Abstract
Background
The use of telehealth as a viable mobility to deliver quality services steadily increases in various levels of the health system. Despite the increasing use of telemedicine in secondary and tertiary health care services, there is a long way to go in the use of this technology in public health and primary health care (PHC). This study aimed to explore the features, approaches, and various dimensions of telehealth in PHC.
Methods
A scoping review was conducted using the Arksey and O'Malley framework. A search was conducted in three bibliographic databases including PubMed, Web of Sciences, and Scopus and in Google Scholar to collect papers published in November 2018 to 2000. Data were extracted according to a predefined form and check for completeness and accuracy by a second reviewer.
Results
Through reviewing papers, the authors extracted information on the general characteristics and features of telehealth services, kinds of PHC services delivered via telehealth, hardware and software facilities used for providing health care through telehealth services packages, as well as their benefits, outcomes and obstacles.
Conclusion
Telehealth can be used for different purposes of PHC through deploying a full range of communication channels available to the public. Due to the opportunistic use of existing devices and platforms, telehealth can provide scalable PHC services nationwide and worldwide. However, implementing telehealth in PHC faces challenges from technical, organizational, and human perspectives. Digital equity (in terms of technology access and e-health literacy) is required to expand telehealth services to the populations in underserved areas.
Keywords: telemedicine, telehealth, primary care, general practice, family doctor, services, guideline, package
Introduction
Advancement and accessibility of healthcare services are among the measures of a society's development. Recent progress in telecommunication technologies has further emphasized the global importance of access to healthcare. It has impacted the methods of medical care and healthcare delivery and, as a result, remote access to health-related services known as telehealth has emerged as one of the most effective paradigms to improve the accessibility of health services.1, 2, 3, 4, 5
National healthcare systems are under pressure to provide prompt, accessible, and high-quality healthcare in cost-efficient ways.6, 7 By bridging the distance between care providers and receivers, telehealth can provide healthcare to hard-to-reach areas and help solve some of the issues patients face within the healthcare system. Telehealth is a new approach to delivering remote health services via real-time communication between the patient and the healthcare provider, using electronic audio and visual means.7,9, 10, 11 With telehealth, information is exchanged over communication networks to monitor the health status of patients and to offer clinical recommendations, consultations, treatment, education, and administrative services.1, 2, 5, 12, 13, 14
Telehealth has various benefits in primary health care (PHC), ranging from seamless access to health services for people in remote places to self-management promotion, patient empowerment, cost reduction of unnecessary referrals, and decreasing the need for commuting to seek medical care. Physicians can share information via telehealth channels for better clinical education, faster diagnosis, disease prevention and quicker therapeutic interventions.1, 2, 5, 11, 12, 13, 15, 16, 17, 18 Telehealth services also open up a new way of communication among patients and family caregivers and improve the sharing of critical information and experiences.14 Use of this technology can also incentivize physicians to recruit and retain in remote and rural areas by allowing them to remotely communicate with their colleagues and take advantage of long-distance education.19 The health system can also overcome the issue of limited resources and facilities by utilizing telehealth.20
In PHC, telehealth can usually be offered when a patient is seeking the doctor's advice about a non-emergency medical problem. It does not replace face-to-face consultation, but complements it by offering timely PHC services in areas facing logistical hurdles to receiving secondary health care.1, 2, 3 PHC as the first contact point of population with health system aims to achieve the equity in population access to the health services.21, 22 Telehealth can contribute to this aim and overcome the challenges.23, 24, 25
In this paper, we aim to determine the characteristics and components of telehealth packages through a scoping systematic review by answering the following questions:
What are the general characteristics of telehealth in PHC?
What kinds of PHC services can be offered in the form of telehealth?
What facilities are used for providing PHC through telehealth?
Methods
This study is a scoping systematic review, and the methodology for this review was based on the framework outlined by Arksey and O'Malley.26 The researchers carried out a preliminary scoping search to determine a terminology for establishing the search terms of the study.
Data Sources and Search Strategy
We searched three electronic databases including PubMed, Web of Science, and Scopus. Google Scholar was also searched for relevant articles published in November 2018 to 2000. The combination of the following keywords, including Telemedicine, Telehealth, Primary Care, General Practice, Family Doctor, Services, Guideline, Package, Primary Health Care, Primary Healthcare, were used to find the studies.
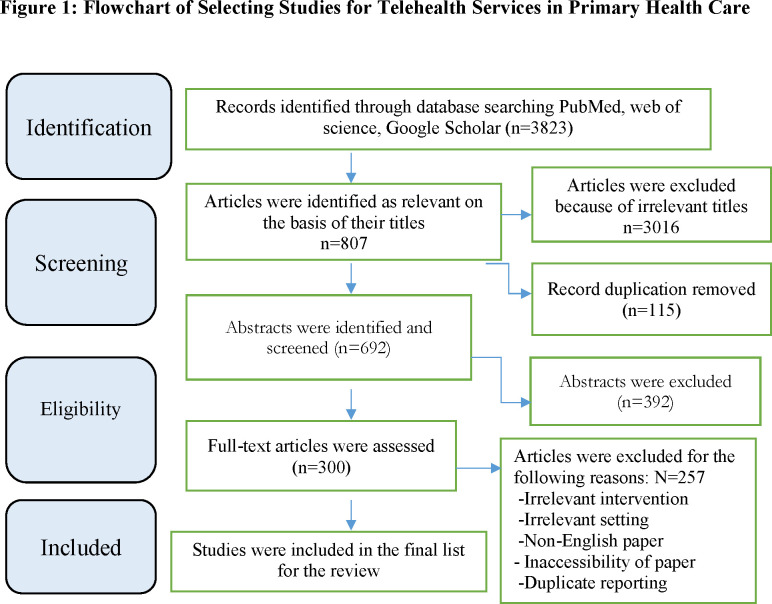
Figure 1 shows the process of articles’ selection.
Figure 1.
Flowchart of Selecting Studies for Telehealth Services in Primary Health Care
Inclusion criteria:
The focus of the study is on the telehealth in PHC
All types of the study
Exclusion criteria:
Non-English studies
Papers where the full text was not available
Data Extraction
Two of the researchers (LB and LRK) examined the full text of all the included studies independently. They extracted data from fully eligible studies into a predefined form. The data extraction form was used including information on: title of the study, author(s)’ name, study type, stud year, study population age, tools/equipment used to provide telehealth, telehealth mode (synchronous or asynchronous), providers involved in telehealth, period of the telehealth delivery, intervention group, control group/s if applicable, the reason for telehealth, intervention type, telehealth outcome, target group of telehealth, and clinical and non-clinical equipment parameters used in telehealth. Any disagreement about the extracted data was resolved by the third researcher (LD).
Results
Out of the 3,823 articles identified from the electronic literature search, 115 were duplicates and were therefore eliminated. After screening the title, abstract, and full text of the papers, a total number of 43 were included for the final review (Figure 1).
Table 1 presents the characteristics of all 43 included studies.27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69 Fourteen out of all the studies were the randomized controlled trial.33, 36, 37, 40, 41, 44, 47, 49, 50, 52, 54, 57, 62, 69 The focus of the studies was the population with over the age of 18, except for one study that focused on children.43
Table 1.
Basic Characteristics and Main Features of the Telehealth Services Provided or Used for Primary Health Care
| First Author | Type of Disease | Country | Purpose of telehealth | Telehealth Delivery | Telehealth Staff | Population Type | Telehealth Services Receiver | Type of study | Age of participant | follow up (month) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chan27 | Type 2 DM | China | Education, monitoring and controlling disease | Two-way synchronous | Primary care group, Specialist | NM | Patient | NM | Elderly(Average age: 73.3) | 2 | |
|
| |||||||||||
| Cottrell28 | Hypertension | UK | Managing hypertension | Synchronous | GP | NM | Patient | Observational | Adults | 6 | |
|
| |||||||||||
| Calvoa29 | COPD | Spain | Telemonitoring and follow-up | Asynchronous | GP, Pulmonologist, Nurse | Urban | Patient, Primary care physician | Controlled trial | Elderly | 7 | |
|
| |||||||||||
| Schuttner30 | Population based primary health care | Zambia | Referral, follow up, and outreach service | Synchronous | Community health workers, GP | Rural | Care Provider | Observational | NM | 8 | |
|
| |||||||||||
| Klein-Wiele31 | Palpitation | Germany | Detecting arrhythmia | One-way asynchronous | GP, Specialist | NM | Patient | Observational | 17-82 | 1 | |
|
| |||||||||||
| Huis in ‘t Veld32 | Neck–Shoulder Pain | Netherlands | reduce pain, reduce disability | Synchronous | Myo-feedback therapist, Technician | NM | Patient | Qualitative study | NM | 1 | |
|
| |||||||||||
| Tabak33 | COPD | Netherlands | Support treatment of COPD through self-management | Two-way | Specialist, Nurse | NM | Patient | RCT | NM | 9 | |
|
| |||||||||||
| Uscher-Pines34 | Minor illnesses | USA | Examining impact of telemedicine services on care | Two-way synchronous | Physician | NM | Patient | Observational | NM | 11 | |
|
| |||||||||||
| Harrison35 | Diseases related to 10 different specialties | UK | Teleconferencing outpatient consultations | Two-way synchronous | GP, Specialist | Urban | Patient | Observational exploratory feasibility study | NM | 5 | |
|
| |||||||||||
| Izquierdo36 | Diabetes | USA | Following the recommendation of remote diabetes team by GPs | NM | GP, Specialist | Rural | Patient | RCT | 55 years of age or older | 7 years | |
|
| |||||||||||
| de Lusignana37 | Chronic Heart Failure | UK | Home telemonitoring | Synchronous/asynchronous | Nurse, Cardiologist, GP, Clinical physiologist | NM | Patient | RCT | Between 65 and 80 | 6 | |
|
| |||||||||||
| Anogianakis38 | Primary care in prison | Greece | To assist primary care team for delivery of health care in prison | NM | GP, Paramedics, Specialist, Nurse | Urban | Patient | Observational (cross-sectional) | NM | 9 | |
|
| |||||||||||
| Trief39 | Diabetes | USA | Improving diabetes control | Synchronous and asynchronous | Dietitian, Nurse, Specialist | Rural | Patient | Observational | Elderly patients | 12 | |
|
| |||||||||||
| Glynn40 | Physical activity | Ireland | Promoting physical activity in primary care | Synchronous and asynchronous | Primary care team | Rural | Young population | RCT | >16 age | 8 | |
|
| |||||||||||
| Mussulman41 | Smoking Cessation | USA | Examining teledelivery of effective tobacco treatment | Synchronous | Counselor, Receptionist, Nurse | Rural | Patient | RCT | >18 | 12 | |
|
| |||||||||||
| Pratt42 | Mental illnesses | USA | Improving self-management | Synchronous and | Nurse | Urban | Patient | Observational | aged 18 and older | 6 | |
|
| |||||||||||
|
| |||||||||||
|
| |||||||||||
| and chronic illness | asynchronous | ||||||||||
|
| |||||||||||
| Levy43 | Spina Bifida | UK | To support continence self-care deficits | Two-way | Nurse | NM | Patients’ family | Observational | 12-18 years | NM | |
|
| |||||||||||
| Bove44 | Hypertension | USA | Self-monitoring | Two-way | GP, Nurse | Urban, Underserved | Patient | RCT | >18 | 6 | |
|
| |||||||||||
| Al Alawi45 | Diabetic retinopathy | Bahrain | Screening | NM | Ophthalmologist, Ophthalmologic technician | NM | Primary care physician | Observational | 24-84 years | NM | |
|
| |||||||||||
| Hatef46 | Diabetic retinopathy | USA | Increasing the completion of the annual eye examination | NA | GP, Specialist | Urban, Underserved | Patient | Observational | 18-75 years | NM | |
|
| |||||||||||
| Odnoletkova47 | Type 2 DM | Belgium | Coaching | NA | Certified diabetes nurse educator | NM | Patient | RCT | 18-75 years | 18 | |
|
| |||||||||||
| Quinn48 | Type 2 diabetes | USA | Evaluate self-efficacy for diabetes self-management | Two-way | Certified diabetes educator, Patient coaching system | NM | Patient | Observational | seven older adults (mean age: 70.3 years) | 2 | |
|
| |||||||||||
| Wakefield49 | Diabetes and hypertension | USA | Evaluating the efficacy of remote monitoring | NA | Nurse | Urban | Patient | RCT | 40-89 years | 6 and 12 | |
|
| |||||||||||
| Deen50 | Depression | USA | Evaluating acceptability, | Two-way | Nurse, Psychologist | NM | Patient | RCT | Mean: 47 | 12 | |
|
| |||||||||||
| initiation and engagement in telepsychotherapy | Psychiatrist, Pharmacist | ||||||||||
|
| |||||||||||
| Tudiver51 | Diabetes | USA | Evaluating acceptability | NA | GP, Dietitian | Mostly rural, urban | Patient | Observational (longitudinal survey) | Mean: 48 | 12 | |
|
| |||||||||||
| Nagrebetsky52 | Type 2 diabetes | UK | Feasibility self-monitoring | Synchronous | GP, Nurse | NM | Patient | RCT | Mean: 58 | 6 | |
|
| |||||||||||
| Bujnowska-Fedak53 | Primary care | Poland | Support real time consultations | Two-way synchronous | GP, Academic | Urban, Rural | GP, Patient | Descriptive | NM | 3 years | |
|
| |||||||||||
| family medicine specialist | |||||||||||
|
| |||||||||||
| Huber54 | Obesity | USA | Improving lifestyle | NM | Wellness coach | NM | Patient | RCT | 18-55 | 6 | |
|
| |||||||||||
| Etherington55 | Cervical Cancer | UK | Screening cervical cancer | Asynchronous | Nurse, Specialist | Urban | Women with minor smear abnormality but normal cervices | Observational | 19-50 | 2 weeks | |
|
| |||||||||||
| Ruas56 | Primary Care | Brazil | Increasing the ability of primary care providers and educating them | Asynchronous | Specialist | NM | Primary Care Physician | Observational (descriptive) | 24-61 | NM | |
|
| |||||||||||
| Salisbury57 | Cardiovascular Disease | UK | Reducing risk of cardiovascular disease | Asynchronous/synchronous | GP, Nurse | Urban/Rural | Patients | RCT | 40-74 | 12 | |
|
| |||||||||||
| Salisbury58 | Chronic Health Conditions | UK | Developing conceptual model for telehealth | NM | GP | NM | Patients, Healthcare professionals | Mixed methods | NM | NM | |
|
| |||||||||||
| Iannitto59 | Diabetes Type II | USA | Managing insulin | NM | GP, Nurse | NM | Patients | Observational (cross-sectional) | >18 | 12 | |
|
| |||||||||||
| Langkamp60 | Children with Developmental Disabilities | USA | Evaluate benefits of school based telemedicine for treating minor illnesses | Asynchronous | GP, Nurse, Certified telehealth assistant in school | Rural | Patient (school-age children with a disability) | Observational (cross-sectional) | 3-21 years Mean: 9.2 years | 12 months | |
|
| |||||||||||
| Larsen61 | Type 2 diabetes | UK | Adjusting the insulin dose to improve glycemic control | Asynchronous/Synchronous | Nurse/GP | NM | Patient | Observational | Mean: 57 | 6 | |
|
| |||||||||||
| Dario62 | Type 2 diabetes | Italy | Telemonitoring for improving health-related quality of life | Synchronous/Asynchronous | Specialist | NM | Patient | RCT | Mean: 73 | 12 | |
|
| |||||||||||
| Blomdahl63 | Disorders in the anterior part of the eye | Sweden | Evaluate technical quality of teleophthalmology | Two-way synchronous | GP, Specialist | Urban | Patient | Observational | NM | 24 | |
|
| |||||||||||
| Thijssing64 | COPD | Netherlands | Improving quality and efficiency of care | Two-way | GP, Specialist | NM | GP | Observational | Mean: 52 | 28 | |
|
| |||||||||||
| Hussain65 | Urinary tract symptoms | UK | Training and supervising | Synchronous | GP, Specialist | NM | GP | Observational | NM | NM | |
|
| |||||||||||
| Backman66 | Cardiac disease | UK | Management | Two-way, synchronous/Asynchronous | Specialist, Nurse | Rural | NM | Review | NM | NM | |
|
| |||||||||||
|
| |||||||||||
| Pecina67 | Dermatologic conditions | USA | Evaluation of telehealth app | Asynchronous | GP, Specialist | NM | NM | Retrospective | Mean: 44 | 1 | |
|
| |||||||||||
| Cottrell68 | Chronic kidney diseases or blood pressure | UK | Evaluate, Management | Asynchronous two-way | GP, Nurse | Underserved, Urban | Patient | Prospective | >50 years | 3-6 | |
|
| |||||||||||
| Bujnowska-Fedak69 | Type 2 diabetes | Poland | Improve quality of life and health status | Two-way | Care provider (mostly GP) | NM | Care provider (mostly GP) | RCT | 18-75 years | NM | |
• NM: Not Mentioned
The studies included in this review originated from 15 countries around the world. The majority of the studies originated from the United States (n=15)34, 36, 39, 41, 42, 44, 46, 48, 49, 50, 51, 54, 59, 60, 67, and the United Kingdom (n=12). 28, 35, 37, 43, 52, 55, 57, 58, 61, 65, 66, 68 Only three studies were from Asian and African countries.27, 30, 45 Diabetes and hypertension were the most frequently targeted diseases27, 36, 39, 45, 46, 47, 48, 49, 51, 52, 61, 62, 69 by the telehealth PHC services.28, 44, 49, 68
In 26 studies, general practitioners were the primary providers of telehealth services.28, 29, 30, 31, 34, 35, 36, 37, 38, 44, 46, 51, 52, 53, 57, 58, 59, 60, 61, 63, 64, 65, 66, 67, 68, 69 A total number of 19 studies used the real-time (synchronous) approach for providing telehealth services.27, 28, 30, 32, 34, 35, 37, 39-42, 52, 53, 57, 61-63, 65, 66 Patients were found to be the primary receivers of telehealth services (n=32).27, 28, 29, 31, 32, 33, 34, 35, 36, 37, 38, 39, 41, 42, 44, 46, 47, 48, 49, 50, 51, 52, 53, 54, 57, 58, 59, 60, 61, 62, 63, 68
The aim of providing telehealth services was various. In some studies, the aim of telehealth was to follow up with patients29, 30 and monitor disease,27, 29, 37, 44, 52, 62 empower people,43, 44 train patients,27, 47 and provide quick and easy access to meet medical needs.30, 31, 43, 53, 61 However, some telehealth services aimed to train and supervise healthcare providers and give a second opinion or consultation. The studies included in this review originated from 15 countries across the world.45, 53, 56, 64, 65
Equipment and devices used for delivering telehealth services included television,27 telephone,34, 35, 39, 41, 44, 46, 48, 50, 54, 57, 59, 66 glucometer,52, 59, 62 camera,27, 35, 36, 45, 46, 60, 63 mobile phone, 40, 43, 48, 52, 61, 68 spirometer,29, 64 pulse-oximeter,29 heart rate monitor,29 computer,30, 33, 39, 41, 45, 69 digital otoscope,60 and telephonic stethoscope.60
Disease management,28, 36, 62, 69 healthcare support in rural areas,30, 41 self-management,27, 33, 39, 42, 48, 51, 58, 59, 61 and cost reduction35, 38, 46 were the most critical achievements of telemedicine services in the reviewed studies.
The critical challenges reported for implementing telemedicine services include lack of resources,27, 69 lack of awareness,27, 30, 48 staff resistance,38, 50 lack of privacy criteria,27, 33, 43 and lack of access to technology.57, 58, 64 (Table 2)
Table 2.
Advantages, Outcomes, Obstacles, and the Required Facilities Reported for Telehealth Services in PHC
| Author | Reported advantage/ benefit | Obstacle | Hardware/software/facilities |
|---|---|---|---|
| Chan27 | Easy to use, empowers patient | Lack of enough resources; lack of awareness; privacy; standard-based encryption | A dual-monitoring Tandberg 880 videoconferencing set-top unit; large screen television; high-resolution portable Canon camera |
|
| |||
| Cottrell28 | Flexible, convenient, easy to use, and acceptable means for managing hypertension with collaboration with responsible health professionals | Not all patients provided feedback using all the means employed; some missing data | Home electronic BP measurements and mobile phones |
|
| |||
| Calvoa29 | Improved the care of patients with severe COPD; improvement in many clinical outcomes; reduction in emergency room visits, hospitalizations, and length of stay | NM | Spirometer; pulse-oximeter; heart rate monitor; blood pressure monitor; modem and telephone line |
|
| |||
| Schuttner30 | Assisting to clinical care in rural areas and potential for epidemiologic and health system applications; improved service outreach; guided clinical activities; and facilitated data collection | Required multiple updates; required literacy and technological proficiency levels | Computers; network; cellular local server; cellular modems; mobile phone |
|
| |||
| Klein-Wiele31 | Decreased hospital admissions, decreased emergency treatments and cardiology referrals | Inability to activate the device and send symptoms | Tele-EKG-Card 100IRTM (Vitaphone, Mannheim, Germany) |
|
| |||
| Huis in't Veld32 | Ease of use, usefulness, time saving, positive impact on the perception of pain intensity and disability | NM | Local area network (wearable sensor, processing unit, feedback unit), wireless communications platform, server |
|
| |||
| Tabak33 | Increased self-care, enhanced motivation for exercise, and ease of consultation | Security; internet access; computer access | Computer and internet access |
|
| |||
| Uscher-Pines34 | Simple and inexpensive, easy to access, and easy to use | Lack of covering all symptoms related to disease in the Teladoc program | Phone or video via internet |
|
| |||
| Robert Harrison35 | Improved communication among physicians of primary and secondary care for enhancing the quality of health care, continuous education of health care providers; cost-effectiveness of health services; and high satisfaction by patients, specialists, and general practitioners | Technical failure such as loss of voice or image; inability of consultants to perform a virtual physical examination | Standard commercial videoconferencing equipment for desktop PCs. This consisted of screen call software, a card to go inside the computer, a telephone handset, and a small video camera that could be mounted on the top or side of a computer monitor. |
|
| |||
| Izquierdo36 | Improved glycaemic control and achievement in behavioral change goals, and improved diabetes care | There was no access to the electronic health record, so the care team was unable to complete patient information. | Web camera, home glucose meter, and blood pressure cuff connected to the home telemedicine unit through an RS-232 serial port |
|
| |||
| de Lusignana37 | Realization of home telemonitoring | Equipment failed due to battery failure that followed by a loss of data in the device memory; video consulting over ordinary telephone lines did not show sustained benefit and was not complied with. | TV-phone 8*8 inch (Model number VC105) |
|
| |||
| Anogianakis38 | Reduced cost of transferring patients out of prison; improved the quality of care for prisoners | Resistance of health care personnel on the provision of support for telemedicine; Ministry of Health resistance; inability of National Health System to interface with the computerized record keeping system of the prison telemedicine program; prison staff resistance to implementation of telehealth; inadequate support from Ministry of Justice leadership and bureaucratic obstacles by low ranked personnel in justice system | Two beds, pharmacy, small clinic equipped with telemedicine network for consultation |
|
| |||
| Trief39 | Improved self-management | Not generalizable | Phone and computer |
|
| |||
| Glynn40 | Cheap, user-friendly technology to promote physical activity in primary care | Not generalizable | Smartphone |
|
| |||
| Mussulman41 | Increased motivation, improved access to high quality smoking cessation treatment in rural areas | NM | Computers, web cams, printers; telephones; polycom PVX software, large bandwidth, a telemedicine technician for internet resource management |
|
| |||
| Pratt42 | Improved self-management, reduced number of hospital admissions, reduced emergency room visits, improved quality of life | NM | Remote health device connected to the phone |
|
| |||
| Levy 43 | Improve self-care | Safety and confidentiality of sensitive health data | Mobile; Skype software |
|
| |||
| Bove44 | Better and faster treatment and management of hypertension; reduction of heart disease | NM | Sphygmomanometer; pedometer, telephone, internet, fax |
|
| |||
| Al Alawi45 | Providing the efficient means of detecting and treating diabetic retinopathy; improving patient information sharing; improving patient status; educating family physicians | NM | Canon camera, computer, internet |
|
| |||
| Hatef46 | Effective and efficient screening of diabetic patients in low-income areas covered by a family physician; screening people in primary care centers without the need for an eye specialist, promoting health, cost-effective | Improved screening | Camera, data transfer software, internet, phone |
|
| |||
| Odnoletkova47 | Increased access to health services | NM | Package with information about the program, a book with advice on nutrition in diabetes and a waist circumference meter with a BMI calculator |
|
| |||
| Quinn48 | Motivation and confidence in elderly people, for self-management; positive attitude towards mobile technology | Anxiety and literacy related to technology may be avoidable barriers | Internet, mobile, personal portal, personal communication service |
|
| |||
| Wakefield49 | Enhanced detection of diabetes | NM | Standard telephone line, blood glucose measurements |
|
| |||
| Deen50 | Improving access to psychotherapy services; patient satisfaction | Rejecting people | Telephone, video equipment in the primary care office |
|
| |||
| Tudiver51 | Telemedicine may be a useful, effective way to deliver healthcare; enhanced patient knowledge; improved self-management | NM | Phone service, web portal, email, fax |
|
| |||
| Nagrebetsky52 | Improved self-monitoring, improved clinical outcomes | NM | Mobile telephone, blood glucose meter, mobile 3G network, web-based monitoring system |
|
| |||
| Bujnowska-Fedak53 | Improved access to primary healthcare; enhanced physician confidence; educating family physicians; making efficient use of expensive resources; and providing easier medical care | NM | Telephone transmission system, communication protocols, configuration equipment and communications, audio equipment, video and audio computers, high quality video systems, and dedicated lines |
|
| |||
| Huber54 | Positive change in physical habits among obese primary care patients. | NM | Telephone |
|
| |||
| Etherington55 | Ease of use | NM | Standard PC, video capture, ISDN connection |
|
| |||
| Ruas56 | NM | NM | PC, the store-and-forward teleconsultation tool (BH Telessau´de), personnel management system of the municipal Department of Health |
|
| |||
| Salisbury57 | Reduced cardiovascular risk, cost-effective benefit in cardiovascular risk reduction, feasibility of delivering an intervention on a wide scale at relatively low cost and using non-clinically trained health advisors supported by computerized algorithms, increases the capacity of the healthcare system to provide an intervention to large numbers of people | Lack of internet access | Telephone, internet, email address, computer systems |
|
| |||
| Salisbury58 | Acceptable to patients and providers; cost-effective; promoted self-management; treatment optimization; care coordination | Not all patients in UK have access to reliable internet connections | NM |
|
| |||
| Iannitto59 | Empowering patient to take an active role in managing their health; saving time for the primary care providers in delivering patient care; opening appointment slots for patients; improving ability to serve patients with diabetes by initiating insulin in a timely manner; high satisfaction with the telehealth system reported by patients and providers | Lack of reimbursement | Telephone and a functioning glucometer |
|
| |||
| Langkamp60 | High level of satisfaction with the program; decreased stress to the child and the parents; increasing the likelihood of a successful medical examination due to greater cooperation by the child. | NM | Digital otoscope, telephonic stethoscope, digital camera, and videoconference camera. |
|
| |||
| Larsen61 | Increased self-care | NM | Mobile phone with pre-loaded software; blood glucose meter and a Bluetooth cradle to link the meter to the phone |
|
| |||
| Dario62 | Reduced hospitalizations; reduced emergency departments’ and specialty care visits; contributing to significant cost reduction; improved adherence to therapy; improved healthcare services’ efficiency through better | NM | Glucometer and a gateway for data transmission to a regional eHealth center. |
|
| |||
| management of chronic diseases; diminished direct costs; decreased travel times for both health professionals and patients | |||
|
| |||
| Blomdahl63 | Reliable system; economic benefits | NM | Three ISDN lines, video camera, Aslit-lamp microscope connected to a Sony three-chip video-camera |
|
| |||
| Thijssing64 | Reduced physical referrals; improved quality of care for these patients; supported GPs in interpreting spirometry results, diagnosing patients and making treatment decisions; improved the communication between GP and pulmonologist | NM | Spirometer that could be linked to a computer, hypertext transfer protocol secured, web-based teleconsultation system-mail and phone |
|
| |||
| Hussain65 | Assistance in training and supervision of GPs; support of GPs for understanding urinary tract ultrasound anatomy and gaining competency in the correct use of an ultrasound machine; provided opportunities for continuous professional development, accreditation and reaccreditations of the GP's ultrasound skills | NM | Ultrasound scanner and a uro-flowmeter, ISDN at 128 Kbit/digital ultrasound machine |
|
| |||
| Backman66 | Supporting diagnoses by GP; assisting in clinical evaluation of cardiac patients; bridging the gap between primary care and specialists; reduction of referrals to secondary care; reduction of misdiagnosis; ease of use; time saving; money saving; benefits to physicians and patients in terms of accessibility, speed of diagnosis, efficiency of management, and resource release | Time consuming | Telephone line, email, or fax |
|
| |||
| Pecina67 | Facilitated access to consultants; facilitated communication of primary care physicians with counselors | Problem in image quality | Any iOS 7.2 or higher device; iPhone operating system |
|
| |||
| Cottrell68 | Reduced blood pressure of patients with hypertension; improved accuracy of diagnosis | NM | Electronic sphygmomanometer; mobile phone; software and BP recording devices |
|
| |||
| Bujnowska-Fedak69 | Patient satisfaction; improved patient-physician communication; improved quality life; disease control | Lack of resources for actual analysis | Personal computer, internet, wireless glucose monitor, and transmitter |
Discussion
This study aimed to investigate telehealth at the PHC level. Our findings revealed that the adults (18-60 years old) were the target of telehealth services in most of the studies. It shows that people of these ages are more willing to use this method, have the necessary technological know-how, and can easily use the tools involved in telehealth.17 The target group of telehealth services in some of the included studies were elderly adults. There is evidence that the telehealth applicability to the seniors has not been a barrier to receiving telehealth services, and older adults have an interest in using telehealth services. People in this age range are more likely to utilize telehealth services if they do not have an additional cognitive load.70 The majority of the telehealth services provided in PHC originated from European and American countries. A possible explanation for this may be the leading position of this country in technical infrastructures and the equipment required for implementing such services.71
The results of our study revealed that the majority of telehealth services used various communication channels such as video conferencing, cellphones, telephones, the web, email, and Skype, considering the situation of the service receiver and the available tools. The variety of communication channels reveals the full range of options for delivering telehealth services. According to the findings of the study done by Dhillon et al., Skype and email were the most popular tools for receiving telehealth services among the participants.70
Most of the participants in the included studies suffered from chronic and non-communicable diseases such as hypertension and Type II diabetes. Patients suffering from chronic conditions usually place substantial financial burdens on the health care system so that the utilization of telehealth services can reduce these pressures.72 Turning to the telehealth approach can act as a solution to the problem of managing care for chronic conditions among aging of the population in different communities. The investigation by Esperance et al. (2016) has concluded that self-management via telehealth services can improve patients’ access to physicians and the quality of care among diabetic patients. Despite being overall pleased with using the telehealth system, the patients in the mentioned study raised concerns on technical issues and the need to learn new information to use the system.73
Xu et al. (2018) conducted a study on the efficacy of telemedicine in providing care to diabetic patients in rural areas. The patients who had used the telemedicine system experienced lower blood sugar levels, better access to health care, less waste of time, and a high degree of satisfaction with the method.74 The higher success rate of telehealth services in this domain can be attributed to the broader adoption of telehealth for managing diabetes compared to other diseases.
Our findings implied that the healthcare providers who made the most use of telehealth services were family doctors. Telehealth can undoubtedly improve the quality of PHC offered by general practitioners through increasing access to physicians. General practitioners can use telehealth to perform examinations and provide consultations to their patients in any place and at any time without even having to go to their offices. This approach can reduce waiting times in doctors’ offices, deliver healthcare services to people living in remote areas, and allow physicians to increase their income through reimbursement systems intended for telehealth services.75
The results revealed the most dominant approach to telehealth services was the synchronous form.27, 28, 30, 32, 34, 35, 37, 39, 40, 41, 42, 52, 53, 57, 61, 62, 63, 65, 66 Real-time communication is considered an effective way of delivering telehealth services in PHC. In the synchronous mode of telehealth, there is a stronger sense of communication between patients and providers. What determines the suitable mode of delivering telehealth services are the patients and the type of disease they have. Moreover, telehealth is a technological phenomenon76 and a directed approach for meeting individuals’ needs.75Therefore, choosing between one-way or two-way as well as synchronous or asynchronous methods must be made accordingly.
Most of the included studies in this review have focused on investigating the effects of these services on rural and underserved areas since those are the areas facing problems with access to healthcare.7 Increasing accessibility and improving patient health can happen by establishing telehealth services in rural areas. However, the rollout of the technology in rural regions is usually slower due to the lack of technical support and lower budgets. Lack of adequate resources can be another barrier to deploying telehealth in underserved areas since they do not have dedicated technical support teams of experts like the large urban areas. Moreover, it should be noted that even though innovation is considered a competitive advantage, rural systems are usually resistant to change.77
According to the findings of our review, it seems the clients mostly received the telehealth services directly by themselves. However, the study by Dhillon et al. found that the elderly preferred to receive telehealth services through the help and support of their families.70 There is evidence that patients whom a supervisor supported were more successful in using this technology.77
Reviewing the main obstacles to the implementation of telehealth revealed that lack of coverage by healthcare insurances and payment plans are among the primary problems holding back the adoption of telehealth networks.11, 78 Barriers also ranged from difficulty in acquiring permits to concerns about privacy3, 11, 13 and the lack of enough information, user perception, skill, education, initial costs, and the providers’ reluctance toward new approaches of health care delivery.9, 79 The study by Souza et al. identified additional factors such as low bandwidth, unsuitable networks, low signal quality, picture quality, and organizational issues as barriers to the implementation of telehealth services.80 Furthermore, a study conducted by Fatehi reported technical, organizational, cultural, sociological, economic, and ethical obstacles.81 The barriers reported by Nesbitt et al. also are similar to the ones identified in our study.78 Regardless of the disadvantages, there were a variety of advantages reported for telehealth services in primary healthcare. They range from self-care promotion to patient empowerment, decreased patient visits, cost reduction, and access improvement to the services. Additional benefits include patients’ time savings, higher commitment to showing up for appointments,75 better clinical results, better access to specialist services, less need for travel, and better screening rates.82
Conclusion
Telehealth can be used for different purposes of primary health care through deploying a full range of communication channels available to the public. Due to the opportunistic use of existing devices and platforms, telehealth can provide scalable primary health care services nationwide and worldwide. However, the implementation of telehealth in PHC faces challenges from technical, organizational, and human perspectives. It seems inevitable to transform the policy context and regulation if telehealth approach is a part of health system agenda. Respect for privacy and confidentiality principles is also crucial. Moreover, digital equity is required to expand telehealth services to the populations in underserved areas. Digital equity can be achieved through addressing existing disparities in internet and technology access and improving e-health literacy among low-income and underserved communities. Under such conditions, telehealth can strengthen primary health care system toward universal health coverage. Since no guideline was reported for implementing telehealth services in primary health care, future research may utilize the findings of this study as a basis for developing the guideline. Analysis of telehealth policies for primary healthcare in different countries could shed light on a deeper understanding of our findings. The current study is limited in this regard and future research may explore this to complement the findings of this study.
Declarations
Ethics approval
Ethical approval for conducting this study has been obtained from the Research Ethics Board at Tabriz University of medical science, Tabriz, Iran (No: IR. TBZMED.REC.1396.1251).
Competing Interests
The authors declare that there is no competing of interest.
Funding
This study was part of MSc thesis and funded by Tabriz University of Medical Sciences
Authors’ Contributions
LB: Data extraction, data organization, treatment of data, and drafting a manuscript. LRK: Data analysis, and manuscript writing, scientific revision and approval. LD: Data examination, writing of manuscript and scientific criticism as well as approval. MF: Data examination, scientific review and approval. All authors have read and approved the final manuscript.
Author Biographies
Leila Beheshti is affiliated with the Student Research Committee in the School of Management and Medical Informatics at Tabriz University of Medical Sciences.
Leila R. Kalankesh (Lrkalankesh@tbzmed.ac.ir) (corresponding author) is an associate professor of medical informatics in the Department of Health Information Technology in the School of Management and Medical Informatics, Health Services Management Research Centre, and the Research Centre of Psychiatry and Behavioral Sciences at Tabriz University of Medical Sciences.
Leila Doshmangir is an associate professor of health policy in the Health Services Management Research Centre in the Department of Health Policy and Management in the School of Management and Medical Informatics at Tabriz University of Medical Sciences.
Mostafa Farahbakhsh is an assistant professor and specialist in the Research Centre of Psychiatry and Behavioral Sciences at Tabriz University of Medical Sciences.
Acknowledgements
The authors would like to thank Dr Faramarz Pourasghar, MD, PhD, for his valuable help.
Notes
- 1.Kim J-E, Song Y-M, Park J-H, Lee J-R. Attitude of Korean primary care family physicians towards telehealth. Korean Journal of Family Medicine. 2011;32((6)):341–51. doi: 10.4082/kjfm.2011.32.6.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung S-G, Kweon H-J, Kim E-T, Kim S-A, Choi J-K, Cho D-Y. Preference and awareness of telemedicine in primary care patients. Korean Journal of Family Medicine. 2012;33((1)):25–33. doi: 10.4082/kjfm.2012.33.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krishna MT, Knibb RC, Huissoon AP. Is there a role for telemedicine in adult allergy services? Clinical & Experimental Allergy. 2016;46((5)):668–77. doi: 10.1111/cea.12701. [DOI] [PubMed] [Google Scholar]
- 4.Burg G. Telemedicine and teledermatology: Karger Medical and Scientific Publishers. 2003 [Google Scholar]
- 5.Knight P, Bonney A, Teuss G, Guppy M, Lafferre D, Mullan J, et al. Positive clinical outcomes are synergistic with positive educational outcomes when using telehealth consulting in general practice: a mixed-methods study. Journal of Medical Internet Research. 2016;18((2)) doi: 10.2196/jmir.4510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tabriz University of Medical Sciences Executive Instructions for Starting a Health Complex: A strategy for extending family doctor program and achieving universal health coverage. 2015 [Google Scholar]
- 7.Zanaboni P, Scalvini S, Bernocchi P, Borghi G, Tridico C, Masella C. Teleconsultation service to improve healthcare in rural areas: acceptance, organizational impact and appropriateness. BMC Health Services Research. 2009;9((1)):238. doi: 10.1186/1472-6963-9-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Higgins WJ, Luczynski KC, Carroll RA, Fisher WW, Mudford OC. Evaluation of a telehealth training package to remotely train staff to conduct a preference assessment. Journal of Applied Behavior Analysis. 2017;50((2)):238–51. doi: 10.1002/jaba.370. [DOI] [PubMed] [Google Scholar]
- 9.Ayatollahi H, Sarabi FZP, Langarizadeh M. Clinicians’ knowledge and perception of telemedicine technology. Perspectives in Health Information Management. 2015;12((Fall)) [PMC free article] [PubMed] [Google Scholar]
- 10.Sanders C, Rogers A, Bowen R, Bower P, Hirani S, Cartwright M, et al. Exploring barriers to participation and adoption of telehealth and telecare within the Whole System Demonstrator trial: a qualitative study. BMC Health Services Research. 2012;12((1)):220. doi: 10.1186/1472-6963-12-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parmar P, Mackie D, Varghese S, Cooper C. Use of telemedicine technologies in the management of infectious diseases: a review. Clinical Infectious Diseases. 2014;60((7)):1084–94. doi: 10.1093/cid/ciu1143. [DOI] [PubMed] [Google Scholar]
- 12.Agency for Clinical Innovation Telehealth Resource Package. Available at URL: https://aci.health.nsw.gov.au/resources/telehealth. [Google Scholar]
- 13.Daniel H, Sulmasy LS. Policy recommendations to guide the use of telemedicine in primary care settings: an American College of Physicians position paper. Annals of Internal Medicine. 2015;163((10)):787–9. doi: 10.7326/M15-0498. [DOI] [PubMed] [Google Scholar]
- 14.Monteagudo JL, Salvador CH, Kun L. Envisioning patient safety in Telehealth: a research perspective. Health and Technology. 2014;4((2)):79–93. doi: 10.1007/s12553-014-0078-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bardsley M, Steventon A, Doll H. Impact of telehealth on general practice contacts: findings from the whole systems demonstrator cluster randomised trial. BMC Health Services Research. 2013;13((1)):395. doi: 10.1186/1472-6963-13-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McPhee E. Telehealth: The general practice perspective. Australian Family Physician. 2014;43((12)):826. [PubMed] [Google Scholar]
- 17.Jones RB, O'Connor A, Brelsford J, Parsons N, Skirton H. Costs and difficulties of recruiting patients to provide e-health support: pilot study in one primary care trust. BMC Medical Informatics and decision making. 2012;12((1)):25. doi: 10.1186/1472-6947-12-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Armfield NR, Coulthard MG, Slater A, McEniery J, Elcock M, Ware RS, et al. The effectiveness of telemedicine for paediatric retrieval consultations: rationale and study design for a pragmatic multicentre randomised controlled trial. BMC Health Services Research. 2014;14((1)):546. doi: 10.1186/s12913-014-0546-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duplantie J, Gagnon M-P, Fortin J-P, Landry R. Telehealth and the recruitment and retention of physicians in rural and remote regions: a Delphi study. Can J Rural Med. 2007;12((1)):30–6. [PubMed] [Google Scholar]
- 20.Anderson R, Becket B, Fahy K, Gorden E, Gray A, Kropp S, LePage S, Liette E, McNicholas F,Phillips B, Pulda K, Renn L. AHIMA telemedicine toolkit. American Health Information Management Association (AHIMA) 2017:p233. [Google Scholar]
- 21.Majdi MR, Mesdaghinia AR, Rakhshani F, Shariati M, Khani H. Design and performance of Iranian national portal for best practice of primary health care. Journal of North Khorasan University of Medical Sciences. 2011;3((2)):65–68. [Google Scholar]
- 22.Asadi F, Hosseini A, Moghaddasi H, Nasr Haydarabadi N. Primary health care information systems in health centers of Tehran, Iran. Health Information Management. 2012;9((1)):1–10. [Google Scholar]
- 23.Odeh B, Kayyali R, Nabhani-Gebara S, Philip N. Implementing a telehealth service: nurses’ perceptions and experiences. British Journal of Nursing. 2014;23((21)):1133–7. doi: 10.12968/bjon.2014.23.21.1133. [DOI] [PubMed] [Google Scholar]
- 24.Saeedi Tehrani S, Noroozi M. Telemedicine: benefits, disadvantages and ethical challenges. Iranian Journal of Medical Ethics and History of Medicine. 2015;8((2)):29–40. [Google Scholar]
- 25.Downes MJ, Mervin MC, Byrnes JM, Scuffham PA. Telemedicine for general practice: a systematic review protocol. Systematic Reviews. 2015;4((1)):134. doi: 10.1186/s13643-015-0115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice. 2005;8((1)):19–32. [Google Scholar]
- 27.Chan WM, Woo J, Hui E, Lau WW, Lai JC, Lee D. A community model for care of elderly people with diabetes via telemedicine. Applied Nursing Research. 2005;18((2)):77–81. doi: 10.1016/j.apnr.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 28.Cottrell E, McMillan K, Chambers R. A cross-sectional survey and service evaluation of simple telehealth in primary care: what do patients think? BMJ Open. 2012;2((6)):e001392. doi: 10.1136/bmjopen-2012-001392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calvo GS, Gómez-Suárez C, Soriano J, Zamora E, Gónzalez-Gamarra A, González-Béjar M, et al. A home telehealth program for patients with severe COPD: the PROMETE study. Respiratory Medicine. 2014;108((3)):453–62. doi: 10.1016/j.rmed.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 30.Schuttner L, Sindano N, Theis M, Zue C, Joseph J, Chilengi R, et al. A mobile phone-based, community health worker program for referral, follow-up, and service outreach in rural Zambia: outcomes and overview. Telemedicine and e-Health. 2014;20((8)):721–8. doi: 10.1089/tmj.2013.0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klein-Wiele O, Faghih M, Dreesen S, Urbien R, Abdelghafor M, Kara K, et al. A novel cross-sector telemedical approach to detect arrhythmia in primary care patients with palpitations using a patient-activated event recorder. Cardiology Journal. 2016;23((4)):422–8. doi: 10.5603/CJ.a2016.0033. [DOI] [PubMed] [Google Scholar]
- 32.Huis in't Veld RM, Huijgen BC, Schaake L, Hermens HJ, Vollenbroek-Hutten MM. A staged approach evaluation of Remotely Supervised Myofeedback Treatment (RSMT) in women with neck—shoulder pain due to computer work. Telemedicine and e-Health. 2008;14((6)):545–51. doi: 10.1089/tmj.2007.0090. [DOI] [PubMed] [Google Scholar]
- 33.Tabak M, Brusse-Keizer M, van der Valk P, Hermens H, Vollenbroek-Hutten M. A telehealth program for self-management of COPD exacerbations and promotion of an active lifestyle: a pilot randomized controlled trial. International journal of chronic obstructive pulmonary disease. 2014;9:935. doi: 10.2147/COPD.S60179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Affairs. 2014;33((2)):258–64. doi: 10.1377/hlthaff.2013.0989. [DOI] [PubMed] [Google Scholar]
- 35.Harrison R, Clayton W, Wallace P. Can telemedicine be used to improve communication between primary and secondary care? Bmj. 1996;313((7069)):1377–80. doi: 10.1136/bmj.313.7069.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Izquierdo RE, Wang D, Huang D, Palmas W, Weinstock RS. Case management with a diabetes team using home telemedicine: acceptance of treatment recommendations by primary care providers in IDEATel. Telemedicine and e-Health. 2015;21((12)):980–6. doi: 10.1089/tmj.2014.0236. [DOI] [PubMed] [Google Scholar]
- 37.de Lusignan S, Wells S, Johnson P, Meredith K, Leatham E, Compliance and effectiveness of 1 year's home telemonitoring The report of a pilot study of patients with chronic heart failure. European journal of heart failure. 2001;3((6)):723–30. doi: 10.1016/s1388-9842(01)00190-8. [DOI] [PubMed] [Google Scholar]
- 38.Anogianakis G, Ilonidis G, Milliaras S, Anogeianaki A, Vlachakis-Milliaras E. Developing prison telemedicine systems: the Greek experience. Journal of Telemedicine and Telecare. 2003;9((2_suppl)):4–7. doi: 10.1258/135763303322596101. [DOI] [PubMed] [Google Scholar]
- 39.Trief PM, Sandberg J, Izquierdo R, Morin PC, Shea S, Brittain R, et al. Diabetes management assisted by telemedicine: patient perspectives. Telemedicine and e-Health. 2008;14((7)):647–55. doi: 10.1089/tmj.2007.0107. [DOI] [PubMed] [Google Scholar]
- 40.Glynn LG, Hayes PS, Casey M, Glynn F, Alvarez-Iglesias A, Newell J, et al. Effectiveness of a smartphone application to promote physical activity in primary care: the SMART MOVE randomised controlled trial. British Journal of General Practice. 2014;64((624)):e384–e91. doi: 10.3399/bjgp14X680461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mussulman L, Ellerbeck EF, Cupertino AP, Preacher KJ, Spaulding R, Catley D, et al. Design and participant characteristics of a randomized-controlled trial of telemedicine for smoking cessation among rural smokers. Contemporary Clinical Trials. 2014;38((2)):173–81. doi: 10.1016/j.cct.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pratt SI, Bartels SJ, Mueser KT, Naslund JA, Wolfe R, Pixley HS, et al. Feasibility and effectiveness of an automated telehealth intervention to improve illness self-management in people with serious psychiatric and medical disorders. Psychiatric Rehabilitation Journal. 2013;36((4)):297. doi: 10.1037/prj0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Levy S, Henderson L, McAlpine C. Growing up with confidence: using telehealth to support continence self-care deficits amongst young people with complex needs. Journal of Innovation in Health Informatics. 2014;21((3)):113–7. doi: 10.14236/jhi.v21i3.58. [DOI] [PubMed] [Google Scholar]
- 44.Bove AA, Homko CJ, Santamore WP, Kashem M, Kerper M, Elliott DJ. Managing hypertension in urban underserved subjects using telemedicine—a clinical trial. American Heart Journal. 2013;165((4)):615–21. doi: 10.1016/j.ahj.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 45.Al Alawi E, Ahmed AA. Screening for diabetic retinopathy: the first telemedicine approach in a primary care setting in Bahrain. Middle East African Journal of Ophthalmology. 2012;19((3)):295. doi: 10.4103/0974-9233.97928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hatef E, Alexander M, Vanderver BG, Fagan P, Albert M. Assessment of annual diabetic eye examination using telemedicine technology among underserved patients in primary care setting. Middle East African Journal of Ophthalmology. 2017;24((4)):207. doi: 10.4103/meajo.MEAJO_19_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Odnoletkova I, Goderis G, Nobels F, Aertgeerts B, Annemans L, Ramaekers D. Nurse-led telecoaching of people with type 2 diabetes in primary care: rationale, design and baseline data of a randomized controlled trial. BMC Family Practice. 2014;15((1)):24. doi: 10.1186/1471-2296-15-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Quinn CC, Khokhar B, Weed K, Barr E, Gruber-Baldini AL. Older adult self-efficacy study of mobile phone diabetes management. Diabetes technology & therapeutics. 2015;17((7)):455–61. doi: 10.1089/dia.2014.0341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wakefield BJ, Holman JE, Ray A, Scherubel M, Adams MR, Hills SL, et al. Outcomes of a home telehealth intervention for patients with diabetes and hypertension. Telemedicine and e-Health. 2012;18((8)):575–9. doi: 10.1089/tmj.2011.0237. [DOI] [PubMed] [Google Scholar]
- 50.Deen TL, Fortney JC, Schroeder G. Patient acceptance of and initiation and engagement in telepsychotherapy in primary care. Psychiatric Services. 2013;64((4)):380–4. doi: 10.1176/appi.ps.201200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tudiver F, Wolff LT, Morin PC, Teresi J, Palmas W, Starren J, et al. Primary care providers’ perceptions of home diabetes telemedicine care in the IDEATel project. The Journal of Rural Health. 2007;23((1)):55–61. doi: 10.1111/j.1748-0361.2006.00068.x. [DOI] [PubMed] [Google Scholar]
- 52.Nagrebetsky A, Larsen M, Craven A, Turner J, McRobert N, Murray E, et al. Stepwise self-titration of oral glucose-lowering medication using a mobile telephone-based telehealth platform in type 2 diabetes: a feasibility trial in primary care. Journal of Diabetes Science and Technology. 2013;7((1)):123–34. doi: 10.1177/193229681300700115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bujnowska-Fedak MM, Staniszewski A, Steciwko A, Puchała E. System of telemedicine services designed for family doctors’ practices. Telemedicine Journal and e-Health. 2000;6((4)):449–52. doi: 10.1089/15305620050503933. [DOI] [PubMed] [Google Scholar]
- 54.Huber JM, Shapiro JS, Wieland ML, Croghan IT, Douglas KSV, Schroeder DR, et al. Telecoaching plus a portion control plate for weight care management: a randomized trial. Trials. 2015;16((1)):323. doi: 10.1186/s13063-015-0880-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Etherington IJ. Telecolposcopy—a feasibility study in primary care. Journal of Telemedicine and Telecare. 2002;8((2_suppl)):22–24. doi: 10.1177/1357633X020080S210. [DOI] [PubMed] [Google Scholar]
- 56.Ruas SSM, Assunção AÁ Teleconsultations by primary care physicians of Belo Horizonte: challenges in the diffusion of innovation. Telemedicine and e-Health. 2013;19((5)):409–14. doi: 10.1089/tmj.2012.0095. [DOI] [PubMed] [Google Scholar]
- 57.Salisbury C, O'Cathain A, Thomas C, Edwards L, Gaunt D, Dixon P, et al. Telehealth for patients at high risk of cardiovascular disease: pragmatic randomised controlled trial. BMJ. 2016;353:i2647. doi: 10.1136/bmj.i2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Salisbury C, Thomas C, O'Cathain A, Rogers A, Pope C, Yardley L, et al. TElehealth in CHronic disease: mixed-methods study to develop the TECH conceptual model for intervention design and evaluation. BMJ Open. 2015;5((2)):e006448. doi: 10.1136/bmjopen-2014-006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Iannitto JM, Dickman K, Lakhani RH, So MJC. Telehealth insulin program: managing insulin in primary care. The Journal for Nurse Practitioners. 2014;10((8)):567–74. [Google Scholar]
- 60.Langkamp DL, McManus MD, Blakemore SD. Telemedicine for children with developmental disabilities: a more effective clinical process than office-based care. Telemedicine and e-Health. 2015;21((2)):110–4. doi: 10.1089/tmj.2013.0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Larsen ME, Turner J, Farmer A, Neil A, Tarassenko L. Telemedicine-supported insulin optimisation in primary care. Journal of telemedicine and telecare. 2010;16((8)):433–40. doi: 10.1258/jtt.2010.100103. [DOI] [PubMed] [Google Scholar]
- 62.Dario C, Toffanin R, Calcaterra F, Saccavini C, Stafylas P, Mancin S, et al. Telemonitoring of type 2 diabetes mellitus in Italy. Telemedicine and e-Health. 2017;23((2)):143–52. doi: 10.1089/tmj.2015.0224. [DOI] [PubMed] [Google Scholar]
- 63.Blomdahl S, Marén N, Lof R. Tele-ophthalmology for the treatment in primary care of disorders in the anterior part of the eye. Journal of Telemedicine and Telecare. 2001;7((suppl 1)):25–26. doi: 10.1177/1357633X010070S110. [DOI] [PubMed] [Google Scholar]
- 64.Thijssing L, Van der Heijden JP, Chavannes NH, Melissant CF, Jaspers MW, Witkamp L. Telepulmonology: effect on quality and efficiency of care. Respiratory Medicine. 2013;20:1e5. doi: 10.1016/j.rmed.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 65.Hussain P, Deshpande A, Shridhar P, Saini G, Kay D. The feasibility of telemedicine for the training and supervision of general practitioners performing ultrasound examinations of patients with urinary tract symptoms. Journal of Telemedicine and Telecare. 2004;10((3)):180–2. doi: 10.1258/135763304323070850. [DOI] [PubMed] [Google Scholar]
- 66.Backman W, Bendel D, Rakhit R. The telecardiology revolution: improving the management of cardiac disease in primary care. Journal of the Royal Society of Medicine. 2010;103((11)):442–6. doi: 10.1258/jrsm.2010.100301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pecina JL, Wyatt KD, Comfere NI, Bernard ME, North F. Uses of Mobile Device Digital Photography of Dermatologic Conditions in Primary Care. JMIR mHealth and uHealth. 2017;5((11)) doi: 10.2196/mhealth.8257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cottrell E, Chambers R, O'Connell P. Using simple telehealth in primary care to reduce blood pressure: a service evaluation. BMJ Open. 2012;2((6)):e001391. doi: 10.1136/bmjopen-2012-001391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bujnowska-Fedak MM, Puchała E, Steciwko A. The impact of telehome care on health status and quality of life among patients with diabetes in a primary care setting in Poland. Telemedicine and e-Health. 2011;17((3)):153–63. doi: 10.1089/tmj.2010.0113. [DOI] [PubMed] [Google Scholar]
- 70.Dhillon JS, Ramos C, Wünsche BC, Lutteroth C, editors. 24th International Symposium on Computer-Based Medical Systems (CBMS) 2011. Designing a web-based telehealth system for elderly people: An interview study in New Zealand. IEEE. [Google Scholar]
- 71.Kalankesh LR, Pourasghar F, Nicholson L, Ahmadi S, Hosseini M. Effect of telehealth interventions on hospitalization indicators: A systematic review. Perspectives in Health Information Management. 2016;13((Fall)) [PMC free article] [PubMed] [Google Scholar]
- 72.Kobb R, Hoffman N, Lodge R, Kline S. Enhancing elder chronic care through technology and care coordination: report from a pilot. Telemedicine Journal and e-HEALTH. 2003;9((2)):189–95. doi: 10.1089/153056203766437525. [DOI] [PubMed] [Google Scholar]
- 73.L'Esperance ST, Perry DJ. Assessing advantages and barriers to telemedicine adoption in the practice setting: A MyCareTeamTM exemplar. Journal of the American Association of Nurse Practitioners. 2016;28((6)):311–9. doi: 10.1002/2327-6924.12280. [DOI] [PubMed] [Google Scholar]
- 74.Xu T, Pujara S, Sutton S, Rhee M. Peer Reviewed: Telemedicine in the Management of Type 1 Diabetes. Preventing Chronic Disease. 2018:15. doi: 10.5888/pcd15.170168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.CHIRON Telemedicine for Primary Care. Available at URL: https://chironhealth.com/telemedicine/providers/primary-care/ [Google Scholar]
- 76.Gill M. A National Telehealth Strategy For Australia–For Discussion. Australian National Consultative Committee on Electronic Health. 2011 [Google Scholar]
- 77.Nesbitt TS, Cole SL, Pellegrino L, Keast P. Rural outreach in home telehealth: Assessing challenges and reviewing successes. Telemedicine Journal & E-Health. 2006;12((2)):107–13. doi: 10.1089/tmj.2006.12.107. [DOI] [PubMed] [Google Scholar]
- 78.Grigsby B, Brega AG, Bennett RE, Devore PA, Paulich MJ, Talkington SG, et al. The slow pace of interactive video telemedicine adoption: the perspective of telemedicine program administrators on physician participation. Telemedicine and e-Health. 2007;13((6)):645–57. doi: 10.1089/tmj.2007.0090. [DOI] [PubMed] [Google Scholar]
- 79.Dixon RF, Stahl JE. “A randomized trial of virtual visits in a general medicine practice.”. Journal of Telemedicine and Telecare. 2009;15((3)):115–7. doi: 10.1258/jtt.2009.003003. [DOI] [PubMed] [Google Scholar]
- 80.de Souza CHA, Morbeck RA, Steinman M, Hors CP, Bracco MM, Kozasa EH, et al. Barriers and benefits in telemedicine arising between a high-technology hospital service provider and remote public healthcare units: A qualitative study in Brazil. Telemedicine and e-Health. 2017;23((6)):527–32. doi: 10.1089/tmj.2016.0158. [DOI] [PubMed] [Google Scholar]
- 81.Fatehi F. Success factors and challenges for establishing the Princess Alexandra Hospital Tele-Endocrinology Clinic in Brisbane, Australia: a qualitative study. Journal of Health and Biomedical Informatics. 2014;1((1)):1–9. [Google Scholar]
- 82.Caffery LJ, Bradford NK, Wickramasinghe SI, Hayman N, Smith AC. Outcomes of using telehealth for the provision of healthcare to Aboriginal and Torres Strait Islander people: a systematic review. Australian and New Zealand Journal of Public Health. 2017;41((1)):48–53. doi: 10.1111/1753-6405.12600. [DOI] [PubMed] [Google Scholar]