Abstract
Background
Studies have demonstrated that elderly people with low back pain (LBP) may have poor postural control compared to healthy older adults. Poor postural control is associated with poor balance performance and a high risk of serious falls. A variety of training strategies are proposed for LBP therapy, particularly core stabilization training. But this treatment for older people with LBP remains unclear.
Methods
31 participants were randomly placed in a core stability training group (TG, n = 15) and a control group (CG, n = 16). The participants in the training group were required to complete 4 sets of core stability training and conventional physiotherapy 4 times per week for 4 weeks, whereas the participants in the control group only completed physiotherapy 4 times per week for 4 weeks. Ultrasound imaging was used to measure transverse abdominal muscle (TrA) thickness before and after the intervention. A 10-cm visual analog scale (VAS), the Oswestry Disability Index (ODI), and mobility functions were applied before and after the intervention. Data are reported as the median and range and were compared using two-way repeated-measures ANOVA,t-tests and chi-squared tests. P < 0.05 was considered significant in all statistical tests.
Results
After intervention, there was a statistically significant difference in scores in the intervention group, especially for VAS, ODI, timed up-and-go,10-m walking and the four-square step test. TrA thickness was increased after core stability training, which was not observed in the control group.
Conclusion
Core stability training is an effective intervention for older women with LBP.
Supplementary Information
The online version contains supplementary material available at 10.1186/s11556-022-00289-x.
Keywords: Low back pain, Core stability exercise, Older women, Exercise
Introduction
Low back pain (LBP) is one of the major disabling health conditions among older adults aged 60 years or older [1]. A study found that 62.5% of older people living in institutions suffer from LBP [2]. People with LBP frequently experience impairment of dynamic balance [3–5], which has a profound impact on physical activity and causes falls, which are a major health risk for older adults.
Older adults, who exhibit alterations in muscular activity patterns, muscular atrophy, higher levels of fat infiltration in muscle, appear to have a greater risk of reduced mobility function, which is more pronounced in those persons with LBP [6]. LBP affects an individual’s muscle function especially the core muscles, such as the transverse abdominus (TrA) [7]. It has been reported that the thickness of the TrA was associated with balance stability in individuals with LBP by using the ultrasound imaging [8]. Another study found that the TrA is the first muscle activated and contracted prior to the movement of the limb [9]. Therefore, daily activities such as walking and chair stand tasks, the TrA may play important roles in stabilizing the body and ensuring the successful performance of tasks. And an exercise intervention for strengthening the core muscles (e.g. TrA) seems to be one of the most effective interventions for balance performance in elderly people with LBP.
Different core stability exercise are reported as an effective intervention for LBP. Which mainly including two rehabilitation approaches: (1) a motor control exercises affecting local muscles (lumbar and lateral abdominal muscles) and (2) a general exercise for global body muscles [10]. Recently, motor control exercises affecting local muscles (lumbar and lateral abdominal muscles) have been seen to improve postural stability and/or reduce back problems in young adults [11]. Core stability training has been reported to be an effective intervention for balance performance [12–14]. Szafraniec et al. [12] reported that 4 weeks of core stability training improved balanced performance in health adults. Zou et al. [13] reported that 4 weeks core stability training improved balance ability in young adults with LBP. A meta-analysis conducted by Wang et al. [14] indicated that core stability training can improve the trunk function balance and mobility of the patients with young LBP patients. For elderly people, balance performance was more important in their daily activities. However, there is a lack of evidence regarding the effects of core stability exercises for balance performance in elderly people with LBP.
Previous studies reported that the incidence rate of LBP in females is higher than that in males [15]. LBP has been found to be an important risk factor for reoccurrence of falls in older women [16]. Therefore, the aim of the present study was to investigate the effects of core stability exercises on core muscles and balance function in elderly women with LBP. The proposed hypothesis was that core stability exercises would improve core muscle thickness and mobility function such as timed up-and-go (TUG) test, 10-m walking test (10 M-WT), and four-square step test (FSST) in older women with LBP.
Materials and methods
Design
In this triple blinded randomized controlled trial(i.e.the participants,the data analyzer and researchers taking measurements was blinded). 34 elderly people with LBP were recruited as volunteers. This sample was divided into two groups (intervention and control) by random lists. Random grouping was performed using SPSS 20.0 software (fixed value: 20190727). The study protocol was approved by the ethics committee of the First Affiliated Hospital of Sun Yat-sen University in Guangzhou, China. It was done in accordance with the Declaration of Helsinki, good clinical practices, and applicable laws and regulations, and it meets standards of the CONSORT guidelines (approval number#2019469). Written informed consent was obtained from all participants before the experiment.
Participants
The calculation of statistical power was performed a priori using G Power Software. We estimated the sample size according to the number of two basic averages. According to previous research [17], the balance data of the experimental group were selected as the effect index. With a power analysis set power of 0.80, effect size of 0.75 [18], and 10% loss rate, 12 participants were required for each group.
Participants with LBP were recruited after responding to a recruitment advertisement that was launched through the local community and different activity centers for the elderly. Then they came to the First Affiliated Hospital of Sun Yat-sen University and were diagnosed by a physician specialized in physical medicine and rehabilitation (physiatrist) .
The inclusion criteria were as follows: (1) age ≥ 60 years; (2) nonspecific LBP for at least 3 months in the last year; (3) a Mini-Mental State Examination (MMSE) score > 24 (out of 30) and Montreal Cognitive Assessment (MoCA) score > 26 (out of 30); and (5) Pain score on the visual analog scale (VAS) ≥ 3 (out of 10). Participants with LBP were excluded from the study if any of the following exclusion criteria were met: (1) a history of spinal surgery, rheumatological diseases of the spine, severe spinal pathologies or deformities, or spinal tumors; (2) a history of recent low-extremity injury, endocrine or neuromuscular disease, arthritis or orthopedic disease, orthostatic hypotension, vision problems, vestibular system disease, or any other physical injury that might affect balance; and (3) the use of psychoactive or antihypertensive drugs (antidepressants, antipsychotics, sedatives/hypnotics, antiepileptics, or antiparkinsonian drugs).
Procedures
The protocol of the present study is showed in Fig. 1.
Fig. 1.
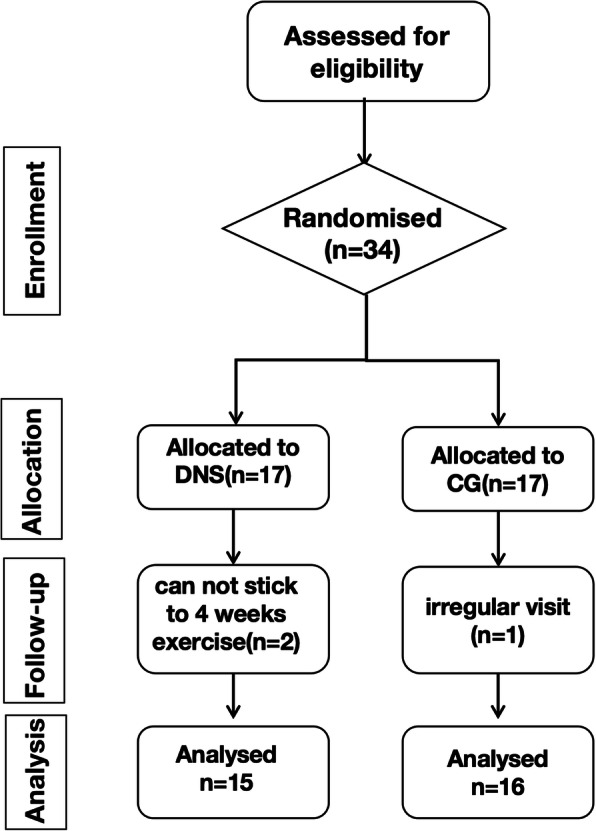
Flowchart showing participate screening and the experimental protocol
Basic evaluations (sociodemographic evaluation, MMSE, MoCA, VAS, ODI)
The experiment was conducted in bright light in a safe and quiet physiotherapy room. At the beginning, sociodemographic information of each participant was recorded in an individual information sheet. Weight, height, and body mass index (BMI) were also assessed. MMSE and MoCA scale was used to assess the cognitive function. The 10-cm VAS and Oswestry Disability Index (ODI) were used to assess the pain-related clinical outcomes. The whole experiment took approximately 30 min.
Pain-related clinical outcomes
Pain intensity was measured by a VAS (0 = no pain, 10 = pain as bad as it could be). The Oswestry disability questionnaire (0 = no disability, 100 = totally disabled) was filled out by the participants. Pain and disability were measured before and after the training [19].
ODI
The ODI is commonly used in clinical trials to measure the functional status of participants with LBP [20]. It is comprised of 10 dimensions, with 6 levels being set in each dimension. Specifically, a score of 0 represents the lowest disability level, while 5 indicates the highest disability level. Moreover, the total score is converted into percentage, with a consequent maximum of 100% [21].
Congitive function (MoCA and MMSE)
The MMSE and MoCA are both global cognitive screening measures with the same range of scores (0–30), the two tests emphasize different aspects of cognition. The MMSE is a 30-question assessment of cognitive function that evaluates attention and orientation, memory, registration, recall, calculation, language and the ability to draw a complex polygon [22]. The MoCA has six cognitive domains: short-term memory, visuospatial abilities, executive functions, attention and working memory, language, and orientation to time and space. The score range is 0 to 30; the threshold for normal cognitive function is ≧26 [23].
Ultrasound imaging measurement
Ultrasound imaging measurement was conducted before and after the training using SonixGPS ultrasound (SonixTablet, Ultrasonix, Canada) with a 15-MHz linear transducer. To standardize the technique, a supine crook-lying position (hips flexed to approximately 135°, knees flexed to 90°) was adopted by all of the participants [24]. And the evaluations were taken by the same researcher. The transducer was positioned at just above the iliac crest in the midaxillary line. Following a deep inspiration and then a forced expiration, participants were asked to continue to breathe out (further expiration). Images were collected during this period. TrA muscle thickness was measured as the distance between the superior and inferior hyperechoic muscle fascias, at the middle of the ultrasound image (Fig. 2). The ultrasound imaging measurement was repeated three times, and the mean values of were used for data analysis.
Fig. 2.

TrA ultrasound image
Mobility functions (TUG, 10 M-WT and FSST)
All the participants completed 3 assessments for mobility functions, which involved the timed up-and-go (TUG) test, 10-m walking test (10 M-WT), and four-square step test (FSST).
The TUG test required the participant to start with standing up from a chair without handles and then walking 3 m as quickly as possible. After that, the participant turned around an obstacle, walked back, and finally sat down on a chair.
In the 10 M-WT test, participants were instructed to walk at their self-perceived comfortable pace. The time to complete 10-m walking was recorded using a stopwatch [25].
The FSST included four squares, and the participant was required to start in the first square (facing the second square) and step over a cane to enter each additional square while moving in a clockwise direction. They then moved in the counter clockwise direction as quickly as possible without touching the canes (Fig. 3). The trials were repeat if the participant’s foot touched the canes.
Fig. 3.
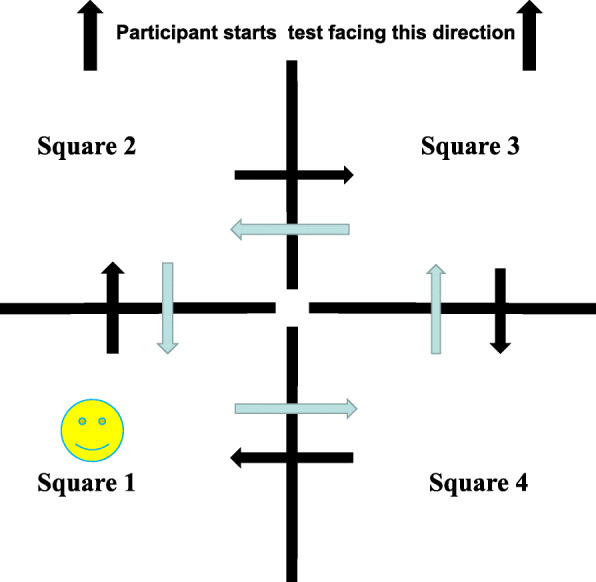
FSST test image
In the three dynamic balance tests, participants could have one or two practice trials before each test. Each test was repeated three times and were assigned randomly to the participants. The completion time were recorded during the experiment, and the mean values were used in the following analysis.
Interventions
All study personnel were trained and certified to implement study protocols in an effort to ensure standardization within and across sites. The intervention period was 4 weeks. Exercise therapists were trained to deliver exercises and physiotherapy.
Core stability group
Participants in the training group (TG) received core stability training (25-30 min) + physiotherapy (40 min).
Participants underwent intervention for 4 weeks (4 sessions per week, 65–70 min each session) .
The education session was performed at the clinic by a trained doctor at the first visit. Moreover, a printed pamphlet with instructions on how to perform the exercises was given to each participant.
Abdominal respiration skills are learned before the intervention, the exercise movements selected in this study were mainly focus on abdominal muscles such as TrA [14]. Exercises were designed 4 sets, two static exercises (Fig. 4, A and B) and two dynamic exercises (Fig. 4, C and D), from 8 to 10 repetitions and contractions from 10 s to 20 s. Rest intervals were set as 10 s between the sets and 2 mins between the exercises. Core muscle stability training for intervention group included:
crawl position exercise (Fig. 4, A)
the quadruped exercise with yoga blocks (Fig. 4, B)
abdomen exercise with swiss ball in supine position (Fig. 4, C)
abdomen exercise with resistance band in supine position (Fig. 4, D)
Fig. 4.
Image of training. Core stabilization exercises: (A). crawl position exercise, (B). the quadruped exercise with yoga blocks, (C). abdomen exercise with swiss ball in supine position (D). abdomen exercise with resistance band in supine position
The physiotherapy treatment included interference wave and magnetic resonance thermal therapy. Two pairs of interference wave electrodes (SK-9SDX, MINATO, Japan) intersected with each other around the painful point of back for 20 min. For magnetic resonance thermal therapy (magneto-vibration heat treatment (LGT-2600B, China), the participants were positioned in a supine position, the foldable electrodes were placed in the participant’s waist pain site, setting mode 1(vibration therapeutic apparatus:50–120 beats/s, temperature:40–58 °C), underwent for 20 min. The training for the TG took about 1 h. There were 4 weeks of training at 4 times per week.
CG group
Participants in the CG received physiotherapy that included interference wave + magnetic resonance thermal therapy for a total of 40 min every time at 4 times a week for 4 weeks.
Statistical analysis
Differences in demographic variables between groups were tested using an independent t-test. Two-way repeated-measures ANOVA was conducted to analyze the data from the ultrasound imaging measurement, VAS, ODI, and dynamic balance tests. The effect size for the statistical analysis was reflected by ƞ2p. The value of low effect size, moderate effect size and high effect size was 0.04, 0.25 and 0.64 [26]. The between-subject factor was the group (TG or CG), and the within-subject factor was time (pre-experiment and post-experiment). Greenhouse-Geisser correction was used when Mauchly’s test of sphericity was violated. Post hoc pairwise comparisons with Bonferroni adjustment were applied when significant interaction effects were observed. The thickness change of Tra was selected to explore the associations between the change of mobility functions. The significance level was set at P < 0.05 for all statistical tests. All data were analyzed using the software SPSS 20.0.
Results
Participants
Participants’ socio-demographic and health characteristics at baseline are shown in Table 1. Briefly, the sample consisted of 31 adults, with a mean age of 64 years. Of the 34 participants who met the inclusion criteria, 31 participants received a final assessment, and the dropout rate was about 9%. More specifically, 2 participants in the TG were excluded because of they could not commit to 4 weeks exercise, and 1 patient in the CG was excluded because of her irregular visits. Therefore, 15 participants ultimately remained in the TG, and 16 participants remained in the CG for analysis. All the participants recruited in the present study were female. There were no significant differences in age, weight, or height between two groups (P ≥ 0.05; Table 1).
Table 1.
Demographic characteristics of the two groups
| Characteristic | TG (n = 15) | CG (n = 16) | t-values | P-values | |
|---|---|---|---|---|---|
| Age (years) | 64.60 (3.71) | 64.12 (2.96) | 0.39 | 0.69 | |
| Sex | Female | Female | – | – | |
| Hand dominance | Right | Right | – | – | |
| Height (m) | 1.58 (4.63) | 1.57 (3.29) | 0.69 | 0.49 | |
| Weight (kg) | 58.40 (5.06) | 56.06 (3.15) | 1.553 | 0.13 | |
| MMSE | 28.93 (0.96) | 29.06 (0.85) | −0.39 | 0.69 | |
| MoCA | 26.66 (0.72) | 26.81 (0.83) | −0.51 | 0.60 | |
| Body mass index (kg/m2) | 23.34 (1.37) | 22.72 (1.20) | 1.337 | 0.19 | |
| Pain duration (years) | 8.40 (3.37) | 7.81 (3.05) | 0.50 | 0.61 | |
| Academic level | Primary education (0-7 years) | 2 (13.33) | 0 | – | 0.28 |
| Secondary education (8-15 years) | 10 (66.67) | 11 (73.33) | – | ||
| Tertiary education (≥16 years) | 3 (20) | 5 (29.41) | – | ||
The categorical variables are expressed as n (%), and the continuous variable are expressed as the mean (standard deviations). kg kilogram, m meter, MMSE Mini-Mental State Examination, MoCA Montreal Cognitive Assessment, VAS visual analog scale, ODI Oswestry disability index, CG control group, TG core stability training group.
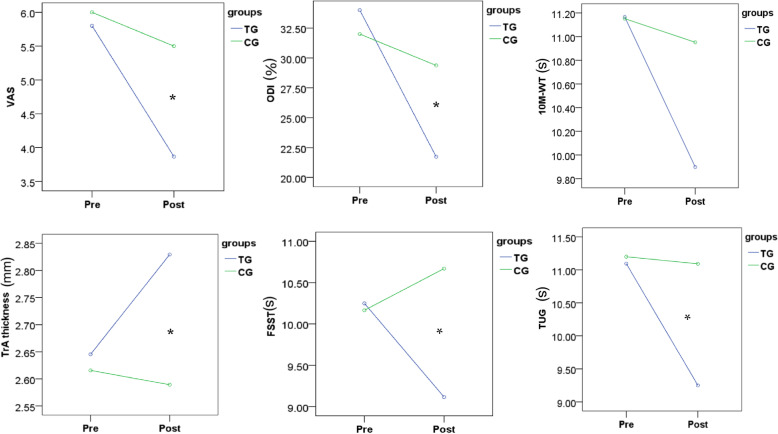
Pre- and post-intervention-related change in all outcome measures
Two-way repeated-measures ANOVA was conducted to analyze the data of TrA thickness, VAS, ODI, and dynamic balance tests. The time effect was not significant in the TrA and FSST parameters [TrA thickness: F (1, 29) = 3.36, P = 0.077, ƞ2p = 0.104; FSST: F (1, 29) = 1.39, P = 0.247, ƞ2p = 0.046]. The time effect was significant for VAS, ODI, TUG, and 10 M-WT [VAS: F (1, 29) = 26.10, P < 0.001, ƞ2p = 0.474, ODI: F (1, 29) = 35.24, P < 0.001, ƞ2p = 0.549, 10 M-WT: F (1, 29) = 6.99, P = 0.013, ƞ2p = 0.194, TUG: F (1, 29) = 27.14, P < 0.001, ƞ2p = 0.483]. The group effect was significant for the VAS, TUG, 10 M-WT, and FSST parameters [VAS: F (1, 29) = 12.30, P = 0.001, ƞ2p = 0.298, 10 M-WT: F (1, 29) = 5.82, P = 0.022, ƞ2p = 0.167, FSST: F (1, 29) = 5.39, P = 0.027, ƞ2p = 0.157, TUG: F (1, 29) = 11.65, P = 0.002, ƞ2p = 0.287]. The group effect was not significant for TrA and ODI [TrA thickness: F (1, 29) = 0.437, P = 0.514, ƞ2p = 0.015;ODI: F (1, 29) = 0.966, P = 0.334, ƞ2p = 0.334]. The time × group interaction effect was significant for TrA thickness [F (1, 29) = 5.98, P = 0.021, ƞ2p = 0.171], VAS [F (1, 29) = 9.05, P = 0.005, ƞ2p = 0.238], ODI [F (1, 29) = 14.77, P = 0.001, ƞ2p = 0.338], FSST [F (1, 29) = 9.48, P = 0.005, ƞ2p = 0.246], and TUG [F (1, 29) = 21.50, P < 0.001, ƞ2p = 0.426]. However, the time × group interaction effect was not significant for 10 M-WT: F (1, 29) = 3.70, P = 0.064, ƞ2p = 0.113.
Figure5 Pre- and Post-intervention-related change in all outcome measures in TG and CG (* indicate significant interaction effects)
Fig. 5.
Presents a Pre- and Post-intervention-related change in all outcome measures
Two-way repeated-measures ANOVA was conducted to analyze the data of TrA thickness, VAS, ODI, and dynamic balance tests (Table 2). As expected, core training and physiotherapy both had positive effects on reducing pain intensity, but there was more reduction in the TG. As for ODI, it only decreased in the TG. Improvements for all the motor functions were observed in only the TG. The TG participants’ TrA thicknesses were significantly changed.
Table 2.
Outcome variables pre- and post-interventions for two groups
| Items | TG | CG | ||
|---|---|---|---|---|
| Outcome variables | Pre | post | Pre | post |
| TrA | 2.64 (0.54) | 2.82 (0.51) | 2.61 (0.64) | 2.58 (0.59) |
| VAS | 5.80 (0.94) | 3.80 (1.35) | 6.00 (0.89) | 5.5 (0.63) |
| ODI | 34.0 (7.78) | 21.72 (8.84) | 32.00 (9.43) | 29.37 (8.66) |
| TUG | 11.09 (0.89) | 9.24 (0.90) | 11.20 (0.76) | 11.09 (1.17) |
| 10 M-WT | 11.16 (1.24) | 9.89 (0.85) | 11.15 (0.69) | 10.95 (1.03) |
| FSST | 10.24 (0.86) | 9.11 (1.09) | 10.16 (1.45) | 10.67 (1.08) |
VAS visual analog scale, ODI Oswestry disability index, CG control group, TG core stability training, TUG timed up-and-go, 10 M-WT 10-m walking test, FSST four-square step test, TrA transverse abdominal muscle.
Associations between the change of TrA thickness and the change of dynamic balance scores from pre- and post-interventions for two groups
Associations between the change of TrA thickness and the change of dynamic balance scores from pre- and post-interventions for two groups were shown in Table 3 All the associations between change of TrA thickness and change scores in dynamic balance were not significant (P ≥ 0.05).
Table 3.
Associations between the change of TrA thickness and the change of dynamic balance scores from pre- and post-interventions for two groups
| TUG | 10 M-WT | FSST | |||
|---|---|---|---|---|---|
| TrA thickness | Core training group | Pearson r | 0.165 | 0.085 | 0.079 |
| P | 0.557 | 0.764 | 0.780 | ||
| Control group | Pearson r | 0.091 | 0.242 | 0.361 | |
| P | 0.737 | 0.366 | 0.369 | ||
Discussion
The aim of this randomized controlled trial was to estimate the effectiveness of core stability training in older women with LBP. To the best of our knowledge, this is the first clinical trial presenting the effects of a 4-week core stability training in older women with LBP, which makes it difficult to compare our study with any previous study. The results showed that training and physiotherapy can both reduce pain compared to the baseline, but the core stability training was more effective in ODI and TrA thickness than the control treatment. For balance function, the findings of TUG, 10 M-WT, and FSST suggested that TG participants’ dynamic balance performance was significantly enhanced.
TUG, FSST, 10 M-WT tests are reliable and valid fall-risk assessments [25, 27, 28]. The study has found that for healthy elderly people and elderly people with balance dysfunction.the cut-off point time for perform the FSST was 11 s, TUG was 12 s [27, 28]. In this study the TUG and FSST assessment in elderly people with LBP were approached this cut-off point value pre intervention. Improvements for all the motor functions were observed only in the TG indicated that core stability training can be effective in older participants with LBP who may have balance deficits. A meta-analysis conducted by Gamble et al. [29] demonstrated that core stability exercise could improve balance ability in stroke patient. Another study conducted by Saravanakumar et al. [30] found that tai chi and yoga significantly improved the dynamic balance performance in older adults. However Tai chi and yoga are physical activity focus on motor balance and regulate emotion. For elderly people with LBP, who exhibit alterations in muscular atrophy, especially the core muscles such as TrA. The core stability exercise focus on core muscles and motor control seem to be more effective.
In the present study, our sample was older people with LBP. Pain induces spinal motility restrictions, lumbar proprioceptive losses, weakening of lower-extremity sensory feedback, and trunk muscle weakness and atrophy [31–33]. Which could have a profound impact on their motor function. In our study, the pain was significantly decreased in the TG compared to the CG. The previous review showed that exercise-based treatment approaches are most likely to result in improvements in pain and function. Which was consistent with our study.
We assessed TrA thickness to assess the effect of core stability training on older people with LBP. This muscle is one of the important muscles in maintaining the stability and proprioceptive sense of the lumbar trunk. It manages the stability of the body trunk through co-contraction without movement of joints. Our results showed TrA thickness was increased in the core stability training group. Which was consistent with a previous study conducted by Kong et al. [34]. In that study, core exercise training significantly increased the thicknesses of the TrA in LBP young adults. However, Park et al. [35] found no significant change in TrA thickness in LBP young adults after 12 times of core exercise training. A potential reason was that the 12 times of training were insufficient to make significant changes in muscle morphology. For elderly people, who could, benefit more from the training than the untrained young adults [36]. Thus in our study TrA thickness was increased after 16 training sessions four times a week of core exercise training.
Associations between change of TrA thickness and the change of dynamic balance were not significant in our study. These findings were inconsistent with those reported in the previous studies [8, 37, 38]. In Halliday et al’s [37] study, after 8-weeks core exercise training, the change of thickness of the TrA was associated with the change of balance stability. Shamsi et al. [8] reported thicknesses of TrA was associated with balance stability in individuals with LBP. The reasons why we did not find the significant sssociations between change of TrA thickness and the change of dynamic balance in this study might be as follows. First, the potential reasons were that the duration of intervention, in Halliday et al’s [37] study, the duration of the intervention was 8-weeks, whereas in our study, the duration of intervention was only for 4 weeks. The shorter duration might not sufficiently lead to significance association between TrA thickness with balance performance. Second, it might related about use the different tools of balance measurements, in Gong et al’s [38] study, the static balance ability was the outcome meassures. However, in our study we assessed the dynamic balance performance.
Our study addresses several gaps in the knowledge and limitations of previous research in this area. Few studies have focused on core exercise for balance performance in older women with LBP. Given the importance of balance performance for independent living in old age and poor balance being associated with falls risk, the intervention for balance performance in elderly people with LBP is worthy of attention. Our results suggested that 4 weeks of core stability training could enhance the balance ability in elderly people with LBP.
A major limitation of the present study is a lack of follow-ups. Another limitation is that we do not measured the stability of the trunk. Third, this study excluded the participants any other physical injury. The sample recruited in the present study might not be able to represent the general older adults. The future study should consider the effects of any other physical injury on balance. Fourth, the short intervention period may be a limiting factor of this study. In the next study, it will be necessary to examine the effects of core training effect on core muscles by lengthening the study period. Fifth, the study only assess the abdominal muscle, the back muscle such as multifidus were not considered in this study.
Conclusions
Our study suggests that core stability training is a promising technique to improve associated symptoms and motor balance in older women with LBP.
Supplementary Information
Acknowledgements
This study was conducted in department of Rehabilitation Medicine, The First Affiliated Hospital, Sun Yat-sen University We are extremely grateful to all study participants for the use of their personal data. We would like to express our deepest gratitude to everyone who participated and cooperated in this study.
Abbreviations
- LBP
Low back pain
- TG
Core stability training group
- CG
Control group
- TrA
Transverse abdominal muscle
- VAS
Visual analog scale
- TUG
Timed up-and-go
- 10 M-WT
10-m walking test
- FSST
Four-square step test
- MMSE
Mini-Mental State Examination
- MoCA
Montreal Cognitive Assessment
- ODI
Oswestry disability index
Authors’ contributions
C.H.W: conceived the design,performed the literature review, L.L: conceived the design, X.C:revised the first draft. L.G: analyzed the data, wrote the first draft of the article, H.J.H:performed the intervention training. Q.H.Y: collected the data. Y.L: collected the data. X.L:collected the data. Z.C.L:collected the data. All authors approved the final version of the manuscript.
Funding
The authors thank the following for their assistance and contribution to the development and achievement of this research:
National Natural Science Foundation of China (grant number 82002375);
National Natural Science Foundation of China (grant number 82172532).
Guangdong Basic and Applied Basic Research Foundation(grant number 2022A1515011229);
Fundamental Research Funds for the Central Universities (grant number G2021KY05101);
The Key Research and Development Project of Shaanxi province (grant number 2022SF-117) .
The funding body had no role in the design of the study, the collection, analysis or interpretation of data or in writing the manuscript. Open Access funding provided by the First Affiliated Hospital of Sun Yat-sen University.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted as a single-blind randomized controlled trial (i.e., where the data analyzer was blind to the study). The study protocol was approved by the ethics committee of the First Affiliated Hospital of Sun Yat-sen University (grant number#2019469) in Guangzhou, China, in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants and the rights of the participants were protected.
Consent for publication
All authors approved the final version to be published.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Le Ge, Email: 786674648@qq.com.
Huanjie Huang, Email: huanghnj@mail.sysu.edu.cn.
Qiuhua Yu, Email: yuqiuhua@mail.sysu.edu.cn.
Yan Li, Email: liyan337@mail2.sysu.edu.cn.
Xin Li, Email: lixin279@mail.sysu.edu.cn.
Zhicheng Li, Email: lizhch59@mail.sysu.edu.cn.
Xi Chen, Email: chenxi8@mail.sysu.edu.cn.
Le Li, Email: lile5@nwpu.edu.cn.
Chuhuai Wang, Email: wangchuh@mail.sysu.edu.cn.
References
- 1.Garcia WJ, Johnson A, Keldermans D, Tang B. Exercise and low Back pain in the older adult: current recommendations. J Allied Health. 2019;48(4):302–307. [PubMed] [Google Scholar]
- 2.Podichetty VK, Mazanec DJ, Biscup RS. Chronic non-malignant musculoskeletal pain in older adults: clinical issues and opioid intervention. Postgrad Med J. 2003;79(937):627–633. doi: 10.1136/pmj.79.937.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, Glynn NW, Weiner DK. A Mind-Body Program for Older Adults With Chronic Low Back Pain: A Randomized Clinical Trial. JAMA Intern Med. 2016;176(3):329–337. doi: 10.1001/jamainternmed.2015.8033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calvo Lobo C, Vilar-Fernández JM, Losa-Iglesias ME, López-López D, Rodríguez-Sanz D, Palomo-López P, Becerro-de B-VR. Depression Symptoms Among Older Adults With and Without Subacute Low Back Pain. Rehabil Nurs. 2019;44(1):47–51. doi: 10.1097/rnj.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 5.Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, Tylavsky FA. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol Ser A Biol Med Sci. 2005;60(11):1420–1424. doi: 10.1093/gerona/60.11.1420. [DOI] [PubMed] [Google Scholar]
- 6.Sions JM, Elliott JM, Pohlig RT, Hicks GE. Trunk muscle characteristics of the multifidi, erector spinae, psoas, and Quadratus Lumborum in older adults with and without chronic low Back pain. J Orthop Sports Phys Ther. 2017;47(3):173–179. doi: 10.2519/jospt.2017.7002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ShahAli S, Arab AM, Ebrahimi E, Shah Ali S, Rahmani N, Negahban H, Kazemnejad A, Bahmani A. Ultrasound measurement of abdominal muscles during clinical isometric endurance tests in women with and without low back pain. Physiother Theory Pract. 2019;35(2):130–138. doi: 10.1080/09593985.2018.1441345. [DOI] [PubMed] [Google Scholar]
- 8.Shamsi M, Sarrafzadeh J, Jamshidi A, Zarabi V, Pourahmadi MR. The effect of core stability and general exercise on abdominal muscle thickness in non-specific chronic low back pain using ultrasound imaging. Physiother Theory Pract. 2016;32(4):277–283. doi: 10.3109/09593985.2016.1138559. [DOI] [PubMed] [Google Scholar]
- 9.Hodges PW, Richardson CA. Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther J. 1997;77(2):132–142. doi: 10.1093/ptj/77.2.132. [DOI] [PubMed] [Google Scholar]
- 10.Brumitt J, Matheson JW, Meira EP. Core stabilization exercise prescription, part I: current concepts in assessment and intervention. Sports Health. 2013;5(6):504–509. doi: 10.1177/1941738113502451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ganesh GS, Kaur P, Meena S. Systematic reviews evaluating the effectiveness of motor control exercises in patients with non-specific low back pain do not consider its principles - a review. J Bodyw Mov Ther. 2021;26:374–393. doi: 10.1016/j.jbmt.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Szafraniec R, Bartkowski J, Kawczyński A. Effects of Short-Term Core Stability Training on Dynamic Balance and Trunk Muscle Endurance in Novice Olympic Weightlifters. J Hum Kinet. 2020;74:43–50. doi: 10.2478/hukin-2020-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou CJ, Li JH, Wu FC, Li YZ, Pan HY, Wu T. The effects of core stability training in nurses with nonspecific low back pain. Medicine (Baltimore) 2021;100(25):e26357. doi: 10.1097/MD.0000000000026357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang XQ, Zheng JJ, Yu ZW, Bi X, Lou SJ, Liu J, Cai B, Hua YH, Wu M, Wei ML, Shen HM, Chen Y, Pan YJ, Xu GH, Chen PJ. A Meta-analysis of Core stability exercise versus general exercise for chronic low Back pain. PLoS One. 2012;7(12):e52082. doi: 10.1371/journal.pone.0052082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Nakamura K, Kawaguchi H, Yoshimura N. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res (Hoboken) 2011;63(10):1425–1431. doi: 10.1002/acr.20562. [DOI] [PubMed] [Google Scholar]
- 16.Palacios-Ceña D, Alonso-Blanco C, Hernández-Barrera V, Carrasco-Garrido P, Jiménez-García R, Fernández-de-las-Peñas C. Prevalence of neck and low back pain in community-dwelling adults in Spain: an updated population-based national study (2009/10-2011/12) Eur Spine J. 2015;24(3):482–492. doi: 10.1007/s00586-014-3567-5. [DOI] [PubMed] [Google Scholar]
- 17.Le G, Yu Q, Wang C, Huang H, Li X, Zhang S, Zhang S. How cognitive loads modulate the postural control of older women with low back pain? BMC Geriatr. 2021;21(1):82. doi: 10.1186/s12877-021-02025-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim B, Yim J. Core stability and hip exercises improve physical function and activity in patients with non-specific low Back pain: a randomized controlled trial. Tohoku J Exp Med. 2020;251(3):193–206. doi: 10.1620/tjem.251.193. [DOI] [PubMed] [Google Scholar]
- 19.Fontana Carvalho AP, Dufresne SS, Rogerio de Oliveira M, Couto Furlanetto K, Dubois M, Dallaire M, Ngomo S, da Silva RA. Effects of lumbar stabilization and muscular stretching on pain, disabilities, postural control and muscle activation in pregnant woman with low back pain. Eur J Phys Rehabil Med. 2020;56(3):297–306. doi: 10.23736/S1973-9087.20.06086-4. [DOI] [PubMed] [Google Scholar]
- 20.Roland M, Fairbank J. The Roland-Morris disability questionnaire and the Oswestry disability questionnaire. Spine (Phila Pa 1976) 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 21.Liu H, Tao H, Luo Z. Validation of the simplified Chinese version of the Oswestry disability index. Spine (Phila Pa 1976) 2009;34(11):1211–1216. doi: 10.1097/BRS.0b013e31819e2b34. [DOI] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of participants for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Abzhandadze T, Rafsten L, Lundgren Nilsson Å, Palstam A, Sunnerhagen KS. Very Early MoCA Can Predict Functional Dependence at 3 Months After Stroke: A Longitudinal, Cohort Study. Front Neurol. 2019;10:1051. doi: 10.3389/fneur.2019.01051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Whittaker JL. Ultrasound imaging of the lateral abdominal wall muscles in individuals with lumbopelvic pain and signs of concurrent hypocapnia. Man Ther. 2008;13(5):404–410. doi: 10.1016/j.math.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Duncan RP, Combs-Miller SA, McNeely ME, et al. Are the average gait speeds during the 10meter and 6minute walk tests redundant in Parkinson disease? Gait Posture. 2017;52:178–182. doi: 10.1016/j.gaitpost.2016.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):30. doi: 10.1037/a0024338. [DOI] [PubMed] [Google Scholar]
- 27.Goh EY, Chua SY, Hong SJ, et al. Reliability and concurrent validity of Four Square Step Test scores in subjects with chronic stroke: a pilot study. Arch Phys Med Rehabil. 2013;94(7):1306–1311. doi: 10.1016/j.apmr.2013.01.027. [DOI] [PubMed] [Google Scholar]
- 28.Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 29.Gamble K, Chiu A, Peiris C. Core stability exercises in addition to usual care physiotherapy improve stability and balance after stroke: a systematic review and Meta-analysis. Arch Phys Med Rehabil. 2021;102(4):762–775. doi: 10.1016/j.apmr.2020.09.388. [DOI] [PubMed] [Google Scholar]
- 30.Saravanakumar P, Higgins IJ, van der Riet PJ, Marquez J, Sibbritt D. The influence of tai chi and yoga on balance and falls in a residential care setting: a randomised controlled trial. Contemp Nurse. 2014;48(1):76–87. doi: 10.1080/10376178.2014.11081929. [DOI] [PubMed] [Google Scholar]
- 31.Ishak NA, Zahari Z, Justine M. Muscle functions and functional performance among older persons with and without low Back pain. Curr Gerontol Geriatr Res. 2016;2016:8583963–8583910. doi: 10.1155/2016/8583963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Russo M, Deckers K, Eldabe S, Kiesel K, Gilligan C, Vieceli J, Crosby P. Muscle control and non-specific chronic low Back pain. Neuromodulation. 2018;21(1):1–9. doi: 10.1111/ner.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kato S, Murakami H, Demura S, et al. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet Disord. 2019;20(1):273. doi: 10.1186/s12891-019-2655-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kong YS, Lee WJ, Park S, Jang GU. The effects of prone bridge exercise on trunk muscle thickness in chronic low back pain patients. J Phys Ther Sci. 2015;27(7):2073–2076. doi: 10.1589/jpts.27.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Park SD, Yu SH. The effects of abdominal draw-in maneuver and core exercise on abdominal muscle thickness and Oswestry disability index in subjects with chronic low back pain. J Exerc Rehabil. 2013;9(2):286–291. doi: 10.12965/jer.130012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bickel CS, Cross JM, Bamman MM. Exercise dosing to retain resistance training adaptations in young and older adults. Med Sci Sports Exerc. 2011;43(7):1177–1187. doi: 10.1249/MSS.0b013e318207c15d. [DOI] [PubMed] [Google Scholar]
- 37.Halliday MH, Pappas E, Hancock MJ, Clare HA, Pinto RZ, Robertson G, Ferreira PH. A randomized clinical trial comparing the McKenzie method and motor control exercises in people with chronic low back pain and a directional preference: 1-year follow-up. Physiotherapy. 2019;105(4):442–445. doi: 10.1016/j.physio.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 38.Gong W. Correlations between transversus abdominis thickness, lumbar stability, and balance of Female University students. J Phys Ther Sci. 2013;25(6):681–683. doi: 10.1589/jpts.25.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.