleep hour increases 0.19 with one unit increase in NA (ns). When the positivity ratio effect is less than its mean, sleep hour decreases 0.03 with one unit increase in the ratio (ns); when the ratio is greater than or equal to its mean, sleep hour increases 0.44 with one unit increase in the ratio (ns).
Affect as a Predictor of Following Night Sleep Quality
An adolescent reporting higher NA is less likely to report a good night’s sleep the following night with odds ratio = 0.56 (95% CI: 0.32, 0.96), whereas an adolescent reporting a higher positivity ratio is more likely to report having a good night’s sleep the following night with odds ratio = 2.41 (95% CI: 1.12–5.19) (see Figure 1). For PA, although the results show a similar trend (odds ratio = 1.07), the association was not statistically significant. Therefore, only the NA and the positivity ratio appear to predict, in the expected direction, whether an adolescent perceives having had enough sleep the following night.
Figure 1.
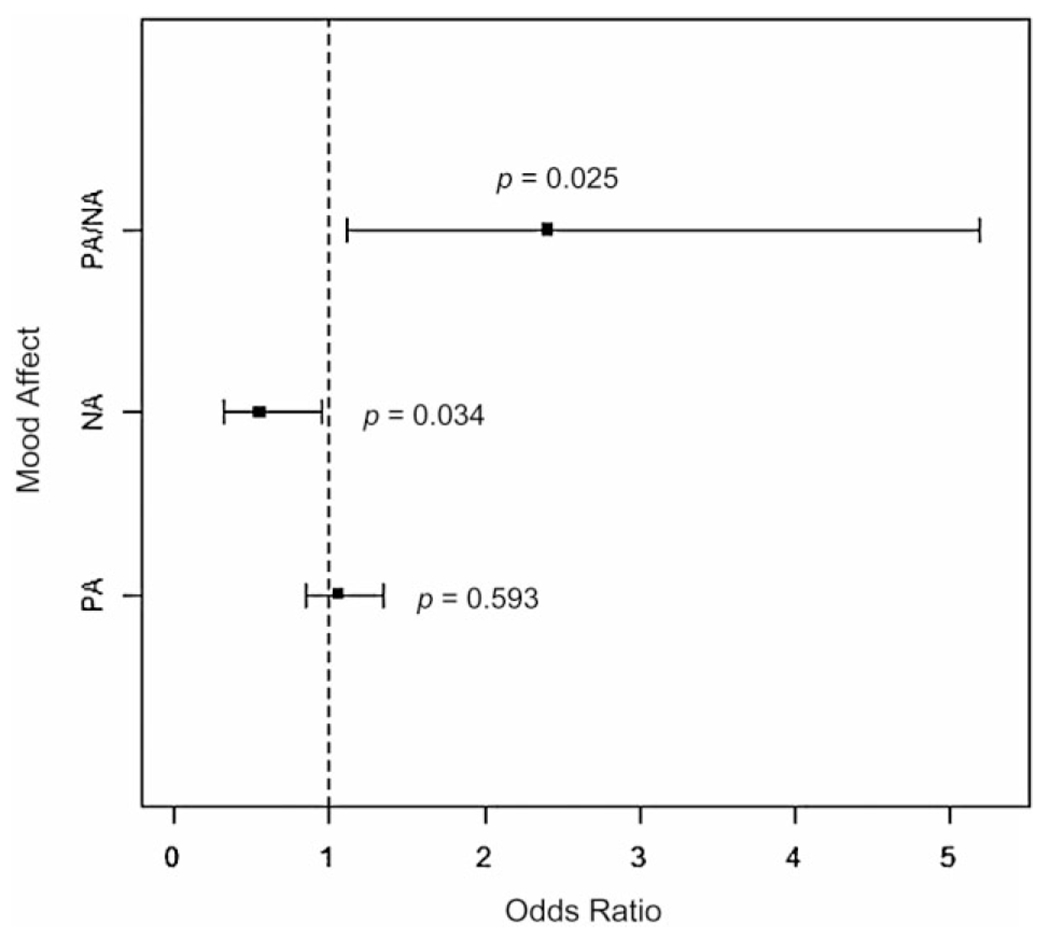
Odds Ratios for Affect Predicting Sleep Quality
Discussion
The purpose of our study was to explore Latina adolescent sleep, mood, and the relationship of sleep (i.e., quality and quantity) with positive and negative moods among Latina adolescents. This study offers initial sleep-mood data specific to Latina adolescents, which can inform further research and current strategies nurses and other health professionals use to promote the well-being of Latina adolescents.
Latina adolescents in this study reported sleep that was on average 2 hr below the 9 hr recommended for adolescents (Carskadon, 2009); there is no research to date to indicate that Latina adolescents require fewer hours of sleep than the recommended 9 hr. Inadequate sleep has been associated with negative outcomes for mental health, physical health, academic behavior, and other behavior problems (Dahl & Lewin, 2002; Danner & Phillips, 2008; Davis et al., 2013; Lee et al., 2012; McKnight-Eily et al., 2011; James et al., 2011; Landis et al., 2009). Compared to their non-Latina peers, Latina adolescents disproportionately report higher rates of depressive symptoms and suicidal ideation (Garcia et al., 2008). They also experience high dropout rates (up to 40% of Latino youth are not completing high school in the United States (PEW, 2004)), which means existing high school student data for Latina students are potentially underestimating health and academic problems because those at greatest risk and with health problems have already left the school environment. Although this study did not examine reasons for inadequate sleep, literature demonstrates a preponderance of stressors (e.g., racism, sibling caretaking, domestic violence, neighborhood safety, poverty, teen dating violence, documentation status of self or family members) and risk factors (e.g., limited physical activity, obesity) experienced by some Latina adolescents that could contribute to inadequate sleep (Garcia & Lindgren, 2009; Garcia & Duckett, 2009). These relationships warrant exploration and, to date, remain understudied.
The relationship of sleep and mood was demonstrated, and among this community sample of Latina adolescents, their negative mood predicted poorer sleep quality the following night. The prevalence of depressive symptoms and suicidal ideation among Latina adolescents necessitates attention to this relationship because having a negative mood is common for many of these youth. This is particularly concerning for youth who might experience both poor sleep quality and inadequate sleep; how often this is occurring among Latina adolescents is unknown, yet it is important. Inadequate sleep that is of high quality is likely to be more protective than inadequate sleep that is of poor quality. There is benefit, then, to understanding the possible mechanisms of action for negative mood to influence sleep quality so that one can intervene.
Feasibility of EMA via Text Messaging
This study demonstrated the feasibility of collecting EMA through SMS-based text messaging with adolescents. This approach capitalizes on real-time data collection protocols and enables the documentation of participants’ thoughts, feelings, and behaviors at the time they are being thought, felt, or done. The development of a university-based system linked to an existing Web-based Application Programming Interface (i.e., Twilio) proved to be efficient and secure. The findings of this study suggest that it is possible to employ realtime data collection protocols using a cell phone and texting technology. Achieving immediate awareness of responses, as well as monitoring compliance daily, allowed timely response to and follow-up with participants.
Implications for Nursing
This study did not test interventions that nurses and other healthcare providers, in addition to parents, can use to encourage adequate sleep and positive mood among Latina adolescents. But the relationship between mood and sleep for Latina adolescents, and the understanding in general of the importance of sleep for adolescents, can inform the ways in which sleep and positive mood are promoted.
It is likely not possible to eliminate negative mood from occurring in some adolescents, and indeed, the etiology of negative mood is multifaceted, complex, and unique to each adolescent. Nevertheless, nurses should seek to understand the stressors and factors in the lives of an adolescent that are contributing to an adolescent having a negative mood. Existing adolescent health literature emphasizes the importance of healthy stress response and coping behaviors (Garcia, Pintor, Vazquez, & Alvarez-Zumarraga, 2013); clinicians should help adolescents recognize their primary coping strategies and offer tools that strengthen positive coping. This has potential to minimize negative mood and indirectly encourage sleep quality.
Nurses in primary care settings, schools, or other community settings are in optimal positions to ask about mood and sleep problems. Nurses can assess for warning signs of maladaptive coping strategies, ruminating behaviors (worrying), emotional arousal, behavioral dysregulation, and high-risk behaviors that can perpetuate the negative mood and subsequent sleep problems (El-Sheikh, Buckhalt, Cummings, & Keller, 2007; Meltzer & Mindell, 2006). In clinic settings, nurses and other health professionals can use developmentally appropriate screening tools to assess sleep during health visits. Often sleep problems are not the primary concern of teens during health visits, and, unless specifically asked about, can be overlooked. Sleep assessment should include all areas of the teen’s sleep habits, including caffeine consumption, evening routine, bedtime, sleep environment (co-sleeping, television in the room, sharing a room), emotional states during bedtime (i.e., sad, worried, scared, or lonely), and presence of nightmares or other parasomnias.
Stress and coping literature offers numerous strategies that have demonstrated success among adolescents in reducing stress and stress response and improving health and well-being, including mood. For example, nurses can teach strategies such as meditation, health realization, mindfulness, yoga, breathing, exercise, and healthy eating behaviors (i.e., Black, Sussman, Johnson, & Milam, 2012; Gould, Dariotis, Mendelson, & Greenberg, 2012; Schonert-Reichl & Lawlor, 2010). Furthermore, helping youth make cognitive shifts by restructuring sleep expectations, and learning and using positive self-statements can be effective ways to improve sleep (Meltzer & Mindell, 2006). It is apparent that a thorough approach is needed to understand each adolescent’s unique composition of risk and protective factors, internal and external, in order to identify causes and interventions that optimize health, including sleep, and minimize health problems.
Existing literature demonstrates numerous strategies that nurses and parents can do or advocate for in promoting adequate, quality sleep among adolescents. Nurses can work with parents to create a home environment conducive for sleep, such as quieting the home at bedtime, decreasing marital discord and fighting before bed, and establishing nightly routines. Similarly, parental oversight of technology use (i.e., text messaging) around bedtime could promote healthy sleep patterns among adolescents, and minimize tiredness (Van den Bulck, 2007) and other harmful effects of insufficient sleep. Lastly, although setting one’s bedtime is an expression of increasing adolescent autonomy and independence (Carskadon, 2011), earlier parent-set bedtimes have been shown to be protective against depression and suicidal ideation as a specific strategy to increase sleep duration among adolescents (Gangwisch et al., 2010). Differences in sleep patterns by gender (Lee, McEnany, & Weekes, 1999) and chronotype (morning/evening) (Dagys et al., 2012) demonstrate the importance of understanding individual adolescent sleep needs and tailoring health promotion messaging and interventions appropriately; these were not examined in this study but are important aspects of consideration in future research and in practice.
Nurses and other healthcare providers can partner with academic institutions to advocate for research-informed practice, specifically high school start times that have demonstrated influence on adolescent sleep, mood, and behavior (Danner & Phillips, 2008; Noland et al., 2009; Owens, Belon, &Moss, 2010).
Limitations
There are several limitations to this study. The pilot nature of the study and small sample size limit the generalizability of the findings. Only females participated, limiting relevance for adolescent males. Data on the participant’s chronotype (morningness versus eveningness) were not collected, nor were there any objective measures of sleep quantity and quality. Participants’ overall mental state (i.e., diagnosis of major depressive disorder or anxiety disorder) could also influence the sleep–mood relationship, and was not considered in these analyses. Future studies could explore the potential mediating role of factors such as chronotype and overall mental health on the relationships between sleep and mood. As previously discussed, given our inability to examine individual adolescent sleep needs, future research must explore methods for tailoring health promotion messaging and interventions appropriately. Finally, we must note that this study is underpowered, which has an impact on our lack of statistically significant findings in some of the results.
Conclusion
Healthcare providers are in unique positions to promote healthy adolescent growth and development, to identify potential risk factors associated with sleep and mood, and to partner with adolescents and their parents/guardians to ensure that basic health needs are met, including adequate sleep. Given the link between sleep and mental health and the fact that Latina adolescents disproportionately have mental health problems, there is reason for concern, attention, and intervention. Nurses and other healthcare providers are positioned to recognize the complex interplay of factors influencing the health of Latina adolescents, including mood and sleep, and to suggest strategies and interventions that minimize health problems associated with negative moods and inadequate or poor sleep, and promote mental health and overall well-being.
Acknowledgments
Funding support was received from a 2012 Midwest Nursing Research Society Seed Grant, a 2011 University of Minnesota Grant-in-Aid award, the University of Minnesota Emerging Child and Family Health Promotion Nursing Scientist Program, and the University of Minnesota School of Nursing Foundation. Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR000114. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Study data were collected and managed using REDCap, an electronic data capture tool hosted at the University of Minnesota. We acknowledge the adolescents willing to pretest the YEMAS system for us, and the participants willing to engage in this study using texting. We also thank the school-based staff who facilitated recruitment and project site activities (Claudia Perez Inzunza, Kevin Burns, Andrea Dickinson).
Footnotes
Conflict of Interest
The authors report no actual or potential conflicts of interest.
Contributor Information
Carolyn Garcia, Associate Professor, School of Nursing, University of Minnesota, Minneapolis, Minnesota.
Lei Zhang, Research Fellow, Biostatistical Design and Analysis Center, University of Minnesota, Minneapolis, Minnesota.
Katie Holt, Home Care Nurse, Pediatric Home Care, School of Nursing, University of Minnesota, Minneapolis, Minnesota.
Rachel Hardeman, Postdoctoral Fellow, Department of Medicine, University of Minnesota and Center for Chronic Disease Outcomes Research, Minneapolis Veterans Affairs Medical Center, Minneapolis, Minnesota.
Barbara Peterson, Clinical Assistant Professor, School of Nursing, University of Minnesota, Minneapolis, Minnesota, USA.
References
- Aldridge AA, & Roesch SC (2008a). Coping with daily stressors: Modeling intraethnic variation in Mexican American adolescents. Hispanic Journal of Behavioral Sciences, 30(3), 340–356. doi: 10.1177/0739986308318708 [DOI] [Google Scholar]
- Aldridge AA, & Roesch SC (2008b). Developing coping typologies of minority adolescents: A latent profile analysis. Journal of Adolescence, 31(4), 499–517. doi: 10.1016/j.adolescence.2007.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armey MF, Crowther JH, & Miller IW (2011). Changes in ecological momentary assessment reported affect associated with episodes of nonsuicidal self-injury. Behavior Therapy, 42(4), 579–588. doi: 10.1016/j.beth.2011.01.002 [DOI] [PubMed] [Google Scholar]
- Berkel C, Knight GP, Zeiders KH, Tein J, Roosa MW, Gonzales NA, & Saenz D. (2010). Discrimination and adjustment for Mexican American adolescents: A prospective examination of the benefits of culturally related values. Journal of Research on Adolescence, 20(4), 893–915. doi: 10.1111/j.1532-7795.2010.00668.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black DS, Sussman S, Johnson CA, & Milam J (2012). Testing the indirect effect of trait mindfulness on adolescent cigarette smoking through negative affect and perceived stress mediators. Journal of Substance use, 17(5–6), 417–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand S, Beck J, Kalak N, Gerber M, Kirov R, Pühse U, & Holsboer-Trachsler E (2011). Dream recall and its relationship to sleep, perceived stress, and creativity among adolescents. Journal of Adolescent Health, 49(5), 525–531. doi: 10.1016/j.jadohealth.2011.04.004 [DOI] [PubMed] [Google Scholar]
- Carbonell DM, Reinherz HZ, & Beardslee WR (2005). Adaptation and coping in childhood and adolescence for those at risk for depression in emerging adulthood. Child & Adolescent Social Work Journal, 22(5–6), 395–416. doi: 10.1007/210560-005-0019-4 [DOI] [Google Scholar]
- Carskadon MA (2009). Adolescents and sleep: Why teens can’t get enough of a good thing. Brown University Child & Adolescent Behavior Letter, 25(4), 1. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=rzh&AN=2010229492&site=ehost-live [Google Scholar]
- Carskadon MA (2011). Sleep in adolescents: The perfect storm. Pediatric Clinics of North America, 58(3), 637–647. doi: 10.1016/j.pcl.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez NR, & French SE (2007). Ethnicity-related stressors and mental health in Latino Americans: The moderating role of parental racial socialization. Journal of Applied Social Psychology, 37(9), 1974–1998. doi: 10.1111/j.1559-1816.2007.00246.x [DOI] [Google Scholar]
- Collins LR, Kashdan TB, & Gollnisch G (2003). The feasibility of using cellular phones to collect ecological momentary assessment data: Application to alcohol consumption. Experimental and Clinical Psychopharmacology, 11(1), 73. doi: 10.1177/0017896910364831 [DOI] [PubMed] [Google Scholar]
- Compas BE, ConnorSmith JK, Saltzman H, Thomsen AH, & Wadsworth ME (2001). Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin, 127(1), 87–127. doi: 10.1037/0033-2909.127.1.87 [DOI] [PubMed] [Google Scholar]
- Crawford JR, & Henry JD (2004). The positive and negative affect schedule (PANAS): Construct validity, measurement properties, and normative data in a large non-clinical sample. British Journal of Clinical Psychology, 43(3), 245–265. doi: 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- Dagys N, McGlinchey EL, Talbot LS, Kaplan KA, Dahl RE, & Harvey A (2012). Double trouble? The effects of sleep deprivation and chronotype on adolescent affect. Journal of Child Psychology & Psychiatry, 53(6), 660–667. doi: 10.1111/j.1469-7610.2011.02502.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl RE, & Lewin DS (2002). Pathways to adolescent health: Sleep regulation and behavior. Journal of Adolescent Health, 31(6), 175–184. doi: 10.1016/S1054-139X(02)00506-2 [DOI] [PubMed] [Google Scholar]
- Danner F, & Phillips B (2008). Adolescent sleep, school start times, and teen motor vehicle crashes. Journal of Clinical Sleep Medicine, 4(6), 533–535. [PMC free article] [PubMed] [Google Scholar]
- Davis AL, Avis KT, & Schwebel DC (2013). The effects of acute sleep restriction on adolescents’ pedestrian safety in a virtual environment. Journal of Adolescent Health, 53(6), 785–790. doi: 10.1016/j.jadohealth.2013.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DHHS. (2001). Mental health: Culture, race, and ethnicity. A supplement to mental health: A report of the surgeon general. Washington, DC: Department of Health and Human Services, U.S. Public Health Service. [PubMed] [Google Scholar]
- Duarté-Vélez YM, & Bernal G (2007). Suicide behavior among Latino and Latina adolescents: Conceptual and methodological issues. Death Studies, 31 (5), 435–455. doi: 10.1080/07481180701244579 [DOI] [PubMed] [Google Scholar]
- Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, & Croft JB (2010). Prevalence of insufficient, borderline, and optimal hours of sleep among high school students—United States, 2007. Journal of Adolescent Health, 46(4), 399–401. doi: 10.1016/j.jadohealth.2009.10.011 [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA, Cummings EM, & Keller P (2007). Sleep disruptions and emotional insecurity are pathways of risk for children. Journal of Child Psychology and Psychiatry, 48(1), 88–96. doi: 10.1111/j.1436-7610.2006.0160.x [DOI] [PubMed] [Google Scholar]
- Elkington KS, Bauermeister JA, & Zimmerman MA (2010). Psychological distress, substance use, and HIV/STI risk behaviors among youth. Journal of Youth and Adolescence, 39(5), 514–527. doi: 10.1007/s10964-010-9524-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes EE, Stepp SD, Dahl RE, Ryan ND, Whalen D, Axelson DA, … Silk JS (2012). Real-world affect and social context as predictors of treatment response in child and adolescent depression and anxiety: An ecological momentary assessment study. Journal of Child and Adolescent Psychopharmacology, 22(1), 37–47. doi: 10.1089/cap.2011.0085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster M, Dyal S, Baezconde-Garbanati L, Chou C, Soto D, & Unger J (2013). Bullying victimization as a mediator of associations between cultural/familial variables, substance use, and depressive symptoms among Hispanic youth. Ethnicity & Health, 18(4), 415–432. doi: 10.1080/13557858.2012.754407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, & Posner K (2010). Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep, 33(1), 97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C, Hardeman R, Kwon G, Lando-King E, Genis T, Brady SS, & Zhang L (2014). Teens text, a lot: Use of YEMAS (Youth Ecological Momentary Assessment System) in trajectory research with adolescents. JMIR mHealth & uHealth, 2(1), e3. doi: 10.2196/mhealth.2576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia C, & Lindgren S (2009). “Life grows between the rocks”: Latino adolescents’ and parents’ perspectives on mental health stressors. Research in Nursing & Health, 32(2), 148–162. doi: 10.1002/nur.20317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia CM, & Duckett LJ (2009). No te entiendo y tú no me entiendes: Language barriers among immigrant Latino adolescents seeking health care. Journal of Cultural Diversity, 16(3), 120–126. [PMC free article] [PubMed] [Google Scholar]
- Garcia C, Pintor J, Vazquez G, & Alvarez-Zumarraga E (2013). Project wings, a coping intervention for Latina adolescents: A pilot study. Western Journal of Nursing Research, 35(4), 434–458. [DOI] [PubMed] [Google Scholar]
- Garcia C, Skay C, Sieving R, Naughton S, & Bearinger L (2008). Family and racial factors associated with suicide and emotional distress among Latino students. Journal of School Health, 78(9), 487–495. doi: 10.1111/j.1746-1561.2008.00334.x [DOI] [PubMed] [Google Scholar]
- Gould LF, Dariotis JK, Mendelson T, & Greenberg MT (2012). A school-based mindfulness intervention for urban youth: Exploring moderators of intervention effects. Journal of Community Psychology, 40(8), 968–982. [Google Scholar]
- Hagenauer MH, Perryman JI, Lee TM, & Carskadon MA (2009). Adolescent changes in the homeostatic and circadian regulation of sleep. Developmental Neuroscience, 31 (4), 276–284. doi: 10.1159/000216538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James JE, Kristjánsson A, & Sigfúsdóttir I (2011). Adolescent substance use, sleep, and academic achievement: Evidence of harm due to caffeine. Journal of Adolescence, 34(4), 665–673. doi: 10.1016/j.adolescence.2010.09.006 [DOI] [PubMed] [Google Scholar]
- Landis AM, Parker KP, & Dunbar SB (2009). Sleep,hunger, satiety, food cravings, and caloric intake in adolescents. Journal of Nursing Scholarship, 41(2), 115–123. doi: 10.1111/j.1547-5069.2009.01262.x [DOI] [PubMed] [Google Scholar]
- Lee KA, McEnany G, & Weekes D (1999). Gender differences in sleep patterns for early adolescents. Journal of Adolescent Health, 24(1), 16–20. doi: 10.1016/S1054-139X(98)00074-3 [DOI] [PubMed] [Google Scholar]
- Lee YJ, Cho S-J, Cho IH, & Kim SJ (2012). Insufficient sleep and suicidality in adolescents. Sleep, 35(4), 455–460. doi: 10.5665/sleep.1722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowry R, Crosby AE, Brener ND,& Kann L (2013). Suicidal thoughts and attempts among U.S. high school students: Trends and associated health-risk behaviors, 1991–2011. Journal of Adolescent Health, 54(1), 100–108. doi: 10.1016/j.jadohealth.2013.07.024 [DOI] [PubMed] [Google Scholar]
- McKnight-Eily L, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, & Perry GS (2011). Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive Medicine, 53(4–5), 271–273. doi: 10.1016/j.ypmed.2011.06.020 [DOI] [PubMed] [Google Scholar]
- Minnesota Department of Education. (2006). Minnesota Student Survey. Minnesota Department of Education. Retrieved January 7, 2007, from http://education.state.mn.us/MDE/Learning_Support/Safe_and_Healthy_Learners/Minnesota_Student_Survey/index.html
- Minnesota Department of Health. (2007). Suicidal thoughts or attempts and youth risk and protective factors: 2007 Minnesota Student Survey statewide data: 9th grade students. Minnesota Department of Health. [Google Scholar]
- Meijer AM, Reitz E, Dekovi M, van den Wittenboer GL, & Stoel RD (2010). Longitudinal relations between sleep quality, time in bed and adolescent problem behaviour. Journal of Child Psychology & Psychiatry, 51(11), 1278–1286. doi: 10.1111/j.1469-7610.2010.02261.x [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, & Mindell JA (2006). Sleep and sleep disorders in children and adolescents. Psychiatric Clinics of North America, 29, 1059–1076. doi: 10.1016/j.psc.2006.08.004 [DOI] [PubMed] [Google Scholar]
- Mulye TP (2009). Trends in adolescent and young adult health in the United States. Journal of Adolescent Health, 45(1), 8. doi: 10.1016/j.jadohealth.2009.03.013 [DOI] [PubMed] [Google Scholar]
- Nielsen. (2010). U.S. teen mobile report calling yesterday, texting today, using apps tomorrow. Retrieved September 28, 2013, from http://www.nielsen.com/us/en/newswire/2010/u-s-teen-mobile-report-calling-yesterday-texting-today-using-apps-tomorrow.html
- Noland H, Price JH, Dake J, & Telljohann SK (2009). Adolescents’ sleep behaviors and perceptions of sleep. Journal of School Health, 79(5), 224–230. doi: 10.1111/j.1746-1561.2009.00402.x [DOI] [PubMed] [Google Scholar]
- Owens JA, Belon K, & Moss P. (2010). Impact of delaying school start time on adolescent sleep, mood, and behavior. Archives of Pediatrics & Adolescent Medicine, 164(7), 608–614. doi: 10.1001/archpediatrics.2010.96 [DOI] [PubMed] [Google Scholar]
- Pallesen S, Saxvig IW, Molde H, Sørensen E, Wilhelmsen-Langeland A, & Bjorvatn B (2011). Brief report: Behaviorally induced insufficient sleep syndrome in older adolescents: Prevalence and correlates. Journal of Adolescence, 34(2), 391–395. doi: 10.1016/j.adolescence.2010.02.005 [DOI] [PubMed] [Google Scholar]
- Peach HD, & Gaultney JF (2013). Sleep, impulse control, and sensation-seeking predict delinquent behavior in adolescents, emerging adults, and adults. Journal of Adolescent Health, 53(2), 293–299. doi: 10.1016/j.jadohealth.2013.03.012 [DOI] [PubMed] [Google Scholar]
- PEW. (2004). Latino teens staying in high school: A challenge for all generations. Pew Hispanic Center Fact Sheet. Retrieved on February 5,2012, from www.pewhispanic.org [Google Scholar]
- Rofey DL, Hull EE, Phillips J, Vogt K, Silk JS, & Dahl RE (2010). Utilizing ecological momentary assessment in pediatric obesity to quantify behavior, emotion, and sleep. Obesity, 18(6), 1270–1272. doi: 10.1038/oby.2009.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute. (2012). SAS system, v. 9.3. Carey, NC: Author. [Google Scholar]
- Schonert-Reichl KA, & Lawlor MS (2010). The effects of a mindfulness-based education program on pre- and early adolescents’ well-being and social and emotional competence. Mindfulness, 1(3), 137–151. [Google Scholar]
- Schwarz SW (2009). Adolescent mental health in the United States: Facts for policymakers. Retrieved February 16, 2011, from http://nccp.org/publications/pdf/text_878.pdf
- Shrier LA, Feldman HA, Black SK, Walls C, Kendall AD, Lops C, & Beardslee WR (2012). Momentary affective states surrounding sexual intercourse in depressed adolescents and young adults. Archives of Sexual Behavior, 41(5), 1161–1171. doi: 10.1007/s10508-011-9787-4 [DOI] [PubMed] [Google Scholar]
- Shrier LA, Shih M, Hacker L, & de Moor C (2007). A momentary sampling study of the affective experience following coital events in adolescents. Journal of Adolescent Health, 40, 357.e1. doi: 10.1016/j.jadohealth.2006.10.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theokas C (2006). Observed ecological assets in families, schools, and neighborhoods: Conceptualization, measurement, and relations with positive and negative developmental outcomes. Applied Developmental Science, 10(2), 61. doi:http://128.104.248.62/ces/4h/educators/documents/TheokasLerner.pdf [Google Scholar]
- Umaña-Taylor AJ, & Updegraff KA (2007). Latina adolescents’ mental health: Exploring the interrelations among discrimination, ethnic identity, cultural orientation, self-esteem, and depressive symptoms. Journal of Adolescence, 30(4), 549–567. doi: 10.1016/j.adolescence.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Vallido T, Peters K, O’Brien L, & Jackson D (2009). Sleep in adolescence: A review of issues for nursing practice. Journal of Clinical Nursing, 18(13), 1819–1826. doi: 10.1111/j.1365-2702.2009.02812.x [DOI] [PubMed] [Google Scholar]
- Van den Bulck J (2007). Adolescent use of mobile phones for calling and for sending text messages after lights out: Results from a prospective cohort study with a one-year follow-up. Sleep, 30(9), 1220–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenze SJ, & Miller IW (2010). Use of ecological momentary assessment in mood disorders research. Clinical Psychology Review, 30(6), 794–804. doi: 10.1016/j.cpr.2010.06.007 [DOI] [PubMed] [Google Scholar]
- Yip T (2013). The effects of ethnic/racial discrimination and sleep quality on depressive symptoms and self-esteem trajectories among diverse adolescents. Journal of Youth and Adolescence. doi: 10.1007/s10964-014-0123-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas L, Gulbas LE, Fedoravicius N, & Cabassa LJ (2010). Patterns of distress, precipitating events, and reflections on suicide attempts by young Latinas. Social Science & Medicine, 70(11), 1773–1779. doi: 10.1016/j.socscimed.2010.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]


