Abstract
Introduction:
Within gender-diverse populations, gender-affirming changes in gender on record may improve mental or behavioral health. This study uses claims data to investigate whether sex assigned at birth (SAB) modifies the association between change in gender on record and mental or behavioral health.
Methods:
Adult Oregon Medicaid beneficiaries with gender identity–related diagnoses and enrolled during 2010–2019 were included. SAB was inferred from medical and pharmacy claims and categorized as assigned female at birth (AFAB), assigned male at birth (AMAB), or unknown SAB. Self-reported gender came from enrollment records. Gender at initial enrollment differing from SAB indicated a change in gender on record. Multivariable logistic regression estimated the association between change in gender on record and mental (anxiety, depression, suicidal ideation, post-traumatic stress disorder) or behavioral health (alcohol, substance, or tobacco use disorders). Analyses were conducted in February 2021.
Results:
This study included 2,940 transgender and nonbinary adults. Of the 1,451 self-reporting female gender and 1,489 self-reporting male, 449 (30.9%) were AMAB and 303 (20.3%) were AFAB classified as changing their gender on record. Predicted probability of mental or behavioral conditions was significantly lower in those who changed their gender on record. SAB modified the association with mental health: AFAB reporting female gender had the highest burdens, followed by AMAB reporting male. Secondary analyses using a modified change in gender definition, or an alternative SAB inference method, found similar trends.
Conclusions:
Oregon Medicaid gender-diverse beneficiaries who changed their gender on record had meaningfully lower probability of mental and behavioral health conditions. People who were AFAB reporting female gender had the highest burdens.
INTRODUCTION
It is well documented that transgender populations have higher rates of poorer mental health and suicidal ideation than cisgender populations.1–4 Emerging evidence suggests mental and behavioral health differs within subgroups of the transgender and nonbinary (TGN) population. Transgender men (i.e., individuals assigned female sex at birth [AFAB]) report poorer outcomes than transgender women (i.e., individuals assigned male sex at birth [AMAB]), and nonbinary individuals report poorer outcomes than either group.2,3,5
The gender affirmation framework posits that decreased access to and increased need for gender affirmation increases likelihood of engaging in high-risk behaviors, such as substance use.6 Legal gender affirmation is especially difficult, as it may involve obtaining a legal name change from a court or letters from medical professionals documenting one’s gender transition.7 Only 11% of respondents to the 2015 U..S Transgender Survey had their preferred name and gender on all identification documents and records, while 68% lacked their preferred name and gender on any.3 Common reasons for not changing gender on record included only being presented binary gender options that did not fit one’s gender identity, not being ready, and worry that changing one’s gender marker might cause loss of benefits or services.3
Gender affirmation may protect TGN individuals against adverse mental and behavioral health outcomes.8,9 In analyses of affirmation comprising gender marker and name changes on passports, driver’s licenses, or other identifying documents, changing gender on record was positively associated with decreased odds of depression, anxiety, psychological distress, and suicide risk.10,11 Even changing some but not all identity documents was associated with decreased prevalence of psychological distress and suicidal ideation compared with changing none.11 These previous studies utilized convenience samples, whereas no population-based study has examined how gender marker changes in healthcare settings, such as on health insurance enrollment or medical records, impact statewide or national health outcomes. Indeed, rules for changing gender on record during Medicaid enrollment vary by state. For example, although reporting gender identity is optional for Oregon Medicaid beneficiaries and does not affect eligibility for services,12 Washington Medicaid beneficiaries must formally change gender marker with the state’s Health Care Authority, and individuals seeking pregnancy coverage must answer “female‖ for the sex assigned at birth (SAB) field.13
Given the evidence supporting differential mental and behavioral health within the transgender population, it is important to distinguish TGN subgroups, rather than assess them as a homogeneous population.14,15 The “2-step‖ method of capturing demographic information separates concepts of sex, which refers to sex assignment at birth based on physical anatomy, and gender, which encapsulates self-identity.14–16 Whereas SAB is binary (male, female), gender identity takes myriad forms. For example, respondents in the 2015 U.S. Transgender Survey listed >500 unique gender terms for themselves, including trans woman, trans man, non-binary, genderqueer, and two-spirit.3 This approach is person-centered: TGN individuals indicate the separation of gender and SAB acknowledges their gender more appropriately.17,18 In a qualitative study, a respondent explained, “If a study asks me if my gender is ‘male, female, or transgender,’ then I will check the ‘male’ option, since transgender isn’t my gender.”17 Using the 2-step method, this person could report AFAB and male gender.14
Another methodological advancement is systematic health systems–based sampling from electronic medical records or administrative claims to identify large TGN samples. Electronic medical records–based methods use demographic data, natural language processing in clinical narratives, and history of sex organ–specific care (e.g., prostate exams or cervical screenings) to infer SAB and gender in TGN populations. These studies were able to characterize 18%–83% of their samples as having transmasculine (male gender and AFAB), transfeminine (female gender and AMAB), or nonbinary gender identity.19–23 Administrative claims–based methods primarily rely on gender dysphoria or gender identity disorder diagnoses to identify TGN samples.24–30 As of August 2021, only 1 claims-based study has attempted to infer SAB, yielding 32.3% of the sample classified as transmasculine (AFAB), 14.7% transfeminine (AMAB), and 53.0% unknown.26
Given the potential for population-level health research using administrative data,14,31,32 this study aimed to develop a method for distinguishing SAB and gender using TGN Medicaid beneficiaries’ administrative claims, and to investigate whether the association between changing one’s gender on record and mental or behavioral health was modified by SAB. These objectives advance the use of administrative claims for studying plan-level samples of TGN beneficiaries, and increase knowledge of differential health and risks within TGN populations.
METHODS
Study Population
This was a retrospective analysis of 2010–2019 Oregon Medicaid administrative claims. The data consist of individual-level daily medical and pharmacy claims, and monthly historical enrollment files for all Oregon Medicaid beneficiaries. The data contain a unique identifier that allowed the analyses to follow individuals over time and across enrollment discontinuities. Oregon Medicaid beneficiaries aged 18–64 years on January 1, 2010 who were enrolled at any time during the study period were included. Beneficiaries dually enrolled in Medicare and Medicaid were excluded owing to their incomplete claims data.
The study population comprised TGN Oregon Medicaid beneficiaries with at least 1 gender identity–related diagnosis during the study period (ICD-9: 302.5x, 302.6, 302.85, ICD-10: F640, F642, F641, F648, F649, Z87.890). Although not all TGN individuals receive these diagnoses, and not all individuals with these diagnoses identify as TGN, this method had high validity in previous health records–based studies.20,22,29,33 Consistent with prior literature, TGN identity was applied both retrospectively and prospectively from the time of gender identity–related diagnosis.21,22,26,34 Although all beneficiaries with these diagnoses were included, a method developed by the Centers for Medicare & Medicaid Services, which assessed frequency and duration of gender identity–related diagnoses and care, was applied to confirm TGN classification.29
Measures
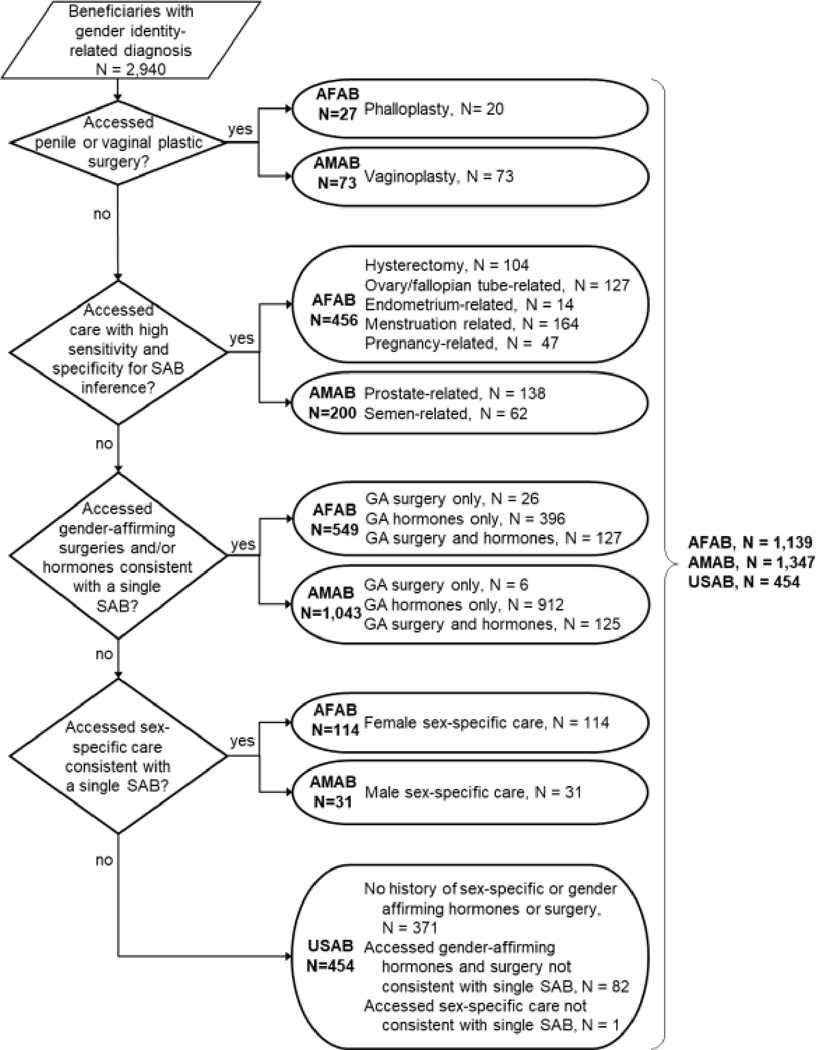
The primary independent variable was change in gender on record. This was operationalized per the “2-step”‖ method, which distinguishes self-reported gender from SAB.14,16 This study developed a hierarchical deterministic approach for inferring SAB based on consultations with Oregon Health & Science University’s Transgender Health Program. Diagnosis, procedure, and drug codes were obtained from published literature24,26,29,35,36; clinical research teams affiliated with Oregon Health & Science University’s Transgender Health Program; and a systematic hand-search of ICD-9/10, Current Procedural Terminology, and National Drug Code lists. Appendix Tables 1‒3 provide all codes included in this algorithm. All codes were reviewed by clinical experts to validate their sensitivity in inferring SAB. Individuals were classified as AFAB, AMAB, or unknown SAB (USAB) in 4 mutually exclusive hierarchical steps (Figure 1). Self-reported gender was obtained from enrollment records. During the study period, Medicaid beneficiaries could only self-report female or male gender, although reporting was optional and did not affect eligibility for services. This yielded 6 potential combinations of the 3 SAB values and 2 gender values. Change in gender on record was characterized as the existence of self-reported gender at initial Medicaid enrollment that differed from SAB (e.g., AFAB and male self-reported gender).
Figure 1.
Methodology for hierarchical sex assigned at birth inference.
AFAB, assigned female sex at birth; AMAB, assigned male sex at birth; SAB, sex assigned at birth; USAB, unknown sex assigned at birth.
Additional characteristics of interest included age at first gender identity–related diagnosis, race and ethnicity, residence in the Portland metropolitan region, and cumulative Medicaid enrollment in years. These variables are associated with health-seeking behaviors and access to culturally competent providers.37
The outcome of interest was the predicted probability of mental (anxiety disorders, depressive disorders, suicidal ideation, and post-traumatic stress disorder) and behavioral health conditions (alcohol use, substance use, and tobacco use disorders). These outcomes were selected based on prior literature suggesting the presence of gender identity–based differences in prevalence.2,5,38 History of ever having these conditions during the study period was identified using Centers for Medicare and Medicaid Services Chronic Conditions Warehouse algorithms, with the exception of suicidal ideation, which used a definition from the Centers for Disease Control and Prevention.39,40
Statistical Analysis
The annual proportion of AFAB, AMAB, and USAB TGN beneficiaries in Oregon’s Medicaid program was descriptively analyzed. Change in gender on record was descriptively analyzed by comparing self-reported gender to SAB. The sample’s demographics were descriptively analyzed by SAB and gender combinations.
Separate multivariable logistic regression models were conducted to understand how change in gender on record for AMAB or AFAB individuals was associated with each of the 7 mental and behavioral health conditions. Models used individual-level data from the full sample, but the primary results report only those with AMAB or AFAB, as change in gender on record for those with USAB could not be established. Models adjusted for age, race, ethnicity, residence in the Portland metropolitan area, and years of enrollment. Post-estimation predicted probabilities were reported to aid interpretation (R “margins”‖ package); pairwise comparisons were computed to assess effect modification (R “emmeans”‖ package).
Two sensitivity analyses were conducted for these models. First, the definition of change in gender on record was modified to capture changes in self-reported gender at any time during the study period, rather than at initial enrollment only. Although this modified definition reflects beneficiaries’ actual practices, the change may not have preceded the diagnoses of interest. Second, a previously published method of assembling a TGN sample26 was applied to the administrative data to enable comparability with prior published work. This extant method uses gender identity–related diagnosis codes or a workaround diagnosis of “endocrine disorder not otherwise specified”‖—which may be used for TGN individuals avoiding a gender identity– related diagnosis—in conjunction with gender-affirming hormone and surgery receipt to infer SAB.26,41 As in the primary model, the change in gender on record variable was constructed using SAB and gender at initial enrollment.
All analyses were conducted in February 2021 using R, version 4.0.3. This study was approved by the Oregon Health & Science University IRB.
RESULTS
A total of 2,940 adult beneficiaries received ≥1 gender identity-related diagnosis and were included in the TGN sample; 92.1% could be confirmed as TGN using a method developed by the Centers for Medicare and Medicaid Services.29 The present study’s method for inferring SAB yielded 1,139 AFAB (38.7%), 1,347 AMAB (45.8%), and 454 USAB (15.4%) individuals (Figure 1).
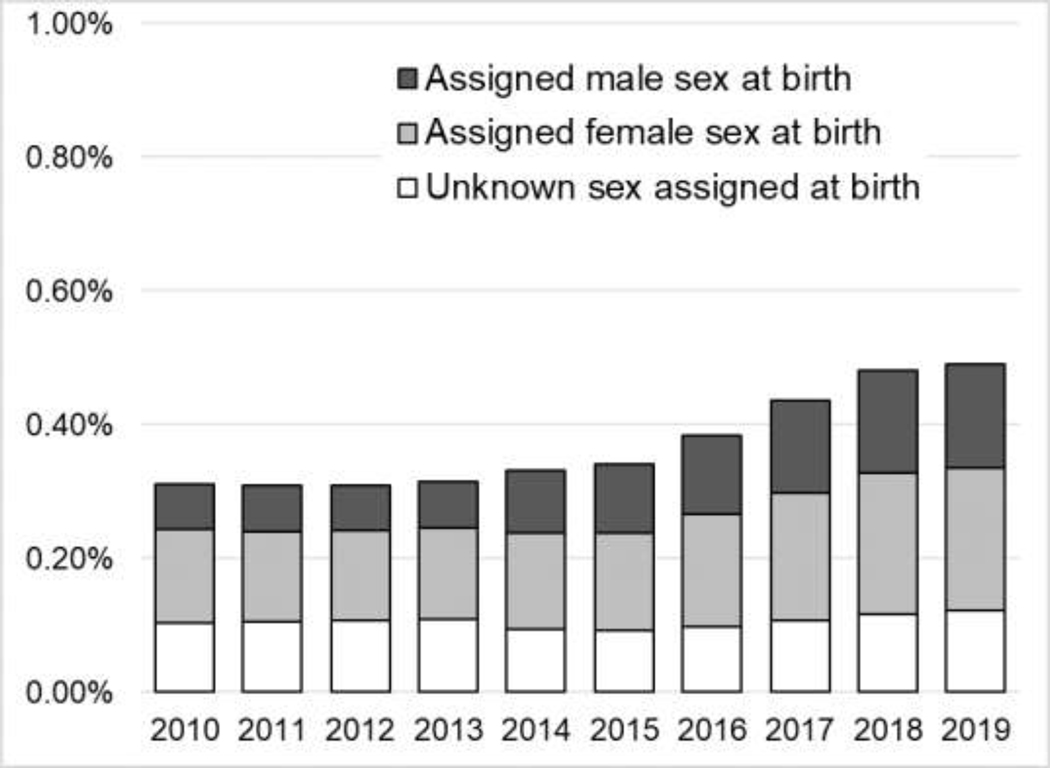
The annual proportion of Medicaid beneficiaries identified as TGN remained stable at 0.31% from 2010 to 2013, then increased steadily to 0.49% in 2019 (Figure 2). The annual proportion of USAB stayed between 0.09% and 0.12%, but AFAB increased from 0.14% to 0.21% and AMAB increased from 0.07% to 0.16% over the study period.
Figure 2.
Annual proportion of Oregon Medicaid transgender and nonbinary beneficiaries, by sex assigned at birth.
Of the 1,451 TGN individuals who self-reported female gender at initial enrollment, 449 (30.9%) were AMAB who were classified as changing their gender on record, while 836 (57.6%) were AFAB. Of the 1,489 who self-reported male gender, 303 (20.3%) were AFAB classified as changing their gender on record, while 898 (60.3%) were AMAB.
The majority of the sample received their first gender identity–related diagnosis between ages 26 and 35 years, were non-Hispanic White, and resided in the Portland metropolitan area (Table 1). Among AFAB, median cumulative enrollment was equivalent between those with male or female gender (4.0 vs 4.0 years), whereas among AMAB, those with female gender had slightly lower median enrollment than those with male gender (2.6 vs 3.0 years, respectively). Appendix Table 4 provides USAB descriptive characteristics.
Table 1.
Characteristics of the 2010‒2019 Oregon Medicaid Transgender and Nonbinary Sample, by Sex Assigned at Birth and Gender
| Characteristic | Assigned female sex at birth | Assigned male sex at birth | ||
|---|---|---|---|---|
|
| ||||
| Female gender (N=836) | Male gender (N=303) | Male gender (N=898) | Female gender (N=449) | |
| Age, years | ||||
| 18‒25 | 105 (12.6) | 28 (9.2) | 86 (9.6) | 38 (8.5) |
| 26‒35 | 546 (65.3) | 187 (61.7) | 502 (55.9) | 251 (55.9) |
| 36‒45 | 129 (15.4) | 50 (16.5) | 169 (18.8) | 86 (19.2) |
| 46‒55 | 37 (4.4) | 27 (8.9) | 94 (10.5) | 52 (11.6) |
| 55‒64 | 19 (2.3) | 11 (3.6) | 47 (5.2) | 22 (4.9) |
| Race/ethnicity | ||||
| Non-Hispanic White | 575 (68.8) | 176 (58.1) | 614 (68.4) | 254 (56.6) |
| Hispanic | 61 (7.3) | 31 (10.2) | 55 (6.1) | 28 (6.2) |
| Other | 51 (6.1) | 15 (5.0) | 52 (5.7) | 24 (5.3) |
| Unknown | 149 (17.8) | 81 (26.7) | 177 (19.7) | 143 (31.8) |
| Residence in Portland metro | 521 (62.3) | 205 (67.7) | 540 (60.1) | 327 (72.8) |
| Years enrollment | 4.00 (2.42–5.92) | 4.00 (2.42–5.92) | 3.00 (1.50–4.46) | 2.58 (1.42–4.75) |
Notes: Age represents age at first gender identity-related diagnosis. Other race/ethnicity includes Black, Asian, and Alaskan Native/American Indian populations. Years of enrollment is reported as median (IQR), while all other values are N (%).
After adjustment for demographic and insurance characteristics, SAB appeared to significantly and meaningfully modify the association between change in gender on record and the predicted probability of mental, but not behavioral, health conditions (Table 2). For all mental health outcomes, AFAB with self-reported female gender had the highest predicted probability followed by AMAB with self-reported male gender, whereas those who changed their gender on record had similar estimates regardless of SAB. For example, the predicted probability of anxiety disorders among AFAB was 73.2% (95% CI=71.82%, 75.52%) among those who did not change their gender on record and 50.09% (95% CI=45.32%, 54.86%) among those who did, whereas among AMAB it was 58.50% (95% CI=55.86%, 61.08%) and 47.68% (95% CI=43.56%, 51.83%). For all behavioral health outcomes, those without changes in gender on record had significantly and meaningfully higher predicted probabilities than those with, and estimates were similar across SAB groups. For example, the predicted probability of substance use disorders among AMAB was 5.70% (95% CI=4.38%, 7.38%) among those who changed their gender on record to female compared with 11.90% (95% CI=10.39%, 13.59%) among those with male on their record (Appendix Table 5 shows USAB model results).
Table 2.
Predicted Probability of Mental/Behavioral Conditions in Transgender and Nonbinary Oregon Medicaid Beneficiaries, by Gender Identity
| Outcomes | Total adult sample (N=2,940) | Assigned female sex at birth | Assigned male sex at birth | ||
|---|---|---|---|---|---|
| Female gender (N=836) | Male gender (N=303) | Male gender (N=898) | Female gender (N=449) | ||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Anxiety disorders | 58.09 (56.10, 60.06) | 73.72 (71.82, 75.52) | 50.09 (45.32, 54.86) | 58.50 (55.86, 61.08) | 47.68 (43.56, 51.83) |
| Depressive disorders | 67.40 (65.47, 69.29) | 78.10 (76.33, 79.78) | 54.15 (49.36, 58.87) | 69.69 (67.21, 72.07) | 59.15 (54.98, 63.20) |
| Suicidal ideation | 11.55 (10.26, 12.98) | 25.06 (23.29, 26.91) | 9.31 (7.10, 12.11) | 20.43 (18.44, 22.57) | 14.51 (12.00, 17.44) |
| Posttraumatic stress disorder | 26.16 (24.36, 28.03) | 38.17 (36.05, 40.33) | 15.97 (13.18, 19.21) | 22.38 (20.31, 24.59) | 18.45 (15.76, 21.48) |
| Alcohol use disorders | 6.54 (5.59, 7.64) | 6.18 (5.25, 7.26) | 2.42 (1.58, 3.68) | 5.22 (4.28, 6.35) | 2.65 (1.86, 3.75) |
| Substance use disorders | 12.14 (10.87, 13.53) | 12.39 (11.06, 13.85) | 4.46 (3.17, 6.22) | 11.90 (10.39, 13.59) | 5.70 (4.38, 7.38) |
| Tobacco use disorders | 14.44 (12.72, 16.34) | 15.31 (13.72, 17.04) | 6.09 (4.69, 7.87) | 13.83 (12.15, 15.71) | 5.28 (4.15, 6.71) |
Notes: Models adjusted for race and ethnicity, residence in Portland metro, age, and years enrolled. Age was calculated as age at time of first diagnosis of the condition, or age at the study midpoint (June 30, 2014) for those without the condition. Years of enrollment was calculated as time from enrollment to first diagnosis of the condition, or as total years of enrollment among those without the condition. Total adult sample includes unknown sex assigned at birth.
In secondary analyses, modifying the definition of change in gender on record to capture change at any time during the study period resulted in 16% more AFAB and 21% more AMAB classified as having a change in gender on record. The magnitude of and patterns in predicted probability of mental and behavioral health conditions using the modified definition were consistent with the primary analysis (Appendix Table 6). Application of a published algorithm to identify TGN beneficiaries in administrative data26 yielded a similarly-sized sample, but higher USAB proportion (56.4%) due to differences in SAB inference. Nevertheless, agreement between SAB inferred in the primary analysis and using the published algorithm was high. Model results were less precise, but demonstrated patterns consistent with the primary analysis (Appendix Figure 1 and Appendix Tables 7–8).
DISCUSSION
Changing gender on administrative records contributes to affirmation and resilience in TGN populations.9,10 This study focused on Oregon, which was an early adopter of state Medicaid coverage for gender-affirming care in 2015. This policy landscape, coupled with the individual-level detail in this study’s administrative data, enabled identification of a large sample of care-seeking TGN beneficiaries and assessment of changes in gender on record. This study complements existing electronic medical records–based and claims-based methods that infer SAB, and implements a deterministic 2-step process for distinguishing SAB and gender.14,16,20,22,26,33 Similar to previous research, 18.7% of this study’s sample changed their gender on record at least once, making it an unreliable substitute for SAB.20 The estimated proportion of TGN beneficiaries in Oregon Medicaid (0.49%) was consistent with U.S. population estimates from a published meta-regression of national surveys (0.39%, 95% CI=0.16%, 0.62%).42 Application of the workaround diagnosis of “endocrine disorder not otherwise specified”‖ used by a previously published algorithm26 identified an additional 67 (2%) TGN beneficiaries for this study’s sensitivity analysis. The rarity of the workaround code in this study’s data is likely due to reimbursement restrictions, as Oregon Medicaid only covers care for an authorized list of diagnoses. However, it may have greater utility in commercial and Medicare settings.
The primary analysis found beneficiaries who changed their gender on record had significantly and meaningfully lower predicted probability of all outcomes, and the association with mental health conditions did appear to be modified by SAB. AFAB who self-reported female gender had higher predicted probability of anxiety disorders, depressive disorders, and suicidal ideation than AMAB reporting male gender, whereas TGN beneficiaries who changed their gender on record had similar and lower predicted probability of all outcomes regardless of SAB. This was consistent with previous literature demonstrating changes in gender on at least some documentation was associated with more favorable mental health.10,11 Additionally, findings of higher prevalence of mental health conditions and substance use in AFAB compared with AMAB were consistent with previous population-based research.2,5
The intention of this study was not to reinforce a binarized gender identity, but rather, to implement a person-centered characterization of separate gender and SAB constructs to the degree possible within the bounds of administrative claims. Indeed, an estimated 20%–30% of TGN individuals identify as nonbinary, and an estimated 88% of nonbinary individuals report their identity documents do not reflect their preferred gender because the available gender options do not fit their gender identity.2–4
Limitations
This study has several important limitations. First, it uses gender identity–related diagnosis codes to assemble a TGN sample. Some TGN individuals perceive these diagnoses as stigmatizing and will avoid them, whereas others do not experience the diagnoses’ pathology.43 Health systems–based sampling methods that also utilized patient narratives and workaround diagnoses such as “endocrine disorder not otherwise specified”‖ to identify TGN individuals without gender identity–related diagnoses increased sample sizes by a modest 0.05%–14.9%.26,33 By contrast, all studies that assessed the specificity of gender identity diagnosis–based methods found acceptably low false positive rates of 3%–11%.20,22,29,33 Second, this study cannot observe care paid by private insurance or out-of-pocket expenditures, which could result in some SAB misclassification. However, the likelihood of unobserved care is low in this Medicaid-insured, low-income population.44,45 Third, only binary gender could be reported during Oregon Medicaid enrollment. Thus, even after applying the 2-step method, the study cannot truly characterize the diversity of gender identities, such as nonbinary identity. Fourth, the cross-sectional design did not permit causal inference. Although the sensitivity analysis identified a subset of beneficiaries who changed their gender on record after their initial enrollment, there were insufficient observations and power to conduct within-subject longitudinal analyses that may have enabled causal inference. Furthermore, the study design and data could not assess the impact of potential confounders such change in gender on other identity documents, extent of social and medical transition, and appropriateness of available gender options.3 Despite these limitations, the findings were highly consistent with previous studies.
CONCLUSIONS
This study developed a method to differentiate SAB and gender using Oregon Medicaid administrative claims, and demonstrated that SAB modifies the relationship between change in gender on record and mental, but not behavioral, health. Future research can validate SAB inference using sources such as birth certificates, examine the differential effects of sex and gender on other risk factors, and utilize longitudinal methods that examine how changing gender on record at an individual level causally affects health outcomes.
Supplementary Material
ACKNOWLEDGMENTS
We thank community members and providers participating in Oregon Health & Science University’s Transgender Health Program for their thoughtful and detailed feedback on our algorithm for inferring sex assigned at birth. We also thank Ellena Rosenthal for their assistance in identifying and compiling diagnosis and procedure codes for this algorithm.
Research reported in this publication was supported by National Institute on Minority Health and Health Disparities (3R01MD011212-0S31 [Administrative Supplement to 1R01MD011212], Principal Investigator: McConnell) and Downing’s time was supported by the National Institute of Drug Abuse (1K01DA050775-01A1, Principal Investigator: Downing). The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
No financial disclosures were reported by the authors of this paper.
Footnotes
CRediT author statement
Kimberly Yee: Conceptualization, Methodology, Software, Validation, Formal analysis, Investigation, Resources, Data Curation, Writing – Original Draft, Writing – Review & Editing, Visualization, Funding acquisition.
Bonnie K. Lind: Methodology, Formal analysis, Writing – Review & Editing, Visualization, Supervision.
Jae Downing: Conceptualization, Methodology, Data Curation, Writing – Review & Editing, Visualization, Funding acquisition.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Becerra-Culqui TA, Liu Y, Nash R, et al. Mental health of transgender and gender nonconforming youth compared with their peers. Pediatrics. 2018;141(5):e20173845. 10.1542/peds.2017-3845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Downing JM, Przedworski JM. Health of transgender adults in the U.S., 2014‒2016. Am J Prev Med. 2018;55(3):336–344. 10.1016/j.amepre.2018.04.045. [DOI] [PubMed] [Google Scholar]
- 3.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 U.S. Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016. https://www.transequality.org/sites/default/files/docs/usts/USTS-Full-Report-Dec17.pdf. Accessed November 8, 2021. [Google Scholar]
- 4.Streed CG Jr., McCarthy EP, Haas JS. Self-reported physical and mental health of gender nonconforming transgender adults in the United States. LGBT Health. 2018;5(7):443–448. 10.1089/lgbt.2017.0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cicero EC, Reisner SL, Merwin EI, Humphreys JC, Silva SG. The health status of transgender and gender nonbinary adults in the United States. PLoS One. 2020;15(2):e0228765. 10.1371/journal.pone.0228765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11‒12):675–689. 10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Transgender Equality. ID Documents Center. https://transequality.org/documents. Accessed October 29, 2021.
- 8.Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, Nemoto T. The role of gender affirmation in psychological well-being among transgender women. Psychol Sex Orientat Gend Divers. 2016;3(3):336–344. 10.1037/sgd0000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughto JMW, Gunn HA, Rood BA, Pantalone DW. Social and medical gender affirmation experiences are inversely associated with mental health problems in a U.S. non-probability sample of transgender adults. Arch Sex Behav. 2020;49(7):2635–2647. 10.1007/s10508-020-01655-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Restar A, Jin H, Breslow A, et al. Legal gender marker and name change is associated with lower negative emotional response to gender-based mistreatment and improve mental health outcomes among trans populations. SSM Popul Health. 2020;11:100595. 10.1016/j.ssmph.2020.100595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scheim AI, Perez-Brumer AG, Bauer GR. Gender-concordant identity documents and mental health among transgender adults in the USA: a cross-sectional study. Lancet Public Health. 2020;5(4):e196–e203. 10.1016/S2468-2667(20)30032-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oregon Health Authority. Oregon Health Plan: Application Guide. https://sharedsystems.dhsoha.state.or.us/DHSforms/Served/he9025.pdf. Accessed October 29, 2021.
- 13.Washington State Health Care Authority. Transhealth program. https://www.hca.wa.gov/health-care-services-and-supports/apple-health-medicaid-coverage/transhealth-program#to-change-your-gender-marker. Accessed October 29, 2021.
- 14.Reisner SL, Deutsch MB, Bhasin S, et al. Advancing methods for US transgender health research. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):198–207. 10.1097/med.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Restar A, Jin H, Operario D. Gender-inclusive and gender-specific approaches in trans health research. Transgend Health. 2021;6(5):235–239. 10.1089/trgh.2020.0054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deutsch MB, Green J, Keatley J, et al. Electronic medical records and the transgender patient: recommendations from the World Professional Association for Transgender Health EMR Working Group. J Am Med Inform Assoc. 2013;20(4):700–703. 10.1136/amiajnl-2012-001472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puckett JA, Brown NC, Dunn T, Mustanski B, Newcomb ME. Perspectives from transgender and gender diverse people on how to ask about gender. LGBT Health. 2020;7(6):305–311. 10.1089/lgbt.2019.0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Suen LW, Lunn MR, Katuzny K, et al. What sexual and gender minority people want researchers to know about sexual orientation and gender identity questions: a qualitative study. Arch Sex Behav. 2020;49(7):2301–2318. 10.1007/s10508-020-01810-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abramovich A, de Oliveira C, Kiran T, Iwajomo T, Ross LE, Kurdyak P. Assessment of health conditions and health service use among transgender patients in Canada. JAMA Netw Open. 2020;3(8):e2015036. 10.1001/jamanetworkopen.2020.15036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ehrenfeld JM, Gottlieb KG, Beach LB, Monahan SE, Fabbri D. Development of a natural language processing algorithm to identify and evaluate transgender patients in electronic health record systems. Ethn Dis. 2019;29(suppl 2):441–450. 10.18865/ed.29.s2.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quinn VP, Nash R, Hunkeler E, et al. Cohort profile: Study of Transition, Outcomes and Gender (STRONG) to assess health status of transgender people. BMJ Open. 2017;7(12):e018121. 10.1136/bmjopen-2017-018121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roblin D, Barzilay J, Tolsma D, et al. A novel method for estimating transgender status using electronic medical records. Ann Epidemiol. 2016;26(3):198–203. 10.1016/j.annepidem.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubin S, Cook T, Liss A, et al. Comparing electronic health record domains’ utility to identify transgender patients. Transgend Health. In press. Online November 25, 2020. 10.1089/trgh.2020.0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;153(7):609–616. 10.1001/jamasurg.2017.6231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dragon CN, Guerino P, Ewald E, Laffan AM. Transgender Medicare beneficiaries and chronic conditions: exploring fee-for-service claims data. LGBT Health. 2017;4(6):404–411. 10.1089/lgbt.2016.0208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jasuja GK, de Groot A, Quinn EK, et al. Beyond gender identity disorder diagnoses codes: an examination of additional methods to identify transgender individuals in administrative databases. Med Care. 2020;58(10):903–911. 10.1097/mlr.0000000000001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDowell A, Progovac AM, Cook BL, Rose S. Estimating the health status of privately insured gender minority children and adults. LGBT Health. 2019;6(6):289–296. 10.1089/lgbt.2018.0238. [DOI] [PubMed] [Google Scholar]
- 28.Nocka K, Montgomery MC, Progovac A, Guss CE, Chan PA, Raifman J. Primary care for transgender adolescents and young adults in Rhode Island: an analysis of the all payers claims database. J Adolesc Health. 2021;68(3):472–479. 10.1016/j.jadohealth.2020.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Proctor K, Haffer SC, Ewald E, Hodge C, James CV. Identifying the transgender population in the Medicare program. Transgend Health. 2016;1(1):250–265. 10.1089/trgh.2016.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Progovac AM, Cook BL, Mullin BO, et al. Identifying gender minority patients’ health and health care needs in administrative claims data. Health Aff (Millwood). 2018;37(3):413–420. 10.1377/hlthaff.2017.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gavrielov-Yusim N, Friger M. Use of administrative medical databases in population-based research. J Epidemiol Community Health. 2014;68(3):283–287. 10.1136/jech-2013-202744. [DOI] [PubMed] [Google Scholar]
- 32.Gross K, Brenner JC, Truchil A, Post EM, Riley AH. Building a citywide, all-payer, hospital claims database to improve health care delivery in a low-income, urban community. Popul Health Manag. 2013;16(suppl 1):S20–S25. 10.1089/pop.2013.0037. [DOI] [PubMed] [Google Scholar]
- 33.Blosnich JR, Cashy J, Gordon AJ, et al. Using clinician text notes in electronic medical record data to validate transgender-related diagnosis codes. J Am Med Inform Assoc. 2018;25(7):905–908. 10.1093/jamia/ocy022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kauth MR, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care for transgender veterans in the Veterans Health Administration: 2006‒2013. Am J Public Health. 2014;104(suppl 4):S532–S534. 10.2105/ajph.2014.302086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lane M, Ives GC, Sluiter EC, et al. Trends in gender-affirming surgery in insured patients in the United States. Plast Reconstr Surg Glob Open. 2018;6(4):e1738. 10.1097/gox.0000000000001738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Solotke MT, Liu P, Dhruva SS, Gulanski B, Shah ND, Ross JS. Medicare prescription drug plan coverage of hormone therapies used by transgender individuals. LGBT Health. 2020;7(3):137–145. 10.1089/lgbt.2019.0306. [DOI] [PubMed] [Google Scholar]
- 37.Garcia J, Crosby RA. Social determinants of discrimination and access to health care among transgender women in Oregon. Transgend Health. 2020;5(4):225–233. 10.1089/trgh.2019.0090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Meyer IH, Brown TN, Herman JL, Reisner SL, Bockting WO. Demographic characteristics and health status of transgender adults in select US regions: Behavioral Risk Factor Surveillance System, 2014. Am J Public Health. 2017;107(4):582–589. 10.2105/ajph.2016.303648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Medicare & Medicaid Services. Chronic Conditions Data Warehouse. https://www2.ccwdata.org/web/guest/condition-categories. Accessed October 29, 2021.
- 40.Hedegaard HSM, Claassen C, Crosby A, Holland K,. Issues in developing a surveillance case definition for nonfatal suicide attempt and intentional self-harm using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) coded data. Natl Health Stat Report. 2018;(108):1–19. [PubMed] [Google Scholar]
- 41.Wolfe HL, Reisman JI, Yoon S, et al. Validating data-driven methods to identify transgender individuals in the Veterans Affairs. Am J Epidemiol. 2021;190(9):1928–1934. 10.1093/aje/kwab102. [DOI] [PubMed] [Google Scholar]
- 42.Meerwijk EL, Sevelius JM. Transgender population size in the United States: a meta-regression of population-based probability samples. Am J Public Health. 2017;107(2):e1–e8. 10.2105/ajph.2016.303578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review. Transgend Health. 2018;3(1):159–169. 10.1089/trgh.2018.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abramowitz J. The effect of ACA state Medicaid expansions on medical out-of-pocket expenditures. Med Care Res Rev. 2020;77(1):19–33. 10.1177/1077558718768895. [DOI] [PubMed] [Google Scholar]
- 45.Gotanda H, Jha AK, Kominski GF, Tsugawa Y. Out-of-pocket spending and financial burden among low income adults after Medicaid expansions in the United States: quasi-experimental difference-in-difference study. BMJ. 2020;368:m40. 10.1136/bmj.m40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.