Abstract
Importance: Primary health care is rapidly developing as an occupational therapy practice area. Yet, to date, little evidence supports occupational therapy’s feasibility and efficacy in primary care settings.
Objective: To report on the implementation and preliminary clinical outcomes of a Lifestyle Redesign® (LR)–occupational therapy (LR–OT) diabetes management intervention in a primary care clinic.
Design: Patients were randomized to be offered LR–OT or to a no-contact comparison group (data not reported). We assessed implementation outcomes using mixed methods.
Setting: Safety-net primary care clinic.
Participants: Clinic providers and staff; English- or Spanish-speaking clinic patients ages 18–75 yr with diabetes and a current hemoglobin A1c (HbA1c) ≥ 9.0%.
Intervention: Eight 1-hr individual sessions of LR–OT focused on diabetes management.
Outcomes and Measures: Clinical and health behavior outcomes were assessed via electronic medical record (EMR) review and self-report surveys of patients receiving LR–OT at initial evaluation and discharge. We assessed implementation outcomes (acceptability, appropriateness, feasibility, fidelity, efficiency, and timeliness) using patient and staff surveys, interviews, focus groups, and observations.
Results: Seventy-three patients were offered LR–OT: 51 completed one or more sessions, and 38 completed the program. Clinical outcomes among program completers indicate beneficial changes in HbA1c, diabetes self-care, and health status. Implementation challenges included a need for patient and staff education, securing adequate workspace, and establishing a referral process. Factors contributing to implementation success included strong buy-in from clinic leadership, colocation, and shared EMR documentation.
Conclusions and Relevance: LR–OT is a feasible approach to enhancing service delivery and clinical outcomes in primary care.
What This Article Adds: This study provides insight into factors that may create challenges or contribute to the success of implementing occupational therapy services within primary health care settings. In addition, this study provides preliminary evidence of occupational therapy’s effectiveness in improving clinical outcomes among ethnically diverse, low-income patients with diabetes in a safety-net primary care setting.
Diabetes mellitus is a significant health problem worldwide. The World Health Organization (2016) has estimated that this condition currently affects 422 million people, with a direct global cost of more than $827 billion annually. Within Los Angeles County (LAC), diabetes is the fifth-leading cause of death, and its prevalence is elevated among disadvantaged groups: 14% of Hispanics and 12% of African-Americans have diabetes versus 7% of Whites, and 14% of people with incomes below the federal poverty level have diabetes versus 8% of those at ≥200% the federal poverty level (LAC Department of Public Health, Office of Health Assessment and Epidemiology, 2012). Diabetes is the leading cause of adult-onset blindness, amputations, and kidney failure, which are long-term complications that adversely affect quality of life (Al-Lawati, 2017).
Diabetes complications that contribute to disability and mortality can be delayed or prevented through health management occupations, such as checking blood glucose and adhering to medication (Pyatak et al., 2018). Patients often need to incorporate lifestyle changes, including healthy eating, exercise, medication regimens, and stress management, into their daily routines. Although patients may be educated on how to perform these occupations, carrying them out consistently over time is often a challenge (Hernandez-Tejada et al., 2012). Occupational therapy supports people in managing chronic diseases, such as diabetes, by using a holistic approach to address barriers to health management. Lifestyle Redesign® (LR), an occupational therapy intervention that teaches people to incorporate health management strategies into their habits and routines and adapt them to changing life circumstances, is effective at improving a range of health outcomes (Clark et al., 1997; Pyatak et al., 2018; Simon & Collins, 2017). Among adults with diabetes, the Resilient, Empowered, Active Living with Diabetes (REAL Diabetes) LR–occupational therapy (LR–OT) intervention significantly improved hemoglobin A1c (HbA1c; average blood glucose levels) and diabetes-related quality of life (Pyatak et al., 2018).
We conducted a hybrid effectiveness–implementation study to evaluate the impact of integrating LR–OT in an interdisciplinary team at a primary care clinic serving an ethnically diverse, urban, low-income population in LAC. Hybrid effectiveness–implementation designs have a dual focus on assessing clinical and implementation outcomes, expediting the translation of research findings into clinical practice by generating more effective implementation strategies and information for decision makers (Curran et al., 2012).
Method
Study Design
The outcomes presented in this article are part of a 1-yr pilot study with two coprimary aims: evaluate the process of implementing LR–occupational therapy in an primary care clinic and assess the impact of LR–OT on health and quality of life among patients with uncontrolled diabetes (HbA1c ≥ 9.0%) through a randomized controlled trial (RCT) implemented within a primary care clinic. In this article, we report on the implementation outcomes of the study (Aim 1) and preliminary pre–post effectiveness findings among patients who completed the LR–OT program only; analysis of RCT findings will be presented in a future article.
Implementation Overview
Implementation of the LR–OT program is summarized in four phases. In Phase 0 (preimplementation), we acquired funding to support a 1-yr pilot study and built relationships with key stakeholders, including the clinic director, director of primary care in the hospital system, and a senior executive within the health system. The research team discussed and negotiated with these stakeholders regarding which populations would be appropriate for LR–OT and logistical considerations, including space and staffing. For example, a key debate was whether to limit services to a single diagnosis or to provide intervention for multiple chronic conditions. Establishing the feasibility of LR–OT within one diagnostic area, and broadening services as a secondary goal, came to be the consensus among the team. With regard to staffing, it was agreed that the study team would initially conduct patient scheduling and reminder calls, with these tasks transitioning to the clinic staff after LR–OT services were established.
In Phase 1 (Months 0–2), before the launch of LR–OT services, providers and clinic staff were educated on the LR–OT program through a formal presentation, including the evidence base for LR–OT, referral criteria, and case studies illustrating a typical course of treatment. The research team also established the occupational therapy workspace and documentation processes, strengthened relationships within the clinic, and developed a referral process using electronic medical record (EMR) messaging. In Phase 2 (Months 3–7), we launched LR–OT services and aimed for full integration within the care team. Providers established effective communication strategies with the occupational therapist and developed a clearer understanding of LR–OT as they collaborated to deliver patient care. During this phase, we worked closely with providers to generate patient referrals and presented progress and updates at each monthly staff meeting, sharing success stories and patient cases.
In Phase 3 of the study (Months 8–12) and beyond, we continued to deliver LR–OT services and conducted strategic planning to facilitate maintenance of LR–OT within the clinic. Since the conclusion of the pilot study, clinic leadership and staff have viewed LR–OT highly favorably, with potential for it to be included in the primary care staffing model systemwide pending further data on its impact on clinical outcomes. Thus, the university has provided financial support for a Doctorate of Occupational Therapy resident to continue clinical services, and the research team has continued to collect outcome data. LR–OT services have expanded to include treatment of hypertension and have been fully incorporated into the clinic workflow, including provision of space and staff support.
Participants
Both clinic staff and patients within the LR–OT program participated in the implementation assessment. Eligible staff included all personnel employed at the clinic: providers (physicians, nurses, medical assistants, clinical pharmacists, social workers, community health workers [CHWs], and case managers), administrative staff (clerks), and clinic leadership (clinic and nursing directors). The study was approved by the institutional review board (IRB) before participant enrollment; patients in LR–OT completed informed consent, and clinic personnel received an information sheet before engaging in study activities.
The following inclusion criteria were used for patients: (1) diagnosis of Type 1 or Type 2 diabetes; (2) ages 18–75 yr; (3) most recent HbA1c level ≥9.0% or HbA1c not measured for ≥12 mo; (4) English or Spanish speaking; and (5) willingness to make lifestyle changes related to diabetes. Exclusion criteria were (1) untreated substance use or behavioral health disorder limiting participation in major life domains and (2) moderate to severe cognitive impairment, as determined by the referring provider. Eligibility determinations were made by the referring provider, with confirmation of objective criteria (Inclusion Criteria 1–4) by the study team via EMR review.
After referral to the study, patients were randomized to either LR–OT or a no-contact comparison group. Patients randomized to LR–OT were offered services, when possible, via “warm handoffs,” in which the provider introduced the patient to the occupational therapist during a clinic visit. Otherwise, patients were recruited by telephone. For patients randomized to the no-contact comparison group, we obtained a waiver of consent from the IRB to extract relevant clinical and demographic data via EMR review. These data will be used for future analyses comparing the LR–OT group with a control group who were not exposed to LR–OT.
Intervention
Patients were offered up to eight 1-hr occupational therapy sessions held every 2–3 weeks. The LR–OT intervention used the REAL Diabetes treatment manual (Pyatak et al., 2015, 2018), which includes seven content modules, each of which offers suggested goals, activities, and client resources. Sessions took place in a private room at the clinic, primarily on an individual basis, although some incorporated family education when relevant to treatment goals. The occupational therapist collaborated closely with other members of each client’s primary care team (via EMR messaging and in-person discussions) to ensure consistency of care among the treatment team. The therapist who delivered LR–OT was English–Spanish bilingual and had advanced training in LR, diabetes education, and motivational interviewing.
Data Collection
We collected data relevant to clinical outcomes as well as six distinct implementation and service outcomes following Proctor et al.’s (2011) implementation evaluation taxonomy. These outcomes included acceptability (perception of intervention as agreeable and satisfactory), appropriateness (perceived relevance or compatibility of intervention in a practice setting), feasibility (extent to which intervention can be successfully used in a practice setting), fidelity (extent to which intervention is implemented as intended), efficiency (degree to which providers work to “top of license”), and timeliness (availability of appointments when needed).
Survey Data
We administered the Barriers and Facilitators for Implementation (BFI) survey (Peters et al., 2002) at pre- and postimplementation to clinic personnel to assess their views on implementing LR–OT in their clinic. Patients receiving LR–OT completed a patient satisfaction survey at discharge (Cronbach’s α = .99), adapted from the American Physical Therapy Association (Goldstein et al., 2000).
Interviews and Focus Group Data
Interviews and focus groups were conducted at three time points. In Phase 1, we conducted key stakeholder interviews to clarify the role of LR–OT within the clinic and larger health care system and to evaluate how LR–OT could be successfully implemented. In Phase 2, we conducted a focus group among clinic staff to evaluate their perceptions of the LR–OT program’s strengths, areas for improvement, and possible future directions. In Phase 3, we conducted individual interviews with the treating occupational therapist; 8 patients (after their discharge from LR–OT) purposively sampled for variation on gender, ethnicity, and clinical outcomes (e.g., improved, worsened, or no change in HbA1c); and the providers who treated these patients to evaluate patient and provider satisfaction and how LR–OT was integrated within patients’ overall care plans. Patients received $20 for completing the interview.
Formative Data
We collected data generated through the routine implementation of LR–OT in the clinic, including referral patterns, patient enrollment and retention, intervention fidelity, and provider communication. Data sources included EMR documentation, minutes at clinic staff meetings, and field notes documenting significant events.
Clinical Data
We conducted EMR review to extract relevant background clinical and demographic data as well as measures of HbA1c, blood pressure, and depressive symptoms (two-item Patient Health Questionnaire; Löwe et al., 2005; Cronbach’s α = .83). Ideally, the baseline value would be within 28 days before the LR–OT start date, and the postintervention value would be within 28 days after the LR–OT discharge date. If multiple values were available, the ones closest to the start and discharge dates were used. If a value within 28 days before the start or 28 days after the discharge could not be found, we searched for a value within 28 days after the start or 28 days before the discharge, again selecting the value closest to the start or discharge date. If no qualifying value could be found, the data were considered missing.
Patients who enrolled in LR–OT completed baseline surveys at their initial evaluation and follow-up surveys at discharge. Surveys included the Summary of Diabetes Self-Care Activities (Toobert et al., 2000), the 20-item Short-Form Survey (SF–20; Stewart et al., 1988; Cronbach’s αs = .81–.88), the Self-Reported Behavioral Automaticity Index (Gardner et al., 2012; Cronbach’s α = .88), the Appraisal of Diabetes Scale (Carey et al., 1991; Cronbach’s α = .73), and self-rated medication adherence (Wilson et al., 2016; Cronbach’s α = .97). All measures have been previously used with adults with diabetes and have been found to be valid and reliable (Carey et al., 1991; Gardner et al., 2012; Löwe et al., 2005; Stewart et al., 1988; Toobert et al., 2000; Wilson et al., 2016). Patients received $20 for completing follow-up assessments. All surveys were available in English and Spanish.
Data Analysis
Qualitative data were transcribed, translated as needed, de-identified, and imported into NVivo 12 software (QSR International, Melbourne, Victoria, Australia) for coding and analysis. Trained research assistants coded data using a modified grounded theory approach. Before coding, the research team closely read several transcripts and developed and defined a set of codes, including a priori codes derived from our implementation taxonomy and codes emergent from interview data, which were periodically reviewed and refined through consensus. Strategies to enhance trustworthiness included data triangulation, maintaining an audit trail, peer debriefing by members of the study team, and prolonged engagement at the study site.
Measures of HbA1c, depressive symptoms, and blood pressure were obtained from each patient’s EMR. We calculated changes in EMR and survey variables as the postintervention value minus the baseline value for each patient, and we evaluated changes using a Wilcoxon signed-rank test. Staff surveys regarding barriers and facilitators could not be evaluated statistically because we had no way of matching up the sources of pre- and postintervention responses; the pre- and postintervention samples are also not statistically independent. Thus, we present the pre–post means without p values.
Results
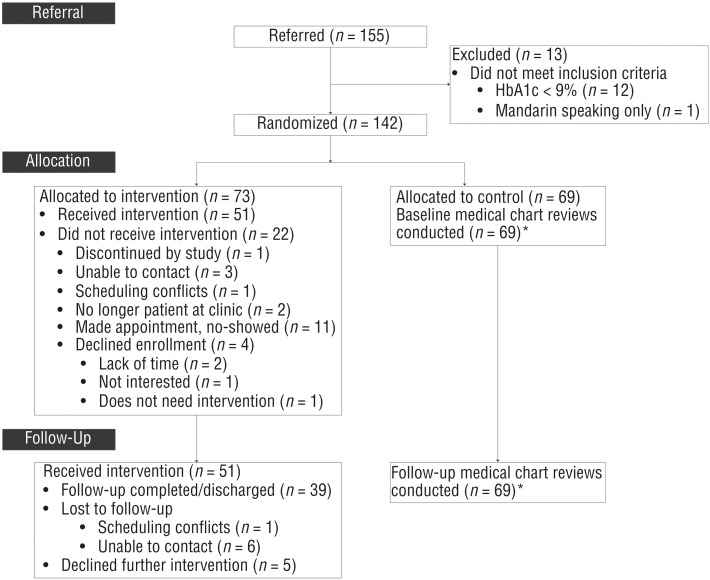
Of 155 patients referred to the study, 73 were randomized to LR–OT and are included in the present analyses. Study flow is detailed in Figure 1, and baseline patient characteristics are presented in Table 1. Overall, baseline characteristics were similar among evaluable patients (those who enrolled in LR–OT and completed both baseline and follow-up surveys) and nonevaluable patients (those who did not enroll in LR–OT or who enrolled but were lost to follow-up). Twenty staff members completed the BFI survey at baseline, and 26 staff members completed it at follow-up. Because the survey was administered anonymously on the recommendation of clinic leadership to facilitate candor, we cannot further characterize these staff members. Eleven staff members completed Phase 1 interviews: 4 occupational therapy practitioners within the larger health system, the assistant clinic director, and 6 providers (disciplines: medicine and pharmacy). Eight staff members participated in the focus group (disciplines: nursing, medicine, pharmacy, and case management). Four providers (disciplines: medicine and pharmacy), 8 patients, and the occupational therapist providing LR–OT completed case-based interviews.
Figure 1.
Consolidated Standards of Reporting Trials (CONSORT) flow diagram describing progress of participants through the study.
Note. An asterisk indicates that the data are not reported in this article. HbA1c = hemoglobin A1c.
Table 1.
Baseline Demographic and Clinical Characteristics Derived From EMR Review
| Variable | Total (N = 73) | Evaluablea (n = 37) | Nonevaluablea (n = 36) | p b |
| Age, yr, M (SD) | 53.3 (9.9) | 52.6 (9.5) | 54.1 (10.4) | .52 |
| Gender, n (%) | .62 | |||
| Female | 48 (66) | 23 (62) | 25 (69) | |
| Ethnicity, n (%) | .82 | |||
| Hispanic/Latino | 56 (77) | 28 (76) | 28 (78) | |
| Non-Hispanic/Latino | 14 (19) | 8 (22) | 6 (17) | |
| Unknown | 3 (4) | 1 (3) | 2 (6) | |
| Diabetes type, n (%) | 1.00 | |||
| T1D | 2 (3) | 1 (3) | 1 (3) | |
| T2D | 71 (97) | 36 (97) | 35 (97) |
Note. EMR = electronic medical record; M = mean; SD = standard deviation; T1D = Type 1 diabetes; T2D = Type 2 diabetes.
Evaluable patients are those who enrolled in Lifestyle Redesign® (LR)–occupational therapy and completed both baseline and follow-up surveys; nonevaluable patients either did not enroll in LR–occupational therapy or enrolled but withdrew or were lost to follow-up and thus did not have follow-up data.
For the age variable, a t test was used; for the gender, ethnicity, and diabetes type variables, Fisher’s exact test was used.
Acceptability
Whereas many providers saw the LR–OT program as acceptable from the outset, others’ perceptions of acceptability increased as they learned more about LR–OT. As the occupational therapist stated, “Even the providers who might’ve been less open to collaboration . . . started to open up more . . . as the study went forward.” Colocation allowed for consistent visibility and communication between the occupational therapist and providers, facilitating informal education on the occupational therapist’s role. One documented consultation described a CHW’s concern about a patient’s difficulty following exercise or diet recommendations. The occupational therapist, who also treated the patient, identified the client’s information processing limitations and suggested strategies for the CHW to implement, including repetition, pacing, and writing down information; this consultation was facilitated by colocation.
Although qualitative acceptability data among providers were largely positive, acceptability items on the BFI (e.g., “The LR–OT program will leave enough room to weigh the wishes of the patient”) did decline slightly at follow-up (mean = 4.06, standard deviation [SD] = 0.42) compared with preimplementation (mean = 4.29, SD = 0.48, range = 0–5; higher is better). Similarly, education also enhanced acceptability among patients who did not initially understand LR–OT. As 1 patient stated, “My doctor signed me up to [occupational therapy] and I didn’t go to the first three [visits] . . . I didn’t know what [occupational therapy] was about.” Key strategies enacted to improve acceptability included a waiting room slideshow educating patients about LR–OT and an informational flyer about what to expect from LR–OT. Among patients who enrolled in LR–OT, the patient satisfaction surveys indicated high acceptability, with a mean score of 4.91 (SD = 0.29, range = 0–5; higher is better) on questions pertaining to acceptability (e.g., “I would recommend this program to family or friends”).
Appropriateness
LR–OT was perceived by providers as being highly compatible with the clinical setting and addressing a gap in existing services. One provider noted, “[The occupational therapist] has been really sharp and in tune with the goals in primary care around health maintenance and disease management . . . what they brought to the table for a lot of our patients was something that a lot of us had been looking for and don’t have the time or resources to be able to provide.” We believe this outcome was largely due to education on the focus of LR–OT; 1 provider came to refer to LR–OT as habit makers and breakers.
This education helped providers gain an understanding of occupational therapy’s broader scope of practice. For example, 1 provider initially believed that the occupational therapist would provide traditional activities of daily living retraining; after education on the focus of LR–OT, this provider became one of the study’s main referral sources. Appropriateness items on the BFI survey (e.g., “The LR–OT program will fit into my ways of working in my practice”) received mean scores of 3.97 (SD = 0.49) at preimplementation and 3.92 (SD = 0.61) at follow-up (range = 0–5).
Referrals.
Of 155 patients referred to the study, 116 referrals (74.8%) were initiated by providers through EMR messaging to the study coordinator, and 39 patients (25.2%) were prescreened for eligibility via EMR review by the research team and suggested to providers; the latter strategy was added to ensure an adequate LR–OT caseload. Providers were able to accurately identify appropriate patients for LR–OT: Of the 116 provider-initiated referrals, 103 patients (88.8%) met eligibility criteria for LR–OT; of the remaining 13 patients, 12 had HbA1c test results after referral that rendered them ineligible, and 1 patient did not meet the language criterion.
Uptake and Retention Within the Lifestyle Redesign–Occupational Therapy Intervention.
Uptake and retention within the LR–OT intervention are detailed in Figure 1. Among the 73 patients who were randomized to LR–OT, 51 patients (69.9%) were seen at least once (17 patients for 1–5 sessions and 34 patients for >5 sessions). These patients completed an average of 6.0 (SD = 2.7) sessions each, and 38 patients (74.5%) remained in care until discharge, whereas 9 patients (17.6%) were lost to follow-up, and 4 patients (7.8%) withdrew. Among patients who had LR–OT, attendance rates compared favorably with their attendance at provider visits: Patients attended 73.0% of scheduled LR–OT visits versus 65.4% of provider visits. Attendance was encouraged with consistent reminder calls, reminder letters mailed to patients’ homes, and regular check-in calls.
Feasibility
Items on the BFI (e.g., “Patients will cooperate in implementing the LR–OT program”) had mean scores of 3.99 (SD = 0.38) at preimplementation and 3.90 (SD = 0.43) at postimplementation (range = 0–5). In qualitative interviews and focus groups, providers and staff perceived LR–OT to be successfully integrated within the clinic. For example, a provider stated, “It’s really unique and important to have [OT] expertise on a primary care team because it’s really not something that anyone else is doing or is expected to be doing or is really trained in doing at that level.” One feasibility challenge was finding adequate and reliable treatment space. Because of a clinic remodel in progress at the time, the occupational therapist did not have a consistent workspace when LR–OT was initiated and was shifted to different spaces to accommodate providers’ schedules. Some spaces were traditional exam rooms, which were small and lacked a workable surface for tabletop activities. After completion of the remodel and negotiation with the clinic team, the occupational therapist began treating patients in a larger suite with a large table for tabletop activities.
Fidelity
Therapist fidelity to domains addressed in the LR–OT treatment manual was 100%, as measured by EMR documentation of LR–OT sessions. Qualitative data indicating patients’ lifestyle changes in the LR–OT treatment manual domains provide further evidence of therapist fidelity. According to the providers, the LR–OT program addressed habits and routines relevant to diabetes, and they stated that LR–OT helped their patients decrease negative health management behaviors and increase positive ones. For example, 1 provider commented on a patient’s decreased alcohol consumption: “I had a patient who drank a lot of alcohol and [the occupational therapist] did . . . amazing work. [The patient] used to drink a tall pack a day or more . . . now [the patient] has cut back on that.” Another provider stated, “[The occupational therapist] really did a great job, and [the patient] is really motivated . . . exercising more . . . really determined to lose more weight.”
Timeliness
Among the 51 patients who completed ≥1 LR–OT sessions, the average time between acceptance and their initial LR–OT visit was 19.4 (SD = 27.7) days. Overall, patients perceived appointments to be convenient, with a mean score of 4.89 (SD = 0.33; scale ranging from 0 to 5) on patient satisfaction survey questions pertaining to timeliness (e.g., “The program offered appointments at convenient times”). Qualitative data suggested satisfactory timeliness; the primary challenge was the occupational therapist’s part-time schedule (0.5 full-time equivalent), which hindered some patients from attending the clinic when the occupational therapist was available or required visits on multiple days to see both the occupational therapist and their primary provider. As a provider noted, “[Occupational therapy] appointments were sometimes made on days when we weren’t going to be there, so then we were asking patients to come in on 2 days during the week, and so that was challenging.”
Efficiency
Items on the BFI (e.g., “The LR–OT program will contribute to my continuing education and professional development”) had mean scores of 4.41 (SD = 0.71) at preimplementation and 3.92 (SD = 0.74) at postimplementation (range = 0–5). Providers noted that LR–OT facilitated more efficient patient care; as 1 provider noted, “[Occupational therapist] integrated like peanut butter and jelly . . . definitely helped [the clinic] practice more efficiently.” The occupational therapist enhanced efficiency by addressing patients’ needs for behavior change support that other providers lacked the time or expertise to adequately undertake, by helping providers tailor treatment regimens to be feasible within patients’ daily lives, and by identifying unmet health care needs and facilitating appropriate referrals.
As the occupational therapist noted, “If [a patient] needed additional services, I could immediately go and request that from the provider.” Shared EMR documentation and colocation were keys to enhancing efficiency. Providers noted that because they could easily access occupational therapy documentation, “we end up finding [out] a lot of things about patients . . . [The occupational therapist] goes into so much detail; [the patient] works this shift and that shift and that’s why they cannot take their insulin.” Similarly, a provider noted that “if there were any [patient] concerns . . . [the occupational therapist] always alerted me that same day . . . so we were able to share in goal setting [and] figure out realistic goals.”
Clinical Outcomes
Changes in clinical outcomes are presented in Table 2. Pre–post changes on survey measures were assessed among the 37 evaluable patients; measures of HbA1c, blood pressure, and depressive symptoms were assessed among the 27–31 patients with appropriate EMR data available. With 37 evaluable patients, there is 80% power to detect an effect size of 0.47, whereas with 27 evaluable patients, the detectable effect size is 0.56. Decrease in HbA1c was correlated with the number of occupational therapy sessions attended (Spearman’s r = −.55, p = .002). These data should be considered preliminary, particularly the EMR-extracted outcomes, which will be compared with the randomized control group in future analyses.
Table 2.
Changes in Clinical Effectiveness Measures
| Outcome | Range (↑↓)a | Baseline, M (SD) | Follow-Up, M (SD) | p b | Effect Sizec [95% CI] |
| HbA1c | (↓) | 10.2 (2.1) | 9.3 (2.0) | .003 | −0.50 [−0.82, −0.19] |
| PHQ–2: Depressive symptoms | 0–6 (↓) | 0.7 (1.4) | 0.4 (1.1) | .47 | −0.12 [−0.40, 0.16] |
| Systolic blood pressure | (↓) | 134.5 (21.3) | 129.5 (17.8) | .22 | −0.21 [−0.66, 0.24] |
| Diastolic blood pressure | (↓) | 72.8 (14.1) | 66.5 (11.5) | .04 | −0.24 [−0.50, 0.01] |
| ADS: Diabetes distress | 9–47 (↓) | 26.3 (6.7) | 24.1 (6.1) | .06 | −0.33 [−0.66, 0.01] |
| Sugary drinks, number/mo | 0+ (↓) | 9.7 (7.7) | 6.9 (5.5) | .33 | −0.37 [−0.94, 0.21] |
| SDSCA: Healthy diet, days/wk | 0–7 (↑) | 3.6 (2.1) | 4.7 (1.4) | <.0001 | 0.54 [0.30, 0.77] |
| SDSCA: Exercise, days/wk | 0–7 (↑) | 2.6 (2.4) | 3.2 (2.3) | .07 | 0.26 [−0.07, 0.59] |
| SDSCA: SMBG, days/wk | 0–7 (↑) | 3.9 (2.7) | 5.2 (2.2) | .003 | 0.51 [0.19, 0.84] |
| SRBAI: SMBG habit strength | 0–28 (↑) | 16.2 (8.3) | 21.5 (6.0) | .002 | 0.67 [0.27, 1.06] |
| SDSCA: Foot care, days/wk | 0–7 (↑) | 4.0 (2.9) | 5.0 (2.5) | .02 | 0.40 [0.04, 0.77] |
| Medication adherence | 0–100 (↑) | 68.2 (23.7) | 78.6 (15.1) | .002 | 0.45 [0.08, 0.83] |
| SF–20: Mental function | 0–100 (↑) | 63.0 (19.3) | 70.3 (22.3) | .02 | 0.37 [0.02, 0.72] |
| SF–20: Physical function | 0–100 (↑) | 51.3 (31.3) | 63.2 (33.2) | .0003 | 0.43 [0.19, 0.67] |
| SF–20: Social function | 0–100 (↑) | 53.5 (36.8) | 64.9 (33.1) | .09 | 0.32 [−0.01, 0.65] |
| SF–20: Role function | 0–100 (↑) | 44.4 (41.5) | 66.7 (43.9) | .0001 | 0.66 [0.34, 0.97] |
| SF–20: Pain | 0–100 (↓) | 43.2 (32.2) | 59.5 (26.0) | .005 | 0.46 [0.13, 0.79] |
| SF–20: Health perception | 0–100 (↑) | 31.1 (22.4) | 50.9 (27.2) | <.0001 | 0.89 [0.55, 1.23] |
Note. ADS = Appraisal of Diabetes Scale; CI = confidence interval; HbA1c = hemoglobin A1c; PHQ–2 = two-item Patient Health Questionnaire; M = mean; SD = standard deviation; SDSCA = Summary of Diabetes Self-Care Activities; SF–20 = 20-item Short-Form General Health Survey; SMBG = self-monitoring of blood glucose; SRBAI = Self-Reported Behavioral Automaticity Index.
Numbers denote range of possible scores for measures with a defined range of scores; arrows indicate which direction is considered a favorable outcome.
A Wilcoxon signed-rank test was used.
Effect size represents Cohen’s d.
Discussion
Our findings closely parallel previous literature on occupational therapy in primary care, most notably those of Donnelly et al. (2013), who identified three overarching themes that contributed to the success of occupational therapy in primary care: providers developing an understanding of occupational therapy through education and the efforts of a physician champion; developing trust through colocation, shared EMR documentation, and interprofessional gatherings; and working in clinics with a culture of collaboration. Similarly, Valasek and Halle (2018) noted the importance of building relationships with physician champions and maintaining a collaborative approach to working on interprofessional teams. The elements contributing to the success of the LR–OT implementation are similar: Colocation and a shared EMR facilitated trust and collaboration with providers, whereas strong buy-in from clinic leadership and a well-established culture of interprofessional collaboration supported integration into the clinic workflow.
Despite the overall success of implementation, it is worth noting that there were slightly worse scores on the BFI at follow-up compared with preimplementation. We posit that this finding may be due to a larger sample size at follow-up (n = 26) compared with preimplementation (n = 20), with more staff with negative views participating. Staff may have also had a more realistic outlook after experiencing the implementation of LR–OT. Although the decline in scores could indicate a decrease in support for the LR–OT program over time, this concern is mitigated by the positive qualitative findings among providers and staff and strong support for program continuation. The change in scores over time underscores the importance of soliciting feedback and addressing barriers to implementation on an ongoing basis to ensure a program’s continued success.
Evidence to support the role of occupational therapy in managing chronic conditions in primary care settings is acutely needed (Leland et al., 2016). Although the clinical outcomes we have reported are preliminary, this study contributes to a growing body of evidence of occupational therapy’s effectiveness in addressing chronic conditions and the feasibility of integrating occupational therapy into primary care settings (e.g., Garvey et al., 2015; Pyatak et al., 2018; Simon & Collins, 2017). Moreover, although the minimum clinically important difference (MCID) for many health outcomes has not been established, a 0.5% change in HbA1c is considered clinically important, and the MCID for the SF–20 subscales ranges from 5 to 10 points (Wyrwich et al., 2005). Thus, the changes noted among patients who received LR–OT are of a sufficient magnitude to translate to noticeable improvements in health and quality of life.
Limitations
One limitation of this study is the representativeness of the study site. The clinic serves a relatively high-need population and provides integrated team-based care, which may be atypical of primary care clinics. Nevertheless, it is noteworthy that LR–OT demonstrated a positive impact even in the context of a rich array of existing services. A second limitation is the short study period. Given a longer implementation period, additional insights may have emerged; moreover, given a longer follow-up of patient outcomes, a long-term intervention effect may be assessed. Third, this study used only one highly skilled occupational therapist; the findings may therefore reflect a therapist effect. Finally, we analyzed pre–post outcomes only among evaluable patients who received LR–OT.
Although we did not find significant differences between evaluable and nonevaluable patients on baseline demographic variables, it is likely that patients who opted to receive the LR–OT intervention were not representative of the sample overall, introducing the possibility of selection bias. These data thus provide only a preliminary estimate of the intervention’s effect on clinical outcomes and should be interpreted with caution. In future analyses, we will compare outcomes among patients randomized to LR–OT with those in the no-contact comparison group, providing a more robust analysis of intervention effect.
Implications for Occupational Therapy Practice
The results of this study have the following implications for occupational therapy practice:
Occupational therapy fills a unique niche within interdisciplinary primary care teams, providing skilled services to support the initiation and maintenance of health management occupations.
Pre–post outcomes of patients receiving diabetes-focused LR–OT in primary care indicate improvements in HbA1c, blood pressure, health behaviors, and overall health status.
Key challenges in providing LR–OT in primary care include a lack of patient and staff knowledge of occupational therapy’s scope of practice and role within primary care, securing adequate and reliable workspace, and establishing a successful referral process and workflow.
Key factors contributing to the success of LR–OT include strong buy-in from clinic leadership, colocation of occupational therapy within the clinic, shared EMR documentation, consistent education of patients and providers regarding the occupational therapy scope of practice, and support for providers in screening patients and initiating referrals.
Conclusion
This study demonstrates the feasibility of a LR–OT diabetes management intervention when implemented in a safety-net primary care clinic. Strong support from clinic leadership and providers, colocation in the clinic, education of patients and providers about occupational therapy, and shared EMR documentation all contributed to the program’s success. In addition, preliminary analyses showed positive pre–post changes in HbA1c, diastolic blood pressure, diabetes self-care, and overall health status. Occupational therapists can play an important role in primary care teams because of their expertise in health behavior change, development of healthy habit and routines, and adaptation to changes in life circumstances.
Acknowledgments
We gratefully acknowledge Grace Cho, Elissa Lee, and Daniel Padilla Vega; the research participants; and the providers and staff at the Los Angeles County Department of Health Services for their support of this project. This research was supported by the Southern California Clinical and Translational Science Institute through National Center for Advancing Translational Sciences Grant UL1TR001855. The views in this article represent the opinions of the authors and not necessarily those of the National Institutes of Health. This study is registered with ClinicalTrials.gov (NCT03293914).
References
- Al-Lawati, J. A. (2017). Diabetes mellitus: A local and global public health emergency. Oman Medical Journal, 32, 177–179. 10.5001/omj.2017.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey, M. P., Jorgensen, R. S., Weinstock, R. S., Sprafkin, R. P., Lantinga, L. J., Carnrike, C. L., Jr., . . . Meisler, A. W. (1991). Reliability and validity of the Appraisal of Diabetes Scale. Journal of Behavioral Medicine, 14, 43–51. 10.1007/BF00844767 [DOI] [PubMed] [Google Scholar]
- Clark, F., Azen, S. P., Zemke, R., Jackson, J., Carlson, M., Mandel, D., . . . Lipson, L. (1997). Occupational therapy for independent-living older adults. A randomized controlled trial. JAMA, 278, 1321–1326. 10.1001/jama.1997.03550160041036 [DOI] [PubMed] [Google Scholar]
- Curran, G. M., Bauer, M., Mittman, B., Pyne, J. M., & Stetler, C. (2012). Effectiveness-implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50, 217–226. 10.1097/MLR.0b013e3182408812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly, C., Brenchley, C., Crawford, C., & Letts, L. (2013). The integration of occupational therapy into primary care: A multiple case study design. BMC Family Practice, 14, 60. 10.1186/1471-2296-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner, B., Abraham, C., Lally, P., & de Bruijn, G. J. (2012). Towards parsimony in habit measurement: Testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. International Journal of Behavioral Nutrition and Physical Activity, 9, 102. 10.1186/1479-5868-9-102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey, J., Connolly, D., Boland, F., & Smith, S. M. (2015). OPTIMAL, an occupational therapy led self-management support programme for people with multimorbidity in primary care: A randomized controlled trial. BMC Family Practice, 16, 59. 10.1186/s12875-015-0267-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein, M. S., Elliott, S. D., & Guccione, A. A. (2000). The development of an instrument to measure satisfaction with physical therapy. Physical Therapy, 80, 853–863. [PubMed] [Google Scholar]
- Hernandez-Tejada, M. A., Campbell, J. A., Walker, R. J., Smalls, B. L., Davis, K. S., & Egede, L. E. (2012). Diabetes empowerment, medication adherence and self-care behaviors in adults with Type 2 diabetes. Diabetes Technology and Therapeutics, 14, 630–634. 10.1089/dia.2011.0287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leland, N. E., Fogelberg, D. J., Halle, A. D., & Mroz, T. M. (2016). Occupational therapy and management of multiple chronic conditions in the context of health care reform. American Journal of Occupational Therapy, 71, 7101090010. 10.5014/ajot.2017.711001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Los Angeles County Department of Public Health, Office of Health Assessment and Epidemiology. (2012). Trends in diabetes: Time for action. Retrieved from http://publichealth.lacounty.gov/wwwfiles/ph/hae/ha/Diabetes_2012_FinalS.pdf
- Löwe, B., Kroenke, K., & Gräfe, K. (2005). Detecting and monitoring depression with a two-item questionnaire (PHQ–2). Journal of Psychosomatic Research, 58, 163–171. 10.1016/j.jpsychores.2004.09.006 [DOI] [PubMed] [Google Scholar]
- Peters, M. A. J., Harmsen, M., Laurant, M. G. H., & Wensing, M. (2002). Ruimte voor verandering? Knelpunten en mogelijkheden voor verandering in de patiëntenzorg [Room for improvement? Barriers to and facilitators for improvement of patient care]. Nijmegen, the Netherlands: Centre for Quality of Care Research, Radboud University Nijmegen Medical Centre. [Google Scholar]
- Proctor, E., Silmere, H., Raghavan, R., Hovmand, P., Aarons, G., Bunger, A., . . . Hensley, M. (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health, 38, 65–76. 10.1007/s10488-010-0319-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyatak, E. A., Carandang, K., & Davis, S. (2015). Developing a manualized occupational therapy diabetes management intervention: Resilient, Empowered, Active Living with Diabetes. OTJR: Occupation, Participation and Health, 35, 187–194. 10.1177/1539449215584310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pyatak, E. A., Carandang, K., Vigen, C. L. P., Blanchard, J., Diaz, J., Concha-Chavez, A., . . . Peters, A. L. (2018). Occupational therapy intervention improves glycemic control and quality of life among young adults with diabetes: The Resilient, Empowered, Active Living with Diabetes (REAL Diabetes) randomized controlled trial. Diabetes Care, 41, 696–704. 10.2337/dc17-1634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon, A. U., & Collins, C. E. (2017). Lifestyle Redesign® for chronic pain management: A retrospective clinical efficacy study. American Journal of Occupational Therapy, 71, 7104190040. 10.5014/ajot.2017.025502 [DOI] [PubMed] [Google Scholar]
- Stewart, A. L., Hays, R. D., & Ware, J. E., Jr. (1988). The MOS Short-Form General Health Survey: Reliability and validity in a patient population. Medical Care, 26, 724–735. 10.1097/00005650-198807000-00007 [DOI] [PubMed] [Google Scholar]
- Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The Summary of Diabetes Self-Care Activities measure: Results from 7 studies and a revised scale. Diabetes Care, 23, 943–950. 10.2337/diacare.23.7.943 [DOI] [PubMed] [Google Scholar]
- Valasek, S., & Halle, A. (2018). Practicing in an established primary care setting: Practical tips and considerations. OT Practice, 23 (15), 8–11, 13. 10.7138/otp.2018.2315.f1 [DOI] [Google Scholar]
- Wilson, I. B., Lee, Y., Michaud, J., Fowler, F. J., Jr., & Rogers, W. H. (2016). Validation of a new three-item self-report measure for medication adherence. AIDS and Behavior, 20, 2700–2708. 10.1007/s10461-016-1406-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2016). Global report on diabetes. Retrieved from https://www.who.int/diabetes/global-report/en/
- Wyrwich, K. W., Tierney, W. M., Babu, A. N., Kroenke, K., & Wolinsky, F. D. (2005). A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Services Research, 40, 577–591. 10.1111/j.1475-6773.2005.0l374.x [DOI] [PMC free article] [PubMed] [Google Scholar]