Abstract
Aims
The aim of this study was to review the current evidence surrounding curve type and morphology on curve progression risk in adolescent idiopathic scoliosis (AIS).
Methods
A comprehensive search was conducted by two independent reviewers on PubMed, Embase, Medline, and Web of Science to obtain all published information on morphological predictors of AIS progression. Search items included ‘adolescent idiopathic scoliosis’, ‘progression’, and ‘imaging’. The inclusion and exclusion criteria were carefully defined. Risk of bias of studies was assessed with the Quality in Prognostic Studies tool, and level of evidence for each predictor was rated with the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach. In all, 6,286 publications were identified with 3,598 being subjected to secondary scrutiny. Ultimately, 26 publications (25 datasets) were included in this review.
Results
For unbraced patients, high and moderate evidence was found for Cobb angle and curve type as predictors, respectively. Initial Cobb angle > 25° and thoracic curves were predictive of curve progression. For braced patients, flexibility < 28% and limited in-brace correction were factors predictive of progression with high and moderate evidence, respectively. Thoracic curves, high apical vertebral rotation, large rib vertebra angle difference, small rib vertebra angle on the convex side, and low pelvic tilt had weak evidence as predictors of curve progression.
Conclusion
For curve progression, strong and consistent evidence is found for Cobb angle, curve type, flexibility, and correction rate. Cobb angle > 25° and flexibility < 28% are found to be important thresholds to guide clinical prognostication. Despite the low evidence, apical vertebral rotation, rib morphology, and pelvic tilt may be promising factors.
Cite this article: Bone Joint J 2022;104-B(4):424–432.
Keywords: Adolescent idiopathic scoliosis, Curve progression, Morphology, Bracing, Flexibility, bone age, Cobb angle, Rotation, Correction, Systematic review, thoracic kyphosis, Rib, vertebrae, Prognostic Studies, pelvic tilt, Medline, univariate analysis, randomized controlled trials
Introduction
Accurate forecasting of curve progression in adolescent idiopathic scoliosis (AIS), using readily available radiological predictors, is challenging due to the multifactorial nature and variable progression of AIS curves. 1 The prognostication of curve progression requires identification of threshold levels of relevant factors and corresponding effect sizes for each predictor to enable clinical risk classification. 2 This allows appropriate follow-up for patients at higher risk, and explanation of the likely outcome.
Under the current International Society on Scoliosis Orthopaedic and Rehabilitation Treatment (SOSORT) treatment guidelines, 3 initially bracing is advised when curves exceed 20° with risk of progression, while patients with curves less than 15° are generally put under observation. Conservative treatment in this review therefore refers to bracing and observation. While bracing is known to alter the natural history of AIS, 4-6 it is important that we evaluate predictors for progression separately for braced and unbraced patients.
A previous systematic review by Van den Bogaart et al 7 summarized evidence for predictors of curve progression in braced patients from the literature up to October 2017. It was concluded strong evidence existed for initial in-brace correction rate predicting brace success, while moderate evidence was present that curve magnitude and curve type were not associated with brace outcomes. The study found inconclusive evidence for most predictors. However, this study used the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) approach according to the 2009 Updated Method Guideline for Systematic Review of the Cochrane Back Review Group, 8 which used a strict criterion to determine the level of evidence for each outcome, in contrast to allowing flexibility in judgement for grading of evidence, as recommended in the newly updated guidelines. 9 Another systematic review with meta-analysis reviewed evidence up to August 2014, 10 and summarized predictors of curve progression in patients under observation, treated with bracing, and postoperative follow-up; pooled estimates showed low to very low evidence to all identified clinical, genetic, radiological, and demographic predictors. However, no clinical thresholds or recommendations were provided.
In view of the recent popularization of 3D low-dose stereoradiograph reconstruction models and the increasing attention to the 3D morphology of AIS, more prognostic studies have been conducted using 3D reconstruction models to obtain more accurate morphological factors. 11,12 New concepts to describe the scoliotic curve, e.g. 3D Cobb angle and plane of maximum curvature, 13,14 have been introduced and are believed to be superior to plain radiological parameters, which are subject to projection bias. 15 Accordingly, it would be appropriate to have an updated evaluation of the current evidence of radiological morphological predictors of scoliosis curve progression.
Methods
Literature search and selection criteria
The literature search and reporting of results in this study were conducted in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines. 16 A literature search was conducted using Embase, Medline, PubMed, and Web of Science to retrieve articles regarding radiological predictors of curve progression in patients with AIS. The search items included ‘adolescent idiopathic scoliosis’, ‘progression’, and ‘imaging’. Synonyms and controlled vocabulary under each search item were included in the search to ensure exhaustive retrieval of data, with suitable modification for each database according to differences in controlled vocabulary and indexation. The detailed search items are included in Supplementary Material. All articles published on or before 31 December 2020 were retrieved and screened. The search and screening processes were conducted by two independent investigators (LPKW, PWHC) and the discrepancies on the final decision of inclusion was settled through discussion. The inclusion and exclusion criteria are detailed in Table I. Both secondary analyses from randomized controlled trials (RCTs) and observational studies were included, since prognostic research is often observational in nature.
Table I.
Inclusion and exclusion criteria.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Patients with adolescent idiopathic scoliosis | Patients who underwent surgery |
| Patients who underwent bracing as treatment, or put under observation with or without exercise | Studies including patients with other types of scoliosis, e.g. degenerative, congenital |
| Studied one or more radiological morphological predictors | Specialized CT, MRI, and electromyography predictors not routinely assessed, e.g. electromyography, neurological factors |
| Studies with a clearly defined outcome of progression | Studies reporting neither p-values nor odds ratios with confidence intervals |
| Longitudinal studies in English | Model development studies without identification of individual predictors |
| Case series, case reports, conference summaries, cross-sectional studies, unpublished literature, commentaries, and reviews |
Data extraction
Predictive factors from each study were extracted and similar ones were grouped for analysis. Other information regarding the study design, sample size, selection criteria of subjects, predictors found, risk of bias, phase of inquiry, and level of evidence were extracted and are listed in Supplementary Table i.
Primary and secondary outcomes
The primary outcomes of this review were the effects of curve magnitude and curve type, brace correction, flexibility, sagittal alignment, and rotation on curve progression. The secondary outcome was identifying different factors associated with curve progression in braced and unbraced patients.
Search results
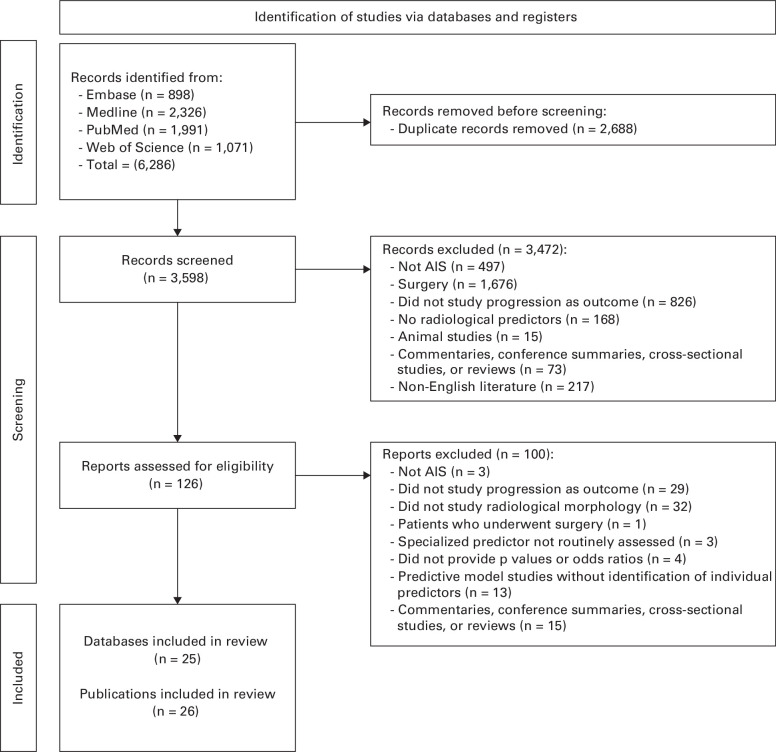
The search results are detailed in the PRISMA flow diagram (Figure 1). The search was conducted on 22 March 2021. A total of 6,286 articles were found; 3,598 articles remained after eliminating duplicates, and were screened by their abstracts. Of these, 126 articles were assessed for eligibility by full-text screening and 26 publications from 25 datasets were finally selected for inclusion. 2,11,12,17-39
Fig. 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses flow diagram. AIS, adolescent idiopathic scoliosis.
Among the 26 publications included, six were classified as confirmatory studies, and 20 were classified as exploratory studies. One dataset included was published as an exploratory and confirmatory investigation. 18,19 In terms of the population, 15 were done on braced patients, six were done on unbraced patients, two were done on a mixed sample of braced and unbraced patients, and three investigated curve progression beyond skeletal maturity. In terms of study design, five were prospective cohort studies, 19 were retrospective cohort studies, one was a retrospective review of data from a RCT, and one was an ambidirectional cohort study. The mean age of participants across studies ranged from 10.4 to 14.7 years and the length of follow-up ranged from 20.7 months to 24.9 years. Sample sizes of studies ranged from 30 to 2,380 patients.
Risk of bias
The risk of bias of these reports was assessed using the six domains of the Quality in Prognostic Studies (QUIPS) tool 40 by the two independent reviewers, and consensus was reached after discussion. For retrospective studies, bias due to attrition is not applicable and therefore not assessed. The QUIPS risk of bias for these studies is detailed in Supplementary Table ii.
Grading of evidence
Quality of evidence for each predictor identified was assessed using the GRADE approach 41 by two independent reviewers (LPKW, PWHC) where the quality of evidence for each predictor was given a rating of ‘high’, ‘moderate’, ‘low’, or ‘very low’. Predictors with evidence mainly coming from confirmatory studies were initially assigned as having a high level of evidence, while those with evidence mainly coming from exploratory studies were assigned a moderate level of evidence. 42 Downgrading of quality of evidence rating was done with reference to five domains: ‘risk of bias’, ‘inconsistency’, ‘imprecision’, ‘indirectness’, and ‘publication bias’, while upgrading of quality of evidence was based on large effect size, dose response relationships, and when all residual confounding was shown to reduce the demonstrated effect. 43 The detailed evidence available for each predictor and the GRADE quality of evidence rating is presented in Supplementary Tables iii and iv. In short, initial Cobb angle, thoracic curve type, flexibility, and in-brace correction were considered as predictors with sufficient evidence, and rib morphology, apical vertebral rotation (AVR), and pelvic tilt (PT) were considered to have less sufficient evidence. For predictors that yielded inconclusive results, the details are summarized in Supplementary Table v.
Results
Initial Cobb angle
There is a high level of evidence that Cobb angle is significantly predictive of curve progression in unbraced patients. Five out of six studies identified the predictive ability of initial curve size. Tan et al 35 found that Cobb angle > 25° was significantly predictive of progression in multivariable regression. Similar results were replicated by Lee et al, 2 who found that patients with Cobb angle > 25.8° had a hazard ratio of 8.8 compared to patients with Cobb angle < 18.4°. Three other studies also showed a relationship between initial Cobb angle and progression, 20,25,38 with Dolan et al 20 identifying an odds ratio (OR) of 1.28 for initial Cobb angle, adjusted for curve type and simplified skeletal maturity stages (SMS). Results were validated in an externally validated model. Dolan et al 20 found 15°, 25°, and 33° to be Cobb angle cut-offs for high risk of progression in thoracic curves with SMS of 1 to 2, 3, and 4+ respectively. The cut-offs became 21°, 30°, and 39°, respectively for lumbar curves. Nault et al 28 is the only study that found no association between 2D and 3D Cobb angle with curve progression. There is limited evidence for initial Cobb angle as a predictor of curve progression in braced patients. Three studies found affirmative evidence for the predictive value of Cobb angle. Cheung and Cheung 18 and Zhang et al 39 both showed that initial Cobb angle predicts progression ≥ 5° adjusted for maturity and other predictors. Zhang et al 39 found that a Cobb angle cut-off of 35° gave an OR of 13.7 to progress more than 5°. Karol 22 reported that initial Cobb angle was associated with progression to the surgical threshold of 50° in univariate analysis, but failed to identify an association with clinically relevant progression ≥ 6°. Six studies found no association between Cobb angle and outcome of progression. However, five of these studied Cobb angle in univariate analysis only, 17,21,23,26,34 without accounting for its interaction with age and maturity. Only Ohrt-Nissen et al 31 showed that initial Cobb angle was not predictive of curve progression after adjusting for age and menarchal status.
Curve type
There is overall moderate evidence that the extent of the thoracic curve predicts progression in unbraced patients. Two studies on unbraced patients identified curve type as a predictor of curve progression. 20,25 Dolan et al 20 found that the presence of a thoracic apex gave an OR of 4.09 (95% confidence interval (CI) 0.88 to 18.96) for curve progression to 45° at skeletal maturity, after adjusting for Cobb angle and simplified SMS. The result did not reach significance, but the effect size was large, and the model was shown to have great predictive value in both an internal and external validation cohort. The Cobb angle cut-offs for high risk of progression differed considerably between thoracic and lumbar curves. Lara et al 25 also found that curve type in African-American patients with AIS significantly predicted incidence of surgery in a multivariable analysis. There is limited evidence that thoracic curves predict progression in braced patients. Among the six studies on this predictor, Thompson et al 36 offered the most evidence. They found that mLenke curve type had some ability in predicting curve outcome, 44 but the effect was not statistically significant (p = 0.087). After controlling for compliance, main thoracic curves were found to predict curve progression to 50° and a higher rate of surgery (p = 0.024). This trend remained after adjusting for Risser stage, but did not reach statistical significance. This result is supported by Ohrt-Nissen et al 31 and Cheung and Cheung. 18 Cheung and Cheung 18 found that thoracic curves had an unadjusted and adjusted OR of 3.32 and 1.635, respectively, compared to lumbar curves. However, Kwan et al 12 found that thoracic curve type did not predict curve progression > 5° in a regression model. Katz and Durrani 23 also found no difference in risk of progression between different curve types, and Zhang et al 39 dropped curve type as a predictor in a stepwise multivariable logistic regression.
Flexibility
There is a high level of evidence that greater flexibility predicts less risk of progression. Three studies with four reports showed positive evidence on flexibility predicting curve progression. Cheung and Cheung, 18 Cheung et al, 19 and Kwan et al 12 found adjusted ORs of 0.958, 0.958, and 0.962, respectively, for risk of curve progression ≥ 5° for every 1% increase in supine flexibility in braced patients. Ohrt-Nissen et al 31 found an OR of 0.95 for every 1% increase in supine side-bending flexibility, adjusted for commonly assessed predictors including Cobb angle, age, and menarchal status. Among these studies, only Cheung and Cheung 18 and Cheung et al 19 tested for prognostic accuracy for flexibility and concluded that flexibility less than 28% in supine radiographs was predictive of poor brace outcome, and this had a sensitivity of 67.9%, a specificity of 64.5%, and an area under curve of 0.720 for outcome prediction.
In-brace correction
There is overall moderate evidence for in-brace correction as a predictor of progression. Six studies with seven reports investigated in-brace correction as a predictive factor. Cheung and Cheung 18 and Cheung et al 19 found correction rate to predict significant progression by the 5° margin with an adjusted OR of 0.979 for every 1% increase in correction rate. A similar effect was replicated in Kwan et al, 12 which found an OR of 0.966 adjusted for a different set of predictors. Katz and Durrani 23 and Ohrt-Nissen et al 31 both identified predictive value of in-brace correction in univariate analysis. Pasha 32 found that in-brace thoracic Cobb angle was predictive of curve progression by least absolute shrinkage and selection operator (LASSO) regression. Karol 22 is the only study that found no significant predictive value of in-brace correction in predicting curve progression ≥ 5°. No studies so far have assessed the performance of in-brace correction cut-offs in differentiating progressed and stable patients.
Rib vertebra angle
There is very limited evidence for the predictive ability for rib morphology in braced patients. Four reports have studied the predictive value of factors related to the rib vertebra angle difference (Mehta angle) (Figure 2), originally proposed by Mehta 45 in the prognostication of infantile idiopathic scoliosis, in AIS patients who received bracing as treatment. Sun et al 34 found that rib vertebra angle difference (RVAD) ≥ 20° and rib vertebra angle on the convex side (RVACx) ≤ 68° predicted curve progression. Pasha 32 found that a combination of an RVACx greater than 60° and higher thoracic apical vertebral rotation was associated with curve progression. Katz and Durrani 23 and Modi et al 27 also found that the in-brace correction and change in RVACx was associated with progression, but did not adjust for other covariates. Due to the absence of studies with multivariable analysis, only a rating of very low level of evidence can be given.
Fig. 2.
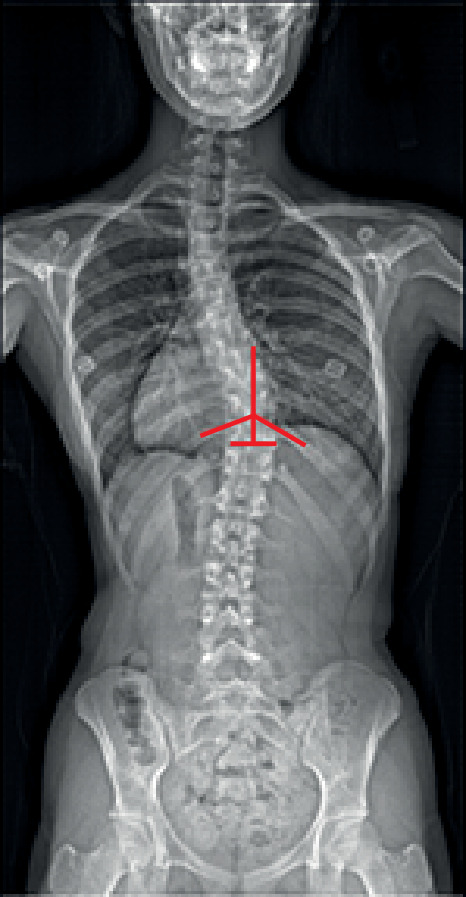
The rib-vertebral angle (RVA) is formed between the longitudinal axis of the apical thoracic vertebra and corresponding rib on the convex and concave sides of the curve. A perpendicular line is drawn at the midpoint of the lower endplate of the apical vertebra. Another line is drawn from the midpoint of the head to the midpoint of the neck of the rib. The rib line is extended medially to intersect with the perpendicular line to make the RVA.
AVR
There is low evidence for AVR as a predictor in braced patients. Four studies shed light on AVR as a predictor in braced AIS patients. Kwan et al 12 conducted a prospective study with 3D reconstruction and found pre-brace AVR (OR 1.063) and AVR reduction velocity at one year (OR 1.19) to be predictive of progression > 5°. Zhang et al 39 and Ohrt-Nissen et al 31 both looked at Nash Moe rotation, 46 and found that it predicted progression. Upadhyay et al 37 found that a reduction of both the Perdriolle rotation and Cobb angle during bracing predicted brace success, 47 while an increase in both predicted failure.
Sagittal alignment: PT
Evidence is very low for PT as a predictor of curve progression in braced patients. Both Catanzano et al 17 and Guo et al 21 found PT to be predictive of curve progression in braced patients. Catanzano et al 17 found that PT > 8.5° significantly predicted good brace outcome (OR 0.7), adjusted for Cobb angle and Risser stage. Guo et al 21 also found PT to be predictive of curve progression in a multivariable analysis adjusting for Cobb angle and Risser stage (p < 0.01).
Predictors with inconclusive evidence
No conclusive evidence was found for predictors including upper and lower intervertebral rotation, torsion, AVR (in unbraced patients), sacral slope, pelvic incidence, T1 and T9 spinopelvic inclination, thoracic kyphosis, lumbar lordosis, wedging, apical vertebral translation, lumbopelvic angle, and several predictors for progression beyond skeletal maturity. There is a paucity of studies investigating these predictors and a lack of multivariable analyses from which to make conclusions. The evidence for these predictors is detailed in Supplementary Table v. While these studies were mostly exploratory in nature, some did offer novel insights on the potential pathomechanism and might include information on some promising predictors. The value for these predictors will be discussed below.
Discussion
In this review, we found that Cobb angle > 25°, thoracic curves, flexibility < 28%, and low in-brace correction are predictive of curve progression with moderate to high evidence. High AVR, high RVAD, low RVACx, and low PT are predictive of progression, but only low to very low evidence is found for these predictors.
Initial Cobb angle is the most assessed radiological predictor in the current clinical evaluation of patients with AIS. Despite the difference in outcome measured by the studies on Cobb angle, several studies agreed that a Cobb angle of 25° is an important cut-off that predicts drastically different potential for progression in patients with Risser stage 2 or below. 2,20,35 Dolan et al 20 looked at the prognostic value of Cobb angle in rather early Simplified Skeletal Maturity Scoring stages, which corresponds to the adolescent growth spurt. 48 Therefore, we can be more confident about initial Cobb angle as a clinically useful predictor for progression in the period of the highest risk. 48 There is sufficient and consistent evidence for Cobb angle as a predictor in unbraced patients. It is well supported by a few confirmatory studies with respectable sample sizes. Cobb angle is also shown to be a clinically useful predictor, as consistent cut-off values have been found, and these cut-offs produce large effect sizes that clearly distinguish stable and progressing patients. It is unlikely that high-quality evidence from prospective studies investigating the entire course of the adolescent growth phase of unbraced patients will emerge due to the proven effectiveness of bracing as a treatment to halt curve progression. 4,5 Therefore, the evidence available may already represent the limit in following the natural history of AIS.
For braced patients, the strongest evidence for Cobb angle as a predictor comes from the large-scale study by Cheung and Cheung, 18 which clearly adjusted for the interaction between maturity and Cobb angle. The other two studies offering positive evidence both have their own flaws. Zhang et al 39 did not provide the criteria for inclusion of variables in the regression model, and baseline characteristics of the cohort are lacking. Karol’s study 22 only arrived at a weaker conclusion that initial curve size predicted progression to 50°, but failed to reach statistical significance in showing that curve size predicted progression by 6°. Most of the studies that obtained negative results did not adjust for maturity or age, 17,21,23,26,34 which are known to be important factors interacting with Cobb angle. Of note, after adjusting for maturity and brace-specific factors such as correction rate, the effect of Cobb angle is much smaller compared to that in unbraced patients. This points towards the effectiveness of bracing in altering the natural history of AIS progression, and that other brace-specific factors may play a greater role in predicting brace outcomes in AIS patients. It is also prudent to note that the Cobb angle at brace weaning is another risk factor of progression after maturity. 49-52 Patients with Cobb angle reaching 40° is a well-established cut-off for adulthood progression. 4,53 Similarly, those with this benchmark at the time of brace-weaning also have the potential for post-maturity progression. This still applies with standardized growth parameters and bone age assessments determining growth cessation. 54-57 In these patients, the prognosis is worse and patients should be counselled appropriately regarding the probable success of bracing. 58,59 Parallel to this, patients with a Cobb angle of 40° at initial presentation may be forewarned of brace failure despite satisfactory compliance. 19
Conflicting evidence arises for the predictive value of curve type in braced patients. Strong evidence comes from the study by Thompson et al, 36 which was confirmatory in nature and well controlled for other predictors. A trend was found when curve types were further classified by the mLenke system, which increases our confidence regarding curve type as a predictor. However, many studies contradict this view. 12,23,39 Due to the heterogeneity in the outcomes and methods of analysis, a pooled estimate cannot be performed to evaluate the true effect size. With some caution, regarding conflicting evidence, we conclude that thoracic curves do predict progression based on the strong evidence from Thompson et al 36 and the large study by Cheung and Cheung. 18 Further classification of curve types may offer additional predictive information, but current evidence shows that the effect size may be too small to detect.
For unbraced patients, although evidence for curve type only comes from two studies, these have consistent results; Dolan et al 20 developed an externally validated model and discovered a large effect size for curve type in predicting curve progression to 45°. The Cobb angle cut-offs for high-risk patients were also much lower in thoracic curves than in lumbar curves. Lara et al 25 also identified curve type as a significant predictor for incidence of surgery.
All three studies on flexibility and in-brace correction found flexibility to be significantly predictive of a lower risk of progression. 12,18,31 These studies all adjusted for commonly assessed clinical predictors, selected either a priori or according to results from univariate analysis, and consistently found an OR of approximately 0.96 per 1% increase in flexibility. Among these studies, only Cheung and Cheung 18 gave a cut-off for flexibility at 28% as a predictor of outcome. We believe that this cut-off value is credible due to the large sample size of the study and receiver operating characteristic curve analysis providing acceptable area under curve, sensitivity, and specificity values. There remains a need for more prospective and external validation studies to obtain cut-off estimates for flexibility to guide clinical use. Nevertheless, this is a useful initial measure to prognosticate the likelihood of success from bracing.
Similarly, most studies investigating in-brace correction found significance in its predictive value. These studies, which demonstrated positive findings, were of low or moderate risk of bias and some of them, including Cheung et al 19 and Kwan et al, 12 showed the independent predictive value of in-brace correction adjusted for a number of different factors. However, no cut-off values for correction rate were found. Since it has also been shown in the literature that in-brace correction is closely correlated to supine flexibility, 60,61 correction rate cut-offs should be discussed and interpreted with reference to the flexibility of the spine. This may also contribute to underestimation of the risk of curve progression. 62 However, no studies have investigated whether correction matching supine flexibility or correction beyond flexibility would produce a better result. Until further evidence arises, obtaining the highest correction rate within the patients’ tolerance should produce the best brace outcome.
Concerning rib morphology, all four studies showed that the RVAD and RVACx of the curve are significantly predictive of curve progression in univariate analysis. However, these studies generally had a high or moderate risk of bias due to poor reporting of the characteristics of the cohort, and insufficient control for existing prognostic factors. Rib morphology might be a promising prognostic factor, but it could not be shown that RVAD and RVACx were independent predictors of curve progression without proper adjustment for other factors. Also, the true underlying anatomical or physiological significance represented by RVAD and RVACx on coronal radiographs is unclear. Pasha 32 found that a RVACx of smaller than 60° in combination with a greater apical axial rotation was selected as a significant predictor of curve progression by LASSO regression. Pasha 32 explained this by pointing out that a drooping rib cage experiences smaller derotation force by the brace, and therefore results in poor correction of the deformity. The underlying anatomical components that constitute the RVAD appearance on coronal radiographs lack concensus. Foley et al 63,64 looked at infantile idiopathic scoliosis and concluded RVAD reflected a true rib-vertebral junctional deformity, while Brink et al 65 looked at AIS patients and concluded that RVAD simply represented greater apical rotation and sagittal wedging of vertebrae. Further studies should be done with 3D models to understand the underlying structural information represented by RVAD before any further reliance can be placed on it.
There is a paucity of evidence for 3D and rotational predictors including torsion, angle of plane of maximal curvature, and intervertebral rotation at the upper and lower ends of the curve in unbraced AIS patients. Only Nault et al 28 and Courvoisier et al 11 provided evidence on this subject, but both were limited by small sample sizes and lacked adjustment for most other commonly assessed predictors. Additionally, Nault et al 28 studied a mixed cohort of braced and unbraced patients and did not provide separate analysis for the two groups. Courvoisier et al 11 have revealed some interesting associations between a number of 3D rotational factors by unsupervised clustering methods, and have shown that four rotation-related factors, namely torsion, AVR, and intervertebral rotation at the upper and lower ends of the curve, could individually predict curve progression independent of the initial curve size. It is possible that the global rotational deformity of the spine may predict curve progression. It is important to note that axial deformity was found to be independent of coronal curve types, which may mean that AIS curves can be understood and prognosticated on the axial plane. For the great potential of axial rotational predictors, more research using 3D reconstruction methods should be done to clarify the role of rotation, and obtain more accurate measurements of rotation in degrees rather than Nash-Moe 66 and Perdriolle 47 grades. At present, evidence remains inconclusive for these predictors.
More evidence regarding AVR is available for braced patients. The strongest evidence comes from Kwan et al, 12 which is a prospective 3D study identifying AVR as an independent predictor. Other studies supporting the predictive value of AVR are studies on plain radiographs which measured rotation by the methods of Nash and Moe 66 or Perdriolle, 47 which were less accurate than 3D reconstruction. The questioned reliability of the measurement methods undermines the credibility of the AVR as a predictor of curve progression. It is also interesting to note, from Upadhyay et al 37 and Kwan et al, 12 that changes in AVR during bracing have some predictive ability on the final outcome. It warrants particular attention that AVR reduction velocity at one year had predictive effect independent of in-brace correction of Cobb angle, which means that in-brace correction of axial rotation can produce additional benefits as well as correction in the coronal view. This highlights the importance of examining the axial morphology in AIS prognostication, and sheds light on the effectiveness of newer types of braces that can produce greater derotational forces. 67 We may conclude that apical vertebral rotation is a significant predictor of curve progression, but further evidence from studies with larger sample sizes using 3D models is required in this area.
Evidence for the predictive value of sagittal assessments of sacral slope, pelvic incidence, and T1 and T9 spinopelvic inclination in braced patients remains inconclusive, because only two studies covered these predictors and conflicting evidence was found. These studies also suffered from poor reporting and questionable statistical analysis. Evidence for PT is only weakly predictive, with two studies 17,21 reporting significance in multivariable analysis adjusted for Cobb angle and Risser stage. However, none of these studies were free of bias. The 8.5° cut-off for PT given by Catanzano et al 17 should be interpreted with care due to the small sample size, and definite conclusions cannot be drawn before further estimates become available. Evidence is also inconclusive for thoracic kyphosis 57 and lumbar lordosis in unbraced patients, as studies with similar methodology found conflicting evidence for these two predictors, and there is a lack of high-quality studies with multivariable analysis to confirm their predictability.
Evidence for wedging in braced patients comes from a single cohort by Cheung et al, 19 which found no significance for apical ratio, but did find that a change in apical ratio could differentiate progressed, stable, and regressed patients. It is inconclusive whether wedging predicts progression due to a paucity of studies, but it is worth exploring change in apical ratio as a factor in future studies, because it may indicate vertebral remodelling during bracing. Evidence for wedging in unbraced patients is also lacking, and no valid conclusion can be made. Additionally, no valid conclusions can be drawn with apical vertebral translation, lumbar pelvic relation, or end-vertebra angle type, as only one study with univariate analysis examined them. 23 Definite conclusions regarding predictive factors for curve progression were also lacking due to a paucity of related studies, as these require long-term follow-up and can be difficult to conduct.
This is the first review to look at the morphological predictors of AIS curve progression using the GRADE method. By grading the level of evidence, we offered clinically relevant cut-offs for prediction of AIS curve progression. This is also the first study to review a large variety of 3D morphological predictors and point out 3D predictors with promising evidence to elucidate further research direction. However, we acknowledge several limitations. First, heterogeneity exists in the body of evidence. These studies varied in terms of the definitions of outcomes and confounders which were controlled, making synthesis of results difficult. Further prognostic studies should aim to include a multivariable analysis adjusted for a set of known predictors confirmed in the literature, to establish if there are new predictors of independent predictive value. Second, publication bias cannot be assessed due to a lack of reporting of effect sizes and CIs in some studies. The lack of assessment of publication bias may undermine the reliability of our use of the GRADE system of evidence for each predictor. Nevertheless, this review still informed us of the strength of evidence for different predictors in attempting to adopt the GRADE framework in systematic reviews of prognostic studies.
In summary, this is the first systematic review that assessed radiological prognostic factors for AIS curve progression using the GRADE approach. We found that Cobb angle > 25° and thoracic curves are the major predictors of curve progression in unbraced patients. Thoracic curves, supine flexibility < 28%, and low in-brace correction rate predict poor outcome in braced patients. Vertebral rotation may be a promising factor despite its current low evidence. This review highlighted a few knowledge gaps in the existing literature that will benefit from future research. More prognostic studies with multivariable analysis, with clear reporting of outcomes and statistical results, should be done. There is a need for investigators to adhere to a standardized outcome assessment for curve progression, e.g. Scoliosis Research Society criteria of progression of 5°. 68 Research effort should focus on identifying relations between different prognostic factors, and clarifying the possible pathomechanism of AIS to allow for identification of prognostic factors that represent the underlying disease-causing mechanism. Finally, more studies using 3D reconstruction models should be done to avoid measurement bias.
Author contributions
L. P. K. Wong: Methodology, Investigation, Data curation, Formal analysis, Writing – original draft.
P. W. H. Cheung: Methodology, Investigation, Data curation, Formal analysis, Validation, Writing – review & editing.
J. P. Y. Cheung: Conceptualization, Methodology, Project administration, Funding acquisition, Supervision, Resources, Software, Investigation, Data curation, Formal analysis, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding statement
The authors disclose receipt of the following financial or material support for the research, authorship, and/or publication of this article: the RGC Research Impact Fund (R5017-18F).
ICMJE COI statement
All authors have no conflicts of interest to disclose.
Open access funding
Open access funding was supported by the RGC Research Impact Fund (R5017-18F).
Open access statement
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Supplementary material
Detailed search strategies and search words across databases including Embase, Medline, Web of Science, and PubMed; tables summarizing key findings and statistical methods for predictors with inconclusive evidence, study characteristics, Quality in Prognostic Studies risk of bias, and key findings and statistical methods for predictors with sufficient and less sufficient evidence.
This article was primary edited by G. Scott.
Contributor Information
Lester P. K. Wong, Email: u3558250@connect.hku.hk.
Prudence W. H. Cheung, Email: gnuehcp6@hotmail.com.
Jason P. Y. Cheung, Email: cheungjp@hku.hk.
References
- 1. Zhang J, Cheuk K-Y, Xu L, et al. . A validated composite model to predict risk of curve progression in adolescent idiopathic scoliosis. EClinicalMedicine. 2020;18:100236. 10.1016/j.eclinm.2019.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee CF, Fong DYT, Cheung KMC, et al. . A new risk classification rule for curve progression in adolescent idiopathic scoliosis. Spine J. 2012;12(11):989–995. 10.1016/j.spinee.2012.05.009 [DOI] [PubMed] [Google Scholar]
- 3. Negrini S, Donzelli S, Aulisa AG, et al. . 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018;13:3. 10.1186/s13013-017-0145-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med. 2013;369(16):1512–1521. 10.1056/NEJMoa1307337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dolan LA, Donzelli S, Zaina F, Weinstein SL, Negrini S. Adolescent idiopathic scoliosis bracing success is influenced by time in brace: comparative effectiveness analysis of BrAIST and ISICO cohorts. Spine. 2020;45(17):1193–1199. 10.1097/BRS.0000000000003506 [DOI] [PubMed] [Google Scholar]
- 6. Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine. 2007;32(20):2198–2207. 10.1097/BRS.0b013e31814b851f [DOI] [PubMed] [Google Scholar]
- 7. van den Bogaart M, van Royen BJ, Haanstra TM, de Kleuver M, Faraj SSA. Predictive factors for brace treatment outcome in adolescent idiopathic scoliosis: a best-evidence synthesis. Eur Spine J. 2019;28(3):511–525. 10.1007/s00586-018-05870-6 [DOI] [PubMed] [Google Scholar]
- 8. Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board, Cochrane Back Review Group . 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34(18):1929–1941. 10.1097/BRS.0b013e3181b1c99f [DOI] [PubMed] [Google Scholar]
- 9. Furlan AD, Malmivaara A, Chou R, et al. . 2015 Updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine. 2015;40(21):1660–1673. 10.1097/BRS.0000000000001061 [DOI] [PubMed] [Google Scholar]
- 10. Noshchenko A, Hoffecker L, Lindley EM, et al. . Predictors of spine deformity progression in adolescent idiopathic scoliosis: a systematic review with meta-analysis. World J Orthop. 2015;6(7):537–558. 10.5312/wjo.v6.i7.537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Courvoisier A, Drevelle X, Dubousset J, Skalli W. Transverse plane 3D analysis of mild scoliosis. Eur Spine J. 2013;22(11):2427–2432. 10.1007/s00586-013-2862-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kwan KYH, Cheung AKP, Koh HY, Cheung KMC. Brace effectiveness is related to 3-dimensional plane parameters in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2021;103-A(1):37–43. 10.2106/JBJS.20.00267 [DOI] [PubMed] [Google Scholar]
- 13. Trac S, Zheng R, Hill DL, Lou E. Intra- and interrater reliability of Cobb angle measurements on the plane of maximum curvature using ultrasound imaging method. Spine Deform. 2019;7(1):18–26. 10.1016/j.jspd.2018.06.015 [DOI] [PubMed] [Google Scholar]
- 14. Wu H-D, Chu W-W, He C-Q, Wong M-S. Assessment of the plane of maximum curvature for patients with adolescent idiopathic scoliosis via computed tomography. Prosthet Orthot Int. 2020;44(5):298–304. 10.1177/0309364620941297 [DOI] [PubMed] [Google Scholar]
- 15. Skalli W, Vergari C. Biomechanics of adolescent idiopathic scoliosis. 2017;75–97. 10.1007/978-4-431-56541-3 [DOI]
- 16. Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Catanzano AA, Esposito VR, Dial BL, et al. . Staying ahead of the curve: the use of spinopelvic parameters to predict curve progression and bracing success in adolescent idiopathic scoliosis. Spine Deform. 2020;8(6):1213–1222. 10.1007/s43390-020-00159-5 [DOI] [PubMed] [Google Scholar]
- 18. Cheung JPY, Cheung PWH. Supine flexibility predicts curve progression for patients with adolescent idiopathic scoliosis undergoing underarm bracing. Bone Joint J. 2020;102-B(2):254–260. 10.1302/0301-620X.102B2.BJJ-2019-0916.R1 [DOI] [PubMed] [Google Scholar]
- 19. Cheung JPY, Cheung PWH, Yeng WC, Chan LCK. Does curve regression occur during underarm bracing in patients with adolescent idiopathic scoliosis? Clin Orthop Relat Res. 2020;478(2):334–345. 10.1097/CORR.0000000000000989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dolan LA, Weinstein SL, Abel MF, et al. . Bracing in adolescent idiopathic scoliosis trial (BrAIST): development and validation of a prognostic model in untreated adolescent idiopathic scoliosis using the simplified skeletal maturity system. Spine Deform. 2019;7(6):890–898. 10.1016/j.jspd.2019.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guo J, Liu Z, Lv F, et al. . Pelvic tilt and trunk inclination: new predictive factors in curve progression during the Milwaukee bracing for adolescent idiopathic scoliosis. Eur Spine J. 2012;21(10):2050–2058. 10.1007/s00586-012-2409-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine. 2001;26(18):2001–2005. 10.1097/00007632-200109150-00013 [DOI] [PubMed] [Google Scholar]
- 23. Katz DE, Durrani AA. Factors that influence outcome in bracing large curves in patients with adolescent idiopathic scoliosis. Spine. 2001;26(21):2354–2361. 10.1097/00007632-200111010-00012 [DOI] [PubMed] [Google Scholar]
- 24. Labrom FR, Izatt MT, Contractor P, et al. . Sequential MRI reveals vertebral body wedging significantly contributes to coronal plane deformity progression in adolescent idiopathic scoliosis during growth. Spine Deform. 2020;8(5):901–910. 10.1007/s43390-020-00138-w [DOI] [PubMed] [Google Scholar]
- 25. Lara T, Astur N, Jones TL, et al. . The risk of curve progression and surgery in African Americans with adolescent idiopathic scoliosis. Spine Deform. 2017;5(4):250–254. 10.1016/j.jspd.2017.01.013 [DOI] [PubMed] [Google Scholar]
- 26. Mao S, Shi B, Xu L, et al. . Initial Cobb angle reduction velocity following bracing as a new predictor for curve progression in adolescent idiopathic scoliosis. Eur Spine J. 2016;25(2):500–505. 10.1007/s00586-015-3937-7 [DOI] [PubMed] [Google Scholar]
- 27. Modi HN, Suh SW, Song HR, Yang JH, Ting C, Hazra S. Drooping of apical convex rib-vertebral angle in adolescent idiopathic scoliosis of more than 40 degrees: a prognostic factor for progression. J Spinal Disord Tech. 2009;22(5):367–371. 10.1097/BSD.0b013e3181836a8a [DOI] [PubMed] [Google Scholar]
- 28. Nault M-L, Mac-Thiong J-M, Roy-Beaudry M, et al. . Three-dimensional spinal morphology can differentiate between progressive and nonprogressive patients with adolescent idiopathic scoliosis at the initial presentation: a prospective study. Spine. 2014;39(10):E601-6. 10.1097/BRS.0000000000000284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ohashi M, Watanabe K, Hirano T, et al. . Predicting factors at skeletal maturity for curve progression and low back pain in adult patients treated nonoperatively for adolescent idiopathic scoliosis with thoracolumbar/lumbar curves. Spine. 2018;43(23):E1403–E1411. 10.1097/BRS.0000000000002716 [DOI] [PubMed] [Google Scholar]
- 30. Ohashi M, Watanabe K, Hirano T, et al. . The natural course of compensatory lumbar curves in nonoperated patients with thoracic adolescent idiopathic scoliosis. Spine. 2019;44(2):E89–E98. 10.1097/BRS.0000000000002779 [DOI] [PubMed] [Google Scholar]
- 31. Ohrt-Nissen S, Hallager DW, Gehrchen M, Dahl B. Flexibility predicts curve progression in providence nighttime bracing of patients with adolescent idiopathic scoliosis. Spine. 2016;41(22):1724–1730. 10.1097/BRS.0000000000001634 [DOI] [PubMed] [Google Scholar]
- 32. Pasha S. 3D spinal and rib cage predictors of brace effectiveness in adolescent idiopathic scoliosis. BMC Musculoskelet Disord. 2019;20(1):384. 10.1186/s12891-019-2754-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shi B, Guo J, Mao S, et al. . Curve progression in adolescent idiopathic scoliosis with a minimum of 2 years’ follow-up after completed brace weaning with reference to the SRS standardized criteria. Spine Deform. 2016;4(3):200–205. 10.1016/j.jspd.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 34. Sun X, Ding Q, Sha S, et al. . Rib-vertebral angle measurements predict brace treatment outcome in Risser grade 0 and premenarchal girls with adolescent idiopathic scoliosis. Eur Spine J. 2016;25(10):3088–3094. 10.1007/s00586-015-4372-5 [DOI] [PubMed] [Google Scholar]
- 35. Tan KJ, Moe MM, Vaithinathan R, Wong HK. Curve progression in idiopathic scoliosis: follow-up study to skeletal maturity. Spine. 2009;34(7):697–700. 10.1097/BRS.0b013e31819c9431 [DOI] [PubMed] [Google Scholar]
- 36. Thompson RM, Hubbard EW, Jo CH, Virostek D, Karol LA. Brace success is related to curve type in patients with adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2017;99-A(11):923–928. 10.2106/JBJS.16.01050 [DOI] [PubMed] [Google Scholar]
- 37. Upadhyay SS, Nelson IW, Ho EK, Hsu LC, Leong JC. New prognostic factors to predict the final outcome of brace treatment in adolescent idiopathic scoliosis. Spine. 1995;20(5):537–545. 10.1097/00007632-199503010-00006 [DOI] [PubMed] [Google Scholar]
- 38. Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B. 2005;14(5):320–324. 10.1097/01202412-200509000-00002 [DOI] [PubMed] [Google Scholar]
- 39. Zhang Y, Yang Y, Dang X, et al. . Factors relating to curve progression in female patients with adolescent idiopathic scoliosis treated with a brace. Eur Spine J. 2015;24(2):244–248. 10.1007/s00586-014-3674-3 [DOI] [PubMed] [Google Scholar]
- 40. Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–286. 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 41. Guyatt GH, Oxman AD, Vist GE, et al. . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. 10.1136/bmj.39489.470347.AD [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Huguet A, Hayden JA, Stinson J, et al. . Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Syst Rev. 2013;2:71. 10.1186/2046-4053-2-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Foroutan F, Guyatt G, Zuk V, et al. . GRADE Guidelines 28: use of GRADE for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol. 2020;121:62–70. 10.1016/j.jclinepi.2019.12.023 [DOI] [PubMed] [Google Scholar]
- 44. Lenke LG, Betz RR, Harms J, et al. . Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A(8):1169–1181. [PubMed] [Google Scholar]
- 45. Mehta MH. The rib-vertebra angle in the early diagnosis between resolving and progressive infantile scoliosis. J Bone Joint Surg Br. 1972;54-B(2):230–243. 10.1302/0301-620X.54B2.230 [DOI] [PubMed] [Google Scholar]
- 46. Nash CL, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51-A(2):223–229. [PubMed] [Google Scholar]
- 47. Perdriolle R, Vidal J. Thoracic idiopathic scoliosis curve evolution and prognosis. Spine. 1985;10(9):785–791. 10.1097/00007632-198511000-00001 [DOI] [PubMed] [Google Scholar]
- 48. Sanders JO, Khoury JG, Kishan S, et al. . Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90-A(3):540–553. 10.2106/JBJS.G.00004 [DOI] [PubMed] [Google Scholar]
- 49. Cheung PWH, Cheung JPY. Does the use of Sanders staging and distal radius and ulna classification avoid mismatches in growth assessment with Risser staging alone? Clin Orthop Relat Res. 2021;479(11):2516–2530. 10.1097/CORR.0000000000001817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cheung PWH, Canavese F, Luk KDK, Cheung JPY. An insight of how multiple skeletal maturity indices can be used for growth assessment: relationship between the simplified olecranon, simplified digital, and distal radius and ulna classifications. J Pediatr Orthop B. 2021;30(4):371–380. 10.1097/BPB.0000000000000760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Cheung JPY, Luk KDK. Managing the pediatric spine: growth assessment. Asian Spine J. 2017;11(5):804–816. 10.4184/asj.2017.11.5.804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cheung JPY, Cheung PWH, Samartzis D, Cheung KMC, Luk KDK. The use of the distal radius and ulna classification for the prediction of growth: peak growth spurt and growth cessation. Bone Joint J. 2016;98-B(12):1689–1696. 10.1302/0301-620X.98B12.BJJ-2016-0158.R1 [DOI] [PubMed] [Google Scholar]
- 53. Weinstein SL, Dolan LA, Spratt KF, Peterson KK, Spoonamore MJ, Ponseti IV. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289(5):559–567. 10.1001/jama.289.5.559 [DOI] [PubMed] [Google Scholar]
- 54. Bian Z, Guo Y, Lyu X, Yang Z, Cheung JPY. Relationship between hand and wrist bone age assessment methods. Medicine (Baltimore). 2020;99(39):e22392. 10.1097/MD.0000000000022392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Cheung JPY, Cheung PWH, Samartzis D, Luk KDK. APSS-ASJ Best Clinical Research Award: predictability of curve progression in adolescent idiopathic scoliosis using the distal radius and ulna classification. Asian Spine J. 2018;12(2):202–213. 10.4184/asj.2018.12.2.202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Cheung JPY, Cheung PWH, Samartzis D, Luk KDK. Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res. 2018;476(2):429–436. 10.1007/s11999.0000000000000027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Cheung JPY, Chong CHW, Cheung PWH. Underarm bracing for adolescent idiopathic scoliosis leads to flatback deformity: the role of sagittal spinopelvic parameters. Bone Joint J. 2019;101-B(11):1370–1378. 10.1302/0301-620X.101B11.BJJ-2019-0515.R1 [DOI] [PubMed] [Google Scholar]
- 58. Cheung JPY, Cheung PWH, Luk KDK. When should we wean bracing for adolescent idiopathic scoliosis? Clin Orthop Relat Res. 2019;477(9):2145–2157. 10.1097/CORR.0000000000000781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Cheung PWH, Cheung JPY. Sanders stage 7b: using the appearance of the ulnar physis improves decision-making for brace weaning in patients with adolescent idiopathic scoliosis. Bone Joint J. 2021;103-B(1):141–147. 10.1302/0301-620X.103B1.BJJ-2020-1240.R1 [DOI] [PubMed] [Google Scholar]
- 60. Cheung JPY, Yiu KKL, Vidyadhara S, Chan PPY, Cheung PWH, Mak KC. Predictability of supine radiographs for determining in-brace correction for adolescent idiopathic scoliosis. Spine. 2018;43(14):971–976. 10.1097/BRS.0000000000002503 [DOI] [PubMed] [Google Scholar]
- 61. He C, To M-T, Cheung JPY, et al. . An effective assessment method of spinal flexibility to predict the initial in-orthosis correction on the patients with adolescent idiopathic scoliosis (AIS). PLoS One. 2017;12(12):e0190141. 10.1371/journal.pone.0190141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Kawasaki S, Cheung PWH, Shigematsu H, et al. . Alternate In-Brace and Out-of-Brace radiographs are recommended to assess brace fitting and curve progression with adolescent idiopathic scoliosis follow-up. Global Spine J. 2021;2021:21925682211032560. 10.1177/21925682211032559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Foley G, Aubin CE, Labelle H, et al. . The rib vertebra angle difference and its measurement in 3D for the evaluation of early onset scoliosis. Stud Health Technol Inform. 2012;176:238–241. [PubMed] [Google Scholar]
- 64. Foley G, Aubin C-E, Parent S, et al. . Physical significance of the rib vertebra angle difference and its 3-Dimensional counterpart in early-onset scoliosis. Spine Deform. 2013;1(4):259–265. 10.1016/j.jspd.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 65. Brink RC, Schlösser TPC, van Stralen M, et al. . What is the actual 3D representation of the rib vertebra angle difference (Mehta Angle)? Spine. 2018;43(2):E92–E97. 10.1097/BRS.0000000000002225 [DOI] [PubMed] [Google Scholar]
- 66. Nash CL, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51-A(2):223–229. 10.2106/00004623-196951020-00002 [DOI] [PubMed] [Google Scholar]
- 67. Strube P, Gunold M, Müller T, et al. . Influence of curve morphology and location on the efficacy of rigid conservative treatment in patients with adolescent idiopathic scoliosis. Bone Joint J. 2021;103-B(2):373–381. 10.1302/0301-620X.103B2.BJJ-2020-1113.R2 [DOI] [PubMed] [Google Scholar]
- 68. Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine. 2005;30(18):2068–2075. 10.1097/01.brs.0000178819.90239.d0 [DOI] [PubMed] [Google Scholar]