Abstract
Background
The main adverse effect is gastroesophageal reflux disease (GERD), with concern on the development of Barrett's esophagus and esophageal adenocarcinoma in the long term. However, the relationship between SG and GERD is complex. The aim of this study is to systematically evaluate all published data existing in the literature to evaluate the effect of sleeve gastrectomy on GERD, esophagitis, BE in order to clarify the long-term clinical sequelae of this procedure.
Materials and methods
This systematic review was conducted in accordance with the guidelines for Preferred Reporting Items for Systematic Review. The work has been reported in line with the PRISMA criteria [19]. We evaluated the quality and risk of bias of this Systematic Review using AMSTAR 2 checklist [20]. Published studies that contained outcome data for primary sleeve gastrectomy associated with the primary and secondary outcomes listed below were included. The UIN for ClinicalTrial.gov Protocol Registration and Results System is: NCT05178446 for the Organization UFoggia.
Results
49 articles were eligible for inclusion that met the following criteria: publications dealing with patients undergoing laparoscopic SG, publications describing pre- and postoperative GERD symptoms and/or esophageal function tests, articles in English, human studies and text complete available.
Conclusions
We have controversial data on LSG and GERD in the literature as there is a multifactorial relationship between LSG and GERD. The most recent studies have shown satisfactory control of postoperative reflux in most patients and low rates of de novo GERD. These data are leading to wider acceptance of LSG as a bariatric procedure even in obese patients with GERD.
Keywords: Sleeve gastrectomy, Bariatric surgery, Obesity, Gastrectomy, Gastric sleeve, Stomach staple, Gastroesophageal reflux, Reflux, Metaplasia, Barrett's esophagus
Highlights
-
•
The aim of this study is to evaluate the effect of sleeve gastrectomy on GERD.
-
•
In the literature there are controversial results on the onset of GERD after LSG.
-
•
Satisfactory control of postoperative reflux in most patients and low rates of de novo GERD.
-
•
These data are leading to wider acceptance of LSG as a bariatric procedure even in obese patients with GERD.
1. Introduction
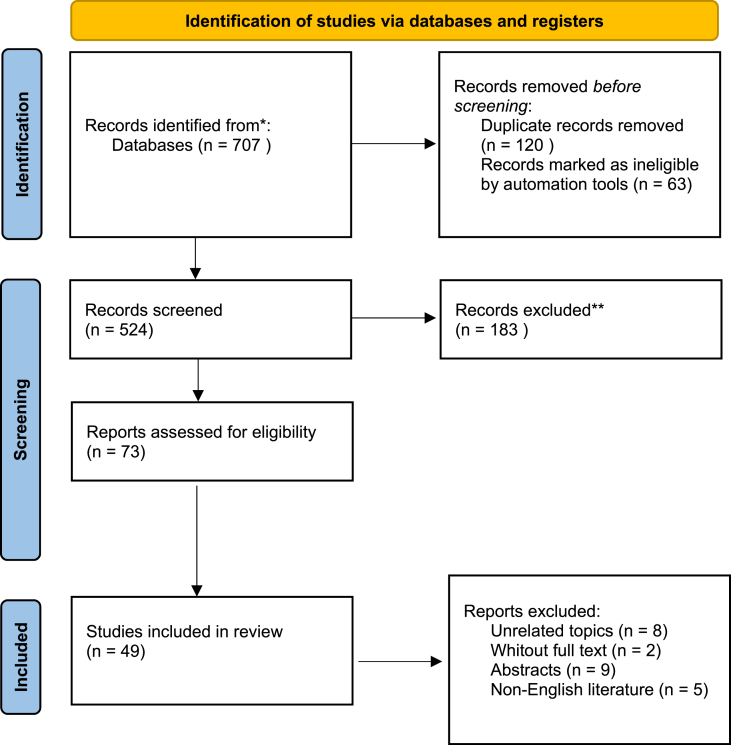
Obesity is classified as one of the most severe global public health problems. Over 2.1 billion adults worldwide are considered overweight or obese; 640 million of these are classified as obese. Sleeve gastrectomy (SG) has become the most common procedure performed in the world since 2014 [1] because it is well defined, it is easier to perform than other types of bariatric surgery, the learning curve is shorter, the morbidity and mortality rates are low, and it leads to effective weight loss [2]. Obese patients develop obesity-related comorbidities including type 2 diabetes mellitus (T2DM), hypertension, dyslipidemia, coronary artery disease, certain types of cancer, and gastroesophageal reflux disease (GERD) [[3], [4], [5], [6], [7]]. The main adverse effect is gastroesophageal reflux disease (GERD), with concern on the development of Barrett's esophagus and esophageal adenocarcinoma in the long term. However, the relationship between SG and GERD is complex [[8], [9], [10], [11], [12]]. Different mechanisms involved: disruption of the angle of His, partial sectioning of sling fibers of the lower esophageal sphincter (LES), reduced gastric compliance due to gastric fundus removal, occurrence of hiatal hernia (HH), or reduced antral function. In contrast, other studies have reported a decreased prevalence of GERD after SG [[13], [14], [15]] explained by several mechanisms including weight loss, decreased acid production and accelerated gastric emptying. The measured increase in GERD prevalence ranged from 2.1% to 34.9% in the analyzed literature. There was marked heterogeneity between the studies in regard to a number of factors including preoperative BMI, method of evaluating GERD, exclusion criteria, length of follow-up, and operative technique [[16], [17], [18]] [[16], [17], [18]] [[16], [17], [18]].(see fig 1)
Figure 1.
PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers only.
The aim of this study is to systematically evaluate all published data existing in the literature to evaluate the effect of sleeve gastrectomy on GERD, esophagitis, BE in order to clarify the long-term clinical sequelae of this procedure.
2. Materials and methods
This systematic review was conducted in accordance with the guidelines for Preferred Reporting Items for Systematic Review. The work has been reported in line with the PRISMA 2020 criteria [19].
We evaluated the quality and risk of bias of this Systematic Review using AMSTAR 2 checklist [20].
A systematic search was performed using electronic searches in EMBASE, Medline, Cochrane Library, and Psychinfo. Free text search in all fields was performed for “Sleeve Gastrectomy”, “Bariatric Surgery”, “Obesity”, “Gastrectomy”, “Gastric Sleeve”, “Stomach Staple”, “Gastroesophageal Reflux”, “Gastro - Esophageal reflux "," Reflux "," Metaplasia "," Barrett's esophagus “and” Barrett's esophagus”. The search included all study designs, with additional non-research captured studies identified through bibliographic cross-references.
Published studies that contained outcome data for primary sleeve gastrectomy associated with the primary and secondary outcomes listed below were included.
The UIN for ClinicalTrial.gov Protocol Registration and Results System is: NCT05178446for the Organization UFoggia (https://clinicaltrials.gov/ct2/show/NCT05178446).
3. Results
Figure (PRISMA Flow Chart) shows the study selection flowchart. Through the literature search, we identified 707 citations. We removed any duplicates and were left with 120 references. After excluding irrelevant reports by reviewing titles and abstracts, we then retrieved 73 full-text articles that were eligible. There were 8 articles with unrelated topics, 2 without full text, 9 conference abstracts, and 5 non-English/Chinese literatures excluded. Ultimately, 49 original articles were included, as shown in the study flowchart(Table 1). [[22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61], [62], [63], [64], [65], [66], [67], [68], [69]].
Table 1.
Systematic review.
| Investigatiors Table 1: Systematic Review |
Title of study | Year | Patients (n) | Preoperative BMI (kg/m^2) | Reflux evaluation | Follow-up (mo) | GERD (%) |
Bougie size (F) | |
|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | ||||||||
| M.E. Abd Ellatif et al. [16] | Long term predictors of success after laparoscopic sleeve gastrectomy | 2014 | 1395 | 46 | Upper GI endoscopy | 84 | 11.4 | <36 (837) - >44 (558) | |
| Albanopoulos et al. [17] | The impact of laparoscopic sleeve gastrectomy on weight loss and obesity-associated comorbidities: the results of 3 years of follow up | 2016 | 88 | 47.8 | Symptoms | 36 | 27 | 9.2 | 34 |
| Alexandrou et al. [18] | Laparoscopic sleeve gastrectomy for morbid obesity: 5 year results | 2015 | 30 | 55.5 ± 1.7 | Esofagogastroscopy | 60 | 16 | 29 | |
| Althuwaini et al. [19] | Prevalence and predictors of gastroesophageal reflux disease after laparoscopic sleeve gastrectomy | 2018 | 213 | 47,84 | GERD-Health-Related-Quality of Life questionnaire | 12 | 47% | 32 | |
| Angrisani et al. [20] | Five year results of laparoscopic sleeve gastrectomy: effects on gastroesophageal reflux disease symptoms and co-morbidities | 2016 | 105 | group1: <50; group2:>50 | symptoms, gastrointestinal endoscopy, double contrast barium swallow | 60 | group 1: 31% group 2: 25% | group 1: 18,2% group: 20% | 40 |
| Arman et al. [21] | Long-term (11+years) outcomes in weight patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy | 2016 | 110 | 38,8 | medication use | 132 | 11.1 | 21.4 | 34 |
| Barr et al. [22] | GERD and acid reduction medication use following gastric bypass and sleeve gastrectomy | 2017 | 147 | 49.1 ± 8 | acid reduction medication (ARM) utilization, Gastroesophageal reflux disease health-related quality of life (GERD-HRQL) | 12 | N.R. | N.R. | 36–40 |
| Barry et al. [23] | Laparoscopic vertical sleeve gastrectomy: a 5 year veterans affairs review | 2017 | 223 | 45.4 (from 33 to 56.6) | medication use | 60 | 56 | 13 | 34 |
| Berry et al. [24] | Sleeve gastrectomy outcomes in patients with BMI between 30 and 35-3 years of follow-up | 2018 | 252 | 32.3 (30–35) | gastrointestinal endoscopy, barium esophagogram, esophageal manometry, esophageal pH test | 36 | 25,43 | 64,6 improvement of their symptoms - 2.4 de novo symptoms | 36 |
| Borbely et al. [25] | De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux | 2018 | 222 | 49.6 ± 7.2 | questionnaires, upper endoscopy, 24 h-pH manometry, esophagogram, medication use | 32 | 25 silent GERD preop - 23 with preoperative diagnosis of GERD | 52 | 32 |
| Boza et al. [26] | Long-term outcomes of laparoscopic sleeve gastrectomy as a primary bariatric procedure | 2014 | 161 | 34.9 (33.3–37.5) | GERD symptoms questionnaires, endoscopy | 60 | 4.3 | 26.7 | 60 |
| Braghetto et al. [27] | Prevalence of Barrett's esophagus in bariatric patients undergoing sleeve gastrectomy | 2016 | 231 | 38.4 + 3.1 | clinical evaluation, Endoscopy | 60 | 0 (patients with GERD didn't undergo sleeve gastrectomy) | 23.2 | 34 |
| Braghetto et al. [28] | Late esophagogastric anatomic and functional changes after sleeve gastrectomy and its clinical consequences with regards to gastroesophageal reflux disease | 2019 | 248 | 38.4 ± 3,4 | reflux symptoms and Upper gastrointestinal ednoscopy | 60 | 0 | 65,1 | N.R. |
| Burgerhart et al. [29] | Effect of sleeve gastrectomy on gastroesophageal reflux | 2014 | 20 | 47.6 ± 6.1 | esophageal function tests (high resolution manometry and 24-h pH impedence metry); reflux disease questionnaire | 3 | 70 | 20 | 34 |
| Carabotti et al. [30] | Impact of laparoscopic sleeve gastrectomy on upper gastrointestinal symptoms | 2013 | 97 | respondent patients: 45.9; non respondent patients: 43.3 | questionnaire for upper GI symptoms following Roma III criteria | 13 | 27 | 25,67 | 42 |
| Carter et al. [31] | Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy | 2011 | 206 | 46.6 | symptoms, medication use, upper gastrointestinal radiography | 24 | 34.6 | 49 complained of immediate GERD symptoms; 47.2had persistent GERD symptoms that lasted >1 month after LSG; 33.8% were taking medication specifically for GERD after LSG | 34 |
| Castagneto Gissey et al. [32] | 10-year follow-up after laparoscopic sleeve gastrectomy: outcomes in a monocentric series | 2018 | 182 | 46.6 ± 7.3 | clinical symptomatology referred by patients on a symptom assessment scale, esophagogastroduodenoscopy if necessary | 120 | 18.9 | 42.9 | 48 |
| Catheline et al. [33] | Five year results of sleeve gastrectomy | 2013 | 65 | 49.9 ± 9.1 range (35.7–71.8) | PPI medication, symptoms, endoscopy | 60 | 11.1 | 33.3 | 34 |
| Chuffart et al. [34] | Long-term results after sleeve gastrectomy for gastroesophageal reflux disease: a single-center French study | 2017 | 64 | 47 ± 8 | upper GI endoscopy, symptoms, medication (PPI) | 72 | 26.8 | 42 | 36 |
| Coupaye et al. [35] | Gastroesophageal reflux after sleeve gastrectomy: a prospective mechanistic study | 2018 | 119 | 43.3 ± 5.7 | HRM(high-resolution esophageal manometry), APM(ambulatory 24-h esophageal pH monitoring), upper endoscopy | 12 | 34 | 52 (patients without preoperative GERD); 56,25 (patients with preoperative GERD) | 36 |
| Dakour Aridi et al. [36] | Gastroesophageal reflux disease after laparoscopic sleeve gastrectomy with concomitant hiatal hernia repair: an unresolved question | 2017 | 165 | 44.1 ± 10.7 (LSG), 42.7 ± 15.3 (LSG + HHR) | symptoms, PPI use | 24 | 41.6 (LSG)61.8 (LSG + HHR) | 46.2 (LSG) - 41.4 (LSG + HHR) | 36/40 |
| Del Genio et al. [37] | Sleeve Gastrectomy and development of “de novo” gastroesophageal reflux | 2014 | 25 | 46.1 (38–58) | multichannel intraluminal impedance and pH (MII-pH), High-resolution manometry with impedance (HRiM), questionnaire | 13 (11–17) | N.R. | N.R. | 40 |
| DuPree et al. [38] | Laparoscopic sleeve gastrectomy in patients with preexisting Gastroesophageal Reflux disease. A National Analysis | 2014 | 4832 | 47.9 | REflux symptoms and Upper gastrointestinal ednoscopy | 6 | 44.5 | 84.1 continued to have GERD symptoms | N.R. |
| Felsenreich et al. [39] | Update: 10 years of sleeve gastrectomy- the first 103 patients | 2018 | 103 | 49 ± 9.1 | gastroscopies, manometries, 24-h pH metries, reflux symptom index questionnaire | 120 | N.R. | 57 | N.R. |
| DM Felsenreich et al. [40] | Reflux, Sleeve Dilation, and Barret's Esophagous after Laparoscopic Sleeve Gastrectomy: Long-Term Follow-Up | 2017 | 43 | 49.5 ± 9,6 | REflux symptoms and Upper gastrointestinal ednoscopy | 129 | 0 | 38 | 42–48 |
| Flolo et al. [41] | Five-year outcomes after vertical sleeve gastrectomy for severe obesity: a prospective cohort study | 2017 | 168 | 46.2 ± 6.4 | symptoms, medication use | 60 | 12 | 35 | 32 |
| Gadiot et al. [42] | Long-term results of laparoscopic sleeve gastrectomy for morbid obesity: 5 to 8-year results | 2017 | 277 | 44.8 ± 6.7 | symptoms | 60 | 10.1 | 7 (9pz) | N.R. |
| Garg et al. [43] | Mid to long term outcomes of laparoscopic sleeve gastrectomy in Indian population: 3–7 years results - a retrospective cohort study | 2017 | 424 | 46.67 ± 15.8 | upper gastrointestinal endoscopy, GERD severity symptom questionnaire, PPI intake | 60 | 16.5 | 2.8 | 36 |
| Gemici et al. [44] | Outcomes of laparoscopic sleeve gastrectomy by means of esophageal manometry and pH-metry, before and after surgery | 2020 | 62 | 47.91 ± 6.23 | Upper gastrointestinal endoscopy, 24 h pH-monitoring (APM), Esophageal manometry (EM) | 36 | N.R. | N.R. | 36 |
| Genco et al. [45] | Gastroesophageal reflux disease and Barrett's esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication | 2017 | 162 | 45.8 ± 6.3 | visual analogue scale (VAS) evaluation of GERD symptoms, PPIs consumption recording, esophagogastroduodenoscopy (EGD) | 58 | 33.6 | 68.1 | 48 |
| Georgia et al. [46] | 24-h multichannel intraluminal impedance PH-metry 1 year after laparoscopic sleeve gastrectomy: an objective assessment of gastroesophageal reflux disease | 2017 | 12 | 48.97 | 24-h multichannel intraluminal impedance-pH metry (MIIpH) pre-and 12 months post-LSG; symptoms; EGD | 12 | 42.06.00 | 83.33 | 38 |
| Hendricks et al. [47] | Impact of sleeve gastrectomy on gastroesophageal reflux disease in a morbidly obese population undergoing bariatric surgery | 2016 | 919 | N.R. | symptoms, PPI treatment, upper gastrointestinal endoscopy (UGI), esophagogastroduodenoscopy (EGD), pH manometry | 24 | group B 1% (13) | group A 3% (25) | 38 |
| Himpens et al. [48] | Long-term results of laparoscopic sleeve gastrectomy for obesity | 2010 | 53 | 39 (range, 31–57; SD, 5.4) | Bariatric analysis and reporting outcome system (BAROS) score | 72 | 3.3 | 23 | 34 |
| Hirth et al. [49] | Laparoscopic sleeve gastrectomy: long-term weight loss outcomes | 2015 | 16 | 43.5 | medications, symptoms | 84 | 35 | 35 | 32 |
| Howard et al. [50] | Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients | 2011 | 28 | 55.5 range (39–80) | upper gastrointestinal radiographic swallow study, GERD score questionnaire, symptoms, medication use | 32 | 25 | 39 | 38 |
| Kehagias et al. [51] | Efficacy of sleeve gastrectomy as sole procedure in patients with clinically severe obesity (BMI <50 kg/m^2) | 2013 | 203 | 43.2 ± 2.8 | PPi prescription | 36 | 0 | 7,4 | 32 |
| Kowalewski et al. [52] | Long-term outcomes of laparoscopic sleeve gastrectomy-a single-center, retrospective study | 2018 | 84 | 51.6 | typical symptoms, PPi therapy | 96 | N.R. | 60 | 36 |
| Lemaitre et al. [53] | Laparoscopic sleeve gastrectomy in the South Pacific. Retrospective evaluation of 510 patients in a single institution | 2016 | 384 | 47.8 ± 7.8 | PPi therapy, endoscopic diagnosis, symptoms | 24 | N.R. | 9.4 | 33 |
| Lim et al. [54] | Correlation between symptomatic gastro-esophageal reflux disease (GERD) and erosive esophagitis (EE) post vertical sleeve gastrectomy (VSG) | 2019 | 63 | 42.1 ± 1.2 | questionnaire that included documentation of reflux symptomatology, medication use; EGD | 13 | 31.7 | 47.6 | 36 |
| Menenakos et al. [55] | Laparoscopic sleeve gastrectomy performed with intent to treat morbid obesity: a prospective single-center study of 261 patients with a median follow-up of 1 year | 2010 | 261 | 45.2 (range 32.1–72.7) | upper gastrointestinal endoscopy | 12 | N.R. | 25 | 38 |
| Nocca et al. [56] | Five-year results of laparoscopic sleeve gastrectomy for the treatment of severe obesity | 2017 | 1050 | 44.58 ± 7.71 | symptoms | 60 | 21.27 | 39.1 | 36 |
| Pilone et al. [57] | Gastroesophageal reflux after sleeve gastrectomy: new onset and effect on symptoms on a prospective evaluation | 2019 | 104 | 44.2 ± 4.2 | GERD-HRQL questionnaire, EGDS, PPI use | 12 | 27.9 | 10.6 | 32 |
| Pok et al. [58] | Laparoscopic sleeve gastrectomy in Asia: long term outcome and revisional surgery | 2016 | 61 | 37.3 ± 8.1 (range20.8–75.3) | symptoms | 60 | N.R. | 17 | 36 |
| Rawlins et al. [59] | Sleeve gastrectomy 5 year outcomes of a single institution | 2013 | 49 | 65 (range 39–106) | patient report | 60 | N.R. | 11 | 26.4 |
| Rebecchi et al. [60] | Gastroesophageal reflux disease and laparoscopic sleeve gastrectomy: a physiopathologic evaluation | 2014 | 71 | 44.3 ± 3.8 | gastroesophageal reflux disease symptom assessment scale (GSAS), esophageal manometry and 24-h pH monitoring, DeMeester composite reflux score | 48 | group A: 42.3 group B: 0 | group A: symptoms improved group B: 5.4 | 36 |
| Sharma et al. [61] | Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy | 2014 | 32 | 47.8 | Carlsson Dent Questionnaire and GERD questionnaire to assess Symptom-Severity score, upper GI endoscopy, radionuclide scintigraphy | 12 | 6.25 (2pz) | 78.1 | 36 |
| Sheppard et al. [62] | Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity | 2015 | 205 | 48.5 ± 9.7 | symptoms, medication use | 12 | 25.5 | 58 increased PPI - 42 continued the same treatment - 0 decreased | 50 |
| Soricelli et al. [63] | Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy | 2018 | 219 | 46.2 ± 7.2 | EGD, VAS evaluation of GERD symptoms, PPI consumption | 66 | 40.9 | 70.2 | 48 |
| Viscido et al. [64] | Laparoscopic sleeve gastrectomy: endoscopic findings and gastroesophageal reflux symptoms at 18-month follow-up | 2018 | 109 | 47.8 ± 16 | questionnaire, GERD symptoms, EGD | 18 | 33 | 44 | 42 |
4. Discussion
Obesity is one of the risk factors for GERD, which has resulted in a significant increase in the incidence of GERD worldwide [70].
Obesity has been reported to increase the incidence of GERD with an OR of 1.73 and Barrett's esophagus with an OR of 1.24; esophageal adenocarcinoma is the most serious complication of GERD (OR, 2.45) [71,72].
Numerous studies have been performed in the literature with controversial results on the onset of GERD after LSG.
Albanopoulos et al., Alexandrou et al. and Althuwaini et al. [22,23] showed that LSG seemed to precipitate GERD symptoms, dissection near the angle of His, and drastic reduction in gastric capacity increased the chance that patients would maintain or develop new GERD symptoms.
The studies by Arman et al., Borbely et al. and Braghetto et al. [26,30,32] found that LSG is associated with a significantly higher likelihood that acid-lowering medications are needed to control GERD symptoms 12 months after LSG compared with gastric bypass. LSG leads to a considerable rate of postoperative GERD. De novo GERD consist of approximately half of preoperative silent GERD and completely de novo GERD. Most patients with preoperative silent GERD have become symptomatic after LSG. Barrett's esophagus could be a late complication after SG and bariatric surgeons should be aware of the important association between GERD and obesity.
Burgerhart et al. [34] confirm that it seems likely that the increase in acid exposure after LSG is due to the modified anatomy, which leads to a decrease in the resting pressure of Les. The study results support the idea that in patients with significant preoperative symptoms of GERD, gastric bypass surgery may be more appropriate than LSG.
Del Genio et al. and DuPree et al. [42,43] claim that LSG is an effective restrictive procedure that creates delayed esophageal emptying without compromising the function of the LES. Retrograde movements and increased acid exposure are likely due to postprandial stasis and regurgitation. LSG did not reliably relieve or improve GERD symptoms and induced GERD in some previously asymptomatic patients.
Indeed, Flolo et al. [46] confirmed that the incidence of GERD more than doubled from baseline at 2 years and further increased at a rate of 35% at 5 years.
De novo gastroesophageal reflux symptoms appear between the third and sixth postoperative year. This unfavorable evolution may have been prevented in some patients by continuous follow-up outpatient visits beyond the third year.
The new onset of postoperative GERD is an unfortunate side effect of LSG, and more studies reflecting the aggressive closure of healing defects are needed to determine if this provides a long-term solution to this problem.
LSG can increase the prevalence of GERD despite satisfactory weight loss.
In the study by Menenakos et al. [60] about 25% of patients developed or worsened their GERD symptoms, all responsive to PPi treatment (65 out of 261 patients). Heartburn was significantly relieved after the postoperative first trimester. Symptoms of GERD are especially common in the first few months. Gastroesophageal reflux is the main complication. Proton pump inhibitor treatment is mostly effective in controlling patients' symptoms. Endoscopic surveillance is desirable in the long term for these patients.
Rebecchi et al. and Sharma et al. [65,66] concluded that in obese patients with GERD, LSG improves symptoms and controls reflux in most cases, whereas in patients with no preoperative evidence of GERD, de novo reflux is rare. Therefore, LSG should be considered an effective option for the surgical treatment of obese patients with GERD. The presence of GERD cannot be considered a contraindication to sleeve gastrectomy. There is improvement in Gerd as assessed by the symptom questionnaires. The new onset of GERD detected on scintigraphy may not be pathological as there is a decrease in total acid production after surgery; however, it still remains an important issue and needs long-term follow-up [[74], [75], [76]].
The limitations of this study are high heterogeneity and no data from randomized controlled trials. Several studies had varying selection criteria when offering surgery to people with and without GERD. There was a lack of data on the standardization of surgical technique. The follow-up time interval was variable, and long-term subgroup analysis was performed in an attempt to compensate for this. Some studies aimed to study reflux specifically, while others reported it as secondary outcomes. Studies using physiological and invasive techniques to investigate GERD have found higher rates than those using symptomatology alone.
5. Conclusions
We have controversial data on LSG and GERD in the literature as there is a multifactorial relationship between LSG and GERD. The most recent studies have shown satisfactory control of postoperative reflux in most patients and low rates of de novo GERD. Compared to LSG, obese patients receiving LRYGB had a lower risk of new onset or worsening of GERD. Some patients have been converted to LRYGB treatment due to severe reflux after LSG. Therefore, we recommend LRYGB as the preferred treatment for obese patients with GERD.
These data are leading to wider acceptance of LSG as a bariatric procedure even in obese patients with GERD, provided a tubular cuff is created, as recently stated in the 5th International Consensus Conference on sleeve gastrectomy [73].
In conclusion, bariatric surgery has become safer as surgeons gain experience in evaluating and treating obese patients, but careful medical evaluation is mandatory before choosing the type of bariatric surgery, especially for those patients who already have GERD.
Sources of funding
GIOVANNA PAVONE, NICOLA TARTAGLIA, ALESSANDRO PORFIDO, PIERCARMINE PANZERA, MARIO PACILLI, ANTONIO AMBROSI declare haven't been funded.
Ethical approval
The ethics committee of our institution approved the study.
Consent
Informed consent was obtained from all individual participants included in the study.
Author contribution
NICOLA TARTAGLIA and GIOVANNA PAVONE performed the study conception and design.
ALESSANDRO PORFIDO analyzed and interpreted the data.
MARIO PACILLI and PIERCARMINE PANZERA contributed to acquisition of the data.
ANTONIO AMBROSI revised the manuscript.
Trial registry number
-
1.
Name of the registry: ClinicalTrials.gov
-
2.
Unique Identifying number or registration ID: NCT05178446
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked): https://register.clinicaltrials.gov/prs/app/action/SelectProtocol?sid=S000BJ15&selectaction=Edit&uid=U0005YQF&ts=2&cx=-xs6cux
Guarantor
The Guarantors are Professor Nicola Tartaglia and Professor Antonio Ambrosi.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
GIOVANNA PAVONE, NICOLA TARTAGLIA, ALESSANDRO PORFIDO, PIERCARMINE PANZERA, MARIO PACILLI, ANTONIO AMBROSI declare no conflict of interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2022.103584.
Contributor Information
Giovanna Pavone, Email: Giovanna.Pavone@Unifg.It.
Nicola Tartaglia, Email: Nicola.Tartaglia@Unifg.It, Nicola.Tartaglia@Unifg.It.
Alessandro Porfido, Email: Alessandroporfido@Live.It.
Piercarmine Panzera, Email: Piercarminepanzera@Gmail.Com.
Mario Pacilli, Email: Mario.Pacilli@Unifg.It.
Antonio Ambrosi, Email: Antonio.Ambrosi@Unifg.Ti.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Angrisani L., Santonicola A., Iovino P., et al. Bariatric surgery and endoluminal procedures: IFSO Worldwide Survey 2014. Obes. Surg. 2017 doi: 10.1007/s11695-017-2666-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carlin A.M., Zeni T.M., English W.J., et al. Michigan Bariatric Sur- gery Collaborative. The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity. Ann. Surg. 2013;257:791–797. doi: 10.1097/SLA.0b013e3182879ded. [DOI] [PubMed] [Google Scholar]
- 3.Visscher T.L.S., Seidell J.C. The public health impact of obesity. Annu. Rev. Publ. Health. 2001;22:355–375. doi: 10.1146/annurev.publhealth.22.1.355. [DOI] [PubMed] [Google Scholar]
- 4.Pi-Sunyer F.X. Medical hazards of obesity. Ann. Intern. Med. 1993;119(7):655–660. doi: 10.7326/0003-4819-119-7_part_2-199310011-00006. [DOI] [PubMed] [Google Scholar]
- 5.Must A., Spadano J., Coakley E.H., Field A.E., Colditz G., Dietz W.H. The disease burden associated with overweight and obesity. J. Am. Med. Assoc. 1999;282(16):1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 6.Field A.E., Coakley E.H., Must A., et al. Impact of overweight on the risk of developing common chronic diseases during a 10- year period. Arch. Intern. Med. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 7.Lukanova A., Björ O., Kaaks R., et al. Body mass index and cancer: results from the Northern Sweden health and disease cohort. Int. J. Cancer. 2006;118(2):458–466. doi: 10.1002/ijc.21354. [DOI] [PubMed] [Google Scholar]
- 8.Genco A., Soricelli E., Casella G., et al. Gastroesophageal reflux disease and Barrett's esophagus after laparoscopic sleeve gastrecto- my: a possible, underestimated long-term complication. Surg. Obes. Relat. Dis. 2017;13:568–574. doi: 10.1016/j.soard.2016.11.029. [DOI] [PubMed] [Google Scholar]
- 9.Felsenreich D.M., Kefurt R., Schermann M., et al. Reflux, sleeve dilation, and Barrett's esophagus after laparoscopic sleeve gastrec- tomy: long-term follow-up. Obes. Surg. 2017 doi: 10.1007/s11695-017-2748-9. [DOI] [PubMed] [Google Scholar]
- 10.Stenard F., Iannelli A. Laparoscopic sleeve gastrectomy and gastro- esophageal reflux. World J. Gastroenterol. 2015;21(36):10348–10357. doi: 10.3748/wjg.v21.i36.10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan A., Kim A., Sanossian C., et al. Impact of obesity treatment on gastroesophageal reflux disease. World J. Gastroenterol. 2016;22:1627–1638. doi: 10.3748/wjg.v22.i4.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mion F., Dargent J. Gastro-oesophageal reflux disease and obesity: pathogenesis and response to treatment. Best Pract. Res. Clin. Gastroenterol. 2014;28:611–622. doi: 10.1016/j.bpg.2014.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Chopra A., Chao E., Etkin Y., et al. Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg. Endosc. 2012;26:831–837. doi: 10.1007/s00464-011-1960-2. [DOI] [PubMed] [Google Scholar]
- 14.Pallati P.K., Shaligram A., Shostrom V.K., et al. Improvement in gas- troesophageal reflux disease symptoms after various bariatric pro- cedures: review of the Bariatric Outcomes Longitudinal Database. Surg. Obes. Relat. Dis. 2014;10:502–507. doi: 10.1016/j.soard.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Sucandy I., Chrestiana D., Bonanni F., et al. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesi- ty. The importance of preoperative evaluation and selection. N. Am. J. Med. Sci. 2015;7:189–193. doi: 10.4103/1947-2714.157624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tartaglia N., Iadarola R., Di Lascia A., Cianci P., Fersini A., Ambrosi A. What is the treatment of tracheal lesions associated with traditional thyroidectomy? Case report and systematic review. World J. Emerg. Surg. 2018 Mar 23;13:15. doi: 10.1186/s13017-018-0175-4. PMID: 29588652; PMCID: PMC5865337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cianci P., Tartaglia N., Altamura A., Di Lascia A., Fersini A., Neri V., Ambrosi A. Cervical esophagotomy for foreign body extraction: a case report and extensive literature review of the last 20 years. Am. J. Case Rep. 2018 Apr 5;19:400–405. doi: 10.12659/ajcr.908373. PMID: 29618719; PMCID: PMC5900799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anania G., Agresta F., Artioli E., Rubino S., Resta G., Vettoretto N., Petz W.L., Bergamini C., Arezzo A., Valpiani G., Morotti C., Silecchia G., SICE CoDIG (Colon DxItalian Group) Laparoscopic right hemicolectomy: the SICE (Società Italiana di Chirurgia Endoscopica e Nuove Tecnologie) network prospective trial on 1225 casescomparing intra corporeal versus extra corporeal ileo-colic side-to-side anastomosis. Surg. Endosc. 2020 Nov;34(11):4788–4800. doi: 10.1007/s00464-019-07255-2. Epub 2019 Nov 18. Erratum in: Surg Endosc. 2019 Dec 12;: PMID: 31741153; PMCID: PMC7572335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shea B.J., Reeves B.C., Wells G., Thuku M., Hamel C., Moran J., Moher D., Tugwell P., Welch V., Kristjansson E., Henry D.A. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017 Sep 21;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abd Ellatif M.E., Abdallah E., Askar W., Thabet W., Aboushady M., Abbas A.E., El Hadidi A., Elezaby A.F., Salama A.F., Dawoud I.E., Moatamed A., Wahby M. Long term predictors of success after laparoscopic sleeve gastrectomy. Int. J. Surg. 2014;12(5):504–508. doi: 10.1016/j.ijsu.2014.02.008. Epub 2014 Feb 18. PMID: 24560848. [DOI] [PubMed] [Google Scholar]
- 22.Albanopoulos K., Tsamis D., Natoudi M., Alevizos L., Zografos G., Leandros E. The impact of laparoscopic sleeve gastrectomy on weight loss and obesity-associated comorbidities: the results of 3 years of follow-up. Surg. Endosc. 2016 Feb;30(2):699–705. doi: 10.1007/s00464-015-4262-2. Epub 2015 Jun 20. PMID: 26091999. [DOI] [PubMed] [Google Scholar]
- 23.Alexandrou A., Athanasiou A., Michalinos A., Felekouras E., Tsigris C., Diamantis T. Laparoscopic sleeve gastrectomy for morbid obesity: 5-year results. Am. J. Surg. 2015 Feb;209(2):230–234. doi: 10.1016/j.amjsurg.2014.04.006. Epub 2014 Jun 20. PMID: 25034410. [DOI] [PubMed] [Google Scholar]
- 24.Althuwaini S., Bamehriz F., Aldohayan A., Alshammari W., Alhaidar S., Alotaibi M., Alanazi A., Alsahabi H., Almadi M.A. Prevalence and predictors of gastroesophageal reflux disease after laparoscopic sleeve gastrectomy. Obes. Surg. 2018 Apr;28(4):916–922. doi: 10.1007/s11695-017-2971-4. PMID: 29043549. [DOI] [PubMed] [Google Scholar]
- 25.Angrisani L., Santonicola A., Hasani A., Nosso G., Capaldo B., Iovino P. Five-year results of laparoscopic sleeve gastrectomy: effects on gastroesophageal reflux disease symptoms and co-morbidities. Surg. Obes. Relat. Dis. 2016 Jun;12(5):960–968. doi: 10.1016/j.soard.2015.09.014. Epub 2015 Sep 26. PMID: 26775051. [DOI] [PubMed] [Google Scholar]
- 26.Arman G.A., Himpens J., Dhaenens J., Ballet T., Vilallonga R., Leman G. Long-term (11+years) outcomes in weight, patient satisfaction, comorbidities, and gastroesophageal reflux treatment after laparoscopic sleeve gastrectomy. Surg. Obes. Relat. Dis. 2016 Dec;12(10):1778–1786. doi: 10.1016/j.soard.2016.01.013. Epub 2016 Jan 19. PMID: 27178613. [DOI] [PubMed] [Google Scholar]
- 27.Barr A.C., Frelich M.J., Bosler M.E., Goldblatt M.I., Gould J.C. GERD and acid reduction medication use following gastric bypass and sleeve gastrectomy. Surg. Endosc. 2017 Jan;31(1):410–415. doi: 10.1007/s00464-016-4989-4. Epub 2016 Jun 10. PMID: 27287901. [DOI] [PubMed] [Google Scholar]
- 28.Barry R.G., Amiri F.A., Gress T.W., Nease D.B., Canterbury T.D. Laparoscopic vertical sleeve gastrectomy: a 5-year veterans affairs review. Medicine (Baltim.) 2017 Sep;96(35) doi: 10.1097/MD.0000000000007508. PMID: 28858079; PMCID: PMC5585473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berry M.A., Urrutia L., Lamoza P., Molina A., Luna E., Parra F., Domínguez M.J., Alonso R. Sleeve gastrectomy outcomes in patients with BMI between 30 and 35-3 Years of follow-up. Obes. Surg. 2018 Mar;28(3):649–655. doi: 10.1007/s11695-017-2897-x. PMID: 28975492; PMCID: PMC5803286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Borbély Y., Schaffner E., Zimmermann L., Huguenin M., Plitzko G., Nett P., Kröll D. De novo gastroesophageal reflux disease after sleeve gastrectomy: role of preoperative silent reflux. Surg. Endosc. 2019 Mar;33(3):789–793. doi: 10.1007/s00464-018-6344-4. Epub 2018 Jul 12. PMID: 30003346. [DOI] [PubMed] [Google Scholar]
- 31.Boza C., Daroch D., Barros D., León F., Funke R., Crovari F. Long-term outcomes of laparoscopic sleeve gastrectomy as a primary bariatric procedure. Surg. Obes. Relat. Dis. 2014 Nov-Dec;10(6):1129–1133. doi: 10.1016/j.soard.2014.03.024. Epub 2014 Apr 14. PMID: 25500284. [DOI] [PubMed] [Google Scholar]
- 32.Braghetto I., Csendes A. Prevalence of Barrett's esophagus in bariatric patients undergoing sleeve gastrectomy. Obes. Surg. 2016 Apr;26(4):710–714. doi: 10.1007/s11695-015-1574-1. PMID: 25855575. [DOI] [PubMed] [Google Scholar]
- 33.Braghetto I., Korn O. Late esophagogastric anatomic and functional changes after sleeve gastrectomy and its clinical consequences with regards to gastroesophageal reflux disease. Dis. Esophagus. 2019 Jun 1;32(6):doz020. doi: 10.1093/dote/doz020. PMID: 31076757. [DOI] [PubMed] [Google Scholar]
- 34.Burgerhart J.S., Schotborgh C.A., Schoon E.J., Smulders J.F., van de Meeberg P.C., Siersema P.D., Smout A.J. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes. Surg. 2014 Sep;24(9):1436–1441. doi: 10.1007/s11695-014-1222-1. PMID: 24619293. [DOI] [PubMed] [Google Scholar]
- 35.Carabotti M., Silecchia G., Greco F., Leonetti F., Piretta L., Rengo M., Rizzello M., Osborn J., Corazziari E., Severi C. Impact of laparoscopic sleeve gastrectomy on upper gastrointestinal symptoms. Obes. Surg. 2013 Oct;23(10):1551–1557. doi: 10.1007/s11695-013-0973-4. PMID: 23636996. [DOI] [PubMed] [Google Scholar]
- 36.Carter P.R., LeBlanc K.A., Hausmann M.G., Kleinpeter K.P., deBarros S.N., Jones S.M. Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Surg. Obes. Relat. Dis. 2011 Sep-Oct;7(5):569–572. doi: 10.1016/j.soard.2011.01.040. Epub 2011 Mar 22. PMID: 21429818. [DOI] [PubMed] [Google Scholar]
- 37.CastagnetoGissey L., Casella Mariolo J.R., Genco A., Troisi A., Basso N., Casella G. 10-year follow-up after laparoscopic sleeve gastrectomy: outcomes in a monocentric series. Surg. Obes. Relat. Dis. 2018 Oct;14(10):1480–1487. doi: 10.1016/j.soard.2018.06.021. Epub 2018 Jul 2. PMID: 30093311. [DOI] [PubMed] [Google Scholar]
- 38.Catheline J.M., Fysekidis M., Bachner I., Bihan H., Kassem A., Dbouk R., Bdeoui N., Boschetto A., Cohen R. Five-year results of sleeve gastrectomy. J. Vis. Surg. 2013 Nov;150(5):307–312. doi: 10.1016/j.jviscsurg.2013.08.008. Epub 2013 Sep 21. PMID: 24060743. [DOI] [PubMed] [Google Scholar]
- 39.Chuffart E., Sodji M., Dalmay F., Iannelli A., Mathonnet M. Long-term results after sleeve gastrectomy for gastroesophageal reflux disease: a single-center French study. Obes. Surg. 2017 Nov;27(11):2890–2897. doi: 10.1007/s11695-017-2698-2. PMID: 28474318. [DOI] [PubMed] [Google Scholar]
- 40.Coupaye M., Gorbatchef C., Calabrese D., Sami O., Msika S., Coffin B., Ledoux S. Gastroesophageal reflux after sleeve gastrectomy: a prospective mechanistic study. Obes. Surg. 2018 Mar;28(3):838–845. doi: 10.1007/s11695-017-2942-9. PMID: 28993985. [DOI] [PubMed] [Google Scholar]
- 41.Dakour Aridi H., Asali M., Fouani T., Alami R.S., BY Safadi. Gastroesophageal reflux disease after laparoscopic sleeve gastrectomy with concomitant hiatal hernia repair: an unresolved question. Obes. Surg. 2017 Nov;27(11):2898–2904. doi: 10.1007/s11695-017-2702-x. PMID: 28455802. [DOI] [PubMed] [Google Scholar]
- 42.Del Genio G., Tolone S., Limongelli P., Brusciano L., D'Alessandro A., Docimo G., Rossetti G., Silecchia G., Iannelli A., del Genio A., del Genio F., Docimo L. Sleeve gastrectomy and development of "de novo" gastro esophageal reflux. Obes. Surg. 2014 Jan;24(1):71–77. doi: 10.1007/s11695-013-1046-4. PMID: 24249251. [DOI] [PubMed] [Google Scholar]
- 43.DuPree C.E., Blair K., Steele S.R., Martin M.J. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease : a national analysis. JAMA Surg. 2014 Apr;149(4):328–334. doi: 10.1001/jamasurg.2013.4323. PMID: 24500799. [DOI] [PubMed] [Google Scholar]
- 44.Felsenreich D.M., Ladinig L.M., Beckerhinn P., Sperker C., Schwameis K., Krebs M., Jedamzik J., Eilenberg M., Bichler C., Prager G., Langer F.B. Update: 10 Years of sleeve gastrectomy-the first 103 patients. Obes. Surg. 2018 Nov;28(11):3586–3594. doi: 10.1007/s11695-018-3399-1. PMID: 30047101. [DOI] [PubMed] [Google Scholar]
- 45.Felsenreich D.M., Kefurt R., Schermann M., Beckerhinn P., Kristo I., Krebs M., Prager G., Langer F.B. Reflux, sleeve dilation, and Barrett's esophagus after laparoscopic sleeve gastrectomy: long-term follow-up. Obes. Surg. 2017 Dec;27(12):3092–3101. doi: 10.1007/s11695-017-2748-9. PMID: 28593484. [DOI] [PubMed] [Google Scholar]
- 46.Flølo T.N., Andersen J.R., Kolotkin R.L., Aasprang A., Natvig G.K., Hufthammer K.O., Våge V. Five-year outcomes after vertical sleeve gastrectomy for severe obesity: a prospective cohort study. Obes. Surg. 2017 Aug;27(8):1944–1951. doi: 10.1007/s11695-017-2605-x. PMID: 28224471. [DOI] [PubMed] [Google Scholar]
- 47.Gadiot R.P., Biter L.U., van Mil S., Zengerink H.F., Apers J., Mannaerts G.H. Long-term results of laparoscopic sleeve gastrectomy for morbid obesity: 5 to 8-year results. Obes. Surg. 2017 Jan;27(1):59–63. doi: 10.1007/s11695-016-2235-8. PMID: 27178407. [DOI] [PubMed] [Google Scholar]
- 48.Garg H., Aggarwal S., Misra M.C., Priyadarshini P., Swami A., Kashyap L., Jaiswal R. Mid to long term outcomes of Laparoscopic Sleeve Gastrectomy in Indian population: 3-7 year results - a retrospective cohort study. Int. J. Surg. 2017 Dec;48:201–209. doi: 10.1016/j.ijsu.2017.10.076. Epub 2017 Nov 6. PMID: 29122706. [DOI] [PubMed] [Google Scholar]
- 49.Gemici E., Kones O., Seyit H., Surek A., Cikot M., Bozkurt M.A., Alis H. Outcomes of laparoscopic sleeve gastrectomy by means of esophageal manometry and pH-metry, before and after surgery. WideochirInne Tech Maloinwazyjne. 2020 Mar;15(1):129–135. doi: 10.5114/wiitm.2019.83198. Epub 2019 Feb 25. PMID: 32117496; PMCID: PMC7020704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Genco A., Soricelli E., Casella G., Maselli R., Castagneto-Gissey L., Di Lorenzo N., Basso N. Gastroesophageal reflux disease and Barrett's esophagus after laparoscopic sleeve gastrectomy: a possible, underestimated long-term complication. Surg. Obes. Relat. Dis. 2017 Apr;13(4):568–574. doi: 10.1016/j.soard.2016.11.029. Epub 2016 Dec 9. PMID: 28089434. [DOI] [PubMed] [Google Scholar]
- 51.Georgia D., Stamatina T., Maria N., Konstantinos A., Konstantinos F., Emmanouil L., Georgios Z., Dimitrios T. 24-h multichannel intraluminal impedance PH-metry 1 Year after laparocopic sleeve gastrectomy: an objective assessment of gastroesophageal reflux disease. Obes. Surg. 2017 Mar;27(3):749–753. doi: 10.1007/s11695-016-2359-x. PMID: 27592124. [DOI] [PubMed] [Google Scholar]
- 52.Hendricks L., Alvarenga E., Dhanabalsamy N., Lo Menzo E., Szomstein S., Rosenthal R. Impact of sleeve gastrectomy on gastroesophageal reflux disease in a morbidly obese population undergoing bariatric surgery. Surg. Obes. Relat. Dis. 2016 Mar-Apr;12(3):511–517. doi: 10.1016/j.soard.2015.08.507. Epub 2015 Oct 1. PMID: 26792456. [DOI] [PubMed] [Google Scholar]
- 53.Himpens J., Dobbeleir J., Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann. Surg. 2010 Aug;252(2):319–324. doi: 10.1097/SLA.0b013e3181e90b31. PMID: 20622654. [DOI] [PubMed] [Google Scholar]
- 54.Hirth D.A., Jones E.L., Rothchild K.B., Mitchell B.C., Schoen J.A. Laparoscopic sleeve gastrectomy: long-term weight loss outcomes. Surg. Obes. Relat. Dis. 2015 Sep-Oct;11(5):1004–1007. doi: 10.1016/j.soard.2015.02.016. Epub 2015 Feb 24. PMID: 25980329. [DOI] [PubMed] [Google Scholar]
- 55.Howard D.D., Caban A.M., Cendan J.C., Ben-David K. Gastroesophageal reflux after sleeve gastrectomy in morbidly obese patients. Surg. Obes. Relat. Dis. 2011 Nov-Dec;7(6):709–713. doi: 10.1016/j.soard.2011.08.003. Epub 2011 Aug 16. PMID: 21955743. [DOI] [PubMed] [Google Scholar]
- 56.Kehagias I., Spyropoulos C., Karamanakos S., Kalfarentzos F. Efficacy of sleeve gastrectomy as sole procedure in patients with clinically severe obesity (BMI ≤50 kg/m(2)) Surg. Obes. Relat. Dis. 2013 May-Jun;9(3):363–369. doi: 10.1016/j.soard.2011.12.011. Epub 2012 Jan 13. PMID: 22342326. [DOI] [PubMed] [Google Scholar]
- 57.Kowalewski P.K., Olszewski R., Walędziak M.S., Janik M.R., Kwiatkowski A., Gałązka-Świderek N., Cichoń K., Brągoszewski J., Paśnik K. Long-termout comes of laparoscopic sleeve gastrectomy-a single-center, retrospective study. Obes. Surg. 2018 Jan;28(1):130–134. doi: 10.1007/s11695-017-2795-2. PMID: 28707172; PMCID: PMC5735208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lemaître F., Léger P., Nedelcu M., Nocca D. Laparoscopic sleeve gastrectomy in the South Pacific. Retrospective evaluation of 510 patients in a single institution. Int. J. Surg. 2016 Jun;30:1–6. doi: 10.1016/j.ijsu.2016.04.002. Epub 2016 Apr 8. PMID: 27063637. [DOI] [PubMed] [Google Scholar]
- 59.Lim C.H., Lee P.C., Lim E., Tan J., Chan W.H., Tan H.C., Ganguly S., Tham K.W., Eng A. Correlation between symptomatic gastro-esophageal reflux disease (GERD) and erosive esophagitis (EE) post-vertical sleeve gastrectomy (VSG) Obes. Surg. 2019 Jan;29(1):207–214. doi: 10.1007/s11695-018-3509-0. PMID: 30238218. [DOI] [PubMed] [Google Scholar]
- 60.Menenakos E., Stamou K.M., Albanopoulos K., Papailiou J., Theodorou D., Leandros E. Laparoscopic sleeve gastrectomy performed with intent to treat morbid obesity: a prospective single-center study of 261 patients with a median follow-up of 1 year. Obes. Surg. 2010 Mar;20(3):276–282. doi: 10.1007/s11695-009-9918-3. Epub 2009 Jul 28. PMID: 19636644. [DOI] [PubMed] [Google Scholar]
- 61.Nocca D., Loureiro M., Skalli E.M., Nedelcu M., Jaussent A., Deloze M., Lefebvre P., Fabre J.M. Five-year results of laparoscopic sleeve gastrectomy for the treatment of severe obesity. Surg. Endosc. 2017 Aug;31(8):3251–3257. doi: 10.1007/s00464-016-5355-2. Epub 2016 Dec 23. PMID: 28008465. [DOI] [PubMed] [Google Scholar]
- 62.Pilone V., Tramontano S., Renzulli M., Zulli C., Schiavo L. Gastroesophageal reflux after sleeve gastrectomy: new onset and effect on symptoms on a prospective evaluation. Obes. Surg. 2019 Nov;29(11):3638–3645. doi: 10.1007/s11695-019-04046-5. PMID: 31267475. [DOI] [PubMed] [Google Scholar]
- 63.Pok E.H., Lee W.J., Ser K.H., Chen J.C., Chen S.C., Tsou J.J., Chin K.F. Laparoscopic sleeve gastrectomy in Asia: long term outcome and revisional surgery. Asian J. Surg. 2016 Jan;39(1):21–28. doi: 10.1016/j.asjsur.2015.03.006. Epub 2015 May 8. PMID: 25964106. [DOI] [PubMed] [Google Scholar]
- 64.Rawlins L., Rawlins M.P., Brown C.C., Schumacher D.L. Sleeve gastrectomy: 5-year outcomes of a single institution. Surg. Obes. Relat. Dis. 2013 Jan-Feb;9(1):21–25. doi: 10.1016/j.soard.2012.08.014. Epub 2012 Sep 6. PMID: 23201209. [DOI] [PubMed] [Google Scholar]
- 65.Rebecchi F., Allaix M.E., Giaccone C., Ugliono E., Scozzari G., Morino M. Gastroesophagealreflux disease and laparoscopic sleeve gastrectomy: a physiopathologic evaluation. Ann. Surg. 2014 Nov;260(5):909–914. doi: 10.1097/SLA.0000000000000967. PMID: 25379861. [DOI] [PubMed] [Google Scholar]
- 66.Sharma A., Aggarwal S., Ahuja V., Bal C. Evaluation of gastroesophageal reflux before and after sleeve gastrectomy using symptom scoring, scintigraphy, and endoscopy. Surg. Obes. Relat. Dis. 2014 Jul-Aug;10(4):600–605. doi: 10.1016/j.soard.2014.01.017. Epub 2014 Jan 28. PMID: 24837563. [DOI] [PubMed] [Google Scholar]
- 67.Sheppard C.E., Sadowski D.C., de Gara C.J., Karmali S., Birch D.W. Rates of reflux before and after laparoscopic sleeve gastrectomy for severe obesity. Obes. Surg. 2015 May;25(5):763–768. doi: 10.1007/s11695-014-1480-y. PMID: 25411120. [DOI] [PubMed] [Google Scholar]
- 68.Soricelli E., Casella G., Baglio G., Maselli R., Ernesti I., Genco A. Lack of correlation between gastroesophageal reflux disease symptoms and esophageal lesions after sleeve gastrectomy. Surg. Obes. Relat. Dis. 2018 Jun;14(6):751–756. doi: 10.1016/j.soard.2018.02.008. Epub 2018 Feb 13. PMID: 29571635. [DOI] [PubMed] [Google Scholar]
- 69.Viscido G., Gorodner V., Signorini F., Navarro L., Obeide L., Moser F. Laparoscopic sleeve gastrectomy: endoscopic findings and gastroesophageal reflux symptoms at 18-month follow-up. J. Laparoendosc. Adv. Surg. Tech. 2018 Jan;28(1):71–77. doi: 10.1089/lap.2017.0398. Epub 2017 Dec 11. PMID: 29227187. [DOI] [PubMed] [Google Scholar]
- 70.Richter J.E., Rubenstein J.H. Presentation and epidemiology of gas- troesophageal reflux disease. Gastroenterology. 2018;154:267–276. doi: 10.1053/j.gastro.2017.07.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Eusebi L.H., Ratnakumaran R., Yuan Y., et al. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 72.Singh S., Sharma A.N., Murad M.H., et al. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: a systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2013;11:1399–1412. doi: 10.1016/j.cgh.2013.05.009. e1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gagner M., Hutchinson C., Rosenthal R. Fifth International Consensus Conference: current status of sleeve gastrectomy. Surg. Obes. Relat. Dis. 2016;12:750–756. doi: 10.1016/j.soard.2016.01.022. [PMID: 27178618 DOI: [DOI] [PubMed] [Google Scholar]
- 74.Tartaglia N., Di Lascia A., Vovola F., Cianci P., Fersini A., Pacilli M., Pavone G., Ambrosi A. Bilateral central neck dissection in the treatment of early unifocal papillary thyroid carcinomas with poor risk factors A mono-institutional experience. Ann. Ital. Chir. 2020;91:161–165. PMID: 32149727. [PubMed] [Google Scholar]
- 75.Pacilli M., Tartaglia N., Gerundo A., Pavone G., Fersini A., Ambrosi A. Energy based vessel sealing devices in thyroid surgery: a systematic review to clarify the relationship with recurrent laryngeal nerve injuries. Medicina (Kaunas) 2020 Nov 27;56(12):651. doi: 10.3390/medicina56120651. PMID: 33260912; PMCID: PMC7760641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tartaglia N., Pavone G., Lizzi V., Vovola F., Tricarico F., Pacilli M., Ambrosi A. How emergency surgery has changed during the COVID-19 pandemic: a cohort study. Ann. Med. Surg. (Lond.) 2020 Dec 5;60:686–689. doi: 10.1016/j.amsu.2020.12.001. PMID: 33312562; PMCID: PMC7719013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.