Abstract
Antineoplastic uptake by blast cells in acute myeloid leukemia (AML) could be influenced by influx and efflux transporters, especially solute carriers (SLCs) and ATP-binding cassette family (ABC) pumps. Genetic variability in SLC and ABC could produce interindividual differences in clinical outcomes. A systematic review was performed to evaluate the influence of SLC and ABC polymorphisms and their combinations on efficacy and safety in AML cohorts. Anthracycline intake was especially influenced by SLCO1B1 polymorphisms, associated with lower hepatic uptake, showing higher survival rates and toxicity in AML studies. The variant alleles of ABCB1 were related to anthracycline intracellular accumulation, increasing complete remission, survival and toxicity. Similar findings have been suggested with ABCC1 and ABCG2 polymorphisms. Polymorphisms of SLC29A1, responsible for cytarabine uptake, demonstrated significant associations with survival and response in Asian populations. Promising results were observed with SLC and ABC combinations regarding anthracycline toxicities. Knowledge of the role of transporter pharmacogenetics could explain the differences observed in drug disposition in the blast. Further studies including novel targeted therapies should be performed to determine the influence of genetic variability to individualize chemotherapy schemes.
Keywords: SLCO1B1, ABCB1, SLC29A1, ABCG2, ABCC1, polymorphism, anthracyclines, cytarabine, acute myeloid leukemia
1. Introduction
Acute myeloid leukemia (AML) is a clinically and biologically heterogeneous hematologic malignant disease characterized by an excess of blast cells in bone marrow and blood. Approximately 60–80% of young AML patients achieve complete remission (CR) using conventional 3 + 7 schedules of anthracyclines and cytarabine, which might be followed by an allogeneic hematopoietic stem cell transplant (allo-HSCT) to prevent relapse [1,2]. Unfortunately, half of these patients finally relapsed or died from different causes, including: low efficacy eliminating the minimal residual disease, severe toxicity of chemotherapy, refractory disease. This interindividual variability of outcomes between AML patients could be related to their genetic variability [3,4].
Drug uptake by blast cells can be affected by different transporters, including influx and efflux transporters, especially solute carriers (SLCs) and ATP-binding cassette family (ABC) pumps, respectively [3,4]. Previous pharmacogenetic studies have suggested that single nucleotide polymorphisms (SNPs) of SLC and ABC transporters may play a promising role in drug exposure and have been associated with clinical response and toxicity [3,4,5,6,7]. However, the findings and the interpretation of these individual studies appear contradictory and inconclusive. Furthermore, for new targeted therapies, potential drug–drug interactions with P-glycoprotein (P-gp), breast cancer resistance protein (BCRP) and organic anion transporting polypeptides (OATP) were tested in preclinical studies, but the influence of SNPs in these transporters is unknown in these new therapies. We performed a systematic review of all the studies that have analyzed polymorphisms of membrane transporters in AML patients.
2. Materials and Methods
Search Strategy and Selection of Studies
A systematic search was performed following the PRISMA guidelines by two independent reviewers (JEMV and ASA) [8]. Pubmed, EMBASE, the Cochrane Central Register, the Web of Science and the Database of Abstracts of Reviews of Effects (DARE) databases were searched without restrictions. In addition, the reference lists of important studies and reviews were hand searched. The reference lists of relevant reviews and studies were manually searched. The last literature search was conducted on 26 January 2022. This systematic review was included in the PROSPERO registry (ID 314292).
Similar keywords were used in different databases: (“ATP-binding cassette transporters” [MeSH Terms] or “organic anion transporters” [MeSH] or “organic cation transport proteins” [MeSH]) and “acute myeloid leukemia” [MeSH].
Studies that fulfilled the following criteria were included: (1) studies based on clinical data in AML patients (excluding preclinical and in vitro studies); (2) AML studies analyzing the associations between ABC and/or SLC polymorphisms and clinical response to chemotherapy; and (3) AML studies analyzing the impact on safety of ABC and/or SLC polymorphisms.
3. Results
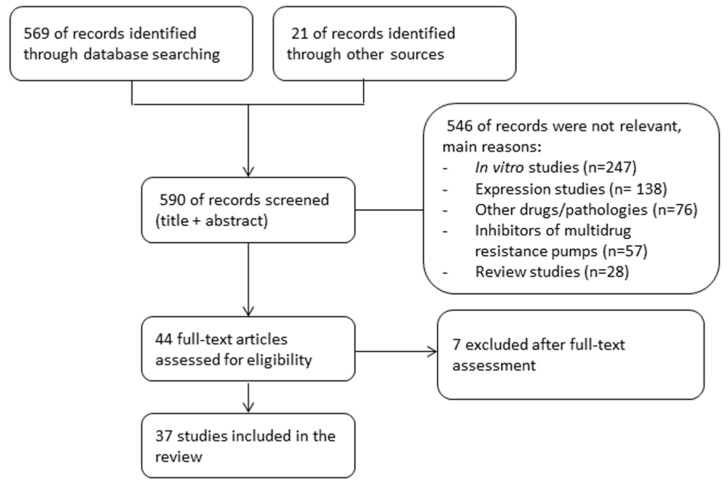
Our systematic search obtained 569 citations from databases and journals and 21 records were identified through other sources (Figure 1). Of the 44 citations selected for full reading, 37 fulfilled the inclusion criteria and were included. The agreement in the study selection between the reviewers was excellent (kappa = 0.97).
Figure 1.
Summary of evidence search and selection.
3.1. Influx Transporters: SLC Family
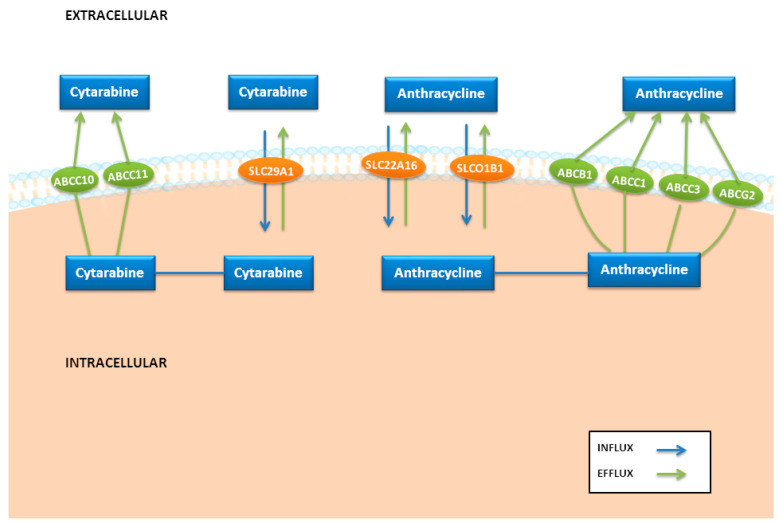
The intake by blast cells and other tissues of the antineoplastics employed in AML therapy and other xenobiotics is mediated by SLC transporters, a family that includes more than 400 transporters. Different SLC transporters have been related to anthracycline uptake, especially the organic anion transporter polypeptide-1B1 (OATP1B1, encoded by SLCO1B1) and the organic cation transporter SLC22A16 (Figure 2). However, cytarabine is mainly transported by human equilibrative nucleoside transporter (hENT1 and hENT2, encoded by the SLC29A1 and SCL29A2 genes; Figure 2), and in lower proportions by the human concentrative nucleoside transporters (hCNT3 encoded by the SLC28A3 gene).
Figure 2.
Key candidate genes involved in drug transport in acute myeloid leukemia.
The OATP1B1 (SLCO1B1) is predominantly expressed in the liver and is involved in the hepatic uptake and plasma clearance of several organic anionic compounds, including anthracyclines and other drugs such as statins [9,10,11,12]. The most relevant SLCO1B1 polymorphisms are 521T>C (rs4149056), 388A>G (rs2306283) and 597C>T (rs2291075), which are partially in linkage disequilibrium. The minor allele of rs4149056 has been consistently associated with a lower hepatic uptake and higher drug circulating concentrations, increasing the plasma levels and the risk of toxicity in tissues [10,11]. In AML studies (Table 1), the variant allele of SLCO1B1 rs4149056 was associated with a higher liver toxicity in adult patients [5] and higher overall survival (OS) in AML children [13]. In a recent study, the wild-type TT genotype of this SNP was related to a higher induction death, probably associated with a higher idarubicin uptake in tissues and therefore a higher potential toxicity [14]. The previous study in AML pediatric patients also obtained a higher OS and event-free survival (EFS) in carriers of the variant allele of the SLCO1B1 polymorphism (rs2291075), as well as those of the SLCO1B1 haplotype *1A/*1A,*1B/*1B (rs2291075, rs4149056 and rs2306283) [13].
Table 1.
Characteristics of the studies included in the systematic review for influx transporters.
| SNP | Study | n | Age (Range) | Ethnia (Country) |
HWE | LMA Status (%) | Chemotherapy Scheme | Clinical Outcomes |
|---|---|---|---|---|---|---|---|---|
| SLCO1B1 | ||||||||
| T521C rs4149056 |
Iacobucci et al., 2012 [5] | 94 | 51 (19–65) |
Caucasian (Italy) |
Yes | De novo (80.9%) Secondary (19.1%) |
Ara C + IDA + FLUDA + GO |
|
| Drenberg et al., 2016 [13] 1 | 164 | 9.1 (0–21) |
White (70%) Black (20%) Others (10%) |
Yes | De novo | Ara C + DAUNO + ETOP + MIT |
|
|
| Megías-Vericat et al., 2021 [14] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| 597C>T rs2291075 |
Drenberg et al., 2016 [13] 1 | 164 | 9.1 (0–21) |
White (70%) Black (20%) Others (10%) |
Yes | De novo | Ara C + DAUNO + ETOP + MIT |
|
| 388A>G rs2306283 |
Drenberg et al., 2016 [13] 1 | 164 | 9.1 (0–21) |
White (70%) Black (20%) Others (10%) |
Yes | De novo | Ara C + DAUNO + ETOP + MIT |
|
| SLC22A12 | ||||||||
| T1246C rs11231825 |
Iacobucci et al., 2012 [5] | 94 | 51 (19–65) |
Caucasian (Italy) |
Yes | De novo (80.9%) Secondary (19.1%) |
Ara C + IDA + FLUDA + GO |
|
| rs528211 (G>A) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs2360872 (C>T) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs505802 (A>G) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs524023 (G>A) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs9734313 (T>C) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs11231825 (C>T) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs11606370 (A>C) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs893006 (T>G) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| SLC22A16 | ||||||||
| rs12210538 1226A>G |
Megías-Vericat et al., 2021 [14] | 225 | 52.5 (16–78) |
Caucasian (Spain) |
Yes | De novo | Ara C + IDA |
|
| rs714368 146A>G |
Megías-Vericat et al., 2021 [14] | 225 | 52.5 (16–78) |
Caucasian (Spain) |
Yes | De novo | Ara C + IDA |
|
| SLC25A37 | ||||||||
| rs7818607 (C>A) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs8534 (C>T) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
|
CNT1
(SLC28A1) |
||||||||
| G565A rs2290272 |
Müller et al., 2008 [18] | 139 | 46.3 (15–86) |
Jews (61.2%) Arabs (38.8%) |
Yes | De novo | Ara C + ANT ± FLUDA ± MIT |
|
| C1561T rs2242046 |
Seeringer et al., 2009 [19] 3 | 322 | <60 | Caucasian (Germany) |
NR | NR (normal cytogenetic status) | Ara C + IDA + ETOP |
|
| rs8025045 (G>T) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) | Asian (China) |
Yes | De novo | Ara C + ANT |
|
| SLC28A2 | ||||||||
| rs10519020 (G>C) |
Drenberg et al., 2016 [13] 1 | 164 | 9.1 (0–21) |
White (70%) Black (20%) Others (10%) |
Yes | De novo | Ara C + DAUNO + ETOP + MIT |
|
| SLC28A3 | ||||||||
| rs11140500 (C>T) |
Yee et al., 2013 [16] 2 | 154 | NR | Caucasian (Europe) | NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
|
hENT1
(SLC29A1) |
||||||||
| C469A rs3734703 |
Kim et al., 2013 [44] 4 | 97 | 50 (16–76) | Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
| Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| Cao et al., 2017 [20] | 206 | 67.2 (22–98) | Asian (China) |
Yes | De novo | Ara C + ANT |
|
|
| C>T rs9394992 |
Wan et al., 2014 [45] | 100 | 43 (17–76) |
Asian (China) |
Yes | De novo | Ara C + DAUNO or IDA |
|
| Amaki et al., 2015 [46] | 39 | 54 (23–71) |
Asian (Japan) |
Yes | De novo | Ara C + IDA or DAUNO (consolidation: Ara C high doses) |
|
|
| Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| T>C rs324148 |
Wan et al., 2014 [45] | 100 | 43 (17–76) |
Asian (China) |
Yes | De novo | Ara C + DAUNO or IDA |
|
| Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| A>C rs693955 |
Amaki et al., 2015 [46] | 39 | 54 (23–71) |
Asian (Japan) |
Yes | De novo | Ara C + IDA or DAUNO (consolidation: Ara C high doses) |
|
| Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| rs507964 (A>C) |
Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
| rs747199 (C>G) |
Kim et al., 2016 [43] | 103 | 50.4 (16–76) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
Abbreviations: AMSA: amsacrine; ANT: anthracycline; BUSUL: busulfan; CR: complete remission; DAUNO: daunorubicin; DFS: disease-free survival; EFS: event-free survival; ETOP: etoposide; FLUDA: fludarabine; GO: gemtuzumab–ozogamicin; HWE: Hardy–Weinberg equilibrium; IDA: idarubicin; MIT: mitoxantrone; NR: not reported; OS: overall survival; RFS: relapse-free survival; RR: rate of relapse; TX: hematologic transplant. 1—This study [13] analyzed 1936 SNPs of 225 genes with a multi-SNP-based approach (including ABC and SLC transporters). Only SNPs with significant results were cited. 2—This study [16] analyzed 1659 SNPs of 42 genes with multi-SNP based approach. Only SNPs with significant results were cited. 3—This study [19] included SNPs of genes potentially involved in the response to Ara C (hCNT1, hENT1, hENT2, DCK, CDA), but only specified the SNPs with significant effect. 4—This study [44] included 139 SNPs of 10 genes potentially involved in the response to Ara C, but only specified the SNPs with significant effect.
SLC22A12 encodes a solute carrier that is mainly expressed in kidney and other tissues and is involved in urate–anion exchange [15]. Moreover, it is associated with the transport of different drugs, especially uricosurics (allopurinol and oxypurinol). The wild-type homozygote of SLC22A12 rs11231825 showed a higher infusion-related reactions after gemtuzumab ozogamicin administration (Table 1) [5]. An association between the wild-type genotypes of different SLC22A12, SLC25A37 and SLC28A3 polymorphisms showed a lower disease-free survival (DFS), although these associations were lost after the correction for multiple testing (Table 1) [16].
SLC22A16 encodes an organic cation transporter of L-carnitine, a metabolism cofactor related to different disease states. This carrier also imports several drugs, including anthracyclines. This transporter is constitutively expressed in the brain and kidney. SLC22A16 is over-expressed in AML and is related to the growth and viability of the blast cells, providing a potential target for future AML therapies [17]. In breast cancer cohorts, variant alleles of SLC22A16 (rs714368) were found to be related to higher exposure levels of doxorubicin and doxorubicinol [6] and dose delays by anthracycline toxicities (lower with rs714368, rs6907567, rs723685 and higher with rs12210538) [7]. In a recent AML study, associations were not observed between SLC22A16 rs12210538 and rs714368 and response or safety outcomes (Table 1) [14].
The concentrative nucleoside transporter hCNT1 encoded by the SLC28A1 gene has a substrate specificity for physiological pyrimidine nucleosides. Besides this function, hCNT1 has been implicated in tumor suppression. Various SLC28A1 SNPs were analyzed in several AML studies [18,19,20] (Table 1). Carriers of the SLC28A1 rs2242046 polymorphism showed a higher neutropenia [19], whereas studies with SLC28A1 rs2290272 [18] and SLC28A1 rs8025045 [20] did not find any clinical association. SLC28A2 encodes a sodium-dependent selective transporter of purines expressed in the kidney and other tissues. Only a pediatric AML study found a lower OS and EFS with the wild-type genotype of SLC28A2 rs10519020 [13].
hCNT3 (SLC28A3 gene) is a sodium-dependent pyrimidine and purine nucleoside carrier expressed in the pancreas, trachea, bone marrow and mammary glands. hCNT3 is a minor cytarabine transporter compared to hENT1, and this carrier has been associated with the uptake of different anthracyclines [21]. In four pediatric cancer cohorts, the variant alleles of SLC28A3 rs7853758 and rs885004 were correlated with cardiotoxicity associated with anthracyclines (doxorubicin and daunorubicin) [22,23,24,25], whereas this finding with SLC28A3 rs7853758 was not reproduced in cohorts of breast cancer [26,27] or B-cell lymphoma [28]. SLC28A3 rs7853758 and rs885004 SNPs are in high linkage disequilibrium and have been related to lower expression in different cell lines [29,30]. Only one study in AML patients has reported an association of SLC28A3 rs11140500 with a lower DFS, but the significance disappeared after Bonferroni correction (Table 1) [16].
hENT1 (encoded by the SLC29A1 gene) is responsible for up to 80% of cytarabine influx in blast cells. Schemes with high doses of cytarabine (2–3 g/m2 daily), used in consolidation or intensification therapy, can saturate the pump-mediated transport of hENT1 with concentrations >10 µmol/L and produce free diffusion into the cell [31,32]. Nevertheless, intracellular cytarabine concentrations obtained with induction therapy (200 mg/m2) are mediated by hENT1 [33]. Moreover, the intracellular influx is strongly correlated with the abundance of hENT1 in cell surface [34], so the bioavailability and clinical response depend on hENT1 expression [35]. In addition, SLC29A1 expression can be affected by hypoxia inducible factor 1 (Hif-1) at the promoter or by the transcription factor peroxisome proliferator activated receptorα (PPARα) [36,37]. In AML, patients with a low SLC29A1 mRNA expression had a significantly shorter DFS and OS in an adult cohort [38], but this had no influence in a pediatric AML cohort [39].
Two nonsynonymous and four synonymous polymorphisms were identified in a functional study of SLC29A1, but no influence in cytarabine uptake was measured [40]. In contrast, the haplotype of three SLC29A1 polymorphisms (−1345C>G, −1050G>A and 706G>C) was correlated with higher mRNA expression [41]. Another study showed only a modest elevation in hENT1 gene expression with the variant −706G>C, but no influence on cytarabine toxicity in normal blood cells [42]. The minor alleles of SLC29A1 polymorphisms only reach relevant frequencies in Asian populations, as is reflected in AML studies (Table 1). The variant A allele SLC29A1 rs3734703 was associated with a lower OS and RFS alone [43] or combined with TYMS rs2612100 [44], but a higher CR was related to the A allele [20] and CC + AA genotypes [43]. The SLC29A1 rs9394992 polymorphism was related to a lower CR [43], OS, DFS and mRNA expression, and a higher relapse rate (RR) [45], but no influence was found in another cohort [46]. Similarly, the variant allele of SLC29A1 rs324148 (alone or in combination rs9394992) was associated with a lower OS, DFS and mRNA expression, and a higher RR [45], as well as a higher CR haplotype ht3 with rs3734703, rs9394992, rs693955, rs507964 and rs747199 but had no effect alone [43]. On the other hand, the SLC29A1 rs693955 polymorphism was correlated to a lower time to relapse and neutropenia recovery [4].
3.2. Efflux Transporters: ABC Family
The ABC family of transporters includes several efflux pumps involved in the active efflux of drugs and xenobiotics from inside the cells with a potential increase in drug resistance [47]. The effect of these pumps is well-known in anthracycline disposition in blast cells and tissues, highlighting ABCB1, ABCC1, ABCC3 and ABCG2 (Figure 2) [47,48]. In addition, cytarabine uptake is influenced by two members of the “multidrug resistance-associated protein” (MRP) family, MRP7 and MRP8 (encoded by ABCC10 and ABCC11 genes), which have been related to deoxynucleotide efflux (Figure 2) [49,50].
The P-glycoprotein (P-gp), encoded by the ABCB1 gene, is the most studied efflux pump of the ABC family. The pharmacogenetics of ABCB1 have been widely analyzed in AML patients (Table 2), especially ABCB1 3435C>T (rs1045642), 2677G>A/T (rs2032582) and 1236C>T (rs1128503) polymorphisms [13,16,19,20,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69]. An in vitro study associated the P-gp expression with a lower intracellular daunorubicin accumulation [70]. The pharmacokinetics of daunorubicin and its metabolite daunorubicinol were not affected by ABCB1 polymorphisms, nor was mRNA expression in an Indian AML cohort [69]. However, previous studies in breast cancer have shown a higher doxorubicin clearance and lower peak levels of doxorubicinol with the wild-type haplotype of ABCB1 [47].
Table 2.
Characteristics of the studies included in the systematic review for polymorphisms of the ABC transporter family.
| SNP | Study | n | Age (Range) | Ethnia (Country) | HWE | LMA Status (%) | Chemotherapy Scheme | Clinical Outcomes |
|---|---|---|---|---|---|---|---|---|
| ABCB1 | ||||||||
| C3435T rs1045642 |
Illmer et al., 2002 [51] | 405 | 53 (17–78) |
Caucasian (Germany) |
Yes | De novo | Ara C+ MIT + ETOP + AMSA |
|
| Kaya et al., 2005 [52] | 28 | 36 (20–64) |
Arabs (Turkey) |
NR | NR | Ara C + ANT |
|
|
| Kim DH et al., 2006 [53] | 81 | 39 (15–72) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| Van der Holt et al., 2006 [54] 1 | 150 (130) | 67 (60–85) |
Caucasian (Netherlands) |
No | De novo: 79Secondary: 21 | Ara C + DAUNO |
|
|
| Hur et al., 2008 [55] | 200 | 44 (NR) | Asian (South Korea) |
Yes | De novo | Ara C + ANT |
|
|
| Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
|
| Green et al., 2012 [57] | 100 | 63 (20–85) |
Caucasian (Europe) |
Yes | De novo (normal karyotype) | Ara C + ANT or MIT +/or Others |
|
|
| Scheiner et al., 2012 [58] 2 | 109 (44) | 34 (<1–86) |
Others: White (69.7%) Non-white (30.3%) |
No | De novo: 72.5Secondary: 18.3 | Ara C + IDA |
|
|
| Falk et al., 2014 [59] 3 | 201 | 59 (18–85) |
Caucasian (Sweden) |
Yes | De novo (normal karyotype) | Ara C + DAUNO or IDA ± ETOP +/or Others |
|
|
| He et al., 2014 [60] | 215 | 43.6 (14–57) |
Asian (China) |
Yes | De novo | Ara C (high doses) |
|
|
| He et al., 2015 [61] | 263 | 45.4 (14–58) |
Asian (China) |
Yes | De novo (intermediate cytogenetic risk) | Ara C + DAUNO ± MIT |
|
|
| Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
|
| Short et al., 2020 [64] | 104 | 68 (24–88) |
Caucasian (86%) Black (13%) |
NR | AML 82De novo: 43.9Secondary: 56.1 | GO + DAC |
|
|
| G2677T/A rs2032582 |
Van den Heuvel et al., 2001 [65] | 30 | 34.6 (1–67) |
Caucasian (Netherlands) |
NR | Relapsed: 100 | Ara C + ANT + Others |
|
| Illmer et al., 2002 [51] | 405 | 53 (17–78) |
Caucasian (Germany) |
Yes | De novo | Ara C+ MIT + ETOP + AMSA |
|
|
| Kaya et al., 2005 [52] | 28 | 36 (20–64) |
Arabs (Turkey) |
NR | NR | Ara C + ANT |
|
|
| Kim DH et al., 2006 [53] | 81 | 39 (15–72) |
Asian (South Korea) |
Yes | De novo | Ara C + IDA |
|
|
| Van der Holt et al., 2006 [54] 1 | 150 (142) | 67 (60–85) |
Caucasian (Netherlands) |
Yes | De novo: 79Secondary: 21 | Ara C + DAUNO |
|
|
| Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
|
| Kim YK et al., 2010 [66] | 94 | 38 (17–79) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA +BH-AC |
|
|
| Green et al., 2012 [57] | 100 | 63 (20–85) |
Caucasian (Europe) |
Yes | De novo (normal karyotype) | Ara C + ANT or MIT +/or Others |
|
|
| Falk et al., 2014 [59] 3 | 201 | 59 (18–85) |
Caucasian (Sweden) |
Yes | De novo (normal karyotype) | Ara C + DAUNO or IDA ± ETOP +/or Others |
|
|
| He et al., 2014 [60] | 215 | 43.6 (14–57) |
Asian (China) |
Yes | De novo | Ara C (high doses) |
|
|
| He et al., 2015 [61] | 263 | 45.4 (14–58) |
Asian (China) |
Yes | De novo (intermediate cytogenetic risk) | Ara C + DAUNO ± MIT |
|
|
| Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
|
| C1236T rs1128503 |
Illmer et al., 2002 [51] | 405 | 53 (17–78) |
Caucasian (Germany) |
Yes | De novo | Ara C+ MIT + ETOP + AMSA |
|
| Van der Holt et al., 2006 [54] 1 | 150 (115) | 67 (60–85) |
Caucasian (Netherlands) |
Yes | De novo: 79Secondary: 21 | Ara C + DAUNO |
|
|
| Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
|
| Kim YK et al., 2010 [66] | 94 | 38 (17–79) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA +BH-AC |
|
|
| Green et al., 2012 [57] | 100 | 63 (20–85) |
Caucasian (Europe) |
Yes | De novo (normal karyotype) | Ara C + ANT or MIT +/or Others |
|
|
| Scheiner et al., 2012 [58] 2 | 109(44) | 34 (<1–86) |
Others: White (69.7%) Non-white (30,3%) |
Yes | De novo: 72.5Secondary: 18.3 | Ara C + IDA |
|
|
| Falk et al., 2014 [59] 3 | 201 | 59 (18–85) |
Caucasian (Sweden) |
Yes | De novo (normal karyotype) | Ara C + DAUNO or IDA ± ETOP +/or Others |
|
|
| He et al., 2014 [60] | 215 | 43.6 (14–57) |
Asian (China) |
No | De novo | Ara C (high doses) |
|
|
| He et al., 2015 [61] | 263 | 45.4 (14–58) |
Asian (China) |
Yes | De novo (intermediate cytogenetic risk) | Ara C + DAUNO ± MIT |
|
|
| Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
|
| Short et al., 2020 [64] | 104 | 68 (24–88) |
Caucasian (86%) Black (13%) |
NR | AML 82De novo: 43.9Secondary: 56.1 | GO + DAC |
|
|
| G1199A rs2229109 |
Green et al., 2012 [57] | 100 | 63 (20–85) |
Caucasian (Europe) |
Yes | De novo (normal karyotype) | Ara C + ANT or MIT +/or Others |
|
| Falk et al., 2014 [59] 3 | 201 | 59 (18–85) |
Caucasian (Sweden) |
Yes | De novo (normal karyotype) | Ara C + DAUNO or IDA ± ETOP +/or Others |
|
|
| C174967T rs6980101 |
Kim YK et al., 2007 [67] | 49 | 37 (17–69) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA |
|
| G146792C rs10256836 |
Kim YK et al., 2007 [67] | 49 | 37 (17–69) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA |
|
| T134575A rs17327442 |
Kim YK et al., 2007 [67] | 49 | 37 (17–69) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA |
|
| A113516G rs4148732 |
Kim YK et al., 2007 [67] | 49 | 37 (17–69) |
Asian (South Korea) |
NR | De novo (t (8,21) and inv (16)) | Ara C + IDA |
|
| C193T rs121918619 |
Monzo et al., 2006 [67] | 110 | 44 (16–60) |
Caucasian (Spain) |
Yes | De novo (intermediate cytogenetic risk) | Ara C + IDA + ETOP |
|
| Illet144Met | Monzo et al., 2006 [68] | 110 | 44 (16–60) |
Caucasian (Spain) |
NR | De novo (intermediate cytogenetic risk) | Ara C + IDA + ETOP |
|
| rs3842 (A>G) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) |
Asian (China) |
Yes | De novo | Ara C + ANT |
|
| rs2235015 (G>T) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) | Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| rs2235033 (T>C) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| rs1922242 (A>T) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| rs1922240 (T>C) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| rs1989830 (C>T) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| rs2235040 (G>A) |
Rafiee et al., 2019 [63] | 942 | 9.7 (0–30) |
Caucasian (81%) Black (13%) Asian (5%) Others (1%) |
Yes | De novo | Ara C + IDA + ETOP ± GO |
|
| ABCB11 | ||||||||
| rs4668115 (G>A) |
Drenberg et al., 2016 [13] 4 | 164 | 9.1 (0–21) |
White (70%) Black (20%) Others (10%) |
Yes | De novo | Ara C + DAUNO + ETOP + MIT |
|
| ABCC1 | ||||||||
| T2684C | Mahjoubi et al., 2008 [82] | 111 | NR | Arabs (Iran) |
NR | 52 AMLNR | NR |
|
| C2007T rs2301666 |
Mahjoubi et al., 2008 [82] | 111 | NR | Arabs (Iran) |
NR | 52 AMLNR | NR |
|
| G2012T rs45511401 |
Mahjoubi et al., 2008 [82] | 111 | NR | Arabs (Iran) |
NR | 52 AMLNR | NR |
|
| C2665T | Mahjoubi et al., 2008 [82] | 111 | NR | Arabs (Iran) |
NR | 52 AMLNR | NR |
|
| T825C rs246221 |
Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
| T1062C rs35587 |
Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
| G4002A rs2230671 |
Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
| rs4148350 (G>T) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
| rs129081 (C>G) |
Kunadt et al., 2020 [83] 5 | 160 | 46 (18–60) |
Caucasian (Germany) |
Yes | NK AMLDe novo: 93.1Secondary: 6.9 | Ara C + DAUNO |
|
| rs212090 (A>T) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) |
Asian (China) |
Yes | De novo | Ara C + ANT |
|
| Kunadt et al., 2020 [83] 5 | 160 | 46 (18–60) |
Caucasian (Germany) |
Yes | NK AMLDe novo: 93.1Secondary: 6.9 | Ara C + DAUNO |
|
|
| rs212091 (A>G) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) |
Asian (China) |
Yes | De novo | Ara C + ANT |
|
| Kunadt et al., 2020 [83] 5 | 160 | 46 (18–60) |
Caucasian (Germany) |
Yes | NK AMLDe novo: 93.1Secondary: 6.9 | Ara C + DAUNO |
|
|
| rs3743527 (C>T) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) |
Asian (China) |
Yes | De novo | Ara C + ANT |
|
| rs4148380 (G>A) |
Cao et al., 2017 [20] | 206 | 67.2 (22–98) |
Asian (China) |
Yes | De novo | Ara C + ANT |
|
| ABCC2 | ||||||||
| G4544A rs8187710 |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
| ABCC3 | ||||||||
| 45 + 1226 (T>G) rs4148405 |
Yee et al., 2013 [16] 6 | 154 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| Butrym et al., 2021 [85] | 95 | 61 (22–90) |
Caucasian (Poland) |
Yes | De novo | Ara C + DAUNO or low dose Ara C or AZA |
|
|
| rs1989983 (G>A) |
Yee et al., 2013 [16] 6 | 54 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs2301835 (C>T) |
Yee et al., 2013 [16] 6 | 154 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs2277624 (A>G) |
Yee et al., 2013 [16] 6 | 154 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs8079740 (A>G) |
Yee et al., 2013 [16] 6 | 154 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| rs757420 (T>C) |
Yee et al., 2013 [16] 6 | 154 | NR | Caucasian (Europe) |
NR | NR | Ara C + ETOP + BUSUL (pre-TX) |
|
| C211T rs4793665 |
Müller et al., 2008 [18] | 139 | 46.3 (15–86) |
Jews (61.2%) Arabs (38.8%) |
Yes | De novo | Ara C + ANT ± FLUDA ± MIT |
|
| Butrym et al., 2021 [88] | 95 | 61 (22–90) |
Caucasian (Poland) |
Yes | De novo | Ara C + DAUNO or low dose Ara C or AZA |
|
|
| ABCG2 | ||||||||
| G34A rs2231137 |
Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
NR | De novo: 75Secondary: 25 | Ara C + ANT |
|
| Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
|
| Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| C421A rs2231142 |
Müller et al., 2008 [18] | 139 | 46.3 (15–86) |
Jews (61.2%) Arabs (38.8%) |
Yes | De novo | Ara C + ANT ± FLUDA ± MIT |
|
| Hampras et al., 2010 [56] | 261 | 61.5 (20–85) |
Caucasian (86%) Others (14%) (USA) |
Yes | De novo: 75Secondary: 25 | Ara C + ANT |
|
|
| Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
|
| Tiribelli et al., 2013 [98] | 125 | 59.2 (20–84) |
Caucasian (Italy) |
Yes | NR | Ara C + IDA + FLUDA ± ETOP |
|
|
| Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) |
Caucasian | Yes | De novo | Ara C + IDA |
|
|
| Ile619Ile (C>T) |
Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
| rs2231149 (C>T) |
Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
| rs2231162 (C>T) |
Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
| rs2231164 (C>T) |
Wang et al., 2011 [97] | 141 | 32 (5–70) |
Asian (China) |
NR | De novoMixed with ALL | Ara C + DAUNO/MITO |
|
Abbreviations: ALL: acute lymphoblastic leukemia; AML: acute myeloid leukemia; AMSA: amsacrine; ANT: anthracycline; AZA: azacitidine; BH-AC: N4-behenoyl-1D-arabinofuranosycytosine; BUSUL: busulfan; CIR: cumulative incidence of relapse; CR: complete remission; DAC: decitabine; DAUNO: daunorubicin; DFS: disease-free survival; EFS: event-free survival; ETOP: etoposide; FLUDA: fludarabine; GO: gemtuzumab ozogamicin; HWE: Hardy–Weinberg equilibrium; IDA: idarubicin; MIT: mitoxantrone; NK: normal karyotype; NR: not reported; ORR: overall response rate; OS: overall survival; RFS: relapse-free survival; RR: rate of relapse; R/R: relapse/refractory; TX: hematologic transplant. 1—Allele frequency and treatment outcomes only reported in 115 patients for C1236T, 142 patients for G2677T/A and 130 patients for C3435T. 2—Allele frequency only reported in 103 patients and treatment outcomes only in 44 patients (AML M3 subtype, secondary AML and patients with comorbidities or poor performance status were excluded). 3—A total of 100 patients were previously collected and published in Green et al., 2012 [57]. 4—This study [13] analyzed 1936 SNPs of 225 genes with a multi-SNP-based approach (including ABC and SLC transporters). Only SNPs with significant results were cited. 5—This study [83] included 48 SNPs within 7 genes of 7 ABC transporters (ABCA2, ABCA3, ABCB1, ABCB2, ABCB5, ABCB7 and ABCC1), but only specified the SNPs with significant effect. 6—This study [16] analyzed 1659 SNPs of 42 genes with a multi-SNP-based approach. Only SNPs with significant results were cited.
Lower pump function was related to the variant alleles of ABCB1, favoring anthracycline intracellular accumulation with a higher potential efficacy and toxicity [61,71,72], but some studies did not reproduce this effect [51,54,58]. Following this hypothesis, better responses (higher CR and survival rates) has been reported in AML cohorts with different ABCB1 polymorphisms [51,57,59,61,63,65,66,67,68], whereas in other studies, these SNPs showed no influence or a worse response [20,53,54,55,56,58,62,64] (Table 2). This finding of a higher CR and OS with variant alleles of ABCB1 3435C>T, 2677G>A/T and 1236C>T was reproduced in two meta-analyses [73,74]. The study of Rafiee et al. showed an association between these 3 ABCB1 SNPs and a higher EFS and DFS and a lower relapse rate on gemtuzumab ozogamicin, highlighting the role of P-gp in calicheamicin efflux [64].
The toxicity of anthracyclines has only been evaluated in four AML studies, showing no associations in two studies [54,56] and relevant anthracycline related-toxicities in two studies [60,62]. He et al. found higher nausea and vomiting grades (3/4) with wild-type genotypes of ABCB1 3435C>T and 2677G>A/T (alone and in haplotype) in an Asian cohort [60]. On the other hand, in a Caucasian cohort, the variant alleles of ABCB1 3435C>T, 2677G>A/T and 1236C>T and their haplotypes were associated with higher organ toxicities (renal, hepatic and neutropenia), as well as with higher induction death [62]. In other malignancies, ABCB1 SNPs were correlated with higher cardiotoxicity [22,23,75,76], but this was not reproduced in these AML studies [54,56,60,62], nor in a large study analyzing the potential correlation between ABCB1 polymorphisms and the left ventricular ejection fraction (LVEF) [77].
ABCB11 encodes a canalicular transporter of bile salts also called the “bile salt export pump” (BSEP) which has been associated with the efflux of some anticancer drugs in liver cells. The ABCB11 rs4668115 and ABCB4 rs2302387 polymorphisms reduced transporter expression and were found to be related to ≥grade 3 transaminitis after anthracycline infusion (mithramycin) in patients with refractory thoracic malignancies [78]. The wild-type genotype of ABCB11 rs4668115 was correlated with a lower OS and EFS in AML patients (Table 2) [13].
ABCC1 encodes the MRP1 pump, which mediates the export of organic anions and drugs from the cytoplasm, including methotrexate, antivirals and anthracyclines. The function of this pump confers resistance to anticancer drugs by decreasing their accumulation in cells and by mediating ATP- and GSH-dependent drug export [79]. Pharmacokinetic in vitro studies have shown decreased transport and higher maximum velocity (Vmax) of doxorubicin disposition with ABCC1 (rs60782127) [80], whereas MRP expression reduced the intracellular daunorubicin accumulation [70]. Previous studies in other cancers have associated ABCC1 (rs3743527, rs246221, rs4148350) with higher cardiotoxicity [22,23,27,81]. A small cohort performed in an Arab population correlated the expression of 4 ABCC1 SNPs with a lower CR, drug sensitivity and relapsed/refractory disease in acute leukemia (Table 2) [82]. Subsequently, several AML studies analyzed the role of different ABCC1 genotypes in clinical outcomes and safety (Table 2) [20,56,62,83]. Despite the fact that the association between cardiotoxicity and ABCC1 polymorphisms was not reproduced in AML [20,56,62,83], ABCC1 rs4148350 was related to hepatotoxicity [62], ABCC1 rs212090 with gastrointestinal toxicity and rs212091 and rs3743527 with myelosuppression [20]. In addition, the ABCC1 rs212090 and rs3743527 variant alleles showed lower survival rates, whereas ABCC1 rs129081 increased OS and DFS [83].
ABCC2 expresses MPR2, an export pump localized to the apical membrane of polarized cells, especially those hepatocytes with functions in biliary transport. This protein appears to contribute to the drug resistance of different anticancer drugs including anthracyclines [84]. Polymorphisms of ABCC2 have been correlated with anthracycline toxicities in other malignancies: cardiotoxicity in non-Hodgkin lymphoma (rs45511401) [26], in survivors of HSCT (rs8187710) [85] and in pediatric cancer (rs4148350) [22], febrile neutropenia in breast cancer (rs4148350) [27] and leucopenia in osteosarcoma (17222723) [86]. In AML patients, only one cohort has analyzed ABCC2 rs8187710, without any significant influence in response or toxicity [62].
ABCC3 encodes a protein that may play a role in biliary transport and the intestinal excretion of organic anions, which is also related to drug efflux. The expression of ABCC3 was found to be significantly higher in AML patients resistant to daunorubicin [87]. Clinical studies in AML cohorts corroborated this finding with ABCC3 polymorphisms (Table 2) [16,18,88]. A lower DFS was reported with variant alleles of ABCC3 polymorphisms (rs4148405, rs1989983, rs2301835, rs8079740), whereas other ABCC3 (rs2277624, rs757420) SNPs showed a higher DFS [16]. A similarly higher OS was observed with the variant allele of ABCC3, rs4793665 [18]. A recent cohort reproduced the previous findings of lower OS rates with the minor allele of ABCC3, rs4148405 [88].
The ABCC10 and ABCC11 genes encode the MRP7 and MRP8 pumps which can efflux cytarabine in blast cells [49,50]. Unfortunately, we have not found any studies regarding the genetic variability of ABCC10 and ABCC11 in AML populations. Sorafenib, an FLT3 inhibitor employed in AML, produces the inhibition of ABC pumps, avoiding the efflux of cytarabine by MRP7 and MRP8 pumps and thereby increasing the cytarabine-sensitivity of blast cells [89,90].
The ABCG2 gene expresses the “breast cancer resistant protein” (BCRP), a well-known ABC pump responsible for anthracycline efflux [91]. BCRP is localized in the cell membranes of epithelial cells of the small intestine, liver, kidney, brain and placenta [92]. In AML, an overexpression of ABCG2 was observed in 33% of blast cells and this BCRP expression correlated with a worse prognosis and lower OS [93,94,95,96]. The two most common ABCG2 SNPs are rs2231137 and rs2231142, and the minor alleles of these SNPs are related to a reduced level of BCRP expression [92]. No influence in anthracycline pharmacokinetics was reported with ABCG2 in an AML cohort with daunorubicin (rs2231137, rs2231142, rs769188) [69] or a breast cancer cohort with doxorubicin (rs2231142) [47]. Several studies have described the impact of ABCG2 genotypes in AML (Table 2) [18,56,62,97,98]. Contradictory results were observed with ABCG2 rs2231137, showing a lower OS and lower risk of toxicities ≥ grade three with the GG wild-type genotype in a Caucasian cohort [56], but a higher OS and DFS in a mixed AML/ALL Asian cohort [97] and no influence in a Caucasian cohort [62]. On the other hand, three different cohorts reproduced an increase in OS in wild-type ABCG2 rs2231142 carriers [56,97,98] and cardiac and lung toxicities were associated with the variant allele in another study [62]. Similar OS and DFS increases were obtained with the wild-type genotype of ABCG2 rs2231149, as well as with its haplotype with the ABCG2 rs2231137 and rs2231142 polymorphisms [97]. No effect in LVEF was observed with 16 different ABCG2 polymorphisms in a large study [77].
3.3. SNP-SNP Combinations of Transporters
Most of the included pharmacogenetic studies employed the candidate genes approach based on the pharmacologic pathway of the drugs. The drug intake depends on the combination of input and output transporters, but only a few studies analyzed the genetic variability of both types of carriers together. A recent study explored the combination of SLC wild-type genotypes (functional SLCO1B1 and/or SLC22A16), ensuring the anthracycline uptake in cells, with the variant genotypes of ABC pumps (defective expression of ABCB1, ABCC1, ABCC2 or ABCG2), avoiding anthracycline expulsion [14]. Several novel findings were reported with the combinations of ABCB1 and SLC polymorphisms, including higher hepatic and renal toxicities, mucositis and neutropenia, as well as a higher incidence of induction death (Table 3). All of these are probably associated with a higher intracellular idarubicin accumulation and have been previously reported with ABCB1 SNPs [62]. In addition, the combination of the SLC22A16 rs714368 wild-type genotype with the variant allele of ABCG2 rs2231142 was related to a higher cardiac toxicity (Table 3), reproducing the previous association [62]. On the other hand, no associations were found with ABCC1 rs4148350 and ABCC2 rs8187710 SNPs combined with SLCO1B1/SLC22A16 wild-type genotypes. Combinations of SLCO1B1 and ABC polymorphisms were also described with irinotecan [99,100] and statins [101,102]. Regarding cytarabine intake, two different studies analyzed the combined influence of SNPs in SLC29A1 with genes of the main enzymes of the cytarabine pathway (DCK, CDA, etc.) [43,44], but the combination with ABC pumps was not explored.
Table 3.
Characteristics of the studies included in the systematic review for SNP–SNP combinations of ABC and SLC transporters.
| SNP | Study | n | Age (Range) | Ethnia (Country) | HWE | LMA Status (%) | Chemotherapy Scheme | Clinical Outcomes |
|---|---|---|---|---|---|---|---|---|
| ABCB1 + SLC | ||||||||
|
ABCB1 C3435T rs1045642 SLCO1B1 rs4149056 (T>C) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 C3435T rs1045642 SLC22A16 rs12210538 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 G2677T/A rs2032582 SLCO1B1 rs4149056 (T>C) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 G2677T/A rs2032582 SLC22A16 rs12210538 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 G2677T/A rs2032582 SLC22A16rs714368 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 C1236T rs1128503 SLCO1B1 rs4149056 (T>C) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 haplotype 1 SLCO1B1 rs4149056 (T>C) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 haplotype 1 SLC22A16 rs12210538 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
|
ABCB1 haplotype 1 SLC22A16 rs714368 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
| ABCC1 + SLC | ||||||||
|
ABCC1 rs4148350 SLCO1B1/SLC22A16 |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
| ABCC2 + SLC | ||||||||
|
ABCC2 rs8187710 SLCO1B1/SLC22A16 |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
| ABCG2 + SLC | ||||||||
|
ABCG2 rs2231142 (C>A) SLC22A16 rs714368 (A>G) |
Megías-Vericat et al., 2017 [62] | 225 | 52.5 (16–78) | Caucasian | Yes | De novo | Ara C + IDA |
|
Abbreviations: AML: acute myeloid leukemia; CR: complete remission; HWE: Hardy–Weinberg equilibrium; IDA: idarubicin; NR: not reported; OS: overall survival. 1—The ABCB1 haplotype included the polymorphisms rs1128503, rs1045642 and rs2032582.
4. Conclusions
Transporters of the SLC and ABC families play crucial roles in the absorption, disposition and elimination of antineoplastic drugs. In AML, the expression of these transporters has been proposed as one of the main drug resistance mechanisms and has been widely studied for standard chemotherapy 3 + 7 schedules based on anthracyclines and cytarabine. However, the impact of genetic variability in the SLC and ABC genes remains controversial. This review aims is to demonstrate that polymorphisms in transporter genes may have a potential impact on the clinical outcomes of AML therapy.
Despite this, only a few studies have analyzed the role of SLC carriers in AML therapy; promising findings were obtained with polymorphisms in the SLCO1B1 and SLC29A1 genes. Variant alleles of SLCO1B1 were correlated with a lower function, decreasing anthracycline hepatic uptake and metabolism [10,11] and showed higher survival rates and toxicity in AML studies [5,13,14]. Polymorphisms of SLC29A1, responsible for cytarabine uptake, showed a relevant impact on CR and survival rates, especially in Asian populations [20,42,43,44,45].
Meanwhile, the variant alleles of ABCB1 have been widely studied in AML, demonstrating a clear association with lower pump function, as well as higher CR and survival rates in meta-analyses [73,74]. The influence of ABCB1 polymorphisms in anthracycline-related toxicities remains more controversial in AML, with scarce relevant findings [60,62] and without evidence of higher cardiotoxicity unlike studies in other malignancies [22,23,75,76]. Encouraging relationships were discovered in AML studies with ABCC1 [20,62,82,83] and ABCG2 polymorphisms [56,62,97,98].
SNP–SNP combinations of transporters could play a crucial role in characterizing the anthracycline pathway, which involves complex pharmacokinetic and pharmacodynamic mechanisms, although this was only evaluated in a Caucasian AML cohort [14]. In addition, it has been hypothesized that SNP–SNP combinations could increase the power of detection of significant associations where individual SNPs of SLC or ABC genes only demonstrate a minor effect that could be affected by their combination [103]. Combinations of transporters with other relevant SNPs such as enzymes have been explored in previous studies in AML with cytarabine [43,44].
The influence of ABC pumps in anthracycline pharmacokinetics has been suggested in vitro [70,80] and studies in other cancers [47], but a population pharmacokinetic study performed in AML failed to reproduce these findings with ABCB1 and ABCG2 polymorphisms [68]. Furthermore, the AML studies included did not analyze the influence of transporter SNPs together in drug pharmacokinetic levels and clinical response. In this line, a study in AML demonstrated a correlation between cytarabine plasma level and CDA genotype, the main enzyme responsible for liver metabolism of cytarabine [104]. In chronic myeloid leukemia, a relevant decrease in imatinib clearance was associated with variant alleles of ABCB1 and SLCO1B3 [105]. Similarly, in acute lymphoblastic leukemia, the SLCO1B1 521T>C SNP reduced methotrexate clearance [106]. Previous reviews focused on the impact of ABC and SLC SNPs in drug bioavailability have found the same limited evidence of PK studies in the AML context [47,107,108].
The influence of genetic variability in AML therapy has been previously analyzed by other authors, especially focused of the main SNPs of the cytarabine and anthracycline metabolic pathways [3,4,109,110] or only in SNPs of transporter genes [47,107,108,111]. Pinto et al. [112] recently performed a systematic review of the general state of pharmacogenetics in AML including, as a novelty, polymorphisms with a potential impact in new targeted therapies (e.g., FLT3 inhibitors, GO, hypomethylating agents and IDH inhibitors). On the other hand, our review centers on evaluating the influence of polymorphisms in transporter genes (SLC and ABC and their combinations) in AML studies, which was briefly explained in this recent review [112].
Most of the reported pharmacogenetic studies were performed in patients treated with a standard 3 + 7 scheme with a candidate genes approach. The importance of pharmacogenetics for the multiple new drugs recently approved for AML treatment remains unknown. Although these therapies are more tolerable than classical antineoplastics, potential drug–drug interactions involving P-gp, BCRP and OATP transporters have been described [113]. The genetic variability of SLC and ABC genes should be analyzed in further studies involving these novel therapies. In this line, a higher response to gemtuzumab ozogamicin was reported with the variant alleles of ABCB1 in a pediatric cohort [63], but no influence was observed in adult AML patients treated with gemtuzumab ozogamicin and decitabine [64].
In conclusion, pharmacogenetic studies based on candidate genes have reported relevant associations between SNPs in transporters (SLC and ABC) with AML outcomes and safety profiles. Unfortunately, most of these studies were observational and involved retrospective cohorts, and only anecdotally were these transporter genes analyzed together with metabolic enzymes, molecular targets and DNA repair genes. In the future, randomized clinical trials on larger populations including those of different age, ethnic and therapy groups should be developed in order to validate the clinical benefit of pharmacogenetics in AML patients.
Author Contributions
J.E.M.-V. and P.M. participated in discussions and development of the manuscript, A.S.-A., D.M.-C. and J.L.P. contributed to correcting the draft manuscript, provided additional recommendations and have read and approved the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by grants from the “Instituto Carlos III” (PIE13/00046) and the “Instituto Investigación Sanitaria La Fe” 2013/0331 and 2019-052-1 assigned to the Pharmacy and Hematology Departments. In addition, this work was partially supported by the Cooperative Research Thematic Network (RTICC), grant RD12/0036/014 (ISCIII & ERDF).
Conflicts of Interest
P.M. reports these potential conflicts of interest, AbbVie: advisory board, speakers bureau, research support; Astellas: research support, consultant, speakers bureau, advisory board; Agios: consultant; Tolero Pharmaceutical: consultant; Glycomimetics: consultant; Forma Therapeutics: consultant; Celgene: research support, consultant, speakers bureau, advisory board; Daiichi Sankyo: research support, consultant, speakers bureau, advisory board; Incyte: speakers bureau, advisory board; Janssen: research support, speakers bureau, advisory board; Karyopharm: research support, advisory board; Novartis: research support, speakers bureau, advisory board; Pfizer: research support, speakers bureau, advisory board; Teva: research support, speakers bureau, advisory board. D.M.-C. reports these potential conflicts of interest, Astellas: speakers bureau, advisory board; Daiichi Sankyo: advisory board; Jazz Pharmaceuticals: advisory board, speakers bureau; Novartis: advisory board; Teva: speakers bureau, advisory board. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tallman M.S., Wang E.S., Altman J.K., Appelbaum F.R., Bhatt V.R., Bixby D., Coutre S.E., De Lima M., Fathi A.T., Fiorella M., et al. Acute Myeloid Leukemia, Version 3.2019, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2019;17:721–749. doi: 10.6004/jnccn.2019.0028. [DOI] [PubMed] [Google Scholar]
- 2.Medeiros B.C., Chan S.M., Daver N.G., Jonas B.A., Pollyea D.A. Optimizing survival outcomes with post-remission therapy in acute myeloid leukemia. Am. J. Hematol. 2019;94:803–811. doi: 10.1002/ajh.25484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Megías-Vericat J.E., Montesinos P., Herrero M.J., Bosó V., Martínez-Cuadrón D., Poveda J.L., Sanz M.Á., Aliño S.F. Pharmacogenomics and the treatment of acute myeloid leukemia. Pharmacogenomics. 2016;17:1245–1272. doi: 10.2217/pgs-2016-0055. [DOI] [PubMed] [Google Scholar]
- 4.Megias-Vericat J.E., Martinez-Cuadron D., Herrero M.J., Alino S.F., Poveda J.L., Sanz M.A., Montesinos P. Pharmaco-genetics of metabolic genes of anthracyclines in acute myeloid leukemia. Curr. Drug Metab. 2018;19:55–74. doi: 10.2174/1389200218666171101124931. [DOI] [PubMed] [Google Scholar]
- 5.Iacobucci I., Lonetti A., Candoni A., Sazzini M., Papayannidis C., Formica S., Ottaviani E., Ferrari A., Michelutti A., Simeone E., et al. Profiling of drug-metabolizing enzymes/transporters in CD33+ acute myeloid leukemia patients treated with Gemtuzumab-Ozogamicin and Fludarabine, Cytarabine and Idarubicin. Pharm. J. 2012;13:335–341. doi: 10.1038/tpj.2012.13. [DOI] [PubMed] [Google Scholar]
- 6.Lal S., Wong Z.W., Jada S.R., Xiang X., Chen Shu X., Ang P.C., Figg W.D., Lee E.J., Chowbay B. Novel SLC22A16 polymorphisms and influence on doxorubicin pharmacokinetics in Asian breast cancer patients. Pharmacogenomics. 2007;8:567–575. doi: 10.2217/14622416.8.6.567. [DOI] [PubMed] [Google Scholar]
- 7.Bray J., Sludden J., Griffin M.J., Cole M., Verrill M., Jamieson D., Boddy A.V. Influence of pharmacogenetics on response and toxicity in breast cancer patients treated with doxorubicin and cyclophosphamide. Br. J. Cancer. 2010;102:1003–1009. doi: 10.1038/sj.bjc.6605587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee H.H., Leake B.F., Kim R.B., Ho R.H. Contribution of Organic Anion-Transporting Polypeptides 1A/1B to Doxorubicin Uptake and Clearance. Mol. Pharmacol. 2017;91:14–24. doi: 10.1124/mol.116.105544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Niemi M., Pasanen M.K., Neuvonen P.J. Organic Anion Transporting Polypeptide 1B1: A Genetically Polymorphic Transporter of Major Importance for Hepatic Drug Uptake. Pharmacol. Rev. 2011;63:157–181. doi: 10.1124/pr.110.002857. [DOI] [PubMed] [Google Scholar]
- 11.Oshiro C., Mangravite L., Klein T., Altman R. PharmGKB very important pharmacogene: SLCO1B1. Pharm. Genom. 2010;20:211–216. doi: 10.1097/FPC.0b013e328333b99c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Durmus S., Naik J., Buil L., Wagenaar E., van Tellingen O., Schinkel A.H. In vivo disposition of doxorubicin is affected by mouse Oatp1a/1b and human OATP1A/1B transporters. Int. J. Cancer. 2014;135:1700–1710. doi: 10.1002/ijc.28797. [DOI] [PubMed] [Google Scholar]
- 13.Drenberg C.D., Paugh S.W., Pounds S.B., Shi L., Orwick S.J., Li L., Hu S., Gibson A.A., Ribeiro R.C., Rubnitz J., et al. Inherited variation in OATP1B1 is associated with treatment outcome in acute myeloid leukemia. Clin. Pharmacol. Ther. 2016;99:651–660. doi: 10.1002/cpt.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Megías-Vericat J.E., Martínez-Cuadrón D., Herrero M.J., Rodríguez-Veiga R., Solana-Altabella A., Boluda B., Balles-taLópez O., Cano I., Acuña-Cruz E., Cervera J., et al. Impact of combinations of single-nucleotide polymorphisms of anthracycline transporter genes upon the efficacy and toxicity of induction chemo-therapy in acute myeloid leukemia. Leuk. Lymphoma. 2021;62:659–668. doi: 10.1080/10428194.2020.1839650. [DOI] [PubMed] [Google Scholar]
- 15.Yee S.W., Giacomini K.M. Emerging Roles of the Human Solute Carrier 22 Family. Drug metabolism and disposition: The biological fate of chemicals. Drug Metab. Dispos. 2021;50 doi: 10.1124/dmd.121.000702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yee S.W., Mefford J.A., Singh N., Percival M.M., Stecula A., Yang K., Witte J.S., Takahashi A., Kubo M., Matsuda K., et al. Impact of polymorphisms in drug pathway genes on disease-free survival in adults with acute myeloid leukemia. J. Hum. Genet. 2013;58:353–361. doi: 10.1038/jhg.2013.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Y., Hurren R., MacLean N., Gronda M., Jitkova Y., Sukhai M.A., Minden M.D., Schimmer A.D. Carnitine transporter CT2 (SLC22A16) is over-expressed in acute myeloid leukemia (AML) and target knockdown reduces growth and viability of AML cells. Apoptosis. 2015;20:1099–1108. doi: 10.1007/s10495-015-1137-x. [DOI] [PubMed] [Google Scholar]
- 18.Müller P., Asher N., Heled M., Cohen S.B., Risch A., Rund D. Polymorphisms in transporter and phase II metabolism genes as potential modifiers of the predisposition to and treatment outcome of de novo acute myeloid leukemia in Israeli ethnic groups. Leuk. Res. 2008;32:919–929. doi: 10.1016/j.leukres.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 19.Seeringer A., Yi-Jing H., Schlenk R., Doehner K., Kirchheiner J., Doehner H. 9242 Pharmacogenetic factors in metabolism, transport and toxicity of cytarabine treatment in patients with AML. Eur. J. Cancer Suppl. 2009;7:572–573. doi: 10.1016/S1359-6349(09)71933-0. [DOI] [Google Scholar]
- 20.Cao H.X., Miao C.F., Yan L., Tang P., Zhang L.R., Sun L. Polymorphisms at microRNA binding sites of Ara-C and an-thracyclines-metabolic pathway genes are associated with outcome of acute myeloid leukemia patients. J. Transl. Med. 2017;15:235. doi: 10.1186/s12967-017-1339-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gray J.H., Owen R.P., Giacomini K.M. The concentrative nucleoside transporter family, SLC28. Pflügers Archiv. 2004;447:728–734. doi: 10.1007/s00424-003-1107-y. [DOI] [PubMed] [Google Scholar]
- 22.Visscher H., Ross C.J., Rassekh S.R., Barhdadi A., Dubé M.P., Al-Saloos H., Sandor G.S., Caron H.N., van Dalen E.C., Kremer L.C., et al. Canadian Pharmacogenomics Network for Drug Safety Consortium. Pharmacogenomic prediction of anthracycline-induced cardio-toxicity in children. J. Clin. Oncol. 2012;30:1422–1428. doi: 10.1200/JCO.2010.34.3467. [DOI] [PubMed] [Google Scholar]
- 23.Visscher H., Ross C.J., Rassekh S.R., Sandor G.S., Caron H.N., Van Dalen E.C., Kremer L.C., Van Der Pal H.J., Rogers P.C., Rieder M.J., et al. Validation of variants inSLC28A3andUGT1A6as genetic markers predictive of anthracycline-induced cardiotoxicity in children. Pediatr. Blood Cancer. 2013;60:1375–1381. doi: 10.1002/pbc.24505. [DOI] [PubMed] [Google Scholar]
- 24.Aminkeng F., Bhavsar A.P., Visscher H., Rassekh S.R., Li Y., Lee J.W., Brunham L.R., Caron H.N., van Dalen E.C., Kremer L.C., et al. Canadian Phar-macogenomics Network for Drug Safety Consortium. A coding variant in RARG confers susceptibility to anthracy-cline-induced cardiotoxicity in childhood cancer. Nat Genet. 2015;47:1079–1084. doi: 10.1038/ng.3374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sági J.C., Egyed B., Kelemen A., Kutszegi N., Hegyi M., Gézsi A., Herlitschke M.A., Rzepiel A., Fodor L.E., Ottóffy G., et al. Possible roles of genetic variations in chemotherapy related cardiotoxicity in pediatric acute lymphoblastic leukemia and osteosarcoma. BMC Cancer. 2018;18:704. doi: 10.1186/s12885-018-4629-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wojnowski L., Kulle B., Schirmer M., Schlüter G., Schmidt A., Rosenberger A., Vonhof S., Bickeböller H., Toliat M.R., Suk E.-K., et al. NAD(P)H Oxidase and Multidrug Resistance Protein Genetic Polymorphisms Are Associated With Doxorubicin-Induced Cardiotoxicity. Circulation. 2005;112:3754–3762. doi: 10.1161/CIRCULATIONAHA.105.576850. [DOI] [PubMed] [Google Scholar]
- 27.Vulsteke C., Pfeil A.M., Maggen C., Schwenkglenks M., Pettengell R., Szucs T.D., Lambrechts D., Dieudonné A.-S., Hatse S., Neven P., et al. Clinical and genetic risk factors for epirubicin-induced cardiac toxicity in early breast cancer patients. Breast Cancer Res. Treat. 2015;152:67–76. doi: 10.1007/s10549-015-3437-9. [DOI] [PubMed] [Google Scholar]
- 28.Reichwagen A., Ziepert M., Kreuz M., Gödtel-Armbrust U., Rixecker T., Poeschel V., Reza Toliat M., Nürnberg P., Tzvetkov M., Deng S., et al. Association of NADPH oxidase poly-morphisms with anthracycline-induced cardiotoxicity in the RICOVER60 trial of patients with aggressive CD20(+) B-cell lymphoma. Pharmacogenomics. 2015;16:361–372. doi: 10.2217/pgs.14.179. [DOI] [PubMed] [Google Scholar]
- 29.Zeller T., Wild P., Szymczak S., Rotival M., Schillert A., Castagne R., Maouche S., Germain M., Lackner K., Rossmann H., et al. Genetics and beyond--the tran-scriptome of human monocytes and disease susceptibility. PLoS ONE. 2010;5:e10693. doi: 10.1371/journal.pone.0010693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dimas A.S., Deutsch S., Stranger B.E., Montgomery S.B., Borel C., Attar-Cohen H., Ingle C., Beazley C., Arcelus M.G., Sekowska M., et al. Common Regulatory Variation Impacts Gene Expression in a Cell Type–Dependent Manner. Science. 2009;325:1246–1250. doi: 10.1126/science.1174148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.White J.C., Rathmell J.P., Capizzi R.L. Membrane transport influences the rate of accumulation of cytosine arabinoside in human leukemia cells. J. Clin. Investig. 1987;79:380–387. doi: 10.1172/JCI112823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessel D., Hall T.C., Rosenthal D. Uptake and phosphorylation of cytosine arabinoside by normal and leukemic human blood cells in vitro. Cancer Res. 1969;29:459–463. [PubMed] [Google Scholar]
- 33.Sundaram M., Yao S.Y., Ingram J.C., Berry Z.A., Abidi F., Cass C.E., Baldwin S.A., Young J.D. Topology of a Human Equilibrative, Nitrobenzylthioinosine (NBMPR)-sensitive Nucleoside Transporter (hENT1) Implicated in the Cellular Uptake of Adenosine and Anti-cancer Drugs. J. Biol. Chem. 2001;276:45270–45275. doi: 10.1074/jbc.M107169200. [DOI] [PubMed] [Google Scholar]
- 34.Gati W.P., Paterson A.R., Larratt L.M., Turner A.R., Belch A.R. Sensitivity of acute leukemia cells to cytarabine is a correlate of cellular es nucleoside transporter site content measured by flow cytometry with SAENTA-fluorescein. Blood. 1997;90:346–353. doi: 10.1182/blood.V90.1.346.346_346_353. [DOI] [PubMed] [Google Scholar]
- 35.Zhang J., Visser F., King K.M., Baldwin S.A., Young J.D., Cass C.E. The role of nucleoside transporters in cancer chemotherapy with nucleoside drugs. Cancer Metastasis Rev. 2007;26:85–110. doi: 10.1007/s10555-007-9044-4. [DOI] [PubMed] [Google Scholar]
- 36.Eltzschig H.K., Abdulla P., Hoffman E., Hamilton K.E., Daniels D., Schonfeld C., Loffler M., Reyes G., Duszenko M., Karhausen J., et al. HIF-1–dependent repression of equilibrative nucleoside transporter (ENT) in hypoxia. J. Exp. Med. 2005;202:1493–1505. doi: 10.1084/jem.20050177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Montero T.D., Racordon D., Bravo L., Owen G.I., Bronfman M.L., Leisewitz A.V. PPARalpha and PPARgamma regulate the nucleoside transporter hENT1. Biochem. Biophys. Res. Commun. 2012;419:405–411. doi: 10.1016/j.bbrc.2012.02.035. [DOI] [PubMed] [Google Scholar]
- 38.Galmarini C.M., Thomas X., Calvo F., Rousselot P., Rabilloud M., El Jaffari A., Cros E., Dumontet C. In vivo mechanisms of resistance to cytarabine in acute myeloid leukaemia. Br. J. Haematol. 2002;117:860–868. doi: 10.1046/j.1365-2141.2002.03538.x. [DOI] [PubMed] [Google Scholar]
- 39.Jaramillo A.C., Hubeek I., Broekhuizen R., Pastor-Anglada M., Kaspers G.J.L., Jansen G., Cloos J., Peters G.J. Expression of the nucleoside transporters hENT1 (SLC29) and hCNT1 (SLC28) in pediatric acute myeloid leukemia. Nucleosides Nucleotides Nucleic Acids. 2020;39:1379–1388. doi: 10.1080/15257770.2020.1746803. [DOI] [PubMed] [Google Scholar]
- 40.Osato D.H., Huang C.C., Kawamoto M., Johns S.J., Stryke D., Wang J., Ferrin T.E., Herskowitz I., Giacomini K.M. Functional characterization in yeast of genetic variants in the human equilibrative nucleoside transporter, ENT1. Pharmacogenetics. 2003;13:297–301. doi: 10.1097/00008571-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Myers S.N., Goyal R.K., Roy J.D., Fairfull L.D., Wilson J.W., Ferrell R.E. Functional single nucleotide polymorphism haplotypes in the human equilibrative nucleoside transporter 1. Pharm. Genom. 2006;16:315–320. doi: 10.1097/01.fpc.0000189804.41962.15. [DOI] [PubMed] [Google Scholar]
- 42.Parmar S., Seeringer A., Denich D., Gärtner F., Pitterle K., Syrovets T., Ohmle B., Stingl J.C. Variability in transport and biotransformation of cytarabine is associated with its toxicity in peripheral blood mononuclear cells. Pharmacogenomics. 2011;12:503–514. doi: 10.2217/pgs.10.200. [DOI] [PubMed] [Google Scholar]
- 43.Kim J.-H., Lee C., Cheong H.S., Koh Y., Ahn K.-S., Kim H.-L., Shin H.D., Yoon S.-S. SLC29A1 (ENT1) polymorphisms and outcome of complete remission in acute myeloid leukemia. Cancer Chemother. Pharmacol. 2016;78:533–540. doi: 10.1007/s00280-016-3103-x. [DOI] [PubMed] [Google Scholar]
- 44.Kim K.I., Huh I.-S., Kim I.-W., Park T., Ahn K.-S., Yoon S.-S., Yoon J.-H., Oh J.M. Combined interaction of multi-locus genetic polymorphisms in cytarabine arabinoside metabolic pathway on clinical outcomes in adult acute myeloid leukaemia (AML) patients. Eur. J. Cancer. 2012;49:403–410. doi: 10.1016/j.ejca.2012.07.022. [DOI] [PubMed] [Google Scholar]
- 45.Wan H., Zhu J., Chen F., Xiao F., Huang H., Han X., Zhong L., Zhong H., Xu L., Ni B., et al. SLC29A1 single nucleotide polymorphisms as independent prognostic predictors for survival of patients with acute myeloid leukemia: An in vitro study. J. Exp. Clin. Cancer Res. 2014;33:90. doi: 10.1186/s13046-014-0090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Amaki J., Onizuka M., Ohmachi K., Aoyama Y., Hara R., Ichiki A., Kawai H., Sato A., Miyamoto M., Toyosaki M., et al. Single nucleotide polymorphisms of cytarabine metabolic genes influence clinical outcome in acute myeloid leukemia patients receiving high-dose cytarabine therapy. Int. J. Hematol. 2015;101:543–553. doi: 10.1007/s12185-015-1766-4. [DOI] [PubMed] [Google Scholar]
- 47.International Transporter Consortium. Giacomini K.M., Huang S.M., Tweedie D.J., Benet L.Z., Brouwer K.L., Chu X., Dahlin A., Evers R., Fischer V., et al. Membrane transporters in drug development. Nat. Rev. Drug Discov. 2010;9:215–236. doi: 10.1038/nrd3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lal S., Wong Z.W., Sandanaraj E., Xiang X., Ang P.C.S., Lee E.J.D., Chowbay B. Influence of ABCB1 and ABCG2 polymorphisms on doxorubicin disposition in Asian breast cancer patients. Cancer Sci. 2008;99:816–823. doi: 10.1111/j.1349-7006.2008.00744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Guo Y., Köck K., Ritter C.A., Chen Z.-S., Grube M., Jedlitschky G., Illmer T., Ayres M., Beck J.F., Siegmund W., et al. Expression of ABCC-Type Nucleotide Exporters in Blasts of Adult Acute Myeloid Leukemia: Relation to Long-term Survival. Clin. Cancer Res. 2009;15:1762–1769. doi: 10.1158/1078-0432.CCR-08-0442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hopper-Borge E., Xu X., Shen T., Shi Z., Chen Z.-S., Kruh G.D. Human Multidrug Resistance Protein 7 (ABCC10) Is a Resistance Factor for Nucleoside Analogues and Epothilone B. Cancer Res. 2009;69:178–184. doi: 10.1158/0008-5472.CAN-08-1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Illmer T., Schuler U.S., Thiede C., I Schwarz U., Kim R.B., Gotthard S., Freund D., Schäkel U., Ehninger G., Schaich M. MDR1 gene polymorphisms affect therapy outcome in acute myeloid leukemia patients. Cancer Res. 2002;62:4955–4962. [PubMed] [Google Scholar]
- 52.Kaya P., Gündüz U., Arpaci F., Ural A.U., Guran S. Identification of polymorphisms on theMDR1 gene among Turkish population and their effects on multidrug resistance in acute leukemia patients. Am. J. Hematol. 2005;80:26–34. doi: 10.1002/ajh.20427. [DOI] [PubMed] [Google Scholar]
- 53.Kim D.H., Park J.Y., Sohn S.K., Lee N.Y., Baek J.H., Jeon S.B., Kim J.G., Suh J.S., Do Y.R. Multidrug resistance-1 gene polymorphism associated with the treatment outcomes in de novo acute myeloid leukemia. J. Clin. Oncol. 2005;23:6550. doi: 10.1200/jco.2005.23.16_suppl.6550. [DOI] [PubMed] [Google Scholar]
- 54.Van Der Holt B., Vandenheuveleibrink M., Van Schaik R.H.N., Van Der Heiden I.P., Wiemer E.A.C., Vossebeld P.J.M., Löwenberg B., Sonneveld P. ABCB1 gene polymorphisms are not associated with treatment outcome in elderly acute myeloid leukemia patients. Clin. Pharmacol. Ther. 2006;80:427–439. doi: 10.1016/j.clpt.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 55.Hur E.-H., Lee J.-H., Lee M.J., Choi S.-J., Lee J.-H., Kang M.J., Seol M., Jang Y.E., Lee H.-J., Kang I.-S., et al. C3435T polymorphism of the MDR1 gene is not associated with P-glycoprotein function of leukemic blasts and clinical outcome in patients with acute myeloid leukemia. Leuk. Res. 2008;32:1601–1604. doi: 10.1016/j.leukres.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 56.Hampras S.S., Sucheston L., Weiss J., Baer M.R., Zirpoli G., Singh P.K., Wetzler M., Chennamaneni R., Blanco J.G., Ford L., et al. Genetic polymorphisms of ATP-binding cassette (ABC) proteins, overall survival and drug toxicity in patients with Acute Myeloid Leukemia. Int. J. Mol. Epidemiol. Genet. 2010;1:201–207. [PMC free article] [PubMed] [Google Scholar]
- 57.Gréen H., Falk I.J., Lotfi K., Paul E., Hermansson M., Rosenquist R., Paul C., Nahi H. Association of ABCB1 polymorphisms with survival and in vitro cytotoxicty in de novo acute myeloid leukemia with normal karyotype. Pharm. J. 2010;12:111–118. doi: 10.1038/tpj.2010.79. [DOI] [PubMed] [Google Scholar]
- 58.Scheiner M.A.M., Vasconcelos F.d.C., Matta R.R.d., Figueira R.D.B., Jr., Maia R.C. ABCB1 genetic variation and P-glycoprotein expression/activity in a cohort of Brazilian acute myeloid leukemia patients. J. Cancer Res. Clin. Oncol. 2012;138:959–969. doi: 10.1007/s00432-012-1170-x. [DOI] [PubMed] [Google Scholar]
- 59.Jakobsen Falk I., Fyrberg A., Paul E., Nahi H., Hermanson M., Rosenquist R., Höglund M., Palmqvist L., Stockelberg D., Wei Y., et al. Impact of ABCB1 single nucleotide polymorphisms 1236C>T and 2677G>T on overall survival in FLT3 wild-type de novo AML patients with normal karyotype. Br. J. Haematol. 2014;167:671–680. doi: 10.1111/bjh.13097. [DOI] [PubMed] [Google Scholar]
- 60.He H., Yin J.-Y., Xu Y.-J., Li X., Zhang Y., Liu Z.-G., Zhou F., Zhai M., Li Y., Li X.-P., et al. Association of ABCB1 Polymorphisms with the Efficacy of Ondansetron in Chemotherapy-induced Nausea and Vomiting. Clin. Ther. 2014;36:1242–1252.e2. doi: 10.1016/j.clinthera.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 61.He H., Yin J., Li X., Zhang Y., Xu X., Zhai M., Chen J., Qian C., Zhou H., Liu Z. Association of ABCB1 polymorphisms with prognostic outcomes of anthracycline and cytarabine in Chinese patients with acute myeloid leukemia. Eur. J. Clin. Pharmacol. 2015;71:293–302. doi: 10.1007/s00228-014-1795-6. [DOI] [PubMed] [Google Scholar]
- 62.Megías-Vericat J.E., Montesinos P., Herrero M.J., Moscardó F., Bosó V., Rojas L., Martínez-Cuadrón D., Hervás D., Boluda B., García-Robles A., et al. Impact of ABC single nucleotide polymorphisms upon the efficacy and toxicity of induction chemotherapy in acute myeloid leukemia. Leuk. Lymphoma. 2017;58:1197–1206. doi: 10.1080/10428194.2016.1231405. [DOI] [PubMed] [Google Scholar]
- 63.Rafiee R., Chauhan L., Alonzo T.A., Wang Y.-C., Elmasry A., Loken M.R., Pollard J., Aplenc R., Raimondi S., Hirsch B.A., et al. ABCB1 SNP predicts outcome in patients with acute myeloid leukemia treated with Gemtuzumab ozogamicin: A report from Children’s Oncology Group AAML0531 Trial. Blood Cancer J. 2019;9:51. doi: 10.1038/s41408-019-0211-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Short N.J., Richard-Carpentier G., Kanagal-Shamanna R., Patel K.P., Konopleva M., Papageorgiou I., Pemmaraju N., Borthakur G., Ravandi F., DiNardo C.D., et al. Impact of CD33 and ABCB1 single nucleotide polymorphisms in patients with acute myeloid leukemia and advanced myeloid malignancies treated with de-citabine plus gemtuzumab ozogamicin. Am. J Hematol. 2020;95:E225–E228. doi: 10.1002/ajh.25854. [DOI] [PubMed] [Google Scholar]
- 65.van den Heuvel-Eibrink M.M.V.D., Wiemer E.A.C., de Boevere M.J., van der Holt B., Vossebeld P.J.M., Pieters R., Sonneveld P. MDR1 gene–related clonal selection and P-glycoprotein function and expression in relapsed or refractory acute myeloid leukemia. Blood. 2001;97:3605–3611. doi: 10.1182/blood.V97.11.3605. [DOI] [PubMed] [Google Scholar]
- 66.Kim Y.-K., Bae S.-Y., Kim H.N., Kim N.Y., Kim H.J., Bang S.-M., Jo D.-Y., Won J.-H., Lee N.-R., Kwak J.-Y., et al. Prognostic Impact of DNA Repair and MDR-1 Gene Polymorphisms In De Novo Acute Myeloid Leukemia with t(8;21) or Inv(16) Blood. 2010;116:1714. doi: 10.1182/blood.V116.21.1714.1714. [DOI] [Google Scholar]
- 67.Kim Y.-K., Kim H.-N., Lee I.-K., Bang S.-M., Jo D.-Y., Won J.-H., Kwak J.-Y., Yim C.-Y., Yang D.-H., Lee J.-J., et al. Prognostic Significance of ABCB1 (MDR1) Gene Polymorphisms in De Novo Acute Myeloid Leukemia with t(8;21) or inv(16) Blood. 2007;110:4271. doi: 10.1182/blood.V110.11.4271.4271. [DOI] [Google Scholar]
- 68.Monzo M., Brunet S., Urbano-Ispizua A., Navarro A., Perea G., Esteve J., Artells R., Granell M., Berlanga J., Ribera J.M., et al. Genomic polymorphisms provide prognostic information in intermediate-risk acute myeloblastic leukemia. Blood. 2006;107:4871–4879. doi: 10.1182/blood-2005-08-3272. [DOI] [PubMed] [Google Scholar]
- 69.Varatharajan S., Panetta J., Abraham A., Karathedath S., Mohanan E., Lakshmi K.M., Arthur N., Srivastava V.M., Nemani S., George B., et al. Population pharmacokinetics of Daunorubicin in adult patients with acute myeloid leukemia. Cancer Chemother. Pharmacol. 2016;78:1051–1058. doi: 10.1007/s00280-016-3166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borg A.G., Burgess R., Green L.M., Scheper R.J., Yin J.A.L. P-glycoprotein and multidrug resistance-associated protein, but not lung resistance protein, lower the intracellular daunorubicin accumulation in acute myeloid leukaemic cells. Br. J. Haematol. 2000;108:48–54. doi: 10.1046/j.1365-2141.2000.01793.x. [DOI] [PubMed] [Google Scholar]
- 71.Seedhouse C.H., Grundy M., White P., Li Y., Fisher J., Yakunina D., Moorman A., Hoy T., Russell N., Burnett A., et al. Sequential Influences of Leukemia-Specific and Genetic Factors on P-Glycoprotein Expression in Blasts from 817 Patients Entered into the National Cancer Research Network Acute Myeloid Leukemia 14 and 15 Trials. Clin. Cancer Res. 2007;13:7059–7066. doi: 10.1158/1078-0432.CCR-07-1484. [DOI] [PubMed] [Google Scholar]
- 72.Lamba J., Strom S., Venkataramanan R., Thummel K.E., Lin Y.S., Liu W., Cheng C., Lamba V., Watkins P.B., Schuetz E. MDR1 genotype is associated with hepatic cytochrome P450 3A4 basal and induction phenotype. Clin. Pharmacol. Ther. 2006;79:325–338. doi: 10.1016/j.clpt.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 73.Megías-Vericat J.E., Rojas L., Herrero M.J., Bosó V., Montesinos P., Moscardó F., Poveda J.L., Sanz M.Á., Aliño S.F. Influence of ABCB1 polymorphisms upon the effectiveness of standard treatment for acute myeloid leukemia: A systematic review and meta-analysis of observational studies. Pharm. J. 2015;15:109–118. doi: 10.1038/tpj.2014.80. [DOI] [PubMed] [Google Scholar]
- 74.Megías-Vericat J.E., Rojas L., Herrero M.J., Bosó V., Montesinos P., Moscardó F., Poveda J.L., Sanz M.Á., Aliño S.F. Positive impact of ABCB1 polymorphisms in overall survival and complete remission in acute myeloid leukemia: A systematic review and meta-analysis. Pharm. J. 2016;16:1–2. doi: 10.1038/tpj.2015.79. [DOI] [PubMed] [Google Scholar]
- 75.Hertz D.L., Caram M.V., Kidwell K.M., Thibert J.N., Gersch C., Seewald N.J., Smerage J., Rubenfire M., Henry N.L., Cooney K.A., et al. Evidence for association of SNPs in ABCB1 and CBR3 but not RAC2, NCF4 SLC28A3 or TOP2B with chronic cardiotoxicity in a cohort of breast cancer patients treated with anthracyclines. Pharmacogenomics. 2016;17:231–240. doi: 10.2217/pgs.15.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Rossi D., Rasi S., Franceschetti S., Capello D., Castelli A., De Paoli L., Ramponi A., Chiappella A., Pogliani E.M., Vitolo U., et al. Analysis of the host pharmacogenetic background for prediction of outcome and toxicity in diffuse large B-cell lymphoma treated with R-CHOP21. Leukemia. 2009;23:1118–1126. doi: 10.1038/leu.2008.398. [DOI] [PubMed] [Google Scholar]
- 77.Lubieniecka J.M., Graham J., Heffner D., Mottus R., Reid R., Hogge D., Grigliatti T.A., Riggs W.K. A discovery study of daunorubicin induced cardiotoxicity in a sample of acute myeloid leukemia patients prioritizes P450 oxidoreductase poly-morphisms as a potential risk factor. Front. Genet. 2013;4:231. doi: 10.3389/fgene.2013.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sissung T.M., Huang P.A., Hauke R.J., McCrea E.M., Peer C.J., Barbier R.H., Strope J.D., Ley A.M., Zhang M., Hong J.A., et al. Severe Hepatotoxicity of Mithramycin Therapy Caused by Altered Expression of Hepatocellular Bile Transporters. Mol. Pharmacol. 2019;96:158–167. doi: 10.1124/mol.118.114827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stride B.D., Grant C.E., Loe D.W., Hipfner D.R., Cole S.P.C., Deeley R.G. Pharmacological Characterization of the Murine and Human Orthologs of Multidrug-Resistance Protein in Transfected Human Embryonic Kidney Cells. Mol. Pharmacol. 1997;52:344–353. doi: 10.1124/mol.52.3.344. [DOI] [PubMed] [Google Scholar]
- 80.Conrad S., Kauffmann H.-M., Ito K.-I., Leslie E., Deeley R.G., Schrenk D., Cole S. A naturally occurring mutation in MRP1 results in a selective decrease in organic anion transport and in increased doxorubicin resistance. Pharmacogenetics. 2002;12:321–330. doi: 10.1097/00008571-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 81.Semsei A.F., Erdelyi D.J., Ungvari I., Csagoly E., Hegyi M., Kiszel P.S., Lautner-Csorba O., Szabolcs J., Masat P., Fekete G., et al. ABCC1polymorphisms in anthracycline-induced cardiotoxicity in childhood acute lymphoblastic leukaemia. Cell Biol. Int. 2012;36:79–86. doi: 10.1042/CBI20110264. [DOI] [PubMed] [Google Scholar]
- 82.Mahjoubi F., Akbari S., Montazeri M., Moshyri F. MRP1 polymorphisms (T2684C, C2007T, C2012T, and C2665T) are not associated with multidrug resistance in leukemic patients. Genet. Mol. Res. 2008;7:1369–1374. doi: 10.4238/vol7-4gmr482. [DOI] [PubMed] [Google Scholar]
- 83.Kunadt D., Dransfeld C., Dill C., Schmiedgen M., Kramer M., Altmann H., Röllig C., Bornhäuser M., Mahlknecht U., Schaich M., et al. Multidrug-related protein 1 (MRP1) polymorphisms rs129081, rs212090, and rs212091 predict survival in normal karyotype acute myeloid leukemia. Ann. Hematol. 2020;99:2173–2180. doi: 10.1007/s00277-020-04163-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Cui Y., König J., Buchholz J.K., Spring H., Leier I., Keppler D. Drug resistance and ATP-dependent conjugate transport mediated by the apical multidrug resistance protein, MRP2, permanently expressed in human and canine cells. Mol. Pharmacol. 1999;55:929–937. [PubMed] [Google Scholar]
- 85.Armenian S.H., Ding Y., Mills G., Sun C., Venkataraman K., Wong F.L., Neuhausen S.L., Senitzer D., Wang S., Forman S.J., et al. Genetic susceptibility to anthracycline-related congestive heart failure in survivors of haematopoietic cell transplantation. Br. J. Haematol. 2013;163:205–213. doi: 10.1111/bjh.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Windsor R.E., Strauss S.J., Kallis C., Wood N.E., Whelan J.S. Germline genetic polymorphisms may influence chemotherapy response and disease outcome in osteosarcoma: A pilot study. Cancer. 2012;118:1856–1867. doi: 10.1002/cncr.26472. [DOI] [PubMed] [Google Scholar]
- 87.Varatharajan S., Abraham A., Karathedath S., Ganesan S., Lakshmi K.M., Arthur N., Srivastava V.M., George B., Srivastava A., Mathews V., et al. ATP-binding casette transporter expression in acute myeloid leukemia: Association with in vitro cytotoxicity and prognostic markers. Pharmacogenomics. 2017;18:235–244. doi: 10.2217/pgs-2016-0150. [DOI] [PubMed] [Google Scholar]
- 88.Butrym A., Łacina P., Bogunia-Kubik K., Mazur G. ABCC3 and GSTM5 gene polymorphisms affect overall survival in Polish acute myeloid leukaemia patients. Curr. Probl. Cancer. 2021;45:100729. doi: 10.1016/j.currproblcancer.2021.100729. [DOI] [PubMed] [Google Scholar]
- 89.Hu S., Chen Z., Franke R., Orwick S., Zhao M., Rudek M.A., Sparreboom A., Baker S.D. Interaction of the Multikinase Inhibitors Sorafenib and Sunitinib with Solute Carriers and ATP-Binding Cassette Transporters. Clin. Cancer Res. 2009;15:6062–6069. doi: 10.1158/1078-0432.CCR-09-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hu S., Niu H., Inaba H., Orwick S., Rose C., Panetta J., Yang S., Pounds S., Fan Y., Calabrese C., et al. Activity of the Multikinase Inhibitor Sorafenib in Combination with Cytarabine in Acute Myeloid Leukemia. JNCI J. Natl. Cancer Inst. 2011;103:893–905. doi: 10.1093/jnci/djr107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Doyle L.A., Yang W., Abruzzo L.V., Krogmann T., Gao Y., Rishi A.K., Ross D.D. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc. Natl. Acad. Sci. USA. 1998;95:15665–15670. doi: 10.1073/pnas.95.26.15665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Chen L., Manautou J.E., Rasmussen T.P., Zhong X.B. Development of precision medicine approaches based on interindividual variability of BCRP/ABCG2. Acta Pharm. Sin. B. 2019;9:659–674. doi: 10.1016/j.apsb.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ross D.D., Karp J.E., Chen T.T., Doyle L.A. Expression of breast cancer resistance protein in blast cells from patients with acute leukemia. Blood. 2000;96:365–368. doi: 10.1182/blood.V96.1.365. [DOI] [PubMed] [Google Scholar]
- 94.Benderra Z., Faussat A.-M., Sayada L., Perrot J.-Y., Chaoui D., Marie J.-P., Legrand O. Breast Cancer Resistance Protein and P-Glycoprotein in 149 Adult Acute Myeloid Leukemias. Clin. Cancer Res. 2004;10:7896–7902. doi: 10.1158/1078-0432.CCR-04-0795. [DOI] [PubMed] [Google Scholar]
- 95.Benderra Z., Faussat A.M., Sayada L., Perrot J.-Y., Tang R., Chaoui D., Morjani H., Marzac C., Marie J.-P., Legrand O. MRP3, BCRP, and P-Glycoprotein Activities are Prognostic Factors in Adult Acute Myeloid Leukemia. Clin. Cancer Res. 2005;11:7764–7772. doi: 10.1158/1078-0432.CCR-04-1895. [DOI] [PubMed] [Google Scholar]
- 96.Tiribelli M., Geromin A., Michelutti A., Cavallin M., Pianta A., Fabbro D., Russo D., Damante G., Fanin R., Damiani D. Concomitant ABCG2 overexpression and FLT3-ITD mutation identify a subset of acute myeloid leukemia patients at high risk of relapse. Cancer. 2010;117:2156–2162. doi: 10.1002/cncr.25753. [DOI] [PubMed] [Google Scholar]
- 97.Wang F., Liang Y.-J., Wu X.-P., Chen L.-M., To K.K.W., Dai C.-L., Yan Y.-Y., Wang Y.-S., Tong X.-Z., Fu L.-W. Prognostic value of the multidrug resistance transporter ABCG2 gene polymorphisms in Chinese patients with de novo acute leukaemia. Eur. J. Cancer. 2011;47:1990–1999. doi: 10.1016/j.ejca.2011.03.032. [DOI] [PubMed] [Google Scholar]
- 98.Tiribelli M., Fabbro D., Franzoni A., Fanin R., Damante G., Damiani D. Q141K polymorphism of ABCG2 protein is associated with poor prognosis in adult acute myeloid leukemia treated with idarubicin-based chemotherapy. Haematologica. 2013;98:e28–e29. doi: 10.3324/haematol.2012.075895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rhodes K.E., Zhang W., Yang D., Press O.A., Gordon M., Vallböhmer D., Schultheis A.M., Lurje G., Ladner R.D., Fazzone W., et al. ABCB1, SLCO1B1 and UGT1A1 gene polymorphisms are associated with toxicity in metastatic colorectal cancer patients treated with first-line irinotecan. Drug Metab. Lett. 2007;1:23–30. doi: 10.2174/187231207779814328. [DOI] [PubMed] [Google Scholar]
- 100.Sai K., Saito Y., Maekawa K., Kim S.-R., Kaniwa N., Nishimaki-Mogami T., Sawada J.-I., Shirao K., Hamaguchi T., Yamamoto N., et al. Additive effects of drug transporter genetic polymorphisms on irinotecan pharmacokinetics/pharmacodynamics in Japanese cancer patients. Cancer Chemother. Pharmacol. 2010;66:95–105. doi: 10.1007/s00280-009-1138-y. [DOI] [PubMed] [Google Scholar]
- 101.Peters B.J., Rodin A.S., Klungel O.H., van Duijn C.M., Stricker B.H.C., Slot R.V., de Boer A., der Zee A.-H.M.-V. Pharmacogenetic interactions between ABCB1 and SLCO1B1 tagging SNPs and the effectiveness of statins in the prevention of myocardial infarction. Pharmacogenomics. 2010;11:1065–1076. doi: 10.2217/pgs.10.81. [DOI] [PubMed] [Google Scholar]
- 102.Neve E.P.A., Artursson P., Ingelman-Sundberg M., Karlgren M. An Integrated in Vitro Model for Simultaneous Assessment of Drug Uptake, Metabolism, and Efflux. Mol. Pharm. 2013;10:3152–3163. doi: 10.1021/mp400202d. [DOI] [PubMed] [Google Scholar]
- 103.Lane H.-Y., Tsai G.E., Lin E. Assessing Gene-Gene Interactions in Pharmacogenomics. Mol. Diagn. Ther. 2012;16:15–27. doi: 10.1007/BF03256426. [DOI] [PubMed] [Google Scholar]
- 104.Donnette M., Solas C., Giocanti M., Venton G., Farnault L., Berda-Haddad Y., Hau L.T.T., Costello R., Ouafik L., Lacarelle B., et al. Simultaneous determination of cytosine arabinoside and its metabolite uracil arabinoside in human plasma by LC-MS/MS: Application to pharmacokinetics-pharmacogenetics pilot study in AML patients. J. Chromatogr. B. 2019;1126–1127:121770. doi: 10.1016/j.jchromb.2019.121770. [DOI] [PubMed] [Google Scholar]
- 105.Yamakawa Y., Hamada A., Nakashima R., Yuki M., Hirayama C., Kawaguchi T., Saito H. Association of genetic poly-morphisms in the influx transporter SLCO1B3 and the efflux transporter ABCB1 with imatinib pharmacokinetics in patients with chronic myeloid leukemia. Ther. Drug Monit. 2011;33:244–250. doi: 10.1097/FTD.0b013e31820beb02. [DOI] [PubMed] [Google Scholar]
- 106.Zhang H., He X., Li J., Wang Y., Wang C., Chen Y., Niu C., Gao P. SLCO1B1c. 521T>C gene polymorphisms are associated with high-dose methotrexate pharmacokinetics and clinical outcome of pediatric acute lymphoblastic leukemia. Zhonghua Er Ke Za Zhi—Chin. J. Pediatr. 2014;52:770–776. [PubMed] [Google Scholar]
- 107.Bruhn O., Cascorbi I. Polymorphisms of the drug transporters ABCB1, ABCG2, ABCC2 and ABCC3 and their impact on drug bioavailability and clinical relevance. Expert Opin. Drug Metab. Toxicol. 2014;10:1337–1354. doi: 10.1517/17425255.2014.952630. [DOI] [PubMed] [Google Scholar]
- 108.Bruckmueller H., Cascorbi I. ABCB1, ABCG2, ABCC1, ABCC2, and ABCC3 drug transporter polymorphisms and their impact on drug bioavailability: What is our current understanding? Expert Opin. Drug. Metab. Toxicol. 2021;17:369–396. doi: 10.1080/17425255.2021.1876661. [DOI] [PubMed] [Google Scholar]
- 109.Roumier C., Cheok M.H. Pharmacogenomics in acute myeloid leukemia. Pharmacogenomics. 2009;10:1839–1851. doi: 10.2217/pgs.09.130. [DOI] [PubMed] [Google Scholar]
- 110.Emadi A., E Karp J. The clinically relevant pharmacogenomic changes in acute myelogenous leukemia. Pharmacogenomics. 2012;13:1257–1269. doi: 10.2217/pgs.12.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Vasconcelos F.C., de Souza P.S., Hancio T., de Faria F.C.C., Maia R.C. Update on drug transporter proteins in acute myeloid leukemia: Pathological implication and clinical setting. Crit. Rev. Oncol. 2021;160:103281. doi: 10.1016/j.critrevonc.2021.103281. [DOI] [PubMed] [Google Scholar]
- 112.Pinto-Merino Á., Labrador J., Zubiaur P., Alcaraz R., Herrero M.J., Montesinos P., Abad-Santos F., Saiz-Rodríguez M. Role of Pharmacogenetics in the Treatment of Acute Myeloid Leukemia: Systematic Review and Future Perspectives. Pharmaceutics. 2022;14:559. doi: 10.3390/pharmaceutics14030559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Megías-Vericat J.E., Solana-Altabella A., Ballesta-López O., Martínez-Cuadrón D., Montesinos P. Drug-drug interactions of newly approved small molecule inhibitors for acute myeloid leukemia. Ann. Hematol. 2020;99:1989–2007. doi: 10.1007/s00277-020-04186-0. [DOI] [PubMed] [Google Scholar]