Abstract
Identifying factors associated with COVID-19 vaccination acceptance among vulnerable groups, including autistic individuals, can increase vaccination rates and support public health. The purpose of this study was to determine differences among autistic adults who reported COVID-19 vaccination acceptance from those who did not. In this study we describe COVID-19 vaccination status and self-reported preferences among autistic adults and identify related factors. Vaccine accepters were more likely to report increased loneliness during COVID-19, lived in more populous counties (p = 0.02), and lived in counties won by President Biden in the 2020 US presidential election (p < 0.001). Positive correlations were found between desire to protect others, concern about contracting COVID-19, and trusting vaccine safety (p < 0.001). Concern about vaccine safety was common among the vaccine hesitant, while lack of concern about COVID-19 overall was not. Identifying health promotion strategies based on self-reported, lived experiences about COVID-19 among vulnerable groups is key for public health impact.
Keywords: Autism, Disability, Health equity, Health communication, Public health
1. Introduction
Identifying patterns of COVID-19 vaccination acceptance and hesitancy among vulnerable groups is a critical and timely priority that informs clinical practice and public health resource allocation [1]. Autistic individuals have a higher risk of complications and hospitalization from COVID-19 likely due to multiple co-occurring medical and psychiatric diagnoses that require service delivery in group settings [2], [3], [4], [5]. Healthcare providers and advocacy groups have called for COVID-19 vaccine prioritization of autistic individuals given their increased risk for hospitalization and longer length of hospital stays [6]. Preliminary research has found that significant side effects are not associated with autistic populations who received a COVID-19 vaccine [7]. However, research identifying vaccination rates and vaccine acceptance or hesitancy amongst autistic individuals is lacking. Delays in adding autism as a condition for vaccine priority may further contribute to inequities in vaccine access among this group [6], [8], [9]. Misinformation about COVID-19 vaccination is surging, particularly on social media, and causing significant challenges to public health [10]. As attacks on COVID-19 vaccines dominate discourse amongst the unvaccinated, it is clear that a robust public health strategy is needed to continue progress toward minimizing the impact of COVID-19 through reduced community transmission. The core features of autism spectrum disorder (ASD) include social and communication differences [11] and may contribute to this population being more susceptible to vaccine misinformation and therefore are a critical public health priority.
Understanding the reasons for vaccine hesitancy is crucial for crafting public health responses tailored to specific populations to maximize impact and ensure health equity. For autistic adults specifically, stereotypes can paint an inaccurate and oversimplified picture of the heterogeneity of the autism spectrum [12]. It is imperative that lived experiences of autistic adults are prioritized to ensure the breadth of the community is captured. Correspondingly, the benefits of autism research are also maximized when self-reported measures of autistic individuals are utilized, rather than parent, caregiver, or other proxy reporters that are more commonly employed. Research demonstrates that there can be significant discordance between autistic individuals and proxy reporters [13]. This incongruence may be magnified further in vaccine research, as parents of autistic children report significantly higher levels of vaccine hesitancy [14]. Therefore, we investigated COVID-19 acceptance and hesitancy among autistic adults and associations with demographic characteristics, COVID-19 impact, and county-level contextual factors.
2. Methods
A subset of participants from the 2018 Pennsylvania Autism Needs Assessment [15] of Pennsylvania adults aged 18 who agreed to future contact were invited to participate in this study (n = 431). In the 2018 PANA, all state residents enrolled in Medicaid with a service claims or encounter for a primary autism spectrum diagnosis (ICD-9 299.XX or ICD 10 F84.X) received recruitment materials by mail to participate in the survey [16], [17]. An ASD diagnosis in claims data has demonstrated high positive predictive value when compared to community diagnoses or review by expert clinicians [17], [18]. In addition to the claims-based approach, potential respondents to the 2018 PANA were also reached through ASD-specific advocacy and policy organizations across Pennsylvania. All participants needed to self-report a formal ASD diagnosis, which was not verified by clinical interview. Responses were reported by autistic adults, although respondents were able to receive support to complete the survey from a caregiver if needed. Analysis was conducted on individuals with complete responses to items related to experiences with COVID-19 that were received between March 29 and July 26, 2021 (n = 168, complete response rate 39%). Compared with non-respondents, respondents were more likely to be white (86.9% vs. 75.2%, p < 0.001).
Our survey included a set of 17 questions specifically related to COVID-19 experiences, including vaccination acceptance, hesitancy, and status (full survey attached in Supplementary Material). Questions were incorporated from several surveys to measure various COVID-19 related constructs and were adapted to be more accessible to autistic adults. Items related to COVID-19 impact were based on the Coronavirus Impact Scale [19], which asks about changes across various life domains, including stress, access to care, and physical activity. The item assessing willingness to be vaccinated was adopted from a Kaiser Family Foundation (KFF) survey [20], which asked respondents to select from a list of reasons that contributed to their vaccine willingness. Respondents could also select items describing their hesitancy using concepts based on a survey of perceived barriers to a COVID-19 vaccine from Guidry et al. (2021) [21], which we adapted based on research team consensus. Similarly, the question capturing vaccine acceptance was developed internally by the research team and agreed through consensus. We used the COVID-19 Community Response Survey Guidance from Johns Hopkins University [22] to inform our item regarding loneliness, which asks whether the frequency that respondents felt lonely during the pandemic had increased, decreased, or remained the same compared to before the pandemic.
We identified the COVID-19 vaccine acceptance group as those who reported they had received at least one dose or were planning to receive the vaccine, and the COVID-19 vaccine hesitancy group as those who had not received at least one dose and did not plan to receive the vaccine. We compared these groups by self-reported gender, marital status, race/ethnicity, medical insurance coverage, living arrangement status, and age. We identified changes in daily and exercise routines, healthcare access, and loneliness during the COVID-19 pandemic. County-level 2010 US Census population density and certified percentage of the 2020 US presidential election votes won by President Biden were also included [23], [24]. Comparisons were conducted using Chi-Square analyses and T-tests. All analyses were completed using Stata version 17.0 [25] and R version 4.1.1 [26]. Reasons for COVID-19 vaccination acceptance or hesitancy were ranked by frequency, and co-occurrence was investigated with phi-coefficient [27] correlation plots.
3. Results
78.3% of survey respondents reported that they had received or were planning to receive a COVID-19 vaccine, with 55.4% reporting that they had received at least one dose. In comparison, 42% of adults in Pennsylvania received at least one dose of a COVID-19 vaccine as of April 2, 2021 [28], the sample median response date. 77.7% of adults in Pennsylvania received at least one dose as of July 26, 2021, the last date of sample data collection [29].
Respondents who reported increased loneliness during the COVID-19 pandemic were more likely to accept COVID-19 vaccination. Higher population county-level density and percentage of votes for President Biden in the 2020 US presidential election were associated with a greater probability of accepting COVID-19 vaccination (Table 1 ).
Table 1.
Sample Demographic Characteristics by COVID-19 Vaccine Receipt Status.
| Not received and not planning to receive (n = 37) |
Received or planning to receive (n = 131) |
p-value | |
|---|---|---|---|
| Person-level factors | |||
| Gender | 0.82 | ||
| Man | 65% | 70% | |
| Woman | 27% | 23% | |
| Other | 8% | 7% | |
| Marital Status | 0.92 | ||
| Married | 8% | 8% | |
| Never Married | 92% | 92% | |
| Race/Ethnicity | 0.93 | ||
| Non-White | 14% | 13% | |
| White | 86% | 87% | |
| Medical Insurance | 0.89 | ||
| Private | 22% | 21% | |
| Public | 78% | 79% | |
| Living Arrangement | 0.43 | ||
| Family/Roommate | 84% | 78% | |
| Independent or Other | 16% | 22% | |
| Daily Routine | 0.61 | ||
| Change | 84% | 87% | |
| No Change | 16% | 13% | |
| Exercise Routine | 0.22 | ||
| Change | 46% | 57% | |
| No Change | 54% | 43% | |
| Medical Care Access | 0.13 | ||
| Change | 35% | 23% | |
| No Change | 65% | 77% | |
| Loneliness | 0.023 | ||
| Increased | 24% | 45% | |
| Same/Decreased | 76% | 55% | |
| Age in years, mean (SD) | 30 (8) | 32 (9) | 0.36 |
| County-level factors | |||
| Pop. Density, mean (SD) | 768 (1882) | 2122 (3428) | 0.022 |
| 2020 Biden Vote %, mean (SD) | 41 (13) | 53 (15) | < 0.001 |
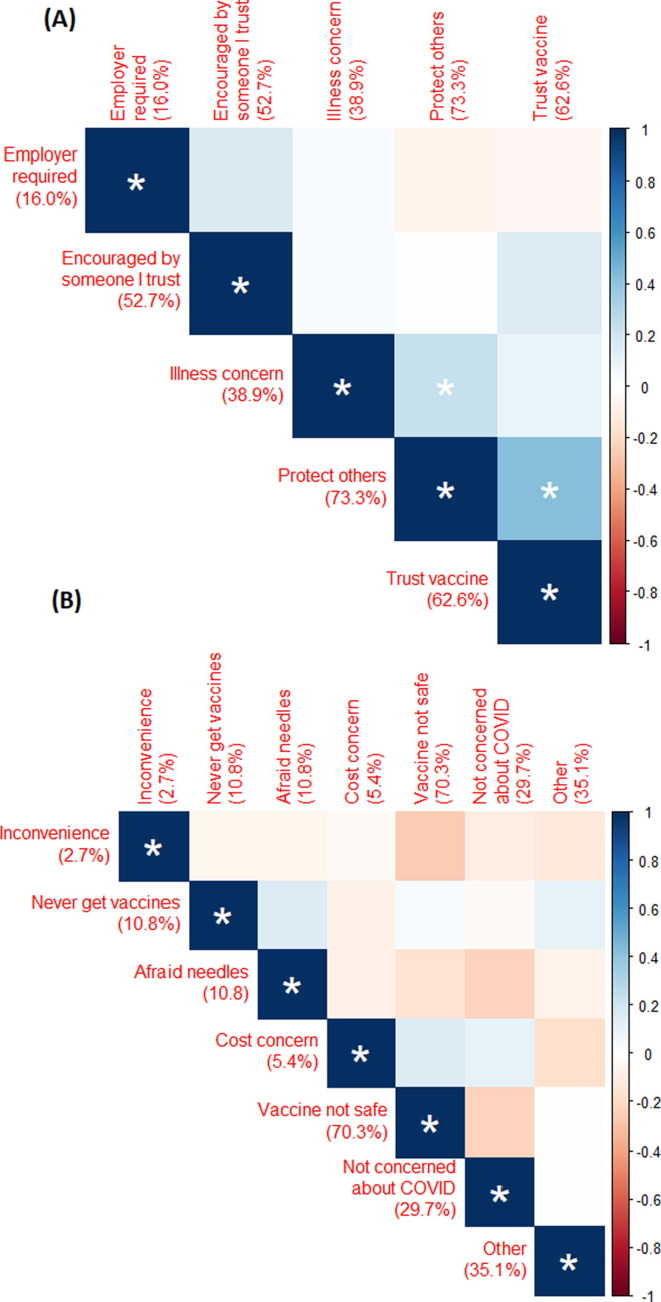
The most frequent reason for accepting COVID-19 vaccination was a desire to protect others from infection (73.3%). The most common reason for vaccine hesitancy was concern about vaccine safety (70.3%). Trusting vaccine safety and protecting others co-occurred (correlation: 0.425, p-value: < 0.001), as did protecting others and concern about getting seriously ill (correlation: 0.234, p-value: < 0.001) (Fig. 1 ).
Fig. 1.
Correlation Plots of Motivations for Receiving or Planning to Receive (A) or Not Receiving and Not Planning to Receive (B) a COVID-19 Vaccine. The magnitude of the phi coefficient representing a correlation between variables in an intersecting row and column of the matrix is indicated by color. Coefficients with p < 0.05 are indicated by a *. The percentage of the sample that indicated each reason is shown in red next to the reason label. Blue shades represent a tendency for the intersecting row and column reasons to both be reported, while red shades represent a tendency for one to be reported when the other was not. The two coefficients with p < 0.05 suggest that the co-occurrence was frequent enough to be unlikely under the null hypothesis of no association.
4. Discussion
This study presents timely information about COVID-19 vaccination status, preferences, and opinions of autistic adults based on their own lived experience. Self-reported information about vaccination acceptance and hesitancy among autistic adults is critical to ensuring that public health strategies reach vulnerable groups and promote health equity. Initial research has been limited to vaccination hesitancy among parents of children on the autism spectrum [14], which may be differentially impacted by the complex history of vaccine safety and autism occurrence [30], [31], and there is a dearth of research directly engaging the growing group of transition age youth and adults on the autism spectrum.
Many responses were collected in late March and early April 2021 when vaccine eligibility and availability was still limited. The true vaccination rate by July 26, 2021 was likely between 55.4%, the percentage reporting they received at least one dose, and 78.3%, the percentage receiving or planning to receive a vaccine. This rate is similar to or higher than the general population in Pennsylvania (77.7%) as of July 26, 2021 [29], suggesting that COVID-19 vaccination was a priority among autistic adult survey respondents. The difference in vaccination rate among this study sample as compared to the total Pennsylvania population (55.3% vs. 42%) at the time of the median survey response date indicates that vaccination of autistic individuals was prioritized as a result of individual health preferences and possibly public health efforts. A closer examination of Pennsylvania’s strategies to promote the COVID-19 vaccination among autistic individuals and to the broader population may support the identification of strategies and best practices for replication in other states and for other public health issues. Although our sample originated from one state, Pennsylvania is a large US state and has a diverse range of rural, suburban, and urban areas with political, cultural, and geographic diversity that mirrors the country as a whole [32], suggesting that it is plausible that the identified factors associated with vaccine hesitancy and acceptance are generalizable. In 2020, 83.8% of the Pennsylvania population age 18 and older was white, compared to 86.9% of respondents in this study who reported they were white [33]. Despite our survey’s broad representativeness, we recognize that ableism, racism, and other forms of systemic discrimination interact to produce complex barriers to health service access among autistic adults who are also members of one or more underrepresented groups defined by race/ethnicity, sexual orientation, gender, socioeconomic status, and other identities [34].
The desire to get a COVID-19 vaccination to protect others from infection indicates that the risk for disease transmission may have been effectively communicated to this group. The desire to protect others from COVID-19 infection also demonstrates that valuing the health of community members, families, and friends is likely a priority for this group. This finding is underscored by the positive association of loneliness with COVID-19 vaccination uptake, reinforcing the social impact that COVID-19 mitigation efforts likely had on autistic adults and suggests that loneliness was a motivating factor in seeking vaccination. Autistic adults were also willing to receive the COVID-19 vaccination to protect others, which reinforces the importance of social connections as a motivating factor [35]. It may also be that autistic individuals who value COVID mitigation strategies are more isolated than their peers. These findings are important for crafting public health messaging about COVID-19, other vaccinations, and potentially other health interventions (such as handwashing or other disease control measures) to this group. The impact of loneliness also suggests that re-emergence into and engagement with communities is desired by autistic adults, which may motivate vaccination acceptance in this group. Research has found that despite social and communication differences that are a part of the autism experience, autistic adults do desire social connections [36], [37]. The suggestion that autistic individuals do not desire social relationships is a longstanding myth that fails to recognize the diversity of the autism community and increased awareness of this is important for public health communication [12]. This calls to action the need for supports in the community, such as those funded by Medicaid through robust home and community-based waivers, to be in place and available in order to maximize the participation of autistic individuals in their communities.
However, some factors appear to predict vaccine hesitancy among autistic adults. Vaccine hesitancy has been a paramount issue in the roll-out of COVID-19 vaccinations. Misinformation about the COVID-19 vaccine has been a rampant public health issue [10] and adults on the autism spectrum, given social and communication differences that are core aspects of a diagnosis of ASD [11], may be especially vulnerable to vaccine falsities being shared as has been demonstrated in other populations [10]. The decreased likelihood of COVID-19 vaccination among adults in areas that voted less often for President Biden indicates that community characteristics, including urbanicity, healthcare access, and political beliefs, likely impact autistic adults similarly to the overall population. This finding points to the potential need for targeted outreach strategies about COVID-19 vaccination in these communities. The intersection of political beliefs and adults with disabilities is understudied and is a key area for future research to support clinicians in developing informed clinical approaches and implementing health interventions. For instance, the Centers for Disease Control and Prevention (CDC) offers guidance for clinicians to tailor messaging to individual needs and communication style [38]. Clinicians from the University of Minnesota recently offered a framework for clinicians to respond to vaccine misinformation through data and collaboration [39]. Storytelling and visual images have been found to be helpful tools for vaccine-hesitant parents [40], [41] and may prove especially useful for communicating information to individuals with social and communication differences. A lack of access to services as autistic adults age beyond the service cliff [42] may exacerbate the impact of limited healthcare access in rural areas or areas of provider shortages on not only COVID-19 vaccination, testing, and treatment options but also the supports needed by this group to improve documented poor outcomes across community engagement [43].
Concerns about vaccine safety outweighed the potential impact of contracting COVID-19 in our sample. For instance, well over half (70.3%) of those not planning to receive a COVID-19 vaccine were concerned about the safety of the vaccines, and less than a third (29.7%) said they were not concerned about contracting COVID-19. This finding calls for enhanced health communication strategies targeting people, including adults with disabilities, who lack trust in the vaccine or development process. Information about the vaccine development or approval processes may be needed among this group and research on effective communication of this information is likely needed as well. Adapted health promotion approaches to address these needs are a priority area for future research [44]. Integrating lived experiences maximizes the impact and effectiveness of research [45], and incorporating self-advocates on the autism spectrum at all stages of the research process, including the design and interpretation of findings, is a fundamental next step for all future research, particularly on topics like vaccination where community buy-in is essential to optimal outcomes. There may be unique opportunities to develop and test strategies with autistic adults, as they frequently interact with service providers and often live with families who may serve as information delivery opportunities or challenges. However, there may be disproportionate access to these service providers given the documented service cliff and service access barriers documents among autistic transition age youth and adults [46], [47], [48]. Transdisciplinary strategies may be needed to adopt and adapt health communication advances for diverse populations, including those with social and communication needs, for clinicians from other diseases, including diabetes, cancer, and dental care [49]. Involving autistic self-advocates across all avenues of information dissemination is also vital to ensure accessibility, and it will be crucial for public health officials to prioritize and proactively seek their input.
While this study and the findings are important and have many strengths, it is important to acknowledge the limitations. One limitation is that adults who completed the 2018 PANA through recruitment from ASD advocacy organizations self-reported their ASD diagnosis and it was not validated by clinical interview. Another potential limitation includes the diversity of our study sample. While there were no statistically significant differences in race/ethnicity between respondents and non-respondents, it should be noted that the modal respondent was a white male approximately 30 years of age. Still, the proportion of respondents of color was only slightly lower than the age-adjusted proportion of persons of color in the state population. Given that COVID-19 has disproportionately impacted and exacerbated existing racial and ethnic health disparities, it is important to consider how identity shapes vaccine willingness and hesitancy. Age is also an important factor, especially given that older adults are at a higher risk of complications from COVID-19 and may access public health messaging differently from younger peers. Future research would benefit from oversampling and further prioritizing the voices of autistic people of color and older ages in all aspects of public health, and particularly in COVID-19 research.
The findings from this study present important implications for policy and practice. The successes of COVID-19 vaccination in Pennsylvania, among autistic adults and to eligible populations in general, and the reasons for vaccine hesitancy can be used to better inform and prioritize health promotion materials and outreach efforts. Continued efforts to mitigate vaccine misinformation [10] will be especially critical to address concerns about vaccine safety among this population. Timely research to support public health efforts is needed, especially as the prevalence of autism continues to increase. It may be that the social and communication components of an autism diagnosis require distinct crafting of public health messaging materials at the onset of a public health crises to communicate information clearly. Public health communication released to combat misinformation that has spread may also need specific modifications. Social stories are a powerful tool for conveying information to autistic individuals [50], and widespread rollout of COVID-19 social stories, such as those from the Autism Services, Education, Resource, and Training (ASERT) Collaborative [51], can help provide accurate information through a visual and accessible format. It remains unclear if or how the increased risk for co-occurring medical or psychiatric diagnoses may impact vaccine hesitancy or acceptance. Research demonstrates that most individuals with chronic health risks have strong levels of COVID-19 vaccine acceptance, although 20% remain hesitant about vaccination [52]. Identifying successful health communication strategies regarding COVID-19 vaccination for vulnerable groups is a key component of a comprehensive, national public health strategy. A diverse array of dissemination strategies that incorporate the principles of universal design and accessibility, meaning that the materials are created to be usable by everyone, are needed [53]. Organizations like the Autistic Self Advocacy Network (ASAN) and the ASERT Collaborative have become hubs of COVID-19 information for the autism community, housing videos, animations, easy-read and plain language fact sheets, and public health communication materials that not only are beneficial to autistic individuals but to a broader audience of those with and without communication differences. Implementing similar strategies in COVID-19 vaccination outreach campaigns exemplified by ASAN and the ASERT Collaborative can improve health outcomes, equity, and supports clinicians and public health agencies in engaging across diverse patient groups.
Declaration of Competing Interest
Dr. Shea receives wages for contract work focused on data and program needs from the Office of Developmental Programs in Pennsylvania.
Acknowledgments
Acknowledgements
The authors are grateful to the autistic adults who participated in this study.
Funding
This study was supported by Community Participation, Service Needs, and Health Outcomes among Autism with Autism funded the US Department of Defense Award W81XWH-20-1-0435 and the Autism Intervention Research Network on Physical Health funded by the US Department of Health and Human Services Health Resources and Services Administration Award 1 UT2MC39440-01-00.
Authors’ Contributions
LS had full access to all of the data in the study and takes responsibility for the integrity of the data and accuracy of data analyses. LS, BKL, MSS, and DV obtained funding. LS, AB, BKL, MSS, and DV conceptualized and designed the study. LS, AB, BKL, and DV conducted the statistical analysis. LS, AB, KKM, DC, and KA interpreted data. All authors drafted and critically revised the manuscript and approved the final version for submission.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.04.060.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Nuti S.V., Armstrong K. Lay Epidemiology and Vaccine Acceptance. JAMA. 2021;326(4):301. doi: 10.1001/jama.2021.11130. [DOI] [PubMed] [Google Scholar]
- 2.Karpur A., Vasudevan V., Shih A., Frazier T. Brief Report: Impact of COVID-19 in Individuals with Autism Spectrum Disorders: Analysis of a National Private Claims Insurance Database. J Autism Dev Disord. 2022;52(5):2350–2356. doi: 10.1007/s10803-021-05100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Croen L.A., Zerbo O., Qian Y., Massolo M.L., Rich S., Sidney S., et al. The health status of adults on the autism spectrum. Autism. 2015;19(7):814–823. doi: 10.1177/1362361315577517. [DOI] [PubMed] [Google Scholar]
- 4.Schott W., Tao S., Shea L. COVID-19 risk: Adult Medicaid beneficiaries with autism, intellectual disability, and mental health conditions. Autism. 2022;26(4):975–987. doi: 10.1177/13623613211039662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koyama A.K., Koumans E.H., Sircar K., Lavery A., Hsu J., Ryerson A.B., et al. Severe Outcomes, Readmission, and Length of Stay Among COVID-19 Patients with Intellectual and Developmental Disabilities. Int J Infect Dis. 2022;116:328–330. doi: 10.1016/j.ijid.2022.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hotez E., Hotez P.J., Rosenau K.A., Kuo A.A. Prioritizing COVID-19 vaccinations for individuals with intellectual and developmental disabilities. EClinicalMedicine. 2021;32 doi: 10.1016/j.eclinm.2021.100749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brondino N., Bertoglio F., Forneris F., et al. A Pilot Study on Covid and Autism: Prevalence, Clinical Presentation and Vaccine Side Effects. Brain Sci. 2021;11(7) doi: 10.3390/brainsci11070860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Autism Society. The Autism Society of America and National Disability Organizations Encourage the Autism and I/DD Community to be Prioritized for COVID-19 Vaccination. Accessed January 31, 2022, https://www.autism-society.org/news/the-autism-society-of-america-and-national-disability-organizations-encourage-the-autism-and-i-dd-community-to-be-prioritized-for-covid-19-vaccination/.
- 9.Diament M. CDC Urged To Prioritize COVID-19 Vaccines For People With Developmental Disabilities. Accessed 31 January 2022, https://www.disabilityscoop.com/2021/03/01/cdc-urged-to-prioritize-covid-19-vaccines-for-people-with-developmental-disabilities/29216/.
- 10.Yousuf H., van der Linden S., Bredius L., et al. A media intervention applying debunking versus non-debunking content to combat vaccine misinformation in elderly in the Netherlands: A digital randomised trial. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. J Am Acad Child Adolesc Psychiatry. 2011;50(6):540–542. doi: 10.1016/j.jaac.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 12.John R.PS., Knott F.J., Harvey K.N. Myths about autism: An exploratory study using focus groups. Autism. 2018;22(7):845–854. doi: 10.1177/1362361317714990. [DOI] [PubMed] [Google Scholar]
- 13.Keith J.M., Jamieson J.P., Bennetto L. The Importance of Adolescent Self-Report in Autism Spectrum Disorder: Integration of Questionnaire and Autonomic Measures. J Abnorm Child Psychol. 2019;47(4):741–754. doi: 10.1007/s10802-018-0455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bonsu N., Mire S.S., Sahni L.C., Berry L.N., Dowell L.R., Minard C.G., et al. Understanding Vaccine Hesitancy Among Parents of Children With Autism Spectrum Disorder and Parents of Children With Non-Autism Developmental Delays. J Child Neurol. 2021;36(10):911–918. doi: 10.1177/08830738211000505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shea L.L., Verstreate K., Nonnemacher S., Song W., Salzer M.S. Self-reported community participation experiences and preferences of autistic adults. Autism. 2021;25(5):1295–1306. doi: 10.1177/1362361320987682. [DOI] [PubMed] [Google Scholar]
- 16.Grosse S.D., Nichols P., Nyarko K., Maenner M., Danielson M.L., Shea L. Heterogeneity in Autism Spectrum Disorder Case-Finding Algorithms in United States Health Administrative Database Analyses. J Autism Dev Disord. 2021;28 doi: 10.1007/s10803-021-05269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke J.P., Jain A., Yang W., Kelly J.P., Kaiser M., Becker L., et al. Does a claims diagnosis of autism mean a true case? Autism. 2014;18(3):321–330. doi: 10.1177/1362361312467709. [DOI] [PubMed] [Google Scholar]
- 18.Coo H., Ouellette-Kuntz H., Brownell M., Shooshtari S., Hanlon-Dearman A. Validating an administrative data-based case definition for identifying children and youth with autism spectrum disorder for surveillance purposes. Can J Public Health. 2017;108(5):e530–e538. doi: 10.17269/CJPH.108.5963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stoddard J, Reynolds EK, Paris R, et al. The Coronavirus Impact Scale: Construction, Validation, and Comparisons in Diverse Clinical Samples, 2021. [DOI] [PMC free article] [PubMed]
- 20.Hamel L, Lopes L, Muñana C, Artiga S, Brodie M. KFF/The Undefeated Survey on Race and Health. Accessed January 31, 2022, https://www.kff.org/report-section/kff-the-undefeated-survey-on-race-and-health-main-findings/.
- 21.Guidry J.P.D., Laestadius L.I., Vraga E.K., Miller C.A., Perrin P.B., Burton C.W., et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi: 10.1016/j.ajic.2020.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johns Hopkins University. COVID-19 Community Response Survey Guidance. Accessed 15 March 2022, https://www.nlm.nih.gov/dr2/JHU_COVID-19_Community_Response_Survey_v1.3.pdf.
- 23.Pennsylvania Department of State. President of the United States - County Breakdown Results. Accessed June 23, 2021, https://www.electionreturns.pa.gov/General/CountyBreakDownResults?officeId=1&districtId=1&ElectionID=83&ElectionType=G&IsActive=0.
- 24.United States Census Bureau. Census of Population and Housing. Accessed June 23, 2021, https://data.census.gov.
- 25.StataCorp. Stata Statistical Software: Release 17. StataCorp LLC. https://www.stata.com/.
- 26.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing. https://www.R-project.org/.
- 27.Guilford J.P. The phi coefficient and chi square as indices of item validity. Psychometrika. 1941,;6(1):11–19. doi: 10.1007/BF02288569. [DOI] [Google Scholar]
- 28.Pennsylvania Department of Health. COVID-19 Vaccine Dashboard. Accessed July 19, 2021, https://www.health.pa.gov/topics/disease/coronavirus/Vaccine/Pages/Dashboard.aspx.
- 29.United States Centers for Disease Control and Prevention. COVID-19 Vaccinations in the United States. Accessed July 26, 2021, https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-Jurisdi/unsk-b7fc.
- 30.Flaherty D.K. The Vaccine-Autism Connection: A Public Health Crisis Caused by Unethical Medical Practices and Fraudulent Science. Ann Pharmacotherapy. 2011;45(10):1302–1304. doi: 10.1345/aph.1Q318. [DOI] [PubMed] [Google Scholar]
- 31.Davidson M. Vaccination as a cause of autism-myths and controversies. Dialogues Clin Neurosci. 2017;19(4):403–407. doi: 10.31887/DCNS.2017.19.4/mdavidson. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tamari J. The Divided States of Pennsylvania. Accessed July 19, 2021, https://www.inquirer.com/politics/election/a/pennsylvania-2020-differences-america-democrats-republicans-20201025.html.
- 33.United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). Bridged-Race Population Estimates 1990-2020 Request. CDC WONDER Online Database Accessed 4 February 2022. https://wonder.cdc.gov/bridged-race-v2020.html.
- 34.Jones D.R., Nicolaidis C., Ellwood L.J., Garcia A., Johnson K.R., Lopez K., et al. An Expert Discussion on Structural Racism in Autism Research and Practice. Autism Adulthood. 2020;2(4):273–281. doi: 10.1089/aut.2020.29015.drj. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maitland C.A., Rhodes S., O’Hare A., Stewart M.E. Social identities and mental well-being in autistic adults. Autism. 2021;25(6):1771–1783. doi: 10.1177/13623613211004328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chan D.V., Doran J.D., Galobardi O.D. Beyond Friendship: The Spectrum of Social Participation of Autistic Adults. J Autism Dev Disord. 2022 doi: 10.1007/s10803-022-05441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Causton-Theoharis J., Ashby C., Cosier M. Islands of Loneliness: Exploring Social Interaction Through the Autobiographies of Individuals With Autism. Intell Develop Disabil. 2009;47(2):84–96. doi: 10.1352/1934-9556-47.2.84. [DOI] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention (CDC). How to Tailor COVID-19 Vaccine Information to Your Specific Audience. Accessed January 31, 2022, https://www.cdc.gov/vaccines/covid-19/hcp/tailoring-information.html.
- 39.Pitt M.B., Hendrickson M.A. Providing a Second Opinion to Dr. Google with the WWW Framework. J General Internal Med : JGIM. 2021;37(1):222–224. doi: 10.1007/s11606-021-06895-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shelby A., Ernst K. Story and science: How providers and parents can utilize storytelling to combat anti-vaccine misinformation. Human Vaccines Immunotherapeut. 2013;9(8):1795–1801. doi: 10.4161/hv.24828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Healy C.M., Pickering L.K. How to Communicate With Vaccine-Hesitant Parents. Pediatrics (Evanston) 2011;127(Supplement_1):S127–S133. doi: 10.1542/peds.2010-1722S. [DOI] [PubMed] [Google Scholar]
- 42.Ishler K.J., Biegel D.E., Wang F., Olgac T., Lytle S., Miner S., et al. Service Use Among Transition-Age Youth with Autism Spectrum Disorder. J Autism Dev Disord. 2022;52(3):1051–1065. doi: 10.1007/s10803-021-04999-6. [DOI] [PubMed] [Google Scholar]
- 43.Song W., Shea L., Nonnemacher S.L., Brusilovskiy E., Townley G., Salzer M.S. Community Participation Comparison Between Adults on the Autism Spectrum and Adults in the General Population. J Autism Dev Disord. 2022;52(4):1610–1621. doi: 10.1007/s10803-021-05059-9. [DOI] [PubMed] [Google Scholar]
- 44.Agaronnik N., Campbell E.G., Ressalam J., Iezzoni L.I. Communicating with Patients with Disability: Perspectives of Practicing Physicians. J Gen Intern Med. 2019;34(7):1139–1145. doi: 10.1007/s11606-019-04911-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Beames J.R., Kikas K., O'Gradey-Lee M., Gale N., Werner-Seidler A., Boydell K.M., et al. A New Normal: Integrating Lived Experience Into Scientific Data Syntheses. Front Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.763005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Roux AM, Shattuck PT, Rast JE, Rava JA, Anderson KA. National Autism Indicators Report: Transition into young adulthood. 2015.
- 47.Shea L., Tao S., Marcus S.C., Mandell D., Epstein A.J. Medicaid Disruption Among Transition-Age Youth on the Autism Spectrum. Med Care Res Rev. 2021 doi: 10.1177/10775587211051185. 10775587211051185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Turcotte P., Mathew M., Shea L.L., Brusilovskiy E., Nonnemacher S.L. Service needs across the lifespan for individuals with autism. J Autism Dev Disord. 2016;46(7):2480–2489. doi: 10.1007/s10803-016-2787-4. [DOI] [PubMed] [Google Scholar]
- 49.Tran P., Tran L., Tran L. A Cross-Sectional Comparison of US Adult Diabetes Screening Levels by Disability Status. J Prim Prev. 2021;42(5):459–471. doi: 10.1007/s10935-021-00641-4. [DOI] [PubMed] [Google Scholar]
- 50.Saad M.A.E. The effectiveness of social stories among children and adolescents with Autism Spectrum Disorders: Meta- analysis. Psycho Educ Res Rev. 2016;5(2):50–59. [Google Scholar]
- 51.ASERT Collaborative. COVID-19 Vaccine Social Stories. Accessed January 31, 2022, https://paautism.org/resource/covid-19-vaccine-social-stories/.
- 52.Tsai R., Hervey J., Hoffman K., Wood J., Johnson J., Deighton D., et al. COVID-19 Vaccine Hesitancy and Acceptance Among Individuals With Cancer, Autoimmune Diseases, or Other Serious Comorbid Conditions: Cross-sectional, Internet-Based Survey. JMIR Public Health Surveill. 2022;8(1):e29872. doi: 10.2196/29872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Connell B, Jones M, Mace R, et al. The principles of universal design: Version 2.0. Center for Universal Design, North Carolina State University; 1997.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.