Abstract
The continuum of care throughout pregnancy, childbirth, and postnatal period is one of the vital strategies for improving maternal and neonatal health and preventing maternal and neonatal mortalities and morbidities. The level and determinants of the complete continuum of care for maternal health services reported by different studies were extremely varied in Ethiopia. Therefore, this meta-analysis aimed to estimate the overall prevalence of a complete continuum of maternal health care services utilization and its associated factors in Ethiopia. Databases such as PubMed/MEDLINE, Science Direct, DOJA, African journals online, Cochrane library, Google scholar, web of science, and Ethiopian universities’ institutional repository were used to search for relevant studies. A total of seven studies with 4854 study participants were involved in this study. Data were extracted by two reviewers and exported to STATA Version 11 for analysis. The I2 statistics and Egger’s test were used to assess heterogeneity and publication bias, respectively. The random-effects random effects model was used to estimate the level of complete continuum of care for maternal health services. The pooled prevalence of complete continuum of maternal healthcare services utilization was 25.51%. Employed mothers (OR = 3.16, 95%CI = 1.82, 5.47), first antenatal ante natal care visit before 16 weeks (OR = 7.53, 95% CI = 2.94, 19.29), birth preparedness and complication readiness plan (OR = 1.95, 95% CI = 1.12, 3.41), secondary and above educational status (OR = 2.97, 95% CI = 2.00, 4.41), planned pregnancy (OR = 6.86, 95% CI = 3.47, 13.58) and autonomy (OR = 3.73, 95% CI = 2.24–6.23) were significantly associated with continuum of maternal healthcare services utilization. In conclusion, the national level of complete continuum of maternal healthcare service utilization was low in Ethiopia. Being employed mothers, first ante natal care visit before 16 weeks, birth preparedness and complication readiness plan, secondary and above educational status, autonomy, and planned pregnancy were the major determinants of continuum of maternal healthcare services utilization.
Keywords: associated factors, continuum of care, Ethiopia, maternal health services
Introduction
Worldwide, around 303,000 mothers died as a result of pregnancy-related complications in 2015; an average of 830 maternal deaths happened per day. The majority of these deaths (99%) occurred in low- and middle-income countries.1,2
Maternal mortality was more prevalent in sub-Saharan Africa (SSA) and accounts for 62% of the global maternal deaths. Besides this, 1 in 30 mothers suffers pregnancy-related complications in this region. 3 Furthermore, the risk of neonatal morbidity and mortality was the highest in SSA (92 deaths/1000 live births) and it was around 15 times greater than that in developed countries.3–6 The majority of these maternal and neonatal mortalities resulted from preventable causes. 1
The continuum of care (CoC) for maternal and child health services was one of the vital strategies to decrease maternal and newborn deaths7–9 and attain the universal target of maternal mortality reduction (70 maternal deaths per 100,000 live births). 10 Evidence indicated that nearly 80% of maternal mortality and approximately two-thirds of neonatal mortality could be avoided if effective maternal health care is provided throughout pregnancy, delivery, and following birth.11,12 Besides, more than 99% coverage of the complete continuum of maternal healthcare services utilizations could avoid around 41%–72% of neonatal mortalities globally.13,14
Although the term “continuum of care” for reproductive, maternal, newborn, and child health (RMNCH) refers to integrated service delivery for mothers and children from pre-pregnancy to delivery, the immediate postnatal period, and childhood,8,15–20 in this study, we used a narrower scope of a CoC, focusing on continuity of care throughout pregnancy, delivery, and early years of the newborn’s life (mainly the use of at least four ante natal care (ANC) visits during pregnancy, skill birth attendant (SB) during delivery, and at least 1 postnatal visit within 6 weeks following childbirth). This definition was drawn by considering Federal ministry of health maternal and child health care recommendations.10,21,22
The magnitude of a continuum of maternal healthcare service utilization was variable across different countries. It was 12% in Bangladeshi, 17 27% in Pakistan, 12 8% in Ghana, 18 and 41% in Nepal. 16 The Ethiopian Demographic Health Survey (EDHS) 2019 report showed that 74% of women received at least one ANC, 43% had four or more ANC visits, 50% of the mother delivered by a skilled birth attendant, and 34% of women received a post natal care (PNC) check-up in the first 2 days following delivery. 23 Different studies done in a rural part of Ethiopia indicated that the magnitude of complete continuum of maternal healthcare services utilization ranges from 9.7% 10 to 47%. 13
Evidence indicated that different factors affect the continuum of maternal healthcare services utilization. Some of these factors were lack of women involvement in their healthcare decision-making, low educational status, unwanted pregnancy, poorest wealth quintile, not being exposed to mass media, rural residency, longer distance to a health facility, being a farmer, late initiation of ANC, and lack of communication with the husband or family members.17,24–27
Although there are some fragmented primary studies on the coverage and determinants of continuum of maternal healthcare services utilization in Ethiopia, the national level of continuity of maternal healthcare services utilization was unknown. Besides, the prevalence of complete continuum of maternal healthcare services utilization was significantly different across the studies. Furthermore, determinants of continuum maternal healthcare services utilization were variable among those studies. Therefore, this meta-analysis aimed to estimate the pooled prevalence of complete continuum of maternal healthcare services utilization and its associated factors in Ethiopia. The result of this study will provide important input for policymakers and clinicians about continuum of maternal healthcare services utilization and this finding will enforce them to design evidence-based strategies for improvement of a continuum of maternal healthcare services utilization in Ethiopia.
Materials and methods
This systematic review and meta-analysis was intended to determine the overall prevalence of complete continuum of maternal healthcare services utilization and its associated factors in Ethiopia. The protocol for this systematic review and meta-analysis was not registered in the PROSPERO. However, registration of this study on PROSPERO is ongoing. A standard systematic review and meta-analysis reporting PRISMA checklist was used to present the findings (Supplemental Table S1).
Databases and search strategies
Three authors (D.A., A.M., and A.D.) explored all relevant studies systematically from different international databases (PubMed/MEDLINE, science direct, DOJA, African journals online, Cochrane library, Google scholar, and web of science). At the outset, studies were exhaustively searched by using the full title (“The level and determinants of complete CoC for maternal health services in Ethiopia”) and keywords (“level,” “proportion,” “magnitude,” “completion,” “complete,” “continuum,” “mothers,” “maternal” odd ratio (OR) “maternity,” “care,” “determinants,” “associated factors,” “predictors,” “Ethiopia”). Boolean operators “OR” or “AND” were used in combination or independently to connect these keywords and to establish the search terms. Furthermore, reference lists of all included published and unpublished studies were assessed to find other missed studies. Moreover, institutional repository from Mekelle, Jima, Addis Abeba, Gondar, and Harameya University was used to search important gray literature, specifically unpublished thesis reports, doctoral theses, and call for papers. Search details for PubMed were level (All Fields) AND (complete (All Fields) OR “completion” (All fields)) AND “continuum” (All Fields) AND (“mothers” (MeSH Terms) OR “mothers” (All Fields) OR “maternal” (All Fields) OR “maternity” (All fields) OR “maternity” (MeSH Terms)) AND care (All Fields) AND (“determinants” (All Fields) OR “associated factors” (All fields) OR “Predictors” (All fields)) AND (“Ethiopia” (MeSH Terms) OR “Ethiopia” (All Fields)). The search periods for this systematic review and meta-analysis were between 1 January 2010 and 9 December 2021 (Supplemental Table S2).
Eligibility criteria
To declare inclusion and exclusion criteria for this systematic review and meta-analysis, the authors followed the PICO approach mainly CoCoPop (Condition, Context, and Population) questions for prevalence studies.
Inclusion criteria
Study area: studies conducted in Ethiopia.
Study setting: studies conducted in rural or urban settings and at health institutions or community-based settings.
Study design: observational studies (cross-sectional, cohort, and case-control study), which reports either the prevalence/coverage/magnitude or determinants/associated factors/predictors of continuum maternal healthcare services utilization.
Population: Low-risk mothers.
Publication condition: Both published and unpublished studies.
Time: Studies published between 1 January 2010 and 9 December 2021 and unpublished studies which were conducted and stored in the Ethiopian university institutional repository between 1 January 2010 and 9 December 2021 (G.C).
Exclusion criteria
Studies that have a different outcome of interest, without full content, qualitative studies, and conference reports were excluded. Besides this, studies with different operational definitions and measurements of complete continuum of maternal healthcare services utilization were excluded from this systematic review and meta-analysis. In addition, studies were excluded if they had a poor quality score for the Newcastle–Ottawa quality assessment scale. However, no study was excluded as a result of poor quality scores.
Outcome measurement, study selection, and quality assessment
This systematic review and meta-analysis had two outcomes (complete continuum of maternal healthcare services utilization and its associated factors). Completed continuum of maternal healthcare services utilization was considered when the mother had received the sum of all three services (at least four ANC visits at the health facility, delivered by the skilled birth attendant, and at least 1 PNC within 6 weeks following delivery).
Employment
In this study, being employed was considered when a mother was recruited at least in one of the following institutions (non-governmental organization, governmental institution, or private institution) and had monthly salaries.
All studies identified from different international databases and Ethiopian universities’ institutional repositories were exported to Endnote 7 reference manager for screening purposes. Then, studies were screened by using the following criteria (duplication, relevancy, accessibility of full text, and outcomes of interest). Finally, studies that fulfilled the inclusion criteria were included for analysis. A standard quality assessment tool (Newcastle–Ottawa quality assessment Scale adapted for cross-sectional studies) were used to assess the quality of the studies 28 and the qualities of studies were assessed by two reviewers (D.A. and S.B.) individually using the following components: The first component was selection, which was graded by five stars, the second was comparability and graded by two stars, and the third was the outcome and assessed by three stars. Disparities at the time of quality assessment were resolute through discussion and consensus by involving the third reviewer (A.D.). Articles that had ⩾7 points out of 9 were considered to be high-quality and included in this study (Supplemental Table S3).
Data extraction process
Two reviewers (D.A. and S.B.) extracted all necessary data separately from seven primary studies by using a predesigned data abstraction form. The first author’s name, publication year, study region, study setting, residency of participants involved in the studies, study period, sample size, sampling technique, and prevalence of continuum of maternal healthcare services utilization with 95% CI. Besides this, AOR with a 95% confidence interval for significant risk factors of continuum of maternal healthcare services utilization was extracted. When disagreements happened between the two reviewers, the third reviewer (A.D.) resolved disagreements through discussion and detailed re-evaluation of each study.
Data synthesis and statistical analysis
A random effects model was applied to determine the pooled prevalence of continuum of maternal healthcare services utilization (I2 = 98.8%, p < 0.001).29–31 To identify the source of heterogeneity for the pooled prevalence of continuum of maternal healthcare service utilization, subgroup analysis was performed by using the following characteristics (sample size, sampling technique, and residency). However, the possible source of heterogeneity was not detected. Besides, sensitivity analysis was done to check the effect of individual studies on the national level of continuum of maternal healthcare services utilization. Publication bias was objectively assessed by using Egger’s regression test 32 and the results of egger’s regression test revealed no publication bias between the studies (p-value = 0.055). The associations between determinants and continuum of maternal healthcare services utilization were assessed by using both fixed and random effect models.
Result
Search results
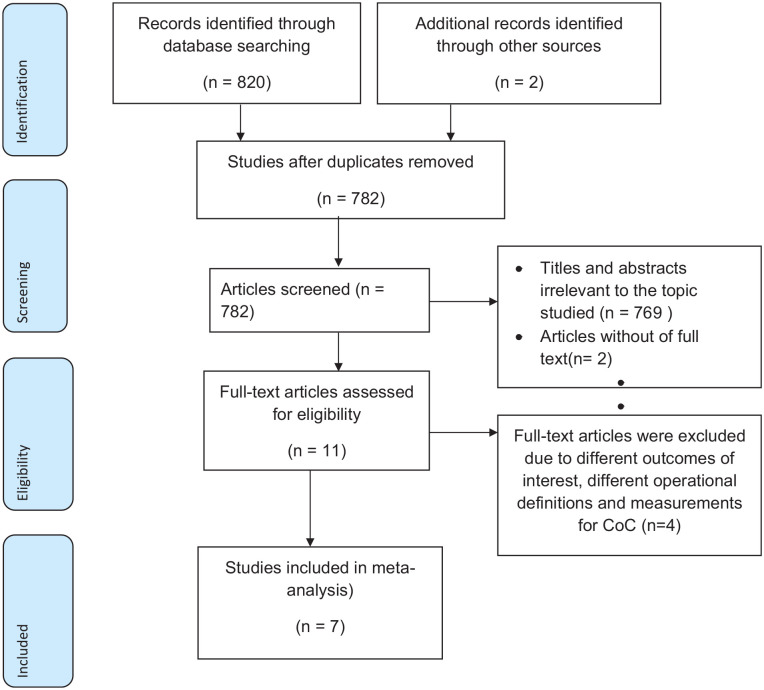
A total of 822 studies were searched from different international databases and Ethiopian universities’ institutional repositories using different comprehensive searching strategies. All retrieved studies were transferred to Endnote 7 reference manager for screening. Then a total of 815 studies were removed due to duplication, different outcomes of interest, unrelated titles, and inaccessibility of full text. Finally, seven studies that fulfilled the inclusion criteria were included in this study (Figure 1).
Figure 1.
Flowchart describing study selection for systematic review and meta-analysis of the level and determinants of complete CoC for maternal health services in Ethiopia.
Characteristics of included studies
A total of seven studies were included to assess the pooled prevalence of complete continuum of maternal healthcare services utilization and its associated factors in Ethiopia. A total of 4854 study participants were involved to estimate the overall prevalence of complete continuum of maternal healthcare services utilization and its associated factors. From the included studies, six studies were published in different international journals between 2018 and 2021 G.C. Three regions in Ethiopia were represented in this study. Five studies were from the Amhara region,13,33,34 and the rest were from the Tigray 35 and the Southern Nations, Nationalities, and Peoples Region (SNNPR) regions. 10 All included studies were cross-sectional studies and have a low risk of bias (Table 1).
Table 1.
Shows a descriptive summary of seven studies reporting the level and determinants of continuum of care for maternal health services in Ethiopia.
| Author | Publication year | Region | Study area | Study design | Sample size | Prevalence | Quality |
|---|---|---|---|---|---|---|---|
| Haile et al. 10 | 2020 | SNNPR | Arbaminch | Cross-sectional | 438 | 9.7 | Low risk |
| Tizazu et al. 34 | 2021 | Amhara | Debre Birhan | Cross-sectional | 647 | 37.2 | Low risk |
| Asratie et al. 13 | 2020 | Amhara | Motta | Cross-sectional | 819 | 47 | Low risk |
| Atnafu et al. 33 | 2020 | Amhara | Dabat | Cross-sectional | 565 | 21.6 | Low risk |
| Emiru et al. 36 | 2020 | Amhara | West Gojjam | Cross-sectional | 1281 | 12.1 | Low risk |
| Yohannes et al. 35 | 2018 | Tigray | Mekelle | Cross-sectional | 490 | 35.3 | Low risk |
| Sertsewold et al. 21 | 2021 | Amhara | Siyadebirena wayu | Cross-sectional | 614 | 16.1 | Low risk |
SNNPR: southern nations, nationalities, and peoples region.
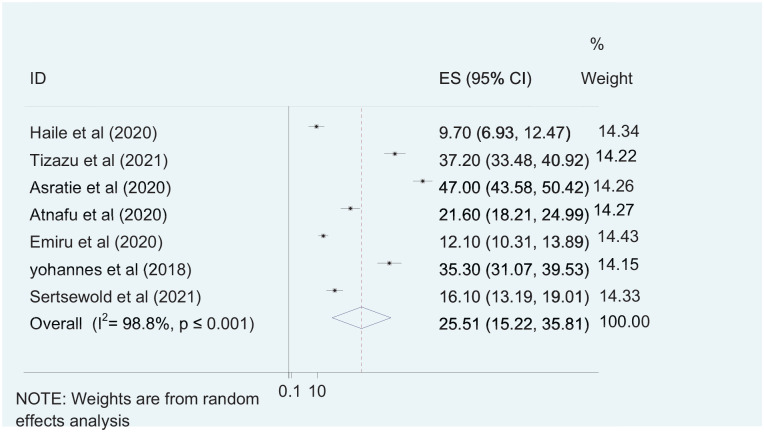
The pooled prevalence of complete continuum of maternal healthcare services utilization
Seven primary studies were included to assess the pooled prevalence of complete continuum of maternal healthcare services utilization.10,13 The pooled prevalence of complete continuum of maternal healthcare services utilization was 25.51% with 95% CI (15.22, 35.81). Marked type of heterogeneity was detected between the included studies (I2 = 98.8%). Therefore, the random effect model was used to assess complete continuum of maternal healthcare services utilization The highest prevalence of complete continuum of maternal healthcare services utilization was reported by Asratie et al. 13 (47%), which was done in the Amhara region, while the lowest complete continuum of maternal healthcare services utilization (9.7%) was reported in the SNNPR region by Haile et al. 10 (Figure 2).
Figure 2.
Forest plot showing the national level of complete continuum of maternal healthcare services utilization in Ethiopia.
Handling heterogeneity
Subgroup analysis
Significant heterogeneity was observed among included primary studies. Therefore, subgroup analysis was done to identify the source of heterogeneity and minimize the random variations between the point estimates of primary studies and pooled prevalence of continuum maternal healthcare service utilization by using sample size, sampling technique, and residency. In the subgroup analysis, the overall complete continuum of maternal healthcare services utilization was found to be 27.36% in studies with a sample size less than 500, 36.37% in studies conducted only in an urban setting, and 43.13% in studies with cluster sampling technique (Table 2).
Table 2.
Subgroup analysis of complete continuum of maternal healthcare services utilization in Ethiopia (n = 7).
| Subgroup | Number of studies | Prevalence (95% CI) | I2 and p-value |
|---|---|---|---|
| Sample size | |||
| <500 | 3 | 27.36 (8.18,46.54) | (98.9%, p ⩽ 0.001) |
| ⩾500 | 4 | 24.16 (9.87,38.45) | (99.1%, p ⩽ 0.001) |
| Residency | |||
| Urban | 2 | 36.37 (33.57, 39.17) | (0%, p = 0.509) |
| Both urban and rural | 5 | 21.26 (9.71, 32.80) | (98.9%, p ⩽ 0.001) |
| Sampling technique | |||
| Multi-stage | 5 | 18.80 (11.68, 25.92) | (96.9%, p ⩽ 0.001) |
| Cluster | 2 | 43.13 (32.53, 51.73) | (93.1%, p ⩽ 0.001) |
CI: confidence interval.
Sensitivity analysis for the included studies
Sensitivity analysis was done to check the effect of individual studies on the national level of continuum of maternal healthcare services utilization. In the sensitivity analysis, the pooled prevalence continuum of maternal healthcare services utilization was observed high (28.16%) and low (21.89%) when Haile et al. 10 and Asratie et al. 13 were omitted respectively (Table 3).
Table 3.
Prevalence of continuum of maternal healthcare utilization when study omitted in Ethiopia.
| Study omitted | Prevalence of continuum of maternal healthcare utilization (95% CI) |
|---|---|
| Haile et al. 10 | 28.16 (16.56, 39.77) |
| Tizazu et al. 34 | 23.57 (12.77, 34.36) |
| Asratie et al. 13 | 21.89 (13.51, 30.27) |
| Atnafu et al. 33 | 26.17 (14.18, 38.16) |
| Emiru et al. 36 | 27.78 (15.91, 39.64) |
| Yohannes et al. 35 | 23.90 (12.83, 34.96) |
| Sertsewold et al. 21 | 27.09 (14.88, 39.31) |
CI: confidence interval.
Publication bias
Publication biases among the included studies were assessed objectively by using Egger’s regression test and the results indicated that there was no publication bias between the studies (p-value = 0.055).
Determinants of complete continuum care for maternal health services in Ethiopia
The effect of a mother’s employment status on the continuum of maternal healthcare services utilization was assessed by using two studies.10,35 The finding of this study revealed that the pooled effect of being employed mothers was significantly associated with the continuum of maternal healthcare services utilization and employed mothers were 3.16 more likely to have complete CoC for maternal health services than non-employed mothers (OR = 3.16, 95% CI = 1.82, 5.47). There was no heterogeneity between the studies (I2 = 0, p-value = 0.401) (Figure 3).
Figure 3.
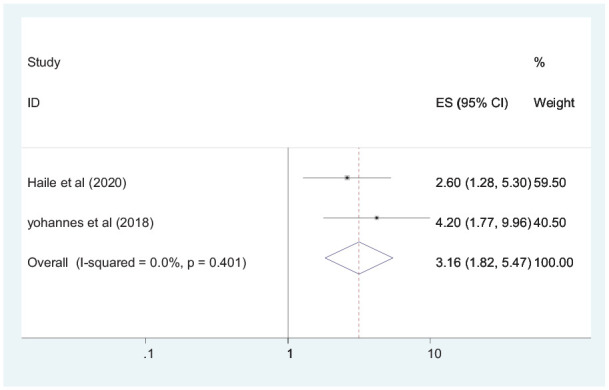
Forest plot showing the association between employed status and complete continuum of care for maternal health services in Ethiopia.
The pooled effect of the first ANC visit on continuum of maternal healthcare services utilization was evaluated by using three primary studies.10,34,36 The result of this study revealed that the first ANC visit before 16 weeks was significantly associated with the continuum of maternal healthcare services utilization and the likelihood of having a continuum of maternal healthcare services was 7.53 times higher in those women who had their first ANC visit before 16 weeks (OR = 7.53, 95% CI = 2.94, 19.29), with moderate heterogeneity (I2 = 78.8%, p-value = 0.009) (Figure 4). Based on Egger’s regression test, there was no publication bias between the studies (p-value = 0.468).
Figure 4.
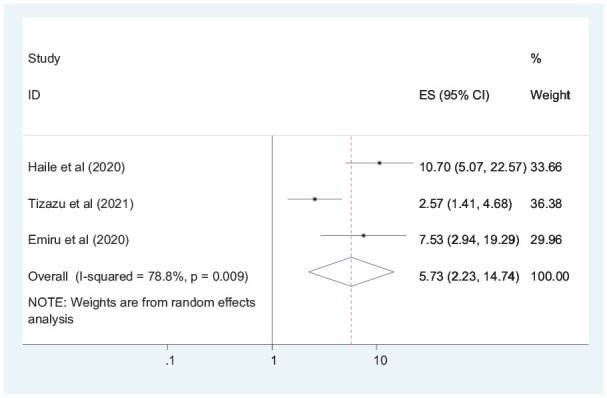
Forest plot showing pooled odds ratio for the association between first ANC visit and continuum of maternal healthcare services utilization.
The pooled effect of planned pregnancy on the complete continuum of maternal healthcare services utilization was examined by using three primary studies.10,35,36 Accordingly, the likelihood of continuum of maternal healthcare services utilization was 6.86 times higher in those women who had planned pregnancy compared with their counterparts (OR = 6.86, 95% CI = 3.47, 13.58), with mild heterogeneity (I2 = 37.6%, p-value = 0.201). Egger’s regression test showed that there was heterogeneity with a p-value of 0.581 (Figure 5).
Figure 5.
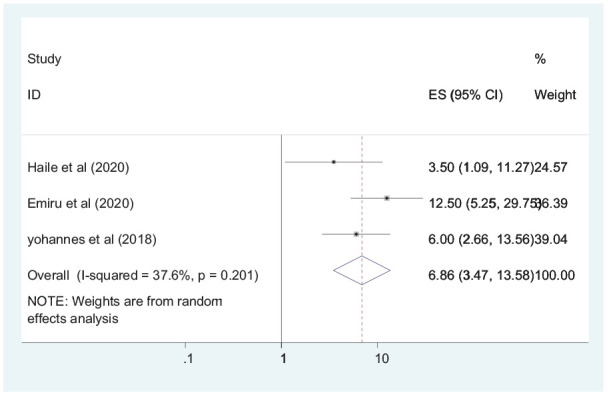
Forest plot showing pooled odds ratio for the association between planned pregnancy and complete continuum of maternal care.
A total of two primary studies10,34 were included to assess the association between birth preparedness and complication readiness plan and continuum of maternal healthcare services utilization. Accordingly, women who had good birth preparedness and complication readiness plan were 1.95 times more likely to have a complete continuum of maternal care for maternal health services (OR = 1.95, 95% CI = 1.12, 3.41), with a mild type of heterogeneity between two variables (I2 = 48.3%, p value = 0.164). As a result, the association between two variables was evaluated by using a random effect model (Figure 6).
Figure 6.
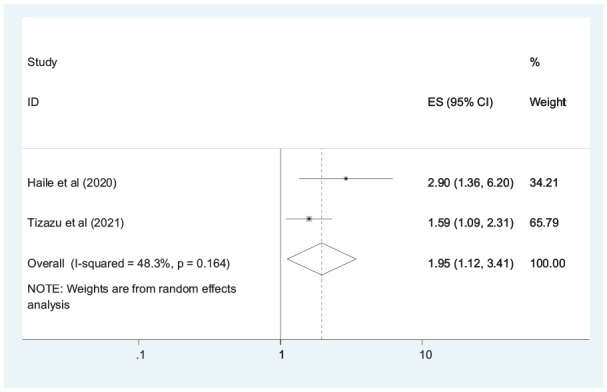
Forest plot showing pooled odds ratio for the association between birth preparedness and complication readiness plan and CoC for maternal health services.
Five studies were included to determine the pooled effects of educational status on the continuum of maternal healthcare services utilization.13,21,34–36 The findings revealed that secondary and above educational status were significantly associated with the continuum of maternal healthcare services utilization and the likelihood of having continuum of maternal healthcare services were 2.97 times higher in those mothers who had secondary and above educational status (OR = 2.97, 95% CI = 2.00, 4.41) (Figure 7). There was no heterogeneity between the studies (I2 = 0, p value = 0.861). Egger’s regression test showed that there was no publication bias with a p-value of 0.054.
Figure 7.
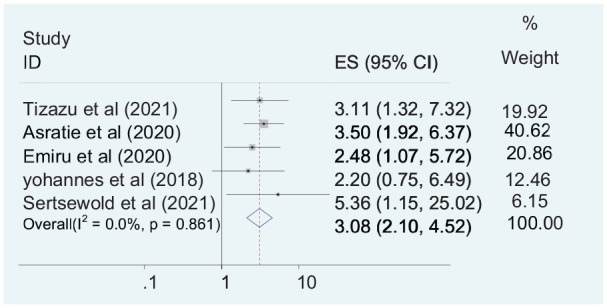
Forest plot showing pooled odds ratio for the association between educational status and a complete CoC for maternal health services.
Furthermore, the pooled effects of autonomy were significantly associated with the continuum of maternal healthcare service utilization, which was assessed by using two studies.13,21 Accordingly, autonomous mother was 3.73 times more likely to have a continuum of maternal healthcare services utilization (OR = 3.73, 2.24–6.23) (Figure 8). There was no heterogeneity between the studies (I2 = 0, p value = 0.684).
Figure 8.
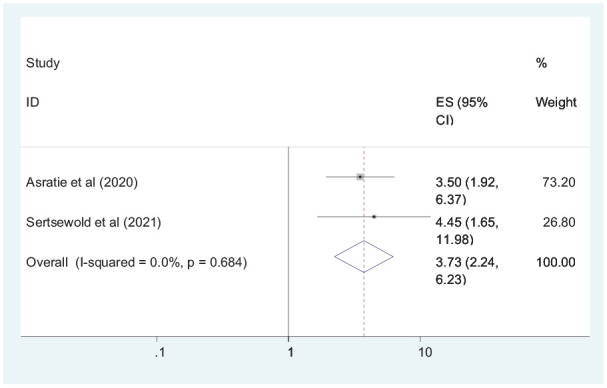
Forest plot shows the association between continuum of maternal healthcare services utilization and autonomy.
Discussion
This systematic review and meta-analysis aimed to assess the pooled prevalence and associated factors of a continuum of maternal healthcare services utilization in Ethiopia. To the best of our knowledge, this meta-analysis is the first of its kind in determining the national coverage and associated factors of complete continuum of maternal healthcare services utilization in Ethiopia and estimating the national level and its determinants may enable policymakers and clinicians at different levels to design evidence-based strategies for improvement of maternal healthcare services utilization.
The overall coverage of the complete continuum of maternal healthcare services utilization was 25.51% with 95% CI (15.22, 35.81). This finding was in line with a study finding in Pakistan, which shows the coverage of continuum of maternal health care services utilization as 27%. 12 However, this finding was higher than a study finding in Ghana and Tanzania with a reported prevalence of complete continuum of maternal health care services utilization of 8% 18 and 10% 37 respectively. The possible explanation for the above variation could be attributed to variation in the study setting, study period, and accessibility of health facilities. Besides this, variation in sociocultural and women’s health-seeking behavior between the studies settings might contribute to this difference. Furthermore, maternal health services are a free service in Ethiopia; as a result, most women might use these services in the recommended manner and have higher coverage maternal healthcare services utilization.
This finding was lower than a study finding in Nepal, which reports the prevalence of complete continuum of maternal health care services as 41%. 16 The possible explanation for this difference could be due to low maternal health services coverage; mainly low ANC coverage institutional delivery and PNC utilization in Ethiopia. According to the Ethiopian min EDHS 2019 report, only 43% of mothers had four or more ANC visits, 50% of the mother delivered by a skilled birth attendant, and 34% of mothers received a PNC check-up in the first 2 days following delivery. 23
The pooled prevalence of continuum of maternal healthcare services utilization was found to be higher in studies conducted in an urban setting than those studies done both in urban and rural areas with a pooled prevalence of 36.37% and 21.26%, respectively. The possible explanation for this variation could be because mothers in urban areas might have good exposure to mass media, good health-seeking behavior, a better understanding of the components of maternal health services, and the advantages of a continuum of maternal health services.
This study found that mothers with secondary and above educational status were more likely to utilize a complete continuum of maternal health care services than illiterate mothers. This finding was consistent with a study finding in Nepal. 24 The possible explanation could be because educated mothers can understand the formal communication with the health care providers, use modern health care services, have good knowledge on obstetric complications and danger signs, and have a better understanding of the advantage of the continuum of maternal health care services. Besides this, educated mothers may have more cultural perspectives to cooperate with health professionals and have the autonomy to seek care for maternal health and child services. 38 So, improving the educational status of women is crucial to increase continuum maternity care.
The finding of this study revealed that being an employed mother was significantly associated with the continuum of maternal health services utilization. This finding was in agreement with the EDHS finding in Ethiopia and Egypt. 39 The possible explanation could be due to the fact that employed women might have a better economy, be more autonomous, and decide freely on their healthcare compared with unemployed mothers.40,41 As a result, they might receive all components of maternal health services through pregnancy, delivery, and the postpartum period in a continuous manner.
This study found that the first ANC visit before 16 weeks was significantly associated with continuum of maternal healthcare service utilization. This finding was supported by a study finding in Khammouane Province, Lao PDR. 26 Early initiation of ANC will provide an opportunity for mothers to capture necessary information on the type and time of maternal health services and to familiarize themselves with the health facility environment.6,7,19 Giving great attention to the early initiation of ANC visits and promoting adherence of women to the ministry of health ANC visit will improve the uptake of a continuum of maternity care.
Being an autonomous mother was significantly associated with complete continuum of maternal healthcare services utilization. The possible explanation could be due to incased self-confidence, and freely decision-making abilities in autonomous women. Besides, autonomous women might decide on their social and healthcare needs without others’ influence and might have better continuity of maternal healthcare services.
Furthermore, birth preparedness and complication readiness plan were significantly associated with continuum of maternal healthcare services utilization. The possible explanation could be well-prepared mothers might follow the ministry of health’s maternal healthcare services recommendation strictly. In addition to this, well-prepared mothers might have better social support to get maternal health services and have a greater chance to deliver by the skilled birth attendant as well as continuously receive PNC visits. 42
Finally, women with planned pregnancies were more likely to utilize maternal healthcare services continuously. This finding was consistent with a study finding in Ghana. 18 The possible explanation could be women with unwanted pregnancies might not give attention to their pregnancy status and might not receive maternal healthcare services timely and in the recommended manner compared with those women with planned pregnancy. 43 Furthermore, studies in Bangladesh17,44 and low- and middle-income countries45,46 revealed that unintended pregnancy was the major determinant of ANC, SB, and PNC service utilization. Adequate counseling of family planning options (which plays a key role in reducing unintended pregnancies) and coordination of family planning services with maternal healthcare service could contribute to the improvement of completion of the continuum of maternal healthcare service utilization by reducing unintended conceptions.
This study has some limitations. Lack of studies from most regions and the self-administer cities may affect the generalizability of this study. Furthermore, significant heterogeneity was detected across studies which undermine the pooled estimate of complete CoC for maternal health services. Sub-group analysis was done by using sample size, sampling technique, and residency. However, the possible source of heterogeneity was not identified.
Conclusion
The overall prevalence of complete continuum of maternal healthcare services utilization was low in Ethiopia. Being employed mothers, being autonomous, first ANC visit before 16 weeks, having birth preparedness and complication readiness plan, secondary and above educational status, and having planned pregnancy were significantly associated with continuum of maternal healthcare services utilization. To improve the utilization of the continuum of maternal healthcare services, it is crucial to work on the improvement of women’s autonomy, educational status, and birth preparedness and complication readiness plan. Furthermore, great attention should be given to early initiation of ANC visit and promoting adherence of women to the ministry of health ANC visit recommendations. For the researchers, it is better to assess the effect of preconception care as well as the quality of each maternal healthcare service (quality of ANC, institutional delivery, and PNC) on the completion of continuum of maternal healthcare services utilization.
Supplemental Material
Supplemental material, sj-doc-1-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health
Supplemental material, sj-docx-3-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health
Footnotes
Author contribution(s): Dagne Addisu: Conceptualization; formal analysis; methodology; validation; writing – original draft.
Maru Mekie: Data curation; methodology; software; writing – review & editing.
Abenezer Melkie: Formal analysis; methodology; software; supervision; writing – review & editing.
Habtamu Abie: Data curation; formal analysis; methodology; validation; writing – review & editing.
Eniyew Dagnew: Formal analysis; investigation; methodology; validation; writing – review & editing.
Minale Bezie: Formal analysis; investigation; methodology; writing – review & editing.
Alemu Degu: Formal analysis; methodology; validation; writing – review & editing.
Shimeles Biru: Data curation; formal analysis; investigation; methodology; software; writing – review & editing.
Ermias Sisay Chanie: Data curation; formal analysis; methodology; validation; writing – review & editing.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval and consent to participate: Not applicable. This study estimated the pooled prevalence of continuum of maternal healthcare services utilization from the already published primary studies and gray literature. So, we did not use primary data that needs ethical approval and consent to participate. However, ethical issues such as plagiarism, misconduct, data fabrication/falsification, double submission/publication, and so on have been seriously observed by the authors during the data extraction, manuscript writing, and submission.
Availability of data and materials: All the datasets used in this study are accessible in the published article and its Additional files.
ORCID iD: Dagne Addisu  https://orcid.org/0000-0002-6087-6384
https://orcid.org/0000-0002-6087-6384
Supplemental material: Supplemental material for this article is available online.
References
- 1. World Health Organization (WHO). Trends in maternal mortality: 1990-2015: estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO, 2015. [Google Scholar]
- 2. Owili PO, Muga MA, Mendez BR, et al. Quality of maternity care and its determinants along the continuum in Kenya: a structural equation modeling analysis. PLoS One 2017; 12(5): e0177756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Owili PO, Muga MA, Chou Y-J, et al. Associations in the continuum of care for maternal, newborn and child health: a population-based study of 12 sub-Saharan Africa countries. BMC Public Health 2016; 16(1): 414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wang H, Liddell CA, Coates MM, et al. Global, regional, and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014; 384(9947): 957–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Carroli G, Rooney C, Villar J. How effective is antenatal care in preventing maternal mortality and serious morbidity? Sheng Zhi Yu Bi Yun [Reprod Contracep] 2005; 26(5): 300–314. [Google Scholar]
- 6. Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth 2015; 15(1): 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mothupi MC, Knight L, Tabana H. Measurement approaches in continuum of care for maternal health: a critical interpretive synthesis of evidence from LMICs and its implications for the South African context. BMC Health Serv Res 2018; 18(1): 539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kerber KJ, De Graft-Johnson JE, Bhutta ZA, et al. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet 2007; 370(9595): 1358–1369. [DOI] [PubMed] [Google Scholar]
- 9. Usman M, Anand E, Siddiqui L, et al. Continuum of maternal health care services and its impact on child immunization in India: an application of the propensity score matching approach. J Biosoc Sci 2021; 53: 643–662. [DOI] [PubMed] [Google Scholar]
- 10. Haile D, Kondale M, Andarge E, et al. Level of completion along continuum of care for maternal and newborn health services and factors associated with it among women in Arba Minch Zuria woreda, Gamo zone, Southern Ethiopia: a community based cross-sectional study. PLoS One 2020; 15(6): e0221670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Landers C. Maternal and newborn health: a global challenge (The State of the World’s Children). New York: UNICEF, 2009. [Google Scholar]
- 12. Iqbal S, Maqsood S, Zakar R, et al. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res 2017; 17(1): 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Asratie MH, Muche AA, Geremew AB. Completion of maternity continuum of care among women in the post-partum period: magnitude and associated factors in the northwest, Ethiopia. PLoS One 2020; 15(8): e0237980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Darmstadt GL, Bhutta ZA, Cousens S, et al. Evidence-based, cost-effective interventions: how many newborn babies can we save? Lancet 2005; 365(9463): 977–988. [DOI] [PubMed] [Google Scholar]
- 15. World Health Organization (WHO). PMNCH fact sheet: RMNCH continuum of care. WHO, 2011, https://www.who.int/pmnch/about/continuum_of_care/en/ (accessed December 2022). [Google Scholar]
- 16. Chalise B, Chalise M, Bista B, et al. Correlates of continuum of maternal health services among Nepalese women: evidence from Nepal Multiple Indicator Cluster Survey. PLoS One 2019; 14(4): e0215613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khan MN, Harris ML, Loxton D. Assessing the effect of pregnancy intention at conception on the continuum of care in maternal healthcare services use in Bangladesh: evidence from a nationally representative cross-sectional survey. PLoS One 2020; 15(11): e0242729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yeji F, Shibanuma A, Oduro A, et al. Continuum of care in a maternal, newborn and child health program in Ghana: low completion rate and multiple obstacle factors. PLoS One 2015; 10(12): e0142849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci 2014; 24(suppl.): 93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ram F, Singh A. Is antenatal care effective in improving maternal health in rural Uttar Pradesh? Evidence from a district level household survey. J Biosoc Sci 2006; 38(4): 433–448. [DOI] [PubMed] [Google Scholar]
- 21. Sertsewold SG, Debie A, Geberu DM. Continuum of maternal healthcare services utilisation and associated factors among women who gave birth in Siyadebirena Wayu district, Ethiopia: community-based cross-sectional study. BMJ Open 2021; 11: e051148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Management Protocol on Selected Obstetrics Topics (FMOH). Obstetric management protocol for hospitals. 2021st ed. Addis Ababa: FMOH, 2021, p. 208. [Google Scholar]
- 23. Ethiopian Public Health Institute (EPHI) and International Classification of Functioning, Disability and Health (ICF). Ethiopian mini demographic and health survey 2019: key indicators. Rockville, MD: EPHI and ICF, 2019. [Google Scholar]
- 24. Tamang TM. Factors associated with completion of continuum of Care for Maternal Health in Nepal. In: Proceedings of the IUSSP XXVIII international population conference, Cape Town, South Africa, 29 October–4 November 2017. [Google Scholar]
- 25. Enos JY, Amoako RD, Doku IK. Utilization, predictors and gaps in the continuum of care for maternal and newborn health in Ghana. Int J MCH AIDS 2021; 10(1): 98–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sakuma S, Yasuoka J, Phongluxa K, et al. Determinants of continuum of care for maternal, newborn, and child health services in rural Khammouane, Lao PDR. PLoS One 2019; 14(4): e0215635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Serván-Mori E, Heredia-Pi I, García DC, et al. Assessing the continuum of care for maternal health in Mexico, 1994-2018. Bull World Health Organ 2021; 99(3): 190–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa, ON, Canada: Ottawa Hospital Research Institute (OHRI), 2011. [Google Scholar]
- 29. Higgins JPT, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003; 327(7414): 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Borenstein M, Hedges LV, Higgins JPT, et al. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 2010; 1(2): 97–111. [DOI] [PubMed] [Google Scholar]
- 31. DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 2007; 28(2): 105–114. [DOI] [PubMed] [Google Scholar]
- 32. Peters JL, Sutton AJ, Jones DR, et al. Comparison of two methods to detect publication bias in meta-analysis. JAMA 2006; 295(6): 676–680. [DOI] [PubMed] [Google Scholar]
- 33. Atnafu A, Kebede A, Misganaw B, et al. Determinants of the continuum of maternal healthcare services in Northwest Ethiopia: findings from the primary health care project. J Pregnancy 2020; 2020: 4318197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tizazu MA, Sharew NT, Mamo T, et al. Completing the continuum of maternity care and associated factors in Debre Berhan Town, Amhara, Ethiopia, 2020. J Multidiscip Healthc 2021; 14: 21–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Yohannes GH, Woldie T, Gkidane A. Complete continuum of care for maternal health services and its associated factors among women in Mekelle town, North Ethiopia: a community based cross sectional study, 2018. https://www.pdffiller.com/210144910-mekelle-university-electronic-library-thesis (accessed November 2022).
- 36. Emiru AA, Alene GD, Debelew GT. Women’s retention on the continuum of maternal care pathway in west Gojjam zone, Ethiopia: multilevel analysis. BMC Pregnancy Childbirth 2020; 20: 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mohan D, LeFevre AE, George A, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plann 2017; 32(6): 791–799. [DOI] [PubMed] [Google Scholar]
- 38. Weitzman A. The effects of women’s education on maternal health: evidence from Peru. Soc Sci Med 2017; 180: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hamed A, Mohamed E, Sabry M. Egyptian status of continuum of care for maternal, newborn, and child health: Sohag Governorate as an example. Int J Med Sci Public Health 2018; 7(6): 417–426. [Google Scholar]
- 40. Wayack-Pambè M, Thiombiano BG, Kaboré I. Relationship between women’s socioeconomic status and empowerment in Burkina Faso: a focus on participation in decision-making and experience of domestic violence. Afr Popul Stud 2014; 28: 1146–1156. [Google Scholar]
- 41. Samari G, Pebley A. Individual and household determinants of women’s autonomy: recent evidence from Egypt. UCLA CCPR population working papers, no. PWP-CCPR-2015-004, 28 April 2015. Los Angeles, CA: California Center for Population Research (CCPR), University of California, Los Angeles (UCLA). [Google Scholar]
- 42. Nawal D, Goli S. Birth preparedness and its effect on place of delivery and post-natal check-ups in Nepal. PLoS One 2013; 8(5): e60957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Exavery A, Kanté AM, Hingora A, et al. How mistimed and unwanted pregnancies affect timing of antenatal care initiation in three districts in Tanzania. BMC Pregnancy Childbirth 2013; 13(1): 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Khan MN, Harris ML, Loxton D. Does unintended pregnancy have an impact on skilled delivery care use in Bangladesh? A nationally representative cross-sectional study using Demography and Health Survey data. J Biosoc Sci 2021; 53: 773–789. [DOI] [PubMed] [Google Scholar]
- 45. Khan MN, Harris ML, Shifti DM, et al. Effects of unintended pregnancy on maternal healthcare services utilization in low- and lower-middle-income countries: systematic review and meta-analysis. Int J Public Health 2019; 64(5): 743–754. [DOI] [PubMed] [Google Scholar]
- 46. Guliani H, Sepehri A, Serieux J. Determinants of prenatal care use: evidence from 32 low-income countries across Asia, Sub-Saharan Africa and Latin America. Health Policy Plan 2014; 29(5): 589–602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-doc-1-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health
Supplemental material, sj-docx-2-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health
Supplemental material, sj-docx-3-whe-10.1177_17455057221091732 for Continuum of maternal healthcare services utilization and its associated factors in Ethiopia: A systematic review and meta-analysis by Dagne Addisu, Maru Mekie, Abenezer Melkie, Habtamu Abie, Enyew Dagnew, Minale Bezie, Alemu Degu, Shimeles Biru and Ermias Sisay Chanie in Women’s Health