Abstract
Depression disproportionally affects people at risk of acquiring or living with HIV and is associated with worse health outcomes; however, depression care is not routinely integrated with HIV prevention and treatment services. Selection of the best depression intervention(s) for integration depends both on the prevalence and severity of depression among potential users. To inform depression care integration in a community-based setting in Lima, Peru, we retrospectively analyzed routinely collected depression screening data from men who have sex with men and transgender women seeking HIV prevention and care services (N=185). Depression was screened for using the Patient Health Questionnaire-9. Prevalence of any depression (PHQ-9 ≥5) was 42% and was significantly associated with the last sexual partner being “casual” (p=0.01). Most (81%) depressive symptoms were mild to moderate (≥5 PHQ-9 ≤14). Integrating depression care with HIV prevention and treatment services in Peru should begin by implementing interventions targeting mild to moderate depression.
Keywords: HIV, depression, MSM, transgender, integrated care
INTRODUCTION
Globally, depression among people at risk of or living with HIV (PLWH) significantly worsens health outcomes (Mayer et al., 2019; Poteat et al., 2020; Remien et al., 2019; Romo et al., 2019; Scheer & Pachankis, 2019; Tran et al., 2019). Untreated depression is associated with behaviors that increase HIV risk, including substance use, condomless intercourse, and attrition from HIV prevention programs (Agnew-Brune et al., 2019; Brown et al., 2006; Carney et al., 2019; Fendrich et al., 2013; Lennon et al., 2012; Romo et al., 2019). For PLWH, depression doubles the risk of mortality (Ironson et al., 2017), lowers uptake and adherence to medical care (Kunzweiler et al., 2018; Tao et al., 2018), and increases viral load (Meffert et al., 2019). Evidence supports the benefits of depression care for these populations (Sherr et al., 2011; Sikkema et al., 2015; Sikkema et al., 2010; van Luenen et al., 2018), and public policy promotes integrated mental health and HIV services as essential to ending the HIV epidemic (Chibanda, 2017; Fauci et al., 2019; Kulisewa et al., 2019); however, such integration is uncommon, constituting a mental health and HIV service “gap” (Chibanda, 2017).
A significant barrier to integrated depression and HIV services stems from a reliance on—and a simultaneous global shortage of—mental health professionals (e.g., psychiatrists, social workers). In low- and middle-income countries (LMICs), for example, there is on average less than one psychiatrist for every 100,000 persons (WHO, 2018). Even high-income settings like the US report a shortage of mental health professionals, especially in rural locations (Butryn et al., 2017). At the same time, LMICs are home to >90% of PLWH (UNAIDS, 2018). Therefore, integrated depression/HIV care models relying on mental health professionals are unlikely to be feasible in many settings.
Promising, alternative, mental health service models shift most service delivery from professionals to non-specialist health workers (NSHWs)—individuals not formally trained in mental health care. (Raviola et al., 2019). In these models, NSHWs screen patients and deliver evidence-based, low-intensity, non-pharmacological, psychological treatment for mild to moderate depression, referring patients with severe depression to mental health professionals. NSHWs already play a critical role in delivering HIV prevention and care services in LMICs (Bemelmans et al., 2016) and are consequently well-positioned to be cross-trained in basic mental health care.
HIV in Peru disproportionally affects men who have sex with men (MSM) and transgender women (TW), with prevalence rates of 13% (Castillo et al., 2015; Clark et al., 2014) and 30% (Silva-Santisteban et al., 2012), respectively, compared to the general adult population HIV prevalence rate of 0.01–0.03% (De Boni et al., 2014). Though Peru has dramatically scaled national access to mental health services (Toyama et al., 2017), the national HIV program lists depression as a risk factor for suboptimal antiretroviral therapy (ART) adherence (MINSA, 2020), depression care is not integrated with HIV services.
Here, we report depression prevalence and severity among attendees at a community-based clinic serving MSM and TW at risk for or living with HIV in Lima, Peru, to inform depression care integration in this setting.
MATERIALS AND METHODS
Participants, Procedures
We conducted a retrospective analysis of clinic data from individuals seeking HIV testing between August 2017 and December 2018 at Epicentro Salud, a non-profit organization providing free or low-cost sexual health services for LGBTQ people in Lima. Epicentro’s clientele is mostly mestizo/a, 20–35 years of age, and predominantly men who self-identify as gay and some TW. A physician assesses HIV/STI risk using an in-house assessment which includes depression screening. HIV testing is conducted using the Determine HIV-1/2 Ag/Ab Combo rapid test (ALERE Healthcare, SLU); clients testing positive are linked to free government-provided care. Clients with mild or greater depression are provided psychoeducation and referred to existing community-based mental health services for further evaluation. Those with moderately severe or greater depression and/or suicidal ideation are attended to by a staff psychologist and receive additional evaluation, referrals, and accompaniment to specialized mental health services.
Measures
The in-house risk assessment comprises 21 questions regarding age; clinic visit motive; sexual and gender self-identification (homosexual or gay, bisexual, heterosexual, transgender); presence of STI symptoms; number of days since last sexual intercourse; and most recent partner type and behaviors (stable/regular, casual, “one-nighter”; condom use; and, alcohol and/or drug use). Depression screening is conducted using the Spanish version of the Patient Health Questionnaire-9 (PHQ-9) (Kroenke et al., 2001), validated for Peru (Calderon et al., 2012). Standard PHQ-9 cut-off scores are used: minimal/no depression (PHQ-9 = 0–4); mild depression (PHQ-9 = 5–9); moderate depression (PHQ-9 = 10–14); moderately-severe depression (PHQ-9 = 15–19); and severe depression (PHQ-9 = 20–27) (Kroenke et al., 2001).
Data Analysis
Depression prevalence and severity were calculated using the PHQ-9 cutoff scores. To assess the relationship between depression, sexual health, and sexual behavior, we conducted statistical tests of bivariate association considering one characteristic at a time. Categorical variables were tested using Pearson’s chi-square test. Continuous variables were tested using a two-sample t-test (for apparently normally distributed data) and Wilcoxon’s rank-sum test (for clearly skewed data). All tests were conducted using R version 3.5.2 (2018).
Statement on Human Subjects
The research ethics committees for Epicentro in Peru and the University of South Florida designate retrospective studies utilizing existing data with no personal identifiers as non-human subjects research.
RESULTS
Study Population
Data from 185 MSM and TW presenting for sexual health services were analyzed. Median patient age was 27 years (range 17–58), and 58% (107/185) were seeking routine HIV and/or STI testing (i.e., not due to a specific sexual risk). Eighty-five percent (158/185) of persons identified as homosexual/gay; 9% (17/185) bisexual; 3% (5/185) heterosexual; and 3% (5/185) TW. Thirteen percent (24/181) reported living with HIV, of which 83% (20/24) were new infections detected during the visit (see Table I).
Table I:
Descriptive characteristics of Peruvian MSM and TW seeking HIV services in Lima, Peru (N = 185)
| Characteristics | Total*n (%) | PHQ-9† < 5 | PHQ-9 ≥ 5 | P value§§ |
|---|---|---|---|---|
| n (%) | n (%) | |||
| Age, years | 27 (23–33)‡ | 27 (23–32)‡ | 27 (23–34)‡ | 0.70 |
| Clinic visit motive | 0.85 | |||
| Routine check-up | 107 (58) | 63 (59) | 44 (41) | |
| Recent known sexual risk behavior | 78 (42) | 44 (56) | 34 (44) | |
| Self-identification § | 0.83 | |||
| Homosexual or gay | 158 (85) | 93 (59) | 65 (41) | |
| Bisexual | 17 (9) | 9 (53) | 8 (47) | |
| Heterosexual | 5 (3) | 3 (60) | 2 (40) | |
| Transgender woman | 5 (3) | 2 (40) | 3 (60) | |
| HIV result | 0.48 | |||
| Positive | 24 (13) | 16 (67) | 8 (33) | |
| Negative | 157 (87) | 89 (57) | 68 (43) | |
| STI symptoms present ¶ | 0.70 | |||
| Yes | 47 (26) | 26 (55) | 21 (45) | |
| No | 135 (74) | 81 (60) | 54 (40) | |
| Most recent sexual intercourse | ||||
| Days ago | 14 (6–30)‡ | 7 (6–30)‡ | 18 (7–56)‡ | 0.07 |
| Partner type | 0.01 | |||
| Stable/regular partner | 68 (37) | 48 (71) | 20 (29) | |
| Casual or ‘one-nighter’ | 117 (63) | 59 (50) | 58 (50) | |
| Condom used | 0.64 | |||
| Yes | 106 (58) | 64 (60) | 42 (40) | |
| No | 77 (42) | 43 (56) | 34 (44) | |
| Alcohol and/or drug use** | 0.38 | |||
| Yes | 34 (18) | 17 (50) | 17 (50) | |
| No | 150 (82) | 90 (60) | 60 (40) |
Due to missing data, not all variables sum to the total N.
PHQ-9: Patient Health Questionnaire
median (IQR)
Though not mutually exclusive categories, clinic attendees self-identified as belonging to only one of these groups.
STI symptoms included: burning while urinating; perianal/genital warts; ulcers on penis and/or in anus; penile and/or anal discharge; and genital rash.
Drugs included: marijuana, cocaine, poppers, and other.
P-values are based on Pearson’s chi-square test for all qualitative characteristics, two-sample t-test for age, and Wilcoxon’s rank-sum test for “days ago” (due to high skewness and extreme values in data).
Depression Prevalence and Severity
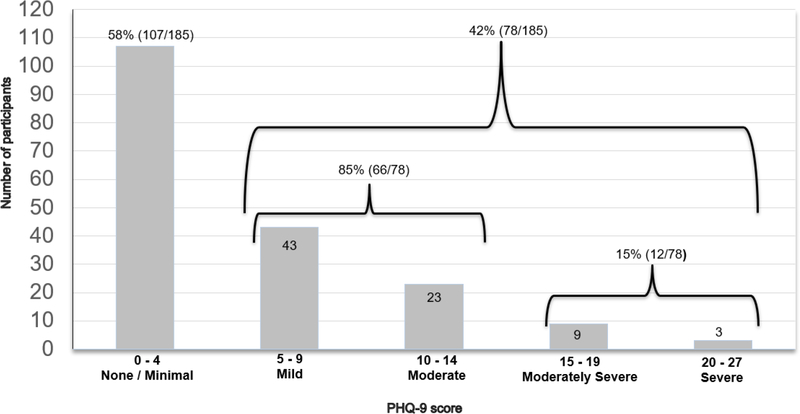
Depression prevalence (PHQ-9 ≥5) was 42% (78/185), of which 81% (66/78) of participants had mild to moderate depression severity (5≤ PHQ-9 ≤14). Depression severity per the 6 PHQ-9 cutoff scores was: minimal/none (PHQ-9 = 0–4): 58% (107/185); mild (PHQ-9 = 5–9): 23% (43/185); moderate (PHQ-9 = 10–14): 12% (23/185); moderately-severe (PHQ-9 = 15–19): 5% (9/185); and severe (PHQ-9 = 20–27): 2% (3/185) (see Figure 1).
Figure 1:
Distribution of the prevalence and severity of depression among Peruvian MSM and TW (N = 185)
Bivariate Analysis
In bivariate analysis, mild or greater depression (PHQ-9 ≥5) was significantly associated with the most recent sexual partner being “casual” versus a stable/regular partner (p=0.01). There was a marginally significant relationship (p=0.07) of persons with mild or greater depression to go longer without sexual intercourse than those with minimal/no depression (see Table I). No association between depression and HIV infection was observed.
DISCUSSION
In this retrospective analysis from MSM and TW seeking sexual health services at a community-based health center, greater than minimal depression (PHQ-9 ≥5) was detected in 42% of clinic attendees. In contrast, the prevalence of any depression in this sample was 15 times greater than the 2.8% point prevalence of depression among adult Peruvians in metropolitan Lima (MINSA, 2013); however, the use of different instruments, variability of, and populations limits direct comparison.
Our study complements other reports of depression among Peruvian MSM and TW. Maldonado et al. (Maldonado Ruiz et al., 2015) found that the frequency of a major depressive episode among recipients of ART in a public hospital in Lima (N=205) was higher than the general population but not associated with ART adherence. In another study, depressive symptoms were prevalent in 44.5% of a study population comprised of Peruvian MSM and TW diagnosed with HIV for >1 year (N=302) (Ferro et al., 2015). Again, depression was not associated with ART adherence; however, it was highly correlated with problem alcohol use. We found that depression was significantly associated with the last sexual partner being casual. While the relationship between mood and sexual behavior is complex, a possible interpretation of this finding is that participants with depressive symptomology sought to self-remedy a negative mood state—albeit in a transitory manner—by seeking contact with others (Bancroft et al., 2003).
A central finding in this study was that most (81%) depression scores fell in the mild to moderate range of severity (5≤ PHQ-9 ≤14). Moderate levels of depression—but neither low nor high depression levels—are associated with increased sexual risk-taking in MSM at risk of HIV (Koblin et al., 2006) and living with HIV (O’Cleirigh et al., 2013). If future research bears out this association in Peruvian MSM and TW, efforts towards integrating depression care with HIV services should target moderate depression because of its unique association with HIV risk and because it may be the most prevalent of depression severities. Importantly, we do not advocate the non-prioritization of severe depression care for these populations. Instead, we recommend that depression screening in HIV service settings allows for meaningful differentiation of depression severity (as opposed to only “some depressive symptomology” versus “no depression”) and that the treatment offered is commensurate to the detected depression severity.
There is also an opportunity to capitalize on a global movement to increase access to mental health care for all people integrating existing NSHW-delivered interventions into HIV services. Over 90 LMICs (Keynejad et al., 2018) are currently implementing low-intensity depression interventions disseminated by the World Health Organization’s (WHO) Mental Health Gap Programme (mhGAP) (WHO, 2010). These countries could start by expanding these interventions into HIV service delivery platforms, training a “ready workforce” of NSHW delivering HIV services (Chibanda, 2017). Doing so could be a significant step towards providing mental health services for people at risk of or living with HIV.
Limitations
As a retrospective, cross-sectional analysis of existing data, important factors which could impact depression, were unaddressable (e.g., trauma history; stigma; detailed alcohol/drug use information; ART adherence). Further, the PHQ-9 assesses depressive symptoms during the previous two weeks; a definitive depression diagnosis requires additional clinical assessment (Reynolds, 2010). Finally, the small sample size and low number of TW precluded tests of association of depression with HIV and other morbidities or sub-population comparisons, and our findings are not generalizable beyond this sample.
CONCLUSIONS
Integrating depression care with HIV prevention and treatment services in Peru could begin by training NSHW in existing low-intensity depression interventions targeting mild to moderate depression.
ACKNOWLEDGMENTS:
The authors express gratitude to Epicentro for provision of these data and their important work towards integration of depression and HIV care in Lima, Peru and to Caroline Muster for manuscript preparation support.
STATEMENT OF FUNDING:
The project was supported by the National Institutes of Health awards NIDA K99/R00DA046311. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
DECLARATION OF INTEREST STATEMENT: The others declare no conflicts of interest.
REFERENCES
- Agnew-Brune CB, Balaji AB, Mustanski B, Newcomb ME, Prachand N, Braunstein SL, Brady KA, Hoots BE, Smith JS, Paz-Bailey G, Broz D, & Group N-YS (2019). Mental health, social support, and HIV-related sexual risk behaviors among HIV-negative adolescent sexual minority males: three US cities, 2015. AIDS Behav, 23(12), 3419–3426. 10.1007/s10461-019-02525-5 [DOI] [PubMed] [Google Scholar]
- Bancroft J, Janssen E, Strong D, & Vukadinovic Z (2003). The relation between mood and sexuality in gay men [journal article]. Arch Sex Behav, 32(3), 231–242. 10.1023/a:1023461500810 [DOI] [PubMed] [Google Scholar]
- Bemelmans M, Baert S, Negussie E, Bygrave H, Biot M, Jamet C, Ellman T, Banda A, van den Akker T, & Ford N (2016). Sustaining the future of HIV counselling to reach 90–90-90: a regional country analysis. J Int AIDS Soc, 19(1), 20751. 10.7448/IAS.19.1.20751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown LK, Tolou-Shams M, Lescano C, Houck C, Zeidman J, Pugatch D, Lourie KJ, & Project SSG (2006). Depressive symptoms as a predictor of sexual risk among African American adolescents and young adults. J Adolesc Health, 39(3), 444 e441–448. 10.1016/j.jadohealth.2006.01.015 [DOI] [PubMed] [Google Scholar]
- Butryn T, Bryant L, Marchionni C, & Sholevar F (2017). The shortage of psychiatrists and other mental health providers: Causes, current state, and potential solutions [Expert Commentary]. International Journal of Academic Medicine, 3(1), 5–9. 10.4103/ijam.Ijam_49_17 [DOI] [Google Scholar]
- Calderon M, Galvez-Buccollini JA, Cueva G, Ordonez C, Bromley C, & Fiestas F (2012). [Validation of the Peruvian version of the PHQ-9 for diagnosing depression]. Rev Peru Med Exp Salud Publica, 29(4), 578–579. 10.1590/s1726-46342012000400027 [DOI] [PubMed] [Google Scholar]
- Carney B, White J, Xu X, Sunil T, Daniels C, Byrne M, Ganesan A, Deiss R, Macalino G, Agan BK, & Okulicz JF (2019). Relationship between depression and risk behaviors in a US Military population with HIV infection. AIDS Care, 31(9), 1152–1156. 10.1080/09540121.2019.1595522 [DOI] [PubMed] [Google Scholar]
- Castillo R, Konda KA, Leon SR, Silva-Santisteban A, Salazar X, Klausner JD, Coates TJ, & Caceres CF (2015). HIV and Sexually Transmitted Infection Incidence and Associated Risk Factors Among High-Risk MSM and Male-to-Female Transgender Women in Lima, Peru. J Acquir Immune Defic Syndr, 69(5), 567–575. 10.1097/QAI.0000000000000667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chibanda D (2017). Depression and HIV: integrated care towards 90–90-90. Int Health, 9(2), 77–79. 10.1093/inthealth/ihw058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark JL, Konda KA, Silva-Santisteban A, Peinado J, Lama JR, Kusunoki L, Perez-Brumer A, Pun M, Cabello R, Sebastian JL, Suarez-Ognio L, & Sanchez J (2014). Sampling methodologies for epidemiologic surveillance of men who have sex with men and transgender women in Latin America: an empiric comparison of convenience sampling, time space sampling, and respondent driven sampling. AIDS Behav, 18(12), 2338–2348. 10.1007/s10461-013-0680-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Boni R, Veloso VG, & Grinsztejn B (2014). Epidemiology of HIV in Latin America and the Caribbean. Curr Opin HIV AIDS, 9(2), 192–198. 10.1097/COH.0000000000000031 [DOI] [PubMed] [Google Scholar]
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, & Giroir BP (2019). Ending the HIV Epidemic: A Plan for the United States. JAMA, 321(9), 844–845. 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- Fendrich M, Avci O, Johnson TP, & Mackesy-Amiti ME (2013). Depression, substance use and HIV risk in a probability sample of men who have sex with men. Addict Behav, 38(3), 1715–1718. 10.1016/j.addbeh.2012.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferro EG, Weikum D, Vagenas P, Copenhaver MM, Gonzales P, Peinado J, Cabello R, Lama JR, Sanchez J, & Altice FL (2015). Alcohol use disorders negatively influence antiretroviral medication adherence among men who have sex with men in Peru. AIDS Care, 27(1), 93–104. 10.1080/09540121.2014.963013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ironson G, Fitch C, & Stuetzle R (2017). Depression and Survival in a 17-Year Longitudinal Study of People With HIV: Moderating Effects of Race and Education. Psychosom Med, 79(7), 749–756. 10.1097/PSY.0000000000000488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keynejad R, Dua T, Barbui C, & Thornicroft G (2018). WHO Mental Health Gap Action Programme (mhGAP) Intervention Guide: a systematic review of evidence from low and middle-incomecountries. Evid Based Ment Health, 21(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, & Buchbinder S (2006). Risk factors for HIV infection among men who have sex with men. AIDS, 20(5), 731–739. 10.1097/01.aids.0000216374.61442.55 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JB (2001). The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med, 16(9), 606–613. 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulisewa K, Stockton MA, Hosseinipour MC, Gaynes BN, Mphonda S, Udedi MM, & Pence BW (2019). The Role of Depression Screening and Treatment in Achieving the UNAIDS 90–90-90 Goals in Sub-Saharan Africa. AIDS Behav, 23(Suppl 2), 153–161. 10.1007/s10461-019-02593-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunzweiler CP, Bailey RC, Okall DO, Graham SM, Mehta SD, & Otieno FO (2018). Depressive Symptoms, Alcohol and Drug Use, and Physical and Sexual Abuse Among Men Who Have Sex with Men in Kisumu, Kenya: The Anza Mapema Study. AIDS Behav, 22(5), 1517–1529. 10.1007/s10461-017-1941-0 [DOI] [PubMed] [Google Scholar]
- Lennon CA, Huedo-Medina TB, Gerwien DP, & Johnson BT (2012). A role for depression in sexual risk reduction for women? A meta-analysis of HIV prevention trials with depression outcomes. Soc Sci Med, 75(4), 688–698. 10.1016/j.socscimed.2012.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado Ruiz H, Peña Olano RF, & Tomateo Torvisco JD (2015). Frecuencia de episodio depresivo mayor y factores relacionados en pacientes infectados por el virus de la inmunodeficiencia humana en tratamiento antirretroviral de gran actividad (TARGA) en un hospital público de Lima. Rev Neuropsiquiatr, 78, 3–13. http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S0034-85972015000100002&nrm=iso [Google Scholar]
- Mayer KH, Sullivan PS, & Beyrer C (2019). Silver bullets and structural impediments to HIV prevention. Lancet HIV, 6(11), e729–e732. 10.1016/S2352-3018(19)30274-7 [DOI] [PubMed] [Google Scholar]
- Meffert SM, Neylan TC, McCulloch CE, Maganga L, Adamu Y, Kiweewa F, Maswai J, Owuoth J, Polyak CS, Ake JA, & Valcour VG (2019). East African HIV care: depression and HIV outcomes. Glob Ment Health (Camb), 6, e9. 10.1017/gmh.2019.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministerio de Salud (MINSA), Instituto Nacional de Salud Mental (2013). Estudio Epidemiológico de Salud Mental en Lima Metropolitana y Callao – Replicación 2012. Informe General. Anales de Salud Mental, XXIX, 1–392. [Google Scholar]
- Ministerio de Salud (MINSA) (20120). Norma técnica de salud de atención integral del adulto con infección por el virus de la inmunodeficiencia humana (VIH). http://bvs.minsa.gob.pe/local/MINSA/4479.pdf
- O’Cleirigh C, Newcomb ME, Mayer KH, Skeer M, Traeger L, & Safren SA (2013). Moderate levels of depression predict sexual transmission risk in HIV-infected MSM: a longitudinal analysis of data from six sites involved in a “prevention for positives” study. AIDS Behav, 17(5), 1764–1769. 10.1007/s10461-013-0462-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteat TC, Celentano DD, Mayer KH, Beyrer C, Mimiaga MJ, Friedman RK, Srithanaviboonchai K, Safren SA, & Team HS (2020). Depression, sexual behavior, and HIV treatment outcomes among transgender women, cisgender women and men who have sex with men living with HIV in Brazil and Thailand: a short report. AIDS Care, 32(3), 310–315. 10.1080/09540121.2019.1668526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raviola G, Naslund JA, Smith SL, & Patel V (2019). Innovative Models in Mental Health Delivery Systems: Task Sharing Care with Non-specialist Providers to Close the Mental Health Treatment Gap. Curr Psychiatry Rep, 21(6), 44. 10.1007/s11920-019-1028-x [DOI] [PubMed] [Google Scholar]
- Remien RH, Stirratt MJ, Nguyen N, Robbins RN, Pala AN, & Mellins CA (2019). Mental health and HIV/AIDS: the need for an integrated response. AIDS, 33(9), 1411–1420. 10.1097/QAD.0000000000002227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds WM (2010). The PHQ-9 works well as a screening but not diagnostic instrument for depressive disorder. Evid Based Ment Health, 13(3), 96. 10.1136/ebmh.13.3.96 [DOI] [PubMed] [Google Scholar]
- Romo ML, George G, Mantell JE, Mwai E, Nyaga E, Strauss M, Odhiambo JO, Govender K, & Kelvin EA (2019). Depression and sexual risk behavior among long-distance truck drivers at roadside wellness clinics in Kenya. PeerJ, 7, e7253. 10.7717/peerj.7253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheer JR, & Pachankis JE (2019). Psychosocial Syndemic Risks Surrounding Physical Health Conditions Among Sexual and Gender Minority Individuals. LGBT Health, 6(8), 377–385. 10.1089/lgbt.2019.0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Clucas C, Harding R, Sibley E, & Catalan J (2011). HIV and depression--a systematic review of interventions. Psychol Health Med, 16(5), 493–527. 10.1080/13548506.2011.579990 [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Dennis AC, Watt MH, Choi KW, Yemeke TT, & Joska JA (2015). Improving mental health among people living with HIV: a review of intervention trials in low- and middle-income countries. Glob Ment Health (Camb), 2. 10.1017/gmh.2015.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Drabkin AS, Meade CS, Hansen NB, & Pence BW (2010). Mental health treatment to reduce HIV transmission risk behavior: a positive prevention model. AIDS Behav, 14(2), 252–262. 10.1007/s10461-009-9650-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva-Santisteban A, Raymond HF, Salazar X, Villayzan J, Leon S, McFarland W, & Caceres CF (2012). Understanding the HIV/AIDS epidemic in transgender women of Lima, Peru: results from a sero-epidemiologic study using respondent driven sampling. AIDS Behav, 16(4), 872–881. 10.1007/s10461-011-0053-5 [DOI] [PubMed] [Google Scholar]
- Tao J, Vermund SH, & Qian HZ (2018). Association Between Depression and Antiretroviral Therapy Use Among People Living with HIV: A Meta-analysis. AIDS Behav, 22(5), 1542–1550. 10.1007/s10461-017-1776-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toyama M, Castillo H, Galea JT, Brandt LR, Mendoza M, Herrera V, Mitrani M, Cutipe Y, Cavero V, Diez-Canseco F, & Miranda JJ (2017). Peruvian Mental Health Reform: A Framework for Scaling-up Mental Health Services. Int J Health Policy Manag, 6(9), 501–508. 10.15171/ijhpm.2017.07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX, Ho RCM, Ho CSH, Latkin CA, Phan HT, Ha GH, Vu GT, Ying J, & Zhang MWB (2019). Depression among Patients with HIV/AIDS: Research Development and Effective Interventions (GAPRESEARCH). Int J Environ Res Public Health, 16(10). 10.3390/ijerph16101772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Joint United Nations Programme on HIV/AIDS (UNAIDS). (2018). The Global HIV/AIDS Epidemic. US Department of Health & Human Services and supported by the Secretary’s Minority AIDS Initiative Fund (SMAIF) https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics [Google Scholar]
- van Luenen S, Garnefski N, Spinhoven P, Spaan P, Dusseldorp E, & Kraaij V (2018). The Benefits of Psychosocial Interventions for Mental Health in People Living with HIV: A Systematic Review and Meta-analysis. AIDS Behav, 22(1), 9–42. 10.1007/s10461-017-1757-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO). (2010). WHO Mental Health Gap Action Programme (mhGAP). [Google Scholar]
- World Health Organization (WHO). (2018). Psychiatrists and nurses (per 100 000 population). World Health Organization; https://www.who.int/gho/mental_health/human_resources/psychiatrists_nurses/en/ [Google Scholar]