Individuals with type II diabetes mellitus (T2DM) are at an increased risk of adverse cardiovascular outcomes leading to an estimated $37.3 billion expenditure per annum in cardiovascular disease-associated care in T2DM.1 Increased genetic risk of elevated blood pressure (BP) may predispose T2DM individuals to increased risk of adverse cardiovascular events. Furthermore, whether a higher underlying genetic risk of elevated BP influences the impact of intensive glycemic control on cardiovascular outcomes in T2DM patients is not known. We conducted a post-hoc analysis of the multi-ethnic Action to Control Cardiovascular Risk in Diabetes (ACCORD)2 trial participants to evaluate the association of a BP polygenic risk score (PRS) with BP traits and adverse cardiovascular outcomes in T2DM.
Anonymized study data is available publicly through NCBI dbGAP (accession number: phs001411.v1.p1). The genome-wide array-based genotyping details for the cohort have been described elsewhere.3 Genotype imputation was performed using the NHLBI BioData Catalyst imputation server and the Trans-omics for Precision Medicine (TOPMed Freeze 8) reference panel. PLINK 2.0 was used to construct the PRS using the effect estimates from previously reported genome-wide significant loci (N=1,033 SNPs).4 The previously validated PRS was derived using the 901 SBP GWAS loci plus additional loci that were GWAS significant for DBP or Pulse Pressure.4 The average of three BP measurements obtained using Omron 907 device following 5 minutes of rest was used. As previously described, the BP values were corrected for baseline antihypertensive use (+15mmHg for SBP and +10 mmHg for DBP).4, 5 Multivariable-adjusted regression modeling accounting for age, age2, sex, BMI, randomization arm, prior cardiovascular event history, serum creatinine, fasting blood glucose, low-density lipoprotein levels, and first 10 PCs of genetic ancestry were used to assess the relationship of PRS with SBP and DBP. Multivariable-adjusted Cox regression modeling accounting for the abovementioned variables, SBP and DBP was used to examine the association of BP PRS with adverse cardiovascular outcomes (primary outcome of the ACCORD trial [composite of nonfatal myocardial infarction, stroke, or cardiovascular death])2. Proportional hazard assumptions were assessed using Schoenfeld residuals. Likelihood ratio test and Harrell’s C-statistic was used to compare the Cox proportional hazard model with and without BP PRS. We also examined the interaction between the glycemic control approach (intensive [target HbA1c: <6%] versus standard [target HbA1c: 7–7.9%]) and PRS on the primary outcome. All statistical analyses were completed using SAS 9.4 (Cary, NC). A two-sided type I error of 0.05 was deemed statistically significant.
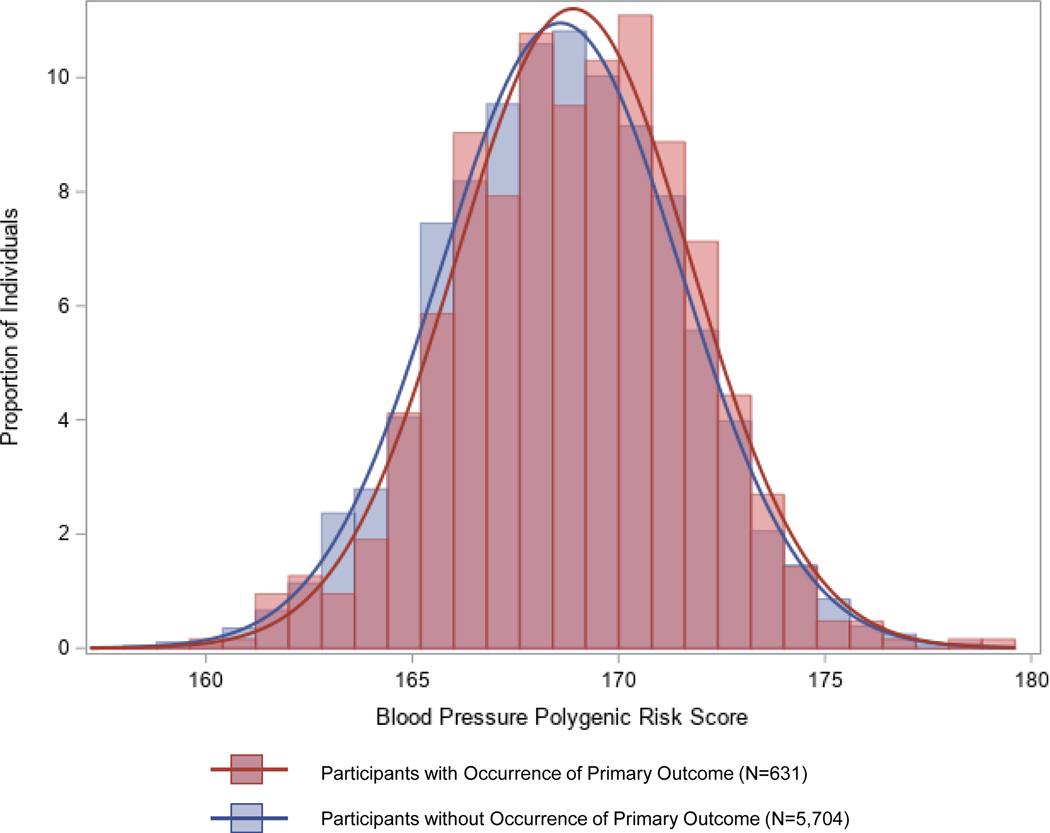
Among 6,335 of 10,251 ACCORD participants with genetic data available (median age: 62.1 [57.8, 67.1] years), there were 37.3% females, 30.4% non-White individuals, with median SBP of 147 (136, 160) mmHg, DBP of 83 (75, 90) mmHg, HbA1C of 8.1% (7.6, 8.8), and a median BP PRS of 168.4 (166.6, 170.6)(Figure 1). In the multivariable-adjusted model, per SD increase in BP PRS was associated with higher SBP (β±SE:1.93±0.23; P=4.6×10−17;R2:0.04) and DBP (β±SE:0.65±0.14; P=2.1×10−6; R2:0.09), respectively. In the multivariable-adjusted model, per SD increase in the BP PRS was associated with a 12% higher hazard (HR:1.12, 95%CI:1.02–1.23) for the occurrence of adverse cardiovascular events. There was no interaction between glycemic control therapy and the BP PRS on the primary outcome (p>0.10). Based on the likelihood ratio test, the survival model performed better with the inclusion of BP PRS for the association with primary outcome (LRχ2: 5.67;P=0.02). The inclusion of BP PRS (With BP PRS:0.66 [95%CI:0.63–0.69]) in the multivariable-adjusted model (Without BP PRS:0.65 [95%CI:0.62–0.68]) showed modest discrimination (ΔC-statistic:0.01 [95% CI:−0.02–0.04]).
Figure 1. Distribution of the Blood Pressure Polygenic Risk Score Among Individuals with Type II Diabetes Mellitus: Stratified by Adverse Cardiovascular Outcomes.
The histogram and curve and in red represent the distribution of the polygenic risk score among individuals who developed the primary outcome during the follow-up period. The histogram and curve and in blue represent the distribution of the polygenic risk score among individuals who did not developed the primary outcome during the follow-up period.
In this study, we demonstrate that BP PRS is associated with BP traits and with an increased risk of adverse cardiovascular outcomes in a high-risk multi-ethnic T2DM population. The risk of adverse cardiovascular outcomes among T2DM patients with high BP PRS did not differ by glycemic therapy approach. These results invigorate the potential implications of utilizing BP PRS in the primordial prevention of microvascular and macrovascular complications in T2DM through early intensification of lifestyle measures such as healthy diet, exercise, smoking cessation, weight management, and BP control among those with high genetic risk. Our findings indicate that differences in the genetic risk of high BP do not entirely explain the lack of cardiovascular benefit of intensive glycemic control therapy in long-standing T2DM.2 Notwithstanding, the BP PRS may be especially useful in new-onset T2DM or those with insulin resistance to assess the risk of cardiovascular outcomes and to guide intensified risk factor control. Our study is limited by the availability of a subset of the trial population for analysis and lack of adequate power for interaction testing. Further evaluation of BP PRS in large multi-ethnic population-based cohorts and among those without T2DM is needed to enhance the generalizability of the study findings. In summary, BP PRS is associated with BP traits and adverse cardiovascular events in a multi-ethnic cohort of T2DM patients and may be used to guide intensive lifestyle measures and risk-factor control in T2DM.
Acknowledgments:
Sources of Funding: Dr. Pankaj Arora is supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health (NIH) award R01HL160982 and K23HL146887, and by the Doris Duke Charitable Foundation COVID-19 Fund to Retain Clinician Scientists (Grant #2021255); UAB COVID-19 CARES Retention Program (CARES at UAB). The authors thank the investigators, staff, and participants of the ACCORD study for their support and contributions and for giving us access to this rich data set. We would like to thank the 10,251 subjects who participated in ACCORD, as well as the ACCORD clinical investigators at over 70 sites in the US and Canada. We also extend our appreciation to the following industry contributors to ACCORD: Abbott Laboratories (Abbott Park, IL); Amylin Pharmaceutical (San Diego, CA); AstraZeneca Pharmaceuticals LP (Wilmington, DE); Bayer HealthCare LLC (Tarrytown, NY); Closer Healthcare Inc. (Tequesta, FL); GlaxoSmithKline Pharmaceuticals (Philadelphia, PA); King Pharmaceuticals, Inc. (Bristol, TN); Merck & Co., Inc. (Whitehouse Station, NJ); Novartis Pharmaceuticals, Inc. (East Hanover, NJ); Novo Nordisk, Inc. (Princeton, NJ); Omron Healthcare, Inc. (Schaumburg, IL); Sanofi-Aventis US (Bridgewater, NJ); Schering-Plough Corporation (Kenilworth, NJ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funders.
Non-Standard Abbreviations and Acronyms
- ACCORD
Action to Control Cardiovascular Risk in Diabetes
- DBP
Diastolic Blood Pressure
- PRS
Polygenic Risk Score
- SNP
Single Nucleotide Polymorphism
- SBP
Systolic Blood Pressure
- T2DM
Type II Diabetes Mellitus
Footnotes
Data Availability: The ACCORD database is available upon request from the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository (https://biolincc.nhlbi.nih.gov/studies/accord/). The ACCORD GWAS data have been deposited in the database of Genotypes and Phenotypes (dbGAP, Study Accession phs001411.v1.p1).
Conflicts of Interest: None of the other authors had any conflicts of interest or financial disclosures to declare.
References
- 1.American Diabetes A. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021;44:S125–S150. [DOI] [PubMed] [Google Scholar]
- 2.Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, Byington RP, Goff DC Jr., Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr., et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morieri ML, Gao H, Pigeyre M, Shah HS, Sjaarda J, Mendonca C, Hastings T, Buranasupkajorn P, Motsinger-Reif AA, Rotroff DM, et al. Genetic Tools for Coronary Risk Assessment in Type 2 Diabetes: A Cohort Study From the ACCORD Clinical Trial. Diabetes Care. 2018;41:2404–2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evangelou E, Warren HR, Mosen-Ansorena D, Mifsud B, Pazoki R, Gao H, Ntritsos G, Dimou N, Cabrera CP, Karaman I, et al. Genetic analysis of over 1 million people identifies 535 new loci associated with blood pressure traits. Nat Genet. 2018;50:1412–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tobin MD, Sheehan NA, Scurrah KJ and Burton PR. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24:2911–35. [DOI] [PubMed] [Google Scholar]