Abstract
This study was a 10-week double-blind, placebo-controlled pilot trial of mirtazapine for anxiety in youth with autism spectrum disorder (ASD). Participants were ages 5 to 17 years with ASD and clinically significant anxiety (Pediatric Anxiety Rating Scale [PARS] score ≥10). Thirty participants were randomized to mirtazapine (7.5–45 mg/day) or placebo in a 2:1 ratio. The co-primary outcome measures were the PARS and the Clinical Global Impressions-Improvement subscale (CGI-I). Mirtazapine resulted in a statistically significant within group decrease in anxiety on the PARS (ES 1.76, p < 0.001). The improvement in PARS score for mirtazapine versus placebo was clinically meaningful but not statistically significant (ES = 0.63, p = 0.64). Forty-seven percent of participants assigned to mirtazapine (95% CI 22%: 74%) and 20% assigned to placebo (95% CI 2%: 60%) were rated “much improved” (CGI-I = 2) or “very much improved” (CGI-I = 1) for anxiety, p = 0.46. No statistically significant differences in mean 10-week changes between mirtazapine and placebo occurred on any outcome measure. There were no statistically significant differences in adverse effect frequency between mirtazapine and placebo. The results are consistent with mirtazapine’s safety and tolerability and meet three of four pre-specified indicators of efficacy (statistically significant change in total PARS score for mirtazapine, numerically greater reduction in total PARS score for mirtazapine than placebo, numerically higher number of responders to mirtazapine than placebo, but not greater than 50% of participants receiving mirtazapine rated as responders). Implementation of a larger randomized controlled trial of mirtazapine for the treatment of anxiety in this population is supported.
Clinical trial registration information: Mirtazapine Treatment of Anxiety in Children and Adolescents with Pervasive Developmental Disorders; https://clinicaltrials.gov; NCT01302964.
Subject terms: Drug development, Autism spectrum disorders
Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental condition characterized by deficits in social communication and interaction as well as restricted, repetitive patterns of behavior, interests, or activities [1]. Comorbid anxiety is common among children and adolescents with ASD. A prospective study including 75 children with ASD (ages 9–13 years; mean full-scale intelligence quotient [IQ] 77, range: <25–170) and 52 typically developing controls found that 69% of youth with ASD had clinically significant anxiety, compared to 8% of typically developing children [2]. The presenting signs and symptoms of anxiety among children with ASD were highly varied, both aligning with and differing from the Diagnostic and Statistical Manual of Mental Disorders (DSM)-specified anxiety disorders [2]. Distinct presentations of anxiety among children with ASD included fears of change, uncommon phobias such as of toilets or of specific songs, and social fears that are related to confusion about interaction rather than negative evaluation by others. A birth cohort study of 31,220 individuals (median age 22.8 years) comparing rates of anxiety disorders in patients with ASD to age- and sex-matched controls demonstrated that those with ASD were 3.5 times more likely to have a lifetime history of an anxiety disorder [3]. In this study, the cumulative incidence of anxiety disorders among those with ASD by the age of 30 years was 50%. The authors of this study postulate that the psychosocial sequelae associated with ASD including difficulties developing and maintaining relationships and challenges succeeding academically and vocationally may contribute to the development of anxiety disorders [3]. Furthermore, a meta-analysis demonstrated that 39.6% of youth with ASD have at least one comorbid anxiety disorder based on the DSM, Fourth Edition (DSM-IV) criteria [4]. The most common disorder was specific phobia (29.8%), followed by obsessive-compulsive disorder (OCD) (17.4%), and social anxiety disorder (16.6%). Moreover, higher levels of anxiety are associated with more severe symptoms of ASD as measured by the Children’s Social Behavior Questionnaire [5]. Severe anxiety in youth with ASD has also been associated with increased aggression, decreased participation in social activities, and poor social relationships [6].
Double-blind, placebo-controlled studies on the pharmacologic treatment of anxiety as the primary target symptom in children and adolescents with ASD and Pervasive Developmental Disorders (PDDs) are lacking. Small retrospective and open-label studies have assessed the effect of selective serotonin reuptake inhibitors (SSRIs) on anxiety in PDDs. Steingard et al. conducted an open-label study of sertraline in nine children with autistic disorder (ages 6–12 years old) that had “transition-induced behavioral deterioration” [7]. Five of the nine subjects showed clinically significant improvement in symptoms of irritability or anxiety or a combination of the two, on dosages of sertraline of 25 to 100 mg/day. Four subjects developed interfering agitation and two subjects lost the beneficial effects of sertraline over time. A retrospective study of open-label citalopram (5-40 mg daily) for target symptoms including anxiety, aggression, stereotypies, and preoccupations was completed in 17 children with PDDs (ages 4–15 years) [8]. Ten of the participants (59%) were judged to be “much improved” or “very much improved” on the Clinical Global Impressions-Improvement subscale (CGI-I) [8]. Four of the 17 children (23.5%) experienced treatment-limiting adverse effects including increased agitation (n = 2), insomnia (n = 1), and tics (n = 1). In a prospective, open-label study of 18 youth with PDDs (mean age 11.3 ± 3.6 years), low-dose fluvoxamine (1.5 mg/kg/day) was administered to target compulsive behavior and/or anxiety-related symptoms [9]. No statistically significant overall change in CGI-I scores or a measure of repetitive behavior occurred, nor was fluvoxamine associated with a statistically significant change in anxiety scores, as measured by the Screen for Child Anxiety Related Disorders (SCARED) [9]. Three of the 18 youth (16.7%) in this study required premature discontinuation of fluvoxamine due to behavioral activation [9]. A recently published randomized controlled trial of fluoxetine for the primary target symptoms of obsessive-compulsive behaviors in children and adolescents with ASD was published [10]. The Spence Children’s Anxiety Scale was used to measure change in symptoms and experiences of anxiety as a secondary outcome measure, although no statistically significant difference was found between fluoxetine and placebo [10].
There is a need to determine whether medications with a different mechanism of action from SSRIs are safe, tolerable, and efficacious for the treatment of anxiety in ASD. Buspirone, a serotonin (5-HT)1A receptor partial agonist and dopamine (D2) antagonist, has Food and Drug Administration (FDA)-approval for the treatment of generalized anxiety disorder (GAD) in adults. A retrospective chart review including 31 youth with ASD (ages 8–17 years, without intellectual disability) treated with buspirone for comorbid anxiety disorders demonstrated that 18 of the subjects (58%) were either “much improved” or “very much improved” on the CGI-I and nine of the subjects (29%) were “minimally improved” [11]. An open-label study assessed the effect of buspirone on anxiety and irritability in 22 children and adolescents with ASD (ages 6–17 years) [12]. Nine participants (41%) showed a “marked response” and seven participants (32%) showed a “moderate response,” as measured by the CGI-I after six to eight weeks of treatment. A 24-week, randomized, placebo-controlled trial including 166 children with ASD (ages 2–6 years) assessed the efficacy of buspirone for the treatment of restricted and repetitive behaviors [13]. There was no statistically significant drug-placebo difference in the Autism Diagnostic Observation Schedule (ADOS) composite score which measures overall symptoms of ASD. There was a statistically significant decrease in the ADOS Restricted and Repetitive Behavior score for the buspirone 2.5 mg twice daily group but the buspirone 5 mg twice daily and placebo groups showed no change. Anxiety was a secondary outcome measure of the study and there was a statistically significant improvement in anxiety over time with buspirone 2.5 mg twice daily, but the placebo group also showed statistically significant improvement, as measured by an anxiety composite score (Aberrant Behavior Checklist [ABC] Irritability subscale, Leiter emotion regulation). There was no statistically significant improvement in anxiety in the buspirone 5 mg twice daily group [13].
Mirtazapine, a central presynaptic α2-adrenergic antagonist, increases norepinephrine (NE) release which results in increased synaptic serotonin 5-HT levels facilitated by the stimulation of α1-adrenergic receptors on 5-HT neuron cell bodies. Mirtazapine also blocks serotonin 5-HT2 and 5-HT3 receptors [14], a mechanism likely responsible for the anxiolytic and hypnotic effects of the drug [15].
Mirtazapine has an FDA approval for the treatment of major depressive disorder in adults. There is also some evidence to support the anxiolytic effects of mirtazapine. Open-label studies have demonstrated benefit from mirtazapine in children with GAD and social phobia [16, 17]. Compared to SSRIs, mirtazapine may have more rapid anxiolytic and antidepressant effects in adults [18], and a lower risk of pharmacokinetic interactions [19].
The effectiveness of mirtazapine for anxiety in 26 individuals (ages 3.8–23.5 years) with PDDs was previously reported in a naturalistic, retrospective study [20]. All but one of the subjects had received previous unsuccessful trials of psychotropic medications (mean number 5.5 ± 5.4). Seventeen subjects were taking concomitant psychotropic medications at the time of mirtazapine initiation. Open-label mirtazapine (dose range 7.5–45 mg daily; mean 30.3 ± 12.6 mg daily) was prescribed for a variety of target symptoms including anxiety. Twenty-five of 26 subjects completed at least four weeks of treatment with mirtazapine, with a mean duration of treatment of 150 ± 103 days. Baseline and endpoint ratings were obtained using the CGI Scale. Outcome measures were assessed after a mean of five months of treatment (range 11-368 days). Nine of 26 subjects (34.6%) were judged responders (“much improved” or “very much improved”) on the CGI-I, showing improvement in anxiety as well as irritability, hyperactivity, and depression. For the entire group of subjects, mirtazapine led to a statistically significant improvement in CGI Severity subscale (CGI-S) ratings (p < 0.04). The modest rate of response of approximately 35% may be reflective of the severity of illness of the sample (mean CGI-S rating = “markedly ill” and multiple prior unsuccessful medication trials).
The goal of the current study was to perform a pilot randomized controlled trial to assess the safety, tolerability, and preliminary efficacy of mirtazapine for the treatment of anxiety associated with ASD and PDDs. Subjects with the DSM-IV PDD diagnoses of autistic disorder, Asperger’s disorder, and PDD not otherwise specified (NOS) were eligible for the study. These three diagnostic subtypes were subsumed by the equivalent DSM, Fifth Edition (DSM-5) diagnosis of ASD [1], which is the diagnostic term used in the remainder of this manuscript to describe our sample. To our knowledge, this is the first prospective, randomized, double-blind, placebo-controlled trial of a pharmacologic treatment for the primary target of anxiety in children and adolescents with ASD.
Methods
Study design
The study was a 10-week randomized, double-blind, placebo-controlled pilot trial of mirtazapine in youth with ASD. The study was conducted at the Christian Sarkine Autism Treatment Center/James Whitcomb Riley Hospital for Children/Indiana University School of Medicine, and the Lurie Center for Autism/Massachusetts General Hospital (MGH) for Children/Harvard Medical School between August 2010 and October 2017. The study was approved by the Indiana University Institutional Review Boards and Partners Healthcare Institutional Review Board, respectively. Guardians of all participants provided written informed consent prior to study involvement. Assent was obtained from youth when possible.
Study participants were youth ages 5 to 17 years inclusive with a diagnosis of ASD and clinically significant anxiety as evidenced by a Pediatric Anxiety Rating Scale (PARS) score of ≥ 10 at screen and baseline. All subjects had an abbreviated IQ of ≥ 50 on the Stanford Binet, Fifth Edition (SB5) [21]. Participants were diagnosed via clinical interview completed by a board-certified child and adolescent psychiatrist experienced in providing clinical care to youth with ASD, based on the DSM-IV diagnostic criteria, and corroborated by the Autism Diagnostic Interview-Revised (ADI-R) [22] administered by research reliable raters.
Subjects with a diagnosis of Rett’s disorder, childhood disintegrative disorder, OCD, post-traumatic stress disorder (PTSD), major mood disorder, psychotic disorder, or substance use disorder were excluded. These diagnoses were determined using the Anxiety and Related Disorders Interview Schedule (ADIS-IV) [23]. Additional exclusion criteria included: use of other antidepressants, buspirone, or benzodiazepines, use of linezolid (due to risk of serotonin syndrome), and a previous adequate trial of mirtazapine (defined as a dosage of at least 15 mg for at least four weeks). Other non-benzodiazepine and non-antidepressant psychotropic medications including stimulants, sleep aids (including melatonin), and atypical antipsychotics were permitted if the dose was stable for at least 60 days prior to study initiation and remained stable throughout the trial. In addition, non-pharmacologic treatments (e.g., applied behavioral analysis, cognitive behavioral therapy, occupational therapy, speech/language therapy) were permitted as long as the treatment approach was stable for at least 60 days prior to study initiation and remained stable throughout the trial.
At the screening visit, all subjects underwent a psychiatric diagnostic evaluation, medical history, and physical examination. Laboratory studies included a complete blood cell count with differential, a comprehensive metabolic panel (including electrolytes, renal function tests, liver function tests, glucose), and thyroid function tests, ideally obtained in the fasting state. A urine pregnancy test was also completed for female participants of childbearing potential. The following standardized scales and testing were also administered/conducted at screen: ADI-R; ADIS-IV; SB5; Peabody Picture Vocabulary Test, Fourth Edition (PPVT-4); [24] and the Vineland Adaptive Behavior Scales, Second Edition (Vineland II) [25]. Suicidality was assessed at each visit by directly asking the subject (when verbal skills were sufficient) and the caregiver about any thoughts or behaviors that directly or indirectly might indicate suicidality (e.g., morbid thoughts, self-injury, statements about life not worth living), when indicated by positive responses. At screen, The Columbia-Suicide Severity Rating Scale (C-SSRS) was administered per the instructions at www.cssrs.columbia/ed/clinical_trials.html. The C-SSRS was also administered at each subsequent visit following the first report of suicidality.
Following screening and baseline measures, participants were randomly assigned to either mirtazapine or placebo in a 2:1 ratio as the optimal way of gathering more preliminary data on safety and tolerability of mirtazapine in this population. Randomization was not stratified by site or patient characteristics. Treatment group was assigned by the unblinded investigational drug service based on a computer-generated randomization list. All participants, guardians, raters, and investigators remained blind to study assignment. Mirtazapine (7.5 mg) and matching placebo capsules, identical in appearance and taste, were prepared by the University of California San Francisco Drug Product Services Laboratory (Christian Sarkine Autism Treatment Center site) and the MGH Clinical Trials Pharmacy (Lurie Center for Autism site). Participants randomized to mirtazapine initially received 7.5 mg nightly. For subjects weighing less than 50 kg, the dose was increased by 7.5 mg per week to a maximum total daily dose of 45 mg. For subjects weighing more than 50 kg, the dose was increased by 7.5 or 15 mg per week depending on clinical response and tolerability to a maximum total daily dose of 45 mg. The medication was dosed either once or twice daily depending on tolerability. The optimal dose was achieved by week 6 of treatment; subjects remained at this dosage until the end of the study. Subjects were evaluated in person at weeks 2, 4, and 6. Telephone visits for monitoring of adverse effects and dosage adjustment occurred at weeks 1, 3, 5, and 8. Additional unscheduled telephone visits were permitted when needed. A final in-person visit was conducted at week 10. Assessment of adverse effects was completed during each interaction. Vital signs, height, and weight were assessed at each clinic visit.
Compliance with the study medication was assessed at each visit by reviewing the study drug diary completion and the pill count of the number of capsules prescribed, dispensed, and returned. The percent compliance was calculated at each visit. If compliance fell below 70% of the prescribed dosage for a given interval between visits, subjects and parents were counseled on study drug compliance and given warning that a repeat lapse could lead to termination from the study (barring extenuating circumstances).
The co-primary outcome measures were the PARS and the CGI-I [26] which were assessed at each clinic visit (PARS) and each follow-up in-clinic visit (weeks 2, 4, 6, and 10) (CGI-I). The PARS is a 5-item scale which assesses severity across common anxiety disorders in children including GAD, social anxiety disorder, and separation anxiety disorder. Secondary outcome measures included the SCARED [27], Child and Adolescent Symptom Inventory (CASI) Anxiety Items [28], ABC [29], Children’s Sleep Habit Questionnaire (CSHQ) [30], which was administered at baseline and weeks 2, 4, 6, and 10, and the CGI-S [26] and Developmental Disability-Child Global Assessment Scale (DD-CGAS) [31] which were administered at baseline and week 10.
Statistical analysis
The study was designed to have 80% power to detect a standardized effect size of 0.7 for 10-week within group changes in clinical outcomes for mirtazapine, with 20 participants assigned to mirtazapine. The corresponding effect size required for detecting between group differences with 10 participants assigned to placebo was 1.1. Given that the trial was not powered to demonstrate moderate between-group differences, the analysis considered four indicators of efficacy pre-specified in the protocol: statistically significant reduction in total PARS score with mirtazapine, 50% or more participants receiving mirtazapine rated as responders, numerically greater reduction in total PARS score for mirtazapine than placebo, and numerically higher number of responders to mirtazapine than placebo. Statistical significance tests comparing change between mirtazapine and placebo were considered exploratory.
Data analyses were intent-to-treat and included all observed data for participants who did not complete the study. Baseline measures were summarized for participants randomized to mirtazapine and placebo using frequencies and percentages for categorical variables and means and standard deviations for continuous variables and ordinal scale scores. Repeated measures regression models tested for changes in mean ratings on clinical scales, except for the CGI-I, and for mean changes in vital signs. Covariates for the regression models were treatment (mirtazapine or placebo), time (in categories), and treatment x time interaction. Statistical significance of 10-week changes and differences in 10-week changes between mirtazapine and placebo were assessed using linear contrasts of the model parameters. Estimated effect sizes (ES) were calculated by dividing the model-estimated mean 10-week changes and their differences by the pooled standard deviation at baseline [32]. Models assumed equal means between mirtazapine and placebo at baseline to improve efficiency and allowed unstructured covariance between repeated measurements. All outcome data collected prior to week six for the participant assigned to mirtazapine who withdrew due to adverse effects were included in these analyses. Missing outcome data were not imputed.
Participants with CGI-I ratings of “much improved” (CGI-I = 2) or “very much improved” (CGI-I = 1) were classified as responders, and those with less improvement (CGI-I ≥ 3) were classified as non-responders. The planned analysis specified fitting a repeated measures logistic regression model for change in the probability of response over time. However, this model could not be fit to the observed data due to 0% response within treatment groups for some timepoints. Instead, probabilities of response at 10 weeks for mirtazapine and placebo and the odds ratio comparing them, along with corresponding exact confidence intervals, were calculated. Fisher’s exact test assessed the statistical significance of the 10-week comparison in probability of response. The participant assigned to mirtazapine who withdrew due to adverse effects did not have a 10-week CGI-I rating and did not contribute data to these calculations. We did not impute a CGI-I score for the participant who withdrew prior to 10 weeks because excluding the participant was more consistent with the repeated measures analysis for binary data specified in the protocol, which relies on the MCAR assumption for missing data.
Statistical analyses were conducted using SAS/STAT software, (version 9.4, SAS Institute, Cary, NC). Statistical tests were two-sided. A Bonferroni multiple testing correction was applied to results for the PARS and the CGI-I to account for our choice of two co-primary outcome measures; p-values and confidence intervals reported in the results and tables reflect this correction. All other statistical tests were performed at the test-wise alpha = 0.05 significance level.
Results
Study participants
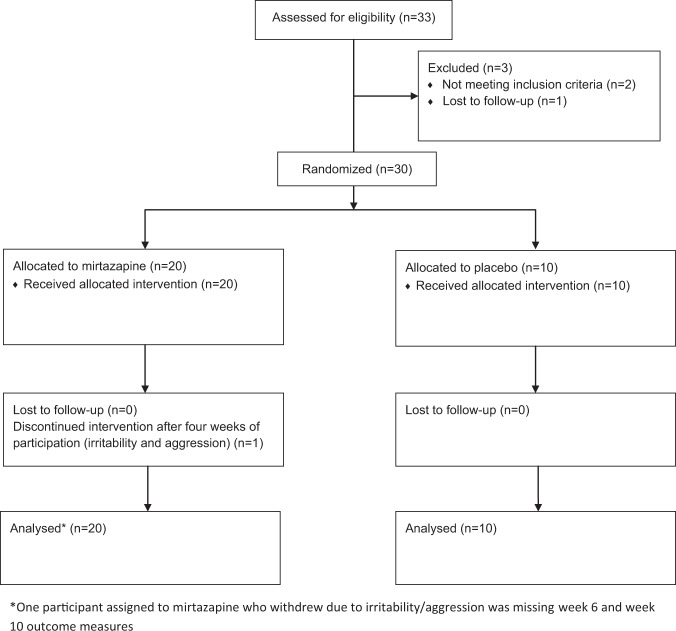
Thirty-three subjects were screened for participation in the study. Three subjects failed to meet the inclusion/exclusion criteria for the study, including IQ < 50, not meeting DSM-IV diagnostic criteria for included subtypes of PDD, and lost to follow-up, respectively (Fig. 1). Thirty eligible children were randomly assigned to mirtazapine (N = 20) or placebo (N = 10) after obtaining informed consent. Table 1 presents baseline characteristics of the sample. Participants were 80% male with an age range of 5-17 years (mean age 11 years). One participant assigned to mirtazapine withdrew after four weeks of study participation due to symptoms of irritability and aggression. The remaining 29 participants remained in the study for the full 10-week treatment period. Ten subjects in the mirtazapine group took concomitant psychotropic medications (three a sleep aid [melatonin = 2, clonidine = 1], four a stimulant, one an atypical antipsychotic and two a sleep aid [melatonin = 2] and a stimulant). Three subjects in the placebo group took concomitant psychotropic medications (one a sleep aid [melatonin = 1] and two a stimulant).
Fig. 1.
CONSORT flow diagram of participant disposition from screening through study completion.
Table 1.
Baseline characteristics of youth with ASD randomly assigned to Mirtazapine or Placebo.
| Mirtazapine (n = 20) | Placebo (n = 10) | |
|---|---|---|
| Age, Mean (SD) | 10.9 (3.6) | 11.3 (4.1) |
| Male, n (%) | 17 (85%) | 7 (70%) |
| White, n (%)1 | 17 (85%) | 9 (90%) |
| Black or African American, n (%) | 1 (5%) | 1 (10%) |
| Asian, n (%) | 1 (5%) | 0 (0%) |
| Other Race, n (%) | 1 (5%) | 0 (0%) |
| Hispanic or Latino, n (%)2 | 2 (11%) | 2 (20%) |
| DSM-IV Diagnosis, n (%) | ||
| Autistic Disorder | 13 (65%) | 8 (80%) |
| Asperger’s Disorder | 3 (15%) | 1 (10%) |
| PDD NOS | 4 (20%) | 1 (10%) |
| IQ, Mean (SD) | 84.9 (22.5) | 89.6 (23.6) |
| PPVT-4 Score, Mean (SD) | 88.6 (27.5) | 93.1 (22.2) |
| Vineland Adaptive Behavior II Composite Score, Mean (SD) | 73.1 (12.3) | 73.6 (12.5) |
| Clinical Global Impression–Severity subscale, n (%)3 | ||
| 4: Moderately Ill | 7 (35%) | 2 (20%) |
| 5: Markedly Ill | 13 (65%) | 8 (80%) |
| Pediatric Anxiety Rating Scale, 5-Item Total, Mean (SD) | 18.5 (2.9) | 18.1 (2.8) |
| Screen for Childhood Anxiety Related Emotional Disorders, Mean (SD) | 33.5 (13.9) | 28.1 (8.8) |
| Child and Adolescent Symptom Inventory, Anxiety, Mean (SD) | 26.0 (10.3) | 19.7 (6.5) |
| Aberrant Behavior Checklist, Mean (SD) | ||
| I - Irritability | 15.3 (8.2) | 16.4 (9.9) |
| II - Lethargy/Social Withdrawal | 14.9 (8.3) | 6.2 (4.4) |
| III - Stereotypic Behavior | 7.8 (5.7) | 4.4 (4.5) |
| IV - Hyperactivity/Noncompliance | 21.5 (10.7) | 17.5 (13.2) |
| V - Inappropriate Speech | 5.6 (3.8) | 3.7 (2.9) |
| Children’s Sleep Habit Questionnaire, Mean (SD) | 51.2 (9.5) | 47.7 (6.8) |
| Developmental Disability-Child Global Assessment Scale, Mean (SD) | 55.7 (6.1) | 57.7 (6.1) |
1Participants could select more than one race. No participants selected American Indian/Alaskan Native, or Native Hawaiian/Other Pacific Islander.
2Hispanic or Latino ethnicity was missing for two youth.
3No youth were rated 6 (Severely Ill) or 7 (Extremely Ill).
4ASD Autism spectrum disorder; PDD NOS Pervasive developmental disorder not otherwise specified; IQ intelligence quotient; PPVT-4 Peabody Picture Vocabulary Test, Fourth Edition.
Efficacy
Nine of the 19 participants assigned to mirtazapine who completed 10-week assessments (47%, corrected 95% CI 22%: 74%) and two of the 10 participants assigned to placebo (20%, corrected 95% CI 2%: 60%) were rated as “much improved” (CGI-I = 2) or “very much improved” (CGI-I = 1) for anxiety. There was no statistically significant difference in the probability of treatment response based on the CGI-I, a co-primary treatment outcome measure, between mirtazapine and placebo (corrected p = 0.46, Fisher’s exact test). The estimated odds ratio comparing response to mirtazapine versus placebo was 3.6 (corrected 95% CI 0.5: 28.0). Table 2 presents mean 10-week changes in the remaining clinical ratings. There were no statistically significant differences in mean 10-week changes between mirtazapine and placebo for either the PARS, a co-primary treatment outcome measure, or for any of the secondary outcome measures. The ES comparing improvement on the PARS between mirtazapine and placebo was 0.63.
Table 2.
Model-estimated Mean changes from baseline (95% Confidence Intervals) for study outcomes at 10 weeks.
| Mirtazapine (N = 20)1 | ES2 | p | Placebo (N = 10) | ES2 | p | Mirtazapine-Placebo | ES2 | p | |
|---|---|---|---|---|---|---|---|---|---|
| Pediatric Anxiety Rating Scale, 5-Item Total3 | −4.9 (−7.3, −2.6) | 1.76 | <0.001 | −3.2 (−6.5, 0.2) | 1.13 | 0.07 | −1.8 (−5.9, 2.4) | 0.63 | 0.64 |
| Screen for Childhood Anxiety Related Emotional Disorders | −9.7 (−15.4, −4.0) | 0.77 | 0.003 | −5.1 (−12.6, 2.4) | 0.41 | 0.17 | −4.6 (−13.2, 4.1) | 0.36 | 0.29 |
| Child and Adolescent Symptom Inventory Anxiety Items | −9.4 (−14.1, −4.8) | 0.98 | <0.001 | −5.5 (−11.9, 0.8) | 0.58 | 0.09 | −3.9 (−11.6, 3.8) | 0.41 | 0.31 |
| Aberrant Behavior Checklist | |||||||||
| I - Irritability | −3.7 (−7.5, 0.1) | 0.43 | 0.053 | −3.3 (−8.5, 2.0) | 0.38 | 0.21 | −0.5 (−6.9, 6.0) | 0.06 | 0.88 |
| II - Lethargy/Social Withdrawal | −4.9 (−7.6, −2.1) | 0.59 | 0.001 | −2.0 (−5.7, 1.7) | 0.24 | 0.28 | −2.9 (−7.2, 1.5) | 0.35 | 0.19 |
| III - Stereotypic Behavior | −2.8 (−4.3, −1.2) | 0.50 | 0.001 | −1.9 (−4.0, 0.2) | 0.34 | 0.08 | −0.9 (−3.3, 1.5) | 0.16 | 0.46 |
| IV - Hyperactivity/Noncompliance | −5.0 (−8.1, −1.9) | 0.43 | 0.003 | −1.0 (−5.4, 3.3) | 0.09 | 0.62 | −3.9 (−9.3, 1.4) | 0.34 | 0.14 |
| V - Inappropriate Speech | −0.7 (−1.9, 0.5) | 0.19 | 0.26 | −0.5 (−2.1, 1.2) | 0.13 | 0.56 | −0.2 (−2.2, 1.8) | 0.06 | 0.84 |
| Children’s Sleep Habit Questionnaire | −4.3 (−7.1, −1.4) | 0.49 | 0.004 | −3.9 (−7.5, −0.2) | 0.44 | 0.04 | −0.4 (−4.6, 3.8) | 0.05 | 0.85 |
| Developmental Disability-Child Global Assessment Scale | 4.6 (1.9, 7.3) | 0.76 | 0.002 | 1.8 (−1.9, 5.5) | 0.30 | 0.32 | 2.8 (−1.7, 7.4) | 0.46 | 0.21 |
1One participant assigned to mirtazapine who withdrew due to an adverse effect was missing week 6 and week 10 measurements.
2Effect sizes were calculated by dividing the absolute value of the model-estimated mean 10-week change from baseline (mirtazapine and placebo) or the model-estimated mean treatment difference at 10 weeks (mirtazapine-placebo) by the pooled standard deviation at baseline.
3The Pediatric Anxiety Rating Scale (PARS) 5-item total score was a co-primary outcome measure for the study. The corresponding confidence intervals and p-value have been adjusted to reflect a Bonferroni correction accounting for the study’s two co-primary outcomes, the PARS and the Clinical Global Impressions-Improvement subscale.
Symptoms of anxiety as assessed by the PARS (Fig. 2) as well as the SCARED and the CASI-Anxiety Items (secondary outcome measures) decreased substantially and to a statistically significant degree and for youth taking mirtazapine (Table 2; standardized effect size (ES) = 1.76, t27 = −4.91, corrected p < 0.001 PARS; ES = 0.77, t33 = −3.48, p = 0.003 SCARED; ES = 0.98, t29 = −4.15, p < 0.001 CASI-Anxiety Items). Children and adolescents taking placebo experienced more modest but still clinically meaningful decreases in anxiety symptoms (ES > 0.40, Table 2). Youth taking mirtazapine also experienced statistically significant reductions in the ABC subscales for Lethargy/Social Withdrawal (ES = 0.59, t30 = −3.57, p = 0.001); Stereotypic Behavior (ES = 0.50, t32 = −3.55, p = 0.001); and Hyperactivity/Noncompliance (ES = 0.43, t26 = −3.30, p = 0.003); a statistically significant reduction in problematic sleep habits as assessed by the CSHQ (ES = 0.49, t32 = −3.08, p = 0.004); and improvement in general functioning as assessed by the DD-CGAS (ES = 0.76, t28 = 3.52, p = 0.002). Children on placebo experienced a significant reduction in problematic sleep habits as assessed by the CSHQ (ES = 0.44, t35 = −2.13, p = 0.04) but experienced smaller (ES < 0.40) and non-statistically significant reductions for the remaining scales.
Fig. 2. Graphical representation of changes in mean scores on the Pediatric Anxiety Rating Scale (PARS) between mirtazapine and placebo over the 10-week trial.
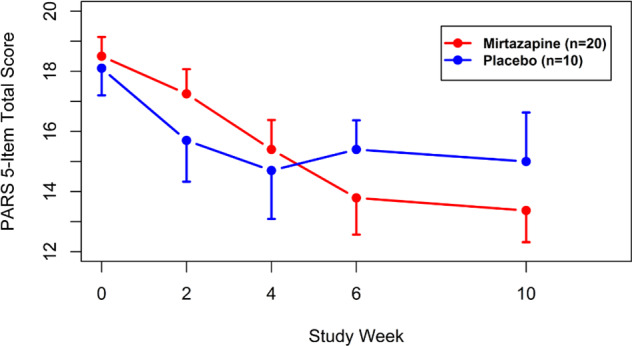
Mean PARS 5-item total score (points) and standard error of the mean (error bars) by treatment group and study week. One participant assigned to mirtazapine withdrew from the study due to an adverse effect after week 4; calculations for mirtazapine at study weeks 6 and 10 were based on data from the remaining 19 participants.
The mean (SD) dosage of mirtazapine at 10 weeks was 41.8 (5.2) mg per day. Of the 19 participants assigned to mirtazapine and remaining in the study at 10 weeks, the 10-week dosage frequency was two (15%) at 30 mg, three (23%) at 37.5 mg, and eight (62%) at 45 mg for weight < 50 kg; and one (17%) at 37.5 mg and five (83%) at 45 mg for weight ≥ 50 kg. The mean (SD) dosage of placebo at 10 weeks was 40.5 (7.2) mg per day. For the 10 participants assigned to placebo, the 10-week dosage frequency was one (13%) at 22.5 mg, three (38%) at 37.5 mg, and four (50%) at 45 mg for weight < 50 kg and 2 (100%) at 45 mg for weight ≥50 kg. The mean (SD) dose per kg weight was 1.2 (0.6) mg/kg for mirtazapine and 1.1 (0.5) mg/kg for placebo. A post-hoc statistical test found no correlation between improvement in total PARS score and dose per kg weight (estimated Pearson rho = 0.2, p = 0.47) for mirtazapine. Fourteen of the subjects randomized to mirtazapine received the drug twice daily and six received it once a day. Nine of the subjects randomized to placebo received it twice daily and one received it once a day.
Safety and tolerability
No participant experienced a severe adverse event or suicidality during the study. All participants experienced one or more adverse effects. Table 3 lists the adverse effects documented during treatment with mirtazapine and placebo in order of descending frequency. The most commonly reported adverse effects among participants treated with mirtazapine were sedation/drowsiness, appetite increase, and irritability. The most commonly reported adverse effects among participants treated with placebo were sedation/drowsiness, stomach/abdominal discomfort, aggression, and vomiting. There were no statistically significant differences in adverse effect frequency between mirtazapine and placebo (p > 0.10 all effects).
Table 3.
Adverse effect frequency by treatment group.
| Mirtazapine | Placebo | ||||
|---|---|---|---|---|---|
| N | % | N | % | p1 | |
| Sedation/drowsiness | 12 | 60 | 6 | 60 | 1.00 |
| Appetite increase | 10 | 50 | 2 | 20 | 0.24 |
| Irritability | 7 | 35 | 3 | 30 | 1.00 |
| Nausea | 6 | 30 | 3 | 30 | 1.00 |
| Stomach or abdominal discomfort | 5 | 25 | 4 | 40 | 0.43 |
| Aggression | 5 | 25 | 4 | 40 | 0.43 |
| Diarrhea | 5 | 25 | 2 | 20 | 1.00 |
| Sadness | 4 | 20 | 3 | 30 | 0.66 |
| Vomiting | 3 | 15 | 4 | 40 | 0.18 |
| Nasal congestion or cold | 4 | 20 | 2 | 20 | 1.00 |
| Nightmares or dreams | 4 | 20 | 2 | 20 | 1.00 |
| Constipation | 3 | 15 | 3 | 30 | 0.37 |
| Headache | 3 | 15 | 2 | 20 | 1.00 |
| Difficulty falling asleep | 3 | 15 | 1 | 10 | 1.00 |
| Enuresis | 3 | 15 | 1 | 10 | 1.00 |
| Appetite decrease | 2 | 10 | 2 | 20 | 0.58 |
| Fever | 2 | 10 | 2 | 20 | 0.58 |
| Social withdrawal2 | 2 | 10 | 2 | 20 | 0.58 |
| Concentration difficulty | 2 | 10 | 1 | 10 | 1.00 |
| Dizziness/faintness | 2 | 10 | 1 | 10 | 1.00 |
| Unspecified or not otherwise listed nose/throat2,3 | 2 | 10 | 1 | 10 | 1.00 |
| Localized rash | 2 | 10 | 1 | 10 | 1.00 |
| Anxiety/nervousness/worry | 2 | 10 | 0 | 0 | 0.54 |
| Body-focused repetitive behavior2 | 2 | 10 | 0 | 0 | 0.54 |
| Change in speech | 2 | 10 | 0 | 0 | 0.54 |
| Dry mouth | 2 | 10 | 0 | 0 | 0.54 |
| Interrupted sleep/other sleep problems | 2 | 10 | 0 | 0 | 0.54 |
| Self-injurious behavior | 2 | 10 | 0 | 0 | 0.54 |
| Sinus condition | 2 | 10 | 0 | 0 | 0.54 |
| Tiredness/fatigue | 2 | 10 | 0 | 0 | 0.54 |
| Allergies not otherwise specified | 1 | 5 | 1 | 10 | 1.00 |
| Restlessness/agitation | 1 | 5 | 1 | 10 | 1.00 |
| Stereotypy | 1 | 5 | 1 | 10 | 1.00 |
| Flu or upper respiratory problems | 0 | 0 | 2 | 20 | 0.10 |
Adverse effects are listed in order of descending frequency. Effects reported by two or more participants are included in the table. Adverse effects reported by one participant assigned to mirtazapine (5%) and no participants assigned to placebo were accidental injury, compulsions2, decreased motor activity, disinhibition, ear infection, emotional outburst, euphoria/giddiness, eye irritation, hair problems, increased motor activity, intermittent nosebleed, other pain, sensory sensitivity2, sore throat, sweating, taste abnormality, throat infection, unspecified or not otherwise listed musculoskeletal effect (muscle twitching in both arms)2, and unspecified or not otherwise listed psychological/behavioral effect (firesetting)2. Adverse effects reported by one participant assigned to placebo (10%) and no participants assigned to mirtazapine were indigestion and unspecified or not otherwise listed effect, mouth (inflamed salivary gland)2.
1Frequencies were compared using Fisher’s exact test.
2Effects originally classified by study physician as not otherwise specified and reclassified by study staff.
3One participant each assigned to mirtazapine reported laryngitis and hoarseness; one participant assigned to placebo reported itchy throat.
Children taking mirtazapine experienced a statistically significant increase in body mass index (BMI) of 0.7 kg/m2 (95% CI: 0.3, 1.2; t28 = 3.54, p = 0.001), but there was no statistically significant difference in 10-week change between mirtazapine and placebo (mean difference = 0.5 kg/m2; 95% CI: −0.2, 1.3; t28 = 1.49; p = 0.15), nor was there a statistically significant 10-week change for placebo (mean change=0.2 kg/m2; 95% CI: −0.4, 0.8; t28 = 0.69; p = 0.50). Children taking mirtazapine also experienced a statistically significant increase in heart rate relative to children taking placebo (mean difference = 10.7 beats per minute [bpm]; 95% CI: 1.9, 19.5; t27 = 2.49; p = 0.02). Estimated mean 10-week changes were 6.1 bpm (95% CI: −0.3, 12.5; t32 = 1.93; p = 0.06) for mirtazapine and −4.6 bpm (95% CI: −12.6, 3.4; t36 = −1.16; p = 0.25) for placebo. There were no statistically significant differences in 10-week changes in systolic or diastolic blood pressure between mirtazapine and placebo (systolic mean difference = −0.6 mmHg; 95% CI: −7.6, 6.3; t27 = −0.19; p = 0.85; diastolic mean difference=3.4 mmHg; 95% CI: −3.8, 10.6; t28 = 0.97; p = 0.34), and no statistically significant 10-week changes for either mirtazapine (systolic mean change = −2.3 mmHg; 95% CI: −7.1, 2.5; t33 = −0.96; p = 0.34; diastolic mean change = 1.9 mmHg; 95% CI: −2.6, 6.4; t31 = 0.85; p = 0.40) or placebo (systolic mean change = −1.6 mmHg; 95% CI: −7.8, 4.5; t35 = −0.54; p = 0.59; diastolic mean change = −1.6 mmHg; 95% CI: −7.6, 4.5; t31 = −0.52; p = 0.60).
Discussion
The results from this study do not provide independent evidence that mirtazapine reduces symptoms of anxiety in comparison with placebo in children and adolescents with ASD; however, based on the achievement of three out of four pre-specified indicators of efficacy, the study does support the implementation of a larger randomized controlled trial powered to provide conclusive evidence on the efficacy of mirtazapine for anxiety in this population.
Forty-seven percent of the subjects randomized to mirtazapine were considered treatment responders (“much improved” or “very much improved” on the CGI-I), which is higher than the 34.6% response rate observed in a retrospective study of mirtazapine in PDDs [20], and just shy of the 50% threshold established for one pre-specified indicator of efficacy.
With regard to treatment response, it should be noted that two out of the 10 participants who received placebo responded (20%), and the placebo group experienced a mean 3.2 point reduction in PARS score. A similar placebo response rate of 29% and a mean 3.1 point reduction in PARS score was observed in the double-blind, placebo-controlled trial of fluvoxamine for the treatment of children and adolescents with primary anxiety disorders conducted by the Research Units on Pediatric Psychopharmacology Anxiety Study Group [33]. The current pilot trial was powered to detect an effect size of 1.1, which is smaller than the pooled effect size (1.38) for the treatment of anxiety with SSRIs in two placebo-controlled studies in the broader population of children and adolescents treated with sertraline or fluvoxamine but substantially larger than the pooled effect size for both SSRIs (0.36) and the combined results for all anti-anxiety medications (0.38) including pregabalin, hydroxyzine, venlafaxine, benzodiazepines, SSRIs, buspirone, and complementary/alternative medication in adults [34].
Mirtazapine was observed to be both safe and well tolerated among children and adolescents with ASD. There were neither serious adverse events nor occurrences of suicidality reported. No adverse effects were statistically significantly more likely to occur in participants treated with mirtazapine than with placebo. The most common adverse effect was sedation/drowsiness, reported by 60% of participants in each group. Appetite increase, the second most common effect, was reported more frequently by participants taking mirtazapine (50%) compared with 20% of participants taking placebo. Weight gain was also observed in the mirtazapine group. Participants in the mirtazapine group experienced an increase in BMI of 0.7 kg/m2 over the 10-week treatment period. While the difference in 10-week change in BMI was not statistically significantly different between mirtazapine and placebo, increased BMI was not observed in the placebo group. Weight gain associated with the use of mirtazapine in youth with ASD requires further study. Although there was a statistically significant increase in heart rate in the mirtazapine group compared to the placebo group, the increase of six bpm is unlikely to be clinically significant. Nineteen out of 20 participants randomized to mirtazapine remained in the study for the entire 10-week treatment period, highlighting the tolerability of mirtazapine. The five percent discontinuation rate is lower than discontinuation rates (range, 16.7–23.5%) reported in retrospective and open-label trials of SSRIs for anxiety in children (ages 4–15 years) with PDDs [8, 9].
Strengths of this study include that it is the first randomized, double-blind, placebo-controlled trial of a medication for the primary treatment of anxiety associated with ASD. Second, the study retention rate was very high allowing for the collection of a maximal amount of data on safety, tolerability, and potential efficacy. Third, all of the subjects received thorough diagnostic assessments, including a comprehensive clinical interview completed by a board-certified child and adolescent psychiatrist experienced in providing clinical care to youth with ASD in conjunction with the use of standardized diagnostic instruments and rating scales. Finally, all participants, guardians, raters, and investigators remained blind to the study assignment and the placebo capsules were identical in taste and appearance to the mirtazapine capsules.
The main limitations of this study are the small sample size, the heterogeneity of the sample, and the overall lack of diversity in the sample. The study included both children and adolescents, as well as participants with a broad range of cognitive abilities. Additionally, the exclusionary criteria of several other psychiatric disorders may make the results less generalizable to clinical populations. Results for secondary outcome measures (all clinical measures other than the PARS and CGI-I) should be interpreted in light of the absence of multiple testing correction for outcomes not designated as primary. Finally, because the duration of the trial was 10 weeks long, we are unable to comment on the maintenance of response beyond this point and the potential worsening of adverse events or emergence of new ones.
In conclusion, the results of this study show that mirtazapine is safe and well-tolerated and may have potential efficacy for treating anxiety in youth with ASD. A larger randomized controlled trial powered to provide more definitive evidence of the safety, tolerability and efficacy of mirtazapine for the treatment of anxiety in children and adolescents with ASD is needed. Given the results of this pilot study, we estimate the potential effect size of mirtazapine compared to placebo, a 1.8 point or 0.6 pre-treatment standard deviation difference in PARS scores, indicates the need for 216 or more equally allocated enrollees completing ten weeks of treatment to thoroughly evaluate efficacy in the future. These results also support the choice of the PARS as a primary outcome measure for future trials targeting anxiety in this population. Finally, future clinical investigations of mirtazapine for youth with ASD should be designed assuming a substantial placebo effect.
Author contributions
Christopher J. McDougle. Substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Robyn P. Thom. Substantial contributions to the conception or design of the work; or the acquisition, analysis or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Caitlin T. Ravichandran. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting the work or revising it critically for important intellectual content. Final approval of the version to be published. Michelle L. Palumbo. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Laura C. Politte. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Jennifer E. Mullett. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Christopher J. Keary. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Craig A. Erickson. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Kimberly A. Stigler. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. Lauren Mathieu-Frasier. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Final approval of the version to be published. David J. Posey. Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work. Drafting of the work or revising it critically for important intellectual content. Final approval of the version to be published. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding
This work was funded by Autism Speaks.
Competing interests
Dr. McDougle is a consultant to Precidiag, Receptor Life Sciences, and Sage Therapeutics, and receives royalties from Oxford University Press and Springer Publishing. Dr. Thom receives research support from Precidiag. Dr. Palumbo receives research support from Otsuka Pharmaceuticals. Dr. Keary serves on the advisory board and receives research support from Ovid Therapeutics. Dr. Erickson is a consultant to Autifony, Stalicla, Scitoto Bioscience, Impel, and Confluence Pharmaceuticals. He is an inventor on patents describing methods of treatment in neurodevelopmental disorders held by the Cincinnati Children’s Hospital Research Foundation. Drs. Ravichandran and Politte, Ms. Mullett, Dr. Stigler, Ms. Mathieu-Frasier, and Dr. Posey have no disclosures or conflicts of interest to report.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.American Psychiatric Association: Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- 2.Kerns CM, Winder-Patel B, Iosif AM, Nordahl CW, Heath B, Solomon M, et al. Clinically significant anxiety in children with autism spectrum disorder and varied intellectual functioning. J Clin Child Adolesc Psychol. 2020. 10.1080/15374416.2019.1703712. [DOI] [PMC free article] [PubMed]
- 3.Kirsch AC, Huebner ARS, Mehta SQ, Howie FR, Weaver AL, Myers SM, et al. Association of comorbid mood and anxiety disorders with autism spectrum disorder. JAMA Pediatr. 2020;174:63–70. doi: 10.1001/jamapediatrics.2019.4368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Steensel FJA, Bögels SM, Perrin S. Anxiety disorders in children and adolescents with autistic spectrum disorders: a meta-analysis. Clin Child Fam Psychol Rev. 2011;14:302–17. doi: 10.1007/s10567-011-0097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Steensel FJA, Bögels SM, Dirksen CD. Anxiety and quality of life: clinically anxious children with and without autism spectrum disorders compared. J Clin Child Adolesc Psychol. 2012;41:731–8. doi: 10.1080/15374416.2012.698725. [DOI] [PubMed] [Google Scholar]
- 6.Delli CKS, Polychronopoulou SA, Kolaitis GA, Antoniou, SG A- Review of interventions for the management of anxiety symptoms in children with ASD. Neurosci Biobehav Rev. 2018;95:449–63. doi: 10.1016/j.neubiorev.2018.10.023. [DOI] [PubMed] [Google Scholar]
- 7.Steingard RJ, Zimnitzky B, DeMaso DR, Bauman ML, Bucci JP. Sertraline treatment of transition-associated anxiety and agitation in children with autistic disorder. J Child Adolesc Psychopharmacol. 1997;7:9–15. doi: 10.1089/cap.1997.7.9. [DOI] [PubMed] [Google Scholar]
- 8.Couturier JL, Nicolson R. A retrospective assessment of citalopram in children and adolescents with pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2002;12:243–8. doi: 10.1089/104454602760386932. [DOI] [PubMed] [Google Scholar]
- 9.Martin A, Koenig K, Anderson GM, Scahill L. Low-dose fluvoxamine treatment of children and adolescents with pervasive developmental disorders: a prospective, open-label study. J Autism Dev Disord. 2003;33:77–85. doi: 10.1023/A:1022234605695. [DOI] [PubMed] [Google Scholar]
- 10.Herscu P, Handen BL, Arnold LE, Snape MF, Bregman JD, Ginsberg L, et al. The SOFIA Study: Negative multi-center study of low dose fluoxetine on repetitive behaviors in children and adolescents with autistic disorder. J Autism Dev Disord. 2020;50:3233–44. doi: 10.1007/s10803-019-04120-y. [DOI] [PubMed] [Google Scholar]
- 11.Ceranoglu TA, Wozniak J, Fried R, Galdo M, Hoskova B, Fong MD, et al. A retrospective chart review of buspirone for the treatment of anxiety in psychiatrically referred youth with high-functioning autism spectrum disorder. J Child Adolesc Psychopharmacol. 2019;29:28–33. doi: 10.1089/cap.2018.0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Buitelaar JK, van der Gaag RJ, van der Hoeven J. Buspirone in the management of anxiety and irritability in children with pervasive developmental disorders: results of an open-label study. J Clin Psychiatry. 1998;59:56–59. doi: 10.4088/JCP.v59n0203. [DOI] [PubMed] [Google Scholar]
- 13.Chugani DC, Chugani HT, Wiznitzer M, Parikh S, Evans PA, Hansen RL, et al. Efficacy of low-dose buspirone for restricted and repetitive behavior in young children with autism spectrum disorder: A randomized trial. J Pediatr. 2016;170:45–53.e1-4. doi: 10.1016/j.jpeds.2015.11.033. [DOI] [PubMed] [Google Scholar]
- 14.Schatzberg A, DeBattista C, Manual of clinical psychopharmacology. 8th ed. Arlington, VA: American Psychiatric Publishing, Inc.; 2015.
- 15.de Boer T. The pharmacologic profile of mirtazapine. J Clin Psychiatry. 1996;57:19–25. [PubMed] [Google Scholar]
- 16.Gambi F, De Berardis D, Campanella D, Carano A, Sepede G, Salini G, et al. Mirtazapine treatment of generalized anxiety disorder: A fixed dose, open label study. J Psychopharmacol. 2005;19:483–7. doi: 10.1177/0269881105056527. [DOI] [PubMed] [Google Scholar]
- 17.Mrakotsky C, Masek B, Biederman J, Raches D, Hsin O, Forbes P, et al. Prospective open-label pilot trial of mirtazapine in children and adolescents with social phobia. J Anxiety Disord. 2008;22:88–97. doi: 10.1016/j.janxdis.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 18.Thompson C. Mirtazapine versus selective serotonin reuptake inhibitors. J Clin Psychiatry. 1999;60:18–22. [PubMed] [Google Scholar]
- 19.Owen J, Nemeroff C. New antidepressants and the cytochrome P450 system: focus on venlafaxine, nefazodone, and mirtazapine. Depress Anxiety. 1998;7:24–32. doi: 10.1002/(SICI)1520-6394(1998)7:1+<24::AID-DA7>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- 20.Posey DJ, Guenin KD, Kohn AE, Swiezy NB, McDougle CJ. A naturalistic open-label study of mirtazapine in autistic and other pervasive developmental disorders. J Child Adolesc Psychopharmacol. 2001;11:267–77. doi: 10.1089/10445460152595586. [DOI] [PubMed] [Google Scholar]
- 21.Janzen HL, Obrzut JE, Marusiak CW. Test Review: Roid, G. H. (2003). Stanford-Binet Intelligence Scales, Fifth Edition (SB:V). Itasca, IL: Riverside Publishing. Can J Sch Psychol. 2004;19:235–44. doi: 10.1177/082957350401900113. [DOI] [Google Scholar]
- 22.Lord C, Rutter M, Le Couteur A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J Autism Dev Disord. 1994;24:659–85. doi: 10.1007/BF02172145. [DOI] [PubMed] [Google Scholar]
- 23.Anxiety Disorders Interview Schedule (ADIS-IV) Child/Parent Version Combination Specimen Set - Wendy K. Silverman; Anne Marie Albano - Oxford University Press. https://global.oup.com/academic/product/anxiety-disorders-interview-schedule-adis-iv-childparent-version-combination-specimen-set-9780195186741?cc=us&lang=en&. Accessed 23 June 2020.
- 24.PPVT-4 Peabody Picture Vocabulary Test 4th Edition. https://www.pearsonassessments.com/store/usassessments/en/Store/Professional-Assessments/Academic-Learning/Brief/Peabody-Picture-Vocabulary-Test-%7C-Fourth-Edition/p/100000501.html. Accessed 23 June 2020.
- 25.Vineland Adaptive Behavior Scales – Second Edition (VinelandTM-II) - TSLAT. http://www.txautism.net/evaluations/vineland-adaptive-behavior-scales-second-edition-vinelandtm-ii. Accessed 23 June 2020.
- 26.CGI - Clinical Global Impressions scale. https://eprovide.mapi-trust.org/instruments/clinical-global-impressions-scale. Accessed 23 June 2020.
- 27.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): A replication study. J Am Acad Child Adolesc Psychiatry. 1999;38:1230–6. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Sukhodolsky DG, Scahill L, Gadow KD, Arnold LE, Aman MG, McDougle CJ, et al. Parent-rated anxiety symptoms in children with pervasive developmental disorders: Frequency and association with core autism symptoms and cognitive functioning. J Abnorm Child Psychol. 2008;36:117–28. doi: 10.1007/s10802-007-9165-9. [DOI] [PubMed] [Google Scholar]
- 29.Aman MG, Singh NN, Stewart AW, Field CJ. The aberrant behavior checklist: a behavior rating scale for the assessment of treatment effects. Am J Ment Defic. 1985;89:485–91. [PubMed] [Google Scholar]
- 30.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23:1043–51. doi: 10.1093/sleep/23.8.1d. [DOI] [PubMed] [Google Scholar]
- 31.Wagner A, Lecavalier L, Arnold LE, Aman MG, Scahill L, Stigler KA, et al. Developmental disabilities modification of the children’s global assessment scale. Biol Psychiatry. 2007;61:504–11. doi: 10.1016/j.biopsych.2007.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Borm GF, Fransen J, Lemmens WAJG A simple sample size formula for analysis of covariance in randomized clinical trials. 10.1016/j.jclinepi.2007.02.006. [DOI] [PubMed]
- 33.Pine DS, Walkup JT, Labellarte MJ, Riddle MA, Greenhill L, Klein R, et al. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N. Engl J Med. 2001;344:1279–85. doi: 10.1056/NEJM200104263441703. [DOI] [PubMed] [Google Scholar]
- 34.Hidalgo RB, Tupler LA, Davidson JRT. An effect-size analysis of pharmacologic treatments for generalized anxiety disorder. J Psychopharmacol. 2007;21:864–72. doi: 10.1177/0269881107076996. [DOI] [PubMed] [Google Scholar]